Abstract
Few large epidemiological studies have evaluated the association between dietary advanced glycation end products (AGEs) and cancer risk. We evaluated the relationship between dietary AGE intake and the incidence of total cancer and site‐specific cancers in a population‐based prospective study in Japan. Participants were 14,173 men and 16,549 women who were 35 years of age or older in 1992. Dietary intake was assessed via a validated food frequency questionnaire. Intake of the AGE N ε‐carboxymethyl‐lysine (CML) was estimated using databases of CML content in foods determined using ultraperformance liquid chromatography–tandem mass spectrometry. Cancer incidence was confirmed through regional population‐based cancer registries. During a mean follow‐up period of 13.3 years, 1954 men and 1477 women developed cancer. We did not observe a significant association between CML intake and the risk of total cancer in men or women. In men, compared with the lowest quartile of CML intake, the hazard ratios of liver cancer for the second, third, and highest quartiles were 1.69 (95% CI: 0.92–3.10), 1.48 (95% CI: 0.77–2.84), and 2.10 (95% CI: 1.10–3.98; trend p = 0.04). Conversely, a decreased relative risk of male stomach cancer was observed for the second and highest quartiles of CML intake versus the lowest quartile, with hazard ratios of 0.73 and 0.67, respectively (trend p = 0.08). Our finding on the potential harmfulness of consuming AGEs on liver cancer risk is intriguing and warrants further study.
Keywords: AGEs, cancer, cohort studies, diet, epidemiology
A high intake of advanced glycation end products Nε‐carboxymethyl‐lysine was associated with an increased risk of liver cancer in Japanese men. Our finding suggests the potential harmfulness of consuming advanced glycation end products on liver cancer risk.
Abbreviations
- AGEs
advanced glycation end products
- CI
confidence intervals
- CML
N ε‐carboxymethyl‐lysine
- FFQ
food frequency questionnaire
- HMGB1
high mobility group box protein‐1
- MET
metabolic equivalent task
- RAGE
receptor for advanced glycation end products
- sRAGE
soluble receptor for advanced glycation end products
- UPLC–MS/MS
ultraperformance liquid chromatography–tandem mass spectrometry.
1. INTRODUCTION
Advanced glycation end products are complex compounds formed by the nonenzymatic glycation between reducing sugars and free amino groups of proteins or lipids, termed the Maillard reaction. AGEs are produced and then accumulate endogenously in the body during the aging process or via glucose metabolism. 1 Other sources are exogenous AGEs derived from foods. The formation of dietary AGEs is accelerated by food preparation and processing steps that use a high temperature for a long period of time, including grilling, roasting, frying, and baking. 2 , 3 High AGE levels are common in highly processed foods such as bread, biscuits, cooked meats, and foods containing high sugar levels. Of dietary AGEs consumed, 10%–30% are absorbed intestinally and enter the circulation. 4 The ingestion of foods with high AGE content can increase the blood and tissue concentrations of AGEs, and exogenous AGE levels are usually much higher than those of endogenously produced AGEs, 5 although the association between dietary intake and circulating levels of AGEs has shown conflicting results in human studies. 6 , 7
AGEs have been associated with metabolic diseases such as diabetes and atherosclerosis as well as aging. 1 , 5 AGEs and their receptor (RAGE) are implicated in oxidative stress and inflammation. 1 , 5 Although the role of AGEs in cancer is unknown, oxidative stress related to AGEs may have critical consequences to cancer‐associated DNA damage. 8 The presence of AGEs in human tumors and higher circulating AGE levels among cancer patients have been demonstrated. 9 , 10 AGEs promoted proliferation, migration, and invasion of cancer cell lines. 11 , 12 Therefore, dietary AGEs, a major source of exogenous AGEs, may be associated with the development of cancer.
N ε‐carboxymethyl‐lysine has been the product most commonly used to estimate dietary AGEs, because CML is thought to be one of the most abundant AGEs in the body and has a well characterized chemical structure. To date, five prospective studies have evaluated the association between dietary AGEs and cancer risk. The NIH‐AARP Diet and Health Study showed that CML intake was positively associated with the risk of pancreatic cancer in men 13 ; it also reported a positive association between CML intake and postmenopausal breast cancer. 14 Another US‐based study, the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial, reported that higher CML intake was associated with an increased risk of breast cancer. 15 These studies estimated the CML content of foods using a database based on an ELISA. However, the accuracy and reliability of the contents based on this technique are reported to be questionable. CML values have been shown to be overestimated with ELISA for high‐fat products such as butter, olive oil, and mayonnaise and underestimated for carbohydrate‐rich foods such as cereals, biscuits, and cookies compared with a more accurate technique, namely UPLC–MS/MS. 16 , 17 By contrast, the European Prospective Investigation into Cancer and Nutrition (EPIC) study estimated dietary CML and other two AGEs, N ε‐(1‐carboxyethyl)‐lysine and N δ‐(5‐hydro‐5‐methyl‐4‐imidazolon‐2‐yl)‐ornithine, using databases based on UPLC–MS/MS. They observed that dietary CML was inversely associated with the risks of colorectal cancer and hepatocellular carcinoma, and positively associated with gallbladder cancer. 18 , 19
Based on previous conflicting results, we evaluated the associations between dietary CML intake using databases based on UPLC–MS/MS and the incidence of total and site‐specific cancers in a population‐based prospective study in Japan. This cohort study is the first on dietary AGEs and cancer in Asians, whose dietary habits differ from those in the West.
2. MATERIALS AND METHODS
2.1. Participants and design
This study utilized data from the Takayama study in Japan, the details of which have been described previously. 20 The cohort has been followed to study the associations between lifestyle factors and mortality or cancer incidence. The subjects were 36,990 residents who were 35 years of age or older and were not hospitalized in September 1992. In total, 31,552 residents (85.3%) participated in the study and completed a self‐administered questionnaire including an FFQ. 20 The questionnaire included demographic characteristics, medical history, physical activity, smoking status, and reproductive factors. This study was approved by the institutional review board of the Gifu University Graduate School of Medicine (26–277).
2.2. Dietary AGE intake and other exposure variables
The FFQ comprises questions on the consumption frequency of foods and dishes (169 items) and the usual portion size of meals during the previous year. 21 The missing data for FFQ were assigned the mode categories by sex and 10‐year age group. The intake of each nutrient and food group was estimated with this information using the Japanese Standard Table of Food Composition, 5th revised and enlarged edition. 22 To quantify the intake of dietary AGEs, we estimated dietary CML intake using databases based on UPLC–MS/MS. The details of CML intake estimation have been described elsewhere. 23 Briefly, we used a public repository at the University of Dresden based on UPLC–MS/MS. 24 A great contribution to this repository came from measurements made by Hull et al. 25 We also used another database of CML levels in foods by Scheijen et al., measured using UPLC–MS/MS. 26 CML values were assigned to each food with different cooking methods. Some CML contents varied between both databases even for the same foods with the same cooking methods. The databases of Scheijen et al. and Hull et al. contained CML values for 34.9% and 24.2% of the cumulative number of foods in our FFQ, respectively. So, the database of Scheijen et al. were given priority. Because the values of Hull et al. were an average of 21% higher than those of Scheijen et al. for the foods included in our FFQ, the values from Hull et al. were divided by 1.21. The CML values for powdered milk and almonds were derived from Drusch et al. and Zhang et al., respectively (0.2% of the cumulative number of foods). 27 , 28 When a CML value was not available for a food with a certain preparation method, we used values for similar foods according to the cooking methods. These assignments covered 56.3% of the cumulative number of foods, and these foods accounted for 79.3% and 82.1% of total energy in men and women, respectively. As for the values still missing by UPLC–MS/MS, we referred to the database based on ELISA by Uribarri et al., 2 except for meat products and starchy foods. By comparing the values measured by Uribarri et al. with those of Scheijen et al. and Hull et al., conversion factors were calculated according to food group. After these processes, we assigned CML values to 61.3% of the cumulative number of foods, and these foods accounted for 82.7% and 86.1% of total energy in men and women, respectively. Finally, we assigned median CML values according to food group and cooking method for the remaining foods. In our FFQ, the food items with the highest CML values per weight were roasted peanuts, biscuits, cakes, and so on. Pork steak, hamburg steak, and fried rice had the highest CML values per serving. Fresh fruits and vegetables and alcohol beverages had almost zero CML values.
Smokers were defined as people who had smoked a total of at least 20 packs of cigarettes throughout their lifetime. The number of years of smoking was determined for ever smokers. Physical activity was assessed by asking the participants how much time on average they spent on various intensities of physical activities during the previous year. The period spent on each intensity‐level activity (h/week) was multiplied by the corresponding energy expenditure, expressed as a MET, and the sum score of the product was regarded as the physical activity score (METs h/week). The details of the physical activity assessment including validity are described elsewhere. 29
2.3. Outcomes and follow‐up
After we excluded 830 people who were diagnosed with any cancer before baseline and/or reported a positive history of cancer in the baseline questionnaire, 14,173 men and 16,549 women aged 35–101 years were included in the analysis. Data on death and emigration were obtained from residential registers or family registers. Cause of death was identified from death certificates provided by the Legal Affairs Bureau. The incidence of cancer was confirmed mainly through two regional population‐based cancer registries in Gifu. The causes of cancer were coded according to the International Classification of Diseases and Health Related Problems, 10th Revision. Cancer was defined as code C00‐C97. Follow‐up was conducted until the date of cancer diagnosis, date of death, date of moving out of the study area, or the end of March 2008, whichever came first. During the mean follow‐up period of 13.3 years, 1954 men and 1477 women developed cancer. The mortality‐to‐incidence ratio was 0.49, and 23.1% of patients were ascertained by death certificate‐only registration. For such cases, a backward tracking review of the incidence date was conducted based on the description given in the death certificate. As a result, only 7.7% of patients had an unknown incidence date before the date of death, indicating satisfactory completeness of cancer registration in this cohort. During the study period, 1535 persons (5.0%) moved out of the study area. Among 238 participants whose date of emigration was unknown (0.8%), their last date of residence in the study area was assigned as their censored date.
We further investigated the association between the intake of dietary AGEs and the incidence of site‐specific cancers that had 40 or more cases each for men and women so that there would be 10 cases or more in each intake group; cancers of the esophagus (C15), stomach (C16), colon (C18), rectum (C19–20), liver (C22), gallbladder and biliary duct (C23–24), pancreas (C25), lung (C33–C34), bladder (C67), and prostate (C61) for men and cancers of the stomach, colon, rectum, liver, gallbladder and biliary duct, pancreas, lung, breast (C50), cervix (C53), endometrium (C54), and ovary (C56) for women were taken for analysis. When a person had developed a primary cancer at two or more sites, only the first cancer was applied. Lung cancer was analyzed separately for never and ever smokers.
2.4. Statistical analysis
CML intake was controlled for energy intake by the energy density method (g/1000 kcal of total energy). The study participants were categorized into quartile groups (Q1–Q4) according to their energy‐adjusted CML intake. The characteristics of the participants were calculated as the mean (standard deviation) or the percentage of each category according to the quartile groups of CML intake for each sex.
Hazard ratios and 95% CIs for total and site‐specific cancers were estimated for the quartile groups of CML intake using the Cox proportional hazards model. The reference group was set as the lowest quartile of CML intake. After potential cancer risk factors were identified through a literature review, the confounders included age (years, continuous), body mass index (quartiles), education years (≤8, 9–11, 12–14, ≥15 years), history of diabetes (yes, no), physical activity score (METs h/week, continuous), smoking status (never, former, current smoker who had smoked for 30 years or less, current smoker who had smoked for 31 years or more), alcohol consumption (g/day, continuous), total energy intake (kcal/day, continuous), and menopausal status (premenopausal, postmenopausal). 30 , 31 We additionally adjusted for salt intake (quartiles) for stomach cancer; height (quartiles), aspirin use (yes, no), and total fiber, red meat, and processed meat intake (quartiles) for colon and rectal cancers; coffee consumption (none, from once a month to six times per week, once per day or more) for liver cancer; and height (quartiles), age at menarche (≤12, 13–14, 15–16, ≥17 years), age at first delivery (no, ≤20, 20–25, 26–30, ≥31 years), age at menopause (≤49, ≥50 years), number of children (0, 1, 2, ≥3), and hormone replacement therapy (yes, no) for cancers of the breast, cervix, endometrium, and ovary. Dummy variables were created for missing data for categorical covariates. Tests for a linear trend were performed using the median values of CML intake for each category.
Sensitivity analysis was conducted when the median CML values based on UPLC–MS/MS according to food group and cooking method were assigned to the foods with missing values instead of using the CML values based on ELISA. In addition, the analysis was limited to those who had no history of diabetes because AGEs are closely associated with glucose metabolism. Last, cases who were diagnosed with cancer in the first 2 years were excluded from the analysis because they might have had latent cancers at baseline.
All analyses were performed using SAS version 9.4 (SAS Institute). p‐values were calculated by a two‐sided test. A p‐value of less than 0.05 was considered statistically significant in all analyses.
3. RESULTS
The characteristics of the participants are shown according to the quartile groups of energy‐adjusted CML intake in Tables 1 and 2. Men with higher CML intake were more likely to be older, be more educated, have reported a history of diabetes, be physically less active, have never smoked, have lower alcohol consumption, and have higher total energy, protein, and fat intake. In women, similar associations were observed, except that younger age and greater physical activity were associated with higher CML intake.
TABLE 1.
Characteristics of study participants at baseline (men)
| No. of valid response | Mean (SD) or % | Intake of N ε‐carboxymethyl‐lysine (CML) | ||||
|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |||
| No. of participants | 14,173 | 3544 | 3543 | 3543 | 3543 | |
| Age (years) | 14,173 | 55.1 (12.3) | 53.6 (11.3) | 53.9 (11.8) | 55.5 (12.6) | 57.4 (13.2) |
| Body mass index (kg/m2) | 13,367 | 22.5 (2.8) | 22.5 (2.7) | 22.5 (2.7) | 22.5 (2.9) | 22.5 (2.9) |
| Height (cm) | 13,606 | 164.5 (6.9) | 164.4 (6.8) | 164.8 (6.7) | 164.7 (7.0) | 164.3 (6.9) |
| History of diabetes (yes, %) | 14,173 | 6.3% | 5.0% | 4.6% | 6.1% | 9.5% |
| Education years (%) | 14,006 | |||||
| ≤8 years | 23.0% | 22.1% | 21.5% | 23.8% | 24.4% | |
| 9–11 years | 35.2% | 40.8% | 36.1% | 32.8% | 31.1% | |
| 12–14 years | 30.5% | 29.3% | 32.5% | 30.8% | 29.2% | |
| ≥15 years | 11.4% | 7.7% | 10.0% | 12.6% | 15.4% | |
| Physical activity score (METs h/week) | 14,173 | 27.4 (41.1) | 28.4 (42.2) | 28.8 (42.3) | 27.4 (40.1) | 24.8 (39.4) |
| Smoking status (%) | 13,766 | |||||
| Never | 16.6% | 13.7% | 15.1% | 18.0% | 19.8% | |
| Former | 29.6% | 25.6% | 27.6% | 30.0% | 35.2% | |
| Current (for <30 years) | 31.4% | 35.7% | 34.3% | 30.9% | 24.7% | |
| Current (for ≥30 years) | 22.4% | 25.0% | 23.0% | 21.1% | 20.3% | |
| Alcohol consumption (g/day) | 14,173 | 41.2 (41.2) | 61.0 (50.3) | 44.1 (39.4) | 34.6 (34.5) | 25.1 (28.2) |
| CML intake (mg/day) | 14,173 | 2.74 (1.23) | 1.80 (0.62) | 2.49 (0.79) | 2.98 (1.03) | 3.71 (1.43) |
| Total energy intake (kcal/day) | 14,173 | 2604 (874) | 2421 (721) | 2591 (801) | 2665 (909) | 2739 (1006) |
| Carbohydrate intake (g/day) | 14,173 | 362 (117) | 349 (98) | 369 (111) | 371 (124) | 361 (131) |
| Protein intake (g/day) | 14,173 | 92.9 (37.6) | 72.0 (24.6) | 88.6 (30.1) | 98.6 (36.2) | 112.3 (44.5) |
| Fat intake (g/day) | 14,173 | 60.1 (28.8) | 41.1 (17.1) | 55.8 (21.5) | 65.3 (26.5) | 78.2 (33.7) |
Abbreviations: SD: standard deviation; MET, metabolic equivalent of task; Q1–Q4: the quartile groups of energy‐adjusted CML intake.
TABLE 2.
Characteristics of study participants at baseline (women)
| No. of valid response | Mean (SD) or % | Intake of N ε‐carboxymethyl‐lysine (CML) | ||||
|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |||
| No. of participants | 16,549 | 4138 | 4137 | 4137 | 4137 | |
| Age (years) | 16,549 | 56.3 (13.2) | 57.7 (13.8) | 56.1 (13.3) | 56.0 (12.9) | 55.3 (12.6) |
| Body mass index (kg/m2) | 15,578 | 22.0 (2.9) | 21.9 (3.1) | 22.0 (3.0) | 22.1 (2.9) | 22.0 (2.8) |
| Height (cm) | 15,832 | 151.9 (6.4) | 151.3 (6.7) | 151.8 (6.5) | 152.2 (6.3) | 152.4 (6.1) |
| History of diabetes (yes, %) | 16,549 | 2.9% | 2.1% | 2.5% | 3.7% | 3.5% |
| Menopausal status (pre) | 16,141 | 39.5% | 36.3% | 40.2% | 39.5% | 41.8% |
| Education years (%) | 16,280 | |||||
| ≤8 years | 28.1% | 34.3% | 28.4% | 26.5% | 23.0% | |
| 9–11 years | 39.1% | 41.2% | 39.1% | 38.7% | 37.3% | |
| 12–14 years | 28.3% | 21.9% | 28.3% | 30.3% | 32.8% | |
| ≥15 years | 4.6% | 2.6% | 4.2% | 4.5% | 6.9% | |
| Physical activity score (METs h/week) | 16,549 | 19.0 (29.2) | 16.1 (26.4) | 19.0 (29.2) | 20.1 (30.3) | 20.7 (30.4) |
| Smoking status (%) | 14,801 | |||||
| Never | 82.4% | 77.2% | 82.4% | 85.3% | 84.7% | |
| Former | 4.6% | 5.0% | 4.5% | 3.9% | 5.1% | |
| Current (for <30 years) | 11.1% | 14.9% | 11.2% | 9.5% | 8.7% | |
| Current (for ≥30 years) | 1.9% | 3.0% | 1.9% | 1.3% | 1.5% | |
| Alcohol consumption (g/day) | 16,549 | 7.7 (16.8) | 11.7 (24.8) | 7.9 (15.6) | 6.0 (11.6) | 5.1 (10.2) |
| CML intake (mg/day) | 16,549 | 2.57 (1.18) | 1.73 (0.71) | 2.35 (0.88) | 2.74 (1.00) | 3.48 (1.29) |
| Total energy intake (kcal/day) | 16,549 | 2127 (788) | 1930 (713) | 2090 (772) | 2147 (779) | 2340 (831) |
| Carbohydrate intake (g/day) | 16,549 | 312 (111) | 310 (108) | 315 (117) | 308 (111) | 316 (108) |
| Protein intake (g/day) | 16,549 | 81.7 (34.3) | 63.5 (25.2) | 77.6 (29.2) | 85.6 (32.2) | 100.3 (38.3) |
| Fat intake (g/day) | 16,549 | 55.3 (27.1) | 38.8 (19.4) | 51.6 (22.0) | 59.0 (24.6) | 71.8 (30.1) |
Abbreviations: SD, standard deviation; MET, metabolic equivalent of task; Q1–Q4, the quartile groups of energy‐adjusted CML intake.
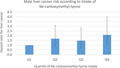
There were no significant multivariate‐adjusted hazard ratios of total cancer between the quartiles of CML intake in men (Table 3). Compared with men in the lowest quartile of CML intake, men in the second, third, and highest quartiles had increased risks of liver cancer with a significant linear trend (hazard ratios: 1.69, 1.48, and 2.10, respectively, trend p = 0.04). Conversely, a decreased relative risk of male stomach cancer was observed for the second and highest quartiles of CML intake versus the lowest quartile, with hazard ratios of 0.73 and 0.67, respectively (trend p = 0.08). In women, no significant associations were observed between CML intake and total and any site‐specific cancer (Table 4).
TABLE 3.
Multivariate‐adjusted hazard ratios (95% CI) for total cancer and site‐specific cancer according to intake of N ε‐carboxymethyl‐lysine among men
| Intake of N ε‐carboxymethyl‐lysine (CML) | Trend p | ||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| No. of subjects | 3544 | 3543 | 3543 | 3543 | |
| Person years | 46,628 | 47,135 | 45,114 | 43,068 | |
| Total cancer (C00–C97) | |||||
| No. of cancers | 490 | 455 | 489 | 520 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 0.93 (0.82–1.07) | 1.02 (0.89–1.16) | 1.05 (0.91–1.20) | 0.34 |
| Esophageal cancer (C15) | |||||
| No. of cancers | 26 | 14 | 12 | 14 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 0.70 (0.36–1.38) | 0.74 (0.35–1.55) | 0.97 (0.45–2.07) | 0.86 |
| Stomach cancer (C16) | |||||
| No. of cancers | 119 | 91 | 122 | 98 | |
| Hazard ratio (95% CI) a | 1.00 (Ref.) | 0.73 (0.54–0.98) | 0.94 (0.69–1.27) | 0.67 (0.47–0.96) | 0.08 |
| Colon cancer (C18) | |||||
| No. of cancers | 70 | 49 | 65 | 65 | |
| Hazard ratio (95% CI) b | 1.00 (Ref.) | 0.72 (0.49–1.07) | 0.99 (0.66–1.48) | 1.00 (0.64–1.58) | 0.69 |
| Rectal cancer (C19–C20) | |||||
| No. of cancers | 30 | 43 | 25 | 42 | |
| Hazard ratio (95% CI) b | 1.00 (Ref.) | 1.59 (0.96–2.64) | 0.97 (0.52–1.79) | 1.61 (0.86–3.00) | 0.29 |
| Liver cancer (C22) | |||||
| No. of cancers | 18 | 28 | 23 | 35 | |
| Hazard ratio (95% CI) c | 1.00 (Ref.) | 1.69 (0.92–3.10) | 1.48 (0.77–2.84) | 2.10 (1.10–3.98) | 0.04 |
| Gallbladder and biliary duct cancer (C23–24) | |||||
| No. of cancers | 10 | 16 | 14 | 13 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 1.54 (0.69–3.47) | 1.22 (0.51–2.87) | 0.96 (0.38–2.42) | 0.72 |
| Pancreas cancer (C25) | |||||
| No. of cancers | 21 | 19 | 13 | 25 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 0.86 (0.46–1.63) | 0.58 (0.28–1.21) | 1.03 (0.53–2.00) | 0.98 |
| Lung cancer (C33–C34)_ever smokers (n = 11,478) | |||||
| No. of cancers | 72 | 58 | 70 | 63 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 0.77 (0.54–1.09) | 0.92 (0.65–1.31) | 0.78 (0.54–1.15) | 0.34 |
| Lung cancer (C33–C34)_never smokers (n = 2288) | |||||
| No. of cancers | 0 | 2 | 0 | 8 | |
| Hazard ratio (95% CI) | – | – | – | – | – |
| Bladder cancer (C67) | |||||
| No. of cancers | 35 | 21 | 29 | 33 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 0.58 (0.34–1.01) | 0.80 (0.47–1.35) | 0.84 (0.49–1.45) | 0.77 |
| Prostate cancer (C61) | |||||
| No. of cancers | 32 | 37 | 52 | 54 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 1.08 (0.67–1.75) | 1.47 (0.92–2.34) | 1.37 (0.84–2.24) | 0.13 |
Note: Hazard ratios adjusted for age (years), body mass index (quartiles), education years (≤8, 9–11, 12–14, ≥15 years), history of diabetes (yes, no), physical activity score (METs h/week), smoking status (never, former, current smoker who had smoked for 30 years or less, current smoker who had smoked for 31 years or more), alcohol consumption (g/day), and intakes of total energy (kcal/day).
Abbreviations: CI: confidence interval; MET, metabolic equivalent of task; Q1–Q4: the quartile groups of energy‐adjusted CML intake.
Additionally adjusted for salt intake (g/day), in addition to the variables described above.
Additionally adjusted for height (quartiles), aspirin use (yes, no) and intakes of red meat and processed meat (g/d), in addition to the variables described above.
Additionally adjusted for coffee consumption (none, once a month to six times per week, ≥once per day), in addition to the variables described above.
TABLE 4.
Multivariate‐adjusted hazard ratios (95% confidence interval) for total cancer and site‐specific cancer according to intake of N ε‐carboxymethyl‐lysine among women
| Intake of N ε‐carboxymethyl‐lysine (CML) | Trend p | ||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| No. of subjects | 4138 | 4137 | 4137 | 4137 | |
| Person years | 55,180 | 56,569 | 56,878 | 56,625 | |
| Total cancer (C00–C97) | |||||
| No. of cancers | 404 | 354 | 360 | 359 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 0.92 (0.80–1.07) | 0.94 (0.81–1.09) | 0.97 (0.84–1.13) | 0.72 |
| Stomach cancer (C16) | |||||
| No. of cancers | 73 | 56 | 56 | 48 | |
| Hazard ratio (95% CI) a | 1.00 (Ref.) | 0.81 (0.56–1.17) | 0.80 (0.54–1.18) | 0.74 (0.49–1.13) | 0.17 |
| Colon cancer (C18) | |||||
| No. of cancers | 59 | 67 | 48 | 57 | |
| Hazard ratio (95% CI) b | 1.00 (Ref.) | 1.20 (0.83–1.74) | 0.84 (0.55–1.28) | 1.05 (0.68–1.62) | 0.82 |
| Rectal cancer (C19–C20) | |||||
| No. of cancers | 25 | 30 | 15 | 22 | |
| Hazard ratio (95% CI) b | 1.00 (Ref.) | 1.11 (0.63–1.96) | 0.53 (0.26–1.07) | 0.77 (0.39–1.54) | 0.21 |
| Liver cancer (C22) | |||||
| No. of cancers | 19 | 15 | 20 | 16 | |
| Hazard ratio (95% CI) c | 1.00 (Ref.) | 0.94 (0.47–1.86) | 1.33 (0.69–2.54) | 1.10 (0.54–2.21) | 0.60 |
| Gallbladder and biliary duct cancer (C23–C24) | |||||
| No. of cancers | 21 | 11 | 19 | 19 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 0.57 (0.28–1.20) | 0.95 (0.50–1.79) | 1.02 (0.53–1.96) | 0.78 |
| Pancreas cancer (C25) | |||||
| No. of cancers | 14 | 22 | 17 | 16 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 1.70 (0.86–3.33) | 1.29 (0.63–2.64) | 1.27 (0.61–2.67) | 0.68 |
| Lung cancer (C33–C34)_ever smokers (n = 2607) | |||||
| No. of cancers | 15 | 12 | 5 | 11 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 1.24 (0.57–2.67) | 0.58 (0.21–1.62) | 1.33 (0.58–3.03) | 0.83 |
| Lung cancer (C33–C34)_never smokers (n = 12,194) | |||||
| No. of cancers | 17 | 11 | 12 | 9 | |
| Hazard ratio (95% CI) | 1.00 (Ref.) | 0.65 (0.30–1.39) | 0.65 (0.30–1.39) | 0.50 (0.21–1.16) | 0.10 |
| Breast cancer (C50) | |||||
| No. of cancers | 43 | 45 | 49 | 43 | |
| Hazard ratio (95% CI) d | 1.00 (Ref.) | 0.96 (0.63–1.46) | 1.02 (0.67–1.55) | 0.88 (0.56–1.36) | 0.63 |
| Cervical cancer (C53) | |||||
| No. of cancers | 11 | 15 | 8 | 14 | |
| Hazard ratio (95% CI) d | 1.00 (Ref.) | 1.50 (0.67–3.38) | 0.85 (0.33–2.19) | 1.40 (0.59–3.29) | 0.69 |
| Endometrial cancer (C54) | |||||
| No. of cancers | 6 | 9 | 14 | 14 | |
| Hazard ratio (95% CI) d | 1.00 (Ref.) | 1.28 (0.45–3.63) | 1.91 (0.72–5.03) | 1.74 (0.65–4.66) | 0.20 |
| Ovarian cancer (C56) | |||||
| No. of cancers | 13 | 7 | 23 | 10 | |
| Hazard ratio (95% CI) d | 1.00 (Ref.) | 0.53 (0.21–1.35) | 1.81 (0.89–3.66) | 0.80 (0.34–1.90) | 0.69 |
Note: Hazard ratios adjusted for age (years), body mass index (quartiles), education years (≤8, 9–11, 12–14, ≥15 years), history of diabetes (yes, no), physical activity score (METs h/week), smoking status (never, former, current smoker who had smoked for 30 years or less, current smoker who had smoked for 31 years or more), alcohol consumption (g/day), and intakes of total energy (kcal/day).
Abbreviations: CI: confidence interval; MET, metabolic equivalent of task; Q1–Q4: the quartile groups of energy‐adjusted CML intake.
Additionally adjusted for salt intake (g/day), in addition to the variables described above.
Additionally adjusted for height (quartiles), aspirin use (yes, no) and intakes of red meat and processed meat (g/day), in addition to the variables described above.
Additionally adjusted for coffee consumption (none, once a month to six times per week, ≥once per day), in addition to the variables described above.
Additionally adjusted for height (quartiles), age at menarche (≤12, 13–14, 15–16, ≥17 year), age at first delivery (no, ≤20, 20–25, 26–30, ≥31 year), age at menopause (≤49, ≥50 year), number of children (0, 1, 2, ≥3), and hormone replacement therapy (yes, no), in addition to the variables described above.
To evaluate whether modifying factors exist in the association between CML intake and male liver cancer, participants were stratified by history of diabetes (yes, no), age (≥55, <55 years), smoking (ever, never), and alcohol consumption (≥23, <23 g of ethanol equivalent; Table S1). Because the number of male liver cancer was not sufficient to divide into quartiles after stratification, the tertiles of CML intake were applied for the stratified analyses. The significance for interaction was assessed using the product term of the CML intake and the stratifying factor. There was no significant interaction by diabetes, age, smoking or alcohol consumption, although the hazard ratios of liver cancer for the highest tertile versus the lowest tertile of CML intake were 2.15 among ever smokers (trend p = 0.01) and 0.45 among never smokers (trend p = 0.40). Similarly, those were 1.86 among those with no history of diabetes (trend p = 0.03) and 1.18 among those with history of diabetes (trend p = 0.75).
When we performed sensitivity analysis without using the data based on ELISA, the results were not altered substantially; compared with the lowest quartile of CML intake, the hazard ratios of total cancer for the second, third, and highest quartiles were 0.98 (95% CI: 0.86–1.12), 1.01 (95% CI: 0.8–1.15), and 1.06 (95% CI: 0.93–1.22), respectively, in men (trend p = 0.34) and 0.90 (95% CI: 0.78–1.04), 0.94 (95% CI: 0.82–1.09), and 0.99 (95% CI: 0.85–1.15), respectively, in women (trend p = 0.93). The hazard ratio of male liver cancer for the highest quartile versus the lowest quartile of CML intake was 2.02 (95% CI: 1.07–3.81; trend p = 0.04). The hazard ratios of male stomach cancer for the second and highest quartiles versus the lowest quartile of CML intake were 0.80 (95% CI: 0.60–1.06) and 0.68 (95% CI: 0.49–0.96), respectively (trend p = 0.06).
The associations between CML intake and total and site‐specific cancers were not substantially altered in men and women by excluding those who had a history of diabetes (899 men and 487 women; Tables S2 and S3).
When we re‐analyzed the data after excluding cancer cases during the first 2 years of follow‐up (205 men and 139 women), the nonsignificant associations between CML intake and total cancer did not change among men and women. The hazard ratio of male liver cancer for the highest quartile versus the lowest quartile of CML intake was 2.17 (95% CI: 1.07–4.38; trend p = 0.04). The hazard ratios of male stomach cancer for the second and highest quartiles versus the lowest quartile of CML intake were 0.73 (95% CI: 0.53–0.99) and 0.66 (95% CI: 0.46–0.96), respectively (trend p = 0.13).
4. DISCUSSION
In this prospective study in Japan, we did not observe a significant association between CML intake and the risk of total cancer in men or women. Higher CML intake was significantly associated with an increased risk of male liver cancer. Conversely, we found decreased risks of stomach cancer for the second and highest quartiles of CML intake in men. There were no significant associations between CML intake and any site‐specific cancer in women.
We found that CML intake was positively associated with the risk of liver cancer in men. The liver is responsible for the clearance and catabolism of circulating AGEs. 32 Absorbed AGEs preferentially accumulate in hepatic tissue. 6 So, the detrimental effects of AGEs might be more likely to occur in the liver. Experimental studies have suggested that a high AGE diet plays a role initiating liver inflammation. 33 , 34 Dietary AGEs enhance the accumulation of toxic AGE and upregulate RAGE mRNA expression leading to AGE–RAGE interactions, which releases proinflammatory molecules and induces oxidative stress in hepatocytes and hepatic stellate cells. 34 RAGE regulates tumorigenesis in inflammation‐associated liver carcinogenesis, while sRAGE has a protective role in hepatocellular injury by neutralizing the effects mediated by the AGE–RAGE. 35 , 36 One case–cohort study reported an inverse association between hepatocellular carcinoma and circulating CML and sRAGE among Finnish male smokers, 37 whereas the association between dietary intake and circulating levels of AGEs is unsure. 6 , 7 The EPIC study, another study on dietary AGEs and liver cancer, observed an inverse association between dietary CML and hepatocellular carcinoma in men and women combined; this contradict our study that observed a positive association between dietary CML and liver cancer in men. The subjects of the EPIC study had a little younger average age (51 year) than those of this study (55 year). The foods contributing to CML intake in the EPIC study was cereals (35%), meat (19%), cakes and biscuits (14%) and dairy (11%). The main food sources of dietary CML in this study were cereals (27%), meat (15%), dairy (12%), and pulses (8%). Bread and whole grains are commonly consumed in Western countries, whereas rice and refined grains are widely consumed in Japan. The AGE content of bread was much higher than that of rice. Whole grain intake was reported to be associated with a reduced risk of hepatocellular carcinoma in Western populations. 38 The associations between dietary AGEs and diseases may be different between Western and Asian countries, where diets differ greatly.
The increased risks of liver cancer in relation to higher CML intake were observed among ever smokers but not among never smokers. Smoking may modify the association between dietary AGEs and liver cancer. AGE precursors are present in tobacco and AGEs accumulation in tissues has been demonstrated to be higher in smokers than in nonsmokers. 39 Smoking, another determinant of exogenous AGEs, may contribute to the body's total AGE load together with dietary AGEs and enhance the effects of AGEs on liver cancer. Conversely, the positive association between dietary AGEs and liver cancer seemed to be more pronounced in nondiabetic men than in those with diabetes. Increased endogenous AGEs due to diabetes might reduce the effects of dietary AGEs on liver cancer. However, neither smoking nor diabetes significantly modified the association between dietary AGEs and liver cancer, and the EPIC study reported no interaction by diabetes, age, smoking, or alcohol consumption. Future studies are needed to confirm whether these modifying effects exist and to clarify the role of exogenous and endogenous AGEs on liver cancer.
Positive association between dietary AGEs and liver cancer was not observed among women. The EPIC study has not reported the association by sex. 19 Although the reason for the sex difference is unknown, it is possible that the dietary sources of CML are not exactly the same for men and women (Table S4). Whereas cereals and meat contributed more to CML in men, a variety of foods contributed more evenly to CML in women. Meat consumption was reported to not only contain AGEs, but also to be associated with greater accumulation of AGEs in the body. 39 As sex difference in lipoprotein or glucose metabolism in response to dietary intake has been suggested, 40 there might also be sex differences in the response of oxidative stress and inflammation to dietary AGEs.
Contrary to the hypothesis that dietary AGEs might influence cancer development, we observed a decreased risk of stomach cancer among men with high CML intake. The risk estimates for stomach cancer in women were similar to those for men, although they were not significant, perhaps due to the relatively small number of female stomach cancer. The explanation for this inverse association is not clear. RAGE was overexpressed in the mucosa with gastric cancer compared with the noncancerous tissues. 41 , 42 Subjects with the variant genotypes associated with enhanced RAGE signaling (82Gly/Ser and 82Ser/Ser) had a significantly higher risk of gastric cancer compared with the wild‐type carriers (82Gly/Gly). 43 A recent experiment has suggested that CML modification of HMGB1 enhances the cancer‐promoting effect of HMGB1. 44 Conversely, the final products of the Maillard reaction, called “melanoidins,” have been demonstrated to exhibit biological activities including antioxidant activity, metal chelating ability, and lipid peroxidation inhibitory activity, particularly in the gastrointestinal tract. 45 It was also suggested that melanoidins derived from food proteins inhibit urease–gastric mucin adhesion and suppress Helicobacter pylori colonization. 46 So, these mechanisms in the gut might counteract the harmful effects of AGE–RAGE on stomach cancer. Another cohort study has suggested an inverse association between dietary CML and colorectal cancer risk. 18
The previous two cohorts that estimated CML intake using the ELISA‐based database have reported a positive association between dietary intake of AGEs and the risk of pancreatic 13 and breast cancer. 14 , 15 These results may not exactly be comparable with our study by the UPLC–MS/MS‐based database that observed no significant association between dietary AGEs and pancreatic or breast cancer. The dietary sources that contributed the most to CML intake were fats and oils followed by meat products in those studies, different from those in our cohort (cereals followed by meat products). More prospective studies are warranted on the association between dietary AGEs and site‐specific cancers in diverse populations.
The strengths of our study include its use of databases for the CML content of food based on HPLC–MS/MS as well as its prospective design. The good participation rate, long follow‐up period, and the consideration of several confounding factors are also strengths. However, several limitations should be mentioned. Our FFQ was not validated for the assessment of CML intake. The Spearman correlation coefficients between the FFQ and 12 1‐day diet records kept over a 1‐year period for total energy, carbohydrate, protein, and fat intake were 0.44, 0.34, 0.38, and 0.24, respectively, for men and 0.53, 0.45, 0.63, and 0.52, respectively, for women. The CML values of foods on our FFQ were not completely covered by previous Western databases. In particular, the values for some foods typical to the Japanese diet were missing, although they were likely to be low in CML. For example, udon (a white wheat‐based noodle) and tempura (a dish of deep‐fried seafood or vegetables in light batter) were assigned CML values with reference to the values for boiled pasta and grilled cod, respectively. Sashimi (a dish of uncooked fish cut into small pieces) was assigned a CML of 0. In addition, the cooking methods, including the amount and duration of heat exposure, may differ between Japanese and Western diets, even for the same foods with the same cooking methods. However, measurement errors by such misclassifications are likely to have occurred independently of cancer incidence. We estimated only the CML intake in foods because CML has been used as a surrogate marker to estimate the AGE contents of foods and is commonly used in epidemiological studies, although other dietary AGEs might be differently associated with the risk of cancer. The information on exposure, including the FFQ, was collected only at baseline and changes in lifestyle habits were not evaluated during the follow‐up period. We did not obtain information regarding infections with H. pylori and hepatitis virus, although these are major risk factors for stomach and liver cancer. The sample size was limited, and therefore precluded analyses of several cancers with a small number of cases. Dietary patterns or lifestyle habits might have changed due to preclinical signs or underlying disease. However, the exclusion of cancer cases during the first 2 years of follow‐up did not change the results significantly.
In conclusion, this prospective study observed that high CML intake was significantly associated with an increased risk of liver cancer in Japanese men. Our finding suggests the potential harm of consuming AGEs on liver cancer risk. Furthermore, as dietary AGEs might have differential effects depending on the site of cancer, the associations between dietary AGEs and site‐specific cancers need to be further investigated.
DISCLOSURE
The authors have no conflict of interest. Dr. Chisato Nagata is a current Editorial Board Member of Cancer Science.
ETHICAL APPROVAL
Approval of the research protocol by an Institutional Reviewer Board: This study protocol was approved by the institutional review board of the Gifu University Graduate School of Medicine (26–277).
Informed Consent: Consent was waived due to the valid reasons for lack of consent at the time of the survey, the difficulty in obtaining consent now, and the public necessity of this research.
Supporting information
Tables S1–S4
ACKNOWLEDGMENTS
The Ministry of Education, Culture, Sports, Science, and Technology of Japan (Grant/Award Number: 15 K15222).
Wada K, Nakashima Y, Yamakawa M, et al. Dietary advanced glycation end products and cancer risk in Japan: From the Takayama study. Cancer Sci. 2022;113:2839‐2848. doi: 10.1111/cas.15455
Funding information
This work was supported by a grant from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (15 K15222).
REFERENCES
- 1. Chaudhuri J, Bains Y, Guha S, et al. The role of advanced glycation end products in aging and metabolic diseases: bridging association and causality. Cell Metab. 2018;28:337‐352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Uribarri J, Woodruff S, Goodman S, et al. Advanced glycation end products in foods and a practical guide to their reduction in the diet. J Am Diet Assoc. 2010;110:911, e912‐916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Snelson M, Coughlan MT. Dietary advanced glycation end products: digestion, metabolism and modulation of gut microbial ecology. Nutrients. 2019;11:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Koschinsky T, He CJ, Mitsuhashi T, et al. Orally absorbed reactive glycation products (glycotoxins): an environmental risk factor in diabetic nephropathy. Proc Natl Acad Sci USA. 1997;94:6474‐6479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Uribarri J, Cai W, Peppa M, et al. Circulating glycotoxins and dietary advanced glycation endproducts: two links to inflammatory response, oxidative stress, and aging. J Gerontol A Biol Sci Med Sci. 2007;62:427‐433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kellow NJ, Coughlan MT. Effect of diet‐derived advanced glycation end products on inflammation. Nutr Rev. 2015;73:737‐759. [DOI] [PubMed] [Google Scholar]
- 7. Semba RD, Ang A, Talegawkar S, et al. Dietary intake associated with serum versus urinary carboxymethyl‐lysine, a major advanced glycation end product, in adults: the energetics study. Eur J Clin Nutr. 2012;66:3‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Turner DP. The role of advanced glycation end‐products in cancer disparity. Adv Cancer Res. 2017;133:1‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. van Heijst JW, Niessen HW, Hoekman K, Schalkwijk CG. Advanced glycation end products in human cancer tissues: detection of Nepsilon‐(carboxymethyl)lysine and argpyrimidine. Ann N Y Acad Sci. 2005;1043:725‐733. [DOI] [PubMed] [Google Scholar]
- 10. Foster D, Spruill L, Walter KR, et al. AGE metabolites: a biomarker linked to cancer disparity? Cancer Epidemiol Biomarkers Prev. 2014;23:2186‐2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sharaf H, Matou‐Nasri S, Wang Q, et al. Advanced glycation endproducts increase proliferation, migration and invasion of the breast cancer cell line MDA‐MB‐231. Biochim Biophys Acta. 2015;1852:429‐441. [DOI] [PubMed] [Google Scholar]
- 12. Riehl A, Németh J, Angel P, Hess J. The receptor RAGE: bridging inflammation and cancer. Cell Commun Signal. 2009;7:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jiao L, Stolzenberg‐Solomon R, Zimmerman TP, et al. Dietary consumption of advanced glycation end products and pancreatic cancer in the prospective NIH‐AARP diet and health study. Am J Clin Nutr. 2015;101:126‐134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Peterson LL, Park S, Park Y, Colditz GA, Anbardar N, Turner DP. Dietary advanced glycation end products and the risk of postmenopausal breast cancer in the National Institutes of Health‐AARP diet and health study. Cancer. 2020;126:2648‐2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Omofuma OO, Turner DP, Peterson LL, Merchant AT, Zhang J, Steck SE. Dietary advanced glycation end‐products (AGE) and risk of breast cancer in the prostate, lung, colorectal and ovarian cancer screening trial (PLCO). Cancer Prev Res. 2020;13:601‐610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nowotny K, Schröter D, Schreiner M, Grune T. Dietary advanced glycation end products and their relevance for human health. Ageing Res Rev. 2018;47:55‐66. [DOI] [PubMed] [Google Scholar]
- 17. Niquet‐Léridon C, Jacolot P, Niamba CN, Grossin N, Boulanger E, Tessier FJ. The rehabilitation of raw and brown butters by the measurement of two of the major Maillard products, N(ε)‐carboxymethyl‐lysine and 5‐hydroxymethylfurfural, with validated chromatographic methods. Food Chem. 2015;177:361‐368. [DOI] [PubMed] [Google Scholar]
- 18. Aglago EK, Mayén AL, Knaze V, et al. Dietary advanced glycation end‐products and colorectal cancer risk in the European prospective investigation into cancer and nutrition (EPIC) study. Nutrients. 2021;13:3132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mayén AL, Aglago EK, Knaze V, et al. Dietary intake of advanced glycation endproducts and risk of hepatobiliary cancers: a multinational cohort study. Int J Cancer. 2021;149:854‐864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shimizu H. The basic report on takayama study. Department of Public Health, Gifu University School of Medicine, Gifu; 1996. [Google Scholar]
- 21. Shimizu H, Ohwaki A, Kurisu Y, et al. Validity and reproducibility of a quantitative food frequency questionnaire for a cohort study in Japan. Jpn J Clin Oncol. 1999;29:38‐44. [DOI] [PubMed] [Google Scholar]
- 22. Council for Science and Technology; Ministry of Education C, Sports, Science and Technology, Japan , ed. Standard Tables of Food Composition in Japan (5th Revised and Enlarged Edition) (in Japanese). Tokyo National Printing Bureau; 2005. [Google Scholar]
- 23. Nagata C, Wada K, Yamakawa M, et al. Dietary intake of Nε‐carboxymethyl‐lysine, a major advanced glycation end product, is not associated with increased risk of mortality in Japanese adults in the Takayama study. J Nutr. 2020;150:2799‐2805. [DOI] [PubMed] [Google Scholar]
- 24. Dresden TU. AGE database. https://lemchem.file3.wcms.tu‐dresden.de/.
- 25. Hull GL, Woodside JV, Ames JM, Cuskelly GJ. Validation study to compare effects of processing protocols on measured N (ε)‐(carboxymethyl)lysine and N (ε)‐(carboxyethyl)lysine in blood. J Clin Biochem Nutr. 2013;53:129‐133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Scheijen J, Clevers E, Engelen L, et al. Analysis of advanced glycation endproducts in selected food items by ultra‐performance liquid chromatography tandem mass spectrometry: presentation of a dietary AGE database. Food Chem. 2016;190:1145‐1150. [DOI] [PubMed] [Google Scholar]
- 27. Drusch S, Faist V, Erbersdobler HF. Determination of Nϵ‐carboxymethyllysine in milk products by a modified reversed‐phase HPLC method. Food Chem. 1999;65:547‐553. [Google Scholar]
- 28. Zhang G, Huang G, Xiao L, Mitchell AE. Determination of advanced glycation endproducts by LC‐MS/MS in raw and roasted almonds (Prunus dulcis). J Agric Food Chem. 2011;59:12037‐12046. [DOI] [PubMed] [Google Scholar]
- 29. Suzuki I, Kawakami N, Shimizu H. Reliability and validity of a questionnaire for assessment of energy expenditure and physical activity in epidemiological studies. J Epidemiol. 1998;8:152‐159. [DOI] [PubMed] [Google Scholar]
- 30. World Cancer Research Fund/American Institute for Cancer Research . Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. AICR; 2007. [Google Scholar]
- 31. World Cancer Research Fund/American Institute for Cancer Research Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Continuous Update Project Expert Report 2018. 2018. Available at dietandcancerreport.org.
- 32. Hyogo H, Yamagishi S. Advanced glycation end products (AGEs) and their involvement in liver disease. Curr Pharm des. 2008;14:969‐972. [DOI] [PubMed] [Google Scholar]
- 33. Patel R, Baker SS, Liu W, et al. Effect of dietary advanced glycation end products on mouse liver. PLoS One. 2012;7:e35143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Takeuchi M, Takino J, Sakasai‐Sakai A, et al. Involvement of the TAGE‐RAGE system in non‐alcoholic steatohepatitis: novel treatment strategies. World J Hepatol. 2014;6:880‐893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pusterla T, Nèmeth J, Stein I, et al. Receptor for advanced glycation endproducts (RAGE) is a key regulator of oval cell activation and inflammation‐associated liver carcinogenesis in mice. Hepatology. 2013;58:363‐373. [DOI] [PubMed] [Google Scholar]
- 36. Basta G, Navarra T, De Simone P, Del Turco S, Gastaldelli A, Filipponi F. What is the role of the receptor for advanced glycation end products‐ligand axis in liver injury? Liver Transpl. 2011;17:633‐640. [DOI] [PubMed] [Google Scholar]
- 37. Moy KA, Jiao L, Freedman ND, et al. Soluble receptor for advanced glycation end products and risk of liver cancer. Hepatology. 2013;57:2338‐2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Yang W, Ma Y, Liu Y, et al. Association of intake of whole grains and dietary fiber with risk of hepatocellular carcinoma in US adults. JAMA Oncol. 2019;5:879‐886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kellow NJ, Coughlan MT, Reid CM. Association between habitual dietary and lifestyle behaviours and skin autofluorescence (SAF), a marker of tissue accumulation of advanced glycation endproducts (AGEs), in healthy adults. Eur J Nutr. 2018;57:2209‐2216. [DOI] [PubMed] [Google Scholar]
- 40. Knopp RH, Paramsothy P, Retzlaff BM, et al. Gender differences in lipoprotein metabolism and dietary response: basis in hormonal differences and implications for cardiovascular disease. Curr Atheroscler Rep. 2005;7:472‐479. [DOI] [PubMed] [Google Scholar]
- 41. Wang D, Li T, Ye G, et al. Overexpression of the receptor for advanced glycation Endproducts (RAGE) is associated with poor prognosis in gastric cancer. PLoS One. 2015;10:e0122697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zhou Y, Liu SX, Zhou YN, Wang J, Ji R. Research on the relationship between RAGE and its ligand HMGB1, and prognosis and pathogenesis of gastric cancer with diabetes mellitus. Eur Rev Med Pharmacol Sci. 2021;25:1339‐1350. [DOI] [PubMed] [Google Scholar]
- 43. Gu H, Yang L, Sun Q, et al. Gly82Ser polymorphism of the receptor for advanced glycation end products is associated with an increased risk of gastric cancer in a Chinese population. Clin Cancer Res. 2008;14:3627‐3632. [DOI] [PubMed] [Google Scholar]
- 44. Kishi S, Nishiguchi Y, Honoki K, et al. Role of glycated high mobility group Box‐1 in gastric cancer. Int J Mol Sci. 2021;22:5185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tagliazucchi D, Bellesia A. The gastro‐intestinal tract as the major site of biological action of dietary melanoidins. Amino Acids. 2015;47:1077‐1089. [DOI] [PubMed] [Google Scholar]
- 46. Hiramoto S, Itoh K, Shizuuchi S, et al. Melanoidin, a food protein‐derived advanced maillard reaction product, suppresses Helicobacter pylori in vitro and in vivo. Helicobacter. 2004;9:429‐435. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S4


