Abstract
Background and Aims
An important but much less researched burden of human immunodeficiency virus (HIV) in Sub‐Saharan Africa includes the associated mental health outcomes of living with the virus. This study aimed to estimate the prevalence of depression, anxiety, and stress, and describe some of the socio‐demographic associations among people living with HIV (PLHIV) in Ghana.
Methods
A cross‐sectional study was conducted at the Cape Coast Teaching Hospital, Ghana. Simple random sampling was used to recruit 395 PLHIV who access HIV‐related services at the antiretroviral therapy clinic. The Depression, Anxiety, and Stress Scale‐21 was used to assess prevalence of depression, anxiety, and stress. Frequencies and percentages were used to estimate the prevalence and multivariable logistic regression was used to evaluate sociodemographic factors associated with depression, anxiety, and stress.
Results
The prevalence estimates of depression, anxiety, and stress among PLHIV were 28.6% (95% confidence interval [CI] 24.4–33.3), 40.8% (95% CI = 36.0–45.8), and 10.6% (95% CI = 7.9–14.1), respectively. Females reported higher prevalence of depression (32.2%; 95% CI = 27.2–37.7), anxiety (44.0%; 95% CI = 38.4–49.6), and stress (12.6%; 95% CI = 9.4–17.0) compared to depression (17.5%; 95% CI = 11.1–26.4), anxiety (30.9%; 95% CI = 22.5–40.7), and stress (4.1%; 95% CI = 1.2–10.4) among males. PLHIV without a regular partner were about 0.63 increased odds of experiencing anxiety compared to those with a regular partner (AOR = 0.63, 95% CI = 0.40–1.00: p = 0.049). PLHIV without formal education were about 0.49 and 0.44 increased odds to experience anxiety and stress, respectively compared to those with tertiary education.
Conclusions
Generally, the levels of stress, anxiety, and depression are high among PLHIV, but disproportionately higher among females. Mental health assessment and management should be integrated into the HIV care services. There should be capacity building for health care workers to offer differentiated service delivery based on mental health care needs of PLHIV.
Keywords: anxiety, depression, Ghana, mental health, people living with HIV, stress
1. BACKGROUND
Human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) remains a global menace and impacts significantly on the lives of individuals and their families despite the significant advances in its prevention and treatment. It is claimed that full gains of prevention and treatment will not be achieved without addressing the mental health needs of people living with HIV (PLHIV). 1 In Ghana, it is estimated that there are about 342,307 people (122,321 males and 219,986 females) living with HIV, representing a 12‐month prevalence rate of about 2%. 2 The chronicity of HIV/AIDS is not only impacting on physical health but is also having enormous challenges on psychological wellbeing. 3 In particular, HIV‐related stigma, depression, anxiety, and stress have been reported among PLHIV. 4 , 5 , 6
Thus, a major burden of living with HIV relates to the negative mental health outcomes and the psychosocial impact of the disease, including stigma, depression, anxiety, self‐esteem, loneliness, and reduced quality of life. 3 , 4 Studies suggest that PLHIV often suffer from depression and anxiety disorders as they adjust to the diagnosis, struggle with the meaning of a positive test result, adapt to life with chronic, life‐threatening illness, and witness of the death of a family member or a friend with HIV/AIDS. 7 , 8
Evidence suggests higher estimates of mental disorders in PLHIV. Recent studies from high‐income countries, for example, the United States, suggest a 36% prevalence of depression and 16% anxiety disorders among a large national sample of HIV‐positive men and women during the previous 12 months. 9 In sub‐Sahara Africa, the prevalence of mental disorders among PLHIV during a period of 3 months was estimated to be as high as 19%. 10 For example, it is estimated that 32% and 34.4% of people living with HIV in South Ethiopia suffer from depression and anxiety, respectively. 4
Given the evidence of strong association of poor mental health outcomes with living with HIV, there is a need for both targeted and universal mental health screening and having mental health prevention and treatment options integrated into HIV care regimes. 1 Although mental health has been integrated into the care of HIV/AIDS mostly in high‐income countries as a result of substantial evidence supporting the linkage between mental health and HIV, little is still known in sub‐Sahara African countries, including Ghana. 8
Considering that Ghana is a signatory to the UN 2030 Agenda for Sustainable Development, we believe a carefully designed study like the current one can, potentially, contribute evidence that supports the country's broad efforts towards attaining Goal 3 of the Sustainable Development Agenda: “Ensuring healthy lives and promote well‐being for all at all ages.” 11 Specifically, this study sought to estimate the prevalence of mental health challenges and describe some of the socio‐demographic associations among PLHIV presenting to a teaching hospital in Ghana. This paper focuses on the prevalence and factors associated with depression, anxiety, and stress.
2. METHODS
2.1. Study design and study area
This is a hospital‐based analytical cross‐sectional study conducted at the Cape Coast Teaching Hospital in Ghana, between May and December 2021. The hospital has the highest number of clients at the antiretroviral therapy (ART) clinic in the Central Region of Ghana. It is a 400‐bed capacity teaching hospital affiliated with the School of Medical Sciences at the University of Cape Coast, Ghana.
3. POPULATION AND SAMPLING PROCEDURE
The population for this study included all adults (aged 18 years and above) living with HIV/AIDS who received service from the Cape Coast Teaching Hospital. Data available from the facility in the year 2019 suggested that there were 3972 PLHIV presenting to the facility. The inclusion criteria for this study were adults aged at least 18 years with a confirmed diagnosis of HIV/AIDS for at least 12 months and receiving care at the Cape Coast Teaching Hospital. The first 6 months of ART are critical in the care of PLHIV. Some PLHIV may not respond as expected to the treatment or may even deteriorate clinically. 3 This would have affected the findings of this study. Therefore, people living with HIV on ART for 12 months were considered eligible for this study.
The sample size was predetermined by applying the Miller and Brewer's formula: at 95% confidence level, n = . Where: n= desired sample size, N = target population (3972), a = level of statistical significance (0.05), and 1 is a constant. 12
Therefore, n (the predetermined sample size) = 363. However, to make up for incomplete data, the sample size was increased by 10% bringing the predetermined sample size to 399. 13
A simple random sampling technique was used to recruit participants. The sample frame was determined by acquiring the list of all adults living with HIV/AIDS who received service from the ART clinic from the hospital's records department. Each name in the sample frame was numbered. A random number generator was used to generate random numbers and registered the name in the sample frame corresponding to the numbers to constitute the sample. This was continued until the required number of participants (399) was met.
4. MEASURES
Data were collected using a self‐report anonymous questionnaire. The questionnaire had three sections. The first section focused on socio‐demographic characteristics of participants (e.g., age, gender, education, marital status, employment status, information on antiretroviral medication, other underlying physical health conditions, and support networks). The final section of the questionnaire comprised the Depression, Anxiety and Stress Scale‐21 (DASS‐21)—a set of three self‐report scales designed to measure the states of depression, anxiety, and stress among adults. 14 Each of the three DASS‐21 subscales contains seven items with similar contents. DASS‐21 is a 21‐item self‐report scale on a 4‐point scale: 0—(did not apply to me at all—never), 1—(applied to me some of the time—sometimes), 2—(applied to me a considerable degree—often), and 3—(applied to me most of the time—almost always). Some example items are “I found it hard to wind down,” “I experienced trembling,” I felt down‐hearted and blue.” Participants indicated how much a statement applied to them over the previous 1 week. Scores for depression, anxiety, and stress were calculated by summing the scores for the relevant items: depression (normal = 0–4, mild = 5–6, moderate = 7–10, severe = 11–13, and extremely severe = 14+), anxiety (normal = 0–3, mild = 4–5, moderate = 6–7, severe = 8–9, and extremely severe = 14+), and stress (normal = 0–7, mild = 8–9, moderate = 10–12, severe = 13–16, extremely severe = 17+). DASS‐21 has satisfactory Cronbach alpha for each subscale (depression = 0.88, anxiety = 0.82, and stress = 0.90). 15
Five research assistants with at least a bachelor's degree were recruited to assist with data collection. They were trained on the type of information to be collected from participants and how to uphold the ethical position of the data collection process and the entire study protocol. The training lasted for 4 h and ensures that they understood the data collection instrument. The questionnaires were administered privately to each participant by the first author or a trained research assistant at a convenient place at the ART clinic (e.g., selected consulting rooms). Averagely, it took each participant approximately 20 min to complete the questionnaire. Participants who were not literate were assisted by the first author or research assistants to complete the questionnaire. Three hundred and ninety‐five questionnaires were returned with complete data, yielding a response rate of 99%.
Pre‐testing of the instrument was conducted to establish the appropriateness of the instrument and determine how feasible they would translate into the local dialect in the full‐scale study. The instrument was administered to 40 people and the feedback from pretesting was used to improve the use of the instrument.
This study was performed in accordance with the Helsinki Declaration and approved by the Ethics Review Committee of Cape Coast Teaching Hospital, Ghana (reference: CCTHERC/EC/2021/028). The purpose of the study, anonymity, voluntary participation, and confidentiality of the information were explained to participants to seek their written consent. Only those who gave written informed consent were included in the study. Participants could withdraw from the study at any point without any adverse effect. The hospital where the study was carried out gave permission for the study to be carried out.
5. DATA ANALYSIS
STATA version 16 was used for the statistical analysis. Frequencies and percentages were used to estimate the prevalence, summary statistics was based on the distribution of the data. For normally distributed variables, mean and standard deviation was used. Bivariable analysis using t‐test or χ 2 test (as appropriate) and multivariable logistic regression were used to evaluate sociodemographic factors and risky health behaviors associated with depression, anxiety, and stress. Age and gender were the only a priory variable. Sociodemographic variables were included in the final logistics model regardless of the statistical significance of their bivariable associations with the outcomes. However, variables with acute sparse data were excluded. 16 For ease of data interpretation, each of the outcomes (depression, anxiety, and stress) were dichotomized. The response categories “mild,” “moderate,” “severe,” and “extremely severe” were merged and renamed “depressed,” “anxious,” and “stressed,” while the remaining response category, “normal,” was maintained to indicate “normal mood level,” “normal anxiety level,” and “normal stress level.” Statistical significance was based on the p‐value (p < 0.05) and associated 95% confidence interval (95% CI).
6. RESULTS
6.1. Demographic data of participants
Out of 395 participants recruited for this study, 52.2% (n = 206) were within the 40–59 years group (mean: 46.79; SD: ±12.53), and 75.4% (n = 298) of the participants were female. It was found that 61.8% (n = 244) of the participants were without a regular partner and 16.7% (n = 66) reported having additional comorbidities. Additionally, 77.7% (n = 307) of the participants were self‐employed (Table 1).
Table 1.
Socio‐demographic and clinical characteristics of participants (N = 395)
| Characteristic | Category | n (% or SD) |
|---|---|---|
| Age (years) | ||
| Mean | 46.7 (12.5) | |
| 20–39 | 122 (30.8) | |
| 40–59 | 206 (52.2) | |
| 60–80 | 67 (17.0) | |
| Gender | ||
| Male | 97 (24.6) | |
| Female | 298 (75.4) | |
| Marital status | ||
| Currently with a regular partner | 151 (38.2) | |
| Currently without a regular partner | 244 (61.8) | |
| Religion | ||
| Christian | 355 (89.9) | |
| Islam | 31 (7.8) | |
| Traditionalist | 3 (0.8) | |
| No religion | 6 (1.5) | |
| Employment status | ||
| Employed by other | 12 (3.0) | |
| Employed by self | 307 (77.7) | |
| Unemployed | 76 (19.2) | |
| Educational level | ||
| Tertiary | 38 (9.6) | |
| Nontertiary | 246 (62.3) | |
| No education | 111 (28.1) | |
| Do you drink alcohol? | ||
| Yes | 17 (4.3) | |
| No | 378 (95.7) | |
| Have a comorbid condition(s) | ||
| Yes | 66 (16.7) | |
| No | 329(3.3) |
The topmost co‐morbid conditions were hypertension (60.6%, n = 40) followed by diabetes (7.6%, n = 5) and asthma (6.1%, n = 4) (Figure 1).
Figure 1.
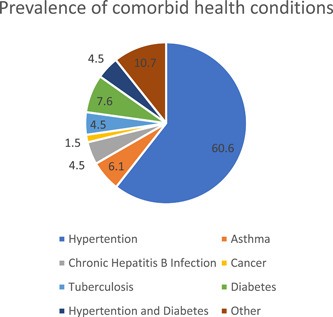
Prevalence of comorbid health conditions among participants (N = 66). “Other conditions” included peptic ulcer and uterine fibroids.
6.2. Prevalence estimates of depression, anxiety, and stress
Overall, varying prevalence estimates of depression (8.6%; 95% CI = 24.4–33.3), anxiety (40.8%; 95% CI = 36.0–45.8), and stress (10.6%; 95% CI = 7.9–14.1) were reported during the past week among PLHIV. As shown in Table 2, notably, relative to males, higher estimates were reported among females across the three outcomes.
Table 2.
Prevalence estimates of depression, anxiety, and stress among participants (N = 395)
| Characteristics | Variables | |||||
|---|---|---|---|---|---|---|
| Depression | Anxiety | Stress | ||||
| n (%) | 95% CI | n (%) | 95% CI | n (%) | 95% CI | |
| Overall | 113 (28.6) | 24.4–33.3 | 161 (40.8) | 36.0–45.8 | 42 (10.6) | 7.9–14.1 |
| Female | 96 (32.2) | 27.2–37.7 | 131 (44.0) | 38.4–49.6 | 37 (12.4) | 9.4–17.0 |
| Male | 17 (17.5) | 11.1–26.4 | 30 (30.9) | 22.5–40.7 | 4 (4.1) | 1.2–10.4 |
Abbreviation: CI, confidence interval.
7. FACTORS ASSOCIATED WITH DEPRESSION, ANXIETY, AND STRESS
7.1. Depression
Overall, only gender showed a statistically significant independent association with depression. Specifically, the multivariable logistic analysis (Table 3) showed that females were at approximately 0.5 increased odds of experiencing depression during the previous week compared to males (AOR = 0.48, 95% CI = 0.25–0.91: p = 0.03).
Table 3.
Factors associated with depression, anxiety, and stress
| Characteristics | Depression | Anxiety | Stress | ||||||
|---|---|---|---|---|---|---|---|---|---|
| χ 2 (p) | AOR (95% CI) | p | χ 2 (p) | AOR (95% CI) | p | χ 2 (p) | AOR (95% CI) | p | |
| Age | 1.16 (0.56) | ‐ | ‐ | 1.04 (0.59) | ‐ | ‐ | 1.97 (0.37) | ‐ | ‐ |
| 20–39 | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| 40–59 | ‐ | 1.23 (0.59–2.58) | 0.58 | ‐ | 1.65 (0.85–3.21) | 0.14 | ‐ | 0.63 (0.21–1.84) | 0.39 |
| 60–80 | ‐ | 1.38 (0.70–2.66) | 0.36 | ‐ | 1.35 (0.74–2.47) | 0.33 | ‐ | 0.87 (0.35–2.17) | 0.77 |
| Gender | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Male | 7.73 (0.003) | Ref | ‐ | 5.15 (0.02) | Ref | ‐ | 5.73 (0.01) | Ref | ‐ |
| Female | ‐ | 0.48 (0.25–0.91) | 0.03 | ‐ | 0.78 (0.45–1.34) | 0.36 | ‐ | 0.34 (0.11–1.04) | 0.06 |
| Marital status | 1.42 (0.14) | ‐ | ‐ | 5.92 (0.01) | ‐ | ‐ | 0.43 (0.31) | ‐ | ‐ |
| Currently with a regular partner | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| Currently without a regular partner | ‐ | 0.87 (0.53–1.42) | 0.56 | ‐ | 0.63 (0.40–1.00) | 0.05 | ‐ | 1.81 (0.89–3.69) | 0.10 |
| Religion | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Christian | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| Islam | ‐ | 1.13 (0.47–2.73) | 0.78 | ‐ | 0.89 (0.41–1.96) | 0.77 | ‐ | 3.84 (0.49–29.99) | 0.20 |
| Employment status | 1.01 (0.59) | ‐ | ‐ | 4.34 (0.11) | ‐ | ‐ | 3.21 (0.20) | ‐ | ‐ |
| Employed by other | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| Employed by self | ‐ | 1.29 (0.35–4.76) | 0.70 | ‐ | 2.45 (0.65–9.26) | 0.19 | ‐ | 2.70 (0.52–14.05) | 0.23 |
| Unemployed | ‐ | 0.85 (0.47–1.55) | 0.60 | ‐ | 0.79 (0.46–1.38) | 0.41 | ‐ | 1.06 (0.40–2.80) | 0.91 |
| Educational level | 6.93 (0.03) | ‐ | ‐ | 10.52 (0.01) | ‐ | ‐ | 8.86 (0.01) | ‐ | ‐ |
| Tertiary | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| Nontertiary | ‐ | 1.10 (0.47–2.58) | 0.83 | ‐ | 0.54 (0.24–1.24) | 0.15 | ‐ | 0.40 (0.10–1.62) | 0.19 |
| No formal education | ‐ | 0.62 (0.37–1.03) | 0.07 | ‐ | 0.49 (0.30–0.79) | 0.004 | ‐ | 0.44(0.21–0.89) | 0.02 |
| Do you drink alcohol | 1.37 (0.18) | ‐ | ‐ | 0.001 (0.58) | ‐ | ‐ | 0.92 (0.26) | ‐ | ‐ |
| Yes | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| No | ‐ | 1.95 (0.68–5.65) | 0.22 | ‐ | 1.06 (0.36–3.09) | 0.92 | ‐ | 1.50 (0.36–6.12) | 0.58 |
| Comorbid conditions | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Yes | 0.001 (0.54) | Ref | ‐ | 0.001 (0.54) | Ref | ‐ | 1.70 (0.14) | Ref | ‐ |
| No | ‐ | 1.00 (0.54–1.87) | 0.99 | 1.14 (0.64–2.03) | ‐ | ‐ | 1.69 (0.73–3.90) | 0.22 | |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval.
7.2. Anxiety
Marital status (AOR = 0.63, 95% CI = 0.40–1.00: p = 0.049) and educational level (AOR = 0.49, 95% CI = 0.30–0.79: p = 0.004) were associated with increased odds of reporting anxiety among participants. Participants without a regular partner were about 0.63 increased odds of experiencing anxiety during the previous week compared to those with a regular partner. Also, participants with no formal education were about 0.49 increased odds of experiencing anxiety during the past week compared to those with tertiary education (Table 3).
7.3. Stress
Similarly, across the total sample, only two factors showed significant bivariate associations with stress (i.e., gender and educational level), but in the logistic model, only education level showed an independent association with stress. Participants without formal education were about 0.44 increased odds of experiencing stress over the past week compared to those with tertiary education (AOR = 0.44, 95% CI = 0.21–0.89: p = 0.02) (Table 3).
8. GENDER DIFFERENCES IN FACTORS ASSOCIATED WITH DEPRESSION, ANXIETY, AND STRESS
The statistical analysis was stratified according to gender to assess the bivariable and multivariable associations of the three outcomes. Interestingly, in both the bivariable and multivariable analyses, no association reached the desired threshold of statistical significance among females (Table 4). However, in males, educational level was associated with depression (AOR = 0.11, 95% CI = 0.02–0.73: p = 0.02) and anxiety (AOR = 0.18, 95% CI = 0.04–0.86: p = 0.03). Males living with HIV without formal education were about 0.11 increased odds of experiencing depression over the past week compared to those with tertiary education. Also, male participants without formal education were about 0.18 increased odds of experiencing anxiety over the past week compared to those with tertiary education (Table 5).
Table 4.
Factors associated with depression, anxiety, and stress among females
| Characteristics | Depression | Anxiety | Stress | ||||||
|---|---|---|---|---|---|---|---|---|---|
| χ 2 (p) | AOR (95% CI) | p | χ 2 (p) | AOR (95% CI) | p | χ 2 (p) | AOR (95% CI) | p | |
| Age | 2.78 (0.25) | ‐ | ‐ | 0.48 (0.79) | ‐ | ‐ | 1.16 (0.56) | ‐ | ‐ |
| 20–39 | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| 40–59 | ‐ | 1.44 (0.62–3.34) | 0.40 | ‐ | 1.68 (0.78–3.61) | 0.185 | ‐ | 0.71 (0.23–2.22) | 0.56 |
| 60–80 | ‐ | 1.75 (0.82–3.72) | 0.15 | ‐ | 1.46 (0.73–2.92) | 0.28 | ‐ | 0.84 (0.31–2.23) | 0.72 |
| Marital status | 1.09 (0.35) | ‐ | ‐ | 2.40 (0.14) | ‐ | ‐ | 1.05 (0.35) | ‐ | ‐ |
| Currently with a regular partner | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| Currently without a regular partner | ‐ | 0.73 (0.42–1.28) | 0.28 | ‐ | 0.69 (0.41–1.16) | 0.159 | ‐ | 1.84 (0.87–3.91) | 0.11 |
| Religion | 0.04 (>0.99) | ‐ | ‐ | 0.24 (0.67) | ‐ | ‐ | 3.64 (0.06) | ‐ | ‐ |
| Christian | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| Islam | ‐ | 1.14 (0.43–3.05) | 0.79 | ‐ | 1.50 (0.58–3.83) | 0.40 | ‐ | ‐ | ‐ |
| Employment status | 0.94 (0.63) | ‐ | ‐ | 2.75 (0.25) | ‐ | ‐ | 2.75 (0.25) | ‐ | ‐ |
| Employed by other | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| Employed by self | ‐ | 1.70 (0.43–6.73) | 0.45 | ‐ | 1.84 (0.45–7.50) | 0.397 | ‐ | 2.96 (0.53–16.63) | 0.22 |
| Unemployed | ‐ | 0.88 (0.44–1.74) | 0.71 | ‐ | 0.60 (0.32–1.15) | 0.12 | ‐ | 0.98 (0.34–2.86) | 0.97 |
| Educational level | 2.44 (0.30) | ‐ | ‐ | 6.19 (0.05) | ‐ | ‐ | 5.11 (0.08) | ‐ | ‐ |
| Tertiary | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| Nontertiary | ‐ | 0.57 (0.19–1.68) | 0.31 | ‐ | 0.32 (0.11–0.88) | 0.027 | ‐ | 0.30 (0.06–1.59) | 0.16 |
| No formal education | ‐ | 0.76 (0.19–1.30) | 0.31 | ‐ | 0.55 (0.33–0.93) | 0.024 | ‐ | 0.48 (0.23–1.00) | 0.05 |
| Do you drink alcohol | 2.61 (0.18) | ‐ | ‐ | 0.52 (0.54) | ‐ | ‐ | 2.17 (0.15) | ‐ | ‐ |
| Yes | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| No | ‐ | 2.36 (0.67–8.32) | 0.18 | ‐ | 1.39 (0.39–4.93) | 0.61 | ‐ | 1.95 (0.43–8.75) | 0.38 |
| Comorbid conditions | 0.45 (0.63) | ‐ | ‐ | 0.16 (0.76) | ‐ | ‐ | 0.32 (0.65) | ‐ | ‐ |
| Yes | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| No | ‐ | 0.79 (0.40–1.58) | 0.50 | ‐ | 0.94 (0.50–1.79) | 0.86 | ‐ | 1.35 (0.54–3.39) | 0.53 |
Abbreviation: CI, confidence interval.
Table 5.
Factors associated with depression, anxiety, and stress among males
| Characteristics | Depression | Anxiety | Stress | ||||||
|---|---|---|---|---|---|---|---|---|---|
| χ 2 (p) | AOR (95% CI) | p | χ 2 (p) | AOR (95% CI) | p | χ 2 (p) | AOR (95% CI) | p | |
| Age | 1.99 (0.37) | ‐ | ‐ | 2.11 (0.35) | ‐ | ‐ | 1.81 (0.41) | ‐ | ‐ |
| 20–39 | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| 40–59 | ‐ | 0.86 (0.13–5.68) | 0.88 | ‐ | 2.58 (0.54–12.31) | 0.24 | ‐ | ‐ | ‐ |
| 60–80 | ‐ | 0.28 (0.04–1.86) | 0.19 | ‐ | 1.02 (0.25–4.14) | 0.97 | ‐ | 2.88 (0.19–44.61) | 0.45 |
| Marital status | 0.54 (0.59) | ‐ | ‐ | 1.78 (0.19) | ‐ | ‐ | 0.57 (0.63) | ‐ | ‐ |
| Currently with a regular partner | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| Currently without a regular partner | ‐ | 2.26 (0.41–12.51) | 0.35 | ‐ | 0.36 (0.11–1.14) | ‐ | ‐ | 0.95 (0.07–13.84) | 0.97 |
| Religion | 0.13 (>0.99) | ‐ | ‐ | 1.54 (0.24) | ‐ | ‐ | 1.28 (0.32) | ‐ | ‐ |
| Christian | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| Islam | ‐ | 2.65 (0.21–32.98) | 0.45 | ‐ | 0.36 (0.06–2.11) | 0.25 | ‐ | 0.42 (0.02–8.36) | 0.57 |
| Employment status | 0.91 (0.64) | ‐ | ‐ | 2.38 (0.30) | ‐ | ‐ | 0.07 (0.97) | ‐ | ‐ |
| Employed by other | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| Employed by self | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Unemployed | ‐ | 1.08 (0.20–5.93) | ‐ | ‐ | 2.26 (0.55–9.29) | ‐ | ‐ | 0.40 (0.02–9.51) | 0.57 |
| Educational level | 16.27 (<0.001) | ‐ | ‐ | 9.60 (0.01) | ‐ | ‐ | 1.67 (0.43) | ‐ | ‐ |
| Tertiary | ‐ | Ref | ‐ | Ref | ‐ | ‐ | Ref | ‐ | |
| Nontertiary | ‐ | 2.77 (0.35–21.78) | 0.93 | ‐ | 1.07 (0.16–7.10) | 0.94 | ‐ | 0.31 (0.01–11.60) | 0.53 |
| No formal education | ‐ | 0.11 (0.02–0.73) | 0.02 | ‐ | 0.18 (0.04–0.86) | 0.03 | ‐ | 0.11 (0.00–2.90) | 0.18 |
| Do you drink alcohol | 0.003 (>0.99) | ‐ | ‐ | 0.61 (0.66) | ‐ | ‐ | 0.28 (1.00) | ‐ | ‐ |
| Yes | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| No | ‐ | 1.91 (0.10–37.10) | 0.67 | ‐ | 0.64 (0.05–7.57) | 0.72 | ‐ | ‐ | ‐ |
| Comorbid conditions | 1.82 (0.23) | ‐ | ‐ | 0.40 (0.53) | ‐ | ‐ | 4.82 (0.09) | ‐ | ‐ |
| Yes | ‐ | Ref | ‐ | ‐ | Ref | ‐ | ‐ | Ref | ‐ |
| No | ‐ | 5.51 (0.76–39.94) | 0.09 | ‐ | 2.28 (0.45–11.47) | 0.32 | ‐ | 10.91 (0.63–188.49) | 0.10 |
Abbreviation: CI, confidence interval.
9. DISCUSSION
This study assessed the prevalence estimates of depression, anxiety, and stress and identified some of the socio‐demographic factors associated with these mental health challenges among PLHIV presenting to a teaching hospital in Ghana. Key findings indicate relatively high prevalence estimates of depression, anxiety, and stress. Approximately, 4 out of 10 PLHIV experienced depression, about 1 out of 5 reported anxieties, and 1 out of 10 self‐reported stress during the previous week. Relative to estimates reported by previous studies from high‐income countries, the estimates in the current study appear higher. 16 , 17 In the United Kingdom, the prevalence estimates of depression and anxiety among people living with HIV in the past 2 weeks were 19.8% and 13.1%, respectively. 16
Interestingly, it does appear that the estimates of the current study are comparable to estimates from other low‐ and middle‐income countries. For example, a cross‐sectional study in South Ethiopia using the hospital anxiety and depression scale indicated 32.0% and 34.4% prevalence of depression and anxiety, respectively among PLHIV. 4 Similarly, a study in India using DASS‐21 reported that 50% PLHIV suffered from depression. 3 Although the prevalence estimates of depression and anxiety (as reported by the current and previous studies) are high, the values still differ, particularly, when the estimates are viewed in actual counts/values. The prevalence estimates of depression, anxiety, and stress among PLHIV have been observed to differ worldwide. 16 , 17 , 18 , 19 , 20 , 21 , 22 Differences in the estimates have been attributed to different settings and methodological approaches used by available studies. In addition, cultural difference in response to surveys on mental health issues and social desirability bias due to social or self‐stigma might have contributed more to the similarities (than differences) in the estimates across low‐ and middle‐income countries.
The current study has also shown that females are more likely than males to report depression, anxiety, and stress. This evidence is consistent with findings from similar studies. 4 , 19 , 23 Generally, this finding is not surprising for the reason that females tend to experience and report more internalizing problems than males. 24 This study's findings further indicate that, a vast majority of PLHIV do not drink alcohol. It appears that, the estimates from this study are not consistent with findings of similar studies which indicate a high incidence of alcohol use among PLHIV. 28 , 29 , 30 Maladaptive means of coping may lead to an increase in the use of alcohol among PLHIV and may impact their health negatively. 29 , 30 The low consumption of alcohol among PLHIV in this current study, may be associated with the use an adaptive coping strategy. PLHIV require a great deal of social and emotional support to help them deal with the psychosocial burden of living with the virus. 25 However, within the socio‐cultural setup of Ghana, sexually transmitted diseases are highly stigmatized and gender inequality is still pervasive; women continue to experience inequality, lower social status, and increased vulnerability to discrimination and various forms of abuse. 25 In these circumstances, women living with HIV are more likely (than men) to experience social adversities, social ostracism and isolation, and an inability to attract meaningful social support, thereby increasing their vulnerability to negative mental health outcomes such as loneliness, depression, and anxiety.
The study findings suggest also that PLHIV without a regular partner are more likely to report anxiety compared to those with a regular partner. A cross‐sectional study in Zambia also found high prevalence of depression among unmarried, widowed, and divorced women. 19 People who are in less stressful marriages may be less vulnerable to mental health challenges. 26 Although marriage may not necessarily militate against the onset of mental illness in partners, meaningful spousal support may promote resilience and could present as a potential protective factor against mental health challenges among persons in marital relationships. 27 For PLHIV, having a supportive spouse is critical to promoting resilience in the face of mental health challenges. 28
The key finding that PLHIV without formal education (compared to those with tertiary education) are at increased odds of experiencing anxiety and stress is worth some comments. This evidence could be pointing to an outcome of the functional health literacy that PLHIV with formal/tertiary education must have received by virtue of having had formal classroom education. HIV/AIDS literacy remains a detailed part of the health education curriculum from basic schools through tertiary educational institutions in Ghana. 29 The implication is that, on the one hand, PLHIV who have had some formal education are more likely to hold educated beliefs about the virus and to draw on their acquired classroom knowledge and HIV literacy contents to inform their health behavior choices and coping strategies. PLHIV who have had no formal education, on the other hand, may struggle (possibly without success) in their attempt to generate alternative courses of action, as they lack educated knowledge about the virus and how to live with it. While further research is needed to clarify this supposed association between functional health literacy and reduced negative mental health outcomes in PLHIV who have formal/tertiary education background, perhaps, this finding also underscores a need to consider designing a functional health literacy program targeted at PLHIV without formal education who present to antiretroviral clinics in Ghana.
The strengths of this study include the use of a standardized measure to assess the prevalence estimates of depression, anxiety, and stress. The application of standardized measures strengthens a study's contributions to relatively valid estimates of outcomes. Also, the sample size used for this study was representative of the population of PLHIV presenting to the Cape Coast Teaching Hospital. However, this study had some limitations. The study was a cross‐sectional survey, therefore did not establish cause and effect relationship between associated factors and outcomes (depression, anxiety, and stress). Notably, this study failed to measure antiretroviral adherence/medical adherence, number of years lived with HIV/illness duration, and social adversities experienced due to HIV, while most of the included “exposure variables” were socio‐demographic factors which in themselves may not necessarily be modifiable (risk or protective) factors related to the outcomes. It is important to consider this point in designing related studies in the future, particularly, in Ghana and other sub‐Saharan contexts.
10. CONCLUSIONS
The levels of depression, anxiety, and stress are high among PLHIV in Ghana, and females report disproportionately higher levels. However, the effects of mental health problems among PLHIV are often underestimated, and this is more serious in a resource‐constrained country like Ghana and its sub‐Saharan context. The mental health care system in Ghana is grossly underfunded and provides little by way of screening and treatment for PLHIV. It is important for the managers of the healthcare system to integrate mental health assessment and management in the HIV care services. There is a need to build the capacity of health care workers to offer differentiated service delivery based on the mental health care needs of PLHIV. Primary care providers should be trained to provide mental health care services such as mental health assessment, counseling, and psychosocial support to PLHIV.
AUTHOR CONTRIBUTIONS
Sampson Opoku Agyemang: conceptualization, data curation, formal analysis, methodology, project administration, writing—original draft, writing—review & editing. Jerry Ninonni: conceptualization, data curation, methodology, project administration, supervision, writing—original draft, writing—review & editing. Lydia Bennin: conceptualization, data curation, methodology, project administration, writing—review & editing. Elizabeth Agyare: data curation, project administration, writing—review & editing. Leveana Gyimah: project administration, writing—review & editing. Kafui Senya: project administration, writing—review & editing. Emmanuel Birikorang: formal analysis, methodology, writing—review & editing. Emmanuel Nii‐Boye Quarshie: formal analysis, methodology; supervision, writing—original draft, writing—review & editing. Nyonuku Akosua Baddoo: methodology, project administration, supervision, writing—review & editing. Stephen Ayisi Addo: conceptualization, project administration, writing—review & editing. Dorcas Obiri‐Yeboah: conceptualization, formal analysis, methodology, project administration, supervision, writing—original draft, writing—review & editing. All authors have read and approved the final version of the manuscript. Corresponding author had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
This study was performed in accordance with the Helsinki Declaration and approved by the Ethics Review Committee of Cape Coast Teaching Hospital, Ghana (reference: CCTHERC/EC/2021/028). The purpose of the study, anonymity, voluntary participation, and confidentiality of the information were explained to participants to seek their written consent. Participants could withdraw from the study at any point without any adverse effect.
TRANSPARENCY STATEMENT
Sampson Opoku Agyemang affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted.
ACKNOWLEDGMENTS
We wish to thank all those who helped in the recruitment and data collection. We acknowledge all PLHIV who participated in this study. Our sincere thanks go to the staff of antiretroviral therapy clinic, Cape Coast Teaching Hospital for their assistance during the study. We thank the World Health Organisation Ghana country office for the financial support for this project. The funder was not involved in the development of the proposal, collection, and interpretation of data nor the project implementation.
Opoku Agyemang S, Ninonni J, Bennin L, et al. Prevalence and associations of depression, anxiety, and stress among people living with HIV: a hospital‐based analytical cross‐sectional study. Health Sci Rep. 2022;5:e754. 10.1002/hsr2.754
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article. However, the data are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Remien RH, Stirratt MJ, Nguyen N, Robbins RN, Pala AN, Mellins CA. Mental health and HIV/AIDS: the need for an integrated response. AIDS. 2019;33(9):1411‐1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ghana AIDS Commission . Ghana's HIV Fact Sheet. Off Pres Ghana. 2019;523:1‐6. [Google Scholar]
- 3. Deshmukh N, Borkar A, Deshmukh J. Depression and its associated factors among people living with HIV/AIDS: can it affect their quality of life? J Fam Med Prim Care. 2017;6(3):549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Duko B, Toma A, Asnake S, Abraham Y. Depression, anxiety and their correlates among patients with HIV in South Ethiopia: an institution‐based cross‐sectional study. Front Psychiatry. 2019;10:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McGrath JW, Winchester MS, Kaawa‐Mafigiri D, et al. Challenging the paradigm: anthropological perspectives on HIV as a chronic disease. Med Anthropol. 2014;33(4):303‐317. 10.1080/01459740.2014.892483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mahungu TW, Rodger AJ, Johnson MA. HIV as a chronic disease. Clin Med J R Coll Physicians London. 2009;9(2):125‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Green G, Smith R. The psychosocial and health care needs of HIV‐positive people in the United Kingdom: a review. HIV Med. 2004;5(suppl 1):4‐46. [DOI] [PubMed] [Google Scholar]
- 8. Collins PY, Holman AR, Freeman MC, Patel V. What is the relevance of mental health to HIV/AIDS care and treatment programs in developing countries? A systematic review. AIDS. 2006;20(12):1571‐1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bing EG, Burnam MA, Longshore D, et al. Psychiatric disorders and drug use among human immunodeficiency virus‐infected adults in the United States. Arch Gen Psychiatry. 2001;58(8):721‐728. [DOI] [PubMed] [Google Scholar]
- 10. Bhana A, Abas MA, Kelly J, van Pinxteren M, Mudekunye LA, Pantelic M. Mental health interventions for adolescents living with HIV or affected by HIV in low‐ and middle‐income countries: systematic review. BJPsych Open. 2020;6(5):1‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. WHO . The Sustainable Development Goals Report. 2020;4–5.
- 12. Miller RL, Brewer JD. The A‐Z of Social Research—A Dictionary of Key Social Science Research Concepts. Sage; 2003. [Google Scholar]
- 13. Bryman A. Why do researchers integrate/combine/mesh/blend/mix/merge/fuse quantitative and qualitative research. In: Manfred MB, ed. Advances in Mixed Methods Research. Sage; 2008:87‐100. [Google Scholar]
- 14. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335‐343. [DOI] [PubMed] [Google Scholar]
- 15. Henry JD, Crawford JR. The short‐form version of the Depression Anxiety Stress Scales (DASS‐21): construct validity and normative data in a large non‐clinical sample. Br J Clin Psychol. 2005;44(2):227‐239. [DOI] [PubMed] [Google Scholar]
- 16. Babyak MA. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression‐type models. Psychosom Med. 2004;66(3):411‐421. http://www.psychosomaticmedicine.org/cgi/doi/10.1097/01.psy.0000127692.23278.a9 [DOI] [PubMed] [Google Scholar]
- 17. McGowan JA, Brown J, Lampe FC, Lipman M, Smith C, Rodger A. Resilience and physical and mental well‐being in adults with and without HIV. AIDS Behav. 2018;22(5):1688‐1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lu HF, Hsiao FH, Sheng WH, et al. Prevalence and predictors of depression among people living with HIV/AIDS. Nurs Res. 2018;67(5):379‐386. [DOI] [PubMed] [Google Scholar]
- 19. Rai P, Verma BL. A study on depression in people living with HIV/AIDS in South‐West part of Uttar Pradesh, India. South East Asia J Public Heal. 2015;5(1):12‐17. [Google Scholar]
- 20. Chipanta D, Stöckl H, Toska E, et al. Facing the quality of life: physical illness, anxiety, and depression symptoms among people living with HIV in rural Zambia—a cross‐sectional study. AIDS Care—Psychol Socio‐Medical Asp AIDS/HIV. 2021;12:1‐9. 10.1080/09540121.2021.1966693 [DOI] [PubMed] [Google Scholar]
- 21. Yousuf A, Musa R, Isa MLM, Arifin SRM. Anxiety and depression among women living with HIV: prevalence and correlations. Clin Pract Epidemiol Ment Heal. 2020;16(1):59‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Saadat M, Behboodi Z, Saadat E. Comparison of depression, anxiety, stress, and related factors among women and men with human immunodefi ciency virus infection. J Hum Reprod Sci. 2015;8(1):48‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tran BX, Ho RCM, Ho CSH, et al. Depression among patients with HIV/AIDS: research development and effective interventions (gapresearch). Int J Environ Res Public Health. 2019;16(10):1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mekonen T, Belete H, Fekadu W. Depressive symptoms among people with HIV/AIDS in Northwest Ethiopia: comparative study. BMJ Open. 2021;11(7):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Abadiga M. Depression and its associated factors among HIV/AIDS patients attending ART clinics at Gimbi General hospital, West Ethiopia, 2018. BMC Res Notes. 2019;12(1):1‐8. 10.1186/s13104-019-4553-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Amare T, Getinet W, Shumet S, Asrat B. Prevalence and associated factors of depression among PLHIV in Ethiopia: systematic review and meta‐analysis, 2017. AIDS Res Treat. 2018;2018:5462959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Williams K, Frech A, Carlson DL. A handbook for the study of mental health. In: Scheid TL, Brown TN, eds. A Handbook for the Study of Mental Health. 2nd ed. Cambridge Unversity Press; 2012:306‐320. [Google Scholar]
- 28. Folayan MO, Cáceres CF, Sam‐Agudu NA, Odetoyinbo M, Stockman JK, Harrison A. Psychological stressors and coping strategies used by adolescents living with and not living with Hiv infection in Nigeria. AIDS Behav. 2017; 21(9):2736‐2745. http://link.springer.com/10.1007/s10461-016-1534-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wardell JD, Shuper PA, Rourke SB, Hendershot CS. Stigma, coping, and alcohol use severity among people living with HIV: a prospective analysis of bidirectional and mediated associations. Ann Behav Med. 2018; 52(9):762‐772. https://academic.oup.com/abm/article/52/9/762/4822985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Brown JL, DeMartini KS, Sales JM, Swartzendruber AL, DiClemente RJ. Interventions to reduce alcohol use among HIV‐infected individuals: a review and critique of the literature. Curr HIV/AIDS Rep. 2013;10(4):356‐370. http://link.springer.com/10.1007/s11904-013-0174-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Barnett E, de Koning K, Francis V. Health & HIV/AIDS education in primary & secondary schools in Africa & Asia Education Research Paper No. 14; 1995:94.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article. However, the data are available from the corresponding author upon reasonable request.


