Abstract
Background:
In the United States, the COVID-19 pandemic led to a nationwide quarantine that forced individuals to adjust their daily activities, potentially impacting the burden of foot and ankle disease. The purpose of this study was to compare diagnoses made in an orthopaedic foot and ankle clinic during the shelter-in-place period of the COVID-19 pandemic to diagnoses made during the same months of the previous year.
Methods:
A retrospective review of new patients presenting to the clinics of 4 fellowship-trained orthopaedic foot and ankle surgeons in a major United States city was performed. Patients in the COVID-19 group presented between March 22 and July 1, 2020, during the peak of the quarantine for this city. Patients in the control group presented during the same period of 2019. Final diagnosis, chronicity of symptoms (acute: ≤1 month), and mechanism of disease were compared between groups.
Results:
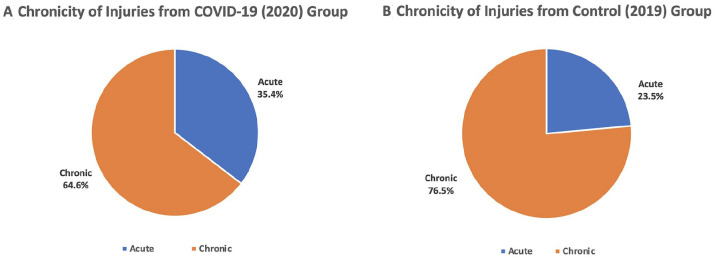
A total of 1409 new patient visits were reviewed with 449 visits in the COVID-19 group and 960 visits in the control group. The COVID-19 group had a significantly higher proportion of ankle fractures (8.7% vs 5.4%, P = .020) and stress fractures (4.2% vs 2.2%, P = .031), but a smaller proportion of Achilles tendon ruptures (0.7% vs 2.5%, P = .019). The COVID-19 group had a higher proportion of acute injuries (35.4% vs 23.5%, P < .001).
Conclusion:
There was a shift in prevalence of pathology seen in the foot and ankle clinic during the COVID-19 pandemic, which may reflect the adoption of different activities during the quarantine period and reluctance to present for evaluation of non-urgent injuries.
Level of Evidence:
Level III, retrospective cohort study.
Keywords: COVID-19, foot and ankle, orthopaedics, pandemic, quarantine
Introduction
The first case of coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS CoV-2), was confirmed in the United States on January 22, 2020. 8 The rapid spread of the virus and increasing number of deaths led to the World Health Organization declaring it a pandemic on March 11, 2020. 23 In an attempt to control the spread of the virus, many state and municipal governments enacted quarantine and social distancing protocols. Specifically, the city of Chicago declared a stay-at-home ordinance to begin on the evening of March 21, 2020. 15 As a result, businesses classified as nonessential were forced to shut down, including fitness centers and city parks. As businesses adjusted to the pandemic, employees were forced to work from home, placed on furlough, or ultimately let go from their jobs.
These restrictions resulted in a sudden change to the daily activities and exercise routines of individuals in the community. With limited access to fitness centers, organized sports, and public parks, there was a concern that the quarantine would result in decreased physical activity. Tison et al 21 found an overall decrease in activity levels across the world by analyzing daily step counts during COVID-19 compared to previous baselines. Other reports using web-based surveys demonstrated variable results, with a proportion of individuals decreasing their physical activity whereas others had a constant or overall increase in their exercise habits.3,10,16,19,22 Although the pandemic affected different individuals in different ways, there were certainly substantial changes in the activities performed on a daily basis for many Americans.
The daily routines of the orthopaedic surgery community also changed with the COVID-19 pandemic. Many states and institutions temporarily ceased elective surgeries, and the health care system utilized telemedicine to provide care when possible.6,11,17,18 However, treatment of orthopaedic injuries requiring emergent or urgent management continued to proceed. Analysis of patient presentations to an orthopaedic trauma service showed a change in mechanism of injuries and timing of presentation.12,14,20 Although these reports are useful to analyze the effects of the COVID-19 pandemic on emergent or urgent orthopaedic injuries and subsequent care, there is a lack of information regarding the impact of COVID-19 on patient presentations to other orthopaedic subspecialties in the outpatient setting.
The purpose of the present study was to compare diagnoses made following new patient evaluations at an orthopaedic foot and ankle clinic during the months of the COVID-19 pandemic to diagnoses made during the same months of the previous year. We hypothesized that there would be an increase in the proportion of patients presenting for overuse injuries and a decrease in the proportion of patients presenting for chronic injuries.
Methods
Patient Selection
The current study was approved by the institutional review board at the institution where the study took place, and no funding was received. Clinical records from a group of 4 fellowship-trained orthopaedic foot and ankle surgeons located in Chicago, Illinois, were retrospectively reviewed between March 22, 2020, and July 1, 2020, and the same dates in the previous year. March 22, 2020, represented the first full day of the stay-at-home order for Chicago, and the end of June represented the transition of restrictions to Phase IV reopening, known as “Gradual Reopening.” 2 Inclusion criteria were patients presenting with new complaints to an orthopaedic foot and ankle clinic within the study dates. Patients were excluded if they had no presenting complaint or if they had previously been seen by a member of our group for the presenting complaint. Patients presenting during the specified time period in the year 2020 were designated as the COVID-19 group, and those presenting during the previous year (2019) were designated as the control group. At our practice, nearly all (>90%) of patients presenting to clinic are under the primary care of an orthopaedic foot and ankle surgeon and not treated by an advanced practice provider (APP) alone. Thus, despite staffing changes during the pandemic resulting in the decreased availability of APPs, both study groups represent an accurate and complete picture of patients presenting to the clinic during the respective time periods. All clinics were open with limited hours during the shutdown period, though all patients who needed to be seen were accommodated.
Data Collection
Once a patient was deemed eligible for inclusion in the study, his or her clinical records were further reviewed and collected data was stored on a secure spreadsheet. Demographic data including age at the time of visit, gender, and body mass index (BMI) were recorded. Workers’ compensation status and primary insurance payor were collected. The diagnosis for the patient’s presenting complaint was characterized. The anatomic area (forefoot, midfoot, hindfoot, ankle, and proximal to ankle), symptom duration prior to presentation and whether the injury required operative intervention were identified. Diagnoses were classified as acute (symptom ≤1 month) or chronic (symptom duration >1 month). Diagnoses were further classified as fractures if the final diagnosis was identified as an ankle fracture, metatarsal fracture, phalanx fracture, calcaneus fracture, or other foot fracture. Diagnoses were classified as overuse conditions if the final diagnosis was identified as plantar fasciitis, a stress fracture, Achilles tendonitis, Achilles tendon rupture, peroneal tendon injury, shin splints, sesamoiditis, ankle sprains, or other tendonitis.
Statistical Analysis
Study data were analyzed using Stata 16.1 (Statacorp, College Station, TX). Descriptive statistics for all continuous variables are reported as the mean with ranges, and frequency statistics are reported for all noncontinuous variables. Two sample t tests were used to compare age and BMI between groups. Pearson χ2 tests were used to compare gender and worker’s compensation status between groups. Binomial probability tests with a probability of .5 were used to compare absolute numbers of presenting patients with specific diagnoses between groups. Pearson χ2 tests were used to compare proportions of patients presenting with specific diagnoses between groups. The level of significance was set at P <.05.
Results
A total of 1409 new patient visits were included, with 449 visits (31.9%) in the COVID-19 group and 960 visits (68.1%) in the control group. The mean age and BMI of the entire study cohort were 48.5 years (range 10-94) and 28.7 (range 16.0-61.3), respectively. The cohort was 61.6% female (868/1409), 3.1% (44/1409) had workers’ compensation status, and 18.0% (254/1409) had Medicare as their primary insurance. Comparisons of BMI, age, gender, and workers’ compensation status did not show any statistically significant differences between the COVID-19 and control groups (P > .05 for each).
The COVID-19 group had a 53.2% reduction in the absolute number of new patient visits over the time period studied compared with the previous year (P < .001).
Table 1 shows comparisons of the proportion of the most frequent diagnoses in the study and control groups. Fifty-nine patients (13.1%) in the COVID-19 group and 129 patients (13.3%) in the control group had various other diagnoses that were too infrequent to form a meaningful comparison, or no formal diagnosis was made during the visit. The COVID-19 group had significantly higher proportions of ankle fractures (8.7% vs 5.5%, P = .025) and stress fractures (4.2% vs 2.3%, P = .044), but a smaller proportion of Achilles tendon ruptures (0.7% vs 2.5%, P = .019). The COVID-19 group had a significantly higher proportion of acute injuries than the control group (35.4% vs 23.5%; P < .001) (Figure 1). There was a statistically significant increase in hindfoot diagnoses between the COVID-19 and control groups (14.7% vs 9.9%, P = .008). There were no statistically significant differences in diagnoses involving the forefoot, midfoot, ankle, or proximal to the ankle (P > .05). There was no difference in patients indicated for surgery between the COVID-19 and control groups (16.48% vs 16.35%, P = .952). There was no difference between diagnoses classified as fractures (16.0% in the COVID-19 group vs 12.4% in the control group, P = .063) or those classified as overuse conditions (32.7% in the COVID-19 group vs 33.9% in the control group, P = .680).
Table 1.
Comparison of Most Common Diagnoses During the COVID-19 Pandemic (2020, n = 449) and Control (2019, n = 960) Time Periods.
| Prevalence, n (%) | P Value | |
|---|---|---|
| Achilles tendon rupture | .019 | |
| 2020 | 3 (0.7) | |
| 2019 | 24 (2.5) | |
| Achilles tendonitis | .971 | |
| 2020 | 25 (5.6) | |
| 2019 | 53 (5.5) | |
| Ankle fracture | .020 | |
| 2020 | 39 (8.7) | |
| 2019 | 52 (5.4) | |
| Ankle sprain | .499 | |
| 2020 | 42 (9.4) | |
| 2019 | 101 (10.5) | |
| Arthritis | .143 | |
| 2020 | 54 (12.0) | |
| 2019 | 91 (9.5) | |
| Foot fractures | .853 | |
| 2020 | 26 (5.8) | |
| 2019 | 58 (6.0) | |
| Hallux rigidus | .445 | |
| 2020 | 23 (5.1) | |
| 2019 | 59 (6.2) | |
| Hallux valgus | .096 | |
| 2020 | 21 (4.7) | |
| 2019 | 67 (7.0) | |
| Metatarsalgia | .666 | |
| 2020 | 14 (3.2) | |
| 2019 | 26 (2.7) | |
| Neuropathy | .420 | |
| 2020 | 13 (2.9) | |
| 2019 | 21 (2.2) | |
| Other tendonitis | .224 | |
| 2020 | 17 (3.8) | |
| 2019 | 25 (2.6) | |
| Plantar fasciitis | .940 | |
| 2020 | 29 (6.5) | |
| 2019 | 61 (6.4) | |
| PTTI | .579 | |
| 2020 | 26 (5.8) | |
| 2019 | 63 (6.6) | |
| Stress fracture | .031 | |
| 2020 | 19 (4.2) | |
| 2019 | 21 (2.2) |
Abbreviation: PTTI, posterior tibial tendon insufficiency.
Bold indicates statistical significance (P < 0.05).
Figure 1.
The proportion of (A) new patients who presented with acute (duration <1 month) or chronic (duration >1 month) symptoms during the COVID-19 pandemic and (B) control group from the previous year. The COVID-19 group had a significantly higher proportion of acute injuries (35.4% vs 23.5%, P < .001).
Table 2 shows comparisons between each cohort when stratified by symptom chronicity within the fracture and overuse diagnosis subgroups (Table 2). The COVID-19 group had a higher proportion of acute overuse conditions (14.7% vs 10.8%, P = .038) and acute fractures (14.0% vs 8.4%, P = .001), but a lower proportion of chronic overuse conditions (23.0% vs 18.0%, P = .034). There was no difference in patient age between patients with acute vs chronic injuries (P = .673).
Table 2.
Comparison of Fractures and Overuse Diagnoses During COVID-19 (2020, n = 449) and Control (2019, n = 960) Time Periods.
| Prevalence, n (%) | P Value | |
|---|---|---|
| Fracture a | .055 | |
| 2020 | 72 (16.0) | |
| 2019 | 118 (12.3) | |
| Fracture—acute | .001 | |
| 2020 | 63 (14.0) | |
| 2019 | 81 (8.4) | |
| Fracture—chronic | .069 | |
| 2020 | 9 (2.0) | |
| 2019 | 37 (3.9) | |
| Overuse b | .652 | |
| 2020 | 173 (38.5) | |
| 2019 | 382 (39.8) | |
| Overuse—acute | .023 | |
| 2020 | 72 (16.0) | |
| 2019 | 112 (11.7) | |
| Overuse—chronic | .025 | |
| 2020 | 101 (22.5) | |
| 2019 | 270 (28.1) |
Fracture: diagnoses including ankle fractures, metatarsal fracture, phalanx fractures, calcaneal fractures, and other fractures.
Activity related: diagnoses including plantar fasciitis, stress fractures, achilles tendonitis, achilles tendon rupture, posterior tibial tendon insufficiency, peroneal tendon injury, shin splints, sesamoiditis, ankle sprain, and other tendonitis.
Bold indicates statistical significance (P < 0.05).
Discussion
In this investigation, we show a significant change in the prevalence of pathology presenting to an orthopaedic foot and ankle outpatient clinic during the COVID-19 pandemic. When compared to the same time period of the previous year, a greater proportion of patients presented with specific diagnoses including ankle fractures and stress fractures during the pandemic, but a lower proportion of patients presented with Achilles tendon ruptures. No differences were seen in other diagnoses made between these 2 time periods. In addition, a greater proportion of patients presented with acute symptoms during the COVID-19 pandemic. Furthermore, during the pandemic, there was a higher proportion of patients presenting with acute overuse injuries and acute fractures, and fewer with chronic overuse injuries. These results supported our hypothesis.
A possible explanation for the results observed in the present study is a change in patient behavior and willingness to present to a health care system during the stay-at-home order. The lower proportion of chronic complaints may indicate that patients were reluctant to present to clinic with nonurgent injuries secondary to a fear of exposure to COVID-19. It is also possible that these patients preferred to seek care over telemedicine, which was introduced gradually to our practice beginning shortly after the shelter-in-place mandate was issued. Moverman et al 13 reported that a majority of patients presenting for elective surgery during the pandemic had concerns of contracting the virus or risk of transmission to a family member because of difficulty with social distancing during the check-in process or in waiting rooms and excessive exposure to medical staff.
Furthermore, in a metropolitan area, patients may rely on public transportation or ride-share services that would increase their exposure of contracting the virus, thus acting as a deterrent for presentation of chronic issues. Additionally, the community was likely aware that treatment options during this time were limited: there was a hold on elective surgery and temporary closures of physical therapy facilities, which may have influenced patients’ decision to present to a surgeon’s office. Ultimately, patients with chronic injuries may have thought the increased risk of contracting the virus by leaving their home outweighed the benefit of a foot and ankle evaluation for an issue they have been coping with for more than 1 month. On the other hand, patients who sustained acute injuries may have made the decision to present to clinic because of an uncertainty of their symptoms, acute change in their function, or out of necessity for urgent injuries such as an unstable ankle fracture.
A change in daily activities and exercise routines during the stay-at-home order may explain the changes in injury patterns observed in this investigation. During the quarantine, many businesses had to adapt to the new restrictions, resulting in employees either furloughed, unemployed, or working from home. These individuals now had new schedules that may have allowed for additional time to exercise. However, variable results have been demonstrated when asking individuals whether their physical activity increased, remained constant, or decreased during the pandemic.3,10,16,19,22 In addition, quarantine restrictions also resulted in the closure of fitness centers, city parks, and other recreational areas, which led to an increased emphasis on staying active and promotion of new exercise regimens to mitigate the potential negative effects of a sedentary lifestyle.5,7,9 Because of the decreased accessibility to these facilities, the specific type of exercise and location where exercises were performed changed during COVID-19.4,10 These changes in activity level, exercise type, and location could affect the type of injuries sustained during the pandemic. For example, patients may have begun new high-repetition exercises on unfamiliar surfaces that may increase the risk of stress fractures of the foot and ankle as was seen in our cohort. Additionally, individuals were no longer allowed to participate in team sports as a method of social distancing. This may explain the lower proportion of Achilles tendon ruptures, which is usually sustained during explosive movements requiring sudden contraction of the gastrocnemius-soleus complex typically seen in team sports, such as basketball.
Similar findings to the present study have been observed in other orthopaedic subspecialties during the COVID-19 pandemic. Park et al 14 found a greater proportion of patients with acute presentations to the orthopaedic trauma service during quarantine. Lubbe et al 12 demonstrated a greater time to presentation (0.41 days vs 1.31 days) to a level 1 trauma center during COVID-19 when compared to previous years and attributed it to patient reluctance to present to the hospital because of the risk of viral exposure. This indicates that even with acute injuries, the decision to present for evaluation was not straightforward for patients, and was likely made because of the severity of their new symptoms.
Additionally, the change in physical activities as a result of quarantine restrictions may have resulted in different injury mechanisms. Staunton et al 20 evaluated patients presenting to a general orthopaedic hospital and observed a lower proportion of patients reporting injury from sport-related activity and higher proportion of patients reporting injury from personal exercise. Park et al 14 also reported a significantly lower proportion of patients presenting with sports injuries to the orthopaedic trauma service. In pediatrics, there was a greater number of fractures sustained at home and smaller proportion of fractures sustained related to sports or playgrounds. 1 Overall, in the trauma and pediatrics subspecialties, changes in patient presentations were observed related to location of injury, mechanism of injury, and timing of presentation associated with the COVID-19 pandemic.
The greatest strength of the present study is that it describes the impact of the COVID-19 pandemic and quarantine on the type of injuries seen in a foot and ankle clinic, which has not been previously described. The use of a control group from the same time period 1 year prior reduces potential confounders such as seasonal variations in injury patterns. Furthermore, our study included a large number of patients all within the same practice, which provided consistency in diagnostic workup, treatment plans, and allowed us to follow patients over time.
The current study also has limitations. The retrospective nature of this study did not allow us to track specifics regarding injury mechanism because of heterogeneity of patient records. Injury mechanism was inferred by the patient’s diagnosis because a description of the mechanism was not always included in the patient record, or may have been unreliable. Because of the limitations of the retrospective chart review, we were not able to collect information such as mode of transportation to clinic, or change in activity level or mobility status, which may have yielded further insight into our cohort. Furthermore, our results reflect injury patterns of patients who presented to our practice and were affected by the restrictions imposed in our geographic area and may not be generalizable to other locations, practice settings, or the community at large. Data regarding foot and ankle pathology presenting to the emergency department during the study periods was not available for our cohort; therefore, we were unable to make a comparison between our cohort and patients who may have presented with similar complaints to the emergency department. The effects of insurance were not analyzed in this study because of limitations of data availability, but they could have an influence on a patient’s ability to present to clinic, in conjunction with their mobility status and access to transportation. There is the possibility that patients with acute stress injuries waited until later in their injury course to present, causing them to be categorized into chronic stress injury group or not categorized at all if presenting outside of the study window. Finally, it is most likely the case that the number and kinds of patients presenting to clinic changed over time after the study period concluded; however, these data were not collected for the present study.
Conclusion
In conclusion, the COVID-19 pandemic and subsequent stay-at-home order resulted in a significant shift in prevalence of pathology and symptom duration experienced by new patients presenting to a US orthopaedic foot and ankle clinic. This shift may reflect both the adoption of different activities during the quarantine period and a reluctance to present to a medical environment for evaluation of nonurgent injuries.
Footnotes
Ethical Approval: Ethical approval for this study was obtained from Rush University Medical Center Institutional Review Board (ID 17052101).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Nabil Mehta, MD,  https://orcid.org/0000-0002-7255-4569
https://orcid.org/0000-0002-7255-4569
Daniel D. Bohl, MD, MPH,  https://orcid.org/0000-0002-7599-4244
https://orcid.org/0000-0002-7599-4244
References
- 1. Bram JT, Johnson MA, Magee LC, et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop. 2020;40(8):373-379. doi: 10.1097/BPO.0000000000001600 [DOI] [PubMed] [Google Scholar]
- 2. City of Chicago. Reopening Chicago. 2020. https://www.chicago.gov/city/en/sites/covid-19/home/reopening-chicago.html (accessed September 20, 2020).
- 3. Constandt B, Thibaut E, De Bosscher V, Scheerder J, Ricour M, Willem A. Exercising in times of lockdown: an analysis of the impact of COVID-19 on levels and patterns of exercise among adults in Belgium. Int J Environ Res Public Health. 2020;17(11). doi: 10.3390/ijerph17114144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Di Renzo L, Gualtieri P, Pivari F, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020;18(1):229. doi: 10.1186/s12967-020-02399-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dwyer MJ, Pasini M, De Dominicis S, Righi E. Physical activity: benefits and challenges during the COVID-19 pandemic. Scand J Med Sci Sports. 2020;30(7):1291-1294. doi: 10.1111/sms.13710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Eble SK, Hansen OB, Ellis SJ, Drakos MC. The virtual foot and ankle physical examination. Foot Ankle Int. 2020;41(8):1017-1026. doi: 10.1177/1071100720941020 [DOI] [PubMed] [Google Scholar]
- 7. Fuzeki E, Groneberg DA, Banzer W. Physical activity during COVID-19 induced lockdown: recommendations. J Occup Med Toxicol. 2020;15:25. doi: 10.1186/s12995-020-00278-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Harcourt J, Tamin A, Lu X, et al. Severe acute respiratory syndrome coronavirus 2 from patient with coronavirus disease, United States. Emerg Infect Dis. 2020;26(6):1266-1273. doi: 10.3201/eid2606.200516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jimenez-Pavon D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people. Prog Cardiovasc Dis. 2020;63(3):386-388. doi: 10.1016/j.pcad.2020.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lesser IA, Nienhuis CP. The impact of COVID-19 on physical activity behavior and well-being of Canadians. Int J Environ Res Public Health. 2020;17(11). doi: 10.3390/ijerph17113899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH, 3rd, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28(11):e469-e476. doi: 10.5435/JAAOS-D-20-00380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lubbe RJ, Miller J, Roehr CA, et al. Effect of statewide social distancing and stay-at-home directives on orthopaedic trauma at a southwestern level 1 trauma center during the COVID-19 pandemic. J Orthop Trauma. 2020;34(9):e343-e348. doi: 10.1097/BOT.0000000000001890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moverman MA, Puzzitiello RN, Pagani NR, Barnes CL, Jawa A, Menendez ME. Public perceptions of resuming elective surgery during the COVID-19 pandemic. J Arthroplasty. 2021;36(2):397-402.e2. doi: 10.1016/j.arth.2020.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Park C, Sugand K, Nathwani D, Bhattacharya R, Sarraf KM. Impact of the COVID-19 pandemic on orthopedic trauma workload in a London level 1 trauma center: the “golden month.” Acta Orthop. 2020;91(5):556-561. doi: 10.1080/17453674.2020.1783621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Petrella D, Clair S, Johnson S, Pratt G. Gov. J.B. Pritzker issues order requiring residents to “stay at home” starting Saturday. Chicago Tribune. March 20, 2020. [Google Scholar]
- 16. Phillipou A, Meyer D, Neill E, et al. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: initial results from the COLLATE project. Int J Eat Disord. 2020;53(7):1158-1165. doi: 10.1002/eat.23317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sarac NJ, Sarac BA, Schoenbrunner AR, et al. A review of state guidelines for elective orthopaedic procedures during the COVID-19 outbreak. J Bone Joint Surg Am. 2020;102(11):942-945. doi: 10.2106/JBJS.20.00510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Siow MY, Walker JT, Britt E, et al. What was the change in telehealth usage and proportion of no-show visits for an orthopaedic trauma clinic during the COVID-19 pandemic? Clin Orthop Relat Res. 2020;478(10):2257-2263. doi: 10.1097/CORR.0000000000001396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stanton R, To QG, Khalesi S, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17(11):4605. doi: 10.3390/ijerph17114065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Staunton P, Gibbons JP, Keogh P, Curtin P, Cashman JP, O’Byrne JM. Regional trauma patterns during the COVID-19 pandemic. Surgeon. 2021;19(2):e49-e52. doi: 10.1016/j.surge.2020.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tison GH, Avram R, Kuhar P, et al. Worldwide effect of COVID-19 on physical activity: a descriptive study. Ann Intern Med. 2020;173(9):767-770. doi: 10.7326/M20-2665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wang X, Lei SM, Le S, et al. Bidirectional influence of the COVID-19 pandemic lockdowns on health behaviors and quality of life among Chinese adults. Int J Environ Res Public Health. 2020;17(15):5575. doi: 10.3390/ijerph17155575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020