Abstract
Purpose
This report describes a case of conjunctival chronic lymphocytic leukemia (CLL) in a 73 year-old female with a prior history of CLL thought to be in remission who presented with bilateral chronic conjunctivitis.
Observation
Examination revealed bilateral conjunctival injection, mildly purulent discharge, and the presence of large follicle-like lesions involving the bilateral superior and inferior palpebral conjunctiva. Conjunctival cultures grew Corynebacterium species. The patient was treated with topical antibiotics and steroids which improved the conjunctival injection and discharge, but the follicle-like lesions persisted. A conjunctival biopsy was performed and was consistent with the diagnosis of chronic lymphocytic leukemia. Fundoscopic exam did not demonstrate posterior uveal or retinal involvement. She was referred to her oncologist for further evaluation and management. Marked clinical improvement was noted after starting treatment with ibrutinib.
Conclusions and importance
This case demonstrates a rare ocular manifestation of the most common form of leukemia. It happened to present with common, nonspecific symptoms of eye redness, discharge, and follicular reaction consistent with a bilateral chronic conjunctivitis. Clinical appearance and symptoms improved with topical steroids and eventually resolved with systemic bruton kinase inhibitor therapy.
Keywords: Conjunctiva, Chronic lymphocytic leukemia, Conjunctivitis
1. Introduction
In this report we discuss a case of conjunctival chronic lymphocytic leukemia (CLL) in a patient with a history of CLL thought to be in remission who presented with bilateral chronic conjunctivitis. CLL is the most common form of leukemia in the Western world.1 Diagnosis requires an absolute clonal lymphocyte count of 5.0 × 109 cells/L or more and a specific immune-phenotype, determined by flow cytometry. Lymphocytes often express CD19, CD20, CD23, and CD5. Imaging and lymph node biopsies are not required for diagnosis.1 Small lymphocytic lymphoma (SLL) is a manifestation of the same disease in which cells predominantly infiltrate lymph nodes and other tissues and spare the peripheral blood and bone marrow. Treatment is not required unless the patient develops symptoms or severe cytopenia.1 For patients requiring treatment, there are a variety of effective and well tolerated treatment options including alkylating agents, purine analogs, anti-CD20 monoclonal antibodies, and bruton tyrosine kinase inhibitors.2
Ocular involvement in leukemias may be due direct infiltration or secondary to anemia or thrombocytopenia, hyper-viscosity, or the patient's immunocompromised state. Ocular involvement in CLL is rare.3,4 In one prospective case series examining ocular involvement in CLL, there was no association between ocular involvement and hematologic parameters or disease stage.3
The conjunctiva is a critical site for initiating and regulating the immune response of the ocular surface and contains T and B lymphocytes in the epithelium and lymphoid follicles in the stroma. The lymphatic vessels drain into the preauricular and submandibular lymph nodes. While conjunctival involvement of leukemias is rare, the conjunctiva is unsurprisingly an important site of extra-nodal lymphoma development, with approximately 15% of extra-nodal lymphomas involving the ocular adnexa and 25–30% of these cases involving the conjunctiva.5
2. Case presentation
The patient is a 74 year-old Asian woman with a history of right sphenoid wing meningioma status-post resection complicated by bilateral ischemic optic neuropathy and chronic lymphocytic leukemia (CLL) thought to be in remission who presented in with complaints of bilateral ocular redness, irritation, and discharge. Visual acuities were 20/150 in the right eye and 20/80 in the left eye. Right eye vision was worse than baseline of 20/40 and left eye was at baseline. Slit lamp examination revealed bilateral conjunctival injection, mildly purulent discharge, and the presence of large follicle-like lesions involving the superior and inferior palpebral conjunctiva. The remainder of the examination, including dilated fundus examination, was unremarkable, with the exception of mild optic disc pallor in both eyes which was stable from previous documentation. She was diagnosed with CLL in 2013 after a lymphocytic leukocytosis (17.5 × 109 cells/L, 69% lymphocytes) was noted incidentally on a routine complete blood cell count. Cells expressed ZAP70 and PAX5; flow cytometry demonstrated expression of CD19, CD20, CD21, CD22, CD23, CD5, and CD52+, with partial expression of CD11c.
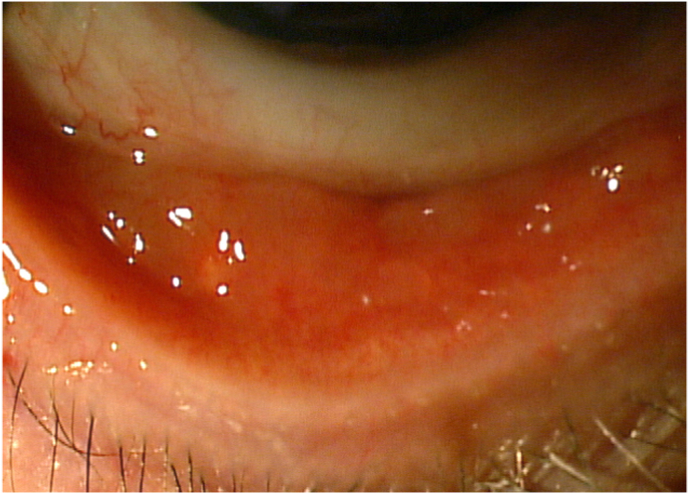
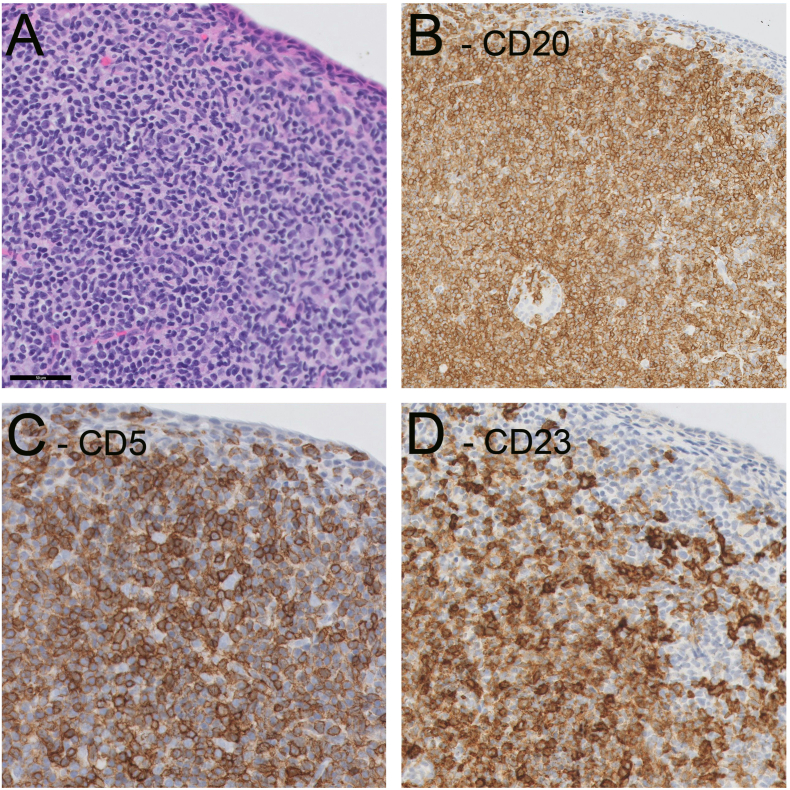
Conjunctival cultures were obtained and the patient was started on topical antibiotics (moxifloxacin 0.5% QID) and steroids (prednisolone acetate 1% QID). The culture was positive for Corynebacterium species; the patient's conjunctival injection and discharge soon resolved and vision improved. However, the follicle-like lesions persisted (Fig. 1). Seven weeks following presentation, a conjunctival biopsy specimen was sent in formalin from the right inferior palpebral conjunctiva. The hematoxylin and eosin stain revealed a heterogeneous lymphocytic infiltrate with small to medium-sized cells with variable nuclei, primarily involving the conjunctival substantia propria, but also with patchy involvement of the epithelium. Immunostaining revealed dim, aberrant CD5 staining as well as strong CD23 staining within CD20-positive B cells, which was consistent with a diagnosis of conjunctival CLL (shown in Fig. 2).1
Fig. 1.
Photograph demonstrating inferior palpebral conjunctival injection and follicle-like lesions.
Fig. 2.
Conjunctival biopsy results. Measurement standard bar is located in box A and is equal to 50 μm. A) Hematoxylin-eosin staining demonstrates heterogeneous lymphocytic infiltrate with sheets of small to medium-sized cells with variably rounded and angulated nuclei primarily involving the substantia propria. B) CD20 immunostaining reveals diffuse population of B cells. C) CD5 demonstrates strong membranous staining of T cells and dim staining of B cells. D) CD23 stains B cells and matches pattern of CD20 staining which is consistent with chronic lymphocytic leukemia. Images courtesy of Dr. Peter Pytel.
We referred the patient for evaluation by her oncologist as well the retina service. Retinal evaluation did not reveal any relevant posterior segment pathology, such as posterior uveal infiltration or retinal infiltration. She was initially diagnosed with CLL in 2013 after incidental leukocytosis was noted on routine blood testing. Her disease was indolent and she had not undergone chemotherapy. Oncology pursued a systemic work-up including a complete blood count with differential. At the time the patient was not experiencing fever, chills, night sweats, or unintentional weight loss. Given a rising white blood cell (WBC) count (50.1 × 109 cells/L from 40 × 109 cells/L), she was re-enrolled in a trial for treatment with quercetin. Quercetin is a naturally occurring flavonoid and commercially available dietary supplement that inhibits many protein kinases, including PIM1 kinase expressed on cells in CLL. In one small trial it was demonstrated to stabilize cell counts in patients with CLL.6 Approximately 10 months following the initial presentation, she experienced worsening of conjunctival CLL symptoms in the left eye and decreased vision to 20/200. Her oncologist recommended initiating treatment with a bruton's tyrosine kinase inhibitor, ibrutinib, for these symptoms. The frequency of topical prednisolone 1% was also increased to BID from every other day in the left eye. The ocular symptoms were controlled with eventual resolution of conjunctival lesions. Visual acuity was restored to baseline. The prednisolone was tapered to every other day. The patient self-discontinued the steroids two years following initial presentation and remains asymptomatic. She continues to be followed on an outpatient basis and also underwent bilateral cataract extraction.
3. Discussion
Ocular involvement of CLL/SLL and conjunctival CLL/SLL are relatively rare, although the true incidence is unknown due to descriptions in the literature being limited to case reports and series.3,4,7,8 To our knowledge, this the first reported case of conjunctival infiltration of CLL. Although the role of the conjunctiva in regulating the immune response of the ocular surface is still an area of investigation, it is perhaps unsurprising that this malignancy can present in a tissue rich with lymphocytes. The patient's known history of CLL was key for guiding the workup and histopathologic diagnosis, which reinforces the importance of reviewing a patient's full medical history in an ophthalmologic evaluation. Presenting symptoms of conjunctival injection, conjunctival follicles and mild discharge are nonspecific. Although a conjunctival biopsy was anticipated, the presence of a mildly purulent conjunctivitis at the time of initial presentation necessitated ruling out an infectious etiology, as a conjunctival biopsy in the presence of an active infection could lead to subconjunctival spread of an infectious microorganism.
There is no established local chemotherapy regimen for conjunctival CLL but the inflammation was quelled with chronic topical steroids. CLL is a chronic disease and treatment is pursued when patients are symptomatic from lymphadenopathy or the disease progresses to cause severe cytopenia. The ocular manifestation of this patient's CLL did impact her treatment as she was eventually started on systemic chemotherapy by her oncologist due to worsening ocular involvement and visual symptoms. The treatment with ibrutinib was effective. Several months after starting ibrutinib, the patient was noted to have more improvement in her ocular symptoms and clinical appearance compared to topical steroids alone or topical steroids and quercetin.
Patient consent
The patient provided written consent to publish this case including the use of images.
Funding sources
The authors did not receive any funding in relation to this manuscript.
Authorship
Farida Hakim, MD reviewed the case details and wrote the initial draft of the manuscript. Asim V. Farooq, MD was the ophthalmologist that performed the conjunctival biopsy, conceptualized the case report, and provided final edits to the manuscript. All authors attest that they meet the current ICJME criteria for Authorship.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Asim Farooq is a consultant to GlaxoSmithKline.
Acknowledgements
Dr. Peter Pytel, Department of Pathology at the University of Chicago for his role in and providing images of histopathology for this report, and Dr. Dimitra Skondra, retina specialist at the Department of Ophthalmology and Visual Science at the University of Chicago, for evaluating this patient.
References
- 1.Nabhan C., Rosen S.T. Chronic lymphocytic leukemia: a clinical review. JAMA. 2014;312(21):2265–2276. doi: 10.1001/jama.2014.14553. [DOI] [PubMed] [Google Scholar]
- 2.Sharma S., Rai K.R. Chronic lymphocytic leukemia (CLL) treatment: so many choices, such great options. Cancer. 2019;125(9):1432–1440. doi: 10.1002/cncr.31931. [DOI] [PubMed] [Google Scholar]
- 3.Buchan J., McKibbin M., Burton T. The prevalence of ocular disease in chronic lymphocytic leukaemia. Eye (Lond). 2003;17(1):27–30. doi: 10.1038/sj.eye.6700277. [DOI] [PubMed] [Google Scholar]
- 4.Coupland S.E., Foss H.D., Bechrakis N.E., Hummel M., Stein H. Secondary ocular involvement in systemic “memory” B-cell lymphocytic leukemia. Ophthalmology. 2001;108(7):1289–1295. doi: 10.1016/s0161-6420(01)00594-2. [DOI] [PubMed] [Google Scholar]
- 5.Tanenbaum R.E., Galor A., Dubovy S.R., Karp C.L. Classification, diagnosis, and management of conjunctival lymphoma. Eye Vis (Lond) 2019;6:22. doi: 10.1186/s40662-019-0146-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baron B.W., Thirman M.J., Giurcanu M.C., Baron J.M. Quercetin therapy for selected patients with PIM1 kinase-positive chronic lymphocytic leukemia/small lymphocytic lymphoma: a pilot study. Acta Haematol. 2018;139(2):132–139. doi: 10.1159/000486361. [DOI] [PubMed] [Google Scholar]
- 7.Mohsenin A., Sinard J., Huang J.J. Necrobiotic xanthogranuloma and chronic lymphocytic leukemia of the conjunctiva masquerading as scleritis and uveitis. Clin Ophthalmol. 2012;6:2045–2047. doi: 10.2147/OPTH.S35743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jain V.K., Singh U., Prakash G., Vashishta R.K., Singh V. Rare primary presentation of chronic lymphocytic leukemia as chronic orbital space occupying lesion. Int J Ophthalmol. 2016;9(1):173–174. doi: 10.18240/ijo.2016.01.30. [DOI] [PMC free article] [PubMed] [Google Scholar]