Abstract
Background and Aims
Under‐prescription is defined as the exclusion of medications indicated for the treatment of certain conditions without any rationale for not prescribing them. The under‐prescription of medications is highly prevalent among older adults (≥65 years) receiving polypharmacy. This study aimed to assess the prevalence of the under‐prescription of medications using the Screening Tool to Alert to Right Treatment (START) criteria version 2 and to identify the predictors of having potential prescribing omissions (PPOs).
Methods
This cross‐sectional, face‐to‐face interview study was carried out between September 2021 and February 2022. The study comprised community‐dwelling older adults taking at least one medication on a regular basis. The study questionnaire included the patients' demographics, clinical data, and comorbidities. PPOs were identified using the START criteria. The χ 2 test was used to assess the association between under‐prescription of medication and the demographic/clinical variables. Multivariable logistic regression was performed to explore factors associated with under‐prescription of medications as the dependent variable and taking all variables that showed a p < 0.05 in the bivariate analysis as independent.
Results
A total of 444 older adults agreed to participate in this study. The mean age of participants was 71 ± 8.6; the majority of them, 305 (68.7%), were men. Polypharmacy was present in 261 patients (58.8%) and underprescribing of medications in 260 patients (58.6%). The highest percentage of under‐prescribing of medications was reported with statins in 115 patients (44.2%) followed by aspirin in 93 (35.7%), and angiotensin‐converting enzyme inhibitors in 61 (23.4%). The results of the multivariable analysis showed that patients with underprescribed medications had higher odds of polypharmacy (odds ratio [OR]: 2.015, confidence interval [CI] 95% 1.362–2.980, p < 0.001) and higher Charlson Comorbidity Index (OR 2.807, CI 95% 1.463–5.85, p = 0.02).
Conclusion
The present findings highlight that PPOs are highly prevalent among community‐dwelling older adults in Lebanon. Multimorbidity and polypharmacy were the identified predictors for under‐prescription of medications in this population.
Keywords: elderly, inappropriate prescribing, START screening tool
1. INTRODUCTION
While an average of one in every 11 persons worldwide is currently 65 years or older, this proportion is expected to rise to one in six persons by 2050, thus creating a major shift in the global demography. 1 Lebanon is reported to have the most number of older adults in the Middle East, where 10% of its total population will be aged over 65 years by 2050. 1 This necessitates further emphasis on this age group as they greatly contribute to the increased healthcare needs and the country's financial burden. 2 Several different factors are accountable for this demographic shift, most pivotal of which is the major improvement in medical care delivery. Despite this improvement, major public health concerns are emerging among the older population including complications associated with polypharmacy, morbidity, and mortality due to adverse drug outcomes, potentially inappropriate medications (PIMs), and potential prescribing omissions (PPOs). 3 , 4
The World Health Organization defines patients as older adults if they are 65 years or older. 5 In this population, polypharmacy is frequently observed due to physicians’ reliance on separate treatment guidelines for multiple morbidities, lower treatment threshold for chronic disease, the ongoing use of preventative medications, and the normal aging process. 6 Polypharmacy is defined as consuming five or more regular medications, which may be clinically indicated and beneficial in specific conditions (e.g., hypertension, diabetes mellitus) and patient populations (e.g., patients with multimorbidity). 6 , 7 However, polypharmacy may oftentimes comprise the use of medications in the absence of strong indications and result in decreased patient compliance, increased risk of drug–drug interactions (DDI), and increased risk for complications in patients with multiple conditions. 7 , 8
PIM is another healthcare problem that is frequently seen among older adults. These are considered medications that should be avoided in older individuals due to a high risk of adverse effects among this population and/or a lack of proof of their advantages when safer and equally or more effective therapeutic options are available. 9 It is worth mentioning that exposure to the latter phenomenon is very common. According to the literature, it is reported that around 20%–65% of older adults are currently exposed to at least one PIM; meanwhile, about one in every five medications prescribed to older adults was found inappropriate by a study. 10 , 11 , 12 This is alarming as such malpractice may result in negative consequences; including adverse drug reactions (ADRs), unnecessary hospitalization and healthcare utilization, and increased financial burden. 13
Despite the high prevalence of polypharmacy among older adults, many of them are still deprived of some essential medications for their treatment plan. 14 , 15 , 16 Under‐prescription of medications is defined as the exclusion of medications that are indicated or needed for the treatment of a certain condition without any rationale for not prescribing them. 14 This prescription pattern is surprisingly prevalent among older adults receiving polypharmacy (22%–77%) based on data from previously published studies. 14 , 15 , 16 Under‐prescription of medications is associated with ADRs (such as a greater risk of cardiovascular events, disability, and mortality). 16 , 17 It is worth mentioning that under‐prescription of medications does not take into account that some patients may truly have a good reason not to initiate the treatment, which limits the reliability of its definition. Previously, under‐prescribing of medications focused on the treatment of specific diseases (e.g., heart failure, diabetes, dementia, depression, and osteoporosis) or symptoms (e.g., pain). In this regard, several criteria have been designed in an attempt to identify PIMs and PPOs, such as the STOPP (Screening Tool of Older People's Prescriptions) and START (Screening Tool to Alert to Right Treatment) criteria. 18 The STOPP criterion was developed to identify PIMs and the START criterion was designed to identify PPOs. The interventional utilization of these tools significantly improves medication appropriateness and reduces the incidence of ADRs in older adults. 18 These tools were originally developed in Ireland and published for the first time in 2008, where a panel of only Irish and UK experts were involved in the primary version's validation. 19 The criteria were classified according to the major physiological systems affected by specific medications or medication classes. 19 Recently, these criteria were revised by 19 experts from 13 European countries with the aim of a wider input from different experts. Such review supported the tools' reflection of Europe‐wide prescribing practices in the general population of older adults and enhanced the application of the STOPP/START version 2. 18
Appropriate polypharmacy is defined as an optimized medication regimen based on clinical practice guidelines to improve the patient's clinical outcomes. 6 Thus, it is necessary to consider whether each medication has been prescribed appropriately or inappropriately, in an effort to achieve an “appropriate polypharmacy” in older adults. 6
Under‐prescription of medications in older adults has not been addressed in Lebanon yet. We, therefore, aimed in this study to assess the prevalence of under‐prescribing of medications using the START criteria version 2 and to identify the predictors of having PPOs.
2. MATERIALS AND METHODS
2.1. Study design and population
This cross‐sectional face‐to‐face interview study was carried out between September 2021 and February 2022 after receiving ethical approval from Lebanese International University 2021RC‐037‐LIUSOP. All participants provided verbal consent before completing the questionnaire. The study comprised older adults taking at least one chronic medication and presenting to one of 30 community pharmacies located across Lebanon to fill their own prescription.
2.2. Data collection
A sample of 30 community pharmacies was randomly selected from list provided by the order of Lebanese pharmacists' using the Statistical Package for the Social Sciences (SPSS) version 25, and the pharmacist in charge was briefed about the study's objectives and granted his or her permission to perform the study on their premises. Three researchers each attended 10 pharmacies for 2 days at first to determine the average number of older adults served per day. A minimum of 1 week was then assigned for each researcher to visit these pharmacies and interview potential older adults. The three researchers were extensively trained in conducting interviews with older adults before data collection following the National Institute on Aging recommendations for obtaining an older patient's medical history. 20 A random group of five older adults was then interviewed in an attempt to evaluate the researchers' interview skills.
A face‐to‐face interview was undertaken with older adult outpatients, who agreed to participate, in the pharmacy consulting area. The patients were assessed initially through simple questions before the study to confirm their orientation and concentration using the Short‐Orientation‐Memory‐Concentration (SOMC) such as asking them about the current date, time, and location, where a score more than or equal to 20/28 was considered normal. 21
The study questionnaire included patients' demographics (i.e., age, weight, height, level of education, marital status) and clinical data (i.e., past medical history, current medical problems, number of medications taken daily including the name/dosage/and frequency of each medication, in addition to over‐the‐counter medications and multivitamins) to evaluate the applied therapy. Comorbidities of the patients were also self‐reported and the Charlson Comorbidity Index (CCI) was used to quantify the presence of co‐existing diseases using an online calculator. 22 All the reported comorbidities were based on a previous diagnosis by a physician and only patients with established diagnosis were included. Patients were interviewed in Arabic.
PPOs were identified by comparing patients' profiles to the START criteria. The evaluation of medication under‐prescribing of medications was performed by one of the study researchers to minimize variability and reduce any possible bias. The list of medications for each patient was reviewed, when a medication was not prescribed but is clinically indicated in concordance with one of the START criteria, it was recorded as under‐prescribed.
3. STATISTICAL ANALYSES
The SPSS version 25 was utilized for data analysis. For the patient characteristics and under‐prescribing of medications analysis, descriptive statistics were used. Mean and standard deviation were used to describe quantitative factors, while frequencies described qualitative data. The χ 2 test was used to assess the association between under‐prescription of medication and the demographic/clinical variables. Multivariable logistic regression was performed to explore factors associated with under‐prescription of medications as the dependent variable and taking all variables that showed a p < 0.05 in the bivariate analysis as independent. Statistical significance was set at p value of less than 0.05.
4. RESULTS
A total of 600 older adults were approached for interviewing, 444 agreed to participate making a response rate of 74%. Patient's characteristics are presented in Table 1. The mean age of participants was 71 ± 8.6 (range 65–97 years) and the majority 305 (68.7%) were men. Cigarette smoking and alcohol consumption were reported in 242 (45.5%) and 79 (17.8%) by the participants, respectively. The majority of the study participants 194 (43.7%) resided in Mount Lebanon and 191 (43%) have a monthly income between 1 and 3 million Lebanese pounds. The most common reported comorbidities among the patients were hypertension 292(65.8%), coronary artery disease 224 (50.5%), and diabetes mellitus 190 (42.8%). Approximately half of the patients had a CCI greater or equal to 5. The median number of medications taken per patient was 5 (range 1–18).
Table 1.
Demographics and clinical variables (n, %) unless otherwise specified
| Characteristics | Frequency (%) |
|---|---|
| Age in years | |
| Mean (SD): 71 (6.8) | Range: 65–85 |
| Sex | |
| Male | 305 (68.7) |
| Female | 139 (31.3) |
| Smoker | |
| Yes | 242 (54.5) |
| Alcohol consumption | |
| Yes | 79 (17.8) |
| Place of residence | |
| Mount Lebanon | 194 (43.7) |
| Beirut | 87 (19.6) |
| Baalbek–Hermel | 81 (18.2) |
| South Lebanon | 39 (8.8) |
| North Lebanon | 21 (4.7) |
| Nabatiye | 15 (3.4) |
| Other | 7 (1.6) |
| Marital status | |
| Married | 360 (81.1) |
| Single | 84 (18.9) |
| Education | |
| No schooling | 132 (29.7) |
| High school | 183 (41.2) |
| University | 129 (29.1) |
| Monthly income | |
| Less than 1 million Lebanese pounds (LBP) | 104 (23.4) |
| 1–3 million LBP | 191 (43) |
| 3.1–5 million LBP | 112 (25.2) |
| More than 5 million LBP | 37 (8.3) |
| Medical condition | |
| Hypertension | 292 (65.8) |
| Coronary artery disease | 224 (50.5) |
| Diabetes mellitus | 190 (42.8) |
| Dyslipidemia | 114 (25.7) |
| Thyroid disease | 41 (9.2) |
| Deep vein thrombosis (DVT) | 38 (8.6) |
| Stroke | 34 (7.7) |
| Chronic obstructive pulmonary disease (COPD) | 29 (6.5) |
| Osteoporosis | 28 (6.3) |
| Heart failure | 24 (5.4) |
| Depression | 24 (5.4) |
| Rheumatoid arithritis | 16 (3.6) |
| Charlson Comorbidity Index (CCI) | |
| Mild (1–2) | 65 (14.6) |
| Moderate (3–4) | 166 (37.3) |
| Severe (≥5) | 213 (47.9) |
| Polypharmacy | 261 (58.8) |
| Underprescribing | 260 (58.6) |
Abbreviation: COPD, chronic obstructive pulmonary disease; DDI, Drug‐drug interaction; DVT, Deep vein thrombosis.
Polypharmacy was present in 261 patients (58.8%) and under‐prescribing of medications in 260 patients (58.6%). Of patients with polypharmacy, 170 (65.1%) were undertreated, in contrast to 90 (49.2%) of patients using four or less medications. Of patients who were under‐prescribed, 65.1% used five medications or more. The highest percentage of under‐prescribing of medications was reported with statins in 115 patients (44.2%) followed by aspirin in 93 (35.7%), and ACE inhibitors in 61 (23.4%). The mean PPOs was 1.6 ± 0.82 with a range of 1–4 medications. Table 2 shows the most frequently under‐prescribed medications.
Table 2.
PPOs according to START Criteria (n = 260)
| Underprescribed drug (n = 424) | Number of patients (%) (n = 260) | Condition |
|---|---|---|
| Statins (115/424) | 115 (44.2) | Documented history of coronary, cerebral, or peripheral vascular disease, where the patient's functional status remains independent for activities of daily living and life expectancy ˃5 years |
| Diabetes mellitus plus ≥ 1 co‐existing major cardiovascular risk factor present | ||
| Aspirin (93/424) | 93 (35.7) | Documented history of atherosclerotic coronary, cerebral or peripheral vascular disease in patients with sinus rhythm |
| Following an acute MI | ||
| ACE inhibitors (61/424) | 61 (23.4) | Chronic heart failure |
| Following acute myocardial infarction | ||
| Beta blockers (30/424) | 30 (11.5) | With chronic stable angina |
| Clopidogrel (27/424) | 27 (10.4) | Ischemic stroke |
| PVD | ||
| Anticoagulants (26/424) | 26 (10) | Following diagnosis of DVT |
| Chronic atrial fibrillation | ||
| Calcium/vitamin D (21/424) | 21 (8.0) | Osteoporosis |
| PPI (12/424) | 12 (4.6) | For patients over 80 years old on antiplatelets |
| Antihypertensives (8/424) | 8 (3.0) | Systolic blood pressure consistently ˃160 mmHg |
| Bisphosphonates (7/424) | 7 (2.7) | Osteoporosis |
| Beta agonist (7/424) | 7 (2.7) | COPD |
| DMARD (7/424) | 7 (2.7) | Rheumatoid arthritis |
| Antidiabetics (5/424) | 5 (1.9) | Diabetes mellitus |
| Antidepressants (3/424) | 3 (1.1) | Depression |
| Fiber supplements (2/424) | 2 (0.8) | Constipation |
Abbreviations: ACE inhibitors, angiotensin‐converting enzyme inhibitors; DMARD, disease‐modifying antirheumatic drug; MI, myocardial infarction; PPI, proton pump inhibitor; PPO, potential prescribing omission; PVD: peripheral vascular disease.
Of the 260 patients with PPOs, 142 (31.9%) had only 1 PPOs, 82 (18.7%) had 2 PPOs, 26 (5.6%) had 3 PPOs, and only 10 (2.3%) had 4 PPOs. Figure 1. displays the number of under‐prescribed medications per patient.
Figure 1.
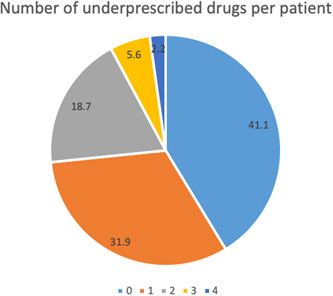
Number of potential prescribing omissions (PPOs) per patient (0 = 0 PPO, 1 = 1 PPO, 2 = 2 PPOs, 3 = 3 PPOs, 4 = 4 PPOs)
The results of the bivariate analysis showed that the monthly income p = 0.01, polypharmacy p < 0.001, and CCI p < 0.001were all significantly associated with under‐prescribing of medications (Table 3). The results of the multivariable analysis showed that only polypharmacy (OR 2.015, CI 95% 1.362–2.980, p < 0.001) and higher CCI (OR 2.807, CI 95% 1.463–5.85, p = 0.02) were statistically significant at 5% level of significance (Table 4).
Table 3.
Bivariate analysis of factors associated with under‐prescription of medications
| Characteristics | PPOs | p Value | |
|---|---|---|---|
| No (n = 184) | Yes (n = 260) | ||
| Age | |||
| 65–75 | 140 (76.1) | 181 (69.6) | 0.09 |
| >75 | 44 (23.9) | 79 (30.4) | |
| Gender | |||
| Male | 130 (71.0) | 175 (67.3) | 0.51 |
| Female | 53 (29.0) | 85 (32.7) | |
| Marital status | |||
| Married | 150 (81.5) | 210 (80.8) | 0.29 |
| Single | 14 (18.5) | 50 (19.2) | |
| Smoking | |||
| Yes | 109 (59.2) | 133 (51.2) | 0.16 |
| No | 75 (40.8) | 127 (48.8) | |
| Alcohol intake | |||
| Yes | 35 (19.0) | 44 (16.9) | 0.71 |
| No | 149 (81.8) | 216 (83.1) | |
| Monthly income | |||
| <3 million Lebanese pounds | 135 (73.4) | 160 (61.5) | 0.01* |
| >3 million Lebanese pounds | 49 (26.6) | 100 (38.5) | |
| Educational level | |||
| No schooling | 48 (26.1) | 84 (32.3) | 0.24 |
| High school | 81 (44.0) | 102 (39.2) | |
| University degree | 55 (29.9) | 74 (28.5) | |
| Polypharmacy | |||
| Yes | 91 (49.5) | 170 (65.4) | <0.001* |
| No | 93 (50.5) | 90 (34.6) | |
| Charlson Comorbidity Index | |||
| Mild (1–2) | 43 (23.4) | 22 (8.5) | <0.001* |
| Moderate (3–4) | 50 (27.2) | 68 (26.2) | |
| Severe (≥5) | 91 (49.5) | 170 (65.4) | |
Abbreviation: PPOs, potential prescribing omissions.
Significant.
Table 4.
Multivariable logistic regression analysis taking the under‐prescription of medications as the dependent variable
| Characteristics | AOR (95% CI) | p Value |
|---|---|---|
| Monthly income | 0.497 (0.233–1.058) | 0.07 |
| Polypharmacy | 2.015 (1.362–2.980) | <0.001* |
| Charlson Comorbidity Index | 2.807 (1.463–5.385) | 0.02* |
Abbreviation: AOR, adjusted odds ratio.
Significant.
5. DISCUSSION
Our study reported a high prevalence of PPOs s and found that polypharmacy and multimorbidity were significantly associated with under‐prescribing of medications in older adult outpatients in Lebanon. Despite the increase in multimorbidity and polypharmacy among older adults, omission of potentially beneficial medications remains widespread, where the odds of under‐prescribing of medications usually increase with the number of administered medications. 16 While optimizing polypharmacy should be of a major concern among healthcare personnel, avoiding under‐prescribing of medications in the process should not be of less importance.
According to the START criteria, and similar to other studies, at least one PPO was detected among more than half of the participants. This is in line with data from Gallagher et al.'s (58%), Beer et al.'s (56.7%), and Barry et al.'s (57.9%) studies. 17 , 23 , 24 This prevalence is high in comparison with other studies: Gorup et al.'s (42.9%), Ryan et al.'s (22.7%), and Ubeda et al.'s (44%) studies. 15 , 16 , 25 In Meid et al.'s study, however, medication underuse was detected in 69.1% of the total enrolled participants. Among the potential reasons behind this variability in PPO prevalence could be the variation in study designs and study populations. 26
More importantly, more than two‐third (65.1%) of patients receiving five or more medications were undertreated which is similar to that reported by Steinman et al. (64%) but way higher than that reported by Kujiper et al. in their study (43%). 27 , 28 Similarly, this notable variation in undertreatment may be in part related due to heterogeneity of study design and studied participants. Among undertreated patients, a mean of 1.6 medications were lacking, which nears that reported in the latter study (1.4) but exceeded that reported by Steinman et al. (1.0). 27 , 28 Similar to Ryan et al.'s study, PPOs detected in this study were identified by Fifteen of the 22 criteria (68.2%) in START with a marked predominance of cardiovascular medications. 15 Although PPOs related to the endocrine system (2%), central nervous system (1.2%), and gastrointestinal system were reported, thus opposing Ryan et al.'s study, these PPOs were markedly limited. 15
The most frequently omitted medications in this study (statins: 46%) mirrors other preceding findings reported by previous studies, where it has been seen in up to 60% of the enrolled patients. 29 , 30 , 31 This may reflect the decreased communication between healthcare personnel overseeing those patients, controversial opinions among them, increased concern about the risk‐benefit ratio of statins among the frail geriatrics especially with the poor pool of reports and clinical trials in the older adults. It has been also suggested in Glynn et al.'s study that the pattern of preventive medicines prescription to be generally affected by frailty of the individuals. 31 Neutel et al. also proposed that statin prescribing omission is affected by the patient's BMI. 32 Similarly, in Meid et al.'s study, BMI was positively correlated with under‐prescribing of medications (p = 0.018), while frail participants had more than two‐fold increased odds of undertreatment (p = 0.006). 26
Aspirin (35.7%) was the second commonest medication under‐prescribed in this study. Likewise, aspirin was the mainly identified cardiovascular PPO in Ryan et al.'s study. 15 While aspirin has an evident benefit in secondary cardiovascular complications prevention and is considered generally safe in older adults, its use may be sometimes withheld because of increased risk of bleeding with age. However, in the current study, no clear relationship has been found between age and under‐prescribing of medications which refutes such a suggestion. Another common medication under‐prescribing of medications which was evident in our study is ACEI under‐prescribing of medications (23.4%). ACE inhibitors were also most frequently indicated but not prescribed in Jabri et al.'s study (62.9%) in Iraq. 33 A common misunderstanding that is present among physicians is the unnecessity of ACE inhibitor/ARB in case of normal blood pressure. However, given their ability to improve survival, decrease cardiac remodeling, and decrease readmission rate, ACE inhibitor/ARB should be prescribed for ACS patients even if they are normotensive. This finding should be highlighted as less than half of ACS patients (40%) were found to be discharged with optimal secondary prevention medications, according to a former study conducted by Safwan et al. in Lebanon. 34
Similar to Candeias et al.'s, Ryan et al.'s, and Gallagher et al.'s studies, CCI (p = 0.02) in the present study was a pivotal determinant of underscription. 15 , 23 , 35 Based on recently reported studies, undertreatment among older adults was mainly reported for major cardiovascular diseases (including hyperlipidaemia), osteoporosis, COPD, depression, and cancer. 36 , 37 , 38 Preventative statin administration for cardiovascular conditions was mainly lacking in our study. This may be in part due to the “treatment‐risk paradox” where high‐risk populations tend to receive less‐intensive treatment regimens.
A significant association was also detected between under‐prescribing of medications and polypharmacy (p < 0.001). This may be a result of physicians' fear of complex medication regimens, ADRs, medication‐medication interactions, and decreased adherence with polypharmacy. However, the medications described in the START criteria have well‐established evidence in the older adults, which disapproves their reluctance. On the flip side, in Steinman et al., Ryan et al.'s (p = 0.28), and Gorup et al.'s studies, the incidence of PPOs was independent of the total number of prescribed medications and polypharmacy. 15 , 16 , 27 This negates the chance of reducing undertreatment with the increase in the number of medications, as concluded by Meid et al. in their study where the odds for medication underuse was minimized with the increase in the number of medications (p < 0.001). 26 Furthermore, in contrast to our study, Gorup et al. and Barry et al. detected a significant impact of age on the presence of PPOs in their studies especially in patients older than 85 years (p < 0.01). 16 , 24 On the contrary, an inverse relationship with age—a decline in incidence with increased age—was reported in Meid et al.'s and Ubeda et al.'s studies. 25 , 26 Under‐prescription of medications was also more likely to be seen among females according to Barry et al.'s (odds ratio 2.29, confidence interval 1.65–3.19, p < 0.01) and Jabari et al.'s (p = 0.028) studies but had no effect in our study. 24 , 33
5.1. Strengths and limitations
This is a multicentered study that is the first to assess polypharmacy and under‐prescribing of medications in Lebanon, as well as other predictors of under‐prescribing of medications using a validated instrument. The attended pharmacies were located in different Lebanese districts, therefore endorsing the representative of the sample and generalizability of the data. However, under‐estimation and overestimation of under‐prescription are still possible due to incomplete documentation from the patient or lack of knowledge about a rationale condition for therapeutic omission from the prescribing physician. Recall bias concerning the history of used medications is also possible. Moreover, we did not assess whether polypharmacy was appropriate in this study or not through checking for PIMs. In addition, this study was limited to community‐dwelling active and cognitively conscious geriatrics. Finally, this is a cross‐sectional study which impedes the possibility of drawing causal interpretations from the collected data.
6. CONCLUSION
In conclusion, the present findings highlight that PPOs are highly prevalent among community‐dwelling older adults in Lebanon. Multimorbidity and polypharmacy were the identified predictors for under‐prescription of medications in this population, while other participants' characteristics (i.e., age, gender, and economic status) had no impact. Our findings amplify the importance of ongoing prescribing review using the START tool to optimize patient care, particularly as patients get older, receive more medications or develop more illnesses. Further research is planned to study the association between PPOs and detrimental health outcomes among older individuals.
AUTHOR CONTRIBUTIONS
Conceptualization and methodology: Bahia Chahine. Formal analysis: Bahia Chahine and Venise Hanna. Writing—original draft preparation: Farah Al Souheil and Venise Hanna. Writing—review and editing: Bahia Chahine, Farah Al Souheil, and Venise Hanna. All authors have read and approved the final version of the manuscript. We had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
CONFLICT OF INTEREST
The author declares no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Bahia Chahine affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
ETHICS STATEMENT
Ethical approval was obtained for the study (Ref: 2021RC‐037‐LIUSOP).
ACKNOWLEDGMENT
There was no relevant financial support related to this research.
Hanna V, Chahine B, Al Souheil F. Under‐prescription of medications in older adults according to START criteria: a cross‐sectional study in Lebanon. Health Sci. Rep. 2022;5:e759. 10.1002/hsr2.759
DATA AVAILABILITY STATEMENT
The datasets used and analyzed during the current study are available on reasonable request.
REFERENCES
- 1. United Nations . Department of Economics and Social Affairs. Population Dynamics. 2019 Revision of World Population Prospects; 2019. Accessed May 28, 2021. https://population.un.org/wpp/
- 2. Abdulrahim S, Ajrouch KJ, Antonucci TC. Aging in Lebanon: challenges and opportunities. Gerontologist. 2015;55(4):511‐518. 10.1093/geront/gnu095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bootman JL, Harrison DL, Cox E. The health care cost of drug‐related morbidity and mortality in nursing facilities. Arch Intern Med. 1997;157(18):2089‐2096. [PubMed] [Google Scholar]
- 4. Merle L, Laroche ML, Dantoine T, Charmes JP. Predicting and preventing adverse drug reactions in the very old. Drugs Aging. 2005;22(5):375‐92. [DOI] [PubMed] [Google Scholar]
- 5. Kowal P, Dowd JE. Definition of an older person. Proposed Working Definition of an Older Person In Africa for the MDS Project. World Health Organization; 2001. [Google Scholar]
- 6. Rankin A, Cadogan CA, Patterson SM, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev. 2018;9(9):CD008165. 10.1002/14651858.CD008165.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Avery T, Payne R. Polypharmacy and Medicines Optimisation: Making it Safe and Sound. The King's Fund; 2013. [Google Scholar]
- 8. Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 19992012. JAMA. 2015;314(17):1818‐1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhang X, Zhou S, Pan K, et al. Potentially inappropriate medications in hospitalized older patients: a cross‐sectional study using the Beers 2015 criteria versus the 2012 criteria. Clin Interv Aging. 2017;12:1697‐1703. 10.2147/CIA.S146009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Reeve E, Wiese MD, Hendrix I, Roberts MS, Shakib S. People's attitudes, beliefs, and experiences regarding polypharmacy and willingness to deprescribe. J Am Geriatr Soc. 2013;61(9):1508‐1514. [DOI] [PubMed] [Google Scholar]
- 11. Chahine B. Potentially inappropriate medications prescribing to elderly patients with advanced chronic kidney by using 2019 American Geriatrics Society Beers Criteria. Health Sci Rep. 2020;3(4):e214. 10.1002/hsr2.214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Opondo D, Eslami S, Visscher S, et al. Inappropriateness of medication prescriptions to elderly patients in the primary care setting: a systematic review. PLoS One. 2012;7(8):e43617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Blanco‐Reina E, Ariza‐Zafra G, Ocaña‐Riola R, León‐Ortíz M, Bellido‐Estévez I. Optimizing elderly pharmacotherapy: polypharmacy vs. undertreatment. Are these two concepts related? Eur J Clin Pharmacol. 2015;71(2):199‐207. 10.1007/s00228-014-1780-0 [DOI] [PubMed] [Google Scholar]
- 14. Cherubini A, Corsonello A, Lattanzio F. Underprescription of beneficial medicines in older people: causes, consequences and prevention. Drugs Aging. 2012;29(6):463‐475. 10.2165/11631750-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 15. Ryan C, O'Mahony D, Kennedy J, Weedle P, Byrne S. Potentially inappropriate prescribing in an Irish elderly population in primary care. Br J Clin Pharmacol. 2009;68(6):936‐947. 10.1111/j.1365-2125.2009.03531.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gorup EC, Šter MP. Number of medications or number of diseases: what infuences underprescribing? Eur J Clin Pharmacol. 2017;73(12):1673‐1679. 10.1007/s00228-017-2336-x [DOI] [PubMed] [Google Scholar]
- 17. Beer C, Hyde Z, Almeida OP, et al. Quality use of medicines and health outcomes among a cohort of community dwelling older men: an observational study. Br J Clin Pharmacol. 2011;71(4):592‐599. 10.1111/j.1365-2125.2010.03875.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. O'Mahony D, O'Sullivan D, Byrne S, O'Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2[published correction appears in Age Ageing. 2018;47(3):489]. Age Ageing. 2015;44(2):213‐218. 10.1093/ageing/afu145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gallagher P, Ryan C, Byrne S, Kennedy J, O'Mahony D. STOPP (Screening Tool of Older Person's Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46(2):72‐83. 10.5414/cpp46072 [DOI] [PubMed] [Google Scholar]
- 20.Collaborative network to advance deprescribing research for older adults with multiple chronic conditions. National Institutes of Health—Office of Extramural Research. Accessed August 20, 2019. https://grants.nih.gov/grants/guide/rfa-files/RFA-AG-19-005.html
- 21. Wade DT, Vergis E. The short orientation‐memory‐concentration test: a study of its reliability and validity. Clin Rehabil. 1999;13(2):164‐170. 10.1191/026921599673848768 [DOI] [PubMed] [Google Scholar]
- 22. Hall WH, Ramachandran R, Narayan S, Jani AB, Vijayakumar S. An electronicapplication for rapidly calculating Charlson comorbidity score. BMC Cancer. 2004;4:94. 10.1186/1471-2407-4-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gallagher P, Lang PO, Cherubini A, et al. Prevalence of potentially inappropriate prescribing in an acutely ill population of older patients admitted to six European hospitals. Eur J Clin Pharmacol. 2011;67(11):1175‐1188. 10.1007/s00228-011-1061-0 [DOI] [PubMed] [Google Scholar]
- 24. Barry PJ, Gallagher P, Ryan C, O'mahony D. START (screening tool to alert doctors to the right treatment)—an evidence‐based screening tool to detect prescribing omissions in elderly patients. Age Ageing. 2007;36(6):632‐638. 10.1093/ageing/afm118 [DOI] [PubMed] [Google Scholar]
- 25. Ubeda A, Ferrándiz L, Maicas N, Gomez C, Bonet M, Peris JE. Potentially inappropriate prescribing in institutionalised older patients in Spain: the STOPP‐START criteria compared with the Beers criteria. Pharm Pract (Granada). 2012;10(2):83‐91. 10.4321/s1886-36552012000200004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Meid AD, Quinzler R, Freigofas J, et al. Medication underuse in aging outpatients with cardiovascular disease: prevalence, determinants, and outcomes in a prospective cohort study. PLoS One. 2015;10(8):e0136339. 10.1371/journal.pone.0136339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Steinman MA, Landefeld CS, Rosenthal GE, Berthenthal D, Sen S, Kaboli PJ. Polypharmacy and prescribing quality in older people. J Am Geriatr Soc. 2006;54:1516‐1523. [DOI] [PubMed] [Google Scholar]
- 28. Kuijpers MA, van Marum RJ, Egberts AC, Jansen PA, OLDY (OLd people Drugs & dYsregulations) Study Group . Relationship between polypharmacy and underprescribing. Br J Clin Pharmacol. 2008;65(1):130‐133. 10.1111/j.1365-2125.2007.02961.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gaw A. The care gap: underuse of statin therapy in the elderly. Int J Clin Pract. 2004;58(8):777‐785. 10.1111/j.1368-5031.2004.00300.x [DOI] [PubMed] [Google Scholar]
- 30. De Wilde S, Cook DG, Carey IM, Hilton SR, Whincup PH. Underuse of statins among older people. Lancet. 2003;362(9385):746‐747. 10.1016/s0140-6736(03)14216-x [DOI] [PubMed] [Google Scholar]
- 31. Glynn RJ, Schneeweiss S, Wang PS, Levin R, Avorn J. Selective prescribing led to overestimation of the benefits of lipid‐lowering drugs. J Clin Epidemiol. 2006;59(8):819‐828. 10.1016/j.jclinepi.2005.12.012 [DOI] [PubMed] [Google Scholar]
- 32. Neutel CI, Morrison H, Campbell NR, de Groh M. Statin use in Canadians: trends, determinants and persistence. Can J Public Health. 2007;98(5):412‐416. 10.1007/BF03405430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jabri AM, Assad HC, Al‐Jumaili AA. Pharmacist role to enhance the prescribing of hospital discharge medications for patients after heart attack. Saudi Pharm J. 2020;28(4):473‐479. 10.1016/j.jsps.2020.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Safwan J, Hamwi H, Shamsedeen L, et al. Evaluation of the adherence to the discharge management for secondary prevention of acute coronary syndrome in Lebanon. J Cardiol Clin Res. 2017;5(2):1097. [Google Scholar]
- 35. Candeias C, Gama J, Rodrigues M, Falcão A, Alves G. Potentially inappropriate medications and potential prescribing omissions in elderly patients receiving post‐acute and long‐term care: application of screening tool of older people's prescriptions/screening tool to alert to right treatment criteria. Front Pharmacol. 2021;12:747523. 10.3389/fphar.2021.747523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kuzuya M, Masuda Y, Hirakawa Y, et al. Underuse of medications for chronic disease in the oldest of community‐dwelling older frail Japanese. J Am Geriatr Soc. 2006;54:598‐605. [DOI] [PubMed] [Google Scholar]
- 37. Soumerai SB, McLaughlin TJ, Spiegelman D, Hertzmark E, Thibault G, Goldman L. Adverse outcomes of underuse of beta‐blockers in elderly survivors of acute myocardial infarction. JAMA. 1997;277:115‐121. [PubMed] [Google Scholar]
- 38. Lee DS, Tu JV, Juurlink DN, et al. Risk‐treatment mismatch in the pharmacotherapy of heart failure. JAMA. 2005;294:1240‐1247. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available on reasonable request.


