Highlights
-
•
Malnutrition screening of outpatients in a Gynecologic Oncology clinic setting is feasible.
-
•
Malnutrition was infrequently detected through outpatient screening of new patients with suspected gynecologic malignancy.
-
•
The prevalence of malnutrition in individuals with newly-diagnosed ovarian cancer is low.
-
•
Optimizing nutrition remains important, especially later in the cancer course when malnutrition is likely more prevalent.
Keywords: Nutrition; Malnutrition; Ovarian, fallopian tube, and peritoneal cancer; Quality improvement
Abstract
Introduction
Malnutrition is an independent risk factor for poor surgical outcomes, early chemotherapy discontinuation, and increased mortality. We evaluated the feasibility of outpatient malnutrition screening in patients with suspected gynecologic malignancy. We estimated the prevalence of malnutrition using Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition (AND-ASPEN) criteria in patients undergoing surgery for newly-diagnosed ovarian carcinoma (OC).
Methods
Patients scheduling a new clinic appointment for suspected gynecologic malignancy from 2/2018–2/2019 completed the Malnutrition Screening Tool via phone. Patients with positive screening test were recommended expedited Nutrition consultation. To estimate the prevalence of malnutrition in patients with newly-diagnosed OC, formal malnutrition evaluation by a Registered Dietician was ordered during hospitalization for all patients undergoing surgery (primary cytoreduction and interval cytoreduction) for newly-diagnosed OC.
Results
Of 187 outpatients screened, 29 (16%) had a positive malnutrition screen. Eleven of 29 (38%) were willing to schedule outpatient Nutrition appointment; four were evaluated. Two (1% of all outpatients screened) were diagnosed with malnutrition. 107 patients underwent surgery for primary OC; 70 received Nutrition consult. Only 3 of 70 (4%) were formally diagnosed with malnutrition using AND-ASPEN criteria.
Conclusion
Outpatient screening of patients with suspected gynecologic malignancy for malnutrition is feasible. However, the prevalence of malnutrition detected through outpatient screening and in the newly-diagnosed OC population is surprisingly low, suggesting that outpatient screening at time of initial consultation may not be ideal timing. Improving access to dietitians during chemotherapy and later in the cancer course when malnutrition is likely more prevalent may be beneficial.
1. Introduction
Individuals who lack adequate calories, protein, or other nutrient needed for tissue maintenance and repair experience undernutrition. While malnutrition refers to any nutritional imbalance and includes both undernutrition and overnutrition, the focus of this study is undernutrition, and in this manuscript, “malnutrition” is used synonymously with “undernutrition.” Malnutrition is an independent risk factor for poor surgical outcomes, early discontinuation of chemotherapy, and increased mortality in individuals with cancer (Caillet et al., 2017, Phippen et al., 2011). Individuals with newly diagnosed ovarian cancer have particularly high rates of malnutrition, with rates reported between 30 and 67% (Yim et al., 2016, Gupta et al., 2010, Laky et al., 2007, Chantragawee and Achariyapota, 2016) depending on the population and method used to diagnose malnutrition. Ovarian cancer patients with moderate to severe malnutrition have lower overall survival and progression free survival compared to those who are well-nourished (Yim et al., 2016, Gupta et al., 2010). Importantly, early nutritional support may improve cancer survival, suggesting that malnutrition may be a modifiable risk factor and not solely a marker for worse outcomes (Gupta et al., 2010, Trestini et al., 2018). This finding signifies the importance of early identification and intervention to improve nutritional status in oncology patients with malnutrition.
The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) mandates that patients receive nutrition screening within 24 h of hospital admission, with a full nutrition assessment in patients who screen “at risk” (JCAHO Board of Directors, 1995). Our institution complies with these guidelines, but most gynecologic oncology patients are not admitted to the hospital until immediately after surgery. Since malnutrition negatively impacts surgical outcomes, screening prior to planned surgery may allow for earlier intervention and potentially improved outcomes. We therefore decided to develop and determine the feasibility of an outpatient nutrition screening program with expedited evaluation and intervention in our Gynecologic Oncology clinic.
Surprisingly, among gynecologic oncology patients who underwent surgery at the University of Washington Medical Center (UWMC) between 2017 and 2018, only 6.5% had a diagnosis code of malnutrition recorded. Registered dietitians at UWMC utilize the Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition (AND-ASPEN) criteria for diagnosing malnutrition, considered a gold standard for nutrition evaluation (White et al., 2012). Refer to Table 1 for the AND-ASPEN criteria used to diagnose malnutrition in cancer patients. Our rate of malnutrition of 6.5% is significantly lower than the 30–67% rate of malnutrition in this patient population previously reported in the literature (Yim et al., 2016, Gupta et al., 2010, Laky et al., 2007, Chantragawee and Achariyapota, 2016). Potential reasons for this discordance could include under-identification of malnutrition due to failure of the physician to add a malnutrition diagnosis/code to a patient’s chart, or inability of our current inpatient screening process to adequately identify patients at risk for malnutrition. Alternatively, the actual rate of malnutrition in our patient population may be lower than previously thought: criteria for malnutrition by AND-ASPEN may be more stringent than prior methods and thus fewer patients meet diagnostic criteria, or rates of malnutrition at time of surgery may have improved with increasing use of neoadjuvant chemotherapy or due to geographic and socioeconomic differences in our patient population. We therefore sought to determine the prevalence of malnutrition using formal AND-ASPEN criteria in all patients undergoing surgery for newly-diagnosed ovarian, fallopian tube, and peritoneal carcinoma. We chose to study newly-diagnosed ovarian carcinoma patients rather than the heterogeneous group of all gynecologic cancer patients because prevalence and reasons for malnutrition significantly differ depending on the cancer type, and individuals with ovarian cancer have the highest reported rates of malnutrition (Laky et al., 2007).
Table 1.
AND-ASPEN criteria for diagnosis of malnutrition (White et al., 2012) (Malnutrition in the context of chronic illness such as cancer).
| Clinical characteristic* | Moderate | Severe |
|---|---|---|
| Inadequate energy intake | <75% of estimated energy requirement for ≥ 1 month | ≤75% of estimated energy requirement for ≥ 1 month |
| Weight loss | 5% over 1 month 7.5% over 3 months 10% over 6 months 20% over 1 year |
>5% over 1 month >7.5% over 3 months >10% over 6 months >20% over 1 year |
| Loss of muscle mass (e.g. wasting of temporalis; pectoralis; deltoids; interosseus; latissimus dorsi, trapezius; quadriceps; gastrocnemius) | Mild | Severe |
| Loss of subcutaneous fat (e.g. orbital, triceps, fat overlying ribs) | Mild | Severe |
| Fluid accumulation (e.g. extremities; vulvar/scrotal edema; ascites) | Mild | Severe |
| Diminished functional status (as measure by hand grip strength) | N/A | Measurably reduced |
Must have 2 of 6 characteristics to meet criteria for malnutrition. Scoring: ≥2 indicators in the severe category = severe malnutrition; ≥2 indicators in the moderate category OR 1 severe + 1 moderate = moderate malnutrition; <2 indicators = no malnutrition.
Given the potential impact improved nutrition may have on oncology outcomes and the discrepancy in rates of malnutrition between UWMC patients and the literature, this quality improvement project therefore had two aims: to evaluate the feasibility of outpatient nutrition screening with expedited evaluation and intervention in patients with any suspected gynecologic malignancy, and to determine the prevalence of malnutrition using formal AND-ASPEN criteria in patients undergoing surgery for newly-diagnosed ovarian, fallopian tube, and peritoneal carcinoma.
2. Methods
This project was performed for Quality Improvement purposes and approval by the Institutional Review Board at the University of Washington was not required.
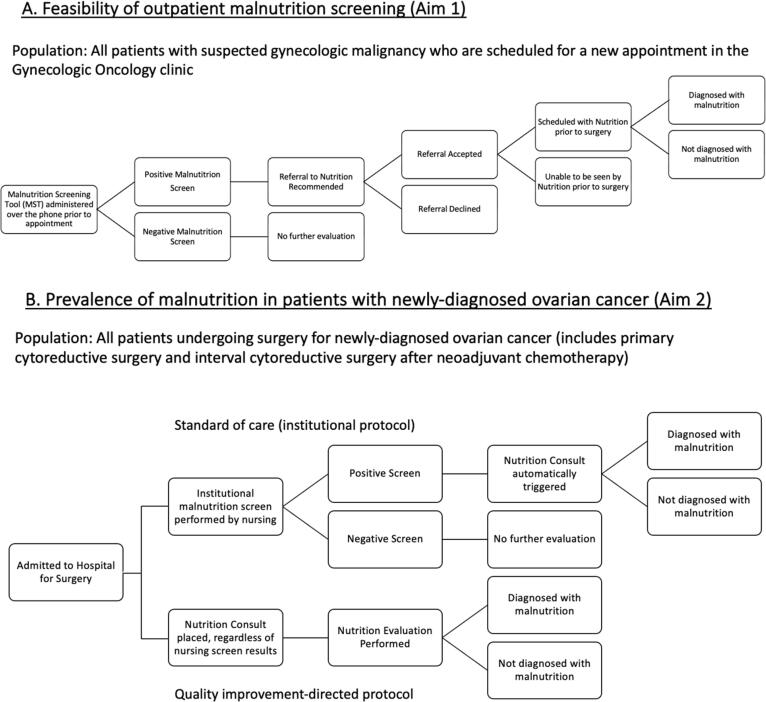
Aim 1 (Feasibility of outpatient nutrition screening in patients with suspected gynecologic malignancy): Patients with a suspected gynecologic malignancy (including ovarian/fallopian tube/peritoneal, endometrial, cervical, vulvar, or vaginal cancer) scheduling a new appointment at the University of Washington Gynecologic Oncology clinic between February 2018 and February 2019 were administered the Malnutrition Screening Tool (MST) (Mulnutrition Screening Tool, 2013) over the phone by a Patient Care Coordinator. The MST consists of two simple questions: “Have you recently lost weight without trying, and if yes, how much weight have you lost?”; and “Have you been eating poorly because of a decreased appetite?” Patients with a positive screening test were informed by the Patient Care Coordinator using a standardized script that they might have a diagnosis of malnutrition and were recommended to have an outpatient nutrition consultation with a Registered Dietitian. For patients who were amenable, an attempt was made to schedule an appointment with outpatient nutrition, and for those planned to undergo surgery, prior to their scheduled surgery whenever possible. If patients declined a nutrition consultation, their reason for decline was recorded. Refer to Fig. 1A for a flow diagram of this process. When patients were evaluated by a Registered Dietitian, complete evaluation included a history and physical exam, and assessment of energy intake, weight loss, body fat, muscle mass, and functional status including hand grip strength. The presence or absence of malnutrition was determined using AND-ASPEN criteria (Table 1).
Fig. 1.
Flow diagram of malnutrition screening and evaluation processes in the outpatient and inpatient settings. A. Feasibility of outpatient malnutrition screening. Patients with suspected gynecologic malignancy who were scheduled for a new patient appointment were administered the Malnutrition Screening Tool. Those with a positive screen were recommended a Nutrition referral. When referral was accepted and scheduled, the patient was formally evaluated for malnutrition by the Registered Dietitian using AND-ASPEN criteria. B. Estimating the prevalence of malnutrition in patients with newly-diagnosed ovarian cancer. Patients undergoing primary cytoreductive surgery or interval cytoreductive surgery for newly-diagnosed ovarian cancer were included. Upon admission, all patients received both standard of care processes per our institutional protocol (top portion of diagram) and the Quality Improvement (QI)-directed protocol (bottom portion of diagram). Although in standard of care, patients would normally only be formally assessed by a Registered Dietitian if they had a positive screening test, in this study per the QI-directed protocol, all patients were to receive a formal Nutrition Consult, regardless of whether their inpatient nursing screen for malnutrition was positive or negative.
Aim 2 (Prevalence of malnutrition in patients with newly-diagnosed ovarian carcinoma): All patients undergoing surgery for treatment of newly-diagnosed epithelial ovarian, fallopian tube, or peritoneal carcinoma (collectively referred to as ovarian cancer) who underwent surgery between February 2018 and February 2019 were included. Patients were considered to have newly diagnosed ovarian cancer if they were receiving front-line/first-line therapy; patients undergoing primary cytoreductive surgery and those undergoing interval cytoreductive surgery after neoadjuvant chemotherapy were therefore included as “newly-diagnosed.” Patients undergoing surgery for recurrence or for other reasons were excluded. Patients initially suspected to have epithelial ovarian cancer but ultimately found to have benign, borderline, non-epithelial ovarian cancer, or non-ovarian cancer on final pathology were excluded in final data analysis.
In order to estimate the prevalence of malnutrition in this population and as part of our Quality Improvement (QI) initiative, patients were planned to have a nutrition consult placed by their provider immediately upon admission after their surgery. A Registered Dietitian (RD) performed a full formal evaluation for malnutrition using the AND-ASPEN criteria during their inpatient hospitalization. Refer to Fig. 1B for a flow diagram of this process. The prevalence of malnutrition was determined by the percentage of patients evaluated by an RD who were formally diagnosed with malnutrition based on that evaluation.
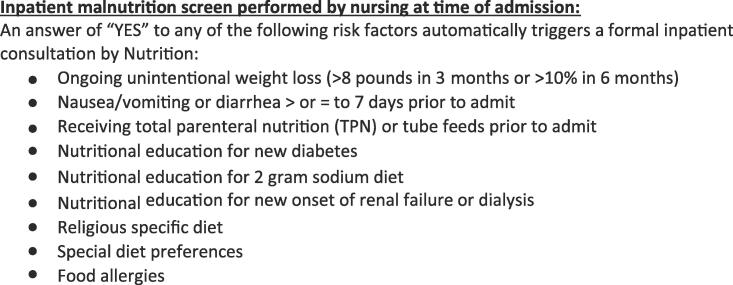
In addition to the above-specified QI protocol (where all patients should have a formal nutrition consult placed and undergo evaluation), all patients also received the usual standard of care (Fig. 1B). As part of routine care at our institution, all patients admitted to the University of Washington are screened by the nurses on admission for malnutrition using a hospital-designed screening tool (Fig. 2). An answer of “YES” to any of the questions is considered a positive screening test, and automatically triggers an inpatient consultation by Nutrition. However, due to our QI protocol described above to determine the true prevalence of malnutrition, even patients with a negative nursing screen were still planned to receive a formal nutrition evaluation during the study period.
Fig. 2.
Inpatient malnutrition screen performed by nursing at time of admission. All patients are screened by nursing at time of admission using the displayed assessment. Any answer of “yes” constitutes a positive malnutrition screen, and triggers an automatic Nutrition consultation.
Data was abstracted from medical records. All outpatient and inpatient Registered Dietitian notes were reviewed to determine presence or absence of malnutrition diagnosis. We assessed the performance of our current inpatient screening process by nursing. We compared the rate of malnutrition identified through routine care (inpatient screening by nursing with subsequent nutrition consult/full assessment for positive screens) versus the rate of malnutrition identified using universal nutrition consult for all inpatients. In addition, we also evaluated concordance between the inpatient nursing screen and the outpatient MST for individuals who had received both.
3. Results
3.1. Outpatient screening results
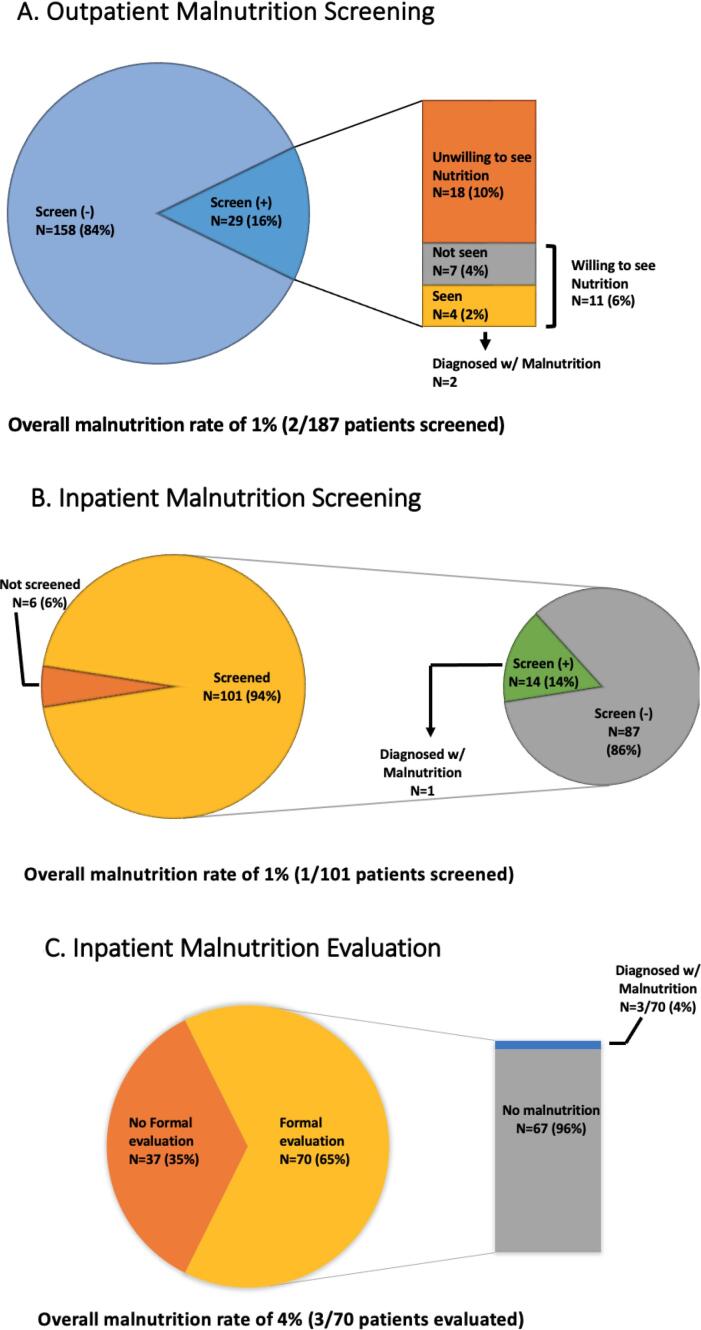
An estimated 884 patients (with both benign and malignant conditions) were seen in clinic for a new consult during the study period. A total of 187 patients (21%) with a suspected gynecologic cancer diagnosis were screened by the patient care coordinators in the outpatient setting when scheduling their initial appointment. Please refer to Table 2 for patient characteristics. Of the 187 screened, 29 (16%) had a positive malnutrition screen. 11/29 (38%) were willing to schedule an appointment with Nutrition (Fig. 3A). Four of these 11 patients were successfully evaluated by Nutrition in the outpatient setting, and two patients were diagnosed with malnutrition. Thus, of all outpatients screened, 2/187 (1%) were diagnosed with malnutrition. One patient had stage IVB grade 3 endometrial cancer, and the other patient had a pelvic mass which was ultimately found to be benign. Of the 35 patients ultimately diagnosed with ovarian cancer specifically, 8 (23%) screened positive. None were diagnosed with malnutrition.
Table 2.
Outpatient Demographic Data.
| Total patients | 187 | |
|---|---|---|
| Median age (years) | 57 | |
| Ultimate diagnosis | Ovary/fallopian tube/peritoneal cancer | 34 |
| Cervical cancer | 10 | |
| Uterine cancer | 53 | |
| Vulvar/Vaginal cancer | 7 | |
| Borderline | 4 | |
| Benign | 60 | |
| Unknown/lost to follow-up | 14 | |
| Cancer of non-GYN origin | 5 |
Fig. 3.
Malnutrition screening and Nutrition evaluation. A. Outpatient screening using Malnutrition Screening Tool (MST). Of 187 patients initially screened, 2 patients (1%) were ultimately diagnosed with malnutrition. B. Inpatient screening via nursing assessment upon admission. Of 101 patients initially screened, 1 patient (1%) was ultimately diagnosed with malnutrition. C. Inpatient formal Nutrition evaluation, regardless of initial screening results. Of 70 patients formally evaluated, 3 patients (4%) were diagnosed with malnutrition.
Eighteen of 29 (62%) patients with a positive malnutrition screen declined outpatient Nutrition evaluation. Fourteen patients did not give a reason for declining, one patient declined because she did not think it was needed, two stated they were “unsure,” and one had already met with Nutrition previously. Of the 7 patients with a positive malnutrition screen who were not seen despite showing interest, the most common reason was scheduling difficulty. Three patients reported “no appointment available prior to surgery”, two reported “unable to coordinate with new patient visit” and one reported “wanted a different day.”.
3.2. Inpatient results
During the study period, 107 patients underwent primary cytoreductive surgery (N = 56) or interval cytoreduction (N = 51) for a new diagnosis of epithelial ovarian cancer. Additional patient characteristics are reported in Table 3. 101/107 (94%) received inpatient malnutrition screening by nursing per our institution’s standard protocol. Fourteen of these patients (14%) screened positive, all received an inpatient Nutrition consult, and one was formally diagnosed with malnutrition, with an overall malnutrition rate of 1% (1/107 screened) identified using our institution’s current standards (Fig. 3B).
Table 3.
Inpatient Demographic Data.
| Total patients | 107 | |
|---|---|---|
| Median age (years) | 63 | |
| Cancer type | Ovarian Fallopian tube Peritoneal |
95 9 3 |
| Histology | High-grade serous | 75 |
| Low-grade serous | 4 | |
| Endometrioid | 13 | |
| Clear cell | 12 | |
| Mucinous adenocarcinoma | 2 | |
| Carcinosarcoma | 1 | |
| Stage | I | 25 |
| II | 7 | |
| III | 44 | |
| IV | 30 | |
| Incompletely staged | 1 | |
| Chemotherapy | Neoadjuvant | 51 |
| Adjuvant | 56 |
Per our specified QI protocol, in order to determine the prevalence of malnutrition, all patients undergoing surgery for primary ovarian cancer were supposed to receive a formal Nutrition consult, regardless of the results of the inpatient nursing screen. Of the 107 total patients who underwent surgery for ovarian cancer, 70 (65%) were actually evaluated by Nutrition per protocol. Three of the 70 patients evaluated were formally diagnosed with malnutrition, making the rate of malnutrition by AND-ASPEN criteria in patients undergoing primary surgery for ovarian, fallopian tube, or peritoneal carcinoma 4% (Fig. 3C). Of these three patients with malnutrition, one had an aborted debulking surgery, one had an anastomotic leak, and one had a postoperative ICU admission.
Only 15% of patients with a positive MST screen as an outpatient were identified on inpatient screening as “at-risk,” despite similar questions about weight loss on both screening tools, raising questions about the adequacy of our institution’s current inpatient screening method. In addition, of the 3 patients ultimately diagnosed with malnutrition by our specified protocol of universal nutrition consult, two of these patients (66%) had a negative inpatient screening by nursing on admission and would have been missed by our current standard of care.
4. Discussion
Outpatient nutrition screening with expedited evaluation and intervention may be feasible in patients with suspected or confirmed gynecologic malignancy. In our Gynecologic Oncology clinic, 16% had a positive screen, and 1% (2 of 187) were formally diagnosed with malnutrition. However, several barriers to implementation were identified. First, coordinating appointments was challenging. Of the 11 patients willing to meet with Nutrition in the outpatient setting, only four were able to schedule coordinated appointments and six of the remaining seven reported scheduling difficulty as their barrier to being seen. The availability of our registered dietitian was limited, and many patients were unwilling to return to clinic for nutrition consult on a separate day from their oncology appointment due to living a considerable distance away. One potential solution to this barrier could be offering virtual nutrition consults through telemedicine. This study was performed prior to the COVID-19 pandemic, when telemedicine was not routinely being used. Telemedicine is now routinely offered and would likely allow for more flexible scheduling and decrease the amount of time spent in physicians’ offices during an inherently stressful time. Second, a lack of patient education and understanding regarding the importance of nutritional support also contributed to lower rates of evaluation. 62% (18/29) of patients with a positive screen declined an outpatient nutrition consult. Fourteen did not give a reason for declining, but 3 of the 4 patients who gave a reason for declining stated they did not think a nutrition consult was needed or were unsure. The use of online nutrition education modules as part of new patient teaching could potentially mitigate this barrier.
We hypothesized that screening for malnutrition in the outpatient setting, especially prior to planned surgery, would be a valuable addition to gynecologic cancer care since malnutrition negatively impacts surgical outcomes and identification of malnutrition pre-operatively would allow for earlier intervention. Early nutritional support may improve cancer survival, suggesting that malnutrition may be a modifiable risk factor and not solely a marker for worse outcomes (Gupta et al., 2010, Trestini et al., 2018). If we identified malnutrition pre-operatively, we would initiate nutritional support prior to surgery, or in some cases, severely malnourished patients with ovarian cancer would be recommended to undergo neoadjuvant chemotherapy rather than primary cytoreductive surgery.
However, given the significantly lower than anticipated rate of malnutrition detected through outpatient screening of only 1%, outpatient screening for malnutrition at the time of initial Gynecologic Oncology consultation may not be clinically indicated. In addition, while early intervention is indicated for patients with malnutrition to hopefully improve surgical outcomes, all patients at our institution (regardless of nutrition status) already consume immuno-nutrition protein shakes both prior to and after surgery through our Enhanced Recovery After Surgery pathway. This practice may further diminish the impact of a separate outpatient nutrition assessment prior to surgery. Undergoing initial evaluation for a suspected cancer diagnosis and preparing for surgery is a very stressful time for many patients. Patients may have been less likely to accept a nutrition referral if they were feeling overwhelmed. In one study of malnutrition screening performed in a Radiation Oncology clinic for gynecologic patients undergoing radiation therapy, patients were more likely to decline a nutrition referral when it was placed at initial consultation or within the first week of treatment (Croisier et al., 2022). Forty of 50 patients with a positive malnutrition screen accepted a nutrition referral placed during or after treatment; in contrast, the majority (7 of 10) of referrals declined had been placed at initial consultation or within the first week of treatment, suggesting patients may be more receptive to nutrition referral later in their treatment course. Optimizing nutrition status must be integrated into cancer care, but patients may be more willing to see Nutrition if consultation is recommended slightly later in their course rather than at the same time as their initial Gynecologic Oncology appointment.
Similar to our outpatient findings, we detected a surprisingly low rate of malnutrition in individuals undergoing surgery for newly-diagnosed ovarian carcinoma of only 4%. Prior studies suggested rates of 30–67% (Yim et al., 2016, Gupta et al., 2010, Laky et al., 2007, Chantragawee and Achariyapota, 2016). There are several possible explanations for this discrepancy. Most notably, 48% (51/107) of ovarian cancer patients in this project received neoadjuvant chemotherapy and we hypothesize they may have had time to improve their nutritional status prior to admission for surgery. In one study evaluating patients who underwent neoadjuvant chemotherapy for ovarian cancer, 47% of patients had an albumin level < 3.5 g/dL, whereas only 5.5% of patients had persistently low albumin level at time of interval debulking surgery (Gill et al., 2017). Our study likely included a significantly higher proportion of patients who received neoadjuvant chemotherapy compared to prior studies, some of which excluded patients receiving neoadjuvant chemotherapy and some of which were conducted at a time when neoadjuvant chemotherapy administration may have been less commonly administered. Additionally, this project was done at a single institution, and nutritional status at baseline of patients residing in the Pacific Northwest may not be generalizable to other areas of the United States or other countries. Prior estimates of malnutrition used a variety of methods to ascertain malnutrition status, but many studies used the Subjective Global Assessment (SGA) or Patient Generated-Subjective Global Assessment (PG-SGA). While AND-ASPEN is considered more objective than the SGA and we had hypothesized that it may be more stringent, recent studies suggest that AND-ASPEN has good agreement with SGA (Hipskind et al., 2020, Burgel et al., 2021); so we suspect that the lower rates of malnutrition observed in our study are more likely due to patient population rather than the assessment tool.
Although the overall prevalence of malnutrition in patients with primary ovarian carcinoma appears to be low, it was notable that our current inpatient nutrition screening process failed to identify 2 of 3 of patients diagnosed with malnutrition through the universal nutrition assessment. 85% of patients with a positive outpatient screen using the MST were also missed on the inpatient screen despite almost identical questions about weight loss. These findings raised concern that our current inpatient screening process may need to be modified. Since this project was completed, our institution has subsequently changed to using the MST for inpatient screening, which is much simpler to perform and is a validated screening tool. Altering the timing of inpatient nutrition screening may also be beneficial. Most patients receive the screen postoperatively when they arrive to the floor from the Post Anesthesia Care Unit; this time is an extremely busy time for nursing and patients may also have residual effects of anesthesia which could limit their ability to appropriately answer questions.
This project had several limitations. It took place at a single institution, and the findings may not generalize to institutions across the country. Less than half of the new patients seen in our clinic received the MST, potentially resulting in unintended biases. In addition, the overall sample sizes were relatively small. The outpatient and inpatient study populations overlapped to some degree, but not every inpatient who underwent surgery for ovarian cancer received the MST outpatient screening test and Nutrition consult as an inpatient, which would have provided additional information. Nonetheless, our study adds further understanding to the current body of literature on malnutrition in individuals with ovarian cancer. To the best of our knowledge, no other studies have evaluated to the feasibility of outpatient nutrition screening in a Gynecologic Oncology clinic setting, and this study does demonstrate feasibility of the process. Due to the surprisingly low prevalence of malnutrition detected through outpatient screening of new patients, our study findings suggest that outpatient screening of new patients with suspected gynecologic malignancy may not be the most ideal timing and use of resources. However, nutrition remains a very important aspect of cancer care. Optimizing our inpatient screening process, and improving access to Dietitians during chemotherapy or later in a patient’s cancer course when malnutrition is likely more prevalent may be beneficial.
CRediT authorship contribution statement
Katrin E. Eurich: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing, Visualization. Alysun Deckert: Methodology, Writing – review & editing. Bonnie Smith: Methodology, Writing – review & editing. Kay Kolahi: Methodology, Writing – review & editing. Kathryn P. Pennington: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing, Visualization, Supervision, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This work was supported in part by the Ovarian Cancer & Survivorship Research Fund (KP).
References
- Caillet P., Liuu E., Raynaud Simon A., Bonnefoy M., Guerin O., Berrut G., Lesourd B., Jeandel C., Ferry M., Rolland Y., Paillaud E. Association between cachexia, chemotherapy and outcomes in older cancer patients: a systematic review. Clin. Nutr. 2017;36(6):1473–1482. doi: 10.1016/j.clnu.2016.12.003. [DOI] [PubMed] [Google Scholar]
- Phippen N.T., Lowery W.J., Barnett J.C., Hall L.A., Landt C., Leath C.A. Evaluation of the Patient-Generated Subjective Global Assessment (PG-SGA) as a predictor of febrile neutropenia in gynecologic cancer patients receiving combination chemotherapy: a pilot study. Gynecol. Oncol. 2011;123(2):360–364. doi: 10.1016/j.ygyno.2011.07.093. [DOI] [PubMed] [Google Scholar]
- Yim G.W., Eoh K.J., Kim S.W., Nam E.J., Kim Y.T. Malnutrition identified by the nutritional risk index and poor prognosis in advanced epithelial ovarian carcinoma. Nutr. Cancer. 2016;68(5):772–779. doi: 10.1080/01635581.2016.1159702. [DOI] [PubMed] [Google Scholar]
- Gupta D., Lis C.G., Vashi P.G., Lammersfeld C.A. Impact of improved nutritional status on survival in ovarian cancer. Support. Care Cancer. 2010;18(3):373–381. doi: 10.1007/s00520-009-0670-y. [DOI] [PubMed] [Google Scholar]
- Laky B., Janda M., Bauer J., Vavra C., Cleghorn G., Obermair A. Malnutrition among gynaecological cancer patients. Eur. J. Clin. Nutr. 2007;61(5):642–646. doi: 10.1038/sj.ejcn.1602540. [DOI] [PubMed] [Google Scholar]
- Chantragawee C., Achariyapota V. Utilization of a scored patient-generated subjective global assessment in detecting a malnourished status in gynecologic cancer patients. Asian Pac. J. Cancer Prev. 2016;17:4401–4404. [PubMed] [Google Scholar]
- Trestini I., Carbognin L., Sperduti I., et al. Prognostic impact of early nutritional support in patients affected by locally advanced and metastatic pancreatic ductal adenocarcinoma undergoing chemotherapy. Eur. J. Clin. Nutr. 2018;72:772–779. doi: 10.1038/s41430-018-0155-5. [DOI] [PubMed] [Google Scholar]
- JCAHO Board of Directors: 1995 Comprehensive Accreditation. Manual for Hospitals. Oakbrook, IL, 1995.
- White J.V., Guenter P., Jensen G., et al. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition) JPEN J. Parenter. Enteral Nutr. 2012;36:275–283. doi: 10.1177/0148607112440285. [DOI] [PubMed] [Google Scholar]
- “Mulnutrition Screening Tool.” Abbott Nutrition, May 2013, static.abbottnutrition.com/cms-prod/abbottnutrition-2016.com/img/Malnutrition%20Screening%20Tool_FINAL_tcm1226-57900.pdf.
- Croisier E., Morrissy A., Brown T., et al. Nutrition risk screening and implications for patients with gynaecological cancers undergoing pelvic radiotherapy and/or other treatment modalities: a retrospective observational study. Nutr. Diet. 2022;79:217–228. doi: 10.1111/1747-0080.12712. [DOI] [PubMed] [Google Scholar]
- Gill S.E., McGree M.E., Weaver A.L., et al. Optimizing the treatment of ovarian cancer: neoadjuvant chemotherapy and interval debulking versus primary debulking surgery for epithelial ovarian cancers likely to have suboptimal resection. Gynecol. Oncol. 2017;144:266–273. doi: 10.1016/j.ygyno.2016.11.021. [DOI] [PubMed] [Google Scholar]
- Hipskind P., Rath M., JeVenn A., et al. Correlation of new criteria for malnutrition assessment in hospitalized patients: AND-ASPEN Versus SGA. J. Am. Coll. Nutr. 2020;39:518–527. doi: 10.1080/07315724.2019.1699476. [DOI] [PubMed] [Google Scholar]
- Burgel C.F., Teixeira P.P., Leites G.M., et al. Concurrent and predictive validity of AND-ASPEN malnutrition consensus is satisfactory in hospitalized patients: a longitudinal study. JPEN J. Parenter. Enteral Nutr. 2021;45:1061–1071. doi: 10.1002/jpen.1980. [DOI] [PubMed] [Google Scholar]