Abstract
AIM
To compare the efficacy of vitrectomy combined with air or silicone oil in the treatment of idiopathic macular hole (IMH).
METHODS
According to the results of high-definition optical coherence tomography (HD-OCT), 75 cases (75 eyes) of IMH in stage II-IV (Gass stage) in the General Hospital of Chinese PLA from January 2017 to December 2019 were collected for this retrospective study. The best corrected visual acuity (BCVA) and minimum diameter of IMH (MMHD) were measured. Eyes underwent vitrectomy combined with internal limiting membrane peeling operation, and were divided into disinfection air group (30 eyes) and silicone oil group (45 eyes) according to the intraocular tamponade. For MMHD≤400 µm (MMHD1), there were 23 eyes in air group and 16 eyes in silicone oil group. For MMHD2>400 µm (MMHD2), there were 7 eyes in air group and 29 eyes in silicone oil group. One month after surgery, the closure rates of IMH and BCVA were compared and analyzed. According to HD-OCT, the closure shape was graded with A (bridge closure) and B (good closure).
RESULTS
The closure rates of air group and silicone oil group were 86.67% and 95.56% respectively with no significant difference (P>0.05); For MMHD1, those of air group and silicone oil group were 95.65% and 100% respectively with no significant difference (P>0.05); For MMHD2, those of air group and silicone oil group were 57.14% and 93.10% respectively, and those of the silicone oil group were higher than the air group (P<0.05). There was no significant difference in the closure shape grade between MMHD1 air group and silicone oil group (P>0.05). The proportion of Grade B in MMHD2 silicone oil group was higher than that in the air group (P<0.05). BCVA of each group after operation was better than that before operation, and there was no significant difference between air group and silicone oil group. While among them, MMHD1 air group was better than silicone oil group (P<0.05), and there was no significant difference between MMHD2 air group and silicone oil group (P>0.05).
CONCLUSION
For smaller IMH (≤400 µm), the efficacy of vitrectomy combined with air should be considered better than silicone oil; for larger IMH (>400 µm), the efficacy of silicone oil may be better than air.
Keywords: idiopathic macular hole, vitreoretinal surgery, silicone oil, air
INTRODUCTION
Macular hole is a full-thickness tissue defect in the retinal neuroepithelial layer of the macular region, which can cause visual loss, visual distortion and other clinical manifestations. Clinical treatment are mainly vitrectomy and internal limiting membrane peeling combined with different intraocular tamponade[1]–[2]. Expansile gas is the favorite tamponade, but due to some incidents of infection in China in recent years, it could not be obtained stably clinically. In fact, disinfected airusually has excellent effect on idiopathic macular hole (IMH) in some situations[3]–[5], but in the meantime there are still a lot of failed reports[6]–[7], whose main cause is due to the insufficient duration. So sometimes silicone oil is needed to be used. But because of the well-known side effects and limitation, it is often hard to make a choice between disinfected air and silicone oil. There are few articles comparing the effects of air and gas on IMH surgery, but articles about air vs silicone oil has not been found. At present, there is no clear guidance for these two tamponades, and the choice relies mainly on the experience of the operators. In this study, we tried to explore the rule and compare the effects of them according to the closure rates, the closure shape, complications, and the improvement of vision.
SUBJECTS AND METHODS
Ethical Approval
All patients' data and essential information were retrieved from medical records during the period from January 2017 to December 2019 in the Ophthalmology Department of Chinese PLA General Hospital. All the patients had been given explanation and signed informed consent before every operation under the supervision by the Medical Management Division of the hospital. And tenets of the Declaration of Helsinki were adhered to for this study.
Inclusion criteria: 1) macular full-thickness hole with stage II or above by optical coherence tomography (OCT) measurement; 2) course of disease ≤2y. Exclusion criteria: 1) refractive stromal opacity affecting fundus examination or treatment; 2) history of ocular trauma, surgery or intraocular injection; 3) patients with refractive power <-6.00 D or axial length>26 mm; 4) patients with previous vitreoretinal surgery; 5) patients with optic neuropathy; 6) patients with heart, lung, liver, kidney dysfunction or other intolerable surgical treatments; 7) patients with incomplete key follow-up records.
All patients underwent best corrected visual acuity (BCVA), intraocular pressure (IOP), slit lamp microscope, fundus preset lens, fundus color photography and macular OCT examination. Zeiss Cirrus HD5000-OCT was used to scan IMH center with the scanning depth of 2 mm and the scanning range of 6×6 mm2. Four diameter lines of 0°, 45°, 90°, and 135° were selected. The minimum value of the four diameter lines measured by the built-in tool of OCT was selected as MMHD. BCVA was performed with international standard visual chart and converted to logarithm of the minimum angle of resolution (logMAR) visual acuity.
All eyes underwent conventional three channel pars plana vitrectomy. The posterior vitreous cortex was detached and cut. Internal limiting membrane was peeled from the upper vascular arch to the lower. Intraocular tamponade with air or silicone oil was employed at the end of the intervention. The 30 cases (30 eyes) were filled with air and 45 cases (45 eyes) with silicone oil. All operations were performed by three experienced doctors. After the operation, the patient kept a facedown position, air group for seven days and silicone oil group for two weeks. All cases were not combined with cataract surgery.
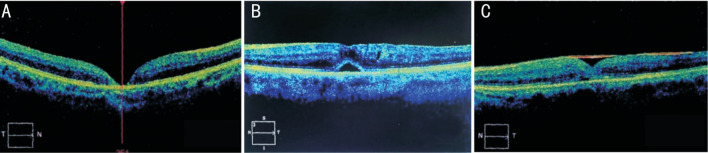
One month after the operation, BCVA, IOP, slit lamp microscope, fundus color photography and OCT were performed with the same equipment and method as before. The closure rates, complications and BCVA of air group and silicone oil group in different MMHD intervals before and after the treatment were compared and analyzed. The disappearance of neuroepithelial layer defect in macular area showed by OCT examination was regarded as IMH closure, while its existence was regarded as IMH unclosed (Figure 1A)[8]. According to the reference[9], the closed IMHs were divided into two grades: A (bridge closure) and B (good closure). Grade A: Subretinal fluid was still present in the class a fovea (Figure 1B). Grade B: fovea was restored to a basically normal structure (Figure 1C).
Figure 1. The closing condition was assessed by HD-OCT one month after surgery.
A: Sketch map for unclosed IMH (neuroepithelial layer defect in macular area still existed); B: Classification of IMH closure-Grade A (subretinal fluid was still present in the fovea); C: Classification of IMH closure-Grade B (fovea was restored to a basically normal structure). IMH: Idiopathic macular hole.
Statistical Analysis
SPSS 21.0 was used for statistical analysis, and the measurement data was expressed as mean±standard deviation (mean±SD). The t-test was used to compare the common data between the two groups and between the groups in different MMHD intervals. Fisher exact probability test was used to test the closure rates and closure grade ratio of IMH after operation. BCVA before and after operation was compared with paired t-test. P<0.05 was statistically significant.
RESULTS
Totally 75 patients (75 eyes) with IMH who underwent vitrectomy combined with internal limiting membrane peeling were included in this study. There were 21 males and 54 females with the average age of 61.2±8.1y. The courses of disease ranged from two weeks to 24mo. The average course was 3.8±7.2mo.
In the air group, there were 8 males and 22 females with the average age of 63.1±9.6y and the average course of 3.6±8.5mo. In the silicone oil group, there were 13 males and 32 females with the average age of 58.7±7.0y and the average course of disease of 4.0±6.5mo. There was no significant difference in age and course of disease between the two groups (all P>0.05). In the range of MMHD ≤400 µm (MMHD1) there were 23 eyes in air group and 16 eyes in silicone oil group; the average of MMHD were (277.6±43.9) and (303.4±43.1) µm respectively; the average of BCVA were 1.23±0.46 and 1.27±0.50 respectively; there was no statistical difference (P>0.05). In the range of MMHD>400 µm (MMHD2) there were 7 eyes in air group and 29 eyes in silicone oil group; the average of MMHD were (491.6±70.8) and (525.4±103.6) µm respectively; the average of BCVA were 1.41±0.32 and 1.40±0.39 respectively; there was no statistical difference (P>0.05).
One month after operation, IMHs were closed in 26 eyes out of 30 eyes in air group, and the closure rate was 86.67%. IMHs were closed in 43 eyes out of 45 eyes in silicone oil group, and the closure rate was 95.56%. There was no significant difference in IMH closure rate between the two groups (P>0.05). In MMHD1, IMHs were closed in 22 eyes out of 23 eyes in air group, and the closure rate was 95.65%; IMHs were all closed in 16 eyes in silicone oil group, and the closure rate was 100.0%, there was no significant difference between the two groups (P>0.05). In MMHD2, IMHs were closed in four eyes out of seven eyes in air group (57.14%), and in 27 eyes out of 29 eyes in silicone oil group (93.1%), so the silicone oil group showed a better result than the air group (P<0.05). The closure rate of MMHD1 in air group was higher than that of MMHD2 (P<0.05), while the closure rate of different MMHD didn't exist significant difference in silicone oil group (P>0.05), but the rate of absolute value in MMHD1 was higher than that in MMHD2 (Table 1).
Table 1. The overall closure rate of IMH and the closure rate in different sizes of IMH 1mo after surgery.
| Groups | Eyes | Overall closure rate | MMHD1 closure rate | MMHD2 closure rate |
| Air | 30 | 86.67 | 95.65 | 57.14b |
| Silicone oil | 45 | 95.56 | 100 | 93.10a |
aThe difference between silicone oil group and air group was statistically significant (P<0.05); bThe difference between MMHD1 and MMHD2 under the same tamponade was statistically significant (P<0.05).
%
One month after operation, there was no significant difference in closure grade between MMHD1 air group and silicone oil group (P>0.05), but the proportion of Grade B in MMHD2 silicone oil group was higher than that in air group (P<0.05; Table 2).
Table 2. Closure grade of IMH one month after operation.
| Groups | MMHD1 |
MMHD2 |
||||
| Grade A (eyes) | Grade B (eyes) | Proportion of Grade B | Grade A (eyes) | Grade B (eyes) | Proportion of Grade B | |
| Air | 7 | 15 | 68.18% | 3 | 1 | 25.00% |
| Silicone oil | 6 | 10 | 62.50% | 5 | 22 | 81.48%a |
aThe difference between silicone oil group and air group was statistically significant (P<0.05).
The postoperative BCVA of the air group, the silicone oil group and the subgroup according to the MMHD were improved compared with the preoperative (all P<0.05). There was no significant difference in the postoperative BCVA between the overall air group and the overall silicone oil group, while the MMHD1 air group was better than the silicone oil group (P<0.05), and there was no significant difference between the MMHD2 air group and the silicone oil group (P>0.05; Table 3).
Table 3. Comparison of BCVA in different MMHD one month after operation.
| Groups | Preop. BCVA |
Postop. BCVA |
||||
| Overall | MMHD1 | MMHD2 | Overall | MMHD1 | MMHD2 | |
| Air | 1.06±0.27 | 0.93±0.30 | 1.12±0.23 | 0.63±0.21b | 0.57±0.15b | 0.82±0.27b |
| Silicone oil | 1.10±0.25 | 0.96±0.25 | 1.18±0.26 | 0.75±0.21b | 0.69±0.17a,b | 0.79±0.24b |
aThe difference between silicone oil group and air group was statistically significant (P<0.05); bThe difference between postop. BCVA and the preop. BCVA under the same tamponadewas statistically significant (P<0.05).
According to the literature, ocular hypertension (OHT) has been defined as a postsurgical IOP>21 mm Hg or an increase of >10 mm Hg over the IOP baseline[10], and ocular hypotony has been defined as a postsurgical IOP≤7 mm Hg[11]. There were seven eyes (15.56%) with ocular hypertension in silicone oil group and none in air group. Under the treatment with captopril hydrochloride and brinzolamide eye drops, all the IOP returned to normal within one week. There were two eyes (6.7%) with ocular hypotony in the air group, but without retinal nor choroidal detachment.
One month after the operation, there was no significant change in the lens of all eyes in the air group, but the lens opacity of three eyes deteriorated in the silicone oil group. No serious complications such as endophthalmitis occurred in all cases.
DISCUSSION
The closure of macular hole is mainly due to the release of traction in the vertical and tangential directions[12], and the top pressure of tamponade on the neuroepithelium at the edge of the hole[13]. It is generally considered that inert gas is a relatively ideal tamponadematerial because of its long duration effect and few side effects[14]–[15]. However, in recent years, most of Chinese medical institutions lack of inert gas because of infection and related problems. So, the surgeons could only choose between disinfected air and silicone oil.
In this retrospective study, there was no difference in the overall closure rates of IMH between air group and silicone oil group. Venkatesh et al[16] studied various quantitative parameters of IMH by observing pre- and post-operative OCT images, and found a significant negative correlation of IMH closure with MMHD. Similarly, we found that the closure rate of MMHD1 in air group was higher than that of MMHD2; although there was no difference in silicone oil group between MMHD1 and MMHD2, MMHD1 was higher than MMHD2 in absolute value. Furthermore, we subdivided MMHD and compared air group with silicone oil group again. There was no significant difference in MMHD1 closure rates between the two groups; the closure rate of MMHD2 silicone oil group was higher than that of air group. The results showed that the two tamponades both have satisfactory closure effects for smaller IMH, and there was little difference between them; for larger IMH, the closure rate of silicone oil was obviously higher than that of air.
There are many factors influencing IMH closure, including macular choroidal thickness and blood supply[17], duration of IMH[18], MMHD and other parameters of IMH[19]. But for the necessary conditions, there are two elements: the movement of the traction of the vitreoretinal interface, and the dry environment of the macular interface[20]–[21]. The jacking force of the bubble leads the anatomic reattachment of neuroepithelium and RPE, and further promoting the healing of IMH with the functional recovery of retinal pigment epithelium (RPE) pump. At the same time, this kind of top pressure which can isolate subretinal fluid plays a role as the bridge in the healing of neuroepithelium in IMH, besides, it could restrict the cell composition and growth factor from entering the subretinal space[22]. The time required for IMH closure are various: It is generally considered as three to five days, but longer durations are often reported. In addition, there are many cases with IMH reopening because of gas absorption. For example, Özkan et al[23] found that, in the study of 52 cases of IMH three cases' (5.76%) IMHs had closed at first, but relapsed at different time point with the inert gas filling absorption. The results showed that some IMHs need longer duration than general inert gas. Thus, silicone oil still has its applicability even if inert gas is available. By comparing air and silicone oil, we found that for smaller IMH, there was no difference in the closure rate, while for larger IMH, using silicone oil could significantly improve the closure rate. In addition, when using air, the closure rate of MMHD2 was significantly lower than that of MMHD1, which indicated that it was not appropriate to select air for larger MMHD. On the other side, it was further confirmed that silicone oil should be selected to improve the closure rate of larger hole.
There was no significant difference in BCVA between the overall air group and the overall silicone oil group. Because some studies had shown that the improvement of visual function was closely related to both the MMHD and the closure rate of IMH[24]–[25], each group was subdivided according to MMHD in our study. It was found that BCVA of MMHD1 air group was better than silicone oil group, but significant difference was not found in MMHD2 between the two tamponades. There are many determinants of visual acuity after IMH surgery. For the comparison of air and silicone oil, the main factors are the closure rate, closure shape and complications[26]–[27]. There was no significant difference in the closure rate and shape between the two MMHD2 groups. The difference of BCVA was mainly due to the complications of silicone oil, such as complicated cataract and secondary glaucoma. In addition, the side effects of silicone oil on visual acuity include promoting preretinal proliferation and even causing macular fold[28]. Besides, there are many reports about the damage of optic nerve and optic chiasm caused by silicone oil drops[29]. In our study, the silicone oil group was better than the air group in terms of the closure rate and closure shape in MMHD2 because of the better efficacy of continuous top pressure. But at the same time, the complications of silicone oil offset those advantages. As a result, there was no significant difference in BCVA between the two MMHD2 groups.
Through this study, it can be concluded that for smaller IMH, choosing air can obtain better vision with similar closure rate, and relieve patients from pain and complications; for larger IMH, choosing silicone oil can achieve better closure efficacy with similar postoperative vision.
Except for the size of IMH, age, axial length, epiretinal membrane, etc[30]–[32], may be the influenced factors to the closure of IMH. It has to say that was a defect in this research. And if the observation elements were extended, that would be more complete.
Acknowledgments
Authors' contributions: Yin L: contributed to the conception of the study and wrote the manuscript; Liu AQ: conducted the statistical analysis and wrote the manuscript; Jin X: conducted the statistical analysis; Jia L: retrieved from medical records; Wang FX: contributed to the analysis and constructive instructions.
Conflicts of Interest: Yin L, None; Liu AQ, None; Jin X, None; Jia L, None; Wang FX, None.
REFERENCES
- 1.Frisina R, Gius I, Tozzi L, Midena E. Refractory full thickness macular hole: current surgical management. Eye (Lond) 2022;36(7):1344–1354. doi: 10.1038/s41433-020-01330-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu J, Hu ZZ, Zheng XH, Li YL, Huang JL, Cao EB, Yuan ST, Xie P, Liu QH. Displacement of the retina after idiopathic macular hole surgery with different internal limiting membrane peeling patterns. Int J Ophthalmol. 2021;14(9):1408–1412. doi: 10.18240/ijo.2021.09.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tao JW, Chen H, Chen YQ, Yu JX, Xu JW, Mao JB, Lin L, Shen LJ. Efficacy of air tamponade treatment of idiopathic macular holes of different diameters and of follow-up intravitreal air tamponade for persistent holes. Retina. 2022;42(5):877–882. doi: 10.1097/IAE.0000000000003394. [DOI] [PubMed] [Google Scholar]
- 4.He F, Dong FT, Yu WH, Dai RP. Recovery of photoreceptor layer on spectral-domain optical coherence tomography after vitreous surgery combined with air tamponade in chronic idiopathic macular hole. Ophthalmic Surg Lasers Imaging Retina. 2015;46(1):44–48. doi: 10.3928/23258160-20150101-07. [DOI] [PubMed] [Google Scholar]
- 5.Yu YP, Liang XD, Wang ZY, Wang J, Liu XX, Chen JQ, Liu W. Internal limiting membrane peeling and air tamponade for stage iii and stage iv idiopathic macular hole. Retina. 2020;40(1):66–74. doi: 10.1097/IAE.0000000000002340. [DOI] [PubMed] [Google Scholar]
- 6.Veith M, Vránová J, Němčanský J, Studnička J, Penčák M, Straňák Z, Mojžíš P, Studený P, Piñero DP. Surgical treatment of idiopathic macular hole using different types of tamponades and different postoperative positioning regimens. J Ophthalmol. 2020;2020:8858317. doi: 10.1155/2020/8858317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao XY, Meng LH, Zhang WF, Yu WH, Chen YX, Min HY. PUMCH experience and strategy for the management of idiopathic macular hole: a retrospective cohort study. Int Ophthalmol. 2022;42(4):1133–1145. doi: 10.1007/s10792-021-02099-z. [DOI] [PubMed] [Google Scholar]
- 8.Kang SW, Ahn K, Ham DI. Types of macular hole closure and their clinical implications. Br J Ophthalmol. 2003;87(8):1015–1019. doi: 10.1136/bjo.87.8.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu PP, Sun YY, Dong CY, Song D, Jiang YR, Liang JH, Yin H, Li XX, Zhao MW. A new method to predict anatomical outcome after idiopathic macular hole surgery. Graefes Arch Clin Exp Ophthalmol. 2016;254(4):683–688. doi: 10.1007/s00417-015-3116-x. [DOI] [PubMed] [Google Scholar]
- 10.Liesenborghs I, Schouten JSAG, Berendschot TTJM, Beckers HJM, Nuijts RMMA, Visser N, Webers CAB. Risk factors for the development of ocular hypertension after keratoplasty: a systematic review. Cornea. 2020;39(3):394–402. doi: 10.1097/ICO.0000000000002209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abbas A, Agrawal P, King AJ. Exploring literature-based definitions of hypotony following glaucoma filtration surgery and the impact on clinical outcomes. Acta Ophthalmol. 2018;96(3):e285–e289. doi: 10.1111/aos.13601. [DOI] [PubMed] [Google Scholar]
- 12.Chen N, Zheng K. Internal limiting membrane peeling without vitrectomy for laser-induced macular holes in two children. Eur J Ophthalmol. 2022;32(3):NP41–NP45. doi: 10.1177/1120672121990633. [DOI] [PubMed] [Google Scholar]
- 13.Alberti M, la Cour M. GAS-FOVEAL CONTACT: a new approach to evaluating positioning regimens in macular hole surgery. Retina. 2018;38(5):913–921. doi: 10.1097/IAE.0000000000001654. [DOI] [PubMed] [Google Scholar]
- 14.González-Cortés JH, Olvera-Barrios A, Treviño-Rodríguez HA, González-Cantú JE, M-Hamsho J. Closure of stage 2 macular hole with a low-dose intravitreal injection of perfluoropropane. Cir Cir. 2019;87(5):564–567. doi: 10.24875/CIRU.18000363. [DOI] [PubMed] [Google Scholar]
- 15.Bikbova G, Oshitari T, Baba T, Yamamoto S, Mori K. Pathogenesis and management of macular hole: review of current advances. J Ophthalmol. 2019;2019:3467381. doi: 10.1155/2019/3467381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Venkatesh R, Mohan A, Sinha S, Aseem A, Yadav NK. Newer indices for predicting macular hole closure in idiopathic macular holes: a retrospective, comparative study. Indian J Ophthalmol. 2019;67(11):1857–1862. doi: 10.4103/ijo.IJO_364_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sul S, Gurelik G, Korkmaz Ş, Ozsaygili C. Choroidal thickness in macular holes. Int Ophthalmol. 2019;39(11):2595–2601. doi: 10.1007/s10792-019-01108-6. [DOI] [PubMed] [Google Scholar]
- 18.Fallico M, Jackson TL, Chronopoulos A, et al. Factors predicting normal visual acuity following anatomically successful macular hole surgery. Acta Ophthalmol. 2021;99(3):e324–e329. doi: 10.1111/aos.14575. [DOI] [PubMed] [Google Scholar]
- 19.Baumann C, El-Faouri M, Ivanova T, Patton N, Ch'ng SW, Dhawahir-Scala F, Jalil A. Manchester Revisional Macular Hole Study: predictive value of optical coherence tomography parameters on outcomes of repeat vitrectomy, extension of internal limiting membrane peel, and gas tamponade for persistent macular holes. Retina. 2021;41(5):908–914. doi: 10.1097/IAE.0000000000002959. [DOI] [PubMed] [Google Scholar]
- 20.Shiode Y, Morizane Y, Matoba R, Hirano M, Doi S, Toshima S, Takahashi K, Araki R, Kanzaki Y, Hosogi M, Yonezawa T, Yoshida A, Shiraga F. The role of inverted internal limiting membrane flap in macular hole closure. Invest Ophthalmol Vis Sci. 2017;58(11):4847–4855. doi: 10.1167/iovs.17-21756. [DOI] [PubMed] [Google Scholar]
- 21.Bonińska K, Nawrocki J, Michalewska Z. Mechanism of “flap closure” after the inverted internal limiting membrane flap technique. Retina. 2018;38(11):2184–2189. doi: 10.1097/IAE.0000000000001861. [DOI] [PubMed] [Google Scholar]
- 22.Chen X, Yao Y, Hao XL, Liu XC, Liu TC. A comparative study of vitrectomy combined with internal limiting membrane peeling for the treatment of idiopathic macular hole with air or C3F8 intraocular tamponade. J Ophthalmol. 2018;2018:1672501. doi: 10.1155/2018/1672501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Özkan B, Karabaş VL, Yılmaz Tuğan B, Altıntaş Ö. Limited vitrectomy in patients with idiopathic macular hole. Balkan Med J. 2019;36(6):320–323. doi: 10.4274/balkanmedj.galenos.2019.2018.12.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehta N, Lavinsky F, Larochelle R, et al. Assessing the ability of preoperative quantitative spectral-domain optical coherence tomography characteristics to predict visual outcome in idiopathic macular hole surgery. Retina. 2021;41(1):29–36. doi: 10.1097/IAE.0000000000002797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu BS, Cui WN, Niu R, Chen Q, Nie ZT, Wei JT, Hu BJ. Refractive outcomes after vitrectomy combined with phacoemulsification of idiopathic macular holes. Int J Ophthalmol. 2021;14(2):250–254. doi: 10.18240/ijo.2021.02.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park SH, Park KH, Kim HY, Lee JJ, Kwon HJ, Park SW, Byon IS, Lee JE. Square grid deformation analysis of the macula and postoperative metamorphopsia after macular hole surgery. Retina. 2021;41(5):931–939. doi: 10.1097/IAE.0000000000002955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shukla D, Kalliath J. Internal limiting membrane peeling for large macular hole: tailoring the rhexis to the shape of the hole. Indian J Ophthalmol. 2022;70(1):182–186. doi: 10.4103/ijo.IJO_906_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hirata A, Takano A, Kawaji T, Nakamura KI. Macular pucker formation after macular hole surgery with inverted internal limiting membrane flap technique and silicone oil tamponade. Am J Ophthalmol Case Rep. 2020;19:100847. doi: 10.1016/j.ajoc.2020.100847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lam SC, Chan AYY, Yuen HKL. Extraocular silicone oil migration to orbit and retrolaminar region: case report and systematic review. Graefes Arch Clin Exp Ophthalmol. 2020;258(12):2799–2807. doi: 10.1007/s00417-020-04855-w. [DOI] [PubMed] [Google Scholar]
- 30.Chaudhary K, Mak MYK, Gizicki R, Muni RH, Wong DT, Altomare F, Berger AR. Proportion of patients with macular hole surgery who would have been favorable ocriplasmin candidates: a retrospective analysis. Retina. 2017;37(1):76–79. doi: 10.1097/IAE.0000000000001143. [DOI] [PubMed] [Google Scholar]
- 31.Wu LL, Ho TC, Yang CH, Yang CM. Vitreo-retinal relationship and post-operative outcome of macular hole repair in eyes with high myopia. Graefes Arch Clin Exp Ophthalmol. 2016;254(1):7–14. doi: 10.1007/s00417-015-2986-2. [DOI] [PubMed] [Google Scholar]
- 32.Abdul-Kadir MA, Lim LT. Update on surgical management of complex macular holes: a review. Int J Retina Vitreous. 2021;7(1):75. doi: 10.1186/s40942-021-00350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]