Abstract
This case involves a patient with severe COVID-19 pneumonia and massive pulmonary embolism requiring mechanical ventilation. His clinical course was complicated by delirium likely triggered by his critical illness and failed initial extubation, isolation from family, and escalating fear and desperation. In hopeful preparation for subsequent successful extubation, a unique approach was taken to decrease the risk of panic, delirium, and decompensation leading to reintubation. As a means of orienting him to his treatment pathway and to provide encouragement for continued recovery, an impromptu patient-directed checklist was constructed. The recovery checklist, written in simplified language, outlined the stages of severe illness that the patient had overcome after his emergent intubation. The list also outlined the tasks he needed to complete prior to hospital discharge. Unexpectedly, the checklist received a great deal of engagement from both the patient and medical team and played an important role in this patient’s successful recovery and rehabilitation.
Keywords: anxiety, COVID, disease management, health outcomes, managed care, patient-centeredness, prevention, quality improvement, education
Background
COVID-19, caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), creates a variable clinical picture ranging from asymptomatic to severe respiratory failure and death. Respiratory failure is thought to be caused by altered lung perfusion secondary to pulmonary edema and atelectasis which may lead to irreversible structural lung damage. Additionally, SARS-CoV-2 appears to cause extensive alterations to the clotting mechanisms in the body—a topic still under intense investigation. 1 Severity of illness often necessitates intensive care unit (ICU) cares for COVID-19 pneumonia patients, with some patients requiring mechanical ventilatory support. Medical care in the ICU often involves sedatives, paralytics, and other psychoactive medications in concordance with life preserving medical treatments; however, these interventions also lead to an increased risk of delirium. 2
Delirium is a well-recognized contributor to intensive care unit (ICU) morbidity and mortality, affecting up to 80% of ICU patients and resulting in longer hospital stays and a higher 6-month mortality rate. 2 The DSM-V has defined delirium as a “disturbance in attention and awareness” which develops over a “short period of time” with a “disturbance in cognition.” This may present quickly and may involve a combination of disorientation, memory deficit, and perception disturbances. 3 In an effort to improve ICU outcomes by specifically targeting delirium the “ABCDEF Bundle” has been developed and utilized internationally. This bundle includes pain management, awakening and breathing trials, considerations in medication use for pain and sedation, delirium assessment and management, early mobility and family and patient and engagement. 4
Though the ability to provide patient engagement and education in complex illness recovery is limited in the acute ICU setting, finding a means of giving a better understanding of invasive treatments may enable more patient autonomy. Some have defined patient education in other care models as “the empowering process that. . . not only provides information to the patients but also leads them to an interpretation of their own preferences.” 5
Patient and family engagement, through an educational checklist, was the impromptu intervention in this case. Checklists are commonly used as a means of breaking down information into sizable achievements in everyday life; utilizing a checklist format for a patient engagement and education tool may enhance aspects of recovery and provide motivation to press forward through difficult stages of illness. How education may impact delirium, hospital course, and the ongoing recovery challenges remain to be explored.
The essential goal of our patient case was “recover and return home.” Unfortunately, even when recovery is achieved, the care during critical illness often results in significant survivorship trauma. Challenges include deficits in function, cognition and mental health for months to years.6,7 These are significant aspects of health that need attention as the paths of primary care and critical care converge. How the medical team’s communication during critical illness affect outcomes of survivorship of critical or serious illness has yet to be explored systematically.
To understand the direct patient impact of these cares, we incorporate the voice of our patient. Prior report of patient voice in scientific literature has been shared in regard to the “Get to Know Me” board, a means of sharing personal details of the patient to enhance humanism in medicine. 8 Another patient shared his reflections of “delirium” in the Journal of the Intensive Care Society. 9 Incorporating patient views in scientific literature may bear great significance for building more meaningful patient centered outcomes over binary outcomes of mortality and hospital length of stay.
Case Presentation
Here we present a case of a middle-aged father, husband, and active community member. He was diagnosed with COVID-19 pneumonia by PCR testing; his initial symptoms included fatigue, fever, and cough a week before hospitalization for progressive hypoxia. On admission to hospital, he made a steady recovery with Hi-Flow oxygen and COVID-19 directed therapies. However, several days into his hospitalization he experienced sudden respiratory failure with oxygen saturations in the low 60’s. He was emergently intubated and transferred to the ICU. This case focuses on his ICU course where he was cared for by a team of multiple veteran critical care attending physicians, fellows, resident physicians from internal and family medicine, nurses, and care aids.
His rapid clinical decompensation was due to massive (resulting in severe cardiac strain) bilateral pulmonary emboli which necessitated mechanical ventilatory support and emergent thrombolytic therapy. The combination of severe COVID-19 pneumonia, superimposed ventilator associated bacterial pneumonia, acute heart failure caused by the pulmonary emboli, renal failure, and bacteremia created an extremely fragile clinical scenario.
His clinical course steadily improved, and he was ready for extubation on the fifth day of his ICU admission. Due to the emergent intubation and sedation, he had no comprehensible memory of the days leading to this extubation, and no means of explaining his current medical condition which included substantial muscle atrophy, a great number of support lines and tubes, and disconcerting machine support surrounding his hospital bed. Throughout that day, he showed increasing levels of anxiety and delirium, evidenced both by vital measurements and his Richmond Agitation Sedation Scale (Table 1) that wavered from −1 to +1. 10 Due to escalating delirium, he developed aggressive behaviors and subsequently struggled to remove his lines and catheters. After extensive attempts at supportive care by the medical team, medication targeting delirium and anxiety, and reorientation with the help of his wife, his agitation and delirium caused a decline in respiratory status. Approximately 20 h after his initial extubation, he required re-intubation with increased sedation, paralysis, proning, attention to ventilator dyssynchrony causing trauma to his lungs, and treatment of ventilator-associated pneumonia and systemic bacteremia.
Table 1.
Richmond Agitation Severity Scale (RASS) Score breakdown. 10
| Score | Term | Description |
|---|---|---|
| +4 | Combative | Overtly combative or violent; immediate danger to staff |
| +3 | Very agitated | Pulls on or removes tube(s) or catheter(s) or has aggressive behavior toward staff |
| +2 | Agitated | Frequent nonpurposeful movement or patient–ventilator dyssynchrony |
| +1 | Restless | Anxious or apprehensive but movements not aggressive or vigorous |
| 0 | Alert and calm | |
| −1 | Drowsy | Not fully alert, but has sustained (more than 10 s) awakening, with eye contact, to voice |
| −2 | Light sedation | Briefly (less than 10 s) awakens with eye contact to voice |
| −3 | Moderate sedation | Any movement (but no eye contact) to voice |
| −4 | Deep sedation | No response to voice, but any movement to physical stimulation |
| −5 | Unarousable | No response to voice or physical stimulation |
Communication with his family had occurred daily by telephone since his admission to the medical intensive care unit. This initially included updates on his condition and efforts to understand the patient better with the use of the “Get to Know Me” board. 8 During the day of reintubation, additional communications were required to understand the source of his panic and to develop customized preventative measures for delirium. Per his wife, the patient appreciated knowing specific steps in completion of tasks in everyday life; he would often make his own personalized checklists to avoid becoming overwhelmed. It was thought that his lack of understanding in regards to his medical care likely contributed to his worsening panic and delirium.
In order to orient him to his medical cares, a customized checklist (Figure 1) was developed by a family medicine resident rotating in the ICU, with the hope that checking off completed items would help educate and motivate the patient. In addition to adding personalized future recovery goals, items were added that had already been achieved early in his ICU course while he was sedated.
Figure 1.
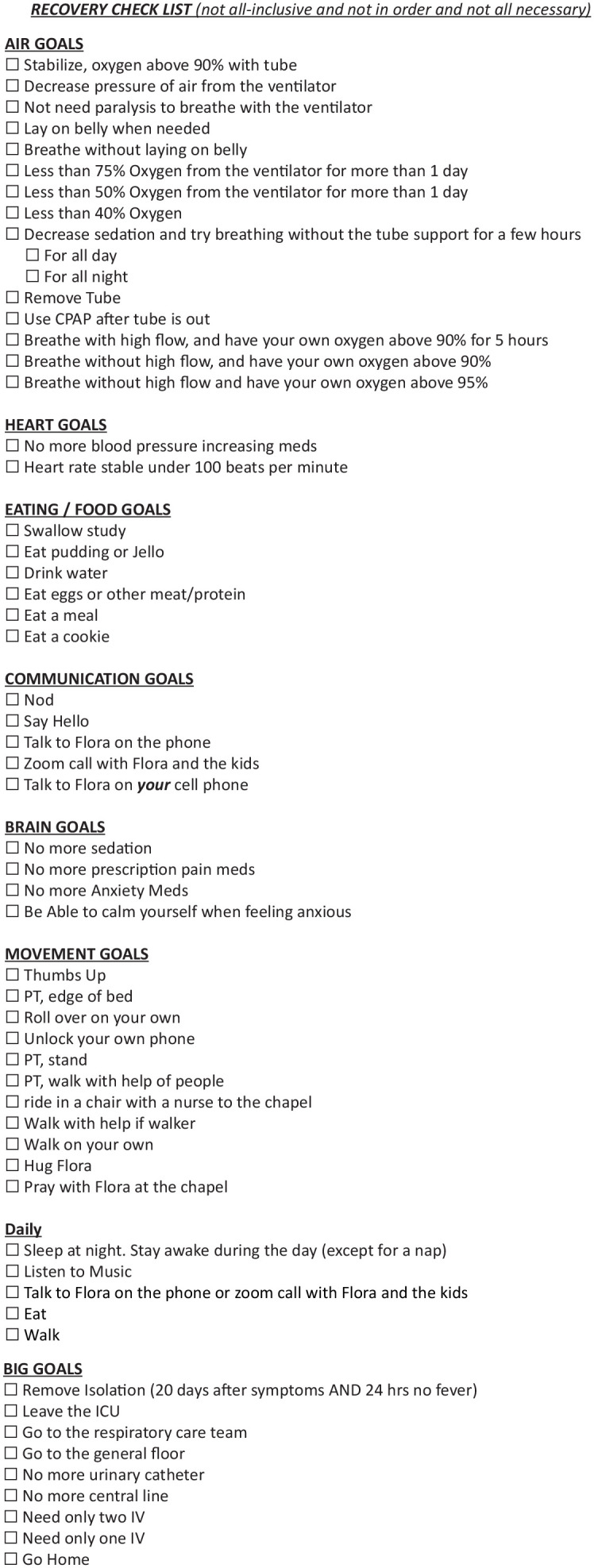
The checklist as written for the patient presented in this case.
During the days following his re-intubation, the entire ICU team voluntarily checked items off the checklist while the patient was sedated. Several handwritten achievements were also added to the list by nursing staff, such as “pressing the call light.” There were reports that the staff practiced reassuring communication even while the patient was intubated and sedated, telling him what he had accomplished from the checklist that day.
Five days after his re-intubation, he was ready to be extubated again. In the hours following extubation, he repeatedly requested to review the checklist, focusing intensely on the respiratory achievements leading up to his successful extubation. There were no comments of hopelessness or entrapment as had occurred previously; there was minimal evidence of confusion. He remained calm, showed only mild intermittent anxiety, and delirium was absent. His illness steadily improved, and he was discharged to the general floor 30 h following his successful extubation. At the patient’s request, the checklist was brought down to the general floor and his post-hospital rehab facility, where he continued to utilize it daily with the additional help of his wife once isolation was discontinued. About 59 days after initial symptoms developed, the patient was discharged from his rehabilitation facility, he returned home with a great deal of his physical health regained and the likely achievable goal of full recovery.
PATIENT PERSPECTIVE- by Joel Emilio, Esq (patient); Editing by Sumera Ahmad, MD; and Ashley Stantz, MD for clarity.
I had just learned a few days prior that I had tested positive for COVID when a telehealth nurse recommended I go into the clinic for a chest x-ray. When the staff saw that I was struggling to catch my breath I was transferred from my smaller local emergency department to another hospital.
The message that I heard was consistent: they were going to treat me with remdesivir and provide me oxygen. I had the expectation that I could be discharged in a little more than a week once the virus was gone. About 4 days after I was admitted, I felt like I couldn’t catch my breath and began to panic. I was surrounded by doctors and nurses who were preparing to transfer me to the ICU. I remember hearing them say they needed to “intubate” me.
While I was on the ventilator my consciousness wandered between sleep and briefly waking from time to time. I remember being in a great deal of pain and having a lot of horrifying dreams. Unlike most dreams I’ve had in my life, I couldn’t wake or figure out if I was even still alive. I remember having hallucinations that I couldn’t escape from, and the pain and confusion that wouldn’t subside.
I know that I woke up and was briefly taken off the ventilator. The people I saw consistently were the same people I started not to trust. My nurses were associated with the pain and confusion I was feeling. I doubted whether I was still alive and at one point I mentioned that I must have been “in hell” because time was not moving, my pain was constant, and I had lost all hope that I could beat whatever it was I was up against. The understanding of my COVID infection had gone at that point. I was confused and hopeless.
I remember waking up in a propped-up position and being attended to by a nurse. I had an intuition where I was at a tipping point between life and death. I remember thinking that I had to stay awake as long as possible because of my fear about what was waiting for me if I fell asleep again.
My doctor made sure to inform me why I was there and what had happened to me. She asked me to repeat a few times that I was very sick with COVID and that it had caused me to develop blood clots in my lungs and heart. It was the first time I had felt like I had some kind of understanding, but I was not completely trusting the situation.
Both my doctor and nurse were very optimistic that I was starting to stabilize and made sure to emphasize the milestones I had reached. It was at that time they drew my attention to a checklist they had taped to the wall. They took the time to show me all the steps I needed to take in order to get where I wanted to go—“back home again.” Even though it made sense to me, I didn’t trust still.
Then my doctor started showing me the things that were happening back home and what was waiting for me in great detail. These details made me realize I wasn’t making this up in my head. This helped me understand that I was still alive. I started trusting my doctors and nurses. It took me a while to get my full faculties back and I had my ups and downs in the hospital while I was recovering. I remember asking my attendants to continue to read the checklist to me to make sure it was still real.
The mental and emotional toll that I went through had to be the greatest challenge I’ve ever experienced. I cannot overstate how important it was for me to be able to see something tangible, to hear in great detail my condition and my path to getting home, and also what was waiting for me at home.
Discussion
As is increasingly common in the era of COVID-19, there is a need for unconventional and creative interventions to tackle unclear and often poorly understood problems which arise during patient care. There are minimal studies on the benefits of patient education in the ICU; none of these studies appear to directly invite the patient to take an active part in their understanding of the recovery process.
Through this checklist, the ICU team implemented an approach toward patient and family engagement through education and active participation. This was individualized to our patient with the critical illness from COVID-19. While we adhered to the hospital policy of visitor restriction, family discussions over the telephone enabled knowing the patient as a person, which allowed us to address his specific needs. As expected, his critical illness was compounded with periods of delirium, agitation, and decompensation before he improved. The checklist helped our patient engage in personally meaningful goals of recovery, which motivated him to participate actively in a challenging recovery. The use of a checklist could possibly help overcome patient communication and educational barriers for those hospitalized with complex illness outside of the realm of the COVID-19 pandemic.
The medical condition most greatly affected by the checklist appears to have been the patient’s delirium, as seen by the resolution and absence of delirium when the checklist was implemented. As previously mentioned, there are active strategies that aim to improve patient outcomes and reduce the occurrence of delirium, which is known to cause increased morbidity and mortality. An additional measure to consider would be the addition of a “G” to the ABCDEF bundle, adding patient-focused “Goals” to the bundle to incorporate milestones of recovery. 4
There are concerns with the use of a checklist. Time, a precious and limited commodity in the ICU, is needed to customize a list for each patient. For example, individualized achievements for this patient include hugging his wife, visiting the hospital chapel, and speaking with his children on his own phone; as noted in his perspective, these were crucial to his recovery. However, there is a benefit to understanding the personal aspects of a patient’s life for both the patient and team caring for them. 8 There is also a concern for the mental wellbeing of a patient who regresses or declines, thus losing previously achieved tasks. This may cause a sense of defeat or failure; however, this evidence of decline may also provide an introduction for changing goals of care (ie, end of life discussions). Finally, in studying the benefits of a checklist, a measurable assessment needs to be developed. While vitals and the Richmond Agitation Sedation Scale noted in this case report are valuable clues to the patient’s overall health, they are not specific for a delirium diagnosis and they are easily confounded by the non-delirium aspect of a patient’s illness.11 -14
Conclusion
There continues to be immense value in creativity and ingenuity in medicine, as in the unique idea of a checklist often developed through an outside perspective such as the family medicine resident developing a checklist while rotating in an ICU. This checklist appears to have helped remarkably well according to this single patient and may have benefit to a great many more patients in the future. Additionally, this case reaffirmed that understanding and individualizing a patient’s care is highly valuable, providing understanding of their humanity and enabling genuine compassion and connection. Finally, understanding their own medical illness with specific goals for recovery may greatly help patients overcome the psychological strain of critical conditions. This understanding may also benefit the patients’ families and loved ones.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Ashley Stantz  https://orcid.org/0000-0003-1815-4174
https://orcid.org/0000-0003-1815-4174
Gregory Garrison  https://orcid.org/0000-0001-6903-4610
https://orcid.org/0000-0001-6903-4610
Christopher Boswell  https://orcid.org/0000-0002-9034-3415
https://orcid.org/0000-0002-9034-3415
References
- 1. Gattinoni L, Gattarello S, Steinberg I, et al. COVID-19 pneumonia: pathophysiology and management. Eur Respir Rev. 2021;30(162):210138. doi: 10.1183/16000617.0138-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brummel NE, Jackson JC, Pandharipande PP, et al. Delirium in the ICU and subsequent long-term disability among survivors of mechanical ventilation. Crit Care Med. 2014;42(2):369-377. doi: 10.1097/CCM.0b013e3182a645bd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 4. Pun BT, Balas MC, Barnes-Daly MA, et al. Caring for critically ill patients with the ABCDEF bundle: results of the ICU Liberation Collaborative in over 15,000 adults. Crit Care Med. 2019;47(1):3-14. doi: 10.1097/CCM.0000000000003482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reach G. Patient autonomy in chronic care: solving a paradox. Patient Prefer Adherence. 2013;8:15-24. doi: 10.2147/PPA.S55022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Eakin MN, Patel Y, Mendez-Tellez P, Dinglas VD, Needham DM, Turnbull AE. Patients’ outcomes after acute respiratory failure: a qualitative study with the PROMIS framework. Am J Crit Care. 2017;26(6):456-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dziadzko V, Dziadzko MA, Johnson MM, Gajic O, Karnatovskaia LV. Acute psychological trauma in the critically ill: patient and family perspectives. Gen Hosp Psychiatry. 2017;47:68-74. [DOI] [PubMed] [Google Scholar]
- 8. Gajic O, Anderson BD. “Get to know me” board. Crit Care Explor. 2019;1(8):e0030. doi: 10.1097/CCE.0000000000000030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Garrett RM. Reflections on delirium – a patient’s perspective. J Intensive Care Soc. 2019;20(3):258-262. doi: 10.1177/1751143719851352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond agitation-sedation scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338-1344. doi: 10.1164/rccm.2107138 [DOI] [PubMed] [Google Scholar]
- 11. Brummel NE, Girard TD. Preventing delirium in the intensive care unit. Crit Care Clin. 2013;29(1):51-65. doi: 10.1016/j.ccc.2012.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Colombo R, Corona A, Praga F, et al. A reorientation strategy for reducing delirium in the critically ill. Results of an interventional study. Minerva Anestesiol. 2012;78(9):1026-1033. [PubMed] [Google Scholar]
- 13. Hwang SL, Chang Y, Ko WJ, Lee MB. Stress-reducing effect of physician’s tape-recorded support on cardiac surgical patients in the intensive care unit. J Formos Med Assoc. 1998;97(3):191-196. [PubMed] [Google Scholar]
- 14. Lewis SR, Pritchard MW, Schofield-Robinson OJ, Evans DJ, Alderson P, Smith AF. Information or education interventions for adult intensive care unit (ICU) patients and their carers. Cochrane Database Syst Rev. 2018;10(10):CD012471. doi: 10.1002/14651858.CD012471.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]


