Abstract
AIM
To investigate the effects of school-based comprehensive intervention on myopia development in elementary school children.
METHODS
As a part of the Wenzhou Epidemiology of Refraction Error Study, there were 1524 participating elementary students (730 girls, 47.9%) in grades 1 to 3 from three campuses of one school, aged 7.3±0.9y, who were examined twice every year for a 2.5y follow up period. Comprehensive intervention and other reminders were given at school every semester for the intervention group. The control group did not receive comprehensive intervention and did not have reminders of it.
RESULTS
There were 651 students in the intervention group [mean age 7.3±0.9y; 294 (45.2%) girls] and 737 students in the control group [mean age 7.2±0.9y; 346 (46.9%) girls]. Overall mean myopia progression during the 2.5y follow-up was -0.49±1.04 diopters (D) in the intervention group and -0.65±1.08 D in the control group (P=0.004). The majority that not get myopia at baseline spherical equivalent (SE≤-1.0 D). Their mean myopia progression during the 2.5y follow-up was -0.37±0.89 D in the intervention group and -0.51±0.93 D in the control group (27.5% reduction, P=0.009); Overall, mean axial length elongation was less in the intervention group (0.56±0.32 mm) than in the control group (0.61±0.38 mm, 10.5% reduction, P=0.009). The percentage of close reading distance (<30 cm) in the intervention group was less than in the control group (73.4% vs 76.2%, P<0.001), the percentage of everyday perform eye exercises in the intervention group was more than in the control group (27.8% vs 20.7%, P<0.001) 30mo later.
CONCLUSION
The comprehensive intervention program at elementary school has a significant alleviating effect on myopia progression for children during the 2.5y follow-up, especially for those non-myopia at baseline.
Keywords: myopia progression, axial length, comprehensive intervention, school children
INTRODUCTION
Myopia is a global health problem and nearly 50% of the global population has been estimated to be affected by 2050[1]–[2]. The increasing prevalence and severity of myopia in school-age children during the last decades has become a major health problem in East Asia[1]–[5]. This increase is too rapid to be explained by genetic changes, and implies the involvement of environmental factors[3]–[10]. Thus, by modifying environmental exposure it is potentially possible to prevent or mitigate myopia onset and/or progression in children. Myopia is one of the six categories of disease prevention for schools stipulated by the 1992 Students' Common Disease Control Programme of China[11]. This program includes establishing recommendations for schoolchildren myopia control such as an eye exercise system, increased outdoor activities, the use of standardized classroom desks and chairs, and specific lighting requirements.
Many randomized controlled trials (RCTs) and epidemiological studies have reported that myopia is significantly associated with environmental factors, such as time outdoors, inadequate lighting when reading or writing, and time spent on hand-held devices and near work[1]–[7]. Results for reading posture, Chinese eye exercises, and time spent using computers have been inconsistent[12]–[15]. Only a few countries such as the Singapore have practiced health care education and screening of ocular diseases in children, with improved control of myopia progression[16]–[17].
In the Wenzhou Epidemiology of Refraction Error (WERE) study, school-based comprehensive intervention was offered to children, teachers, and parents with a 2.5y follow-up. The study aimed to evaluate the effects of comprehensive intervention on the prevention of myopia in elementary school children.
SUBJECTS AND METHODS
Ethical Approval
Ethics Committee of the Eye Hospital of Wenzhou Medical University approved this study. The study obtained permission from the parents and teachers from school. The research clung to the tenets of the Declaration of Helsinki. The nature of the study and details regarding the eye examination and questionnaire were explained to the parents and children, and informed written consent was obtained from at least one parent.
Study Design
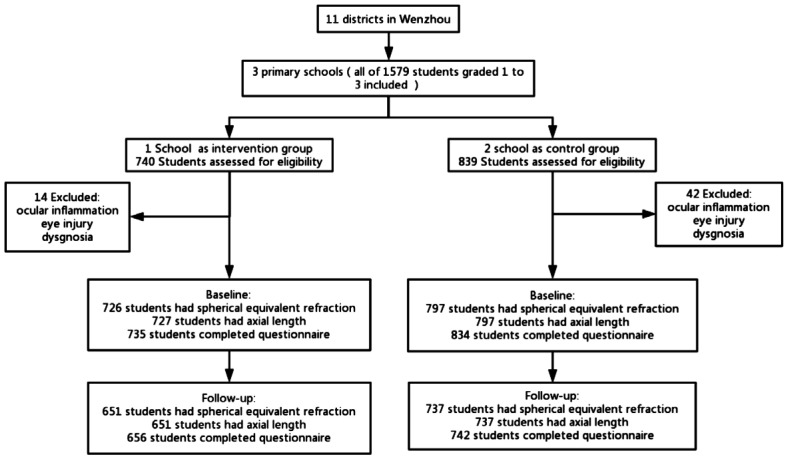
The study was a prospective, interventional school-based research in which grades 1-3 children were selected from the WERE study and followed for 2.5y (September 2012 to March 2015; Figure 1).
Figure 1. Flow chart of participant recruitment.
One school as the intervention group, two schools as the control group. These three schools were selected from the same subgroup of schools and had similar campus cultures, quality of education and socioeconomic status in their communities.
Participants
The subjects of our study were from three branch campuses of one school from Lucheng district in Wenzhou. These three branch campuses of one school had similar campus cultures, quality of education and socioeconomic status. They were in the same urban area and located in three adjacent districts less than two kilometers apart.
In total, 1579 students in grades 1-3 from these 3 campuses were eligible. Students with ocular inflammation, trauma, dysgnosia, and uncooperation (unable or unwilling to participate) behavior were excluded. At baseline, 1524 of the 1579 sampled and registered students were examined, and 1388 (87.9%) completed all the eye examinations during the 2.5y follow-up.
Comprehensive Intervention
The number of students in the one campus was approximately equal to the sum of other two. The campus with the most students was served as intervention group, whereas the other two campuses served as control group. The interventions were provided every semester to the intervention group; none was provided to the control group.
Intervention methods included education intervention and behaviour intervention. First, students, their parents and teachers received ocular health-related knowledge education, which included a powerpoint presentation, 3-D model eyes, eyeglasses, and other displays. Different ways to prevent myopia, such as correct near work related behaviours, increase outdoor activities, use standardized classroom desks and chairs, and use specific lighting were taught or adopted. Theme class meetings about ocular health were provided to every class in the intervention school at the beginning of every semester (which was approximately every 6mo). The intervention started at the beginning of October 2012. Parents and teachers were also educated on ocular health at the first semester. In addition, a handbook of ocular health prepared by the research team was issued to the children and their parents. Second, children were cultivated to develop correct near-work related behaviours. Behavioural intervention was implemented during their classes. The researchers corrected their reading posture and near-work distance. Teachers also encouraged students to go outside during class breaks.
Questionnaires
Both the intervention and control groups were asked to complete a self-administered questionnaire after theme class meetings about ocular health every semester. The questionnaire included the students' demographic characteristics, near work related behaviors (such as reading/writing distance, continuous near work time, frequency of perform eye exercises and so on), near work time and outdoor activities time. Near work time included time spent doing homework, extra-curriculum reading, video games, and computer use. Questions about time spent in outdoor activities concerned both leisure and sports. The average daily time spent on near work and outdoor activities was calculated using the formula: [(hours spent during a weekday) ×5+ (hours spent on a weekend day) ×2]/7.
The questionnaire was distributed to each class unit. Before children answered the questionnaire, researchers explained each question and instructed them how to answer it.
Eye Examinations
The participants underwent eye examinations given by 4 trained ophthalmic nurses, two experienced senior optometrists and two ophthalmic graduate students a week after theme class meetings about ocular health every semester. Visual acuity and noncycloplegic refraction were assessed each semester (6 times total), axial length (AL) was assessed annually for 2y (3 times). The autorefractor measurements were performed without cycloplegia by skilled optometrists. Each eye was measured at least three times by an autorefractor (Topcon RM8900, Topcon Co., Tokyo, Japan). Three reliable measurements were then be averaged.
IOL Master (Carl Zeiss Meditec AG, Jena, Germany) was used to measure AL. The measurements of AL were considered valid if individual measurements varied by no more than 0.02 mm. Because of difficulties in getting the IOL master on a regular basis and introducing it into the examination plan, measurement was only taken once per year. Children with best-corrected visual acuity worse than 20/25 at baseline were excluded.
Statistical Analysis
Myopia was defined as spherical equivalent (SE=spherical error+0.5×cylinder error) ≤-1.0 diopters (D). t-tests and Chi-square tests were used to compare the covariate distributions of the intervention and control groups in the descriptive analysis of baseline characteristics. Comparisons of refractive error and AL at the 2.5y follow-up in the two groups were tested by t-test. The near work activity and outdoor activity data were from the questionnaire survey conducted on the 1388 students. All P-values were based on 2-sided tests (P<0.05).
RESULTS
Baseline Measurements
During the study period, 1388 (87.9%) students were followed for 2.5y. There were 651 students in the intervention group (46.9%) and 737 (53.1%) in the control group; 45.2% in the intervention and 46.9% in the control groups were girls. The mean age was 7.3±0.9y in the intervention group and 7.2±0.9y in the control group. There were no significant differences between the intervention group and the control group in the prevalence of myopia, mean SE, and AL at baseline (Table 1).
Table 1. Baseline characteristics, spherical equivalent and axial length of the intervention and control groups.
| Variable | All children (n=1388) | Intervention group (n=651) | Control group (n=737) | P |
| Age, mean±SD (y) | 7.3±0.9 | 7.3±0.9 | 7.2±0.9 | 0.003 |
| Girls, n (%) | 640 (46.1) | 294 (45.2) | 346 (46.9) | 0.505 |
| Body mass index, mean±SD | 16.4±2.3 | 16.5±2.4 | 16.4±2.3 | 0.556 |
| Prevalence of myopia, n (%) | 190 (13.7) | 94 (14.4) | 96 (13.0) | 0.445 |
| Grade 1 | 32 (6.7) | 12 (5.9) | 20 (7.2) | 0.587 |
| Grade 2 | 73 (14.2) | 34 (14.5) | 39 (13.9) | 0.846 |
| Grade 3 | 85 (21.6) | 48 (22.3) | 37 (20.7) | 0.691 |
| SE, mean±SD (D) | -0.24±0.94 | -0.24±0.92 | -0.24±0.97 | 0.984 |
| AL, mean±SD (mm) | 23.04±0.84 | 23.06±0.82 | 23.03±0.86 | 0.449 |
| Near-work time, mean±SD (h/d) | 5.42±2.55 | 5.53±2.57 | 5.31±2.52 | 0.21 |
| Outdoor activity time, mean±SD (h/d) | 1.74±1.04 | 1.81±1.04 | 1.68±1.04 | 0.014 |
SE: Spherical equivalent; AL: Axial length.
At baseline, there were no significant differences in two groups in near work-related behaviors, the time spent on near work in the two groups was similar (P=0.210), whereas outdoor activity was slightly different (intervention group: 1.81±1.04 h/d, control group:1.68±1.04 h/d (P=0.014).
Myopia Cumulative Progression
There was a significant difference in the myopic shift in the two groups. The overall mean myopia progression during the 2.5y follow-up was -0.49±1.04 D in the intervention group and -0.65±1.08 D in the control group (P=0.004; Table 2).
Table 2. Spherical equivalent and axial length during 2.5y follow-up for the complete intervention and control groups.
| Parameters | Intervention group (n=651) | Control group (n=737) | Difference | P |
| SE, mean±SD (D) | ||||
| Baseline | -0.24±0.92 | -0.24±0.97 | 0 | 0.984 |
| 6mo | -0.34±1.01 | -0.34±1.11 | 0 | 0.990 |
| 12mo | -0.42±1.08 | -0.48±1.2 | 0.06 | 0.365 |
| 18mo | -0.50±1.24 | -0.61±1.29 | 0.11 | 0.107 |
| 24mo | -0.67±.41 | -0.74±1.52 | 0.07 | 0.395 |
| 30mo | -0.72±1.52 | -0.89±1.63 | 0.17 | 0.053 |
| Baseline to 30mo | -0.49±1.04 | -0.65±1.08 | 0.16 | 0.004 |
| AL, mean±SD (mm) | ||||
| Baseline | 23.06±0.82 | 23.03±0.86 | 0.03 | 0.449 |
| 12mo | 23.32±0.86 | 23.29±0.92 | 0.03 | 0.570 |
| 24mo | 23.62±0.94 | 23.63±0.99 | -0.01 | 0.793 |
| Baseline to 24mo | 0.56±0.32 | 0.61±0.38 | -0.05 | 0.009 |
SE: Spherical equivalent; AL: Axial length.
In the nonmyopic children at baseline, the mean increase in myopia over the 2.5y was also smaller in the intervention group (-0.37±0.89 D) than in the control group [-0.51±0.93 D; difference of 0.14 D (27.5%), P=0.009]. The 0.14 D difference indicates a 27.5% lower myopic progression rate in the intervention group (Table 3). About 70% of the relative progression reduction occurred in the last 6mo (Table 2).
Table 3. Spherical equivalent and axial length at 2.5y follow-up of children either nonmyopic or myopic at baseline in the two groups.
| Parameters | Nonmyopic at baseline (n=1198) |
Myopic at baseline (n=190) |
||||||
| Intervention group | Control group | Difference | P | Intervention group | Control group | Difference | P | |
| SE, mean±SD (D) | ||||||||
| Baseline | 0.03±0.57 | 0.04±0.53 | -0.01 | 0.698 | -1.85±0.88 | -2.13±1.06 | 0.28 | 0.051 |
| Base to 12mo | -0.15±0.50 | -0.19±0.59 | 0.04 | 0.300 | -0.33±0.95 | -0.56±0.78 | 0.23 | 0.065 |
| Base to 24mo | -0.34±0.75 | -0.38±0.83 | 0.04 | 0.362 | -0.94±1.47 | -1.25±1.34 | 0.31 | 0.133 |
| Base to 30mo | -0.37±0.89 | -0.51±0.93 | 0.14a | 0.009 | -1.13±1.49 | -1.55±1.46 | 0.42b | 0.048 |
| AL, mean±SD (mm) | ||||||||
| Baseline | 22.94±0.74 | 22.89±0.73 | 0.05 | 0.293 | 23.76±0.85 | 23.89±1.08 | -0.13 | 0.366 |
| Base to 12mo | 0.23±0.14 | 0.24±0.21 | -0.01 | 0.574 | 0.38±0.19 | 0.43±0.30 | -0.05 | 0.203 |
| Base to 24mo | 0.51±0.29 | 0.57±0.36 | -0.06c | 0.008 | 0.78±0.34 | 0.84±0.41 | -0.06d | 0.247 |
SE: Spherical equivalent, baseline to 30mo a(27.5%), b(27.1%); AL: Axial length, baseline to 24mo c(10.5%), d(0.71%).
Among the myopes at baseline, the overall mean myopia progression during the 2.5y follow-up was -1.13±1.49 D in the intervention group and -1.55±1.46 D in the control group [a difference of 0.42 D (27.1%), P=0.048; Table 3].
Change in Axial Length
The mean overall elongation of AL during the 2y follow-up in the intervention group (0.56±0.32 mm) was significantly less than in the control group (0.61±0.38 mm, P=0.009; Table 2). The difference in AL elongation was 0.06 mm in nonmyopic and in myopic at baseline children, but this difference was statistically significant only among the children who were nonmyopic at baseline. It did not reach significance in those who were myopic at baseline because the myopic at baseline group was smaller sample and had a slightly larger variance (Table 3).
Change in Near-work Factors
As expected, the percent of close reading distance (<30 cm) in the intervention group was less than in the control group (73.4% vs 76.2%, P<0.001) after comprehensive intervention (Table 4). Time spent in near work during the 2.5y follow-up decreased during the first 1.5y in the intervention group by -0.25 h/d and -0.14 h/d in the control group (P=0.020). But by 2.5y the difference was no longer significant. The intervention group spent slightly more time outdoors than the control group at baseline (1.81 h/d vs 1.67 h/d; P=0.014). But the two groups showed a similar small increase over 2.5y (difference in increase, P=0.196).
Table 4. Near-work parameters during 2.5y follow-up for the intervention and control groups.
| Near-work factor | Baseline |
30mo later |
||||
| Intervention group | Control group | P | Intervention group | Control group | P | |
| Reading/writing distance | 0.125 | <0.001 | ||||
| <30 cm | 312 (72.2) | 342 (75.7) | 408 (73.4) | 477 (76.2) | ||
| ≥30 cm | 120 (27.8) | 110 (24.3) | 148 (26.6) | 149 (23.8) | ||
| Continuous reading/writing time | 0.688 | 0.210 | ||||
| <30min | 102 (24.9) | 105 (23.8) | 46 (8.4) | 72 (11.7) | ||
| ≥30min | 307 (75.1) | 337 (76.2) | 499 (91.6) | 543 (88.3) | ||
| Continuous electronic game time | 0.293 | 0.442 | ||||
| <30min | 270 (63.2) | 269 (58.8) | 249 (46.1) | 274 (45.1) | ||
| ≥30min | 157 (36.8) | 181 (40.2) | 291 (53.9) | 334 (54.9) | ||
| Posture when hold a pen when writing | 0.757 | 0.602 | ||||
| Correct | 376 (89.7) | 403 (89.8) | 484 (87.6) | 536 (86.0) | ||
| Incorrect | 43 (10.3) | 46 (10.2) | 69 (12.5) | 87 (14.0) | ||
n (%)
DISCUSSION
Baseline Compared to Other Studies
In the present longitudinal study of Wenzhou school children, the prevalence of myopia was 6.7%, 14.7%, and 21.6% in 1st, 2nd, and 3rd grade students at baseline. It is difficult to compare these refractive prevalences to those in other locations, because of criteria and procedural differences. For example, the prevalence of myopia was 0.2%, 13.3%, and 38.8% in 1st, 2nd, and 3rd grade students in Guangzhou[3]. The slightly lower prevalence of myopia in the 1st and 2nd grade student in Guangzhou may be due to their use of cycloplegia. But then the sudden increase in myopia from grade 3 to grade 5 with little increase in higher grades is unusual and difficult to explain. Lyu et al[5] reported that the prevalence of myopia was 7.4%, 18.0%, and 28.5% in 6, 7, and 8 year old children in Chaoyang District, Beijing. Despite the use of cycloplegia, their children had a slightly higher prevalence and a slightly higher progression rate of myopia than in the Wenzhou sample. In contrast, much lower prevalences of myopia in elementary school children have been shown in many settings where educational pressures are not as great as in China[15]–[16],[18]–[20].
Treatment Effect on Myopia Progression
The present study showed a statistically significant slower progression of myopia for the intervention group in the overall sample and for the nonmyopic baseline sample. The myopic baseline group showed the same reduced progression (27%) but the smaller sample was barely significance. The 30-month myopia progression rate for the overall control sample was only -0.65 D which leaves little room for reduction (only 0.16 D) of intervention sample. Our control myopes progressed to -1.55 D and the 27% progression reduction was based on a -0.42 D reduction, which is clinically meaningful. In fact, this reduction is equal to that shown by several more invasive optical and pharmacological therapies. These other procedures induced about a 25% reduction in the first year but had almost no effect after that. Our health educational intervention started more slowly and had its strongest effect in the last half year of the program.
There is a coarse quantitative consistency between the SE refraction and AL measurements. The differences in AL progression between the intervention and control groups were small but statistically significant during the 2y. The mean 2.0-year myopia shift and elongation of AL were both smaller in the intervention group than in the control group. This is important because some studies have been questioned when they do not show a change in AL progression even though myopia progression slows[21].
Comprehensive Intervention
We suggest that long-term comprehensive intervention is useful. The intervention significantly slowed the rate of myopia progression and identified some effect on reading habits and little effect on outdoor activity and reading time.
Near work related behaviors were changed after the comprehensive Intervention. Our intervention group reported better habits included longer reading distance (≥30 cm) and perform eye exercises everyday than the control group at the end of study, even they were worse than at baseline. Near work related behaviors have been found to be associated with refractive errors in children. Another large school-based sample study among Chinese children (6-10y) reported that various near work related behaviors, included maintaining an inappropriate near work distance, selecting inadequate lighting environments and continuing to perform near work without a rest period, were risk factors for myopic progression[12]. French et al[22] reported a similar result, that the development of myopia during early childhood was affected by lifestyle and reading habits. A longer-term intervention process may be needed to help children cultivate and keep measurable healthy behavior changes that can substantially slow myopic refractive error progression.
Both the nonmyopic and myopic children at baseline showed less myopia progression by 0.14 D (0.06 D/y) for the nonmyopic children and 0.42 D (0.17 D/y) for the myopic children, than their control group over 2.5y, a 27.5% and a 27.1% reduction. So ocular comprehensive intervention was shown to be as effective as many optical or drug based procedures in other studies when children were in their lower grades and not myopic[23]. AL elongation in those who were not myopic at baseline was slower in intervention group than control group but not in those who were myopic at baseline.
Low dose atropine and OrthoK appear to be most effective in reducing myopia[24]. But one method requires parents to instill eye drops each morning and the other requires wearing contact lenses each night. These requirements may be onerous to many families. The comprehensive intervention is not as effective but is far less invasive and unpleasant than these procedures, and authors do not yet even show the best way to present this procedure. Some less onerous optical methods have been shown to be promising, and in combination with the comprehensive intervention might have a stronger effect in reducing myopia.
The comprehensive intervention appeared to have no effect on time spent performing near work including homework, reading, playing videogames, and using a computer for study. In addition, they did not increase outdoor time significantly. But as we know, these students had heavier academic loads with grade increase. Students must perform more near work due to their increased homework and extra-curricular activities in the higher grades. Previous studies have demonstrated that children of East Asian ethnicity reported spending more time in near work than children of European ethnicity[25]. Comprehensive intervention could not have an impact on time spent on near work, when the children were compelled to perform a very heavy academic load.
Interestingly, the intervention group reported slightly more time spent on outdoor activities than the control group at baseline and at the end of study. However, the amount of time spent outdoors for either group is less than usually needed to reduce myopia, and no one has ever shown that a mean difference of only 6 to 9min could produce a measurable change in myopia progression. Many studies have suggested that outdoor activity reduces myopia onset and progression[22],[26]–[28]. A cluster randomized trial of children in grade 1 reported an additional 40-minute class of outdoor activities during the school day reduced myopia progression (0.17 D)[29].
Nonetheless, the study had some potential limitations. First, this study used noncycloplegic refraction data. Gwiazda et al[30] have shown in the COMET study that noncycloplegic refractions are only 0.23 D more myopic than cycloplegic refractions. Accordingly, noncycloplegic refractometry may result in an accurate slightly higher prevalence of myopia. So the authors intend to emphasize the association between the intervention program and the myopic shift in daily life, rather than the prevalence of myopia. Secondly, the authors used a simple questionnaire, in which the data were self-reported so they would be subject to recall errors. Recall bias may have been minimized by only requesting information about the previous week.
In summary, this prospective interventional school-based study suggests that comprehensive intervention can delay the onset age of myopia in emmetropes and reduce myopia progression in myopes with a significant impact over a 2.5-year period. The procedure is not an optical or pharmacological therapy, so it can be used as the basic intervention the government can institute. In time it may be possible to recommend one or more promising optical or drug therapies for general use. The authors will attempt to identify the exact relationships between comprehensive intervention, near work habits, and refractive error in a future study.
Childhood myopia is now an increasingly important problem in China as long as ophthalmic clinicians and teachers cannot offer systematic effective health therapies and education to the children. Thus, comprehensive intervention is a potentially important measure to improve ocular health. Knowledge about a health problem and strong health consciousness are the prerequisites to incentivize healthy behavior. The present study confirms that to a modest extent a well-organized comprehensive intervention program can reduce the incidence and progression of myopia in young schoolage children.
Acknowledgments
Foundation: Supported by National Natural Science Foundation of China (No.81873683).
Conflicts of Interest: Jiang DD, None; Chen J, None; Thorn F, None; Mao GY, None; Li CC, None; Lin Z, None; Vasudevan B, None; Huang XQ, None; Chen YY, None.
REFERENCES
- 1.Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379(9827):1739–1748. doi: 10.1016/S0140-6736(12)60272-4. [DOI] [PubMed] [Google Scholar]
- 2.Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 3.Guo L, Yang J, Mai J, Du X, Guo Y, Li P, Yue Y, Tang D, Lu C, Zhang WH. Prevalence and associated factors of myopia among primary and middle school-aged students: a school-based study in Guangzhou. Eye (Lond) 2016;30(6):796–804. doi: 10.1038/eye.2016.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsai DC, Fang SY, Huang N, Hsu CC, Chen SY, Chiu AWH, Liu CJL. Myopia development among young schoolchildren: the myopia investigation study in Taipei. Invest Ophthalmol Vis Sci. 2016;57(15):6852–6860. doi: 10.1167/iovs.16-20288. [DOI] [PubMed] [Google Scholar]
- 5.Lyu Y, Zhang H, Gong Y, Wang D, Chen T, Guo X, Yang S, Liu D, Kang M. Prevalence of and factors associated with myopia in primary school students in the Chaoyang District of Beijing, China. Jpn J Ophthalmol. 2015;59(6):421–429. doi: 10.1007/s10384-015-0409-x. [DOI] [PubMed] [Google Scholar]
- 6.Matamoros E, Ingrand P, Pelen F, Bentaleb Y, Weber M, Korobelnik JF, Souied E, Leveziel N. Prevalence of myopia in France: a cross-sectional analysis. Medicine (Baltimore) 2015;94(45):e1976. doi: 10.1097/MD.0000000000001976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams KM, Bertelsen G, Cumberland P, et al. Increasing prevalence of myopia in Europe and the impact of education. Ophthalmology. 2015;122(7):1489–1497. doi: 10.1016/j.ophtha.2015.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galvis V, Tello A, Camacho PA, Parra MM, Merayo-Lloves J. Bio-environmental factors associated with myopia: an updated review. Arch De La Sociedad Española De Oftalmol Engl Ed. 2017;92(7):307–325. doi: 10.1016/j.oftal.2016.11.016. [DOI] [PubMed] [Google Scholar]
- 9.Morgan IG, Rose KA. Myopia: is the nature-nurture debate finally over? Clin Exp Optom. 2019;102(1):3–17. doi: 10.1111/cxo.12845. [DOI] [PubMed] [Google Scholar]
- 10.Zadnik K, Mutti DO. Who says there's nothing new under the Sun? Optom Vis Sci. 2015;92(11):e392–e393. doi: 10.1097/OPX.0000000000000753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Regulations of the ministry of health of the People's Republic of China (No.1)—school hygiene work. http://www.moh.gov.cn/publicfiles/business/htmlfiles/mohwsjdj/s3584/200804/16491.htm.
- 12.You X, Wang L, Tan H, He X, Qu X, Shi H, Zhu J, Zou H. Near work related behaviors associated with myopic shifts among primary school students in the Jiading District of Shanghai: a school-based one-year cohort. PLoS One. 2016;11(5):e0154671. doi: 10.1371/journal.pone.0154671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xiong SY, Sankaridurg P, Naduvilath T, Zang JJ, Zou HD, Zhu JF, Lv MZ, He XG, Xu X. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017;95(6):551–566. doi: 10.1111/aos.13403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Low W, Dirani M, Gazzard G, Chan YH, Zhou HJ, Selvaraj P, Au Eong KG, Young TL, Mitchell P, Wong TY, Saw SM. Family history, near work, outdoor activity, and myopia in Singapore Chinese preschool children. Br J Ophthalmol. 2010;94(8):1012–1016. doi: 10.1136/bjo.2009.173187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin Z, Vasudevan B, Jhanji V, Mao GY, Gao TY, Wang FH, Rong SS, Ciuffreda KJ, Liang YB. Near work, outdoor activity, and their association with refractive error. Optom Vis Sci. 2014;91(4):376–382. doi: 10.1097/OPX.0000000000000219. [DOI] [PubMed] [Google Scholar]
- 16.Robaei D, Kifley A, Rose KA, Mitchell P. Refractive error and patterns of spectacle use in 12-year-old Australian children. Ophthalmology. 2006;113(9):1567–1573. doi: 10.1016/j.ophtha.2006.02.066. [DOI] [PubMed] [Google Scholar]
- 17.Seet B. Myopia in Singapore: taking a public health approach. Br J Ophthalmol. 2001;85(5):521–526. doi: 10.1136/bjo.85.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang LL, Dalal K, Yin MM, Yuan DG, Andrews JY, Wang SM. The KAP evaluation of intervention on fall-induced injuries among elders in a safe community in Shanghai, China. PLoS One. 2012;7(3):e32848. doi: 10.1371/journal.pone.0032848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yan F, Zhi-wei X, Dan X, Jian L. Analysis on effect of KAP intervention and its influencing factors among female sex workers. Chinese Journal of Disease Control & Prevention. 2007(06):544–547. [Google Scholar]
- 20.Jianming G, Yuming L, Peizhen H, Qin X. Effect of health education intervention on myopia among primary and middle school students in Guangzhou City. Chin J School Doctor. 2010;24(12):906–908. [Google Scholar]
- 21.Fu AC, Chen XL, Lv Y, Wang SL, Shang LN, Li XH, Zhu Y. Higher spherical equivalent refractive errors is associated with slower axial elongation wearing orthokeratology. Cont Lens Anterior Eye. 2016;39(1):62–66. doi: 10.1016/j.clae.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 22.French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian schoolchildren. Ophthalmology. 2013;120(10):2100–2108. doi: 10.1016/j.ophtha.2013.02.035. [DOI] [PubMed] [Google Scholar]
- 23.Gwiazda JE, Hyman L, Norton TT, Hussein MEM, Marsh-Tootle W, Manny R, Wang Y, Everett D, Group COMET Accommodation and related risk factors associated with myopia progression and their interaction with treatment in COMET children. Invest Ophthalmol Vis Sci. 2004;45(7):2143–2151. doi: 10.1167/iovs.03-1306. [DOI] [PubMed] [Google Scholar]
- 24.Huang JH, Wen DZ, Wang QM, et al. Efficacy comparison of 16 interventions for myopia control in children. Ophthalmology. 2016;123(4):697–708. doi: 10.1016/j.ophtha.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 25.Cook A, White S, Batterbury M, Clark D. Ocular growth and refractive error development in premature infants with or without retinopathy of prematurity. Invest Ophthalmol Vis Sci. 2008;49(12):5199–5207. doi: 10.1167/iovs.06-0114. [DOI] [PubMed] [Google Scholar]
- 26.Wu PC, Tsai CL, Hu CH, Yang YH. Effects of outdoor activities on myopia among rural school children in Taiwan. Ophthalmic Epidemiol. 2010;17(5):338–342. doi: 10.3109/09286586.2010.508347. [DOI] [PubMed] [Google Scholar]
- 27.Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, Mitchell P. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115(8):1279–1285. doi: 10.1016/j.ophtha.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 28.Jin JX, Hua WJ, Jiang X, Wu XY, Yang JW, Gao GP, Fang Y, Pei CL, Wang S, Zhang JZ, Tao LM, Tao FB. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: the Sujiatun Eye Care Study. BMC Ophthalmol. 2015;15:73. doi: 10.1186/s12886-015-0052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.He MG, Xiang F, Zeng YF, Mai JC, Chen QY, Zhang J, Smith W, Rose K, Morgan IG. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314(11):1142–1148. doi: 10.1001/jama.2015.10803. [DOI] [PubMed] [Google Scholar]
- 30.Gwiazda J, Norton TT, Hou W, Hyman L, Manny R, Group COMET Longitudinal changes in lens thickness in myopic children enrolled in the correction of myopia evaluation trial (COMET) Curr Eye Res. 2016;41(4):492–500. doi: 10.3109/02713683.2015.1034372. [DOI] [PMC free article] [PubMed] [Google Scholar]