Abstract
Background
Diabetic kidney disease (DKD) is the most common cause of end-stage renal disease (ESRD), but the mechanism between DKD and ESRD remains unclear. Some experts have put forward the “microbial-centered ESRD development theory”, believing that the bacterial load caused by gut microecological imbalance and uremia toxin transfer are the core pathogenic links. The purpose of this study was to analyze the genomic characteristics of gut microbiota in patients with ESRD, specifically DKD or non-diabetic kidney disease (NDKD).
Methods
In this cross-sectional study, patients with ESRD were recruited in a community, including 22 DKD patients and 22 NDKD patients matched using gender and age. Fecal samples of patients were collected for 16S rDNA sequencing and gut microbiota analysis. The distribution structure, diversity, and abundance of microflora in DKD patients were analyzed by constructing species evolutionary trees and analyzing alpha diversity, beta diversity, and linear discriminant analysis effect size (LEfSe).
Results
The results of our study showed that there were statistically significant differences in the richness and species of gut microbiota at the total level between DKD patients and NDKD patients. The analysis of genus level between the two groups showed significant differences in 16 bacterial genera. Among them, Oscillibacter, Bilophila, UBA1819, Ruminococcaceae UCG-004, Anaerotruncus, Ruminococcaceae, and Ruminococcaceae NK4A214 bacteria in DKD patients were higher than those in NDKD patients.
Conclusions
16S rDNA sequencing technology was used in this study to analyze the characteristics of intestinal flora in ESRD patients with or without diabetes. We found that there was a significant difference in the intestinal flora of ESRD patients caused by DKD and NDKD, suggesting that these may be potential causative bacteria for the development of ERSD in DKD patients.
Keywords: End-stage renal disease (ESRD), diabetic kidney disease (DKD), non-diabetic kidney disease (NDKD), gut microbiota, 16S rDNA
Introduction
Chronic kidney disease (CKD) is one of the most common chronic diseases worldwide. Epidemiological studies have shown that the prevalence of CKD is 10.8% in China, 13% in the United States, and 8% to 16% worldwide (1-3). More and more basic and clinical studies have confirmed that CKD is closely related to obesity, diabetes, primary and secondary glomerulonephritis, hypertension, and hyperlipidemia, among other conditions, leading to heart disease (4), stroke (5), cancer (6), cognitive impairment (7), and other diseases. These diseases increase the mortality of patients with CKD (8). For patients with diabetic kidney disease (DKD), once damage to kidney structure and function begins, it enters an irreversible process. The occurrence and development of DKD is very quick. End-stage renal disease (ESRD) appears earlier in DKD patients than in those with other diseases, seriously threatening the safety and quality of life of patients.
Recent study has shown that intestinal microbial dysregulation is also one of the key factors leading to the occurrence and development of CKD (9). The human gut is a diverse and vibrant microecosystem, with more than 1,000 species of 300 trillion bacteria, 10 times the number of cells in our body, with at least 160 dominant floras in each person (10). Changes in the structure of intestinal flora are the result of the combined action of host genotype and environmental factors (11). The most significant changes occur in early childhood, including delivery type (vaginal delivery or cesarean section) (12), and then change with microbial exposure, diet, age, geographical location, antibiotic use and other factors (13,14). In a healthy person, Bacteroides and Firmicutes account for more than 90% of the gut flora, including Clostridium, Clostridium tender, Bacteroides, Eubacteria, Prevotella, Porphyromonas, Ruminococcus, and Lactobacillus, among others. In addition, other classes with less abundance are Proteobacteria (Enterobacteriaceae, Helicobacter pylori, and Desatella), Actinobacteria (Bifidobacteria and Collinia aerogenesis), Methanoarchaea, and Microphyla veratum, among others (15). Normally, there is a “dynamic balance” between gut microbes and the body, promoting and maintaining the health of the body in a balanced physiological state. Once this balance is upset, it can lead to various gastrointestinal and even extra-gastrointestinal diseases, including obesity (16), hypertension (17), cancer (18), depression (19), and cardiovascular disease (20). Similarly, the occurrence and development of obesity and CKD will also directly affect the structure and/or abundance of intestinal flora (17,21-24).
Recent study has revealed that there is an association between intestinal flora and CKD (25). Some experts have put forward the “microbial-centered theory of CKD development”, believing that the bacterial load caused by intestinal microecological imbalance and uremia toxin transfer are the core pathogenic factors. The intestinal excretion of urea in patients with CKD is significantly increased, which increases the pH of the intestinal lumen. This can damage the intestinal barrier, increase the bacteria with urease, uricase, indole, and paraccresol-forming enzymes, and decrease the bacterial families that form short-chain fatty acid (SCFA) enzymes (26). With the increasing number of bacteria responsible for intestinal protein fermentation, harmful products affecting protein fermentation are also increased, mainly phenols and indoles, leading to uremic toxicity and systemic inflammation (27). Many substances secreted by the microbiome may become uremic toxins in the CKD environment and can be absorbed by the body (28,29). In a basic experiment, significantly lower levels of 11 metabolites were detected in the plasma of sterile mice with renal insufficiency compared with mice without specific pathogens, suggesting that these metabolites may be derived from abnormal intestinal flora (30).
DKD is often accompanied by intestinal microbiota disorder, which is characterized by a decrease in beneficial bacteria and an increase in opportunistic pathogens. In a meta-analysis, patients with diabetes had a decrease in beneficial intestinal bacteria, such as Bacteroidetes (Bacteroidetes or Bacteroidetes orders), and an increase in the relative abundance of Firmicutes (negative Bacteroidetes, Selenomonas, or Vestoriaceae) and Actinobacteria (31). Tao et al. (32) found that Firmicutes were reduced and Proteobacteria were increased in DKD patients compared with healthy people and diabetic patients without kidney disease. However, no studies have explored the changes in intestinal flora and its metabolites in end-stage DKD. Some studies (29,30) have explored the possibility of gut microbiota as a marker for noninvasive diagnosis and individualized treatment of metabolic diseases, but it is not clear which bacteria are more suitable as biomarkers for end-stage DKD.
We used 16S rDNA-based high-throughput sequencing technology to explore the differences in intestinal flora between ESRD patients with DKD and non-diabetic kidney disease (NDKD), and explored the microbial markers related to end-stage DKD. We present the following article in accordance with the MDAR reporting checklist (available at https://atm.amegroups.com/article/view/10.21037/atm-22-2926/rc).
Methods
Study subjects
A total of 44 ESRD patients (male and female) aged 45–75 were enrolled from June 2020 to December 2020. There were 22 patients in the DKD group and 22 patients in the NDKD group (relevant case data are shown in website: https://cdn.amegroups.cn/static/public/atm-22-2926-01.xlsx). All patients were diagnosed and assessed according to the inclusion criteria by professional physicians in the Department of Endocrinology, Metabolism, and Nephrology according to the guidelines. All patients were given high quality low protein, low salt and low fat diabetic diet. The study was approved by the Jinxia Community Health Service Centre (No. JXSQ2021003), and was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was signed by all participants. The enrolled patients were all local residents, living in similar areas, with similar dietary structure and no racial difference s. All patients used insulin to control blood glucose.
Inclusion criteria
The diagnostic criteria for ESRD are in line with the Kidney Disease: Improving Global Outcomes (KDIGO) 2012 Clinical Practice Guidelines. ESRD was defined as estimated glomerular filtration rate (eGFR) of less than 15 mL/min/1.73 m2 and duration more than 3 months, regardless of whether there was kidney damage. DKD diagnostic criteria were in line with the Chinese guidelines for the prevention and treatment of type 2 diabetes (2020 edition), based on persistently increased urine albumin-to-creatinine ratio (UACR) and/or decreased eGFR, while excluding other CKD. The NDKD group met the ESRD diagnostic criteria and excluded patients with renal insufficiency caused by DKD.
Exclusion criteria
The exclusion criteria were as follows: (I) pregnant patients or patients with acute infection or kidney transplantation; (II) patients with acute complications or other serious diseases, such as malignant tumors, acute cardiovascular and cerebrovascular diseases, blood diseases, or connective tissue diseases; (III) patients with diarrhea, constipation, or other gastrointestinal diseases; (IV) those who received antibiotics in the last 12 weeks; (V) patients with a blood transfusion history in the last 12 weeks; (VI) those who used adrenal corticosteroids or immunosuppressants in the last 12 weeks; (VII) patients who used laxatives or cathartic drugs in the past 12 weeks.
Measurement of general indicators
Age, height, weight, waist circumference, and hip circumference of patients in the DKD group and NDKD group were collected. The height, weight, waist circumference, and hip circumference were examined according to the unified standards after standardized training. Body mass index (BMI) and waist-to-hip ratio (WHR) were recorded and calculated. The medical histories of patients in the two groups were collected, including medication history, dialysis history, living schedule, and diet, among others.
Blood sample collection
Subjects abstained from high-sugar and high-fat foods, alcohol, smoking, and coffee, and did not exercise vigorously the day before blood collection.
For the determination of laboratory indicators, early morning fasting (fasting for at least 8 hours) venous blood was collected from the median cubital vein, and glycated hemoglobin, total cholesterol (TC), total triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), serum creatinine, blood urea nitrogen (BUN), cystatin C (CysC), fasting plasma glucose (FPG), fasting insulin (FINS), hemoglobin (Hb), parathyroid hormone (PTH), uric acid, albumin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), and hepatitis B virus antigen and antibody were detected.
The calculation formula of the insulin resistance index, namely the homeostatic model assessment for insulin resistance (HOMA-IR), was as follows: HOMA-IR = FPG (mmol/L) × FINS (mIU/L)/22.5.
Collection of stool specimens
For collecting stool samples, Sterile cotton swabs were used to take samples from the middle section of the subject’s stool. One sample was used for routine stool tests and occult blood tests, while the other sample was labeled with name and retention time and stored in a refrigerator at −80 ℃ for fecal 16s rDNA sequencing. Subsequently, beta diversity analysis was performed, including: (I) principal component analysis (PCA) and principal coordinates analysis (PCoA); (II) non-metric multidimensional scaling (NMDS) analysis; (III) unweighted pair group method with arithmetic mean (UPGMA) analysis. Heat maps and significance analysis were performed for species differences between groups.
Statistical methods
SPSS22.0 statistical software was used for statistical analysis. All statistical inferences were tested for non-inferiority. The statistical significance test level was set as unilateral 0.025, and 95% confidence interval was used to estimate the parameters. When the data does not meet the parameter method condition, the data conversion method can be used to make it meet the condition. If the data still does not meet the criteria, consider a nonparametric approach. If the above conditions are not met, the data conversion method can be used to meet the above conditions. Two independent sample t test was used for comparison between groups of normally distributed measurement data. For measurement data with non-normal distribution, Wilcoxon rank sum test was used for comparison between groups.
Results
General information
Table 1 summarizes and compares the baseline demographic characteristics, medical history, and other indicators of all subjects. Results showed that in ESRD patients with diabetes, glycosylated hemoglobin, systolic pressure, fasting glucose ferritin, and glomerular filtration rate were higher than those in ESRD patients without diabetes. The incidence rates of history of eye disease, beta 2 microglobulin, blood phosphorus, serum creatinine, serum prealbumin, and uric acids were lower than those in ESRD patients without diabetes.
Table 1. Comparison of medical records between the diabetic and non-diabetic groups.
| Indicators | Diabetic patients (n=22) | Non-diabetic patients (n=22) | P value |
|---|---|---|---|
| Gender, n (%) | |||
| Female | 11 (50.00) | 11 (50.00) | 1 |
| Male | 11 (50.00) | 11 (50.00) | |
| Education, n (%) | |||
| Junior high school or below | 19 (86.36) | 16 (72.73) | 0.455 |
| High school or technical secondary school | 3 (13.64) | 6 (27.27) | |
| Drinking history, n (%) | |||
| Yes | 9 (40.91) | 5(19.05) | 0.119 |
| No | 13 (59.09) | 17 (80.95) | |
| Current drinking, n (%) | |||
| Yes | 0 (0.00) | 2 (4.76) | 0.455 |
| No | 22 (100.00) | 20 (95.24) | |
| Smoking history, n (%) | |||
| Yes | 10 (45.45) | 7 (31.82) | 0.353 |
| No | 12 (54.55) | 15 (68.18) | |
| Current smoking, n (%) | |||
| Yes | 4 (18.18) | 4 (18.18) | 1 |
| No | 18 (81.82) | 18 (81.82) | |
| Dietary habit, n (%) | |||
| Carnivorous diet | 1 (4.55) | 1 (9.52) | 0.381 |
| Vegetarian diet | 16 (72.73) | 16 (52.38) | |
| Meat and vegetarian balanced diet | 5 (22.73) | 5 (38.10) | |
| Picky eating, n (%) | |||
| Yes | 4 (18.18) | 2(4.76) | 0.37 |
| No | 18 (81.82) | 20 (95.24) | |
| Exercise frequency, n (%) | |||
| Rarely | 12 (54.55) | 11 (50.00) | 0.576 |
| Sometimes | 9 (40.91) | 8 (36.36) | |
| Often | 1 (4.55) | 3 (13.64) | |
| Dialysis duration, n (%) | |||
| Less than 1 year | 11 (50.00) | 6 (27.27) | 0.183 |
| 1 to 5 years | 7 (31.82) | 7 (31.82) | |
| More than 5 years | 4 (18.18) | 9 (40.91) | |
| History of thyroid disease, n (%) | |||
| Yes | 1 (4.55) | 3 (13.64) | 0.6 |
| No | 21 (95.45) | 19 (86.36) | |
| History of cardiovascular disease, n (%) | |||
| Yes | 6 (27.27) | 3 (13.64) | 0.455 |
| No | 16 (72.73) | 19 (86.36) | |
| History of digestive diseases, n (%) | |||
| Yes | 3 (13.64) | 1 (4.55) | 0.6 |
| No | 19 (86.36) | 21 (95.45) | |
| History of eye disease, n (%) | |||
| No | 11 (50.00) | 3 (13.64) | 0.01 |
| Yes | 11 (50.00) | 19 (86.36) | |
| History of kidney disease, n (%) | |||
| No | 15 (68.18) | 11 (50.00) | 0.33 |
| Kidney stone | 4 (18.18) | 4 (18.18) | |
| Nephritis | 3 (13.64) | 7 (31.82) | |
| History of hypertension, n (%) | |||
| No | 2 (9.09) | 2 (9.09) | 0.422 |
| 1–5 years | 11 (50.00) | 8 (36.36) | |
| 5–10 years | 4 (18.18) | 2 (9.09) | |
| More than 10 years | 5 (22.73) | 10 (45.45) | |
| History of hyperlipidemia, n (%) | |||
| Yes | 4 (18.18) | 4 (18.18) | 1 |
| No | 18 (81.82) | 18 (81.82) | |
| History of gout, n (%) | |||
| Yes | 11 (50.00) | 11 (50.00) | 1 |
| No | 11 (50.00) | 11 (50.00) | |
| Taking calcium supplements | |||
| Yes | 18 (81.82) | 16 (72.73) | 0.472 |
| No | 4 (18.18) | 6 (27.27) | |
| Age (years) | 60.0 (52.8, 66.5) | 57.0 (48.8, 67.0) | 0.411 |
| Weight (kg) | 56.8 (53.1, 68.1) | 57.5 (51.1, 65.4) | 0.865 |
| BMI (kg/m2) | 23.1 (20.8, 24.6) | 22.5 (21.5, 24.4) | 1 |
| Waist (cm) | 82.0 (73.8, 86.8) | 80.75 (76.0, 89.5) | 0.849 |
| Hip (cm) | 88.5 (85.1, 94.5) | 88.5 (84.6, 95.3) | 0.945 |
| Waist-hip ratio | 0.910 (0.9, 1.0) | 0.895 (0.9, 1.0) | 0.822 |
| SBP (mmHg) | 145.0 (128.8, 155.5) | 128.5 (114.3, 144.3) | 0.012 |
| DBP (mmHg) | 79.5 (72.0, 85.3) | 82.0 (61.8, 85.0) | 0.73 |
| FPG (mmol/L) | 11.5 (7.7, 15.3) | 5.7 (5.3, 6.7) | 0.000 |
| Fasting C-peptide (ng/mL) | 9.5 (5.7, 15.7) | 10.8 (6.9, 16.2) | 0.533 |
| Glycosylated hemoglobin (A1C) (%) | 6.9 (6.3, 7.5) | 5.5 (5.1, 5.9) | 0.000 |
| TG (mmol/L) | 1.3 (0.9, 2.1) | 1.4 (1.1, 1.9) | 0.935 |
| TC (mmol/L) | 4.7 (3.9, 5.3) | 3.9 (3.1, 5.0) | 0.123 |
| LDL-C (mmol/L) | 3.2 (2.1, 3.9) | 2.470 (1.7, 3.6) | 0.199 |
| HDL-C (mmol/L) | 0.940 (0.8, 1.2) | 0.895 (0.8, 1.1) | 0.579 |
| Na (mmol/L) | 139.735 (136.5, 141.1) | 140.350 (137.6, 142.4) | 0.139 |
| K (mmol/L) | 5.090 (4.6, 5.3) | 5.0 (3.9, 5.6) | 0.725 |
| Cl (mmol/L) | 1.425 (98.0, 102.2) | 101.510 (99.6, 105.6) | 0.119 |
| Ca (mmol/L) | 2.210 (2.0, 2.3) | 2.225 (2.2, 2.3) | 0.672 |
| P (mmol/L) | 1.690 (1.3, 1.9) | 2.425 (1.9, 2.9) | 0.002 |
| AST (IU/L) | 12.3 (8.5, 17.3) | 12.935 (8.2, 16.2) | 1 |
| ALT (U/L) | 10.930 (6.6, 15.0) | 12.380 (8.2, 16.8) | 0.253 |
| GGT (U/L) | 18.770 (12.8, 28.7) | 21.710 (16.3, 35.5) | 0.162 |
| ALP (U/L) | 78.340 (60.9, 105.4) | 74.830 (62.2, 86.5) | 0.466 |
| Total albumin (g/L) | 67.870 (64.2, 70.8) | 68.010 (65.0, 69.7) | 0.789 |
| Albumin (g/L) | 38.870 (37.6, 40.8) | 40.155 (39.2, 41.5) | 0.162 |
| Globulin (g/L) | 29.0 (25.7, 31.0) | 27.950 (23.2, 29.7) | 0.181 |
| Pre-albumin (mg/L) | 280.0 (206.5, 331.0) | 328.5 (280.3, 356.5) | 0.042 |
| TBIL (μmol/L) | 4.930 (4.1, 6.1) | 6.250 (4.6, 8.2) | 0.068 |
| DBIL (μmol/L) | 1.8 (1.3, 2.0) | 2.060 (1.7, 2.6) | 0.082 |
| IBIL (μmol/L) | 3.1 (2.7, 4.2) | 4.150 (3.0, 5.2) | 0.117 |
| TBA (μmol/L) | 2.930 (1.6, 6.1) | 2.915 (1.8, 3.7) | 0.593 |
| Serum Cr (μmol/L) | 791.930 (559.1, 1,117.1) | 1,132.190 (11.3, 16.6) | 0.004 |
| BUN (mmol/L) | 21.710 (16.5, 27.2) | 23.760 (18.8, 28.1) | 0.313 |
| Glomerular filtration rate GFR | 5.315 (3.6, 7.4) | 3.055 (2.4, 3.8) | 0.002 |
| UA (μmol/L) | 373.635 (342.0, 459.5) | 454.935 (387.9, 515.2) | 0.024 |
| Cystatin C (mg/L) | 6.865 (6.3, 7.3) | 7.225 (6.5, 8.7) | 0.253 |
| CO2 combining power (mmol/L) | 24.280 (20.1, 25.1) | 21.050 (18.4, 25.0) | 0.215 |
| RBC (1012/L) | 3.730 (3.5, 4.4) | 4.185 (3.7, 4.6) | 0.149 |
| Hb (g/L) | 105.5 (93.5, 112.0) | 107.5 (99.8, 122.8) | 0.366 |
| WBC (109/L) | 5.755 (5.0, 6.8) | 6.075 (3.8, 6.6) | 0.734 |
| PLT (109/L) | 176.0 (156.8, 211.0) | 171.0 (129.5, 222.0) | 0.565 |
| PTH (pmol/L) | 16.370 (6.0, 34.6) | 24.4 (14.5, 39.3) | 0.178 |
| β2 microglobulin (μg/L) | 19,861.280 (16,686.5, 258.0) | 26,835.260 (22,584.1, 28,808.5) | 0.018 |
| Folate (ng/mL) | 17.4 (5.2, 40.0) | 40.0 (4.8, 40.0) | 0.789 |
| Ferritin (ng/mL) | 141.060 (37.0, 229.0) | 51.5 (21.7, 106.7) | 0.024 |
| Hs CRP (mg/L) | 0.7 (0.2, 4.6) | 0.6 (0.2, 2.0) | 0.5 |
| PINP (ng/mL) | 282.75 (192.8, 422.6) | 347.5 (305.3, 652.4) | 0.183 |
Measurement data are expressed as median (5% CI, 95% CI), and P<0.05 indicated a statistical difference. BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; TG, total triglyceride; TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; AST, aspartate aminotransferase; ALT, alanine aminotransferase; GGT, gamma-glutamyl transpeptidase; ALP, alkaline phosphatase; TBIL, total bilirubin; DBIL, direct bilirubin; IBIL, indirect bilirubin; TBA, total bile acid; Cr, creatinine; BUN, blood urea nitrogen; UA, uric acid; RBC, red blood cell; Hb, hemoglobin; WBC, white blood cell; PLT, platelet; PTH, parathyroid hormone; Hs CRP, hypersensitive C-reactive protein; PINP, propeptide of Type I procollagen.
OUT (operational taxonomic units) cluster analysis
A total of 44 samples were sequenced for high-throughput sequencing, and the abundance information of each sample in each OUT was counted. The abundance of each OUT indicated the species richness of the sample. In the figure, different color graphs represent different groups: DD represents the diabetic group, EE represents the non-diabetic group, and the overlap between different color graphs represents the common OUT number between the two groups. The results showed that 810 OUT species were unique to the diabetic group and 319 OUT species were unique to the non-diabetic group, and there were 1,200 OUT species in both groups. The abundance of OUT in the diabetic group was higher than that in the non-diabetic group, and there were different strains in the two groups. Therefore, the corresponding core microorganisms under different conditions were identified (Figure 1).
Figure 1.

Venn diagram Red is the diabetic group and blue is the non-diabetic group. DD, diabetic group; EE, non-diabetic group.
Sample complexity analysis
Dilution curves (Figure 2) were used to test whether the sample met the requirements of experimental sampling volume. When the amount of data randomly extracted in this study was 30,000, the curve gradually tended to balance, so the amount of sequencing data in this study was reasonable. The hierarchical clustering curve (Figure 3) indicated that the samples were rich in species, and the descending smoothing indicated that the species were evenly distributed. The cumulative box diagram (Figure 4) showed that when the sample size of this study was 44, the curve tended to be gentle, indicating that the sample size was sufficient.
Figure 2.

Dilution curves. The abscissa represents the amount of sequencing data, the ordinate represents the number of observed OUT, and curves in different colors represent different samples. OUTs, operational taxonomic units.
Figure 3.

Hierarchical clustering curves. Different color curves represent different samples, the abscissa represents different OUT, and the ordinate represents abundance. Different colored curves represent different samples. OUT, operational taxonomic unit.
Figure 4.
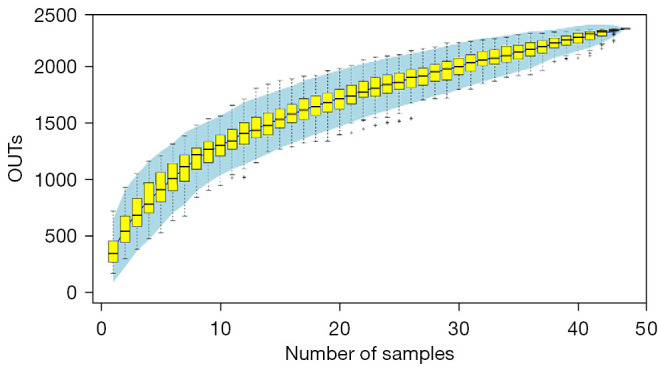
Cumulative box diagram. The abscissa represents the extracted sample number. The ordinate represents the corresponding OUT number. OUT, operational taxonomic unit.
α-diversity analysis
The difference in α diversity index between the two groups was analyzed (Table 2). Observed species and Chao1 results showed that the species in the diabetic group were more abundant than those in the non-diabetic group, and the difference was statistically significant. Ace results indicated that the species richness of the diabetic group was higher than that of the non-diabetic group, but there was no statistical difference. Shannon and PD whole tree results suggested that the diversity of bacterial colonies was higher in the diabetic group than in the non-diabetic group, and the difference was statistically significant. Simpson and Coverage results indicated that the diversity of bacterial colonies was higher in the diabetic group than in the non-diabetic group, but there was no statistical difference. Overall, species abundance was higher in the diabetic group than in the non-diabetic group.
Table 2. Comparison of α diversity parameters between the diabetic and non-diabetic groups.
| Indicators | Diabetes (n=22) | Non-diabetes (n=22) | P value |
|---|---|---|---|
| Shannon | 4.324 (3.5, 5.4) | 3.426 (2.7, 4.6) | 0.074 |
| Simpson | 0.887 (0.8, 0.9) | 0.780 (0.7, 0.9) | 0.074 |
| Ace | 440.248 (371.4, 557.2) | 370.577 (317.2, 485.4) | 0.057 |
| Goods_coverage | 0.998 (1.0, 1.0) | 0.999 (1.0, 1.0) | 0.06 |
| Chao1 | 419.537 (364.0, 532.2) | 351.877 (319.2, 478.2) | 0.041* |
| Observed species | 335.000 (294.3, 474.5) | 267.500 (218.0, 385.5) | 0.030* |
| PD whole tree | 27.619 (24.9, 33.3) | 24.775 (23.3, 29.3) | 0.049* |
All data were expressed as median M (P25, P75), and P<0.05 indicated a statistical difference. *, P<0.05. PD, phylogenetic diversity.
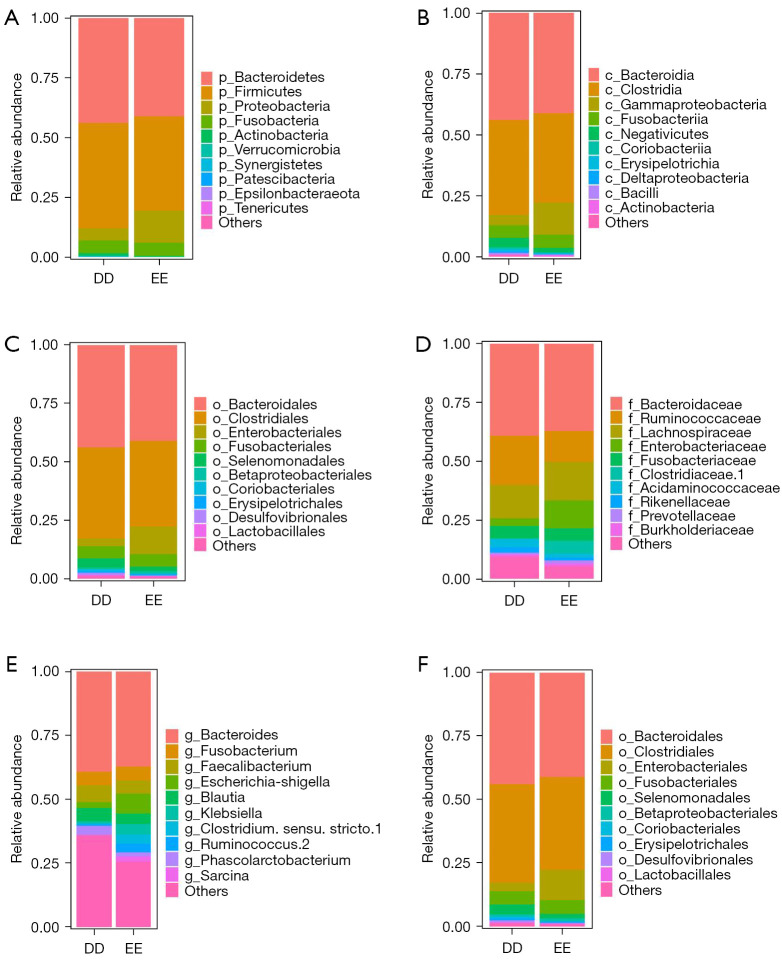
Species composition
According to the taxonomic level, the phylum, class, order, family, genus, and species were plotted on the same horizontal species distribution map, generating the relative abundance map of species. Figure 5 shows two groups of highly abundant species at different levels. At the level of phyla classification, the proportion of Firmicutes in the diabetic group was the highest, followed by Bacteroidetes, Fusobacteria, and Proteobacteria. In the non-diabetic group, the proportion of Bacteroidetes was the highest, followed by Firmicutes, Proteobacteria, and Clostridium. Small amounts of Actinobacteria and Verrucomicrobia were also detected in both groups. The increased ratio of Firmicutes to Bacteroidetes is closely related to the inflammatory status of the body. In this study, the ratio of Firmicutes to Bacteroidetes in the diabetic group was greater than 1, while the ratio of Firmicutes to Bacteroidetes in the non-diabetic group was less than 1. At the level of genus classification, Bacteroidia accounted for the highest proportion in both groups. Table 3 shows the relative abundance of two groups of species with high abundance at different taxonomic levels. Figure 6 shows the clustering heat map at the gate classification level. The results showed that the relative abundance of species was different between the two groups at different classification levels.
Figure 5.
Histogram of the relative abundance of the two groups of strains with high abundance at different levels. (A) Phylum, (B) class, (C) order, (D) family, (E) genus, (F) species. DD group, diabetic group; EE group, non-diabetic group.
Table 3. Relative abundance of species with different taxonomic levels in the diabetic and non-diabetic groups.
| Taxonomic rank | Bacterial strain | Diabetic group | Non-diabetic group |
|---|---|---|---|
| Phylum | Bacteroidetes | 0.439 | 0.412 |
| Firmicutes | 0.440 | 0.393 | |
| Proteobacteria | 0.050 | 0.134 | |
| Fusobacteria | 0.052 | 0.054 | |
| Actinobacteria | 0.011 | 0.004 | |
| Verrucomicrobia | 0.004 | 0.001 | |
| Others | 0.001 | 0.001 | |
| Patescibacteria | 0.000 | 0.000 | |
| Tenericutes | 0.000 | 0.000 | |
| Epsilonbacteraeota | 0.000 | 0.000 | |
| Synergistetes | 0.001 | 0.000 | |
| Class | Bacteroidia | 0.439 | 0.412 |
| Clostridia | 0.389 | 0.366 | |
| Gammaproteobacteria | 0.041 | 0.131 | |
| Fusobacteriia | 0.052 | 0.054 | |
| Negativicutes | 0.039 | 0.019 | |
| Erysipelotrichia | 0.007 | 0.005 | |
| Actinobacteria | 0.003 | 0.003 | |
| Bacilli | 0.005 | 0.003 | |
| Others | 0.007 | 0.003 | |
| Deltaproteobacteria | 0.008 | 0.002 | |
| Coriobacteriia | 0.008 | 0.001 | |
| Order | Bacteroidales | 0.439 | 0.412 |
| Clostridiales | 0.389 | 0.366 | |
| Enterobacteriales | 0.033 | 0.118 | |
| Fusobacteriales | 0.052 | 0.054 | |
| Selenomonadales | 0.039 | 0.019 | |
| Betaproteobacteriales | 0.008 | 0.011 | |
| o_Others | 0.012 | 0.009 | |
| Erysipelotrichales | 0.007 | 0.005 | |
| Desulfovibrionales | 0.008 | 0.002 | |
| Lactobacillales | 0.004 | 0.002 | |
| Coriobacteriales | 0.008 | 0.001 | |
| Family | Bacteroidaceae | 0.393 | 0.373 |
| Lachnospiraceae | 0.140 | 0.162 | |
| Ruminococcaceae | 0.209 | 0.132 | |
| Enterobacteriaceae | 0.033 | 0.118 | |
| Others | 0.097 | 0.055 | |
| Clostridiaceae 1 | 0.003 | 0.054 | |
| Fusobacteriaceae | 0.052 | 0.054 | |
| Acidaminococcaceae | 0.036 | 0.016 | |
| Rikenellaceae | 0.021 | 0.013 | |
| Prevotellaceae | 0.007 | 0.012 | |
| Burkholderiaceae | 0.008 | 0.011 | |
| Genus | Bacteroides | 0.393 | 0.373 |
| Others | 0.359 | 0.256 | |
| Escherichia-Shigella | 0.023 | 0.077 | |
| Fusobacterium | 0.052 | 0.054 | |
| Faecalibacterium | 0.065 | 0.052 | |
| Blautia | 0.052 | 0.042 | |
| Klebsiella | 0.010 | 0.041 | |
| Ruminococcus 2 | 0.006 | 0.035 | |
| Clostridium sensu stricto 1 | 0.003 | 0.034 | |
| Sarcina | 0.000 | 0.020 | |
| Phascolarctobacterium | 0.036 | 0.016 | |
| Species | Others | 0.337 | 0.262 |
| Uncultured bacterium | 0.161 | 0.230 | |
| Bacteroides dorei | 0.183 | 0.132 | |
| Uncultured organism | 0.181 | 0.130 | |
| Escherichia coli | 0.023 | 0.077 | |
| Bacteroides thetaiotaomicron | 0.027 | 0.049 | |
| Uncultured Bacteroides sp. | 0.008 | 0.045 | |
| Klebsiella variicola | 0.010 | 0.041 | |
| Bacteroides ovatus V975 | 0.026 | 0.019 | |
| Human gut metagenome | 0.020 | 0.013 | |
| Gut metagenome | 0.023 | 0.003 |
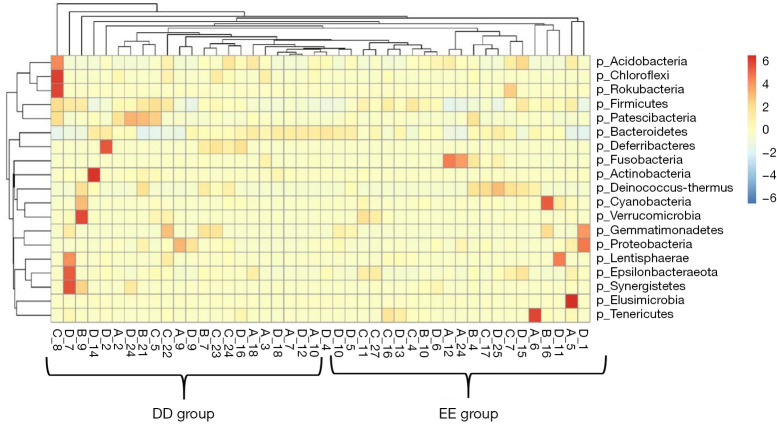
Figure 6.
Cluster heat map of differential enrichment among groups of all samples at the phylum level. The abscissa is the sample and the ordinate is the differential strain. DD group, diabetic group; EE group, non-diabetic group.
β-diversity analysis
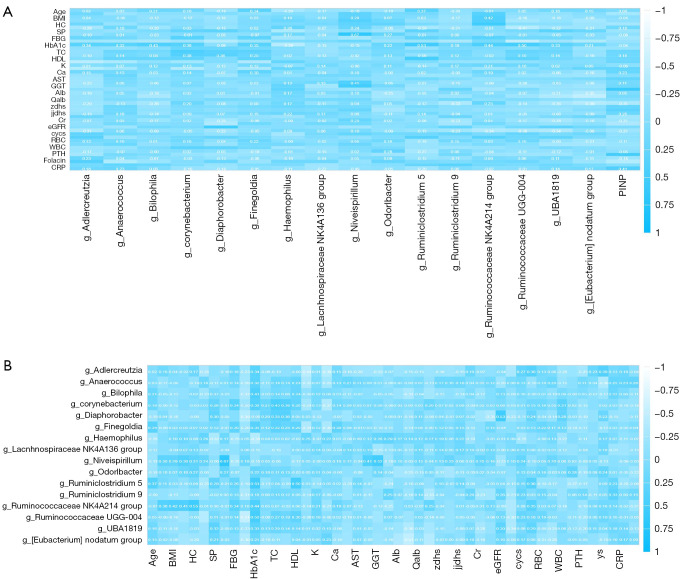
The UniFrac distance method was used to analyze whether there was a statistical difference in the intestinal flora offset between the two groups. As shown in Figure 7, PC1 and PC2 showed a significant separation trend, and PC1 could explain 59.89% of the difference while PC2 could explain 12.65% of the difference. The figure shows differences in the flora between the two groups.
Figure 7.
Correlation analysis between clinical indicators and different microflora. (A) Correlation diagram between personal history and different strains. (B) Correlation diagram with clinical test indicators and different strains. BMI, body mass index; HC, hemoglobin concentration; SP, systolic pressure, FBG, fasting blood glucose; HbA1c, glycosylated hemoglobin, Type A1C; TC, total cholesterol; HDL, high density lipoprotein cholesterol; AST, aspartate aminotransferase; GGT, gamma-glutamyl transpeptidase; Cr, creatinine; eGFR, estimated glomerular filtration rate; RBC, red blood cell; WBC, white blood cells; PTH, parathyroid hormone; CRP, hypersensitive C-reactive protein; PINP, propeptide of Type I procollagen.
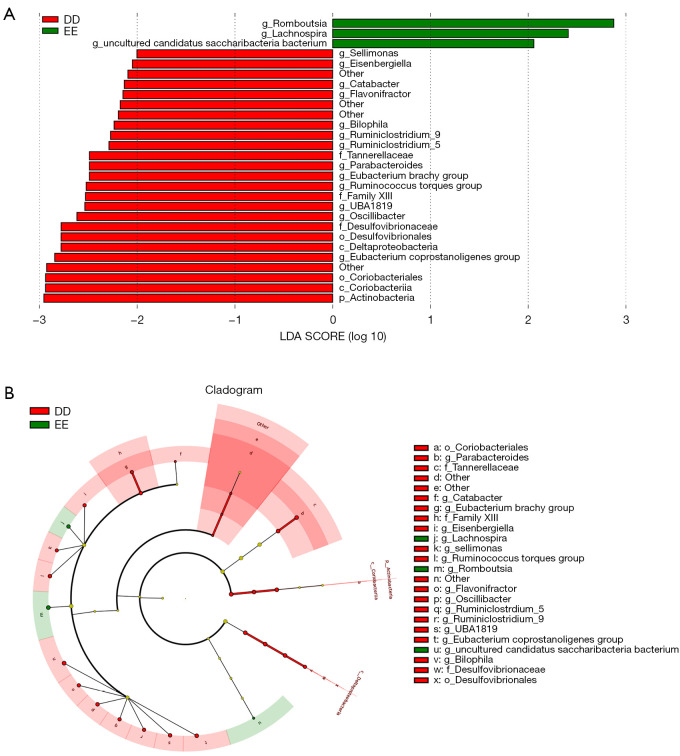
Differential species analysis
Figure 8 shows the different microflora between the two groups. A total of 23 types of bacteria were different between the two groups, including 1 phylum, 2 classes, 2 orders, 2 families, and 16 genera. At the genus level, there were more Romboutsia bacteria, Helicobacter pilosa, and Candidatus Saccharibacteria bacterium in the non-diabetic group. More Actinobacteria, Coriobacteriia, Deltaproteobacteria, Coriobacteriales, Desulfovibrionales, Desulfovibrionaceae, Family XIII, Tannerellaceae, g_Sellimonas, Sellimonas genus, Ruminococcus, Parabacteroides, Oscillibacter, UBA1819, Ruminiclostridium 5, Ruminiclostridium 9, Bilophila, Flavonifractor, Catabacter, Eisenbergiella, and Eubacterium were found in the diabetic group. These different bacteria may be the dangerous strains causing uremia in patients with DKD.
Figure 8.
LEfSe diagram (A) and evolutionary tree (B) of dominant bacteria in the two groups. DD group, diabetic group; EE group, non-diabetic group; LDA, Linear discriminant analysis.
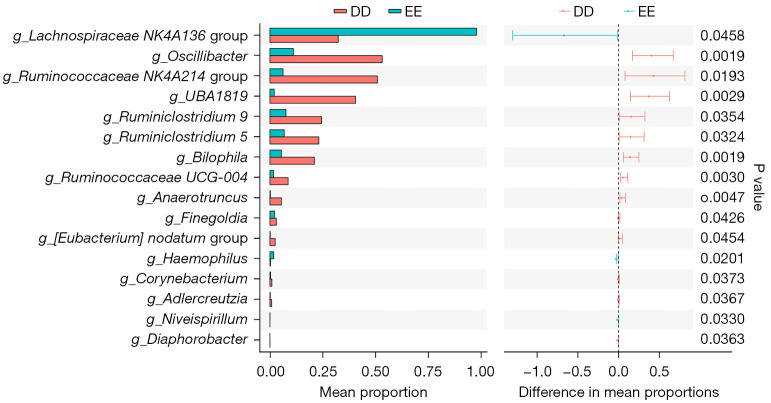
The t-test was used to find species with significant differences (P<0.05) (Table 4 and Figure 9). The different strains were mainly Oscillibacter, Bilophila, UBA1819, Ruminococcaceae UCG-004, Anaerotruncus, Ruminococcaceae NK4A214, Haemophilus, Ruminiclostridium 5, Niveispirillum, Ruminiclostridium 9, Diaphorobacter, Adlercreutzia, Corynebacterium, Finegoldia, Eubacterium Nodatum, and Lachnospiraceae NK4A136.
Table 4. Species with significant differences between the diabetic and non-diabetic groups.
| Strain | Relative abundance in the diabetic group | Relative abundance in the non-diabetic group | P value | Differentials | Lower 95% CI | Upper limit of 95% CI |
|---|---|---|---|---|---|---|
| g_Oscillibacter | 0.532 | 0.111 | 0.002 | 0.421 | 0.171 | 0.671 |
| g_Bilophila | 0.211 | 0.054 | 0.002 | 0.157 | 0.063 | 0.250 |
| g_UBA1819 | 0.406 | 0.020 | 0.003 | 0.386 | 0.147 | 0.625 |
| g_Ruminococcaceae UCG-004 | 0.086 | 0.017 | 0.003 | 0.069 | 0.026 | 0.113 |
| g_Anaerotruncus | 0.054 | 0.002 | 0.005 | 0.052 | 0.018 | 0.087 |
| g_Ruminococcaceae NK4A214 group | 0.510 | 0.062 | 0.019 | 0.447 | 0.080 | 0.815 |
| g_Haemophilus | 0.003 | 0.018 | 0.020 | 0.015* | 0.028* | 0.003* |
| g_Ruminiclostridium 5 | 0.232 | 0.068 | 0.032 | 0.164 | 0.015 | 0.314 |
| g_Niveispirillum | 0.000 | 0.001 | 0.033 | 0.001* | 0.001* | 0.000* |
| g_Ruminiclostridium 9 | 0.244 | 0.076 | 0.035 | 0.168 | 0.012 | 0.324 |
| g_Diaphorobacter | 0.000 | 0.000 | 0.036 | 0.000 | 0.000 | 0.001 |
| g_Adlercreutzia | 0.008 | 0.002 | 0.037 | 0.007 | 0.000 | 0.013 |
| g_Corynebacterium | 0.009 | 0.003 | 0.037 | 0.006 | 0.000 | 0.012 |
| g_Finegoldia | 0.030 | 0.022 | 0.043 | 0.009 | 0.000 | 0.017 |
| g_Eubacterium Nodatum group | 0.025 | 0.001 | 0.045 | 0.023 | 0.001 | 0.046 |
| g_Lachnospiraceae NK4A136 group | 0.324 | 0.980 | 0.046 | 0.656* | 1.298* | 0.013* |
*, P value is less than 0.05. CI, confidence interval.
Figure 9.
Genera with significant differences as determined by the t-test. DD group, diabetic group; EE group, non-diabetic group.
Correlation analysis was conducted between the above-mentioned different species and clinical indicators, and a heat map was drawn, as shown in Figure 9. The results showed that there was a negative correlation between alcohol consumption in personal medical history and g_Niveispirillum bacteria. Smoking in personal medical history was positively correlated with g_Finegoldia, g_Lachnospiraceae NK4A136 group, and g_Ruminococcaceae NK4A214. There was a positive correlation between meat and vegetable consumption and g_Anaerococcus. Picky eaters were negatively correlated with g_Diaphorobacter and positively correlated with g_Ruminococcaceae NK4A214 group. Dialysis duration was positively correlated with g_Ruminococcaceae NK4A214 group and g_Eubacterium Nodatum group. Previous cardiovascular history was negatively associated with g_Ruminiclostridium 9. History of eye disease was negatively correlated with g_Bilophila, g_Diaphorobacter, g_Ruminococcace AEucG-004, and g_UBA1819. There was a significant positive correlation between history of hyperlipidemia and g_Corynebacterium. There was a significant negative correlation between lipid and g_Haemophilus. History of diabetes was negatively correlated with g_Bilophila. Diabetes and g_Bilophila, g_Diaphorobacter, g_Niveispirillum, g_Ruminiclostridium 5, g_Ruminiclostridium 9, g_Ruminococcace AEucG-004, g_UBA1819, and g_Eubacterium Nodatum group were significantly correlated, while history of gout was positively correlated with g_Ruminiclostridium 9 and g_Eubacterium Nodatum group.
Relationship between clinical indicators and microflora of the two groups
Blood HbA1C was positively correlated with g_Bilophila, g_Corynebacterium, g_Finegoldia, g_Ruminiclostridium 5, g_Ruminococcaceae NK4A214 group, and g_Ruminococcaceae UCG-004, but negatively correlated with g_Haemophilus and g_Corynebacterium. Serum cholesterol was positively correlated with g_Corynebacterium, g_Diaphorobacter, and g_Finegoldia. LDL-C was positively correlated with g_Corynebacterium and g_Diaphorobacter. HDL-C was positively correlated with g_Ruminiclostridium 5. BUN was negatively correlated with g_Diaphorobacter. eGFR was positively correlated with g_Diaphorobacter and g_UBA1819. Uric acid (UA) was negatively correlated with g_Adlercreutzia, g_Ruminococcaceae NK4A214 group, g_Ruminococcaceae UCG-004, and g_UBA1819.
Discussion
The gut-kidney axis theory holds that the intestine and kidney are closely related in substance metabolism, immunity, inflammatory response, intestinal mucosal barrier, and intestinal bacterial structure and function. The continuous decline of GFR in DKD patients leads to the accumulation of a large amount of metabolic waste in the body, which cannot be excreted through the kidney, but is excreted through the intestinal wall and affects the intestinal tract. Therefore, the intestinal environment is disturbed and the balance of intestinal flora is aggravated. Recent studies (25,31) have found that changes in the quantity and quality of the intestinal microbiome can be observed in both DKD and ESRD patients, which vary significantly in different stages of disease, different individuals, and different comorbidities. Therefore, understanding the structure, function, and related influencing factors of intestinal flora in DKD patients and identifying its role in the occurrence and progression of ESRD will help guide the early screening and diagnosis of DKD and facilitate the development of new targets for ESRD treatment based on microecological reconstruction.
Gut microbiota is closely related to the occurrence and development of type 2 diabetes mellitus (T2DM) (33). Gut microbiota and its metabolites, such as short chain fatty acids (SCFA), not only participate in the host’s physiological and metabolic regulation (34,35), but also regulate the immune response in the gut, so that immune cells can respond faster to infection (36), and maintain the intestinal homeostasis (37). Intestinal flora is an important factor in the environmental factors of diabetes (38). Changes in the structure of intestinal flora and imbalance of intestinal flora can lead to the occurrence of diabetes (39). In pre diabetes and T2DM patients, the bacterial abundance of butyrate production and the functional potential of butyrate production are reduced. In addition, insulin resistance is closely related to microbial variation (40). After intestinal flora imbalance, the beneficial metabolites produced by intestinal flora such as short chain fatty acids (SCFA) and bile acids (BAS) are reduced. SCFA and bas play an important role in maintaining blood glucose homeostasis, improving IR and reducing inflammatory response (41,42), while lipopolysaccharide and peptidoglycan (PG) are increased. After ingestion into the blood, they enhance the activation of Toll like receptor-4 (TLR-4) and other inflammatory signal pathways, leading to systemic inflammatory response, thus further promoting IR and T2DM (43). Metformin is the cornerstone of T2DM treatment. Firmicutes were decreased and SCFA-producing bacteria abundance increased in T2DM patients treated with metformin compared with placebo (44). Dipeptidyl peptidase 4 (DPP-4) inhibitors can also change the composition and activity of intestinal microbiota in C57BL/6J mice, inhibit the growth of O. verericigenes, increase Lactobacillus, and decrease toll-like receptor 2 (TLR2) and toll-like receptor 4 (TLR4) (45). Proteobacteria abundance in diabetic mice was significantly increased after treatment with dapagliflozin, which has renal protective effects (46). However, after insulin treatment, the number of aerobic bacteria in the intestinal tract of T2DM patients decreased, while the number of anaerobic bacteria increased (47). After metabolic surgery for T2DM patients, decreased blood glucose was associated with increased abundance and diversity of Bacteroides (48). In basic experiments, after fecal bacteria transplantation (FMT) treatment, vibrio desulphurization was reduced and A. muciniphila increased compared with placebo in mice (49). The hypoglycemic mechanisms of drug therapy, insulin therapy, surgical therapy, and microbiota transplantation therapy based on intestinal microecological reconstruction are different, and changes in the abundance and diversity of microbiota can also be observed. In our study, all patients in the DKD group were treated with insulin, which avoided the influence of different drug treatments on experimental results. Compared with the NDKD group without insulin treatment, the intestinal flora abundance was statistically different. These findings indicate that the intestinal flora of T2DM or DKD patients might be correlated with blood glucose treatment.
In this study, personal history, including alcohol consumption, smoking, and dietary habits, was found to be correlated with some bacterial genera. Past cardiovascular history was negatively correlated with g_Ruminiclostridium 9. History of eye disease was negatively correlated with g_Bilophila, g_Diaphorobacter, g_Ruminococcaceae G-004, and g_UBA1819. History of hyperlipidemia was positively and significantly correlated with g_Corynebacterium. Lipid level was negatively correlated with g_Haemophilus. History of gout was negatively correlated with g_Ruminiclostridium 9 and g_Eubacterium Nodatum group. Although the above results showed that there was a statistically significant correlation between the disease and the microflora, further research is needed to determine whether this correlation is only a phenomenon of uremia combined with diabetes, or a phenomenon of personal history and other diseases themselves.
Studies have shown that some important pathogenic bacteria proliferate abnormally in DKD and ESRD, such as Klebsiella pneumoniae, Acinetobacter, Enterobacter, and Legionella (27,35,50-54). Dysregulation of intestinal flora and related changes in host metabolism and inflammation may determine the development of DKD and ESRD (55). In an animal experiment, it was found that intestinal flora of DKD mice showed an abnormal Firmicutes/Bacteroides ratio, Allobaculum and Anaerosporobacter could worsen GFR, and Blautia could act as a protective factor of DKD (56). Study has examined that Prevotella and Lactobacillus were decreased in the intestinal flora of DKD patients, while Fusobacteria were increased (57). Our study also found a similar situation, in which the proportion of Firmicutes in the DKD group was the highest, followed by Bacteroidetes, Clostridium, and Proteobacteria, while the proportion of Bacteroidetes in the NDKD group was the highest, followed by Firmicutes, Proteobacteria, and Clostridium. In this study, the ratio of Firmicutes/Bacteroidetes in the DKD group was greater than 1, while that in the NDKD group was less than 1. The main differences between the two groups were g_Odoribacter, g_Ruminiclostridium, g_Adlercreutzia, g_Lachnospiraceae, NK4A136 group, g_Ruminococcaceae (Ruminococcus) NK4A214 group, Oscillibacter, Bilophila, UBA1819, Ruminococcaceae UCG-004, Anaerotruncus, and Ruminococcaceae NK4A214, among others. The increased ratio of Firmicutes to Bacteroidetes aggravated the inflammatory response of the host. Closely related to the production of SCFA are g_Odoribacter, g_Ruminiclostridium, g_Adlercreutzia, and g_Lachnospiraceae NK4A136. Changes in the abundance of this set and g_Ruminococcaceae (Ruminococcus) NK4A214 group accelerated the process of the disease.
The species abundance of flora in patients with diabetes nephropathy is higher than that in patients with non-diabetes nephropathy. It is mainly caused by the imbalance of intestinal flora, which is manifested by the increase in the species and number of conditional pathogens. Research shows that the abnormal proliferation of conditional pathogens, such as Klebsiella pneumoniae, Acinetobacter, Enterobacter and Legionella, aggravates the host’s inflammatory response (58). G_ Odoribacter, g_ ruminiclorstridium, g_ Adlercreutzia and G_ LachnospiraceaeNK4A136. The increase of this group and g_u_ruminococcaceae nk4a214 group accelerated the process of DKD (59). In prediabetes, or impaired glucose tolerance (IGT), researchers observed a significant decrease in Clostridium (60) and butyric-producing bacteria (39) in the intestinal flora, while there was an increase in Dolella. When T2DM was advanced, researchers found that the intestinal flora of rats changed from enrichment of Firmicutes to enrichment of Bacteroidetes (61). At this time, the intestinal flora was characterized by an increase in the abundance of Bacteroidetes and a decrease in the abundance of Firmicutes (62,63). At the DKD stage, compared with the T2DM group alone, the intestinal flora of patients showed a significant increase in the abundance of Proteobacteria and Spironella (64). Gut microbiota levels were significantly higher in T2DM patients than in the normal group when 16S rDNA testing was performed (65). In our study, the α diversity analysis of the two groups showed similar results. Compared with the NDKD group, the abundance of the DKD group was higher. There were more Actinobacteria, Coriobacteriia, Deltaproteobacteria, Coriobacteriales, Desulfovibrionales, Desulfovibrionaceae, Family XIII, Tannerellaceae, g_Sellimonas, Sellimonas, Ruminococcus, Parabacteroides, Oscillibacter, UBA1819, Ruminiclostridium 5, Ruminiclostridium 9, Bilophila, Flavonifractor, Catabacter, Eisenbergiella, and Eubacterium. It is suggested that these might be the dangerous strains of ESRD caused by DKD, and hyperglycemia may change the characteristics of the bacterial community of DKD patients.
The imbalance of intestinal flora and DKD can influence each other, but the mechanism is not clear. The renin-angiotensin system (RAS) is a key factor in the development of DKD (66). Study has shown that intestinal flora can activate local and systemic RAS, and the cascade reaction further aggravates renal injury, resulting in irreversible damage of DKD, which progresses to ESRD (67). Chronic inflammatory responses play an important role in the progression of DKD. Lipopolysaccharide (LPS) is the surface antigen of gram-negative bacteria, which plays a strong inflammatory and immune activation role through TLR2 and TLR4-related pathways, and participates in mediating the inflammatory response of the host. LPS was closely correlated with DKD and ESRD (68). Reduced production of SCFAs also aggravates kidney damage in DKD. The disturbance of intestinal flora affects SCFAs of the host, inhibits the activation of G-protein coupled receptor 41 (GPCR41) and GPCR43, affects the release of peptide tyrosine tyrosine (PYY) and glucagon-like peptide 1 (GLP-1), and thus affects the process of DKD (69). In our experiment, we found that in ESRD patients, the strains were different between the DKD and NDKD groups through cross-sectional matching and 16S rDNA detection of gut microorganisms: Oscillibacter, Bilophila, UBA1819, Ruminococcaceae UCG-004, Anaerotruncus, Ruminococcaceae NK4A214 group, Haemophilus, Ruminiclostridium 5, Niveispirillum, Ruminiclostridium 9, Diaphorobacter, Adlercreutzia, Corynebacterium, Finegoldia, and Lachnospiraceae, among others. Corynebacterium, one of the most clinically important non-thermally sensitive Corynebacteria, can cause different forms of infection, especially in patients with potential risk factors and comorbidities (including immunocompromised subjects) that are associated with continuous dialysis treatment (70). Lachnospiraceae was negatively correlated not only with the increase of renal function index and serum metabolites, but also strongly negatively correlated with serum creatinine and positively correlated with eGFR (P<0.05) (71). The abundance of Lachnospiraceae was significantly increased in ESRD patients with periodontal disease. In addition, other study has shown that this strain is also significantly elevated in patients with renal fibrosis (72). The anomalies of the above strains deserve further investigation.
In conclusion, 16S rDNA sequencing technology was used in this study to analyze the characteristics of intestinal flora in ESRD patients with or without diabetes. We found that there was a significant difference in the intestinal flora of ESRD patients caused by DKD and NDKD, including 1 phylum, 2 classes, 2 orders, 2 families, and 16 genera. The strains with the greatest differences were Oscillibacter, Bilophila, UBA1819, Ruminococcaceae UCG-004, Anaerotruncus, and Ruminococcaceae NK4A214. However, due to the limited number of subjects in this study, and because this was only a cross-sectional study, larger sample clinical studies are still needed for verification and to find the key microbiota that cause the progression of DKD into ESRD.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: This study was supported by Key-Area Research and Development Program of Guangdong Province, China (No. 2019B020230001).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Jinxia Community Health Service Centre (No. JXSQ2021003) and informed consent was taken from all individual participants.
Footnotes
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at https://atm.amegroups.com/article/view/10.21037/atm-22-2926/rc
Data Sharing Statement: Available at https://atm.amegroups.com/article/view/10.21037/atm-22-2926/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-2926/coif). The authors have no conflicts of interest to declare.
References
- 1.Chen TK, Knicely DH, Grams ME. Chronic Kidney Disease Diagnosis and Management: A Review. JAMA 2019;322:1294-304. 10.1001/jama.2019.14745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA 2007;298:2038-47. 10.1001/jama.298.17.2038 [DOI] [PubMed] [Google Scholar]
- 3.Zhang L, Wang F, Wang L, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet 2012;379:815-22. 10.1016/S0140-6736(12)60033-6 [DOI] [PubMed] [Google Scholar]
- 4.Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004;351:1296-305. 10.1056/NEJMoa041031 [DOI] [PubMed] [Google Scholar]
- 5.Seliger SL, Gillen DL, Longstreth WT, Jr, et al. Elevated risk of stroke among patients with end-stage renal disease. Kidney Int 2003;64:603-9. 10.1046/j.1523-1755.2003.00101.x [DOI] [PubMed] [Google Scholar]
- 6.Stengel B. Chronic kidney disease and cancer: a troubling connection. J Nephrol 2010;23:253-62. [PMC free article] [PubMed] [Google Scholar]
- 7.Kurella Tamura M, Xie D, Yaffe K, et al. Vascular risk factors and cognitive impairment in chronic kidney disease: the Chronic Renal Insufficiency Cohort (CRIC) study. Clin J Am Soc Nephrol 2011;6:248-56. 10.2215/CJN.02660310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tonelli M, Wiebe N, Culleton B, et al. Chronic kidney disease and mortality risk: a systematic review. J Am Soc Nephrol 2006;17:2034-47. 10.1681/ASN.2005101085 [DOI] [PubMed] [Google Scholar]
- 9.Jazani NH, Savoj J, Lustgarten M, et al. Impact of Gut Dysbiosis on Neurohormonal Pathways in Chronic Kidney Disease. Diseases 2019;7:21. 10.3390/diseases7010021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thursby E, Juge N. Introduction to the human gut microbiota. Biochem J 2017;474:1823-36. 10.1042/BCJ20160510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Costea PI, Hildebrand F, Arumugam M, et al. Enterotypes in the landscape of gut microbial community composition. Nat Microbiol 2018;3:8-16. 10.1038/s41564-017-0072-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ochoa-Repáraz J, Kasper LH. The Second Brain: Is the Gut Microbiota a Link Between Obesity and Central Nervous System Disorders? Curr Obes Rep 2016;5:51-64. 10.1007/s13679-016-0191-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yatsunenko T, Rey FE, Manary MJ, et al. Human gut microbiome viewed across age and geography. Nature 2012;486:222-7. 10.1038/nature11053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.David LA, Maurice CF, Carmody RN, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 2014;505:559-63. 10.1038/nature12820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arumugam M, Raes J, Pelletier E, et al. Enterotypes of the human gut microbiome. Nature 2011;473:174-80. 10.1038/nature09944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Le Chatelier E, Nielsen T, Qin J, et al. Richness of human gut microbiome correlates with metabolic markers. Nature 2013;500:541-6. 10.1038/nature12506 [DOI] [PubMed] [Google Scholar]
- 17.Yang T, Santisteban MM, Rodriguez V, et al. Gut dysbiosis is linked to hypertension. Hypertension 2015;65:1331-40. 10.1161/HYPERTENSIONAHA.115.05315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garrett WS. Cancer and the microbiota. Science 2015;348:80-6. 10.1126/science.aaa4972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zalar B, Haslberger A, Peterlin B. The Role of Microbiota in Depression - a brief review. Psychiatr Danub 2018;30:136-41. 10.24869/spsih.2018.136 [DOI] [PubMed] [Google Scholar]
- 20.Bansilal S, Castellano JM, Fuster V. Global burden of CVD: focus on secondary prevention of cardiovascular disease. Int J Cardiol 2015;201 Suppl 1:S1-7. 10.1016/S0167-5273(15)31026-3 [DOI] [PubMed] [Google Scholar]
- 21.Duranton F, Cohen G, De Smet R, et al. Normal and pathologic concentrations of uremic toxins. J Am Soc Nephrol 2012;23:1258-70. 10.1681/ASN.2011121175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lynch SV, Pedersen O. The Human Intestinal Microbiome in Health and Disease. N Engl J Med 2016;375:2369-79. 10.1056/NEJMra1600266 [DOI] [PubMed] [Google Scholar]
- 23.Wilck N, Matus MG, Kearney SM, et al. Salt-responsive gut commensal modulates TH17 axis and disease. Nature 2017;551:585-9. 10.1038/nature24628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pluznick J. A novel SCFA receptor, the microbiota, and blood pressure regulation. Gut Microbes 2014;5:202-7. 10.4161/gmic.27492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rukavina Mikusic NL, Kouyoumdzian NM, Choi MR. Gut microbiota and chronic kidney disease: evidences and mechanisms that mediate a new communication in the gastrointestinal-renal axis. Pflugers Arch 2020;472:303-20. 10.1007/s00424-020-02352-x [DOI] [PubMed] [Google Scholar]
- 26.Wong J, Piceno YM, DeSantis TZ, et al. Expansion of urease- and uricase-containing, indole- and p-cresol-forming and contraction of short-chain fatty acid-producing intestinal microbiota in ESRD. Am J Nephrol 2014;39:230-7. 10.1159/000360010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vaziri ND, Wong J, Pahl M, et al. Chronic kidney disease alters intestinal microbial flora. Kidney Int 2013;83:308-15. 10.1038/ki.2012.345 [DOI] [PubMed] [Google Scholar]
- 28.Barba C, Soulage CO, Caggiano G, et al. Effects of Fecal Microbiota Transplantation on Composition in Mice with CKD. Toxins (Basel) 2020;12:741. 10.3390/toxins12120741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li DY, Tang WHW. Contributory Role of Gut Microbiota and Their Metabolites Toward Cardiovascular Complications in Chronic Kidney Disease. Semin Nephrol 2018;38:193-205. 10.1016/j.semnephrol.2018.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mishima E, Fukuda S, Mukawa C, et al. Evaluation of the impact of gut microbiota on uremic solute accumulation by a CE-TOFMS-based metabolomics approach. Kidney Int 2017;92:634-45. 10.1016/j.kint.2017.02.011 [DOI] [PubMed] [Google Scholar]
- 31.Que Y, Cao M, He J, et al. Gut Bacterial Characteristics of Patients With Type 2 Diabetes Mellitus and the Application Potential. Front Immunol 2021;12:722206. 10.3389/fimmu.2021.722206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tao S, Li L, Li L, et al. Understanding the gut-kidney axis among biopsy-proven diabetic nephropathy, type 2 diabetes mellitus and healthy controls: an analysis of the gut microbiota composition. Acta Diabetol 2019;56:581-92. 10.1007/s00592-019-01316-7 [DOI] [PubMed] [Google Scholar]
- 33.Hou K, Zhang S, Wu Z, et al. Reconstruction of intestinal microecology of type 2 diabetes by fecal microbiota transplantation: Why and how. Bosn J Basic Med Sci 2022;22:315-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rinninella E, Raoul P, Cintoni M, et al. What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms 2019;7:14. 10.3390/microorganisms7010014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shreiner AB, Kao JY, Young VB. The gut microbiome in health and in disease. Curr Opin Gastroenterol 2015;31:69-75. 10.1097/MOG.0000000000000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gomes AC, Hoffmann C, Mota JF. The human gut microbiota: Metabolism and perspective in obesity. Gut Microbes 2018;9:308-25. 10.1080/19490976.2018.1465157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kumar M, Singh P, Murugesan S, et al. Microbiome as an Immunological Modifier. Methods Mol Biol 2020;2055:595-638. 10.1007/978-1-4939-9773-2_27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qin J, Li Y, Cai Z, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 2012;490:55-60. 10.1038/nature11450 [DOI] [PubMed] [Google Scholar]
- 39.Zhang X, Shen D, Fang Z, et al. Human gut microbiota changes reveal the progression of glucose intolerance. PLoS One 2013;8:e71108. 10.1371/journal.pone.0071108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wu H, Tremaroli V, Schmidt C, et al. The Gut Microbiota in Prediabetes and Diabetes: A Population-Based Cross-Sectional Study. Cell Metab 2020;32:379-390.e3. 10.1016/j.cmet.2020.06.011 [DOI] [PubMed] [Google Scholar]
- 41.Rossen NG, Fuentes S, van der Spek MJ, et al. Findings From a Randomized Controlled Trial of Fecal Transplantation for Patients With Ulcerative Colitis. Gastroenterology 2015;149:110-118.e4. 10.1053/j.gastro.2015.03.045 [DOI] [PubMed] [Google Scholar]
- 42.Veprik A, Laufer D, Weiss S, Rubins N, Walker MD. GPR41 modulates insulin secretion and gene expression in pancreatic beta-cells and modifies metabolic homeostasis in fed and fasting states. FASEB journal: official publication of the Federation of American Societies for Experimental Biology. 2016;30(11):3860-9. 10.1096/fj.201500030R [DOI] [PubMed] [Google Scholar]
- 43.Gomes JMG, Costa JA, Alfenas RCG. Metabolic endotoxemia and diabetes mellitus: A systematic review. Metabolism 2017;68:133-44. 10.1016/j.metabol.2016.12.009 [DOI] [PubMed] [Google Scholar]
- 44.de la Cuesta-Zuluaga J, Mueller NT, Corrales-Agudelo V, et al. Metformin Is Associated With Higher Relative Abundance of Mucin-Degrading Akkermansia muciniphila and Several Short-Chain Fatty Acid-Producing Microbiota in the Gut. Diabetes Care 2017;40:54-62. 10.2337/dc16-1324 [DOI] [PubMed] [Google Scholar]
- 45.Olivares M, Neyrinck AM, Pötgens SA, et al. The DPP-4 inhibitor vildagliptin impacts the gut microbiota and prevents disruption of intestinal homeostasis induced by a Western diet in mice. Diabetologia 2018;61:1838-48. 10.1007/s00125-018-4647-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang M, Shi FH, Liu W, et al. Dapagliflozin Modulates the Fecal Microbiota in a Type 2 Diabetic Rat Model. Front Endocrinol (Lausanne) 2020;11:635. 10.3389/fendo.2020.00635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Deng ZM, Wang LB, Guan B, et al. Clinical study of berberine probiotics regulation of intestinal flora combined with metformin is superior to insulin therapy in the treatment of type 2 diabetes. Diabetes New World 2017;20:72-3. [Google Scholar]
- 48.Cortez RV, Petry T, Caravatto P, et al. Shifts in intestinal microbiota after duodenal exclusion favor glycemic control and weight loss: a randomized controlled trial. Surg Obes Relat Dis 2018;14:1748-54. 10.1016/j.soard.2018.07.021 [DOI] [PubMed] [Google Scholar]
- 49.Zhang PP, Li LL, Han X, et al. Fecal microbiota transplantation improves metabolism and gut microbiome composition in db/db mice. Acta Pharmacol Sin 2020;41:678-85. 10.1038/s41401-019-0330-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shi K, Wang F, Jiang H, et al. Gut bacterial translocation may aggravate microinflammation in hemodialysis patients. Dig Dis Sci 2014;59:2109-17. 10.1007/s10620-014-3202-7 [DOI] [PubMed] [Google Scholar]
- 51.Strid H, Simrén M, Stotzer PO, et al. Patients with chronic renal failure have abnormal small intestinal motility and a high prevalence of small intestinal bacterial overgrowth. Digestion 2003;67:129-37. 10.1159/000071292 [DOI] [PubMed] [Google Scholar]
- 52.Simenhoff ML, Saukkonen JJ, Burke JF, et al. Bacterial populations of the small intestine in uremia. Nephron 1978;22:63-8. 10.1159/000181424 [DOI] [PubMed] [Google Scholar]
- 53.Wang F, Zhang P, Jiang H, et al. Gut bacterial translocation contributes to microinflammation in experimental uremia. Dig Dis Sci 2012;57:2856-62. 10.1007/s10620-012-2242-0 [DOI] [PubMed] [Google Scholar]
- 54.Hida M, Aiba Y, Sawamura S, et al. Inhibition of the accumulation of uremic toxins in the blood and their precursors in the feces after oral administration of Lebenin, a lactic acid bacteria preparation, to uremic patients undergoing hemodialysis. Nephron 1996;74:349-55. 10.1159/000189334 [DOI] [PubMed] [Google Scholar]
- 55.Shamsaddini A, Gillevet PM, Acharya C, et al. Impact of Antibiotic Resistance Genes in Gut Microbiome of Patients With Cirrhosis. Gastroenterology 2021;161:508-521.e7. 10.1053/j.gastro.2021.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li Y, Su X, Gao Y, et al. The potential role of the gut microbiota in modulating renal function in experimental diabetic nephropathy murine models established in same environment. Biochim Biophys Acta Mol Basis Dis 2020;1866:165764. 10.1016/j.bbadis.2020.165764 [DOI] [PubMed] [Google Scholar]
- 57.Kramer H, Kuffel G, Thomas-White K, et al. Diversity of the midstream urine microbiome in adults with chronic kidney disease. Int Urol Nephrol 2018;50:1123-30. 10.1007/s11255-018-1860-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huang L, Thonusin C, Chattipakorn N, et al. Impacts of gut microbiota on gestational diabetes mellitus: a comprehensive review. Eur J Nutr 2021;60:2343-60. 10.1007/s00394-021-02483-6 [DOI] [PubMed] [Google Scholar]
- 59.Lin JR, Wang ZT, Sun JJ, et al. Gut microbiota and diabetic kidney diseases: Pathogenesis and therapeutic perspectives. World J Diabetes 2022;13:308-18. 10.4239/wjd.v13.i4.308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Allin KH, Tremaroli V, Caesar R, et al. Aberrant intestinal microbiota in individuals with prediabetes. Diabetologia 2018;61:810-20. 10.1007/s00125-018-4550-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Piccolo BD, Graham JL, Stanhope KL, et al. Diabetes-associated alterations in the cecal microbiome and metabolome are independent of diet or environment in the UC Davis Type 2 Diabetes Mellitus Rat model. Am J Physiol Endocrinol Metab 2018;315:E961-72. 10.1152/ajpendo.00203.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Adachi K, Sugiyama T, Yamaguchi Y, et al. Gut microbiota disorders cause type 2 diabetes mellitus and homeostatic disturbances in gut-related metabolism in Japanese subjects. J Clin Biochem Nutr 2019;64:231-8. 10.3164/jcbn.18-101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Leite AZ, Rodrigues NC, Gonzaga MI, et al. Detection of Increased Plasma Interleukin-6 Levels and Prevalence of Prevotella copri and Bacteroides vulgatus in the Feces of Type 2 Diabetes Patients. Front Immunol 2017;8:1107. 10.3389/fimmu.2017.01107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gradisteanu Pircalabioru G, Corcionivoschi N, Gundogdu O, et al. Dysbiosis in the Development of Type I Diabetes and Associated Complications: From Mechanisms to Targeted Gut Microbes Manipulation Therapies. Int J Mol Sci 2021;22:2763. 10.3390/ijms22052763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Amar J, Serino M, Lange C, et al. Involvement of tissue bacteria in the onset of diabetes in humans: evidence for a concept. Diabetologia 2011;54:3055-61. 10.1007/s00125-011-2329-8 [DOI] [PubMed] [Google Scholar]
- 66.Saldanha da Silva AA, Rodrigues Prestes TR, Lauar AO, et al. Renin Angiotensin System and Cytokines in Chronic Kidney Disease: Clinical and Experimental Evidence. Protein Pept Lett 2017;24:799-808. 10.2174/0929866524666170818160809 [DOI] [PubMed] [Google Scholar]
- 67.Lu CC, Ma KL, Ruan XZ, et al. Intestinal dysbiosis activates renal renin-angiotensin system contributing to incipient diabetic nephropathy. Int J Med Sci 2018;15:816-22. 10.7150/ijms.25543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cani PD, Bibiloni R, Knauf C, et al. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 2008;57:1470-81. 10.2337/db07-1403 [DOI] [PubMed] [Google Scholar]
- 69.Hou K, Wu ZX, Chen XY, et al. Microbiota in health and diseases. Signal Transduct Target Ther 2022;7:135. 10.1038/s41392-022-00974-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rezaei Bookani K, Marcus R, Cheikh E, et al. Corynebacterium jeikeium endocarditis: A case report and comprehensive review of an underestimated infection. IDCases 2018;11:26-30. 10.1016/j.idcr.2017.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang Q, Zhang Y, Zeng L, et al. The Role of Gut Microbiota and Microbiota-Related Serum Metabolites in the Progression of Diabetic Kidney Disease. Front Pharmacol 2021;12:757508. 10.3389/fphar.2021.757508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hu X, Xie Y, Xiao Y, et al. Longitudinal analysis of fecal microbiome and metabolome during renal fibrotic progression in a unilateral ureteral obstruction animal model. Eur J Pharmacol 2020;886:173555. 10.1016/j.ejphar.2020.173555 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as