Abstract
Background and Aims
hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) represent the major transfusion–transmissible pathogens worldwide. The risk of transmission is relatively high in African countries, mainly due to unreliable screening methods of blood donations. In Burkina Faso, predonation screening using rapid diagnostic tests (RDTs) is widespread, raising the major question of the transfusion safety in the country. The objective of this study was to assess the risk of transmission of HBV, HCV, and HIV through blood transfusion in the context of the use of RDTs for screening of the blood donations.
Methods
In this cross‐sectional study, a total of 417 serum samples obtained from blood donors tested negative for HBsAg, anti‐HCV, and anti‐HIV using RDTs were retested for the same markers using chemiluminescent immunologic assays. Total antibodies to HBV core (anti‐HBc) were tested on randomly selected samples. HBV‐DNA and HCV‐RNA viral loads (VLs) were quantified on HBsAg and anti‐HCV positive samples, respectively. To assess possible occult hepatitis B infection (OBI), HBV‐DNA‐VL was quantified on 313 randomly selected HBsAg‐negative samples.
Results
HBsAg and anti‐HCV were found respectively in 6 (6/417; 1.4%) and 11 (11/417; 2.6%) samples. No samples were reactive for anti‐HIV. Total anti‐HBc were detected in 217 out of the 319 randomly selected samples (217/319; 68.02%). HBV‐DNA was detected in four (4/313; 1.27%) samples, including two (2/6; 33.33%) of the six HBsAg positive samples and two (2/313; 0.6%) of the HBsAg‐negative samples, suggesting two cases of occult HBV infection. All anti‐HCV antibody‐positive samples were HCV‐RNA negative.
Conclusion
This study shows that RDTs are not sufficiently sensitive for the screening of blood donations. Our results highlight the urgent need to think about the extension of sensitive immunological tests in all blood transfusion centers and also the implementation of nucleic acid amplification techniques.
Keywords: blood donation, Burkina Faso, HBV, HCV, HIV, RDTs
1. INTRODUCTION
According to the World Health Organization (WHO), viral hepatitis remains a real concern worldwide, mainly in Sub‐Saharan Africa and South‐East Asia. Each year, about 1.34 million people die from hepatitis infections and 96% of these deaths are attributable to hepatitis B virus (HBV) and hepatitis C virus (HCV). 1 With an estimated 36.9 million people living with human immunodeficiency virus (HIV) and more than 35 million deaths to date, HIV infection continues to be a major global public health problem. 2 HBV, HCV, and HIV represent the major transfusion–transmissible pathogens worldwide. The risk of transmission of these pathogens varies geographically and it is relatively high in many African countries due to the lack of quality assurance and the use of unreliable detection methods like rapid diagnostic tests (RDTs) for the screening of blood donations. 3 , 4 , 5 The performance of these tests is highly variable, but top tests ranked by the WHO comparative study allow effective screening of blood donors. However, top tests tend to be more expensive, which leads to the selection of less effective tests that are most often cheaper.
To address this situation, the WHO advocates the implementation of various strategies including mandatory screening of all blood donors for major transfusion–transmissible infections by high‐quality laboratory testing. 6 In addition, WHO considers the implementation of transfusion safety as a key step towards the elimination of viral hepatitis as a health problem by 2030 in low‐ and middle‐income countries (LMICs). 1
In Burkina Faso, with respective prevalence rates of 9.1%, 3.6%, and 0.8% in the general population, HBV, HCV, and HIV infections remain major public health problems. 7 , 8 Likewise, high prevalences of these pathogens were also reported among blood donors 9 , 10 , 11 , 12 , 13 highlighting the risk of transmission through blood transfusion. Blood transfusion safety (BTS) in the country is effective since 2000 and is implemented by the National Blood Transfusion Center (NBTC). BTS relies upon the systematic screening of all blood products for HIV‐1/2, HBV, HCV, and syphilis infections using enzyme‐linked immunosorbent assay (EIA) and/or chemiluminescent immunologic assay (CLIA). With these assays, the residual transmission risk was evaluated to be 1/1366 for HIV, 1/408 for HBV, and 1/213 for HCV. 14 However, because EIA and CLIA are not available everywhere, and centralized testing has shown its limitations, several health facilities implement BTS through rapid test‐based screenings. Although offering economic advantages for resource‐limited countries, the imperfect sensitivity of these tests, raise concerns about the safety of the blood transfusion system. 13 Previous studies reported data on the performance of the rapid tests in blood donors suggesting a potential risk of posttransfusion infections. 15 , 16 , 17 , 18 To our knowledge, although widely used for the biological qualification of donations in Burkina Faso, no studies to date have evaluated the residual risk of pathogen transmission following the use of RDTs. Indeed, most of the used RDTs have neither been accredited nor evaluated beforehand for the screening of blood products. This study aimed to assess the risk of transmission of HBV, HCV, and HIV through blood donations in Burkina Faso screened with RDTs.
2. MATERIALS AND METHODS
2.1. Study design and setting
This cross‐sectional descriptive study was conducted between November 2019 and March 2020 in four health centers of Burkina Faso, the Regional Hospital (RH) of Banfora in the “Cascades” region, the RH of Dédougou in the “Boucle du Mouhoun” region, the Medical Center (MC) of Pô in the Centre‐South region and the MC of Gourcy in the North region (Figure 1). The RHs of Banfora and Dédougou are 90 and 180 km, respectively from the Bobo‐Dioulasso Regional Blood Transfusion Centers (RBTCs). As for the MCs of Pô and Gourcy, they are respectively 147.5 and 140.5 km from the RBTC of Ouagadougou. However, not being able to cover the entire national territory (NBTC), these health facilities are authorized and obliged to implement BTS through rapid test‐based screening. All of them have a blood bank department and were randomly selected from 39 health centers that use RDTs for the screening of blood.
Figure 1.
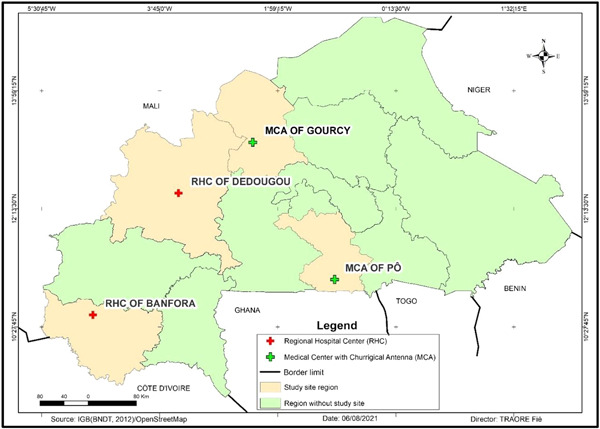
Map showing the localization of the study sites.
2.2. Study population and data collection
We enrolled blood donors screened negative for hepatitis B surface antigen (HBsAg), HCV antibodies (anti‐HCV), and HIV‐1/2 antigen/antibodies (anti‐HIV) using RDTs, and who signed an informed consent form to participate in the study. Venous whole blood sample was collected from each participant into a dry tube. Sera were obtained after centrifugation of the samples at 4000 rpm for 5 min and were stored at −80°C until analysis. In addition, sociodemographic characteristics and knowledge about viral hepatitis were recorded using a structured questionnaire. These data included age, sex, education, occupation, marital status, viral hepatitis transmission routes, and immunization status. Detailed information about the RDTs used during the study period at each site are presented in Table 1.
Table 1.
Characteristics of the RDTs used during the study period for predonation screening of HBsAg, anti‐HCV, and anti‐HIV‐1/2
| Characteristics | HBsAg RDTs | Anti‐HCV RDTs | HIV‐1/2 RDT | ||||
|---|---|---|---|---|---|---|---|
| CHIL® HBsAg | SD Bioline® HBsAg | JusCheck® Cassette Test Rapid HBsAg | CHIL® HCV cassette | SD Bioline® HCV | HCV Gold Rapid Screen Test Strip | Alere determine HIV‐1/2 Ag/Ab Combo test | |
| Sites where tests were used | Pô |
|
|
Pô |
|
|
|
| Laboratory | CHIL Medical Supplies Ltd., Turkey |
Standard Diagnostics. South Korea |
AllTest Biotech Co., Ltd., China |
CHIL Medical Supplies Ltd., Turkey |
Standard Diagnostics. South Korea |
Span Biotech Ltd., China |
Orgenics Ltd. |
| Reaction principle | IC | IC | IC | IC | IC | IC | IC |
| Specimen type | Plasma/serum | Plasma/serum | Whole blood/plasma/serum | Plasma/serum | Plasma/serum | Whole blood/plasma/serum | Whole blood/plasma/serum |
| Storage temperature (°C) | 10–30 | 1–30 | 2–30 | 10–30 | 1–30 | 4–30 | 2–30 |
| Sample volume | 2–3 drops | 100 µl | 75 µl | 2–3 drops | 100 µl | 70–75 µl | 50 µl |
| Analytical threshold | 2 ng/ml | 3 ng/ml | 1 ng/ml | – | – | – | 12 pg/ml |
| Se according the manufacturer | 98.84% | 100% | >99.9% | 98.84% | 100% | >99.9% | HIV‐1/2: 100% |
| Sp according the manufacturer | 98.94% | 100% | 99.5% | 98.94% | 100% | 99.5% | 99.75% |
| Unit cost (USD) | $ 0.73 | $1.54 | – | $0.73 | – | $2.65 | $1.16 |
Abbreviations: HCV, hepatitis C virus; HIV, human immunodeficiency virus; IC, immunochromatographic; RDT, rapid diagnostic test.
2.3. Laboratory analysis
All serum samples were tested for HBsAg, anti‐HCV, and anti‐HIV using the CLIA on the Cobas® 6000 analyzer (Elecsys® HBsAg II, Elecsys® Anti‐HCV II, Elecsys® HIV combi PT; Roche Diagnostics). Total anti‐HBc were tested on samples randomly selected using CMIA (Elecsys® Anti‐HBc II; Roche Diagnostics). HBV‐DNA and HCV‐RNA viral loads (VLs) were quantified respectively on HBsAg and anti‐HCV‐reactive samples using the Roche Molecular System (COBAS AmpliPrep/COBAS Taqman HBV Test Version 2.0; COBAS AmpliPrep/COBAS Taqman HCV Test Version 2.0). To detect possible occult hepatitis B infection, HBV‐DNA‐VL was quantified in HBsAg‐negative samples randomly selected (COBAS AmpliPrep/COBAS Taqman HBV Test Version 2.0). The manufacturer's reported limits of detection for HBsAg, HIV (p24 antigen), HBV DNA, and HCV RNA were 0.1 (0.88ng/ml), ≤2, 20, and 15 IU/ml, respectively. As for Elecsys® Anti‐HCV II, the sensitivity and specificity were 100% and 99.9%, respectively, and 100% for both for Elecsys® Anti‐HBc II. With respect to the cost of testing, serological markers have been estimated to cost approximately $7.00 per test, and approximately $25.00 for molecular testing. All tests were performed according to the manufacturer's instructions.
2.4. Statistical analysis
Statistical analyses were performed using STATA SE version 14.0 software. We used proportions to describe categorical variables and means (standard deviation) to describe continuous variables. Risk of transmission was computed for each pathogen considering CLIA as a gold standard. Statistical inferences were based on 95% confidence intervals (CIs).
2.5. Ethical considerations
This study received the approval of the Ethics Committee of the “Institut de Recherche en Sciences de la Santé” before its implementation (17‐2019/CEIRS‐20062019). All participants and legally authorized representatives of illiterate participants provided written informed consent and donors who were tested positive for one or several markers, were referred to a Health Center. The research was performed in accordance with the Declaration of Helsinki.
3. RESULTS
3.1. Sociodemographic characteristics of participants and their knowledge about hepatitis viruses
During the study period, a total of 2994 blood donors were tested, and 57 (1.9%) were found positive for HIV, 252 (8.4%) for HBV, 90 for anti‐HCV (3.0%), and 46 (1.5%) for syphilis. Of the blood donors screened negative for these markers (2549), 417 from Banfora (n = 122/417; 29.2%), Dédougou (n = 116/417; 27.8%), Pô (n = 125/417; 29.9%), and Gourcy (n = 57/417; 12.9%) were enrolled. The mean age of the donors was 33.45 years (age range: 18–57 years), 297 (297/417; 71.2%) were male and 211 (211/417; 50.6%) were students. The age group from 18 to 29 years was the most represented with 303 (303/417; 72.6%) participants. Among the donors, 214 (214/417; 51.3%) had heard of viral hepatitis and 102(102/417; 24.5%) had knowledge of transmission routes. As for their hepatitis B immunization status, only 14 (14/417; 3.4%) of the participants reported being fully vaccinated. The detailed characteristics of the study population are summarized in Table 2.
Table 2.
Sociodemographic characteristics and knowledge about viral hepatitis of blood donors
| Characteristic | Total number (N = 417) | Percentage (%) |
|---|---|---|
| Sex | ||
| Male | 297 | 71.22 |
| Female | 120 | 28.78 |
| Age (years) | ||
| (18–20) | 107 | 25.65 |
| (20–30) | 196 | 47.00 |
| (30–40) | 71 | 17.03 |
| 40+ | 43 | 10.31 |
| Level of education | ||
| None | 70 | 16.79 |
| Elementary | 46 | 11.03 |
| Secondary/higher | 301 | 72.18 |
| Occupation | ||
| Employee | 42 | 10.07 |
| Merchant | 67 | 16.07 |
| Farmer | 66 | 15.83 |
| Student (secondary high schools/universities) | 211 | 50.60 |
| Others | 31 | 7.43 |
| Marital status | ||
| Single | 268 | 64.27 |
| Married | 149 | 35.73 |
| Heard about viral hepatitis | ||
| No | 203 | 48.68 |
| Yes | 214 | 51.32 |
| Knowledge of transmission route | ||
| No | 315 | 75.54 |
| Yes | 102 | 24.46 |
| Immunization status | ||
| Not vaccinated | 216 | 51.80 |
| Don't know | 187 | 44.84 |
| Fully vaccinated | 14 | 3.36 |
3.2. Risk of transmission
Using the CLIA method, HBsAg and anti‐HCV were detected respectively in 6 (1.4%; 95% CI: 0.5–3.1) and 11 (2.6%; 95% CI: 1.3–4.7). No samples were reactive for HIV‐1/2 infection. Of the 319 randomly selected samples, including the six HBsAg‐reactive samples, total anti‐HBc was detected in 217 (68.02%; 95% CI: 62.2–72.7). HBV‐DNA was detected in four (1.275%; 95% CI: 0.03, 2.94) samples including two (2/6; 33.33%) in the sikx reactive HBsAg samples and two (2/313; 0.6%) in the nonreactive HBsAg samples, this latter result arguing for two cases of occult hepatitis B. In HBsAg‐reactive samples, HBV‐DNA‐VL were 16.400 and 932 IU/ml, and for occult hepatitis B infection (OBI) cases, they were 21 and 38 IU/ml. All HBV‐DNA detectable samples were reactive for anti‐HBc. HCV‐RNA was not detected in any of the anti‐HCV‐reactive samples. The serological and molecular results are summarized in Table 3.
Table 3.
Serological and molecular results
| Markers | N | % | 95% CI |
|---|---|---|---|
| HBsAg | |||
| Nonreactive | 411 | 98.56 | |
| Reactive | 6 | 1.44 | (0.52, 3.10) |
| Anti‐HCV | |||
| Nonreactive | 406 | 97.36 | |
| Reactive | 11 | 2.64 | (1.32, 4.67) |
| anti‐HBc (n = 319) | |||
| Nonreactive | 102 | 31.98 | |
| Reactive | 217 | 68.02 | (62.16, 72.72) |
| HBV DNA (IU/ml) (n = 313) | |||
| Undetectable | 309 | 98.72 | |
| Detectable | 4 | 1.27 | (0.03, 2.94) |
Abbreviations: CI, confidence interval; HBV, hepatitis B virus; HCV, hepatitis C virus.
A multivariable logistic regression analysis reported a statistically significant correlation between knowledge of viral hepatitis (transmission routes) and HBsAg seronegativity (odds ratio [OR] = 6.38; 95% CI: 1.15–35.40; Table 4). However, no significant association between anti‐HCV and anti‐HBc positivity and participants' demographics was found.
Table 4.
Factor associated with HBsAg and anti‐HCV seroreactivity using CLIA
| HBsAg | Anti‐HCV | ||||||
|---|---|---|---|---|---|---|---|
| Variable | N | n (%) | OR (95% CI) | p | n (%) | OR (95% CI) | p value |
| Age group | 0.4923 | 0.789 | |||||
| (18–20) | 107 | 3 (2.86%) | 1 | 3 (2.80%) | 1 | ||
| (20–30) | 196 | 2 (1.02%) | 0.35 (0.06, 2.13) | 5 (2.55%) | 0.89 (0.20, 3.80) | ||
| (30–40) | 71 | 0 (0.00%) | 1 | 3 (4.23%) | 1.5 (0.29, 7.65) | ||
| 40+ | 43 | 1 (2.33%) | 0.81 (0.08, 8.01) | 0 (0.00%) | |||
| Gender | 0.8066 | 0.1047 | |||||
| Male | 297 | 4 (1.35%) | 1 | 10 (3.37%) | 1 | ||
| Female | 120 | 2 (1.67%) | 1.24 (0.22, 6.87) | 1 (0.83%) | 0.24 (0.03, 1.90) | ||
| Education | 0.9527 | ||||||
| None | 70 | 0 (0.00%) | 2 (2.86%) | 1 | |||
| Elementary | 46 | 0 (0.00%) | 0 (0.00%) | ||||
| Secondary/higher | 301 | 6 (1.99%) | 9 (2.99%) | 1.04 (0.22, 4.96) | |||
| Occupation | 0.9965 | 0.9297 | |||||
| Employee | 42 | 1 (2.38%) | 0 (0.00%) | ||||
| Merchant | 67 | 0 (0.00%) | 2 (2.99%) | 1 | |||
| Farmer | 66 | 0 (0.00%) | 2 (3.03%) | 0.9 (0.18, 4,42) | |||
| Student | 211 | 5 (2.37%) | 0.99 (0.11, 8.74) | 7 (3.32%) | 0.91 (0.18, 4.49) | ||
| Other | 31 | 0 (0.00%) | 0 (0.00%) | ||||
| Marital status | 0.2973 | 0.5448 | |||||
| Single | 268 | 5 (1.87%) | 8 (2.99%) | 1 | |||
| Married | 149 | 1 (0.67%) | 0.35 (0.04, 3.07) | 3 (2.01%) | 0.66 (0.17, 2.56) | ||
| Heard about viral hepatitis | 0.0979 | 0.8281 | |||||
| No | 203 | 1 (0.49%) | 5 (2.46%) | 1 | |||
| Yes | 214 | 5 (2.34%) | 4.83 (0.55, 41.72) | 6 (2.80%) | 1.14 (0.34, 3.80) | ||
| Knowledge of transmission routes | 0.0279 | 0.1843 | |||||
| No | 315 | 2 (0.63%) | 10 (3.17%) | 1 | |||
| Yes | 102 | 4 (3.92%) | 6.38 (1.15, 35.40) | 1 (0.98%) | 0.3 (0.04, 2.89) | ||
| Immunization status | 0.1215 | 0.2444 | |||||
| Not vaccinated | 216 | 5 (2.31%) | 1 | 4 (1.85%) | 1 | ||
| Don't know | 187 | 1 (0.53%) | 0.22 (0.03, 1.96) | 7 (3.74%) | 2.06 (0.59, 7.15) | ||
| Fully vaccinated | 14 | 0 (0.00%) | 1 | 0 (0.00%) | |||
Abbreviations: CI, confidence interval; CLIA, chemiluminescent immunologic assay; HCV, hepatitis C virus; OR, odds ratio.
4. DISCUSSION
In Burkina Faso, BTS implemented by the NBTC consists of systematic screening for HIV, HBV, HCV, and syphilis using sensitive methods including EIA and/or CLIA techniques. However, two previous studies conducted in Blood Banks in Burkina Faso pointed out a significant residual risk of about 0.3%, 0.5%, and 0. 07% for HBV, HCV, and HIV, respectively. 14 , 19 To increase the population's access to blood products, several health centers are authorized to practice blood transfusion after screening their donations with RDTs. We evaluated the risk of posttransfusion transmission of these major pathogens and found 6 (1.4%) HBsAg‐reactive and 11 (2.6%) anti‐HCV‐reactive samples were missed by RDTs. These findings are in line with studies reporting low sensitivity of RDTs evaluated in African blood donors. 18 , 20 However, the 2.6% anti‐HCV detected in RDT‐negative samples appears high. This could be related to evidence that CLIA results were likely false positive. The nondetection of HCV RNA on all anti‐HCV‐reactive samples could be a confirmation.
No case of HIV infection was detected, suggesting the good quality of the Alere Determine HIV‐1/2 Ag/Ab Combo test, which has been approved by the national regulation structure (Agence Nationale de la Régulation Pharmaceutique) in Burkina Faso and also has WHO prequalification. In addition, a national screening algorithm for HIV using this test is available and is evaluated regularly contributing to reduce the risk of false results. Another explanation could be the low HIV prevalence estimated to 0.8% in the general population. 8
Except for SD Bioline® tests, all tests used for HBV and HCV predonation screening have not been evaluated and approved in Burkina Faso, and do not have WHO prequalification. Consequently, information on their diagnostic performance on local samples are lacking and there is a risk of missing positive cases with these tests. The routine use of not registered tests in the country could be explained by the fact that the ordering of tests is mostly managed by nonspecialists in the field. Another reason may be the level of corruption in the health sector. 21 This situation highlights the urgency of setting up a national system for evaluating tests before they are used in blood transfusion.
An overall prevalence of 68.02% of total anti‐HBc was found, indicating an important circulation of HBV in Burkina Faso. 7 , 22 Therefore, we wondered whether in this high proportion of anti‐HBc‐positive blood donors, OBI may be a matter of concern. Indeed, OBI represents a potential threat for BTS mainly in LMICs where the use of nucleic acid amplification techniques (NAAT) is not widespread. 23 OBI is defined as the presence of replication‐competent HBV DNA in the liver and/or in the blood of HBsAg‐negative people. OBI can be categorized either as seropositive or seronegative for anti‐HBc and anti‐HBs antibodies. 24 The rate of detection of HBV‐DNA in HBsAg‐negative/anti‐HBc positive samples is estimated to be 1.6%–38%. 25 In our study, occult HBV infection OBI cases were detected in two (0.6%) blood donors with HBV‐DNA VL of 21 and 38 IU/ml. This prevalence is close to that reported by Fopa et al. 23 in Cameroon (0.56%), but lower than that observed by Diarra et al. 26 in Burkina Faso (7.3%), Olotu et al. 27 in Nigeria (5.4%) and Said et al. 25 in Egypt (17.2%). These differences could be explained by the fact that HBV‐DNA was screened in both anti‐HBc negative and positive samples in our study. Other factors such as the studied population and the techniques used for HBV‐DNA detection may be involved. The high total anti‐HBc prevalence was also predictable as all participants were born before the implementation of the hepatitis B vaccine in the national immunization program in 2006. Indeed, only 3.36% of the participants were fully vaccinated (Table 2).
Our results showed that HBV DNA was not detected on four HBsAg‐reactive samples. This could be due to the very low level of viral DNA that could not be detected by the COBAS Version 2.0 used in this study (analytical sensitivity: 20 IU/ml) for molecular analysis. In addition, since a confirmatory test for HBsAg was not used, false positive results cannot be excluded.
Based on these overall results, the implementation of sensitive methods in blood centers in Burkina Faso should be strongly considered. CLIA tests, because of their operating cost and capacity, are not suitable for small blood banks. However, they could be used in regional centers, and made accessible to peripheral blood banks through a centralized testing system. High‐performance RDTs could therefore significantly improve patient blood safety. To date, NAAT tests are available in almost all health centers in Burkina because of the response to the COVID‐19 pandemic. Thus, the detection of OBI cases by applying NAAT to pooled samples could be an interesting option since studies have reported transfusion transmission of HBV with blood components from donors with OBI. 28
In our study, assessment of participants' knowledge about viral hepatitis revealed that half of the donors (48.68%) had never heard of viral hepatitis and 75.54% had no information on transmission routes, confirming data we reported earlier. 13 Interestingly, a positive correlation (OR: 6.38; 95% CI: 1.15, 35.40) was found between the knowledge of the transmission routes and HBV seronegativity in the participants of this study (Table 4). Communication, information, and education activities must be organized for potential blood donors to raise awareness about this scourge. In addition, since students represented the main population of blood donors in our study (50.6%), awareness modules could be integrated into their curriculum.
Taking into account the objectives, the major limitation of our study was the relatively small sample size, which did not allow having a comprehensive picture of the magnitude of the transmission risk. Large‐scale studies are therefore needed. Another limitation is the absence of confirmation step HBsAg, anti‐HCV, and anti‐HIV assays.
In conclusion, our study showed a potential risk of transmission of HBV (1.44%) when using RDTs for qualification of blood donations. In addition, although HCV RNA was not detected in any samples confirming HCV infection, 11 anti‐HCV‐reactive samples were missed by the rapid tests. These results highlight the need to implement sensitives techniques in blood transfusion in Burkina Faso. OBI cases were also diagnosed in at least 0.6% of the donors. As Burkina Faso is a country of high endemicity for HBV, further confirmed here by high anti‐HBc positivity in our study cohort (about 68%), the implementation of NAAT in blood transfusion centers for the detection of OBI cases, while cost‐effective, should be definitely considered. This will constitute the main point of a high quality of our blood transfusion system.
AUTHOR CONTRIBUTIONS
Armel M. Sanou: Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; writing – original draft; writing – review and editing. Achille S. Nikiéma: Conceptualization; data curation; investigation; methodology; writing – review and editing. Seimbou Zalla: Conceptualization; data curation; investigation; methodology; writing – review and editing. Mamadou Ouattara: Methodology; formal analysis; software; writing – review and editing. Mariam Seynou: Methodology; formal analysis; software; writing – review and editing. Alice Kiba‐Koumare: Supervision; writing – review and editing. Delphine Napon‐Zongo: Supervision; writing – review and editing. Roger Sombié: Supervision; writing – review and editing.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
Armel M. Sanou affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained. All authors have read and approved the final version of the manuscript. Armel M. Sanou had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
ACKNOWLEDGMENTS
The authors thank all the participants in the study. The authors also thank the staff of the different study sites (CHR Banfora, CHR Dédougou, CMA Gourcy, CMA Po) for their active participation in the patient enrollment and sample collection phases. Finally, our gratitude to colleagues for their critical review of this article. This study was supported by grants from the ROCHE Diagnostics France and the “Institut de Recherche en Sciences de la Santé (IRSS).”
Sanou AM, Nikièma AS, Zalla S, et al. Residual risk of hepatitis B virus transmission through blood donations in Burkina Faso screened with rapid diagnostic tests. Health Sci Rep. 2022;5:e748. 10.1002/hsr2.748
DATA AVAILABILITY STATEMENT
All data generated or analyzed during this study are included in this article and its Supporting Information files data and can be requested from the corresponding author.
REFERENCES
- 1. World Health Organization . Global hepatitis report. Geneva, Switzerland. 2017. Accessed February 3, 2019. http://apps.who.int/iris/bitstream/10665/255016/1/9789241565455-eng.pdf
- 2. World Health Organization . HIV/AIDS Fact sheets. November 2020. Accessed January 10, 2021. https://www.who.int/news-room/fact-sheets/detail/hiv-aids
- 3. Bloch EM, Vermeulen M, Murphy E. Blood transfusion safety in Africa: a literature review of infectious disease and organizational challenges. Transfus Med Rev. 2012;26(2):164‐180. 10.1016/j.tmrv.2011.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Keleta YT, Achila OO, Haile AW, et al. Seroprevalence of transfusion transmitted infections among blood donors in Gash Barka Zonal Blood Transfusion Center, Barentu, Eritrea, 2014 through 2017. BMC Hematol. 2019;19(5):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kabamba AT, Kalunga BT, Mwamba CM, et al. Epidemiological aspects and molecular characterization of the hepatitis B virus among blood donors in Lubumbashi, Democratic Republic of Congo. Transfus Clin Biol. 2021;28(1):30‐37. [DOI] [PubMed] [Google Scholar]
- 6. Tagny CT, Mbanya D, Tapko JB, Lefrère JJ. Blood safety in Sub‐Saharan Africa: a multi‐factorial problem. Transfusion. 2008;48(6):1256‐1261. [DOI] [PubMed] [Google Scholar]
- 7. Meda N, Tuaillon E, Kania D, et al. Hepatitis B and C virus seroprevalence, Burkina Faso: a cross‐sectional study. Bull World Health Organ. 2018;96(11):750‐759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. UNAIDS . Country factsheets Burkina Faso. Estimates adults and children living with HIV and AIDS; 2019. pp. 1–10. Accessed January 10, 2021. https://www.unaids.org/en/regionscountries/countries/burkinafaso
- 9. Nagalo MB, Sanou M, Bisseye C, et al. Seroprevalence of human immunodeficiency virus, hepatitis B and C viruses and syphilis among blood donors in Koudougou (Burkina Faso) in 2009. Blood Transfus. 2011;9:419‐424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nagalo BM, Bisseye C, Sanou M, et al. Seroprevalence and incidence of transfusion‐transmitted infectious diseases among blood donors from regional blood transfusion centres in Burkina Faso, West Africa. Trop Med Int Health. 2012;17(2):247‐253. [DOI] [PubMed] [Google Scholar]
- 11. Candotti D, Diarra B, Bisseye C, et al. Molecular characterization of hepatitis B virus in blood donors from Burkina Faso: prevalence of quasi‐subgenotype A3, genotype E, and mixed infections. J Med Virol. 2016;88:2145‐2156. [DOI] [PubMed] [Google Scholar]
- 12. Yooda AP, Soubeiga ST, Nebie KY, et al. Impact of multiplex PCR in reducing the risk of residual transfusion‐transmitted. Mediterr J Hematol Infect Dis. 2018;10(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sanou AM, Toyé R, Kagoné T, et al. Analytical performance of eight rapid point‐of‐care tests routinely used for the detection of HBsAg in Burkina Faso: a cross‐sectional study. J Clin Virol. 2020;129:104546. [DOI] [PubMed] [Google Scholar]
- 14. Yooda AP, Sawadogo S, Soubeiga ST, et al. Residual risk of HIV, HCV, and HBV transmission by blood transfusion between 2015 and 2017 at the Regional Blood Transfusion Center of Ouagadougou, Burkina Faso. J Blood Med. 2019;10:53‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dwyre DM, Fernando LP, Holland PV. Hepatitis B, hepatitis C and HIV transfusion‐transmitted infections in the 21st century. Vox Sang. 2011;100:92‐98. [DOI] [PubMed] [Google Scholar]
- 16. Allain JP, Candotti D, Soldan K, et al. The risk of hepatitis B virus infection by transfusion in Kumasi, Ghana. Blood. 2003;101(6):2419‐2425. [DOI] [PubMed] [Google Scholar]
- 17. Owusu‐ofori S, Temple J, Sarkodie F, Anokwa M, Candotti D, Allain JP. Predonation screening of blood donors with rapid tests: implementation and efficacy of a novel approach to blood safety in resource‐poor settings. Transfusion. 2005;45:133‐140. [DOI] [PubMed] [Google Scholar]
- 18. Laperche S, Francophone African Group for Research in Blood Transfusion . Multinational assessment of blood‐borne virus testing and transfusion safety on the African continent. Transfusion. 2013;53:816‐826. [DOI] [PubMed] [Google Scholar]
- 19. Wongjarupong N, Oli S, Sanou M, et al. Distribution and incidence of blood‐borne infection among blood donors from Regional Transfusion Centers in Burkina Faso: a comprehensive study. Am J Trop Med Hyg. 2021;104(4):1577‐1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mutocheluh M, Owusu M, Kwofie TB, Akadigo T, Appau E, Narkwa PW. Risk factors associated with hepatitis B exposure and the reliability of five rapid kits commonly used for screening blood donors in Ghana. BMC Res Notes. 2014;7:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Réseau National de Lutte Anti‐Corruption (RENLAC) . Etat de la corruption au Burkina Faso. Rapport. 2020. Accessed April, 10 2022. https://secureservercdn.net/50.62.90.29/118.c3a.myftpupload.com/download/rapports/Rapport-Ren-Lac-2020.pdf
- 22. Polaris Observatory C. Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. Lancet Gastroenterol Hepatol. 2018;3(6):383‐403. [DOI] [PubMed] [Google Scholar]
- 23. Fopa D, Candotti D, Tagny CT, et al. Occult hepatitis B infection among blood donors from Yaoundé, Cameroon. Blood Transfus. 2019;17:403‐408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Raimondo G, Locarnini S, Pollicino T, et al. Update of the statements on biology and clinical impact of occult hepatitis B virus infection. J Hepatol. 2019;71:397‐408. [DOI] [PubMed] [Google Scholar]
- 25. Said ZN, Sayed M.H. Salama II, et al. Occult hepatitis B virus infection among Egyptian blood donors. World J Hepatol. 2013;5(2):64‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Diarra B, Yonli AT, Sorgho PA, Compaore TR. Occult hepatitis B virus infection and associated genotypes among HBsAg‐negative subjects in Burkina Faso. Mediterr J Hematol Infect Dis. 2018;10:e2018007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Olotu AA, Oyelese AO, Salawu L, et al. Occult hepatitis B virus infection in previously screened, blood donors in Ile‐Ife, Nigeria: implications for blood transfusion and stem cell transplantation. Virol J. 13, 2016:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Candotti D, Boizeau L, Laperche S. Occult hepatitis B infection and transfusion‐transmission risk. Transfus Clin Biol. 2017;24(3):189‐195. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article and its Supporting Information files data and can be requested from the corresponding author.


