Abstract
Aim:
Controlled sequential elevation of the head and thorax (CSE) during active compression-decompression (ACD) CPR with an impedance threshold device (ITD) augments cerebral (CerPP) and coronary (CorPP) perfusion pressures. The optimal CSE is unknown.
Methods:
After 8 min of untreated VF, 40 kg anesthetized female pigs were positioned on a customized head and thorax elevation device (CED). After 2 min of automated ACD+ITD-16 CPR to ‘prime the system’, 12 pigs were randomized to CSE to the highest CED position over 4-min or 10-min. The primary outcome was CerPP after 7 minutes of CPR. Secondarily, 24-sec (without a priming step) and 2-min CSE times were similarly tested (n=6 group) in a non-randomized order. Values expressed as mean ± SD.
Results:
After 7 min of CPR, CerPPs were significantly higher in the 4-min vs 10-min CSE groups (53 ± 14.4 vs 38.5 ± 3.6 mmHg respectively, p=0.03) whereas CorPP trended higher. The 4-min CSE group achieved 50% of baseline (50% BL) CerPP faster than the 10-min group (2.5 ± 1.2 vs 6 ± 3.1 minutes, p=0.03). CerPP values in the 2-min and 4-min CSE groups were significantly higher than in the 24-sec group. With CSE, CerPPs and CorPPs increased over time in all groups.
Conclusions:
By optimizing controlled sequential elevation timing, CerPP values achieved 50% of baseline within less than 2.5 minutes and >80% of baseline after 7 minutes of CPR. This novel CPR approach rapidly restored CerPPs to near normal values non-invasively and without vasopressors.
Keywords: Active compression-decompression CPR, Cardiac arrest, Cardiopulmonary Resuscitation, Cerebral perfusion pressure, Coronary perfusion pressure, Head Up CPR, Head and thorax elevation Impedance threshold device, Medical device, Patient positioning
Introduction
Controlled sequential elevation (CSE) of the head and thorax during cardiopulmonary resuscitation (CPR) in animals increases cerebral perfusion pressure (CerPP), cerebral blood flow, and coronary perfusion pressure (CorPP). With elevation, venous blood drains rapidly from the brain to the heart, decreasing intracranial pressure (ICP) and lowering the arterial and venous pressure waves simultaneously and repetitively concussing the brain with each compression.1,2 However, conventional CPR is not effective with head and thorax elevation over a prolonged period of time as it does not generate enough forward blood flow to pump ‘uphill’ over time.3–5 Additional circulatory adjuncts are needed, such as an impedance threshold device (ITD), to generate and sustain forward flow upward to the brain.6
Initial animal studies demonstrating proof-of-concept of the head and torso elevation to improve perfusion pressures were performed with a whole-body tilt table, an automated CPR device (LUCAS 2.0), and an ITD-16.7 While this approach works, over time blood pools in the lower extremities and can make CSE less effective and potentially even harmful. 8 Subsequent effort with selective elevation of the head and thorax to 30°,4 during active compression-decompression (ACD) CPR + ITD-16 showed that brain blood flow was doubled versus the flat position. More recent pig studies focused on identifying an optimal elevation angle or height. While no optimal elevation angle was observed, those studies demonstrated that a controlled head and thorax elevation sequence over 10 minutes resulted in nearly normal CerPP after prolonged ACD+ITD CPR. 9
The optimal speed of CSE during CPR remains unknown. It is also unknown if some CPR is needed to ‘prime’ the cardio-cerebral circuit prior to maximal CSE. To address these knowledge gaps, the current investigation tested the hypothesis that CerPP will be optimized by first performing ACD+ITD-16 CPR with the head and thorax partially elevated using a customized elevation device (CED) in the lowest height for two minutes followed by a CSE over two minutes to the maximum CED height compared to other CSE speeds.
Materials and Methods
This study was approved by the Institutional Animal Care Committee of the Hennepin Healthcare Research Institute. Experiments were done in compliance with the 2011 Guideline for the Care and Use of Laboratory Animals. A certified and licensed veterinarian assured protocol performance.
Study design and measurements
Surgical preparation, anesthesia, data monitoring and recording procedures used in this study have been previously described.3,4,7 This study was performed in 24 healthy Yorkshire female farm pigs weighing approximately 40 Kg. After acclimatizing, pigs were fasted overnight. Initial sedation with intramuscular ketamine (10 ml of 100 mg/ml) was followed by inhaled isoflurane (1-1.5%). Once sedated, intubation was performed using a 7.5 mm endotracheal tube and ventilation was provided using an anesthesia machine (Narkomed, North American Drager, Telford, PA) with a tidal volume of 10 ml/Kg. The respiratory rate and FiO2 were adjusted to maintain adequate oxygen saturation (>92%) and normocapnia (ETCO2= 40 mmHg) as measured with a CO2SMO Plus (Novametrix Systems, Wallingford, CT). An esophageal probe was used to monitor temperature, which was kept between 36.5° and 37.5°C using a warming blanket as needed. Intracranial pressure (ICP) was measured using a micromanometer-tipped catheter (Mikro-Tip transducer, Millar Inc, Houston, TX, USA) inserted through a burr hole in the skull into the parietal lobe. Central aortic blood pressures (MAP) were recorded continuously with a Millar catheter placed via left femoral artery cannulation in the descending thoracic aorta at the level of diaphragm. A Millar catheter was placed in the right femoral vein, and advanced to the right atrium to monitor right atrial pressure (RA). Fluoroscopy was performed to confirm catheter placement. Euvolemia was maintained with normal saline to maintain the mean right atrial pressure between 5 and 9 mmHg. All animals received intravenous heparin as a bolus (100 units/kg) hourly. Arterial blood gases (ABG) were acquired through the femoral artery catheter and analyzed Gem Premier 3000 device (Instrumentation Laboratory, Lexington, MA).
All haemodynamic parameters, including electrocardiographic monitoring, MAP, RA pressure, ETCO2 and ICP were monitored and recorded continuously with a digital system (BIOPAC MP 150, BIOPAC Systems, Inc., CA, USA). CerPP was calculated as the difference between MAP and mean ICP. CorPP was calculated as the difference between the CPR decompression phase aortic and RA pressures.
Ventricular fibrillation (VF) was induced by direct electrical intra-cardiac current through an electrophysiology catheter in the right ventricle. ACD CPR was performed with a customized automatic piston device (Caztek Engineering, St. Paul, MN) at a rate of 100 per minute with a 50% duty cycle and depth of 22.5% of the antero-posterior chest diameter. The force of decompression was not measured directly. What was constant was the active decompression excursion distance of 4 cm from the baseline pre-CPR and pre-VF level of the sternum. Based upon prior studies this equates to an upwards force of about 8-10 kg.
An ITD with a resistance of 16 cm H20 (ITD-16) (ResQPOD-16™, ZOLL Minneapolis, Roseville, MN) was attached to the endotracheal tube.
Pigs were placed in the horizontal plane. The position of the body was changed using a customized head and thorax elevation device (CED). This device was designed to provide pigs undergoing CPR with similar elevation heights to a human device (EleGARD™) Patient Positioning System, Advanced CPR Solutions). The CED was electrically-coupled to the chest compressor and delivered ACD CPR at a 90° angle to the mid-sternum continuously, regardless of the body position. During CPR the CED was first adjusted to be in the lowest elevation position, elevating the head 10 cm and heart 7 cm above the horizontal plane while the lower thorax, abdomen and lower extremities remained without any elevation. (Fig. 1) The CED was sequentially elevated to a maximum head and heart height of 22 cm and 8 cm, respectively. (Fig. 1). The CED rise time was adjustable. During the preparatory phase, the pig’s extremities were secured such that the upper legs were positioned laterally to the head and the lower legs were extended downwards.
Figure 1.
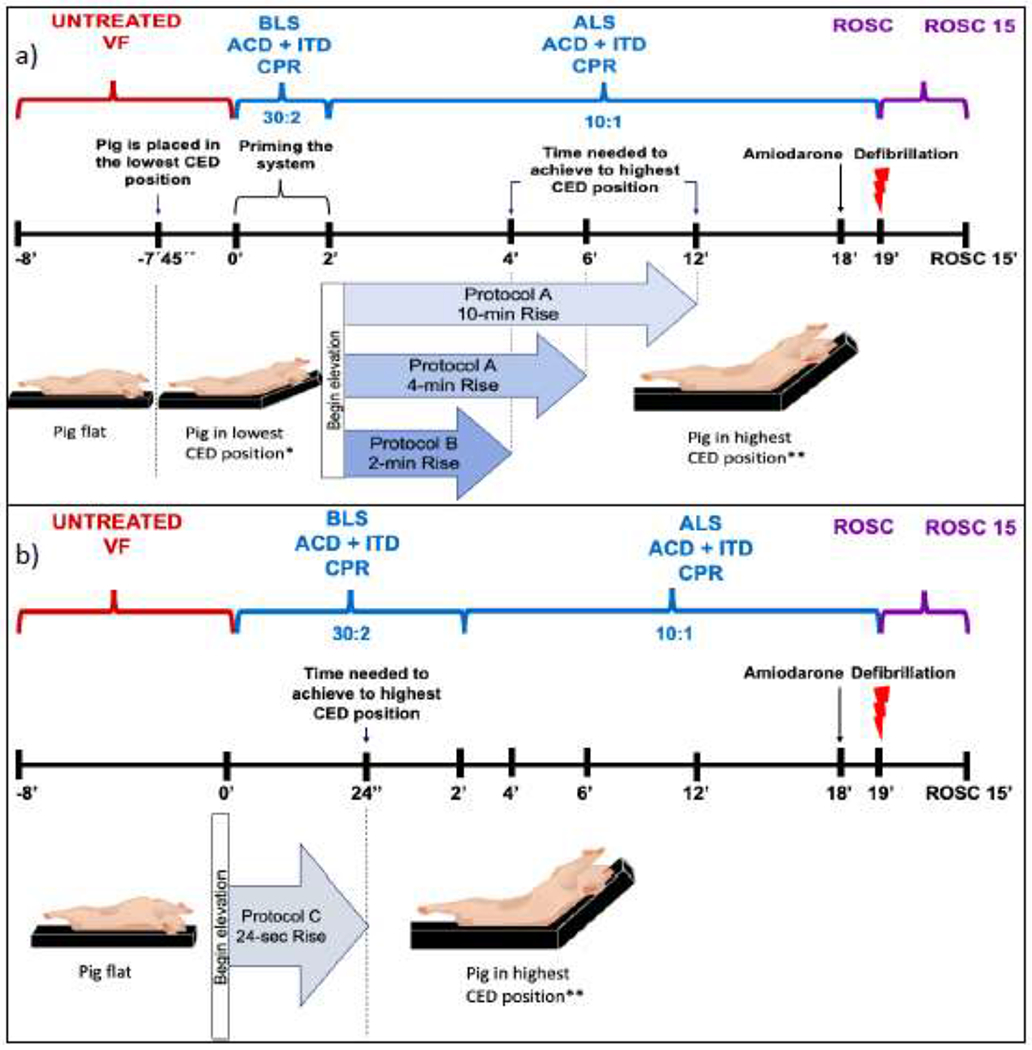
a Study timeline for Protocol A and B. Pigs were studied with elevation rise times of 2-, 4-, and 10-minutes, respectively.
b Study timeline for Protocol C. Pigs were studied with elevation rise time of 24 seconds, without CPR prior to elevation of the head and thorax.
Abbreviations: active compression decompression (ACD) plus impedance threshold device (ITD), cardiopulmonary resuscitation (CPR), customized head and thorax elevation device (CED), ventricular fibrillation (VF), basic life support (BLS), advanced life support (ALS), return of spontaneous circulation (ROSC).
* When the pig was in the lowest CED elevation the heart was elevated 7 cm and the midbrain 10 cm.
** When the pig was in the highest CED elevation the heart was elevated 8 cm and the midbrain 22 cm.
Experimental Protocols
Protocol A is outlined in Fig. 1.a Once stable haemodynamics were observed for at least 15 minutes, defined as having a MAP of >70 mmHg and a mean RA of 5-10 mmHg, an arterial blood gas analyses were performed at baseline, at 10 min of CPR and one minute immediately after ROSC. The isoflurane was then discontinued, three minutes later VF was induced, and positive pressure ventilation was then discontinued. After 7 minutes and 45 seconds, the CED was elevated to the lowest position. Fifteen seconds later, ACD+ITD-16 CPR was started with a 30: 2 compression: ventilation ratio for the first 2 minutes to simulate basic life support (BLS). After 2 minutes of BLS ACD+ITD-16 CPR, the CED was activated to elevate the head and thorax over either 4 (3 cm/min) or 10 (1.2 cm/min) minutes based upon the randomization assignment to the same target final head elevation height of 22 cm. Simultaneously, asynchronous ACD+ITD-16 CPR was performed continuously for 16 min with a 10:1 compression: ventilation ratio to simulate advanced life support (ALS). After the first spontaneous gasp, respiratory effort or “gasping” during CPR was inhibited by administrating a bolus of 60 mg succinylcholine. After a total of 18 minutes of CPR, 25 mg dose of amiodarone was administered via the femoral vein. One minute later defibrillation was performed with 200 joules (X™ Series defibrillator, ZOLL Medical, Chelmsford, MA). Up to 3 defibrillation shocks were delivered, as needed. After return of spontaneous circulation (ROSC), the head and thorax remained elevated for 15 minutes, as long as the MAP was >65 mmHg. Pigs were then euthanized with concentrated potassium chloride.
Protocol B (Fig. 1.a) was similar to Protocol A except the elevation rise time after 2 minutes of BLS CPR in the lowest position on the CED was 2 minutes, thereby achieving the maximum CED head height elevation of 22 cm and heart elevation of 8 cm within 4 minutes from the start of CPR.
A fourth study group was tested using Protocol C (Fig. 1.b) After 8 minutes of untreated VF, these pigs reached the maximum CED height over 24 seconds without a ‘priming step’. In other words, they went from the flat horizontal plane to the highest position in 24 seconds. Protocol A and C were similar in terms of ventilation, ACD+ITD-16 CPR, duration, drug administration, time to defibrillation and time arterial blood gases were analyzed. Animals in Protocol B and C were not randomized.
Statistical Analyses
Based upon prior studies we hypothesized a priori that it would take some time, between 2-4 minutes, to observe the effects of the proposed CSE. The time frame of 2-4 minutes after CSE was in the highest position during the 4-min versus 10-min rise elevation study was the time period of primary interest. For the purposes of describing the current results, we selected 7 minutes, which is in the middle of this time period of primary interest. We estimated the mean CerPP would be approximately 50% higher in Protocol A in the 4 min elevation rise time versus the 10 min rise time group based upon prior studies.4,9 Assuming an alpha of 0.05 and 80% power, we calculated a sample size of 6 pigs per group to detect an 80% difference. Data were expressed as mean ± standard deviation and pressures in mmHg. Statistical analysis was performed using STATA 13 (StataCorp LP, College Station, Texas). CerPP mean values were compared using a Student’s unpaired t test. All statistical tests were two-sided, and a p value of less than 0.05 was required to reject the null hypothesis.
Secondary outcomes that were measured included duration of time needed to achieve 50% of CerPP and CorPP values (50%BL) after the start of CPR, CerPP after 18 minutes of CPR, MAP and CorPP after 7 minutes of CPR, time to first spontaneous gasp, and ROSC rates. A post hoc ANOVA analysis was used to compare CerPP values in groups A, B and C. Subsequent comparisons were performed with a Tukey Kramer test. All values are presented as mean ± SD.
Results
There were 6 pigs in each study group (4-min, 10-min, 2-min and 24-sec rise time). At baseline there were no differences in haemodynamic parameters (CerPP, CorPP, MAP and ICP) (Table 1) or blood gases between the four study groups (Table 2).
Table 1.
Haemodynamic measurements of the different rates of elevation during ACD + ITD CPR.
| N = 24 | Baseline | 7 Minutes CPR | 18 Minutes CPR | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Rise Time Group | 10-Minute | 4-Minute | 2-Minute | 24-Seconds | 10-Minute | 4-Minute | 2-Minute | 24-Seconds | 10-Minute | 4-Minute | 2-Minute | 24-Seconds |
| AO Systolic |
87±17 | 88±16 | 75±7 | 77±8 | 66±4 | 81±1* | 85±14 | 55±9 | 69±13 | 79±27 | 80±20 | 74±24 |
| AO Diastolic |
73±15 | 74±15 | 68±30 | 63±7 | 45±2 | 55±20 | 59±14 | 42±12 | 48±14 | 55±28 | 59±22 | 52±19 |
| ICP Diastolic |
16±2 | 15±2 | 13±6 | 14±3 | 11±3 | 9±5 | 12±4 | 7±3 | 7±2 | 6±3 | 7±4 | 5±5 |
| RA Systolic |
1±5 | 3±5 | 5±0.9 | 4±4 | 56±4 | 74±13 | 59±15 | 70±13 | 65±14 | 73±12 | 57±13 | 70±18 |
| RA Diastolic |
1±6 | 4±5 | 11±15 | 4±4 | 7±3 | 4±3 | 10±6 | 6±2 | 7±5 | 3±3 | 9±8 | 7±6 |
| CerPP Mean |
64±15 | 66±17 | 62±8 | 59±8 | 39±4 | 53±14* | 53±15 | 32±12 | 46±13 | 57±19 | 58±20 | 54±20 |
| CorPP |
72±20 | 70±17 | 73±8 | 67±5 | 38±3 | 51±20 | 48±17 | 30±11 | 40±14 | 52±28 | 50±20 | 45±15 |
| ITP Diastolic |
3±1 | 3±1 | 2±0.3 | 3±1 | −4±1 | −5±1 | −4±2 | −4±2 | −3±1 | −4±1 | −5±3 | −5±3 |
| ETCO2 Mean | 44±2 | 44±1 | 44±2 | 43±1 | 51±10 | 50±6 | 52±6 | 42±7 | 50±8 | 47±8 | 49±7 | 46±8 |
Values are mean ± standard deviation.
Abbreviations: active compression decompression (ACD), aortic pressure (Ao), cerebral perfusion pressure (CerPP), coronary perfusion pressure (CorPP), end tidal CO2 (ETCO2), intracranial pressure (ICP), intrathoracic pressure (ITP), right atrial pressure (RAP), systole or compression phase (sys), diastole or decompression phase (dias).
p≤0.05 when comparing 4-min vs 10-min controlled sequence elevation groups.
Table 2 -.
Arterial blood gases results obtained before the start of cardiac arrest and after return of spontaneous circulation (ROSC) for the four different elevation rise time groups.
| Time point | Baseline |
ROSC |
||||||
|---|---|---|---|---|---|---|---|---|
| Elevation rise time groups | 24-s | 2-min | 4-min | 10-min | 24-s | 2-min | 4-min | 10-min |
| PH | 7.47±0.02 | 7.44±0.05 | 7.46±0.01 | 7.46±0.02 | 7.05±0.06 | 7.11±0.05 | 7.10±0.03 | 7.07±0.09 |
| PCO2 | 43±2 | 42±2 | 43±4 | 42±2 | 87±14 | 83±12 | 74±13 | 80±21 |
| PaO2 | 90±16 | 97±12 | 103±13 | 106±26 | 80±17 | 64±22 | 77±38 | 70±18 |
| HCO3− | 32±1 | 28±2 | 31±3 | 30±2 | 25±1 | 23±1 | 23±2 | 22±2 |
| BE | 8±2 | 5±2 | 7±3 | 6±2 | −6±1 | −8±1 | −7±2 | −7±2 |
| SaO2 | 97±1 | 97±1 | 98±1 | 98±2 | 86±9 | 76±7 | 83±9 | 81±14 |
Values shown as mean ± standard deviation.
BE = base excess.
In Protocol A, as soon as the pigs were elevated to the lowest position on the CED before the start of CPR, there was an immediate and significant decrease in ICP, as shown in representative pressure tracings in Fig. 2. With CSE, while still in untreated VF, the ICP (mmHg) decreased from 20.4 ± 1.8 in the flat position (Fig. 1.a) to 15.6 ± 1.8 in the lowest CED position (Fig 1.a) in all 12 pigs (p< 0.001). By contrast, the MAP (mmHg) remained constant (15.6 ± 4.7 vs 16.8 ± 5.3, respectively, p = 0.68) and CerPP (mmHg) increased significantly (−4.8 ± 4.9 vs 1.3 ± 5.6, respectively, p= 0.03).
Figure 2.
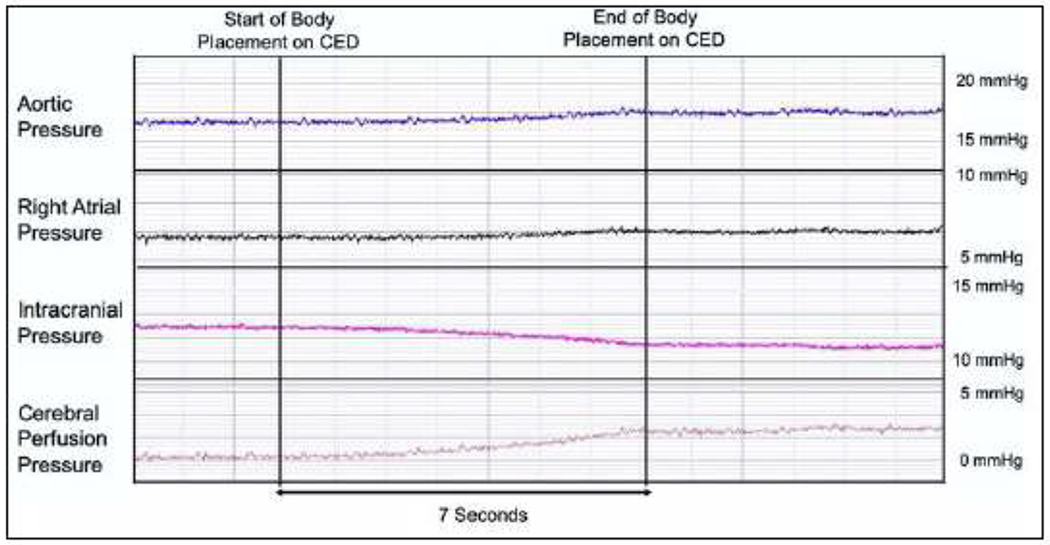
Changes in aortic, right atrial, intracranial, and cerebral perfusion pressures in a representative tracing during the transition from a flat position to the lowest position on the customized elevation device (see Figure 1.a) after 8 minutes of untreated ventricular fibrillation immediately prior to the start of CPR.
CerPP (mmHg) after 7 minutes of CPR, the primary study outcome, was significantly higher in the 4-min (53 ± 14.4) versus 10-min rise group (38.5 ± 3.6) (p=0.03). The 4-min CSE group reached 50%BL (minutes) CerPP values significantly faster (minutes) than the 10-min rise group (2.5 ± 1.2 vs 6.0 ± 3.1, p = 0.03, respectively) (Fig 3.a). Time to 50% BL (minutes) CorPP trended faster in the 4-min rise group (3.5 ± 2 versus 8.4 ± 5.8, p = 0.08, respectively). The systolic blood pressure (mmHg) was significantly higher in the 4-min rise group (80.5 ± 15) versus the 10-min rise group (66 ± 4) (p<0.05) at 7 minutes, and CorPP (mmHg) trended higher in the 4-min rise group as well (50.8 ± 20.2 vs 38.3 ± 2.5, respectively, p=0.16). In contrast to the increase in the MAP over time, there was a slow but steady decrease in mean diastolic ICP values over time (Table 1). In the absence of exogenous vasopressors, CerPP and CorPP values in the 4-min rise groups were 82% and 70% of baseline values after 7 minutes of CPR, and 89% and 72% after 18 minutes of CPR, respectively. (Table 1) The head and heart remained were kept elevated in the highest CED position after ROSC. Fifteen minutes after ROSC, CerPP (mmHg) values remained constant in the 4-min and 10-min elevation groups (72.0 ± 8.7 vs 73.6 ± 5.6, p=0.71). The values were approximately 10% higher than the respective baseline values.
Figure 3.
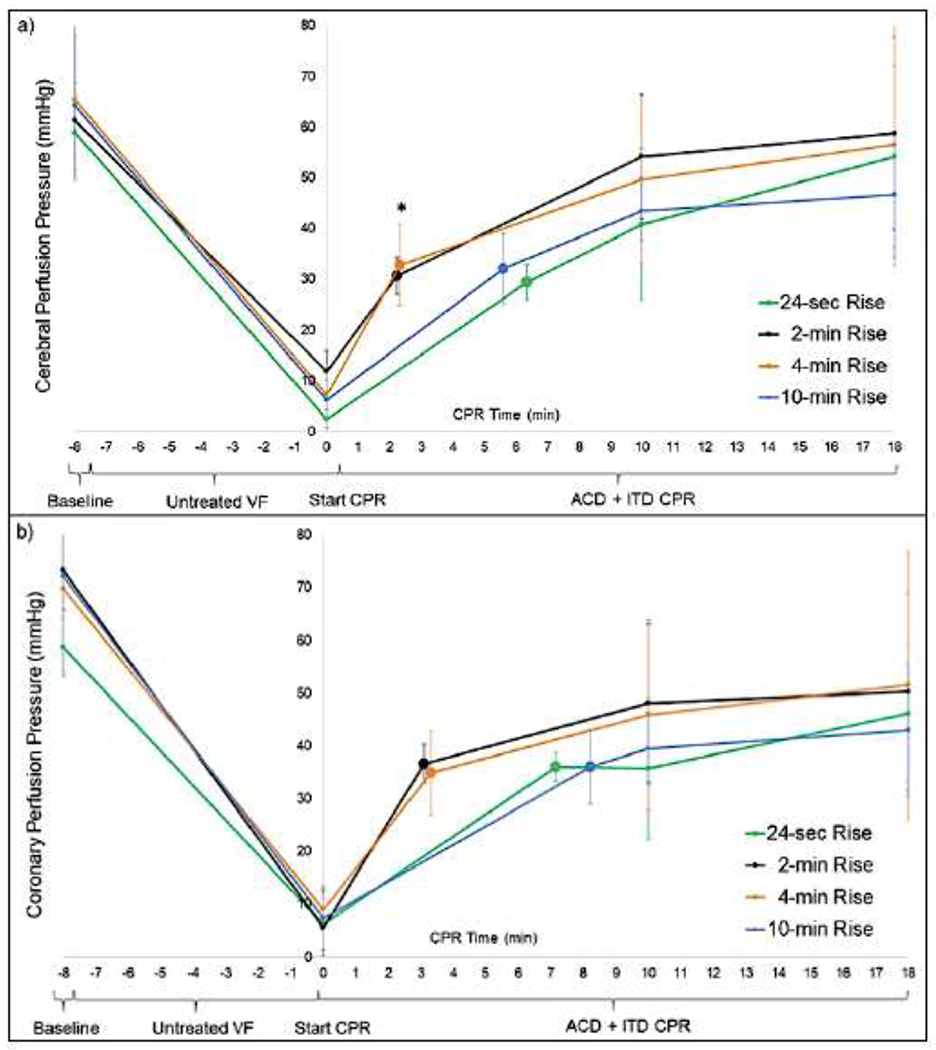
Time, in minutes, to achieve 50% of baseline cerebral perfusion pressure (CerPP) (Figure 3.a) and coronary perfusion pressure (CorPP) (Figure 3.b) for the four different controlled sequence elevation (CSE) groups (24-sec, 2-min, 4-min, 10-min) during ACD ITD-16 CPR. *p≤0.05 when comparing 4-min vs 10-min controlled sequence elevation groups.
To determine the optimal speed of elevation but still maintain the observed benefits associated with CSE, the 4-min rise time group was compared in a non-randomized manner with a 2-min rise time group in Protocol B. The respective CerPP and CorPP values were nearly equivalent between the 2- and 4-minute rise time groups, as shown in Table 1 and Fig. 3 The systolic and diastolic blood pressures were the highest in the 2-min rise time group. Additionally, the decompression phase RAP and the systolic and diastolic ICP values remained relatively constant throughout CPR, as shown in Fig. 4.
Figure 4.
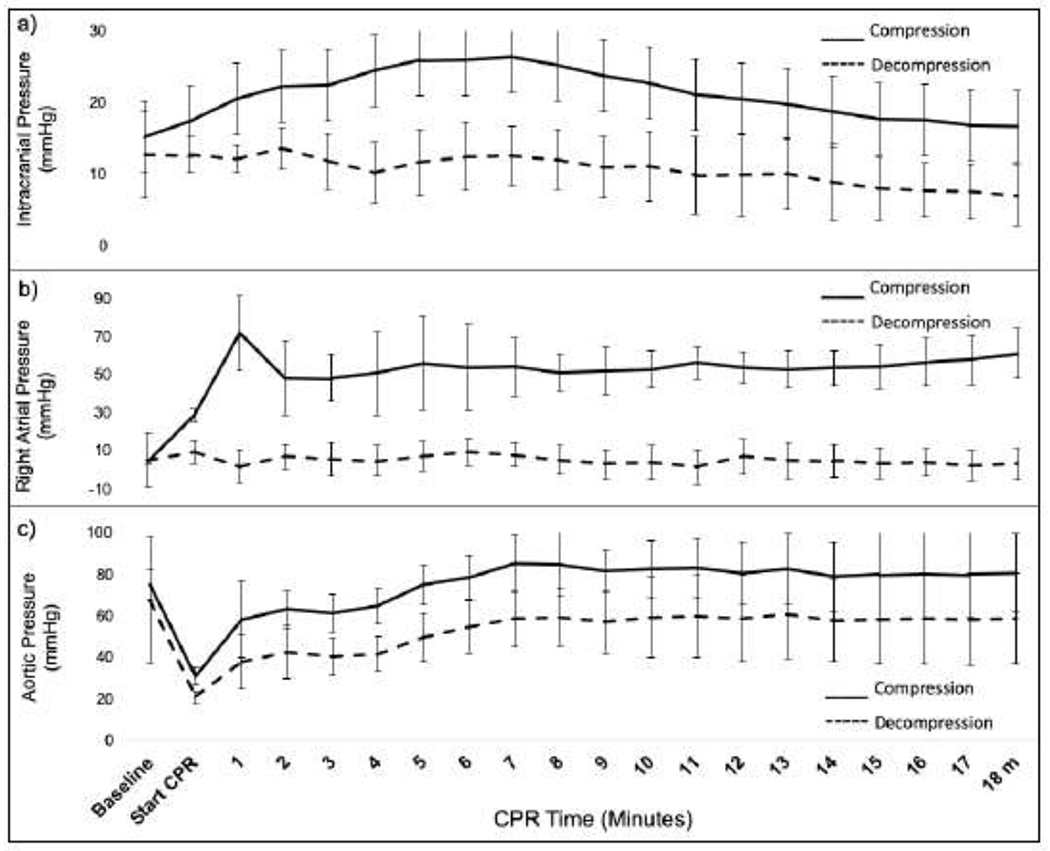
Hemodynamic parameters (mean ± SD, mmHg) using a device-controlled assisted elevation over 2-minutes sequence (n=6 pigs) during active compression-decompression combined (ACD) CPR combined with an impedance threshold device (ITD). a) Intracranial pressure b) Right atrial pressure c) Aortic pressure.
Protocol C was designed to compare the optimal rise time results from studies in Protocol A and B with a rapid elevation over 24-sec time, without a priming step, to simulate simply elevating the head and thorax on a transport bed capable of elevation of the upper body at the level of the waist. A comparison of CerPPs between all three protocols using a showed significantly lower values in the 24-sec rise time group when compared with the 2-min (p = 0.031) and 4min rise time groups (p = 0.032) of pigs at 7 minutes (Table 1). In addition, ETCO2 values after 7 minutes of CPR in the 24-sec rise group trended lower 10 mmHg less than the 2-, 4- and 10-min ‘priming step’ groups. (Table 1) Time to 50%BL (minutes) CerPP trended longer in the 24-sec rise group versus the combined 2- and 4-min CSE groups (6.6 ± 6.4 vs 2.4 ± 2.1, p=0.18)
Time to first gasp (seconds) trended earlier in the 4-min versus 10-min rise time group (217.2 ± 41.7 vs 285.6 ± 73.4 respectively, p=0.07). The time to first gasp was longer in the 24-sec rise time group (300.3±72.7) in comparison with the 2-min rise time group (263.61 ± 69.05). There was no difference in ABG values between the four groups. All animals were successfully defibrillated and had a ROSC irrespective of rate of elevation.
Discussion
The purpose of this study was to optimize the sequence and speed of head and thorax elevation to rapidly enhance cerebral perfusion pressures during CPR. The 4-min controlled elevation sequence resulted in a rapid and prolonged benefit, with CerPP ultimately reaching 89% of baseline values. CerPP after 7 minutes of CPR, the primary study endpoint, was significantly higher with the 4-min rise time versus the 10-min rise time. CerPP values with the 2-min CSE time resulted in CerPP values that were equivalent to those achieved with the 4-min rise time. Prior studies demonstrated that the rise in cerebral perfusion pressure observed with elevation of the head and thorax during CPR with an ITD paralleled changes in cerebral blood flow, measured using microsphere, in terms of magnitude and effect.4,7
The 2-min rise time reduced the potential for harm from too rapid (24-sec) or too slow (10-min). This new non-invasive step-wise approach lowered ICP, reduced potential for an arterial-venous wave concussion with every compression, and optimized cardiopulmonary and cerebral circulation. In addition, after 7 minutes of CPR the CorPP in both the 4-min and 2-min CSE trended 30% higher than the 10-min CSE group and these differences were sustained over time. Sustained cerebral and coronary perfusion pressure of this magnitude in the absence of exogenous vasopressors have not, to our knowledge, been previously reported.
A strong positive correlation between early CPR and survival rate is well established in animals and humans.10–12 The current results describe a novel way to assess the effectiveness of any given method of CPR, time to achieve 50% of normal vital organ perfusion pressure. As shown in Fig. 3, 50% BL CerPP and CorPP was achieved in 2.5 and 3.5 minutes respectively when using the 4-min elevation timing sequence. Results were similar with the 2-min rise time. Many previously described CPR methods, especially conventional manual closed chest CPR, do not achieve 50% BL CerPP or CorPP values at any time.3,13 The identification of an innovative CPR methodology to achieve 50% BL CerPP within 2-3 minutes and nearly normalize CerPP values during prolonged ACD+ITD CPR represents an important step forward in the evolution of CPR.
The current results also highlight the immediate benefits of elevating the head and heart to the lowest position on the CED before chest compressions and of the priming step before CSE to the highest CED position. Elevation just prior to CPR immediately reduced venous cerebral congestion associated with lying supine and ventricular fibrillation, and this is reflected by a significant decreased of ICP within seconds. Further, the importance of propelling circulation by means of the priming step was demonstrated by differences in the 24-sec rise group versus the other groups. The 24-sec rapid rise group perfusion pressures, without a priming step, trended lower than the 2- and 4-min rise time groups. The priming step was intentionally performed with the head and thorax in the lowest position on the CED in the 2-, 4- and 10- min rise groups, to start circulation and increase the arterial pressure head before elevating the head further.
The neuroprotective effect of CSE is also reflected in time to first spontaneous gasp. The gasping reflex is a well-known auto-resuscitation phenomenon and it decreases intrathoracic pressure and increases in venous return, decreases in ICP, increases in aortic pressure, CorPP, CerPP, cardiac output and cardiac contractility14 and is an independent predictor of survival with favorable neurological function after cardiac arrest.15,16 17 With the optimized 2 and 4-min rise time sequence, time to first gasp trended nearly 1 minute faster than in the 24-sec and 10-min rise groups.
This study has some limitations. This study was an animal model with healthy pigs, without any comorbidities commonly seen in human cardiac arrest. However, an assessment of the optimized CSE in cardiac arrest patients is ongoing. Brain blood flow was not measured. However, prior head and thorax elevation studies have shown a close relationship between blood flow and CerPP and CorPP.4,7 A clinical outcome, such as neurologically intact survival was not studied. The 2-minute and 24-second rise groups were studied in a non-randomized manner; however, these groups provide important information that can have direct impact clinically about the fastest and safest way to perform head and thorax elevation. Like defibrillation, rapid initiation of ACD+ITD CPR plus elevation of the head and thorax is likely important to give a patient the best chance of survival. However, it is difficult to translate what happens in the laboratory into real life. The arrest may not be witnessed. There may not be bystander CPR. Devices such as ACD CPR or the ITD may not immediately be on scene. It may take longer for a CED device to arrive and be applied. However, some important elements of the resuscitation can be controlled. First, CPR should be performed supine or relatively flat prior to elevating the head and thorax to provide priming of the cardio-cerebral circuit. Second, a circulatory adjunct such as the ITD or ACD+ITD should be present prior to initiation of head and thorax elevation. Lastly, the use of an automated CED device provides optimal patient positioning and execution of CSE.
Conclusion
These studies demonstrate it is possible to rapidly generate and sustain nearly normal CerPP pressures during ACD+ITD-16 CPR by using a customized mechanical head and thorax elevation device, a priming step, and a controlled timing sequence to elevate the head and thorax over a 2-min period. This protocol offers substantial physiological advantages versus slower or more rapid head and thorax elevation timing sequences. Further studies are needed to determine if these advances will improve patient outcomes.
Supplementary Material
Acknowledgments
This study was funded, in part, by a NIH NHBLI SBIR phase I grant.
Contract number 1R43HL139184-01
Conflict of interest statement
Dr. Lurie founded Advanced CPR Solutions LLC to develop novel resuscitation technologies including head up CPR devices. No other authors have a financial conflict of interest.
This study was funded, in part, by a NIH NHBLI SBIR phase I grant. Contract number 1R43HL139184-01
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Carolina Rojas-Salvador, Department of Emergency Medicine, University of Minnesota, Minneapolis, MN, USA.
Johanna C Moore, Department of Emergency Medicine, Hennepin Healthcare, Minneapolis, MN, USA. Hennepin Healthcare Research Institute, Minneapolis, MN, USA.
Bayert Salverda, Hennepin Healthcare Research Institute, Minneapolis, MN, USA.
Michael Lick, Hennepin Healthcare Research Institute, Minneapolis, MN, USA.
Guillaume Debaty, Université Grenoble Alps/CNRS/CHU de Grenoble Alpes/TIMC-IMAG UMR 5525, Grenoble, France.
Keith G Lurie, Department of Emergency Medicine, Hennepin Healthcare, Minneapolis, MN, USA. Hennepin Healthcare Research Institute, Minneapolis, MN, USA.
References
- 1.Petersen LG, Petersen JC, Andresen M, Secher NH, Juhler M. Postural influence on intracranial and cerebral perfusion pressure in ambulatory neurosurgical patients. Am J Physiol Regul Integr Comp Physiol. 2016;310(1):R100–104. [DOI] [PubMed] [Google Scholar]
- 2.Tasker RC. Intracranial pressure: influence of head-of-bed elevation, and beyond. In: Pediatr Crit Care Med. Vol 13. United States: 2012:116–117. [DOI] [PubMed] [Google Scholar]
- 3.Ryu HH, Moore JC, Yannopoulos D, et al. The Effect of Head Up Cardiopulmonary Resuscitation on Cerebral and Systemic Hemodynamics. Resuscitation. 2016;102:29–34. [DOI] [PubMed] [Google Scholar]
- 4.Moore JC, Segal N, Lick MC, et al. Head and thorax elevation during active compression decompression cardiopulmonary resuscitation with an impedance threshold device improves cerebral perfusion in a swine model of prolonged cardiac arrest. Resuscitation. 2017;121:195–200. [DOI] [PubMed] [Google Scholar]
- 5.Aufderheide TP, Frascone RJ, Wayne MA, et al. Standard cardiopulmonary resuscitation versus active compression-decompression cardiopulmonary resuscitation with augmentation of negative intrathoracic pressure for out-of-hospital cardiac arrest: a randomised trial. Lancet. 2011;377(9762):301–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pepe PE, Scheppke KA, Antevy PM, et al. Confirming the Clinical Safety and Feasibility of a Bundled Methodology to Improve Cardiopulmonary Resuscitation Involving a Head-Up/Torso-Up Chest Compression Technique. Crit Care Med. 2019;47(3):449–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Debaty G, Shin SD, Metzger A, et al. Tilting for perfusion: head-up position during cardiopulmonary resuscitation improves brain flow in a porcine model of cardiac arrest. Resuscitation. 2015;87:38–43. [DOI] [PubMed] [Google Scholar]
- 8.Moore JC, Segal N, Debaty G, Lurie KG. The “do’s and don’ts” of head up CPR: Lessons learned from the animal laboratory. Resuscitation. 2018;129:e6–e7. [DOI] [PubMed] [Google Scholar]
- 9.Moore JC, Salverda B, Lick M, et al. Controlled Progressive Elevation Maximizes Cerebral Perfusion Pressure during Head Up CPR in a Swine Model of Cardiac Arrest. Laboratory Studies of CPR and Post-Arrest Recovery; 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lurie KG, Nemergut EC, Yannopoulos D, Sweeney M. The Physiology of Cardiopulmonary Resuscitation. Anesth Analg. 2016;122(3):767–783. [DOI] [PubMed] [Google Scholar]
- 11.Metzger AK, Herman M, McKnite S, Tang W, Yannopoulos D. Improved cerebral perfusion pressures and 24-hr neurological survival in a porcine model of cardiac arrest with active compression-decompression cardiopulmonary resuscitation and augmentation of negative intrathoracic pressure. Crit Care Med. 2012;40(6):1851–1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hasselqvist-Ax I, Riva G, Herlitz J, et al. Early Cardiopulmonary Resuscitation in Out-of-Hospital Cardiac Arrest. New England Journal of Medicine. 2015;372(24):2307–2315. [DOI] [PubMed] [Google Scholar]
- 13.Kim T, Shin SD, Song KJ, et al. The effect of resuscitation position on cerebral and coronary perfusion pressure during mechanical cardiopulmonary resuscitation in porcine cardiac arrest model. Resuscitation. 2017;113:101–107. [DOI] [PubMed] [Google Scholar]
- 14.Srinivasan V, Nadkarni VM, Yannopoulos D, et al. Spontaneous gasping decreases intracranial pressure and improves cerebral perfusion in a pig model of ventricular fibrillation. Resuscitation. 2006;69(2):329–334. [DOI] [PubMed] [Google Scholar]
- 15.Debaty G, Labarere J, Frascone RJ, et al. Long-Term Prognostic Value of Gasping During Out-of-Hospital Cardiac Arrest. J Am Coll Cardiol. 2017;70(12):1467–1476. [DOI] [PubMed] [Google Scholar]
- 16.Knor J, Seblova J, Skulec R, Seblova D, Jiri M. The presence of gasping predicts long-term survival in out-of-hospital cardiac arrest patients. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2018;162(1):32–35. [DOI] [PubMed] [Google Scholar]
- 17.Bobrow BJ, Zuercher M, Ewy GA, et al. Gasping during cardiac arrest in humans is frequent and associated with improved survival. Circulation. 2008;118(24):2550–2554. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


