Abstract
Introduction
Injuries around the elbow pose a challenging problem for orthopaedic surgeons. The complex bony architecture of the joint should be restored and the thin soft tissue envelope needs to be handled with meticulous care. Elbow instability is a complication seen after dislocations and fractures of the elbow and remains a treatment challenge. The purpose of this study was to provide subjective and objective results following the surgical treatment of unstable elbow dislocations with an external hinged fixation technique.
Methods
Forty-six consecutive patients with complex trauma of the elbow with instability after ligament reconstruction were enrolled between January 2017 and December 2019. The parameters used to quantify the subjective and objective functional results were the Mayo Elbow Score (MES, objective) and Oxford Elbow Score (OES, subjective), and clinical stability of the elbow joint. We also performed a radiological follow-up of the fractures.
Results
The mean MES and OES scores were good at the 12-month follow-up. We had 38 patients with stable joints and 8 patients with minor instability. Using the stress test, we saw a significant difference in the affected joint under varus stress (6.7 ± 1.8 mm) compared to the healthy joint (5.8 ± 1.2 mm) laterally. Furthermore, medially the gap was significantly larger (5.8 ± 0.8 mm, treated elbow) than the contralateral gap under valgus stress (4.3 ± 0.8 mm) (p <0.001). Twenty-one complications occurred in 46 patients (46%): Seven patients had a clinical change of elbow axis: Three valgus (6%), four varus (9%); Superficial wound infection occurred in one case (2%) and ulnar nerve dysfunction in two (4%). The most common medium-term complication was post-traumatic osteoarthritis in eight cases (17%). Heterotopic ossification occurred in five patients (11%) and elbow stiffness in five cases (11%).
Conclusion
The use of the hinged elbow external fixator in the treatment of complex elbow trauma is a valid therapeutic adjunct to ligamentous reconstruction showing encouraging results with acceptable complications.
How to cite this article
Meccariello L, Caiaffa V, Mader K, et al. Treatment of Unstable Elbow Injuries with a Hinged Elbow Fixator: Subjective and Objective Results. Strategies Trauma Limb Reconstr 2022;17(2):68–73.
Keywords: Complications, Dislocation, Fracture, Hinged external fixator, Instability, Ligament, Outcomes
Introduction
Injuries around the elbow pose a challenging problem for the orthopaedic surgeon.1 The complex bony architecture of the joint should be restored and the thin soft tissue envelope requires meticulous care.1,2 Fracture fixation and ligament repair should be stable enough to permit early postoperative mobilization to prevent post-traumatic stiffness and pain.3,4 In fracture-dislocations with severe soft tissue swelling, the risk and benefit of an extensive approach need to be weighed against a less invasive method providing adequate stability to allow early postoperative joint mobilization4 (Figs 1 and 2).
Figs 1A to M.
(A to C) Clinical photographs of a 48-year-older man with an open elbow injury, radial nerve palsy and metacarpal injuries on the left side; (D and E) The 3D-angio CT showed the elbow dislocation without arterial injuries; (F and G) The hinged external fixator is in place with an extension to the wrist; (H to J) The postoperative CT showed the reduction of radio-humeral and ulnar-humeral joints; (K) After 2 weeks we unlocked the hinged external fixation from the wrist external fixation; (L and M) Radiographs showing good reduction after 6 weeks of use
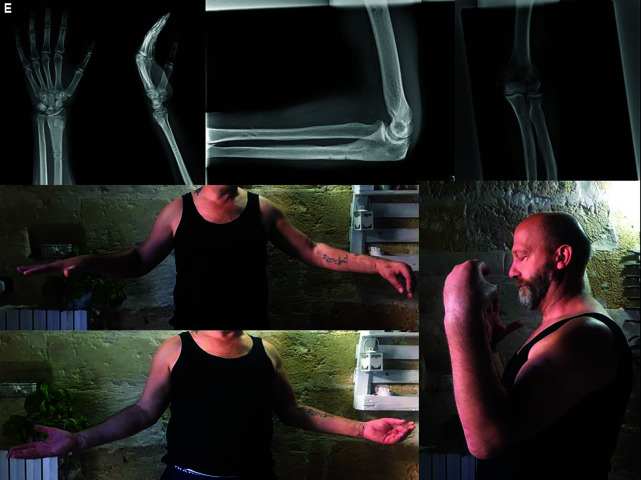
Figs 2A to E.
(A and B) Twelve months after surgery on the left side, the radiographs showed fracture healing of the elbow and wrist and little bone metaplasia around the MCL and LCL; (C to E) The elbow had a good range of motion, yet the radial nerve palsy persisted
This is not always possible in cases with open fractures, a floating elbow (Fig. 1), multi-ligament injuries with soft tissue damage, polytrauma, irreducible elbow dislocations, or in the elderly population where internal fixation is further compromised by demineralized bone.1–6 One of the most common problems encountered is elbow instability, which may arise through chronic overuse syndromes or as post-traumatic sequelae.4–6 Patients with chronic instability classically present with pain, apprehension, or mechanical subluxation of the elbow joint. External fixation appears to be an appealing adjunct to minimal surgical intervention, as it protects the fixation required and provides adequate stability to the joint for early postoperative motion around the rotation arc7 (Fig. 3).
Figs 3A to M.
(A) Seventy-year-old female had a left elbow posterolateral dislocation with an intra-articular fracture of the capitellum after a low energy trauma; (B and C) After reduction and casting in the emergency department, the CT showed the fracture and persistent elbow dislocation; (D to F) In the acute setting, we performed surgery with osteosynthesis, and applied a hinged external fixator; (G) Postoperative clinical image; (H and I) After 12 months radiographs showed good elbow alignment without osteoarthritis; (J to M) Excellent clinical outcomes after 12 months
The aim of the study was to evaluate a group of patients in whom external fixation was used as an adjunct to manage severe injuries to the elbow, including unstable dislocations, fracture-dislocations and chronic instability and to provide subjective and objective results utilizing this technique.
Material and Methods
From January 2017 to December 2019, all consecutive patients with acute instability, dislocations and fractures of the elbow joint were registered from three Italian Trauma Level I Centres and screened for this study.
From these fractures, we excluded patients with other injuries according to the characteristics described in Table 1.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Acute instability, dislocations and fractures of the elbow joint | Patients not treated with external fixation |
| Usage of elbow arthroplasty or radial head arthroplasty | |
| Isolated radial, capitellar or proximal ulna fractures | |
| Extension of fracture lines into the ulnar or humeral shaft | |
| Bilateral elbow injures | |
| Age under 16 years | |
| Haematological or oncological pathology | |
| Previous injuries, deformities or diseases at the contralateral upper limb |
All injury types were classified using plain radiographs and CT scans.5–7 The patients were informed in a clear and comprehensive way about the type of treatment and other possible surgical and conservative alternatives. Patients were treated according to the ethical standards of the Helsinki Declaration and were invited to read, understand, and sign the informed consent form.
In all cases, we applied a hinged elbow fixator using the Cittieffe hinged elbow fixator (Calderara di Reno, Bologna, Italy). All patients underwent the same rehabilitation protocol, starting active flexion and extension on day 5, with periodic follow-up examinations, frame stability checks and regular pin site care. After 6 weeks, the external fixator was removed, and full passive and active movement of the elbow was allowed. From 12 weeks, the patients commenced light upper extremity weight training and started an endurance programme simulating desired work requirements.
The patients received indomethacin 75 mg once a day for 4 weeks to prevent heterotopic ossification.8 To study bone healing on radiographs, we used the Non-union Scoring System (NUSS) in retrospective mode.9
The criteria to evaluate the injured elbow with a healthy elbow during the follow-up were the duration of surgery, objective quality of life and the elbow function measured by the MES,10 the subjective quality of life and the elbow function measured by OES10 and the clinical stability of the elbow joint. In addition, we measured the medial and lateral joint space by varus and valgus stress ultrasound examinations of the elbow.11 The elbow alignment was measured using the trochleocapitellar index in adults as described by Rollo et al.10 This is a ratio between the angle of the capitellum and the trochlea. Bone union was measured using the radiographic union score as described by Whelan et al.12 The evaluation endpoint was set at 12 months after surgery. Longer follow-up was performed when possible, to detect complications occurring after the evaluation endpoint, such as early post-traumatic osteoarthritis.
Statistical Analysis
Descriptive statistics were used to summarise the characteristics of the study group, including the means and standard deviations of all continuous variables. We compared the injured side to the uninjured, healthy side as an in-patient control. The t test was used to compare continuous outcomes. The Chi-square test (subgroups of 10 patients or more) or Fisher's exact test (subgroups smaller than 10 patients) were used to compare categorical variables. The statistical significance was defined as p <0.05. We used Pearson's correlation coefficient (r) to compare the correlation between the patient-reported outcomes and quality of life.
The reliability and validity of the correlation between functional outcome results and the trochleocapitellar index were determined using Cohen's kappa (κ).
Results
Forty-six patients were treated, of which 32 were male and 12 were female. The mean age was 43 years (range 16–93 years). The left side was affected in 25 cases (54%) and the right side in 21 cases (46%). The average duration of follow-up was 28 months (range 12–36 months). A fall from a height was the most cause of injury. There were 38 closed injuries and five compound fractures. Further demographic details are described in Table 2.
Table 2.
Demographic description of the patients treated with hinged external fixation
| Characteristics | Descriptive |
|---|---|
| Average age, years (SD; range) | 43 (14, 16–93) |
| Left side (n, %) | 25 (54%) |
| Right side (n, %) | 21 (46%) |
| Type of accident | |
| Fall from height (n, %) | 12 (269%) |
| Car accident (n, %) | 6 (13%) |
| Motorcycle accident (n, %) | 8 (17%) |
| Work-related accident (n, %) | 10 (22%) |
| Agricultural accident (n, %) | 6 (13%) |
| Low energy trauma (n, %) | 4 (9%) |
| Type of injuries | |
| Distal humeral fracture (n, %) | 8 (17%) |
| Dislocation (n, %) | 14 (30%) |
| Chronic instability (n, %) | 8 (17%) |
| Elbow stiffness (n, %) | 10 (21%) |
| Elbow osteoarthritis (n, %) | 6 (13%) |
| Closed injury (n, %) | 38 (83%) |
| Open injury | 8 (17%) |
| Occupation | |
| Agricultural industry | 8 (17%) |
| Industrial sector | 19 (41%) |
| Tertiary sector | 9 (20%) |
| Retired | 10 (22%) |
The lateral collateral ligament complex (LCL) was injured in 23 cases (50%) (Table 3), the coronoid acting as the primary bony static stabilizer was involved in 17 cases (37%), and there were 14 (30%) cases with avulsion of the common extensor origin tendon. There were two (4%) ulnar nerve lesions. The average Injury Severity Score (ISS) was 3.5 (range 1–24) and the average Glasgow Coma Score (GCS) was 14 (range 7–15).
Table 3.
Description of associated injures of the patients treated with the hinged elbow fixation
| Associated ligamentous injuries | |
| Medial collateral ligament (n, %) | 16 (35%) |
| Lateral collateral ligament complex (n, %) | 23 (50%) |
| Coronoid (n, %) | 17 (37%) |
| Common origin of extensors (n, %) | 14 (30%) |
| Common origin of flexors (n, %) | 9 (20%) |
| Anconeus muscle (n, %) | 1 (2%) |
| Brachialis muscle (n, %) | 2 (4%) |
| Triceps muscle or insertion (n, %) | 3 (6%) |
| Biceps muscle (n, %) | 5 (11%) |
| Associated nerve injuries | |
| Ulnar (n, %) | 0 |
| Median (n, %) | 0 |
| Radial (n, %) | 2 (4%) |
| General patient status | |
| Average Injury Severity Score (SD; range) | 3.5 (±2; 1–24) |
| Average Glasgow Coma Score (GCS); (SD; range) | 14 (±2; 7–15) |
The mean surgical time was 87 minutes (range 21–123 minutes). The time to complete bone union was 87 days (range 59–112). In patients with intra-articular fractures, we observed 28 different complications, the most common being post-traumatic osteoarthritis in eight cases (17%). An overview of outcomes is listed in Table 4. At 12 months after the surgery, the average arcs of flexion-extension and pronation-supination were statistically worse on the injured sides (p <0.05). Varus and valgus stress showed an increased widening of the joint spaces on the injured sides (p <0.05).
Table 4.
Comparison of outcomes for the injured and uninjured elbows
| Description of results | Injured side | Uninjured side | p-value |
|---|---|---|---|
| Average time to bone healing according to NUSS in days (SD; range) | 86 (±11; range 59–112) | Not applicable | |
| Numbers of complications (percent of total) | Clinical valgus elbow: 3 (6%) Clinical varus elbow: 4 (9%) Superficial wound infection: 1 (2%) Post-traumatic osteoarthritis: 8 (17%) Heterotopic ossification: 5 (11%) Elbow stiffness: 5 (11%) Ulnar nerve dysfunction: 2 (4%) |
Not applicable | |
| Arc of flexion-extension (SD; range) | 104° (±22°; 66–180°) | 172° (±2°; 167–180°) | <0.05 |
| Arc of prono-supination (SD; range) | 153° (±11°; 90–180°) | 172° (±7°; 165–180°) | <0.05 |
| Lateral joint widening with varus stress in mm (SD; range) | 6.7 (±1.8; 3.2–9.3) | 5.8 (±1.2; 1.2–8.7) | <0.05 |
| Medial joint widening with valgus stress in mm (SD; range) | 5.8 (±0.8; 3.3–8.6) | 4.3 (±0.8; 3.2–6.8) | <0.05 |
| Trochleocapitellar index healed in normal clinical alignment (SD; range) | 0.68 (±9.8; range 0.49–0.89) | 0.81° (±7.2; 0.67–1) | <0.05 |
| Trochleocapitellar index healed in clinical valgus alignment (SD; range) | 0.43 (±16.7; 0.28–0.64) | Not applicable | |
| Trochleocapitellar index healed in clinical varus alignment (SD; range) | 0.86 (±7.5; 0.82–1) | Not applicable | |
| Correlation between clinical-radiographic results and patients outcomes, κ (SD; range) | 0.58 (±0.16; 0.39–0.82) | 0.92 (±0.05; 0.87–1) | <0.05 |
SD, standard deviation
Collateral ligament tears were sutured with either an anchor (25) or with a transosseous suture, and nine cases required osteosynthesis utilizing plate, cannulated screws or K wire fixation. The quality of life and elbow function immediately after treatment of the injury with external fixation, measured using the MES, was 64 points (±25; range 26–100) for the injured sides, and 95 points (±3; range 90–100) for the uninjured side. After 12 months, the MES increased to 75 points (±16; range 42–100) while the uninjured side remained stable at 95 points (±3; range 90–100).
The subjective quality of life and elbow function with the external fixator, measured using the OES, increased from 66 points directly after treatment (±26; range 22–100) to 71 points (±25; range 36–100), as the uninjured side remained stable at 92 points after treatment (±6; range 84–100) and 92 points after 12 months (±8; range 78–100).
In total, 21 complications occurred in 46 patients (46%): Seven patients had a clinical change of elbow axis [three valgus (6%), four varus (9%); superficial wound infection occurred in one case (2%) and ulnar nerve dysfunction in two (4%)]. The most common medium-term complication was post-traumatic osteoarthritis in eight cases (17%). It is unknown whether this is a direct result of the initial trauma, and how external fixation stability affects the natural history of post-traumatic osteoarthrosis. Heterotopic ossification occurred in five patients (11%) and elbow stiffness in five cases (11%) (Table 4). The residual joint instability with approximately 1 mm of extra joint widening of the affected joint is statistically relevant yet clinically less relevant as this did not result in gross instability of the elbows.
Discussion
A fracture-dislocation of the elbow joint is a complex injury, which requires anatomical stable reduction to maintain well-aligned articular surfaces and prevent joint instability and additional soft tissue insult. These injuries are notorious for sequelae such as instability, rigidity and early osteoarthrosis.
Indications for the use of an articulated external fixator include acute instability, instability after osteosynthesis or ligamentous repair, chronic subluxation, open fractures, fracture-dislocations in uncooperative patients and complex injuries in the elderly population. We have used external fixation in patients with elbow instability, fractures and dislocations with good results,13 and several publications have reported on the use of hinged external fixation in the treatment of both acute and chronic elbow instability.13 Yu et al. reported the outcomes of 20 cases with acute complex instability of the elbow treated with hinged external fixation.14 Interestingly, these authors did not repair the LCL when using a hinged external fixator.13,14
In our series, the most common soft tissue injury was the LCL complex, and the coronoid was involved as the most frequent bony injury of the elbow together with radial head fractures.13
Our series and the literature support the use of articulated external fixation combined with minimally invasive fracture repair or ligament reconstruction, avoiding the need for an extensive approach required for a formal repair of the affected ligaments, as the hinged fixator protects minimal repair from excessive strain. This facilitated early recovery and effective early rehabilitation and movement. This aims to prevent scarring and stiffness in these patients.14,15 It is not possible to review post-traumatic elbow instability due to fracture-dislocation while ignoring the osseous injury, and the results of different fracture patterns are difficult to compare. We focused on the treatment of the ligamentous structures of the elbow joint and excluded patients with larger osseous lesions. To the best of our knowledge, this is the largest study about the use of a hinged elbow fixator for isolated ligamentous injuries of the elbow joint.
Attention to detail remains vital when applying the fixator, as complications can occur if anatomical safe zones are not respected. Osteoporotic bone or compromised soft tissues are often seen in the elderly population, which can affect the outcome of surgical reconstruction. In such circumstances, the hinged external fixator becomes an invaluable adjunct offering added stability to permit early joint movement. It is also now possible to limit the surgical approach to obtain optimal joint reduction with minimal internal fixation. Simple realignment of the metaphyseal fragments utilizing the fixator, if properly applied, can neutralise all the dislocating forces around the elbow.16 Hinged elbow fixators have been used in cases where residual instability is seen after ligament repair or fracture reduction.11,17
Conclusion
The medium-term range of motion and subjective results, as shown in this study, support the validity of hinged elbow fixation in acute elbow injuries combined with the ligamentous repair. This device is tolerated well by patients when applied correctly, and the potential complications with external fixation are manageable. External hinged fixation is a stable and effective method, which could significantly improve the treatment outcomes and reduce wound complications for ligamentous injuries around the elbow. It does however rely on careful patient selection, attention to detail in its application and a specific follow-up protocol to achieve good short- and long-term outcomes.
Orcid
Luigi Meccariello http://orcid.org/0000-0002-3669-189X
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Stavlas P, Gliatis J, Polyzois V, et al. Unilateral hinged external fixator of the elbow in complex elbow injuries. Injury. 2004;35(11):1158–1166. doi: 10.1016/j.injury.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Lerner A, Stein H, Calif E. Unilateral hinged external fixation frame for elbow compression arthrodesis: the stepwise attainment of a stable 90-degree flexion position: a case report. J Orthop Trauma. 2005;19(1):52–55. doi: 10.1097/00005131-200501000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed I, Mistry J. The management of acute and chronic elbow instability. Orthop Clin North Am. 2015;46(2):271–280. doi: 10.1016/j.ocl.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 4.Feranec M, Hart R, Kozák T. Hinged external fixation in orthopaedic and trauma surgery of the elbow. Acta Chir Orthop Traumatol Cech. 2013;80(6):391–395. 24750966 [PubMed] [Google Scholar]
- 5.Wyrick JD, Dailey SK, Gunzenhaeuser JM, et al. Management of complex elbow dislocations: a mechanistic approach. J Am Acad Orthop Surg. 2015;23(5):297–306. doi: 10.5435/JAAOS-D-14-00023. [DOI] [PubMed] [Google Scholar]
- 6.Ebrahimzadeh MH, Amadzadeh-Chabock H, Ring D. Traumatic elbow instability. J Hand Surg Am. 2010;35(7):1220–1225. doi: 10.1016/j.jhsa.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Tarassoli P, McCann P, Amirfeyz R. Complex instability of the elbow. Injury. 2017;48(3):568–577. doi: 10.1016/j.injury.2013.09.032. [DOI] [PubMed] [Google Scholar]
- 8.Rollo G, Meccariello L, Rotini R, et al. Efficacy of the “Salento technique”, a modified two-incision approach in distal biceps brachii tendon repair. Surgical description and outcomes analysis. J Clin Orthop Trauma. 2019;10(5):959–964. doi: 10.1016/j.jcot.2019.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calori GM, Colombo M, Mazza EL, et al. Validation of the Non-Union Scoring System in 300 long bone non-unions. Injury. 2014;45(Suppl 6):S93–S97. doi: 10.1016/j.injury.2014.10.030. [DOI] [PubMed] [Google Scholar]
- 10.Rollo G, Rotini R, Eygendaal D, et al. Effect of trochleocapitellar index on adult patient-reported outcomes after noncomminuted intra-articular distal humeral fractures. J Shoulder Elbow Surg. 2018;27(7):1326–1332. doi: 10.1016/j.jse.2018.02.073. [DOI] [PubMed] [Google Scholar]
- 11.Hopf JC, Berger V, Krieglstein CF, et al. Treatment of unstable elbow dislocations with hinged elbow fixation-subjective and objective results. J Shoulder Elbow Surg. 2015;24(2):250–257. doi: 10.1016/j.jse.2014.09.034. [DOI] [PubMed] [Google Scholar]
- 12.Whelan DB, Bhandari M, Stephen D, et al. Development of the radiographic union score for tibial fractures for the assessment of tibial fracture healing after intramedullary fixation. J Trauma. 2010;68(3):629–632. doi: 10.1097/TA.0b013e3181a7c16d. [DOI] [PubMed] [Google Scholar]
- 13.Sakai K, Shirahama M, Shiba N, et al. Primary hinged external fixation of terrible triad injuries and olecranon fracture-dislocations of the elbow. Kurume Med J. 2016;63(1.2):7–14. doi: 10.2739/kurumemedj.MS6300003. [DOI] [PubMed] [Google Scholar]
- 14.Yu S, Wang W, Liu S, et al. Arthrolysis and delayed internal fixation combined with hinged external fixation for elbow stiffness associated with malunion or nonunion of capitellum fracture. J Shoulder Elbow Surg. 2015;24(6):941–946. doi: 10.1016/j.jse.2015.01.019. [DOI] [PubMed] [Google Scholar]
- 15.Castelli A, D'amico S, Combi A, et al. Hinged external fixation for Regan–Morrey type I and II fractures and fracture-dislocations. J Orthopaed Traumatol. 2016;17(2):175–179. doi: 10.1007/s10195-016-0395-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maniscalco P, Pizzoli AL, Brivio LR, et al. Hinged external fixation for complex fracture-dislocation of the elbow in elderly people. Injury. 2014;45:S53–S57. doi: 10.1016/j.injury.2014.10.024. [DOI] [PubMed] [Google Scholar]
- 17.Donohue KW, Mehlhoff TL. Chronic elbow dislocation: evaluation and management. J Am Acad Orthop Surg. 2016;24(7):413–423. doi: 10.5435/JAAOS-D-14-00460. [DOI] [PubMed] [Google Scholar]