Abstract
Background:
The Center for Disease Control and Prevention (CDC) reports that liver disease is a significant cause of morbidity and mortality in the US, afflicting 4.5 million people in 2018, or approximately 1.7% of the American adult population.
Objective:
To determine the prevalence and risk factors associated with liver disease among older Mexican Americans over 18 years of follow-up.
Methods:
Non-institutionalized Mexican Americans aged ≥67 years (N = 1938) from the Hispanic Established Population for the Epidemiologic Study of the Elderly (1995/96-2012/13) were studied. Measures included socio-demographic variables, self-reported liver disease, language of interview, medical conditions, hand-grip strength, physical and cognitive function, depressive symptoms, and body mass index. Generalized estimating equation models were used to estimate the odds ratio and 95% confidence interval (CI) of liver disease over time.
Results:
The mean age at baseline was 74.9 ± 6.0 years and 58.4% were female. The prevalence of liver disease ranged from 2.4% to 8.4%. Over time, the odds ratio of reporting liver disease was 1.17 (CI = 1.12-1.22). Older age, Spanish interview, arthritis, diabetes, heart failure, cancer, and high scores on the Mini-Mental-State-Examination were factors associated with greater odds of reporting liver disease over time. Married participants reported lower odds of liver disease over time.
Conclusions:
The prevalence of liver disease in this population was high, ranging from 2.4% to 8.4%. Diabetes, heart failure, arthritis, and cancer were risk factors for liver disease. Screening for liver function among patients with these morbidities may help prevent liver disease in this population with high rates of diabetes and obesity.
Keywords: liver disease, non-alcoholic fatty liver disease, Mexican Americans, geriatrics, hepatology, language barriers
Introduction
The Centers for Disease Control and Prevention (CDC) has found that liver disease is a major cause of morbidity and mortality in the US, affecting 4.5 million people in 2018, or about 1.7% of the adult American population. 1 Chronic liver disease comprises of a variety of conditions, including but not limited to fatty liver, steatohepatitis, and cirrhosis. In 2020, 51 642 deaths were reported as a consequence of liver disease, most often due to liver failure and gastrointestinal bleeds.1,2 Mortality from liver disease has progressively increased across all age groups in the US.3 -5 However, the death rate is highest among older adults, with an age-adjusted mortality per 10 000 persons approaching 30 and above for adults ages 65 and older. 6 About 80% of patients on the transplant waitlist from 2004 to 2013 suffered from either hepatitis C virus (HCV), alcoholic liver disease, or nonalcoholic fatty liver disease (NAFLD). 7 The epidemiology of liver disease has changed in recent decades in the US, with NAFLD surpassing HCV and alcoholic liver disease as the leading cause. 8
Several studies of prospective cohorts have found substantial disparities in the prevalence of liver disease between various US ethnic groups.8 -11 At 6.7%, Hispanic Americans have the highest prevalence of liver disease in the US, after Japanese Americans. 8 Hispanics also have a higher incidence of liver disease, in addition to worse outcomes relative to the general US population. 12 NAFLD, the leading cause of liver disease in America, appears to disproportionately affect Hispanic Americans, possibly due to a propensity for visceral fat deposition.13,14 Among both the youth and adult population, Hispanic Americans are more likely to suffer from diabetes, metabolic syndrome, hyperlipidemia, which are known risk factors for NAFLD.15 -18 Additionally, Hispanic Americans have more limited access to healthcare compared to the general population, further contributing to the disparity. 19 The literature is clear in describing the strong association of liver disease with the Hispanic and Mexican American population. In the US, Mexican Americans make up the largest portion of the Hispanic population. 20
Development of liver disease with advanced age has been well established in the literature.21 -23 This occurs by several mechanisms, including decreases in blood flow, liver volume, metabolism, and detoxification that occur with increasing age.24,25 Also, insulin resistance increases with age, contributing in particular to the development of NAFLD in the elderly population. 26
Numerous risk factors for liver disease have been well documented. NAFLD is strongly associated with body fat content and associated factors, including high body mass index (BMI), high waist circumference, type 2 diabetes mellitus, metabolic syndrome, hypertriglyceridemia and polycystic ovarian syndrome, many of which conditions are also highly prevalent in the Mexican American population.14,27 NAFLD is thought to make up about 75% of cases of chronic liver disease, and 2% to 15% of cases of cirrhosis, with numbers anticipated to rise.28,29 As expected, alcohol consumption is the leading risk factor for alcoholic liver disease, the second most common etiology of liver disease.8,14 Intravenous drug use and unsafe sexual practices are associated with the development of HCV and hepatitis B virus (HBV), although in recent years the incidence of HBV has dropped significantly due to the wide availability of a vaccine.5,27 A systematic review found that socioeconomic factors such as lower education and income are linked to increased rates of obesity, intravenous drug use and alcohol consumption, all factors in the development of liver disease. 14 A study based on data from the Fourth National Health and Nutrition Examination Survey showed that men were also more likely than women to develop liver disease in the general population, regardless of etiology. 27
The literature currently documents the epidemiology of liver disease as it relates to race/ethnicity, sex, and a wide range of determinants.8 -11,27 Metabolic syndrome, insulin resistance, and restricted access to healthcare are some of the predisposing factors for liver disease in the general Hispanic American population.15,19 However, the prevalence and associated risk factors of liver disease have not been thoroughly investigated among older Mexican Americans. Given the increased prevalence of liver disease among Hispanics and the higher mortality among older adults due to liver disease, 5 it is necessary to further examine this expanding community in the American population. The purpose of this study was to determine the prevalence and factors associated with liver disease among elderly Mexican Americans over the span of 18 years.
Methods
Data for this study can be found in the Hispanic Established Population for the Epidemiologic Study of the Elderly (H-EPESE), an ongoing longitudinal study of Mexican Americans aged 65 years and older who are residents of Arizona, California, Colorado, New Mexico, and Texas. The sampling plan, cohort characteristics, and data for the H-EPESE can be found at the National Archive of Computerized Data on Aging. 30 The original H-EPESE sample consisted of 3050 participants interviewed in 1993/94 at baseline and followed-up every 2 or 3 years. Face-to-face interviews were conducted in the subjects’ preferred language (English or Spanish) to obtain the data by trained interviewers. 16
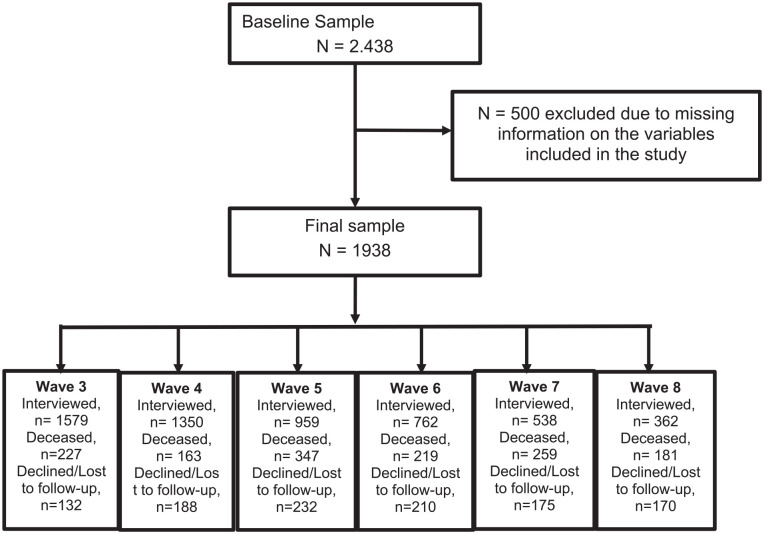
The current study used data obtained from wave 2 (1995-1996, hereafter baseline) to wave 8 (2012-2013). The first wave (1992-1993) was not included because the variable of self-reported liver disease was not collected, and therefore only those aged 67 years and older were examined in this study. The average follow-up period was 9.2 ± Standard Deviation (SD) of 4.9 years. We excluded participants with missing information (N = 500) on socio-demographics, alcohol consumption, comorbidities (hypertension, heart failure, diabetes, heart attack, stroke, or cancer), body mass index (BMI), depressive symptoms, cognitive and physical function, and handgrip strength. The final sample included 1938 subjects. Compared to the included sample, excluded subjects tended to be US-born, unmarried, with fewer years of education. They were also less likely to consume alcohol in the last month; to report stroke, depressive symptoms, heart attack, heart failure or cancer; and to have a lower BMI and score low on the Mini-Mental-State-Examination (MMSE) and the Short Physical Performance Battery (SPPB). At the end of follow-up, 266 participants were re-interviewed in person, while 170 participants declined interviews or were lost to follow-up, and 1406 participants were confirmed dead through the National Death Index or reports from relatives at the end of follow-up (Figure 1).
Figure 1.
Flow chart of sample.
Self-reported liver disease was assessed by asking each subject the following question: “Has a doctor or other health care professional ever told you that you had liver disease” (Yes or No). The type of liver disease was not specified in the survey.
Sociodemographic data included sex, age, years of education, marital status, and country of birth. Alcohol consumption was assessed with the question: “In the past month, have you had any beer, wine or liquor” (Yes or No). Pertinent medical history included self-reported hypertension, heart failure, diabetes, heart attack, stroke, and cancer. BMI was derived from the subjects’ weight in kilograms and height in meters squared (kg/m2). Criteria for obesity was a BMI ≥ 30 kg/m2. 31 The Center for Epidemiologic Studies Depression Scale (CES-D ≥ 16) was used to determine high depressive symptoms. 32 Cognitive function was determined by the MMSE. 33 Physical function was evaluated with the Short Physical Performance Battery (SPPB) to test balance, repeated chair-stands, and walking speed.34 -36 A dynamometer was used to measure handgrip strength of the dominant hand. 37
T-tests and chi-square were used to determine the distribution of sociodemographic variables and health characteristics of participants by liver disease at baseline. The 95% Confidence interval (CI) and odds ratio (OR) of risk factors for liver disease were estimated with generalized estimating equation (GEE) models using the GENMOD procedure in SAS. Repeated measure of participants was accounted for using a logit link binomial distribution and autoregressive correlation. Aside from sex, education, and nativity, all variables included in the study were analyzed as time varying. Those participants who died, refused to participate, or were lost to follow-up were included until their last interview date over the 18 years of follow-up. Additional analyses were conducted among those who survived the 18-years of follow-up, among those who did not survive, and without excluding those with self-reported liver disease at baseline. All analyses were performed using SAS for Windows (SAS Institute, Inc., Cary, NC). A significance level of .05 was used.
Results
Table 1 presents the baseline descriptive characteristics of the overall sample and by liver disease. The mean age was 74.9 ± 5.9 years, 58.4% were female, 54.6% were married, 56.4% were US born and the mean years of education was 4.9 ± 3.9 years. Mean BMI, MMSE and SPPB scores were 28.0 ± 5.2, 24.0 ± 4.5 and 8.2 ± 3.0, respectively. The mean handgrip strength was 30.7 ± 7.7 kg in men and 19.5 ± 5.6 kg in women. The most common comorbidities were hypertension (45.9%), arthritis (44.5%), and diabetes (27.2%). Twelve percent had major depressive symptoms. Participants with liver disease were significantly more likely to be younger; report arthritis (63.8%), diabetes (44.7%), heart failure (21.3%), or depressive symptoms (27.7%); and score lower in the SPPB and in handgrip strength (in women). The percent of those with liver disease increased from 2.4 at baseline to 8.4 in wave 8 (Figure 2).
Table 1.
Baseline Descriptive Characteristics of the Sample by Self-Reported Liver Disease (N = 1938).
| Variables | Overall N (%) | Liver disease N (%) | No liver disease N (%) | P-value |
|---|---|---|---|---|
| Total | 1938 | 47 (2.4) | 1891 (97.6) | |
| Age (years), mean ±SD | 74.9 ± 5.9 | 73.5 ± 4.4 | 74.9 ± 6.0 | .0381 |
| Gender | ||||
| Female | 1132 (58.4) | 33 (70.2) | 1099 (58.1) | .0965 |
| Male | 806 (41.6) | 14 (29.8) | 792 (41.9) | |
| Marital status (married) | 1058 (54.6) | 25 (53.2) | 1033 (54.6) | .8452 |
| Education (years), mean ±SD | 4.9 ± 3.9 | 5.2 ± 4.1 | 4.9 ± 3.9 | .5771 |
| Language of Interview (Spanish) | 1563 (80.7) | 37 (78.7) | 1526 (80.7) | .7350 |
| Nativity | ||||
| Foreign-born | 845 (43.6) | 22 (46.8) | 823 (43.5) | .6536 |
| US-born | 1093 (56.4) | 25 (53.2) | 1068 (56.5) | .6536 |
| Alcohol consumption | 362 (18.7) | 7 (14.9) | 355 (18.8) | .5003 |
| Obesity (BMI ≥ 30 kg/m2) | 615 (31.7) | 14 (29.8) | 601 (31.8) | .7716 |
| Arthritis | 862 (44.5) | 30 (63.8) | 832 (44.0) | .0069 |
| Hypertension | 889 (45.9) | 23 (48.9) | 866 (45.8) | .6695 |
| Diabetes | 527 (27.2) | 21 (44.7) | 506 (26.8) | .0064 |
| Heart attack | 165 (8.5) | 5 (10.6) | 160 (8.5) | .5973 |
| Heart failure | 228 (11.8) | 10 (21.3) | 218 (11.5) | .0405 |
| Stroke | 137 (7.1) | 2 (4.3) | 135 (7.1) | .7700 |
| Cancer | 123 (6.4) | 6 (12.8) | 117 (6.2) | .0676 |
| MMSE, mean ± SD | 24.0 ± 4.5 | 24.3 ± 3.8 | 24.0 ± 4.5 | .7084 |
| BMI, mean ± SD | 28.0 ± 5.2 | 27.9 ± 5.9 | 28.0 ± 5.2 | .8824 |
| Depressive symptoms (CES-D ≥ 16) | 229 (11.8) | 13 (27.7) | 216 (11.4) | .0007 |
| SPPB, mean ± SD | 8.2 ± 3.0 | 6.9 ± 2.9 | 8.2 ± 3.0 | .0019 |
| Male Grip Strength (kg), mean ± SD | 30.7 ± 7.7 | 30.6 ± 7.2 | 30.7 ± 7.7 | .9508 |
| Female Grip Strength (kg), mean ± SD | 19.5 ± 5.6 | 17.9 ± 6.4 | 19.6 ± 5.5 | .0084 |
Abbreviations: BMI, Body Mass Index; CES-D, Center for Epidemiologic Studies Depression Scale; SPPB, Short Physical Performance Battery.
Figure 2.
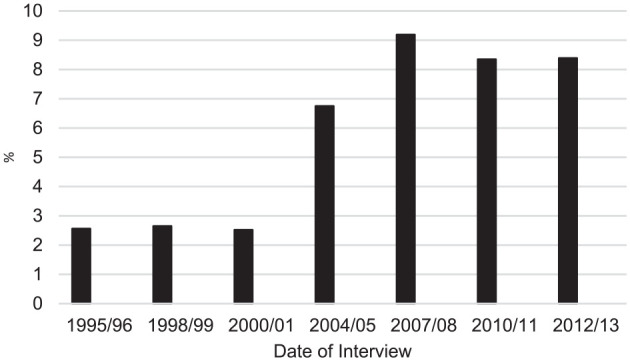
Percent of older Mexican American participants with liver disease over time (N = 1938).
Table 2 shows the results of the GEE model for self-reported liver disease as a function of sociodemographic, behavioral and health characteristics among older Mexican Americans without self-reported liver disease at baseline. Over time, there was a greater likelihood of reporting liver disease (OR = 1.17,95% CI = 1.12-1.22). Older age (OR = 1.06,95% CI = 1.00-1.22), having the interview conducted in Spanish (OR = 2.87,95% CI = 1.11-7.47), presence of arthritis (OR = 2.12,95% CI = 1.32-3.40), diabetes (OR = 1.64,95% CI=1.05-2.58), heart failure (OR = 2.70,95% CI = 1.58-4.26) or cancer (OR = 2.03,95% CI=1.10-3.76) and high cognitive function (OR = 1.10, CI = 1.05-1.17) were factors associated with greater odds of reporting liver disease over time. Married participants (OR = 0.61,95% CI = 0.38-0.98) and those with a high level of education (OR = 0.93,95% CI = 0.86-1.00) had lower odds of reporting liver disease over time. When the analyses were conducted among only the survivors and among the deceased, the findings were similar. When those participants with self-reported liver disease at baseline were included in the analyses, we found that cancer was associated with self-reported liver disease (OR = 1.99,95% CI = 1.26-3.16).
Table 2.
Generalized Estimating Equation Models for Self-Reported Liver Disease Over Time Among Older Mexican Americans Without Self-Reported Liver Disease at Baseline (N = 1891).
| Predictor variables | OR 95% CI | P-value |
|---|---|---|
| Time (years) | 1.17 (1.12-1.22) | <.0001 |
| Age (years) | 1.06 (1.00-1.11) | .0469 |
| Sex (female) | 1.11 (0.60-2.02) | .7551 |
| Marital status (married) | 0.61 (0.38-0.98) | .0422 |
| Education (years) | 0.93 (0.86-1.00) | .0638 |
| Interviewed in Spanish | 2.87 (1.11-7.47) | .0303 |
| Nativity (US-born) | 0.98 (0.61-1.58) | .9438 |
| Alcohol consumption | 0.92 (0.48-1.76) | .8051 |
| Obesity (BMI ≥ 30 kg/m2) | 1.25 (0.80-1.96) | .3227 |
| Arthritis | 2.12 (1.32-3.40) | .0018 |
| Hypertension | 0.76 (0.45-1.26) | .2800 |
| Diabetes | 1.64 (1.05-2.58) | .0299 |
| Heart attack | 0.69 (0.31-1.54) | .3687 |
| Heart failure | 2.70 (1.71-4.26) | <.0001 |
| Stroke | 1.30 (0.61-2.77) | .4882 |
| Cancer | 2.03 (1.10-3.76) | .0237 |
| MMSE | 1.10 (1.05-1.17) | .0004 |
| Depressive symptoms (CES-D ≥ 16) | 1.00 (0.88-1.72) | .9972 |
| SPPB | 1.05 (0.98-1.05) | .1170 |
| Grip strength | 1.02 (0.98-1.05) | .3613 |
Abbreviations: BMI, Body Mass Index; CES-D, Center for Epidemiologic Studies Depression Scale; MMSE, Mini-Mental-State-Examination; SPPB, Short Physical Performance Battery.
Discussion
The purpose of our study was to determine the prevalence and factors associated with self-reported liver disease among Mexican Americans aged 67 years and older over the span of 18 years. The prevalence of self-reported liver disease ranged from 2.4% to 8.4%. Age, language of interview (Spanish), arthritis, diabetes, heart failure, cancer and high MMSE scores were factors associated with greater odds of self-reported liver disease over time. Married participants and those with high level of education were at a decreased risk of self-reported liver disease over time.
Liver disease prevalence in our sample at baseline was 2.4%, above the national average of 1.7% in the adult American population. 1 This finding is consistent with other literature reporting that liver disease disproportionately affects Mexican Americans, suggesting that the association exists even as this population ages. 8
Heart failure, diabetes and arthritis were clear risk factors for liver disease in this population. The relationship between these medical conditions and liver disease has been previously established.38 -40 Heart failure can passively congest the liver or cause hepatic necrosis via hypoperfusion.38,39 Type 2 diabetes is strongly associated with obesity and the development of NAFLD, which can progress to steatohepatitis and cirrhosis. 40 The exact mechanism by which this occurs is complex and not fully understood, but the literature suggests that liver fat deposition is a result of insulin resistance and excessive lipid availability.41,42 Several studies have shown that the deposition of fat in the liver interferes in multiple cellular pathways, resulting in inhibited hepatic regeneration through higher p21 expression, increased γ-H2AX expression with telomere shortening, and decreased autophagy.43,44 A cross-sectional study found that both a personal and family history of diabetes were significantly associated with nonalcoholic steatohepatitis. 45 Arthritis can contribute to liver disease as a side effect of pharmacotherapy such as methotrexate and nonsteroidal anti-inflammatory drugs or as an association with associated autoimmune disorders such as autoimmune hepatitis, primary sclerosing cholangitis and primary biliary cirrhosis. 46
More years of education appeared to be a protective factor for liver disease. This result is corroborated by studies showing that less education, which is more common among Mexican Americans, correlates with higher rates of HBV, HCV and alcohol use, all of which contribute to liver disease. 27 The increased likelihood of liver disease among those interviewed in Spanish was particularly interesting. This finding has not been reported in the literature regarding Mexican Americans and liver disease, however it is to be expected and further exemplifies how limited English proficiency is a barrier to healthcare access.34 -36 Given the ever-growing prevalence of Spanish speakers in the US, special attention should be given to Mexican Americans with limited English proficiency in order to screen for liver disease and mitigate the effect of associated risk factors.
Our finding also showed that better mental status was associated with a greater likelihood of liver disease. This contrasted with numerous established studies which strongly correlate liver disease with worsening cognition.47 -49 There are several possible explanations for this. Participants with lower cognitive function may have been less likely to visit the doctor to receive the diagnosis of liver disease and report it to the survey. There is also the possibility of a survivorship bias; fewer individuals with severe liver disease would live to be aged 67 years and older, and therefore, the surviving participants would likely have a milder form of the disease, with more preserved cognitive function. Although our study did not demonstrate handgrip strength as a factor associated with liver disease, this hypothesis is consistent with studies on handgrip strength that show it to be a strong predictor of mortality in the Mexican American population. 37 This finding further supports the notion that the participants were not suffering from severe liver disease, but rather a milder form.
Our study has a few limitations. First, the data was self-reported, calling to question the reliability of the participants’ answers. Second, the absence of medical charts, imaging or laboratory tests limited the specifics of each participants’ particular liver disease diagnosis. These 2 limitations present possible issues with validity, however, we suspect patients would be more likely to under report rather than over report a diagnosis of liver disease given the limited healthcare access and literacy in this population. Third, information was not collected on disease duration, severity, or management. Fourth, we excluded less healthy participants, which could have underestimated the association with liver disease of sociodemographic, behavioral and health characteristics. Fifth, data on alcohol use was limited; alcohol history was assessed by alcohol use in the past month, which does not delineate between excessive and acceptable amounts of consumption. Sixth, our study focuses on associations and risk factors for liver disease from a statistical perspective but does not provide new insight into pathophysiology and diagnosis of liver disease. Finally, our findings are generalizable only to Mexican Americans living in the Southwest region of the US. 50 Nonetheless, a major strength of our study is its evaluation of the factors contributing to and protective of liver disease over time in the older Mexican American population. To date, no study has closely examined this condition in this ever-growing portion of the US population. The study draws strength from its large sample size representative of the Mexican American population and its prospective design.
Conclusion
The current literature shows that the Mexican American population is disproportionately affected by liver disease. This study confirms that this trend continues among the elderly Mexican American population as well. Our findings suggest that arthritis, heart failure, cancer, diabetes, and interviewing in Spanish increase the risk of developing liver disease; however, more years of education and being married appear to be protective factors. This study provides much needed insight into the aging Mexican American population with respect to liver disease. More research is needed to further understand the etiology of this disease, as well as methods to improve the resultant morbidity and mortality in this population.
Acknowledgments
The authors acknowledge the assistance of Sarah Toombs Smith, PhD, ELS, Sealy Center on Aging, in article preparation. Dr. Toombs Smith received no compensation for this effort beyond her university salary.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute on Aging, the National Institute on Minority Health and Health Disparities, Texas Resource Center on Minority Aging Research, and the UTMB Claude Pepper Center (R01 AG10939, R01 AG017638, R01 MD010355, 1P30 AG059301-01, P30-AG024832, and P30AG059301).
ORCID iDs: Ronan P. Allencherril  https://orcid.org/0000-0002-1266-9102
https://orcid.org/0000-0002-1266-9102
Soham Al Snih  https://orcid.org/0000-0002-0681-4641
https://orcid.org/0000-0002-0681-4641
References
- 1. Centers for Disease Control and Prevention. National Center for Health Statistics; 2019. Accessed December 9, 2021. https://www.cdc.gov/nchs/fastats/liver-disease.htm [Google Scholar]
- 2. Schlichting P, Christensen E, Fauerholdt L, Poulsen H, Juhl E, Tygstrup N. Main causes of death in cirrhosis. Scand J Gastroenterol. 1983;18(7):881-888. doi: 10.3109/00365528309182110 [DOI] [PubMed] [Google Scholar]
- 3. Kim D, Adejumo AC, Yoo ER, et al. Trends in mortality from extrahepatic complications in patients with chronic liver disease, from 2007 through 2017. Gastroenterology. 2019;157(4):1055-1066.e11 doi: 10.1053/j.gastro.2019.06.026 [DOI] [PubMed] [Google Scholar]
- 4. Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: Observational study. BMJ. 2018;362:k2817. doi: 10.1136/bmj.k2817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. QuickStats: death rates for chronic liver disease and cirrhosis, by sex and age group—National Vital Statistics System, United States, 2000 and 2015. MMWR Morb Mortal Wkly Rep. 2017;66:1031. www.cdc.gov/mmwr/volumes/66/wr/mm6638a9.htm [DOI] [PubMed] [Google Scholar]
- 6. Kim D, Bonham CA, Konyn P, Cholankeril G, Ahmed A. Mortality trends in chronic liver disease and cirrhosis in the United States, before and during COVID-19 pandemic. Clin Gastroenterol Hepatol. 2021;19(12):2664-2666.e2 doi: 10.1016/j.cgh.2021.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547-555. doi: 10.1053/j.gastro.2014.11.039 [DOI] [PubMed] [Google Scholar]
- 8. Setiawan VW, Stram DO, Porcel J, Lu SC, Le Marchand L, Noureddin M. Prevalence of chronic liver disease and cirrhosis by underlying cause in understudied ethnic groups: the multiethnic cohort. Hepatology. 2016;64(6):1969-1977. doi: 10.1002/hep.28677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rich NE, Oji S, Mufti AR, et al. Racial and ethnic disparities in nonalcoholic fatty liver disease prevalence, severity, and outcomes in the United States: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2018;16(2):198-210.e2. doi: 10.1016/j.cgh.2017.09.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McPherson S, Anstee QM. Changing epidemiology of chronic liver disease among ethnic groups in the United States. Hepatology. 2016;64(6):1843-1846. doi: 10.1002/hep.28783 [DOI] [PubMed] [Google Scholar]
- 11. Williams CD, Stengel J, Asike MI, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140(1):124-131. doi: 10.1053/j.gastro.2010.09.038 [DOI] [PubMed] [Google Scholar]
- 12. Carrion AF, Ghanta R, Carrasquillo O, Martin P. Chronic liver disease in the Hispanic population of the United States. Clin Gastroenterol Hepatol. 2011;9(10):834-841. quiz e109-10. doi: 10.1016/j.cgh.2011.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Weston SR, Leyden W, Murphy R, et al. Racial and ethnic distribution of nonalcoholic fatty liver in persons with newly diagnosed chronic liver disease. Hepatology. 2005;41(2):372-379. doi: 10.1002/hep.20554 [DOI] [PubMed] [Google Scholar]
- 14. Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34(3):274-285. doi: 10.1111/j.1365-2036.2011.04724.x [DOI] [PubMed] [Google Scholar]
- 15. Heiss G, Snyder ML, Teng Y, et al. Prevalence of metabolic syndrome among Hispanics/Latinos of diverse background: the Hispanic Community Health Study/Study of Latinos. Diabetes Care. 2014;37(8):2391-2399. doi: 10.2337/dc13-2505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Reina SA, Llabre MM, Vidot DC, et al. Metabolic syndrome in Hispanic youth: Results from the Hispanic Community Children’s Health Study/study of Latino Youth. Metab Syndr Relat Disord. 2017;15(8):400-406. doi: 10.1089/met.2017.0054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tortolero SR, Goff DC, Jr, Nichaman MZ, Labarthe DR, Grunbaum JA, Hanis CL. Cardiovascular risk factors in Mexican-American and Non-Hispanic white children: the Corpus Christi Child Heart Study. Circulation. 1997;96(2):418-423. doi: 10.1161/01.CIR.96.2.418 [DOI] [PubMed] [Google Scholar]
- 18. Haffner SM, D’Agostino R, Saad MF, et al. Increased insulin resistance and insulin secretion in nondiabetic African-Americans and Hispanics compared with non-Hispanic whites: the insulin resistance atherosclerosis study. Diabetes. 1996;45(6):742-748. [DOI] [PubMed] [Google Scholar]
- 19. Pérez-Escamilla R, Garcia J, Song D. Health care access among Hispanic immigrants: ¿Alguien está Escuchando? [Is Anybody Listening?]. NAPA Bull. 2010;34(1):47-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lopez G. Hispanics of Mexican Origin in the United States, 2013. Pew Research Center’s Hispanic Trend Project; 2015. [Google Scholar]
- 21. Kim IH, Kisseleva T, Brenner DA. Aging and liver disease. Curr Opin Gastroenterol. 2015;31(3):184-191. doi: 10.1097/MOG.0000000000000176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kamimura K, Sakamaki A, Kamimura H, et al. Considerations of elderly factors to manage the complication of liver cirrhosis in elderly patients. World J Gastroenterol. 2019;25(15):1817-1827. doi: 10.3748/wjg.v25.i15.1817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ghavimi S, Azimi H, Patel N, Shulik O. Geriatric hepatology: the hepatic diseases of the, elderly and liver transplant. J Dig Dis Hepatol. 2019;3:167. doi: 10.29011/2574-3511.000067 [DOI] [Google Scholar]
- 24. Li CH, Ge XL, Pan K, Wang PF, Su YN, Zhang AQ. Laser speckle contrast imaging and oxygen to see for assessing microcirculatory liver blood flow changes following different volumes of hepatectomy. Microvasc Res. 2017;110:14-23. doi: 10.1016/j.mvr.2016.11.004 [DOI] [PubMed] [Google Scholar]
- 25. Schmucker DL. Age-related changes in liver structure and function: Implications for disease ? Exp Gerontol. 2005;40(8-9):650-659. doi: 10.1016/j.exger.2005.06.009 [DOI] [PubMed] [Google Scholar]
- 26. Barzilai N, Huffman DM, Muzumdar RH, Bartke A. The critical role of metabolic pathways in aging. Diabetes. 2012;61(6):1315-1322. doi: 10.2337/db11-1300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Flores YN, Yee HF, Jr, Leng M, et al. Risk factors for chronic liver disease in blacks, Mexican Americans, and Whites in the United States: results from NHANES IV, 1999-2004. Am J Gastroenterol. 2008;103(9):2231-2238. doi: 10.1111/j.1572-0241.2008.02022.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Younossi ZM, Stepanova M, Afendy M, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol. 2011;9(6):524-530.e1. [DOI] [PubMed] [Google Scholar]
- 29. Li B, Zhang C, Zhan Y-T. Nonalcoholic fatty liver disease cirrhosis: a review of its epidemiology, risk factors, clinical presentation, diagnosis, management, and prognosis. Can J Gastroenterol Hepatol. 2018;2018:2784537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Markides KS, Chen N-W, Angel R, Palmer R. Data from: Hispanic Established Populations for the Epidemiologic Study of the Elderly (HEPESE) Wave 8, 2012-2013 [Arizona, California, Colorado, New Mexico, and Texas]. 2016. doi: 10.3886/ICPSR36578.v2 [DOI] [Google Scholar]
- 31. National Institute of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert panel on the identification, evaluation, and treatment of overweight in adults. Am J Clin Nutr. 1998;68(4):899-917. doi: 10.1093/ajcn/68.4.899 [DOI] [PubMed] [Google Scholar]
- 32. Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Physiol Meas. 1977;1(3):385-401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- 33. Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-198. doi: 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- 34. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85-M94. [DOI] [PubMed] [Google Scholar]
- 35. Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556-561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Freiberger E, de Vreede P, Schoene D, et al. Performance-based physical function in older community-dwelling persons: a systematic review of instruments. Age Ageing. 2012;41(6):712-721. doi: 10.1093/ageing/afs099 [DOI] [PubMed] [Google Scholar]
- 37. Al Snih S, Markides KS, Ray L, Ostir GV, Goodwin JS. Handgrip strength and mortality in older Mexican Americans. J Am Geriatr Soc. 2002;50(7):1250-1256. doi: 10.1046/j.1532-5415.2002.50312.x [DOI] [PubMed] [Google Scholar]
- 38. Giallourakis CC, Rosenberg PM, Friedman LS. The liver in heart failure. Clin Liver Dis. 2002;6(4):947-967. doi: 10.1016/s1089-3261(02)00056-9. [DOI] [PubMed] [Google Scholar]
- 39. Giallourakis CC. Liver complications in patients with congestive heart failure. Gastroenterol Hepatol. 2013;9(4):244-246. [PMC free article] [PubMed] [Google Scholar]
- 40. Tolman KG, Fonseca V, Dalpiaz A, Tan MH. Spectrum of liver disease in type 2 diabetes and management of patients with diabetes and liver disease. Diabetes Care. 2007;30(3):734-743. doi: 10.2337/dc06-1539 [DOI] [PubMed] [Google Scholar]
- 41. Tilg H, Moschen AR, Roden M. NAFLD and diabetes mellitus. Nat Rev Gastroenterol Hepatol. 2017;14(1):32-42. doi: 10.1038/nrgastro.2016.147 [DOI] [PubMed] [Google Scholar]
- 42. Tarantino G, Caputi A. JNKs, insulin resistance and inflammation: a possible link between NAFLD and coronary artery disease. World J Gastroenterol. 2011;17(33):3785-3794. doi: 10.3748/wjg.v17.i33.3785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Aravinthan A, Scarpini C, Tachtatzis P, et al. Hepatocyte senescence predicts progression in non-alcohol-related fatty liver disease. J Hepatol. 2013;58(3):549-556. [DOI] [PubMed] [Google Scholar]
- 44. Amir M, Czaja MJ. Autophagy in nonalcoholic steatohepatitis. Expert Rev Gastroenterol Hepatol. 2011;5(2):159-166. doi: 10.1586/egh.11.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Loomba R, Abraham M, Unalp A, et al. Association between diabetes, family history of diabetes, and risk of nonalcoholic steatohepatitis and fibrosis. Hepatology. 2012;56(3):943-951. doi: 10.1002/hep.25772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Selmi C, De Santis M, Gershwin ME. Liver involvement in subjects with rheumatic disease. Arthritis Res Ther. 2011;13(3):226. doi: 10.1186/ar3319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Orr JG, Homer T, Ternent L, et al. Health related quality of life in people with advanced chronic liver disease. J Hepatol. 2014;61(5):1158-1165. doi: 10.1016/j.jhep.2014.06.034 [DOI] [PubMed] [Google Scholar]
- 48. Bajaj JS, Wade JB, Sanyal AJ. Spectrum of neurocognitive impairment in cirrhosis: Implications for the assessment of hepatic encephalopathy. Hepatology. 2009;50(6):2014-2021. doi: 10.1002/hep.23216 [DOI] [PubMed] [Google Scholar]
- 49. Seo SW, Gottesman RF, Clark JM, et al. Nonalcoholic fatty liver disease is associated with cognitive function in adults. Neurology. 2016;86(12):1136-1142. doi: 10.1212/WNL.0000000000002498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. García C, Ailshire JA. Biological risk profiles among Latino subgroups in the health and retirement study. Innov Aging. 2019;3(2):igz017. doi: 10.1093/geroni/igz017 [DOI] [PMC free article] [PubMed] [Google Scholar]