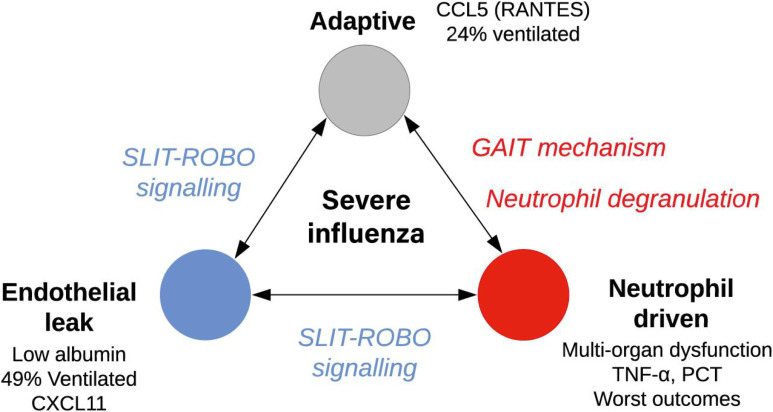
P010 - ARDS Ruler
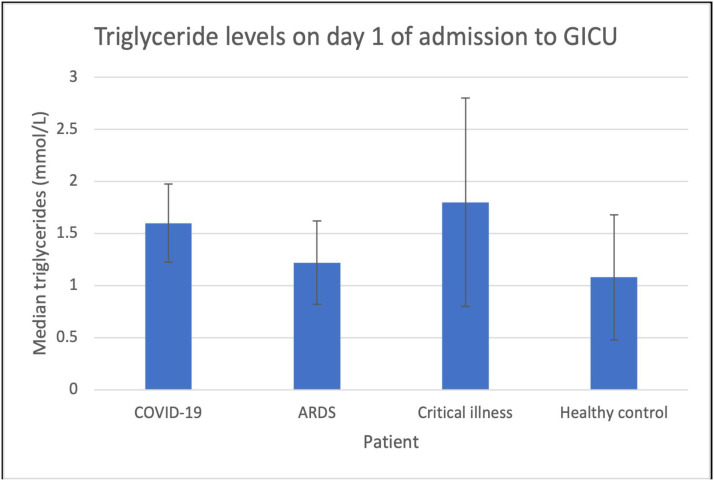
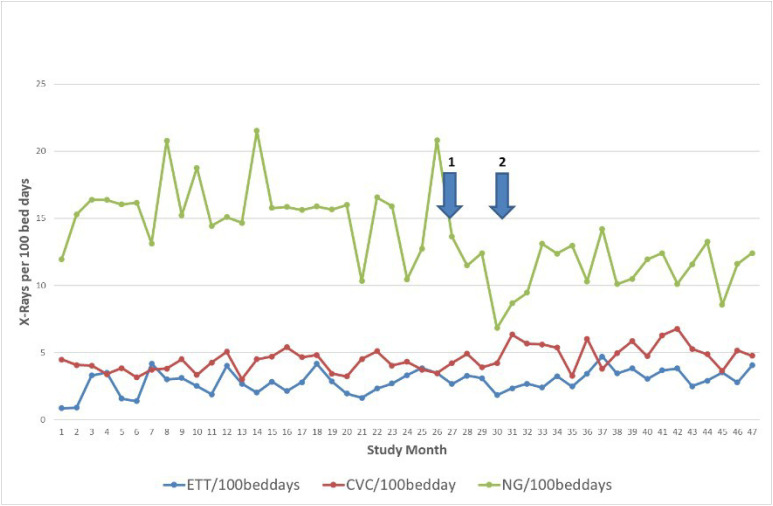
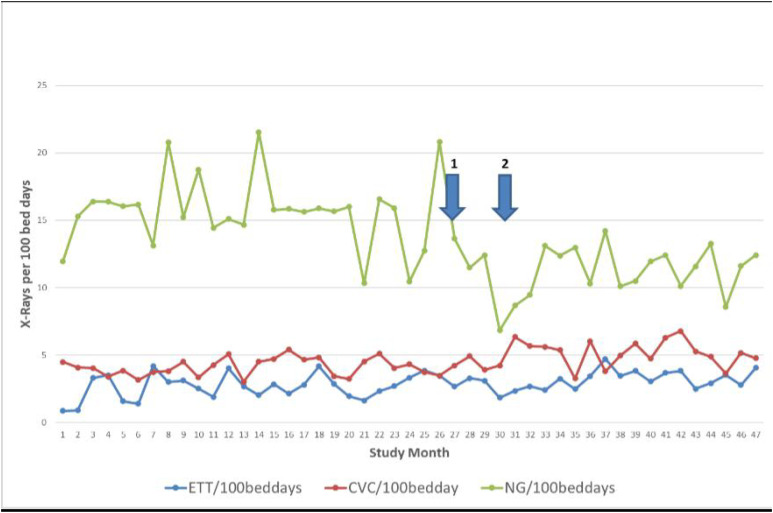
Acute Respiratory Distress Syndrome
Carl Tua1 and Michael Buttigieg 2
1Mater Dei Hospital, Malta
2Mater Dei Hospital
Abstract
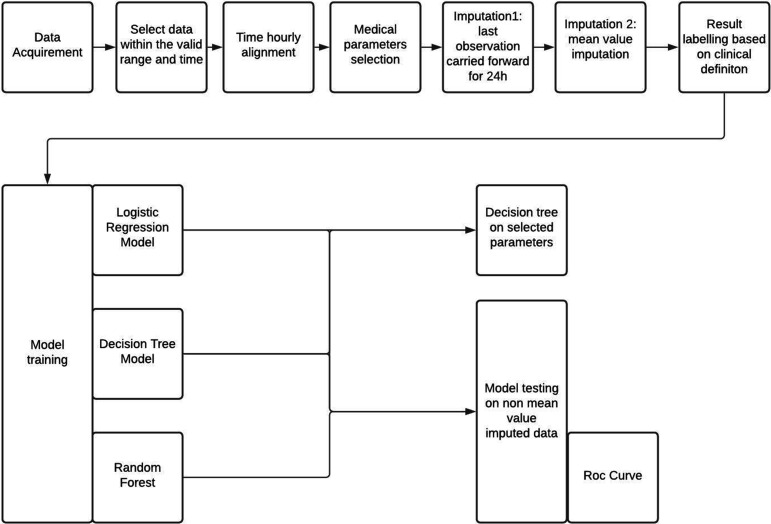
Introduction: Following the publication of the ARDS Network (ARDSnet) trial over two decades ago lung protective ventilation with low tidal volumes has become a mainstay in the evidence based management of acute respiratory distress syndrome (ARDS). The ARDSnet trial protocol uses the Devine formula which is based on height and gender to calculate the predicted body weight (PBW) which is then used to calculate the tidal volume in ml/kg.1-2
The first step to calculating a safe tidal volume is measuring the patient’s height. Visual estimates of patient’s height are often inaccurate and measurements in some patient groups can be challenging. Various methods have been suggested to aid accuracy and ease of measurement. Once the height is known the second step is to use the Devine formula to calculate the PBW. This is often done using online calculators or using tables with height and the PBW. The third and final step is multiplying the PBW by the desired tidal volume in ml/kg typically starting at 6ml/kg.
During the COVID-19 pandemic, the combination of various factors such as greatly increased doctor and nursing workload, use of personal protective equipment (PPE), concerns over the use of reusable equipment such as tape measures and difficult access to online calculators for PBW calculation when donned in PPE in some COVID-19 units made measuring height and calculating a safe tidal volume particularly challenging.3
Objectives: To develop a quick, safe way of calculating lung protective tidal volumes for ARDS patients including in COVID-19 Intensive care units.
Methods: We used the Devine formula to calculate the PBW in males and females at every centimeter (cm) from 152cm to 200cm. Males PBW= 50 + (0.91 × [height in centimeters − 152.4]) Female PBW= 45.5 + (0.91 × [height in centimeters − 152.4]). We then multiplied the PBW by 6 to generate a 6ml/kg PBW tidal volume.
Using image editing software, we then designed gender specific rulers with cm markings to measure height placed beside the corresponding calculated PBW and tidal volume 6ml/kg for that height. We also placed the ARDSnet PEEP/Fio2 titration table. The resulting ruler when printed to scale can then be used as a disposable measuring tape that allows height, PBW and 6ml/kg tidal volume to be calculated easily with one measurement and without the need to resort to calculators, tables or reusable equipment.
Results:
Conclusions: These JPEG images can be downloaded and printed to scale. Once printed the ARDS ‘rulers‘ allow easy and quick measurement of height, PBW and 6ml/kg tidal volume with one measurement without resorting to calculators or tables. As they are simply printed on standard paper, they are single use and therefore do not pose an infection control risk.
References
1. Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-1308.
2. Pai MP, Paloucek FP. The origin of the "ideal" body weight equations. Ann Pharmacother. 2000;34(9):1066-1069. Martin, D.C., Richards, G.N. Predicted body weight relationships for protective ventilation – unisex proposals from pre-term through to adult. BMC Pulm Med 17, 85 (2017).
3. Freitag E, Edgecombe G, Baldwin I, Cottier B, Heland M. Determination of body weight and height measurement for critically ill patients admitted to the intensive care unit: A quality improvement project. Aust Crit Care. 2010;23(4):197-207
P011
Lung protective and acute respiratory distress syndrome ventilation strategies in the age of COVID19
Acute Respiratory Distress Syndrome
Ben Deeming and Sophie Selley
HENE
Abstract
Introduction: The global COVID pandemic has led to an increase in UK intensive care unit (ICU) admissions requiring invasive mechanical ventilation (IMV) for severe acute respiratory distress syndrome (ARDS). Whilst the optimal management strategies of COVID ARDS are still the topic of research and debate, existing ARDS guidelines1 provide a framework for best practice. The University Hospital of North Durham (UHND) ICU is a 10 bed combined critical care unit which, during the pandemic, cared for significantly more patients requiring IMV for ARDS. We set out to quantify the number of patients requiring IMV and assess the number of these patients receiving optimal ARDS treatments based on the existing ARDS guidelines.1
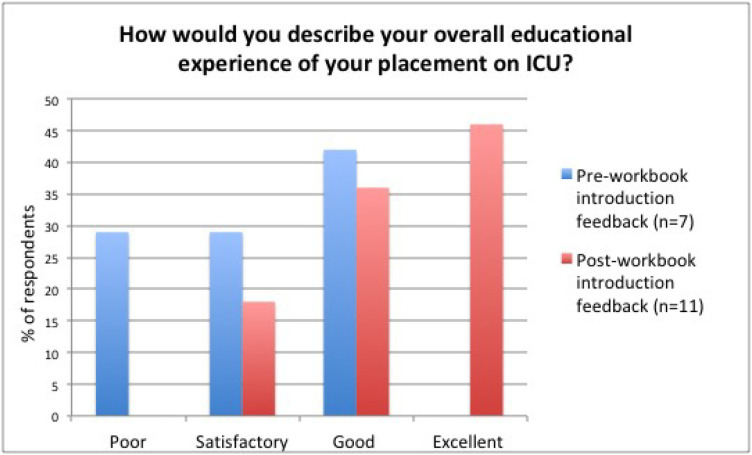
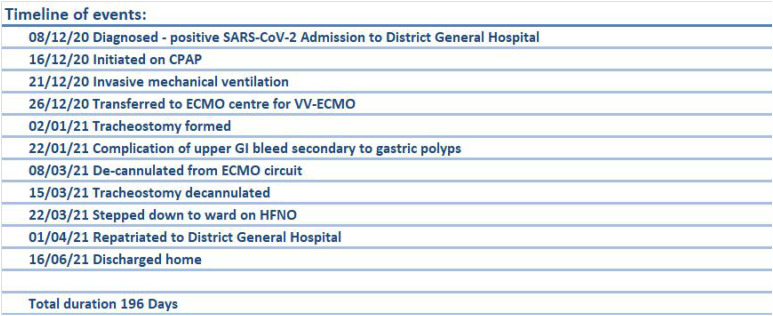
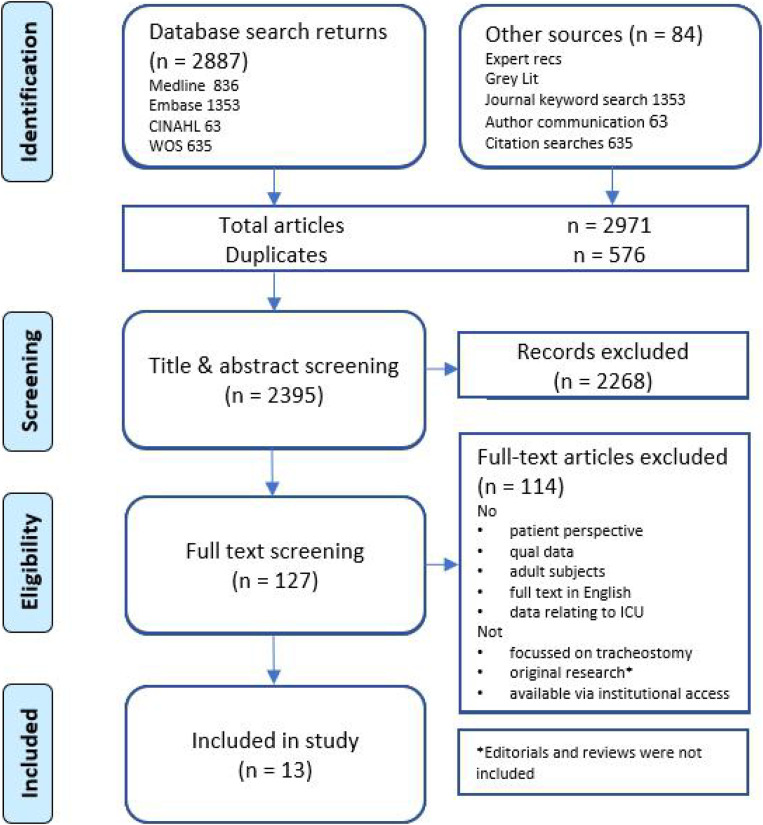
Figure 1.
Male and female ARDS Rulers. Height (cm), PBW (kg) and Tidal volume (6ml/kg) can be read from left to right.
Objectives: Assess performance against best practice guidelines for ventilation in ARDS with standards of 100% of ventilated patients having weight, ideal body weight (IBW), demispans and target tidal volumes documented, ARDS identified and delivered tidal volumes <8ml/kg.
Methods: Prospective case review with inclusion criteria of adult (>18) patients admitted to UHND ICU in January 2021 requiring IMV for any indication. A range of clinical data was collected including arterial blood gas results, ventilator settings and treatments instigated.
Results: 40 patients underwent IMV during the audit, a 250% increase on similar period in 2017, with a mean age of 53. Respiratory failure was the primary indication for ventilation in 48% of which 84% was secondary to COVID. The average length of ventilation and stay was 4.9 days and 7.5 days respectively. Clear documentation of data relevant to ARDS ventilation was poor. 68% of patients had documented weight, 0% an IBW, 5% demispans and 25% target tidal volume.
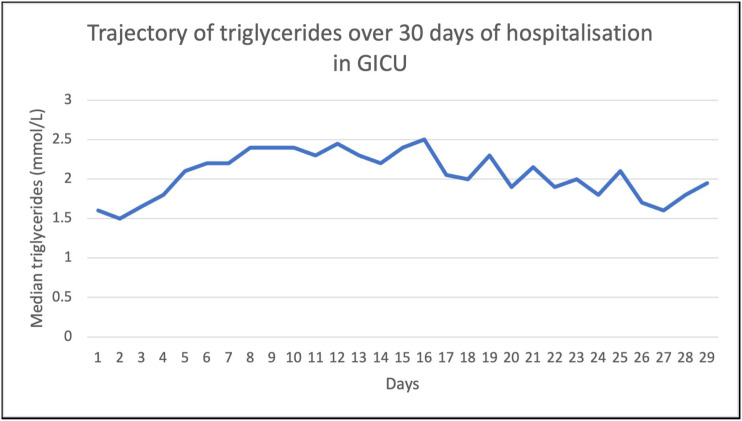
63% fulfilled criteria for ARDS by the Berlin definition,2 44% of these ‘severe’. Only 20% had ARDS documented as a clinical problem. Despite this the majority (88%) had appropriate delivered tidal volumes (6-8ml/kg) with an average delivered tidal volume of 7.4ml/kg. Recommended ARDS ventilation strategies, depending on severity, were used largely appropriately with 52% of ARDS patients having high positive end-expiratory pressure (PEEP), 76% paralysed and 48% proned. None were referred for extra-corporeal membrane oxygenation (ECMO).
ARDS patients without a label of ARDS (‘missed ARDS’) demonstrated less conformance to guidelines than those with positively ‘identified ARDS’, with less paralysis and proning across both moderate and severe cases and two patients receiving inappropriately high tidal volumes (>8ml/kg).
Conclusions: Despite a significant increase in workload from the pandemic and perhaps consequently less complete documentation, the vast majority of patients with ARDS received appropriate lung protective ventilation. However, there is poor labelling of patients with ARDS, which this audit may suggest leads to those patients being less likely to receive ARDS treatments such as paralysis and proning, emphasising the importance of identification of ARDS. We suggest improvements in documentation could be made with proformas for ventilated patients prompting IBW and target tidal volume calculation, as well as serial PF ratios to identify and stratify patients with ARDS, serving as a prompt for consideration of paralysis, proning or ECMO referral.
References
1. Faculty of Intensive Care Medicine. Guidelines on the Management of Acute Respiratory Distress Syndrome (2018). Available from: https://www.ficm.ac.uk/sites/default/files/ficm_ics_ards_guideline_-_july_2018.pdf [Accessed 20th July 2021]
2. The ARDS Definition Task Force. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA. 2012;307(23):2526-2533
P012
Natural History and Trajectory of non-COVID-19 Acute Respiratory Distress Syndrome patients. An observational study for comparison to COVID-19 populations.
Connor Toal 1 , Alex Fowler2, Brijesh Patel3, Zudin Puthucheary1 and John Prowle1
1William Harvey Research Institute, Queen Mary University of London
2William Harvey Research Institute, Queen Mary University of London
3Division of Anaesthetics, Pain Medicine & Intensive Care, Department of Surgery & Cancer, Faculty of Medicine, Imperial College London, London, UK
Abstract
Introduction: Previous studies on acute respiratory distress syndrome (ARDS) relate trajectories to initial degree of hypoxia1,2 Further work is required to deduce whether previous ARDS frameworks are applicable to COVID-19 ARDS patients.
Objectives: How does hypoxia progression influence outcomes in non-COVID ARDS patients and does this differ from COVID-19 ARDS patients?
Methods: Mechanically ventilated patients that met the Berlin ARDS Criteria1 were selected from the Medical Information Mart for Intensive Care (MIMIC) database.3 Daily blood gas and ventilatory settings were analysed, from the point of intubation to death or discharge, allowing longitudinal analysis with high granularity. Our primary outcome was how the trajectory of patients was dependent on their hypoxia progression. Secondary outcomes included how base characteristics and initial clinical parameters affect trajectory and outcomes. Comparative analysis was performed between the results of this study and a previous large COVID-19 ARDS study4
Results: 1,575 ICU admissions were included in the study. All results report this study first followed by the COVID-19 study.4 Overall survival rate was higher (70.2% vs 57.7%); less patients had initial moderate or severe hypoxia (54.5% vs 76.8%); less patients had worsening of hypoxia over the first 7 days (18.9% vs 31.8%); and more patients improved their hypoxia status (33.1% vs 23.5%).
This study showed a smaller proportion of hypoxia non-resolvers compared to the COVID study (32.6% vs 57.9%). However, non-resolvers in the two studies had similar survival rates (58.6% vs 60.4%). Length of ICU stay (LOS) and duration of invasive mechanical ventilation (IMV) was significantly less in this study compared to the COVID-19 study regardless of hypoxia resolver status.
Conclusions: Non-COVID ARDS patients have a more predictable natural history and trajectory compared to COVID-19 ARDs patients. Respiratory failure occurs less frequently and is quicker to resolve, resulting in a lower proportion of hypoxia non-resolvers. However hypoxia non-resolvers of both populations have similar survival outcomes. Despite this, COVID ARDS patient have much longer ICU length of stay and length of ventilation which has significant implications for provision of critical care resources. Further analysis of the impact of COVID-19 therapies on these outcomes is needed.
References
1. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: The Berlin definition. JAMA - J Am Med Assoc [Internet]. 2012;307(23):2526–2533. Available from: https://jamanetwork.com/journals/jama/fullarticle/1160659
2. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA [Internet]. 2016;315(8):788–800. Available from: https://jamanetwork.com/journals/jama/fullarticle/2492877
3. Johnson, A., Bulgarelli, L., Pollard, T., Horng, S., Celi, L. A., and Mark R. MIMIC-IV (version 1.0). PhysioNet. 2021.
4. Patel B V., Haar S, Handslip R, Auepanwiriyakul C, Lee TM-L, Patel S, et al. Natural history, trajectory, and management of mechanically ventilated COVID-19 patients in the United Kingdom. Intensive Care Med [Internet]. 2021;47(5):549–565. Available from: /pmc/articles/PMC8111053/
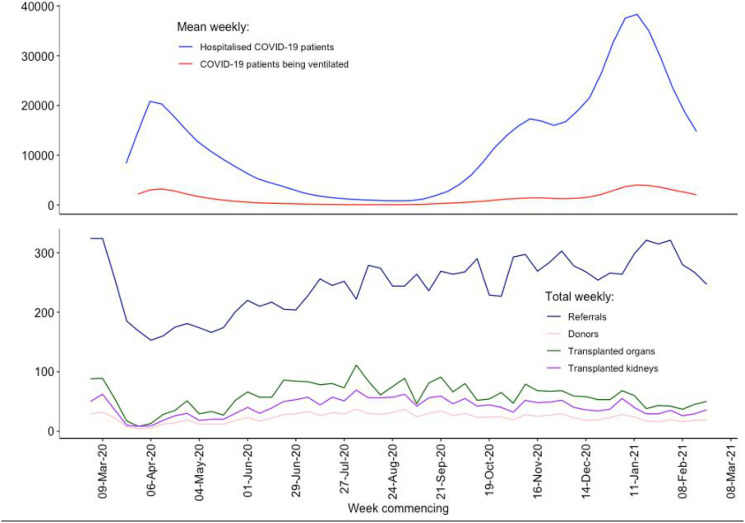
P014
Evaluation of neutrophil microvesicles function in a novel tri-culture model of pulmonary vascular inflammation
Eirini Sachouli, Diianeira Maria Tsiridou, Claudia Peinador Marin, Masao Takata, Anthony C. Gordon and Kieran P. O’Dea
Division of Anaesthetics, Pain Medicine and Intensive Care, Imperial College London, Chelsea and Westminster Hospital, London, UK
Abstract
Introduction: Microvesicles (MVs) are cell-derived membrane-encapsulated particles carrying functional molecular cargo and surface markers derived from their parental cells. Within blood, increased levels of circulating neutrophil-derived microvesicles (N-MVs) are associated with clinical severity in sepsis and severe burns injury patients suggesting potential as biomarkers and mediators of organ injury.1,2 We previously found a dramatic increase of circulating MVs uptake within the pulmonary vasculature by lung-marginated monocytes in a mouse model of endotoxemia.3 As a major site for accumulation of inflammatory cells during sepsis, uptake of N-MVs within pulmonary vascular microenvironment could influence inflammatory processes contributing to indirect acute lung injury.
Objectives: To determine N-MVs target cell-specific interactions and functions within the pulmonary vascular microenvironment by developing an in vitro monocyte-neutrophil-endothelial cell ‘tri-culture’ model of inflammation.
Methods: Neutrophils and peripheral blood mononuclear cells (PBMCs) were isolated from healthy volunteer blood by density gradient centrifugation, and monocytes from PBMCs by negative immunomagnetic bead selection (Miltenyi). N-MVs were generated by fMLP stimulation of isolated neutrophils. For establishing the tri-culture model, confluent human lung microvascular endothelial cells were pre-treated with low-dose tumour necrosis factor (TNF) to promote uniform leukocyte adherence. After renewal of media, neutrophils and monocytes were added to endothelial cells, allowed to adhere and then incubated with N-MVs for 3hrs. Expression of neutrophil and monocyte activation markers, and generation of neutrophil extracellular traps (NETs) were evaluated via flow cytometry. Production of soluble TNF was measured by ELISA. For uptake experiments, N-MVs were labelled with CFSE fluorescent dye, and cell-associated fluorescence was quantified by flow cytometry.
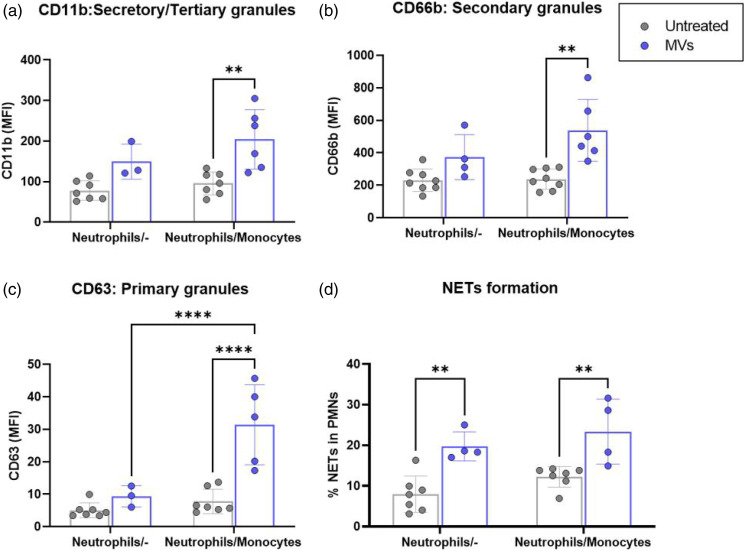
Results: Addition of N-MVs to tri-cultures resulted in significant upregulation of surface activation markers on neutrophils: the tertiary and secretory granule marker, CD11b (Figure 1(a)); the secondary granule marker, CD66b (Figure 1(b)); and the primary granule marker, CD63 (Figure 1(c)). These responses were reduced in the absence of monocytes. By contrast, N-MVs induced increased levels of NETs (Figure 1(d): myeloperoxidase/Sytox-green positive events) independently of monocytes. Monocyte activation by N-MVs was indicated by increased expression of tissue factor compared to untreated controls (MFI: 149.0±23.6 vs. 7.106±2.78, p<0.0001) and production of TNF in tri-culture supernatant (285.4±171.6 vs 1.98±1.64 pg/mL, p<0.01). Lastly, we demonstrated uptake of CFSE-labelled N-MVs by both neutrophils (MFI: 34.5±13.7) and monocytes (MFI: 197.0±177.0). Interestingly, the addition of a blocking anti-CD18 antibody significantly reduced uptake by neutrophils (MFI: 16.6±7.2, p < 0.05), but not by monocytes.
Figure 1.
N-MVs activation of neutrophilis is dependent (a-c) or the presence of monocytes (d). Flow Cytometric values of neutrophil surface activation markers refers to as mean of fluorescence intensity (MFI).The formation of NETs was assessed as the percentage of neutrophils(%) that co-express myleperoxidase (MPO) and Sytox-Green. Data expressed as mean with ± SD and analysed with Two-Way ANOVA with Turkey’s multiple comparison test. n = 3–7, **p<0.01, ****p<0.001. The blue dots represent the addition of N-MVs while grey are the untreated controlls.
Conclusions: We developed a physiologically-relevant tri-culture model to study inflammatory crosstalk between N-MVs with myeloid leukocytes sequestered within pulmonary vasculature during sepsis. We demonstrated that N-MVs are likely taken up by both marginated monocytes and neutrophils within the pulmonary vasculature, and that they are capable of producing significant activation of marginated neutrophils, indirectly via monocyte-dependent mechanisms or directly via induction of NETs. Our results suggest a central role for circulating N-MVs as a strong mediator of acute intravascular inflammation within the lungs, leading ultimately to pulmonary endothelial dysfunction and development of indirect acute lung injury.
Acknowledgements: Funded by NIHR Research Professorship (RP-2015-06-18) and the Chelsea & Westminster Health Charity.
References
1. O’Dea KP, Porter JR, Tirlapur N, Katbeh U, Singh S, Handy JM, Takata M. Circulating microvesicles are elevated acutely following major burns injury and associated with clinical severity. PloS One. 2016;11(12):e0167801.
2. Nieuwland R, Berckmans RJ, McGregor S, Böing AN, Th M. Romijn FP, Westendorp RG, Hack CE, Sturk A. Cellular origin and procoagulant properties of microparticles in meningococcal sepsis. Blood, The Journal of the American Society of Hematology. 2000;95(3):930-935.
3. O’Dea KP, Tan YY, Shah S, V Patel B, C Tatham K, Wilson MR, Soni S, Takata M. Monocytes mediate homing of circulating microvesicles to the pulmonary vasculature during low-grade systemic inflammation. Journal of extracellular vesicles. 2020;9(1):1706708.
P015
Outcome of prophylactic noninvasive ventilation following planned extubation in high-risk patients: A two year prospective observational study
Adult & Paediatric critical care in low and middle-income countries
Supradip Ghosh1 and Ashutosh Meena 2
1Fortis Escorts Healthcare and Reasearch Centre, Faridabad, Haryana, India
2Imperial Healthcare NHS trust
Abstract
Introduction: Extubation failure (EF) in high risk mechanically ventilated patients is as high as 20-25%,1,2 resulting in increased morbidity, mortality and length of hospital stay. It is more relevant in times of global health pandemic that we look out for the strategies which can potentially reduce the burden on healthcare system. Prophylactic use of Non-Invasive ventilation (NIV) is recommended following extubation in patients at high risk of EF. Most studies2,4 so far have addressed the issue of prophylactic NIV use in setting of Randomized control trials. Therefore, we conducted a prospective cohort study in a real-world scenario looking for the overall impact of prophylactic NIV in patients at high risk of EF.
Objective: Evaluate risk factors and outcome associated with EF in the selected population group.
Material and Method: Consecutive adult patients (≥18 years) admitted in the mixed intensive care unit (ICU) of a tertiary care centre, between January 2018 and December 2019, who passed a spontaneous breathing trial (SBT) following at least 12 hours of invasive mechanical ventilation and put on prophylactic NIV for being at a high risk of EF, were prospectively followed throughout their hospital stay. Extubation failure (EF) was defined as developing respiratory failure within 72 hours post-extubation requiring reintubation or still requiring NIV support at 72 hours post-extubation.
Results: A total of 85 patients were included in the study. 11.8% of patients had extubation failure at 72 hours with an overall reintubation rate of 10.5%. Higher age (p < 0.05), longer duration of invasive ventilation (p < 0.05), and higher sequential organ failure assessment (SOFA) score at extubation (p < 0.05) were identified as risk factors for extubation failure in univariate analysis. However, in the multivariate analysis, only a higher SOFA score remained statistically significant in forward logistic regression analysis (p < 0.05). We found a clear trend toward worsening organ function score in the extubation failure group in the first 72 hours post-extubation, suggesting extubation failure as a risk factor for organ dysfunction. Cumulative fluid balance was higher both at extubation and in subsequent 3 days postextubation in the failure group, but the differences were not statistically significant. Overall, ICU mortality in the study population was 9.49% and was significantly higher in failure group (50% vs 4%, p < 0.001).
Conclusions: Higher age, longer duration of invasive ventilation, and higher baseline SOFA score at extubation remain risk factors for extubation failure even in this high-risk subset of patients on prophylactic NIV. Extubation failure is associated with the worsening of organ function. A trend toward higher cumulative fluid balance both at extubation and post-extubation, suggests de-resuscitation as a potentially helpful strategy in preventing extubation failure.
References
1. Thille AW, Boissier F, Ben-Ghezala H, Razazi K, Mekontso-Dessap A, Brun-Buisson C, Brochard L. Easily identified at-risk patients for extubation failure may benefit from noninvasive ventilation: a prospective before-after study. Crit Care. 2016;20:48. doi: 10.1186/s13054-016-1228-2. PMID: 26926168; PMCID: PMC4770688.
2. Nava S, Gregoretti C, Fanfulla F, Squadrone E, Grassi M, Carlucci A, Beltrame F, Navalesi P. Noninvasive ventilation to prevent respiratory failure after extubation in high-risk patients. Crit Care Med. 2005;33(11):2465-70. doi: 10.1097/01.ccm.0000186416.44752.72. PMID: 16276167.
3. Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, Navalesi P, Antonelli M, Brozek J, Conti G, Ferrer M, Guntupalli K, Jaber S, Keenan S, Mancebo J, Mehta S; Members Of The Steering Committee; Raoof S Members Of The Task Force. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426. doi: 10.1183/13993003.02426-2016. PMID: 28860265.
4. Ferrer M, Sellarés J, Valencia M, Carrillo A, Gonzalez G, Badia JR, Nicolas JM, Torres A. Non-invasive ventilation after extubation in hypercapnic patients with chronic respiratory disorders: randomised controlled trial. Lancet. 2009 Sep 26;374(9695):1082-8. doi: 10.1016/S0140-6736(09)61038-2. Epub 2009 Aug 12. PMID: 19682735.
P016
A review of re-intubations in a mixed general and neurosciences unit and the development of extubation check list
Airway management
Antony Thomas and Juiliana Hamzah
Salford Royal NHS Foundation Trust
Abstract
Introduction: Patients who require re-intubation are more likely to have prolonged ICU stays and to die in critical care.1 This may be a particular problem in patients with neurological disease.2
Objectives: To review the electronic intubation records in a mixed general and neurosciences unit to identify reintubations in critical care. To identify patient factors and risk factors associated with re-intubations and to use this information to improve patient care.
Methods: All intubations are recorded using a structured note on our unit. The records between January 2019 and November 2020 were reviewed together with the patients’ other electronic records. The numbers of critical care intubations per patient were calculated and the reasons for re-intubation were classified. Chi-squared tests were used to compare categorical data.
Results: There were 3657 admissions for 3164 patients admitted in the study period. 367 (12%) died on the unit and 1525 (48%) had a neurological diagnosis. The mean APACHE 2 score was 11 (SD 6). We identified 455 intubations in 342 patients. Of these 342 patients, 81 (23%) had more than one intubation in critical care (2=53, 3=24, 4=4). Of the 261 patients with single intubation, 81 died (31%) and 136 (52%) had a neurological disease of which 34 (25%) died. The corresponding figures for the 81 patients with multiple intubations were 24 deaths (30%), 39 (48%) had a neurological diagnosis of whom 8 died (21%). None of these findings was significantly different between the single and multiple intubation groups. 154 of the first intubations in critical care were documented as reintubations, having had their primary intubations prior to admission. This gave a total of 256 reintubations (56% of all intubations). Of the reasons for reintubation, 181 (70%) had had a failed trial of extubation (33 of these had signs of laryngeal oedema (27 or 82% female)), 52 had had a tube obstruction or leak and only 10 had self-extubated.
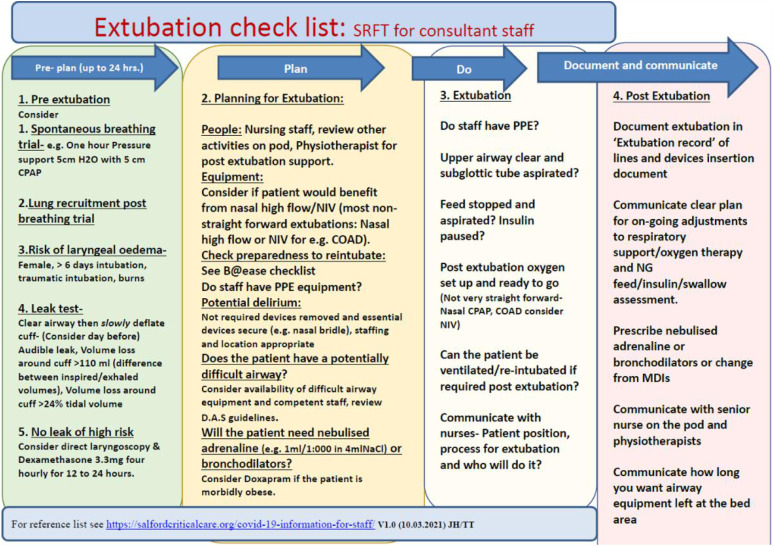
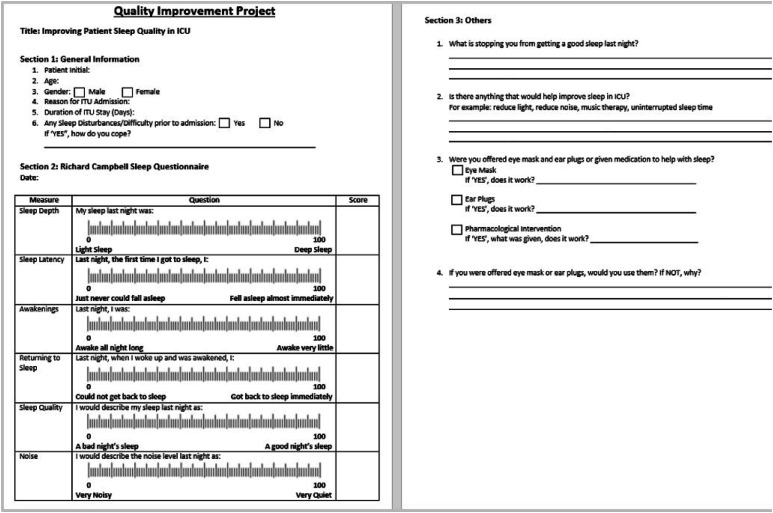
Conclusions: On our unit, there was no difference in the mortality or the number of patients with a neurological diagnosis between patients who had had one or more than one intubation on the unit. Over half of all the intubations on our unit were reintubations, most were associated with trials of extubation. To address this problem, we produced a checklist to facilitate best practices around trials of extubation. This is shown in Figure 1.3
Figure 1.
■■■.
References
1. Frutos-Vivar F, Esteban A, Apezteguia C, et al. Outcome of reintubated patients after scheduled extubation. J Crit Care. 2011;26(5):502–509.
2. Godet T, Chabanne R, Marin J, et al. Extubation Failure in Brain-injured Patients. Anesthesiology. 2017;126(1):104–114.
P017
Accidental tooth ingestion in the Intensive Care Unit
Airway management
Yap Suhao 1 and Lynn Yeo2
1Ministry of Health Holdings
2National Healthcare Group
Abstract
Introduction: Dislodgement of teeth is not uncommon in anaesthesia and intensive care. This is usually due to airway manipulation during intubation for surgical procedures or resuscitation. Many patients have risks factors for dislodgement of teeth, such as pre-existing dental pathology, poor dentition, restorative dental work and features of a difficult airway.
Objective: To emphasize the importance of dental assessment and maintenance of oral hygiene in the ICU.
Methods: A 67-year-old man, known to have poor dentition and loose teeth, was emergently intubated for low conscious level due to subdural haematoma with mass effect. He underwent burrhole surgery for decompression but remained intubated as he developed pneumocephalus and conscious state did not improve. His upper incisor was noted to be dislodged, 2 days after admission to the Intensive Care Unit (ICU). A search began--direct laryngoscopy, chest X-ray and abdominal X-ray were performed and there was a 1cm calcific density projected over the left abdomen, likely the dislodged tooth. He did not present with any abdominal symptoms of intestinal obstruction or perforation and it was assumed that the tooth had been egested uneventfully after a few days.

Results: Dislodgement of loose teeth or dental prostheses can occur without any signs or symptoms in the critically ill patient. These patients may have low conscious levels or are sedated and intubated so they are not able to communicate to the nursing staff that dislodgement has occurred. If loose teeth or dental prostheses that have been aspirated into the tracheo-bronchial tree chronic lung infections, asthmatic symptoms, lung collapse or lung abscess can develop. These need to be identified and removed as soon as possible, usually be flexible or rigid bronchoscopy as they serve as a nidus of infection. Rarely, open thoracotomy may be required for removal. If the loose teeth are ingested, it typically passes through the digestive system and is expelled in the stool. However, swallowed dentures may lead to hollow viscus necrosis, perforation, fistulae formation, bleeding and obstruction.
In our ICU, there is at least once daily oral toileting for all patients. This is performed more frequently for patients who are on nasogastric feeding or are unconscious. Oral toileting can be done by one of the 2 methods--using a disposable pre-prepared oral swab stick with sodium bicarbonate or with swabs soaked with chlorhexidine 0.2% mouth wash. Any nursing staff can easily carry out this procedure and it includes simple daily inspection for loose teeth, sores, ulcers or thrush.
Conclusion: In the critically ill patient, in whom there are many medical issues to sort out, it is still important to care for the dental health of the patient, to avoid further complications. Basic dental assessment should be performed routinely and regularly by nursing staff, as soon as the patient is stabilized. Adequate training and oral care protocols should be in place. Loose teeth or dental prosthesis should involve a dentist for evaluation and removal.
References
1. Abidia RF. Oral Care in the Intensive Care Unit: A Review. J Contemp Dent Pract 2007;8(1): 076-082.
2. N Yokoo, A Igarashi, M Sato, M Nakane, K Kawamae. Importance of dental assessment in the intensive care unit: two cases of accidental metal crown migration detected by daily routine chest roentgenograms Yamagata Med J 2014: 32(1): 36-39
3. Gachabayov M, Isaev M, Orujova L, Isaev E, Yaskin E, Neronov D. Swallowed dentures: Two cases and a review. Ann Med Surg (Lond). 2015;4(4):407-413.
4. L Abeysundara, A Creedon, D Soltanifar. Dental knowledge for anaesthetists, BJA Education 2016 16(11): Pages 362–368
5. Khoo Teck Puat Hospital guidelines. (2020). Work Instruction for Oral Hygiene SWI-NURS/INPT-01-03-01
P019
Life-threatening tracheobronchial obstruction with blood clot, managed using whole endotracheal tube suction
Airway management
Neil Roberts, Barney Scrace, Venkat Reddy and Nick Marshall
Royal Cornwall Hospitals NHS Trust
Abstract
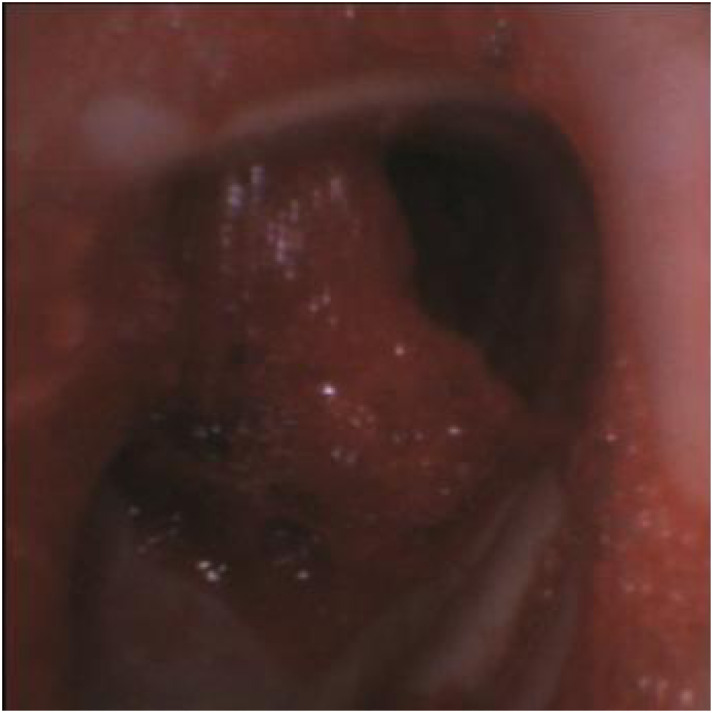
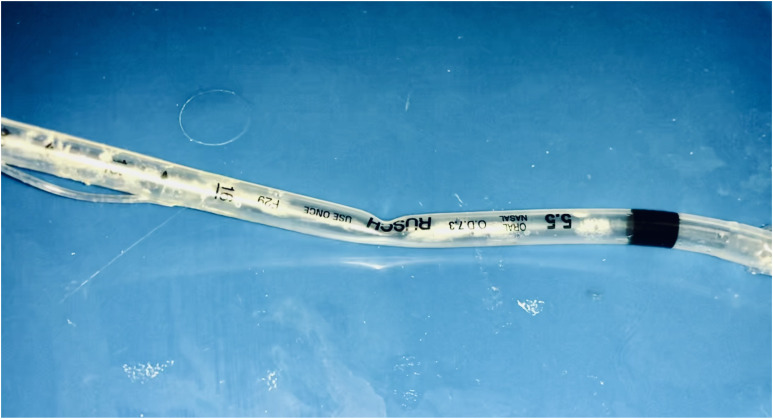
Introduction: Tracheobronchial obstruction due to blood clot after mucosal injury is a rare complication of tracheal instrumentation which may occur during airway surgery (eg tracheostomy), or during a minor procedure such as use of a bougie at intubation. This situation poses several challenges, including potential ongoing bleeding, obstruction of both distal and proximal airways, ball-valve behaviour, and the potential for complete airway occlusion at any stage with subsequent failure of ventilation. We present a case of life-threatening tracheal clot (Image 1) following bougie-facilitated tracheal intubation for a patient undergoing incision and drainage of an abscess.
Image 1.
View of obstructing tracheal clot on fibreoptic bronchoscopy.
Objectives: To describe a novel, life-saving management option for tracheobronchial clot, in the context of previous research.
Methods: A literature search was performed on Pubmed and GoogleScholar using search terms ‘tracheal/tracheobronchial’ ‘obstruction’ ‘blood clot’ ‘mucus plug’ ‘suction’. The authors reviewed this in context of a recent emergency case.
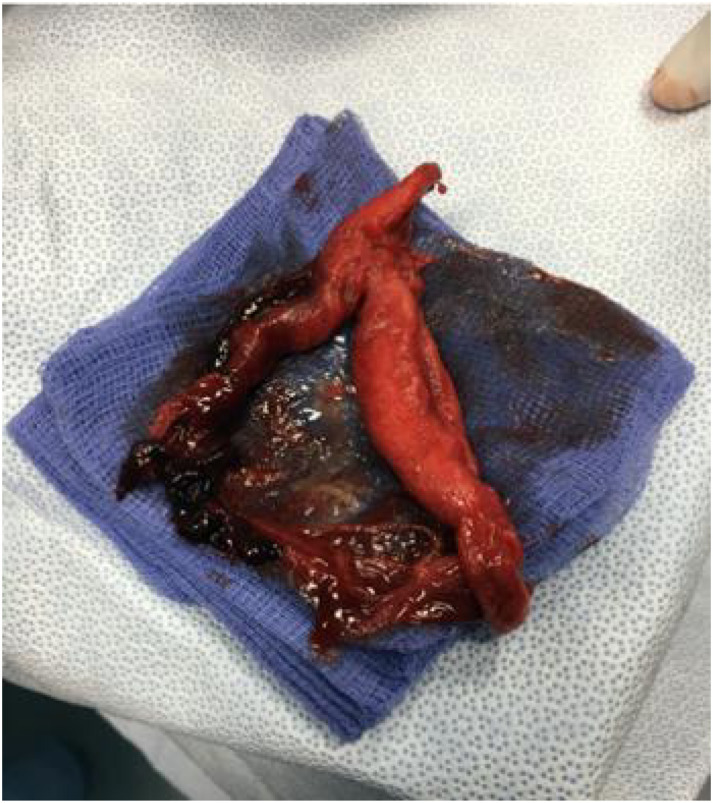
Results: There are several case reports of emergency management of tracheobronchial obstruction, usually either bleeding due to airway injury (for example at tracheostomy), or from large mucus plugs. Most are removable using standard suction catheters, or using suction via fibreoptic bronchoscopy. If this is unsuccessful, rigid bronchoscopy and optical grasping forceps may be indicated. Should all these tactics fail, as in this case, the endotracheal tube may be advanced onto the clot under fibreoptic vision, then connected directly to the suction and removed – along with the complete clot (Image 2).
Image 2.
Clot once retrieved using endotracheal tube as suction device.
Conclusions: The use of whole endotracheal tube suction in life-threatening tracheobronchial clot is a simple technique using standard kit available in all anaesthetic rooms, and may save lives where standard rescue methods fail.
References
1. ■■■
P020
Why can’t we purchase kidneys? A ethical review of presumed consent organ donation compared against a regulated organ marketplace.
Brain death, organ donation and transplantation
Jennifer Lewis
Guys and St Thomas’ NHS Foundation Trust
Abstract
Introduction: For those living with certain life limiting diseases, an organ transplant is the only option to return to normalcy and a life free of intensive medical investigation and treatment. The demand for organs, notably kidneys is growing internationally and far outstrips the supply available through either deceased or living donors.1 England has recently moved to a presumed consent model for organ donation in part to increase the number of organs available for transplant.2
Objectives: The objective of this research was to examine the likely impact a presumed consent model of organ donation will have on organ donation rates within England. A particular focus was placed on the ethical arguments for an against a model of this type. Alternative organ donation models are possible, a review of the controversial idea of selling organs has also been examined.3,4 The ethics concerning altruism, autonomy and the interplay between economic and health benefits from a utilitarian and Kantian viewpoint will be considered.3,4,5
Methods: This review has been conducted using sources from both medical and philosophical literature.
Results/Conclusion: The presumed consent model of organ donation is unlikely to make a difference to the number of transplants conducted in England.3 Although its efficacy as a project cannot be exclusively measured in terms of successful organ donation. The engagement of key stakeholders and importantly the general public in the discourse surrounding organ donation is vital, a change in organ donation law should initiate this process. In comparison the controversial idea of selling organs is a more efficacious way of increasing the number of organs available for donation. A black-market for organs (which currently exists in many countries) violates human rights, allows for exploitation and the undermines the sanctity of human life,4 however commercialisation does not necessarily result in exploitation if the marketplace is carefully controlled and governed. The review will conclude with a proposal for an independent regulator for the sale of organs, which will be both transparent, economically viable and ultimately save more lives.
References
1. World Health Organization. Global status report on noncommunicable diseases 2014: World Health Organization; 2014.
2. NHS Blood and Transplant. What can you donate? https://www.organdonation.nhs.uk/helping-you-to-decide/about-organ-donation/what-can-you-donate/n.d
3. Cohen C. The case for presumed consent to transplant human organs after death. Transplant Proc. 1992;24(5):2168-2172.
4. Orentlicher D. Financial incentives for organ procurement: Ethical aspects of future contracts for cadaveric donors. Archives of Internal Medicine. 1995;155(6):581-589.
5. Alpinar-Sencan Z. Reconsidering Kantian arguments against organ selling. Medicine, health care, and philosophy. 2016;19(1):21-31.
P021
Cause of death and consent rates during the COVID-19 pandemic
Brain death, organ donation and transplantation
Nicholas Plummer 1 , Harry Alcock 1 , Susanna Madden2, Alex Manara2, Dan Harvey2, Dale Gardiner2
1Nottingham University Hospitals NHS Trust
2NHS Blood and Transplant
Abstract
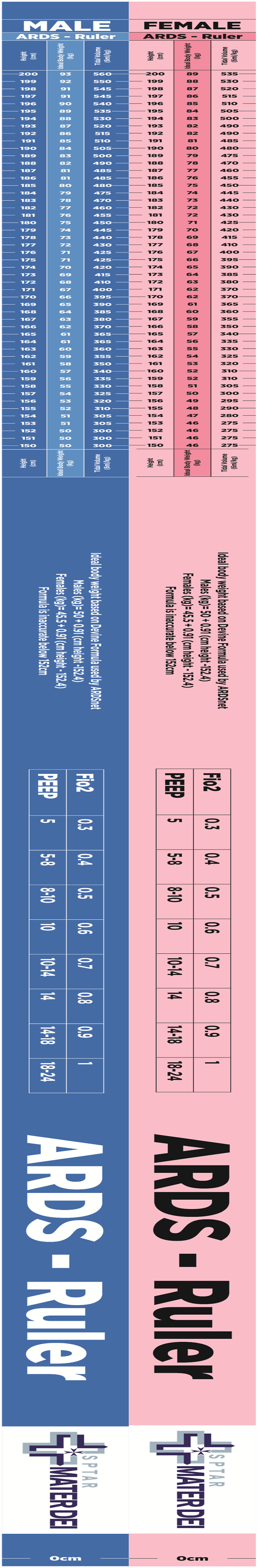
Introduction: The COVID-19 pandemic of 2020-21 impacted all aspects of the UK health service. Organ donation acceptance criteria were initially revised to safeguard critical care resources, and prioritised younger donors and donation after brain death (DBD) over donation after circulatory death (DCD).1 These were later returned to the original criteria prior to the “second wave” in September 2020; yet referrals and donation numbers remained below pre-pandemic levels throughout 2020. This data was further confounded by England changing from an opt-in model to presumed consent for donation.2
Objectives: We aimed to assess the impact of the COVID-19 pandemic on causes of death, and the subsequent effect on numbers of potential donors, referral rates (adjusted for the altered referral criteria during the first wave), and consent rates for donation.
Methods: Mortality, referral, and consent rate data were acquired from the Potential Donor Audit (PDA) database held by NHS Blood and Transplant. The two pandemic “waves” (defined as 11/3/2020-10/08/2020 and 11/08/2020-10/03/2021) were compared to their corresponding periods from 2019-20. Event counts were compared using exact Poisson tests, and proportions using two-sample z-tests.
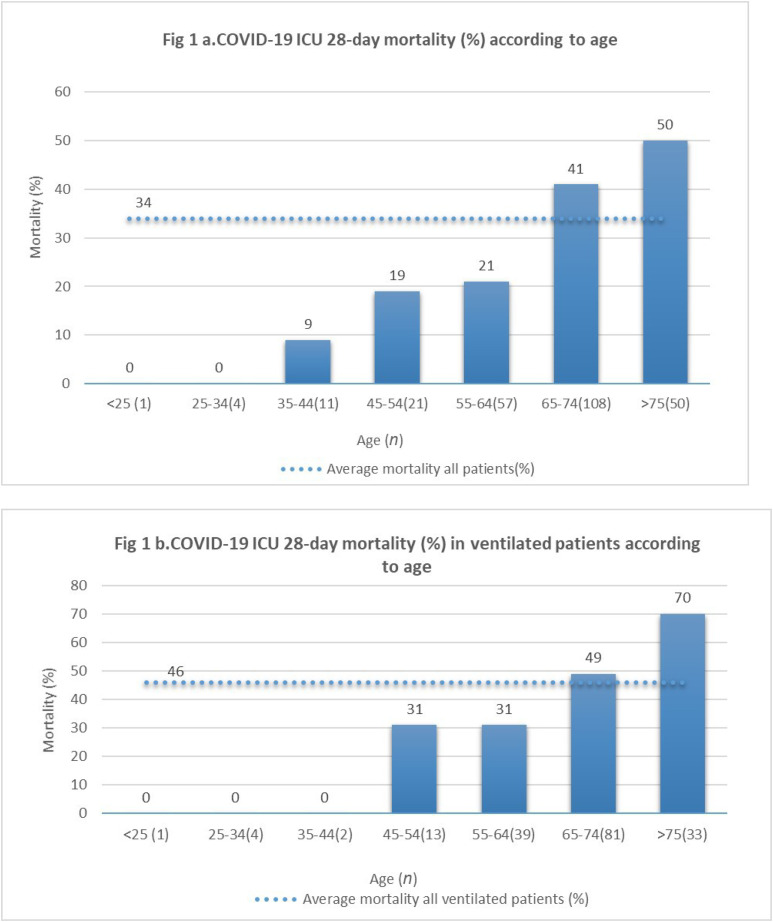
Results:
All-cause mortality was higher during both “waves” (p<0.001) than the previous year, with excess in-ICU non-COVID-19 mortality during the second wave (p=0.024, see figure). Mortality from cardiac arrest (p<0.001), catastrophic brain injury (p<0.001), and head trauma (p=0.280) were reduced in both waves, and deaths in ICU from suicide and self-harm were reduced in the second wave (p=0.002).
After accounting for COVID-19 positive patients and those outside of the adjusted age-criteria, there was no difference in referral rates for potential DBD patients (99% in all cases) but fewer DCD patients meeting criteria were referred during both waves (89% vs 93%, p=0.003, and 85% vs 92%, p<0.001).
There were fewer eligible donors during both waves (p<0.001). Fewer eligible families were approached during the first wave (42% vs 58%, p<0.001) but more were approached during the second (58% vs 54%, p=0.001) than in the preceding twelve months. There was no significant difference in Specialist Nurse in Organ Donation (SNOD) presence during approaches, nor family consent rates. Additionally, there was no difference in the proportion of patients who subsequently went on to donate.
Conclusions: The reduction in donations – and hence transplantation – during the COVID-19 pandemic was multifactorial. There was a significant reduction in causes of mortality that are most associated with donation, likely driven by an increased number of deaths in the community who never ‘made it’ to hospital. Potential DCDs were referred less frequently during both waves, although this was secondary to the change in acceptance criteria during the first wave. Additionally, fewer eligible families were approached during the first wave, further reducing donation potential.
Despite fewer eligible donors, consent rates, the relationship between SNOD presence and consent, and progression to donation remained unchanged, suggesting that the foundations underpinning the organ donation programme remained resilient.
Future work should focus on validating factors predicting family consent3 in the context of COVID-19 and assessing the ongoing impact of presumed consent.
References
1. NHS Blood and Transplant. COVID-19 Planning for Infection Surges. NHS Blood and Transplant; 2021. Accessed August 19, 2021. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/21165/pol301.pdf
2. Gardiner D, McGee A, Shaw D. Two fundamental ethical and legal rules for deceased organ donation. BJA Education. 2021;21(8):292-299. doi:10.1016/j.bjae.2021.03.003
3. Curtis RMK, Manara AR, Madden S, et al. Validation of the factors influencing family consent for organ donation in the UK. Anaesthesia. Online first. doi:10.1111/anae.15485
P022
Organ donation rates during the COVID-19 pandemic: Comparing the approach taken during the first two waves
Brain death, organ donation and transplantation
Nicholas Plummer 1 , Harry Alcock 1 , Susanna Madden2, Alex Manara2, Dan Harvey2 and Dale Gardiner2
1Nottingham University Hospitals NHS Trust
2NHS Blood and Transplant
Abstract
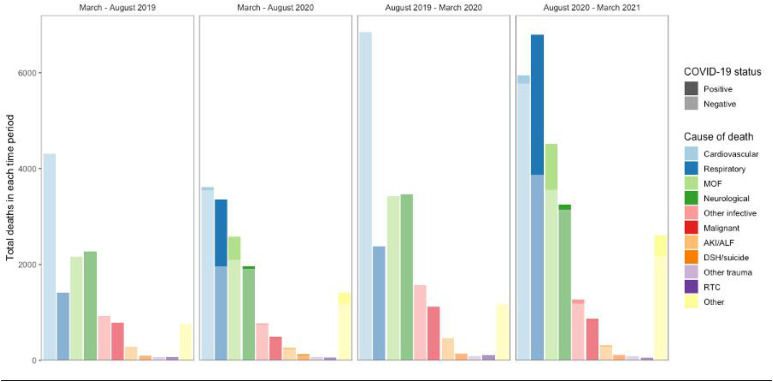
Introduction: In response to the COVID-19 pandemic the many UK transplant units had to close or reduce activity, with deceased donation and transplantation down 80% in March-May 2020. Donor age criteria were reduced in the “first wave” to protect ICU capacity, and donation after brain death (DBD) was prioritised over donation after cardiac death (DCD). From June onwards, an NHSBT recovery plan aimed to reopen programmes, with the aim to return to a position of exploring all eligible donors and reviewing their potential on a case-by-case basis,1 but the ability of such programmes was impacted by a further rise in COVID-19 cases (“second wave”).
Objectives: We aimed to compare the performance of NHSBT referral, donation, and transplantation strategies during the first two “waves” of COVID-19. Wave one was defined as 11/3/20 to 10/8/20, and wave two 11/8/20 to 10/3/21.
Methods: Mortality and transplant data were acquired from the Potential Donor Audit (PDA) and national transplant registries. COVID-19 healthcare utilisation data was acquired via the PHE API. Correlation between features were assessed using Pearson’s product-moment correlation coefficient and means compared using Student’s t-test.
Results:
Weekly referral rates during the first wave were strongly inversely correlated to COVID-19 critical care utilisation (r=-0.82, 95%CI -.93 to -0.60) but moderately positively correlated during the second (r=0.61, 95%CI 0.31 to 0.80). Total transplanted organs were inversely correlated throughout (r=-0.64, 95%CI -0.78 to -0.44) with no difference between waves (p=0.055), although renal transplants were less effected during the second wave (p<0.001).
The mean “transplant gap” (difference between organs retrieved and transplanted) was significantly higher in the second wave (5.9 per week, 95%CI 3.4 to 8.5, p<0.001). The DBD/DCD ratio was significantly lower in the second wave (reduced from 3.3 to 2.0, 95%CI for reduction 0.5-2.1, p=0.001).
Conclusion: Referral rates to NHSBT improved during the second wave, and the ratio of DBD to DCD fell, both reflecting positively on the change of approach taken. Although total organ transplants fell during both waves, this is strongly correlated to critical care utilisation by COVID-19 patients, suggesting an impact on the ability for transplant centres to access critical care resources post-operatively. The relative sparing of renal transplants (who rarely require critical care post-operatively) and increasing transplant gap in the second wave fits with this assessment, although concerns regarding risks of COVID-19 in transplant recipients - especially in renal patients2- during periods of high burden of disease in hospital likely also contributed to reduced transplant rates,3 and the higher transplant gap could additionally be associated with the increase in DCD donation during the second wave.4
References
1. NHS Blood and Transplant. COVID-19 Planning for Infection Surges. NHS Blood and Transplant; 2021. Accessed August 19, 2021. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/21165/pol301.pdf
2. Akalin E, Azzi Y, Bartash R, et al. Covid-19 and Kidney Transplantation. New England Journal of Medicine. 2020;382(25):2475-2477. doi:10.1056/NEJMc2011117
3. Ravanan R, Callaghan CJ, Mumford L, et al. SARS-CoV-2 infection and early mortality of waitlisted and solid organ transplant recipients in England: A national cohort study. Am J Transplant. 2020;20(11):3008-3018. doi:10.1111/ajt.16247
4. Manara AR, Murphy PG, O’Callaghan G. Donation after circulatory death. Br J Anaesth. 2012;108(Suppl 1). 108-121. doi:10.1093/bja/aer357
P023
Retrospective review of patients with out-of-hospital cardiac arrest: Post-resuscitation care pathway drives improved patient survival
Cardiac arrest
Shambavi Vettikumaran, Shona Johnson, Suzanne Maton, Liza Keating, William Orr and Tracey Realey
Royal Berkshire NHS Foundation Trust
Abstract
Introduction: In England, overall, around 9% of patients who undergo an OOHCA survive to hospital discharge. Post-resuscitation care remains the least well-defined component of the crucial ‘chain of survival’ and was a focus of the 2013 Cardiovascular Disease Outcomes Strategy. At the RBH we have collaborated across teams with the emergency medical services (EMS), emergency department (ED), cardiology and critical care working to improve outcomes and ensure the right patients undergo timely angiography and percutaneous intervention (PCI) with subsequent admission to critical care.
In 2016, we analysed 3428 patients with OOHCA presenting to the RBH between October 2012 and May 2015 and established a local OOHCA protocol in collaboration with EMS, ED, interventional cardiology and critical care and demonstrated better than expected survival to hospital discharge at 19.5%.
Objectives: The aim of this review was to ascertain if the currently observed outcomes, which were previously better than expected at 19.5%, have been maintained.
Methods: We undertook a retrospective chart review of EMS data, ED records, Myocardial ischaemia National Audit Project (MINAP) and Trust coding data from 2018 to 2021. We identified 5785 adult patients with spontaneous OOHCA in which cardiopulmonary resuscitation was commenced or continued by EMS. Outcomes for the RBH were compared to current national statistics and to our previous 2012- 2015 data. A chi-squared test to evaluate comparison of proportions was used.
Results: Overall, locally 21.7% of patients with an OOHCA survived to discharge compared to 9.1% for England (P <0.0001). A greater proportion than in the previous audit (32.6% vs 22%) underwent coronary intervention. Although survival to hospital discharge in those undergoing PCI was lower in 2018 – 2021 at 51.5% compared to 62.4% in 2012 – 2015.
Conclusions: High survival rates at the RBH have been maintained for all patients admitted to critical care following an OOH CA compared to the national average with a greater proportion undergoing coronary intervention.
References
1. Cardiovascular disease outcomes strategy (DoH 2013) MedCalc Software Ltd. Comparison of proportions calculator. https://www.medcalc.org/calc/comparison_of_proportions.php (Version 20; accessed May 28, 2021)
2. G. D. Perkins, et al. European Resuscitation Council Guidelines 2021: Executive summary, Resuscitation (2021), https://doi.org/10.1016/j.resuscitation.2021.02.003
3. Out of Hospital Cardiac Arrest Outcomes Registry. www.warwick.ac.uk/go/ohcao
4. G. D. Perkins, et al. (2021) Epidemiology of cardiac arrest Guidelines. Retrieved from: https://www.resus.org.uk/library/2021-resuscitation-guidelines/epidemiology-cardiac-arrest-guidelines#references
P024
Prophylactic antibiotic use in post-arrest care
Cardiac arrest
Charlie Dunmore and Eoghan O’Callaghan
Aintree University Hospital
Abstract
Introduction: Despite significant advances in post-ROSC care, survival following an Out Of Hospital Cardiac Arrest (OOHCA) remains poor. Targeted temperature management is accepted practice in optimising survival and neurological recovery following admission to Critical Care, despite suggested increased risks of VAP. An increasing evidence-base suggests prophylactic antibiotics within 12 hours of admission can reduce the incidence of early-onset VAP and could lead to shorter ICU/hospital stays.1 This project looks into how our unit complies with this and examines the relevance in the ICU setting.
Methods: Retrospective analysis was conducted on routine patient data for all adults admitted to our ICU, based at a large tertiary centre teaching hospital, following an OOHCA with ROSC. This data was collected during the periods of September 2019-20 and November 2019-2020 respectively. Data collected included age, Arctic Sun use, positive sputum cultures within five days of admission, ventilator hours, ICU/hospital days and overall survival outcomes. A departmental guideline outlining post-arrest management including prophylactic antibiotics was published in March 2019 and was available to all staff on the local intranet.
Results: Average age was 55. Our re-audit data showed that 87% of our patients were started on prophylactic antibiotics from day one of admission, an improvement from 84% the previous year. Data gathered in the most recent cycle demonstrated that the Arctic Sun was documented as being utilised in only 40.9%, on average seven hours into their admission. 29% grew at least one potentially pathogenic organism in their sputum in the first five days, with two more patients colonising shortly beyond this period. Average daily CPIS trended upwards from 1.84 on day one, to 2.67 on day five. 40.9% survived to hospital discharge, spending an average of 86.26 hours on a ventilator, six days of their admission on ICU and 14.7 total days in hospital.
Discussion: The majority of our patients are started on prophylactic antibiotics on admission, although this aspect of the bundle appears to be less strictly adhered to, possibly because of varying opinions amongst clinicians. A significant proportion of ventilated patients grew potentially harmful organisms, which alongside raised CPIS supports a high incidence of VAP. Similar results were seen in both cycles, supporting the use of a short course of antibiotics for these patients.
Acknowledgements: I would like to thank the ICU audit department at Aintree University Hospital.
References
1. François B, Cariou A, Clere-Jehl R, et al. Prevention of Early Ventillator-Associated Pneumonia after Cardiac Arrest. New England Journal of Medicine 2019; 381:1831-1842
P025
Levosimendan within critical care. Coronary stenting verses no coronary stenting: an observational study
Cardiovascular monitoring
Gemma Millen, Lucy Cooper and Mark Snazelle
East Kent Hospital University Foundation Trust
Abstract
Introduction: Levosimendan acts as a vasodilator opening ATP-sensitive potassium channels in vascular smooth muscle, increasing myocardial oxygen supply, and reducing preload and afterload. It protects against ischemia-reperfusion injury and activating stunned myocardium in patients following cardiac intervention.1
An Observational Study was designed to review the impact of Levosimendan in the first 24 hours of treatment by measuring Cardiac Index (CI). This data was collected in a district general hospital which offers primary percutaneous coronary intervention.
Objectives: To observe the impact of Levosimendan on CI during cardiogenic shock in patients who received coronary stenting vs no coronary stenting.
Methods: Patients requiring Levosimendan, due to cariogenic shock, were observed over an 8 year period. These patients were subject to inclusion and exclusion criteria.
| Inclusion | Exclusion |
|---|---|
| >18yrs old | Patients unlikely to survive >24hrs |
| Myocardial stunning with decreased organ perfusion | un-correctable medical conditions |
| Ejection Fraction <35% or regional wall abnormalities | Right heart failure due to pulmonary embolus |
| CI <2.5L/min/m² or dobutamine up to 10mcg/kg/min | High output failure due to thyrotoxicosis, arrhythmias, anaemia or massive blood loss |
| hypertrophic cardiomyopathy | |
| uncorrected stenotic valve disease in patients with no definite procedure planned. |
CI studies were performed on onset of Levosimendan, 12 hours and 24 hours from initiation.
Results: Manual data of 71 patients with a median age of 62 years. The male to female ratio was 76% vs 21% and the average organ support for the patients consisted of three organs
| Reason for admission | No of patients |
|---|---|
| Cardiac Arrest | 41 |
| STEMI | 22 |
| NSTEMI | 4 |
| OTHER (Sepsis) | 4 |
The patients were then observed for changes in CI at onset, 12hour and 24hour post Levosimendan infusion, in three groups;
| Group A | Patients receiving coronary stenting |
| Group B | Patient who didn’t receive coronary stenting |
| Group C | Septic Patients not assessed for coronary stenting |
| APACHE II Score | |
| ALL GROUPS | 18.5 |
| Group A | 19.5 |
| Group B | 16.5 |
| Group C | 17 |
The overall CI in all patients improved from onset to 24hrs of commencement of Levosimendan from a median CI of 1.83L/min/min² to 2.77L/min/m²
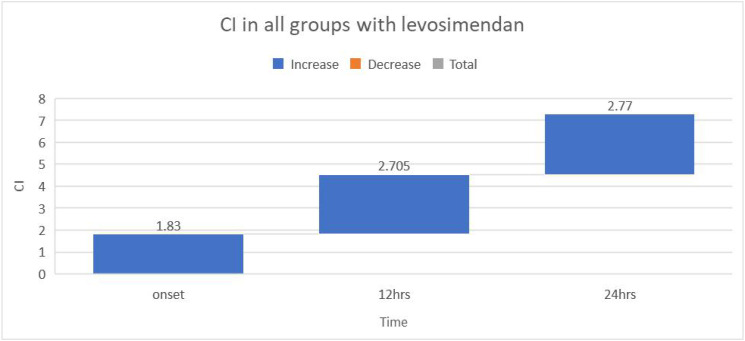
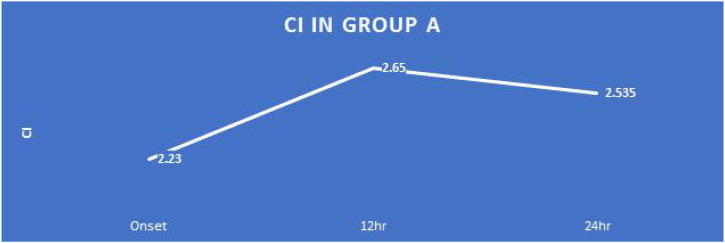
The patients’ CI in Group A, improved overall from onset of 2.23L/min/m² to 24 hour CI of 2.535L/min/m², however the CI at 12hrs was most improved to 2.65L/min/m². The overall mortality for this group of patients was 58%.
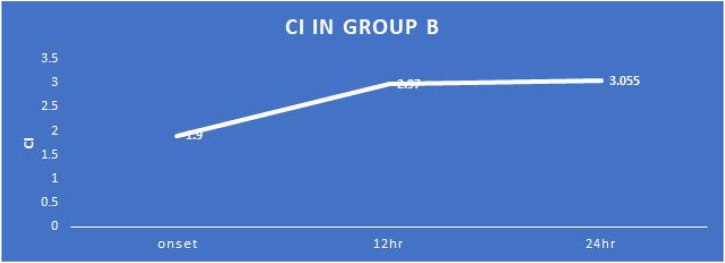
Patients in Group B show a consistenly improved median CI over the 24hrs from a CI of 1.9L/min/m² to 3.055L/min/m². The overall mortality for this group was 39%.
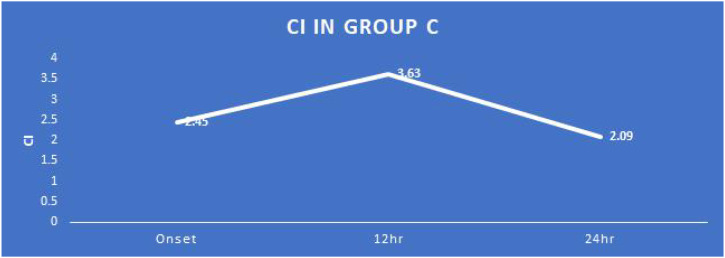
The data collected for patients in Group C is comparatively small and may well be excluded for this, however, the data showed a varying CI of onset 2.45L/min/m² to 2.09L/min/m². All the patients survived in this group.
Conclusion: The observational data for all three groups shows an overall improvement in CI, however there are some variations. Overall mortality of patients in Group B are improved from Group A, however the sample size and severity scoring is markedly different between the groups. APACHE II scores were higher in Group A, predicting a worse mortality. By definition, the patient groups being discussed have very high mortality and so isolation of the true benefit of Levosimendan will only be possible with large sample size.2 We postulate that due to cost, Levosimendan may be used too late. Further study into timing of administration of Levosimendan use in post coronary intervention group and use as first line therapy is warranted. We suggest future randomised controlled trials with larger patient groups, closer observation of the demographic data, severity scores, timing, administration and other variables. This would provide further evidence base to compare Levosimendan use verses standard therapy.
References
1. Manakers. Use of Vasopressors and Inotropes. https://www.uptodate.com/contents/use-of-vasopressors-and-inotropes?search=use%20of%20vasopressors%20and%20inotropes&source=search_result&selectedTitle=1∼150&usage_type=default&display_rank=1 (accessed 06/08/2021).
2. Brookes L, et al. REVIVE II and SURVIVE: Use of levosimendan for the treatment of acute decompensated heart failure. http://www.medscape.org/viewarticle/523043 (accessed 08/08/2021).
P026
Unusual case of BRASH syndrome precipitated by atrial fibrillation with a fast ventricular response
Cardiovascular monitoring
Luke Western 1 , Jessica Bialan2 and Benjamin Millette 3
1Oxford University Hospitals
2King’s College Hospital NHS Foundation Trust
3Buckinghamshire Healthcare NHS Trust
Abstract
Introduction: BRASH syndrome is a recently described clinical syndrome consisting of bradycardia, renal failure, atrioventricular (AV) nodal blockade, shock, and hyperkalaemia. It often arises from initial renal injury, causing an accumulation of AV nodal blocking medication and potassium. This induces bradycardia which contributes to a cardiogenic shock. This further injures the kidney in a vicious circle of pathology.1
BRASH syndrome justifies its definition as a distinct clinical entity as prognosis and management differ significantly from routine adult life support algorithms, and temporary transvenous cardiac pacing can be avoided with appropriate critical care management. It is considered a largely underdiagnosed entity.1
Objectives: We present a case of BRASH syndrome preceded by fast atrial fibrillation (AF). This complicated the clinical picture, and this case is discussed to increase awareness of the syndrome and promote timely identification and management.
Methods: We detail the clinical context and management of a patient with BRASH syndrome and discuss relevant literature.
Results: A 60-year-old gentleman presented with worsening shortness of breath over one week and unremarkable blood results. ECG revealed AF with a ventricular rate of 140 which didn’t respond to 10mg Bisoprolol and the team proceeded to DC cardioversion. Within two hours of cardioversion, he became haemodynamically unstable (systolic 80mmhg, heart rate 32) despite fluid resuscitation. He became oliguric and a refractory hyperkalaemia of 7.2 was noted. He developed new right bundle branch block and significant impairment in left ventricular function on echocardiography.
Temporary pacing was considered, however, BRASH was identified as a differential and following admission to the intensive care unit for haemofiltration and inotropic support with isoprenaline, he improved rapidly. Haemofiltration likely reduced the hyperkalaemia and beta-blocker in circulation and broke the BRASH syndrome cycle.1,2 He recovered to his baseline over the following three weeks on the cardiovascular ward and was discharged home.
Conclusions: It is very likely that AF with a fast ventricular response contributed to the precipitation of BRASH syndrome. Furthermore, DC cardioversion resulted in the rapid deterioration due to high doses of long-acting beta-blocker administered prior to the procedure. Early discussion of BRASH syndrome allowed the team to avoid unnecessary temporary transvenous pacing and proceeding with haemofiltration and inotropic therapy.
We recommend awareness of BRASH syndrome as a potential complication of cardioversion of acutely decompensated AF patients and be aware of the risks of high doses of long-acting AV blockers in those vulnerable to accumulation.
References
1. Farkas JD, et al. BRASH Syndrome: Bradycardia, Renal Failure, AV Blockade, Shock, and Hyperkalemia. The Journal of Emergency Medicine 2020;59:216–223. https://doi.org/10.1016/j.jemermed.2020.05.001.
2. Tieu A, et al. Beta-Blocker Dialyzability in Maintenance Hemodialysis Patients. CJASN 2018;13:604–611. https://doi.org/10.2215/CJN.07470717.
P027
The role of a family communications team in the intensive care unit during the COVID-19 pandemic
Communication
Jasmin Ranu 1 and David Hepburn2
1Cardiff University
2Grange University Hospital
Abstract
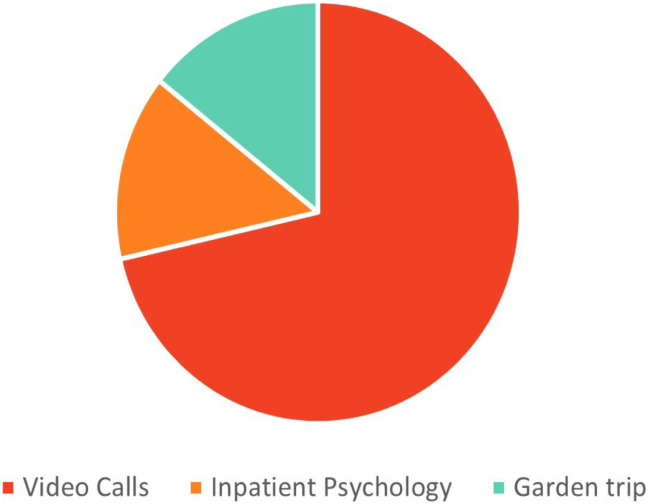
Introduction: The COVID-19 pandemic has added pressures onto Intensive Care Units (ICUs), including family visiting being commonly restricted to end of life.1,2 ICU care is based on adopting a patient and family-centred approach.3,4 To continue providing care in this way, many ICUs across the UK began initiating daily phone calls with families,1 or developing a dedicated family liaison team.1,2 The Aneurin Bevan University Health Board created a dedicated family communications team (FCT), originally split across two hospitals and later combined after the ICUs were merged. The medical team would handover to the FCT daily, who would call patient’s families to update them on their clinical picture and future plans.
Objectives: To explore family perceptions of the FCT throughout the COVID-19 pandemic.
Methods: A telephone questionnaire was created and retrospectively completed by families of patients admitted to ICU between November 2020 and May 2021. Families of patients who had since died were excluded. Families were randomly selected to allow for a distribution of participants across the study period. Data was added to that previously collected from the first wave within the health board to compare the general satisfaction of the FCT and analysed to look for strengths and weaknesses.
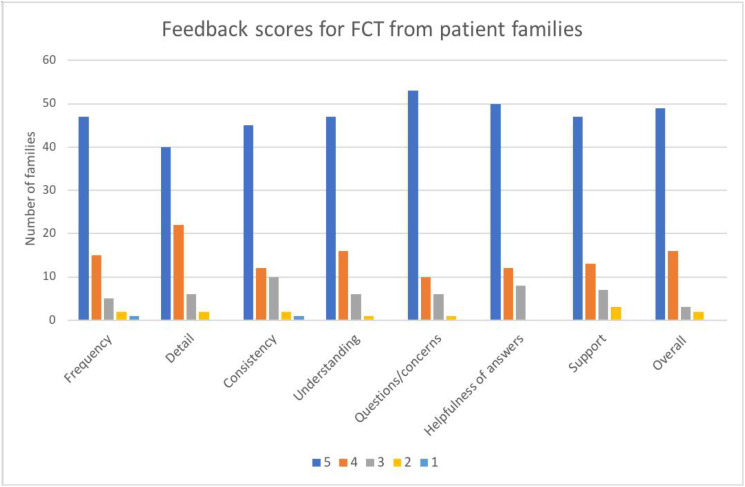
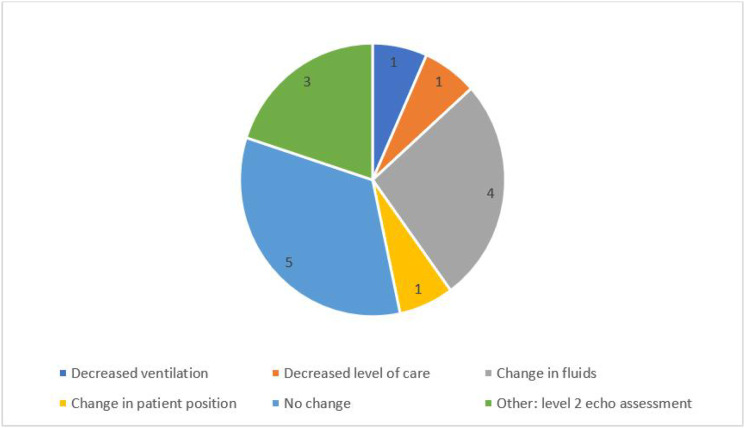
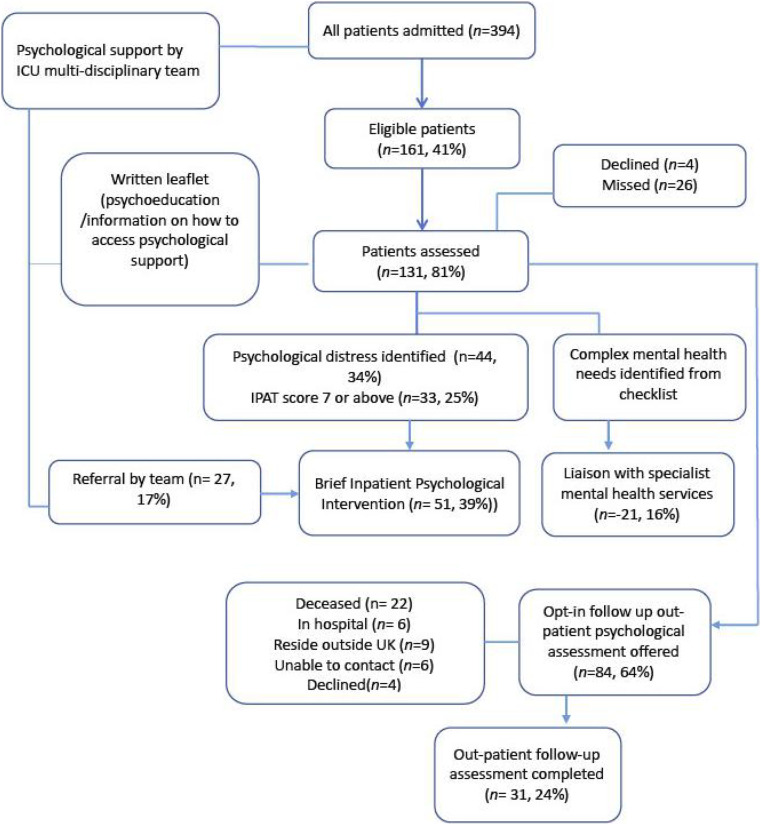
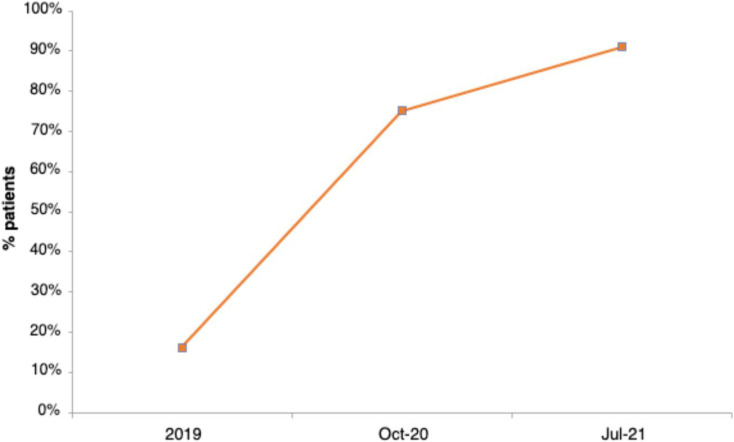
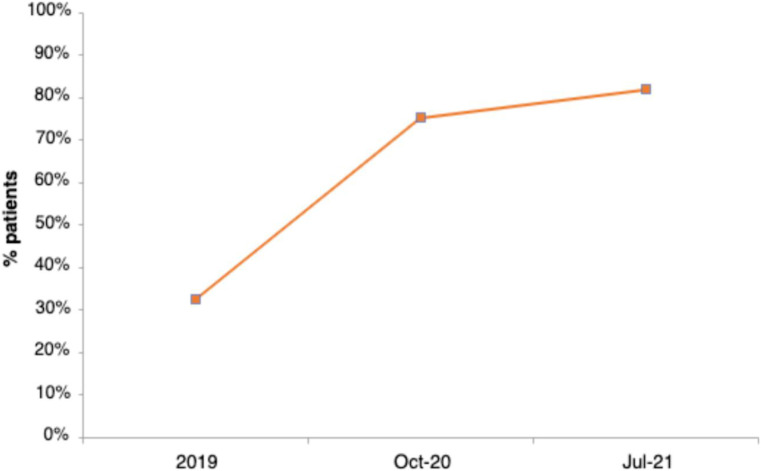
Results: The responses of 44 families of patients were added to the 26 previously collected – resulting in 70 family participants. The majority of responses to each question were scored at the maximum (figure 1). Of the 70 families, 65 (92.9%) rated the FCT overall as a 4 or 5 out of 5. There was little difference in satisfaction rates between the two hospitals (average overall score 4.73 vs 4.52 in wave 1 and 2 of the pandemic respectively), nor was there a change in satisfaction of the service over time.
Conclusions: The FCT received a fundamentally positive response, with majority of families scoring the service at the maximum across each domain measured. This study suggests that a dedicated FCT may have a role in the future of ICUs, both if visiting were to be restricted again in the future, or as a new normal.
Figure 1.
■■■.
References
1. Boulton AJ, Jordan H, Adams CE, et al. Intensive care unit visiting and family communication during the COVID-19 pandemic: A UK survey. J Intensive Care Soc Epub ahead of print 6 April 2021. DOI: 10.1177/17511437211007779.
2. Rose L, Yu L, Casey J, et al. Communication and Virtual Visiting for Families of Patients in Intensive Care during COVID-19: A UK National Survey. Ann Am Thorac Soc Epub ahead of print 22 February 2021. DOI: 10.1513/AnnalsATS.202012-1500OC.
3. Mitchell ML, Coyer F, Kean S, et al. Patient, family-centred care interventions within the adult ICU setting: an integrative review. Aust Crit Care 2016; 29(4): 179-193.
4. Van Mol MM, Boeter TG, Verharen L, et al. Patient- and family-centred care in the intensive care unit: a challenge in the daily practice of healthcare professionals. J Clin Nurs 2017; 26(19-20): 3212-3223.
P028
The infodemic in the pandemic: improving multidisciplinary ICU communication and responsiveness using QR code feedback
Communication
Brendan Spooner 1 , Emma Sherry2, Aimee Yonan2, Fahad Zahid2, Faisal Baig2, Martin LeBreuilly2, David Balthazor2 and Louisa Murphy2
1University Hospitals Coventry and Warwickshire
2UHB
Abstract
Introduction: During this pandemic our email inboxes, social media, general news and work meetings have become saturated with new information, guidelines, protocols and practices all subject to constant amendment. It has become an infodemic. This constant stream has caused cognitive fatigue to a workforce that is under severe pressure.1 Nonetheless, there is a need to report relevant information to the frontline on ICU in a timely and digestible way. It is also especially important for staff feedback to be assimilated rapidly. Therefore, having an agile communication strategy for the ICU workforce has never been more important.
Objectives: To introduce a communication and feedback strategy that met the needs of the evolving MDT workforce during the pandemic.
Methods: A multidisciplinary project team was assembled. The project had two arms – communication and feedback.
There was a need for an agile communication strategy for COVID ICU updates including to those re-deployed staff members. The aim was to achieve a suitable balance of relevant information without overwhelming colleagues with multiple daily emails. The group chose a weekly 1-page infographic poster that could easily be displayed, emailed and communicated via WhatsApp groups (see Figure 1). Update information was collated from multiple sources and distilled into a single page that was easy and quick to read.
Figure 1.
Example infographic.
Rapid feedback was collated from a QR code displayed in ICU rest areas, a suggestion/feedback box located next to the ICU and a dedicated email address. This information was fed to relevant stakeholders for them to act on to improve care, working practices and staff wellbeing.
Results: A pre-implementation survey of 31 multidisciplinary ICU staff members suggested staff felt very uninformed and uncertain about COVID ICU practice. From October 2020, 19 weekly updates were produced (until the end of the second wave). They were distributed to over 400 staff members and were widely shared amongst WhatsApp groups. They were displayed in 24 locations across critical care. As the processed matured colleagues would approach the project team with relevant updates that they wished to publicise. The team processed 137 pieces of feedback about a wide variety of issues on the ICU. Many were acted on for improvements. Other areas of the organisation adopted the QR code feedback strategy.
Feedback on the strategy has been excellent with 100% of those who saw the infographic finding it useful and staff felt more informed (post implementation survey of 29 colleagues). There were however several big challenges. Many of the issues raised via feedback were not within the gift of the project team to address. The rapidly changing and expanding workforce was hard to access.
Conclusion: Rapidly implementing a multidisciplinary digital communication and feedback strategy was possible during the pandemic. Results suggest it improved colleagues’ perception of being informed during the rapid changes that were necessary during the pandemic. The simplicity of QR code feedback generated much scope for improvement.
References
1. Kearsley R and Duffy CC. The COVID-19 information pandemic: how have we managed the surge? Anaesthesia 2020; 75: 993-996.
P029
Ready to talk? Evaluation of confidence in end-of-life communication among intensive care nurses
Communication
Jane Whitehorn 1 , Stephanie Cronin2, Kirsty Boyd3, Michelle McCool2, Susan Somerville2, Natalie Pattision4, Nazir Lone5 and Janine Wilson2
1Edinburgh Napier University
2NHS Lothian
3Edinburgh University
4University of Hertfordshire/East & North Herts NHS Trust
5NHS Lothian/Edinburgh University
Abstract
Introduction: Over 45,000 people receive critical care in Scotland annually and more than 12% of those admitted to intensive care die on the unit.1 Death of a family member in critical care leads to complicated grief in up to 52% of relatives.2 Caring for dying patients and their families contributes to burnout in up to 51% of team members.3 Clear, honest, and timely communication by the multidisciplinary team can help mitigate these adverse outcomes. However, the role of nurses in end-of-life (EOL) conversations can be unclear and passive.4
Objectives: To explore confidence in communication around EOL care among intensive care nurses and identify unmet educational needs.
Methods: Registered nursing staff of a 40 bedded, general ICU/HDU in the Royal Infirmary of Edinburgh completed an anonymous online survey during spring 2021 to assess their confidence in communication around EOL care, to explore the nature of EOL conversations, and identify key topics for further education. The survey was adapted from a validated tool5 designed to assess the level of knowledge, awareness, attitudes, and confidence of staff providing palliative care. No ethical approval was required.
Results: 32% (n=77) of invited ICU nurses responded to the survey. The majority of respondents were involved in EOL conversations on at least a monthly basis (58%, n=45). Over the previous 6 months, 81% (n=62) of nurses were involved in planned EOL discussions with patients/families whilst 71% (n=55) had taken part in impromptu conversations. Both planned and spontaneous EOL discussions were initiated by an ICU consultant more than twice as often as the patient’s nurse (planned n=57 vs 20, spontaneous n=37 vs 15). Among nurses with two or under years of experience in ICU, only 10% had initiated an EOL conversation with patients or their families in the previous six months.
31% of respondents were unsure or unconfident in their ability to speak with patients about death and dying and 21% felt similarly about talking with family members.
Only 22% of nurses said that they had received undergraduate training in EOL communication, whilst 40% had received postgraduate training. Further education in EOL care was requested by 99% of respondents, with the most required topics including communication relating to organ donation (n=49) and sharing bad news with patients and families (n=33).
Discussion: This study showed the significant involvement of ICU nurses in EOL communication. It highlighted the need for more undergraduate and postgraduate education in EOL communication and inclusion of critical care specific content. Improved education could increase nurses’ confidence and build a stronger multidisciplinary team approach to EOL communication. Better support for nurses in their role could decrease staff burnout. More effective and timely EOL communication may reduce the risk of complicated grief experienced by family members and promote better patient and family centred care.
References
1. Scottish Intensive Care Society Audit Group. Public Health Scotland. Audit of critical care in Scotland 2020 reporting on 2019. 2020. Available from: https://www.sicsag.scot.nhs.uk/Publications/_docs/2020-08-11-SICSAG-report.pdf?1
2. Kentish-Barnes N, Chaize M, Seegers V, Legriel S, Cariou A, Jaber S, Lefrant JY, Floccard B, Renault A, Vinatier I, Mathonnet A. Complicated grief after death of a relative in the intensive care unit. European Respiratory Journal. 2015;45(5):1341-1352. Available from: https://doi.org/10.1183/09031936.00160014
3. Malaquin S, Mahjoub Y, Musi A, Zogheib E, Salomon A, Guilbart M, Dupont H. Burnout syndrome in critical care team members: A monocentric cross sectional survey. Anaesthesia Critical Care & Pain Medicine. 2017;36(4):223-228. Available from: http://dx.doi.org/10.1016/j.accpm.2016.06.011
4. Ong KK, Ting KC, Chow YL. The trajectory of experience of critical care nurses in providing end‐of‐life care: A qualitative descriptive study. Journal of clinical nursing. 2018;27(1-2):257-268. Available from: https://doi.org/10.1111/jocn.13882
5. Phillips J, Salamonson Y, Davidson PM. An instrument to assess nurses’ and care assistants’ self-efficacy to provide a palliative approach to older people in residential aged care: A validation study. International Journal of Nursing Studies. 2011;48(9):1096-1100. Available from: https://doi.org/10.1016/j.ijnurstu.2011.02.015
P030
Introduction of a night time safety brief; improving patient safety in Critical Care at Sheffield Teaching Hospitals
Communication
Rachel Ward
Sheffield Teaching Hospitals
Abstract
Introduction: Since the onset of the Coronavirus pandemic in March 2020 we have had to change our day to day working practice in a large Critical Care department, with up to 36 patients across two floors. Prior to the pandemic, each floor functioned as an almost separate unit, with level 2 patients in one area and level 3 patients in another.
Patients requiring level 3 care are now present on both floors although the staffing for each floor has not changed to reflect this. Therefore, out of hours more complex patients are being cared for by staff who have less experience in caring for these patients.
The introduction of safety briefings in clinical care is based on concepts in aviation, where they are designed to make safety-consciousness routine practice.
Objectives: The introduction of a nighttime safety brief aimed to improve safety and communication across Critical Care with the key objectives of introducing all medical and senior nursing staff working across critical care, identifying bed pressures and ill patients. Aims included Increasing visibility of the airway registrar, identifying the skill mix of the staff across the units and initiating contact between medical staff and the nurse in charge across each floor.
Methods: A preliminary survey of medical and nursing staffing was undertaken to explore the attitudes of staff to the current arrangement and the perception of a need for change.
A ‘Night Time Safety Brief’ was developed by creating a proforma of key topics to be discussed and an agenda for a nightly meeting that was designed to take no more than five minutes and targeted to key information sharing.
The location and timing of the briefing was designed to be convenient by liaising with key stakeholders in the meeting. The tool was then implemented with all medical critical care staff and the nurse in charge from each unit meeting to undertake the safety brief following the independent medical handover of each of the units.
A follow up survey was undertaken to assess the impact of the safety brief and staff opinions on the introduction of the brief.
Results: Every member of staff surveyed felt that the introduction of the brief was beneficial. 76% of staff surveyed felt that they were more comfortable working the shift simply by having met the medical and nursing staff from across the floor to better understand the skill mix and points of contact. 90% of staff surveyed felt that the brief would positively impact on patient safety.
Conclusions: Briefings in intensive care are tools that increase the awareness of safety issues among front line staff and foster a culture of safety, making it part of the routine in a clinical area. A simple and effective brief has been developed and used in this tertiary hospital with the aim of improving patient safety.
In this hospital with critical care split across two clinical areas, this has shown to improve communication and team working in a busy tertiary teaching hospital.
P031
Safer discharge of patients from the critical care unit - Improving communications with primary care
Communication
lexandra Cockroft1, Sofia Arkhipkina 2 and Timothy Fudge2
1The Northern Hospital
2Salford Royal NHS Foundation Trust
Abstract
Introduction: For patients who survive to hospital discharge following admission to the critical care unit (CCU), the sequelae of critical illness is often prolonged, and can encompass physical and psychological complications. Support is provided to high-risk patients by Salford Royals’ (SRFT) CCU follow-up clinics however, most patient’s ongoing care in the community is provided by general practitioners (GP). Provision of CCU discharge information to primary care is often inadequate or absent, meaning identifying and treating long-term CCU complications can be challenging.
Objectives: We aimed to understand the concerns hospital staff have surrounding CCU discharge communication and the concerns of GPs looking after patients who have had recent CCU admissions. We aimed to improve CCU communication with GPs to enhance safety and quality of ongoing care, in order to increase the support available to patients and their families following critical illness.
Methods: To confirm anecdotal concerns, questionnaires were sent to CCU consultants and junior doctors at SRFT, and GPs in Salford. Questionnaire results were analysed in focus groups and used to create a CCU specific discharge summary. The discharge summary was developed using PDSA methodology.
Results: Consultants (77%) had concerns regarding handover of patient information to ongoing care providers. Juniors (45%) were not confident in providing information regarding CCU long-term complications. Consequently, half of GPs did not find hospital discharge summaries useful in providing information about a CCU admission. No GPs felt confident in signposting patients to CCU follow-up services, with only 14% aware of the SRFT CCU follow-up clinic. Both GPs and CCU consultants agreed a CCU specific discharge summary would be beneficial.
A CCU specific discharge summary was developed and revised with expert opinion from the multidisciplinary team to tackle the issues stated. The discharge summary includes details of diagnoses, organ support, length of stay, ceiling of care, complications addressed by the CCU follow-up team and a CCU discharge information leaflet outlining commonly experienced symptoms and local follow-up services.
Conclusions: This CCU specific discharge summary has enabled SRFT’s CCU to effectively deliver relevant information to GP’s, to ensure continuity of care following discharge. Effective and safe handover of patients between care settings is crucial, to ensure care providers are well informed, and patients managed appropriately. Improving the communication interface between care providers will ensure clinicians are well informed, enabling the safe and timely community management of patients, post-critical care.
P032
Does COVID Affect Clot Formation?
COVID-19
Toby Katz1, Ed Walter 1 , Benjamin Mensah1, Mathew Rogers1, Ashley Tomlison2 and Lucas Alvarez-Belon2
1Royal Surrey NHS Hospital
2Royal Surrey County Hospital
Abstract
Introduction: Covid infection is associated with an increased rate of thrombosis, up to 50%,1 but the reasons for this are unclear.
Rotem is a form of viscoelastic measurement of blood coagulation, allowing graphical representation of the time a clot takes to form (clotting time (CT) and clotting formation time (CFT)), its strength (firmness of the clot after 5 min (A5) and maximum clot firmness (MCF)), and dissolution (maximum lysis (ML). Rotem provides four analyses to each sample: Intem (measure of intrinsic pathway), Extem (extrinsic pathway), Heptem (similar to Intem, excluding heparin effects) and Fibtem (isolating fibrinogen function).
In one study, Covid infection was associated with a reduced clotting time and an increased maximum clot firmness overall.2 The same study also suggested a possible increase in Fibtem MCF value for COVID patients, suggesting a strong influence of fibrinogen on the clot.
This clinical effectiveness audit was designed to determine if (1) Covid patients in the Royal Surrey County Hospital also displayed increased clotting tendencies compared with patients without, as measured by Rotem and fibrinogen levels, and (2) whether fibrinogen levels correlate with Fibtem MCF levels.
Methods: A retrospective data analysis from all Rotem analyses in ICU between June 2020 and February 2021 was performed.
To compare coagulation in patients with and without Covid, data were tested for normality using Shapiro-Wilks testing. Normal data were compared by the Student t-test; non-normal data were compared by the Mann-Whitney U-test. A p-value < 0.05 was taken as statistically significant.
In the second part, correlation between fibrinogen values and Fibtem MCF values was assessed using a Pearson correlation coefficient.
Results: 163 patients had Rotem analyses performed, of whom 12 (7.4%) had a positive Covid test.
The median Fibtem A5 in Covid patients was 21 mm compared with 13 mm in non-Covid patients, and median MCF was 25 mm compared with 16 mm, indicating a significant increase in the clot strength by the fibrin component between patients with and without Covid. No other Rotem differences were found.
There was also a statistically significant difference between fibrinogen levels in COVID (median 6.2) and non-COVID (median 3.05) patients, suggesting a significant contribution of fibrinogen to clotting in COVID.
Finally, the study demonstrated a strong positive correlation between fibrinogen levels, as measured by the laboratory, and corresponding Rotem MCF values in all patients (R2 = 0.8105), and in patients with Covid (R2 = 0.905).
Discussion: There was a significant increase in the clot firmness due to the fibrin component, and fibrinogen levels, in patients with Covid infection, compared with those without, consistent with a previous study.2
Rotem measurement of clot strength by fibrin correlated very well with fibrinogen levels.
This study suggests that the increase in thrombosis in Covid may be in part related to increased fibrinogen activity.
The study may be limited by small numbers of patients, and the heterogeneity of the patients within each group.
References
1. Bompard F, Monnier H, Saab I, et al. Pulmonary embolism in patients with COVID-19 pneumonia. Eur Respir J 2020; 56: 2001365. doi:10.1183/13993003.01365-2020.
2. van Veenendaal N, Scheeren TWL, Meijer K, van der Voort PHJ. Rotational thromboelastometry to assess hypercoagulability in COVID-19 patients. Thromb Res. 2020; 196: 379-381. doi:10.1016/j.thromres.2020.08.046.
P033
High-flow nasal oxygen therapy for respiratory support in SARS-CoV-2 pneumonia in adult intensive care patients. A Belgian observational study
COVID-19
Anne-Laure Van Massenhove, Geoffrey Horlait, Maxime Regnier and Jean Paul
Mangion chu ucl Namur
Abstract
Introduction: The worldwide COVID-19 pandemic was a major challenge for all medical actors and in particular for intensive care units.1 Its management is essentially supportive and in its severe form, requires high-flow oxygen therapy for which the ideal application modalities remain to be defined.2
Objectives: This study compares data from two waves during which the management differed substantially: early invasive ventilation during the first wave versus high flow oxygen therapy (Optiflow™ Nasal High Flow, Fisher & Paykel Healthcare) with salvage mechanical invasive ventilation during the second wave.
Methods: This single-center observational study included 108 patients: 21 from the first wave and 87 from the second. The two groups were comparable in terms of age, sex, obesity, hypertension, diabetes, and underlying lung disease. The study was conducted from March 2020 to March 2021.
The primary outcome was length of hospitalisation. The secondary outcomes were duration of mechanical ventilation and patient mortality at 28 days. As the two groups were matched, the main difference was dexamethasone corticosteroid therapy for 10 days for the second wave.
Results: The results show a higher mortality in the "high flow oxygen therapy” group when compared to the “early mechanical ventilation” group. This result could be explained by patient fatigue before being placed on mechanical ventilation but also by a higher frequency of pneumonia and bacteraemia in the latter group probably linked to the systematic administration of steroids. On the other hand, the duration of hospitalisation and the duration of mechanical ventilation are shorter in the high flow oxygen therapy group.3
Conclusion: High-flow oxygen therapy can be considered as an alternative to conventional ventilation in the event of respiratory distress following a SARS-CoV-2 infection. Further research should be co-considered.
Conflict of interest: None declared. This study was conducted in accordance with the Declaration of Helsinki.
References
1. Gattinoni L, Coppola S, Cressoni M, et al. COVID-19 Does Not Lead to a “Typical” Acute Respiratory Distress Syndrome. American Journal Of Respiratory And Critical Care Medecine. 2020; 201(10): 1299-1300. https://doi.org/10.1164/rccm.202003-0817LE
2. Catala I, COVID grave: et si l’intubation n’était pas la solution? Medscape. https://francais.medscape.com/voirarticle/3605845 (10 april 2020).
3. Alhazzani W, Møller MH, Arabi YM, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med. 2020; 46:854–887. https://doi.org/10.1007/s00134-020-06022-5
P034
Education - Supporting redeployed staff during the covid-19 pandemic
COVID-19
Rebecca Sumnall
UHL
Abstract
Introduction: The COVID-19 pandemic required a significant increase in Critical Care bed capacity resulting in many non-Critical Care staff being redeployed to work in Critical Care.1 There were a variety of professions redeployed as ITU ‘nurses’ including non-critical care nurses, Operating Department Practitioners (ODPs) and medical and dental staff. Training was developed for these members of staff in order for them to support the critical care team during the surge.
Objectives: NHS England produced a guide to provide principles for increasing the workforce in response to exceptional demand in adult critical care services. In it they stated that staff moved from other areas will be required to be supported to ensure safe practice, safe patient care and staff wellbeing, with appropriate supervision and delegation of care.2 These non-critical care staff needed training to care for critically ill covid-19 patients.3
During the second wave of covid-19 medical and dental staff were redeployed to act as category ‘B’ nurses.2 Training had been provided to prepare nurses and ODPs for these roles and this was adapted to be delivered to medical and dental staff acting as ‘nurses’.
Methods: Training was developed to support the development of staff redeployed to critical care to support the surge response. On completion of the training session staff were asked to complete an online survey to enable evaluation of the training, to understand their experiences, and develop any future training.
Results: Post course evaluation was conducted to assess the effectiveness, quality and impact of the education intervention. Training was provided to 30 Doctors and Dentists over five sessions in the period 27 January—11 February 2021. Evaluations were sent to all staff that attended the training and 19 were returned (63% response rate). 17 (89%) of the respondents said that attending the training had helped them whilst doing clinical nursing shifts in ITU.
Conclusion: The integration of redeployed staff into the Critical Care team allowed the additional patients to be cared for as safely. These staff required training to provide them with the information to care for these patients safely and evaluation of this training is important to aid future planning.
References
1. Aziz S, Arabi Y, Alhazzani W, Evans L, Citerio, G, Fishchoff K et al. Managing ICU surge during the COVID-19 crises: rapid guidelines. Intensive Care Medicine. 2020; 8: 1-23.
2. NHS England. Coronavirus: principles for increasing the nursing workforce in response to exceptional increased demand in adult critical care. 2020. Available on: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/specialty-guide-critical-care-workforce-v1-25-march-2020.pdf. Accessed on: 12/07/2020.
3. Marks S, Edwards S, Jerge EH Rapid Deployment of Critical Care Nurse Education during the COVID-19 pandemic. Nurse Leader 2021; 19(2): 165–169.
P035
Intensive Care Unit outcomes of COVID-19: A National Cohort study from Malta
COVID-19
Carl Tua 1 , Christabel Mizzi2, Karen Sapiano2, Stephanie Santucci2, Matthew Drake2, Bernice Spiteri3, Nicole Grech2, Stephen Sciberras2 and Michael Buttigieg2
1Mater Dei Hospital, Malta
2Mater Dei Hospital
3Mater Dei
Abstract
Introduction: The COVID-19 virus has caused a massive strain on medical services worldwide. Throughout 2020 and 2021, hospitals and their Intensive Care Units (ICUs) have been inundated with patients suffering from critical illness due to COVID-19, many of whom developed multi-organ failure and required prolonged ICU stays.1 Malta is a Mediterranean island with a population of 500,000 people, with one main acute general hospital (Mater Dei Hospital) with a single 20-bed ICU. This meant that the COVID-19 pandemic surge had to be managed locally by increasing ICU capacity without access to a referral network of other hospital ICUs at different phases of the pandemic or the possibility of referral to ECMO services abroad.
Objectives: Establish the demographics and outcomes of all patients admitted to ICU with COVID-19 in Malta.
Methods: A single centre prospective cohort study conducted in the Intensive Care Units caring for COVID-19 patients at Mater Dei Hospital, Malta. Data was collected on admission and then daily until death or discharge from ICU.
Results: The COVID-19 pandemic resulted in 252 patients being admitted to ICU from March 2020 to May 2021. The peak of admissions occurred in March 2021 with a maximum of 21 admissions in a week resulting in a peak of 33 COVID-19 ICU beds being utilized. This represents 165% of the normal 20 bed ICU capacity. There were 9 readmissions, these were excluded from data analysis. All patients admitted to ICU were treated with Dexamethasone and Remdesivir, and Tocizulimab from January 2021, unless contraindicated.
Overall ICU mortality was 34% and increased to 46% in those requiring mechanical ventilation. Males were responsible for 75% of admissions but gender was not associated with ICU mortality. Older patients and those with ischemic heart disease (IHD) and diabetes had a significantly increased mortality as were those patients with a higher Sequential Organ Failure Assessment (SOFA) and lower PaO2/FiO2 (P/F) on admission (Table 1).
Table 1.
Demographic and clinical status according to 28-day survival status. Continuous values reported as median with [Interquartile Range] and Kruskal Wallis test performed. Categorical values expressed as number (%) and Fisher exact test used.
| 28 Day Status | p-Value | |||
|---|---|---|---|---|
| All Patients | Alive | Dead | ||
| Number (%) | 252 | 166 (66) | 86 (34) | |
| Demographics | ||||
| Age (IQR) | 67 (61–73) | 65 (57–72) | 71 (67–76) | <0.001 |
| Male (%) | 188 (75) | 124 (75) | 64 (74) | 1 |
| BMI > 35 (%) | 37 (15) | 22 (13) | 15 (17) | 1 |
| Ischemic Heart Disease (%) | 47 (19) | 21 (13) | 26 (30) | 0.001 |
| Hypertension (%) | 151 (60) | 92 (55) | 59 (69) | 0.057 |
| Diabetes (%) | 94 (37) | 54 (33) | 40 (47) | 0.039 |
| Immunosuppression (%) | 4 (2) | 2 (1) | 2 (2) | 0.61 |
| First 24 Hours | ||||
| SOFA Score | 2 (2–3) | 2 (2–3) | 3 (2–4) | <0.001 |
| P/F ratio (IQR) | 96 (77–129) | 101 (80–135) | 87 (71–114) | 0.012 |
| Organ Support During Admission | ||||
| Continuous Renal Replacement Therapy (%) | 50 (20) | 17 (10) | 33 (48) | <0.001 |
| Mechanical Ventilation (%) | 173 (69) | 94 (57) | 79 (92) | |
The total number of patients requiring intubation during their admission was 173 (69%) with a median time to intubation of two days [IQR 1-4]. Proning was used for 124 (69%) of the mechanically ventilated patients for a median of 2 days per patient [IQR: 1 - 3], similarly muscle relaxant infusion was also used in 124 of mechanically ventilated patients (69%) for a median of three days per patient [IQR: 2 - 5]. The median duration of mechanical ventilation was 11 days [IQR: 6 - 22.2] with a maximum of 63 days. Tracheostomies were performed in 59 (34%) of mechanically ventilated patients with a median duration of 14.5 days intubated prior to tracheostomy [IQR: 13 - 17]. The median length of stay was 11.5 days [7-23].
Figure 1.
1a. COVID-19 ICU 28-day mortality (%) according to age, 1b. COVID-19 ICU 28-day mortality (%) in ventilated patients according to age. n = total number of patients in age range.
Conclusion: This observational study represents all COVID-19 ICU admissions that occurred in Malta from March 2020 to May 2021 in the single institution caring for these patients in the country. We have demonstrated a predominantly male, elderly admission population with an increased mortality associated with age, ischemic heart disease and diabetes. Overall ICU mortality was 34% and 46% in ventilated patients, which is comparable to that found in other national databases.2
References
1. Phua J, Weng L, Ling L, Egi M, Lim CM, Divatia JV, Shrestha BR, Arabi YM, Ng J, Gomersall CD, Nishimura M, Koh Y, Du B; Asian Critical Care Clinical Trials Group. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8(5):506-517. doi: 10.1016/S2213-2600(20)30161-2.
2. Armstrong RA, Kane AD, Kursumovic E, Oglesby FC, Cook TM. Mortality in patients admitted to intensive care with COVID-19: an updated systematic review and meta-analysis of observational studies. Anaesthesia. 2021;76(4):537-548.
P036
Incidence of venous thrombo-embolism in SARS COVID-19 in a district general critical care unit
COVID-19
Philip Taylor 1 and Steven Lobaz2
1Sheffield Trus
2Barnsley Trust
Abstract
Introduction: SARS COVID-19 is known to produce a hypercoagulable state in which micro and macro-thrombi form, leading to reduced arterial oxygen saturation, organ failure, and increased need for mechanical ventilation – all of which increase mortality. Currently there is conflicting evidence regarding the efficacy of heparin anticoagulation on the incidence of venous thrombo-embolism (VTE) in COVID-19 and throughout the pandemic clinical guidance for heparin use has been updated from standard to intermediate dosing for thromboprophylaxis. Studies show rates of 21-31%1,2 for symptomatic VTE in ICU COVID-19 patients receiving standard dose prophylactic dalteparin.
Objectives: This service evaluation presents local data on incidence of VTE and mortality in critical care COVID-19 patients and provides a summary discussion of the latest trials on prevention of VTE in COVID-19 and their recommendations.
Methods: A retrospective evaluation was undertaken on patients admitted to Barnsley Hospital Critical Care Unit during March – December 2020 with confirmed COVID-19 during wave one (27/03/20 – 14/06/20) and wave two (15/06/20 – 03/12/20) of the pandemic. The primary outcome was incidence of VTE, which was defined by either: D-dimer ≥ 3 mg/L; a positive ultrasound doppler (USS); or by computed tomography pulmonary angiography (CTPA). Mortality data was also collected.
Results: Data was collected on 96 patients (n=73 male, n=23 female). VTE occurred in 30.2% of patients with n=14 confirmed by CTPA, n=1 confirmed by USS, and n=15 with D-dimer ≥ 3 mg/L (but not already confirmed by CTPA or USS). Male and female mortality in the intubated group for both waves was 58.3% and 56.0% respectively. Between waves one and two there was a 28% decrease in mortality across all patients, a 27% decrease in the rate of intubation, and a 20% decrease in mortality in the intubated-only population. Mortality across both waves in the standard and intermediate dalteparin dose populations was 67% and 19% respectively. Table 1 summarises mortality data for the different sub-populations.
Table 1.
Mortality data for the different sub-populations.
| All patients | Total in population | Died | Mortality as % of population |
|---|---|---|---|
| Both waves | 96 | 35 | 36.5 |
| Wave 1 | 39 | 17 | 43.6 |
| Wave 2 | 57 | 18 | 31.6 |
| Intubated population only | |||
| Both waves | 30 | 17 | 56.7 |
| Wave 1 | 16 | 10 | 62.5 |
| Wave 2 | 14 | 7 | 50.0 |
| CPAP population only | |||
| Both waves | 51 | 9 | 17.6 |
| Wave 1 | 13 | 2 | 15.4 |
| Wave 2 | 38 | 7 | 18.4 |
| Standard dose dalteparin | |||
| Both waves | 24 | 16 | 66.7 |
| Wave 1 | 23 | 15 | 65.2 |
| Wave 2 | 1 | 1 | 100.0 |
| Intermediate dose dalteparin | |||
| Both waves | 47 | 9 | 19.1 |
| Wave 1 | 10 | 0 | 0.0 |
| Wave 2 | 37 | 9 | 24.3 |
Conclusion: Our data shows a VTE rate consistent with the literature. Statistical analysis of the data was undertaken using Fisher’s exact test. Overall mortality between waves one and two was not significantly different at the P<0.05 level. Reduction in mortality across both waves in the standard and intermediate dose dalteparin populations was significant at the P<0.01 level. However, due to advances in care developed throughout the pandemic, we cannot say if the reduction in mortality is due to the use of intermediate dose dalteparin, as there are other factors to consider. Despite this, its use, combined with other treatments, is consistent with an improved outcome in COVID-19 ICU patients. Current best evidence from INSPIRATION and REMAP-CAP/ATTACC/ACTIV-4a trials3,4 recommends giving treatment dose low-molecular-weight heparin (LMWH) to all COVID-19 hospitalised patients, but to reduce to intermediate dose if admitted to critical care/ICU providing there is no evidence of VTE, as defined above. Trials currently show no benefit of routine treatment dose dalteparin over intermediate dose in critical care for COVID-19 patients.
References
1. Poissy J, Goutay J, Caplan M, et al. Pulmonary Embolism in COVID-19 Patients: Awareness of an Increased Prevalence. Circulation 2020; 142(2): 184-186.
2. Klok FA, Kruip M, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020; 191: 145-147.
3. The ATTACC, ACTIV-4a and REMAP-CAP Investigators. Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with Covid-19. N Engl J Med 2021
4. INSPIRATION Investigators. Effect of Intermediate-Dose vs Standard-Dose Prophylactic Anticoagulation on Thrombotic Events, Extracorporeal Membrane Oxygenation Treatment, or Mortality Among Patients With COVID-19 Admitted to the Intensive Care Unit. JAMA 2021
P038
Thrombocytopaenia in critically ill COVID-19 patients: An observational study from a single centre
Ashani Ratnayake 1 , Prabhashini Kumarihamy2, Ayeshani Rajapakse3, Hiranya Abeysinghe2, Sahan Perera2 and Shanika Medagama2
1Ministry of Health
2District Base Hospital - Theldeniya
3District Base Hospital- Theldeniya
Abstract
Introduction: SARS-CoV-2 infection can cause manifestations in multiple systems in the body.1 Haematological system is one such system which can be affected by both SARS-CoV-2 infection and critical illness. There are some studies that have shown that thrombocytopaenia can be associated in patients with SARS-CoV-2 infection.2 There is minimal data on its prevalence and outcome on critically ill patients. One study has shown that low platelet is associated with worsening of respiratory parameters and long term adverse outcome in critically ill.3 Identifying the presence of thrombocytopaenia and its consequences is important to manage critically ill COVID-19 patients.
Objectives: To identify the prevalence and consequences of thrombocytopaenia and the presence of other causes of thrombocytopaenia in critically ill COVID-19 patients.
Methods: A retrospective observational study was done in COVID designated Intensive care unit and High dependency unit in Base Hospital- Teldeniya, Sri Lanka. All patients with positive SARS-CoV-2 testing who later develops pneumonia with oxygen dependency and requiring ICU or HDU care were included in the study. Data was collected from patient records for the duration from 1st of January 2021 to 30th of June 2021. Their demographic data, data related to platelet counts and other causes leading to thrombocytopaenia were collected. Thrombocytopaenia was categorised as mild (platelet count 100-150× 109/L), Moderate (50-100×109/L) and severe (less than 50×109/L)
Results: Total of 189 patients were admitted to either ICU or HDU requiring oxygen therapy due to COVID pneumonia during the study period. The mean age was 60.59 years with SD of 14.9. Age range was 16 to 94 years. 63 patients (33.33%) had thrombocytopenia with 8 (12.69%), 19 (30.15%) and 36 (57.14%) had severe, moderate, and mild thrombocytopenia respectively. 28 (44.4%) of the patients had low platelets at the time of admission. 28.5% of the patients had another cause for thrombocytopenia. Figure 1 shows other causes contributed to thrombocytopenia. Out of the patents who had thrombocytopenia 17 (26.9%) patients died. This was equal to 48.7% of all critical care deaths. The proportion of death among patients with thrombocytopenia was fund to be significant compared to that of patients with a normal platelet count. (p=0.045)
Figure 1.
Other causes of thrombocytopenia found in the sample.
Conclusions: Thrombocytopenia may arise due to multiple aetiologies in critically ill patients. Our study shows that at least 1/3 of the critically ill patients with COVID-19 infection develop thrombocytopenia at some point of their course of illness. It is important to have an insight on the progression of the illness and the outcome in order to plan discharge and follow up for these patients.
References
1. Gavriatopoulou M, Korompoki E, Fotiou D, et al. Organ-specific manifestations of COVID-19 infection. Clin Exp Med. 2020;20(4):493-506. doi:10.1007/s10238-020-00648-x
2. Xiaolong Z, Yajun G, Hongjian Yu, Zhenyu L, Yuliang W, Thrombocytopenia Is Associated with COVID-19 Severity and Outcome: An Updated Meta-Analysis of 5637 Patients with Multiple Outcomes, Laboratory Medicine, Volume 52, Issue 1, 10–15, https://doi.org/10.1093/labmed/lmaa067
3. Zhu Y, Zhang J, Li Y, Liu F, Zhou Q, Peng Z. Association between thrombocytopenia and 180-day prognosis of COVID-19 patients in intensive care units: A two-center observational study. PLoS One. 2021;16(3):e0248671. doi:10.1371/journal.pone.0248671
P039
Parameters that affect the outcome in ICU patients with critical COVID - 19 infection
COVID-19
Aristeidis Vakalos and Ilias Tsioulis
Xanthi General Hospital
Abstract
Introduction: COVID - 19 pandemic continues to affect millions worldwide, while the critical form of the disease requires ICU hospitalization to manage not only respiratory failure but multiple organ dysfunctions as well.
Objectives: Our retrospective observational study aimed to test the hypothesis that there is a difference in mean values of indexes pointing to organ dysfunction on ICU admission day, like BUN over Creatinine ratio, BUN over Albumin ratio, and PaCO2 over HCO3 ratio among patients with confirmed critical COVID - 19 infection who died and patients who survived ICU.
Methods: During late 2020 to 2021, 69 patients indicated with the diagnosis of critical COVID - 19 disease admitted to ICU. The patients were separated into two groups. Group A involved all patients who survived ICU and group B all patients who died in ICU. We looked for statistically significant differences between the medians values of two groups according to BUN/Cr, BUN/Alb, PaCO2/HCO3 ratios on the ICU admission day, performing unpaired t-test or Mann-Whitney Test according to equal S.D.s assumption.
Results: (Table)
| Group A/B | Mean | Max | Min | S.D | p-value |
|---|---|---|---|---|---|
| BUN/Cr | 41.3/29.4 | 315/58.6 | 5.18/7.41 | 71.9/9.87 | 0.2440 |
| BUN/Alb | 8.93/14.2 | 35.6/58.2 | 2.91/4.33 | 8.1/10.06 | 0.0039 |
| PaCO2/HCO3 | 1.65/2.2 | 2.58/4.57 | 1.3/1.13 | 0.38/0.80 | 0.0085 |
Conclusions: According to our data, there was a strong statistically significant difference detected between the two groups according to BUN/Alb and PaCO2/HCO3, while the BUN/Cr ratio had no statistically significant difference. Our data suggest that prerenal disorder took place early and was already present on ICU admission day, although not statistically greater in group B. However, a renal disorder associated with albumin levels was greater in group B, and acute type II respiratory failure was by far greater in patients that died in the ICU, pointing that oxygenation disorder was not the only impact of COVID - 19 infection on the ICU admission day.
P040
Optimising filter lifespan in critically ill patients with SARS-CoV-2 receiving renal replacement therapy: an observational study in a district general hospital
COVID-19
Christina Evans, Radha Sundaram, John Hunter and Lisa Gemmell
NHS Greater Glasgow and Clyde
Abstract
Introduction: Acute kidney injury (AKI) and need for renal replacement therapy (RRT) is a known complication of SARS-Coronovirus-2 (SARS-CoV-2) in critically ill patients.1 Early evidence suggested SARS-CoV-2 patients have increased incidence of filter cartridge failure on RRT.2,3 Frequent filter changes can lead to reduced therapy delivery, increased cost and anaemia. To mitigate this, our intensive care unit developed a new protocol for patients with SARS-CoV-2 requiring RRT to balance the benefits of preserving filter lifespan and risks of anticoagulation associated bleeding.
Objectives: To investigate whether an increased citrate dose and an adjusted RRT prescription would increase the filter lifespan for patients with SARS-CoV-2.
Methods: We performed a retrospective observational study looking at all patients admitted to our Level 3 critical care unit since the pandemic in March 2020 to date. Data was collected from Ward Watcher, a Scottish Intensive Care Society Audit Group (SICSAG) database and the CAREVUE electronic patient records. We introduced a modified RRT prescription for continuous venovenous haemodiafiltration (CVVHDF) with a citrate dose of 4mmol/l, increasing the dialysate flow rate to 1500ml/hr to mitigate the risk of increased citrate load.
Results: During the period for data collection, the unit had 106 patients with SARS-CoV-2 of whom 15 required RRT. The median duration spent on RRT was 188 hours (range 24-677). Eight patients were managed exclusively on the adjusted protocol. The average lifespan of a filter in SARS-CoV-2 patients on the standard protocol was 37 hours compared to 45 (range 6-70) hours using the adjusted protocol. The median number of filters per patient per RRT day on the adjusted protocol was 0.3 (range 0.2 -1). It also allowed more therapy to be delivered with patients spending on average 79% of the day on RRT.
There were no adverse bleeding outcomes and no documented evidence of citrate toxicity or acid-base disturbances
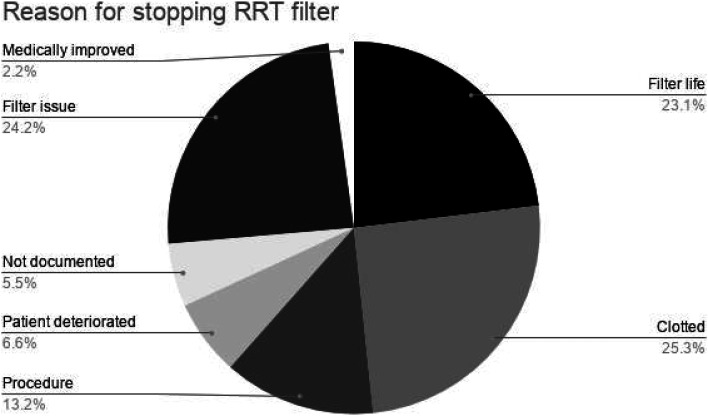
Conclusion: This small study showed an increase in filter life for patients on an increased citrate dose protocol of CVVHDF without any adverse outcomes. This results in cost savings and more appropriate resource usage during a pandemic without increased bleeding risk. Another suggested measure to reduce frequent filter malfunctions was that centres returned to using heparin anticoagulation, but this is known to have increased bleeding risk.4
References
1. Hirsch JS, Ng JH, Ross DW, et al. Acute kidney injury in patients hospitalized with COVID‐19. Kidney Int. 2020;98:209‐218.
2. Shankaranarayanan D, Muthukumar T, Tarek Barbar T, et al. Anticoagulation Strategies and Filter Life in COVID-19 Patients Receiving Continuous Renal Replacement Therapy. CJASN 2021; 16(1): 124-126.
3. Argenziano MG., Bruce SL, Slater CL. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. 2020;369:m1996.
4. M Bai, M Zhou, L He, et al. Citrate versus heparin anticoagulation for continuous renal replacement therapy: an updated meta-analysis of RCTs. Intensive Care Med. 2015;41(12):2098-2110.
P041
Reducing harm from Covid-ICU proning related peripheral neuropathies – comparing patient outcomes for 2020 and 2021 surges and recommendations for future care
COVID-19
Jack Jeffrey, Emma Cahill, Caroline Miller, Joel O’Sullivan, Andrew Sanders and Dominic Power
University Hospitals Birmingham NHS Foundation Trust
Abstract
Introduction: Prone positioning is commonly used when treating ventilated Covid-19 patients. Whilst there have been some reports of ICU proning-related injuries to the brachial plexus well before the pandemic (Goettler et al. 2002), it is usually a very uncommon complication.
Despite guidance from the Faculty of Intensive Care Medicine on the care of the proned patient, cases of peripheral neuropathies following ICU admission have significantly increased during the Covid-19 pandemic at our centre (Miller et al. 2021).
Nerve injury is associated with reduced quality of life, impaired activity participation and persistent pain (Bailey et al. 2009).
Objectives: The aim of this quality improvement project was to identify the effect that new guideline development and related healthcare professional education had on the number and severity of peripheral neuropathies identified following Covid-19 ICU admission.
Methods: Between March 2020 and May 2021, we collected clinical data from patients who sustained peripheral neuropathies during their inpatient stay for Covid-19. Data were collected via face-to-face patient assessments within acute nerve clinics or post-ICU rehabilitation wards. A grading system was used to categorise the peripheral nerve injuries into severe, intermediate and mild (Power et al. 2020).
Electronic ICU clinical noting was examined to identify the frequency and duration of each proning episode for each patient who presented with nerve injury. Following the first surge in 2020 updated proning guidelines were developed with ICU team leaders and disseminated. This involved face-to-face education of frontline staff.
Results: At our centre 93 patients survived Covid ICU between March - June 2020 (surge 1) and 21 of those sustained nerve injury (22.58%). 309 patients survived Covid ICU between September 2020 - May 2021 (surge 2) and 12 of those sustained nerve injury (3.88%).
For patients who sustained nerve injury, the average number of prones changed between surges from 6 to 13. The average duration of each episode of proning changed from 17.8hrs to 18.6hrs.
Despite the increase in prone frequency, nerve injury occurrence reduced (proportionate to the number of patients who survived Covid ICU) by 82%. 14/21 (66%) injuries acquired in the first surge were of high grade and 4/12 (33%) were of high grade during the second surge.
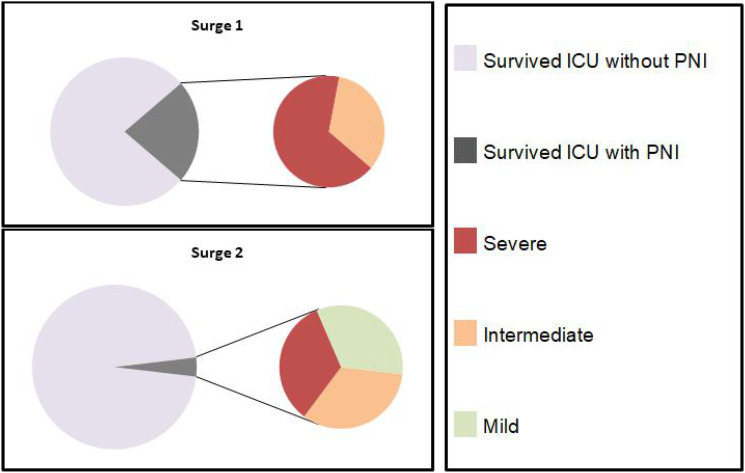
Conclusion: Optimising positioning of the proned ventilated patient may reduce the incidence of nerve injury. However, we must also acknowledge that changes in medical management between surges (i.e. use of dexamethasone, remdesivir) may have contributed to this.
Individuals still developed severe injury despite this change in practice. Further research looking into risk factors and further methods of optimising the prone positioning on ICU is warranted to reduce the occurrence of this potentially life-changing injury.
References
1. Goettler CE, Pryor JP and Reilly PM. Brachial plexopathy after prone positioning. Crit Care 2002; 6 (6); 540–542.
2. Miller C, O'Sullivan J and Jeffrey J, et al. Brachial plexus neuropathies during the COVID-19 pandemic: a retrospective case series of 15 patients in critical care. Phys Ther 2021; 101 (1); pzaa191.
3. Bailey R, Kaskutas V and Fox I, et al. Effect of upper extremity nerve damage on activity participation, pain, depression, and quality of life. J Hand Surg Am 2009; 34(9); 1682-1688.
4. Power D, Miller C & O’Sullivan J, et al. A response to: Commentary on Prone Position Plexopathy during the COVID-19 pandemic, https://www.boa.ac.uk/resources/knowledge-hub/a-response-to-commentary-on-prone-position-plexopathy-during-the-covid-19-pandemic.html (2020, accessed 3 August 2021).
P042
Use of Procalcitonin in critical care unit as a guide to antibiotics use in COVID -19 patients
COVID-19
Chidiebele Ikenga
Lancashire Teaching Hospitals Foundation Trust
Abstract
Introduction: At the start of the pandemic first wave in March 2020, it was observed the usual markers of infection like the white blood cells (WBC) and c-reactive proteins (CRP) were also much elevated in patients in COVID -19 patients too. This made it difficult to differentiate the viral response from bacterial co-infection which were often present in patients. Our centre in the at the later stages of the first waves, commenced the use of Procalcitonin (PCT) as a possible guide to antibiotics use.
Procalcitonin (PCT) is a biomarker used to predict likelihood of bacterial infection.1 It is a 114 amino acid peptide precursor of calcitonin hormone. In absence of infection, gene expression down regulated and restricted to neuroendocrine glands, leads to regulated peptide secretion and no increase in procalcitonin.2,3 The reverse occurs in presence of bacterial infection where gene expression is unregulated.
Objectives:
• Evaluate the use of Procalcitonin (PCT) as a guide of antibiotics use
• Evaluate the correlation between pro-calcitonin and other inflammatory markers
• Evaluate the use of PCT trend in determining the continuation and de-escalation of antibiotics and relationship to outcome
• To evaluate if the trust guidelines on PCT use is being followed
Methods: This was a Retrospective study. Data of Covid-19 patients admitted in ICU of Royal preston hospital from 3 march to 1 June 2020 were reviewed. Initially at the start of COVID-19, PCT test was not readily available, and its use restricted to ICU and emergency department. The study population was grouped into two groups of patients
• those that did not have PCT done and
• group that had PCT tests done during their stay in the critical care unit. Study done between 6 June and 15 August 2020
Medical records were obtained from the hospital’s medical online system Quadramed and allied records. Data collection and statistical analysis were with Excel and STAT Direct respectively
Results: Data from 53 patients were used in this study. They were categorized into PCT and non PCT groups with 25 patients belonging to the PCT group. There was positive correlation between PCT and Inflammatory markers in the PCT group. There was a correlation between rise in PCT and positive culture after septic screens. There is a significant difference in duration of antibiotics use in both groups with calculated p value of 0.0085. There was no significant difference in mortality across both groups.
Conclusions:
• There was good compliance with trust antibiotics guidelines and PCT use
• Observed Correlation between measured inflammatory markers and PCT
• Significant relationship between reduced duration of antibiotics and PCT use
References
1. Christ-Crain M, Müller B. Procalcitonin in bacterial infections--hype, hope, more or less? Swiss Med Wkly. 2005;135(31–32):451-460. PMID: 16208582
2. S. F. Mitsuma, M. K. Mansour, J. P. Dekker, J. Kim, M. Z. Rahman, A. Tweed-Kent, P. Schuetz, Promising New Assays and Technologies for the Diagnosis and Management of Infectious Diseases, Clinical Infectious Diseases, Volume 56, Issue 7, 2013, Pages 996–1002
3. DynaMed. Procalcitonin-guided Antibiotic Therapy. EBSCO Information Services. Accessed August 19, 2020. https://www.dynamed.com/drug-review/procalcitonin-guided-antibiotic-therapy
P043
Intensive Care Unit Therapy Support Worker - Response to the COVID 19 Pandemic
COVID-19
Rachel Blake 1 , Jennifer Wainwright1, Zoe Van Willigen2 and Rachel Corbett1
1University Hospital Southampton
2University Hopsital Southampton
Abstract
Background: We are a team of four Therapy Support Workers, who work on GICU on the Early Mobilisation Project (EMP). We have highlighted the response of our role during the first and second surge as we were unable to complete our traditional job role on EMP due to a variety of factors.
The first surge saw an increased number of redeployed staff and a shortage of PPE, so we began the RESTORE project (REhab Step-down Therapy OutrEach). During the second surge we saw an increased number of patients, increased BMI and increased dependency and this resulted in an un-manageable caseload of patients stepping down to the wards. This led to the PIRT project (Post Intensive care Rehab Team).
Method: RESTORE was created in response to help with the transition from GICU to the ward, as it is well documented that this transition can feel like ‘falling from a cliff’. Therapists would visit GICU step down patients on the ward to manage expectations, give timely information about their ICU stay, and reassure patients around anxiety, flashbacks and nightmares.
The PIRT team treated patients from GICU on the wards and focused on those needing assistance of two or more for their rehab. This allowed the ward team to manage their already busy caseload of patients and discharge planning, while PIRT focused on physical and non-physical therapy sessions of GICU step down patients. With the addition of this team, it allowed for longer sessions with patients and enabled them to progress their rehab with adequate staff to support them.
Results: Both projects were hugely successful, we were able to help patients and colleagues throughout the pandemic as our job role evolved and adapted. Neither project was sustainable due to staffing needs, but it is something we would love to have funding for in the future.
From the PIRT project, we helped to reduce length of stay from 25.5 days to 16, we gave 231 therapy inventions over a 5-week period, which included a holistic approach of trips outside, shopping, cooking, showing and visits to chaplaincy as well as physical rehab such as standing and walking.
The feedback given from patients during both projects highlighted how much of an impact we made and how beneficial it could be going forward. “It felt … like having a family member come and visit whilst they couldn’t have their own in”. “Positivity it gives to patients is priceless.” When asked “Overall how would you evaluate the rehab team?” “Indisposible”.
Conclusions: Both projects were a joining of forces as we worked cohesively with colleagues on different wards and in different teams. RESTORE and PIRT helped with providing a holistic journey and continuity for patients. The project naturally incorporated the University Hospital Southampton’s values of working together, patients first and always improving, and we were proud of all that was achieved.
P044
Any place for dead space? A retrospective cohort study of the diagnostic utility of alveolar dead space fraction for pulmonary embolism in COVID-19 patients
COVID-19
John O’Rourke, Daniel Horner and Bethany MacDonald
Salford Royal NHS Foundation Trust
Abstract
Introduction: The difference between the end-tidal carbon dioxide (ETCO2) and arterial carbon dioxide (PaCO2) represents alveolar dead space. This is commonly characterised as the alveolar dead space fraction (AVDSf), which is calculated using the equation (PaCO2 - ETCO2)/PaCO2. The AVDSf can be easily calculated in the intensive care unit using routinely documented data.
Pulmonary embolism (PE) increases dead space and so it is hypothesised that AVDSf may be a useful diagnostic tool for PE. Research in the Emergency Department setting has shown that AVDSf can help exclude PE when combined with other diagnostic tests.
Patients with COVID-19 are at high risk of concurrent PE but diagnosis in invasively ventilated patients is challenging due to limitations with routine assessment, infection control issues and clinical instability. No studies have assessed the potential role of AVDSf in this diagnostic process.
Objective: We sought to investigate the diagnostic utility of AVDSf prior to Computed Tomography Pulmonary Angiogram (CTPA) in invasively ventilated patients with COVID-19 and suspected PE.
Methods: This was a retrospective, single-centre cohort study, delivered as a service evaluation with formal R&D approval and oversight (Ref: S20HIP17). All invasively ventilated patients with confirmed COVID-19 who underwent CTPA between March 2020 and April 2021 at a large UK intensive care unit were included. AVDSf values were derived from routine data taken at the closest available timepoint prior to the CTPA. Consultant radiologist reporting of the CTPA images was used as the reference standard for PE diagnosis.
Results: 48 CTPAs were included in the final analysis. Therapeutic-dose anticoagulation was given before CTPA in 45.8% (n=22) of cases. The mean pre-CTPA PaO2/FiO2 (P/F ratio) was 134 mmHg (IQR 56.1). The 28-day mortality was 70.4%.
52.1% of CTPAs demonstrated a PE (n=25). Of these PEs, 8 were classified as central or lobar, 11 as segmental and 6 as subsegmental. The mean difference in AVDSf between PE positive CTPA and PE negative CTPA was 0.02 (0.34 vs 0.32). This difference was not statistically significant (p=0.255). At a threshold of 0.33 the sensitivity was 0.56 and specificity was 0.48. AVDSf did not provide diagnostic utility at any cut-off point (AUC=0.561).
Conclusion: This study is the first to investigate the utility of AVDSf in diagnosing PE in COVID-19 patients. Our findings suggest there is no value in using single AVDSf values to guide decisions on diagnostic imaging in patients with severe COVID-19 and suspected PE. Given research has demonstrated the potential for AVDSf to reduce imaging requests in patients with a low pre-test probability of PE, further research may be appropriate in ambulatory COVID-19 patients. Additionally, the interpretation of trends in AVDSf, rather than its calculation at a single timepoint, could be investigated as a diagnostic tool for PE in critically unwell, ventilated patients.
P045
Oxygen indices in COVID-19 mechanically ventilated patients with acute hypoxic respiratory failure: A cohort study
COVID-19
Luke Bracegirdle, Alexander Jackson, Michael Grocott, Andrew Cumpstey and Ahilanandan Dushianthan
University Hospital Southampton NHS Foundation
Abstract
Introduction: Hypoxic respiratory failure, a hallmark of severe COVID-19, often requires oxygen therapy.1 Mechanical ventilation carries a high mortality.2 We evaluate trends in oxygen indices (PaO2/FiO2 ratio, CaO2, O2ER) in COVID-19 patients throughout an intensive care admission and correlation with clinical outcomes.
Objectives: To establish the trends in oxygen indices in mechanically ventilated adult COVID-19 patients throughout an intensive care admission.
Methods: We performed a retrospective observational cohort study in a UK university hospital (ethics through REACT COVID-193), including all adult COVID-19 patients requiring mechanical ventilation between 01/03/20 and 31/03/21. We collected baseline characteristics, clinical outcomes and oxygen parameters.
Results: 184 patients met inclusion criteria, providing 34592 blood gas data points over 30-days. The median age was 59.5 (IQR 51, 67), and median BMI 30 (IQR 25.8, 35.5). The majority were men (62.5%) of white ethnicity (70.1%). Median mechanical ventilation duration was 15-days (IQR 8, 25) and 133 patients (72.3%) survived 30-days. Oxygen indices are presented in Table 1. Non-survivors exhibited lower oxygen extraction; there was an averaged mean difference in O2ER of -0.06 (95% CI -0.09, -0.03) across days one to seven and -0.09 (95% CI -0.10, -0.07) across days one to 30. While both survivors and non-survivors had sub-physiological CaO2 (which trended down throughout their ICU admission), non-survivors tended to exhibit higher values; there is an averaged mean difference of 0.23 (95% CI 0.13, 0.34) across day one to day seven and 0.28 (95% CI 0.21, 0.35) across days one to 30.
Table 1.
Oxygen indices. 95% CI, 95% confidence interval; CaO2, ml O2 100ml-1 arterial blood; FiO2, fraction of inspired oxygen; PaO2, partial pressure of arterial oxygen.
| Oxygen variable | Survivors | Non-Survivors | Difference | 95% CI | p-value |
|---|---|---|---|---|---|
| PaO2 (kPa) | |||||
| Day 1 | 10.46 | 10.19 | -0.27 | -0.64, 0.10 | 0.16 |
| Day 2 | 10.02 | 9.63 | -0.40 | -0.65, -0.15 | <0.01 |
| Day 3 | 9.80 | 9.41 | -0.40 | -0.64, -0.15 | <0.01 |
| Day 4 | 9.67 | 9.32 | -0.36 | -0.58, -0.13 | <0.01 |
| Day 5 | 9.67 | 9.04 | -0.62 | -0.83, 0.41 | <0.01 |
| Day 6 | 9.58 | 9.17 | -0.41 | -0.66, -0.17 | <0.01 |
| Day 7 | 9.76 | 9.39 | -0.37 | -0.64, -0.09 | <0.01 |
| Day 1-7 | 9.86 | 9.48 | -0.38 | -0.49, -0.28 | <0.01 |
| Day 1-30 | 9.81 | 9.23 | -0.58 | -0.65, -0.52 | <0.01 |
| PaO2 (kPa)/FiO2 ratio | |||||
| Day 1 | 19.93 | 19.12 | -0.82 | -1.75, 0.12 | 0.09 |
| Day 2 | 20.80 | 19.37 | -1.44 | -2.28, -0.59 | <0.01 |
| Day 3 | 20.54 | 17.91 | -2.64 | -3.41, -1.87 | <0.01 |
| Day 4 | 20.50 | 16.40 | -4.10 | -4.83, -3.38 | <0.01 |
| Day 5 | 19.83 | 16.02 | -3.81 | -4.56, -3.06 | <0.01 |
| Day 6 | 19.48 | 15.43 | -4.05 | -4.88, -3.21 | <0.01 |
| Day 7 | 20.47 | 14.68 | -5.80 | -6.50, -5.09 | <0.01 |
| Day 1-7 | 20.22 | 17.16 | -3.06 | -3.38, -2.75 | <0.01 |
| Day 1-30 | 21.87 | 15.17 | -6.71 | -6.90, -6.52 | <0.01 |
| CaO2 (ml/dL) | |||||
| Day 1 | 16.04 | 16.35 | 0.31 | 0.06, 0.56 | 0.02 |
| Day 2 | 15.46 | 15.80 | 0.34 | 0.09, 0.59 | <0.01 |
| Day 3 | 15.11 | 15.29 | 0.17 | -0.08, 0.43 | 0.19 |
| Day 4 | 14.89 | 14.99 | 0.10 | -0.15, 0.35 | 0.44 |
| Day 5 | 14.57 | 14.71 | 0.14 | -0.14, 0.42 | 0.33 |
| Day 6 | 14.26 | 14.40 | 0.14 | -0.14, 0.42 | 0.32 |
| Day 7 | 13.99 | 14.02 | 0.03 | -0.28, 0.33 | 0.86 |
| Day 1-7 | 14.93 | 15.16 | 0.23 | 0.13, 0.34 | <0.01 |
| Day 1-30 | 13.48 | 13.76 | 0.28 | 0.21, 0.35 | <0.01 |
Conclusions: As a novel cause of respiratory failure, COVID-19 offers a unique opportunity to study a homogenous cohort. In mechanically ventilated adult COVID-19 patients, oxygen indices are abnormal. Despite having similar CaO2 values, oxygen extraction differs significantly between survivors and non-survivors, suggesting COVID-19 causes impaired oxygen utilisation. Urgent further evaluation is warranted.
References
1. Sivaloganathan AA, Nasim-Mohi M, Brown MM, et al. Noninvasive ventilation for COVID-19-associated acute hypoxaemic respiratory failure: experience from a single centre. British Journal of Anaesthesia, Elsevier; 2020; 125(4): e368-e371
2. ICNARC. ICNARC report on COVID-19 in critical care: England, Wales and Northern Ireland [Internet]. Intensive care national audit & research centre; 2021 Available from: https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports
3. Burke H, Freeman A, Dushianthan A, et al. Research Evaluation Alongside Clinical Treatment in COVID-19 (REACT COVID-19): an observational and biobanking study. BMJ Open 2021; 11: e043012
P046
A Service Evaluation of Venous Thromboembolism Prophylaxis Dosing during the first COVID-19 wave in the Intensive Care Unit, Queen Alexandra Hospital Portsmouth
COVID-19
Chloe Parfit and Jonarthan Thevanayagam
Queen Alexandra Hospital
Abstract
Introduction: In December 2019 the first case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified. Its predominant features are respiratory symptoms; however, in severe disease, coagulopathy is commonplace. Published reports from the early pandemic and emerging evidence described an increased incidence of venous thromboembolism (VTE) in these patients.
Objectives: Evaluation of changes in VTE prophylaxis in patients with COVID-19 and its impact on VTE rates.
Method: We performed a service evaluation of all patients admitted to ICU at Queen Alexandra Hospital (QAH) Portsmouth with confirmed COVID-19. Patients admitted from 10/03/2020 to 12/05/2020 were included. Interrogation of the computerised clinical and radiology systems were used. Patients were investigated for VTE based on clinical suspicion and observed until discharge from ICU, death, or transfer. We also evaluated adverse bleeding risks.
Standard thromboprophylaxis for QAH is Enoxaparin, as per tables 1 and 2.
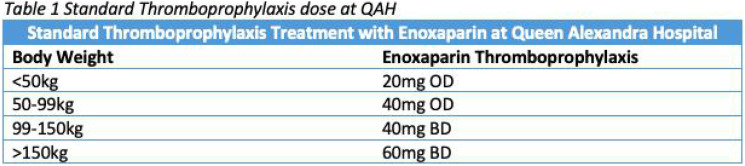
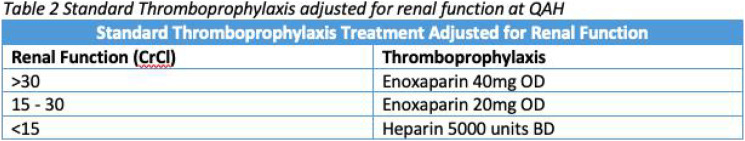
Covid enhanced prophylaxis is defined in table 3.
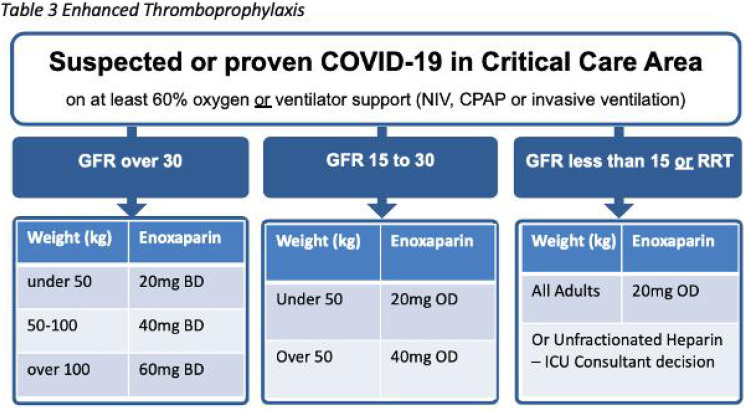
Results: 69 patients were admitted to ICU at QAH between 10/03/2020 to 12/05/2020 with confirmed COVID-19. Of these patients 37 were investigated for VTE. 17 patients had a thromboembolic event. 15 patients had a PE, of which 2 also had embolic strokes. 2 patients had a DVT. 45 patients received standard thromboprophylaxis, 18 received COVID prophylaxis, 4 received treatment dose, and 1 patient received no thromboprophylaxis. Data was unavailable for 1 patient. Adverse events were only found in 1 patient receiving treatment dose and the patient not on thromboprophylaxis.
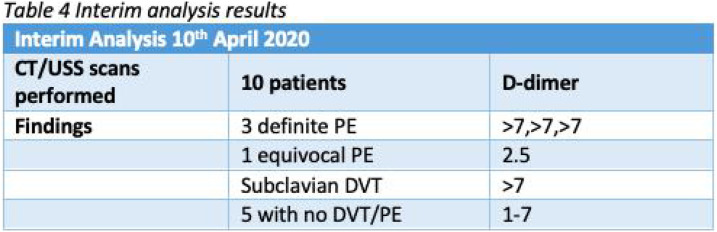
After interim analysis, on the 11th April 2021, the ICU venous thromboprophylaxis policy was changed to enhanced prophylaxis for patients being treated for COVID-19.
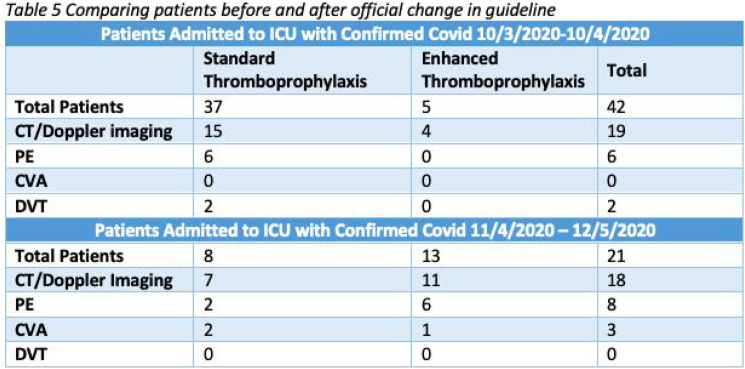
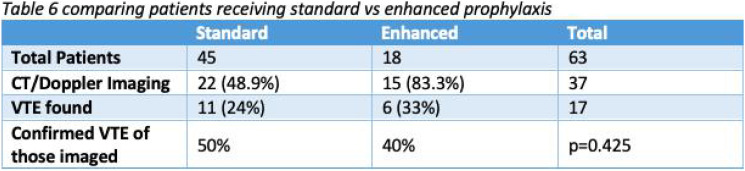
Conclusions: This evaluation was able to identify early the increased risk of VTE in COVID patients, and the utility of d-dimers to help consider VTE. The interim analysis demonstrated 50% of patients investigated had confirmed VTE. Following this analysis, along with emerging evidence and recommendations by national bodies, the VTE prophylaxis guideline was changed on the 11 April 2020 to enhanced dosing.
The overall rate of confirmed VTE in our cohort was 27%. However, of those who underwent CT imaging, positive findings were found in 46%. 85% of patients admitted after 10/4/2020 were investigated for VTE, which reflects increased recognition of the issue and team confidence in transferring COVID patients. Owing to the low initial imaging rate, the evaluation is likely to have underestimated thrombosis rates.
Comparing VTE rates between those who received standard and enhanced VTE prophylaxis showed no significant effect (p-value 0.425), indicating that VTE prophylaxis is unlikely to confer substantial benefit, and the low adverse event rates in both groups signal no significant harm from enhanced prophylaxis.
In conclusion, this study demonstrates VTE is a significant concern in patients being treated for COVID-19 in an ICU setting. Non-peer reviewed data from large trials, suggest that anticoagulation may be of benefit in hospitalised but not intensive care patients. We continue to be guided by current evidence and still implement enhanced thromboprophylaxis in our guideline despite the equipoise demonstrated.
References
1. Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. [Internet] 2020;18(6):1421-1424. Available from: https://pubmed.ncbi.nlm.nih.gov/32271988/doi:10.1111/jth.14830
2. Malas MB, Naazie IN, Elsayed N, Mathlouthi A, Marmor R, Clary B. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: A systemic review and meta-analysis. Lancet 2020;29:100639. Available from: https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30383-7/fulltext doi: 10.1016/j.eclinm.2020.100639
3. British Thoracic Society. BTS Guidance on Venous Thromboembolic Disease in patients with COVID-19. BTS; 2020 [updated 2021 Feb; cited 2021 Aug]. Available from: https://www.brit-thoracic.org.uk/document-library/quality-improvement/covid-19/bts-guidance-on-venous-thromboembolic-disease-in-patients-with-covid-19/
4. REMAP-CAP. Therapeutic anticoagulation for patients with severe COVID-19. [internet]. 2020. Available from: https://www.remapcap.org/covid19publications/therapeutic-anticoagulation-for-patients-with-severe-covid-19
5. Berger J, Connors J. Anticoagulation in COVID-19: reaction to the ACTION trial. Lancet 2021; 397(10291):2226-2228. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)01291-5/fulltext
P047
Intensive Care COVID positive admissions and outcomes in relation to frailty parameters
COVID-19
Matthew Jones 1 , Christian. P Subbe2 and Chris Thorpe3
1Cardiff University
2Bangor University
3Department of Anaesthetics, Ysbyty Gwynedd
Abstract
Introduction: Frailty assessment using the Clinical Frailty Scale (CSF),1 has been incorporated into COVID decision aids; frailty highlights risk of poor outcome which can guide future care.2 The ITU patient population has trended towards a younger, fitter and less co-morbid population.3 Yet COVID is a disease that disproportionately effects the elderly; people aged over 65 years represent more than 50% of ITU admissions and account for 80% of mortality.4 There are subsequent ethical considerations as to how resources were and continue to be allocated; an understanding of how frailty has impacted clinical decisions can drive improvements in future practice (5). Frailty has sustained relevance in a critical care environment with continual scarcity of resources.3
Objectives: To undertake a service evaluation of the mortality and hospital outcomes of positive COVID patients admitted to Ysbyty Gwynedd ITU from 01/03/2020 to 01/06/2021. To consider the effect of measured pre-admission frailty of patients on ITU admissions and outcomes.
Method: Service evaluation of outcomes for patients testing positive for COVID-19 and admitted to Intensive Care. Patients aged 18 or over were considered eligible for the evaluation and patients with suspected COVID that tested negative were excluded. Retrospective data was sourced from the ICNARC database, handover notes and clinical files. CFS scores were used to dichotomise the cohort into two distinct groups; one group with CFS scores 1-4 was defined as fit or vulnerable and the second group scoring between 5-9 was defined as frail. Patients were then assigned a pandemic ‘wave’ based on their date of admission: admission between 01/03/2020 to 01/09/2020 were assigned ‘Wave 1’ and between 01/09/2020 to 01/06/2021 ‘Wave 2’.
Results: 72 COVID patients were included in the service evaluation; 65% of patients were male, the mean age was 59 years (SD 13) and the mean ICNARC score was 13.4 (SD 6.8). The overall in-hospital mortality was 30.6%. The frail group of patients experienced worse outcomes than their fitter counterparts; in-hospital mortality rate was higher (35.8% vs 29.3%), mean LOS in survivors longer (25 vs 17 days), and ventilator use more frequent (64.3% vs 46.6%). The average CFS score of the admitted ITU patient increased over time (see Figure 1). In Wave 1 5.9% of admitted patients were classified as frail compared to 21.8% in the Wave 2.
Figure 1.
shows how the CFS of admitted ITU patients varied between Wave 1 and Wave 2.
Conclusions: Frailty is a useful tool to highlight risk of poor outcome in COVID patients. A higher proportion of frail patients were admitted in Wave 2; this could indicate a greater confidence to treat this patient population with fewer resource constraints. It is important to consider frailty alongside broader clinical information for use in clinical decision making regarding ITU intervention and subsequent pathways of care. Frailty might be an important tool to ensure care does not disadvantage those who can be considered both fit and elderly.
References
1. Pugh RJ, Ellison A, Pye K, Subbe CP, Thorpe CM, Lone NI, et al. Feasibility and reliability of frailty assessment in the critically ill: a systematic review. Critical Care. 2018;22(1):1-11.
2. Moug S, Carter B, Myint PK, Hewitt J, McCarthy K, Pearce L. Decision-making in COVID-19 and frailty. Multidisciplinary Digital Publishing Institute; 2020.
3. Pugh RJ, Bailey R, Szakmany T, Al Sallakh M, Hollinghurst J, Akbari A, et al. Long‐term trends in critical care admissions in Wales. Anaesthesia. 2021.
4. Hubbard RE, Maier AB, Hilmer SN, Naganathan V, Etherton-Beer C, Rockwood K. Frailty in the face of COVID-19. Age and ageing. 2020.
5. Lamblin A, de Montgolfier S. COVID-19 and ethical considerations: valuable decision-making tools from the leading medical societies in France. Anaesthesia, critical care & pain medicine. 2020;39(3):365.
P048
Utilising anti-Xa for monitoring therapeutic heparin during COVID-19
COVID-19
John Warburton and Mariam Gebahi
University Hospitals Bristol & Weston NHS Foundation Trust
Abstract
Introduction: There are increased rates of thrombotic events such as strokes, pulmonary embolism, cutaneous and alveolar micro-thrombosis in COVID-19 patients in intensive care.1,2 Using anti-Xa, which is a direct measure of heparin activity, for dose titration leads to a greater time in therapeutic range and fewer dose adjustments than using APTTr.3 It was considered therefore that anti-Xa would be a more accurate method for monitoring heparin dosing in COVID-19 patients.
Objectives:
• To analyse and compare APTTr versus anti-Xa during therapeutic heparin monitoring in critical care patients with Covid-19
•To assess compliance with a new anti-Xa heparin monitoring protocol using the following standards (expected 100%). COVID-19 positive patients in critical care prescribed heparin:
1. Must have an Anti-Xa level test 5-7 hours after starting the infusion (target 6 hours)
2. Must have the correct dose alteration in response to the Anti-Xa levels
3. Must have received an adjustment of the heparin infusion rate within 2 hours of the Anti-Xa level result
Methods: From April 2020 both anti-Xa levels and APTTr were run concurrently on the same blood sample for all COVID-19 positive patients receiving therapeutic unfractionated heparin on critical care. The reference ranges used were ≥0.5 to <0.8 and ≥1.5 to <2.5 respectively. The results were mapped against the respective dosing titration protocols to determine the discrepancy rate in assessing whether levels were low, in range or high for each test.
Following the implementation of a new therapeutic unfractionated heparin titration protocol, using anti-Xa instead of APTTr in COVID-19 patients, an audit was conducted in these patients to determine the adherence to the new protocol. Audit data collected retrospectively April to June 2020 inclusive from Philips and ICE.
Results: Therapeutic unfractionated heparin was given to 24 Covid-19 positive patients between April and December 2020 with a total of 482 samples (mean 20 samples per treatment course). The agreement rate between anti-Xa and APTTr was 44% i.e. results were both in range, both low or both high. In 35% of the paired samples the anti-Xa was judged to be in range, whereas the APTTr result suggested a dose increase was needed.
The shorter audit period highlighted 13 eligible patients (59 paired samples) on therapeutic heparin during audit period. The adherence to standards 1,2 and 3 were 67%, 98% and 95% respectively. 21 sample results were excluded from standard 3 because the time of rate adjustment or acknowledgment was not recorded. For the remainder the mean time to adjustment of infusion rate following a sample being sent was 42 minutes.
Conclusion: The 56% discordance rate is higher than reported elsewhere in the literature (46-49%) potentially demonstrating the effect of COVID-19 on APTTr reliability. The high rate of disagreement between the two tests suggests that if APTTr had been used for dosing in COVID-19 patients that significantly higher rates of heparin would have been used. With respect to the audit element sample timing and documentation of result acknowledgement, regardless of whether it necessitates a change in rate or not, needs to be improved.
References
1. Adie SK, Farina N. Impact of COVID-19 on monitoring of therapeutic unfractionated heparin [published online ahead of print, 2020 Aug 19]. Journal of Thrombosis and Thrombolysis. 2020;1-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7437961/. (accessed 28 December 2020).
2. Mondal S, Quintili A.L, Karamchandani, K, Bose S. Thromboembolic disease in COVID-19 patients: A brief narrative review. Journal of intensive care 2020; 8(70) 2020. https://jintensivecare.biomedcentral.com/articles/10.1186/s40560-020-00483-y (accessed 28 December 2020).
3. Whitman-Purves E, Coons JC, Miller T, DiNella JV, Althouse A, Schmidhofer M, Smith RE. Performance of Anti-Factor Xa Versus Activated Partial Thromboplastin Time for Heparin Monitoring Using Multiple Nomograms. Clin Appl Thromb Hemost. 2018; 24(2):310-316.
P049
Effect of Dexamethasone protocol on peak C-reactive protein, incidence of positive blood cultures and ICU mortality in invasively ventilated SARS-CoV-2 patients
COVID-19
Marat Mazalkou and Hannah Hildrey
Peterborough City Hospital
Abstract
Introduction: Severe COVID-19 viral pneumonitis, requiring invasive mechanical ventilation, has a mortality rate approaching 45%.1 The RECOVERY trial demonstrated that Dexamethasone protocol (6 mg a day for up to 10 days, commenced early) decreased 28 days’ mortality for this cohort from 41.4% to 29.3% (OR 0.64; 95% CI 0.51-0.81).2 More generally, a study confirmed corticosteroids’ beneficial effect in COVID-19 patients which was more prominent in females, younger patients (<65) and with higher C-reactive protein (CRP) levels (in excess of 150 mg/L). Importantly, it did not increase incidence of bacteremia or fungemia.3 In another study, responders to corticosteroids (more than 50% of CRP levels reduction in 72 hours) had reduced risk of death ( 25.2% vs. 47.8% in non-responders; OR 0.37, P<0.001).4
In our district general hospital, the Dexamethasone protocol was introduced and used consistently at the beginning of COVID-19 second wave. Therefore, an impact of this intervention could be detected by comparing the outcomes between SaRS-CoV-2’ patients admitted during Wave-1 versus Wave-2.
Concomitant antibiotics (Co-amoxiclav and Clarithromycin) were introduced at the same time, but this practice varied.
Objectives: To detect impact of Dexamethasone protocol on COVID-19 invasively ventilated ICU patients’ outcomes by using retrospective analysis.
Methods: The information on ICU mortality, peak CRP levels (irrespectively of peak-time, but most manifested within 10 days from admission) and incidence of positive blood cultures (if resulted from both sampling tubes) was collected from trust databases after the last patient’s ICU discharge.
Wave-1 was defined as SARS-CoV-2 PCR confirmed patients admitted to the hospital from 1/3/2020 until 31/5/2020. Wave-2 period was from 1/10/2020 until 28/2/2021.
Mann Whitney U test was used for CRP numbers.
Results: Number of ICU patients requiring mechanical ventilation: 34 (W-1) versus 39 (W-2). There was no statistical difference in age and gender. ICU mortality was: 41% (W-1) versus 44% (W-2). Incidence of bacteremia was: 24% (W-1) versus 46% (W-2). The bulk of the difference was due to coagulase negative coccal flora and Staphylococcus epidermidis; increase from 1 to 11 cases.
Medians (quartiles 1 - 3) of peak CRP levels were: 336 (264 - 415) (W-1) versus 264 (172 - 379) (W-2), P-0.042. The difference was even more pronounced when looking at peak CRPs of W-2 survivors: median 234 (150 - 270). It was statistically significant for this group in comparisons between W-2 non-survivors and W-1 survivors, P - 0.021 and 0.017 correspondingly.
Conclusion: Our data (bearing in mind loss of some due to inter-hospital transfers and overall limited numbers) did not demonstrate any significant difference in ICU mortality of mechanically ventilated patients which could be attributed to the protocol.
Statistically significant differences in average peak CRP levels between the COVID-19 waves (especially for Wave-2 ICU survivors) may be explained by the Dexamethasone protocol impact. This agrees with previous data.4
There was a significant increase in incidence of positive blood cultures due to bacterial flora usually considered contaminants.
References
1. Zheng JL, et al. Case fatality rates for patients with COVID-19 requiring invasive mechanical ventilation, a meta-analysis. Am J Respir Crit Care Med 2021; 203(1): 54-66
2. The RECOVERY Collaborative Group. Dexamethasone in hospitalised patients with COVID-19. N Engl J Med 2021; 384: 693-704
3. Ho KS, et al. Impact of corticosteroids in hospitalised COVID-19 patients. BMJ Open Respiratory Research 2021; 8: e000766.
4. Cui Z, et al. Reduction in C-reactive protein levels after corticosteroid therapy is associated with reduced mortality in patients with COVID-19. J Hosp Med 2021; 16(3): 142-148
P050
Non-invasive ventilation strategy and outcomes of patients with Covid-19 acute hypoxic respiratory failure: A retrospective observational study
COVID-19
Rob Mackay 1 , Rebecca Egglestone2 and Ahilanadan Dushianthan2
1Royal Bournemouth Hospital
2University Hospital Southampton
Abstract
Introduction: COVID-19 has presented as a wide spectrum of severity, from asymptomatic transmission to acute hypoxic respiratory failure (AHRF). Non-invasive ventilation (NIV) has been increasingly used during the pandemic, partially driven due to resource constraints. There has, however, been varying opinions of the best strategy managing the acute hypoxic respiratory failure, of immediate versus delayed intubation, and the role of NIV.
Objectives: With this trial we aimed to explore non-invasive ventilation as a primary ventilation strategy with its outcomes. Also, looking at duration of therapy and associated patient characteristics which may help predict NIV success or failure.
Method: This was a single-centre retrospective observational study (REC reference 17/NW/0632) between 19/3/20 and 12/3/21. Patients managed with NIV only or NIV prior to invasive mechanical ventilation (IMV) were included. Patients receiving only NIV outside ICU and NIV as part of weaning from IMV were excluded. The term NIV is used to include both continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP).
Data was taken from electronic health records used in the ICU. NIV was applied via a full facemask or a facemask covering the nose and mouth. NIV failure was defined by the need for intubation and IMV or death during hospital stay.
Results: Between 19/3/20 and 12/3/21 309 patients were admitted to ICU with confirmed Covid-19 and AHRF. Of these 250 (80.9%) were initially managed with NIV and 59 (19.1%) were intubated immediately.
Of those managed with NIV, 137 (54.8%) received NIV only, and 113 (42.5%) were subsequently intubated. 18 patients managed purely on NIV did not survive, with NIV their ceiling of treatment. Therefore 119 (47.6%) patients were successfully managed with NIV. NIV success patients were termed Group 1, NIV failure requiring IMV as Group 2. Group 2 was subdivided based on duration of NIV therapy prior to intubation.
Within Group 2, 36 (31.9%) were intubated within 24 hours (2a), 37 (32.8%) within 24-96 hours (2b) and 40 (35.4%) after more than 96 hours (2c) of NIV. The hospital mortality for groups 2a, 2b, 2c were 19.4%, 35.1% and 47.5% respectively.
Multivariate analysis showed the APACHE II score (OR 1.25, 95% CI 1.11-1.14, p<0.001) and PaO 2 /FiO 2 ratio<13.3kPa (OR 4.73, 95% CI 1.82- 13.2, p = 0.002) predicted the need for intubation and invasive mechanical ventilation.
Conclusion: Almost half the patients of the NIV cohort required eventual intubation. A high APACHE II or SOFA score and hypoxaemia on admission were significant in this group. Of note despite worse APACHE II and SOFA scores the patients who were intubated <24 hours after failing NIV had a better survival rate than those intubated later.
We were unable to comment if the poorer outcomes were due to disease progression regardless of intervention or delayed mechanical ventilation. However, nearly 50% of patients with AHRF due to Covid-19 improved without IMV and with better outcomes. While further trials are needed comparing NIV and IMV it appears that NIV can play a definite role in the management of acute hypoxaemic respiratory failure secondary to Covid-19 (Figure 2).
Figure 2.
Kaplan-Meir survival curves according to A) mode of ventilation and B) duration od NIV prior to intubation.
P051
Peer support and collaboration amongst Critical Care Outreach Teams: The role of a new regional peer support network during the Covid-19 pandemic
COVID-19
Sophie Hadfield 1 , Linzie Balshaw2, Rebecca Shields2, Valerie Osborne3, Viranga Brooks4 and Victoria Metaxa1
1Kings College Hospital NHS Foundation Trust
2Kingston Hospital NHS Foundation Trust
3Guy and St Thomas’ NHS Foundation Trust
4Princess Royal Universtiy Hosptial
Abstract
Introduction: Critical care outreach teams (CCOT) provide an outward facing service for critical care, supporting acutely unwell patients on the wards. During the last two surges of the coronavirus (Covid-19) pandemic, CCOTs played a pivotal role in providing support to ward teams. This was particularly in respect to the management of acute non-invasive respiratory support, which was being delivered outside of Critical Care areas at a scale not previously seen in the United Kingdom.
Objectives: We describe the structure, role and effect of a newly created South London Network (SLCCON) in supporting CCOT teams from different hospitals with these challenges.
Methods: SLCCON
The SLCCON was established in June 2019, and it comprises of 25 individuals, both nurses and doctors. The SLCCON represents seven hospitals within South London, including both district generals and larger tertiary referral hospitals.
The aim of the network was to explore the opportunities for collaborative working and standardisation of CCOT service delivery.
Survey: A cross-sectional, anonymous online survey (SurveyPlanet), containing 13 mixed questions, was emailed to all members of the SLCCON (n=25). The aim of the survey was to understand the impact of the network on individual and team experience.
Questions were generated by two senior team members in consultation with CCOT leads from one other hospital.
The survey was emailed in August 2021 with one reminder emailed at two weeks.
Results: Out of 14 (56%) respondents who completed the survey, 8 (57%) were service leads and 6 (43%) were team members. Eleven (79%) respondents had attended network meetings, and of these, 11 (100%) thought the network meetings had been useful in providing peer support. The main perceived benefits of the network were opportunities to collaborate with colleagues and the sharing of practice (Figure 1). In addition, respondents perceived access to guidelines from other hospitals and advice on maintaining patient safety during the pandemic to be the most important support received from the network (Figure 2). All participants expressed a wish for the network to continue. Respondents suggested further potential going forwards to share and standardise data collection and practice, and to collaborate on publications and the delivery of education.
Figure 1.
The value of the SLCCON to respondents:
Figure 2.
Type of support provided by the SLCCON during the Covid-19 pandemic
Discussion: Despite the relatively low number of responses, the results indicate a positive impact of the SLCCON. The opportunity to share practice and the provision of important wellbeing and peer support during a period of extreme pressure and stress, demonstrates the importance of the network. The future of SLCCON was associated with educational, research and data sharing opportunities
P052
COVID-19 – Thrombolysis For Acute Limb Ischaemia
COVID-19
Joseph Gavin, Eleanor Zinkin and Ruth Van Hoogstraten
The Lister Hospital
Abstract
Introduction: It is now well established that COVID-19 is linked to acute thrombosis. We present a case of an intubated and ventilated patient who received thrombolysis for acute limb ischemia. Shortly after intubation for respiratory failure secondary to COVID-19, a patient in their 50s developed a cold pulseless hand which was reviewed by vascular surgeons and radiologically diagnosed as acute arterial thrombosis resulting in an ischaemic hand.
Objectives: Provide evidence for the use of systemic thrombolysis to treat thrombotic complications of COVID-19.
Methods: Different treatment modalities were discussed within the multidisciplinary team. It was decided that the patient was unstable for transfer to theatre as he was in the proned position with severe respiratory failure. Therefore, systemic thrombolysis was administered to the patient twice over a period of 24 hours.
Results: Following administration of Alteplase the patient went on to recover perfusion to the hand as well as making a remarkable respiratory improvement. This allowed for extubation within a matter of days. The patient survived to discharge without functional limitation of the hand. 6 months post discharge the patient is working full time in a manual capacity.
Conclusions: We provide evidence that systemic thrombolysis can be considered as an option for acute limb ischemia in ventilated patients with COVID-19 for which conventional treatment options are not viable. With the knowledge that COVID-19 is a prothrombotic illness, it is possible that the thrombolysis of intercurrent pulmonary emboli contributed to respiratory recovery.
P053
Psychological impact on the healthcare professionals during covid 19 pandemic in intensive care units - a multicenter study in sri lanka
COVID-19
Krishakeesen Kamalanathan 1 , Tharuka Kalhari2 and Nayana Fernando2
1National hospital of Sri Lank
2University Hospital, Sir John Kotelawala Defence University
Abstract
Introduction: Intensive care units (ICU) health care professionals working in a challenging environment during the Covid 19 pandemic.1 Expansion of ICU provision, working long shifts with limited resources with precarious infrastructure expose them to more stressful environments and potentially affect their mental health.2
Objectives: To identify the prevalence of psychological impact and assess the associated factors among ICU health care professionals (doctors and nurses) in five Sri Lankan hospitals from July to August 2021.
Methods: It’s a descriptive study carried out in five hospitals in Sri Lanka caring for covid 19 patients. Data were collected anonymously and voluntarily using web-based (Google form) and printed standardized questionnaires examining anxiety symptoms (Generalized Anxiety Disorder-7 (GAD-7)), depression (Patient Health Questionnaire (PHQ-9)), and symptoms of post-traumatic stress disorder (PTSD) (PTSD Checklist-Civilian Version (PCL-6)).
Results: Overall, 233 health care professionals participated, compromising 54 (23.2%) doctors and 179 (76.8%) nurses. Prevalence of moderate to severe anxiety, depression, and PTSD was 42.1%, 51.5%, and 37.8% respectively. Sub-group analysis showed the risk of developing PTSD was more among nurses than doctors (p <0.05). Among doctors, moderate to severe depression prevalence was high (55.5%), while anxiety and PTSD were 31.45% and 24.07%, respectively. In nurses, moderate to severe depression, anxiety, and PTSD were 50.27%, 45.25, and 41.89%. Years of experience in patient care, working long shifts, inadequate personal protective equipment, inadequate staffing of ICU does not associate with significant psychological impact.
Conclusion: A high prevalence of psychological impact was observed in the health care professionals in ICU during the COVID-19 pandemics. Efforts should be made to implement interventions for the mental well-being of the staff.
References
1. Newlin B. Stress Reduction for the Critical Care Nurse: A Stress Education Program. Occupational Health Nursing. 1984;32(6):315-319.
2. Shigemura J, Ursano RJ, Morganstein JC, Kuro-sawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci 2020; 74:281-282
P054
Results of a nationwide survey on the use of non-invasive respiratory support in patients with respiratory failure due to COVID-19 infection
COVID-19
Katie Burke 1 , Ben Messer2, Paul Dark3, Danny McAuley4, Bronwen Connolly5, Gavin Perkins6 and Anthony De Soyza7
1Newcastle upon Tyne Hospitals Trust
2Royal Victoria Infirmary Department of Anaesthesia, North East Assisted Ventilation Service
3Division of Infection, Immunity and Respiratory Medicine, NIHR Biomedical Research Centre, University of Manchester
4Wellcome-Wolfson Institute for Experimental Medicine, Queen’s University Belfast, Belfast, UK; Regional Intensive Care Unit, Royal Victoria Hospital, Belfast, UK
5Wellcome-Wolfson Institute for Experimental Medicine, Queen’s University, Belfast, Northern Ireland
6Warwick Clinical Trials Unit, University of Warwick
7Institute of Cellular Medicine, NIHR Biomedical Research Centre for Ageing, Newcastle University
Abstract
Introduction: Currently patients with COVID-19 related acute respiratory failure (ARF) may receive respiratory support with conventional oxygen therapy, high-flow nasal oxygen (HFNO) or continuous positive airway pressure (CPAP). A proportion of patients will subsequently require invasive ventilation. However, there is insufficient evidence on the relative effectiveness of different modes of non-invasive respiratory support (NIRS). In the absence of robust evidence to guide clinical decisions, there is likely significant variation in their use in UK practice.
The RECOVERY-RS trial sought to address this knowledge gap, aiming to identify the most effective method of non-invasive respiratory support in COVID-19. This survey, conducted whilst RECOVERY-RS was in progress, sought to characterise the current use of NIRS in COVID-19 patients across the UK.
Methods: An anonymous, online survey (10 questions) was distributed via national networks and professional societies. Healthcare professionals involved in managing COVID-19 patients were invited to participate with responses collected over two months from September to October 2020.
Results: Of 145 respondents, the majority were critical care (60%) or respiratory (27%) clinicians. Prior to the COVID-19 pandemic, most reported having “commonly” used HFNO (89%) or CPAP (70%) for infection-related ARF. A small minority (3% HFNO vs 9% CPAP) reported no previous experience of their use.
In COVID-19 patients suitable for intubation and ventilation, 92% of respondents had used CPAP and 61% HFNO to bridge to or prevent intubation. Conversely, 5% reported they would never use CPAP and 8% would never use HFNO as a bridge to intubation. 68% of clinicians chose CPAP as their personal preferred method of NIRS vs 26% HFNO when treating COVID-19 patients. In patients not suitable for invasive ventilation, CPAP was also more frequently used than HFNO (92% vs 61%).
37% worked in trusts enrolled in the RECOVERY-RS trial and the majority (59%) felt that RECOVERY-RS was an important study, addressing a key unanswered research question.
Conclusion: This survey identified that a variety of methods of NIRS are being used for COVID-19 patients in the UK. CPAP predominates as both a ceiling of care treatment and as a bridge to intubation. This appears to represent a change in practice compared to the management of infection-related ARF prior to the COVID-19 pandemic, despite a lack of evidence at that time to suggest superior efficacy of CPAP. The heterogeneous survey results support the need for evidence of the most effective NIRS in COVID-19 in order to deliver optimal and standardised treatment.
P055
COVID-19 Tracheostomy Outcomes from a Tertiary Critical Care Unit
COVID-19
Douglas Findlay and Robert Hart
Queen Elizabeth University Hospital, Glasgow
Abstract
Introduction: The initial phase of the COVID-19 pandemic presented numerous challenges to critical care teams. With little initially known about the disease process, risks to staff were unclear, particularly regarding procedures involving the airway. In addition, the optimal timing for performing percutaneous tracheostomy (PCT) or surgical tracheostomy (ST) remains uncertain.
The Queen Elizabeth University Hospital in Glasgow is a tertiary centre in the West of Scotland. The critical care unit consists of 6 ten bedded pods- 3 HDUs, 2 ICUs and 1 CCU- although the proportion of level 2/3 varied during peaks of the pandemic.
Objectives: This project reviews the tracheostomy practice at the QEUH ICU, a tertiary critical care unit, during the first two waves of the pandemic.
We aimed to identify the median time of tracheostomy performance, the incidence of complications and what proportion were performed via a percutaneous approach.
Methods: A retrospective review of electronic critical care notes on the CareVue platform was performed for all patients >18 years old admitted to ICU during waves 1 & 2.
Patients transferred for ECMO or those with a tracheostomy performed prior to admission (eg: prior to capacity transfer) were excluded.
Results: 143 patients were admitted to the critical care unit with COVID-19. One patient was excluded as they had a tracheostomy in situ prior to admission; 2 patients were referred for ECMO. One patient was missing required documentation, leaving 139 patients for review.
The average age of patient was 61 years. 36 patients underwent tracheostomy, of which 29 were performed using a percutaneous approach. The median day of tracheostomy was day 17 of admission. Only 6 patients underwent a trial of extubation prior to tracheostomy. 9 patients (25%) experienced some form of complication- 6 in the percutaneous cohort. Two of the percutaneous tracheostomy patients subsequently required surgical procedures.
Figure 1.
Adverse events in both surgical and percutaneous cohorts.
Conclusion: Our unit’s timing of tracheostomy was in keeping with other studies. The largest UK multi centre review of tracheostomy practice in COVID-19 patients (COVIDTrach Collaborative et al. 2021) found a median day of tracheostomy of day 15 from admission. A review of other smaller studies showed a range of 9-19 days (Ahn et al. 2020., Angel et al. 2019., Avilés-Jurado et al. 2021., Bertini et al. 2021). A higher proportion of tracheostomies were performed using a percutaneous approach in our cohort when compared to the COVIDTrach dataset (80.6% versus 48%).
This review has prompted unit discussion surrounding use of trial of extubation, optimal timing of tracheostomy and why there were several unplanned extubations/decannulations.
References
1. Hamilton N, Schilder A, Jacob T, Ambler G, Singer M, George M et al. COVIDTrach; a prospective cohort study of mechanically ventilated COVID-19 patients undergoing tracheostomy in the UK. 2020.
2. Ahn, D., Lee, G., Choi, Y., Park, J., Kim, J., Kim, E. and Lee, Y., 2020. Timing and clinical outcomes of tracheostomy in patients with COVID-19. British Journal of Surgery, 108(1), pp.e27-e28.
3. Angel, L., Amoroso, N., Rafeq, S., Mitzman, B., Goldenberg, R., Shekar, S., Troxel, A., Zhang, Y., Chang, S., Kwak, P., Amin, M., Sureau, K., Nafday, H., Thomas, S., Kon, Z., Sommer, P., Segal, L., Moore, W. and Cerfolio, R., 2021. Percutaneous Dilational Tracheostomy for Coronavirus Disease 2019 Patients Requiring Mechanical Ventilation. Critical Care Medicine, Publish Ahead of Print
4. Avilés-Jurado, F., Prieto-Alhambra, D., González-Sánchez, N., de Ossó, J., Arancibia, C., Rojas-Lechuga, M., Ruiz-Sevilla, L., Remacha, J., Sánchez, I., Lehrer-Coriat, E., López-Chacón, M., Langdon, C., Guilemany, J., Larrosa, F., Alobid, I., Bernal-Sprekelsen, M., Castro, P. and Vilaseca, I., 2021. Timing, Complications, and Safety of Tracheotomy in Critically Ill Patients With COVID-19. JAMA Otolaryngology–Head & Neck Surgery, 147(1), p.41.
5. Bertini, P., Forfori, F., Bruschini, L., Corradi, F., Ribechini, A., Brogi, E. and Guarracino, F., 2021. Percutaneous Tracheostomy in COVID-19 Critically Ill Patients: Experience from 30 Consecutive Procedures. International Archives of Otorhinolaryngology, 25(01), e135-e140.
P056
The impact of COVID-19 on Intensive Care recruitment
COVID-19
Kayur Patel 1 , Zeeshan Malik2 and Ajay Gandhi3
1Guy’s & St. Thomas’ Hospital
2Royal Preston Hospital, Lancashire
3St Mary’s Hospital, London
Abstract
Introduction: Recruitment in intensive care has long been discussed, with the pandemic bringing this into sharp focus. Most anaesthetists in training were fully redeployed into ICU rotas or provided technical expertise. As surge rotas settle and a ‘new normal’ is regained, the challenge of ICU consultant recruitment needs to be addressed.
Historically, ICUs have been predominantly staffed by consultants trained in both anaesthetics and intensive care medicine (ICM), but the challenges of this career path have been augmented by COVID-19. Forecasts suggest a concerning supply shortage of both anaesthetic and ICM consultants.1 The latest recruitment round for ICM has been the most competitive year for applications (ratio 2.9:1 in 2021 compared to 1.49:1 in 2020).2 However, the anaesthetic/ICM dual-training contribution to this workforce has worryingly decreased from approximately two-thirds to less than a half. But what factors are causing this and has COVID-19 redeployment worsened this?
Objectives: As we emerge from the second wave of the pandemic, we assessed the attitudes of anaesthetists about future careers in intensive care.
Methods: We performed a brief electronic survey of 100 dual- or single-specialty anaesthetists in training from four LETBs across England who were redeployed to ICU.
Results: Our survey showed that 29% had a negative experience that dissuaded them from pursuing ICM careers or, in some circumstances, relinquish their ICM training number altogether. Promisingly, 64% had a positive experience, and of these 39% reaffirmed their desire to pursue a career in ICU and 13% developed a new interest in pursuing a career in ICU since their redeployment.
Positive factors included, ‘teamwork’, ‘complexity of patients’ and ‘adding variety to my anaesthetic practice’. Prominent negative factors were ‘additional exams’, ‘two separate portfolios’ and ‘high risk of burnout’.
Respondents suggested changes to attract more anaesthetists to dual-accredit with ICM. This included the removal of hurdles such as additional exams, separate portfolios, and duplicated assessments. The additional training time was also highlighted, particularly given that trainees already contribute significantly to ICM rotas.
There was a need for more flexibility in training with dual trainees wanting to undertake advanced training modules like their anaesthetic counterparts. They also reported wanting more anaesthetic sessions in their future job plans possibly reflecting the desire for varied practice as a consultant.
Conclusion: Although COVID-19 has had a positive effect by increasing ICM applications, this may be at the expense of dual-trained anaesthetic/ICM trainees. FFICM should consider the factors which dissuade these applicants and its future impact on skills available in ICU. Both the RCoA and the FFICM have recently announced changes to curricula and e-portfolio which may close some of these gaps.
The pandemic has grabbed the attention of a few anaesthetists and presented an opportunity to work in a team that solves difficult physiological puzzles, rapidly escalates capacity, and increasingly focuses on staff wellbeing. We should capitalise on this and hope that COVID-19 will result in the conversion of some of our anaesthetic colleagues into dual-specialty ICM consultants.
References
1. In-depth review of the anaesthetics and intensive care medicine workforce: Final Report. CfWI, 2015 (bit.ly/2Ujs29P).
2. Open letter to all 2021 ICM National Recruitment applicants. FICM, 2021 (bit.ly/2UnQfRW).
P059
Outcome of Hypertensive patients with Covid-19 Pneumonia requiring Oxygen therapy– A retrospective observational study in a Low-income setting.
COVID-19
Rajapakshe Gedara Ayeshani Ieshwari Rajapakshe
Base Hospital Teldeniya, Ministry of Health, Sri Lanka
Abstract
Introduction: COVID - 19 infection has become a major cause of death worldwide killing millions of people. Many studies on the effects of Hypertension on Covid-19 were published. There are studies, which showed increased in mortality and severity in COVID-19 Pneumonia patients who were having Hypertension.1,2 But some studies concluded that there is no effect of Hypertension on severity of COVID-19 Pneumonia.3 It was also concluded that although Hypertension increases mortality in COVID-19 patients, further evaluation is needed.4 Therefore, it is still not confirmed about the outcome, of patients with Hypertension having COVID- 19 pneumonia.
Objective: To assess the outcome of Hypertensive patients having COVID-19 Pneumonia treated in intensive care (ICU) and high dependency unit (HDU) and to compare it with patients without Hypertension.
Method: A retrospective observational study was conducted in COVID designated Intensive care unit and High dependency unit in Base Hospital Teldeniya, Sri Lanka. All patients with positive COVID-19 test, who developed COVID Pneumonia and were oxygen dependent, requiring ICU or HDU were included in the study. Data collection was done using patient records from 1 of January 2021 to 30 of June 2021.
Results: Total of 189 patients were admitted to either ICU or HDU requiring oxygen therapy due to COVID pneumonia during the study period. Out of them 67% were males and 33% were females. The mean age was 60.59 years with SD of 14.9. Age range was 16 to 94 years. Out of them 87 patients (46.03%) had hypertension. Out of hypertensive patients 48.2% were females and 51.8% were males. Out of the Hypertensive patients 68.53 % of patients had another co-morbid disease and the commonest was diabetes mellitus.
Out of patients with hypertension and admitted to ICU and HDU, 22.47% died in the hospital. It’s a 57.1% from total deaths in ICU and HDU. The difference of the percentage of deaths among hypertensive and non-hypertensive patients were not significant (P=0.188).
Conclusion: With referring to above results there is no significant difference in mortality between hypertensive and non-hypertensive patients with COVID-19 Pneumonia who are dependent on oxygen in ICU and HDU in Base Hospital, Teldeniya, Sri Lanka. Therefore, the outcome of Hypertensive patients who have COVID-19 Pneumonia need to be analyzed further using larger samples.
References
1. Pranata R, Lim MA, Huang I, Raharjo SB, Lukito AA. Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: a systematic review, meta-analysis and meta-regression. Journal of the renin-angiotensin-aldosterone system: JRAAS. 2020;21(2).
2. Du Y, Zhou N, Zha W, Lv Y. Hypertension is a clinically important risk factor for critical illness and mortality in COVID-19: A meta-analysis. Nutrition, Metabolism and Cardiovascular Diseases. 2021;31(3):745-755.
3. Schiffrin EL, Flack JM, Ito S, Muntner P, Webb RC. Hypertension and COVID-19.
4. Zeng Z, Sha T, Zhang Y, Wu F, Hu H, Li H, Han J, Song W, Huang Q, Chen Z. Hypertension in patients hospitalized with COVID-19 in Wuhan, China: a single-center retrospective observational study. MedRxiv. 2020.
P060
Functional Outcomes of COVID19 Patients Receiving Extra Corporeal Membrane Oxygenation- A Single Centre Observational Study
COVID-19
Samantha Cook 1 , Simon Hamilton1 and Stephen Shepherd2
1Barts Health NHS
2Barts Health NHS Trust
Abstract
Introduction: As of March 2020, COVID-19 pneumonia was declared a global pandemic by the World Health Organisation (WHO).1 COVID19 pneumonia typically presents with systematic and/or respiratory manifestations, with a large percentage requiring advanced respiratory support.2 In severe cases COVID-19 pneumonia can induce acute respiratory distress syndrome leading to refractory hypoxaemia and the use of extra-corporeal life support (ECLS) may be appropriate as a rescue therapy.3 The functional outcomes of patients receiving extra-corporeal membrane oxygenation (ECMO) for COVID are unknown and this observational study will present data from the first and second wave of the pandemic.
Objectives: To describe the demographics, functional outcomes and discharge needs of patients receiving ECMO for COVID-19.
Methods: Adults admitted to ICU for ECMO with a confirmed diagnosis of COVID19 were included. Functional outcomes were measured using the Chelsea Physical Assessment Scale (CPAx)4 and ICU mobility score.5 Measurements were taken once patients were deemed appropriate for rehabilitation up to discharge from the hospital. Data collection and analysis was performed by two independent unblinded reviewers.
Results: A total number of n34 patients were included in the review, n21 survived to hospital discharge and were included in the analysis. 71% of patients were male with an average age of 46 (±9.9) The predominant method of ECMO was veno-venous (90%). Mean duration of ECMO was 25.1 days (±19.6) The average time to mobilise post decannulation from ECMO was 10.86 days (±6.61), with an average CPAx score of 30.10 (±8.94) and ICU mobility score of 6.14 (±2.33) on ICU discharge. Functional milestones included on average achieving independent sitting balance at ∼4 weeks and mobilising +/- an aid at ∼6 weeks. There were no significant differences between patients who were mobilised within 7 days of decannulation of ECMO (P= 0.9) Patients who did not require a tracheostomy had reduced ICU length of stay (P= 0.006). There was nil significant difference between patients who received steroids for ICU length of stay (P = 0.143), CPAx (P= 0.357) or ICU mobility scores (P= 0.414) on discharge from ICU. On discharge from hospital 95% of patients required ongoing support which included the following- discharge home with community therapy, in-hospital transfer and referral to a rehabilitation centre.
Conclusions: This data is the first of its kind to present the functional outcomes of patients receiving ECMO during the COVID19 pandemic. Patients receiving ECMO for COVID19 present with high acuity of illness with prolonged mechanical ventilation and ongoing rehabilitation needs at discharge from hospital. Despite a surge in ECMO bed occupancy and redeployment of staff, the therapy team were able to provide high level rehabilitation to patients and a follow up clinic was established to support ongoing needs post hospital care.
References
1. World Health Organization. Coronavirus disease (COVID-19) Situation Report–119. 2020 [accessed Dec 2020]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200518-covid-19-sitrep-119.pdf?sfvrsn=4bd9de25_4.
2. Intensive Care National Audit and Research Centre (2020) ICNARC Report on COVID-19 in Critical Care April 2020. [accessed April 2020] Available from: https://www.icnarc.org/our-audit/audits/cmp/reports
3. Badulak J, Antonini MV, Stead CM, Shekerdemian L, Raman L, Paden ML, Agerstrand C, Bartlett RH, Barrett N, Combes A, Lorusso R, Mueller T, Ogino MT, Peek G, Pellegrino V, Rabie AA, Salazar L, Schmidt M, Shekar K, MacLaren G, Brodie D; ELSO COVID-19 Working Group Members (2021). Extracorporeal Membrane Oxygenation for COVID-19: Updated 2021 Guidelines from the Extracorporeal Life Support Organization. ASAIO J 67(5):485-495.
4. Corner EJ, Wood H, Englebretsen C, Thomas A, Grant RL, Nikoletou D, Soni N, (2013). The Chelsea critical care physical assessment tool (CPAx): validation of an innovative new tool to measure physical morbidity in the general adult critical care population; an observational proof-of-concept pilot study. Physiotherapy. 99(1):33-41.
5. Hodgson C, Needham D, Haines K, Bailey M, Ward A, Harrold M, Young P, Zanni J, Buhr H, Higgins A, Presneill J, Berney S. (2014) Feasibility and inter-rater reliability of the ICU Mobility Scale. Heart Lung;43(1):19-24.
P061
Triglyceride levels in COVID-19 patients during admission in intensive care correlate with disease severity and mortality
COVID-19
Jessie So
University of Southampton
Abstract
Introduction: It has been established that plasma triglyceride levels are raised during infection and inflammation, due to increased adipose tissue lipolysis, fatty acid synthesis and suppressed fatty acid oxidation.1 Increased triglycerides have also been linked to the ‘cytokine storm’ underlying the pathophysiology of coronavirus disease 2019 (COVID-19).2
Severe outcomes in COVID-19 patients have been found to be associated with higher triglyceride levels before the infection.3 Another study found triglycerides to be significantly higher after recovery than during the acute phase of infection.4 There is limited data on the trajectory of triglyceride levels in COVID-19 patients during admission in intensive care. Investigating whether triglyceride levels are a useful predictor of disease severity and mortality would enable earlier detection of high-risk patients.
While triglyceride levels in COVID-19 patients with mild or severe infections were found to be elevated, this was not the case in those with critical illness which included respiratory or multiple organ failure and septic shock.5 The differences in lipid metabolism between COVID-19 patients and patients with critical illness are yet to be elucidated.
Objectives: In this study, triglyceride levels of COVID-19 patients during admission in the general intensive care (GICU) were examined in relation to disease severity and mortality. Triglyceride levels at the beginning of hospitalisation were compared between GICU patients with COVID-19, acute respiratory distress syndrome (ARDS) and critical illness, and healthy controls.
Methods: Data was obtained from medical records of 93 patients with COVID-19 admitted to GICU at University Hospital Southampton, between March 2020 and May 2020. Triglyceride levels were recorded for each day of hospitalisation. Data was also obtained from medical records of 8 critically ill patients, 10 patients with ARDS and 10 healthy volunteers.
Results: The trajectory of triglyceride levels in this cohort of COVID-19 patients started low, then increased over the course of admission (Figure 1).
Figure 1.
Median triglyceride levels of 93 patients with COVID-19 admitted to GICU.
Increased average triglyceride levels correlated with increased risk for severe disease outcome, as indicated by the Sequential Organ Failure Assessment (SOFA) score calculated at the beginning of GICU admission (p<0.05) (Figure 2).
Figure 2.
There is a positive correlation between average triglyceride levels over the course of GICU admission and calculated SOFA score.
Increased triglyceride levels in the first week of GICU admission also correlated with mortality (p<0.05).
When compared with healthy controls and patients admitted to GICU with ARDS, patients with COVID-19 and critical illness had raised triglycerides (Figure 3).
Figure 3.
Comparison of median triglyceride levels on admission to GICU between patients with COVID-19, ARDS and critical illness, and healthy controls.
Conclusions: Increased triglyceride levels in COVID-19 patients over the duration of GICU admission are associated with worse disease outcomes and increased mortality. This provides further evidence for the role of dyslipidaemia in the progression of COVID-19.
References
1. Khovidhunkit W, Kim M, Memon R, Shigenaga J, Moser A, Feingold K et al. Thematic review series: The Pathogenesis of Atherosclerosis. Effects of infection and inflammation on lipid and lipoprotein metabolism mechanisms and consequences to the host. Journal of Lipid Research. 2004;45(7):1169-1196.
2. Sorokin A, Karathanasis S, Yang Z, Freeman L, Kotani K, Remaley A. COVID‐19—Associated dyslipidemia: Implications for mechanism of impaired resolution and novel therapeutic approaches. The FASEB Journal. 2020;34(8):9843-9853.
3. Masana L, Correig E, Ibarretxe D, Anoro E, Arroyo J, Jericó C et al. Low HDL and high triglycerides predict COVID-19 severity. Scientific Reports. 2021;11(1).
4. Roccaforte V, Daves M, Lippi G, Spreafico M, Bonato C. Altered lipid profile in patients with COVID-19 infection. Journal of Laboratory and Precision Medicine. 2021;6:2-2.
5. Wei X, Zeng W, Su J, Wan H, Yu X, Cao X et al. Hypolipidemia is associated with the severity of COVID-19. Journal of Clinical Lipidology. 2020;14(3):297-304.
P063
Mental, physical, and cognitive impairments of COVID-19 patients admitted to intensive care during the pandemic in Chile: an observational, multicentre study
COVID-19
Ana Castro-Avila 1 , Felipe Gonzalez-Seguel2, Agustin Camus-Molina2, Catalina Merino-Osorio2 and Jaime Leppe2
1University of York,
2Clinica Alemana Universidad del Desarrollo
Abstract
Introduction: Mental, physical, and cognitive impairments are common after an intensive care unit (ICU) stay. It remains unknown to what extent the extraordinary increase in bed occupancy during the pandemic could be linked to the severity and frequency of patient’s impairments.
Objective: To determine the frequency, severity, and risk factors for mental, physical, and cognitive impairments at ICU discharge during high and low bed occupancy periods.
Methods: Prospective cohort study in seven Chilean ICUs (ClinicalTrials.gov Identifier: NCT04979897). We included adults, mechanically ventilated >48 hours in the ICU who could walk independently prior to admission. Trained physiotherapists assessed the Medical Research Council Sum-Score (MRC-SS), Montreal Cognitive Assessment (MOCA-blind), Hospital Anxiety and Depression Scale (HADS), Impact of Event Scale-Revised (IES-R), and the World Health Organization Disability Assessment Schedule (WHODAS 2.0) at ICU discharge. Pre-admission employment status, educational level, and Clinical Frailty Scale (CFS) were also collected. We compared periods of low and high bed-occupancy, defined as less or more than 90% of staffed ICU beds occupied. We used t-test for normally distributed, Mann-Whitney for those not normally distributed, and chi-square for categorical variables. We explored risk factors for mental, physical, and cognitive impairments using logistic regression adjusted for age, sex, educational level, and bed occupancy. Analyses were performed in Stata/SE 16.0.
Results: We included 192 patients with COVID-19 of which 126 [66%] were admitted during a high bed-occupancy period (January to April 2021). Majority were male (137 [71%]) and worked full-time (127[66%]). Median [P25-P75] age was 57 [47-67], length of ICU stay was 15[ 11-27] days, and duration of mechanical ventilation (MV) was 9 [6-16.5] days. Seven (4%) patients were clinically frail, 65 (34%) had ICU-acquired weakness (ICU-AW), 134(70%) had cognitive impairment, 122 (64%) had post-traumatic stress symptoms (PTSS), 53 (28%) had depressive symptoms, 106 (55%) had anxiety symptoms, and 148 (77%) had severe disability. Table 1 shows the combined prevalence of physical and mental health problems.
Table 1.
Prevalence of physical and mental problems at ICU discharge (n=192)
| ICU-AW (n=65) | No ICU-AW (n=127) | |
|---|---|---|
| No mental health problems | 5 (2.5%) | 40 (21%) |
| PTSS | 10 (5%) | 26 (14%) |
| PTSS and anxiety | 11 (6%) | 31 (16%) |
| PTSS and depression | 1 (0.5%) | 2 (1%) |
| Depression | 1 (0.5%) | 1 (0.5%) |
| Depression and anxiety | 5 (2.5%) | 2 (1%) |
| Anxiety | 6 (3%) | 10 (5%) |
| PTSS, depression and anxiety | 26 (13.5) | 15 (8%) |
Patients admitted during the high-occupancy period were younger (mean 54, 95% confidence interval [47, 61] vs 61 [58, 64]), more likely to have a higher education qualification(HEQ) (OR 1.67 [0.9, 3.06]), and had a shorter duration of MV (8 [6-13] vs 13 [8-34]; p<0.001) and ICU stay (13 [10-19] vs 21.5 [13-42]; p<0.001). Mental, physical, and cognitive impairments were similar in low and high occupancy periods. Patients with a HEQ were less likely to have ICU-AW (OR 0.23 [0.11, 0.46]), cognitive impairments (OR 0.26 [0.11, 0.6]), symptoms of depression (OR 0.45 [0.22, 0.9]) or anxiety (OR 0.26 [0.13, 0.5]), and severe disability (OR 0.4 [0.18, 0.94]). Females were more likely to have ICU-AW (OR 2.4 [1.13, 4.93]). Older patients were less likely to suffer PTSS (OR 0.97 [0.94, 0.99] per year old).
Conclusions: Majority of patients had at least one mental, physical or cognitive impairment being similar by bed occupancy. Having a higher education qualification was the main protective factor for impairments at ICU discharge. Preventative treatments programmes should target patients with <12 years of education
P064
High Flow Nasal Cannula Oxygen in COVID-19; still an important role to play
COVID-19
Kate Goodchild 1 , Stephen A Spencer2, Lauren Brain2, Benjamin Loh2, Stephen Laver2, Hannah Swinburne2, Jennifer Rossdale2, Aimee Leadbetter2, Caroline McKerr2, Jay Suntharalingam2 and Andrew Georgiou2
1Royal United Hospital Bath
2Royal United Hospitals, Bath
Abstract
Introduction: High flow nasal cannula oxygen (HFNC) has a firm evidence base in the management of hypoxaemic respiratory failure. It has been shown to reduce mortality and increase ventilator free days when compared with use of standard oxygen or continuous positive airway pressure (CPAP), and it has been shown to reduce intubation rates in patients with a P:F ratio of <200mmHg.1 However, provisional data from the use of HFNC in COVID-19 suggest no significant reduction in intubation rates and no mortality benefit over conventional oxygen therapy or CPAP.2 These contradictory findings complicate our understanding of any potential role for HFNC in COVID-19.
In our organisation, all patients with COVID-19 who remained hypoxic despite standard oxygen therapy were initially managed with HFNC and only if they failed this modality were then trialled on CPAP or intubated for invasive mechanical ventilation. HFNC was provided on our physician led Respiratory Support Unit (RSU) with daily critical care input.
Our approach differs to that employed in the most recent multicentre randomised controlled trial of respiratory support in COVID-19 and therefore offers the opportunity to understand how HFNC may be of benefit in patients with COVID-19.
Objectives: To explore the potential role and safety for HFNC in COVID-19.
Methods: Retrospective analysis of all patients with COVID-19 admitted to a single NHS acute Trust between March 2020 and February 2021, who required escalation of respiratory support to HFNC with or without subsequent CPAP or intubation. Data collected included patient demographics, comorbidities, respiratory support requirements, ceiling of treatment and outcomes. Logistic regression analysis was used to compare mortality rates for patients who did or did not receive HFNC.
Results: One hundred and forty-seven patients met inclusion criteria of whom fifty-five (37%) were managed solely on the Respiratory Support Unit (RSU). Nineteen patients (13%) had HFNC as their ceiling of care, of whom nine died. Of those patients deemed appropriate for full escalation, fifty-four (37%) received only HFNC and thirty-two (22%) subsequently required intubation after a trial of HFNC. The relative risk of mortality for patients who received HFNC prior to intubation compared to those who were intubated without HFNC was 0.48 (95% CI 0.26-0.89). There were no safety concerns associated with HFNC.
Conclusion: Our data suggests that HFNC may offer survival benefit in those with care limitations in organ support, as demonstrated by our survival rate of 53% in this patient cohort. HFNC is generally well tolerated and is associated with fewer adverse events than other forms of non-invasive respiratory support. HFNC can be employed as a safe tool for assessing patients’ respiratory support requirements and monitoring trajectory in RSUs, sparing ICU capacity in healthcare systems under strain. Furthermore, it is associated with a favourable mortality profile in those who subsequently require intubation (34% mortality), particularly when compared with the UK national average for mortality in COVID-19 ventilated patients (50%). HFNC may therefore still have a role in the management of patients with COVID-19 with acute hypoxaemic respiratory failure and this warrants further examination.
References
1. Frat Y, et al. High-Flow Oxygen through Nasal Cannula in Acute Hypoxemic Respiratory Failure. N Engl J Med 2015; 372:2185-2196.
2. Perkins K, et al. An adaptive randomized controlled trial of non-invasive respiratory strategies in acute respiratory failure patients with COVID-19. MedRxiv preprint available from: https://doi.org/10.1101/2021.08.02.21261379
P065
Validity of ISARIC 4C prediction model for Severe coronavirus (COVID-19) respiratory failure
COVID-19
Syed Shah Hasan Quadri 1 , Kevin Waterman2, Rui Jun Lim2 and Sandeep Gudibande1
1Lancashire Teaching Hospitals
2Manchester Medical School
Abstract
Introduction: The International Severe Acute Respiratory and emerging infections Consortium- Coronavirus Clinical Characterization Consortium (ISARIC 4C). Mortality Score is a risk stratification score that predicts in-hospital mortality for hospitalised Corona Virus Disease 2019 (COVID-19) patients, produced by the ISARIC 4C consortium.1 ISARIC 4C Mortality score is an easy to use eight variable score (Table 1) that helps in accurate stratification of hospitalized COVID-19 patients by mortality risk at hospital presentation and if applied within the validation cohorts could guide clinician decisions including escalation of care plans.1 It is unknown whether this score is validated for patients with most severe form of the disease. We aimed to evaluate its efficacy in a cohort of patients who all required invasive prone ventilation.
Table 1.
■■■.
| Factors variable | 4C Mortality score points | |
|---|---|---|
| Age (in years) | ≥50 | 0 |
| 50-59 | +2 | |
| 60-69 | +4 | |
| 70-79 | +6 | |
| ≥80 | +7 | |
| Sex at birth | Female | 0 |
| Male | +1 | |
| Number of co-morbidities | 0 | 0 |
| 1 | +1 | |
| ≥2 | +2 | |
| Respiratory rate (breaths/min) | <20 | 0 |
| 20-29 | +1 | |
| ≥30 | +2 | |
| Peripheral oxygen saturation on room air (%) | ≥92 | 0 |
| <92 | +2 | |
| Glasgow coma scale | 15 | 0 |
| ≤15 | +2 | |
| Urea(mmol/L) | ≤7 | 0 |
| 7-14 | +1 | |
| >14 | +3 | |
| CRP (mg/dl) | <50 | 0 |
| 50-99 | +1 | |
| ≥100 | +1 |
Objectives:
1. Validate ISARIC 4c score for a subset of patients admitted to Critical Care, Royal Preston Hospital, requiring invasive ventilation and proning
2. Compare predicted mortality at hospitalization and at Intensive care unit (ICU) admission, with the actual observed mortality
Methods: We analysed 96 patients from our electronic patient record (Quadramed) requiring invasive ventilation and proning, and calculated ISARIC 4c scores and predicted mortality at hospitalization and at ICU admission. We classified them into 4 groups, depending on their scores, as shown in Table 2.
Table 2.
■■■.
| 4C Score | Risk Group | %Mortality |
|---|---|---|
| ≥15 | Very High Risk | 61.5% |
| 9-14 | High Risk | 31.4% |
| 4-8 | Intermediate Risk | 9.9% |
| ≤3 | Low Risk | 1.2% |
Results:
1. 55% of patients were admitted to ICU on same day of hospitalization, 29% within 3 days and 16% beyond 3 days.
2. Overall observed mortality for this cohort of patients was 57(59%) excluding outcome for 11 patients who were transferred out to Other ICUs.
3. The number of patients with predicted low, intermediate, and high risk of death seemed to underestimate the risk of death as their actual mortality was close to 50%. The mortality rate was close to predicted rate in the very high-risk group (Graph 1)
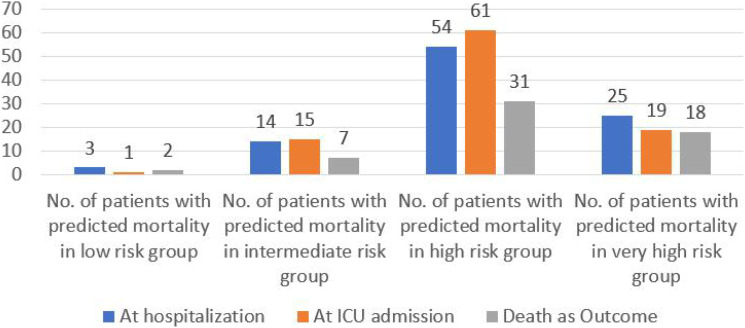
Conclusion: The ISARIC 4C score-based prediction did not accurately reflect the actual observed mortality rates in this cohort of patients, particularly in the low, intermediate, and high risk of death groups. A very high risk of death, as predicted by the score correlated well with the actual mortality. In our opinion the ISARIC 4C scores underestimated the risk of death in this cohort of critically ill patients.
The reasons for the underestimation could be inherent in the pathophysiology of the disease, causing unpredictable progression of disease and development of secondary complications in ICU. It would be interesting to determine if traditional ICU mortality prediction scores like APACHE2 and SOFA3 scores fare any better than ISARIC 4C. Further evaluation on a larger cohort of critically ill patients will be necessary.
References
1. Knight, S., Ho, A., Pius, R., et al. 2020. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ, p.m3339.
2. Wa K, Ea D, Dp W, Je Z. APACHE II: a severity of disease classification system [Internet]. 2021. Available from: https://pubmed.ncbi.nlm.nih.gov/3928249/
3. Jones A, Trzeciak S, Kline J. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation*. 2021.
P066
Compassionate use of pulmonary vasodilators in acute severe hypoxic respiratory failure due to COVID-19
COVID-19
Lewis Matthews 1 , Laurence Baker2, Matteo Ferrari2, Weronika Sanchez2, John Pappachan2, Mike Grocott2 and Ahilalandan Dushianthan2
1University Hospital Southampton NHS FT
2UHS NHS FT
Abstract
Introduction: There have been over 200 million cases and 4.4 million deaths from Covid-19 worldwide. In the UK over half a million have required hospitalisation, with over 130,000 deaths. Although most experience a mild illness the mortality can be over 50% for those requiring mechanical ventilation.1 One potential treatment for severe hypoxaemia is inhaled pulmonary vasodilator (IPVD) therapy, either as nitric oxide (NO) or prostaglandin analogues. Despite the lack of robust evidence IPVDs are often considered recue treatments for refractory hypoxaemia.2,3 Given the disease severity in COVID-19 we implemented a protocol for the use of IPVDs on a compassionate basis for patients with severe hypoxaemia receiving otherwise maximal support. In this study we detail our findings and assess differences between survivors and non-survivors.
Objectives: The primary outcome of this study was percentage changes in PaO2/FiO2 (PF) ratio and Alveolar-arterial (A-a) gradient at 2, 6, 12, 24, 48 and 72 hours following initiation of IPVD therapy. Secondary outcomes were differences in characteristics and response to therapy between survivors and non-survivors who received an IPVD.
Methods: Data from a prospectively maintained research database of patients with SARS-CoV-2 admitted to the ICU at a large teaching hospital were analysed for the time period 14 March 2020 - 11 February 2021. Patients aged 18 years or older who received an IPVD during their admission were eligible for inclusion. An IPVD was considered if the PF ratio was less than 13.3kPa despite rescue therapies (prone positioning, neuromuscular blockade, airway pressure release ventilation). Nitric oxide was commenced at 20ppm and titrated to response. If oxygenation improved Iloprost nebulisers were commenced at 10-30mcg four hourly and NO weaned.
Results: Three-hundred eight patients with SARS-Cov-2 were admitted during the study period of whom 59 (19.2%) received IPVD therapy. Patients receiving an IPVD had a lower PF ratio (14.37 vs. 16.37kPa, p=0.002) and higher APACHE-II score (17 vs. 13, p=0.028) at admission compared to those who did not. Survival to ICU discharge was lower in patients receiving an IPVD (55.9% vs. 81.9%, p<0.001).
The median PF ratio at commencing IPVD therapy was 11.33kPa (9.93-12.91) with a median of 6 days from admission to receiving an IPVD. At 72 hours the median improvement in PF ratio was 33.9% (-4.3-84.1). In patients receiving IPVDs there were no differences in other therapies received (steroids, prone ventilation, ECMO) between survivors (n=33) and non-survivors (n=26), with the exception of renal replacement therapy. At 72 hours changes in PF ratio (70.8 vs. -4.1%) and reduction in A-a gradient (44.7 vs. 14.8%) differed significantly between survivors and non-survivors (both p <0.001).
Conclusion: The response to the compassionate use of IPVDs for patients with acute hypoxic respiratory failure due to Covid-19 differs significantly between survivors and non-survivors. Both NO and inhaled prostaglandins may offer therapeutic options for severe hypoxaemia due to COVID-19, with prostaglandins particularly attractive as they do not require specialist delivery systems. The use of inhaled prostaglandins, and NO where feasible, should be studied in both isolation and combination in adequately powered prospective randomised trials.
References
1. Cao Y, Hiyoshi A, Montgomery S. COVID-19 case-fatality rate and demographic and socioeconomic influencers: Worldwide spatial regression analysis based on country-level data. BMJ Open [Internet]. 2020;10(11). Available from: https://pubmed.ncbi.nlm.nih.gov/33148769/
2. Adhikari NKJ, Dellinger RP, Lundin S, Payen D, Vallet B, Gerlach H, et al. Inhaled nitric oxide does not reduce mortality in patients with acute respiratory distress syndrome regardless of severity: Systematic review and meta-analysis [Internet]. Crit Care Med. 2014; 42:404–412. Available from: https://pubmed.ncbi.nlm.nih.gov/24132038/
3. Moreno Franco P, Enders F, Wilson G, Gajic O, Pannu SR. A comparative effectiveness study of rescue strategies in 1,000 subjects with severe hypoxemic respiratory failure [Internet]. Respir Care. 2016;61:127–133. Available from: https://pubmed.ncbi.nlm.nih.gov/26647448/
P067
Assessing the Psychological Impact of COVID-19 on Intensive Care Workers: A Single-centre Cross-sectional UK-based Study
COVID-19
Natasha Dykes 1 , Oliver Johnson2 and Peter Bamford1
1Countess of Chester Hospital Trust
2Royal Liverpool and Broadgreen University Hospital Trust
Abstract
Introduction: The COVID-19 pandemic presents a unique set of stressors for healthcare professionals across the globe.1 The challenges facing intensive care workers in the United Kingdom (UK) have not previously been seen on this scale. There is a dearth of research establishing the psychological impact of the virus among intense care workers specifically, who may be at the greatest risk of adverse outcomes. Protecting the psychological wellbeing of healthcare workers caring for patients with COVID-19 is essential for the long-term capacity of the health workforce.
Objectives: The objectives of this study were to establish the prevalence of anxiety, depression and post-traumatic stress disorder (PTSD) among a cohort of intensive care workers within the United Kingdom during the COVID-19 pandemic.
Methods: An anonymous questionnaire was designed to incorporate validated screening tools for anxiety (Generalised Anxiety Disorder Scale, GAD-7),2 depression (Patient Health Questionnaire, PHQ-9)3 and post-traumatic stress disorder (Impact of Event Scale–Revised, IES-R).4 Participants were also asked to highlight any factors in particular that contributed significantly to their own perceived mental health status. Additionally, awareness of any available mental health support services was established. All intensive care workers at the Countess of Chester Hospital, UK, were eligible and data was collected over a three week period during the months of June and July 2020
Results: The majority of the 131 respondents were nurses (52.7% [69/131]) or doctors (32.8% [43/141]). Almost one-third (29.8% [39/131]) reported a significant or extreme impact of COVID-19 on their mental health. In total, 16% (21/131) had symptoms of moderate depression, 11.5% (15/131) moderately severe depression and 6.1% (8/131) severe depression. Females had a significantly higher mean PHQ-9 score than males (8.8 and 5.68 respectively, p=0.009). Furthermore, 18.3% (24/131) had moderate anxiety with 14.5% (19/131) having severe anxiety. Mean GAD-7 scores were higher among females than males (8.69 and 6.26 respectively, p=0.028). Additionally, 28.2% (37/131) had symptoms of PTSD (IES-R ≥33). The most commonly cited contributory factors to participants’ self-rated impact on mental health, was the effect of COVID-19 on family (78.6% [103/131]) followed by being busier at work (60.3% [79/131]), the personal risk of contracting COVID-19 (56.5% 74/131]), change in working environment (51.1% [67/131]) and change in working hours (43.5% [57/131]). The majority (58% [76/131]) of participants were either unaware or only vaguely aware of available mental health support services. Surprisingly, only 3.1% (4/131) had accessed support services at the time of data collection.
Conclusion: The psychological impact of COVID-19 on intensive care workers is significant. Healthcare systems are currently ill-prepared to cope with the increased demand for support5. Specific focus and attention must be directed accordingly in order to safeguard the mental health of this key sector of the workforce, who play a crucial role in the fight against COVID-19. Determining and acknowledging the scale of the problem is the first step towards achieving this.
References
1. Morens DM, Daszak P and Taubenberger JK. Escaping Pandora's Box - Another Novel Coronavirus. The New England Journal Of Medicine 2020; 382: 1293-1295. 2020/02/27. DOI: 10.1056/NEJMp2002106.
2. Kroenke K, Spitzer RL and Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606-613. 2001/09/15. DOI: 10.1046/j.1525-1497.2001.016009606.x.
3. Weiss DS. The Impact of Event Scale: Revised. In: Wilson JP and Tang CS-k (eds) Cross-Cultural Assessment of Psychological Trauma and PTSD. Boston, MA: Springer US, 2007, pp.219-238.
4. Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166: 1092-1097. 2006/05/24. DOI: 10.1001/archinte.166.10.1092.
5. Zaka A, Shamloo SE, Fiorente P, et al. COVID-19 pandemic as a watershed moment: A call for systematic psychological health care for frontline medical staff. Journal of Health Psychology 2020; 25: 883-887. DOI: 10.1177/1359105320925148.
P068
ROX index at 12 hours helps predict success of non-invasive respiratory support in patients with COVID pneumonitis.
COVID-19
Melroy Rasquinha, Jonathan Taylor, James Bonnington and Milind Sovani
Nottingham University Hospital NHS Trust
Abstract
Introduction: The ISARIC4C score1 and APACHE II score are used widely to predict mortality in critically ill patients with COVID-19 pneumonitis. These scores, however, do not predict response to specific treatments.
Non-invasive respiratory support (NRS) in the form of CPAP/NIV/HFNC has been extensively used to treat COVID-19 pneumonitis. ROX index2 (SpO2/FiO2/Respiratory Rate) is used to predict failure of HFNC in treatment of Acute Hypoxaemic Respiratory Failure and ARDS. However, there are limited data on its efficacy to predict NRS failure in COVID-19 infection.
Objective: Whether ROX index can be used to predict response to NRS in both patients for escalation to mechanical ventilation and those where NRS is ceiling of care.
Methods: A retrospective study of individuals, SARS-COV-2 positive by RT-PCR, admitted to the ICU and requiring CPAP/NIV/HFNC, in a single centre between October 2020 to January 2021. Respiratory parameters were obtained at initiation of NRS followed by 2, 6 and 12 hours post initiation. NRS failure was defined as the need for mechanical ventilation in those for escalation of support or death in those where NRS was set as ceiling of care.
Results: Data (Table 1) for 104 patients (70 men) were analysed. The mean age and BMI were 58.0 years and 31.4kg/m2, respectively, mean Respiratory Rate was 31 and mean SpO2/FiO2 of 144 on admission. In 10 out of 104 NRS was set as ceiling of care. Most patients were treated with CPAP/NIV, and they often used HFNC for breaks and while eating and drinking. Of the 62 patients that failed NRS, 10 had NRS as ceiling of care and a further 10 died without receiving mechanical ventilation. 42 patients underwent mechanical ventilation. 70 were discharged and 34 (32.7%) died in hospital.
Table 1.
Baseline information and ROX index data. NRS = non-invasive respiratory support.
| NRS success | NRS failure | p value | |
|---|---|---|---|
| N= | 42 | 62 | |
| Male/Female (%) | 69.0/31.0 | 66.1/33.9 | |
| *Mean age (years) / Std Dev | 50.9/12.41 | 62.7/14.11 | p < .0001 |
| Mean BMI kg/m2 / StdDev | 33.35/8.76 | 30.51/7.17 | p=0.07 |
| *Mean APACHE II Score / StdDev | 8.05/2.86 | 9.82/3.36 | p=0.006 |
| *Mean ROX on Admission / StdDev | 5.41/2.28 | 4.91/2.52 | p=0.3049 |
| Mean ROA @ 12 hours /StdDev | 7.53/3.90 | 6.18/3.46 | p=0.066 |
| Mean Change in ROX index at 12 hours / StdDev | 2.12/3.51 | -0.11/2.98 | Mean difference = 2.2 (95% CI 0.99-3.46) p=0.0005 |
Baseline and 12 hour ROX index was not significantly different but the mean change between 0 and 12 hour ROX (2.2, 95% CI 0.99 to 3.46; p=0.0005) was significantly higher in those with NRS success. NRS success was predicted by a ROX index value of >5(OR 2.59, 95% CI 1.15-5.85; p= 0.01) and improvement in ROX score by >1 at 12 hours (OR 3.25, 95% CI 1.43 to 7.4; p=0.025).
Conclusion: There was a significantly higher increase in ROX index at 12 hours in those with NRS success. A 12 hour ROX index of > 5 or an improvement by >1 are good predictors of success. Patients where NRS failed were older, had higher APACHE II and slightly higher ISARIC-4C score as expected.
Discussion: This was a real life study where patients were treated with a combination of CPAP/NIV and HFNC as opposed to just HFNC or CPAP. The advantage of ROX index over P/F ratio is that arterial blood gases are not needed. It can be scored easily by routinely collected vital observations. A large number of patients are likely to be treated outside critical care in light of results from RECOVERY-RS trial3. In these settings, ROX index could be a useful tool for escalation to critical care or planning for symptom palliation as appropriate.
References
1. Knight SR, Ho A, Pius R, et al. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ. 2020: m4334.
2. Roca O, Messika J, Caralt B, et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: the utility of the ROX index. J Crit Care. 2016;35:200–205.
3. Perkins GD, Ji C, Connolly BA, et al. An adaptive randomized controlled trial of non-invasive respiratory strategies in acute respiratory failure patients with COVID-19. Medrxiv. [Preprint]. 2021. https://doi.org/10.1101/2021.08.02.21261379.
P069
To tube or not to tube? The COVID-19 enigma. A single centre experience of early vs late intubation
COVID-19
Huw Griffiths, Egidija Bielskute, Kristyn Dyer, York-Mui Liu and Loku Warnapura
Luton & Dunstable University Hospital - Bedfordshire Hospitals NHS Foundation Trust.
Abstract
Introduction: COVID-19, a disease typified by primary respiratory failure, lacks level one evidence on the most appropriate ventilation strategy when patients require critical care.1
The first wave in the United Kingdom (March - May 2020) was associated with early intubation due to lack of resources, infection control issues and poor evidence for non-invasive ventilation (NIV).
With the availability of more knowledge, NIV was utilised in the second wave (December 2020 - February 2021). This strategy however, delayed intubation for the subgroup of patients who failed the NIV trial.
At our institution, the first wave was characterised by early intubation, and the second wave by late intubation.
Objectives: The primary aim was to compare the mortality statistics of the two waves in our institution.
The secondary aim was to identify variables that could be relative contraindications to intubation, thus contributing to the design of an intubation pathway.
Methods: Retrospective observational study.
Inclusion criteria - COVID-19 patients requiring critical care (HDU or ICU) during the first and second wave.
Variables included: date of admission (DOA), age, gender, date of intubation, comorbidity burden and survival status (obtained from the trust digital records).
These variables were compared between the two groups using an excel spreadsheet.
Results: *The high mortality rate is a reflection of the patient group who presented in extremis having failed an NIV trial and had worsening disease progression. Often failure to deteriorate rapidly whilst on NIV inadvertently ‘delayed’ intubation.
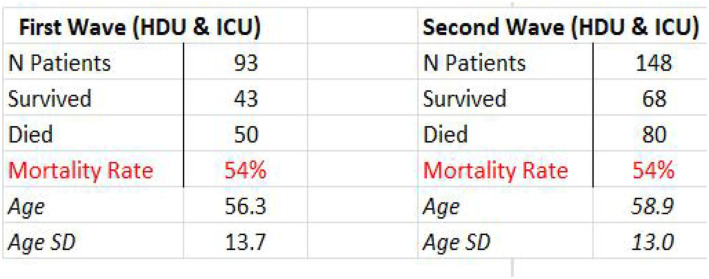
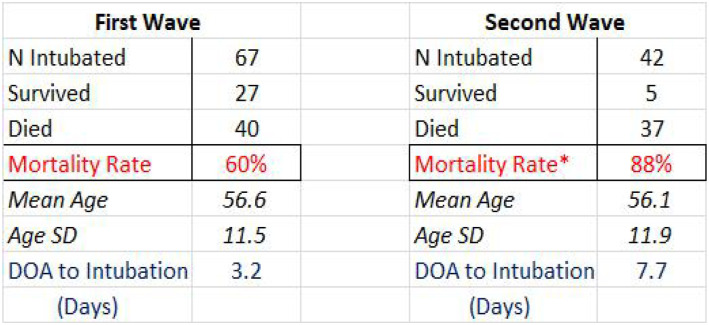
The gender distribution between the two groups was identical with 1/3 female and 2/3 male. The comorbidity burden was also very similar.
The strongest risk factor for mortality in the intubated cohort was age, with those aged over 65 having the worst outcome - Mortality Rate 93% (28/30).
Conclusion: At our institution there was no mortality difference between the two waves.
The second wave was characterised by predominant NIV usage, resulting in a smaller percentage of people requiring intubation. This had major logistical and cost saving benefits as less patients required level 3 care.
The early vs late intubation strategy seems to have no bearing on overall mortality, suggesting disease progression plays a more important role in outcome than ventilation modality.
COVID-19 is likely to be endemic in the population,2 thus devising a critical care pathway is essential to ensure standardisation of care and optimising patient outcomes.
The two waves have been characterised by extremes in approach. Our new pathway aims to take the middle ground of intubating at around day 5. This will allow the benefits of the NIV trial but also detect those deteriorating earlier. Relative contraindication to intubation will be age >65 years.
In summary, this study highlights the benefits of adopting a primary NIV strategy with the caveat that there is a small group of patients who deteriorate irrespective of treatments offered. To ensure the best opportunity for those with severe disease progression, a middle ground of intubating at around day 5 seems the most strategic future approach.
References
1. Torjesen, I. Covid-19: When to start invasive ventilation is “the million dollar question”. BMJ 2021; 372: n121
2. Veldhoen, M, Simas, J.P. Endemic SARS-CoV-2 will maintain post-pandemic immunity. Nat Rev Immunol 2021; 21: 131-132
P070
Retrospective analysis of individualised melatonin regimens and a multidisciplinary targeted approach in managing insomnia during the second wave of COVID-19
COVID-19
Chris Chung and Linsey Christie
Chelsea & Westminster NHS Foundation Trust
Abstract
Introduction: The therapeutic benefits of sleep in the critically ill has been extensively studied in the medical literature.1 Chronic insomnia increases a patient’s risk of delirium, cortical atrophy, diabetes, cancer, cardiovascular death from arterial hypertension, myocardial infarction and heart failure.2 Insomnia reduces interaction during video-calls with family and limits co-operation with physiotherapy, medical and nursing interventions, potentially delaying rehabilitation and recovery.
Objectives: To improve sleep by introducing an individualised melatonin regimen and a multidisciplinary targeted approach to managing insomnia in an adult intensive care unit.
Methods: A retrospective analysis was conducted in a single centre UK adult ICU. Data was retrieved from pharmacy dispensing records, electronic medical notes and prescriptions from September 2020 to March 2021.
The primary outcome was resolution of insomnia. Other information collected included causes of insomnia, referral to psychology for cognitive behavioural therapy (CBT), prevalence and resolution of delirium, adverse effects, and death.
Each patient received a tailor made regimen based on Bellapart et al’s original concept of mimicking the natural endogenous secretion of melatonin.3 However, unlike previous studies3,4,5 dosing was modified and adjusted according to patient response. A loading dose of 0.75 to 3mg was administered at 21:00 followed by a smaller hourly dose of 0.25 to 0.5mg between 22:00 and 03:00. Additionally, the duration of treatment continued for as long as therapeutic benefit was realised, which included post discharge from ICU. Prior experience of conventional melatonin dosing did not demonstrate therapeutic benefit from the original pilot study and when nursing staff inadvertently omitted the hourly dose between 10pm and 3am.
Adverse effects were documented. Sleep hygiene measures were introduced and standardised where possible e.g. ear plugs, eye mask, dim lights, environmental noise reduction and minimal night time physical interventions from nursing and medical staff. The principal investigator referred to psychology patients who expressed fear and anxiety as a cause of insomnia.
Results: 132 patients were admitted during September 2020 to March 2021. 30 patients received tailor made melatonin regimens (22.7%). The medical notes of four (13.3%) patients could not be accessed for data collection and were, therefore, excluded from the study. The primary outcome of resolution of insomnia occurred in 23 out of 26 (88.4%) patients.
At the time of ICU discharge, delirium had occurred in 15 patients (57.7%), resolved in 10 patients (66.7%), three (20%) patients remained intermittently delirious, one remained continuously delirious, and one died.
Mechanical ventilation, environmental noise, necessary medical and nursing interventions throughout the night and infection accounted for 23 (88.4%) of patients’ insomnia. Fear or anxiety were expressed by eight (30.8%) patients as a cause of insomnia whilst medicines e.g. steroids, beta blockers accounted for six patients (26.1%).
Seven patients (26.9%) expressing fear or anxiety were referred to psychology for adjunctive CBT. One patient experienced excessive daytime drowsiness, which resolved with dose regimen adjustment. One patient died of a cause unrelated to melatonin.
Conclusion: An individualised melatonin regimen combined with a multidisciplinary targeted approach can result in resolution of insomnia in ICU patients, with minimal risk of adverse effects.
References
1. Pisani MA, Friese RS, Gehlbach BK, Schwab RJ, Weinhouse GL and Jones SF. Sleep in the intensive care unit. American Journal of Respiratory and Critical Care Medicine 2015;191(7):731-738.
2. Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Groselj LD, Ellis JG, et al. European guideline for the diagnosis and treatment of insomnia. European Sleep Research 2017;26:675-700.
3. Bellapart J, Roberts JA, Appadurai V, Wallis SC, Nunez-Nunez M, Boots RJ. Pharmacokinetics of a novel dosing regimen of oral melatonin in critically ill patients. Clinical Chemistry and Laboratory Medicine 2016;54(3):467-472.
4. Bellapart J, Appadurai V, Lassig-Smith M, Stuart J, Zappala C and Boots R. Effect of exogenous melatonin administration in critically ill patients on delirium and sleep: a randomised controlled trial. Critical Care Research and Practice 2020, article ID 3951828:1-9.
5. Lewis SR, Pritchard MW, Schofield-Robinson OJ, Alderson P, Smith AF. Melatonin for the promotion of sleep in adults in the intensive care unit (review). Cochrane Database of Systemic Reviews.
P071
Exploring the evolving picture of physical outcomes for patients admitted to ICU with COVID-19: A single centre observational study from a London teaching Trust
COVID-19
Claire Bradley and Lori-Anne Penner
Kings College Hospital NHS Foundation Trust
Abstract
Introduction: Prolonged Intensive Care Unit (ICU) admission is frequently accompanied by ICU acquired weakness, impaired mobility and reduced health related quality of life.1,2,3 The COVID-19 pandemic caused a sudden and unprecedented surge in ICU admissions for severe acute respiratory failure in the UK in two distinct waves between March-April 2020 and Jan-Feb 2021. Whilst knowledge surrounding medical management of COVID-19 evolved throughout the pandemic, the impact of this on physical recovery and outcomes is less clear.
Objective: To explore the impact of ICU admission on physical function in COVID-19 survivors across two distinct UK waves.
Methods: A retrospective clinical review of patients admitted to ICU with a primary diagnosis of COVID-19 between March-April 2020 and January-February 2021 was conducted at a large London NHS Foundation Trust. Electronic clinical notes were reviewed, and the following data extracted: age, ethnicity, sex, BMI, duration of sedation, duration of mechanical ventilation, ICU length of stay (LOS) and hospital LOS. Physical impairment was based on the Intensive Care Unit Mobility Score (ICUMS) and defined as significant (≤3), moderate (≤6), mild (≥7) or none (score of 10). Data was analysed using descriptive statistics, reported as absolute numbers, percentages (%) and median (range).
Comparisons were made between data sets from each wave to examine whether greater understanding surrounding the management of COVID-19 translated into improved physical outcomes for those surviving ICU admission.
Results: 444 clinical notes were identified, 287 were excluded as 149 died, 14 were incidental findings of COVID-19, 115 had missing data due to paper notes or transfers in/out of the Trust and 9 were duplicate records. 157 patients were included in the final analysis; 66 from wave 1 and 91 from wave 2.
Baseline patient demographics were equally matched across both waves (table 1). Wave 1 patients were sedated longer (13(0-39) v’s 11(0-83) days), ventilated longer (25(0-277) vs 13(0-175) days) with longer ICU (27(2-67) vs 17(0-189) days) and hospital LOS (49(5-277) vs 32(4-182) days) than those in wave 2 (Table 1).
Table 1.
Patient demographics
| Age | Gender (% Male) | Ethinicity (% White) | BMI | Clinical frailty score | Days sedation | Days ventilated | ICU LOS (days) | Hosp LOS (days) | ICUM ICU D/C | |
|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 (n=66) | 54 (25–78) | 61% | 29% | 26.7 (19.9-59.3) | 3 (1-7) | 13 (0–39) | 25 (0–277) | 27 (2–67) | 49 (5–277) | 3 (0–10) |
| Wave 2 (n - 91) | 58 (24–80) | 60% | 28% | 27.2 (22.0-53.3) | 3 (1-7) | 11 (0–83) | 13 (0-175) | 17 (1–189) | 32 (4–182) | 4 (0–9) |
The median ICUMS at ICU discharge was lower for wave 1 than wave 2 (3 (0-10) V’s 4 (0-9)). A higher percentage of patients in wave 1 were discharged from ICU with severe physical impairment compared to Wave 2 (52% vs 40%). Moderate physical impairment was the most frequent presentation category at ICU discharge for wave 2 patients (Table 2).
Table 2.
Physical impairment at ICU and hospital discharge
| Physical impairment at ICU D/C | Physical impairment at hospital D/C | |||||||
|---|---|---|---|---|---|---|---|---|
| Severe | Moderate | Mild | Nill | Severe | Moderate | Mild | Nill | |
| Wave 1 (n=66) | 34 (52%) | 24 (36%) | 7 (11%) | 1 (1%) | 3 (5%) | 5 (8%) | 34 (53%) | 22 |
| Wave 2 (n - 91) | 36 (40%) | 40 (44%) | 15 (16%) | 3 (4%) | 5 (6%) | 51 (61%) | 24 | |
At hospital discharge 66% of patients in wave 1 and 76% in wave 2 had ongoing rehab needs, although the majority of these were mild (ICUMS ≥7) in both cohorts.
Conclusions: These preliminary data comparisons between the first two waves of the COVID-19 pandemic suggest evolving knowledge and experience of the condition resulted in reduced sedation duration, ventilation days, ICU and hospital LOS. There were also improved physical outcomes for patients at ICU discharge, but long-term rehabilitation needs persisted. Ongoing exploration of the acute and longer-term needs of individuals surviving ICU admission for COVID-19 is required to inform future rehabilitation provision and health care policy.
References
1. Inoue S, Hatakeyama J, Kondo Y, Hifumi T, Sakuramoto H, Kawasaki T, et al. Post‐intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Medicine & Surgery. 2019;6(3):233-246.
2. Lad H, Saumur T, Herridge M, dos Santos C, Mathur S, Batt J, et al. Intensive Care Unit-Acquired Weakness: Not Just Another Muscle Atrophying Condition. International Journal of Molecular Sciences. 2020;21(21):7840.
3. Vanhorebeek I, Latronico N, Van den Berghe G. ICU-acquired weakness. Intensive Care Medicine. 2020;46(4):637-653.
P072
Prescribing practices in a UK Intensive Care Unit during the first wave of the COVID-19 pandemic
COVID-19
Raj Nichani1, Arun Prasad Ravichandran 1 , Aisling Hanna2 and Dominic Wu2
1Royal Oldham Hospital
2Royal Oldham hospital
Abstract
Introduction: Comparatively little is known about drug requirements in patients admitted to ICU with COVID-19 pneumonitis. We analysed drug usage for patients admitted during the first wave of the pandemic, comparing these with a retrospective cohort admitted with Influenza pneumonia.
Methods: Forty-nine ventilated patients with COVID-19 pneumonitis were identified through ICNARC, ten were excluded as duration of stay < 7 days or not needing ventilation. Further three were excluded due to missing data and one due to ECMO escalation.
Results: The median age was 61 years; length of stay 22 days and 68% survived ICU. Table 1 describes the use of Infusions and enteral medications.
| Infusions | Number of patients receiving the drug/ Total number of patients (%) | Median duration of infusion used in hours amongst all patients (survivors) | Hours needing drug/total hours on ICU(%) for all patients receiving drug (survivors) | |
| Propofol | 34/35 (97.1%) | 234.5 (247) | 43.4% (36.6%) | |
| Midazolam | 19/35 (54.2%) | 106 (127) | 21.5% (20.4%) | |
| Opiates: | 35/35 (100%) | 274 (295.5) | 45.7% (39.6%) | |
| Alpha agonists: | 24/35 (68.6%) | 68.5 (68.5) | 13.3% (12.6%) | |
| Muscle relaxants: | 32/35 (91.4%) | 150.5 (129) | 19.9% (19.4%) | |
| Furosemide | 27/35 (77%) | 90 (130) | 14.6% (13.8%) | |
| Prostacyclin Nebuliser | 8/35 (22.8%) | 51 (54.4) | 8% (6.5%) | |
| Enteral Medications | Number of patients receiving drug/Total number of patients (%) | Median number of days used amongst all patients (survivors) | Number of patients receiving drug/Total number of patients (%) | Median number of days used amongst all patients |
| COVID-19, N=35 | Influenza, N=12 | |||
| Carbocisteine | 19/35 (54.2%) | 13 (14) | 1/12 (8.3%) | - |
| Risperidone | 12/35 (34.2%) | 10.5 (13) | 4/12 (33.3%) | 9.5 |
| Clonidine | 11/35 (31.4%) | 11 (11) | 0 (0%) | - |
| Frusemide | 16/35 (45.7%) | 5.5 (5) | 5/12 (41.6%) | 3 |
| Acetazolamide | 11/35 (31.4%) | 7 (7) | 1/12 (8.3%) | 6 |
| Melatonin | 16/35 (45.7%) | 8 (9) | 7/12 (58.3%) | 9 |
| Morphine | 13/35 (37.1%) | 10 (11) | 0 (0%) | - |
| Diazepam | 8/35 (22.8%) | 12 (12) | 0 (0%) | - |
Discussion: Propofol was used in most (43% patient-hours in ICU/median duration = 234 hours). All patients received opiate infusions (mainly morphine or alfentanil in similar proportions) and 91% received muscle relaxants, for prolonged periods. Over half received Midazolam (median 106 hours) as an adjunct or substitute to Propofol as patients were difficult to sedate, required longer ventilation, paralysis and concerns with Propofol associated hypertriglyceridemia. Over two-third received alpha agonist infusions (median 68.5 hours) as adjunctive sedation or delirium management.
Three quarters of patients received a furosemide infusion (median 90 hours), the evidence extrapolated from studies such as FACTT.1 Around three quarters received Human Albumin (median 100 grams over 3 days). Nearly a quarter received nebulized Prostacyclin for refractory hypoxia, often associated with saturation of HME filters and ventilatory difficulties.2
Over half of patients received Carbocisteine (median 13 days). Clonidine and Risperidone to manage delirium were used in a third (median 10.5 and 11 days respectively), as was Acetazolamide to restore pH and aid weaning. Over a third were prescribed enteral opiates and nearly a quarter received benzodiazepines to manage withdrawal symptoms. Just under a half of patients received Melatonin.
Antibiotic usage was high with a median of 3 Antibiotics used (median duration 15 days/61% of patient days). Diagnosing superadded infection such as VAP was challenging3 and we did not routinely monitor serum Procalcitonin levels.
We also compared prescribing habits with 12 influenza patients (11 survivors) identified using similar inclusion criteria and found patients with COVID-19 were older (61 versus 51 years ) with longer ICU stays (median 22 versus 20 days). They were also more likely to receive enteral Carbocisteine, Clonidine, Acetazolamide, Morphine and Diazepam.
Conclusion: We were able to generate valuable data on prescribing in ventilated patients with COVID-19 pneumonitis during the first wave. Through this, we are able to use drug usage as a surrogate for issues such as delirium, drug withdrawal, antibiotic prescribing and nursing workload in general.
References
1. Wiedemann HP, Wheeler AP, Bernard GR, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354(24):2564-2575.
2. The Faculty of Intensive Care Medicine. Clinical guide for the management of critical care for adults with COVID-19 during the Coronavirus pandemic, Critical Care Guidance, Version 6.
3. François B, Laterre PF, Luyt CE, et al. The challenge of ventilator-associated pneumonia diagnosis in COVID-19 patients. Crit Care. 242020. p. 289.
P073
A study on burnout among health care workers of COVID care units of some selected hospitals in Sri Lanka during the COVID 19 pandemic
COVID-19
Tharuka Kalhari Sikuradipathi 1 , Kamalanathan Krishakeesen1 and Nayana Shiranthini Fernando2
1Ministry of Health Sri Lanka
2General Sir John Kotelawala Defence University
Abstract
Introduction: Since the declaration of COVID 19 pandemic by the WHO, the mental health toll the virus has taken on the globe, affects the health care workers in many folds which is reflected by mounting evidence on high levels of anxiety, depression, and stress among HCW.1,2,3 Psychological stresses among HCWs measured in terms of burnout provide valuable evidence to initiate support services in COVID care settings.4 The psychological distress among HCW during a pandemic of current nature, is attributed to being parents of dependent children, being junior in service, longer quarantine period, lack of practical support and stigma5 Though the health system in Sri Lanka is overwhelmingly burdened by the disease little is known about psychological issues of HCW in the country.
Objectives: To Evaluate the prevalence of burnout and to identify some factors associated with burnout among health care workers attached to COVID 19 management settings in Sri Lanka
Methods: A descriptive cross-sectional study was conducted in 8 selected COVID care settings in the country. Data from HCW dealing with COVID care were collected using google forms. Burnout was assessed using the Copenhagen Burnout Inventory with 0-100 scale. A score above 50 is considered as the presence of burnout. Some selected factors associated with burnout was tested with Z test and chi square test.
Results: There were 473 respondents (doctors (33.4%), nurses (51.6%), physiotherapists (4.2%), radiographers (4.2%) and other staff (7.4%)). Sixty-three percent of HCW worked in intensive care facilities. There were 342 (72.5%) females and 125 (26.4%) males. Majority (61%) were between 21 to 30 years. Eighty percent of HCW had no co-morbidities and 91.8% of them were vaccinated against COVID-19.
The overall prevalence of burnout was 70.6 % while the prevalence of personal related, work related and client related burnout were 61.5%, 75% and 71.2% respectively. Burnout of doctors was 65.8% of nurses was 72.5% of physiotherapists was 70% of radiographers was 87.5 and the burnout of other staff was 25%.
Mean burnout score was significantly higher among nurses compared to doctors (p, 0.0033) and female compared to male workers (p, 0.014).
Conclusions: High prevalence of burnout is evident among all categories of HCW in COVID care settings in Sri Lanka. Establishment of necessary support services prioritizing nurses and administrative interventions are recommended.
References
1. Spoorthya M, Pratapab SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review [Internet]. Asian Journal of Psychiatry. 2020 June [cited 2021 June 01]; 51:102119. Available from: https://doi.org/10.1016/j.ajp.2020.102119
2. Khasne RW, Dhakulkar BS, Mahajan HC, Kulkarni AP. Burnout among healthcare workers during COVID-19 pandermic in India: Results of a questionnaire-based survey [Internet]. Indian Journal of Critical Care Medicine. 2020 August [cited 2021 June 01]; 24 (8): 664-671. Available from: http://doi: 10.5005/jp-journals-10071-23518
3. Hu Z, Wang H, Xie J. et al. Burnout in ICU doctors and nurses in mainland China- A national cross-sectional study [Internet]. Journal of Critical Care. 2021 April [cited 2021 June 05]; 65: 265-270. Available from https;//doi.org/10.1016/j.jcrc.2020.12.029
4. World Health Organization, Mental health and psychosocial considerations during the COVID-19 outbreak, 2020. World Health Organization. 2020 March 18 [cited 2021 June 05] Available from: https://apps.who.int/iris/handle/10665/331490
5. Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D, et al. Occurrence, prevention and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis [Internet]. BMJ. 2020 May 5 [cited 2021 June 05]; 369: m1642. Available from: https://doi:10.1136/bmj.m1642
P074
A multi-centre retrospective cohort study to examine the effect of high-dose steroids in COVID-19 pneumonitis admitted to Intensive Care with ARDS
COVID-19
Sanooj Soni1, Sef Carter 2 , David Golding3, Andrew Ritchie1, David Antcliffe1, Ian Rechner3 and Parind Patel2
1Imperial College London
2Imperial College Healthcare NHS Trust
3Royal Berkshire Hospital NHS Foundation Trust
Abstract
Introduction: The use of systemic corticosteroids to suppress SARS-CoV-2–induced lung inflammation is advocated in the treatment of COVID-19 ARDS.1,2 Whilst the evidence for low dose early corticosteroids in COVID-ARDS is well established, the effect of larger steroid doses (i.e. short-term ‘pulse-dose’) is yet to be investigated.
Objectives: The objective of this study was to examine the effect of pulse dose steroids on ventilatory parameters such as oxygenation in COVID-19 patients with and without established fibrosis or organising pneumonia (OP).
Methods: This was a multi-centre, retrospective observational study performed at four teaching hospitals, with the following inclusion criteria: adult patients requiring invasive mechanical ventilation with confirmed PCR SARS-CoV-2 infection; and received high dose steroids for treatment for COVID-ARDS (defined as dose ≥ 20mg dexamethasone or an equivalent dose of methylprednisolone). This study was carried out as a service evaluation within the National Health Service (NHS) and recorded under the auspices of the clinical audit office at Imperial College Healthcare NHS Trust and Institutional Data Protection Office. Study patients were followed for 14 days or until they were discharged from the ICU and physiological or ventilatory variable data was retrospectively collected from patient records.
Results: In total, 92 patients were included: 14 patients 20mg/day dexamethasone; 5 patients 50mg/day dexamethasone; 16 patients 500mg methylprednisolone; and 57 patients 1000mg methylprednisolone.
Our data demonstrate a statistically significant improvement in PaO2/FiO2 (P/F) ratio over time, from baseline to day 14, in those patients who received 1000mg Methylprednisolone (baseline PaO2: 14.47 kPa, Day 3: 17.51 kPa, Day 7: 19.51 kPa, Day 14: 22.87 kPa, p<0.001). Whilst not statistically significant, there was a trend to higher P/F ratios by day 14 in patients who received 500mg Methylprednisolone group. There was no increase in P/F ratios in those patients who received 20mg or 50mg dexamethasone. The increase in P/F ratio was most apparent in those patients who had evidence of fibrosis on CT scan, although some benefit was seen in those patients who did not fibrosis on radiological imaging.
Cross sectional random effects models were used to determine the effect of 1000mg methylprednisolone on improvement in P/F ratio and demonstrate that there was an increase of P/F ratio of more than 0.38 kPa per day in those patients that received 1000mg methylprednisolone. The was no significant effect on compliance measures. There was also a trend to more ventilator free days but no difference in mortality in those patients receiving large dose methylprednisolone. Reassuringly, rates of fungal infection and pneumothorax/pneumomediastinum for patients who received steroids, including those with high dose, were equivocal.
Conclusion: In this study, we present novel data suggesting that large doses of methylprednisolone may be beneficial in patients with severe COVID-19, late in the disease course when ARDS is well established. This benefit was not demonstrated in patients treated with lesser (but still high) doses of steroids (i.e. 20mg or 50mg of dexamethasone) and suggest that larger pulsed-dose steroids may induce reversibility of the disease process, particularly in those who have developed fibrosis.
References
1. Recovery Collaborative group. Dexamethasone in Hospitalized Patients with COVID-19. N Engl J Med 2021; 384:693-704
2. World Health Organization. Corticosteroids for COVID-19. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Corticosteroids-2020.1
P075
Conscious prone positioning of patients with COVID-19 pneumonitis: an audit of practice in the Northwest of England
COVID-19
Kamal Berechid 1 , Noamaan Wilson-Baig2, Andrew Bentley3, Shondipon Laha4, Jane Dean5 and Andrew Martin6
1Health Education England - North West
2Royal Manchester Children’s Hospital
3Manchester University NHS Foundation Trust, Wythenshawe Hospital, Manchester, UK
4Critical Care Unit, Lancashire Teaching Hospitals NHS Foundation Trust, Preston, UK
5East Lancashire Hospitals NHS Trust, Blackburn, UK
6Manchester University NHS Foundation Trust, Manchester Royal Infirmary, Manchester, UK and North West Research and Audit Group
Abstract
Introduction: Prior to the COVID-19 pandemic, evidence in favour of prone positioning was mainly limited to mechanically ventilated patients with ARDS.1 Although there were some reports of oxygenation improvement following conscious prone positioning (CPP) in non ventilated patients,2,3 this intervention was largely unknown outside of critical care units. The pandemic imposed extraordinary pressures on hospitals, encouraging medical teams to innovate and consider CPP in patients with increasing oxygen requirements.4 In April 2020, the Intensive Care Society (ICS) issued guidance for CPP of patients presenting respiratory failure secondary to COVID-19.5
Objectives: The objectives of the study were to assess the practice of CPP and the compliance to ICS guidance in the Northwest of England. We also aimed to evaluate the feasibility of proning and to appraise the impact of position changes on oxygenation. The study was also an opportunity to encourage multidisciplinary teams to consider CPP as a therapeutic tool for patients admitted with COVID-19 pneumonitis in non-critical care areas.
Methods: This was a pragmatic observational prospective cohort study conducted over five weeks in May and June 2020 across seven different hospitals in the Northwest of England. We attempted to capture as many episodes of CPP as possible during this period. We collected various demographics and clinical data related to the patients and to the intervention of proning. We followed up the patients for 28 days from their first episode of CPP. A descriptive statistical analysis was performed using Excel.
Results: Overall, 107 patients were included. Their mean age was 66 years and 55% were candidates for escalation to level 3 care. Among these patients 25% were eventually intubated. Table 1 shows more patients characteristics. A total of 246 episodes of CPP were recorded. Table 2 provides details about CPP episodes. The median duration was 4 hours. Proning was often conducted by patients and physiotherapists, as most (73%) didn’t need assistance. CPAP was used simultaneously in a significant proportion (38%). One fifth of the CPP had to be discontinued, mostly because of discomfort. We focused on the first episode to assess practicalities and effect on oxygenation (Table 3). Only 9% of episodes were reported to follow ICS guidance as most interventions had to be tailored to local logistics and to patients’ comfort. Thirteen per cent of CPP were initiated in morbidly obese patients despite it being mentioned as a relative contraindication. In terms of oxygenation, desaturation occurred within the first 15 minutes in 21% of cases. There was a tendency to improvement of FiO2 and SF ratio after 24 hours of the first CPP.
Table 1.
Patients Characteristics
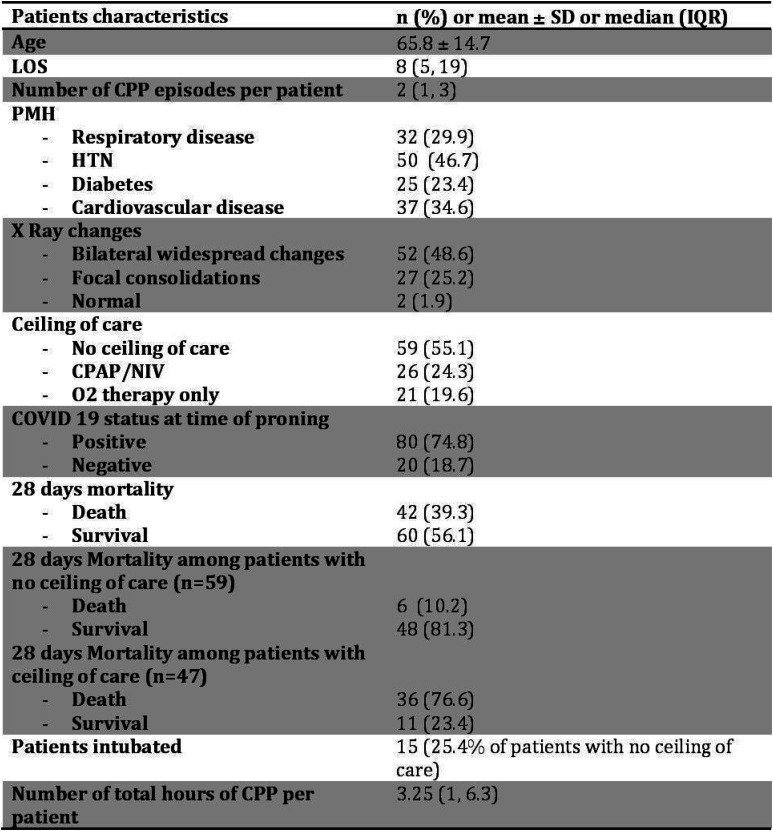
|
Table 2.
Characteristics of CPP therapies
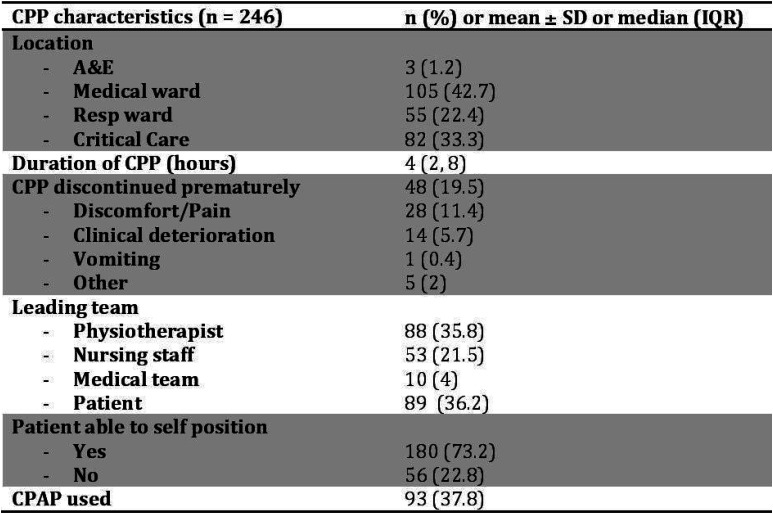
|
Table 3.
Characteristics and impact of first CPP.
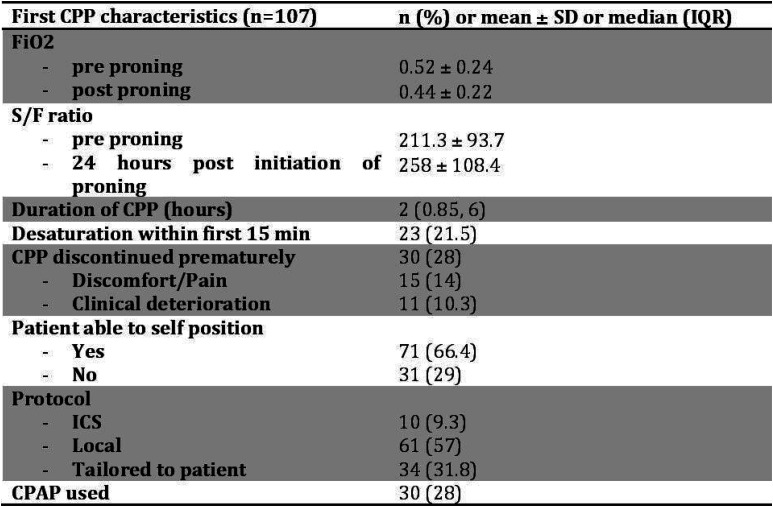
|
Conclusion: In summary, a pragmatic approach often dictated departure from intensive care soceity guidance. Although CPP was largely feasible, it had to be adapted in most cases to the patients, their environment, the logistics, and their ventilatory support. It was often self-administered and didn’t seem to be limited by morbid obesity for example. While the results and experience suggest a positive impact of CPP on oxygenation, only a well-designed comparative trial could determine the role of position changing in preventing intubation or death.
The authors would like to thank the NWRAG and all the local team members, physiotherapists, nurses and doctors, who endeavoured to collect invaluable data under unprecedented clinical circumstances.
References
1. Guérin, C., Reignier, J., Richard, JC., et al. PROSEVA Study Group. Prone Positioning in Severe Acute Respiratory Distress Syndrome. N Engl J Med 2013; 368: 2159–2168
2. Valter C, Christensen AM, Tollund C, Schønemann NK. Response to the prone position in spontaneously breathing patients with hypoxemic respiratory failure. Acta Anaesthesiol Scand. 2003;47:416–418.
3. Scaravilli V, Grasselli G, Castagna L, Zanella A, Isgrò S, Lucchini A, et al. Prone Positioning improves oxygenation in spontaneously breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective study. J Crit Care. 2015;30:1390–1394.
4. Caputo ND, Strayer RJ, Levitan R. Early Self-Proning in Awake, Non-intubated Patients in the Emergency Department: A Single ED’s Experience During the COVID-19 Pandemic. Acad Emerg Med. 2020;27:375-378.
5. Bamford P, Bentley A, Wilson-Baig N, Dean J, Whitmore D. 2020. Intensive Care Society. ICS Guidance for Prone Positioning of the Conscious COVID Patient 2020. Retrieved from https://emcrit.org/wp-content/uploads/2020/04/2020-04-12-Guidance-for-conscious-proning.pdf [Accessed on 20th August 2021]
P076
Critical leg ischemia related to COVID 19 in doubly vaccinated patients
COVID-19
Faryal Zaman1 and Bushra Zaman 2
1Kings College Hospital London - London
2People’s medical College, Pakistan
Abstract
Background: COVID and venous thromboembolism in unvaccinated population is now a well-established entity but this case is unique as the 1) patient had both COVID vaccines and then tested positive for COVID and 2) presented with vague symptoms and had minimum oxygen requirement 3) developed arterial thromboembolism and acute leg ischemia after 4 days of admission leading to limb amputation ultimately. Data on COVID and COVID vaccine’s association with Arterial thromboembolism still needs to be explored. In our case it was challenging to establish whether the thromboembolism was a complication of vaccine, COVID or was that the result of synergistic interaction of both.
Case Presentation: 61 Years old gentleman presented to Emergency Department with vague history of lethargy ongoing for 3-4 weeks and no significant prior co-morbid except sickle cell trait.
He had received both doses of COVID vaccine 2 months before presentation and denied any shortness of breath, cough, fever or pain. On presentation he was de-saturating to 77% on Room air and had bilateral crepitations in his chest with PO2 of 7.4 kPa on ABG and raised inflammatory markers on bloods. His CXR showed changes consistent with COVID and he was started on Dexamethasone. His COVID test came back as positive.
Throughout his stay maximum amount of oxygen required by him was 36% day1 which improved to 28- 32% later, he had not been tachypneic or tachycardiac. His d-dimer was raised at 3000 which was thought to be COVID related, and the decision was taken to perform CTPA to rule out Pulmonary embolism if oxygen requirement worsens.
His oxygen requirement continued to remain static with a little improvement or worsening. His inflammatory markers also got better.
On Day 4 Patient complained of Right Leg pain. On further enquiry he revealed pain has been ongoing for last 2-3 weeks. His legs were bilaterally ice cold to touch and had hair loss in bilateral legs, pulses in both legs down the femoral artery were not palpable bilaterally.
His blood gas Lactate was 2.6 with worsening inflammatory markers but no fever spikes or worsening in oxygen requirement or any other symptoms apart from leg pain.
He was immediately seen by vascular Surgery team and was started on therapeutic anticoagulation suspecting acute leg ischemia.
CT Angio report showed: Occlusion of Right iliac system, common femoral artery part of the SFA and all the popliteal artery and tibial vessels and unstable thrombus in the left common iliac artery causing severe stenosis and occluded left TP trunk.
He was continued on therapeutic anticoagulation and then underwent Right iliofemoral embolectomy, on table angiogram, left common iliac angioplasty via left groin approach and right above knee amputation.
Postoperatively he remained well and was tested COVID negative later. He was then discharged to Rehab from hospital for further care.
Discussion and conclusion: We suggest that COVID patients with significantly raised d-dimers should be investigated for hidden thromboembolic focus in same way in non COVID patients and not just in lungs but in other organ systems as well. There should be some guidelines regarding increased dose prophylaxis or a flowchart to investigate for these thromboembolic association in COVID.
References
1. Nowroozpoor A, Bank MA, Jafari D. Limb ischemia due to extensive arterial thrombosis in the absence of venous occlusion as an unusual complication of critical illness from COVID-19. Case Rep Acute Med. 2021;4(1):23–31
P077
Taking Stock: Mobile Covid-19 airway trolleys, whose responsibility is it?
Critical care organisation, quality management, costing and outcomes
Lois Nunn, Sophie Hawkins, Jagdish Sokhi and Christopher Lockie
Chelsea and Westminster NHS Foundation Trust
Abstract
Introduction: During the COVID-19 pandemic, mobile airway trollies formed an integral part of the emergency airway management. The AAGBI and ICS produced consensus guidelines recommending a COVID-19 airway trolley or pack; however, the maintenance guidance of these trollies is unclear.1
The pandemic placed severe pressure on all critical care staff, especially nursing staff. The airway trolley checks were transitioned to the junior doctors after wave one at Chelsea and Westminster Hospital. Unfortunately, trollies were not adequately checked and stocked. This created potential delays with emergency tracheal intubations, jeopardizing patient safety. Using a Plan Do Study Act (PDSA) approach we attempted to understand the factors affecting our compliance and ultimately improve patient safety.
Objectives:
1. Identify which group of ICU professionals should check the airway trollies
2. Identify the barriers to safety checks?
3. Assess which targeted interventions improve compliance with checks?
Methods: Single centre, prospective data collection (surveys n= 23 and trollies checklist compliance) over a 7 month period. Data on the frequency and accuracy of the checks was collected monthly. Surveys were used to identify appropriate and targeted interventions. Interventions were made at each cycle to address shortfalls in checks.
Results:
1. 87% of staff believed that doctors (SHOs or SpRs) should check the airway trollies.
2. Barriers identified were
1. Lack of time or too busy 68%
2. Lack of organisation (finding stock or understanding equipment) 41%
3. Difficulty in finding the checklists 27%
3. Compliance improved from 34% to 77%, through various interventions (see graph below)
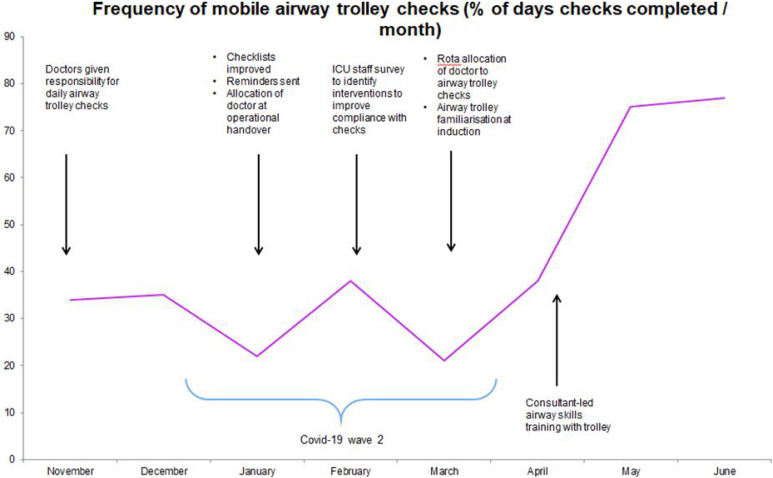
At baseline (November) trolley check compliance was 34%. Changes were made to improve accessibility of checklists and equipment, and daily reminders were added to the morning operational handover. However, this only improved the check frequency to 38%.
A staff survey highlighted recommendations for improvement: daily allocation of checks to a specific doctor and airway education. The trolley check allocation was built into the doctors’ rota and airway trolley education was added to the departmental induction. There was minimal initial change in the following month but further applied education in the form of consultant-led airway skills sessions to engage the doctors in the process saw rates drastically improved to 75% and 77% over the following two months.
Unpredictable challenges which negatively influenced the results were identified. These included surge rotas, including redeployed non-ICU doctors in checks and increased trolley numbers with increased ICU capacity.
Conclusions: This quality improvement project, performed during the height of a pandemic, demonstrates the importance of adaptation and persistence to identify interventions that take into account the evolving clinical environment and human factors. It highlighted the difficulty in building new habits within the daily routine of junior doctors and the necessity of senior lead teaching to build the doctors’ confidence, understanding and engagement with safety processes. Following the rigorous cycles, it is expected that the routine for the trolley checks is sufficient to withstand the rotations of junior doctors and expansion of the department in potential future waves of the pandemic.
References
1. Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia. 2020 Jun;75(6):785-799. doi: 10.1111/anae.15054. Epub 2020 Apr 1. PMID: 32221970; PMCID: PMC7383579.
P078
Service Review of an Enhanced Respiratory Care Area Developed in Response to the Covid-19 Pandemic
Critical care organisation, quality management, costing and outcomes
Abigail Levison1, Jane Dean 2 and Jamie Swales2
1East Lancashire Hospital Trust
2East Lancashire Hospital
Abstract
Introduction: During the second wave of the COVID-19 pandemic, regional modelling predicted an acute surge in the demand for level 2 respiratory beds. Locally, these patients were cared for on the ICU. Capacity expanded from 20 to 42 beds in response to the pandemic, but the anticipated demand could not be met in the existing critical care footprint. Early evidence suggested that CPAP and high-flow oxygen could reduce the requirement for mechanical ventilation by up to 50% for patients with Covid-19.1-2
Objectives and Methods:
• An enhanced respiratory care a rea was created for a cohort of level 2 respiratory patients to provide CPAP and High-Flow oxygen on a 1:4 practitioner to patient ratio with the aim of relieving staffing and bed pressures on ICU whilst providing equitable care and outcomes to that given to patients on the main unit
• Admission criteria stipulated patients should have either single organ failure, independence with self-care, capacity and/or pre-established escalation status
• The area was staffed by an acute care team, a team of practitioners from a variety of professional backgrounds including nursing and AHP’s who normally provided the Trust’s citical care outreach and acute care support through advanced cinical practitioners, non-medical prescribers, practitioners, and specialist HCAs. Physiotherapists and junior doctors were assigned to the unit and supported with their typical professional roles and bedside care.
• A service review was undertaken including analysis of admission data, length of stay and unit mortality. A retrospective clinical audit measuring care delivered against the area’s initial standard operating procedure and objectives was also undertaken against 15% of patient notes.
Results:
•67 patients admitted over 40 days
•247 critical care bed days saved
•Median length of stay 3.68 days
•50.7% patients stepped down to wards; 34.3% escalated to critical care; 14.9% died.
•Median age 63, 2:1 male: female ratio
Conclusion: The enhanced respiratory care area provided an innovative response to the local critical care COVID-19 bed crisis by cohorting level 2 respiratory patients and transformational workforce planning and care modelling. This enabled a rapid and targeted response to the crisis which provided quality care that was at least equivalent to the length of stay and mortality outcomes of the local ICU, whilst significantly reducing ICU bed and workforce pressures.
References
1. Calligaro G, Lalla U, Audley G, Gina P, Miller M, Mendelson M, et al. The utility of high-flow nasal oxygen for severe COVID-19 pneumonia in a resource-constrained setting: A multi-centre prospective observational study. The Lancet Online. 2020
2. Nightingale R, Nwosu N,KutubudinF, Fletcher T, Lewis J, Frost F, et al. Is continuous positive airway pressure (CPAP) a new standard of care for type 1 respiratory failure in COVID-19 patients? A retrospective observational study of a dedicated COVID-19 CPAP service. BMJ Open Respiratory Research. 2020;7(1):e000639.
P079
Monitoring nasogastric tube (NGT) displacement using chest X-ray (CXR) requests: Influence of tube fixation
Critical care organisation, quality management, costing and outcomes
Anthony Thomas, Mahmoud Gaballah and Juiliana Hamzah
Salford Royal Hospital
Abstract
Introduction: Unplanned removal of NGTs is common and associated with multiple complications.1 Methods used to secure these tubes may influence removal rates.2 Following national guidance,3 we confirmed tube placement by CXR. We used the text of CXR requests to estimate the rates of NGT placement and to see how these were influenced by changing how NGTs were secured. We also used similar methodology to review changes to CXR requests mentioning central lines (CVCs) and endotracheal tubes (ETT).
Objectives: To see how CXR requests for NGT placement were influenced by changing the method used to secure these tubes.
MethodsIn a 42 bedded mixed general and neurosurgical unit, in November 2019 we changed the method to secure NGTs from Hollister feeding tube attachment devices (Hollister, IL, USA)., to handcrafted slings made from Micropore (3M, MN, USA) 1.25cm Surgical Tape.4 The text of CXR requests between October 2017 and July 2021 were analysed for text associated with NGTs, CVCs and ETTs. The number of bed days was calculated for each month from October 2017 and CXR rates per 100 bed days were calculated. Mann-Whitney U tests were used to establish if CXR rates changed significantly after November 2019 and after admitting patients with COVID-19 in March 2020. Distributions are shown as medians with [IQR].
Results: There were 15239 CXRs, a median of 330 [IQR 303-357] CXRs requested a month. The fraction mentioning each device was: ETT: 8%, CVC: 13%, NGT: 38% (18% of these also mentioning another device). The rates per 100 patient days per month were: NGT pre-Nov 2019: 15.9 [15.0-16.4]. Post-Nov 2019 11.6 [10.1-12.7] (p<0.001), Nov 2019 to February 2020: 12.0 [8.0-13.3], vs Pre Nov 2019 p=0.008. For CVCs pre-March 2019: 4.1 (3.6-4.6) post March 2019: 5.2 (4.6-5.9) (p< 0.001) for ETTs pre-March 2019: 2.8 (2.0-3.3), post-March 2019: 3.1 (2.4-3.7). Changes in monthly rates are shown in the run chart in Figure 1.
Figure 1.
Number of X-Rays each study month per 100 bed days each device. Arrow show 1.change to Hammock Dressings to secure NG tubes and 2. the start of the covid 19 pandemic.
Conclusions: Changing the method of securing NGTs resulted in a reduction of CXR requests mentioning NGTs, reviewing CXR requests can be used to monitor NGT displacements. The rate of CVC requests increased following March 2020.
References
1. Carrion MI, Ayuso D, Marcos M, et al. Accidental removal of endotracheal and nasogastric tubes and intravascular catheters Crit Care Med 2000; 28: 63-66.
2. Gunther S C, Schwebel C, Vesin A, et al. 2009 Interventions to decrease tube, line, and drain removals in intensive care units: the FRATER study Int Care Med 2009; 35: 1772-1776.
3. NHS Improvement: Nasogastric tube misplacement: continuing risk of death and severe harm https://www.england.nhs.uk/publication/patient-safety-alert-nasogastric-tube-misplacement-continuing-risk-of-death-and-severe-harm/ (2016, accessed 16th August 2021)
4. S.Brown, Hannah Sapir: The Hammock method of NG fixation. https://www.youtube.com/watch?v=sXB-IEPTV44 (2019, accessed 16th August 2021)
P080
Emergency bag checks in ICU: sharing good practice to improve patient safety Critical care organisation, quality management, costing and outcomes
Emergency bag checks in ICU: sharing good practice to improve patient safety
Robyn Beaty, Laura Chase and Sian Moxham
Great Western Hospital, Swindon
Abstract
Introduction: Grab bags containing emergency drugs and equipment are required in ICU for use in arrest or trauma situations around the hospital. Resuscitation Council UK guidelines state that ‘a reliable system of equipment checks, and replacement must be in place and the frequency of the checks should be determined locally’.1 Great Western Hospital ICU guidelines state these should be checked daily. Due to the increased pressure of the Covid-19 pandemic, temporary ICUs were set up and staff unfamiliar with ICU equipment were redeployed. We noticed that checks were not being done on a regular basis. This led to incidents in emergency situations where the correct equipment was not available. We required a robust system that was transferable across different settings to allow staff to easily check kit.
Objectives: To improve the number of days per week bag checks are carried out to 80%.
Methods: A retrospective audit on how often drug and bag checks had been carried out was completed. We then designed QR codes that linked to a kit list allowing for easy recognition of required kit as well as recording of checks. This system had already been successfully introduced at another ICU in our region.2 The QR codes were displayed at all locations of the emergency kit and staff were informed via email, Whatsapp and at handovers of the new system. A reminder was added to the doctors’ daily jobs list and a bag checks champion was nominated after August change over to try to maintain the change.
Results: Fridge drug bags checks that were recorded in February showed drugs were only checked 2 – 4 days a week (28%-57%). The large bags were only recorded as checked on 1 -2 days a week (14%-28%). After intervention 1 (QR code and email sent), this improved to 4-5 days a week for all bag checks (57%-71%). After intervention 2 (morning handover reminders), the results showed all bags being checked between 3-6 days a week (42%-85%). After intervention 3 in June, all bag checks were being carried out 5-7 days a week (71%-100%). There have been no incidents of kit being unavailable since the beginning of QR code use.
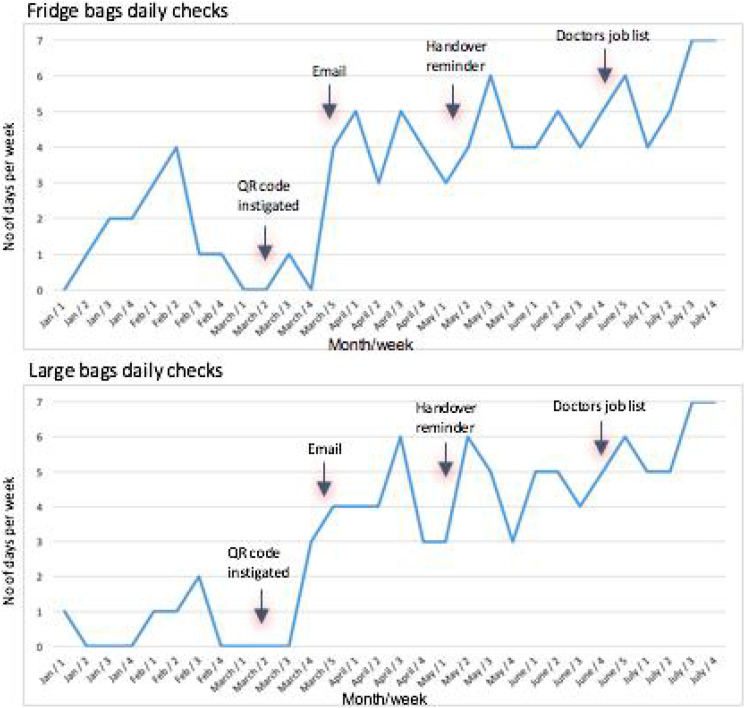
Conclusions: Sharing good practice from other ICUs in our region via rotating trainees has allowed us to put in place a robust system for checking emergency equipment. This system is easy to expand should demand require temporary ICUs again and makes identification of kit easy as pictures can be added for staff who may be unfamiliar. Data is collected centrally allowing for easy record keeping. Going forward we must ensure that the culture of using this system is passed on to each group of trainees.
Example checklists:

Fridge drug bag checks

Large bag checks
References
1. Resuscitation Council UK. Quality Standards: Acute care equipment and drug lists. Nov 2013 Last updated May 2020.
2. Savage B. ICU. North Bristol NHS Trust
P081
Compliance of treatment escalation plan in a district general hospital
Critical care organisation, quality management, costing and outcomes
Clarisse Mizzi 1 , Thomas Gower2, Rumneek Hampal2 and Rahuldeb Sarkar2
1Epsom and St Helier University Hospitals NHS Trust
2Medway NHS Foundation Trust
Abstract
Introduction: Treatment escalation plans (TEPs) allow the clinician and patient to discuss treatment options prior to a potential deterioration. Frailty is becoming increasingly common in the ICU, with frailty associated with higher ICU and hospital mortality.1,2
Objectives: To determine if treatment escalation plans are completed in acute medical admissions. If not completed, we assessed if treatment escalation plans are completed throughout their ward stay. We aimed to evaluate if completion rates varied based on patient clinical frailty score and national early warning score.
Furthermore, we aimed to determine if there were common themes as to possible reasons for non-compliance of TEPs completion.
Methods: Ambidirectional analysis of acute medical admissions data between 9 – 13 Decemebr 2019 was performed. Electronic and paper health records were used to collect treatment escalation plan, clinical frailty score (CFS) and national early warning score (NEWS). Admissions without a treatment escalation plan form were followed-up throughout the data collection period. Frailty was defined as CFS > 4.
A questionnaire was given out to 11 acute medical doctors, from foundation doctors to consultants.
Results: Out of the admissions (N=138), 83% (n = 114/138) did not have a TEP form completed within 24 hours of admission. Out of the 83%, TEP form was completed in 2.6% (n = 3/114) during a 5 day follow-up period. TEP form was completed in 33% (n = 18/54) and 7% (n = 6/84) in the frail (CFS >4) and non-frail (CFS ≤4) respectively (Figure 1). TEP form was completed in 32% (n = 9/28) and 14% (n = 15/110) in patients with NEWS equal or greater than 5 and NEWS 4 or less respectively. Out of the frail patients, 37% (n = 20/54) had a NEWS 5 or greater.
Figure 1.
TEP form completion and non-completion in non-frail (CFS ≤4) and frail patients (CFS >4)
In the thematic analysis of the responses in the questionnaire, themes surrounding lack of completion mentioned were, time constraints during acute take, reluctance in discussing ceilings of care with patients and relatives and hesitancy in deciding TEPs in the first 24 hours of care.
Conclusions: The audit demonstrated that a large proportion of acute medical admissions are not having TEPs discussed and documented. If ceilings of care are not documented within the first 24 hours of admission, TEPs are unlikely to be completed. TEPs compliance is greater in frail and unwell patients however still poor. Opportunities might be being missed to explore patients’ wishes before deteriorating, with less than half of the frail and sick patients having TEPs completed. There is a need to have greater emphasis on clinical engagement in this vital aspect of patient care. Plans need to be put in place for increased collaboration between acute physicians and other specialties including critical care.
References
1. De Biasio Justin C, Mittel Aaron M, Mueller Ariel L, et al. Frailty in Critical Care Medicine: A Review. Anesthesia and Analgesia 2020; 130(6): 1462–1473.
2. Kahlon S, Pederson J, Majumdar SR, et al. Association between frailty and 30-day outcomes after discharge from hospital. Canadian Medical Association Journal 2015; 187(11): 799–804.
P082
Staff experiences of working on a new Critical Care Unit during the COVID 19 pandemic
Critical care organisation, quality management, costing and outcomes
Sian Saha 1 , Harriet Noble1, Andreas Xyrichis2, Eleanor Corcoran1, Tom Best1, Philip Hopkins1 and Louise Rose2
1King’s College Hospital
2King’s College London
Abstract
Introduction: Intensive Care Unit (ICU) design impacts staff well-being1 with relocation to a different ICU layout causing staff stress.2,3 During the COVID-19 pandemic our new critical care centre was opened expediently allowing increased patient capacity and providing a purpose-built environment for ICU patients.
The new single-bed room layout differed to other open plan multi-bed ICUs in the hospital. New design features included large floor-to-ceiling windows with park views, modernised equipment such as computer screens on movable pendants and noise reduction features.
The pandemic accelerated the opening of the new unit and practice was adapted to address surge conditions (e.g., there were two patients in each ‘single’ room, and PPE could only be worn in specific areas of the unit, restricting movement).
Objectives: We sought to understand the impact of the ICU design on staff experiences during pandemic conditions.
Methods: Following ethical approval, staff who had worked on the new unit were invited to participate in a semi-structured interview. The interview guide was based on the Theoretical Domains Framework (TDF),4 a framework to identify the determinants of behaviour change. Interviews were audio recorded, anonymised and transcribed verbatim. We used line-by-line coding and analysed data informed by the TDF.
Results: 21 participants captured experiences of a wide range of multi-disciplinary staff members. The most common domain identified within the data was ‘Environmental context and resources’, including data pertaining to barriers and facilitators of the new unit to effective working:
“Having large bed spaces is perfect for getting people out [of bed]. They are soundproofed as well, so patients were sleeping really well at night.”
Also, ‘social/professional role and identity’ (including group identity, leadership), ‘skills’ (including competence, skills development), and ‘beliefs about consequences’ (perception of the effects of the new units) were frequently identified in positive and negative ways:
“….because of where it [the patient’s room] is located you do not get to see people often. I got forgotten for rolls…..It was a constant struggle”
Medical staff and allied health professionals described advantages over the old unit design including improved team-working, oversight of patients, and mood from the design features. Participants perceived patient benefits from improved lighting and views and stimulation due to access to social media.
Conversely, nurse participants perceived less support, less team-working and increased levels of anxiety due to the single rooms. Nurse experiences improved as patient numbers reduced. However, changes in how nurse teams worked was an ongoing challenge:
“…staffing breaks and things is quite tricky. You need a permanent floater that is never allocated to patients, to try and help people, because they cannot leave their bays.”
Conclusions: Our findings support previous research2 demonstrating increased nurses stress when transitioning to a single-bed room ICU layout. Providing systems to alleviate nurse isolation, promote team-working and reduce stress in future relocations may significantly improve staff well-being (e.g., video-calling and messaging between patient rooms). A multi-disciplinary awareness of the impact on nurses is vital to support strategies to ameliorate the impact of changes during relocation.
Research grant awarded From King’s College Hospital Charity.
References
1. Shepley MMC, Gerbi RP, Watson AE, Imgrund S, Sagha-Zadeh R. The impact of daylight and views on ICU patients and staff. HERD 2011;5(2):46-60.
2. Broyles GW, Washington GT, Lowry LW, Gugliotta B, Eorgan P, Wilhoit K. Innovative solutions. Registered nurses’ perceptions of the work environment before and after adult intensive care unit renovations. Dimens Crit Care Nurs 2008;27(4):180-188.
3. De Matos LBN, Fumis RRL, Nassar Junior AP, Lacerda FH, Caruso P. Single-bed or multibed room designs influence ICU staff stress and family satisfaction, but do not influence ICU staff burnout. HERD 2020;13(2):234-242.
4. Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, (2005) on behalf of the ‘‘Psychological Theory’’ Group: Making psychological theory useful for implementing evidence-based practice: a consensus approach. Quality Safety Health Care 14:26–33.
P083
National standardisation of an induction pathway for trainee advanced critical care practitioners
Critical care organisation, quality management, costing and outcomes
Anita Jones1, Kate McCormick2, Lucy Halpin3, Natalie Gardner4, Caroline McCrea3, Jo-Anne Gilroy5, Louise Houslip6, Ali Hopkins7, Stevie Park8 and Ashton Burden-Selvaraj 8
1The Dudley Group
2University Hospitals Birmingham
3Portsmouth University Hospital
4Kings College Hospital, London
5The Royal Marsden Foundation Trust
6Royal Devon & Exeter Hospital
7Colchester Hospital
8University Hospital Coventry and Warwickshire
Abstract
Introduction: Due to the shortfall in the medical workforce, critical care1 now embraces the advanced practice role. With the introduction of The National Education and Competence Framework for Advanced Critical Care Practitioners (ACCP),2 ACCP’s now have a recognised role and are within the Guidelines for the Provision of Intensive Care services (GPICS).3,4Although trusts are employing trainee ACCP’s (tACCP’s), it is an incredibly daunting process, regardless of professional experience. Throughout many NHS Trusts, ACCP teams have been expanding, with what appeared to be variable inductions for the trainees.
Objectives: A working group of trainees and qualified ACCPs was formed, with the support of The Faculty of Intensive Care Medicine ACCP sub-committee (FICMASC), ACCP clinical leads and University representatives. As a working group we recognised that there were key resources and information available which was often not identified or utilised until later in training. As a group, our intentions were to signpost trainees to these resources early on in their training, standardise the induction process for all tACCP’s. Ultimately, providing an adaptable framework for the trainee and their Trust to navigate the two-year pathway.
Methods: A national consultation was undertaken to evaluate current tACCP induction pathways. This process took the form of a national survey, with questions regarding what should be in an induction for tACCPs. The opinion from the ACCP community was sought to underpin these recommendations. This was then a base for an Induction framework, enabling effective transition from the individual’s base profession to tACCP. The induction guide would be for both the Clinical and Academic aspects of the two-year specialist training program, aiming to effectively support, inform and guide new tACCP’s. In the long run, this guide should also provide the clinical department a structured induction program which sets out the training expectations and scope of practice for the tACCP.
A set of 55 questions were developed, which examined: professional demographics, current induction pathways, HEI (Health Education Institutes) induction pathways specific to ACCPs, technology and study skills, clinical pathway induction and practical skills along with resources for seeking help.
A survey was utilised using a Google Form platform which was shared via multiple social media areas.
The survey then ran for 2 weeks in April 2021 and received a total of 106 respondents.
Members of the working group then took shared responsibility for data analysis which has underpinned the recommendations made within the framework.
Results: The survey showed an overwhelming need for a standardised induction guide. The induction pathway document was then developed by the working group, based on feedback and recommendations from the survey results.
National peer review was also sought prior to the induction document being sent to Faculty of Intensive Care Medicine (FICM) for potential ratification and endorsement.
Conclusion: Once accepted by FICM, the document will be sent out nationally as the recommended framework for Trusts to use for future tACCPs. Once implemented, for a period of a year a further National survey will be sought for evaluation and changes will be made as required.
References
1. Nuffield Trust. Reshaping the workforce to deliver the care patients, 2016. https://www.nuffieldtrust.org.uk/files/2017-01/reshaping-the-workforce-web-final.pdf
2. Department of Health (2008) The National Education and Competence Framework for Advanced Critical Care Practitioners
3. Guidelines for the Provision of Intensive Care Services V2 (2019). https://www.ficm.ac.uk/standards-research-revalidation
4. NHS England. NHS Five Year Forward View [Internet]. 2014. https://www.england.nhs.uk/five-year-forward-view
P085
Trajectories of CRP as a measure of biological mechanisms underlying ethnicity associated outcomes in COVID-19
Data science
Yize Wan, Zudin Puthucheary and John Prowle
Queen Mary University of London
Abstract
Introduction: Patients with Black and Asian ethnic background have been disproportionately affected by COVID-19 with increased disease severity, ICU admission, organ failure, and premature mortality.1-4 We have shown that routinely collected markers including CRP were increased in Black and Asian patients2 potentially reflecting increased systemic inflammation. Characterising these differences is required to address the excess morbidity and mortality in these ethnic groups.
Objectives: To assess CRP as a candidate biological feature that might drive ethnicity associated outcomes of COVID-19.
Methods: Prospective analysis using registry data from all patients aged ≥16 years with an emergency admission to hospitals within Barts Health NHS Trust with SARS-CoV-2 infection during 1 January 2020 – 13 May 2020 (wave 1), and 1 September 2020 - 17 February 2021 (wave 2). Trajectories of routine haematology and clinical biochemistry blood results during hospital admission were assessed, and distinct phenotypes defined using unsupervised longitudinal clustering techniques using day 0 to 15 results. We determined distribution of identified phenotypes within patients categorised by ethnic group. Multivariable logistic regression accounting for predefined baseline risk factors was used to assess association between ethnicity, phenotypes, and 30-day mortality. All analyses were performed using R software v4.02 and the kml package for clustering.5 Results are presented as n (%) and adjusted odds ratios (OR) with 95% confidence intervals.
Results: After excluding those with unknown ethnicity and those with <7 blood results, we assessed 421 (wave 1) and 1057 (wave 2) patients. Three phenotypic clusters were identified based on trajectories of CRP. In wave 1, 38.2% of patients had persistently lower levels of CRP, median ≤100mg/dl (A), 38.0% had an initial peak, median >200mg/dl at day 2-3 followed by a gradual reduction (B), and 23.8% had a higher peak, median >300mg/dl at day 5 remaining persistently elevated through day 15 (C). In wave 2, 65.5% had persistently lower CRP levels (a), 18.0% had a slow secondary rise after around 7 days, peaking around day 14 with median >250mg/dl (b), and 16.6% had an early peak to >200mg/dl followed by a gradual reduction (c). In wave 1, cluster C was associated with highest risk of death by 30 days compared to cluster A (OR 6.21 [3.12-12.36], p<0.001). In wave 2, cluster b (OR 7.29 [4.97-10.71], p<0.001) had higher risk of death compared to cluster a. Greater proportions of ethnic minority patients were within cluster C in wave 1 (23.5% Asian, 31.3% Black, 13.6% White, p<0.001) and in cluster b in wave 2 (22.0% Asian, 19.6% Black, 14.3% White, p=0.01). Inclusion of CRP trajectory attenuated the higher risk of death associated with Asian and Black ethnicity in wave 1 and Asian ethnicity in wave 2.
Table 1.
Baseline characteristics by CRP cluster.
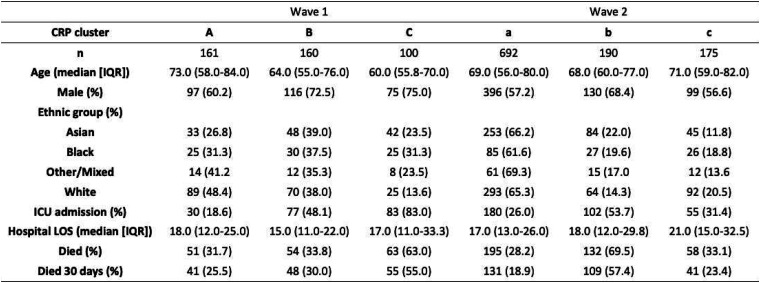
|
Figure 1.
Distribution of CRP clusters by COVID-19 wave and associated 30-day survival by cluster.
Conclusions: Phenotypes based on CRP trajectories during hospital admission are associated with adverse outcomes following COVID-19 infection. Differences in these relationships were evident between first and second waves which were differentiated clinically by widespread use of Dexamethasone, but not IL-6 blockade, in second wave patients. Further work is needed to understand underlying mechanisms behind phenotypes of COVID-19 susceptibility.
Funding: ICS New Investigator Award 2020
References
1. Sze S, Pan D, Nevill CR, et al. Ethnicity and clinical outcomes in COVID-19: A systematic review and meta-analysis. EClinicalMedicine 2020; 29: 100630.
2. Apea VJ*, Wan YI* (equal contributors), Dhairyawan R, Puthucheary AZ, Pearse RM, Orkin CM, Prowle JR. Ethnicity and outcomes in patients hospitalised with COVID-19 infection in East London: an observational cohort study. BMJ Open 2021;11:e042140.
3. Wan YI, Apea VJ, Dhairyawan R, et al. Ethnic disparities in hospitalisation and hospital-outcomes during the second wave of COVID-19 infection in east London. medRxiv07.05.21260026.
4. Wan YI*, Bien Z* (equal contributors), Apea VJ, et al. Acute Kidney Injury in COVID-19: multicentre prospective analysis of registry data. Clin Kidney J 2021: sfab071.
5. Genolini C, Alacoque X, Sentenac M, & Arnaud C. Kml and kml3d: R packages to cluster longitudinal data. Journal of Statistical Software. 2015;65(4); 1–34.
P086
Trajectories of UCR as a measure of biological mechanisms underlying ethnicity associated outcomes in COVID-19
Data science
Yize Wan, Zudin Puthucheary and John Prowle
Queen Mary University of London
Abstract
Introduction: Patients with Black and Asian ethnic background have been disproportionately affected by COVID-19 with increased disease severity, organ failure, intensive care admission, and premature mortality.1-3 The urea-to-creatinine ratio (UCR) has been described as a biochemical signature of persistent critical illness, its hallmark catabolic state and late mortality during prolonged ICU stay.4 Low serum creatinine reflecting reduced muscle mass, which declines rapidly in acute severe illness in combination with net muscle protein breakdown which contribute substrate for increased hepatic urea synthesis, results in markedly elevated UCR.
Objectives: To assess UCR as a candidate biological feature driving ethnicity associated outcomes of COVID-19 disease.
Methods: Prospective analysis using registry data from all patients aged ≥16 years with an emergency admission to hospitals within Barts Health NHS Trust with SARS-CoV-2 infection during 1 January 2020 – 13 May 2020 (wave 1), and 1 September 2020 - 17 February 2021 (wave 2). Trajectories of routine haematology and clinical biochemistry blood results during hospital admission were assessed, and distinct phenotypes defined using unsupervised longitudinal clustering techniques using day 0 to 15 results. We determined distribution of identified phenotypes within patients categorised by ethnic group. Multivariable logistic regression accounting for predefined baseline risk factors was used to assess association between ethnicity, phenotypes, and 30-day mortality. All analyses were performed using R software v4.02 and the kml package for clustering.5 Results are presented as n (%) and adjusted odds ratios (OR) with 95% confidence intervals.
Results: We assessed 459 (wave 1) and 1337 (wave 2) patients after excluding those with unknown ethnicity and those with <7 blood results. Three clusters were identified based on trajectories of UCR. In wave 1, 48.1% of patients had persistently low levels of UCR (A), 38.6% had higher but stable levels (B), and 13.3% had the highest levels peaking after day 7 (C). In wave 2, three clusters were identified in similar proportions: 42.8% (a), 45.1% (b), 12.1% (c). In wave 1, patients in cluster C compared to A had the highest risk of death at 30 days (OR 4.59 [2.27-9.26], p<0.001). In wave 2, both clusters b (OR 1.58 [1.18-2.12], p< 0.001) and c (OR 3.96 [2.62-5.99], p<0.001) had higher risk of death compared to a. Distribution of cluster membership varied by ethnic category. In both waves, greater proportions of patients within cluster A/a were observed in patients with Black ethnicity (65.5% wave 1, 61.1% wave 2) compared to Asian (50.0% wave 1, 37.3% wave 2) and White (39.7% wave 1, 39.6% wave 2) ethnicity. Black ethnicity patients also had lowest proportions in cluster C/c (6.9% wave 1, 6.3% wave 2) compared to Asian (17.4% wave 1, 14.2% wave 2) and White (13.2% wave 1, 12.9% wave 2) ethnicity. Inclusion of UCR trajectory attenuated the higher risk of death seen in Asian patients in wave 1.
Table 1.
Baseline characteristics by UCR cluster.
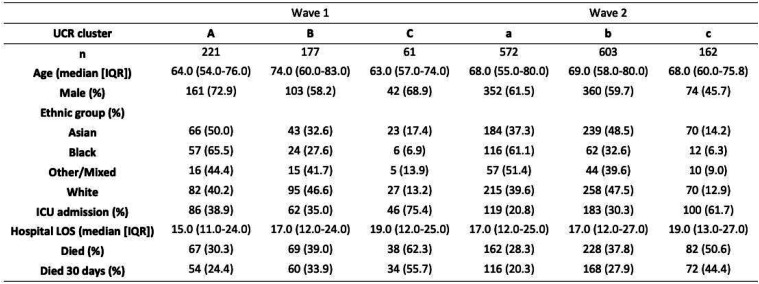
|
Figure 1.
Distribution of UCR clusters by COVID-19 wave and associated 30-day survival by cluster.
Conclusion: Phenotypes based on UCR trajectories during hospital admission are associated with adverse outcomes following COVID-19 infection. Further work is needed to understand phenotypes of prolonged COVID-19 disease muscle wasting and its association with longer-term outcomes.
Funding: ICS New Investigator Award 2020
References
1. Apea VJ*, Wan YI* (equal contributors), Dhairyawan R, Puthucheary AZ, Pearse RM, Orkin CM, Prowle JR. Ethnicity and outcomes in patients hospitalised with COVID-19 infection in East London: an observational cohort study. BMJ Open 2021;11:e042140.
2. Wan YI, Apea VJ, Dhairyawan R, et al. Ethnic disparities in hospitalisation and hospital-outcomes during the second wave of COVID-19 infection in east London. medRxiv07.05.21260026.
3. Wan YI*, Bien Z* (equal contributors), Apea VJ, et al. Acute Kidney Injury in COVID-19: multicentre prospective analysis of registry data. Clin Kidney J 2021: sfab071.
4. Haines RW, Zolfaghari P, Wan Y, et al. Elevated urea-to-creatinine ratio provides a biochemical signature of muscle catabolism and persistent critical illness after major trauma. Intensive Care Med 2019; 45(12):1718-1731.
5. Genolini C, Alacoque X, Sentenac M, & Arnaud C. Kml and kml3d: R packages to cluster longitudinal data. Journal of Statistical Software. 2015;65(4); 1–34.
P087
Finding the Physiologic Switch to Predict Weaning from Mechanical Ventilation in ARDS
Data science
Jingyang Yu
Imperial College London
Abstract
Introduction: Weaning from mechanical ventilation is a necessary process towards liberation for ventilatory support for critically ill patients with respiratory failure and also to prevent ventilator-induced injury.4 However, the timing of its initiation and its impact on the duration of ventilation are unclear. We hypothesized that non-ventilatory parameters in addition to newer perspectives on ventilatory factors may improve prediction for successful weaning. In this study, we took into consideration several ventilatory parameters, standard laboratory blood biomarkers, and demographic parameters.
Objectives: The objectives of this study are two-fold: First, we established statistical models to predict the outcome of a weaning decision based on a real-time physiological situation of the patient. Second, we found significant parameters in the models and tried to use a clear interpretable algorithm to improve the clinical guidance.
Methods: We used an hourly synchronized method to align different medical events. To investigate their statistical relationship, we used imputation methods including the last observation carried forward for 24 hours, and mean value imputation. Next, we used three different machine learning models to investigate the relationships.
Results: For the first part of objectives, statistical models were able to strongly predict indicators for unsuccessful weaning from mechanical ventilation The logistic regression model, decision tree model and random forest model achieved negative predictive values of 81.22%, 79.69% and 80.82% respectively on imputed data set. Among these three models, the decision tree model and random forest model achieved satisfying outcomes on real non-imputed data set, as shown in Figure 1. As for the second part of the objectives, we identified the significant parameters which are: ventilatory parameters: Mean Airway pressure, ventilatory ratio, minute ventilation, Respiratory rate and PF ratio, blood test parameters: SpO2, PaCO2 and demographic parameter age. Based on these significant parameters, we constructed a decision tree showing physiological situations in numeric ranges where patients should not be liberated from mechanical ventilation Figure 2.
Figure 1.
▪▪▪
Figure 2.
▪▪▪
Conclusion: The outcomes of weaning/liberation from mechanical ventilation are related to the physiological condition when the patients start to be weaned. We have identified a set of parameters (ventilatory, demographic and blood based) that indicate a poorer chance of successful weaning, which should be considered. Moreover, significant parameters can be considered in creating the ventilatory protocols to prevent unsuccessful weaning results.1-3
References
1. Jackson CD. What are the parameters for assessing a patient's readiness to be weaned from mechanical ventilation? Available from: https://www.medscape.com/answers/304068-104791/what-are-the-parameters-for-assessing-a-patient39s-readiness-to-be-weaned-from-mechanical-ventilation
2. Lermitte J, Garfield MJ. Weaning from mechanical ventilation. Continuing Education in Anaesthesia Critical Care & Pain. Continuing Education in Anaesthesia Critical Care & Pain; 2005;5(4):113–117.
3. Boles J-M, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. European Respiratory Journal [Internet].
4. Dreyfuss D, Saumon G. Ventilator-induced Lung Injury. American Journal of Respiratory and Critical Care Medicine. American Journal of Respiratory and Critical Care Medicine; 1998;157(1):294–323.
P088
The use of ultrasound for the management of pleural effusions
Echo and ultrasound
Laura-Jane Erunlu, Richard Cowan and Jamie Hornsby
NHS Greater Glasgow and Clyde
Abstract
Introduction: A retrospective audit of our patients in 2017 showed that 31% of patients admitted to our ICU with pneumonia had evidence of pleural effusion on their X-Ray imaging. Of these patients, only 12.5% had the possible effusion assessed further with thoracic ultrasound. Within the population assessed, there were patients who had been treated in ICU for pneumonia, not had their possible effusion assessed beyond X-Ray imaging and had represented to hospital following ICU discharge with empyema.
Objectives: We created a guideline for the assessment and management of pleural effusions in ICU with focus on risk stratification and ultrasound assessment of the effusion to identify effusions that are high risk of being complex/exudative and that need further evaluation with pleural fluid sampling. We then aimed to re audit the assessment of effusions after the introduction of our pleural infection guidelines.
Methods: We reviewed all chest x-rays taken in the level 3 area of our ICU from Dec 2019 to Jul 2021. Images were reviewed and then the electronic patient records of patients with possible effusions were examined. Data were collected and analysed in Microsoft Excel.
Results: 974 X-Rays were reviewed. 329 (34%) of the X-Rays showed evidence of possible pleural effusion. 160 of these x-rays were in patients with a diagnosis of pneumonia. 75 (47%) of x-rays with evidence of effusion in a patient with pneumonia were further investigated with a pleural ultrasound. Following this assessment, 44% of effusions were considered appropriate for pleural fluid sampling. A majority (86%) of the sampled effusions were exudative and required further intervention or management.
Conclusion: The use of our pleural infections guideline increased the proportion of patients who had appropriate assessment of possible pleural effusions in ICU. The effusions that were identified by the guideline as being suitable for pleural fluid sampling were mostly exudative and required further intervention. Given this, in the future we plan to work on further embedding ultrasound assessment of possible pleural effusions in our ICU patients.
P089
Could Echo be closer to the Heart of Training? Point of care echocardiography training in Scotland: A survey of intensive care medicine trainees
Echo and ultrasound
Alistair Rocke and Rosaleen Baruah
David Hall NHS Lothian
Abstract
Introduction: Point of care echocardiography is quick, non-invasive and facilitates the acquisition of critical clinical information where and when it is most required. The provision of point of care ultrasound in critical care is a key recommendation of GPICS1 (Guidelines for the Provision of Intensive Care Services) and clinicians are increasingly performing echo examinations to inform decision making. Training and accreditation in the provision of focused echo examination is delivered as FUSIC (Focused Ultrasound in Intensive Care) Heart; previously as FICE (Focused Intensive Care Echocardiography). Despite increasing expectations of this trained resource, echo competencies do not form part of the intensive care medicine (ICM) training curriculum. Trainees have competing time pressures and variable access to resources enabling achievement of these skills.
Objectives: We aimed to gather national data on echo training experience and accreditation status amongst ICM trainees. We further sought to identify key demographics and perceived challenges that may act as barriers to accreditation to advise future decision making on the provision of training.
Methods: An online survey was sent to all ICM trainees in Scotland during the 2019/20 training year (pre-pandemic). Questions addressed areas of interest including trainee demographics, echocardiography accreditation status, perceived challenges to the accreditation process, availability of mentors and dedicated training time. The survey was designed and analysed using Google Forms.
Results: Of the 66 ICM trainees 34 replied giving a response rate of 52%. 13 (38%) respondents had achieved formal accreditation in echocardiography, 21 (62%) had not.
Accredited trainees
12 of the 13 accredited trainees had FICE and 46% achieved this before starting ICM training. None were allocated dedicated time in their rota to perform scans. Most (85%) came into the ICU on days off. Perceived challenges to accreditation included ‘time available to scan’ (85%), ‘access to mentors’ (46%) and the local ‘availability of FICE course’ (23%).
Unaccredited trainees
13 of the 21 unaccredited trainees (62%) were working towards accreditation. The majority (92%) had no dedicated time in their rota to perform scans. About half (54%) were coming into the ICU on days off. Perceived challenges to completing accreditation included ‘time available to scan’ (95%), ‘access to mentors’ (38%) and ‘funding a course’ (33%). 8 trainees did not have echo accreditation nor were they working towards one (24% of all respondents); of these 4 previously ‘timed out’. Exam pressures, regional availability of mentors and training block time constraints were listed as barriers to completion.
Demographics
Significant demographic disparities were identified as potential barriers to accreditation rates. Dual anaesthetic training (25%), being a female trainee (21%), and training LTFT (0%) were significant barriers to accreditation. Regional disparities existed however stage of training was unrelated.
Conclusion: Most ICM trainees in Scotland are not accredited in echocardiography despite the recognised importance in the provision of critical care services. This survey highlighted specific challenges to the trainee and demographic barriers dependant on region, training programme and gender.
References
1. The Faculty of Intensive Care Medicine. Guidelines for the Provision of Intensive Care Services (GPICS). (2019) Intensive Care Society. 2(4–7): 138-141.
P090
Bringing echocardiography into a district general intensive care unit: improving facilities, training opportunities and information governance
Echo and ultrasound
Angus Perks 1 , Michael Kalogirou2, Rabia Warraich2 and Eimear McKavanagh3
1Barking, Havering and Redbridge University Hospitals, London, United Kingdom
2Royal Free London NHS Foundation Trust, London, United Kingdom
3Guy’s and St Thomas’ NHS Foundation Trust, London, United Kingdom
Abstract
Introduction: Point of care ultrasound (POCUS) and particularly echocardiography has revolutionised the assessment and management of critically unwell patients. However, capabilities for performance of echocardiography, storage of images and scope for training vary significantly between hospitals.
This audit and quality improvement project aimed to assess the current utilisation of echocardiography and the POCUS facilities in Barnet Hospital ICU (North London), with a goal to improving facilities and training opportunities in accordance with ICS and FICM’s Guidelines for the Provision of Intensive Care Services (GPICS).1
Objectives:
1. To assess currently performed echocardiography on ICU: Scan indications, time between request and completion and whether focused studies would be a suitable 1st line alternative in some cases.
2. To audit Barnet ICU echocardiography capabilities and how these comply with the ICS and FICM Standards set out in GPICS1
3. To foster a relationship with the echocardiography department to rationalise use of cardiology services, improve capabilities, training and compliance with the above standards
Methods: A search was conducted through the Barnet Hospital ITUBase Patient Record for all echocardiograms requested between June 2019 and February 2020. This was verified with formal requests through the hospital-wide requesting system. Indication, time to performance and time to report were audited. Additionally, compliance with the Standards & Recommendations set out in GPICS1 regarding echocardiography capabilities of the ICU.
Results: 63 echos were requested, of which 48 were performed on ICU and five post discharge. Four patients died before echo could be performed. Mean time from request to performance was 66 hours. 46/48 echos were reported (95.8%), 39/46 (85%) within 24 hours, with a mean reporting time of 16 hours. Based on indication, is postulated that 70% of scan indications could have been addressed primarily with a focused ‘FUSIC Heart’ level scan.
Interventions implemented after discussion and collaboration with the local echocardiography department included:
• Opportunities for ICU trainees to attend weekly echo teaching meetings
• An appointed ICU echocardiography consultant lead
• Another ultrasound machine with ECG capability was obtained
• A reporting template was introduced to the ITUBase notes system, based on BSE Level 1 and FUSIC Heart reporting formats
• One ultrasound machine was linked to the hospital’s echo image storage and reporting system.
Storing focused echocardiograms on the hospital’s imaging archive allows for remote viewing of images, supervisor review and information governance compliance. The above resulted in an improvement in compliance from 3 FICM standards pre-intervention, to 6 standards and 2 recommendations post-intervention. Further plans include a link echocardiographer with dedicated time for teaching and scanning on ICU as well as connecting remaining ultrasound machines to image storage systems.
Conclusions: Our interventions lay the groundwork to further facilitate POCUS teaching and training, image review and information governance. Fostering a culture of POCUS use in ICU takes time and along with collaboration with cardiology departments, such interventions may expedite further training and acceptance, improve information governance and reduce burdens on echocardiography departments.
References
1. Peck M, Miller A, Fletcher N. Echocardiography and Ultrasound. In: Guidelines for The Provision Of Intensive Care Services [Internet]. 2nd ed. The Faculty of Intensive Care Medicine and Intensive Care Society; 2019. Available from: https://www.ficm.ac.uk/sites/default/files/gpics-v2.pdf
P091
Nurse-led PoCUS in the Management of the Critically Ill COVID-19 Patient
Echo and ultrasound
Eleanor Corcoran 1 and Louise Rose2
1King’s College Hospital
2King’s College London
Abstract
Introduction: Point-of-Care Ultrasound (PoCUS) can rapidly diagnose presence and severity of COVID-19 disease and associated pathologies.1 PoCUS identifies life-threatening complications at the bedside, with the potential to reduce the need for out-of-department transfers for imaging, alongside associated radiation exposure and spread of infection.2 Use of PoCUS by doctors in the intensive care unit (ICU) is becoming increasingly widespread. However, uptake by ICU nurses is poor despite evidence to suggest comparable accuracy in acquiring and reporting PoCUS scans, and the potential benefit to patients as a result of an increased workforce of competent PoCUS clinicians.3-5
Objective: To report findings in critically ill COVID-19 patients identified through nurse-led cardiac and 6-point lung PoCUS.
Method: This case series was part of the national service evaluation led by the Intensive Care Society, SAM, FUSIC, and FAMUS. Conduct was approved by the departmental lead for critical care ultrasound. An ICU nurse trained in Focused Intensive Care Echocardiography (FICE) and Focused Ultrasound in Intensive Care (FUSIC) performed cardiac and 6-point lung PoCUS scans on ICU patients with confirmed COVID-19 disease during the recovery phase. Severity of disease was scored between 0-3 (Table 1) in each lung region (upper anterior; mid-anterior; posterolateral) and a total score calculated (0-18). PoCUS scans were only performed on patients identified by the treating ICU consultant. Correlations between PoCUS findings and patient demographics, key clinical data, physiological parameters, and 30-day outcome were analysed using Pearson’s coefficient. Descriptive statistics analysis (mean; standard deviation/ mode; interquartile range) were used to describe data.
Table 1.
Lung PoCUS severity scoring system.
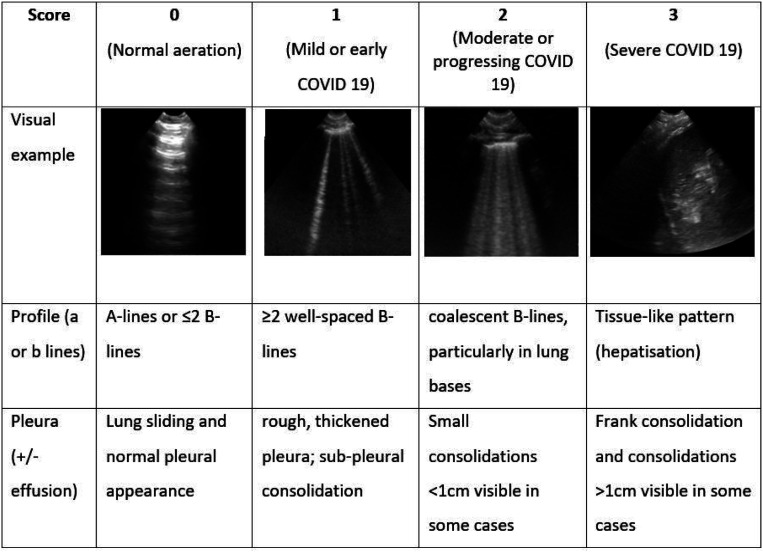
|
Results: A cardiac and 6-point lung PoCUS scan was performed on 15 patients. Fourteen (93%) scans were performed to answer lung-specific clinical questions including assessment of ventilation strategy (ventilation mode; PEEP level) in 5 (33%) patients, extravascular lung water assessment in 9 (60%), and lung assessment prior to tracheostomy decannulation in 1 (7%). Moderate to severe COVID-19 was apparent in all lung fields with severity scores from 6 to 14 (Figure 1). Left ventricular (LV) function was normal in 13 (87%) patients, 2 (13%) demonstrated signs of a dilated right ventricle (RV), and 1 (6%) had impaired LV and RV function (Figure 2). Ten scans identified pathologies that contributed to a change in clinical management immediately following the scan (Figure 3). Interventions included: (1) change in fluid management (increased fluid removal on renal filtration, new furosemide prescription) 4 (27%) patients) and a level 2 echo assessment due to identification of new cardiac pathologies (3 (20%) patients). Five patients had no change in care. We identified a moderate positive correlation between lung severity score and APACHE II (Pearson’s coefficient: 0.69; p value <0.01). Weak correlation was found between lung severity score and white cell count, SOFA score, and PaO2/FiO2. There was no difference in 30-day outcome in patients with a higher lung severity score or abnormal cardiac scan.
Figure 1.
Prevalence of lung severity scores according to lung region using 6-point lung PoCUS
Figure 2.
FICE scan findings
Figure 3.
Number and type of changes made to clinical management after the PoCUS scan
Conclusion: Cardiac and lung PoCUS is a vital tool in the assessment of COVID-19 disease. The addition of ICU nurses to the growing workforce of PoCUS competent clinicians increases availability of real-time imaging.
References
1. Karp J, Burke K, Daubaras SM, McDermott C. The role of PoCUS in the assessment of COVID-19 patients. J Ultrasound. 2021:1-9.
2. Mayo P, Arntfield R, Balik M, Kory P, Mathis G, Schmidt G, et al. The ICM research agenda on critical care ultrasonography. Intensive Care Medicine. 2017;43(9):1257-1269.
3. Mumoli N, Vitale J, Giorgi-Pierfranceschi M, Cresci A, Cei M, Basile V, et al. Accuracy of Nurse-Performed Lung Ultrasound in Patients With Acute Dyspnea: A Prospective Observational Study. Medicine (Baltimore). 2016;95(9):e2925.
4. Chen Z, Hong Y, Dai J, Xing L. Incorporation of point-of-care ultrasound into morning round is associated with improvement in clinical outcomes in critically ill patients with sepsis. J Clin Anesth. 2018;48:62-66.
5. Pontet J, Yic C, Díaz-Gómez JL, Rodriguez P, Sviridenko I, Méndez D, et al. Impact of an ultrasound-driven diagnostic protocol at early intensive-care stay: a randomized-controlled trial. The Ultrasound Journal. 2019;11(1):24.
P092
Focused Ultrasound in Critical Care Outreach for acutely ill and deteriorating patients on the wards
Echo and ultrasound
Brigitta Fazzini
Royal London Hospital, Barts Health NHS Trust
Abstract
Introduction: Focused Ultrasound in Intensive Care (FUSIC) refers to the use of ultrasound by a trained bedside clinician to guide patient management in real-time. Ultrasound is widely applied in practice and there is growing consensus that it is an essential tool for managing acutely ill patients in the intensive care unit (ICU). The Critical Care Outreach Team uses FUSIC as an additional assessment tool to guide management and decision-making plan for deteriorating patients on the wards.
Objectives: To investigate whether how often information gained from FUSIC imaging had an impact on patient care and management decisions in a critical care outreach setting.
Methods: A single-centre observational study at an academic tertiary referral institution. We included all patients reviewed by critical care outreach who were assessed by ultrasound during a 12-month period. Routine procedures for teaching purposes were not included.
Results: Forty-six patients were assessed and supported by a combined focused lung and heart ultrasound performed at the patient bedside on the wards. In 46 patients FUSIC was instrumental in the differential diagnostic workup and in guiding the clinical management. In 32 (70%) patients FUSIC aided fluid therapy or diuresis (in case of pulmonary oedema) and helped targeting fluid balance. In three patients though to have consolidation on chest x-ray we were able to identify significant pleural effusions without needing an additional CT scan. In four patients with hypotension, an additional CT-PA was warranted due to dilated right ventricle (RV) with abnormal septal motion and decreased left ventricle (LV) size ratio (i.e. sign of right heart strain) as highly suspicious of pulmonary embolus. In two young patients with Coronavirus disease 2019 (COVID-19), using FUSIC we identified severe LV dysfunction which was subsequentially diagnosed as myocarditis and Angiotensin-converting enzyme (ACE) inhibitors therapy was commenced within 24 hours. Further diagnosis included cardiac tamponade (n = 2) requiring pericardiocentesis and pneumothorax (n =1). In all cases, the use of ultrasound helped in promptly referring patients to the specialist team (i.e. respiratory or cardiology) and to the ICU consultant.
Conclusions: In our critical care outreach practice, FUSIC is considered an indispensable tool for safe and accurate management of acutely ill and deteriorating patients on the wards.
P093
To drain, or not to drain: diagnostic and therapeutic challenges associated with cardiac tamponade in Right heart sided heart failure and pulmonary hypertension
Echo and ultrasound
Faryal Zaman1, Joao Manuel Ramos 2 and Heira Lansangan3
1Kings College Hospital London - London
2Kings College Hospital London
3King’s College Hospital London
Abstract
Background: In clinical practice, cardiac tamponade is not an “all-or-none” phenomenon, but rather a continuum of hemodynamic impairment. Diagnosis depends on an overall assessment of clinical and echocardiographic findings, hemodynamic measurements, and other corresponding patient-level variables must be considered to make a diagnosis to initiate timely intervention.1
The identification of cardiac tamponade in the presence of severe pulmonary hypertension and right ventricular failure can be even more challenging, because the “classic” findings are often not observed. Our patient clearly had hemodynamic compromise (orthostatic collapses and then persistent hypotension from a large pericardial effusion but did not exhibit the common features of tamponade on ECHO. This can be explained by the pre-existing, markedly elevated right-sided pressures, which prevented typical findings of pulsus paradoxus, right atrial and ventricular diastolic collapse, and equalization of diastolic pressures.1
Case presentation: 44 Years old lady background of Interstitial lung disease, pulmonary artery hypertension, Right heart failure and anti-synthetase syndrome. Recently required Intensive care admission for COVID pneumonitis and was discharged on home oxygen. Now admitted to hospital after she boarded the flight without oxygen and became unwell. She was treated on lines of exacerbation of interstitial lung disease, Right heart failure and moderate pericardial effusion without signs of tamponade in ECHO and was given adequate diuresis and responded very well to it. Her oxygen requirement came down and she clinically improved. Few days after, she developed diarrhea and pre-renal Acute kidney injury while in ward and became borderline hypotensive which improved after her diuretic doses were reduced and then held. She then after few days started to develop orthostatic collapses with hypotension and then became persistently hypotensive. Her CT Pulmonary angiogram showed unchanged moderate circumferential pericardial effusion, and no Pulmonary embolism.
She was reviewed by Critical care outreach team and an urgent bedside Echocardiogram was performed to rule out features of tamponade which showed moderate pericardial effusion, severely dilated Right heart with massive Right ventricular pressures compressing her Left ventricle.
She was urgently reviewed by cardiology and was taken to Intensive care unit for invasive hemodynamic monitoring, where she was given inotropes and inhaled pulmonary artery vasodilators. The decision was taken to cautiously diurese and not to drain the pericardial effusion due to risk of developing further instability by increasing right ventricular expansion causing further collapse and pressure on Left ventricle.
Discussion and conclusion: Our case stresses on the importance of Bedside Echocardiogram in timely identifying the atypical features of cardiac tamponade and to understand the different hemodynamics and mechanism of obstructive shock in patients with pre-existing right sided heart failure.
After the establishing that patient was in obstructive cardiogenic shock with atypical findings of tamponade, the next most important step was to decide whether to drain the pericardial effusion or not.
In our literature search, we found that the drainage of a large pericardial effusion in patients with pulmonary hypertension has been accompanied by catastrophic, sudden hemodynamic collapse and it has been postulated that the presence of pericardial fluid limits right ventricular distension in response to pressure and volume overload. When the pericardial fluid is removed, rapid enlargement of the right ventricle causes: (1) reduced right ventricular systolic function due to muscle fiber distension; and (2) compression of the left ventricle, which leads to impaired diastolic filling and left ventricular outflow track obstruction.¹
References
1. Adams JR, Tonelli AR, Rokadia HK, Duggal A. Cardiac tamponade in severe pulmonary hypertension. A therapeutic challenge revisited. Ann Am Thorac Soc. 2015;12(3):455
P094
Developing Bespoke Simulation Training Using Time-Based Process Mapping to Improve Safety of Emergency Intubation in Critical Care
Education and simulation
Nicola Mortimer Ocean1, Daniel Griffiths 1,2 , C. Forsythe1, C. Tatham1 and Vimal Grover1
1The Royal Marsden NHS Foundation Trust
2St George’s Hospital Medical School, University of London
Abstract
Introduction: Emergency intubations (EI) in critical care units (CCU) are common, complex tasks requiring effective coordination of a multidisciplinary team. Problems can arise when inexperienced staff are unaware of necessary roles and are unfamiliar with the process.1
Responding to a Serious Incident, we designed this quality improvement project (QIP) aiming to improve patient safety during EI. Utilising a novel process mapping approach, we identify areas for optimisation and training. The resulting action cards aim to improve safety by raising awareness of the entire EI process, improving teamwork, and demonstrating an ‘ideal’ EI, which can later be applied to clinical events.
Objectives:
• Establish baseline EI experience, engage stakeholders
• Create time-based process map of EI procedure in our CCU
• Assign tasks to team members, optimise processes, and identify barriers to effectiveness
• Develop individual action cards for EI team members, as teaching tools
• Run trial simulations for training, feedback, and critical observation of action card engagement
• Optimise action cards
• Create bespoke action card based EI simulation package for routine simulation training in our CCU
Methods: We conducted initial qualitative surveys amongst key stakeholders to establish areas of concern. Incorporating these findings, we differentiated the CCU EI process into component parts.
Each component was time-mapped and areas for optimisation were identified. We allocated tasks to team members and developed individual action cards, to coordinate an EI team in series and in parallel. The cards focus on EI process without complicating clinical variables and incorporate Difficult Airways Society guidelines.2
We ran four in situ simulation sessions, testing action cards for ease of engagement and potential to improve patient safety. Each session was an opportunity for observation and feedback; an iterative process of action card and data collection improvement, using rapid plan-do-study-action (PDSA) cycles. The observed interactions of the team, immediate post-simulation discussion, and anonymous written feedback, from participants and critical observers, was analysed using a human factors framework.3
The final action cards walk each team member through an ideal EI and highlight their individual role within the process.
Results: Feedback demonstrated high satisfaction using action cards as a learning tool within simulation; 100% (n=19) had fun and would participate again in the future.
Most participants (90%, n=10) reported learning new skills and knowledge. Feedback also showed enthusiasm for applying the action card format to other emergency scenarios.
From observing the simulation sessions, we noticed two key challenges for EI: unfamiliarity with a team leader role and inexperience with some technical tasks.
In addition, having examined our EI process in detail we have identified areas which could be improved in future QIPs.
Conclusions: In this QIP we used a new approach to design bespoke simulation training for EI in our CCU.
Process efficiency was optimised by time mapping and task allocation. Action card engagement and effectiveness was honed through rapid simulation based PDSA. Development of action cards for simulation training of other clinical scenarios will allow further evaluation of our new approach.
References
1. Russotto V, Myatra SN, Laffey JG, et al. Intubation Practices and Adverse Peri-intubation Events in Critically Ill Patients From 29 Countries. JAMA. 2021;325(12):1164–1172. doi:10.1001/jama.2021.1727
2. Higgs, A., et al. Guidelines for the management of tracheal intubation in critically ill adults. British Journal of Anaesthesia, 2017;120(2): 323–352
3. Education for Scotland. Human Factors of Health and Social Care. {Internet} The Knowledge Network. 2006; cited July 2021. Available at: http://www.knowledge.scot.nhs.uk/hfe/systems-thinking/seips.aspx
P095
NW ICU Logbook - A spreadsheet-based, cloud-compatible, fully-editable logbok for all intensive care practitioners
Education and simulation
Mark Tan
Northwest deanery
Abstract
Introduction: Logbooks are now ubiquitous in medical practice, aiding in provision of evidence of competency for training progression and revalidation processes. The Faculty of Intensive Care Medicine (FICM) recommends all practitioners keep a logbook, but does not mandate a particular one. During COVID19, redeployment from other specialties into ICU has meant many training opportunities have been difficult to evidence.1,2 Logbooks provide an evidence base for documenting educational experiences, identifying opportunities and learning from good practice.3
Objectives: The NorthWest Intensive Care Unit Logbook (NW ICU Logbook) provides a digital, spread-sheet based, easy-to-use, mobile-compatible personal logbook for ICU practitioners of all grades. Originally created for personal use, it has been made available for free for all. We used analytical software to track its use and spread so as to better understand the desire for such logbooks.
Methods: Google Analytics were built into the logbook download website to track views and downloads. Data is collected anonymously and provides evidence of its appeal. Extrapolation of its spread suggests an increased focused on governance within global ICM. Prospective, real-time data is continuously collected regarding website traffic, number of downloads, geographical and device data. This provides a rich source of anonymised data to better understand the use of a product. Already, many businesses use such software, but this method is still relatively new within medicine.
Results: The logbook has been downloaded over 3000 times from over 30 countries. Although interest is heavily centred in the UK, hotspots of downloads have also occurred in India, Egypt and Middle East. This is likely due to existing links and partnerships between hospitals. The logbook has been responsive to change, and several versions have been created based on feedback from users. The global appeal suggests an increased focus on educational governance and therefore presents many opportunities for further data collection and understanding of educational capacity and quality. Furthermore, expansion of the dataset may enable better understanding of human resources for health, caseload and global critical care trends.
Conclusion: There continues to be an interest for an easy-to-use and fit-for-purpose logbook for ICU practitioners. This logbook may form a template for further development. For example, an app would allow anonymised big data to be collected which can provide an evidence-base for regional variation in educational opportunities and achievements. Also, the global interest already shown may allow anonymised data which can add to evidence regarding human resources for health in low resource settings, further contributing to the understanding and advancing larger global health agendas within acute and emergency care.4 This provides a powerful opportunity for organisations to collect data for further research.
References
1. Munro C, Burke J, Allum W, Mortensen N. Covid-19 leaves surgical training in crisis. BMJ. 2021;372:n659.
2. Payne A, Rahman R, Bullingham R, Vamadeva S, Alfa-Wali M. Redeployment of Surgical Trainees to Intensive Care During the COVID-19 Pandemic: Evaluation of the Impact on Training and Wellbeing. J Surg Educ. 2020.
3. Schuttpelz-Brauns K, Narciss E, Schneyinck C, Bohme K, Brustle P, Mau-Holzmann U, et al. Twelve tips for successfully implementing logbooks in clinical training. Med Teach. 2016;38(6):564-569.
4. Diaz JV, Riviello ED, Papali A, Adhikari NKJ, Ferreira JC. Global Critical Care: Moving Forward in Resource-Limited Settings. Ann Glob Health. 2019;85(1).
P096
Manchester’s early critical care nurses - a history - educating our today and tomorrow by learning from our past
Education and simulation
Sharon Whiting 1 , Jane Brooks2 and Elizabeth Toon2
1Critical Care, NMGH, Manchester University Hospitals Foundation Trust
2University of Manchester
Abstract
Introduction: “ Acquire new knowledge whilst thinking over the old, and you may bec ome a teacher of others” 1
Critical care nursing in the 21st Century is at a crossroads. COVID-19 has demonstrated more than ever the central importance of well-educated critical care nurses to the delivery of high quality and safe care. The world has woken up to the fact that neither beds nor ventilators an intensive care unit make. There is much to learn from the past two years that will inform our future. But I believe there is another history - an earlier one that has not yet been told. This is equally important to our learning and identity as nurses. But is in danger of being lost.
The contemporary history of intensive care medicine in Britain describes how innovations and advancements in medicine, surgical techniques, pharmacology, engineering, and science have - since the 1950s - interconnected to create today’s 21st Century critical service.2
We read of the medical greats, the barriers they overcame to become the ‘firsts’ in application of techniques that are commonplace and readily accepted canons in treating the critically ill in our care.
The history occasionally alludes to the nursing role or misses it completely. There is no doubt nursing was fundamental to the proliferation of intensive care in Britain from the 1960s. Yet, this is largely missing from the historical record or written from the medical perspective. A nurse contributor to the Wellcome Witnesses Seminar reflecting on the nursing contribution wrote:
‘ If you did a nursing/ICU seminar you ’ d get another perspective and more nurses attending ’ 2
This is the basis for this research. The finding of nurses lost voices. Captured critical care nurses’ stories will, through a process of narrative analysis, be critically evaluated and shared. Not simply as interesting anecdotes - but as a basis for enhancing professional identity and belonging - to learn from, inspire, and inform the future.
‘ Thinking historically does not just mean thinking about the past; it involves seeing oneself in time, as an inheritor of the legacies of the past and as a maker of the future ’ 3
Objectives: Research aim - to explore this history form the perspective of retired nurses and one ICU at North Manchester General Hospital working between 1967 & 2000.
To share with conference emerging findings. To stimulate a conversation about this hidden history and the possibilities it offers future professional learning.
Methods: Oral history and narrative analysis.
Oral history is described as a research methodology that collects histories of neglected ordinary people that would otherwise be lost.4 And deemed crucial to the capturing of nursing work.5
Results: Ongoing archival work - 13 interviews recorded (2 male nurses/1 consultant). Thematic analysis. Emerging themes: unique professional relationships built as hierarchies flattened. Shared education. Increased autonomy. Separate. Special. Pushed boundaries.
Conclusion: Incomplete, yet this work and sharing stories from the foundations of critical care nursing has the power to motivate and inspire the professional critical care nurse of 2021 – more than education - history, legacy, pride.
References
1. Kan Q. 12 famous Confucius quotes on education and learning. Open Learning. https://www.open,edu/openlearn/education/12-famous-confucius-quotes-on-education-and-learning (2019, accessed 12 August 2021).
2. Reynolds LA and Tansey EM. (Eds) History of British intensive care, c.1950-c.2000. Wellcome Witnesses to Twentieth Century Medicine. 42. 2011. London: Queen Mary, University of London.
3. Seixas P. Conceptualizing the Growth of Historical Understanding. In: Olson D R and Torrancehe N (eds) Handbook of Education and Human Development: New Models of Learning, Teaching, and Schooling. Cambridge MA: Blackwell, 1996.
4. Thompson P. The voice of the past. 3rd ed. Oxford: Oxford University Press. 2000.
5. Beddoe D. Discovering Women’s History. A practical guide to researching the lives of women since 1800. 3rd ed. Harlow Essex: Addison Wesley Longman Ltd. 1998.
P097
Improving the ICU Medical Student placement: An ‘A to E and beyond’ workbook
Education and simulation
Harry Bateman 1 and Georgina Harridge2
1University College London Hospital
2Whittington Hospital
Abstract
Introduction: The North London ICU had never previously hosted a formal Medical Student placement. ICU can be a daunting environment for students with many unwell patients and complex associated presentations, investigations and management steps. Junior Doctors are often busy, which can unfortunately sometimes limit teaching opportunities. We observed that these factors may be negatively impacting the educational experience of the placement. We believed an educational workbook to accompany the placement could provide structure and fill spare student time with valuable learning and discussion topics.
Objective: To improve the overall educational experience for Fourth Year Medical Students undertaking a placement in a North London ICU department.
Methods: Questionnaires were sent to 17 students who had ICU placements prior to January 2021. We requested for general feedback on the placement plus opinion on educational experience and potential value of an ICU workbook. An ICU placement workbook was then produced to accompany the ICU Medical Student placement post January 2021. The workbook was paperless- we produced it on GoogleDocs and emailed it to students in advance of their placement so that they could access it via personal iPads issued by the Medical School. The workbook covered topics related to an ‘A to E and beyond’ approach to assessment of critically unwell ICU patients. The focus was on investigations, interventions and management steps relevant to both ICU and the medical school curriculum and included encouragement of MDT interaction and independent review of patients. Questionnaires were then sent to 25 students who had their ICU placement with the addition of the workbook- we again requested general feedback plus opinion on educational experience and value of the workbook.
Results: 7/17 Students who had their placement pre-workbook introduction responded to the questionnaire compared to 11/25 Students who had placements post-workbook introduction. Prior to introduction of the workbook, 42% of respondents rated the educational experience of their ICU placement as ‘Good’ or ‘Excellent’- this figure increased to 82% following workbook introduction (Figure 1). Pre-workbook introduction, 100% of respondents agreed that the ICU workbook would be a valuable placement addition. This result was mirrored in the feedback by students who had their placement with the addition of the ICU workbook- 100% of respondents agreed it was a valuable addition to the placement. Our project was also able to obtain general feedback comments, which generated ideas for future ways to improve the placement, such as inclusion of an introductory session to ICU basics and attachment of students to specific doctors.
Figure 1.
How would you describe your overall educational experience of your placement on ICU?
Conclusions: Our project was able to both address and generate ways to improve the ICU placement. Although we were limited by a poor response rate, the responses we did receive suggest that the student perception of the educational experience of the ICU placement improved after introduction of the workbook. Respondents unanimously considered the workbook to be a valuable resource. Future steps include encouraging other specialties at the Hospital to undertake similar educational initiatives and hopefully promoting the workbook for use in other ICU departments nationally.
P099
Video demonstration of aseptic blood culture taking from invasive lines at induction and its effects on rates of contamination and false positives
Education and simulation
Alastair Shaw, Paul Candler, Gurmukh Sandhu and David Sperry
Nottingham University Hospitals NHS Trust
Abstract
Introduction: Blood cultures are commonly taken in critical care. They are taken when a patient presents with infective symptoms, or any deterioration where sepsis or an underlying infection must be considered as the cause. Cultures are an essential part of diagnostic work ups as recommended by international guidelines.1 Taking cultures allows causative pathogens to be isolated and antimicrobial treatment rationalised, as recommended by The National Institute for Health Care Excellence for antimicrobial stewardship.2 However, if there is poor technique there is risk of contamination of the blood culture which may lead to diagnostic confusion and delay.
Anecdotally there has been a number of different methods described by clinical staff on how they take cultures in Nottingham University Hospitals Critical Care (NUHCC). The aim of this QI project was to standardise practice amongst new starters in order to reduce contamination rates.
Objectives:
• To increase awareness of correct blood culture technique
• To standardise how new starters learn to take blood cultures on NUHCC
• To reduce the incidence of contamination of blood cultures
Methods: A mixture of qualitative and quantitative methods were used to measure whether the video achieved its objectives. Initially trainees who had not had standardised instruction, answered a short questionnaire on whether they were aware of the procedure of taking blood cultures and if so, how. This was repeated with a new cohort of trainees two weeks after induction after watching an instructional video created with departmental guidance using evidence based educational design.
To quantitatively and objectively assess the implementation of the instructional video, rates of blood culture contamination were assessed. This involved looking at the rate of contamination in August 2020 after induction compared to the rate in August 2021 after the most recent induction.
Results: After including the video in the induction awareness of a standardised procedure for taking blood cultures had increased from 38.5% to 75%.
In both pre- and post-intervention cohorts only 1 trainee in each did not know the standardised procedure. However, in the post-intervention group a higher proportion learnt this from watching the video compared to other methods (being told by colleagues and watching colleagues).
[Contamination rates awaited from the end of the month]
Conclusions: Creating video instruction of the correct procedure has increased the awareness of how to take blood cultures on NUHCC and also made the source of information more reliable. The initial survey indicated previous cohorts had relied on being shown by colleagues or watching them which created much variation in technique.
[Await results of how that has translated into contamination rates]
By using the medium of video trainees can easily look back and refresh their memory if there are any parts of the process that they have forget how to perform. This same video can now be shown to multiple cohorts without variation which may occur with live demonstration. Further videos are planned for arterial line insertion and central line insertion.
References
1. de Backer D, Dorman T. Surviving sepsis guidelines: A continuous move toward better care of patients with sepsis. JAMA - Journal of the American Medical Association [Internet]. 2017;317(8):807–808. Available from: https://jamanetwork.com/journals/jama/fullarticle/2598893
2. NICE. Antimicrobial stewardship: systems and processes for effective antimicrobial medicine use NICE guideline [Internet]. London: NICE; 2015 [cited 2021 Apr 7]. Available from: www.nice.org.uk/guidance/ng15
P100
Developing ‘Trachy Team’: a virtual, gamified, Critical Care tracheostomy MDT ward round: Innovative, future-proof education for an important team skill
Education and simulation
Rebecca Dooley
Brendan McGrath Manchester Foundation Trust
Abstract
Introduction: Critically ill patients requiring a tracheostomy are exposed to the risks of prolonged invasive support and altered airways. Liberation is a multi-specialty process requiring adept collaboration and consistency to optimise rehabilitation, prevent and identify complications. Multidisciplinary team (MDT) tracheostomy ward rounds have been shown to improve quality and safety of care.1–4 The number of UK Intensive Care Units (ICUs) with such teams has not been surveyed. We believe they are uncommon, despite evidence of benefit. Education is a key contributor to improving standards of care. Yet training in collaborative, complex decision-making around tracheostomy care is often left to ad hoc workplace exposure of unreliable educational quality.
Objectives: To design, create and deliver a widely available, flexibly accessed, impactful educational experience suited to all members of the tracheostomy MDT. The experience should enhance the learner’s understanding of each MDT member’s role and value in challenging decision-making around tracheostomy care. The educational tool should represent the latest in tracheostomy care research, guidelines and be patient-focussed.
Methods: Brainstorming of concepts and draft web designs were produced. An educational grant from the National Tracheostomy Safety Project (NTSP) was attained to fund web development and a web development team commissioned. Collaborative working has culminated in our product: ‘Trachy Team’ - a virtual (online) MDT ward round-based educational game. Construction is underway and the game will launch live in October 2021, at the 6th International Tracheostomy Symposium (ITS).
To maximise learner engagement and enjoyment, we have incorporated gamification techniques: points scoring; leader boards; time-limit on game play; strategy and prizes. Medium fidelity is achieved using video footage of real MDT members within the ICU environment and the ability of the player to request further, realistic clinical information.
Traditional pedagogical theories have been considered and techniques incorporated to ensure a variety of learners, and the subject matter are attended to. Honey and Mumford’s ‘activists’ may enjoy the new platform, ‘reflectors’ can benefit from in-game micro-feedback, ‘theorists’ can incorporate new knowledge into their game play and ‘pragmatists’ might benefit from decision-making in the safety of a virtual environment. VARK (Visual, Auditory, Reading and Kinaesthetic) learning styles are addressed with mixed-format media, interactivity and the ability to play live within a team at ITS. More detailed feedback videos will be viewed after the game, ensuring educational value for learners who prefer not to gamify intensely. For those with prior clinical experience, the game will provide space for reflection and the ‘active experimentation’ of Kolb’s Learning Cycle. ‘Demonstrating’ decision-making skills through practice in-game encourages progression through Miller’s Pyramid, paving the way for ascension to the ‘does’: implementing new knowledge in clinical practice. Further, we aim to teach through positive role modelling and provide a library of resources for players to return to.
Results and Conclusion: Kirkpatrick’s model will be used to evaluate effectiveness, with immediate and follow up feedback sought. Results will be used to improve and expand the game, which will then be housed permanently on the NTSP website for learners all over the world to access.
References
1. Claffey HC, Donnelly G, Charles R, Gorman S. Creating an integrated tracheostomy care pathway for patients in an Irish regional hospital setting - the feasibility and effectiveness of a dedicated tracheostomy team. International Journal of Integrated Care 2017; 17:1-2
2. Hopkins BS, Brenner MJ, Raynor TP, Pandian V. How data-driven multidisciplinary tracheostomy teams transform care, prevent harm, and save lives. Otolaryngology - Head and Neck Surgery. 2020; 163(1)
3. Iqbal S, Fong N, Leblanc J, Fata P, Razek T, Khwaja K. Impact of a specialized multidisciplinary tracheostomy team on tracheostomy care in critically ill patients. Canadian Journal of Surgery. 2011; 54(3):167-172
4. Doherty C, Higson M, English C, Marks J, Howarth R, Consterdine K, Bateman N, Beggs R, McGrath B. Improving the quality and safety of paediatric tracheostomy care: Implementation of a weekly multidisciplinary ward round. Anaesthesia and Intensive Care. 2020; 48(2):45
P101
Using multi-disciplinary in-situ simulation to improve management of airway emergencies on an intensive care unit
Education and simulation
Rhys Gravell, Laura-Anne Dymore-Brown
Northwick Park Hospital, London North West University Healthcare trust
Abstract
Introduction: Airway emergencies in the Intensive Care Unit (ICU) are strongly associated with life-threatening sequelae.1 Managing these emergencies can be challenging and stressful and draws upon technical and non-technical skills to ensure effective teamwork and positive patient outcomes. The Fourth National Audit Project (NAP4) for the Royal College of Anaesthetist (RCoA) and Difficult Airway Society (DAS) demonstrated airway emergencies on ICU are associated with increased morbidity and mortality and have been attributed to a lack of education and training.2 Simulation can be used to teach airway emergencies, and they are considered valuable training exercises.3
Objectives: The objectives of this project were to explore the utility of multi-disciplinary in-situ simulation in the management of airway emergencies within the ICU.
Methods: Our quality improvement project was initiated by sending a survey to 52 ICU staff to identify any areas for improvement in managing airway emergencies. Over half of all participants did not feel confident in managing displaced tracheostomy (52%), with only a quarter feeling confident in managing self-extubation (25%). Whilst almost all responders were able to locate the emergency airway trolley, only 62% were able to locate a video laryngoscope or bronchoscopy kit in an emergency. Furthermore, the majority (81%) did not have prior experience of in-situ simulation, but of those that did, 65% found simulation to be very useful.
With the findings from NAP4 in mind, we implemented three changes to try and improve education and training for doctors and nurses working on the ICU. These included improvement of induction for ICU senior house officers, including identification of airway equipment used on ICU and an in-situ session on managing a desaturating patient. The second intervention was running a weekly in-situ simulation programme for all doctors and nurses working on ICU on how to manage displaced tracheostomies. The third intervention was the creation of ‘airway zones’ on the ICU, expanding on the airway trolley that was previously recommended by DAS. The airway zones were dedicated areas on the unit which were labelled and accessible, and included the difficult airway trolley, video laryngoscope and bronchoscope.
Results: On surveying participants’ perceptions following intervention, all participants found the in-situ simulation sessions to be useful, with 92% feeling confident or very confident in managing airway emergencies. Participants were also better able to locate emergency airway equipment.
Conclusion: These findings show an improvement in education and training for managing airway emergencies on an ICU and demonstrate the utility of in-situ simulation as an educational tool on the ICU.
References
1. De Jong, A., et al. 2013. Early identification of patients at risk for difficult intubation in the intensive care unit: development and validation of the MACOCHA score in a multicenter cohort study. Am J Respir Crit Care Med, 187(8), pp. 832-839.
2. Cook, T., Woodall, N. & Frerk, C., 2016. A national survey of the impact of NAP4 on airway management practice in United Kingdom hospitals: closing the safety gap in anaesthesia, intensive care and the emergency department. Br J Anaesth, 117(2), pp. 182-190.
3. Komasawa, N. & Berg, B., 2017. Simulation-based Airway Management Training for Anesthesiologists – A Brief Review of its Essential Role in Skills Training for Clinical Competency. J Educ Perioper Med, 19(4), p. E612.
P102
Ultrasound-guided subclavian venous access: Barriers to skill retention and development following a regional course
Education and simulation
Benjamin Millette 1 , Chris Acott2, Duncan Fraser1, Tim Wait3 and Nicolas Suarez4
1Buckinghamshire Healthcare NHS Trust
2Oxford University Hospitals NHS Foundation Trust
3Birmingham Children’s Hospital
4Oxford University Hospitals
Abstract
Introduction: Subclavian central venous access (SCVA) is an essential skill for practitioners in acute care specialities such as intensive care medicine, emergency medicine and anaesthesia. It has advantages over the femoral and internal jugular sites, including lower rates of infective and thrombotic complications1 and patient comfort. Mechanical complications of SCVA can be mitigated significantly by the use of ultrasound guidance.2 SCVA has become a dying art in the last 20 years in the UK with many trainees in acute care reporting little or no opportunity to learn and develop this skill.
Objectives: We designed and implemented a regional teaching course to promulgate skills in ultrasound-guided (USG) SCVA with a view to minimising the overall rate of central line associated complications. We then followed up participants to assess self-reported skill retention and perceived barriers to development.
Methods: Teaching sessions comprised a lecture followed by in vivo scanning, needling a subclavian phantom and practising sequential needle tip tracking on a separate phantom. We gathered data on participant grade, specialty, previous teaching in SCVA and number of times they had undertaken SCVA. We compared their confidence in performing USG SCVA before and after the training session using a visual analogue scale (VAS) ranging from 0 to 100. We also followed up course participants who had been taught at least 12 months previously to assess number of lines subsequently performed, repeat confidence assessment by VAS and to collect qualitative data on barriers to further skill development. VAS data were compared using the Mann-Whitney U test.
Results: Ninety-four physicians were taught over 9 teaching sessions. 84% had received no previous instruction in USG SCVA. 66% had previously inserted no subclavian lines under ultrasound guidance and 95% had inserted five or fewer. Median confidence in USG SCVA prior to teaching was 9 on the VAS. After this session this rose to 57 (P<0.001 by Mann-Whitney U test). 25 course candidates were invited to complete the follow up survey at a median of 23 months following the course and 13 responded (52%). 11/13 had inserted five or fewer lines since attending the course. Median confidence in USG SCVA was 50 on the VAS and had significantly decreased compared to the post course values (p=.022 by Mann-Whitney U test). Barriers to skill retention and development identified by candidates included lack of senior physicians able to supervise the skill, lack of opportunity to undertake SCVA
Conclusions: We have demonstrated that a short course in USG SCVA is able to increase confidence in performing the procedure in a mixed cohort of candidates of differing specialities and experience levels. However, there is deterioration in this confidence following the course and few candidates seem to have been able to incorporate this skill into their routine practice. Lack of appropriate training opportunities and lack of physicians able to supervise USG SCVA have been identified as the main barriers. Further efforts to focus on “training the trainers” for this skill will be needed to promote skill retention and development in the future.
References
1. Parienti J-J, Mongardon N, Mégarbane B, et al. Intravascular Complications of Central Venous Catheterization by Insertion Site. NEJM. 2015;373(13):1220–1229.
2. Shin HJ, Na HS, Koh WU, et al. Complications in internal jugular vs subclavian ultrasoundguided central venous catheterization: a comparative randomised trial. Intensive Care Med. 2019;45(7):968-976
P103
#ACCPANdev: Identifying the continuing professional development (CPD) needs of Advanced Practitioners (APs) within the UK – a national evaluation
Education and simulation
Sadie Diamond Fox 1 and Sonya Stone2
1Newcastle upon Tyne Hospitals & Northumbria University
2Nottingham University Hospitals & Nottingham University
Abstract
Introduction: The NHS Long-Term Plan1 acknowledges that Advanced Clinical Practitioners (ACPs), which includes the Advanced Critical Care Practitioner (ACCP) role, are central to transforming service delivery to meet dynamic local healthcare needs, and as such there has been a large investment in the training and development of said roles. Recent literature has highlighted that a lack of CPD opportunities and unclear career pathways exist for advanced practitioners.2-4 In light of this, a new academic network is in development – Advanced Critical/Clinical Care Practitioners Academic Network (ACCPAN). The aim is to promote collaborative working in a safe and supportive environment and to ensure high quality education, mentorship, networking and research opportunities. To our knowledge, there is no data that currently exists to evaluate the national perspectives of the CPD needs of advanced practitioners.
Objectives: The study has multiple objectives:
1. Complete thematic review of the relevant literature
2. Determine the perceived CPD needs of ACPs and ACCPs utilising a validated tool (Hennessy-Hicks Training Needs Analysis (HHTNA) manual and questionnaire5)
3. Utilise the above data to prioritise the training needs and aid in the creation of a rolling annual timetable of CPD events co-ordinated by ACCPAN to address said training needs.
Methods: A three-stage, mixed-methods design has been utilised.
• Stage 1 – Exploratory consultation and validation of an adaptation of the HHTNA questionnaire5 with consenting, practising ACP and ACCPs via an online platform (Microsoft Teams and Zeetings). Advertisement of the event was via various social media platforms, utilising the hashtag “#ACCPANdev”.
• Stage 2 - A national service evaluation utilising a cross-sectional, mixed-methods, (single) survey-based design within which the adapted HHTNA questionnaire5 is embedded. This stage of the study is due to commence September 2021.
• Stage 3 – The development and evaluation of various CPD activities aimed at ACPs and ACCPs.
Results: We report here the findings of stage 1 of the study.
A total of 31 eligible participants, from a range of clinical backgrounds (critical and acute care, paediatrics, mental health, and general practice), took part in 1 of 4 semi-structured consultation meetings in May 2021.
An anonymised, interactive questionnaire was completed by participants during the meeting which generated a variety of quantitative and qualitative data, some of which is summarised in Figures 1 and 2. Participants were then presented with the proposed adaptation of the HHTNA questionnaire5 and encouraged to consult on its content. Suggestions for further adaptations were then collated and arranged into themes which reflect the four pillars of advanced practice (clinical; education; leadership and management; research).
Figure 1.
Are CPD and Training needs of APS (Post-qualifying) Currently being Met?
Figure 2.
Perceived CPD needs of APSS.
Conclusions: Stage 1 of our study reflects the findings of national data that the CPD needs of ACP and ACCPs are not being met across all four pillars of advanced practice roles. Thematic analysis of the available literature, together with data obtained from stage 1 of the study has ensured construct validity to our proposed adaptation of the HHTNA questionnaire5 for stage 2 of the study. This study is the first of its kind to address the important subject of ongoing education and development of advanced practitioners.
References
1. NHS. The NHS long term plan. 2019. https://www.longtermplan.nhs.uk/
2. Evans C, Poku B, Pearce R, et al. Characterising the evidence base for advanced clinical practice in the UK: a scoping review protocol. BMJ Open 2020;10: e036192. doi: 10.1136/bmjopen-2019-036192
3. Evans C, Poku B, Pearce R, et al. Characterising the outcomes, impacts and implementation challenges of advanced clinical practice roles in the UK: a scoping review. BMJ Open 2021;11: e048171. doi:10.1136/bmjopen-2020-048171
4. Diamond-Fox S, Waeland D, Boulanger C, et al. A national evaluation of the advanced critical care practitioner role within the United Kingdom. ESICM Lives 2020. Conference proceedings. Intensive Care Medicine Experimental 2020;8(2):000595
5. Hicks, C & Hennessy, D (2011) Hennessy-Hicks Training Needs Analysis (HHTNA) manual and questionnaire. The Global Health Workforce Alliance, World Health Organisation. Online https://www.who.int/workforcealliance/knowledge/toolkit/19/en/
P104
A survey of UK critical care pharmacists research involvement and associated barriers
Education and simulation
Xolani Dereck Gondongwe 1 , Ruth Wan2, Greg Barton3, Cathrine McKenzie4 and Mark Borthwick5
1University College London Hospitals
2Guys and St Thomas’ NHS Foundation Trust
3St Helens and Knowsley Teaching Hospitals NHS Trust
4Kings College London HNS Foundation Trust
5Oxford University Hospitals NHS Foundation Trust
Abstract
Introduction: Pharmacist led research provides evidence of impact of safe, effective and economic advanced pharmaceutical care in critical care medicine. Examples include impact of extracorporeal therapies on drug handling1; sedation delirium management2; medication safety3 and broader pharmacist interventions.4 The New Zealand Hospital Pharmacist Association (NZPHA), Society of Pharmacists of Australia (SHPA) and Royal Pharmaceutical Society (RPS) all identify research as an essential domain for critical care pharmacist (CCP) accreditation. In addition, the UK Critical Care Research Group includes a pharmacist representative. Despite these recommendations, the experience and access to research of CCP in the UK remains unknown. This study sought to describe the research experience of UK CCP along with perceived or actual barriers to CCP engagement with research.
Aim: To capture barriers, facilitators and research experience of the UK CCP
Methods: An electronic survey (Survey Monkey ®.) was designed,5 piloted and revised by investigators. It was distributed to subscribers to the UK Clinical Pharmacy Association Critical Care, pharmacist message board.
Participants provided:
1. Demographic data
2. Their research activity and output in 2 years preceding the survey;
3. Statements of perceived barriers
4. Indicated research roles/ activities they would like to participate in. The study did not require ethical approval. Quantitative data were collected and analysed using Microsoft Excel ®.
Results: Between 30 January and 13 March 2020 we received a 24.0% response rate (n= 61/254), most respondents were located in England (n = 51, 83.6%), they all had more than 5 years critical care experience. All respondents possessed a post graduate qualification with 42.6% (n=26) having at least one post graduate research degree. Fifty respondents (81.9%) indicated involvement in research as chief (n=3) or principal investigator (n=10); pharmacy researcher (either local /regional) service evaluation/ clinical audit /Quality Improvement Project (n=16) or in multicentre studies (n=4). The remaining (n=11, 18.0%) respondents reported no involvement in research activities. Most respondents had no allocated time for research in their current role (n=54, 88.5%). Lack of protected time was identified as the most common barrier to research activity (n=50). Fifteen CCP reported 42 publications in peer reviewed journals and conference abstracts.
Discussion: As far as we are aware this is the first report on UK CCP research activity. An encouraging number reported a research qualification and involvement, (including) leading research activities despite reporting not having allocated time for research activities. Low response rates to this survey limits generalisability of the findings and as such further studies are warranted. Future work should focus on both engaging junior pharmacists and establishing research output metrics including peer reviewed publication and funding awards.
References
1. Abdul-Aziz MH, Roberts JA. Antibiotic dosing during extracorporeal membrane oxygenation: does the system matter? Current Opinion in Anaesthesiology;33(1):71–82.
2. Devlin JW, Pandharipande PP. Do Our Sedation Practices Contribute to Increased Mortality in Coronavirus Disease 2019–Related Acute Respiratory Distress Syndrome? Critical Care Medicine;49(9):1579–1582.
3. Shah N, Jani Y. Implementation of Smart Infusion Pumps: A Scoping Review and Case Study Discussion of the Evidence of the Role of the Pharmacist. Pharmacy;8(4):239.
4. Rudall N, McKenzie C, Landa J, Bourne RS, Bates I, Shulman R. PROTECTED-UK – Clinical pharmacist interventions in the UK critical care unit: exploration of relationship between intervention, service characteristics and experience level. International Journal of Pharmacy Practice 2017:25(4):311–319.
5. Connolly B, Allum L, Shaw M, Pattison N, Dark P. Characterising the research profile of the critical care physiotherapy workforce and engagement with critical care research: a UK national survey. BMJ Open 2018;8(6):e020350.
P106
Lancashire & South Cumbria Critical Care Network Follow Up Clinic Evaluation Project
Follow up clinic
Nicky Williams 1 and Emma Jackson2
1Blackpool Teaching Hospitals
2Manchester University NHS Foundation Trust
Abstract
Introduction: Admission and survival from critical care is not without its far-reaching consequences to both the patient and their families. Follow-up clinic for critical care patients is something that has been established to try to ‘mop up’ some of these consequences. However, resource allocation to this vital line for many patients is patchy and often inadequate. Within the LSCCC Network there are Four Trusts with critical care follow up services. Three sites agreed to participate in the project to evaluate the issues patients report at clinics and the provision of services for ongoing support for these patients.
Objectives: To evaluate the physical, functional, psychological and cognitive issues patient identify at follow up clinic reviews and the service provision for ongoing support for these patients.
Methods: From the period of July 2020 - July 2021 we collected data on patients attending follow up clinics at three sites. We collected basic demographic data, level of care, type of ventilatory support, length of ventilation, length of critical care and hospital stay and COVID-19 status. We used the EQ-5D Health Related Quality of Life score (HRQoL) questionnaire, Health Score and Trauma Screening Questionnaire to assess how respondents rated their own health. We identified physical/functional and psychological issues patients reported at the clinic appointments. We identified onward referrals to other specialities and if these services were available. We identified if patients had returned to work after their admission to critical care and whether patients would benefit from further Follow Up appointments.
Results: We collected data on 249 patients. 58% of these were male and 42% of these patients were admitted due to COVID-19. The median age of our patients was 59 (16-86), with 53% of patients requiring Level 3 care. The median length of invasive ventilation was nine days (0-88 days), non-invasive ventilation was 2 days (0-16 days) and median total ventilation was 11 days (0-100 days). The median length of Critical Care stay was 15 days (3-108 days), and the median hospital length of stay was 28 days (4-280 days). The HRQoL data identified issues in all the dimensions of quality of life and highlighted the problems patients face in their recovery from critical illness. The health score also identified that most patients felt their illness has impacted on the overall health status with some patients reporting significant reductions. The most common physical issues reported were fatigue and muscle weakness, however there was a range of physical issues identified showing the complexity of issues patients have during their recovery. The psychological issues highlighted high levels of anxiety in patients and sleep disturbance, as well as delusional memories and cognitive issues. The Trauma Screening questionnaire also identified self-reported psychological issues with the median score 3 but some patients reporting scores of 10 indicating severe psychological distress. The data identified patients requiring a high number of onward referrals to Medical and Allied Health Professional services to support their recovery. This is due to their being limited clinicians present in the Follow Up Clinics at the different sites. Most clinics had services available for onward referral except Psychology which was only available in one site. In the patients who were working prior to the period of hospitalisation only a limited number had been able to return to work by the time of the clinic appointment. Nearly a quarter of patients were identified as potentially benefitting from further appointments.
Conclusion: We identified that patients in the LSSCC Network who are admitted to Critical care, have significant impairments following a stay in critical care. They often require referral to further specialty services which are not always available within the follow up clinic that they attend. However, what is clear from our data is that our patients they need access to a range of Health and Social Care Professionals when they attend Follow Up Clinics and ability to access further ongoing health and support services.
P107
The Role of Physiotherapy and Occupational Therapy in Post COVID-19 Critical Care Follow-Up Clinic
Follow up clinic
Nichole Yam 1 and Rebecca Allen 2
1NHS
2Barts Health NHS Trust
Abstract
Introduction: The COVID-19 pandemic brought about an influx of patients admitted to critical care with higher length of stay and rates of complications. The subsequent health burden related to impaired recovery is substantial, compounded by the multi-system effects of both critical illness and COVID-19 symptoms (FICM, 2019; NHS, 2021). Emerging evidence demonstrates that the associated combination of long-term physical, cognitive, psychological, and social difficulties are highly debilitating for survivors, impacting on their day-to-day function, identity, quality of life as well as the well-being of their families and carers (NHS, 2021). With significant pressure pushed onto existing respiratory and critical care teams, this has led to the development of a temporary critical care follow-up clinic with multidisciplinary support to address increased needs holistically.
Objectives: The aim of this project was to:
1. highlight the value of having physiotherapy (PT) and occupational therapy (OT) input in COVID-19 critical care follow-up clinic
2. identify post COVID-19 critical care symptoms and issues conducive to the need for physiotherapy and occupational therapy support
3. identify gaps in services and establish community links to improve therapy access, and overall patient care and satisfaction
Methods: The COVID-19 critical care follow-up clinic ran between March 2021 and August 2021. It aimed to review patients approximately three months post-discharge. The inclusion criteria involved anyone admitted to intensive care unit (ICU) with COVID-19 at any of the Barts Health NHS Trust sites. Patients who have a very short stay on intensive care, those with no impairments on hospital discharge, and those who were palliated were excluded. The multidisciplinary team included a critical care consultant, specialist nurse, physiotherapist, occupational therapist, and psychologist.
Clinics ran consisted of four one-hour appointment slots with pre and post meeting and administration time.
Results: A total of 66 clinics were completed during this time frame. Of the patients seen in clinic (n=221), over 50% were still struggling with global weakness, reduced exercise tolerance, fatigue, pain and breathlessness.
Patient Demographics:
| Demographic/Detail | No. Patients |
|---|---|
| Total Patients Seen | 221 |
| New patients | 180 |
| Follow ups | 17 |
| Did not attend | 24 |
| Male | 118 |
| Female | 84 |
| Average age | 53.83 |
| Intubated: | 85 |
| Average hospital LOS | 32.91 |
| Average ITU LOS | 18.53 |
| Average time from discharge | 101.80 |
Therapy Referral during Admission
| Inpatient | Number | % |
|---|---|---|
| Inpatient PT | 191 | 106.1 |
| On-going needs at discharge | 110 | 61.1 |
| Referred but not seen | 4 | 2.2 |
| Inpatient OT | 65 | 36.1 |
| On-going needs at discharge | 52 | 28.9 |
| Referred but not seen | 5 | 2.8 |
Patient Reported Symptoms at Clinic
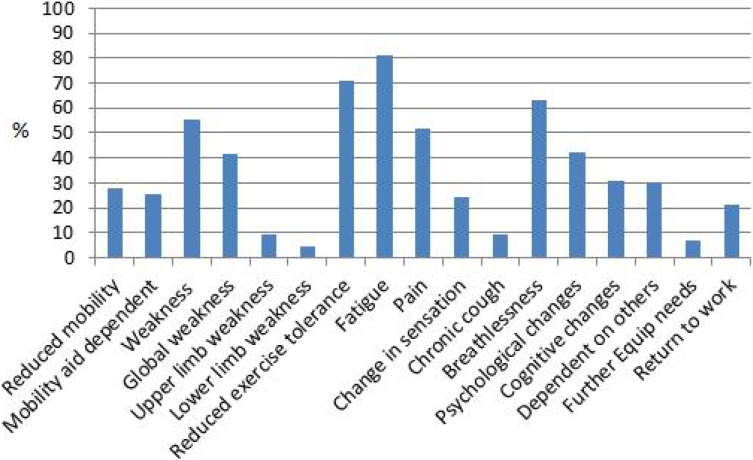
Patient Reported Recovery (%)
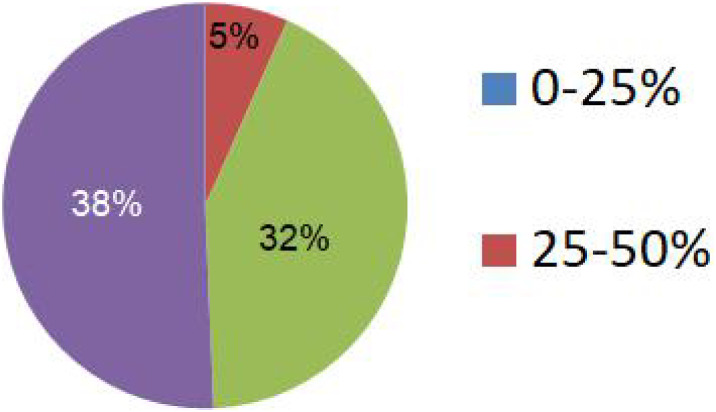
Clinic Therapy Main Interventions
| Referrals/Education | Amount | % |
|---|---|---|
| PT referrals | 8 | 4.4 |
| OT referrals | 26 | 14.4 |
| Long COVID referral | 40 | 22.2 |
| Talking therapies referral | 42 | 23.3 |
| Memory and concentration advice | 56 | 31.1 |
| Fatigue management | 146 | 81.1 |
| Cough suppression advice | 10 | 5.6 |
Clinic MDT Composition
| Clinics with | % |
|---|---|
| PT | 80.3 |
| OT | 78.8 |
| PT & OT | 51.5 |
| Nurse | 18.2 |
| Psychologist | 0 |
Discussion: The main post COVID ITU symptoms were those that linked directly to therapies, specifically fatigue, weakness, reduced mobility, and cognitive issues. Therefore, having specialist knowledge of these issues and the services that can help them within the MDT was imperative to ensuring these patients got the best care possible.
The percentage of clinics ran with just OT/PT and a consultant, the number of therapies referrals, and the specialist advice provided clearly highlights the need for more permanent therapy input in COVID ITU clinics. Having a nurse and psychologist for a fully rounded MDT would be ideal, but it shows that therapists are an invaluable addition and should be a permanent fixture to any post ICU MDT team.
Conclusion: The COVID-19 pandemic has highlighted the importance of holistic multidisciplinary team support in critical illness recovery, particularly the value of the role of physiotherapy and occupational therapy in COVID-19 critical care follow-up clinic is demonstrated in this project. Various therapy interventions were appropriate to addressing on-going symptoms and issues identified in the clinic. This clinic also provided insight onto gaps in existing services, such as rehabilitation for post intensive care acquired weakness.
References
1. Faculty of Intensive Care Medicine and Intensive Care Society. Guidelines for the Provision of Intensive Care Services (GPICS). 2nd edition. 2019. Available from: https://www.ficm.ac.uk/sites/default/files/gpics-v2.pdf [Accessed 9th August 2021].
2. National Health Service. Long COVID: the NHS plan for 2021/22. Available from: https://www.england.nhs.uk/coronavirus/publication/long-covid-the-nhs-plan-for-2021-22/ [Accessed 9th August 2021].
P109
Redesigning our follow up pathway for post critical care discharges.
Follow up clinic
Alex Hunter, Todd Leckie, Kayleigh Cooper, Mary-Kate Standing, Gemma Stoner, Nicola Bean and Luke Hodgson
Worthing Hospital, University Hospitals Sussex NHS Trust
Abstract
Introduction: During the COVID-19 pandemic we were faced with a large number of critical care discharges recovering from prolonged intensive care admission and severe lung injury at our 500 bed hospital in the South East of England. These patients often had complex rehabilitation needs and rehabilitation of these patients had been challenged by social distancing and the reconfiguration of many outpatient departments. Prior to the covid pandemic our rehabilitation pathway consisted of a nurse led follow up that focussed on psychological recovery and, following initial assessment, physiotherapy that included musculoskeletal therapy, 1:1 or small group exercises and respiratory physiotherapy.
We developed a new pathway during the COVID-19 pandemic that united these above services into a “one-stop” multi-disciplinary service that included clinician follow up and utilised smart watch technology from Fitbit watches to aid recovery of our ICU discharges.
Method: Prior to discharge patients had a comprehensive set of assessments to identify physical and psychological needs. This included an incremental shuttle walk test,one minute sit-to-stand test, patient health questionnaire-9 (PHQ-9), generalized anxiety depression questionnaire -7 and Chelsea critical care physical assessment (CPAX). Patients were offered an exercise programme, depending on level of function, and referred to appropriate community services as required. Patients received Fitbit charge 3 watches and were asked to wear these as often as they felt able. At three months following discharge patients attended a multidisciplinary clinic consisting of an intensive care clinician, physiotherapist, and nursing staff. Outcome measures were re-assessed, and the patient had access to ongoing physio, nursing and medical input to support their recovery. Fitbit data was reviewed and incorporated into future goal setting. In addition, patients were invited to a relative and patient support group as an opportunity to meet other critical care survivors and for their relatives to share their experiences of recovery. They were also offered the chance to visit the ICU to aid physiological recovery.
Results: The “one-stop” nature of the clinic allowed a resource efficient means for multi disciplinary care to be delivered to patients. The majority of patients found the support group extremely beneficial. Patients reported they found it helpful being able to share experiences, listen to others and see people at different stages in their recovery. Relatives also found the experience useful to deal with the traumatic experience of a critically ill loved one. Smart watches were well received by patients and over 80% of patients felt the watch aided their recovery. The watches also added a unique dimension to the MDT meeting, able to pick up changes in daily activity levels, rapidly alerting the clinician to a potential problem in that patient.
Conclusion: The service is continually evolving. Future plans aim; to use smart watches for all ICU discharges with an integrated app to promote recovery and allow remote feedback, to use a Post-ICU Presentation Screen (PICUPS) and rehabilitation prescription to inform rehabilitation needs and to include a psychologist into the clinic to improve patient recovery after ICU admission.
References
1. A. Hunter, Todd L, D Fitzpatrick, A Goncalves, A Richardson, L Hodgson. Digitally enhanced recovery from severe COVID-19: a new frontier? Future Healthc J 2020. DOI: 10.7861/fhj.2020-0271
2. Todd L, A Hunter, L Hodgson. Investigating and Innovating COVID-19 Critical Illness Rehabilitation. Critical Eye September 2020.
P110
Osmotic demyelination syndrome - all is not lost!
Imaging in critical care
Aalekh Prasad 1 , Sneha Gurung2 and Sabina Popa2
1Peterborough City Hospital
2Peterborough city hospital
Abstract
Introduction: Osmotic demyelination syndrome (ODS) is characterised by partial destruction of myelin sheath at the pons. The advised rate of correcting chronic hyponatremia in high-risk patients is 4-6 mmol/l in any 24 hour period.1 Risk factors that increase the susceptibility of ODS even at slower rates of correction are alcoholism, malnutrition, liver disease and hypokalaemia.2
Case reports and case series have often shown a high mortality,3 however the prognosis is variable. Some patients do make a full neurological recovery.
Description: A 43-year-old female with known alcoholic liver disease was admitted after a history of fall from stairs and coffee ground vomit. On presentation she was alert with a GCS of 15, maintaining her airway with oxygen saturation of 99% on room air with blood pressure of 124/64 mm Hg and HR of 102/min. She underwent Upper GI endoscopy for banding and was admitted with a diagnosis of alcoholic liver disease with acute on chronic upper GI bleed.
During her admission, the patient was found to be intermittently confused, could move her eyes but had weakness in her arms and legs with a muscle power score of 0/5 and was found to be in type 1 respiratory failure.
She was admitted to critical care, intubated and ventilated for a possible aspiration pneumonia. Intravenous antibiotics were escalated, and hepatic encephalopathy was ruled out.
Lumbar puncture revealed no pathogens. EEG was suggestive of an alpha coma pattern; CT was not suggestive of any acute pathology. MRI showed altered signal intensity of the pons suggestive of osmotic demyelination (central pontine myelinolysis).
Her serum sodium was lowered and supportive therapy was continued. Over the next few days, the patient had a gradual improvement in mentation and oral buccal – lingual movements and could manage her own secretions. Her tetraplegia recovered with a muscle power score of 2/5 in all 4 limbs.
Patient was extubated a discharged to neuro rehabilitation ward after a safe swallow assessment. She was followed up for the next three months and is now able to walk with a frame.
Disussion: Neurological symptoms of ODS typically occur 6-7 days after correction of hyponatremia. The optimal approach to treat is unclear, we tried relowering serum sodium with ongoing supportive therapy. Relowering therapy should be initiated as quickly as possible after the onset of neurologic symptoms. It can reverse the breakdown of the blood-brain barrier that occurs with overly rapid correction and can prevent the infiltration of microglia that is a feature of osmotic demyelination.4
Data in humans is limited to case reports that suggest if relowering is initiated within a few hours after the onset of neurologic symptoms, it is associated with a better outcome.5,6
References
1. Hoorn EJ, Zietse R. Diagnosis and Treatment of Hyponatremia: Compilation of the Guidelines. J Am Soc Nephrol. 2017;28:1340-9.
2. George JC, Zafar W, Bucaloiu ID, Chang AR. Risk Factors and Outcomes of Rapid Correction of Severe Hyponatremia. Clin J Am Soc Nephrol. 2018;13(7):984-992. doi: 10.2215/CJN.13061117. Epub 2018 Jun 5. PMID: 29871886; PMCID: PMC6032596.
3. Martin RJ. Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry 2004;75(Suppl 3): 22-28.
4. Gankam Kengne F, Soupart A, Pochet R, Brion JP, Decaux G. Re-induction of hyponatremia after rapid overcorrection of hyponatremia reduces mortality in rats. Kidney Int. 2009;76(6):614-621. doi: 10.1038/ki.2009.254. Epub 2009 Jul 15. PMID: 19606078.
5. Soupart A, Ngassa M, Decaux G. Therapeutic relowering of the serum sodium in a patient after excessive correction of hyponatremia. Clin Nephrol. 1999;51(6):383-386. PMID: 10404700.
6. Oya S, Tsutsumi K, Ueki K, Kirino T. Reinduction of hyponatremia to treat central pontine myelinolysis. Neurology. 2001;57(10):1931-1932. doi: 10.1212/wnl.57.10.1931. PMID: 11723299.
P111
Comparing Computed Tomography and Transoesophageal Echocardiography to Determine Veno-venous Extracorporeal Membrane Oxygenation Cannulae Position
Imaging in critical care
Clare Russell 1 and Brigitta Fazzini2
1Royal Brompton and Harefield Hospital
2Royal London Hospital, Barts Health NHS Trust
Abstract
Introduction: Precise cannula tip positioning is essential for patient safety and optimal treatment during veno-venous extracorporeal membrane oxygenation (VV-ECMO). Patients at our institution undergo both admission computed tomography (CT) and transoesophageal echocardiography (TOE) following cannulation; however, anecdotal experience suggests these techniques may not agree on cannula location.
Objectives: To determine whether cannulae position discrepancies exist between CT and TOE.
Methods: Service evaluation involving retrospective data analysis of consecutive adult (18-years and over) VV-ECMO patients admitted to Intensive Care Unit, who underwent both CT and TOE within 24-hours. Cannula positions from imaging reports were compared for conformity or otherwise.
Results: During the 21-month review period, 50 were eligible for inclusion. CT and TOE reports agreed on drainage cannula tip positions in 65% (n=15) and disagreed in 35% (n=8), and for return cannulae, reports agreed on tip position in 50% (n=13) and disagreed in 50% (n=13). Of the 21 cannulae position discrepancies between the imaging modalities, 7 were deemed ‘unsafe’ involving cardiac structures, of those 5 were diagnosed by TOE and 2 by CT. Cannula repositioning only occurred if locations were deemed unsafe by the TOE scan regardless of the CT findings.
Conclusion: Our data suggests discrepancies in reported cannula locations between CT and TOE can occur, despite a minimal time between scans; corroborating anecdotal experience. Patient imaging positioning, patient body habitus and movement, and difficulties in interpreting the various cannulae designs using different imaging modalities are the potential causes. A paucity of the literature suggests further research is required to evaluate the function, necessity, practical capabilities, and cost-effectiveness for routine use of both imaging modalities.
P112
Radiopacity of sodium zirconium cryosilicate on plain radiography
Imaging in critical care
Christopher Pennington 1 and Michelle Carey2
1Health Education North East
2South Tees NHS Hospitals Trust
Abstract
Introduction: Sodium zirconium cyclosilicate is a novel potassium binder developed by AstraZeneca and is sold under the brand name Lokelma (TM). It has been approved for use in England in 2020 for the treatment of non-life-threatening hyperkalaemia, and stable hyperkalaemia in patients with chronic kidney disease.1 It is available as powder sachets (5 grams and 10 grams) and is designed to be mixed with water and administered enterally. The starting dose is recommended as 10 grams three times per day, and resolution of hyperkalaemia is usually seen within two days, after which a lower maintenence dose may be administered.
The radiopaque properties of sodium zirconium cyclosilicate have previously been noted on computed tomography before in 2021,2 but, to our knowledge, this has not yet been described on plain radiography.
Case presentation: We present the case of a critically unwell lady in her 50s with COVID-19 pneumonitis. As a feature of her critical illness syndrome, she developed acute renal failure, and required renal replacement therapy. Persistent problems with hyperkalaemia were noted, and sodium zirconium cyclosilicate was administered enterally via a nasogastric tube as directed in the product literature. For unrelated reasons, she also required a chest radiograph within the following hour. On reviewing the radiograph, a radiopaque material was noted in the stomach, and was seen to very clearly outline the major anatomical features of the organ, including the greater and lesser curve, and gastric rugae. After discussion with our local radiology colleagues and finding the material is opaque on computed tomography, we concluded this material must be the recently administered sodium zirconium cyclosilicate.
Investigation: Image of radiograph showing radiopaque material in the stomach of a critically unwell patient.
Discussion: To our knowledge, the radiopaque properties of sodium zirconium cyclosilicate have not been described before in the medical literature as relating to plain radiography. When interpreting plain radiographs, it is important to understand and exclude sources of artefact. As sodium zirconium cyclosilicate becomes widespread in critical care areas, we believe the above-described scenario will be commonly encountered. Moreover, we believe that sodium zirconium cyclosilicate may have additional utility as a well tolerated enteral contrast agent with the added benefit of lowering serum potassium concentration.
References
P113
Introducing a new role: Critical Care Infection Specialist Nurse
Infections and prevention
Felicity Kempson
Liverpool Heart and Chest Hospital
Abstract
Introduction: As a tertiary centre that uses the clinical laboratories based at a different NHS trust, we have previously relied on contracted microbiology input from them. These rounds happened three days a week, which meant that we were not compliant with GPICS version 2 guidelines stating that there should be microbiology input for patients five days a week.1
To address this, we created the role of Critical Care Infection Specialist Nurse. The role aims to ensure five days per week of microbiology input for patients on antibiotics and assist in cascading antimicrobial stewardship information to the rest of the team.
Responsibilities:
Microbiology
• Liaise with the laboratories and feedback advice to the ITU team
• review patients with existing or suspected infections 5 days a week
• Audit antimicrobial use and identify areas for improvement in conjunction with pharmacy
Sepsis
• Promoting the trust Sepsis Policy and providing education for new staff
• Provide direct feedback to sepsis first responders as part of a quality improvement project
Infection Prevention and Control
• Review bacteraemias within the critical care area and report back on these to the Matron and IPC team
• Initiate central line and Peripheral Vascular access surveillance as part of a quality improvement project
My experience so far: I commenced the role in mid-April 2021 and the initial response to the role has been extremely positive.
The majority of the feedback that I have received is that people feel that they have a dedicated person to come to with queries about infection and antimicrobial use.
I have also been told that my role has freed up time for the ITU medical team as I can liaise with the laboratory during office hours for them.
The Consultant Microbiologist has also felt that my role on site has allowed him to get a better understanding of the patients as I can report back any problems daily and provide a detailed history before ward rounds so that he can make a better informed decision for care plans.
The Future: I plan on increasing awareness of proper antimicrobial prescribing policy. Since I commenced the role (mid April – mid June) I have identified 8 patients commenced on antibiotics within the critical care area without any cultures being take prior to administration.
I am also keen to identify possible uses for technology and up to date research that can help us to reduce inappropriate antibiotic usage.
References
1. Davis E. & Mckee R. Section 3.5 Interaction with Other Services: Microbiology, Pathology, Liaison Psychiatry and Radiology in GUIDELINES FOR THE PROVISION OF INTENSIVE CARE SERVICES (online). (2019) [Accessed 22/5/21]. Available at: https://www.ics.ac.uk/ICS/ICS/Pdfs/GPICS_2nd_Edition.aspx
P114
Assessment of knowledge, practice and compliance eye care guidance in neurocritical care unit
Infections and prevention
Sandeep Sharma 1 , Vallish Bhardwaj2 and Vikram Malhotra3
1Addenbrookes Hospital
2Peterborough City Hospital, North West Anglia NHS foundation trust
3Addenbrookes Hospital, CUHNFT
Abstract
Introduction: Ocular complications in critically ill patients is common. Up to 42% of intensive care unit patients can have signs of damage to the corneal surface of the eye (exposure keratopathy), which can lead to secondary complications and ultimately irreversible visual loss1,2 (Rosenberg and Eisen, 2008; Bird et al, 2017). Emergence of COVID-19 pandemic has meant increased number of critical care admission with inherent risk of ocular complication owing to need for non-invasive ventilation, mechanical ventilation and prone ventilation. All these factors have resurfaced need for increased awareness and adherence to national standards related to eye care in critical care3 (Royal college of Ophthalmology and Intensive Care Society joint Ophthalmic service guidance).
Objectives: To study baseline knowledge and awareness of eye care practices in neuro critical care unit.
To measure compliance of national eye care guidance.
Methods: Structured online survey for critical care nurses.
Review of hospital IT software to study snapshot of eye care compliance.
Results: We ran baseline survey of neuro critical care nurses on knowledge and current practice of eye care in ICU. Eye care complications in ICU are common with 1 in 5 individual reporting > 3 ocular complications in last 3 months. Three-quarter of individuals reported to have good to very good knowledge of eye care protocol with 66% aware of current national guidance. 86% of respondents assessed lagophthalmos while 76% assessed conjunctiva and cornea routinely. On the flipside however only 60% routinely documented eye care measures in clinical practice. Importantly, 96% responded that they would benefit from education and training in eye care practices.
Review of hospital records for eye care compliance and documentation validated the findings on the survey. We found 68% compliance rate for assessment of lagophthalmos in all admitted patient in neuro critical care unit. There was 100% compliance to institution of protective measures and appropriate escalation to medical staff.
Graph 1: Baseline survey of knowledge and practice of Eye care in Neuro Critical Care Unit depicting a stepladder pattern in knowledge, practice and documentation of Eye care.
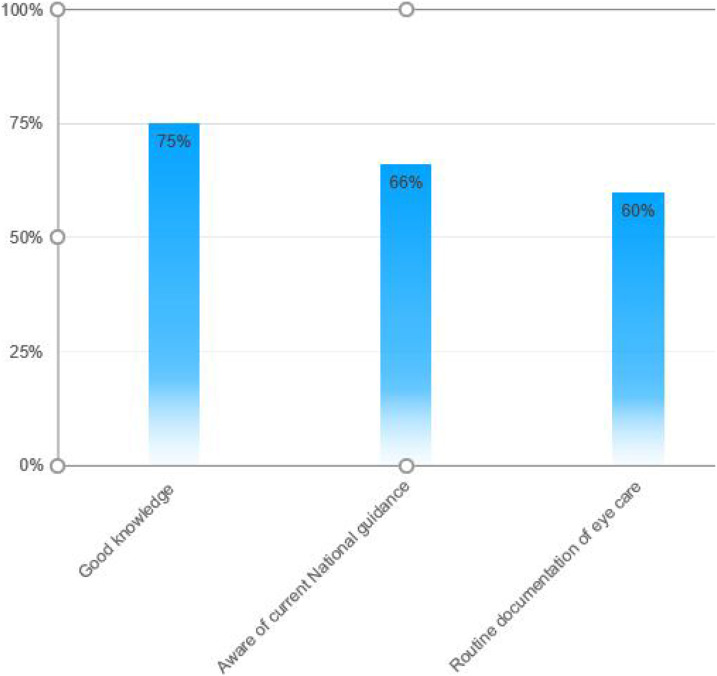
Table 1.
Snapshot audit of eye care practices in Neuro critical care unit.
| No | Standard | Compliance Percentage, n=50 |
|---|---|---|
| 1. | 100% of Assessments of eyelid closure should be done at the onset of the care plan in all ICU patients | 68% |
| 2. | 100% of patient should have protective actions instituted according to the grade of severity of lagophthalmos. | 100% |
| 3. | Assessment of eyes for redness/stickiness or corneal haze should be performed for all ICU patients. | 78% |
| 4. | Medical staff should be alerted and ophthalmology referral should be done if criteria met. | 100% |
Conclusion: Knowledge and awareness of eye care practices fall below national guidance. There is clear gap in knowledge, practice and documentation of eye care practices. Incorporation of eye care module in continuous training program and use of cognitive aids may help to further improve compliance and documentation of eye care practice in future.
References
1. Rosenberg JB, Eisen LA. Eye care in the intensive care unit: narrative review and meta-analysis. Crit Care Med. 2008;36(12):3151–3155
2. Bird B, Dingley S, Stawicki SP, Wojda TR. Exposure keratopathy in the intensive care unit: do not neglect the unseen. 2017. Vignettes in Patient Safety. Ch. 9. https://doi.org/10.5772/intechopen.72791
3. Eye care in Intensive care unit: Ophthalmic services guidance. https://www.rcophth.ac.uk/wp-content/uploads/2020/04/Eye-Care-in-the-Intensive-Care-Unit-2020.pdf
P115
You Care Eye Care: A quality improvement project to prevent eye complications in the intensive care unit
Infections and prevention
Fiona Walker, Karen Jones, Bethany Hastings, Sarah Ackroyd, Fraser Waterson, Zuhair Mustafa, Nikki Hall, Ross Paterson and Cameron Ferguson
NHS Lothian
Abstract
Introduction: 42% of patients in the intensive care unit (ICU) will suffer ocular damage during their stay.1 Multiple mechanisms that usually protect the eye are inhibited, whilst interventions such as positive airway pressure and muscle relaxants further expose the eye to harm.2 This became increasingly evident during the COVID-19 pandemic, where non-invasive ventilation and proning of patients exposed patients to risk of injury.3 Redeployment of Ophthalmologists to ICU during the first wave of the COVID-19 pandemic highlighted the need for a robust and sustainable intervention to reduce the frequency of eye complications in our unit.
Objectives: Our objective was to reduce harm to eyes in all patients within the Royal Infirmary of Edinburgh (RIE) to zero ICU within nine months.
Methods: Our QI project involved initial staff and patient data collection regarding current eye care practices. A fish-bone diagram facilitated group discussions with ICU clinical teams regarding prior eye care practices. A pareto chart identified categories to focus on, with a driver diagram identifying change ideas. Our primary intervention was the design and introduction of a bespoke eye care guideline. Specific outcomes, processes, and balancing measures were set out, and multiple PDSA cycles helped to prompt interventions to ensure consistent and standardised care was delivered. Run charts were regularly reviewed and a variety of interventions were introduced throughout the data collection period as tests of change.
These included:
1. posters highlighting guideline enrolment
2. formal teaching at handovers and on the unit
3. educational emails to staff members
4. prompts on daily reviews to highlight eye care assessments.
Between 28 Sept 2020 - 28 June 21, twenty patients in RIE ICU were randomly selected by the data collection team weekly. Patient outcome - eyes were examined and noted if they had developed any ocular complications during their stay. Patients who had evidence of ocular damage on admission were excluded unless they developed further complications. A single episode was not counted twice. Process outcomes - Eye care guideline adherence was recorded, and non-compliance was rectified following data collection. The data was recorded on run charts, accessible via MS teams, allowing all project team members to review the data remotely.
Results: During our data collection period, the introduction of our guideline and educational interventions reduced the median number of patients who suffered eye complications in ICU by 50% within nine months (Figure 1). Chemosis and evidence of dry eyes were the most common complications. Since initiation of the guideline, our educational interventions have maintained median guideline compliance at 80%.
Figure 1.
■■■.
Conclusion: This is a comprehensive, patient-centred, QI project, utilizing a systematic methodology to introduce a new guideline within ICU.
This project has resulted in a sustained improvement of eye care standards, and reduction of eye complications within RIE ICU. This project was ongoing during the second wave of the COVID-19 pandemic, where constant rotation of medical staff, unfamiliar with ICU, required education to ensure guideline compliance was achieved. Our eye care guideline is now part of a multi-centre project to standardise care across NHS healthboards.
References
1. Hearne B, Hearne E, Montgomery H, Lightman S. Eye Care in the Intensive Care Unit. Journal of the Intensive Care Society. 2018. doi:10.1177/1751143718764529
2. Lightman S, Montgomery H. Eye care in the Intensive Care Unit guideline. https://www.rcophth.ac.uk/wp-content/uploads/2017/11/Intensive-Care-Unit.pdf
3. Sansome S, Lin P-F. British journal of hospital medicine (London). 2020. doi:10.12968/hmed.2020.0228
P116
Tackling VAPs the Up-to-Date Way
Infections and prevention
Catherine McGow, Jennifer Reynolds, Victoria Green and William Angus
Liverpool University Hospital NHS Foundation Trust
Abstract
Introduction: Ventilator-associated pneumonias (VAPs) are the most frequent healthcare associated infection in adult critical care units.1 They are associated with an increased critical care length of stay and patient mortality.2 Early identification of the causative pathogen enables targeted antibiotic therapy; reducing the risk of antibiotic resistance.3 In order to identify the pathogen, there are different techniques to obtain cultures from the airway, commonly endotracheal aspirates are taken on our intensive care unit. Whilst comparing these methods, a recent study showed that the sensitivity of non-directed bronchial lavage (NDBAL) is 63-100%, significantly higher than endotracheal aspirates (EA) that have a sensitivity of 38-82%.4,5 Given the study’s findings we realised we needed to increase the carrying out of NDBAL on our patients as part of a septic screen as well as a screening method for VAPs.
Objectives: Our primary aim was to increase the use of NDBAL sampling for mechanically ventilated patients on the intensive care unit, using a standardised approach.
Methods: To achieve our primary aim, we initially assessed staff members’ knowledge on how to perform a NDBAL using a survey by asking them to recount verbally the steps. The survey was filled in by a member of the team. After realising the significant lack of knowledge around the method, we created an equipment list and guide which was distributed to all staff. Over a couple of weeks, we spent time on the critical care unit teaching the method and helping staff perform the sampling technique. We then reassessed through the same survey to see if knowledge of the approach had improved.
Results: Using our survey of the 40 staff initially assessed – they averaged only 39% of the seven points on our assessment. Post training and creation of the guide this score improved to 67%. Although we note several new staff joined throughout out the training period so not all staff assessed in the second round had received any training.
Conclusion: We are happy with our initial results and hope to continue this work. Due to current training structure trainees rotating often results in projects not continuing and leading to frustration. We have therefore enrolled the critical care unit’s practice educator team to help continue educating the over one hundred nurses who work on our critical care unit. We will aim to reassess the success of this project in the future in two ways – assessing the number of NDBAL samples sent, reassessing knowledge of the procedure and ultimately looking at how many patients treated for VAP have their antibiotics guided by a microbiological sample.
References
1. Vincent JL, Sakr Y, Sprung CL, et al. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 2006; 34: 344–353
2. Hunter JD. Ventilator associated pneumonia. Bmj. 2012;344.
3. Felton T, Mount T, Chadwick P, Ghrew M, Dark P. Surveillance non-directed bronchial lavage allows confident use of focused antibiotics in the management of ventilator-associated pneumonia. Journal of Infection. 2010;60(5):397-399.
4. Cook D, Mandell L. Endotracheal aspiration in the diagnosis of ventilator-associated pneumonia. Chest 2000;117(4 Suppl. 2):e195S-e197S.
5. Campbell GD Jr. Blinded invasive diagnostic procedures in ventilator-associated pneumonia. Chest 2000;117(4 Suppl. 2):e207S-e211S.
P117
Qualitative Research in a Technological Age: Friend or Foe
Information technology
Bronwen Warner1, Alice Harry2, Stephen Brett3, Mary Wells1, David Antcliffe 1
1Charing Cross Hospital
2Royal Free Hospital
3Hammersmith Hospital
Abstract
Introduction: Familiarity with information technology is increasingly widespread. COVID-19 has increased the use of video conferencing and social media within the UK population, including by older people1 This evolving scene has the potential to change how research is conducted.2
Social media has been employed for recruitment to qualitative research,3,4 but mostly in a young cohort. Recruitment through interfaces such as Twitter has the potential to access a larger number of participants, but may not reach all groups, such as older people.
Video conferencing (VC) is increasingly used for qualitative interviewing.5 It simulates in-person communication while avoiding the need to travel but requires access to costly equipment and confidence in engaging with the technology.
Objective: To explore the experience of using technology in a critical care-based qualitative research study.
Methods: The ESCAlation of the eLderly (Age-65years) to criTical carE with COVID-19 (ESCALATE) study uses semi-structured interviews with patients and loved ones to explore views on escalation of older people to critical care during the COVID-19 pandemic.
Recruitment took place using two routes: UK-wide social media advertising; and postal invitations via local databases with telephone follow up. For the former, the study was advertised directly via the social media platform Twitter using a specifically created study account (@covidescalate), showing a brief advert and link to a questionnaire and contact form. Relevant charities were invited to disseminate the advertisement.
In-person interviews were avoided to maximise participant and interviewer safety in the context of the COVID-19 pandemic. Participant preference for mode of interview (VC or telephone) was established. If participants stated in advance that they were not familiar with video technology or found during the interview that they were unable to manage a VC, interviews were conducted by telephone.
Results: There was partial uptake by charities and limited ‘retweeting’ overall. Only one responder meeting eligibility criteria responded via social media advertising, compared with 44 from local postal/telephone recruitment.
Ten interviews were conducted via VC and 12 via telephone, where participants were not familiar with VC. There was no difference in interview duration with VC lasting around 45 minutes and telephone calls lasting around 42 minutes. The researchers found that it was more difficult to pick up on social and non-verbal cues without visual contact but all questions in the topic guide were covered using both media.
There was no difference between choice of VC vs. telephone according to participant ethnicity (BAME vs Caucasian) or sex.
In one case, several participants from one family joined the VC from different locations.
Conclusion: In the ESCALATE study, video conferencing and telephone interviews were both valuable interviewing methods. Social media recruitment was of limited use but this may reflect the participant demographic and research team experience and could still be useful for recruiting certain groups in other studies. Information technology has the potential to increase engagement with research but our experience demonstrates that it must be used flexibly and with consideration.
References
1. Haase KR, Cosco T, Kervin L, Riadi I, O’Connell ME. Older Adults’ Experiences With Using Technology for Socialization During the COVID-19 Pandemic: Cross-sectional Survey Study. JMIR Aging. 2021;4(2):e28010.
2. Richardson SJ, Carroll CB, Close J, Gordon AL, O’Brien J, Quinn TJ, et al. Research with older people in a world with COVID-19: identification of current and future priorities, challenges and opportunities. Age Ageing. 2020;49(6):901–906.
3. Gray MF, Ludman EJ, Beatty T, Rosenberg AR, Wernli KJ. Balancing hope and risk among adolescent and young adult cancer patients with late-stage cancer: a qualitative interview study. J Adolesc Young Adult Oncol. 2018;7(6):673–680.
4. Lefèvre L, Jourdain M, Fournier J-P. Processes and determinants of integration of eGFR in physicians’ drug prescriptions: a qualitative study of semi-structured interviews. Prim Health Care Res Dev. 2019;20.
5. Archibald MM, Ambagtsheer RC, Casey MG, Lawless M. Using Zoom Videoconferencing for Qualitative Data Collection: Perceptions and Experiences of Researchers and Participants. Int J Qual Methods. 2019;18:1609406919874596.
P118
Solving our sepsis problem with technology – where should we focus our resources?
Information technology
Emma Knight and Simon Morton
Bermuda Hospitals Board
Introduction: This retrospective audit reviews the recognition and management of sepsis in patients who required Intensive Care (ICU) admission. It was performed in a small island hospital with ninety acute care patient beds and eight ICU beds.
The data collected will enable us to improve sepsis recognition and management and support clinical decision making through the implementation of an electronic health record (EHR) and electronic alert system.
Objective: To determine where an electronic health record and alert system would be valuable in the recognition and management of sepsis in patients.
Method: Retrospective review of the ICU admissions book over a 12-month period to determine patients that were admitted with sepsis or septic shock from either the Emergency Department (ED) or from an acute ward.
Analysis of documentation of vital signs in paper medical notes versus electronic medical records, and whether appropriate escalation and management was performed.
Results: There were 35 admissions to ICU with a diagnosis of sepsis or septic shock. Of these, 24 sets of notes were reviewed. Eleven patients were excluded because the notes could not be retrieved.
•Documentation of observations was clearer in patients admitted from ED compared with patients admitted from the ward
•Investigations and management received (within 1 hour):
• Bloods, including cultures: 15 patients (63%)
• ABG or VBG for lactate: 11 patients (46%)
• Urine culture: 8 patients (33%)
• IV fluids: 15 patients (63%)
• Oxygen: 12 patients (50%)
• Antibiotics: 10 patients (42%)
Conclusions: Following review of the data collected:
1. The frequency of vital signs documented in ED was more accurate compared with those taken on the ward. This can be attributed to the fact that ED uses an existing medical record. The frequency of observations is automatically adjusted by the MEWS scoring system. We aim to implement an electronic vitals system, on the wards, which uses automated frequency change of observations based on MEWS scoring. This will reduce human error and support early clinical recognition of sepsis.
2. With regards to patient investigations and management in both ED and the wards, the majority of patients (63%) had bloods taken and IV fluids given. However, less than half of the patients (42%) were given antibiotics within an hour of review. This shows that an alert system triggered by MEWS scoring with pop-up alerts that require specific actions such as launching a power plan with order sets for bloods, cultures and antibiotic prescribing can improve the efficiency of sepsis management1 and ultimately reduce the number of sepsis related ICU admissions.
3. Further, our current antibiotic guidelines can be integrated into the electronic system to standardise management.
4. Finally, to make the system user friendly, we aim to use a traffic light colour system and pop-up alerts that require specific actions to reduce click fatigue. Information in alerts and order sets2 will be provided in a succinct, easy to follow manner to optimise user focus.
Reference
1. Guirgis F, Jones L, Esma R. et al. Managing sepsis: Electronic recognition, rapid response teams, and standardised care save lives. J Crit Care. Epub ahead of print 8 April 2017. DOI: 10.1016/j.jcrc.2017.04.005
2. Schubel L, Mosby D, Blumenthal J, et al. Informatics and interaction: Applying human factors principles to optimize the design of clinical decision support for sepsis. Health Informatics Journal. Epub ahead of print 13 May 2019. DOI: 10.1177/1460458219839623
P119
Rapid Response Team, Cambridge university hospital experience
Intensive care MET & RRT
Sarah Ahmed 1 and Sara Hutton2
1Cambridge university hospital NHS foundation trust
2Cambridge university hospital
Abstract
Introduction: Most UK hospitals have a variation of a Critical Care Outreach Team (CCOT) as part of their ICU service. NICE states that the main role of a CCOT is to identify and institute treatment in patients who are deteriorating within the hospital but outside of the ICU and either help to prevent admission to ICU or ensure that admission to a critical care bed happens in a timely manner to ensure best outcome.1 At Addenbrooke’s Hospital, a 1000 bed tertiary and Major Trauma centre, the RRT is a 24/7 service consisting of two resident senior nurses, a resident registrar level doctor and an ICU consultant resident or on-call overnight. Roles include assessing and reviewing critically unwell patients on adult wards and Emergency department, leading cardiac arrests, reviewing ICU discharges, and providing training/teaching courses to all staff grades.
Objectives: This study aimed to evaluate perspectives of hospital staff accessing the Rapid Response Team (RRT) services, to improve safety and efficiency.
Method: In order to effectively sample staff opinion on how well the RRT met staff needs, a short electronic qualitative survey was sent to all staff at Addenbrooke’s Hospital via email, online staff bulletin and social media. 198 responses were returned over a 11-week period (May to July 2021). The survey consisted of a section for demographics, a series of questions rated “strongly agree” to “strongly disagree” and a short answer section for areas for improvement or excellence.
We analysed the responses for key areas: ease of referral, response times, support, issues with communication and areas of improvement.
Results: The results showed that 94% staff members knew how to contact the team, 78% believed that RRT staff respond in a timely manner, 75% of staff felt supported by the RRT, 78% of respondents felt the RRT communicated well with the MDT. Written comments emphasised the need for improvement in communication, the need for more staff in the RRT as response times were sometimes delayed, and confusion over the structure of the RRT and contacting various branches (nurses, registrars or consultants). More training and teaching were also an outcome of the written feedback.
Conclusion: Most survey responses were generally very positive, most felt supported by the RRT and felt communication was good. However, clear areas for improvement were highlighted, such as confusion over structure, confusion over what support was offered by the RRT, and areas of concern over poor communication with patient teams. To mitigate these risks, and enable smoother access to RRT services, we propose to “relaunch” the RRT throughout the trust, so as to clearly state our standard operating practice and knowledge throughout the Trust.
Reflecting on these conclusions, the challenges inherent in a multi-disciplinary Rapid Response Team as opposed to a primary nurse led CCOT become more apparent, which is important to those Trusts changing from CCOT to RRT.
References
1. NICE guideline 94 March 2018, chapter 27 critical care outreach
P120
L-ornithine L-aspartate lowers ammonia and improves cognitive function but not mortality in hepatic encephalopathy from acute on chronic liver failure
Liver failure
Sarah Sawieres, Angela Kc, Catherine Mc Kenzie and Georg Auzinger
Sarah Sawieres Kings College Hospital
Abstract
Introduction: While hyperammonia is the primary cause of hepatic encephalopathy (HE) in acute liver failure (ALF), in acute-on-chronic liver failure (ACLF) its importance is reduced as other factors that may also impair cerebral function. The evidence for improving ammonia and HE using L-ornithine L-aspartate (LOLA) is debated and patients with ACLF underrepresented in randomised trials of LOLA.
Objective: The aim of this project is to explore the efficacy of LOLA in patients with ACLF.
Methods: A retrospective case-control study was performed of patients admitted to the liver intensive therapy unit (LITU) in King’s College Hospital between October 2017 and May 2020. In all patients HE (grade >2 with associated hyper-ammonaemia) was a major and persistent component of the ACLF presentation. LOLA was given as either an IV infusion (20g loading dose over 4hours followed by 20g over 24hours) or oral sachets (3-6g BD-TDS) for an average of 5 days. The non-LOLA treated control group was matched by age, sex, aetiology of liver disease and mortality scores (acute physiology and chronic health evaluation (APACHE) and simplified acute physiology score (SAPS), chronic-liver-failure acute-on-chronic liver failure score (CLIF-C ACLF).
Results: Sixty-seven patients (median age for males was 48(63) and 58(50) for females) patients made up the study cohort; 40 patients who received LOLA had a median ACLF grade of 3, median HE grade of 3 at admission and had a 59% mortality. A further 27 patients made up the control group who had an ammonia >100 and did not receive LOLA, their median ACLF grade was 3, median HE grade was 4 and a 65% mortality. The mean APACHE II score for both cohorts was 25.
Twenty-seven patients in the LOLA group and 13 patients in the non-LOLA group were mechanically ventilated (p=0.7). Median HE grade was 3 for both groups. Thirty-one patients in the LOLA group were on laxative and 10 in the control group (p= 0.157). One patient was on rifaximin prior to starting LOLA and 2 were on rifaximin in the control group (p= 0.157). Fourteen patients in the LOLA group and 12 in the non-LOLA group received haemofiltration (p=0.05). A significant reduction in ammonia (p=0.008) with a mean ammonia of 61 pre LOLA and a mean ammonia of 52 and HE grade (p=0.03) was seen in the group that received LOLA. This group had a mean ammonia of 115(60) pre LOLA 75.5(48) post LOLA. The control group also had a significant reduction in the ammonia (p=0.01) with a mean ammonia at 144.9(50.6) and a late mean ammonia of 76(23) but no significant reduction in the HE grade (p=0.08). Both the control and LOLA group saw a significant reduction in SAPS II score however only the control group had a significant reduction in APACHE II score.
Conclusion: In an intensive care setting, LOLA can reduce HE grade and plasma ammonia in patients with ACLF and HE. LOLA does not appear to improve mortality or non-HE related organ failure severity. Further investigation to assess its efficacy in early administration in ACLF driven by HE is required.
References
1. Butterworth R. Ammonia Removal by Metabolic Scavengers for the Prevention and Treatment of Hepatic Encephalopathy in Cirrhosis. Drugs R D 2021; 21: 123-132 https://doi.org/10.1007/s40268-021-00345-4
2. Butterworth R.. L-Ornithine L-Aspartate: Multimodal Therapeutic Agent for hyperammonemia and Hepatic Encephalopathy in Cirrhosis. J Pharmacol Pharm Res 2019; 2(3):1-9 https://doi.org/10.31038/JPPR.2019234
3. Butterworth R, Kircheis G, Hilger N, McPhail MJW. Efficacy of L-Ornithine L-Aspartate for the Treatment of Hepatic Encephalopathy and hyperammonemia in Cirrhosis: Systemic Review and Meta-Analysis of Randomized Controlled Trials. J clin Exp Hepatol 2018; 8(3) 301-313 https://dx.doi.org/10.1016%2Fj.jceh.2018.05.004
4. Butterworth R, McPhail MJW. L-Ornithine L-Aspartate (LOLA) for Hepatic Encephalopathy in Cirrhosis: Results of Randomized Controlled Trials and Meta-Analyses. Drugs 2019; 79 (Suppl 1): 31-37 https://dx.doi.org/10.1007%2Fs40265-018-1024-1
P121
Predicting outcomes in patients with liver failure in intensive care: Is phosphate a useful biological marker?
Liver failure
Frederick Cripps
Cardiff and Vale University Health Board
Abstract
Introduction: Phosphate level abnormalities in patients with acute liver failure have been observed and discussed across a range of contexts, including as a potential aid in prognosis for liver transplantation, and in paracetamol induced liver failure. 1-3 Hypophosphatemia is generally considered to be associated with better outcomes and possible mechanisms such as increased phosphate use during hepatocyte regeneration have been suggested.4 In the intensive care setting admission with decompensated liver disease still carries a high mortality risk and the clinical value of its prognosis is reflected in the multitude of scoring systems in use and under development.5 In this study we wanted to investigate the potential value of phosphate levels as prognostic marker in liver failure patients admitted to intensive care.
Objectives: To determine whether there is an association between phosphate level on admission and mortality in patients admitted to the intensive care unit with liver failure.
Methods: The study was a retrospective analysis of data collected from patients admitted to Royal Glamorgan Hospital and Prince Charles Hospital intensive care units with acute liver failure or a history of chronic liver failure between December 2018 and December 2020. Patient phosphate was categorised as high, normal, or low based on blood test results at the time of admission to ICU. This was then compared with survival outcomes during that hospital admission.
Results: There were 77 patients admitted with acute or chronic liver failure during the studied period. 5 of these were excluded from the final analysis, 4 due to documented administration of phosphate supplementation prior to ITU admission and blood sampling, and 1 whose phosphate level was not recorded. Survival rates were 16.0% (4 of 25) in patients with high admission phosphate, 63.6% (21 of 33) in patients with normal admission phosphate, and 78.5% (11 of 14) in patients with low admission phosphate. Chi-squared analysis showed statistical significance with X^2(2.76) =18.586 and p<0.001.
Conclusions: Hyperphosphatemia is associated with a poor survival outcome for patients admitted to intensive care with liver failure and hypophosphatemia is associated with improved survival outcomes. Further larger prospective studies are recommended to validate these findings.
References
1. MacQuillan, G.C., Seyam, M.S., Nightingale, P., Neuberger, J.M. and Murphy, N. (2005), Blood lactate but not serum phosphate levels can predict patient outcome in fulminant hepatic failure. Liver Transpl, 11: 1073-1079. https://doi.org/10.1002/lt.20427
2. Baquerizo A, Anselmo D, Shackleton C, Chen TW, Cao C, Weaver M, Gornbein J, Geevarghese S, Nissen N, Farmer D, Demetriou A, Busuttil RW. Phosphorus ans an early predictive factor in patients with acute liver failure. Transplantation. 2003;75(12):2007-2014. doi: 10.1097/01.TP.0000063219.21313.32. PMID: 12829902.
3. Schmidt, L.E. and Dalhoff, K. (2002), Serum phosphate is an early predictor of outcome in severe acetaminophen-induced hepatotoxicity. Hepatology, 36: 659-665. https://doi.org/10.1053/jhep.2002.35069
4. Chung, P.Y., Sitrin, M.D. and Te, H.S. (2003), Serum phosphorus levels predict clinical outcome in fulminant hepatic failure. Liver Transpl, 9: 248-253. https://doi.org/10.1053/jlts.2003.50053
5. de Sausmarez E, Crowest P, Fry S, Hodgson L. Predicting outcome in liver patients admitted to intensive care: A dual-centre non-specialist hospital external validation of the Liver injury and Failure evaluation score. J Intensive Care Soc. 2021;22(2):152-158. doi: 10.1177/1751143720924352. Epub 2020 May 8. PMID: 34025755; PMCID: PMC8120575.
P122
Rationalising glycaemic control in critically ill patients during the Sars–CoV-2 pandemic
Metabolism and endocrinology
Guy Coady 1 , Radha Sundaram1, Rebecca Haggerty1, Chris Smith1, Prash Kumar2 and Kenan Bastekin1
1NHS Greater Glasgow & Clyde
2NHS Ayrshire & Arran
Abstract
Introduction: Poor glycaemic control is associated with worse outcomes in critically ill patients.1,2 A blood glucose target of 6-10 mmol/L was suggested by the NICE-SUGAR trial. In the context of hyperglycaemia, this target is achieved utilising variable rate insulin infusions (VRIIs). Furthermore, there is increasing evidence that critically ill patients with SARS –CoV -2 infection suffer more complications if they are diabetic or have altered glycaemic control.3 Through a series of Plan-Do-Study-Act (PDSA) cycles, we attempted to improve the glycaemic management of critically ill patients in our Intensive Care Unit (ICU) over the last twelve months.
Objectives: Through a retrospective multi-cycle audit and QI project we sought to:
1. Identify our diabetic patient demographics
2. Understand our current practices around use of VRIIs and rationalising of glycaemic management upon discharge from ICU
3. Improve documentation of glycaemic management plan upon discharge.
4. Actively collaborate with the Endocrinology team to produce local guidance.
Methods: The RAH is a 7 bedded Level 3 ICU which admitted 324 patients between August 2020 and August 2021.
All ICU survivors with a length of stay >24 hours were included.
Data was collected retrospectively at the end of each cycle via ICCA Carevue between September 2020 and August 2021 in three cycles. Cycle 1 September 2020-December 2020, Cycle 2 January 2021-May 2021 and Cycle 3 June 2021-Ongoing.
Intervention 1 (post cycle 1): Presentation of baseline data to department
Intervention 2 (post cycle 2): Addition of “Glycaemic Management plan” to ICU discharge form on ICCA Carevue
Intervention 3 (mid cycle 3) Creation of “Guidance on Glycaemic Management at discharge from RAH ICU” departmental guide created
Results:
Cycle 1 results: 56 eligible patients 14 of which were diabetic. 12 of these diabetic patients were discharged on a VRII. Three patients (25%) had a documented glycaemic management plan upon discharge.
Cycle 2 results: 60 eligible patients, 17 were diabetic. 11 of these diabetic patients were discharged on VRII. Six patients (54.5%) had a documented glycaemic management plan upon discharge.
Cycle 3 results: eligible patients, 11 were diabetic. 9 of these diabetic patients were discharged on a VRII. Eight patients (88.8%) had a documented glycaemic management plan upon discharge.
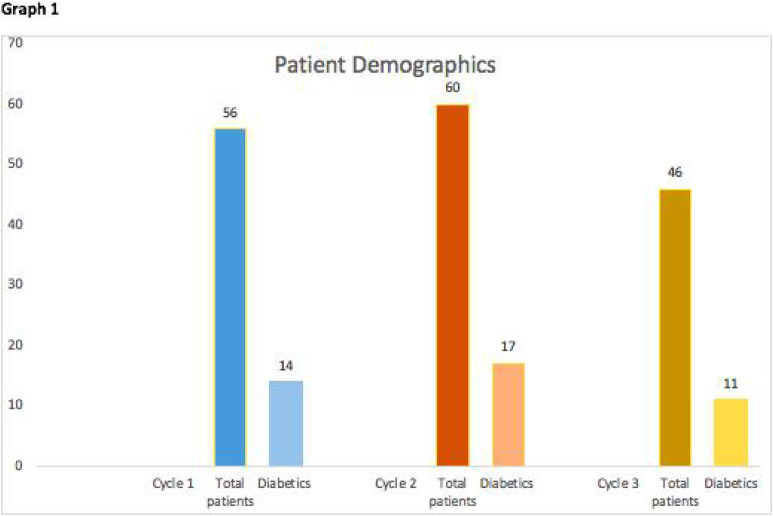
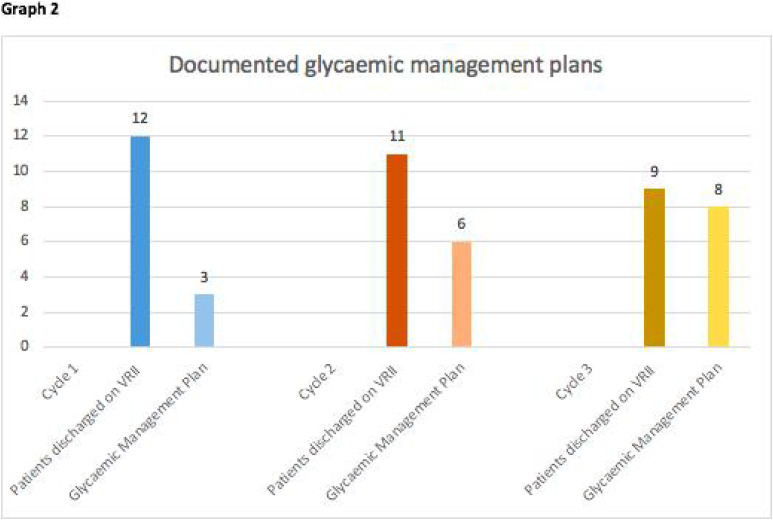
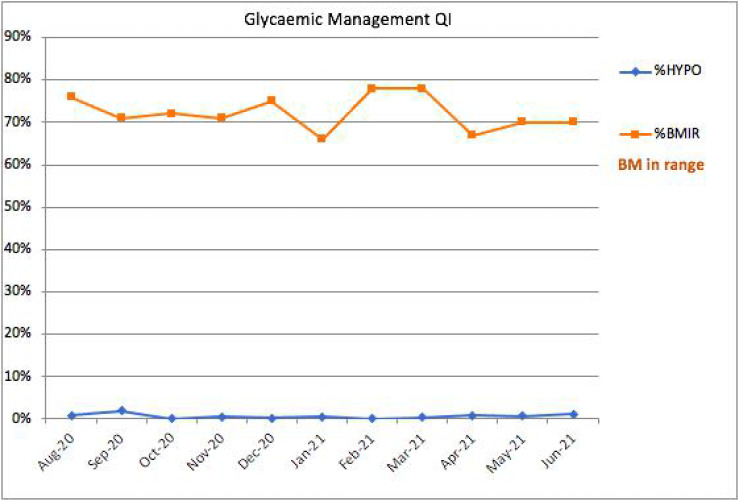
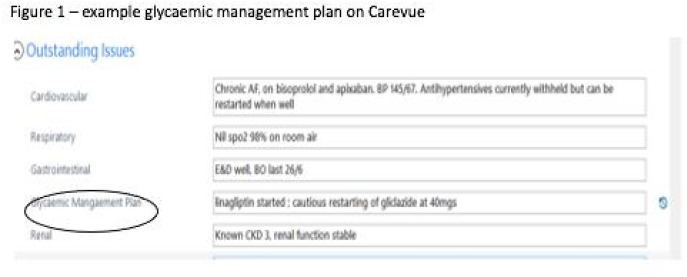
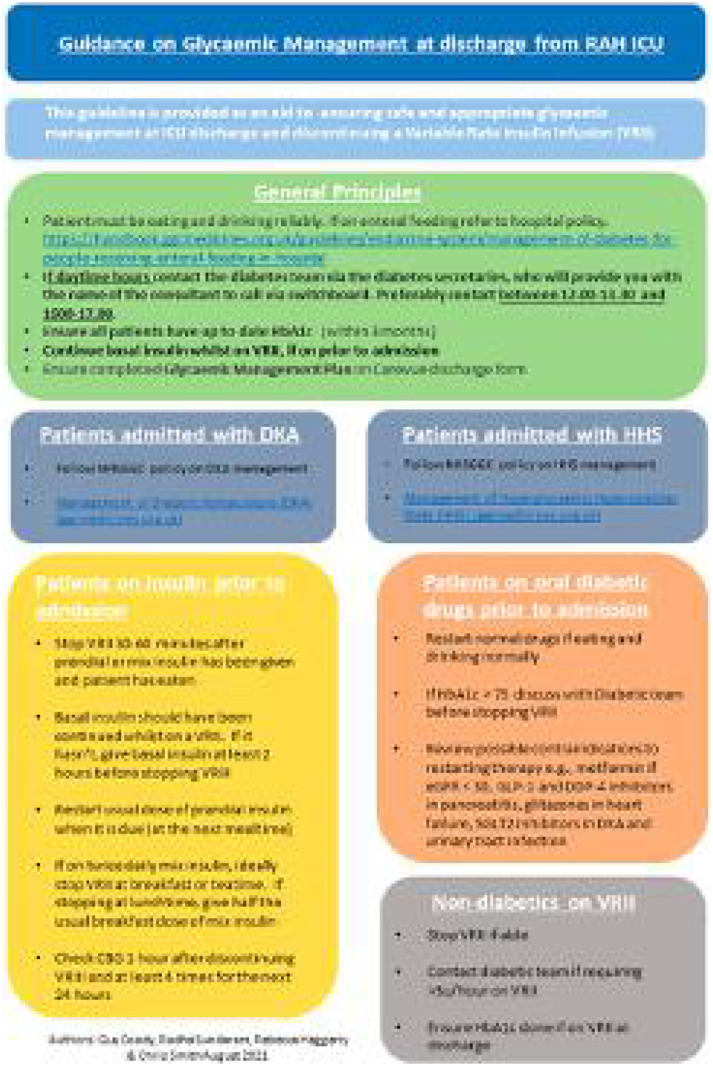
Conclusion: Using PDSA cycles and Quality Improvement methodology, we have demonstrably improved the percentage of diabetic ICU patients with documented glycaemic management plans upon discharge. We have also encouraged formulation of a clear glycaemic plan and involvement of the endocrinology team upon discharge ensuring opportunities are not missed to reduce downstream VRII use where possible. The above guidance document has been a collaborative process between ICM and Endocrinology ensuring that support is available for doctors in ICU.
Randomised control studies such as SWEET-AS have highlighted the long-term impact of diabetes in ICU survivors.4 Our QI work confirms that it is important to understand the needs of the local population and ensure robust guidance is in place when optimising patient’s glycaemic control safely.
References
1. Bode et al. Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States. J Diabetes Sci Technol. 2020; 14: 813-821
2. Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc 2003;78:1471–1478.
3. Falciglia M, et al. Hyperglycemia-related mortality in critically ill patients varies with admission diagnosis. Crit Care Med 2009;37:3001–3009
4. Ali Abdelhamid Y, Phillips LK, White MG, Presneill J, Horowitz M, Deane AM. Survivors of Intensive Care With Type 2 Diabetes and the Effect of Shared-Care Follow-Up Clinics: The SWEET-AS Randomized Controlled Pilot Study. Chest. 2021;159(1):174-185. doi: 10.1016/j.chest.2020.08.011. Epub 2020 Aug 12. PMID: 32800818.
P123
Nutrition Strategies in Acute Spinal Cord Injury - A Narrative Review
Neurointensive care
Alex Gordon 1 and Jessie Welbourne2
1Torbay and South Devon NHS Foundation Trust
2University Hospitals Plymouth NHS Trust
Abstract
Introduction: Spinal cord injury is a condition with a high burden of morbidity and mortality that afflicts a large proportion of young patients. Our intensive care unit had a policy of withholding feeding for 48 hours in the acute phase of injury due to the risk of ileus. Due to the disparity between this approach and the potential hypermetabolic state observed in other critically ill patients, we reviewed the evidence which underlies this practice.
Objectives: To review the evidence base for withholding enteral nutrition in patients with spinal cord injury, and to establish optimal feeding regimen for acute SCI patients with respect to time to enteral feeding and calorie input.
Methods: We conducted a narrative review. We searched the MEDLINE, EMBASE, and Cochrane CENTRAL databases for studies which looked at feeding protocols in the acute phase of spinal cord injuries which measured time as a parameter of these protocols. For inclusion, the population had to be patients in a critical care or acute spinal rehab setting. Outcomes required for inclusion were neurological improvement, neurological complications, time spent on intensive care units, time to ICU discharge, incidence of secondary complications (particularly respiratory or gastrointestinal), other adverse effects, and mortality. Title and abstract screening were undertaken of the 539 articles retrieved by the search strategy, followed by full-text review of 75 articles. Risk of bias was assessed using the Downs and Black checklist.1
Results: Four studies met our inclusion criteria.2-5 There were two pre-post quasi-experimental designs, one randomised controlled trial, and one retrospective observational study. Across studies there was no conclusive evidence of inferiority with earlier feeding (as early as before 24 hours post-injury) compared to delayed enteral feeding. One study demonstrated that patients fed before 24 hours in conjunction with a broader bundle of care had improved neurological outcomes compared to previous non-standardised practice up to a year post-discharge from ICU. Delaying enteral nutrition was shown by one study to lead to longer time to meet pre-determined nutritional targets.
Conclusion: There is little evidence to suggest that delaying enteral feeding is beneficial compared to initiating feeding in the first 24-48 hours following SCI. Delaying feeding may lead to delayed ability to meet nutritional targets and therefore complications associated with malnutrition. There is however little evidence at present of optimal feeding strategy, and further research is required on how one can titrate nutritional requirements to individual patient need.
References
1. Downs SH and Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health 1998; 52: 377-384.
2. Cinotti R, Demeure-Dit-Latte D, Mahe PJ, et al. Impact of a Quality Improvement Program on the Neurological Outcome of Patients with Traumatic Spinal Cord Injury: A Before-After Mono-Centric Study. J Neurotrauma 2019; 36: 3338-3346.
3. Dvorak MF, Noonan VK, Belanger L, et al. Early versus late enteral feeding in patients with acute cervical spinal cord injury: a pilot study. Spine 2004; 29: E175-180.
4. Kuric J, Lucas CE, Ledgerwood AM, et al. Nutritional support: A prophylaxis against stress bleeding after spinal cord injury. Paraplegia 1989; 27: 140-145.
5. Rowan CJ, Gillanders LK, Paice RL, et al. Is early enteral feeding safe in patients who have suffered spinal cord injury? Injury 2004; 35: 238-242.
P124
Neuromuscular sweet syndrome: Intermittent relapsing and remitting inflammatory neuromuscular syndrome
Neurointensive care
Faryal Zaman and Catriona Shaw
Kings College Hospital London - London
Abstract
Background: Sweet disease, also known as acute febrile neutrophilic dermatosis, is a multisystem inflammatory disorder characterized by painful erythematous plaques and aseptic neutrophilic infiltration of various organs. Skin biopsies typically demonstrate dermal infiltration with neutrophils in the absence of vasculitis. Sweet disease responds to systemic corticosteroids.
Sweet disease is primarily a disease of skin, though multiple organs systems can be involved in sweet syndrome including nervous system, muscles, heart, eyes, hematological diseases.
The etiology of sweet syndrome is unknown, although the possible role of an abnormally increased chemotaxis of the neutrophils has been suggested. Cytokines, including granulocyte colony-stimulating factor and IL-6 and antineutrophil cytoplasmic antibody have been implicated in the pathogenesis of sweet syndrome. Granulocyte colony-stimulating factor therapy for granulopenia is known to induce sweet syndrome.2
There are multiple triggers including infections and drugs. In our case the possible trigger was syphilis in past and the organ systems involved in its complications were mainly neuromuscular and hematological.
Case Presentation: This is a case report of a 65-year-old lady who presented with weakness of her left arm and leg with raised Creatinine Kinase and Acute renal injury requiring renal replacement therapy. She had history of undiagnosed intermittent relapsing and remitting neuroinflammatory disorder on the background of Myelodysplastic syndrome, neutrophilic dermatosis (sweet disease), syphilis. She had brain scans which did not show any change from previous scans.
While in patient, she developed seizures followed by high Lactate, creatinine kinase and Aspartate aminotransferases, Type 2 Respiratory failure with persistently low GCS and got intubated.
In Intensive care unit she was given steroids in view of possible sweet syndrome causing neurological, skin and muscle involvement presenting as weakness, Seizures, raised AST, CK and consequently AKI.
After steroids she showed remarkable improvement and then later extubated and shifted to ward.
Discussion and conclusion: Sweet syndrome is a rare syndrome and is the great mimicker. Although still a lot to be explored about this syndrome, intermittent, relapsing/ remitting nature, neutrophilic inflammatory infiltrates primarily dermal and resolution with steroids is pathognomic.
This case the presented with seizures, right sided weakness associated with rhabdomyolysis leadin to AKI requiring renal replacement therapy. Low Glasgow Coma Score and type 2 Respiratory failure postictally on the background of decade long history of relapsing remitting steroid responsive neuroinflammatory disorder led to Intensive care admission. All above mentioned features and biopsy proven neutrophilic dermatosis (skin rash) and Myelodysplastic syndrome comprise parts of sweet syndrome (which encompass multiple organ system including neurological involvement, hematological involvement; with leukemias and Myelodysplastic syndrome (as in our patient), primarily skin involvement and associated with syphilis trigger). In terms of muscle involvement with raised Creatinine Kinase and Aspartate aminotransferases in our case, there have rarely been case reports of neutrophilic myositis with bullous sweet syndrome.3 Corticosteroids remain mainstay of treatment in patient with sweet syndrome. We feel in our case having obtained a muscle biopsy (affected organ) to exclude other causes of raised CK and AST including drugs would have consolidated our suspicion of muscle involvement in sweet syndrome although there was no recent change in drug history or any other possible explanation besides sweet syndrome.
References
1. Hisanaga K, Iwasaki Y, Itoyama Y, Neuro-Sweet Disease Study Group. Neuro-Sweet disease: clinical manifestations and criteria for diagnosis. Neurology. 2005;64(10):1756–1761
2. Hisanaga K, Hosokawa M, Sato N, Mochizuki H, Itoyama Y, Iwasaki Y. “Neuro-sweet disease”: benign recurrent encephalitis with neutrophilic dermatosis. Arch Neurol. 1999;56(8):1010–1013.
3. Sato K, Miura T, Ohtsuka M, Yamamoto T. Bullous Sweet’s syndrome with myositis. Actas Dermosifiliogr. 2018;109(3):284–285.
P125
Anaemia After Subarachnoid Haemorrhage Predicts Higher Mortality and Morbidity
Neurointensive care
Priyavarshini Ramesh 1 and Tonny Veenith2
1University of Birmingham
2Queen Elizabeth Hospital
Abstract
Introduction and Purpose: Subarachnoid haemorrhage (SAH) results in patient morbidity and mortality. The neurocritical care management goal is to facilitate neuroprotection and prevent secondary neurological insults. Literature suggests there is coexistent anaemia in 50% of SAH patients but is inconclusive on the thresholds of blood transfusion in anaemia. Brain injury models suggest there is diffusion cerebral hypoxia in the absence of classic hypoxia, with endothelial dysfunction and perivascular oedema. This supports the belief that low haemoglobin (Hb) after SAH leads to reduced cerebral oxygen delivery and consequently, poor outcomes. The aim of this study was to investigate mortality and morbidity outcomes associated with anaemia after subarachnoid haemorrhage
Methods: We performed a retrospective study of eight hundred and seventy patients with SAH at the Queen Elizabeth Hospital, Birmingham, between January 2016 and August 2019. Data were collected on baseline characteristics, World Federation of Neurosurgical Societies SAH grade, secondary insults such as the occurrence of hypoxia, anaemia and hydrocephalus, and units of blood transfused. The primary outcome was 28-day Modified Rankin Scale score. Secondary outcomes were delayed neurological deficits, length of stay and death in intensive care unit (ICU). Anaemia was defined as Hb ≤9.5g/dL, and severe anaemia as Hb≤8g/dL.
Results: 28.7% (n=250) of patients had anaemia, and 12% had (n=104) severe anaemia. The incidence of anaemia after SAH was associated with increased risk of death or severe disability (p<0.001). It was also associated with worse survival outcomes (p<0.001) and increased length of stay in ICU (p<0.001).
Conclusions: Anaemia is a recognised complication after SAH and is associated with a significant increase in risk of death and severe disability. These results indicate that haemoglobin in patients with SAH should be monitored closely and corrected (if Hb<9.5g/dl) and can guide further study into the causative effect between anaemia and increased mortality and morbidity.
P126
Bridling at the use of nasal bridles? An observational study of their use at Royal Surrey Hospital Intensive Care Unit during the COVID-19 pandemic
Nutrition
Alice Extance, Jessica Zekavica and Michelle Bossy
Royal Surrey Hospital
Abstract
Introduction: Sufficient nutrition has been repeatedly demonstrated to be a vital part of recovery from critical illness.1 Nutrition is often delivered in the intensive care setting via a Nasoenteral (NE) tube if oral diet is impractical or inadequate; this is first line as per ESPEN guidance.2 It has been observed that patients in the intensive care unit (ICU), particularly those who have been intubated due to COVID-19, are at high risk of agitation and delirium which can lead to accidental NE displacement. Nasal Loop Bridles (NLB) are a medical device which can be placed at bedside and are used to reduce the risk of NE tube displacement. The usage of NLBs varies between Trusts. Insertion of a NLB is a medical procedure which should be consented for where possible and clearly documented.
Objectives: To identify all patients who had a NLB placed during the second wave of the COVID-19 pandemic at Royal Surrey Hospital (RSH) ICU, ascertain their reason for insertion, and identify any nutritional deficits incurred prior to NLB insertion. Secondary objectives include assessing quality of documentation of NLB insertion.
Methods: A literature review was undertaken regarding the safety and efficacy of NLBs. This was followed by a retrospective observation of patients admitted to RSH ICU between December 2020 and March 2021. Data was collected on patients who required a NLB, including accrued nutritional deficit prior to placement and adverse incidents. Documentation of NLB rationale and placement was also noted.
Results: 10 patients met inclusion criteria. The most common indications for insertion were delirium and previous tube displacement. Two NLBs were placed prior to any NE displacements therefore resulted in no nutritional losses. In the remaining patients a range of 1-5 NE tubes were accidentally displaced prior to NLB insertion (mean 2.7 tubes). 6-117 hours of feeding were lost prior to NLB placement resulting in a deficit of 744-6843kcal. Two patients were unable to have a NLB when indicated due to stock shortages, resulting in a deficit of 4140 and 6480kcal. No standard documentation was utilised for NLB placement. No major incidents occurred in relation to NLBs.
Conclusion: This study highlights the benefits of NLBs in respect to nutritional delivery in patients who have undergone emergency sedation and ventilation and are at risk of delirium. It has also highlighted the need for improved documentation of this medical procedure. Inferences made from this study, and work by other centres identified in the literature review, suggest that it may be beneficial to consider early or prophylactic NLB placement in this cohort. Further local research could test criteria for use of NLBs including hyperactive delirium, difficulty of initial NE tube insertion and number of previous displaced tubes, in order to elucidate the most effective timing and indication for their use.
References
1. Villet S, Chiolero RL, Bollmann MD, et al. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr 2005; 24:502-509.
2. Singer P, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr 2019: 38: 48-79.
P127
Enteral feed delivery in patients with COVID-19 admitted to a Nightingale intensive care unit (ICU)
Nutrition
Laura McNeill 1 , Andrea Cox1, Karen Robinson1, Niamh Collins1 and Joy Ballance2
1Belfast Health and Social Care Trust
2Belfast Health and Social Care Trust
Abstract
Introduction: Optimal calorie delivery is around 80% of predicted energy requirements.1 Underfeeding critical care patients may cause harm in some long stay patients.2 ESPEN guidelines state if oral intake is not possible, enteral nutrition should commence within 48 hours. Calorie delivery can be increased to 80-100% after day three of admission to ICU.3
The Nightingale ICU was situated on an acute ward which was modified to function as an ICU. This was to facilitate increased admissions of COVID-19. The Nightingale dietetic team were redeployed from acute and community settings in from within the trust, with various levels of ICU experience. The team provided seven day dietetic cover based on a rota, including bank holidays.
Objectives: The aim of this audit was to evaluate enteral feed delivery and the number of days taken to reach target rate of feed compared to the regimen set by the dietitian, in patients with COVID-19 admitted to Nightingale ICU.
Methods: At each review, dietitians calculated enteral feed delivery over the preceding 24 hours as a percentage of the target regimen, from the input recorded on the fluid balance chart. The number of days to reach enteral feed delivery targets were calculated relative to dietetic plans.
All patients who required enteral nutrition from 15/10/2020 until 11/03/2021 were eligible for inclusion. Days where enteral feed was not required, target rate of enteral feed was not yet due to be achieved, parenteral nutrition was required, or following ICU discharge and end of life care were excluded. Days where enteral nutrition delivery information was unavailable were also excluded from the analysis. No imputation was used to estimate missing data.
Results: The data consisted of a total of 116 patients. Following exclusions, the total number of patients included in the analysis was 107. Mean age was 63.6 ± 9.4 years. Mean body mass index (BMI) was 32.7 ± 7.4kg/m2. Number of enteral feed days per patient was 11.
Patients with COVID-19 admitted to Nightingale ICU received a median of 84% of their enteral feeding regimen. The feeding regimen set by the dietitian aimed to achieve target rate of feed by 3.1 days. The data analysis showed the mean number of days until the target was achieved was 3.5 days.
Conclusion: Results are based on a homogenous COVID-19 ICU cohort. Dietetic staffing levels were increased, and seven-day working was provided in response to the COVID-19 pandemic compared to a standard ICU. Quantifying common reasons for feed interruptions could be explored further.
Despite suboptimal COVID-19 Nightingale ICU conditions, enteral feed delivery and time taken to reach target rate of feed was in keeping with ESPEN guidelines.
References
1. Heyland DK, Cahill N, Day AG. (2011) Optimal amount of calories for critically ill patients: depends on how you slice the cake. Crit Care Med 39, 2619-2626.
2. Wei X, Day AG, Ouellette-Kuntz H, et al. (2015) The Association Between Nutritional Adequacy and Long-Term Outcomes in Critically Ill Patients Requiring Prolonged Mechanical Ventilation: A Multicenter Cohort Study. Crit Care Med 43(8), 1569-1579
3. Singer P, Reintam Blaser A, Berger MM, et al. (2019) ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr (38), 48-79.
P128
The rise in urea-to-creatinine ratio, a marker of catabolism, is mitigated by administration of intermittent rather than continuous feeding in critical illness
Nutrition
Luke Flower 1 , Ryan Haines2, Angela McNelly2, Bear Danielle3, Kiran Koelfat4, Steven Olde Daminik5, Nicholas Hart6, Hugh Montgomery7, John Prowle2 and Zudin Puthucheary2
1William Harvey Research Institute, Barts and The London School of Medicine and Dentistry, Queen Mary University of London
2William Harvey Research Institute, Queen Mary University of London
3Department of Nutrition and Dietetics, Guy’s and St Thomas’ NHS Foundation Trust
4Maastricht University, Maastricht, Netherlands
5Department of Surgery, Maastricht University Medical Center, Netherlands
6Guy’s and St Thomas’ NHS Foundation Trust
7University College London
Abstract
Introduction: Rapid muscle loss affects more than 50% of critically ill patients and is associated with significant morbidity and mortality.1 It results from an imbalance between muscle protein synthesis and breakdown. To date, no single intervention has offered effective mitigation.2 Intermittent (as opposed to continous) feeding has been hypothesised to offer benefit, by delivering peaks in essential amino acid concentration, and altered ghrelin, insulin and YY peptide concentrations - all potential anabolic stimuli.3 The ratio of serum urea:creatinine concentration (urea-to-creatinine ratio, UCR: mmol/mmol and thus unitless) is a biomarker of muscle wasting, and rises with catabolism.4
Objective: We sought to assess whether UCR was reduced in those intermittently fed when compared to those continously fed.
Methods: We reanalysed data from a multicentre, controlled trial of critically ill adult patients randomised 1:1 to intermittent or continous nasogastric enteral feeding. All were anticiapted to be mechanically ventilated for >48 hours.
Alongside raw data analysis, we developed a linear mixed effects model to assess the difference in UCR trajectory between feeding groups. K-means clustering anaysis of UCR trajectory was also performed using an unsupervised machine learning technique to investigate metabolic phenotypes. The primary outcome measure was change in UCR from day 0 to the last measure in the 10-day study period.
Results: Overall, 121 patients were included in the original study (62 vs 59 in the intermittent and continuous feed groups, respectively). The median change in UCR was lower in the intermittent than continuous feed group (20.12 [IQR -6.13 – 73.7] vs 36.39 IQR [15.16 – 93.10]: p = 0.05). The linear mixed effects model demonstrated a flatter UCR trajectory in the intermittent than continuous feed group (coefficient -0.245, p = 0.002). This was further supported by the k-means analysis, splitting patients into three separate clusters (A, B, and C) depending on their UCR trajectory and baseline (figure 1). Cluster C had the highest proportion of continuously fed patients (70%) and demonstrated the steepest rise in UCR. Cluster A demonstrated a flatter UCR trajectory, with 60% of patients in the intermittent feeding group. Cluster B demonstrated the flattest trajectory, with most patients (62%) receiving intermittent feed and 70% receiving renal replacement therapy - a cofactor adjusted for in the linear mixed effects model.
Conclusion: Intermittent feeding mitigates the increase in urea-to-creatine ratio seen in critical illness with continuous feeding. This may reflect a reduction in muscle catabolism.
References
1. Puthucheary ZA, Rawal J, McPhail M, et al. Acute skeletal muscle wasting in critical illness [published correction appears in JAMA. 2014;311(6):625. Padhke, Rahul [corrected to Phadke, Rahul]]. JAMA. 2013;310(15):1591-1600. doi:10.1001/jama.2013.278481
2. Flower L, Puthucheary Z. Muscle wasting in the critically ill patient: how to minimise subsequent disability. Br J Hosp Med (Lond). 2020;81(4):1-9. doi:10.12968/hmed.2020.0045
3. McNelly AS, Bear DE, Connolly BA, et al. Effect of Intermittent or Continuous Feed on Muscle Wasting in Critical Illness: A Phase 2 Clinical Trial. Chest. 2020;158(1):183-194. doi:10.1016/j.chest.2020.03.045
4. Haines RW, Zolfaghari P, Wan Y, Pearse RM, Puthucheary Z, Prowle JR. Elevated urea-to-creatinine ratio provides a biochemical signature of muscle catabolism and persistent critical illness after major trauma. Intensive Care Med. 2019;45(12):1718-1731. doi:10.1007/s00134-019-05760-5
P129
A review of Vitamin D testing and replacement in the Intensive Care Unit
Nutrition
Heather Javaid 1 and Alexander Kirk-Patrick2
1Cwm Taf Mogannwg University Health Board
2Gloucestershire Hospitals NHS Foundation Trust
Abstract
Introduction: Critically ill patients deficient in Vitamin D have been shown to have poorer outcomes in observational studies. These include longer length of stay, ventilation time, a higher incidence of sepsis and excess mortality.1-3 The European Society for Clinical Nutrition and Metabolism (ESPEN) set out two recommendations on vitamin D testing in the intensive care unit (ICU)4. These include measuring vitamin D levels and supplementing with vitamin D3 if below 50nmol/L. If below this and tested within the first week of admission a single loading dose is recommended. Our local guidelines also recommend supplementation dependent on vitamin D levels and risk factors.
Objectives: Our objectives were to assess how many ICU patients in a one-year period (2020) were tested for vitamin D levels and on which day of admission they were tested. In addition to this our aim was to see if treatment of Vitamin D deficiency/insufficiency was in line with ESPEN and local guidelines.
Methods: Using the Integrated Clinical Environment (ICE) programme we identified all patients who were tested for vitamin D on ICU during 2020. We then used Intensive Care National Audit and Research Centre (ICNARC) data to identify admission and discharge dates. Using ICE discharge summaries and Electronic Document Management System (EDMS) notes we established those that were prescribed replacement and whether this occurred on the ICU or on the ward after discharge. In accordance with local and NICE5 guidelines those with vitamin D levels under 25nmol/L were deemed deficient and those between 25-50nmol/L were deemed insufficient.
Results: In total 59 patients were tested for Vitamin D levels, with 31 defined as insufficient and 16 defined as deficient. There was a wide range of days on which patients were testing from Day 0 of admission to day 88. The mean day of testing was day 15.
For those patients that had deficient levels 5 cases out of 16 were treated on the ICU. 2 of these were prescribed treatment in line with our local guidelines. 3 were prescribed Vitamin D supplementation but not the correct medication outlined in our guidelines.
For those with insufficient levels on 6 were treated were treated in ICU, 2 with the correct supplementation. Of note 21 patients did not receive any treatment whilst in hospital.
Conclusions: Our small review showed that in our critical care unit there was a wide variability of practice in the day of testing and treatment of both deficient and insufficient patients. Our local guidelines use different cut off definitions as compared to the ESPEN guidelines; however, both share similar principles. It is currently unclear who we should test, when we should test them and how we should treat those with deficiency or insufficiency. The VITdAL-ICU trial showed in their secondary outcome that severe vitamin D deficiency had a lower hospital mortality and from this the VITDALIZE study was prompted. This trial is currently recruiting and hopefully will provide further evidence on vitamin D replacement in critically ill patients.
References
1. Amrein K, Schnedl C, Holl A, Riedl R, Christopher KB, Pachler C, et al. Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial. JAMA 2014;312(15): 20-30.
2. Putzu A, Belletti A, Cassina T, Clivio S, Monti G, Zangrillo A, et al. Vitamin D and outcomes in adult critically ill patients. A systematic review and metaanalysis of randomized trials. J Crit Care 2017;38:109-14.
3. Nair P, Venkatesh B, Centre JR. Vitamin D deficiency and supplementation in critical illness – the known knowns and known unknowns. Critical Care. 2018;22(1):276.
4. Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN Guidelines on Clinical Nutrition in the Intensive Care Unit. Clinical Nutrition 2019; 38: 48-79
5. National Institute for Health and Care Excellence, Clinical Knowledge Summaries. Vitamin D Deficiency in Adults. Available from: https://cks.nice.org.uk/topics/vitamin-d-deficiency-in-adults/
P130
Evaluation of energy and protein delivery compared to targets on day four of critical care in mechanically ventilated adults
Nutrition
Rodney Hall
Blackpool Victoria Hospital - Blackpool, Lancashire
Introduction: The adequacy of enteral nutrition provided to critically ill patients has been highlighted as inadequate. International surveys have shown that actual nutrition delivered is as little as 50-60% of that prescribed. Furthermore, studies looking at feeding patients to target show significant improvements in patient outcomes. Common barriers to the provision of nutrition targets are starting nutrition support late, the presence and/or compliance with a feeding protocols, GI intolerance and its management, fasting practices for bedside procedures and feed stoppages for off the unit procedures/investigations. Closing the gap between nutrition prescription and nutrition delivery can make significant improvements to patient outcomes.
Objective: This study looked at the nutrition adequacy of a prospective cohort of adult general ICU patients. The aim of which was to identify how well the unit performs with nutritional adequacy and to identify any potential areas of feeding practices that would benefit from modification.
Methods: Data was collected prospectively upon daily review by the Dietitian. Information collected included the time to start feeding, volumes delivered of enteral feeds as well as non-nutritional calories and any documented reasons for feed stoppages and/or gaps in feed delivery. Day one was taken as the first full 24hour period on the unit. Targets for day four were set at 80% of 20Kcal and 1.3g protein per Kg of body weight. Where BMI was >30Kg/m2, a 25% adjusted body weight was used with an ideal weight set from BMI 25Kg/m2. Results are presented as the mean percentage targets achieved.
Results: From May to August 2021 data was collected for a total of 28 patients. The average length of stay was 9.3 days. The percentage of obesity in the group was 42%. 100% of patients started enteral nutrition within 48 hours of admission or intubation. Analysis shows that only 40% (11 patients) achieved their energy target and only 21% (6 patients) achieved their protein target on day four. The average feeding hours lost were 4 to 9 hours between days 1 and 4. The main reason for the lost hours was the interpretation of gastric volumes which was documented as high in 60% of the patients.
Conclusions: The study mirrors the findings from international surveys on adequacy highlighting the importance of feeding protocols to assist optimal nutrition delivery in this early phase. There is no Dietetic service at weekends and bank holidays so personalised nutritional targets are not always set by a Dietitian from day one. The unit is good at commencing feeding early however the feed used has a low protein:energy ratio which is reflected in the protein target achievement. Furthermore, lack of consistency in GI intolerance management is reflected in the increased number of non-feeding hours and overall, under achievement of nutritional targets. The results highlight the need for a structured feeding protocol.
References
1. Heyland DK. The prevalence of iatrogenic underfeeding in the nutritionally ‘at risk’ critically ill patient: Results of an International, Multicentre, prospective study. Clin Nutr 2015; 34(4):659-666
2. Fetterplace K, et al. Targeted Full Energy and Protein Delivery in Critically Ill Patients: A Pilot Randomized Controlled Trial (FEED Trial). JPEN 2018; 00:1-11
P131
Critical care dietetic outcomes during the first wave of the COVID-19 pandemic
Nutrition
Rebeca Prichard, Steven Evans and Amelia Jukes
University Hospital of Wales, Cardiff and Vale University Health Board
Abstract
Introduction: The COVID-19 pandemic led to a surge in patients being admitted to the Intensive Care Unit (ICU) and increased dietetic input was required. To meet this demand, non-ICU dietitians were upskilled and service changed from 5 to 7-days.
Objectives: To analyse changes in nutritional outcomes during the COVID-19 pandemic, and how changes to the dietetic service impacted upon dietetic outcomes.
Methods: Data was collected for all ICU patients under dietetic care with COVID-19 between 22/03/2020 and 04/06/2020. Total patient cohort equalled 66. Data was collected until patients were discharged or passed away. All data was analysed using descriptive statistics, and an independent t-test was used to compare COVID-19 feed delivery to previous feed delivery data. Ethical approval was not required.
Results: Of the 66 patients, 62 required enteral nutrition (EN). Feeding was commenced within 48 hours of ICU admission in 92% of patients. Average percentage feed delivery was 82.4% for energy and protein. A total of 60% of patients were initially started on a fluid restricted feed for fluid balance or due to being proned. A total of 50% of patients continued with a fluid restricted feed, 44% received a protocol 1kcal/ml high-protein feed and 6% a peptide or renal feed. Prokinetics were required in 35% of patients. A total of 3% of patients required parenteral nutrition. Of the 70% discharged from ICU alive, 70% were receiving EN at the time of discharge.
Conclusion: A number of barriers to maintaining high standards of patient outcomes arose at the onset of the COVID-19 pandemic. These included disruptions to MDT working, challenges in undertaking face-to-face assessments and an increased caseload and footfall - thereby increasing the demand for ICU trained Dietitians. Despite these barriers, this service evaluation demonstrates that percentage feed delivery remained relatively stable when compared to the pre-COVID 2020 audit (n = 35). An independent-samples t-test showed there was no significant difference in the scores for pre-COVID (M = 85%, SD = 13.4) and COVID (M = 82.4%, SD = 16.8) samples; t (180) = -0.81, p = .42. This is despite 36% of patients requiring proning during COVID vs. 0% pre-COVID, and increased gastrointestinal intolerance evidenced by 35% of patients requiring prokinetics vs. 29% pre-COVID. These factors eliminated the ability to utilise ‘catch-up’ feeding, which in normal circumstances optimises feed delivery. This suggests that changes in dietetic provision, allowed more prompt management of nutritional issues and facilitated the maintenance of the pre-existing high standards of nutritional care. Achieving this degree of feed delivery necessitated adapting feeding regimens to best meet the patient needs and in the absence of dietetic input it is unlikely these feeding strategies would have been utilised.
The COVID-19 pandemic presented challenges to every aspect of the healthcare sector; and reinforced the importance of multidisciplinary teams guiding patient care in the absence of evidence-based guidelines. This service evaluation demonstrates that forward-planning can assure that patient care need not be compromised.
P132
Meeting nutritional requirements in critically-ill patients with COVID-19: Does the patient’s position really matter?
Nutrition
Dawn Lukk and Carolyn May
Royal Papworth Hospital NHS Foundation Trust
Abstract
Introduction: Prone positioning and veno-venous extracorporeal membrane oxygenation
(VV-ECMO) can improve oxygenation in patients with COVID 19-induced acute respiratory distress syndrome (ARDS).1 Enteral feeding in the prone position has challenges, including possible aspiration risk of gastric contents and potential for disruption to enteral feeding.2
National guidelines2 were implemented locally; including a reduction in the maximum acceptable gastric residual volume (GRV) and the avoidance of bolus feeding while patients were in prone position.
Objectives:
• To explore the nutritional adequacy of patients in the prone position with COVID-19 on our critical care unit during the second surge (November 2020-April 2021)
• To compare nutritional adequacy of days when patients were in prone versus supine position
• To identify any factors that impacted on nutritional adequacy
• To provide recommendations for improvement
Methods: Patients with COVID-19 who required intubation, were placed in prone position at any time during their admission and had been assessed by the dietitian, were included.
Total daily energy and protein intakes, from enteral (EN) and parenteral nutrition (PN), propofol and intravenous glucose were obtained from our computerised information system (Metavision) for each full day. If nutritional aims were not met then reasons for this were investigated.
Nutritional adequacy was defined as ≥ 80% of energy and protein received per day.3
Results: Data for 34 patients was collected (see Table 1). A total of 1142 ICU days were included: 106 (9.3%) prone position days and 1036 (90.7%) supine position days.
Table 1.
Patient Characteristics
| Total patients: 34 |
| Patients on ECMO: n=14 |
| Non-ECMO Patients: n=20 |
| Gender: Male n=67 Female n=35 |
| Mean age: 52 years (33-73 years) |
| Mean BMI: 31.2kg/m2 (21.0 -50.0kg/m²) |
| Mean Length of Stay: 30.8 days (16 hours-110 days) |
Patients received EN on 1098 days (96.1%) and PN on 44 days (3.9%). Only 4 of the 44 PN days occurred whilst a patient was in the prone position (0.4%).
On prone position days, patients received an average 80% of their prescribed energy and 56% of their prescribed protein requirements, compared with 95% prescribed energy and 84% prescribed protein on supine position days. The average received across both prone and supine position days was 94% energy and 82% of protein.
The 4 most frequent barriers to meeting protein requirements when in prone position were:
• Reduction of NG feed rate when GRV’s were higher than maximum acceptable volume
• Use of a standard 4g protein/100ml ‘Out of Hours’ enteral feed
• Fasting for procedures
• Failure to give protein supplement boluses when patient returned to supine position
Conclusion: Patient position affected nutritional intake, with energy and protein intake being lower on prone position days compared with supine position days. As only 9.3% of total ICU days were prone position days, average energy and protein received across all days still achieved nutritional adequacy. An increase in a patient’s prone position days during ICU admission is likely to result in greater nutritional deficit, particularly for protein.
Recommendations to improve nutritional adequacy on prone position days:
• Consider use of post-pyloric feeding to increase feed tolerance
• Use of a higher protein ‘out of hours’ enteral feed
• Raised awareness of standard fasting times to ensure minimum disruption to feeding
• Consider administration of protein supplement boluses in prone position when GRV’s are within the accepted range
References
1. Garcia B, Cousin N, Bourel C, Jourdain M, Poissy J, Duburcq T. Prone positioning under VV-ECMO in SARS-CoV-2-induced acute respiratory distress syndrome. Critical Care. 2020;24(1):1-4.
2. CCSG Best practice guidance: Enteral Feeding in Prone Position. (2020). https://www.bda.uk.com/resource/best-practice-guidance-enteral-feeding-in-prone-position.html Date accessed: 17/08/2021.
3. Heyland DK, Cahill N, Day AG. Optimal amount of calories for critically ill patients: depends on how you slice the cake!. Critical care medicine. 2011;39(12):2619-2626.
P133
Nutritional adequacy and accuracy in long-stay critically ill patients as measured by indirect calorimetry
Nutrition
Alexandria Page 1 , Anne Langan1, Angela McNelly2, Yize Wan2, Rupert Pearse2, John Prowle2 and Zudin Puthucheary2
1Barts Health NHS Trust
2Queen Mary University of London
Abstract
Introduction: Nutritional optimisation is recognised as having significant impact on clinical and functional outcomes of critically ill patients.1 Clinical recommendations suggest use of indirect calorimetry guided nutrition in the intensive care unit (ICU),2 and a recent systematic review demonstrated improved outcomes from its use.3 The COVID-19 pandemic has seen a greater proportion of patients with prolonged critical illness, a cohort for whom nutritional optimisation is a key unmet need.4
Objectives: To assess rates of over and underfeeding in a tertiary centre ICU and how these relate to markers of catabolism and persistent critical illness.
Methods: Serial measurements of REE (resting energy expenditure) and RQ (respiratory quotient) by indirect calorimetry were performed using Q-NRG+ device (COSMED, Rome, Italy). Nutritional intake and estimations of requirements were recorded concurrently together with routine clinical observations, and markers of critical illness, catabolism and over or underfeeding.
Results: Across 30 patients, REE was lower than estimated energy requirements, 24.2 (IQR 20.0-28.1) kcal/day/kg IBW vs. 29.1(IQR 25.4-33.1) kcal/day/kg IBW, p<0.001. 41.8% of measurements showed overfeeding (actual calorie intake >110% of REE), and 23.3% showed underfeeding (actual calorie intake <85% of REE). Obese patients (n=15) were underfed (-98kcal/day deficit) compared to non-obese patients (n=15), who were on average overfed (+256kcal/day surplus), p=0.021. Overfeeding was also associated with greater length of ICU admission (R2 0.159, p<0.005). Median day of ICU admission in overfed patients was 39 days (IQR 24-56), and in underfed patients 21.5 (IQR 7.5-45.25). However, there was no significant association between calorie surplus or deficit, and other markers of overfeeding PaCO2, insulin use, urea-creatinine-ratio.
Conclusion: This service evaluation recorded measurements of REE and RQ in critically ill patients with high lengths of ICU stay (up to 66 days). We observed increased rates of overfeeding with increased duration of ICU admission, and increased overfeeding in non-obese patients.
References
1. Singer P. Preserving the quality of life: Nutrition in the icu. Crit Care. 2019;23(Suppl 1).
2. Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38(1):48–79.
3. Duan JY, Zheng WH, Zhou H, Xu Y, Huang HB. Energy delivery guided by indirect calorimetry in critically ill patients: a systematic review and meta-analysis. Crit Care. 2021;25(1).
4. Shryane N, Pampaka M, Castro ALA, Ahmad S, Elliot M, Kim JH, et al. Length of Stay in ICU of Covid-19 Patients in England, March - May 2020. Int J Popul Data Sci. 2020;5(4).
P134
Critical Care Outreach in the COVID-19 era: non-invasive respiratory support and outcomes of acutely ill patients
Outreach
Brigitta Fazzini, Simon Nourse and Ann McGinley
Royal London Hospital, Barts Health NHS Trust
Abstract
Introduction: COVID-19 outbreak has generated an unprecedented surge of deteriorating and critically ill patients with severe and sustained pressures on intensive care units (ICUs) and staff. This has resulted in major staff redeployment from other areas, including some critical care outreach into ICU leaving the wards uncovered. Critical care outreach has the potential to optimise acutely ill and deteriorating patients on the wards and avert critical care admission; but its benefit during a pandemic is unclear.
Objectives: To determine the clinical need for critical care outreach during the Coronavirus disease 2019 pandemic. To evaluate patients’ outcomes to guide decision-making and resource prioritisation.
Methods: We evaluated all consecutive patients referred to critical care outreach during a twelve-month period from 1 March 2020 to 28 February 2021. We reported the cumulative number of activities and interventions, and baseline characteristics, acuity level and clinical outcomes.
Results: Amongst 4849 patients referred, 3913 had a clinical review and of those 895 were COVID-19 positive. Non-invasive ventilation was mostly delivered to COVID-19 patients (COVID-19 +VE: 853/895, 95% vs COVID-19 -VE: 119/3018, 4%) alongside awake positioning (COVID-19 +VE: 232/895, 26% vs COVID-19 -VE: 0/3018, 0%). Compared to pre-pandemic, patients were sicker meeting Level 2 acuity (observed: 51% vs historical: 21%; P= 0.003), however ICU admissions did not increase significantly (observed: 12% vs historical: 9%; P= 0.065), but greater mortality (observed: 14% vs historical: 8%; P= 0.046) was observed.
Conclusion: Critical care outreach support the delivery of non-invasive respiratory support bridging the gap between intensive care units and general wards. Critical care outreach act as a valuable resource in optimising and triaging acutely unwell patients and potentially averting critical care admissions.
P135
Intra-oral kinking of a micro-cuff endotracheal tube: an unusual cause of difficult ventilation
Paediatric intensive care
Dominic Wu 1 and Adam Nicholls2
1Manchester University NHS Foundation Trust
2Royal Manchester Children’s Hospital
Abstract
Background: Intra-oral kinking of endotracheal tube is a rare but not unheard of complication. It could be life-threatening if left unrecognised.
Case presentation: A ten-year-old boy with developmental delay, scoliosis and recurrent chest infections was transferred to our paediatric intensive care (PIC) with SARS-CoV-2 pneumonia.
The child was intubated with a size 5.5 micro-cuff endotracheal tube for critical hypoxic respiratory failure at his local hospital. The intubation was reported to be straightforward, with a grade 1 laryngoscopy view, but he was notably difficult to ventilate and oxygenate on the ventilator. He was transferred by road and was requiring a fraction of inspired oxygen of 0.8 and inhaled nitric oxide at 20 parts per million to maintain oxygen saturations of greater than 94%. The retrieval team also reported that he required a peak inspiratory pressure of as high as 49 cmH2O and positive end-expiratory pressure of 8 cmH2O with a 1:1 I:E ratio to maintain tidal volume of 6 ml/kg for his weight of 30kg. He was fully sedated and paralysed.
The child was examined on arrival to PIC. His trachea was central and there was no wheeze or abdominal distension. The capnography waveforms were of normal appearance. A chest X-ray was also done to exclude endobronchial intubation and obvious pneumothorax. He was noted to be unusually difficult to bag ventilate, and the delivery of tidal volumes were hugely variable with any change in head positioning. He was best ventilated with head-tilt and chin-lift.
Our concerns were escalated when the ‘red-flag’ of inability to pass the suction catheter was highlighted by the nursing team. The course of his tracheal tube was immediately palpated, and a twist was felt in the oropharynx. This finding was confirmed on laryngoscopy, which revealed a significant kink at letter “C” of this micro-cuff tube (Figure 1). The airway was swiftly exchanged, and immediate improvements of both ventilation and gas exchanged were observed.
Figure 1.
A kinked micro-cuff endotracheal tube
Conclusion: The polyvinyl polymers of endotracheal tubes are known to soften at body temperature and have a higher tendency to bent at acute angles,1 where the pilot tubing exists2; and when bending forces are applied away from the anatomical curvature, also known as the “Magill curve” (radius of approximately 140 millimetres), of most conventional tracheal tubes.2-5
Kinking of endotracheal tube at blind spots such as within the pharynx may happen more frequently in paediatrics than in adult critical care practice due to the use of straighter tracheal tubes with smaller wall thickness. We would like to raise awareness of this unusual case of difficult bag ventilation and high airway pressure ventilation. If a well-secured tracheal tube suddenly becomes problematic following, or in relation to positional changes, tube malfunction should be suspected. The integrity of the endotracheal tube must also be interrogated.
Consent obtained from parent
References
1. Ahluwalia C, Kiran S, Chopra V, Kar S. Airway obstruction during one lung ventilation: A shocking twist in the tube. Indian J Anaesth. 2014;58(4):497-499.
2. Hübler M, Petrasch F. Intraoperative kinking of polyvinyl endotracheal tubes. Anesth Analg. 2006;103(6):1601-1602.
3. Hariharan U, Garg R, Sood R, Goel S. Intraoperative kinking of the intraoral portion of an endotracheal tube. J Anaesthesiol Clin Pharmacol. 2011;27(2):290-291.
4. Prakash S, Kumar A, Kumar M, Gogia AR. Successful detection and management of kinked tracheal tube in a patient with severe post-burn contracture of the neck.Indian J Anaesth. 2013;57(1):90-91.
5. Chandler, M. (2002), Tracheal intubation and sore throat: a mechanical explanation. Anaesthesia, 57: 155-161.
P136
Prediction of death within 12 months by ICU clinicians
Palliative and end of life care
James Turner 1 , Kerrie Aldridge2 and Jon Hulme3
1University Hospitals of North Midlands NHS Trust
2University Hospitals Birmingham NHS Foundation Trust
3Sandwell and West Birmingham Hospitals NHS Trust
Abstract
Introduction: The ‘surprise question’, “would you be surprised if this patient died within the next 12 months?” has been proposed as a tool for identification of those who may benefit from advanced care planning, and possibly palliative care, as part of the Gold Standards Framework.1 This predictive ability may have an impact on decisions about treatment escalation planning and communication with patients.
Objectives: To investigate the accuracy of intensive care clinicians’ predictions on the likelihood of death within 12 months.
Methods: An audit on treatment escalation planning was carried out in March 20192: medical records for all hospital admissions, excluding obstetrics, for three 24-hour periods were assessed. Within the audit, intensive care unit (ICU) clinicians were asked the ‘surprise question’ about each patient. After 15 months, the electronic patient record of every patient was accessed to record if the patient had died and compared to the initial prediction to create a list of ‘unexpected survivals’ and ‘unexpected deaths’. The number of days from the index admission to the date of death, if relevant, were calculated.
Results: Of the 282 patients assessed, ICU clinicians would not have been surprised of death within 12-months for 101 (36%) patients. For 207/282 (73%) predictions, clinicians were correct in their assessment; most of these were correct predictions of survival. For 75 patients in whom the prediction was incorrect, 7 (9%) were ‘unexpected deaths’. 5 patients who were not expected to survive 12 months died outside of the 12-month window, and 63 remained alive at the time of the re-audit (15 months after the index admission). Correctly predicting if the patient is likely to die within the time period in question i.e. sensitivity, was 83%. Specificity, the ability to recognise those who did not die, was 72%. The positive predictive value of the surprise question was 33% (proportion of patients who died when expected to) and the negative predictive value 96% (the proportion of patients not dying when not expected to). Of the ‘unexpected survivors’, 61% had a Modified Rankin Scale ≥ 3 (moderate disability or worse), and 41% had a Charlson Comorbidity Index ≥ 3. 74% were over 70 years old, and 54% were over 80 years old.
Conclusions: When asked whether they would be surprised if a specific patient died within 12 months, ICU clinicians are correct most of the time. However, a large proportion of patients not expected to live do survive longer than this. The accuracy of these predictions is in keeping with previous data, which shows in particular that positive predictive value is highly variable.3 A substantial number of patients who survived longer than 12 months after hospital admission were elderly, considerably frail, and had a significant burden of comorbidity. This audit may suggest that doctors who work in intensive care units have a more pessimistic view of survival than is borne out by data, which ought to be considered in communication of risks and benefits of higher level care with patients during treatment escalation planning.
References
1. Thomas K, Armstrong W, GSF Team. Proactive Identification Guidance (PIG) National Gold Standards Framework Centre in End of Life Care 2016, https://www.goldstandardsframework.org.uk/PIG (2016, Accessed 29 June 2021)
2. Aldridge K, Sherwood N, Hulme J. Treatment escalation planning in acutely unwell patients – are we missing opportunities? In: Intensive Care Society State of the Art, Birmingham, UK, 9-11 December 2019, poster 0224. Journal of the Intensive Care Society. 2020;21(2):1-225.
3. White N, Kupeli N, Vickerstaff V, Stone P. How accurate is the 'Surprise Question' at identifying patients at the end of life? A systematic review and meta-analysis. BMC Med. 2017;15(1):139.
P137
Transitioning end of life from critical care to abode
Palliative and end of life care
Avinash Kumar Jha 1 , Sudhindra Gurunath Kulkarni2 and Shondipon Laha2
1Lancashire Teaching Hospitals (LTHTR)
2Lancashire Teaching Hospitals
Abstract
Introduction: An elderly male was admitted to the hospital with back pain and was diagnosed with cervical spine abscess secondary to staphylococcal infection. He underwent surgical evacuation, following which he was admitted to the intensive care unit and progressed to irreversible quadriplegia requiring mechanical ventilator support. After four weeks of therapy and tracheostomy, a multi-disciplinary team discussion included the patient and the family. The outcome decision was to move to end of life care (EoLC), and the patient requested that he wanted to be home with his loved ones during the final hours of his life.
A detailed progression plan was discussed with the family, and the anticipated series of events with the home transfer process and subsequent steps were communicated. Before home transfer, he required pleural effusion drainage to ensure a safe transfer.
On arrival at home, we had a team of palliative care nurses and a consultant. As the family members gathered, a speaking valve with Non-invasive ventilation (NIV) mode was used, which helped the patient speak to the family members.
Once the patient spent adequate time with family, anticipatory medications were administered. The tracheostomy tube was removed and replaced with a face mask. The patient took his last breaths of life at his house amidst his loved ones. He was comfortable and had no signs of distress.
Main body: Around 20% of patients admitted to intensive care in the UK die in hospital1. Unfortunately, a unified approach to end of life planning cannot be applied to all patients; instead, it has to be individualized. The end of life should be based upon a multi-disciplinary team discussion involving shared decision making between patient, family members and the medical team and often leads to the provision of palliation care either in the intensive care unit or on the ward1. However, palliation at home is a more complex process, and several factors need addressing. A pragmatic approach helps provide individualized care and can be tailored as per the patient/ family requests, as shown in Figure 1.
Figure 1.
▪▪▪.
The economics of EoLC at home seems to be more cost-effective than in hospital management, as depicted in Figure 2.2,3
Figure 2.
Cost comparison between community and hospital services in terminally ill.
The focus should be on providing good death, and this can be achieved most simplistically by addressing patient preferences and keeping them patient pain free.4 There are no specific outcome measures to define the quality of death that are not as straightforward as quality-adjusted life years.
Conclusion: Death is an important event not only for families but also for the patient. In certain circumstances, we as health care professionals can aid and enhance this process with a multi-faceted approach. This will lead to a patient-centred delivery of services and can minimize the economic burden on healthcare resources.
References
1. Cosgrove J, Baruah R, Bassford C, et al. care at the end of life: a guide to best practice, discussion and decision-making in and around critical care, ficm.ac.uk/sites/default/files/ficm_care_end_of_life.pdf (2019, accessed 21 August 2021).
2. Welsh Government. Together for health – a delivery plan for the critically ill, wales. nhs.uk/documents/delivery-plan-for-the-critically-ill.pdf (2016, accessed 21 August 2021).
3. Curtis L, Amanda B. Unit costs of health & social care 2017. The report, Personal Social Services Research Unit, University of Kent, UK. 2017.
4. Singer PA, Martin DK, Kelner M. Quality end-of-life care: patients' perspectives. JAMA 1999 281(2):163-168.
P138
The end is just the beginning: Involving bereaved next of kin in qualitative research
Palliative and end of life care
Bronwen Warner 1, Alice Harry 2 , Stephen Brett3, Mary Wells1 and David Antcliffe1
1Charing Cross Hospital
2Royal Free Hospital
3Hammersmith Hospital
Abstract
Introduction: Almost half the UK population die in hospital and more than two thirds of these are aged 75 years or more.1 Older people make up an increasing proportion of patients admitted to critical care and often have poorer outcomes, especially in the context of COVID-19.2 Loved ones are an essential support network for older patients but their ability to provide support was compromised by visiting restrictions during COVID-19. Little is known about the experiences of older patients in ICU and there is limited literature on the experiences of bereaved relatives.3 Bereaved relatives may be the only way to access the experiences of patients who do not survive, but there are a number of barriers to including bereaved relatives in research. Researchers may feel inhibited from imposing what might be seen as an additional burden on families during the aftermath of a bereavement.
The ongoing ESCAlation of the eLderly (age >65years) to criTical carE with COVID-19) (ESCALATE) study includes semi-structured interviews with bereaved loved ones as well as patients and NoK of survivors in the UK.
Objectives: To describe successful involvement of bereaved next of kin in critical care-based research
Methods: This qualitative research uses semi-structured interviews and thematic analysis. Patient and public involvement from an intensive-care focused charity and local palliative care team advice was sought in order to develop recruitment strategies such as detailed, sympathetically worded participant information packs.4 In keeping with the literature,5 the window for recruitment and interview was approximately one year following bereavement. Following ethical approval, participants were recruited via postal invitations with follow up telephone calls if no response after a minimum of one week.
Results: Recruitment was limited by only 40% of bereaved NoK (next of kin) having postal addresses recorded on the hospital systems. 9 /40 bereaved NoK contacted by letter responded and as well as completing a questionnaire, consented to be interview. A further 5/11 contacted by follow-up telephone call agreed to participate (consistent with response rates for patients and NoK of survivors).
All of the interviewed bereaved participants completed the interview according to the interview topic guide, with each interview lasting around 45 minutes. More than half were female, and three quarters were Black, Asian or Minority Ethnic.
Bereaved relatives were keen to share their experience and some even volunteered additional information with the interviewers, such as resources they had created for their local community and personal diaries. Participants reported that they were happy to be interviewed if it would help others in a similar position.
Conclusion: Bereaved relatives of critical care patients are willing to engage in qualitative research. Recruitment is challenging due to practical constraints, but we suggest could be improved through meticulous documentation of contact details and involvement of bereavement services in research. By seeking the views of bereaved loved ones, we can improve care for critically unwell patients at end of life.
References
1. gov.uk. Older people who died in hospital: UK 2017. 2017.
2. Guillon A, Laurent E, Godillon L, Kimmoun A, Grammatico-Guillon L. Long-term mortality of elderly patients after intensive care unit admission for COVID-19. Intensive Care Med. 2021;47(6):710–712.
3. Kentish-Barnes N, McAdam JL, Kouki S, Cohen-Solal Z, Chaize M, Galon M, et al. Research Participation for Bereaved Family Members: Experience and Insights from a Qualitative Study. Crit Care Med. 2015 Sep; 43(9):1839–1845.
4. Devik SA, Hellzen O, Enmarker I. Bereaved family members’ perspectives on suffering among older rural cancer patients in palliative home nursing care: A qualitative study. Eur J Cancer Care (Engl). 2017 Nov; 26(6).
5. Butler AE, Hall H, Copnell B. Bereaved parents’ experiences of research participation. BMC Palliat Care. 2018 Nov; 17(1).
P140
Risk factors for complicated grief among family members bereaved in intensive care unit settings: a systematic review
Palliative and end of life care
Emma Sanderson 1 , Sally Humphreys2, Fiona Walker3, Daniel Harris4, Emma Carduff5, Joanne McPeake3, Kirsty Boyd1, Natalie Pattison6 and Nazir Lone1
1University of Edinburgh
2University of Hertfordshire
3NHS Greater Glasgow and Clyde
4Cambridge University Hospitals NHS Foundation Trust
5Marie Curie Hospice, Glasgow
6University of Hertfordshire/East and North Herts NHS Trust
Abstract
Introduction: Complicated grief arises when an individual experiences prolonged, intense grieving that affects physical and mental health, and impacts on social and emotional wellbeing. Between 5 and 10% experience complicated grief after a death in the general population.1 However, families of intensive care unit (ICU) decedents are at an increased risk of experiencing complicated grief. It is important to try and identify individuals who may be at risk of complicated grief. However, factors associated with complicated grief in ICU and bereavement needs assessment are not available routinely.
Objective: We aimed to conduct a systematic review identifying risk factors associated with complicated grief among family members of ICU decedents.
Methods: MEDLINE, EMBASE, CINAHL, PsycINFO, the Cochrane Library and Web of Science were searched to identify relevant articles. Reference lists were also screened. Studies were included which investigated risk factors for complicated grief in adult family members of patients admitted to adult ICUs. Observational studies and randomised and non-randomised controlled trials were included. Studies were limited to those published in English. Studies were screened and quality appraised, using the Newcastle-Ottawa Scale, in duplicate. Data was extracted for both univariable and multivariable analysis at any time point.
Results: Seven studies conducted across three continents were eligible; all but one were observational study designs. Most included multiple ICUs. Four studies were of high quality. 61 different risk factors were investigated across the studies, although most were only investigated by an individual study. Factors associated with a decreased risk of complicated grief included age of patient and relative, patient declining treatment, preparedness for death and involvement in end-of-life decision-making. Factors associated with increased risk included living alone, being the partner of the deceased, dying while intubated, problematic communication with physician, and not having the opportunity to say goodbye. Several other factors showed an association in univariable analyses but either were not investigated or showed no association in multivariable analysis.
Conclusion: Death is common in ICU settings and bereaved family members are at risk of poor outcomes. Yet, proactive screening and bereavement support are uncommon. This systematic review has identified potentially modifiable risk factors, some of which are specific to the ICU setting, which may help identify family members at highest risk of complicated grief. Our findings highlight the need to develop and tailor bereavement screening and follow-up services for family members bereaved in ICU settings.
References
1. Boelen PA, Smid GE. Disturbed grief: prolonged grief disorder and persistent complex bereavement disorder. BMJ 2017; 357:j2016.
P141
Improving the End of Life (EOL) experience for critically ill patients, families and multidisciplinary teams – a quality improvement (QI) project
Palliative and end of life care
Kirsty Boswell, Tarni Duhre and Radha Sundaram
NHS Greater Glasgow and Clyde
Abstract
Introduction: It is becoming increasingly evident that the provision of good care at the end of life is a vital component of Intensive Care Medicine.1 The Guidelines for provision of intensive care services V2 (GPICSV2) has set out definitive standards and recommendations for care at EOL.2,3
Objectives: In order to conform with the standards and recommendations set out in GPICS V2, the multidisciplinary team at the Royal Alexandra Hospital (RAH) implemented a QI programme adhering to Institute of Healthcare Improvement`s Model for improvement.
Methods: The RAH has 7 Level 3 beds and admitted approximately 350 patients each year. EOL prescribing practices were analysed by identifying the proportion of patients who were appropriately commenced on the End of Life Care Bundle (EoLCB) on Carevue, the electronic database.
Data was initially collected over a twelve month period from February 2019, studying the 78 deaths on the unit. Two exclusion criteria were applied, namely patients who had died within one hour of arrival or had experienced a sudden death. 41 patients satisfied the criteria. The process was repeated seven months later between September 2020 and May 2021 following a period of staff education with involvement from the palliative care team, yielding a total data set of 49 patients following application of exclusion criteria.
Concurrently, a staff survey was carried out and multiple meetings were held with the Palliative Care team to guide the QI journey.
Results: Analysing clinical documentation from February 2019 indicated that whilst the EoLCB was appropriately commenced in 95% of cases, only 61% of cases involved judicious implementation of the End of Life Prescribing Bundle and discontinuation of non-anticipatory care medications.
The staff survey in September 2020 had 33 respondents from participation from all staff groups highlighted the need for staff education on prescribing and use of syringe drivers, need for peer support, bereavement support and death debriefs.
Evaluating how prescribing practices had changed following the period of staff education between September 2020 and May 2021 indicated that 69% of patients were appropriately commenced on the End of Life Prescribing Bundle and 71% of patient had all other medications discontinued upon implementation of EoLCB.
Conclusion: The EOL QI project although a work in progress has demonstrated a modest improvement in prescribing practice at EOL in critically ill patients. A repeat survey and evaluation of all key areas of EOL care is planned in order to achieve the standards set out in GPICSV2.
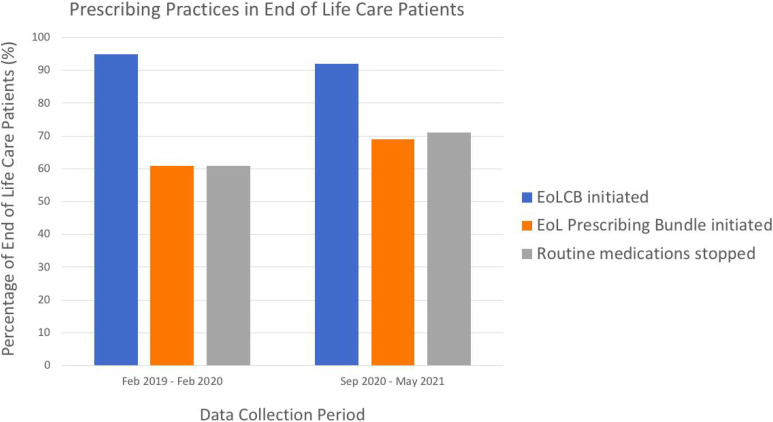
References
1. General Medical Council(2010). Treatment and Care towards the End of Life:Good Practice in Decision Making. Available from: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/treatment-and-care
2. Faculty of Intensive Care Medicine and Intensive Care Society. Guidelines for Provision of Intensive Care Services (2019) available from https://gpics-v2.pdf (ficm.ac.uk)
3. Kon AA, Shepard EK, Sederstrom NO, et al. Defining futile and potentially inappropriate interventions: a policy statement from the Society of Critical Care Medicine Ethics Committee. Crit Care Med 2016; 44: 1769-1774
P142
Improving staff confidence in providing palliative care in the Intensive Care Unit environment
Palliative and end of life care
Hannah Richards 1 , Bethan Roberts2, Catherine Hayle2 and Tom Williams2
1Mersey Deanery
2Wirral University Teaching Hospital
Abstract
Introduction: Whilst ICU patients have high rates of mortality and morbidity hospital specialist palliative care teams are often poorly integrated into Intensive Care Units. We noted that ICU and specialist palliative care team (SPCT) staff lack confidence in providing aspects of holistic end of life (EOL) care in the ICU environment. We therefore sought to establish the particular areas both ICU and SPCT staff found most challenging and run a programme of education and joint working to improve staff confidence and skill in these areas.
Aims: To improve staff confidence in providing holistic palliative care in ICU by identifying areas for development and instigating a programme of joint working, shadowing and formal teaching.
Methods: Online survey sent to all clinical staff working in ICU and hospital specialist palliative care team at Arrowe Park Hospital. Staff asked to self-rate confidence in providing end of life care. 30 core skills identified from national guidance.1 Shadowing sessions, formal teaching (focusing on areas of weakness from initial survey) and increased SPCT input on ITU were then instigated and a follow up survey sent to staff to evaluate the intervention’s impact.
Results: 34 staff responded to the initial survey (22 ICU and 12 SPCT) and 13 staff responded to the follow up (7 ICU and 6 SPCT). Responses were received from clinical staff including medical, nursing and allied health professionals.
Improved confidence (defined as increased staff self rating of extremely or very confident) was seen in every one of the 30 domains surveyed (Figure 1).
Figure 1.
Percentage of staff (both teams) rating confidence “extremely confident” or “very confident” pre and post intervention.
The initial survey revealed significant differences between confidence in providing EoL care between ICU and SPCT staff. SPCT were more comfortable with physical symptoms, 83% being extremely or very confident in managing pain in comparison to 37% of ICU staff. This difference was more marked in spiritual care with 75% of SPCT staff extremely or very confident in this vs 0% of ICU staff. ICU staff were however more comfortable managing withdrawal of life sustaining treatments (eg 36% of ICU staff extremely or very confident in managing the withdrawal of invasive ventilation compared to 0% of SPCT staff).
Following the interventions significant improvements were seen in both teams. ICU staff improved in managing spiritual care with 71% of ICU staff extremely or very confident compared to 0% prior to this intervention. Confidence in managing withdrawal of life sustaining treatment also significantly increased with 72% of critical care staff now extremely or very confident in managing withdrawal of IPPV.
Conclusion: The clear differences seen in the confidence of both teams in providing different aspects of care is a strong indication for the importance of integration of SPCT in the ICU environment. Significant improvement in staff confidence managing all aspects of EOL care was demonstrated with a simple programme of improved joint working and teaching. Sharing knowledge and skills between teams improved the skill set of staff working with palliative care patients in ITU and is vital to ensuring the provision of excellent end of life care in the future.
References
1. The Faculty of Intensive Care Medicine. Care at the end of life: A guide to best practice, discussion and decision-making in and around critical care, https://www.ficm.ac.uk/sites/default/files/ficm_care_end_of_life.pdf (2019, accessed 22nd August 2021)
P143
Correct positioning of central venous catheters in CRS + HIPEC patients
Peri-operative medicine
Ayesha Shajpal 1 and Ben Harris2
1Portsmouth Foundation School Trust
2Basingstoke & North Hampshire Hospitals NHS Trust
Abstract
Introduction: Patients undergoing cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) require a central venous catheter (CVC) for their peri operative and post operative management.1 Post operatively these patients receive total parenteral nutrition (TPN) which requires the CVC tip to be located between the “lower third of the superior vena cava, at the atrio-caval junction, or in the upper portion of the right atrium”.2
Objective: To complete the quality improvement cycle in reviewing our local practice of CVC insertions in this cohort, following implementation of an e-learning module and introduction of Hampshire Hospital Foundation Trust (HHFT) guidelines in 2019.
Methods: 58 patients underwent elective CRS and HIPEC between 1/03/2021 and 31/05/2021 at Basingstoke and North Hampshire Hospital compared to 59 patients over a similar period in 2019.3 A retrospective review of the CVC tip position on initial post-operative chest X-rays (CXR) was compared to results from the first cycle of auditing in 2019. The tip of the CVC was considered in the correct position as indicated by image 1 and if the tip was parallel to the wall of the SVC.4,5
Results: 84% of CVC’s were assessed as having the correct tip position on postoperative CXR which is an improvement from 63% in 2019. The right subclavian vein for CVC access remains the most common at 72% but this a reduction from 88% in 2019 (Figure 1). A total of 9 CVC tips in the 2021 audit were incorrectly positioned; only 2 of which were placed too distally. Interestingly none of the CVC’s with a tip position that was too short were inserted into a left sided vein.
Figure 1.
▪▪▪
Conclusions: Our CRS + HIPEC cohort have an intensive post operative recovery and reducing the need for further invasive post operative interventions such as changing CVC’s are beneficial for these patients. Following educational interventions (e-learning), updates in local guidelines and the increased awareness of the need for 20cm CVC’s has resulted in better placement and reduced need for repositioning of the CVC in the immediate post-operative period. A future iteration of our quality improvement project can investigate the mode of insertion of the central lines – ultrasound guided is recommended for internal jugular access and advised for other central access sites5 – which may further improve practice and successful first pass insertions.
References
1. Durnford S, Boss L, Bell J. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. BJA Educ. 2021;21(5):187–193.
2. Pittiruti M, et al. ESPEN. ESPEN Guidelines on Parenteral Nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr. 2009;28(4):365–377
3. Aplin C. Correct placement of central venous catheters following cytoreductive surgery - Audit. 2019 Jun.
4. Kerr M, McKenna J, Williams D. Audit of current central venous catheter (CVC) insertion depth. Abstract 0163 – E-Poster EPM.161, ICS, 2016
5. Bodenham Chair A, et al. Association of Anaesthetists of Great Britain and Ireland: Safe vascular access 2016. Anaesthesia. 2016;71(5):573–585
P144
Does the implementation of a QI care bundle increase the incidence of direct post-operative critical care admission in patients undergoing emergency laparotomy?
Peri-operative medicine
Adam Garland 1 and CM Oliver2
1Not Selected
2University College London Hospitals Associate professor, UCL Division of Surgery and Interventional Science
Abstract
Introduction: Urgent general surgical admission for complaints requiring emergency laparotomy is the commonest single organ cavity surgery undertaken in the United Kingdom. The risk of death accompanying emergency laparotomy is almost ten times greater than that associated with elective major gastrointestinal surgery. In the United Kingdom, over 30,000 emergency laparotomies are performed every year, with 30-day mortality in excess of 10%.1,2,3 The literature reported that improvements were needed throughout Europe for the provision of post-operative critical care for emergency laparotomy.4,5
Objective: The aim of this review is to establish whether the implementation of a quality improvement care bundle increases the incidence of direct post-operative critical care admission for patients undergoing emergency laparotomy?
Methods: This systematic review was registered with the PROSPERO database 193303. The literature search was performed using Embase (a registered trademark of Elsevier B. V), Medline (U.S library of Medicine) and Web of Science. A systematic review of the literature was performed. Studies assessing patients undergoing emergency laparotomy, care bundles and critical care admission were included. Studies assessing patients undergoing emergency laparotomy were included. The search was restricted to publications relating to humans from 2010 onwards, age >17 years at time of operation. The search was limited to English language publications. The last complete database search was 6 January 2020. Secondary searching included hand searching of references and a review of relevant citations.
Results: 22105 papers were identified using the primary electronic database search. Following restrictions 78 were retained. A further 43 underwent review of the abstract and full text. Eight studies were deemed eligible for data analysis. Six quality improvement initiatives using care bundles or pathways of care were identified for analysis. Studies that selected process measures as markers of quality of care (consultant decision making, risk assessment, early antibiotics and ICU admission) demonstrated that QI bundles increased the uptake and utilisation of both individual and collective process measures.
Conclusions: The organization of perioperative care for emergency laparotomy patients has received a high degree of scrutiny in recent years. Care bundles standardize care for emergency laparotomy. Patient needs are not homogenous and what may benefit one may not benefit another. A proportion of hospitals have successfully implemented admission criteria to facilitate direct admission to critical care for all high risk emergency laparotomy. Simple interventions that achieve cumulative marginal gains for this emergency surgical population must be crafted to fit the individual hospital’s need. Those QI initiatives that have demonstrated the greatest success have had stakeholder buy-in across the hospital community with ongoing education and support for QI leads. This review has highlighted the importance of such pathways in optimizing patient care and critical care resource utilization.
References
1. Clarke A, Murdoch H, Thomas MJ, Cook TM, Peden CJ. Mortality and postoperative care after emergency laparotomy. Eur J Anaesthesiol. 2011;28(1):16-19.
2. NELA project team. First patient report of the National Emergency Laparotomy Audit. Royal College of Anaesthatists. 2015.
3. The Royal College of Surgeons of England Working Group on the Perioperative Care of the High-risk General Surgical Patient. The Higher Risk General Surgical Patient: Towards Improved Care for a Forgotten Group; 2011.
4. Pearse RM, Rhodes A, Moreno R, Pelosi P, Spies C, Vallet B, et al. EuSOS: European surgical outcomes study. Eur J Anaesthesiol. 2011;28(6):454-456.
5. NELA project team. Fifth Patient Report of the National Emergency Laparotomy Audit. Royal College of Anaesthatists. 2019.
P145
Methanol toxicity-an important deferential to consider in appropriate patients with high anion gap metabolic acidosis
Poisoning and toxicology
Eshita Majumder 1 and Kazi Bodruddoza2
1James Cook University Hospital
2Square Hospital
Abstract
Introduction: Methanol is a highly toxic substance and even a relatively small amount of accidental ingestion can lead to fatal outcomes or permanent neurological damage including blindness.
Objectives: Following ingestion, methanol is metabolized in the liver to a toxic compound, formic acid primarily by the enzymes alcohol dehydrogenase and aldehyde dehydrogenase. Profound metabolic acidosis with a high anion gap ensues and can cross the blood-brain barrier causing central nervous system toxicity. In developing countries like Bangladesh where the toxicology screen of methanol is not available, high clinical suspicion is crucial and diagnosis should be made from history and suggestive blood gas analysis. The main treatment modality is using fomepizole and/or intravenous alcohol to prevent the formation of toxic metabolites. If severe poisoning is suspected, early initiation of haemodialysis can lead to favourable outcomes by removing both parent alcohol and metabolites.
Methods: We are reporting four cases of young male patients who presented to a tertiary care hospital in Bangladesh with high anion gap metabolic acidosis following accidental ingestion of methanol. Other than the history of alcohol ingestion, no definitive history was available. As the toxicology screen was not readily available, the provisional diagnosis was reached by the process of elimination from presenting symptoms and signs and bedside arterial blood gas analysis. All four patients were admitted to the critical care unit and as the definite antidotes, fomepizole and intravenous alcohol are unavailable in Bangladesh, haemodialysis was started immediately via temporary femoral catheters.
Results: All four patients presented with gastrointestinal symptoms for 12-24 hours followed by dyspnoea and altered conscious level for a few hours. Blood gas analysis revealed high anion gap metabolic acidosis. Bilateral putaminal necrosis was found in brain imaging in two patients. Immediate haemodialysis was initiated along with supportive care in the critical care unit. Three patients recovered without any neurological and visual sequelae and one patient who presented with pH 6.5 expired despite dialysis.
Conclusion: In a resource constraint setting, simple bedside arterial blood gas analysis can aid in the diagnosis of severe methanol poisoning in suspected patients. In the absence of definitive antidotes for methanol toxicity, early recognition and initiation of heamodialysis can be life-saving.
References
1. Jacobsen D, McMartin KE. Methanol and Ethylene Glycol Poisninigs; Mechanism of Toxicity, Clinical Course, Diagnosis and Treatment. Med Toxicol 1986;1:309-334.
2. Barceloux DG, Bond GR, Krenzelok EP, et al. American Academy of Clinical Toxicology Practice Guidelines on the Treatment of Methanol Poisoning. J Toxicol ClinToxicol 2002;40:415-446.
3. Kumar SS, Seerala Boopathy K, Bhaskar ME. Methanol poisoning--a Chennai experience. J Assoc Physicians India. 2003;51:425-426.
P146
Improving the recognition of abnormal pathology results
Quality and innovation
Matt Harris 1 , Elizabeth Hubberstey2, Yi Lin Lai3 and David Hodgson2
1Nottingham University Hospitals NHS Trust
2University Hospitals of Derby and Burton NHS Trust
3Sherwood Forest Hospitals NHS Trust
Abstract
Introduction: Patients discharged from the Royal Derby Hospital Emergency Department are experiencing adverse outcomes because abnormal blood results are not being recognised. There was a recent serious incident in which a gentleman was discharged without it being recognised that his troponin was >3,000. After presenting to the Emergency Department blood tests including a troponin were sent. These initial blood tests were haemolysed, so a repeat set were sent. The treating clinician subsequently discussed the case with a senior decision maker. It was felt that a troponin was not clinically indicated. The patient was therefore discharged by the treating clinician without chasing the repeat troponin. The patient subsequently re-presented with cardiogenic pulmonary oedema secondary to a missed myocardial infarction. Retrospectively, the previous troponin was noted to be >3,000. Sadly, the patient subsequently died.
Objectives: The project was conducted in an Adult Emergency Department to improve the recognition of abnormal pathology results. The aim was that within three months, all patients would have 100% of their blood results acknowledged prior to discharge.
Methods: We used methods such as process mapping, surveying clinician attitudes and driver diagrams to understand the scope of the problem. Using the Model for Improvement and Plan-Do-Study-Act cycles, we introduced a rule that would make it mandatory to acknowledge blood results in patients discharged from the Emergency Department. We also trialled stickers on patient notes and discharge checklists designed to prompt clinicians to do so.
Results: The percentage of blood results acknowledged increased from zero to a peak of 38%. Although this is a significant increase, it is far short of the 100% target we set. The results suggest that each time a change idea was introduced, there was a transient improvement in the percentage of blood results acknowledged but this was not sustained over the long-term.
Conclusions: Although the project achieved a significant improvement in the percentage of blood results acknowledged, this was far short of our 100% target. In retrospect, perhaps we should have set a more modest target, but in terms of acknowledging blood results in patients discharged from the Emergency Department, we firmly believe that this should be done for 100% of patients 100% of the time. We experienced problems in getting our message across, as well as barriers within the Trust, the department and even within the team. We believe that IT solutions, such as pop up alerts and making it impossible to discharge patients electronically, are the only way to ensure clinicians acknowledge blood results in a sustainable way and would advocate continuation of the project using this as a future approach.
References
1. Care Quality Commission, Derby Hospitals NHS Foundation Trust Quality Report, 2015. [Online]. Available: http://www.cqc.org.uk/sites/default/files/new_reports/AAAB9885.pdf.
2. Merrill D, Reid R. Personal Styles and Effective Performance, New York: CRC Press, 1999.
3. Imperial College. Stakeholder Management, 21 June 2017. [Online]. Available: https://www.imperial.ac.uk/media/imperial-college/administration-and-support-services/staff-development/public/impex/Stakeholder-management-21jun17.pdf
4. University Hospitals of Derby and Burton. Vision, values and objectives, 2019. [Online]. Available: http://www.derbyhospitals.nhs.uk/about/vision-values-objectives
5. Drucker P. The Practice of Management, London: Butterworth-Heinemann, 2007.
P147
Development and Implementation of a Critical Care Cheat Sheet as a Visual Learning Tool
Quality and innovation
Lynsey Russell
NHS Borders
Abstract
Introduction: Transition to the critical care environment for new and redeployed nurses is challenging due to the complex knowledge, skills and technical abilities that underpin safe and effective practice.1
Aim/Objectives: The aim was to develop a visual learning tool to display complex information in a manner that could be quickly consumed and easily understood. This aids comprehension, enhances quality of learning and retention of the material. The infographic (‘Cheat Sheet’) was seen as a unique way to present this multi-modal information. We aimed to engage staff and encourage further information seeking. Bradshaw and Porter (2017)2 state that 65% of people are visual learners - conveying complex information in an easy to understand manner is fundamental to the Cheat Sheet’s success.
Our critical care unit has encountered significant staff turnover in the past 12 months, as well as increased patient numbers and acuity of illness secondary to COVID-19. Lack of a designated clinical nurse educator is an added constraint and adds pressure to experienced critical care nurses to provide education and support to new and redeployed staff.
Methods: We conducted an informal survey of new and redeployed staff, asking which areas of critical care they perceived to be most daunting. We used the PDSA cycle to produce multiple iterations of the resulting infographic. After discussion with colleagues, we produced the final version, focusing on cardiac, respiratory and neuro principles. This incorporates essential aspects of the CC3N Step 1 and 2 Competencies.3
Results: Extensive qualitative feedback has been universally positive and we have had significant interest from other Critical Care Units throughout the country hoping to emulate our success. Staff reported that patients are receiving treatment quicker due to the presence of the ‘cheat sheet’. Electrolyte replacement in initiated promptly and early stages of delirium are picked up and treated appropriately.
Conclusion: The infographic ‘cheat sheet’ first and foremost enhances patient safety. To ensure equity of care delivery, it makes sense to strive for a critical care workforce that is trained to common standards, assuring quality of workforce across geographical boundaries. This leads to an enhanced patient journey and can reduce length of stay. Nurses utilising the ‘cheat sheet’ learn about skills and knowledge needed to deliver safe high quality bedside care to the critically ill patient. Being able to involve and work closely with the multidisciplinary team to best meet the patient’s needs is essential to providing person centred care.
The infographic cheat sheet has been added to our Organisations teaching app which all hospital staff can access. It has been uploaded on to the British Association of Critical Care Nurses website so it can be utilised throughout the UK.
References
1. Deacon KS, Baldwin A, Donnelly KA, Freeman P, Himsworth AP, Kinoulty SM, Kynaston M, Platten J, Price AM, Rumsby N, Witton N (2017). The National Competency Framework for Registered Nurses in Adult Critical Care: An Overview. Journal of the Intensive Care Society. 10: 1-15
2. Bradshaw MJ, Porter S (2017). Infographics. A New Tool for the Nursing Classroom. Nurse Educator. 42 (2): 57-59
3. National Competency Framework for Registered Nurses in Adult Critical Care 2015, Version 2 CC3N
P148
Intravenous fluid stewardship in acutely unwell patients: a Quality Improvement Project
Quality and innovation
Manoj Wickramasinghe 1 , Nicholas Wroe1, Lucy Gurr2 and Tendekayi Msimanga1
1Mid Yorkshire NHS Trust
2Mid Yorkshire NHS trust
Abstract
Introduction: Intravenous fluids (IVF) are a ubiquitous treatment in hospitalised patients. For some conditions, such as hypovolaemic shock, fluids are lifesaving. However, overuse of fluids and fluid overload has been shown to independently predict mortality in the critically ill.
The culture of giving acutely unwell patients fluids stems from a study suggesting that achieving supra-normal physiological parameters with aggressive fluid resuscitation in critically ill patients would optimise tissue perfusion.1 The benefit of aggressive resuscitation has not been shown for critically ill patients - but the culture still permeates.
Furthermore, the choice of intravenous fluid is important – the SMART2 and SALT-ED3 trials showed that fluid resuscitation with a balance crystalloid (Hartmann’s) over 0.9% NaCl caused a lower incidence of acute kidney injury and patients requiring renal replacement therapy.
When considering daily electrolyte and glucose requirements, it is clear that balanced crystalloids or normal saline offer substantially higher amounts of sodium and chloride, not enough potassium and no glucose. Therefore, 4% dextrose/0.18% saline (dex/saline) + KCL is a preferred maintenance IVF – when two 1L bags are given all of the above electrolyte requirements can be met.
Objectives:
• Evaluate current intravenous fluid practice
• Improve knowledge amongst healthcare professionals
• Improve intravenous fluid practice
Methods: We evaluated intravenous fluids prescribed to inpatients on our Acute Admissions Unit (AAU). Data was collected from our electronic health record and prescribing system, over an 8-week period.
Figure 1.
Resuscitation fluids pre and post-interventions
Figure 2:
Maintenance fluids pre and post-interventions
Figure 3.
Total IVF used pre and post-interventions
After four weeks a teaching session was delivered surrounding IVF’s. It was also highlighted that the AAU did not have dex/saline + potassium as a stock fluid and hence it was never available to prescribe – following discussion with pharmacy this was added to the stock. At 6 weeks healthcare professionals were given pocket sized IVF guide badges and the IVF storeroom was rearranged to help nursing staff distinguish between resuscitation and maintenance fluids.
Results: We saw a in the amount of 0.9% NaCl used for both fluid resuscitation and maintenance, and an increase in use of Plasma-lyte for fluid resuscitation. The use of dex/saline + KCL for maintenance fluids was also increased which was unsurprising as there was no stock of this fluid on the ward prior to interventions.
Overall, there was a sizeable reduction in the amount of IVF administered to patients over the four week period (despite there being very similar number of patients in both groups).
Conclusion: On the back of large trials, using balanced crystalloids instead of 0.9% NaCl appears to be a preferred approach for fluid resuscitation in critically ill patients. Furthermore, physiology and knowledge of daily electrolytes requirements would suggest that using dex/saline + KCL is a preferred maintenance IVF. In this QIP we show how several small interventions within a unit can significantly improve IVF stewardship for a sustained period.
References
1. Shoemaker WC, Appel PL, Kram HB, Waxman K, Lee TS. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. 1988;94:1176–1186. doi: 10.1378/chest.94.6.1176.
2. Semler, M., Self, W., Wanderer, J., Ehrenfeld, J., Wang, L., Byrne, D., Stollings, J., Kumar, A., Hughes, C., Hernandez, A., Guillamondegui, O., May, A., Weavind, L., Casey, J., Siew, E., Shaw, A., Bernard, G. and Rice, T., 2018. Balanced Crystalloids versus Saline in Critically Ill Adults. New England Journal of Medicine, 378(9), pp.829-839
3. Self, W., Semler, M., Wanderer, J., Wang, L., Byrne, D., Collins, S., Slovis, C., Lindsell, C., Ehrenfeld, J., Siew, E., Shaw, A., Bernard, G. and Rice, T., 2018. Balanced Crystalloids versus Saline in Noncritically Ill Adults. New England Journal of Medicine, 378(9), pp.819-828.
P149
The introduction of an emergency algorithm folder to reduce cognitive overload and improve teamwork and non-technical skills in an Intensive Care Unit
Quality and innovation
Layla Guscoth, Kate Goodchild and Fiona Kelly
Royal United Hospitals Bath
Abstract
Introduction: The management of emergency scenarios requires prompt action, leadership and effective teamwork with clear and concise communication. Decision making in emergency scenarios can be hampered by environmental and organisational factors and cognitive overload.1 Emergency scenario communication has been further challenged by the physical and mental strain of the COVID-19 pandemic.2 Cognitive aids have been shown to improve clinician performanc3 and improve non-technical skills4. Reducing the mental workload of recalling an emergency algorithm sequence may ensure that all critical steps are followed, enabling more focus on team function.4 We proposed that a folder of emergency algorithms, readily available in our Intensive Care Unit (ICU), may enhance the running of emergency scenarios.
Objectives: We aimed to introduce an ICU algorithm folder for use in emergency scenarios, design and deliver an education programme and measure the effectiveness of this teaching in improving staff awareness of decision-making aids and adherence to emergency algorithms.
Methods: We designed and developed a 12-tabbed emergency algorithm folder including national and local algorithms, divided into clear categories for ease of use and located in an easily accessible central ICU location. We conducted ‘tea trolley teaching’5 to educate staff with the location and folder content and collect feedback regarding content and method of use. We designed a questionnaire to assess the perceived impact of the algorithm folder for emergency scenarios and evaluate confidence in locating and using the algorithms following teaching, including close-ended questions (Yes/No), Likert 5-point Scale (Always-Never) questions and free text.
Results: Thirty-seven multidisciplinary (MDT) ICU team members received teaching (8 doctors, 17 nurses, 1 ACCP, 2 physiotherapists, 9 others). Questionnaire response rate 37/37 (100%). Results are described in Table 1. Confidence in locating the emergency algorithm folder on the ICU improved from 32% to 96% following teaching and 100% of staff would recommend the initiative to other units.
Table 1.
■■■.
| I have used an emergency algorithm previously | 50% |
| I have had difficulty recalling all parts of an algorithm | 86% |
| I believe that an accessible emergency algorithm folder would be useful | 98% |
| I believe that the folder will improve adherence to emergency algorithms | 100% |
| I believe that the folder will improve patient safety | 100% |
| I believe that the folder will improve performance in an emergency | 96% |
Conclusion: Our findings demonstrate that an ICU emergency algorithm folder could improve recall, performance and adherence to algorithms in emergency scenarios and could improve patient safety. Tea trolley teaching was shown to be an effective method of educating the wider multidisciplinary team and raised awareness of the use of emergency algorithms. We now plan to trial the emergency algorithm folder in MDT simulation scenario training and are investigating digital options for the folder.
References
1. Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Br J Anaesth. 2011;106(5):617-631
2. Coughlan C, Nafde C, Khodatars S, Jeanes AL, Habib S, Donaldson E, Besi C, Kooner GK. COVID-19: lessons for junior doctors redeployed to critical care. Postgrad Med J. 2021;97(1145):188-191.
3. Low D, Clark N, Soar J, Padkin A, Stoneham A, Perkins GD, Nolan J. A randomised control trial to determine if use of the iResus© application on a smart phone improves the performance of an advanced life support provider in a simulated medical emergency. Anaesthesia. 2011;66(4):255-262.
4. Marshall SD, Mehra R. The effects of a displayed cognitive aid on non-technical skills in a simulated 'can't intubate, can't oxygenate’ crisis. Anaesthesia. 2014;69(7):669-677.
5. O'Farrell G, McDonald M, Kelly FE. 'Tea trolley' difficult airway training. Anaesthesia. 2015; 70 (1):10
P150
Whole lung lavage using high frequency chest wall oscillation in the treatment of pulmonary alveolar proteinosis.
Quality and innovation
Aimee Gow, Charlotte Chery-Downes and Chinmay Patvardhan
Royal Papworth Hospital
Abstract
Introduction: Pulmonary Alveolar Proteinosis (PAP) is a rare respiratory disease that is characterised by the build-up of alveolar surfactant. There are three types of PAP: hereditary, secondary and auto-immune.1 A whole lung lavage (WLL) is the recognised treatment for PAP and involves washing out the lung with saline and secretion mobilisation before drainage.
High Frequency Chest Wall Oscillation (HFCWO) uses positive and negative pressure changes to create shearing forces that encourage the movement of secretions from peripheral to the larger airways.2 Air pulses are transmitted into a garment at a high frequency increasing oscillatory chest wall compressions. There is a lack of evidence to guide Physiotherapist treatments and Multidisciplinary Team (MDT) management with secretion clearance of the patient using HFCWO.
Objective: This case study highlights therapeutic treatment for PAP using HFCWO during WLL at a Cardiothoracic centre.
Method: WLL was previously performed by Physiotherapists performing manual techniques to the chest wall. A team of Physiotherapists were required due to the duration of the procedure (up to 7 hours). For this case study HFCWO was used as an alternative to manual techniques.
The patient in this case study was a 37 year old male with PAP who underwent a WLL using the Vest Airway Clearance System (Hill Rom, Chicago, USA) due to disease exacerbation.
The patient was sedated and intubated in a supine position with a double lumen endo-tracheal tube (ETT) to facilitate the lavage of one lung whilst the contralateral lung was ventilated. The Vest machine was set to a frequency of 20Hz and the duration was guided by the MDT and ranged from 5 to 10 minute cycles. These cycles continued until the lung was completely lavaged, a total of 13 times. The patient was then ventilated at FiO2 1 for 30 minutes to assist the lavaged lung re-inflate and an arterial blood gas was taken before repeating the process with the other lung.
Results: This case study demonstrated benefits of the use of HFCWO to assist with secretion clearance in WLL including:
• No movement of the ETT on bronchoscopy whilst using HFCWO
• Less labour intensive and physically demanding for Physiotherapist
Utilising the Vest ensured all areas of the patient’s lungs received HFCWO, something not achieved with manual techniques
The day after the procedure the patient reported no pain or discomfort and was mobilising, eating and drinking as normal. The procedure was safe and there were no adverse reactions post-procedure.
Conclusion: The patient will have a further four to six WLLs in consecutive months to avoid repeated exacerbations. This case study demonstrates that the use of HFCWO during WLL to treat an exacerbation of PAP is safe and has no adverse effects.
Further data needs to be collected to investigate the effectiveness of Physiotherapy using HFCWO during WLL on disease exacerbation, infection rates and secretion clearance effectiveness.
Also, to investigate if changing frequency of oscillations and adding postural drainage will improve patient outcome by improving airway clearance and decrease the frequency of WLLs.
References
1. Fijołek J, Wiatr E, Opoka L, Rudziński P, Nierebińska M, Szołkowska M. Atypical image of pulmonary alveolar proteinosis — a case report. Pneumonologia i alergologia polska. 2015; 83(6): 453–456.
2. Hill Rom. The Vest® Airway Clearance System, Model 105. Available from: https://www.hillrom.co.uk/en/products/the-vest-system-105 [Accessed 6th July 2021]
P151
Scheduled replacement of central venous catheters: an evidence-based approach to infection control or an outdated practice?
Quality and innovation
Bindiya Shah 1 , Chenxian Wu2 and Hannah Burns2
1Hillingdon Hospital NHS Foundation Trust
2University College London Hospital
Abstract
Introduction: Healthcare-associated infections, particularly central venous catheter related bloodstream infections (CRBSI), are a major cause of morbidity and mortality.1 Diagnosis of CRBSI requires a positive blood culture from a peripheral vein and clear evidence that the catheter is the source, with either positive paired blood cultures or a positive tip culture and no other apparent source of infection.1
The practise of routinely replacing central venous catheters (CVC) to reduce the risk of CRBSI is controversial. Randomised controlled trials conclude limited benefit of scheduled replacement as well as recognising the increased risk of mechanical complications secondary to repeated invasive procedures.2,3 Therefore, national and international guidelines advise against routine replacement, instead advocating for replacement when clinically indicated in general populations4 as well as haematology and oncology populations.5
Objectives & Methods: We audited the routine management of 843 CVCs in a tertiary intensive care unit specialising in haematology and oncology patients, between the dates February 2019 to December 2020. The main objective was to determine if current practice regarding replacement of CVCs was in keeping with the gold standard established from the existing evidence base. Each CVC documented during this period was retrospectively audited to identify insertion technique, site, dwell time, reason for removal and/or replacement.
Results: Our findings show that CVCs on this unit are being replaced after an average dwell time of 6.40 days on a presumed basis that this reduces the risk of infection. Objective evidence to support this practice in our local population is indeterminable as currently no paired peripheral and catheter cultures or catheter tip cultures are routinely taken when CRBSI is suspected. In addition, CVCs were replaced in 45.2% of patients who were febrile but did not meet diagnostic criteria for CRBSI. Furthermore, planning for long term access is poor with 43 patients having three or more central venous catheters in their inpatient intensive care admission without consideration of a long term peripherally inserted central catheter (PICC).
Conclusion: From our local data and existing evidence base, recommendations for change are as follows:
1. If CRBSI is suspected, paired peripheral and line blood cultures should be sent to allow for confirmation of diagnosis of suspected CRBSI
2. Improve education regarding central venous catheter insertion, site assessment and management of suspected CRBSI
3. Improve the early identification of patients who may need long term central access and could be appropriate candidates for PICC lines rather than pursuing a course of repeated CVC replacement
To increase the impact of these data-driven and evidence-based changes, these recommendations have been implemented through locally published guidelines (Addendum 1). Further endorsement of these recommendations will be established through educational workshops for junior doctors with a focus on optimising insertion conditions and technique, encouraging routine assessment of CVC sites as well as establishing a routine for diagnosing and managing suspected CRBSI. Re-audit is planned in six months to one year after the implementation of changes.
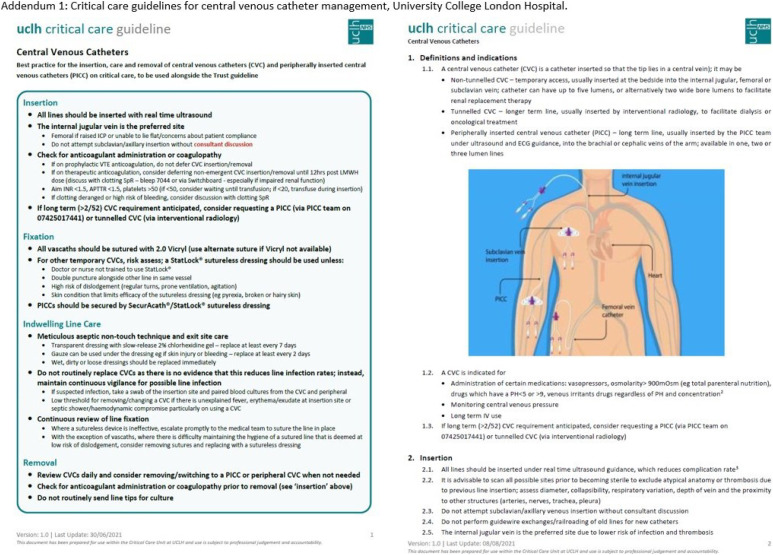
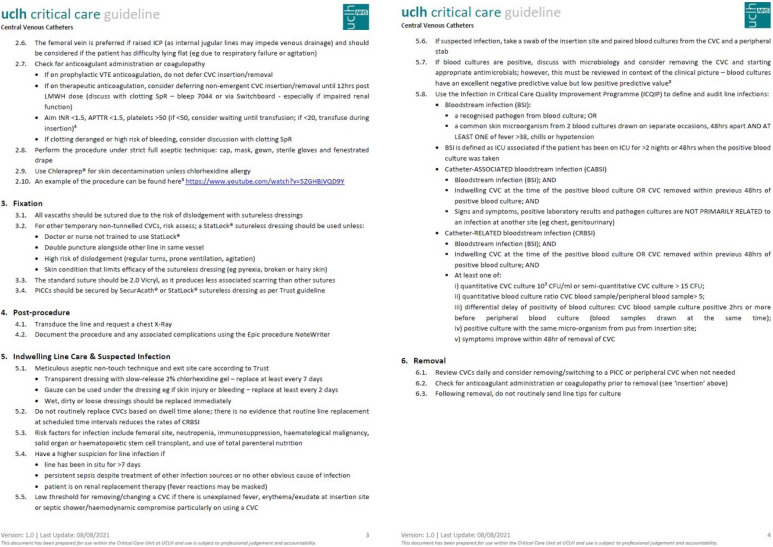
References
1. Gahlot R, Chaitanya N, Kumar V, Yadav G, Anupurba S. Catheter-related bloodstream infections. Int J Crit Illn Inj Sci. 2014 Apr; 4(2):162-167. doi: 4103/2229-5151.134184.
2. Cobb DK, High KP, Sawyer RG, Sable CA. A controlled trial of Scheduled Replacement of Central Venous and Pulmonary Artery Catheters. N Engl J Med. 1992 Oct; 327:1062-1068. doi: 10.1056/NEJM199210083271505.
3. Schalk E, Biehl LM, Färber J, Schlüter D, Vehreschild MJGT, Fischer T. Determination of a Cutoff Time Point for Prophylactic Exchange of Central Venous Catheters for Prevention of Central Venous Catheter-Related Bloodstream Infections in Patients with Hematological Malignancies. Infect Control Hosp Epidemiol. 2017 Jul; 38(7):888-889. doi: 10.1017/ice.2017.92. Epub 2017 May 18.
4. Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A, Browne J, Prieto J, Wilcox M, UK Department of Health. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2014 Jan; 86(Suppl 1:1-70. doi: 10.1016/S0195-6701(13)60012-2.
5. Boll, B, et al. Central venous catheter-related infections in hematology and oncology: 2020 updated guidelines on diagnosis, management, and prevention by the Infectious Diseases Working Party of the German Society of Hematology and Medical Oncology. Ann Hematol. 2021 Jan; 100(1):239-259. doi: 10.1007/s00277-020-04286-x.
P152
Workforce Innovation in the Enhanced Respiratory Care Area
Quality and innovation
Abigail Levison 1 , Jane Dean2 and William Sullivan2
1East Lancashire Hospital Trust
2East Lancashire Hospital
Abstract
Introduction: During the COVI-19 pandemic, the NHS was placed under increased pressure, with the demand for critical care beds and experienced personnel to staff them, being particularly intense.
Early evidence suggested that level 2 respiratory patients receiving high-flow nasal oxygen and/ or continuous positive airway pressure (CPAP) could be safely cared for outside critical care unit (Calligro et al., 2020; Nightingale et al., 2020).
• During the second wave, regional modelling suggested an acute and immediate increase in demand for respiratory critical care beds.
• the existing critical care unit did not have the bed or staff capacity to manage the expected surge in demand.
• An Enhanced Respiratory Care Area was created
• Patient and staff feedback was sought for review
Objectives: To reduce the demand for critical care beds and workforce pressure by provision of a level 2 enhanced respiratory care area.
Methods:
• An 8-bedded unit was created next to the critical care Unit
• 1:4 care model
• Staffed by the Acute care team who normally provide the Trust Critical care outreach service. The team are a diverse group of practitioners consisting of individuals from different professional backgrounds including physiotherapists, paramedics and a variety of nursing specialities; many team members did not have a critical care background. The team consists of Advanced Clinical Practitioners (ACPs), prescribing practitioners, practitioners, including our vascular access practitioner and expert IV access health care assistants.
• The unit was supported by a full-time F3 (redeployed from other areas) and a physiotherapist.
• This meant we had a vast array of experienced and knowledgeable practitioners with a large breadth of skills, many of which overlapped into each other’s roles.
Workforce Innovation: To fully utilize the breadth of skills from the teams and achieve the best patient outcomes, an integrative and inclusive approach to the workforce was adopted where staff performed to their capabilities rather than within the typical professional roles with the needs of the patient always remaining central.
For example: ACT members would clerk patients and prescribe, or perform chest physio if able, junior doctors and physiostherapists would assist with bedside care when able.
Working together in this way meant the team was more responsive to patient needs and could flex to meet surges in demand whilst learning from each other and working collaboratively.
• Overall
• 247 Critical Care bed days saved
• Median LOS 3.68 days
• Patient Feedback
• 100% confidence & trust in the care they received
• Felt they received a high standard of care from efficient, skilled & confident staff
• Staff Feedback
• Praise for the staffing model improving outcomes
• Patient cohort and care helping to encourage patients
Conclusion: Modern healthcare delivery is increasingly dependent on a complex and team-based approach to care provision (Dinh et al., 2019). Professional roles must be flexible and responsive to a changing environment with membersbeing able tyo cross traditional professional boundaries (Academy of Medical Royal Colleges, 2020; Schmutz, Meier & Manser, 2019). Whilst the global pandemic that created our axis of convergence is hopefully never to be repeated, the underpinning principles of working towards a common goal can be replicated.
Enhanced care areas adopting our workforce model could bridge the gap between ward-based care and critical care provision whilst delivering positive patient outcomes and staff satisfaction.
References
1. Calligaro G, Lalla U, Audley G, Gina P, Miller M, Mendelson M, et al. The utility of high-flow nasal oxygen for severe COVID-19 pneumonia in a resource-constrained setting: A multi-centre prospective observational study. The Lancet Online. 2020
2. Nightingale R, Nwosu N, Kutubudin F, Fletcher T, Lewis J, Frost F, et al. Is continuous positive airway pressure (CPAP) a new standard of care for type 1 respiratory failure in COVID-19 patients? A retrospective observational study of a dedicated COVID-19 CPAP service. BMJ Open Respiratory Research. 2020;7(1):e000639.
P153
Improving patient sleep quality in Intensive Care, Queen Alexandra Hospital, Portsmouth
Quality and innovation
Woon Woon Ng, Jonarthan Thevanayagam and Yusuf Siddique
Portsmouth Hospitals University NHS Trust
Abstract
Introduction: It is widely known that sleep disruptions and poor sleep are common in intensive care unit (ICU) patients. Rest is important for physiological and psychological recovery, and poor sleep may contribute to prolonged hospital stay and delirium. Multiple studies have been carried out to assess the efficacy of sleep-promoting interventions in ICU with limited and non-sustained benefit.
Objective: To identify factors contributing to poor sleep quality and to improve patient-assessed sleep quality in ICU using modified Richards-Campbell Sleep Questionnaire (RCSQ).
Methods: The project was carried out in adult intensive care unit, Queen Alexandra Hospital, Portsmouth. Non-ventilated patients who were able to understand and complete RCSQ were included in the project. The questionnaire was completed by the patients aided by a small group of interviewers. Two cycles have been performed. Sleep quality was assessed using 100 mm visual analogue scale RCSQ with scores closer to 100 indicating better sleep. Patients were also asked open ended questions on factors affecting their sleep and interventions offered by staff.
For feasibility purposes, staff time required to complete each questionnaire was also estimated retrospectively.
Results: The average staff time taken to help patients complete the questionnaire was 5-10 minutes, most of this was involved in helping to understand the visual analogue scale and free text questions.
Overall, the median scores for patient rated sleep depth was 36, sleep latency 49, sleep awakenings 50, ease of return to sleep 51.5, sleep quality 45 and noise 69.
There were no significant differences between two cycles as shown in Figure 2.
Ten patients were offered eye mask and ear plugs, which increased marginally between cycle 1 to cycle 2 from 24% to 29%. Only 1 patient felt that eye mask and ear plugs helped improve their sleep, however 9/11 (82%) of those not offered simple interventions would have considered using these.
Figure 1.
Questionnaire with RCSQ used for this project .
Table 1.
Patient numbers and types .
| First cycle | Second cycle | |
|---|---|---|
| Timing | June 2021 | July 2021 |
| No Patients | 17 | 21 |
| Patient type | elective patients | elective and emergency patients |
Conclusion: The current patient rated sleep quality on our intensive care is similar to published reports using RCSQ. However, given this low baseline, there are areas for improvement. The overall noise rating of ICU was better than expected, although 43% still stated it as a factor.
The initial cycles have tested feasibility and allowed finetuning of our methodology. The eventual aim will be for bedside nurse to perform the questionnaire daily.
The project has allowed identification of factors patients believe are affecting their sleep. We plan on doing further cycles to tackle this multifactorial and complex problem. The efficacy of interventions offered will be tested sequentially in cycles to regularly review which changes are beneficial.
Complex and multifactorial issues like this often require ongoing co-ordinated quality improvement programme to find and test solutions, and we have found anecdotally that simply by starting a quality improvement project, awareness of issues increases.
References
1. ■■■.
P154
Making the good better: developing a streamlined competency set for ICU Physiotherapists within an Academic Health Science Centre
Quality and innovation
Laura Mylott 1 , Claire Bradley1, Claire Purkiss2, Kelly Morris3, Kirsty Jerrard1, Debbie McKenzie1, Charlotte Pereira2, Linda Eftychiou4, Elaine Jenkins ap Rees4, Leyla Osman3 and Charles C Reilly1
1King’s College Hospital NHS Foundation Trust
2Royal Brompton and Harefield Hospitals
3Guy’s and St Thomas’ NHS Foundation Trust
4Kings Health Partners (KHP) Cardiovascular and Respiratory Partnership
Abstract
Introduction: “One team, multiple sites” is a principle supporting our Academic Health Sciences Centre (AHSC) partnership vision for academic and clinical excellence. COVID-19 has highlighted the need for co-ordinated cross-organisational working within ICU. There is currently no nationally agreed competency framework for ICU Physiotherapists. Having a streamlined set of competencies across the AHSC would be beneficial for safety, quality of care, training efficiency, workforce development, workforce mobility and further embed collaborative cross-site relationships.
Figure 2.
Box and whisker plots comparing RSCQ scores between cycles.
Table 2.
Factors patients state affect sleep .
| Factors patients reporting that have affected sleep in ICU | Percentage of patients reporting issue as affecting sleep |
|---|---|
| Noise | 43% |
| Pain and discomfort | 27% |
| Other environmental | 27% |
| Healthcare interventions | 11% |
| Uncertain | 29% |
| Lighting | 8% |
Figure 3.
Self-reported factors affecting sleep quality.
Figure 4.
Intended interventions (yellow boxes) to tackle factors affecting sleep quality.
Objective: To develop streamlined competencies for ICU Physiotherapists working within an AHSC.
Methods: Physiotherapy ICU leads from each site in the AHSC were identified via stakeholder mapping. This work stream was facilitated by a dedicated project lead, using a Plan-Do-Study-Act (PDSA) cycle.
Organisational and national competencies1-3 relevant to ICU Physiotherapists were collated. Benchmarking and mapping were completed to identify commonalities and deficits.
Initial meetings were conducted weekly via virtual forums to ensure benchmarking and mapping procedures were validated by all members. Two face-to-face meetings were employed to discuss the ideal competency set based on expert clinical opinion alongside the results from benchmarking and mapping. A whiteboard collaboration platform provided by Miro4 enabled all members to contribute whilst negotiations were facilitated by the project lead. Consensus on decisions pertaining to the streamlined document required all members to be in agreement. The method for achieving this centred on open discussion and regular communication.
Results: The work stream utilised eighteen organisational competency documents and three national documents.1-3 The final competency set was formulated using common themes which allowed for incorporation of specific competencies from each site. Agreement on each theme and specific competencies were easily reached due to the extent of commonality between existing organisational documents.
Rather than using bands to denote progression through competencies the work stream agreed on use of the terms Foundation, Specialist, Advanced and Expert, aligning the document with the Intensive Care Society AHP professional development framework.1 These levels are loosely aligned to the expectations for staff in bands 5-8, though allows staff to develop skills through the levels with no ceiling effect based on paygrade.
The group comprehensively devised the foundation level set of competencies and approved a sign-off procedure using elements from organisational documents, including self-reported confidence measures and senior supervised assessment of competence.
Conclusion: Using quality improvement methodology, the work stream was able to rapidly produce a comprehensive streamlined competency set for foundation level Physiotherapists in ICU across the AHSC. Next steps include gaining workforce feedback as part of a further PDSA cycle to refine the document prior to implementation. Continued collaboration by the work-stream will enable additional competency levels to be built from the foundation set. Education and training aligned to the document is essential for its success. Development of this will extend and reinforce the cross-organisational working and collaboration which is now embedded within the teams. The methodology to date demonstrates a proof of concept which can be utilised with other AHP groups in ICU, other settings or wider regional areas.
References
1. Intensive Care Society. The Faculty of Intensive Care Medicine. Allied Health Professionals: Critical Care Professional Development Framework. December 2018
2. London Transformation and Learning Collaborative. Critical Care Interprofessional skills matrix. https://www.e-lfh.org.uk/wp-content/uploads/2021/05/Skills-Matrix-Version-4-20210504_public_facing.xlsx (2020, Accessed May-August 2021)
3. Coe B, McGrath B, Lynch J, et al. ITC Project: Non-medical competencies for tracheostomy/laryngectomy care-Template for local adaptation. NTSP 2018.
4. Khusid A, Shardin O, Miro. 2021, Miro Whiteboard https://miro.com/about/ (accessed June-August 2021)
P155
Development and evaluation of a Thirst Bundle for adult critically ill patients in a tertiary UK Critical Care (CC)
Quality and innovation
Jenny Clark, Joel Meyer and Sally Archer
Guy’s and St Thomas’ NHS Foundation Trust
Abstract
Introduction & objectives: Interventions to counteract thirst are recommended by experts in intensive care medicine.1 Despite the well documented symptom burden,2 best practice guidelines for thirst treatment are absent in many UK hospitals. This service improvement initiative aimed to agree and pilot the safety, feasibility and efficacy of a topical treatment bundle for thirst with patient and multi-disciplinary (MDT) input.
Methods: A mixed methods implementation programme was completed to develop a proposed thirst assessment and intervention guideline for local use. Work streams included:
1. Patient and staff feedback: A. Patient and staff thirst forum – completion of a SWOT analysis of current thirst practice B. MDT steering group feedback and agreement on intervention proposed from existing evidence base C. ICU survivor feedback on proposed intervention, D. Staff survey on current attitudes and practice
2. Evidence review of current best evidence for treatments via systematic review following PRISMA guidelines (PROSPERO: CRD42020193074)3
3. Local implementation and pilot: A. Local awareness raising including training sessions, thirst intervention leaflets, posters and email communication B. Provision of equipment required for the intervention including ice, spray bottles, menthol balms C. Piloting in an 11 bedded high dependency care, with data collected on reported thirst among all patients by their attending nurse. The thirst intervention was used by nursing staff for those who were assessed as thirsty and then symptoms were reassessed D. Process, outcome and balancing measures were agreed as indicators of safety, feasibility and effectiveness
Results: The resulting intervention included three elements: ice cold swabs, ice cold water sprays and menthol lip balm.4 ICU survivor feedback indicated that the bundle was acceptable. The MDT steering group agreed a range of measures to assess thirst based on the literature and clinical feasibility, including markers based on clinician judgement and patient-reported scales.
During the pilot phase, 111 thirst assessments were completed with 20 patients. Median length of stay was 16 days (range 1-39). 33 assessments were lost to attrition due to incomplete reporting. Of the remaining sample, 51% (n=39) of assessments identified significant thirst. The thirst intervention was used for those who were assessed as thirsty. All assessment methods showed positive trends for the reduction in thirst symptoms. No safety concerns were raised during the period of usage. Oral hygiene practices were not affected following introduction of the bundle.
Conclusion: By combining patient feedback, local MDT knowledge and best available evidence we have agreed a thirst intervention locally for usage across the MDT and completed a pilot phase. Clinical application of the treatment has shown positive trends in reducing the burden of thirst symptoms for critically ill patients, no safety concerns were identified. High rates of incomplete recording during the pilot period shows requirement for further consideration of ease of assessment and scope for further training to embed thirst assessment/intervention into routine practice.
References
1. Puntillo K, Nelson L, Weissman D, et al. Palliative care in the ICU: relief of pain, dyspnea, and thirst—A report from the IPAL-ICU Advisory Board. Intensive Care Med. 2014; 40:235–248.
2. Puntillo KA, Arai S, Cohen NH, et al. Symptoms experienced by intensive care unit patients at high risk of dying. Crit Care Med. 2010;38(11):2155-2160. doi:10.1097/CCM.0b013e3181f267ee
3. Clark J, Archer S. Thirst interventions in adult acute care – what are the recommended management options and how effective are they? A systematic review. 2020. Publication pending.
4. Puntillo K, Arai S, Cooper B, Stotts N, Nelson J. A randomised control trial of an intervention to relieve thirst and dry mouth in intensive care unit patients. Intensive care medicine. 2014; 40: 1295-1302.
Acknowledgements: GSTT Thirst Steering Group: Natalie Holman (Pharmacist), Laura Mylott (Physiotherapist), Sarah-Jane Evans (Nurse), Julie Middlehurst (Nurse), Dr Meyer Joel (Consultant), Dr Andrew Jones (Consultant Intensivist), Jannah Valencia (Nurse), Dr Kathleen Daly (Nurse), Narbhla Donnelly (Dietitian), Micaela Hjerpe (Nurse).
This work was undertaken with support from Guy’s and St Thomas’ NHS Foundation Trust Charity.
P156
Thirst in Critical Care (CC); a multi-disciplinary (MDT) survey of attitudes and current practice
Quality and innovation
Jenny Clark, Joel Meyer and Sally Archer
Guy’s and St Thomas’ NHS Foundation Trust
Abstract
Introduction & objectives: Interventions to alleviate thirst in critically ill patients is recommended internationally.1,2 Previous work at our Trust has established a perception from current and former patients that response to thirst in critical care (CC) can be inconsistent and ineffective. This survey seeks to establish staff attitudes towards thirst in critically ill patients and determine the interventions being used manage thirst symptoms in a large, CC department. The responses would be used to inform service improvement related to thirst in CC.
Methods: A mixed methods survey containing eight questions was circulated to the CC MDT. Questions were selected and piloted by an MDT steering group. The aims were to explore current practices, perceived effectiveness and staff confidence in managing thirst. Internal email and virtual communication boards were used to advertise the survey aiming for a response rate of n> 50-75. The risk of non-sampling errors is acknowledged as a sampling bias risk.
Results: The survey yielded 69 responses of with a mix of critical care professionals represented (ICU Nurses n= 44, AHPs n=16, ICU Doctors n= 9). Median perception of effectiveness of current thirst management was 5/10 (range 1-9). The median confidence level in treating thirst was 5/10 (range 2-9). 25% (n=17) of ICU staff reported they assess thirst regardless of intake status, 29% (n=20) only ask about thirst for patients having oral intake, 9% (n=9) only if the patient is nil by mouth (NBM). Fourteen distinct interventions to alleviate thirst were reported; most frequently used for NBM patients were oral swabs (96%, n=66), saliva gel/spray (68%, n=47) and lip balm (63% n=62%). For patients on oral fluids, additional oral fluids (77%, n=53), ice cubes (53% n=29) and lip balm (41% n=28) were most frequently used. 99% of professionals stated they would act if a patient was thirsty. Proposed improvements to thirst management include routine access to ice, alternative options to oral swabs, clearer distinction of oral hygiene measures from thirst interventions and expertise balancing safety/risks and patient comfort when treating thirst.
Conclusion: This survey highlights potential for improvements in ICU staff confidence and perceived effectiveness of thirst management. Staff reported intention to alleviate thirst when identified. The considerable breadth of thirst interventions reported in this survey, indicates high staff willingness to treat thirst, but considerable variations in current practice. Implementation of a systematic, evidence based approach to thirst management could benefit patients and staff to by promoting consistent, safe and effective thirst management in critically ill adults.
References
1. Puntillo K, Nelson L, Weissman D, et al. Palliative care in the ICU: relief of pain, dyspnea, and thirst—A report from the IPAL-ICU Advisory Board. Intensive Care Med. 2014; 40:235–248.
2. Puntillo KA, Arai S, Cohen NH, et al. Symptoms experienced by intensive care unit patients at high risk of dying. Crit Care Med. 2010;38(11):2155-2160. doi:10.1097/CCM.0b013e3181f267ee
Acknowledgements: GSTT Thirst Steering Group: Natalie Holman (Pharmacist), Laura Mylott (Physiotherapist), Sarah-Jane Evans (Nurse), Julie Middlehurst (Nurse), Dr Meyer Joel (Consultant Intensivist), Dr Andrew Jones (Consultant), Jannah Valencia (Nurse), Dr Kathleen Daly (Nurse), Narbhla Donnelly (Dietitian), Micaela Hjerpe (Nurse).
This work was undertaken with support from Guy’s and St Thomas’ NHS Foundation Trust Charity.
P157
Improving Efficiency and Patient Safety at The Point of Admission; The Introduction of Portable Procedural Equipement Stations
Quality and innovation
Andrew Pinder, Vishal Dhokia, Kathleen Smiley and Debbie Jackson
SHERWOOD FOREST HOSPITALS NHS FOUNDATION TRUST
Abstract
Introduction: Admitting acutely unwell patients to the intensive care unit (ICU) can represent a busy and challenging time, particularly out of hours or in the context of surge into areas not usually utilised for delivery of intensive care. It is usual for the team to perform a number of procedures at the point of admission in order to stabilise the patient.
Objectives: During the Covid-19 surge it was noted that efficiency and potentially patient safety were being compromised by the time taken to locate essential equipment required to carry out the frequent and specialist procedures that are often performed at admission. This quality improvement project set out to address this short fall by introducing mobile workstations that were fully stocked with the required equipment and provided a working surface. Four different stations were introduced a general station (Intravenous, central, and arterial access, blood cultures, nasogastric tube insertion, urinary catheter insertion) and 3 specialist procedure stations an intercostal chest drain station, airway station and a percutaneous tracheostomy/lumbar puncture station. A spare general station was kept stocked in a storeroom so that after use stations could be replaced immediately. Laminated contents lists with photographs of drawer layouts were attached to allow restocking. General stations were sealed before being positioned in designated positions, marked on the floor, in each of the different clinical areas. The stations were designed to be easily cleaned to conform to infection control protocols.
Methods: Medical staff performed an electronic questionnaire before and after the introduction of the equipment stations.
Results: The 12 responders reported performing, on average 4 procedure per admission. Pre-intervention the average reported time taken to find equipment need was reported to be 22.5 minutes, with a further average 18.5 minutes taken by a second member of staff, usually bedside nursing staff. Post intervention these reported times fell to 7.5 minutes and 7 minute respectively, at time saving of 40.7 minutes (65%). In 2018/2019 our unit admitted 788 patients, therefore over a year we could potential save up to 535 hours, with the financial implications being obvious. The post intervention questionnaire contained a significant number of positive comments regarding the stations from staff.
Conclusion: This simple intervention is clearly able to improve patient safety, reduce frustration amongst staff as well as save time and money. The mobile nature of the stations allowed them to be used in other areas when required such as theatre, recovery and the emergency department, a feature which has been particularly beneficial during the Covid-19 surge. Other units may want to consider this set up as a way of improving safety and efficiency.
P158
Facilitators and barriers to music medicine in chronic pain management
Quality and innovation
Clare Keaveney Jimenez 1 and Dominic Harmon2
1College of Anaesthesiologists of Ireland
2University Hospital Limerick
Abstract
Introduction: Creative non-pharmacological approaches to chronic pain management including music, green exercise and virtual reality interventions are proving beneficial to patients. Music, delivered by a music therapist or in other forms without the presence of a therapist, becoming known as music medicine, has established advantageous effects on chronic pain management including reduced self-reported pain, emotional distress and medication requirements.
Challenges can exist in engaging patients in music programmes, with variable recruitment and attrition rates reported in the literature. Facilitators and barriers to the integration of music into chronic pain management pathways must be characterised in order to plan how to optimally deliver such adjuncts to patient therapy.
Objectives: To identify patient perceived facilitators and barriers to using music medicine as part of a chronic pain management strategy.
Methods: A sample of 102 patients who attended a chronic pain clinic were included. Participants completed a questionnaire in which they provided basic demographic information and Likert scale responses to statements examining attitudes towards music medicine.
Results: The majority of respondents (63%) were female. The most common age group among all respondents (47%) was 30-50 years. Participants agreed that music improves their mood and that music has health benefits (97% and 88%, respectively). 87% of respondents agreed that they engage with music regularly, either by listening or performing and 85% agreed that they engage with music for more than 15 minutes each time.
If provided with a plan to use music in their pain management, 68% of respondents agreed or strongly agreed that they would like to participate, 20% were neutral. 58% of respondents agreed or strongly agreed that they would like their general practitioner or pain specialist to discuss the use of music in pain management, 32% were neutral and <10% disagreed or strongly disagreed with this statement.
In terms of barriers, 37% of respondents agreed or strongly agreed that if provided with a plan to use music in management of their pain, they would like to participate, however they do not have time to commit.
68% of respondents agreed or strongly agreed that they prefer choosing their own music to listen to.
Conclusion: Patients with chronic pain are open to using music as part of their pain management and are aware of its potential benefits. Respondents regularly engage with music for significant periods at a time. However, time was identified as a barrier to participation when respondents considered committing to a plan to use music in their pain management. Our results highlight the potential to integrate music with a view to improving pain management in the day-to-day activities of patients with chronic pain.
P159
Providing a pre-hospital radiography service – a novel innovation to improve patient care
Quality and innovation
Sophie Robinson 1 , Matthew Bowker2 and Jazlina Sutanto1
1Northumbria Healthcare NHS Foundation Trust
2Northumbria Healthcare NHS foundation trust
Abstract
Introduction: Avoidable conveyance (AC) is when a patient has to be conveyed to a hospital emergency department unnecessarily. Reducing AC remains a key aim for many organisations including NHS England.1 With this considered, we created a pre-hospital radiography assessment service (termed X-ray Response Team (XRT)). The XRT is a novel, innovative, service that deploys radiographic imaging into the community. The XRT is formed from the multidisciplinary team with a partnership between Northumbria Healthcare NHS Foundation Trust’s Radiology and Emergency Medicine departments and the North East Ambulance Service (NEAS).
Objectives: To provide an efficient service which enables low-risk patients to remain at home whilst streamlining the care of those requiring admission to hospital.
Method: Each mobile XRT deployed consisted of a doctor, radiographer, paramedic and a remote senior supervising doctor. Referrals were received from NEAS call-handlers. Using mobile networks, the FDR Xair (Fujifilm mobile x-ray equipment) was used alongside the trust’s local IT systems to allow image capture and upload. The system incorporates the use of artificial intelligence to allow for quick, accurate reporting of images. The supervising senior doctor would then remotely review the images and liaise with the mobile team regarding whether the patient could remain in their own home and be discharged on scene or if they needed conveyance to hospital for further management.
Results: Over a six month period, 45 patients were assessed by XRT in their homes (mean age = 79). Pelvis/hip imaging was most commonly performed (16) followed by lower limb (13), chest (6) and upper limb (4). Of the 45 patients assessed by XRT, 18 of these patients (40%) were able to remain at home. The remaining 25 patients (60%) were identified as potentially benefiting from novel pathways to facilitate early specialist input from Care of the Elderly or Orthopaedics.
Conclusion: This project has demonstrated the exciting potential for pre-hospital radiology capabilities in vulnerable patients, providing an innovative link between primary and emergency care. This provides a platform for further development of point-of-care capabilities and streamlined referral pathways. There is scope to use this technology in humanitarian and military critical care teams in addition to utilisation in intensive care.
References
1. NHS England (2019). Planning to Safely Reduce Avoidable Conveyance.
P160
Monitoring nasogastric tube (NGT) displacement using chest X-ray (CXR) requests: Influence of tube fixation
Quality and innovation
Tony Thomas, Mahmoud Gaballah and Juliana Hamza
Salford Royal NHS Foundation Trust
Abstract
Introduction: Unplanned removal of NGTs is common and associated with multiple complications.1 Methods used to secure these tubes may influence removal rates.2 Following national guidance,3 we confirmed tube placement by CXR. We used the text of CXR requests to estimate the rates of NGT placement and to see how these were influenced by changing how NGTs were secured. We also used similar methodology to review changes to CXR requests mentioning central lines (CVCs) and endotracheal tubes (ETT).
Objectives: To see how CXR requests for NGT placement were influenced by changing the method used to secure these tubes.
Methods: In a 42 bedded mixed general and neurosurgical unit, in November 2019 we changed the method to secure NGTs from Hollister feeding tube attachment devices (Hollister, IL, USA)., to handcrafted slings made from Micropore (3M, MN, USA) 1.25cm Surgical Tape4. The text of CXR requests between October 2017 and July 2021 were analysed for text associated with NGTs, CVCs and ETTs. The number of bed days was calculated for each month from October 2017 and CXR rates per 100 bed days were calculated. Mann-Whitney U tests were used to establish if CXR rates changed significantly after November 2019 and after admitting patients with Covid-19 in March 2020. Distributions are shown as medians with [IQR].
Results: There were 15239 CXRs, a median of 330 [IQR 303-357] CXRs requested a month. The fraction mentioning each device was: ETT: 8%, CVC: 13%, NGT: 38% (18% of these also mentioning another device). The rates per100 patient days per month were: NGT pre-Nov 2019: 15.9 [15.0-16.4]. Post-Nov 2019 11.6 [10.1-12.7] (p<0.001), Nov 2019 to February 2020: 12.0 [8.0-13.3], vs Pre Nov 2019 p=0.008. For CVCs pre-March 2019: 4.1 (3.6-4.6) post March 2019: 5.2 (4.6-5.9) (p< 0.001) for ETTs pre-March 2019: 2.8 (2.0-3.3), post-March 2019: 3.1 (2.4-3.7). Changes in monthly rates are shown in the run chart in Figure 1.
Figure 1.
Number of X-Rays each study month per 100 bed days each device. Arrow show 1.change to Hammock Dressings to secure NG tubes and 2. the start of the covid 19 pandemic.
Conclusions: Changing the method of securing NGTs resulted in a reduction of CXR requests mentioning NGTs, reviewing CXR requests can be used to monitor NGT displacements. The rate of CVC requests increased following March 2020.
References
1. Carrion MI, Ayuso D, Marcos M, et al. Accidental removal of endotracheal and nasogastric tubes and intravascular catheters Crit Care Med 2000; 28: 63-66.
2. Gunther S C, Schwebel C, Vesin A, et al 2009 Interventions to decrease tube, line, and drain removals in intensive care units: the FRATER study Int Care Med 2009; 35: 1772-1776.
3. NHS Improvement: Nasogastric tube misplacement: continuing risk of death and severe harm https://www.england.nhs.uk/publication/patient-safety-alert-nasogastric-tube-misplacement-continuing-risk-of-death-and-severe-harm/ (2016, accessed 16th August 2021)
4. S.Brown, Hannah Sapir: The Hammock method of NG fixation. https://www.youtube.com/watch?v=sXB-IEPTV44 (2019, accessed 16th August 2021)
P161
Glycaemic control in a general intensive care unit: An ongoing quality improvement project
Quality and innovation
Thomas Roe 1 , Nikitas Nikitas1 and Jastine Rivera2
1University Hospitals Plymouth
2University of Plymouth
Abstract
Introduction: Critical illness-induced hyperglycaemia is estimated to affect 40-90% of critically ill patients irrespective of premorbid diabetes status.1 It is the consequence of various immunological, inflammatory, and hormonal alterations that are induced by critical illness leading to increased hepatic gluconeogenesis and glycogenolysis, and peripheral insulin resistance.2 Hyperglycaemia in critically ill patients is associated with an increase in mortality, and short-term morbidity; including increased ventilator weaning time, infection rate, and intensive care unit (ICU) length of stay.3,4
Objectives: The main objective of this audit was to explore to what degree the targets of glycaemic control (as clarified in the local and national protocols) are achieved in our unit. Secondary objectives include identification of a) factors that strongly affect glucose control in our critically ill patients, b) ways to optimise the current glucose control protocol in the general ICU.
Methodology: Data during the first week of admission, data from 58 critically unwell patients admitted to the general ICU in University Hospitals Plymouth was collected. Average blood glucose concentration (BGC), feeding modality, and degree of absorption were recorded for each four-hour period from admission. Timing of reinstatement of regular diabetic medications and/or variable rate intravenous insulin infusion (VRIII) commencement was also recorded. Time in euglycaemic range (TIER) defined as the percentage of four-hour periods within the euglycaemic range during the first week of admission was used as a performance metric. The euglycaemic range for all patients in this audit was 4.6-10.0mmol/L in concordance with international guidance.5
Results: Pre-admission diabetes status had a profound effect on mean percentage TIER (54.3% versus 84.8% for diabetic and non-diabetic patient respectively). Further stratification for admission HbA1c level above or below 48mmol/mol revealed that well controlled diabetic patients were exempt from this (mean TIER of 72.2% versus 47.6% for less well controlled diabetic patients). A very similar effect was present for diabetic patients with a body mass index above 30kg/m2. Acute steroid use during admission resulted in a marked reduction in TIER for diabetic patients (38.8% versus 64.0%), but this effect was not present in non-diabetic patients. Interestingly, type of nutritional support and degree of absorption of feed did not impact TIER significantly, regardless of diabetic status. Of all patients who received a VRIII, the time interval between the initial hyperglycaemic event and the initiation of the VRIII was on average 6.7 hours. The time interval between hyperglycaemia and return to euglycaemic range was on average 14.4 hours (18.4 hours for diabetic patients versus 10.7 hours in non-diabetic patients).
Conclusions: The results of this audit indicate that patients with raised BMI, poor pre-admission glycaemic control, and/or acute steroid use on the capability of the current protocol to manage glucose levels, particularly in diabetic patients. Additionally, in our unit, there is a prolonged time-period to regain control of BGC levels in these patients. We have suggested a risk stratification tool to be implemented on admission for all patients, aiming to facilitate early identification and appropriate management of abnormal BGC. This quality improvement project should commence re-auditing in Autumn 2021.
References
1. Viana M, Moraes R, Fabbrin A, Santos M, Gerchman F. Assessment and treatment of hyperglycemia in critically ill patients. Revista Brasileira de Terapia Intensiva. 2014;26(1):71-76.
2. Marik P, Bellomo R. Stress hyperglycemia: an essential survival response!. Critical Care. 2013;17(2):305.
3. Callahan L, Supinski G. Hyperglycemia-induced diaphragm weakness is mediated by oxidative stress. Critical Care. 2014;18(3):88.
4. Bilotta F. Glycemia management in critical care patients. World Journal of Diabetes. 2012;3(7):130.
5. Jacobi J, Bircher N, Krinsley J, Agus M, Braithwaite S, Deutschman C, et al. Guidelines for the use of an insulin infusion for the management of hyperglycemia in critically ill patients. Critical Care Medicine. 2012;40(12):3251-3276.
P162
Improving Safety of Handover on an Intensive Care Unit through the use of a Checklist
Quality and innovation
Alice Harry1, Laura White 1 , Mihir Patel2, Katia Florman1, Harriet Pittaway3 and Prashanth Nandhabalan1
1Royal Free Hospital
2Newham Hospital
3NHS England
Abstract
Introduction: Medical handovers take place in a variety of healthcare settings and play an essential role in facilitating the delivery of high quality patient care and preventing harm to patients.1,2 NICE have noted that structured patient handovers are critical to reducing mortality, preventing avoidable adverse events, reducing length of stay, and for improving both staff and patient satisfaction.3
In particular, an effective handover is of paramount importance in the critical care setting which features the highest complexity patients, frequent shift changes and in recent years an increase in number of junior doctors.4
The handover process at Royal Free Hospital Intensive Care Unit (ICU) was targeted for quality improvement and it was suggested that a structured “safety huddle” could improve transfer of care between staff.
Objectives: To improve patient safety in the ICU through adaptation of the doctor-doctor handover.
Methods: For this first Plan-Do-Study-Act (PDSA) cycle, a questionnaire was sent to junior doctors in order to target specific areas for improvement. A baseline audit of current handover practice was carried out between 04/03/21 and 27/05/21 over 56 separate handovers. After analysis of initial results, a ‘safety checklist’ was developed to focus on key safety information which was continually not discussed in handovers. The checklist was then adapted in response to key stakeholder feedback. This was tested on 62 further handovers from 08/06/21 until 18/07/21, with the results audited to assess impact.
Categorical outcomes were presented as proportions, and chi-squared test was used to assess significance of difference in pre- and post-intervention outcomes.
Results: The questionnaire returned 30 responses, which revealed that 45% thought all safety information was not clearly handed over. After the implementation of the safety checklist, statistically significant improvements were noted in all aspects of the handover. Key successes relating to patient factors included an increase in unstable patients being formally flagged from 23% to 90% (p < 0.001), highlighting all patients with treatment limits from 14% to 85% (p < 0.001), those with known or potentially difficult airways from 4% to 64% (p<0.001), those with life threatening allergies from 0% to 50% (p<0.001) and all expected discharges from 19% to 96% (p < 0.001). Greater situational and environmental awareness was also a key benefit, including an increased awareness of medical staffing issues from 18% to 71% (p < 0.001), an increase in both noting of the location of difficult airway trolleys from 2% to 24% (p<0.001) and the identification of the nearest airway trained doctor 18% to 89% (p<0.001) and specifically mentioning relevant infection control issues 11% to 77% (p<0.001).
Conclusions: A structured ‘safety checklist’ has been shown to be highly effective in improving the frequency with which safety information is transferred between incoming and outgoing teams on ICU. This is a simple measure which clearly returns great rewards for both patient care and staff satisfaction. Future PDSA cycles are planned to improve the uptake of the checklist and incorporate its use into standard practice.
References
1. Merten H, Galen LS van, Wagner C. Safe handover. BMJ. 2017;359. doi:10.1136/BMJ.J4328
2. Medical Council G. Good medical practice. Accessed August 15, 2021. www.gmc-uk.org/guidance.
3. Emergency and acute medical care Contents. Nice Guid. 2018;NG94. Accessed August 15, 2021. https://www.nice.org.uk/guidance/ng94/evidence/32.structured-patient-handovers-pdf-172397464671
4. Jigajinni S, Sultan P. The intensive care unit handover: The most stressful part of the shift. Br J Hosp Med. 2010;71(2 SUPPL). doi:10.12968/HMED.2010.71.SUP2.46506
P163
Reducing the risk of air embolism associated with central venous catheter use on the intensive care unit
Quality and innovation
Nazia Zahed 1 , Annabel Rogers2, Alice Sisson2 and Linsey Christie2
1Cheslea and Westminster Hospitals NHS Foundation Trust/Imperial College London
2Cheslea and Westminster Hospitals NHS Foundation Trust
Abstract
Introduction: Air embolism is a rare but potentially catastrophic complication associated with central venous access. Air may be entrained into the vascular space when a catheter is left open to the atmosphere, which can occur with inappropriate configuration of catheter seals. This patient safety initiative was prompted by a serious incident at the project site and supported by a recent safety bulletin released by the Faculty of Intensive Care Medicine (FICM). This bulletin advised that any unused taps should be closed to air and capped off with an appropriate device, with any unused lumens clamped as an additional safety measure.1
Objectives: To evaluate the configuration of central venous catheter (CVC) seals and compare this with the standards outlined in the FICM safety alert. To introduce safety and quality improvement interventions in order to reduce future risk of air embolism.
Methods: This prospective single-centre study was conducted at a 22-bed adult intensive care unit. All patients with central venous access were evaluated by snapshot daily assessment over defined 2-week periods, before and after intervention. Data collected included type of central access, number of lumens available and in use, clamp status of lumens, dividers used and their configuration, and presence of cap devices on lumens. Safety breaches for unused lumens were defined as: unused lumen unclamped; 3-way tap divider open to patient and an unused port; and an unused port left uncapped. Following the baseline data collection, octopus dividers (with built-in non-return ‘bionector’ valves) were introduced instead of 3-way taps. A staff education programme regarding the new devices occurred, which included a simulated patient model demonstrating ‘gold standard’ CVC safety measures.
Results (baseline): 101 CVCs were audited, resulting in 380 intrinsic lumens. 159 (41.8%) lumens were not in use. Of the unused lumens, 50 (31.4%) were attached to a 3-way-tap divider, and 109 (68.6%) had no divider. There were 209 unused ports. Safety breaches involving unused lumens: 26 (16.4%) unclamped, 29 (18.2%) attached to 3-way-tap open to patient and unused port, 2 (1.0%) ports were not capped with an appropriate device. There were 2 cases where composite safety breaches were observed (unclamped lumen and 3-way-tap open to patient and air, however the port was capped appropriately).
Results (following intervention): 135 CVCs were audited, resulting in 515 intrinsic lumens. 119 (23.1%) lumens were not in use. Of the unused lumens, 3 (2.5%) were attached to 3-way-tap, 38 (31.9%) to octopus dividers and 78 (65.5%) had no divider. There were 169 unused ports. Safety breaches involving unused lumens: 30 (25.2%) unclamped, and 2 (1.7%) attached to 3-way-tap open to patient and unused port. All unused ports were capped with an appropriate device. There were 2 cases where composite safety breaches were observed (unclamped lumen and 3-way-tap open to patient and air, however the port was capped appropriately).
Conclusion: The introduction of octopus dividers with built-in non-return valves resulted in a significant reduction in CVC safety breaches, compared with 3-way taps, and is now standard practice in our ICU.
References
1. Air Embolism Safety Alert [Internet]. The Faculty of Intensive Care Medicine. 2021 [cited 18 August 2021]. Available from: https://www.ficm.ac.uk/sites/default/files/air_embolism_safety_alert_sbar.pdf
P164
Maternal critical care: room for improvement?
Quality and innovation
Samuel Leafe 1 , Tiina Tamm2 and Nimisha Patel2
1Royal Berkshire Hospital NHS Foundation Trust
2Frimley Health NHS Foundation Trust
Abstract
Introduction: Critical care of the pregnant or recently pregnant woman has been discussed in detail previously with clear guidelines for organisation of the critical care service.1 The requirement for critical care in the lead up to or following delivery is likely to increase as maternal age and comorbidities increase but it still represents only a small number of cases spread over a large number of hospitals1
Objective: This retrospective audit aimed to evaluate the current service offered at a medium sized district general hospital with a 12 bed intensive care unit to identify areas for improvement.
Method: We reviewed the electronic notes of all pregnant (beyond 20 weeks) or recently pregnant (up to 6 weeks post delivery) patients admitted to intensive care across the audit period. These patients were identified using a database kept within the ICU and by a search of the maternity recording system.
Results: Over the 31 month audit period, there were 25 admissions of pregnant or recently pregnant patients. This represents a rate of 1.98 per 1000 maternities, which is similar to that previously reported, and represented 1.37 percent of total admissions to the ICU across this time. Of these, 80% were postpartum. The reasons for admission were categorised as primary obstetric (44%), secondary to deterioration of chronic medical problems (20%), related to anaesthetic complications (16%), due to acute medical pathologies (12%) or related to complications of operative delivery (8%). The most common reason for admission was following haemorrhage (36%). The mean age of patients was 31.2 years and the mean parity was 2.12. The median length of stay was 31 hours and 15 minutes (range from 11 hours and 38 minutes to 212 hours and 28 minutes). All patients survived to hospital discharge.
Most required mechanical ventilation (92%) and vasopressor support (56%) but none required additional organ support. 92% of admissions were level 3 with the remainder being level 2.
Daily obstetric review occurred for most patients (84%) but midwifery review was only documented for 28% of patients. For those with live infants, only 3 had physical contact with them while in ICU (17%).
Conclusion: This audit demonstrates a small but significant link between our obstetric and intensive care units. The majority of these admissions are short with prompt discharge back to labour ward but do require a high level of care. The significant psychological distress caused by unexpected ICU admission for these patients has been recognised in the national guidance which recommends follow up by the critical care service for all of these admissions.1 The potential to allay the psychological impact of maternal critical care admission should not be underestimated with repeated testimonials highlighting the importance of maximising maternal contact with the neonate and supporting breastfeeding.2
We will work to improve the links between the obstetric and intensive care units and aim to maximise the opportunities for maternal bonding with the newborn and ensure adequate support is offered by the midwifery team.
References
1. Quinn, A, et al. Care of the critically ill woman in childbirth. Enhanced Maternal Care; 2018
2. Dipex Charity. Conditions that threaten women’s lives in childbirth & pregnancy. 2018. Available from: https://healthtalk.org/conditions-threaten-womens-lives-childbirth-pregnancy/overview [Accessed August 22nd 2021]
P165
Innovation of eye care of the critically ill patient within ICU
Quality and innovation
Victoria Coles and Sophie McClure
Cardiff and Vale UHB
Abstract
Introduction: Quality improvement (QI) is a systemic multi-dimensional approach to ensure the care provided by health professionals is safe, effective, person-centred, timely, efficient and equitable (The Health Foundation 2013). Within critical care, standards are set by organisations to provide up to date good quality care to all patients. The author identified an increase in patient proning over the last 12 months due to the Covid-19 pandemic, resulting in a large increase in incidents of eye injury by 30%, with 2 patients receiving ophthalmology treatment and manual closure of the eye. The cases highlighted could have been potentially avoidable with a standardised approach to care.
Objectives: Patients within critical care are high risk for injury due to facial oedema, reduced conscious level and treatment interventions. The Intensive Care Society (ICS) endorsed a guideline to prevent eye injury and increase education surrounding the subject (Intensive Care Society 2020). Variability is still significantly affected in practice with the author’s unit demonstrating a low compliance compared to ICS standards of >90% compliance. The specific aim for the author’s intervention in practice was to implement changes in practice to increase compliance in line with ICS standards for eye care within critical care in 6 months.
Method: Ocular surface disease is common within the author’s practice with 20–42% of patients developing corneal epithelial defects (Johnson & Rolls 2014). Cases highlighted as ‘severe incidents of harm’ within the author’s area of practice could have been avoided with a standardised approach to care. Despite the high number of patients effected by this issue there is a severe lack of education and documentation surrounding eye care within critical care. The team implemented structured educational guidance and documentation to improve compliance within critical care to reach ICS standards. Audit of assessment, treatment and documentation of nursing notes was completed at 3, 6 and 12 month marks whilst using a formative evaluation approach which looks at the improvement project as it evolves and suggests ways in which it can be improved.
Results: Post intervention data identified an increase to 100% of patients receiving eye care. Implementation of the documentation and education to bedside nurses increased assignment of eye grade from 0% to 90% and documentation of eye care increased from 60% to 95%. 95% of nurses were confident in completing eye assessment, grading and relevant treatment compared to 0% pre intervention. Future aims are to monitor all reported eye related injuries and maintain >90% compliance in line with evidenced based practice and national guidelines.
Conclusion: The study identified a significant problem in critical care that was causing potential preventable patient harm. The results of this QI project are generalisable to other areas by increasing patient safety and staff education on the potential harm of ineffective eye care within critical care. Further research and work are required to develop awareness surrounding eye care in the critically ill.
References
1. Intensive Care Society. Eye Care in the Intensive Care Unit (ICU). Ophthalmic Services Guidance, 2020.
2. Johnson K and Roll K. Eye Care for Critically Ill Adults, Version 2. Chatswood, NSW: Agency for Clinical Innovation, 2014, pp.1–43.
3. The Health Foundation. Quality improvement made simple, 2013.
P166
“EMPOWER”: A pilot project of outpatient rehabilitation classes to address the symptoms of Post Intensive Care Syndrome (PICS)
Rehabilitation
Zoe van Willigen and Rachel Devlin
Rachel Corbett University Hospital Southampton
Abstract
Introduction: The EMPOWER (Early Mobilisation PrOject With Extended Rehabilitation) classes at University Hospital Southampton (UHS) originated in direct response to patient voice. During an interview study exploring patient and family experience of rehabilitation on ICU,1 the wife of an ICU patient stated:
“There was no point in spending all of that money on keeping him alive if you’re not gonna get him better. He’s alive, but he’s not… functioning”
Objective: To explore if post ICU outpatient rehabilitation classes can be effective in addressing symptoms of PICS, for patients previously admitted to critical care at UHS.
Methods: Funding was obtained to trial a pilot project of 8 classes over 8 weeks, starting in September 2019. Due to time constraints, original inclusion criteria were abolished and instead a convenience sample of 8 patients were selected, along with a relative if desired. Design was a 3-hour class, once a week, in a small gym venue within an acute hospital setting. Patient transport costs were covered, as had previously been highlighted as an incentive to participation in other studies.2
During the first hour of the class, former ICU patients completed an exercise circuit, while their relatives attended a separate peer support session, facilitated by experienced ICU volunteers. The second hour was an education session, provided by an ICU healthcare professional (e.g., dietitian, occupational therapist). The final hour was for peer support and goal setting.
One participant withdrew from the pilot following the first week and was signposted elsewhere. The demographic details for the remaining 7 participants represent are included in Table 1. In addition, four female relatives also participated and evaluated the pilot.
Table 1.
■■■.
| Age | Gender | Diagnosis | Ventilated Days | ICU LOS | Hospital LOS | Time from hospital d/c to EMPOWER |
|---|---|---|---|---|---|---|
| 70 | M | Surgical | 143 | 151 | 172 | 57 |
| 67 | M | Medical | 9 | 10 | 14 | 69 |
| 60 | F | Surgical | 23 | 26 | 95 | 21 |
| 49 | F | Trauma | 2 | 5 | 23 | 71 |
| 76 | M | Medical | 3 | 5 | 10 | 178 |
| 76 | F | Surgical | 0 | 4 | 60 | 425 |
| 72 | F | Medical | 5 | 9 | 32 | 242 |
Results: Outcome measures reflected the physical, cognitive and psychological domains of PICS. These were collected from assessments at week 1 and week 8, and the mean results are presented in Table 2.
Table 2.
■■■.
| Outcome Measure | Pre- EMPOWER | Post- EMPOWER | % Improvement |
|---|---|---|---|
| HAD ‘Anxiety’ | 6.8 | 5.0 | 26 |
| HAD ‘Depression’ | 6.0 | 5.4 | 10 |
| IPAT (ICU psychological assessment tool) | 8.0 | 3.0 | 54 |
| RCSQ (Richard Campbell Sleep Questionnaire) | 53.7 | 60.6 | 11 |
| TUG (Timed up and go/ seconds) | 9.8 | 6.9 | 30 |
| Pain (VAS score/10) | 3.8 | 2.6 | 32 |
| Grip strength/ kg | 17.3 | 25.3 | 32 |
| SF36 Physical Function | 40 | 65 | 38 |
| SF36 Role- Physical | 7.1 | 39.2 | 82 |
| SF36 Role- Emotional | 19 | 66.5 | 71 |
| SF36 Social function | 53.5 | 80.4 | 33 |
| MOCA (Montreal Cognitive Assessment) | 22.2 | 28.1 | 21 |
| 6MWT (Six-Minute Walk Test/m) | 329 | 410 | 19 |
In addition, qualitative data was collected before and after the 8-week course. Examples of quotes from participants at the start of the pilot include:
“I have reduced my working hours to spend more time at home with her”
“I feel dreadful. I ’ m not getting better. I lose words mid-sentence, and have memory problems”
Feedback following the pilot was very positive. One participant reported:
“It’s been a safe space for me, as a ‘carer’, to express my fears and concerns and to get help, advice and support from people who really understand the issues of post-ICU recovery. Our GP practice really doesn’t seem to provide any after-care/ follow up care for this.”
Conclusion: In this small pilot project of post ICU outpatient rehabilitation classes, all outcome measures improved despite participant heterogeneity. Patient/ relative satisfaction for the classes was high. We have since managed to secure £30k through the Q Exchange to continue the work of EMPOWER following the COVID-19 pandemic.
EMPOWER video link: https://www.youtube.com/watch?v=1-2fmmXn4eo
References
1. van Willigen Z, Ostler C, Thackray D, Cusack R. Patient and family experience of physical rehabilitation on the intensive care unit: a qualitative exploration. Physiotherapy. 2020;109:102-110. doi: 10.1016/j.physio.2020.01.003. Epub 2020 Feb 4. PMID: 32317118.
2. Connolly B, Thompson A, Douiri A, Moxham J, Hart N. Exercise-based rehabilitation after hospital discharge for survivors of critical illness with intensive care unit-acquired weakness: A pilot feasibility trial. Journal of Critical Care. 2015;30(3):589-598. https://doi.org/10.1016/j.jcrc.2015.02.002
P167
Case study of a long term ICU patient requiring ECMO following COVID-19 related respiratory failure
Rehabilitation
Allaina Eden and Jason Lattimer
Royal Papworth Hospital
Abstract
Introduction: Due to the COVID-19 pandemic there has been an unprecedented number of hospital and Intensive Care Unit (ICU) admissions for respiratory failure. This has required a significant and sudden increase in ICU capacity.1,2 Due to severe pulmonary infection and inflammation, patients have presented with acute respiratory distress syndrome (ARDS) with an associated inability to ventilate lungs with poor compliance. This has led to an increased requirement for extra corporeal membrane oxygenation (ECMO) support. This is only available in six commissioned centres across the United Kingdom.3
Objectives: The objective of this abstract is to present a case study of a long-term patient in ICU with a prolonged duration on ECMO. This abstract highlights the complex, mutli-dimensional physiological and psychological impact of recovery and rehabilitation in patients following a severe physical illness.
Methods: Figure 1 shows the timeline of significant events during the patient’s hospitalisation and admission at the ECMO centre.
Figure 1.
▪▪▪.
Due to the nature of a long ICU admission, the patient’s condition fluctuated throughout their stay. Rehabilitation was impacted physically by the patient’s limited ventilatory reserve caused by lung damage due to COVID. A severe sacral moisture lesion also limited their ability to sit in a chair for longer than one hour and perform sustained sitting on the edge of the bed activities. Psychologically the patient was limited due to significant anxiety and agitation. There were a number of barriers and challenges to rehabilitation whilst the patient was on ECMO as well as post ECMO decannulation. These challenges are detailed in Figure 2.
Figure 2.
▪▪▪.
Results: Despite the challenges, the patient was able to participate in physical rehabilitation and was provided psychological support by the psychology team. At their peak ability, the patient was able to perform 12 steps with maximal assistance of three staff. The patient’s Chelsea Critical Care Physical Assessment Tool (CPAx) scores can be seen in Figure 3.
Figure 3.
▪▪▪.
There was marked difference in the patient’s ability to meet the physiological demand of rehabilitation with the ECMO support and without. Following ECMO decannulation the patient struggled with fatigue, hypercapnia and increasing dependency on the ventilator. These issues led to a decline in ability and longer periods of tachypnoea and recovery.
Conclusion: Supporting patients after a critical illness requires physical and psychological rehabilitation from the whole MDT. This example of a patient’s recovery both during and post ECMO support due to COVID-19 shows the complex relationships affecting the patient’s ability to improve and progress.
References
1. UK. Coronavirus (COVID-19) in the UK. Available from: https://coronavirus.data.gov.uk/details/healthcare[Accessed 7th August 2021].
2. NHS England. COVID-19 Hospital Activity. Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-hospital-activity/ [Accessed 7th August 2021].
3. NHS England. Management of surge and escalation in critical care services: standard operating procedure for adult respiratory extra corporeal membrane oxygenation. Available from: https://www.england.nhs.uk/wp-content/uploads/2017/11/Management-of-surge-and-escalation-for-adult-respiratory-extra-corporeal-membrane-oxygenation-revised.pdf [Accessed 7th August 2021].
P168
A case study reflecting on the physiotherapy input with a patient who received extracorporeal membrane oxygenation (ECMO) support following COVID-19
Rehabilitation
Jason Lattimer and Allaina Eden
Royal Papworth Hospital
Abstract
Introduction: The COVID -19 pandemic presented a new range of challenges to clinicians across the world in caring for patients affected by a virus with what at the time was an unknown pathophysiology.1 In meeting this challenge physiotherapists utilised their knowledge and experience in treating patients with acute respiratory distress syndrome (ARDS) to provide the best possible care.
Objectives: The aim of this paper is to review and reflect on physiotherapy treatment for a patient with COVID – 19 who received ECMO support, from admission to discharge home.
Methods: A case study design to provide a detailed review of the treatments used with the patient during their journey, including feedback from the patient. Figure 1 outlines a timeline of key events during their patient journey.
Figure 2.
The Physiotherapy interventions used can be seen in Figure 2
Figure 1.
The Physiotherapy interventions used can be seen in Figure 2
Results:
• Historically the Physiotherapy team within the ECMO centre have believed that chest physiotherapy would be mostly ineffective on patients with low lung volumes. However, in this case study it was shown that with tidal volumes of between 30 – 100mls, expiratory vibrations with saline instillation and suctioning cleared more secretions then suctioning alone.
• Despite the use of foot splinting whilst sedated we still faced challenges with contractures in calves which subsequently limited standing.
• Effective and safe use of SOEOB and tilt-table built up-to standing with support whilst having ECMO in situ.
• The use of PMV whilst ventilated allowed the wider MDT to provide effective support for the patient’s overall wellbeing. The use of PMV was timed with chaplaincy and psychology input, in addition to enabling two-way communication during video and phone calls with the patient’s wife, who at the time was unable to visit due to restrictions. Patient feedback on the use of the PMV “To be able to communicate normally was wonderful, as you are locked into a world where no one understands you and it can be so frustrating to make people understand what you want”.
Conclusions: The patient was successfully weaned from the ECMO, ventilator and tracheostomy was de-cannulated; they were transferred back to their local hospital for ongoing rehab and were eventually discharged home.
This case study introduces a debate as to the effectiveness of manual techniques and suctioning with saline on patients with low lung volumes as it appeared to be beneficial compared to suctioning alone.
The use of the PMV within the ventilator circuit enabled vocalisation much earlier during their admission which not only progressed their swallowing and cough strength rehabilitation but also significantly increased the amount of psychological support they were able to access.
On reflection it seemed appropriate to utilise similar rehabilitation treatment options used in the management of ARDS patients on ECMO, despite the challenges associated with the complex logistical and safety factors when managing this patient group.
References
1. Kumar M, Al Khodor S. Pathophysiology and treatment strategies for COVID-19. Journal of Translational Medicine. 2020; 18(1).
P169
Empowering Patients Post Intensive Care EPPIC
Rehabilitation
Eilis Macleod 1 and Ann Mc Queen2
1Belfast Trust
2Belfast Health & Social Care Trust
Abstract
Introduction: Post Intensive Care Syndrome (PICS) will be the next public health crisis that will occur when the COVID-19 crisis settles. PICS is characterized by physical strength deficits, cognitive decline, and mental health disturbances observed after discharge from critical care that persist for a protracted amount of time.1 Approximately 50% of all the patients, across all ages, admitted to ICU requiring mechanical ventilation develop PICS.The rehabilitation after Critical illness in Adults Guidelines (NICE 2009)2 has led to a change in practice and encouraged exercise in the post-hospital discharge phase however this has not yet been implemented in N.I.
The COVID-ICU team in Belfast HSC Trust established a follow-up service to enhance the physical and psychological recovery of this patient cohort. An MDT including intensive care medicine, Physiotherapy, clinical psychology, pharmacy, speech and language therapy, and dietetics was established.
Methods: A pilot exercise group, EPPIC, was populated from the clinic and referrals were made into the exercise class through SOP (Standard Operating Procedure). Aims of the class were to:
1. improve the individual’s functional capacity through structured exercise
2. utilise the carry over psychological and cognitive benefits gained from exercise
3. empower the patients to start their sickness to wellness journey.
Virtual classes ensured the service captured the regional aspect of the patient cohort. The classes ran for 6 weeks, twice weekly. Exercise prescription was achieved through the FITT principles: frequency, intensity, time, and type of exercise.3 Identification of optimal exercise dose was crucial for maximising results and was achieved through thorough pre-assessment and risk stratification in the SOP.
The classes consisted of functional movements and thus functional training. Typical exercise plans post icu consist of isolation movements with no purpose and function in mind. A functional workout consists of compound exercises like squats, lunges, and deadlifts which require more than one muscle group to work and mimic everyday movement patterns like pull, push, squat, hinge and rotation. By training multiple muscle groups at the same time, it is time-efficient, aids the body to move as a system and enabled the patients to improve function in everyday activities.
Results: The first cohort of patients’ functional capacity improved by 42% and 40% respectively in one min sit to stand and DASI (Duke Activity Status Index) scores. Patient satisfaction scores returned a 5-star excellence rating. Patient feedback stated as each week passed, they could feel themselves getting stronger and more flexible. The second cohort of patients produced similar results with functional capacity improving by 30% and 32% respectively in one min sit to stand and DASI and fatigue scores improved by 24%.
Conclusions: Lancet et al4 reported at 6 months after acute infection, COVID-19 survivors were troubled with fatigue or muscle weakness, sleep difficulties, and anxiety or depression. It is evident that a post icu clinic and appropriate rehabilitation pathways are vital for post ICU, covid and non-covid patients. As mentioned, there is no provision made for this service within the Belfast trust. Results from the pilot showed gains in both cohorts with minimal cost and minimal equipment. “There are only two requirements when it comes to exercise. One is that you do it. The other is that you continue to do it.” Dr Jennie Brand-Millar
References
1. Elliott D, Davidson JE, Harvey MA, Bemis-Dougherty A, Hopkins RO, Iwashyna TJ, et al. Exploring the Scope of Post–Intensive Care Syndrome Therapy and Care. Critical Care Medicine. 2014;42(12):2518–2526.
2. Overview | Rehabilitation after critical illness in adults | Guidance | NICE [Internet]. Nice.org.uk. NICE; 2009 [cited 2019 Oct 30]. Available from: http://www.nice.org.uk/guidance/CG83
3. American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. 10th edition. Lippincott Williams & Wilkins; 2017.
4. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. The Lancet [Internet]. 2021. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)32656-8/fulltext
P170
Impact of a multi-disciplinary intensive care rehabilitation team on ventilator days, length of stay and physical function in a mixed intensive care population
Rehabilitation
Connie Snell 1 , Harriet Shannon2 and Carol Montgomery3
1Somerset NHS Foundation Trust
2University College London
3Lewisham and Greenwich NHS Trust
Abstract
Introduction: Adverse consequences of critical illness are well reported, and include physical, psychological and social effects that can last for years post discharge (Needham et al. 2012). Access to physiotherapy and early rehabilitation have helped to address the physical deterioration experienced by patients in intensive care. The role of other multi-disciplinary team members such as occupational therapy (OT), speech and language therapy (SLT) and psychology is less well defined, but has the potential to support and enhance rehabilitation since they offer alternative, complimentary perspectives.
Objectives: This service evaluation sought to investigate the impact of a multi-disciplinary rehabilitation team on intensive care length of stay, ventilator days and functional ability at the point of discharge.
Methods: The project was registered with the local NHS Trust clinical governance team. Retrospective data were collected at two points, prior to and post implementation of the multi-disciplinary rehabilitation team. Inclusion criteria were adults intubated and ventilated for more than four days requiring active treatment. Those with a long-term tracheostomy or laryngectomy or needing an inter hospital transfer were excluded. Electronic notes were retrospectively extracted to gather demographics, rehabilitation needs, intensive care length of stay, ventilator days and Chelsea Critical Care Physical Assessment (CPAx) scores at admission and discharge.
Results: In total, 589 patients were admitted to intensive care across the two time points. OF these 49 were eligible for inclusion in the pre-implementation group (T1) and 45 in the post-implementation group (T2). There were no statistically significant differences in patient characteristics between patient groups. Patients presented with a range of medical, neurological and respiratory pathologies, with a minority admitted for elective or emergency surgery. Patients in T2 only received physiotherapy, compared to those in T2 who were assessed and treated by OT, SLT and care managed by the rehabilitation coordinator. Joint sessions were completed where appropriate.
There was no statistically significant difference in intensive care length of stay or ventilator days between the two groups. Median (interquartile range) for length of stay and ventilator days were 13 (8-22.5) vs. 14 (10-30) and 9 (5.5-11.5) vs. 10 (6-28.5) days for pre-implementation and post-implementation groups respectively (p=0.163 and p=0.202). There was a statistically significant difference in functional ability (measured by CPAx) at discharge (p=0.037). Patients in the post-implementation group had a median change in score from baseline of 16, compared with 13 in the pre-implementation group (p=0.037). Multiple regression suggested that patient age, frailty, pathology and rehabilitation group made a significant contribution to variance in CPAx score, explaining 18% variance (p=0.033)
Conclusion: The multi-disciplinary rehabilitation team did not significantly impact intensive care length of stay of ventilator days. However, patients receiving multi-disciplinary rehabilitation benefited from the improved physical function at discharge. This suggests that the effects of rehabilitation can be amplified when a wider team is involved. This work was undertaken during the Covid-19 pandemic, where discharge and timely patient flow was severely disrupted. Further research is required to explore further the impact of this innovative approach to the rehabilitation in intensive care.
References
1. Needham, D.M., Davidson, J., Cohen, H., Hopkins, R.O., Weinert, C., Wunsch, H., Zawistowksi, C., Bemis-Doughtery, A., Bernry, S.C. and Bienvenu, O.J.J.C. 2012. Improving long-term outcomes after discharge from intensive care unit: report from stakeholders' conference. 40, 502-509.
P171
Time taken to wake post sedation hold and the impact on functional performance at intensive care unit (ICU) discharge: Do COVID rehabilitation phenotypes exist?
Rehabilitation
Claire Bradley 1 and Charles Reilly2
1Kings College Hospital NHS Foundation Trust
2Kings College Hospital
Abstract
Introduction: The COVID-19 pandemic caused a sudden and unprecedented surge in ICU admissions for severe acute respiratory failure. Whilst there is a wealth of knowledge surrounding risk factors for developing critical care myopathy and effects of prolonged ICU stay on functional outcomes,1,2 little was known about the pathophysiology, treatment or physical outcomes of patients admitted to ICU with COVID-19. In our organisation, patients recovering from the acute phase of COVID-19 demonstrated a range of presentations impacting rehabilitation whist in ICU.
Objective: To explore whether time taken to wake post sedation hold impacts on functional outcomes of patients surviving ICU admission for COVID-19.
Methods: A retrospective review of patients admitted to ICU with a primary diagnosis of COVID-19 between March-April 2020 was conducted at a large London NHS Foundation Trust. Electronic clinical notes were reviewed and the following data extracted: age, ethnicity, sex, BMI, pre-admission clinical frailty score, duration of sedation, days taken to wake from sedation, duration of mechanical ventilation (MV), ICU length of stay (LOS) and hospital LOS. Functional outcomes were defined using the Intensive Care Unit Mobility Score (ICUMS). Data were analysed using descriptive statistics, reported as absolute numbers, percentages (%) and median (range).
Results: 203 patients were identified, 137 were excluded as 58 died, 3 were incidental findings of COVID-19, 67 had missing data due to paper notes or transfers in/out of the Trust and 9 were duplicate records. Sixty-six patients were included in the final analysis (Table 1).
Table 1.
Characteristics of each rehabilitation group.
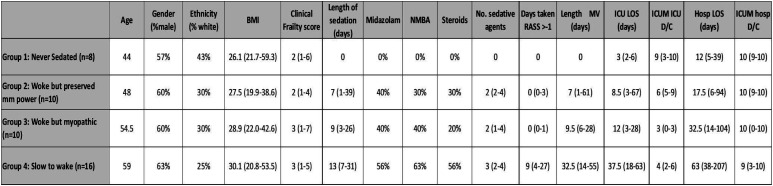
|
Patients could be categorised into four rehabilitation groups:
1 = Never requiring sedation and MV,
2 = Woke from sedation (defined as RASS ≥-1) within 72 hours with preserved muscle power (defined as ICUMS ≥5 on ICU discharge),
3 = Woke from sedation within 72 hours but myopathic (defined as ICUMS ≤4 on ICU discharge),
4 = Slow to wake (> 72 hrs).
Those slow to wake following sedation hold (group 4) had an increased age, BMI, and higher proportion of non-white ethnicity.
Neuromuscular blocking agents (NMBA) and steroid use was more prevalent in group 4 compared to the other groups. There was also increased midazolam administration and higher number of total sedative agents received by these patients.
Those slow to wake had a lower ICUMS at ICU discharge than those waking with preserved strength or never sedated (3, 6, 9 respectively). Those who were slow to wake were ventilated for longer than the other groups. Time taken to wake from sedation also resulted in longer ICU and hospital LOS. Similar functional outcomes at hospital discharge were noted between all 4 groups (Table 1).
Conclusion: Patients slow to wake from sedation following ICU admission for a primary diagnosis of COVID-19 had a longer ICU LOS, reduced functional ability at ICU discharge and a longer hospital LOS.
These preliminary observational clinical data support the testable hypothesis that within in the ICU, COVID rehabilitation phenotypes may exist which warrants further investigation.
References
1. Vanhorebeek I, Latronico N, Van den Berghe G. ICU-acquired weakness. Intensive Care Medicine. 2020;46(4):637-653.
2. Lad H, Saumur T, Herridge M, dos Santos C, Mathur S, Batt J, et al. Intensive Care Unit-Acquired Weakness: Not Just Another Muscle Atrophying Condition. International Journal of Molecular Sciences. 2020;21(21):7840.
P172
Chelsea Critical Care Physical Assessment scores and tracheostomy weaning in cardiothoracic critically ill patients: a retrospective observational study
Rehabilitation
Alicia Page
Royal Papworth Hospital NHS Foundation Trust
Abstract
Introduction: Chelsea Critical Care Physical Assessment tool (CPAx) is a bedside objective tool designed to measure function in critical illness. CPAx has demonstrated validity, reliability and responsiveness, and is widely used, in the critical care population.1 Martin et al2 looked at responsiveness and construct validity of the Chelsea Critical Care Physical Assessment Tool in a cardiothoracic intensive care unit (ICU). They found that CPAx is able to detect clinically important changes in patients’ physical function throughout their hospital stay suggesting good responsiveness. There have been no studies to date that investigate whether there is a relationship between tracheostomy weaning and CPAx score increasing with rehabilitation.
Objective: This retrospective study investigates if a relationship exists between an increasing CPAx score and tracheostomy weaning. Secondary aims include whether an increasing CPAx score indicates when a patient may be ready for decannulation. If there is a relationship between CPAx score and tracheostomy weaning, does this relationship change depending on present condition causing critically illness, i.e. medical or surgical admission?
Methods: A six month retrospective data collection was completed from June 2020 to December 2020, with data collected from the physiotherapist’s electronic notes on Metavision. Inclusion criteria comprised of patients admitted to Royal Papworth Hospital NHS Foundation Trust (RPH) ICU over the 6-month period, requiring tracheostomy insertion. All patients were over 18 years old, had a COVID-19 negative status and must have stayed on ICU for 3 days or more with a tracheostomy (n=28). A negative COVID-19 status was stipulated as the CPAx score has not yet been validated in COVID-19 positive patient group.3 As there is no formalised outcome for tracheostomy weaning a 0-5 scale was created to gain a numerical value of weaning.
Results: Of the 28 patients, 23 patients survived RPH ICU stay; 5 patients died. 14 of the 28 patients were decannulated during their RPH ICU admission, and 9 patients were repatriated to their local hospital prior to decannulation. Spearman’s Rank Correlation Coefficient were applied to the data sets, showing a positive correlation between CPAx score and tracheostomy weaning (CI set at 95%, p = 0.01, r=0.79). Medical cardiothoracic patients e.g. pneumonia and cardiology patients, appear to have a stronger positive correlation (r=0.84) with CPAx and tracheostomy, than surgical cardiothoracic patients (r=0.73).
Conclusions: An increasing CPAx score and improvements in tracheostomy weaning have a strong positive correlation, stronger with medical than surgical cardiothoracic critically ill patients. Although a positive correlation is demonstrated, there was inadequate data to indicate that CPAx scores could be used to indicate when a patient may be ready for decannulation. Prospective research is warranted to investigate the relationships further.
References
1. Corner E, Soni N, Handy J M and Brett S J. Construct validity of the Chelsea critical care physical assessment tool: an observational study of recovery from critical illness. Critical Care 2014; 18:1-10.
2. Martin N, Meehan C, Curran R, Dowling K, Purkiss C, Corner. Responsiveness and Construct Validity of the Chelsea Critical Care Physical Assessment Tool in a Cardiothoracic ICU. In: Intensive Care Society State of the Art 2019.
3. Sire A, Giray E, Taskiran O. Chelsea physical assessment tool for evaluating functioning in post‐intensive care unit COVID‐19 patients. J Medical Virology. 2021;1–3.
P173
Evaluating the use of the FIM FAM as an outcome measure for a new Occupational Therapy service in Critical Care
Rehabilitation
Tom Glithero and Helen Turner
Blackpool Teaching Hospitals NHS Foundation Trust
Abstract
Introduction: Intensive care provides treatment and monitoring of patients who are critically unwell. Recent research1 indicates that due to the seriousness of their condition these patients are at high risk of cognitive, physical, and psychosocial impairments. The Royal college of Occupational therapists2 state Occupational Therapists (OT’s) provide holistic assessment and treatment designed to help people regain their independence following illness, accident or aging and are uniquely trained in both mental and physical health. As emphasised by Coster3 it is essential that an appropriate outcome measure is used to show the impact of the service, allowing a measure of progress over time and evidence of impact to commissioners. The Functional Independence Measure/Functional Assessment Measure (FIM/FAM) was selected as it provides a valid and reliable measure of physical, cognitive, communication and psychosocial function. The tool scores 30 individual categories split into motor and cognitive items from 1-7 with 1 being total dependence and 7 complete independence, flow charts are provided to indicate scores, and these are then collated to provide a total, motor, and cognitive change in patient.
Objectives: To examine how the FIM/FAM was implemented as an outcome measure for a new critical care OT service.
Method: Data was collected for patients admitted to critical care, scores were then recorded on admission, where goals were set and then on discharge from critical care. This data was reviewed in team meetings to establish how it should be collected, analysed, measured, and reported.
Results: Data was collected from 38 patients during a 4-month period. Following this period of evaluation, a discussion was carried out between OT’s and the following aspects were considered learning outcomes:
• Use of specific flow charts provided for each category increased accuracy.
• The time needed to complete the scores was more than other outcomes measures (barthel index, Austoms etc).
• Data from deceased patients and patients transferred to other hospitals should not be included in reported statistics to avoid misrepresentation of therapy input.
• Scores should be recorded following functional assessment rather than point of referral as patients are often sedated at this point, producing inflated therapy input.
• Report data monthly, this covers admission for most patients and mirrors other data collection.
• The categories focus therapy and guide interventions, enabling more holistic treatment plans
Conclusion: While the FIM/FAM provides an accurate measure of change in patients motor and cognitive skills it takes time to complete. This is exacerbated by using the flow charts provided however, their use increases reliability and accuracy while also developing confidence in its use. As confidence and understanding of the tool increased the data begins to indicate possible areas of improvement and direct therapists’ interventions. The tool has provided a good level of information to support a new OT service in critical care however further investigation is needed to gain an accurate understanding of the impact it is having on patient care.
Reference
1. Costigan, F., Duffett, M., Harris, J., Baptitse, S. and Kho, M. (2019) Occupational Therapy in the ICU: A Scoping Review of 221 Documents. Critical Care Medicine, 47:2
2. Coster, W (2013) Making the Best Match: Selecting Outcome Measures for Clinical Trials and Outcome Studies. The American Journal Of Occupational Therapy 67:2
3. Royal college of Occupational therapists (2019) What is occupational therapy? https://www.rcot.co.uk/about-occupational-therapy/what-is-occupational-therapy [Accessed on 16/8/21]
P174
Retrospective audit of ED attendances in intensive care patients to prognostic outcome.
Rehabilitation
Adam Clements, Aditya Kuravi, Ganesh Rajaratnam and Xana Marriot
Walsall Manor Hospital - Walsall Healthcare NHS Trust
Abstract
Introduction: The aim of the audit was to assess the frequency of Emergency Department (ED) attendances before and after Intensive care and correlate this with functional decline and worsening comorbidities. Though the Covid 19 pandemic has highlighted this more starkly1 the implications of prolonged ICU care and increased long term care needs is well established.2
Objectives: A well-structured, comprehensive, multidisciplinary rehabilitation program during and after discharge from the hospital could improve outcomes and prevent further hospital/ED visits.
Method: Data was collected using the ITU admission data base for all > 72 hour ITU patient stays over a two year period of 2017-2018 and 2018-2019 in a district general hospital in the UK. Each individual patient’s number of same hospital ED attendances for twelve months before and after their ITU admission were reviewed and the causes for them assessed, in addition survival data over a two year period was also reviewed.
Results: During 2017-2018 and 2018-2019 a total of 414 and 425 patients were admitted respectively to ITU for more than 72 hours (median= 133.5 hours). Of the total 839 ITU admissions 700 (83.4%) survived ICU stay. 165 (23.6%) of the 700 patients died in subsequent 2 years of ITU discharge. The two year survival rate was 65%.
The most common ITU admissions reason was post-operative monitoring (20%) followed by Type 1 respiratory failure (18%) and Type 2 respiratory failure (15%). The median ED attendance was 0 (Range 0 to 29, mean 0.985, S.D 3.985) in the 17-18 and 0 (Range 0 to 24, mean 1.153, SD 2.154) in the 18-19 cohort in the 12 months prior to ITU admission while the median ED attendance was 0 (Range 0 to 15, mean 0.980, S.D 4.4) in the 17-18 and 0 (Range 0 to 15, mean 1.19, SD 2.0) in the 18-19 cohort in the 12 months following the ITU admission. 98% for 17-18 and 72% for 18-19 of ED reattendances following prolonged ITU stay were due to reasons similar to ITU care. Of the 445 patients with no prior ED attendance in 1 year, 168 or 38% (range 1 to 14) had at least one ED attendance in the 12 months following ITU discharge. The remaining 394 patients with at least one ED attendance prior to ICU, 185 or 47% (1 to 15 Range) had ED attendance 12 months following their ITU discharge.
Conclusion: The results show that ITU admitted patients consume significant health resources before and after their ITU stay. Patients with no prior ED attendances before ITU admission also reattended in substantial numbers. Most of these attendances were related to their initial reason for ITU admission. A comprehensive rehabilitation program both in hospital and following discharge could improve patients’ outcomes, reduce stress on emergency services and improve patient experience. A rehab service was implemented. The need for rehab program for Covid 19 patients during the pandemic has grown immense because of evolving evidence of Long Covid.3
References
1. Curci C, Negrini F, Ferrillo M, et al. Functional outcome after inpatient rehabilitation in postintensive care unit COVID-19 patients: findings and clinical implications from a real-practice retrospective study. Eur J Phys Rehabil Med 2021; 57(3):443-450.
2. Chelluri L, Im KA, Belle SH, et al. Long-term mortality and quality of life after prolonged mechanical ventilation. Crit Care Med 2004;32(1):61-69.
3. Moreno-Pérez O, Merino E, Leon-Ramirez JM, et al. Post-acute COVID-19 syndrome. Incidence and risk factors: A Mediterranean cohort study. J Infect 2021;82(3):378-383.
P175
Prone positioning plexopathies – a retrospective case series
Rehabilitation
Ella Wisken and Laura Grimsey
Norfolk and Norwich University Hospital
Abstract
Introduction: Due to the COVID-19 pandemic, and increased use of prone positioning, there has been an increase in observed plexopathies.
Objectives: To retrospectively analyse data of all COVID-19 admissions to the ICU of an acute hospital, to identify both the prevalence and risk factors for nerve injuries post prone positioning. As well as reviewing current guidance to facilitate best practice and optimise rehabilitation following nerve injury.
Methods: Data from the Norfolk and Norwich University Hospital, a large teaching hospital, was retrospectively collected from the hospitals electronic clinical records system. Data was reviewed for all COVID-19 patients admitted from March-June 2020 and October 2020-March 2021. Patients with nerve injuries were diagnosed from physiotherapy assessment as there were no electrophysiology studies available.
Results: 45 patients were admitted during the first wave. Of these, 1 peroneal nerve injury was identified (2.2% of all patients). Throughout the second wave 225 patients were admitted, with 10 isolated nerve injuries identified in 7 patients. These included 6 lower limb injuries (peroneal nerve) and 4 upper limb injuries (brachial plexus or ulnar nerve). This equates to 3.1% of patients. All these patients were nursed prone during their ITU admission, and no nerve injuries were found in patients who were not proned.
Characteristics of the patients can be seen in Table 1.
Table 1.
Patient Characteristics.
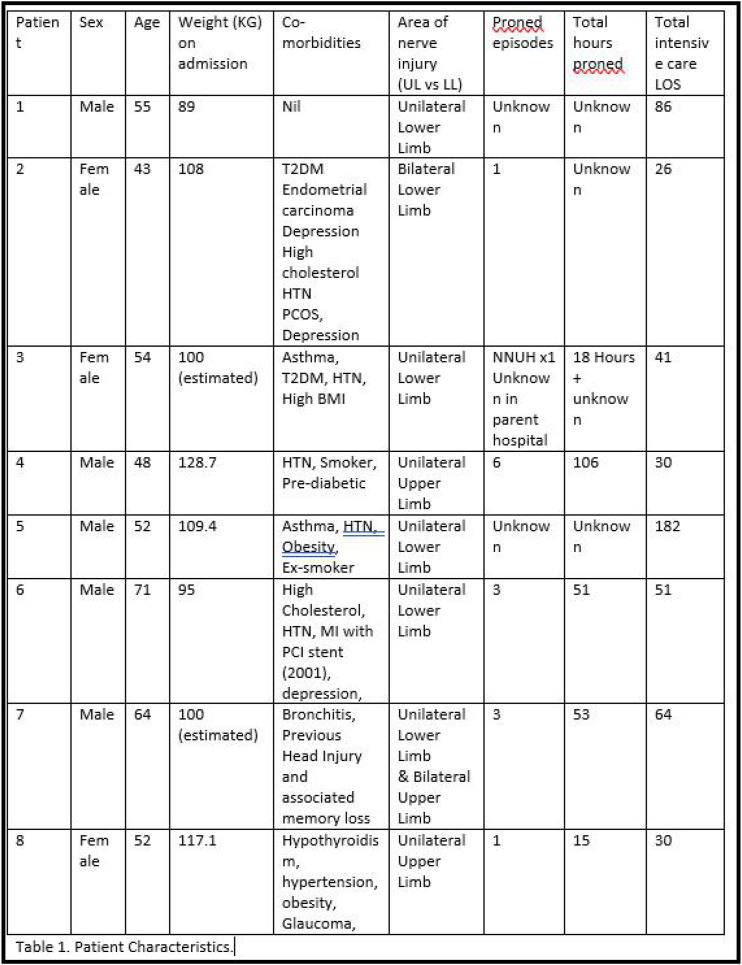
|
In comparison, Miller et al. (2021) found 5.9% of all COVID-19 patients admitted to a large UK hospital suffered an upper limb nerve injury. Malik et al. (2020) found nerve injuries (upper and lower) in 14% of patients. However, both studies took place in rehab settings, not acute.
On average, nerve injuries were diagnosed on day 26 of admission. Early diagnosis is difficult due to prolonged sedation, delirium, and ICU-acquired weakness masking nerve injuries. Therefore, it is likely that the incidence of injury is higher than demonstrated in this series.
Data was missing for 4 patients who were transferred in from other ICUs in the region. However, number of prone episodes varied from 1 to 6, and total hours spent in prone varied from 15 to 106.
Conclusion: This case series demonstrates that nerve injuries are a consequence of prone positioning. Although a very small sample, there seems to be no relation to the frequency of proning or the number of hour’s proned.
Achieving optimum positioning to avoid complications is imperative. This was likely made more difficult in the pandemic due to the cohort of patients (high BMI, large number of co-morbidities) and undue stress with temporary surge support staff and an extreme number of patients.
Guidance has now been published for positioning to avoid brachial plexus injuries (Quick & Brown, 2020). However, there is no guidance published regarding lower limb injuries, which in this case series were more common. In our trust we are in the process of adjusting our proning SOP accordingly to include the above guidelines, as well as an awareness of lower limb positioning to avoid compression or traction. It is important that there is a clear individualised pathway in place.
References
1. Malik GR, Wolfe AR, Soriano R, Rydberg L, Wolfe LF, Deshmukh S, Ko JH, Nussbaum RP, Dreyer SD, Jayabalan P, Walter JM. Injury-prone: peripheral nerve injuries associated with prone positioning for COVID-19-related acute respiratory distress syndrome. BJA: British Journal of Anaesthesia. 2020;125(6):e478.
2. Miller C, O'Sullivan J, Jeffrey J, Power D. Brachial plexus neuropathies during the COVID-19 pandemic: a retrospective case series of 15 patients in critical care. Physical therapy. 2021;101(1):pzaa191.
3. Quick TJ, Brown H, Unit PN. A commentary on prone position plexopathy during the COVID-19 pandemic. British Orthopaedic Association. 2020.
P176
Length of Critical Care Admission Compared to Physical Outcome on discharge from the unit, and Hospital Discharge for C-19 Patients in a Regional Surge Centre
Rehabilitation
Laura Grimsey, Toni Bladon and Helena
Daniell Norfolk and Norwich University Hospital
Abstract
Introduction: Increasing length of stay on critical care is directly associated with increased ICU acquired weakness (ICU-AW) and poorer physical outcomes.1 The Manchester Mobility Score (MMS) has been shown to be a valid and reliable measure of physical function within the intensive care unit, see Table 1.2
Table 1.
Manchester Mobility Score
| 1 | Passive movements, active exercise, chair position in bed |
| 2 | Sit on edge of bed |
| 3 | Hoisted to chair |
| 4 | Standing practice |
| 5 | Transfers with assistance |
| 6 | Mobilising with or without assistance |
| 7 | Mobilising >30m |
| A | Agitated |
| U | Unwell |
Objectives: To establish if the length of critical care stay of COVID-19 patients in a regional surge centre was related to functional ability on discharge, evaluated using the Manchester Mobility Score (MMS) and to compare length of critical care stay with subsequent discharge destination when they left hospital.
Method: This was a retrospective review of critical care patients admitted with COVID-19 between October 2020 and March 2021. Data was extracted from the electronic patients records and inputted into an Excel spreadsheet.
For all patients who survived their critical care admission comparisons were made between; total LOS and their physical outcome on transfer to the ward as evaluated by the MMS and; LOS and discharge destination from hospital.
Results: 206 patients were reviewed, 1 was excluded due to incomplete data and 71 died prior to critical care discharge. Median LOS was 15 (2-145) days.
For this cohort the opposite was seen with the highest incidence of low scores (lower physical function) was found with the shortest LOS (1-5 days) and the majority of patients with higher MMS scores was found with a LOS 6-10 days, this is the opposite to what we may expect for this group. For the patients with a LOS exceeding 31 days the median (range) MMS score was 4 (3-6), with no patients scoring in the lowest 2 brackets.
79% of patients were discharged home followed by 11% to in patient rehabilitation facilities. Of those patients that were discharged home (n=106), 22% had a critical care LOS of 0-5 days and 51% had a critical care LOS of 6-10 days. For patients who were transferred to in-patient rehabilitation (n=11), 55% had a critical care LOS of 31 days or more.
Conclusion: In this review all patients on discharge from the Critical Care unit scored 3 or over on the MMS, which was only possible due to the redeployment of Physiotherapy staff and the joint effort from all of the staff working in Critical Care over the surge period. Patients who survived their admission were most likely to be discharged home. Unusually patients with a shorter length of stay in Critical Care had poorer scores on the MMS on discharge from Critical Care, which is unusual. This maybe due to the increased focus on the patients who were slow to wean and who required more Physiotherapy input.
In terms of discharge destination, a LOS of less than 10 days suggested a higher likelihood of discharge home and a LOS of longer than 31 days was associated with a higher likelihood of the patient being discharged to an in-patient rehabilitation facility. This is more representative of the usual clinical outcomes seen in the critical care cohort.
References
1. Vanhorebeek, I., Latronico, N. and Van den Berghe, G. ICU-acquired weakness. Intensive Care Med 46, 637–653 (2020). https://doi.org/10.1007/s00134-020-05944-4
2. Mcwilliams D, Atkins G, Hodson J, Boyers M, Lea T, Snelson C. Is the manchester mobility score a valid and reliable measure of physical function within the intensive care unit. Intensive Care Med Exp. 2015;3(Suppl 1):A553. doi:10.1186/2197-425X-3-S1-A553
P177
The development of a Specialist Rehabilitation Pathway in Neuro Intensive Care (‘SPIN’). An evaluation of staff perceptions
Rehabilitation
Nicola Seal 1 , Julie Buckley2, Stuart Fraser2, Roger Lightfoot2, Vanessa Sims2 and Stephanie Heslop3
1University Hospital, Southampton NHS
2University Hospital Southampton
3University Hospital Southampton, NHS
Abstract
Introduction: It is well documented that early rehabilitation in General Intensive Care is safe and effective.1 However, there is a paucity of evidence to support early rehabilitation for patients in Neuro Intensive Care, with no established consensus in the United Kingdom. Furthermore, patients with a neurological diagnosis are often excluded from early mobility studies.2
Early rehabilitation in Neuro Intensive Care is a challenging clinical conundrum, requiring a high level of multidisciplinary collaboration, expertise and communication. The complexities of avoiding secondary brain injury and the challenges of rehabilitating patients with neurological deficits often complicates early intervention.2
There is a need to focus on optimising patient recovery in Intensive Care with a co-ordinated rehabilitation approach. A recent publication3 highlights the importance of rehabilitation pathways requiring collaboration between intensive care clinicians and rehabilitation specialists.
Objectives: To devise a rehabilitation pathway for use in Neurosciences Intensive Care, University Hospital Southampton.
To evaluate staff confidence and knowledge of patient rehabilitation within Neurosciences Intensive Care after implementation of the pathway.
Methods: A rehabilitation working group was set up which included a Neurosciences Consultant, Lead Rehabilitation Physiotherapist (Band 7), Lead Respiratory Physiotherapist (Band 7), Lead Early Mobilisation Therapy Technician (Band 4), Neurosciences Therapy manager (Band 8) and Nurse sister with specialist interest in Rehabilitation (Band 6).
A review of the literature relating to safety of mobilising patients in Neurosciences Intensive Care was undertaken to assist development of inclusion criteria.
Expert advice sought from consultant neurosurgeons to ensure safety of initial implementation of rehabilitation.
A review of national guidelines for rehabilitation in intensive care and physiotherapy clinical expertise assisted development of the specific rehabilitation pathway.
A five point Likert rating scale was used to evaluate staff perceptions of the rehabilitation pathway.
The staff Survey included the following statements:
I am aware of the safety considerations when assessing whether my patient can undergo rehabilitation in Neuro Intensive Care (NICU)
I understand which members of the team should lead early rehabilitation in NICU
I understand my individual role as part of the multidisciplinary team to support and progress rehabilitation in NICU
I feel confident in knowing which patients should undertake early rehabilitation in NICU
I understand the importance of setting goals for my patients in NICU
I feel empowered to work as part of the multidisciplinary team to improve patient outcomes and experience in NICU
I know who to seek help from if I am unsure how to facilitate rehabilitation for my patient in NICU
I feel able to contribute more to my patient’s rehabilitation journey
I now get more job satisfaction due to supporting patient rehabilitation in NICU
Free text box for any additional comments on the rehabilitation pathway
Results: This is an ongoing service improvement project. The rehabilitation pathway is being reviewed and will be available to present at conference.
Staff perceptions of the pathway will be available to present at conference.
Conclusions: Pending data and analysis.
References
1. Van Willigan Z, Collings N, Richardson D, Cusack R. Quality improvement: The delivery of true early mobilisation in an intensive care unit. BMJ Quality Improvement Reports 2016;5:u211734.w4726. Available from: doi:10.1136/bmjquality.
2. Kumar MA, Romero FG, Dharaneeswaran K. Early mobilization in neurocritical care patients. Current Opinion in Critical Care. 2020;26(2):147-154. Available from: doi: 10.1097/MCC.0000000000000709. PMID: 32068582.
3. Phillips M, Turner-Stokes L, Wade D, Walton K. Rehabilitation in the wake of COVID-19 A pheonix from the ashes. British Society of Rehabilitation Medicine. 2020 1-20 Available from: https://www.bsrm.org.uk/downloads/covid-19bsrmissue2-11-5-2020-forweb11-5-20.pdf [Accessed 5th August 2021]
P178
A protocol for systematic assessment of psychological distress in critically ill patients
Rehabilitation
Elaine Johnston 1 , Sabrina Monteregge2, Marcela, P. Vizcaychipi3, Lisa Williams2, Elaine Manderson1, Leigh Paxton1, Dorothy Wade4, Trystan Hawkins5 and Erin Thompson6
1Chelsea & Westminster Hospital NHS Foundation Trust
2Chelsea & Westminster Hospital NHS Foundation Trust; Central & North West London NHS Foundation Trust
3Chelsea & Westminster Hospital NHS Foundation Trust; Imperial College London
4University College London; North East London Foundation Trust
5Cwplus
6Chelsea & Westminster Hopsital NHS Foundation Trust; Central & Northwest London NHS Foundation Trust
Abstract
Introduction: Psychological distress is associated with slower physical and psychological recovery for critically ill patients.1 National guidance states that patients should receive assessments and interventions for psychological as well as physical problems throughout the critical care pathway2,3 using a validated measure such as the Intensive Care Psychological Assessment Tool (IPAT).4 However, there is a lack of evidence for the best way to conduct systematic assessment to identify patients at risk of psychological distress in the ICU.
Objective: To develop a protocol for systematic psychological assessment of critically patients to identify level of inpatient psychological intervention needed.
Methods: All patients admitted to a general adult intensive care unit (ICU) over an 8-month period were screened for eligibility for psychological assessment at 48 hours.
Eligiibility : negative score on Confusion Assessment Method for the ICU (CAM-U), patient alert/awake, consents to assessment.
Measures: Acute psychological distress was assessed using the IPAT. A specifically designed checklist was completed to identify known cognitive impairment, past/current mental health or substance misuse history, and current psychosocial stressors/supports.
Validated measures for depression, anxiety, a PTSD screening questionnaire, and a health-related quality of life measure were completed at opt-in follow up assessment 3-12 months post-ICU discharge.
Assessment was adapted for patients with communication impairment or requiring an interpreter.
Level of Intervention/criterion:
• Psychological care by ICU team + written leaflet (psycho-education/psychology service contact details): all eligible patients
• Inpatient psychological intervention1: patients scoring 7 or above on IPAT or who self-referred
• Liaison with specialist mental health services: patients with complex mental health problems/risk or safeguarding concerns
Data collection/analysis:
Demographic/clinical data collected from patient electronic records:
• Age, sex
• Admission type (planned surgical, emergency medical/surgical)
• Highest level of care (level 2 or 3)
• Acute Physiology and Chronic Health Evaluation II (APACHE II) score, Rockwood Clinical Frailty scores (patients >65)
• Length of ICU/hospital stay
• History of mental health problems
• Scores on psychological measures
Data was anonymised and analysed in Excel.
Results: Results are shown in Figure 1 (patient eligibility screening, psychological assessment and intervention data) and Table 1 (patient demographic/clinical data.
Figure 1.
Patient eligibility screening, psychological assesment and intervention data
Table 1.
Patient demographic/clinical data¹validated >65s; 2patients remaining in our hospital (n=114, 207 respectively)
| Demographics | |||
| Sex, male | N (%) | 73 (55.7) | 139 (52.9) |
| Age | Mean (SD) | 60.2 (17.7) | 70 (19.5) |
| Admission type | |||
| Emergency Medical | N (%) | 88 (67.2) | 94 (35.4) |
| Emergency Surgical | N (%) | 26 (19.8) | 74 (28.1) |
| Elective Surgical | N (%) | 15 (11.5) | 95 (36.1) |
| Missing | N (%) | 2 (1.5) | |
| Highest level of care | |||
| L2 | N(%) | 66 (50.4) | 200 (76.0) |
| L3 | N (%) | 65 (49.6) | 63 (24.0) |
| Intubation | |||
| Intubated | N (%) | 40 (30.5) | 45 (17.1) |
| Days intubated | Mean (SD) | 8.5 (10.2) | 5.0 (5.2) |
| APACHE II Score | Mean (SD) | 14.1 (5.6) | 12.5 (6.7) |
| Rockwood Clinical Frailty score1 ≥5 (in over 65s) | N (%) | 16/60 (26.7) | 80/125 (64.0) |
| Prior mental health problems | N (/%) | 29 (22.1) | Not known |
| Length of stay (LOS) | |||
| LOS: ICU | Median (IQR) | 5.0 (2.9, 9.0) | 1 (0.8, 2.0) |
| LOS: post-ICU discharge2 | Median (IQR) | 9 (5, 17.6) | 7 (4, 14) |
Conclusions: Our protocol was effective in ensuring systematic assessment of critically ill patients’ psychological distress in ICU and identifying level of psychological intervention need.
This project received a grant from CWplus.
References
1. Highfield J, Beadman M, Wade D. Psychology: person-centred care a key to successful recovery. In: C. Boulanger, D. McWilliams (eds) Passport to Successful ICU Discharge, Switzerland: Springer Nature, 2020, 135-154. https://doi.org/10.1007/978-3-030-38916-1_10
2. National Institute for Health and Care Excellence. Rehabilitation after critical illness in adults quality standard (QS158). 2017; available at: https://www.nice.org.uk/guidance/QS158 [Accessed 27 July 2021].
3. The Intensive Care Society and the Faculty of Intensive Care Medicine. Guidelines for the Provision of Intensive Care Services. 2nd ed. London: FICM and ICS; 2019; available at: https://www.ficm.ac.uk/sites/default/files/gpics-v2-final2019.pdf[Accessed 27 July 2021].
4. Wade D, Hankins M, Smyth D, Rhone E, Mythen M, Howell DC, Weinman J. Detecting acute distress and risk of future psychological morbidity in critically ill patients: Validation of the Intensive care psychological assessment tool. Critical Care 2014, 18:519.
5. Kusi-Appiah E, Karanikola M, Pant U, Meghani S, Kennedy M, Papathanassoglou E. Tools for assessment of acute psychological distress in critical illness: A scoping review. Aust Crit Care. 2021:S1036-7314(20)30351-30359. doi: 10.1016/j.aucc.2020.12.003. Epub ahead of print. PMID: 33648818.
P179
Embedding clinical pharmacists in critical care rehab carousel clinics
Rehabilitation
Helen Dufton and David Sapsford
Cambridge University Hospitals NHSFT
Abstract
Introduction: Clinical pharmacists specialising in critical care have become integrated into the critical care workforce providing valuable contributions to patient care.1 These findings are supported through the inclusion of clinical pharmacy services within national professional and commissioned standards for critical care.2,3
On admission to critical care, clinical focus changes from management of any chronic conditions to that of immediate preservation of life. This is inherently associated with acute changes in prescribed medicines. Medicines reconciliation on admission to and discharge from critical care is included specifically within the commissioning standards3 and aims to address any discrepancies generated by this change in focus.
Unprecedented pressures experienced during the COVID-19 pandemic have resulted in stretched staff to patient ratios and mobilisation of less experienced staff. This has negatively impacted the end-to-end reconciliation process causing patients to be discharged home with unresolved medicines discrepancies.
In line with recent NICE4 and Intensive Care Society guidance,5 rehabilitation of patients, post-critical care is important in completing unresolved actions and optimising care. Consequently, in September 2020 a carousel rehab clinic was introduced. All professional groups were invited to contribute.
Objectives: To embed a pharmacist within the rehabilitation clinic to focus on any unresolved medicines reconciliation issues.
Methods: Five senior critical care pharmacists (band 8a or above) participated in service provision to the clinic, which ran on two days a week. For consistency and structure, a local SOP and electronic note template was produced. All interventions recommended were discussed with the patient at the time and for GPs to review and action as appropriate in the context of their responsibility for ongoing care.
Data collection for this service evaluation was retrospective and performed by one of the critical care pharmacists who had participated in the clinic. Historic clinic dates for September – November 2020 (inclusive) were reviewed on the electronic scheduling system to identify patients who attended clinic; these were then filtered for pharmacist entries to ascertain:
• Number of patients reviewed
• Number of medication-related interventions made
• Intervention type and medication(s) involved
Results: Over the 3-month period 51 patients were reviewed with a total of 59 medicine interventions made. The average number of interventions per patient was 1.2, with a range of 0 – 7. Eight intervention categories were identified (see Figure 1); the top three of which recommended stopping a medication (27%), reviewing a medication’s need (19%) or restarting a medication (17%). The drugs most frequently intervened on were lansoprazole (12%) and bisoprolol (7%).
Figure 1.
Pie chart depiciting pharmacist clinic intervention type and percentage occurance
Examples of significant clinical interventions made include:
• Stopping acutely initiated bisoprolol (resolution of acute AF secondary to acute sepsis/dehydration on ICU)
• Stopping of acutely started olanzapine for ICU-related agitation/delirium
• Dose optimisation of bisporolol (post recent NSTEMI)
• Re-initiation of atorvastatin (for secondary prevention of IHD)
Conclusion: Medication interventions made by pharmacists in the post ICU rehabilitation clinic setting are clinically significant and add value to patient care both in terms of morbidity and mortality. Our results demonstrate a reduction in polypharmacy burden in line with wider healthcare initiatives.
References
1. Shulman R, McKenzie CA, Landa J, et al. Pharmacists Review and Outcomes: Treatment Enhancing Contributions Tallied, Evaluated and Documented (PROTECTED-UK). J Crit Care 2015; 30:808-813
2. Faculty of Intensive Care Medicines and the Intensive Care Society. Guidelines for the Provision of Intensive Care Services (2), https://www.ics.ac.uk/Society/Guidelines/GPICS/Society/Guidance/GPICS.aspx?hkey=5dda1ac0-eec7-4b9c-881f-e72f4882d639 (2019, accessed 22nd August 2021)
3. NHS England. Adult Critical Care service specifications, https://www.england.nhs.uk/wp-content/uploads/2019/05/Adult-Critical-Care-Service-Specification-FINAL.pdf (2019 [updated 21 January 2021], accessed 22nd August 2021)
4. National Institute for Health and Care Excellence. Rehabilitation after critical illness in adults Clinical guideline [GC83], https://www.nice.org.uk/guidance/cg83 (2009 [updated October 2015 and July 2018], accessed 22nd August 2021)
5. National Post-Intensive Care Rehabilitation Collaborative. Responding to COVID-19 and beyond: A framework for assessing early rehabilitation needs following treatment in intensive care (1), https://www.ics.ac.uk/Society/Guidance/PDFs/Rehabilitation_Framework (2020, accessed 22nd August 2021)
P180
“Rehab on the edge”: The heamodynamic response to the initial active mobilisation in critically ill adults with COVID-19
Rehabilitation
Katie Dowling, Jennie Balls and Steven Glynn
Royal Brompton and Harefield NHS Trust
Abstract
Introduction: SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) has been responsible for one of the largest global viral outbreaks in recent years.1 Admissions to intensive care units (ICU) have increased. A common consequence of prolonged ICU admission is ICU-acquired weakness (ICUAW).2 Rehabilitation in ICU is well established to be beneficial in combating ICUAW and should be started as early as clinically possible.3
Objectives: This study aimed to explore the haemodynamic effects of initial active rehabilitation in this complex patient population.
Methods: During April to June 2020, continuous, prospective cardiovascular and respiratory data (heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP) and peripheral oxygen saturation (SpO2)) were measured for fifteen minutes before, during and for 30 minutes after the initial active rehabilitation session. Active rehabilitation was defined as a sit over the edge of the bed with assistance from therapists as the minimum achieved in the session. The length of the active rehabilitation session, the type of rehabilitation and reason for stopping the session were recorded. Inclusion and exclusion criteria were established a priori. Data were analysed via non-parametric ANOVA.
Results: Initial active physiotherapy rehabilitation was observed in 23 patients (17 male, median age 45 years (IQR 36,51)). Median length of mechanical ventilation prior to starting active rehabilitation was 34 days (IQR 26,40). Four patients were receiving extra-corporeal membrane oxygenation (ECMO) and three patients had been extubated prior to rehabilitation. All patients achieved a sit over the edge of the bed with one patient progressing to a stand. Median length of treatment time was 11 minutes (IQR 8,14). Group analysis did not identify any statistically significant changes in HR (p=0.975), SBP (p=0.907), DBP (p=0.783), MAP (p=0.625) or SpO2 (p=0.666) across the four study periods. There was no clinically significant change across the variables (range -0.5% reduction to 5.9% increase) with minimal changes in cardiovascular changes. No medical intervention such as titration of medication or additional ventilatory support was required during the sessions or as reason for stopping.
Conclusion: This service evaluation suggests that initial active rehabilitation in a group of critically ill adults with COVID-19 at a specialist centre can be performed safely without detrimental cardiovascular changes.
References
1. Kumar, M. and Al Khodor, S. (2020). Pathophysiology and treatments strategies for COVID-19, Journal of Translational Medicine. 18(353) https://doi.org/10.1186/s12967-020-02520-8
2. Batt, J., C. dos Santos, C., Cameron, J. and Herridge, M. (2013) Intensive Care Unit- acquired Weakness. American Journal of Respiratory and Critical Care Medicine, 187(3), 238-246.
3. National Institute for Clinical Excellence (2009) NICE CG83:2013 Rehabilitation after critical illness in adults. London: National Institute for Clinical excellence
P181
ICU and Beyond - establishing a virtual post ICU rehabilitation class. Supporting life after ICU for patients and family
Rehabilitation
Lisa Bashford, Lucy Tomalin, Tara Edwards, Rebecca Fox and Claire McHugh
Northern Devon Healthcare Trust
Abstract
Introduction: A high proportion of patients surviving critical illness have significant, continuing problems characterised by weakness, loss of energy, physical difficulties, anxiety, depression, post-traumatic stress, and for some, impaired cognitive function.1 Enhancing survivorship, and the quality of survival, is now central to the management of critically unwell patients.2 Rehabilitation should be multi-professional, interdisciplinary and coordinated across the recovery continuum from ICU to the patients’ home to optimise patient outcome, increase quality of survival, and promote living and thriving as opposed to just surviving.
A quality improvement project developing ICU therapy supported discharges in Northern Devon Healthcare Trust identified that access to community rehabilitation services was a limitation to optimising recovery after ICU. In 2020 the access to rehabilitation services was further challenged by the Covid-19 pandemic. An MDT rehabilitation class to continue supporting ICU patients following discharge from hospital was identified as an option for improving patient experience and outcomes.
Outpatient rehabilitation classes delivered by the ICU care team were postulated to provide benefits such as continuity of care, timely access and provide peer support whilst complimenting community services.
Objectives:
• To test the effectiveness of an ICU rehabilitation class on patient outcomes
• To establish the patient acceptability and experience of an ICU rehabilitation class
Methods: A test of change methodology was used to pilot a virtual ICU rehabilitation class in 2020 during the Covid-19 pandemic.
Level 3 ICU patients who had a prolonged ICU stay of greater than one week and had extensive rehabilitation needs were identified via the current Covid-19 caseload, the ICU follow-up clinic and from the caseload of the wider ICU supported discharge quality improvement project.
A virtual rehabilitation class was designed including a pre and post assessment using either Attend Anywhere, telephone and a Zoom based class for one hour twice a week for six weeks. Each one hour class included 30 mins exercise and 30 mins education.
MDT delivered education topics included delirium, benefits of exercise, nutrition, speech, breathlessness, pacing, mindfulness and a Q&A session with a consultant.
A broad range of patient outcomes were assessed (Table 1) and a focus group was held following the class to gain feedback on the experience and to inform the evolution of the service design.
Table 1.
Results .
| Outcome measure | Pre Class - mean (range) | Post Class - mean (range) | Change |
|---|---|---|---|
| Fatigue Assessment Scale (FAS) | 22.3 (16-36) | 18.8 (14-26) | -3.5 |
| Generalised Anxiety Disorder-7 Assessment (GAD-7) | 4.7 (1-9) | 3.83 (0-12) | -0.83 |
| Patient Health Questionnaire–9 (PHQ-9) | 6.5 (0-19) | 4.3 (0-17) | -2.17 |
| EQ5D-5L index value | 0.334 (0.016-0.767) | 0.645 (0.314-0.877) | 0.312 |
| EQ5D-5L VAS | 49 (25-70) | 61 (25-75) | 12 |
| 30 second Sit To Stand Test | 10 (3-19) | 15.4 (9-24) | 5.4 |
| Medical Research Council Dyspnoea Scale | 3.5 (3-5) | 2.2 (2-3) | -1.33 |
Results: Nine patients were identified that met the inclusion criteria and six consented to participate in the class.
Improvements were demonstrated across the range of outcome measures (Table 1).
Themes arising from the focus group discussion included an overall feeling of benefit, appreciation of the opportunity to share experiences with others in a similar position and reflection on the option to complete the course online.
Conclusion: A virtual rehabilitation class was well received by patients with improvements shown in both physical and mental wellbeing. Following patient feedback, a further test of change may consider a combination of face to face and virtual class delivery.
References
1. National Institute for Health and Care Excellence. Rehabilitation after critical illness in adults [Internet]. London: NICE; 2009. (Clinical guideline [CG83]). Available from: https://www.nice.org.uk/guidance/cg83.
2. The Faculty of Intensive Care Medicine & Intensive Care Society. Guidelines for the provision of intensive care services [Internet]. 2019 Ed. 2. Available from: https://www.ficm.ac.uk/standards-research-revalidation/guidelines-provision-intensive-care-services-v2
P183
Negative Pressure Ventilation for Acute and Acute-on-Chronic Respiratory Failure: A systematic review and meta-analysis
Respiratory support
Rebecca Egglestone 1 , John Pappachan2, Denny Levett3, Helen Moyses4, David Howard5, Andrew Cumpstey2 and Mike Grocott6
1UHS
2University Hospital Southampton
3University Hospital Sputhampton
4Southampton centre for biomedical research
5Royal National Throat, Nose and Ear Hospital, London, UK
6Southampton University Hospital
Abstract
Introduction: Respiratory failure is the most common organ failure seen in the intensive care unit1 and is managed with non-invasive or invasive positive pressure ventilation (PPV). Negative pressure ventilation (NPV) could offer a safe and effective alternative, however existing devices, such as the iron lung, are heavy and access to the patient for ongoing care is a limitation. The COVID-19 pandemic necessitated intense focus on the rapid design and manufacture of new ventilators,2 most of which were positive pressure ventilators. However, new, light-weight negative pressure ventilators were also designed and appeared to be safe and effective in an early trial in healthy human volunteers.3 These devices have the potential to offer patients an alternative to PPV, without the limitations associated with the early negative pressure devices. They are cheaper to manufacture, and importantly, do not require a pressurised gas supply, which may be of particular benefit to countries with less well-resourced healthcare facilities in which acute and acute-on-chronic respiratory failure continue to cause significant morbidity and mortality.4
Objectives: To address whether acute or acute-on-chronic respiratory failure in hospitalised adults can be safely and effectively managed with NPV.
Methods: This systematic review was registered with the international prospective register of systematic reviews (ID CRD420200220881). MEDLINE, EMBASE, CENTRAL, medRxiv, bioRxiv and Trip databases were searched (from inception to 22nd April 2021). Eligible studies included non-intubated hospitalised adults who received NPV in the management of acute or acute on chronic respiratory failure. We included randomised controlled trials, non-randomised studies of intervention and case series. Risk of bias was assessed using three separate tools due to differing study designs.
Results: 575 unique citations were screened with 14 meeting inclusion criteria. 1032 acute episodes (888 patients) of respiratory failure were managed with NPV, with 234 receiving PPV as a comparator. The majority (n=845, 66.7%) were treated for an acute exacerbation of COPD. 417 patients from four studies were included in the meta-analysis. The effect of NPV on PaCO2, pH and PaO2/FiO2 was similar to PPV with a mean difference -0.39kPa (95% confidence interval (CI): -0.95, 0.18), 0.01 (95% CI: 0.00, 0.02), and -0.16 (95% CI: -1.98, 1.66) respectively. Of those studies not included in the meta-analysis six showed a statistically significantly increase in PaO2 with the use of NPV and 5 showed a statistically significant improvement in PaCO2. Rates of complications were similar with NPV in those studies that compared it to PPV, and NPV appeared to be well tolerated by patients. This systematic review study was limited by a wide range of study designs.
Conclusions: NPV appears to be a safe and effective alternative to PPV in the management of acute exacerbation of COPD. Evidence for its use in other forms of respiratory failure is limited but warrants further investigation.
References
1. Soo A, Zuege DJ, Fick GH, Niven DJ, et al. Describing organ dysfunction in the intensive care unit: a cohort study of 20,000 patients. Critical Care 2019; 23: 186-200.
2. National Audit Office. Cabinet Office and Department of Health & Social Care. Investigation into how government increased the number of ventilators available to the NHS in response to COVID-19. Available from https://www.nao.org.uk/report/increasing-ventilator-capacity-in-response-to-covid-19/. Last accessed 17th April 2021.
3. Exovent Ref: Exovent Development Group. Exovent: a study of a new negative-pressure ventilatory support device in healthy adults. Anaesthesia 2021; 76:623-628.
4. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019 Lancet 2020; 396:1204–1222.
P184
Should we offer mechanical ventilation in patients with acute hypoxaemic respiratory failure and interstitial lung disease? A retrospective observational study
Respiratory support
Robert Mackie, Kay Protheroe, Lai Man Chan, Kaye Cantlay and Ian Forrest
The Newcastle upon Tyne Hospitals NHS Foundation Trust
Abstract
Introduction: ILD is an umbrella term for a group of respiratory diseases which affect the lung interstitum. Patients may present to hospital with known ILD and acute or acute on chronic hypoxaemic respiratory failure or as their first disease presentation. In comparison to other causes of respiratory failure these patients have an increased critical care mortality.1 Decisions not to escalate and admit to the Intensive Care Unit (ICU) can be morally challenging, particularly if functional status prior to hospitalisation is good. However, prior studies have shown ICU mortality is poor (60%) and if invasive mechanical ventilation (IMV) is required this may be as high as 90%.2 Auditing real life outcome data can guide and justify decision making, helping clinicians by preventing moral injury and burnout.
Objectives: To undertake a 10-year case review of the outcomes of patients admitted with AHRF associated with ILD across the four adult ICUs in the foundation trust. To review overall mortality and assess if any patient factors confer more favourable outcomes to guide escalation decisions.
Method: A retrospective search was undertaken using the electronic ICU ward watcher database of all patients > 18 years of age admitted between 2010 and 2020 to the four adult ICUs in the trust using the search terms “pulmonary fibrosis” and “fibrosing alveolitis”. Electronic records were reviewed for all patients identified. Patients were excluded if the primary reason for admission to critical care wasn’t primarily respiratory failure.
Results: 200 admissions were identified, 122 were excluded. A total of 78 admissions were included, average age 64 (65% male). Of those, 6 were repeat admissions, 4 within the same hospital stay – these patients had a 75% mortality. Overall ICU mortality was 56.4%, and hospital mortality was 69%. 45% were mechanically ventilated, with an ICU mortality of 85%.
The 78 admissions were grouped into five categories and their respective mortalities were analysed:
• Chronic Fibrosing idiopathic interstitial pneumonia (IIP) (n=28, ICU Mortality=75%, IMV Mortality=100%)
• Connective Tissue Disease associated (18, 39%, 86%)
• Drug-Induced (6, 17%, 50%)
• Combined Pulmonary Fibrosis and Emphysema (7, 43%, 66%)
• Other (15, 67%, 83%)
• No Prior Diagnosis (4, 50%, 66%).
Conclusion: In this study, ICU mortality was in line with previous reports3,4 with best outcomes seen in the drug-induced or CTD associated groups. Fibrotic IIPs conferred significant in- hospital mortality (85%), with no survivors if IMV was used. Overall, if patients underwent IMV, this led to poor outcomes throughout this cohort with only 11% surviving to hospital discharge.
Decision making regarding ventilation in ILD over the last 10 years has evolved and while this study’s data can’t evaluate this, anecdotally the last patient with fibrotic IIP invasively ventilated on the majority admitting ICU was in 2017. This likely reflects the anecdotally poor outcome experience of the clinicians which has now been borne out by this study’s data.
Limitations to this study include the possibility of exclusion of patients from search results due to the reliance of clinicians inputting correct information and the limited coding terms for ILD on ward watcher.
References
1. Wong MC, Murphy M, Upham J. Management of hypoxaemic respiratory failure in a Respiratory High-dependency Unit. Internal Medicine Journal. 2017;47(7):784-792.
2. Güngör, G, Tatar, D, Saltürk, C, Çimen P, Karakurt Z, Kirakli, C, Adıgüzel N, Ediboglu, Ö, Yılmaz, H, Moçin, ÖY, Balcı M, Yılmaz A. Why do patients with interstitial lung diseases fail in the ICU? a 2-center cohort study. Source Respiratory care 2013; 58(3): 525-531 Publication Date Mar 2013
3. Ciftci F, Dastan AO, Ciledag A, Erol S, Kaya A. Characteristics of patients with interstitial lung disease in the event of acute respiratory failure in ICU. American Journal of Respiratory and Critical Care Medicine. 2018;197.
4. JA. Huapaya, EM. Wilfong, CT Harden, RG. Brower, SK. Danoff. Risk factors for mortality and mortality rates in interstitial lung disease patients in the intensive care unit. European Respiratory Review 2018 27: 180061
P185
Predictors of poor outcome in patients admitted to Intensive Care following failed high-flow nasal oxygen therapy
Respiratory support
Rebecca Spencer 1 and Robert Docking2
1Princess of Wales Hospital, Bridgend
2NHS Greater Glasgow and Clyde
Abstract
Introduction: High-flow nasal oxygen therapy (HFNO) can be effective in the treatment of acute respiratory failure in critically unwell patients. However, in patients who deteriorate despite HFNO, delayed intubation has been shown to worsen ICU outcomes, including mortality, extubation success and duration of ventilation.1 Identification of factors that predict poor ICU outcome during HFNO therapy could aid decision-making regarding escalation and timing of intubation to avoid complications.
Objective: To investigate whether there were any predictors of poor outcome amongst patients who were admitted to an Intensive Care Unit (ICU) following treatment with high-flow nasal oxygen in Medical HDU (MHDU) at a tertiary hospital in Glasgow.
Methods: Between January 2016 and January 2019, there were 106 patients admitted to MHDU who were treated with HFNO, deteriorated and were subsequently admitted to ICU. Data were collected from the patient record, including demographics and physiological parameters. Severity of respiratory failure was calculated using the ROX index,2 measured after one hour of HFNO therapy and immediately prior to ICU admission. Chi-square tests were conducted to assess whether demographics, length of HFNO therapy or ROX index were associated with poor ICU outcome. Caldicott approval was sought and granted for this retrospective cohort analysis.
Results: The majority (62%) of patients were male and median age was 59 years. Median MHDU length of stay was 0.79 days (IQR 0.34-1.91) and patients received a median of 12 hours HFNO (IQR 5-29.5 hours) prior to admission to ICU. Once admitted to ICU, 85.8% received invasive ventilation. Hospital mortality was 43.4%. In a regression analysis, only age and quartile of ROX index immediately prior to ICU admission were significantly associated with ICU outcome, with p values of 0.009 and 0.03 respectively.
Conclusion: Age and low ROX index immediately prior to ICU admission are predictors of poor outcome in patients admitted to MHDU receiving HFNO. The short time spent on HFNO for the majority of patients suggests that direct admission to ICU may be preferrable for patients who would be for full escalation. Our findings may be limited by only including patients who were admitted to ICU, but this allowed for a clear demarcation of those felt to be suitable for escalation.
References
1. Kang L, et al. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Medicine. 41: 623-632
2. Roca R, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy. American Journal of Respiratory and Critical Care Medicine. 199: 1368-1376
P186
Can the alveolar dead space fraction be used in the diagnosis of pulmonary embolism? A literature review
Respiratory support
Bethany Macdonald, John O’Rourke and Daniel Horner
Salford Royal Hospital
Abstract
Introduction: Alveolar dead space fraction (AVDSf) is calculated as the difference between end-tidal and arterial carbon dioxide and can be potentially used to represent the degree of dead space present in the lungs. Pulmonary embolism (PE) increases dead space; measurement of AVDSf could therefore potentially aid in acute diagnosis.
Objectives: We performed a literature review to evaluate the diagnostic accuracy of an abnormal AVDSf measurement for diagnosis of acute PE, across a spectrum of clinical severity.
Methods: Using the Healthcare Databases Advanced Search, Medline and Embase were searched from 1946 to 16/06/2021 using prespecified search terminology and limited to human studies. An additional search of the Cochrane library was conducted. Two reviewers ran concurrent searches and sifted abstracts for results independently. A third senior reviewer adjudicated cases of disagreement. 358 results were identified, 186 from Embase and 172 from Medline. No relevant Cochrane reviews were identified.
Results: We identified 3 studies for final inclusion; 1 systematic review and pooled meta-analysis of 14 observational studies,1 and 2 subsequent single-centre observational studies.2,3 The meta-analysis demonstrated AVDSf to have a pooled sensitivity of 0.73 (95% CI 0.69-0.78) and pooled specificity of 0.61 (95% CI 0.58-0.64) for the diagnosis of acute PE1. The subsequent studies reported sensitivities of 0.68 (95% CI 0.50-0.82) and 0.81 (95% NR) respectively and specificities of 0.74 (95% CI 0.65-0.81) and 0.63 (95% CI NR).2,3 Overall, the studies found that AVDSf was significantly higher in patients with PE than without. Diagnostic accuracy was improved when AVDSf was applied to stable patients with a low pretest probability, through Wells scoring or d-dimer measurement.1,3
Conclusion: Our review found that there is insufficient evidence to support using AVDSf to diagnose acute PE. Particularly, we found no evidence to support using AVDSf to exclude or confirm the diagnosis of PE in critically ill patients with a high pretest probability.
References
1. Manara A, D'hoore W, Thys F. Capnography as a Diagnostic Tool for Pulmonary Embolism: a meta-analysis. Ann Emerg Med 2013;62: 584-591.
2. Yuksel M, Pekdemir M, Yilmaz S, et al. Diagnostic accuracy of noninvasive end-tidal carbon dioxide measurement in emergency department patients with suspected pulmonary embolism84-90. Turk J Med Sci 2016;46: 84-90.
3. Songur Yücel Z, Metin Aksu N, Akkas M. The combined use of end-tidal carbon dioxide and alveolar dead space fraction values in the diagnosis of pulmonary embolism. Pulmonology 2020;26: 192-197.
P187
Use of inhaled nitric oxide in ICU – when is a therapy trial enough?
Respiratory support
Diana Al-Omari 1 , Anna Tchorzewska2, Anthony Wilson2, Andy Haggerty2 and Alexander Parker2
1Manchester University Medical School
2Manchester University NHS Foundation Trust
Abstract
Introduction: Inhaled nitric oxide (iNO) can be utilized as a rescue treatment option in refractory hypoxaemia and in the potential reversal of pulmonary vascular resistance by pulmonary vasodilation.1
Its use remains controversial due to limited evidence regarding efficacy and potential side effects.2 Furthermore, it requires additional equipment and consumables and its infrequent use means staff may be relatively unfamiliar with the treatment.
Objectives: Investigate use of iNO within our adult critical care unit in order to identify potential quality improvements that could be made to the delivery of this therapy.
Clarify the proportion of patients who demonstrated a favourable PaO2/FiO2 (PF) response to iNO.
Methods: We conducted a single-centre retrospective analysis of consecutive patients treated with iNO on the General & Cardiac Intensive Care Unit at Manchester Royal Infirmary between 01/01/2018 and 25/06/2021.
Data was extracted from electronic patient records on patient characteristics, indication for iNO, starting dose, ventilatory characteristics, change in PF ratio and ICU outcome. Results were recorded at iNO initiation, 2, 6, 12 and 24 hours.
A responder was defined by improvement in the PF ratio of ≥20% at any point up to 6 hours after initiation.
Results: 37 patients were identified, mean age 51 years (SD 14). 84% were male and 16% were female. 27 patients (73%) had a diagnosis of COVID-19 pneumonitis (Figure 1).
Primary indication for iNO was acute respiratory failure (ARF) in 32 (86%) and right ventricular failure in 5 (14%) patients.
Prior to iNO, patients had been in ICU for 11 days (SD 11) and had received invasive mechanical ventilation for 163 hours (SD 188). PF ratios at initiation were 12.8kPa (SD 5.0), in keeping with severe ARDS and 13 (39%) were already proned at initiation.
Median troponin result prior to therapy was 21[IQR 14- 81]. 12 patients (32%) had ECHO evidence of raised pulmonary artery pressures.
A starting dose of 20ppm iNO was observed for each patient. By 6 hours, 14/37 patients (37%) were classified as positive responders. There was a significant increase in PF ratios at 6 hours compared to baseline in responders (15.9kPa vs 12.0kPa, p=0.04) but no significant difference at any other time point. There was no difference in the duration of therapy in responders vs non responders (76 vs 85 hours, p=0.72).
Conclusion: iNO therapy may offer short-term improvement in oxygenation in <40% of patients at 6 hours.
Duration of therapy was similar regardless of response. This may suggest reluctance to discontinue therapy once started possibly through fear of precipitating deterioration, belief that iNO has halted decline or reluctance to recognize futility when there are few other therapeutic options.
iNO is typically commenced when patients have already been invasively ventilated for several days. It is unknown whether earlier initiation would affect response.
Use of iNO has increased markedly since the start of the COVID-19 pandemic which should prompt units to evaluate their own practice with this therapy.
References
1. Creagh-Brown BC, Griffiths MJD, Evans TW. Bench-to-bedside review: Inhaled nitric oxide therapy in adults. Crit Care. 2009;13(3):221. doi:10.1186/cc7734
2. GebistorfF AA. Cochrane Library Cochrane Database of Systematic Reviews Inhaled nitric oxide for acute respiratory distress syndrome (ARDS) in children and adults (Review) Inhaled nitric oxide for acute respiratory distress syndrome (ARDS). Children and Adults (Review). Published online 2018. doi:10.1002/14651858.CD002787.pub3
P188
Unexplained hypoxia requiring prone ventilation in a patient with acute disseminated encephalomyelitis
Respiratory support
Alex Jude Fonseca 1 and Sudhindra Kulkarni2
1Royal Preston Hospital, LTHTR
2Royal Preston Hospital - LTHTR
Abstract
Introduction: Acute Disseminated Encephalomyelitis (ADEM) is a rare, immune-mediated, demyelinating disorder of the central nervous system characterized by acute encephalopathy with neurologic deficits and MRI findings consistent with multifocal demyelination requiring immunosuppression for therapy.1,2 Patients seldom develop hypoxia during the course of the illness, requiring prone ventilation to improve oxygenation which is the first line of therapy and a proven standard of care in patients with ARDS.3,4 We would like to present a case of ADEM where a patient developed unexplained hypoxia requiring prone ventilation.
Case description: A 35-year-old male with no significant past medical history presented to our neuro-specialist centre with one day history of severe lower back pain associated with lower limb weakness and numbness. His symptoms, which commenced 10 days post his Covid vaccination, rapidly progressed over 2 days of hospital admission to involve right upper limb & facial weakness. MRI scan of brain and spine showed features of ADEM and pulse Methylprednisolone was initiated. CT thorax and abdomen on admission was unremarkable. He was transferred to the critical care unit in view of progressive ascending paralysis and was intubated on his 5th inpatient day due to involvement of respiratory muscles. Following 4 cycles of plasma exchange with albumin (day 6,7,9 and 10 of hospital admission), he developed unexplained hypoxic episodes which eventually resulted in sustained hypoxia, requiring 100% oxygen. Airway pressures and lung compliance were within normal range. Bedside ultrasound demonstrated good lung sliding in all lung fields and good left ventricular contractility with no evidence of right ventricular dilatation. There was no evidence of pericardial/pleural effusion.
CT thorax repeated on day 9 showed no features of acute thromboembolic disease and there were no signs of lung parenchymal involvement. Formal echocardiography with bubble test showed normal heart with no evidence of patent foramen ovale. Multi-disciplinary discussions involving cardiology, respiratory, neurology teams and regional ECMO centre could not explain the enigma of impaired oxygenation. The patient responded well to 16 hours of prone ventilation on day 10 with decreasing oxygen requirements. In the subsequent 3 months of his inpatient stay, he was weaned off oxygen and was tracheostomised in view of his neurological illness. He continues to receive physiotherapy and neuro rehabilitation which had led to clinical improvement.
Conclusion: The possible reason for hypoxia could be impaired tissue oxygenation post plasma exchange. However, it could be a coincidental finding and there is not much literature to explain this phenomenon and warrants further research.5
References
1. M T, Y M. What is acute disseminated encephalomyelitis (ADEM)? Eur J Paediatr Neurol. 2004;8(5):239-242.
2. McCuddy M, Kelkar P, Zhao Y, Wicklund D. Acute demyelinating encephalomyelitis (ADEM) in COVID-19 infection: A case series. Neurol India. 2020;68(5):1192-1195.
3. Bamford P, Bentley A, Dean J, Whitmore D, Wilson -Baig N. ICS Guidance for Prone Positioning of the Conscious COVID Patient 2020.
4. Guérin C. Prone ventilation in acute respiratory distress syndrome. Eur Respir Rev. 2014;23(132):249-257.
5. Borberg H. Problems of Plasma Exchange Therapy. Berlin, Heidelberg: Springer; 1981.
P190
Improving sedation practices on the ICU
Sedation, analgesia and delirium
Christopher Fine and Roseanna Matt
East Lancashire Hospital Trust
Abstract
Introduction: Sedation is routinely used to facilitate treatment of many patients within ICU. Commonly a combination of propofol and an opioid is used to maintain sedation. Sedation is not without risk, one of the most significant being prolongation of mechanical ventilation and thus length of stay. Other risks include increased risk of critical illness myopathy and muscle wasting, increased incidence of delirium, increased risk of nosocomial pneumonia, immunosuppression and VTEs.1
Due to the risks, the minimum amount of sedation to facilitate treatment should be used. Patients should be kept lightly sedated as this reduces ICU length of stay, iatrogenic harm and morbidity.2 Sedation depth should be reviewed on a regular basis and the depth of sedation be specified by the daily prescribing of a Richmond Agitation Sedation Scale (RASS) level.3
In addition to the targeting of light levels of sedation, patients should also have daily spontaneous awakening trials (SATs) if this is clinically appropriate to assess their suitability for extubation.4
Objectives: To assess the current sedation practices within a large ICU. Data was collected to inform a quality improvement project as part of implementation of ICU Liberation guidelines.
Methods: A retrospective case note review was carried out.
Those ventilated for over 7 days were included. Patients were excluded from data collection if they were on FiO2 > 0.6; recently received muscle relaxants; brain injury; concern regarding patient’s airway or plan for tracheostomy. Of 22 patient notes that were reviewed, 11 were eligible. Data was collected for 7 days from when patients met the inclusion criteria.
Results: Of the 77 patient days reviewed, a target RASS was only prescribed on 4 (5%). 18 (23%) included a SAT where all sedation was stopped. On in depth analysis of day 4’s data, the modal level of sedation achieved was RASS of -4 (range +2 to -5); none of the patients had a target RASS prescribed.
Conclusion: The expected standard is that all patients should have their RASS level prescribed on a daily basis; only 5% met this target. Patients received larger doses of sedative medicines than were clinically necessary and kept sedated to a deeper level than required. There may be a lack of understanding of the importance of prescribing and regularly reviewing sedation level.
The frequency of daily SATs also fell below the expected standard at 23% of patient days. The literature suggests that this should be a nursing led initiative however SATs can be associated with an increased nursing workload and therefore may not be done as often as optimal.5
In order to improve the level of sedation that is received by patients on ICU an education video (https://youtu.be/-OizBQmZAas) was designed and filmed and shared on YouTube and Facebook on assessing levels of sedation using RASS. In addition results of this audit were shared at departmental audit meeting and a teaching programme designed to encourage medical staff to set targets, empower nursing staff to ask for target levels of sedation and encourage the closer titration of sedative medications.
References
1. Schweickert WD, Gehlbach BK, Pohlman AS, Hall JB, Kress JP. Daily interruption of sedative infusions and complications of critical illness in mechanically ventilated patients. Crit Care Med 2004;32(6):1272-1276.
2. Shehabi Y, Bellomo R, Reade MC, et al. Sedation Practice in Intensive Care Evaluation (SPICE) Study Investigators; ANZICS Clinical Trial Groups: Early intensive care sedation predicts long-term mortality in ventilated crucially ill patients. Am J Respir Crit Care Med 2012; 186:724-731.
3. Raising the Standards: RCoA quality improvement compendium [Internet]. 4th ed. London: Royal College of Anaesthetists; 2020 [cited 27 July 2021]. Available from: https://rcoa.ac.uk/sites/default/files/documents/2020-08/21075%20RCoA%20Audit%20RecipeBook_Combined_Final_25.08.2020_0.pdf
4. Kress JP, Pohlman AS, O’Connor MF, et al. Daily interruption of sedation infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 342:1471-1477.
5. Mehta S, Burry L, Cook D, et al. SLEAP Investigators; Canadian Critical Care Trials Group: Daily sedation interruptions in mechanically ventilated critically ill patients care for with a sedation protocol: A randomized controlled trial. JAMA 2012; 308: 1985-1992.
P192
Assessment of the impact of an integrated interprofessional working group to promote the ICU Liberation initiatives – Our story two years on
Sedation, analgesia and delirium
Edmund Lodwick, Reena Mehta and Ritesh Maharaj
King’s College Hospital
Abstract
Introduction: Pain, agitation, delirium, weakness, and sleep deprivation are well recognized symptoms during an ICU stay.1 In 2019, our institution set up an ICU Liberation Working Group (ILWG)2, aiming to reduce the harmful effects of these symptoms. This interprofessional working group encompassed medical, pharmacy, nursing and allied health members and utilised a multifocal approach.
Objectives: To review the impact of various initiatives implemented on the outcomes of the ABCDEF (A2F) bundle in the last two years.
Methods: These initiatives are based on each aspect of the A2F bundle. As shown in Table 1, the interventions were each targeted to one aspect of the A2F bundle and were grouped under four themes of teaching, operational interventions, informatics, and guidelines/policies.
Table 1.
Interventions.
| Bundle Intervention | Assessment, prevention, and management of pain | Both SATs and SBTs | Choice of analgesia and sedation | Assessment, prevention, and management of delirium | Early mobilisation and exercise | Family engagement and empowerment |
|---|---|---|---|---|---|---|
| Teaching, Training + Awareness | Pain management teaching | Online SBT/SAT training. | Dedicated teaching for all ICU doctors. | Dedicated teaching for all ICU doctors and nurses. | Adoption of ‘This Is Me’ initiative | |
| Repeated teaching sessions. | Delirium leaflets for family members | |||||
| Operational | Pharmacy presence on ward rounds | Streamlined rapid delirium assessment. | New mobility equipment including dedicated bedspace hoists | Outdoor family area. | ||
| Nurse champions auditing delirium. | Delirium reduction design in new ICUs | |||||
| SALT involvement | SALT involvement | Patient diaries | ||||
| Informatics | CPOT integration on daily notes | SBT assessment tool | CAM-ICU integration on daily notes | |||
| Guidelines + Policies | Weaning plans for analgesia and sedation | Delirium guideline linked to prescription | Mobilisation checklist |
These interventions were audited regularly, with the results displayed on awareness boards, aiming to encourage staff engagement. An ICU Liberation week was also held to improve awareness and compliance with the A2F bundle.
Results: Audit cycles were performed in April 2019, December 2019, and November 2020, assessing data representing each arm of the A2F bundle. Two-thirds of the audit standards showed a significant improvement after initial interventions were employed. The third cycle showed improvement has been maintained in half of the standards. Unfortunately, adherence did reduce in several fields. The greatest improvement was seen in sedation target documentation.
A further cycle in January 2021 assessed the impact of COVID-19 on A2F application, showing a reduction across most audit criteria. There were, however, improvements in family updates and early mobilisation.
Conclusion: The ongoing work of an interprofessional ILWG has shown a cohesive approach application of the A2F bundle, which has resulted in improved harm prevention and management. The impact of COVID-19 has been shown to have reduced our ability to provide improvements in A2F application.
Ongoing interventions are a bespoke sleep tool and more detailed CAM-ICU assessment, designed to elucidate the underlying causes of sleep disruption and delirium. A focused quality improvement project has started, where specific interventions are to be trialed on one ICU before expectant deployment throughout other ICUs. Data will continue to be collected and presented to further assess the most effective methodology for application of the A2F bundle.
References
1. Ely EW. The ABCDEF Bundle: Science and Philosophy of How ICU Liberation Serves Patients and Families. Crit Care Med. 2017;45(2):321-330. doi:10.1097/CCM.0000000000002175
2. Lewis R, et al. (2019). Development of a Multi- Disciplinary Intensive Care Unit (ICU) liberation working group as n intervention for the management of delirium and introduction of the ABCDEF bundle within the ICU. Journal of the Intensive Care Society;21(2): 1-225 [Intensive Care Society State of the Art, London, UK. 2019] https://doi.org/10.1177/1751143720915029
P193
Analyzing the association of Glasgow Coma Scale scores and Richmond Agitation-Sedation Scale scores with ICU delirium incidence
Sedation, analgesia and delirium
Ayush Sangari 1 , Elizabeth Emhardt2, Barbara Salas3, Brenda Pun2, Andrew Avery2, Robert Freundlich2, Daniel Fabbri2, Matthew Shotwell2 and Joseph Schlesinger2
1Stony Brook School of Medicine
2VUMC
3The Newcastle upon Tyne NHS Foundation Trust
Abstract
Introduction: Clinically, Glasgow Coma Scale (GCS) scores have been indicated to be ‘not useful’ to diagnose delirium,1 though Frisch et al. found that a GCS score < 15 was as diagnostic for delirium as using a rapid checklist for delirium symptoms in elderly patients transported by emergency medical services.2 Meanwhile, there is stronger evidence that Richmond Agitation-Sedation Scale (RASS) scores are correlated with delirium, and non-zero RASS scores have shown to be a very good indicator of delirium in older emergency department patients.3
Objective: This study sought to analyze the association of GCS and RASS scores with delirium incidence in intensive care unit (ICU) patients.
Methods: GCS and RASS scores were recorded throughout the day for 948 adult patients admitted to the Cardiovascular, Surgical, and Trauma ICUs of Vanderbilt University Medical Center from May 2018 to July 2018. Delirium incidence was measured using Confusion Assessment Method (CAM-ICU) scores, considered to be the gold standard for ICU delirium assessment.4 The average, minimum, and maximum GCS and RASS scores were compared for patients with (n=271) and without (n=669) delirium, and logistic regression analysis was used to analyze the association between the calculated scores and ICU delirium incidence after adjusting for potential confounders such as age, sex, length of stay, severity of illness (using Diagnostic Related Group weights), and ICU unit.
Results: Two-sample T-tests indicated that patients with delirium had significantly smaller average (11.94 [10.10, 13.70], p<.001), minimum (3 [3,8], p<.001), and maximum (15 [15,15], p=.03) GCS scores during their stay than the average (14.26 [12.67, 14.97]), minimum (10 [3, 14]), and maximum (15 [15,15]) GCS scores for patients without delirium. Meanwhile, patients with delirium had significantly smaller average (-0.66 [-1.31, -0.28], p<.001), smaller minimum (-4 [-5, -2], p<.001), and higher maximum (1 [0,2], p<.001) RASS scores than patients without delirium [average RASS = (-0.29, [-0.79, -0.05]), minimum RASS = (-2, [-4, -1]), and maximum RASS = (0, [0, 0])]. After adjusting for the aforementioned potential confounders, the performed logistic regression analysis found that lower average GCS scores (OR = .968, 95% OR CI = [0.944, 0.991], p<0.01) and higher maximum RASS scores (OR = 1.136, 95% OR CI = [1.111, 1.161], p<0.001) were significantly associated with delirium incidence.
Conclusions: ICU patients who experienced delirium also had overall lower GCS scores across the board, affirming the conclusion from Frisch et al. that a lower GCS score than a baseline score may be predictive of delirium. Meanwhile, the calculated RASS score data highlights the granularity that exists in the delirium spectrum, from hypoactive to hyperactive. Taken together with the strength of the correlation demonstrated by the adjusted logistic regression analysis, these results suggest that GCS and RASS scores of patients could provide objective insight into the spectrum of ICU delirium severity and complement other developed delirium assessment methods, as delirium assessment moves beyond CAM-ICU’s binary identification approach.5
References
1. Johnson MH. Assessing confused patients. J Neurol Neurosurg Psychiatry 2001;71(Suppl 1):7-12. doi: 10.1136/jnnp.71.suppl_1.i7. PubMed PMID: 11511735; PubMed Central PMCID: PMC1765561.
2. Frisch A, Miller T, Haag A, Martin-Gill C, Guyette FX, Suffoletto BP (2013) Diagnostic Accuracy of a Rapid Checklist to Identify Delirium in Older Patients Transported by EMS. Prehospital Emergency Care 17 (2):230-234. doi:10.3109/10903127.2012.744785
3. Han JH, Vasilevskis EE, Schnelle JF, Shintani A, Dittus RS, Wilson A, Ely EW (2015) The Diagnostic Performance of the Richmond Agitation Sedation Scale for Detecting Delirium in Older Emergency Department Patients. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 22 (7):878-882. doi:10.1111/acem.12706
4. Ely, E., Wesley MPH, Margolin R, Francis J, May L, Truman B, Dittus R, Speroff T, Gautam S, Bernard G, Inouye S, MPH Evaluation of delirium in critically ill patients: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU), Critical Care Medicine 2021 29(7): 1370-1379.
5. Krewulak KD, Rosgen BK, Ely EW, Stelfox HT, Fiest KM (2020) The CAM-ICU-7 and ICDSC as measures of delirium severity in critically ill adult patients. PLoS ONE 15(11): e0242378. https://doi.org/10.1371/journal.pone.0242378
P194
CONTINUOUS INFUSION KETAMINE AS ANALGESIA OR SEDATION IN MECHANICALLY VENTILATED ADULTS IN THE INTENSIVE CARE UNIT: A SCOPING REVIEW
Sedation, analgesia and delirium
Nicholas Richards, William Weatherhead, Mark Bellamy, Simon Howell and Ruben Mujica-Mota
Leeds Teaching Hospitals NHS Trust
Abstract
Introduction: Mechanical ventilation (MV) is a common and often live-saving intervention on the Intensive Care Unit (ICU).1 In order to facilitate this intervention, the majority of patients require medical sedation. Optimising sedation is one of the fundamentals of ICU care, and inadequate sedation has consistently been associated with worse outcomes for patients.2,3
Ketamine provides amnesic, analgesic, and dose dependant anaesthetic effects and is used successfully as an induction agent for hypotensive patients.4 Despite its proven haemodynamic safety, ketamine has not yet been adopted as a routine sedative in ICU.
We present a scoping review of published literature on the use of ketamine as a sedative to facilitate MV on ICU.
Objectives: The scoping review was designed to answer the question ‘What is known about the use of ketamine as a continuous infusion to provide sedation in mechanically ventilated adults in the intensive care unit, and what gaps in the evidence exist?’
Methods: The scoping review was designed using the Preferred Reporting Items for Systematic Reviews and Meta-analysis extension for Scoping Reviews (PRISMA-ScR) checklist and the JBI manual for evidence synthesis. Data was extracted using a dedicated form and reviewed by a minimum of 2 reviewers.
A preliminary search of MEDLINE was made using the terms: (Ketamine) AND (Intensive Care) AND ((Sedation) OR (Analgesia)).
Results: Initial MEDLINE search returned 664 results. 35 potential articles were identified as potentially relevant and assessed for eligibility. A further 5 studies were identified using “keywords” from initial articles, and 15 articles through ‘grey’ literature searches. After assessment, a total of 30 met inclusion criteria (see Figure1).
Figure 1.
Search, inclusion, and exclusion flow diagram.
Articles ranged from years 1981 to 2020, and from 11 different countries.
A total of 1089 mechanically ventilated patients were included from the following ICUs: general/unspecified (507), cardiac (95), medical (249), neurosurgical (108), surgical (90), and trauma (37).
Of the 30 articles included there were a variety of methods used, with 60% being either case reports/series (20%) or retrospective cohort/observational studies (40%). Fewer than half (47%) of the studies used a control or comparator group.
The most frequently reported outcomes were cardiorespiratory parameters, sedation scores, and effects on concurrent analgosedative infusions.
Reported results varied, but commonly found benefits included improved cardiovascular parameters, improved sedation scores, and no negative effects on intracranial pressure (previously a concern in neurosurgical ICUs).
Results are to be interpreted with caution given the quality of most of the studies was assessed as weak to moderate.
Conclusion: This scoping review highlights how limited the literature is on using continuous ketamine infusions on ICU. The variable designs and methodologies employed mean that the quantity and quality of data is currently too sparse to recommend widespread use of ketamine infusions.
The gaps in the knowledge base and literature presented here strongly indicate that further investigation is warranted. These gaps would be addressed by a large multi-centre randomised controlled trial.
References
1. Adhikari N, Fowler R, Bhagwanjee S. Critical care and the global burden of critical illness in adults. Lancet. 2010;376(9749):1339-1346.
2. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2012;41(1):263-306. PubMed PMID: 23269131. Epub 12/28. eng.
3. Reade MC, Finfer S. Sedation and delirium in the intensive care unit. N Engl J Med. 2014;370(5):444-454. PubMed PMID: 24476433. Epub 01/31. eng.
4. Morris C, Perris A, Klein J, et al. Anaesthesia in haemodynamically compromised emergency patients: does ketamine represent the best choice of induction agent? Anaesthesia. 2009;64(5):532-539. PubMed PMID: 19413824. Epub 05/06. eng.
P195
Clinical pharmacist’s views on the role of alpha-2-agonists in practice and research for the management of agitation, sedation and delirium (ASD)
Sedation, analgesia and delirium
Rebekah Eadie 1 , Cathrine McKenzie2, Bronagh Blackwood3, Lydia Emerson4, Leanne Aitken4, Julia Boyd5 and Timothy Walsh6
1South Eastern Health & Social Trust
2Kings College London
3Wellcome-Wolfson Institute for Experimental Medicine, Queens Unversity Belfast
4CITY University of London
5Edinburgh Royal Infirmary
6Royal Infirmary of Edinburgh
Abstract
Introduction: Patients in the intensive care (ICU) commonly receive analgesics and sedatives to facilitate mechanical ventilation. Recommendations suggest patients are kept as lightly sedated as feasible. Studies report an inconsistent association between deep sedation, prolonged ventilation and ICU stay.1
Opinions around patients ‘wakefulness’ include discomfort and the potential increased prevalence of psychological morbidity.2 Alpha-2-agonists (clonidine and dexmedetomidine) are agents used in ASD management and reported to produce lighter sedation.
The aim of this project was to explore ICU pharmacist’s perspective on ASD practice over UK.
Objectives :
• Explore ICU pharmacist’s views on: ASD practices, sedation research priority, importance of A2B clinical trial and the impact of Covid19.
• Determine the prevalence of clonidine and dexmedetomidine prescribing.
Methods : An online survey was devised on SurveyMonkey. The survey was designed in 2 sections: -
1. Respondents provided responses based on a ‘point prevalence’ of clonidine and dexmedetomidine prescriptions, on day of completion.
2. Their local ICU sedation practice, their views on priority of sedation research, the A2B study and whether they believed ASD was more challenging during the Covid19 pandemic.
The online survey was distributed via the UK Clinical Pharmacy Association Critical Care Group (UKCPA CCG), the NIHR Critical Care National Speciality Group (NSG), the UK Critical Care Research Group and Twitter.
The survey remained active for 12 weeks from 30.3.2021 with reminders sent for completion every fortnight.
Results: There were 121 respondents, all but 1 were ICU pharmacists. There are approximately 243 ICU pharmacist posts in the UK, this represents a response rate of approximately 50%.
37 (30%) of respondent reported clonidine (but not dexmedetomidine) was prescribed in their ICU; 7 (6%) described dexmedetomidine only; and 76 (63%) reported both.
In describing ASD during Covid-19 pandemic, 107 (88%) respondents reported it had become more challenging.
83 (69%) of respondents stated that clonidine usage increased during the pandemic (27 (22%) no change). 46 (39%) stated that dexmedetomidine usage increased during the pandemic (50 (42%) no change).
Among the respondents 98 (81%) ‘strongly agreed’, and 20 (17%) ‘agreed’ that research involving ASD is a priority.
A2B is set to compare clinical and cost effectiveness of propofol, clonidine, and dexmedetomidine as primary sedative for ICU patients. 49 (40%) of respondents reported participating in A2B. 65 (54%) respondents felt that A2B was a ‘very important’, and 63 (52%) said it was an ‘important’ research question.
Conclusion: This survey reported widespread use of alpha-2-agonists in ASD practice. Almost two-thirds of ICUs report using both agents. Clonidine use is the most prevalent. Given the paucity of high quality clinical effectiveness and safety data for this drug, clinical trials which assess clinical effectiveness, including ASD are a priority. Respondents endorsed that ASD research is a priority, with ASD management much more challenging during the Covid19 pandemic.
Limitations include that the design was a brief online survey; although had a high pharmacist response it did not incorporate the views of other members of the ICU team.
References
1. Aitken L, Kydonaki K, Blackwood B, et al. Inconsistent relationship between depth of sedation and intensive care outcome: systematic review and meta-analysis.
2. Nikayin S, Rabiee A, Hashem MD, et al. Anxiety symptoms in survivors of critical illness: a systematic review and meta-analysis. General hospital psychiatry 2016;43:23-29.
P196
Plasma concentrations of broad-spectrum beta-lactam antibiotics are significantly lower in critically ill patients with augmented renal clearance
Sepsis and severe infections
Frederik Helsen 1 , Thomas De Corte2, Sarah Van Vooren2, Sofie D’haese2, Veronique Stove3, Alain Verstraete3 and Jan De Waele1
1Dept. of Critical Care Medicine UZ Gent, Ghent, Belgium
2UZ Gent, Ghent, Belgium
3Dept. of Laboraty Medicine, UZ Gent, Ghent, Belgium
Abstract
Introduction: Appropriate dosing of beta-lactam antibiotics in critically ill patients is challenging. Augmented renal clearance (ARC) is considered an important cause of sub therapeutic plasma concentrations. However, data from large cohorts is lacking.
Objectives: Evaluate the correlation between ARC and the steady-state plasma concentration of piperacilline/tazobactam (TZP) or meropenem (MER) in critically ill patients.
Methods: Retrospective analysis of adult critically ill patients receiving continuous infusion of TZP or MER in a single center between March 2016 and April 2019. Inclusion criteria were admission to the intensive care unit (ICU), administration of TZP or MER in continuous infusion after an initial loading dose, age>18y and availability of a plasma concentration of the drugs studied. For the current analysis, patients with acute kidney injury, receiving renal replacement therapy, and patients without a measured creatinine clearance (mCrCl) - based on an 8-hour urinary collection - at the moment of plasma sampling were excluded. Antimicrobial plasma concentrations were determined at steady state (>12 h continuous infusion) by liquid chromatography with tandem mass spectrometry. Measured concentrations were not disclosed to the treating physicians. ARC was defined as a mCrCl >130 mL/min. Only one sample per antibiotic course was considered.
Results: We examined 599 samples (72% TZP, 28% MER) from 545 ICU admissions, obtained from 531 individual patients. Median age of patients was 63 (IQR 53-72) years, 34% were female, 51% were admitted after surgery, site of infection was mostly the respiratory tract (38%) or the abdomen (37%), median BMI 25.2 (IQR 22.4-28.4) kg/m2, serum creatinine 0.81 (IQR 0.66-1.10) mg/dL, APACHE IV score 107 (IQR 80-132), SOFA score 8 (IQR 5-10). ARC was present in 32% of TZP patients and 27% of MER patients. When comparing patients with vs. without ARC, median TZP concentration was 48.6 (IQR 36.7-69.3) vs. 102.0 (IQR 74.5-151.9) mg/L, median MER concentration was 7.6 (IQR 5.7-11.5) vs. 16.7 (IQR 11.1-26.1) mg/L (both p<0.001). There was a strong, negative correlation between mCrCl and TZP or MER concentration (rs = -0.769 and -0.749 respectively, p<0.001).
Conclusions: In this large series of critically ill patients, we confirm steady-state plasma concentrations of broad-spectrum beta-lactam antibiotics are significantly lower in patients with ARC, with median TZP and MER concentrations in ARC samples about half of the concentrations found in non-ARC patients.
P198
Percutaneous dilatational tracheostomy: A decade of a tertiary care teaching hospital experience
Tracheostomy
Shaikh Nissaruddin Maheboob, Siddhartha Banerjee, Mohammed Mansoor Nainthramveetil, Muhammad Zubair Labathkhan, Sumayya Aboobacker, Arshad Hussain Chanda and Ranjan Maxim Mathias
HAMAD MEDICAL CORPORATION
Abstract
Introduction: One of the major indications of performing tracheostomy in ICU is anticipated prolonged mechanical ventilation. Tracheostomy for critically ill patients in ICU can be performed either by surgical approach or by Percutaneous dilatational tracheostomy (PDT) of which the later one has some clear advantage over the former one, like PDT is less time consuming procedure and it can be performed at bed side as well without the need of operation theatre.1 Although early complications in the peri procedural period reported to be life threatening events like hemorrhage, false passage, hypoxia, pneumothorax and death2 but the use of bronchoscopy during the PDT reduces the duration of procedure, morbidity and detects intraoperative complications immediately which is missed by blindly performed PDT approach.3
Objectives: Aim of our study was to find out the outcomes including early complications, impact of bronchoscopy guided procedure and to know the efficacy and safety of airway secured with either endotracheal tube (ETT) or laryngeal mask during the procedure.
Patients and methods: In this retrospective study all patients, who underwent PDT over a period of 10 - years in surgical and trauma intensive care unit were included. Patient’s demographic data, method of airway secured during the procedure, type of PDT, perioperative complications, use of bronchoscopy and outcome were recorded. SPSS version 23 was used to analyze data, and to compare the groups’ t-test and chi square test were used. P value of <0.05 was considered statistically significant.
Results: A total of 342 patients were enrolled in the study. Male predilection was found to be prominent (276/80.7%) and all the patients undergone blue rhino dilatational tracheostomy (252/73.7%). Most of the patient’s airway during the PDT was secured by the ETT (316/92.4%). 75.4% of patients did not have perioperative complications. There was no significant difference in rate of complication whether airway was secured with ETT or laryngeal mask. When the PDT was performed under vision with bronchoscopy, the rate of perioperative complications was significantly lower (p=0.001) [Table 1]
Table 1.
PDT with or without bronchoscopy
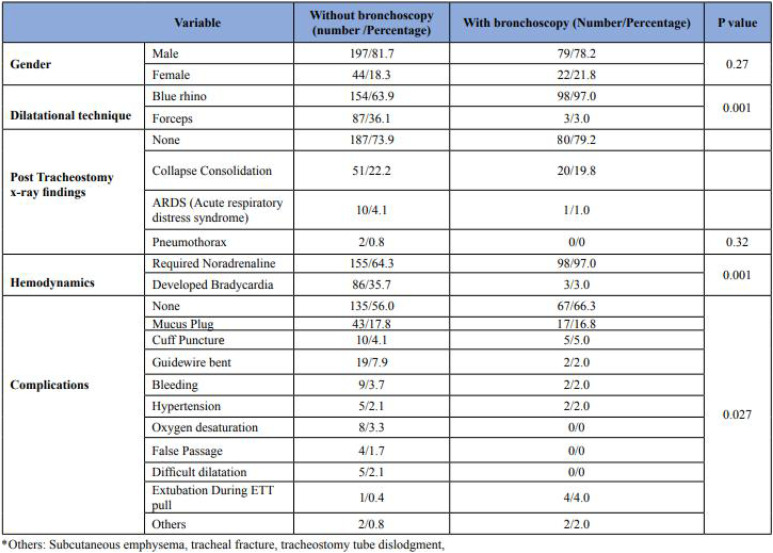
|
Conclusion: PDT is safe to perform with either ETT or laryngeal mask. PDT should be done under vision with bronchoscopy.
References
1. Al Mansoury A, Ali S, Said H. Percutaneous tracheostomy, making it easier. Egy J Bronchol 2018; 12(4): 405-412.
2. Durbin CG Jr. Early complications of tracheostomy. Resp Care 2005; 50(4): 511-515.
3. Romero de Tejada JAG, Gamez Punter RM, Barker IC, Rauz RA, Marco JA, Naranjo OR. Outcomes and complications of bronchoscopic guided percutaneous dilatational tracheostomy. Eurp Resp J 2011; 38: 3716.
P199
A decision making tool and protocol for early cuff deflation and one way valve inline for patients who are ventilated with a tracheostomy – a case series report
Tracheostomy
Susan McGowan 1 , Lindsay Potter2, Ailsa Carmichael2, Jennifer Ritchie2 and Javid Khan2
1National Hospital for Neurology and Neurosurgery, London
2National Hospital for Neurology and Neurosurgery
Abstract
Introduction: Early cuff deflation and one way valve placement inline for patients who are ventilated with a tracheostomy allows for the restoration of verbal communication with concomitant psychological benefits, and enables assessment of bulbar function, delirium, pain, airway patency and speech and language problems.1,2 Such an approach has not been shown to impact respiratory or ventilatory outcomes.3-5 Whilst the benefits may seem obvious, the practice of using one way valves inline has not been widely documented and there are a few published patient selection criteria or protocols, but no national guidelines. Our multidisciplinary team designed a novel decision making tool and protocol to improve specialist service provision.
Objectives: This was a retrospective audit of i) our decision making tool and ii) our protocol for early cuff deflation, one way valve inline placement and ventilator adjustments in a specialist tertiary referral neuroscience intensive care unit.
Methods: The decision making tool and protocol guides the selection of patients and the approach to early cuff deflation. We performed a retrospective analysis of medical and therapy electronic patient records on consecutive patients with whom we had used this tool and protocol over a two year period from December 2018 - December 2020. Data included diagnosis, primary mode of ventilation, aim of first cuff deflation, time tolerated for first cuff deflation (minutes), and number of days between first cuff deflation and decannulation.
Results: Eighteen consecutive patients were selected for early cuff deflation using the decision making tool with the following diagnoses: Encephalitis (5), COVID pneumonitis (5), Guillain Barre Syndrome (4), Intracerebral haemorrhage (1), Posterior communicating artery aneurysm (1), Motor Neurone Disease (1), Syringomyelia (1). At the time of the initial assessment, the ventilation status was: 10 patients on CPAP/PS, 4 on SIMV, 2 on High Flow Oxygen Therapy and 2 on a period of self-ventilation. The decision making tool defined the aim of the initial trial as “laryngeal wean” for 10 patients and “to facilitate communication” for 8. The median time for one way valve use for the initial trial was 10 minutes (range 4-25). There were no deleterious effects from following the protocol. All patients received further one way valve inline trials, and seventeen were weaned from the ventilator without respiratory compromise. One patient with Motor Neurone Disease remained ventilator dependent. Seventeen patients were subsequently decannulated (median 26.5 days after initial cuff deflation, range 12-209).
Conclusions: Eighteen neurointensive care patients were successfully able to use a one way valve inline in accordance with our decision making tool and protocol. It is hoped that our practice will prompt a wider discussion amongst different intensive care multidisciplinary teams about careful patient selection and judicious use of a one way valve inline. We plan to collect patient’s experience of the practice and to update our protocol with emerging evidence around optimal ventilator settings for using one way valves inline.
References
1. Freeman-Sanderson AL, Togher L, Elkins MR, Phipps PR. Return of voice for ventilated tracheostomy patients in ICU: a randomized controlled trial of early-targeted intervention. Critical Care Medicine. 2016; 44(6):1075-1081.
2. Kowalski S, El-Gabalaway R, Macaulay K, Thorkelsson R, Robertson A, Bshouty Z, Girling L. Weaning from mechanical ventilation using tracheostomy cuff deflation and a one-way speaking valve: a historical cohort series. Can J Anesth/J Can Anesth. 2017;64:1286-1288.
3. Sutt AL, Cornwell P, MD Kinneally, Fraser JF. The use of tracheostomy speaking valves in mechanically ventilated patients results in improved communication and does not prolong ventilation time in cardiothoracic intensive care unit patients. Journal of Critical Care. 2015;3.
4. Sutt AL, Fraser J. Speaking valves as part of standard care with tracheostomized mechanically ventilated patients in intensive care unit. Journal of Critical Care. 2015;1119-1120.
5. Sutt AL, Caruana LR, Dunster KR, Cornwell PL, Anstey CM, Fraser JF. Speaking valves in tracheostomised ICU patients weaning off mechanical ventilation – do they facilitate lung recruitment? Critical Care. 2016;20:91.
P201
The value of Fibreoptic Endoscopic Evaluation of Swallowing (FEES) in weaning a patient with a tracheostomy
Tracheostomy
Eibhlin Cleary and Angela Posada
St Georges Hospital
Abstract
Introduction: Fibreoptic endoscopic evaluation of swallowing (FEES) is an established instrumental assessment tool to evaluate laryngeal and pharyngeal structures related to secretion management and swallowing (Langmore, 2001). The various benefits of FEES, have been identified in research findings, including: its ability to visualize aspiration events and pharyngeal secretions (Hiss and Postma 2003). Despite its benefits, FEES remains an underutilised tool across the UK and McGowan et.al (2001) found over 40% of SLTs in the UK seldom or never using either FEES or videofluoroscopy with tracheostomised patients. The literature gives less emphasis to the role of FEES in informing tracheostomy weaning. At St George’s Hospital, a 1,000 bedded hospital with specialisms including, neurology, neurosurgery, Head and Neck, trauma and cardiac the use of FEES to aid tracheostomy weaning has been identified. This study highlights the value of FEES in progressing tracheostomy weaning with a review of outcomes over 12 months in 2019.
Methods: A retrospective analysis was conducted of FEES referrals and assessments completed over 12 months across acute SLT services. These were recorded on a single spreadsheet that collated outcome data per patient referral. Clinical outcomes were collected for secretion severity rating (Murray et.al 1996), penetration aspiration scale (Rosenbek et.al 1996), feeding outcomes, alternative feeding and management recommendations. An analysis of the data demonstrates trends in activity and impact on clinical decision making.
Results: Of the total number of FEES assessments completed (n=78) in 2019 50% were patients with a tracheostomy. 41% of these tracheostomised patients were still receiving mechanical ventilation at the time of the FEES assessment highlighting the acuity of this patient group with 59% of these patients being on a critical care unit. FEES informed tracheostomy weaning decisions in 59% of these patients. 62% of tracheostomised patients who had a FEES assessment had a secretion severity score of 3 on the Murray Secretion Severity Rating Scale (1996) and subsequently FEES informed pharmaceutical secretion management in 29% of this group. 48% of tracheostomised patients who had a FEES assessment had a score of 8 on the Rosenbek (1996) penetration aspiration scale and 18% of patients who were NBM started oral intake following FEES. No patients who had commenced oral intake were made NBM following FEES assessment. Specific dysphagia therapy plans were enabled following FEES in 48% of patients. Referral to ENT following FEES assessment was made in 18% of tracheostomised patients.
Conclusion: This data highlights the value of FEES assessment with patients who have a tracheostomy. St Georges Speech and Language Therapists are increasingly recognising this with 1/2 of the total number of FEES assessments in 2019 being with tracheostomised patients. FEES assessments with this patient group allowed detailed assessment of oral pharyngeal secretion management and dysphagia which in turn influenced tracheostomy weaning decisions and oral feeding. Using FEES early in a patient’s critical care journey can provide objective clinical findings to inform weaning management plans with the overall aim to reduce the time to decannulation.
References
1. Langmore, S., Endoscopic evaluation and treatment of swallowing disorders. 2001, New York, NY: Thieme.
2. Hiss, S. G. and Postma, G. N., 2003, Fiberoptic endoscopic evaluation of swallowing. Laryngoscope, 113(8), 1386–1393.
3. McGowan, S. L., Ward, E. C., Wall, L. R, Shellshear L.R. and AL. Spurgin, 2014, UK survey of clinical consistency in tracheostomy management International Journal of Language Communication Disorder,49 (1), 127–138.
4. Murray, J., Langmore SE, Ginsberg S, Dostie A, (1996) The significance of accumulated oropharyngeal secretions and swallowing frequency in predicting aspiration. Dysphagia. 11(2): 99-103.
5. Rosenbek, J. C., Robbins, J., Roecker, E. B., Coyle, J. L., & Wood, J. L. (1996). A penetration-aspiration scale. Dysphagia, 11(2), 93–98.
P202
The use of the Passy Muir Valve with COVID-19 Veno-Venous Extra Corporeal Membrane Oxygenation patients; a case series
Tracheostomy
Annie Martin
Royal Papworth hospital NHS Foundation Trust
Abstract
Introduction: Our Trust is a large academic and Veno-Venous Extra Corporeal Membrane Oxygenation (VV ECMO) national centre. During the first COVID-19 surge, our centre supported 35 patients using VV ECMO. This case series details the use of the Passy Muir one-way speaking valve (PMV) with four COVID-19 patients on VV ECMO; a new practice at our centre.
Objectives: To describe:
1. Using the PMV in-line with the ventilator circuit with COVID-19 patients on VV ECMO.
2. Benefits, risk assessment and patient experience.
3. Implications on the Physiotherapy service.
Methods: The notes of the four patients were reviewed retrospectively to collect data as per tables one and two.
In line with the Trust PMV guidelines, the four patients who used the PMV were assessed by a Physiotherapist. A risk assessment was completed prior to each session which included: cardiovascular stability, staff competence and discussion with the Critical Care Area (CCA) Multi-Disciplinary Team (MDT).
The PMV is a high-risk device. In accordance with the Trust PMV guidelines, a Physiotherapist led each session and stayed with the patient throughout. This reduced the risks associated with using the PMV in an area where few staff had been trained.
Results: Patient feedback included decreased work of breathing and appreciation for being able to speak with family. Two patients were able to engage with the CCA MDT to make decisions about their care.
Following joint Physiotherapy and Speech and Language Therapy assessment two patients, including one who underwent Fiberoptic Endoscopic Evaluation of Swallowing (FEES), were safe to have oral intake whilst on the PMV. Oral intake whilst ventilated via tracheostomy was not possible at our centre prior to the introduction of the PMV.
Twenty out of a total of 42 PMV sessions were stopped due to lack of Physiotherapist time; the most common reason for ending a PMV session. Two sessions were stopped due to coughing and seven due to patient request.
There were four episodes of adverse events during a total of 42 PMV trials; two episodes of hypotension and two episodes of coughing. On each occurrence the PMV trial was stopped and the patient recovered.
Table 1.
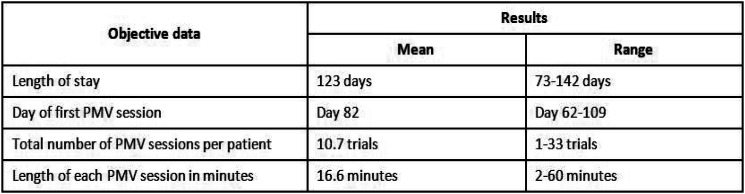
|
Table 2.
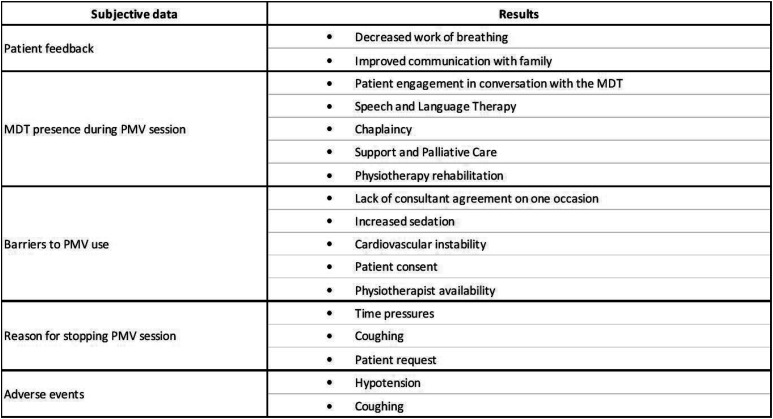
|
Conclusion: The use of the PMV with these four COVID-19 patients on VV ECMO proved safe and effective. It facilitated patient centred care by supporting communication and enabling oral intake.
There were instances where patients were unable to use PMV due to demands on Physiotherapy time and availability. Additional training is required for senior CCA nurses to be competent using the PMV.
Further data collection is required to fully understand the impact, safety and effectiveness of the PMV with this patient group but initial results are encouraging.
P203
Routine early tracheostomies in severe pneumonia: should TRACMAN have put this to bed?
Tracheostomy
Madeleine Wood 1 , Richard Grimwood1, Anthony J Rostron2 and Tom Sams3
1Northern Deanary
2Sunderland Royal Hospital
3Cumberland Infirmary
Abstract
Introduction: Within the North East and Cumbria, a network of 15 adult intensive care units (ICU), Cumberland Infirmary in Carlisle (CIC) is renowned for high rates of early tracheostomies, despite their intensivists having similar training backgrounds. We performed an observation of practice at Cumberland Infirmary and Sunderland Royal Hospital (SRH), to determine if this perceived variation in practice was real.
TRACMAN demonstrated no mortality benefit with early tracheostomies and suggested that intensivists were poor at identifying patients who required ventilation for over 7 days.1 TRACMAN showed no increased harm in the early tracheostomy group. Studies have shown a reduction in sedation and ICU length of stay in patients who underwent early tracheostomies, but the evidence is weak and often conflicting.2,3
Objectives: To establish whether the proportion of patients who underwent tracheostomy and when it was undertaken was different between the two ICUs, and if this translated into a difference in patient outcome.
Methods: Ward watcher data was interrogated between 01/08/2018 and 31/07/2019 for patients admitted with pneumonia as a primary or secondary diagnosis, who had been ventilated for greater than 48 hours. Baseline gender, age, aetiology (community vs hospital acquired) and APACHE II scores were collected to ensure adequately matched groups. Patients with pre-existing tracheostomies were excluded. Data was collected for whether a tracheostomy was performed, when the tracheostomy was performed, number of days sedated, duration of mechanical ventilation, ICU length of stay and survival to ICU discharge.
Results: CIC performed tracheostomies in 82.5% of 40 patients ventilated for over 48 hours for pneumonia, whilst SRH performed tracheostomies in 20% of their 35 patients (p< 0.00001). The median time to tracheostomy was two days at CIC (range 1-7 days) and 8 days at SRH (range 0-16 days) (p<0.001). There was no significant difference in days sedated, duration of mechanical ventilation, length of ICU stay or survival to ICU discharge.
Conclusion: Two similar ICUs had a disparate approach to the timing of tracheostomies in patients with pneumonia. Drawing any conclusions about patient outcomes is not possible with this number of patients. Even with much larger datasets determining differences in relevant patient centred outcomes between early and late tracheostomies is difficult.2
Although TRACMAN provided good evidence that early tracheostomies did not improve 30-day mortality, it is not the whole story. The heterogeneity of ICU patients makes differences in length of stay and consequences of ventilation and sedation, such as delirium, difficult to study. Challenges in long term follow up of ICU patients and the low rates of complications, make study of harm difficult to quantify. Discussion about variation in practice is however important to help us reflect on our practice and apply the evidence available to us.
Neither early tracheostomies for all patients, nor waiting for a set time or number of failed extubations is likely to be universally correct. Further research to identify patients that might benefit from an early tracheostomy would be helpful.
References
1. Young D, Harrison DA, Cuthbertson BH, Rowan K, Collaborators T. Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: the TracMan randomized trial. JAMA. 2013;309(20):2121-2129.
2. Szakmany T, Russell P, Wilkes AR, Hall JE. Effect of early tracheostomy on resource utilization and clinical outcomes in critically ill patients: meta-analysis of randomized controlled trials. Br J Anaesth. 2015;114(3):396-405.
3. Siempos II, Ntaidou TK, Filippidis FT, Choi AMK. Effect of early versus late or no tracheostomy on mortality and pneumonia of critically ill patients receiving mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(2):150-158.
P204
What matters most to ICU patients with a tracheostomy and what are the implications for clinical practice? A qualitative systematic review and metasynthesis
Tracheostomy
Helen Newman 1 , Sarah Wallace2, Gemma Clunie3, Christina Smith4 and Natalie Pattison5
1Royal Free London NHS Foundation Trust; UCL Division of Surgery
2Manchester University NHS Foundation Trust
3Imperial College Healthcare NHS Trust
4UCL Department of Language and Cognition
5University of Hertfordshire/East & North Herts NHS Trust
Abstract
Introduction: Tracheostomy is a common surgical procedure in intensive care involving the insertion of an artificial airway through the front of the neck into the trachea. Most patients with a tracheostomy experience a period of being unable to speak. The evidence-base to support tracheostomy management decisions is poor.1 Much of the literature focuses on timing and technique of insertion and uses hospital outcomes such as mortality or length of stay to measure success. Clinicians lack data on what matters most to patients to support patient-centred management decisions.
Objectives: To describe the key tracheostomy-related concerns and experiences of patients in intensive care and consider practice implications.
Methods:
Design: systematic review and metasynthesis of qualitative literature on patient experience of tracheostomy.
Setting: intensive care.
Population: adults with a tracheostomy.
Inclusion criteria: qualitative data on the experience of tracheostomy from patients’ perspectives; full text in English language.
Exclusion criteria: paediatric or wholly quantitative studies.
Search strategy: comprehensive search: four bibliographic databases; grey literature search; expert recommendation.
Data selection/extraction: search returns were uploaded into EPPI-Reviewer2 software. Titles and abstracts were reviewed by two reviewers, with disagreements arbitrated by a third reviewer. Full-text eligibility was assessed in a similar manner. Metasynthesis was achieved using thematic synthesis.3 Descriptive themes and sub-themes were additionally analysed using the eight dimensions of the Humanisation Value Framework (HVF)4 (Table 1) to generate analytical themes, which were then applied to the research question.
Table 1.
Conceptual framework of the dimensions of humanisation. Reproduced from Todres et al (2009)4 under the Creative Common Licence.
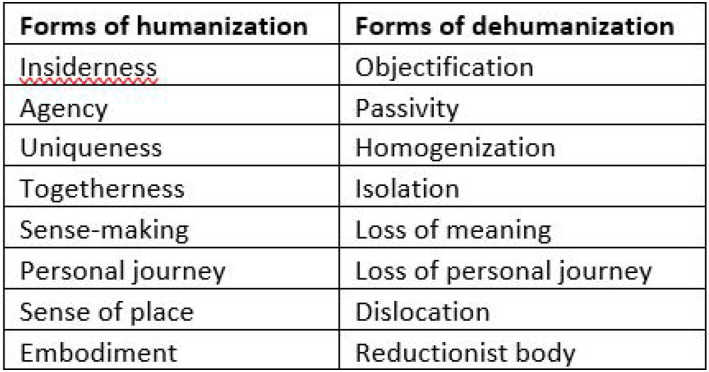
|
Results: Initial searches returned 2971 articles (Figure 1). Full-text screening was completed on 127 articles and 13 articles were included in the metasynthesis. The review encompassed data from 203 participants across 7 countries. Five major descriptive themes emerged: ‘Voice and communication’; ‘Autonomy and self-identity’; ‘Psychological needs and experiences’; ‘Physical needs and experiences’; and ‘Facilitators to wellbeing and recovery’ (Table 2).
Figure 1.
PRISMA flow diagram of search results and article selection process.
Table 2.
Descriptive themes and sub-themes: Autonomy and self-identity
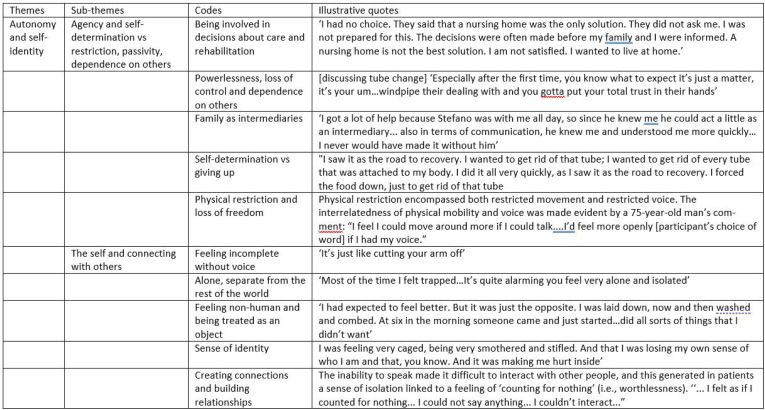
|
The metasynthesis revealed that patients wanted to feel and be treated as humans in a holistic sense: individuals with a unique view of the world; having control over own actions and what was done to them; connected with others; able to make sense of what was happening; continuing their own personal story; and experiencing events through integration of physical senses and their mind’s interpretation. Meeting these needs required humanity in care. Good communication was the medium through which positive patient-centred outcomes were achieved. Poor communication was associated with dehumanising care. Lack of natural voice was a major threat to both good communication and patients’ identities.
Conclusions: Healthcare that focuses on the physical body over the person as a whole risks dehumanisation of patients. Being able to speak helps patients maintain their identity and helps patients and staff jointly achieve positive patient-centred outcomes.
Preserving voice should be given high priority in tracheostomy management decisions, e.g. tube size, cuff deflation and the use of speaking valves. Healthcare staff training should promote understanding of humanised care and identification and management of issues that threaten it. Further research is needed to identify measures to capture humanised care.
Grants: Authors one and three hold HEE/NIHR Clinical Doctoral Research Fellowships
References
1. Wilkinson KA, Martin IC, Freeth H, Kelly K, Mason M. On the right Trach? The National Confidential Enquiry into Patient Outcome and Death. https://www.ncepod.org.uk/2014report1/downloads/OnTheRightTrach_FullReport.pdf (2014, accessed 20 Aug 2021)
2. Thomas J, Graziosi S, Brunton J, Ghouze Z, O’Driscoll P, Bond M (2020). EPPI-Reviewer: advanced software for systematic reviews, maps and evidence synthesis. EPPI-Centre Software. London: UCL Social Research Institute.
3. Thomas J, Harden A (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 8: 45.
4. Todres L, Galvin K, Holloway I (2009). The humanisation of healthcare: a value framework for qualitative research. Int J Qual Stud Heal 1: 1-10.
P205
Tracheostomy confidence on a general intensive care unit: a survey
Tracheostomy
Luke Bracegirdle 1 and Ben Booth2
1University Hospital Southampton NHS Foundation
2University Hospital Southampton NHS Foundation Trust
Abstract
Introduction: The COVID-19 pandemic led to mass redeployment of the clinical workforce to support intensive care units. Many junior doctors and nurses have little to no experience of dealing with patients with a tracheostomy. Tracheostomies are common in the critically unwell, with approximately 12,500 performed each year in England. Indications may include upper airway obstruction, airway protection, weaning, long-term ventilation, or secretion management; the clinical course of COVID-19 means more patients than ever are receiving a tracheostomy as part of their standard care. Complications are common, and the nature of harm may depend on the clinical environment and level of staff training. Despite difficult airway guidelines becoming widely accepted, tracheostomy emergencies were historically managed by relying on individually acquired skills. NAP41 highlighted a number of significant tracheostomy complications. As a consequence, national guidelines for emergency tracheostomy were published in 2012.2 The National Tracheostomy Safety Project advocates for improved care and safety for patients with a tracheostomy.
Objectives: To establish the confidence and competence at dealing with tracheostomy emergencies in a cohort of existing and redeployed general intensive care staff.
Methods: We devised and disseminated a survey to all clinical staff working on the general ICU in a single tertiary university hospital during the COVID-19 second wave. We received 40 responses from a diverse group including doctors of varying grades, ACCPs and nurses of ICU and non-ICU background.
Results: The majority of respondents had looked after a patient with a tracheostomy within the last week. Most had experience with dealing with an emergency and were aware of the national tracheostomy safety project. Despite this, the majority were not confident at dealing with tracheostomy emergencies. Of concern, the majority had received no formal training on dealing with tracheostomy emergencies. The overwhelming majority would like further training.
Conclusion: The clinical course of COVID-19 means many more patients than normal are receiving a tracheostomy as part of their standrad care. There is a clear need and want for further training for clinical staff on dealing with tracheostomy emergencies, especially in the event of a repeat mass redeployment.
References
1. Cook T, Woodall N, Frerk C, Royal College of Anaesthetists (Great Britain), Difficult Airway Society (Great Britain). Major complications of airway management in the United Kingdom: report and findings : 4th National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society : NAP4. 2011.
2. McGrath BA, Bates L, Atkinson D, Moore JA, National Tracheostomy Safety Project. Multidisciplinary guidelines for the management of tracheostomy and laryngectomy airway emergencies. Anaesthesia 2012; 67: 1025–1041
P206
Knowledge of tracheostomy care and emergencies amongst adult intensive care unit staff during the COVID-19 pandemic
Tracheostomy
Shobhit Saxena and Deborah Dawson
St. George’s University Hospitals NHS Foundation Trust
Abstract
Introduction: The COVID-19 pandemic has posed unique challenges to the undertaking of tracheostomies in the critical care setting. With patients quickly overwhelming intensive care units (ICU) worldwide and requiring ventilatory support for extended periods of time, many of them have required tracheostomies to facilitate recovery.1 Whilst considerable attention has been paid to optimising staff safety during the procedure and the timing of the procedure itself,2 it is equally crucial to ensure that critical care staff are well-trained and confident in dealing with routine tracheostomy care and potential emergency scenarios on a day-to-day basis.
Objectives: To qualitatively assess the knowledge of tracheostomy care and emergencies through the administration of a questionnaire to nurses and doctors working in our general adult ICU department. To subsequently construct a teaching curriculum informed by the questionnaire results and deliver a formal course to all ICU staff members caring for tracheostomy patients.
Methods: A 15-item paper questionnaire was designed. In order to gauge a reliable baseline of staff familiarity with tracheostomies, the format used was open questions rather than multiple choice, with pre-determined ideal answers set in line with the guidelines issued by the National Tracheostomy Safety Project (NTSP) and our own Trust. Six questions focused on tracheostomy care and five questions were based on tracheostomy emergency scenarios. The questions and answers were subsequently validated by a panel of consultant ICU nurses with a specialist interest in tracheostomy care and education. The final questionnaire was then distributed to junior doctors and nurses in our ICU department.
Results: A total of 32 completed questionnaires were returned from 60 distributed (53% response rate): 9 from junior doctors and 23 from nursing staff. Of the nurses, 15 were Band 5 and 8 were Band 6. The grade of junior doctor respondents ranged from Foundation Programme Year 1 to Core Training Year 2. The average total of correct answers submitted by doctors was 30.9%, 39.1% by Band 5 nurses and 75% by Band 6 nurses. All respondents stated that they would benefit from a tracheostomy teaching course, highlighting physiology, tracheostomy tube types and emergency simulation as preferred areas of focus. Based on the responses to individual questions, five domains were identified and selected for a proposed teaching curriculum aimed all at ICU clinical staff: (1) Clinical science, (2) Tracheostomy tubes, (3) Suctioning, (4) Cuff management and (5) Emergency scenarios.
Conclusion: The survey indicated that there was a lack of sufficient knowledge relating to tracheostomy care and emergencies amongst junior doctors and Band 5 nurses working in the ICU department and an unmet need for appropriate training dedicated to the subject. There is no doubt that the COVID-19 pandemic caused significant disruption to educational opportunities. Using the areas highlighted from the questionnaire, we propose the delivery of a tracheostomy course aimed at all critical care staff members. Our aim would be to eventually expand the curriculum to also encompass the ward setting, ensuring that all hospital staff responsible for the care of tracheostomy patients are component and confident in doing so.
References
1. McGrath BA, Brenner MJ, Warrillow SJ, et al. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med 2020; 8: 717-725.
2. Kwak PE, Connors JR, Benedict PA, et al. Early outcomes from early tracheostomy for patients with COVID-19. JAMA Otolaryngol Head Neck Surg 2021; 147(3): 239-244.
P207
A comparison of complications associated with percutaneous and surgical tracheostomies
Tracheostomy
Alexandra Cockroft 1 , Andrew Claxton2 and Richard Protheroe2
1The Northern Hospital
2Salford Royal NHS Foundation Trust
Abstract
Introduction: Tracheostomy is a frequently performed procedure in critically ill patients. Both percutaneous dilatation tracheostomy (PDT) and open surgical tracheostomy (OST) can be associated with complications and significant morbidity.
Objectives: We aimed to determine the complications associated with tracheostomies on the Intensive Care Unit (ICU) at Salford Royal Hospital, UK. We aimed to compare the complication rates between PDT and OST.
Methods: We conducted a retrospective analysis of all patients on ICU at Salford Royal Hospital who underwent a tracheostomy, between January 2018 and December 2019. We reviewed procedure related (bleeding, pneumothorax, surgical emphysema, or procedure failure) and maintenance related (bleeding, skin breakdown, swelling, cannula displacement or infection requiring antibiotics) complications.
Results: 161 patients had a tracheostomy inserted: 138 PDT and 23 OST. The number of days to tracheostomy was longer for OST; 15 days (SD 10) vs 11 days (SD 6.4) (p = 0.073). Average length of stay on ICU did not differ between PDT and OST; 28 (SD 24) and 27 (SD 19) days, respectively (p = 0.94). The most common reasons for OST were aberrant vessels over the trachea (30%) and C-spine injury (17%).
Procedure related complications rates did not differ between groups (p = 0.97). The OST group experienced significantly more maintenance related complications than PDT; 30.4% vs 6.5%, respectively (p<0.05). OST experienced higher rates of; infection 13% vs 1.5%, skin breakdown 8.7% vs 1.4%, bleeding 4.3% vs 0.7%, and displacement 4.3% vs 2.9%.
Conclusion: OST are associated with significantly higher rates of maintenance related complications, particularly infection. Further research is needed to develop protocols for identifying those patients who would classically go for OST, who may benefit from a hybrid approach tracheostomy.
P208
Critical care transfer bags: improving maintenance and efficacy off unit
Transfer and retrieval
Sadie Seal1 and Ryoki Arimoto2
1Wexham Park Hospital
2Royal Berkshire Hospital
Abstract
Introduction: The Royal Berkshire Hospital is a busy teaching DGH with a 17 bed adult ICU and over 1000 admissions to intensive care annually.1 It is imperative to have a functional critical care transfer bag for use in critical/emergency situations to help facilitate high quality patient care.
Initially on the unit there was a critical care kit, comprising of three bags with intended weekly checks. The bags contained equipment to help deal with airway emergencies as well as anaesthetic and emergency drugs. These bags however were missing certain key items such as neuromuscular blockers for RSIs and could often go for long periods without being restocked or checked due to time constraints on the unit and the inefficiency of the system.
Objectives: The aim of this QIP was firstly to create a standardised approach to the checking and refilling of critical care bags by making this process as user-friendly and time efficient as possible. This was in order to eliminate the variability we were encountering. Secondly we wished to optimise the essential drugs and equipment available in the bags for emergency situations.
Methods: The project included an initial data collection followed by four phases. The initial data was collected whilst on shift (real time 14 days). Phase 1 (retrospective study 28 days) introduced a kit checklist and the introduction of rocuronium. Phase 2 (retrospective study 42 days) was staff education about the kit and changes. Phase 3 (retrospective study 56 days) introduced a new consolidated transfer bag followed by video communication to staff. Phase 4 (commenced 1/5/21 and finishes 30/9/21) includes further staff training, a new refill station and a refined checklist.
Results: During the initial data collection the mean refill time of the critical care bags was 39 hours with multiple expired drugs and inconsistencies across the different bags on the unit. Interim analysis of data collected up to the start of phase 4 shows significantly reduced refill times, reduced on average to 3 hours. There is also more frequent checking of the transfer bags with ongoing positive qualitative feedback from trainees on the unit regarding the functionality of the bag and its contents.
Conclusion: Preliminary analysis suggests improved efficiency in restocking of the critical care bags, allowing for more time on the unit to focus upon patient care. Qualitative feedback is also suggestive of improved functionality of the transfer bag in emergency situations off of the unit with increased availability of emergency equipment and drugs.
References
1. Intensive Care Units for Training [Internet]. Oxford Intensive Care Medicine. 2021 [cited 11 August 2021]. Available from: https://www.oxfordicm.co.uk/readingintensivecare
P209
How the delivery of a Transfer Practitioner induction program supported the rapid upscale of an Adult Critical Care Transfer Service during a surge of Covid-19
Transfer and retrieval
Amy Formstone, Caroline Hindley, Scott Grier and David Ashton-Cleary
Retrieve
Abstract
Introduction: Retrieve, the South West’s dedicated Adult Critical Care Transfer Service (ACCTS), went live on 2 November 2020. As one of the first ACCTS in the country, every element of Retrieve’s operational and clinical service had to be developed from scratch. Within two months of going live, the service was asked to rapidly expand its service provision to meet the demands of the pandemic. The Transfer Practitioner (TP) training proved to be an essential component of the service’s ability to deliver this.
Retrieve transfers are performed by a Duty Consultant and a TP operating from bases in Cornwall and Bristol. Along with a core leadership team, the twelve newly appointed full-time TPs, all experienced critical care nurses, became essential to the day-to-day delivery of a high quality, safe, service and were a continuous presence at a time of rapid temporary clinician influx.
Objectives: The objective of the TP induction program was to create a cohort of highly trained practitioners who could guide the delivery of a high-quality service even during times of rapid expansion. This induction program was novel and had to be delivered across the challenging geography of the South West region.
Commissioned, developed and launched during the COVID-19 pandemic, Retrieve’s service design needed to be scalable, flexible and agile, during a time of remarkably challenging operational pressure.
Methods: The induction program was developed and led by the Retrieve Base Lead Nurses and was delivered by a multidisciplinary faculty across two base locations, including face-to-face and virtual sessions. Presentations on a variety of clinical transfer-specific topics as well as Retrieve governance and SOP’s. The sessions included small group teaching, equipment familiarisation and a modified Neonatal, Adult and Paediatric Safe Transfer and Retrieval (NAPSTaR) course. The program concluded with the two teams coming together at NHS Nightingale Hospital Bristol for two days of simulation scenarios in a Covid-19 safe manner.
Results: The induction program established and promoted team cohesion. Created a safe space to learn new techniques and ensured the service had an agile and flexible workforce.
Within two months of launch, Retrieve was able to double in size within days of the NHS England instruction to provide additional capacity and capability. Secondary to the success of induction, with TPs a continuous presence for each transfer, Retrieve was able to rapidly onboard forty ‘surge doctors’ helping to provide high-quality transfers. Undertaking both business as usual and a large number of regional and inter-regional capacity transfers, including 100% of regional capacity transfers.1
Conclusion: The induction was a key component of how Retrieve was able to establish a solid foundation.
The transfer practitioners have key buy-in, are engaged in service development and improvement, and take pride in being part of a novel service.
Developing a service during a period of such operational pressure has been challenging, but implementing a considered, systematic, team-focused, equitable induction program was one element of how Retrieve became an agile and flexible service, responsive to providing additional capacity when required.
References
1. Grier S, Carpenter-Clawson C, Ashton-Cleary D, Formstone A, Hindley C. Retrieve Annual Report 2020/2021. Available from: www.retrieve.nhs.uk
P210
Sources of Delays Encountered by a Regional Critical Care Transfer and Retrieval Service
Transfer and retrieval
Victoria Jenkins 1 , Jonathon Dean2, Mamoun Abu-Habsa2 and Simon Finney2
1North East London Critical Care Transfer and Retrieval
2North East London Critical Care and Retrieval Service (NECCTAR)
Abstract
Introduction: NECCTAR, the North East London Critical Care Transfer And Retrieval Service, is a regionally funded retrieval service that provides a comprehensive local, regional, and national critical care transfer capability. Transfer teams may encounter unexpected delays during all parts of a patient’s journey, and from a wide variety of sources. These delays may impact the teams’ ability to provide an efficient service and may heighten risk in some instances. We set out to explore the significance of crew-reported delay incidents and any lessons learnt for refining service processes.
Objectives: Examine the sources, types, and significance of transfer delays formally reported by the critical care transfer team.
Methods: Each NECCTAR transfer included contemporaneous electronic capture of seven checkpoints throughout the journey, from initial tasking through to completion of the job and readiness for another tasking. Sources of delays reported by the NECCTAR team were formally recorded in full and then categorised. Unpaired two-tailed t-tests were used to compare the mean duration of time under NECCTAR care for transfers that had no recorded delay against the cohorts of transfers with recorded delays.
Results: In the period from December 10th to August 22nd, 2021, NECCTAR was tasked 382 times and completed 339 (88.7%) patient transfers. 275 completed transfers had no recorded delays. The mean time under NECCTAR care for a non-delayed job was 140.7 minutes.
The NECCTAR team formally reported delays in 64 transfers, which are summarised in Table 1.
Table 1.
Arterial gases and ventilatory indices pre and post transfer .
| Pre-departure | Arrival | |
|---|---|---|
| FiO2 | 1.0 | 1.0 |
| pH | 7.20 | 7.20 |
| pCO2 (kPa) | 8.65 | 8.96 |
| pO2 (kPa) | 9.87 | 10.7 |
| Haemoglobin (g/L) | 127 | 122 |
| Base excess (mmol/L) | -3.7 | -2.9 |
| Lactate (mmol/L) | 4.4 | 3.6 |
| Peak inspiratory pressure (cm H 2 O) | 32 | 32 |
| Positive end-expiratory pressure (cm H 2 0) | 10 | 8 |
| Tidal volume (ml) | 330 | 400 |
Table 1.
■■■.
| Delay Reason | Number of Jobs | Average Time under NECCTAR Care | Difference (min) | p-value |
|---|---|---|---|---|
| No delay | 275 | 140.7 | - | - |
| Referring site readiness | 21 | 196.7 | 56 | <0.0001 |
| Receiving site readiness | 12 | 168.0 | 27.3 | 0.05 |
| Patient Stabilisation and Optimisation | 11 | 161.5 | 20.8 | NS |
| Vehicle malfunction | 8 | 179.9 | 39.2 | 0.0245 |
| Equipment-Related Malfunctions | 8 | 162.9 | 22.2 | NS |
| Organisational Delays | 3 | 147.7 | 7.0 | NS |
| Road Traffic Collision | 1 | 140.0 | (0.7) | NS |
Conclusion: Any transfer of a critical care patient is recognised to be a high-risk episode, so minimising the duration of these episodes and making the transfer process as timely as possible is of significant importance to their care.1
Intensive care unit readiness and vehicle malfunction are the most significant sources of delay to NECCTAR’s safe and efficient critical care retrieval service. We have improved our referral process to prompt referring and receiving site readiness through specific proformas and instructions.
While stabilisation or optimisation time was reported as a delay in 11 episodes, this is likely an effective use of a critical care retrieval team’s expertise and alternative categorisation may be more appropriate. Referral checklists have since aided in expediting preparation of appropriate patients for non-clinical transfer as the service evolved with pre-and-post intervention impact assessment planned. Delays caused by vehicle malfunction will be mitigated as the fleet of ambulances utilised by NECCTAR is due to be upgraded next year. Significance testing applied to low incidence causes of delay is limited by the small numbers.
NECCTAR continues to capture data to analyse where delays are occurring and whether solutions are effective.
References
1. Foex B, Van Zwanenberg G, Ball J, et al. The Transfer of the Critically Ill Adult. Faculty of Intensive Care Medicine; Intensive Care Society 2019. https://www.ficm.ac.uk/sites/default/files/transfer_critically_ill_adult_2019.pdf (accessed 22nd August 2021)
P211
Translating critical incidents to service development in urban critical care transfer
Transfer and retrieval
Philip Leadbeater, Nicole Tribe, Jonathon Dean, Ben Singer and Mamoun Abu-Habsa
North East London Critical Care Transfer and Retrieval Service
Abstract
Introduction: Clinicians in retrieval and transfer medicine face increased diagnostic uncertainty by virtue of their operational environment.1 Integral to our quality improvement and clinical governance framework is individual case analysis, clinical incident interrogation and follow up of every single patient to the point of discharge from critical care. We describe a case where an adverse clinical incident several hours post patient handover was a driver for implementing process and diagnostic change within our own service.
Objectives: Describe the translation of after-action review of a critical incident into service improvement.
Methods: A 61-year-old patient with severe acute respiratory distress syndrome (ARDS) secondary to coronavirus disease 2019 (COVID-19) developed an ischaemic lower limb. A diagnosis of femoral artery thrombosis was confirmed by computed tomography angiography, necessitating transfer to the regional vascular centre. The transfer was undertaken following emergent intubation of the patient by the referring unit and patient followup proceeded as per our standard operating procedures.
Results: The transition to invasive ventilation demonstrated low lung compliance and a poor alveolar-arterial (A-a) gradient in keeping with established ARDS secondary to COVID-19.2 Deterioration in oxygenation and respiratory mechanics was partially (falsely) attributed to switching from semi-recumbent to supine positioning.
Within 3 hours of handover to the receiving team, a rapid deterioration in oxygenation and ventilation occurred with subsequent diagnosis of tension pneumothorax. This was managed with an intercostal drain which resulted in a significant drop in peak airway pressure (24cm H2O).
Close collaboration between our service and the involved hospitals enabled a detailed multi-service review. A number of missed opportunities were identified for prevention of deterioration due to a tension pneumothorax:
1. Immediate post-intubation x-ray imaging regardless of time-critical nature of transfer
2. Lung POCUS post-intubation or at any point whilst transitioning care
3. Highlighting post-intubation imaging as an immediate post-arrival need at handover
Pre-departure, post-intubation x-ray was added to our checklist as a cognitive aid. We further identified lung point of care ultrasound (POCUS), an established adjunct to clinical examination,3,4 as a potentially missing diagnostic safety-net. Consequently, we set out to introduce a lung POCUS operating policy. This includes a device optimised for the pre-hospital environment (VScan Air, GE Healthcare, USA), training package, decision-aid algorithm, and overarching governance. We will monitor the diagnostic impact of this tool and benchmark against previously published literature.3,4
Conclusion: Robust followup, governance, and stakeholder engagement allowed us to identify an adverse event detected several hours post patient disposition at the receiving site. With an increasing volume and complexity of transfers, diagnostic adjuncts formerly considered the exclusively the domain of in-hospital practice may well become core techniques in retrieval medicine.
References
1. Intensive Care Society. Guidance On: The Transfer of the Critically Ill Adult. London: Intensive Care Society; 2019.
2. Grasselli G, Tonetti T, Protti A, Langer T, Girardis M, Bellani G, et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: a multicentre prospective observational study. Lancet Respir Med. 2020;8(12):1201–1208.
3. Bøtker MT, Jacobsen L, Rudolph SS, Knudsen L. The role of point of care ultrasound in prehospital critical care: a systematic review. Scand J Trauma Resusc Emerg Med. 2018;26(1):51.
4. Hew M, Tay TR. The efficacy of bedside chest ultrasound: from accuracy to outcomes. Eur Respir Rev. 2016;25(141):230.
P212
Designing a framework for long-range critical care transfer away from the epicentre of a crisis
Transfer and retrieval
Lydia Fletcher, James Waiting, Jonathon Dean and Mamoun Abu-Habsa
North East London Critical Care Transfer And Retrieval
Abstract
Introduction: The North East London Critical Care Transfer And Retrieval (NECCTAR) Service provides a complete adult critical transfer capability. During the second wave of the COVID-19 pandemic, London was the epicentre of critical care activity1. Resource pressures escalated rapidly to unprecedented levels of demand.1 Beds for regional decompression became increasingly rare within London, necessitating long-range transfer. These were considered to be journeys over two hours in duration and to hospitals outside of the M25. NECCTAR was the first critical care transport service during this peak to decompress a London-based COVID-19 patient to a bed sourced nationally.
Although longer-range ground transfers are associated with inherent risks, these can be mitigated through a dedicated transfer team and equipment.2,3 NECCTAR was required to rapidly and iteratively design a framework for long-range transfers. The service leadership drew on experience from aeromedical pre-hospital resources. Detailed case review was undertaken to refine the standard operating procedure. As pandemic pressures have reduced, the guidance has now become translatable to longer-distance repatriation and specialist transfers.
Objective: To develop and refine a novel framework for maintaining patient safety during long-range critical care unit transfer.
Methods: Risks associated with long-range critical care ground transfers were broadly identified as patient, staff, and equipment/technical risks. Ethical considerations were prominent in planning. Risks were categorised for standard operating procedure design purposes. Data were contemporaneously recorded for all taskings from point of referral to completion. The risks and their mitigations are summarised in Table 1.
Table 1.
■■■.
| Risk Identified | Mitigation |
|---|---|
| Higher potential for clinical deterioration | Dedicated consultant led patient triage and selection |
| Increased patient exclusion criteria | |
| Higher level of seniority for transferring crew | |
| AAGBI compliant monitoring | |
| Trial on transport ventilator | |
| Patient exposure to environment | Heating packs, ambulance warmers, blankets |
| Focus on packaging/pressure area management | |
| Limited oxygen supply with potential associated high ambient oxygen | Cylinder manifold |
| Oxygen consumption formally calculated | |
| Ambient oxygen sensors | |
| Limited medical intervention available over prolonged/higher risk period | Additional equipment for management and intervention including Hamilton T1 ventilator, defibrillator, and point of care devices |
| Medication provision: adequate infusion/sedation and regular medications | |
| Planned diverts as below | |
| Provision of emergency assistance | Liaison with national ambulance services to plan for roadside rendezvous |
| Formal planning of available route diverts | |
| Crew exposure to environment including aerosolised SARS-CoV-2 | PPE |
| Ambulance ventilation | |
| Overnight rest available if weather conditions prohibit return | |
| Medicolegal and ethical considerations regarding prolonged transfer and distance from family | Ethics discussions |
| Multi-consultant decision making | |
| Family discussion | |
| Executive ownership of risk for transfer | |
| Fatigue with long journey times | Dedicated long-range crew |
| Early planning/tasking | |
| Limited senior decision making capacity | Advance directives to be carried |
| Technical failure of vehicle/inadequate fuel | Pre-planned risk mitigation by ambulance team |
| Limited equipment battery life | Inverter checks, pre-planned charging |
Results: An iteratively designed standard operating procedure was developed. NECCTAR has been referred 29 long-range missions and has completed 20 (68.9%) of these. Long-range taskings are significantly less likely to result in a completed transfer (68.9% v 88.3%, Fisher’s p=0.029), predominately due to unanticipated changes in clinical status prior to departure. The longest duration of time and distance travelled under NECCTAR care was 5 hours, 32 minutes and 278 kilometres, respectively.
All completed long-range transfers were followed up to discharge from intensive care; there were no significant adverse events in this group.
Conclusion: NECCTAR has developed a framework that ensures stringent patient selection and transfers by a dedicated, senior-led crew with multiple risk mitigations. A strong governance process has informed updates to maintain patient safety. This framework has now been adapted for repatriation and specialist transfers and would also be generalisable to major incidents, including biohazard events and natural disasters.
References
1. NHS Providers. COVID-19 pressures: an exploration of hospital activity through the first and second wave. https://nhsproviders.org/news-blogs/blogs/covid-19-pressures-an-exploration-of-hospital-activity-through-the-first-and-second-wave
2. Uusaro, A., Parviainen, I., Takala, J., & Ruokonen, E. (2002). Safe long-distance interhospital ground transfer of critically ill patients with acute severe unstable respiratory and circulatory failure. Intensive care medicine, 28(8), 1122–1125.
3. Moynihan, K., McSharry, B., Reed, P., & Buckley, D. (2016). Impact of Retrieval, Distance Traveled, and Referral Center on Outcomes in Unplanned Admissions to a National PICU. Pediatric critical care medicine: a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies, 17(2), e34–e42.
P213
The first 500 transfers of Retrieve, the South West’s dedicated Adult Critical Care Transfer Service: what does the data tell us?
Transfer and retrieval
Scott Grier1, David Ashton-Cleary2, Amy Formstone2 and Caroline Hindley 2
1Southmead Hospital, Bristol
2Retrieve Adult Critical Care Transfer Service
Abstract
Introduction: Retrieve is the South West’s dedicated Adult Critical Care Transfer Service (ACCTS), commissioned to meet the needs of the COVID-19 pandemic and build a permanent legacy for the region’s critical care patients.
The South West Critical Care Network (SWCCN) has long had an interest in critical care transfer and in 2020, published a retrospective analysis of its transfer activity.1 Whilst there were limitations of the data, it identified a clear need for a transfer service in terms of activity and the need to improve the consistency and quality of transfer care.
Retrieve launched on 2 November 2020 and undertakes all types of critical care transfer, from time-critical and urgent escalations of care to repatriations and capacity transfers. It operates two consultant-led clinical teams 12 hours a day. As a fully digital service, it has collected data about every referral and transfer since then. This dataset is essential in informing the ongoing development of Retrieve as well as other ACCTS across England.
Objectives: To describe the first 500 transfers undertaken by the Retrieve ACCTS and compare this to existing regional data.
Methods: Using the Retrieve electronic patient record and database system, the first 500 transfers that the service undertook were identified and an anonymised dataset downloaded. This data was categorised by type of transfer, time of day, referring and receiving hospitals, patient demographics, referring clinician and specialty.
Results: The first 500 transfers by Retrieve were completed in 258 days, with 161 (32%) being undertaken by the Peninsula team and 339 (68%) by the Severn team. Sixty one percent of transfers (303) were escalations of care to specialist centres, of which 1 in 3 were classified as ‘time critical’. The service undertook 87 repatriations (17% of work).
Capacity transfers (previously called ‘non-clinical transfers’) comprised 22% of transfers (110), including inter-regional mutual aid work undertaken as part of the COVID-19 wave 2 in January and February 2021.
Comparing the data to SWCCN published work, a smaller proportion of transfers were for escalation of care (61% vs 83.2%) and a higher proportion of repatriations (17% vs 10.5%).
Conclusion: The Retrieve data provides valuable insight into the work of a new dedicated ACCTS and is helpful in informing future development regionally and nationally.
The reasons for transfer are similar to published data1 but are skewed by the capacity transfer work generated by the COVID-19 pandemic as well as a strict adherence to database definitions and data integrity.
This data should provide reassurance to those involved in ACCTS development across England that the workload and approximately breakdown of types of transfer matches that which has been anticipated.
References
1. Grier S, Brant G, Gould TH, Vopelius-Feldt J, Thompson J. Critical care transfer in an English critical care network: analysis of 1124 transfers delivered by an ad-hoc system. J Intensive Care Soc, 2020;21:33-39.
P215
Does an Admission for Major Trauma Increase the Risk of Infectious Complications in the Longer Term?
Trauma
Hannah Ballheimer 1 , Emily Beesley1, Jaimin Patel2 and Dhruv Parekh2
1University of Birmingham Medical School
2Institute of Inflammation and Ageing, Queen Elizabeth Hospital
Abstract
Introduction: There is little evidence regarding the effect of major trauma and the development of long-term immune dysfunction.1 However, it is thought that severe injury can contribute to an impaired immune response, leading to chronic immunosuppression, and thus, increasing the risk of subsequent infections and re-hospitalisation. This susceptibility to infection may be due to an alteration in the immunomodulatory molecules that characterise the systemic inflammatory response syndrome (SIRS) and the opposing counter anti-inflammatory response syndrome (CARS).2,3 Following major trauma, immune cells involved in these inflammatory responses may be subject to alterations in gene expression known as epigenetic changes. These may be passed down from parent to daughter cells, allowing for immunosuppressive properties to persist for years after the initial insult has passed.4
Objectives:
1. To compare rates of readmission for infectious complications between patients of major and minor trauma.
2. To compare rates of readmission for all causes between patients of major and minor trauma.
These were assessed at 3 months, 6 months, 9 months, 1 year, 2 years and 3 years.
Methods: In this UK based cohort study, we analysed 1302 trauma patients who were admitted to the Intensive Care Unit of the Queen Elizabeth Hospital between January 2016 and January 2020. Data was collected from TARN and ICNARC databases, with patients divided into major and minor trauma cohorts based on their Injury Severity Score (ISS). Those with an ISS ≥ 15 were categorised into the major trauma cohort, and those with scores < 15 into the minor. Patients were followed up over 3 years and readmission rates for infectious complications were compared between the two cohorts. Additionally, readmission rates for all causes were compared between the cohorts, which included infectious, cardiovascular, gastroenterological, hepatic, neurological, traumatic, renal, respiratory, and orthopaedic causes.
Results: For those readmitted for infectious causes, univariable analysis showed major traumatic injury not to be associated with an increased risk of readmission (HR 0.952, 95% CI 0.155-7.904; p = 0.963). No multivariable analysis could be performed due to the small sample size. Additionally, Kaplan Meier survival analysis did not produce statistically significant results (p = 0.963).
For those readmitted for all causes, univariable analysis showed major trauma to be associated with an increased risk of readmission, but this was not statistically significant (HR1.548; 95% CI, 0.726-3.455; p = 0.248). Similarly, despite multivariable analysis showing major trauma to be associated with an increased risk of admission, this too was not considered to be statistically significant (HR 1.690, 95% CI 0.638-3.669; p = 0.212). Furthermore, Kaplan Meier survival analysis did not produce significant results (p = 0.244).
Conclusion: There were no long-term differences in readmission rates for infectious complications between major and minor trauma patients. There was also no difference in rates of readmission for all causes between the two trauma cohorts. Future research is needed to investigate the link between major trauma and the long-term consequences it may induce of the immune system, and thus, subsequent readmissions.
References
1. Osuka A, Ogura H, Ueyama M, Shimazu T, Lederer JA. Immune response to traumatic injury: harmony and discordance of immune system homeostasis. Acute Med Surg. 2014;1(2):63–69.
2. Brøchner AC, Toft P. Pathophysiology of the systemic inflammatory response after major accidental trauma. Scand J Trauma Resusc Emerg Med. 2009;17(1):43.
3. Ward NS, Casserly B, Ayala A. The Compensatory Anti-inflammatory Response Syndrome (CARS) in Critically Ill Patients. Clin Chest Med. 2008;29(4):617–625.
4. Carson WF, Cavassani KA, Dou Y, Kunkel SL. Epigenetic regulation of immune cell functions during post-septic immunosuppression. Epigenetics. 2011;6(3):273–283.
P216
Positive risk taking in physiotherapy management of poly-trauma patients
Trauma
Lauren Bradley and Zoe Van Willigen
University Hospital Southampton
Abstract
Background: Major trauma is defined as an injury or combination of injuries that are life-threatening and/or life changing.1Responsible for approximately 15,000 deaths in the UK every year; major trauma is the leading cause of death and major disability in under 45’s.2 Following major trauma, patients often have multiple injuries across body systems or “poly-trauma” although this term is poorly defined.
The critical care multidisciplinary team (MDT) is skilled and competent at managing these complex patients. Anecdotally, patients with blunt chest trauma develop secondary complications, such as post-injury pneumonia, within 24-72 hours. Physiotherapists are well placed within critical care teams to assess and begin early management, especially in those with chest trauma. However, often treatment modalities available to physiotherapists are not used until further along the patient journey.
We present a case study that demonstrates the benefit of positive risk taking, including the implementation of treatment modalities to aid secretion clearance and early rehabilitation in a poly-trauma patient. This case study demonstrates well the importance of daily MDT discussion in considering risk versus benefit of early chest physiotherapy in this patient group.
Objectives: This case study aims to demonstrate the benefit of early respiratory physiotherapy treatment in poly-trauma patients, alongside wider MDT discussion on risk versus benefit.
Methods: Treatments included: ventilator hyper-inflation, mechanical insufflation-exsufflation (cough assist), suction, breathing exercises, mobilisation and Positioning.
Treatment was implemented early in the patient journey, guided by clear MDT communication and established to ensure consistency out-of-hours and during the weekend.
Results: Early secretion management and rehabilitation contributed to successful weaning of mechanical ventilation support and extubation. Effective MDT communication allows physiotherapists to proactively treat chest trauma and begin early mobilisation with the support of the critical care environment.
Conclusions: Implementing cough assist and other physiotherapy interventions early in the management of this poly-trauma patient contributed to the prevention of secondary chest complications including post-injury pneumonia. Alongside effective MDT communication, critical care physiotherapists are skilled in the assessment and application of chest management techniques which contribute to the successful early management of poly-trauma patients.
References
1. National Clinical Guideline Centre (UK). Major Trauma: Assessment and Initial Management. London, UK: National Institute for Health and Care Excellence, 2016.
2. The Trauma Audit and Research Network. Performance Comparison: Trauma Care. https://www.tarn.ac.uk/Content.aspx?ca=15 (accessed 27 July 2021).
P218
Doctors well-being during COVID-19 in a tertiary hospital
Wellbeing
Christophe Korthoudt, Kegels Nathalie, Andreas Domen, Greta Moorkens and Vera Saldien
Antwerp University Hospital
Abstract
Introduction: COVID-19 has become the largest medical challenge of the last 50 years, affecting the whole world. Well-being can be scaled through the validated Warwick-Edinburgh Mental Well-being Scale (WEMWBS), mean score 50,7/70 general population sample.1
Objective: The aim of this study was to evaluate the well-being of physicians, during the second wave of the COVID-19 outbreak in a Belgian tertiary hospital, with special attention to anaesthesiologists who have been confronted with overcrowded intensive care units during several months challenging their physical and mental well-being.
Methods: All physicians in a tertiary Belgian hospital were invited to participate by e-mail during the second COVID-outbreak by an online anonymous questionnaire. All included persons gave their informed consent. The demographics collected were age, gender, function, COVID contact, workload and the WEMWBS score, summing 14 equally weighted questions (1 to 5) about mental well-being. SPPS, version 26.0, was used.
Results: 42 residents and 48 staff members completed the online survey with average WEMWBS 50.6±8.0. Participating residents worked significantly more on a COVID-19 department than participating specialists (p=0.02). These residents noticed that their workload was higher (p=0.001) and scored lower on the WEMBWS (48.1±8.2) compared to staff members (52.8±7.3), (p=0.01). Male anaesthesiologists scored significant higher in the WEMWBS compared to their female colleagues (p=0.03).
Conclusion: Physicians with a higher workload due to COVID reported a significantly lower well-being than those with a low workload. This small study showed a significant difference between the well-being of specialists and resident doctors. One out of five doctors experienced negative feelings. Attention should be paid on the prevention and treatment of well-being among healthcare workers, especially female anaesthesiologists.
References
1. Tennant R, Hiller L, Fishwick R. et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life 2007;5:63.
P219
Anything from the trolley? A service improvement project to implement leisure activities and well-being for long stay patients
Wellbeing
Camilla Mills 1 , Katie Dowling 1 and Tanya Nyatsambo2
1Royal Brompton and Harefield NHS Trust
2Royal Brompton Hospital
Abstract
Introduction: Admission to intensive care is a life changing event for people which can result in long term detriments to health, function and quality of life.1 Extensive literature exists and guidelines have been written supporting rehabilitation for these patients.2 More qualitative data is also being carried out on patients’ perspectives of rehabilitation in intensive care. This has highlighted ‘the noxious cycle of ICU’ where patients describe fatigue, boredom and lack of concentration.3
Family presence in intensive care can improve a patient’s recovery.4 The COVID-19 pandemic has led to more isolation for patients due to visiting restrictions. Partaking in creative activities is known to have many benefits for long stay hospital patients and can have positive impacts on their recovery.5 This led us to the development of a leisure activity trolley with the focus on enhancing well-being in long stay patients.
Objectives: The aim of this project is to enhance well-being in intensive care patients. This was done by supporting patients to engage with leisure activities.
Methods: A mixed methods questionnaire was used to collect data from four long stay patients. This data was used to gauge patients’ interests in participating in leisure actives and identify what equipment would be enjoyed. An application to the hospital patient amenities fund was made and funding was secured to purchase a variety of items based on the results of this questionnaire.
All long stay patients throughout the hospital including ITU and step down who were awake and medically stable were invited to participate. Patients were given a pre-activity questionnaire to gather information on their usual interests and rate their current mood using a Likert scale. This informed us to make suggestions on what they may enjoy. We also provided them with our ‘mindfulness menu’ to select what they’d like to do. Patients were then set up with their selected activities and given the option to engage alone or in the company of a therapist (see Image 1).
Image 1.
Playing connect-4 with an ICU patient on ECMO.
A post-activity questionnaire was completed to explore if patients enjoyed the activity. Patient mood following activity was also re-collected using a Likert scale. Patients could continue to partake in the activities chosen, try new ones, or cease to partake all together. Post activity questionnaires were completed after each session.
Results: 37 different patients were approached on 96 occasions. They chose to engage in activities on 87/96 (90%) of occasions (see Table 1 for activities). On average, patients’ moods improved from a Likhert score of 4.6/10 to 7.2/10, a 36% increase, following participation in a leisure activity. Patient satisfaction with activities offered on initial assessment and on discharge also improved. From this small sample size, patient’s well-being was enhanced by participation in leisure activities.
Table 1.
A graph showing activities undertaken.
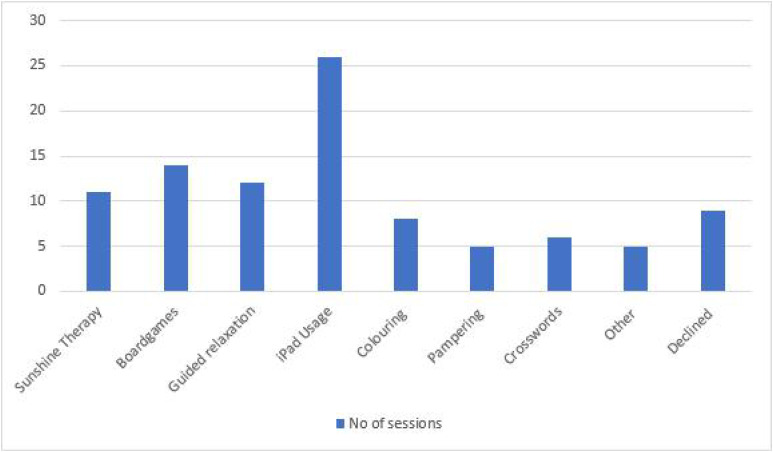
|
Conclusion: Overall, we have found this project to be successful thus far in improving well-being for intensive care patients. We plan to continue to offer these activities for our patients and hope it continues to improve patient wellbeing and recovery.
References
1. Fuke R, Hifumi T, Kondo Y, Hatakeyama J, Takei T, Yamakawa K, Inoue S, Nishida O. Early rehabilitation to prevent postintensive care syndrome in patients with critical illness: a systematic review and meta-analysis. BMJ open. 2018;8(5):e019998.
2. NICE CG83–rehabilitation after critical illness: implementation across a network. Nursing in critical care. 2013;18(1):32-42.
3. Corner EJ, Murray EJ, Brett SJ. Qualitative, grounded theory exploration of patients’ experience of early mobilisation, rehabilitation and recovery after critical illness. BMJ open. 2019;9(2):e026348.
4. Inoue S, Hatakeyama J, Kondo Y, Hifumi T, Sakuramoto H, Kawasaki T, Taito S, Nakamura K, Unoki T, Kawai Y, Kenmotsu Y. Post-intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Medicine & Surgery. 2019;6(3):233-246.
5. Hutcheson C, Ferguson H, Nish G, Gill L. Promoting mental wellbeing through activity in a mental health hospital. British Journal of Occupational Therapy. 2010;73(3):121-128.
P221
Evaluating interventions to promote the psychological wellbeing of critical care patients during the COVID-19 pandemic
Wellbeing
Clare Smedley 1 , Hannah Sainsbury2 and Lyndsay Cheater3
1Clare Smedley
2Countess of Chester Hospital
3Couness of Chester Hospital
Abstract
Introduction: It is well known that a proportion of patients who survive an ICU admission suffer ongoing physical, psychological and cognitive disability referred to as Post Intensive Care Syndrome.1 There is also evidence of increased frequency of anxiety, depression, and PTSD amongst survivors of ICU admission with ARDS,2 as such it is likely that those admitted with COVID-19 may suffer similarly.
There are several factors specific to the COVID-19 pandemic which are likely to exacerbate the effects of an ICU admission on the psychological wellbeing of survivors. These include lack of family visiting, staff wearing PPE, and frequent media content related to pandemic/healthcare. There is little evidence to guide what we can do as ICU staff to promote psychological wellbeing.
Objectives: To evaluate the relative benefits of three interventions trialled for ICU inpatients to help psychological recovery:
• Trips to an outside space - “The Garden”
• Facilitated video calls with family/friends
• Inpatient psychology sessions
Methods: We contacted individuals who survived an ICU admission for level 2 or 3 care having been treated for COVID-19 during March-May 2020. A total of 13 ICU survivors were successfully contacted after being identified from ICU follow up clinic. We collected qualitative data via questionnaires completed over the telephone facilitated by a member of ICU staff.
Results: 8/13 people had a video call with family or friends whilst in ICU and 5 of these identified that a video call was the most helpful of the three interventions for their psychological recovery (Chart 1). Survivors emphasised the joy of being able to see the faces of loved ones but also reported issues with signal and staff availability making it hard to plan video calls.
Chart 1.
Which of the three interventions was most helpful for your psychological recovery?
7/8 patients who had a trip to the garden would recommend this to others. People highlighted positives including feeling fresh air and sunshine, and the change of scenery/ getting away from the ICU. Many people identified being put off a garden trip by the preparation involved and 4/8 people identified feelings of guilt about the amount of staff time required to facilitate a trip to the garden.
Only 4 people remember having review by a member of the psychology team whilst an inpatient but 3/4 found this helped their recovery by helping them understand and explain their experiences. People who did not have access to psychology as an inpatient were asked if they thought they would have benefited from this experience. The majority said “do not know” because of concerns that they would have been too unwell to engage.
Conclusions: In the aftermath of the COVID-19 pandemic we are likely to see lasting impacts on the psychological wellbeing of ICU survivors. Further evidence is needed to evaluate the costs and benefits of measures to promote psychological wellbeing within ICU. However, this project suggests that there are simple interventions with minimal cost implications which can be easily implemented by ICUs to support the psychological recovery of their patients: video calls and trips to an outside space.
References
1. Rawal G, Yadav S, Kumar R. Post-intensive Care Syndrome: an Overview. J Transl Int Med. 2017;5(2):90-92. doi: 10.1515/jtim-2016-0016. PMID: 28721340; PMCID: PMC5506407.
2. Bienvenu OJ, Friedman LA, Colantuoni E, Dinglas VD, Sepulveda KA, Mendez-Tellez P, Shanholz C, Pronovost PJ, Needham DM. Psychiatric symptoms after acute respiratory distress syndrome: a 5-year longitudinal study. Intensive Care Med. 2018;44(1):38-47. doi: 10.1007/s00134-017-5009-4. Epub 2017 Dec 26. PMID: 29279973; PMCID: PMC6020022.
P222
Improving workforce wellbeing and morale; The Intensive Care Positivity Project
Wellbeing
Emily Reynolds 1 , Laura Noble1, George Perrett2, Olivia Ward1, Michelle Dowd3 and Michael Parr1
1Liverpool Hospital
2Westmead Hospital
3Liverpool Hopsital
Abstract
Introduction: Maintaining workforce morale and wellbeing is essential to deliver excellent patient care. In busy and stressful environments many gestures of goodwill may not be considered due to time constraints, conflicting prioritiess and high workload. Recognising the efforts that colleagues make to improve the quality of life of those around them can help to create a positive workplace culture and improve morale.1
Objectives: The Intensive Care Positivity Project was set up to recognise and celebrate the efforts staff make that positively impact their colleagues. The aim was to provide an avenue for feedback so individuals could be thanked for their efforts, and to give the department the opportunity to formally acknowledge those people quietly making a difference to their colleague. This was done by providing nominated individuals with a signed departmental letter containing the positive feedback comments.
Method: We surveyed staff over a three week period asking questions about feedback, its frequency, and how positive feedback affected their workplace performance. We then launched an email address which allowed staff to easily submit messages of thanks. These emails were collated monthly and formal letters from the department were distributed to those nominated. Eighteen months after the introduction of the project the emails were reviewed and analysed using thematic analysis for recurring topics.
Results: The initial survey consisted of 10 questions with answers based upon a 5 point Likert scale. 31 members of staff completed the survey. 100% stated that in the last 3 months they had less than monthly or never received written feedback about their performance. 16% stated that they received verbal feedback on their performance daily or weekly, 16% had received verbal feedback monthly and 68% received it less than monthly or never. No responders strongly agreed that when they had “gone above and beyond” they were recognised for this. 26% agreed that they were recognised, 32% were neutral about the statement and 42% disagreed or strongly disagreed. 61% disagreed or strongly disagreed that there was a clear way to recognise team members who go ‘above and beyond’. 100% of responders agreed or strongly agreed with the three following statements; 1) Positive feedback improves my performance at work 2) Positive feedback improves my job satisfaction, 3) Positive feedback about my performance helps me to feel more invested in the department.
After 18 months 53 emails had been sent, 17 from nursing staff (including nurse educators), 34 from doctors and 2 from allied healthcare professionals. Table 1 summarises the themes. 47% of the emails were relating to assistance with a difficult case or shift, 32% commented on general collegiality. Verbally staff reported that receiving the letters helped to boost morale and made them feel appreciated.
Table 1.
Themes from letters of thanks.
| Teaching | 4 |
| Assistance with difficult clinical case/help with shift | 25 |
| Acts of kindness | 5 |
| General collegibility | 17 |
| Pastoral care | 1 |
| Equipment issues | 1 |
| Total | 53 |
Conclusion: Introducing a formal letter system to recognise and celebrate the efforts of ICU staff has been well received and had a positive impact on individual morale. This positive and cheap intervention may be easily introduced to other units, and our Emergency Department has initiated a similar scheme following our success.
References
1. Barnes S, McDonald M, Kelly F. Positivity in anaesthesia: improving feedback, morale and resilience in our anaesthetic department. Anaesthesia. 2018; 73(Suppl3):89.
P223
Resilience, Quality of life, and Wellbeing in intensive care survivors of Covid-19 critical illness
Wellbeing
Ellen Pauley* (*Joint 1st author) 1 , Thomas Alman* (*Joint 1st author)1, Joanne Thompson2, Lucy Barclay2 and Judith Merriweather2, Timothy Walsh3
1University of Edinburgh
2Edinburgh Critical Care Research Group, Royal Infirmary of Edinburgh
3Usher Institute of Population Health Sciences, Department of Anaesthesia, Critical Care & Pain Medicine, Royal Infirmary of Edinburgh
Abstract
Introduction: The negative impact of Post-Intensive Care Syndrome on the quality of life of critical illness survivors has previously been well characterised.1 Survivors of Covid-19 critical illness are a relatively new cohort in terms of younger age and less prior comorbidity.2 The health-related quality of life, psychological problems, resilience, or wellbeing of survivors of Covid-19 critical illness have not been fully explored.
Objectives: To characterise the resilience, wellbeing, self-efficacy, and quality of life of ICU-survivors, who were admitted with Covid-19, 6-9 months post-hospital discharge. To explore any potential associations with baseline characteristics.
Methods: This was a prospective follow-up study of ICU-survivor patients who were admitted with Covid-19 and discharged alive from the Royal Infirmary Edinburgh or St John’s Hospital, Scotland. Eligible patients were identified by 2 specialist research nurses from the medical records and were contacted via telephone for consent. Paper copies of the questionnaire pack were posted to patients who consented. Demographic characteristics were captured from WardWatcher IT system (age, sex, length of ICU stay). 2 investigators telephoned participants to complete the questionnaires. Outcomes measured were: resilience, using the 10-item Connor-Davidson Resilience Scale (CDRISC), self-efficacy, using the General Self-Efficacy (GSE) Scale, overall health state, using The EuroQol EQ5D-5L Health Questionnaire, and Wellbeing, using 6 10-point visual analogue scales. Statistical analysis was conducted using R-Studio. Associations were tested with Fisher’s exact test for categorical variables, and Kruskal-Wallis for continuous variables. Statistical significance was accepted at p<=0.05.
Results: Of the 52 eligible patients consented to be contacted, 40 (76.9%) completed the questionnaires. 59.6% (31/52) were male; median age was 59.0 (IQR:53.0-66.2), and participants spent median 6.3 (IQR: 4.1-11.0|) days in ICU. Questionnaires were completed median 202 days (IQR:187.5-224.0) from hospital discharge. The median total CDRISC score was 34.5 (IQR: 30.8-38.0), which has previously been defined as normal resilience (27-37/40)3. 12.5% (5/40) and 32.5% (13/40) reported low (<27/40) and high (>=38/40) resilience respectively.3 The median total GSE score was 34.0 (IQR: 30.0-38.0) (international mean: 29.554). For overall health state (EQ5D-5L), the median overall health score was 80.0% (IQR:75.0-81.2), with the results in each domain as follows: Mobility: 27% (11/40) reported moderate or worse problems (with the remainder reporting no problems); Self-care: 10% (4/40) reported moderate or worse problems; Usual activities: 17% (7/40) reported moderate or worse problems; Pain: 17.5% (7/40) reported moderate or worse problems; Anxiety or depression: 17.5% (7/40) reported moderate or worse problems. For the wellbeing measures, participants rated ‘Overall satisfaction with life as a whole’ median 8/10 (IQR: 7-9), and ‘I have a sense of direction and purpose in life’ median 8/10 (IQR:7-9.5). Resilience, self-efficacy, health-related quality of life, and wellbeing were not significantly associated with age, length of ICU- stay, or time between discharge and questionnaire completion.
Conclusion: Overall, ICU-survivors of Covid-19 critical illness reported normal resilience, and high levels of self-efficacy and wellbeing at 6-9 months post-hospital discharge. Many ICU-survivors experienced problems affecting their overall health state, such as with mobility and pain. Future studies are indicated to investigate how to best support ICU-survivors in their recovery.
References
1. Griffith D, Salisbury L, Lee R, Lone N, Merriweather JWT. Determinants of Health-Related Quality of Life After ICU. Crit Care Med 2018; 46: 594–601.
2. ICNARC: Intensive Care National Audit & Research Centre. ICNARC report on COVID-19 in critcal care: England, Wales and Northern Ireland. 2021.
3. Maley JH, Brewster I, Mayoral I, et al. Resilience in Survivors of Critical Illness in the Context of the Survivors’ Experience and Recovery. Ann Am Thorac Soc 2016; 13: 1351–1360.
4. Scholz U, Dona B, Sud S, et al. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Eur J Psychol Assess 2002; 18: 242–251.
P224
Intensive care medical staff wellbeing during the COVID-19 pandemic
Wellbeing
Aisling Hanna 1 , Jamie Tabor1, Nagaraja Ravishanka2 and Laura Coleman2
1Pennine Acute Trust- Royal Oldham Hospital
2Northern Care Alliance, Oldham Care Organisation
Abstract
Introduction: Awareness of medical staff burnout has grown significantly over recent years and has been thrown into the limelight during the COVID-19 pandemic. Extraordinary burden has been placed on the junior members of the workforce during this time. One survey showed over half of junior doctors said they considered changing career.1 Another survey demonstrated that 44% were suffering from burnout or other mental health conditions.2
Objectives: The aim of our survey was to assess trainee welfare and highlight areas for improvement within our intensive care unit.
Methods: Members of the medical workforce within our intensive care unit were asked to complete an online survey in December 2020 and April 2021. Burnout was quantified using an external online survey available via the BMA website.3 Our survey questions covered topics such as expectation and reality of workload, as well as working environment.
Results: The survey was distributed to all non-consultant members of the medical team. These included registrars, core trainees, foundation doctors, clinical fellows and advanced critical care practitioners. 18 responded to the initial survey and 15 to the second. 56% reported high or very high levels of burnout in December compared to 47% in April. No-one reported low burnout at either time point. The majority found the workload to be as expected or higher. Morning intensive care teaching was highlighted as a positive aspect of the working environment in our ICU, while the lack of break spaces was a negative factor.
Conclusions: The findings from our survey correlated with wider national surveys. Although burnout levels improved slightly between December 2020 and April 2021, there is still a long way to go to get this to an acceptable level. Factors that play into this include the workload expectation. More senior members of the team found the workload to be higher than initially expected. One of the factors causing this disparity was that they were expected to supervise others, often those who had been re-deployed from non-ICU specialties with limited experience of critical care. Since these surveys, the out of hours staffing has been increased with the aim to improve the workload burden.
Strict social distancing rules resulted in break space capacity being severely reduced. Room capacity restrictions created a divide between nursing and medical staff as they had no area to share break periods. A coffee afternoon (Brew and a Vent) was organised to bring the team back together, modelled on the Coffee and a Gas scheme from the Association of Anaesthetists.4
The team felt galvanised by regular morning teaching which has resulted in the employment of a teaching fellow to coordinate this going forward. There is clearly large scope for improvement with regards to staff wellbeing, but small steps have been made in the right direction. Our surveys have shown that small interventions can go a long way to improving staff morale, especially when the suggestions for change have come from the juniors themselves.
References
1. Bloomer A. More than half of doctors considering new career due to burnout. Geriatric Medicine Journal, https://www.gmjournal.co.uk/more-than-half-of-doctors-considering-new-career-due-to-burnout (2020, accessed 8thAugust 2021).
2. BMA. Stress and burnout warning over COVID-19 https://www.bma.org.uk/news-and-opinion/stress-and-burnout-warning-over-covid-19 (2020, accessed 8th August 2021).
3. BMA. Wellbeing support services burnout questionnaire, https://questionnaires.bma.org.uk/burnout-questionnaire/?OpenForm (2020, accessed 8th August 2021).
4. Coffee and a Gas, Association of anaesthetists, https://anaesthetists.org/Portals/0/PDFs/Wellbeing/CoffeeGas.pdf?ver=2020-11-09-100833-577 (2021, accessed 8th August 2021)
Swallowing and communication assessment in tracheostomy patients: multi-disciplinary-led quality improvement in a busy tertiary teaching hospital
Tracheostomy
Oral Presentation
Nick Spencer, Sioned Lloyd-Davies, Emma Forbes, Alice Corbett, Jenny Hudson and Alistair Gibson
NHS Lothian
Abstract
Introduction: Intensive care patients often have complex swallowing and communication needs. These require co-ordinated input from the multi-disciplinary team. Increasing evidence highlights the role of speech and language therapy (SLT) within the critical care environment1 and this is represented well in national recommendations specific to patients with tracheostomies. Approximately 10-15% of ICU patients will have a tracheostomy nationally.2 SLT provide expertise in assessment and management of communication and swallowing difficulties, which can vastly improve psychosocial well-being and promote early safe enteral feeding for our patients.3 In 2014 “On the right trache?”4 found that 52% of patients with a tracheostomy suffered with dysphagia, however only 27% critical care patients had input from SLT.
Objectives: To improve the assessment of swallowing and communication in patients undergoing tracheostomy ventilation at the Royal Infirmary of Edinburgh, to comply with Scottish Intensive Care Society Audit Group (SICSAG) quality indicator 2.3. This guidance stipulates all tracheostomy patients should have communication and swallowing needs assessed during ventilator wean.5
Methods: Four distinct areas of intervention were implemented. Pre-populated review text was added to NHS Lothian’s clinical notation system (InterSystems TrakCare®), prompting nursing staff to consider swallowing, tracheostomy issues and SLT referral. These were refined between audit cycles. SLT were invited to join safety briefs to identify tracheostomy patients, as well as other patients with complex swallowing needs. This was an opportunity to raise awareness, educate, and prioritise workload. New guidelines for nurse-led swallowing observations were developed and disseminated amongst teams. Finally, staff were offered relevant educational sessions. Baseline data was collected in 2019; serial data collection was then during October – November 2020 and in June – July 2021 following the interventions.
Results: All patients who received tracheostomy ventilation were audited (n=31). This showed that very few patients had swallowing and communication assessed adequately. Only 16.1% (n=5) patients had a regular nursing swallowing assessment on the majority of critical care days (>50%). Referral to SLT was often very late when patients were approaching de-cannulation and on many occasions by the time the SLT team were involved patients had already been de-cannulated.
Figure 1.
Chart showing proportion of trachestomy patients having swalloing assesment on majority of daily nursing assessments (5 of 31, 2019; 6 of 8, Oct 20; 10 of 11, July 21)
Figure 2.
Chart showing proportion of trachestomy patients having speech and language theraphy review whilst on critical care (10 of 31, 2019; 6 of 8, Oct 20; 9 of 11, July 21).
Following the intervention period, it became apparent that awareness of swallowing requirements had improved. By mid 2021, 58.9% more patients had swallowing assessed as part of daily care. Additionally, 81.2% of patients had SLT reviews on the unit demonstrating a sustained increase from late 2020. There was a notable increase in the quality of assessments after initial SLT review.
Conclusion: Using quality improvement methodology our multidisciplinary team was able to substantially increase the quality of swallowing assessment within our ICU, despite the challenges of the COVID-19 pandemic. Our unit now complies with SICSAG quality indicator 2.3. This is in keeping with national recommendations for a multi-disciplinary approach to care of tracheostomy patients. Patients with increased risk of dysphagia are being identified earlier and are more likely to progress and be established on enteral feeding early, which may subsequently reduce the burden of nasogastric feeding, total parenteral nutrition and even related invasive IV access.
References
1. McRae J, Montgomery E, Garstang Z, et al. The role of speech and language therapists in the intensive care unit. Journal of the Intensive Care Society. 2020; 21(4): 344–348.
2. Abe T, Madotto F, Pham T, et al. Epidemiology and patterns of tracheostomy practice in patients with acute respiratory distress syndrome in ICUs across 50 countries. Critical Care. 2018;22(1): 195.
3. Royal College of Speech and Language Therapists. RCSLT Position statement: critical care and speech and language therapy. Available from: https://www.rcslt.org/wp-content/uploads/media/docs/clinical-guidance/rcslt-position-statement-critical-care.pdf?la=en&hash=42823C17957D 4848818438CBCD5DC3998EF0CDF7. [Accessed March 2021]
4. Wilkinson KA, Martin IC, Freeth H, et al. On the right trach? A review of the care received by patients who underwent a tracheostomy. National Confidential Enquiry into Patient Outcome and Death. 2014.
5. Scottish Intensive Care Society Audit Group. Minimum Standards and Quality Indicators for critical care in Scotland Version 3.0. NHS National Services Scotland, Edinburgh [online]. Available at: http://www.sicsag.scot.nhs.uk/quality/20151215-Quality-Indicators-Booklet-V3-0.pdf [Last accessed: 18/08/2021].
North East London Critical Care Transfer And Retrieval: identification of thresholds for upscaling adult critical care retrieval team resources
Transfer and retrieval
Oral Presentation
Jonathon Dean 1 , Heather Humphreys2, Lydia Fletcher1, James Waiting1, Simon Finney1 and Mamoun Abu-Habsa1
1North East London Critical Care Transfer And Retrieval
2The Health Economics Unit
Abstract
Introduction: The North East London Critical Care Transfer And Retrieval (NECCTAR) service was developed in response to the COVID-19 pandemic to provide an additional resilience layer for intensive care provision. Emergent capability development of the service spanned equipping, training, and operating procedure design with an overarching robust governance and data infrastructure.
An overwhelming need to help sustain critical care provision was such that scalability became a fundamental component of service design.1 Pressures varied, and so the trigger for deployment of a second team was data-driven based on sector critical care occupancy.2 This paper explores population-based thresholds for anticipating a surge in demand on critical care transfer services.
Objectives: Identification of population-based indicators for generalizable thresholds for upscaling retrieval resources.
Methods: The service was deployed as a sector-wide asset within a regional hub including clinical and administration staff. Daily sector-wide situational assessments were undertaken implementing a joint decision model. Occupancy, staffing, and specified risk data variables were prospectively collected along with tasking data. Transfer activity was then analysed alongside sector occupancy data to provide insight into current service provision and to rapidly and flexibly scale resources.
Results: NECCTAR has been tasked 376 times and has completed 333 transfers (88.5%) in the 250 days between December 2020 and August 2021. On average, the transfer team completed 1.5 taskings per day with peaks and troughs. Tasking reasons included clinical retrieval (123, 32.7%), decompression (193, 51.3%), repatriation (59, 15.7%), and compassionate (1, 0.3%). 339 taskings (90.1%) originated within the North East London region, 27 (7.2%) from other London regions, and 7 (1.8%) from the rest of the nation. 208 patients (55.4%) had tested positive for COVID-19 during their admission, and 168 (44.6%) were COVID-19 negative.
Demand for ICU related transfers varied with the waves of the pandemic and NECCTAR scaled to the needs of the sector. A second NECCTAR team was deployed available for a 47-day period from January 12th to Feb 28th 2021. During this period, NECCTAR was tasked 138 times, for an average of 2.9 transfers per day and 110 of these taskings (79.8%) were COVID-19 patients.
Our modelling, data collection, and real-world observation, provided a threshold of 12 sector critical care patients per 100,000 population to trigger the deployment of a second NECCTAR team. The second team was maintained for an additional week after the rate fell below the threshold so that NECCTAR could assist with repatriations and closing of surge beds.
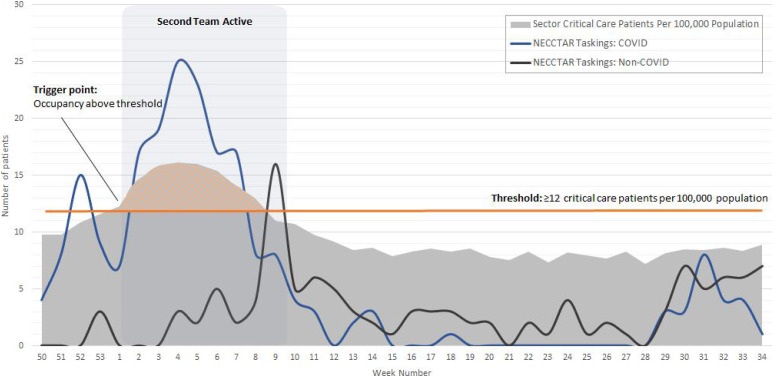
Conclusion: During surge periods, NECCTAR was able to scale its service and match its capabilities to regional requirements and maintain the capability needed to undertake twice as many transfers per day. In periods of high COVID surge activity, greater volumes of COVID-19 decompression moves were undertaken and a second team was deployed to match the sector’s needs.
Extensive data collection and analysis has provided evidence for using a threshold of 12 critical care patients per 100,000 regional population for upscaling service provision, ensuring the allocation of resources is data-driven.
References
1. Barts Health NHS Trust. A winter like no other… How Barts Health responded to the second wave of COVID-19. 2021. Available at: https://www.bartshealth.nhs.uk/download.cfm?doc=docm93jijm4n16833.pdf&ver=30223 (accessed August 2021)
2. NHS Providers. COVID-19 pressures: an exploration of hospital activity through the first and second wave. Available at: https://nhsproviders.org/news-blogs/blogs/covid-19-pressures-an-exploration-of-hospital-activity-through-the-first-and-second-wave (accessed August 2021)
Gone so soon? Causes of cessation of critical care in older major trauma patients
Trauma
Oral Presentation
Michael Tonkins, Paul Bramley, Jonathan Loveday and Chris Yeoman
Sheffield Teaching Hospitals NHS Foundation Trust
Abstract
Introduction: In the UK the mean age of major trauma patients rose from 36.1 years in 1990 to 63.6 years by 2017.1 Older trauma patients are known to have shorter admissions to critical care, however the reasons for this are not understood.2 The exact circumstances in which critical care of trauma patients ceased are not collected nationally, necessitating investigation using patient-level data.
Objectives: To describe the causes of cessation of critical care of older trauma patients at our institution.
Methods: Adult patients aged over 60 with an injury severity score >15, who were admitted to critical care due to trauma between 2017-2019 were eligible for inclusion. Prospectively collected Trauma Audit and Research Network (TARN) data were linked with clinical notes and hospital episode statistics data. National summary statistics for England and Wales were provided by TARN for comparison purposes. The primary outcome measure was cause of cessation of critical care.
Results: 178 patients from our institution (the ‘local chort’) and 6,011 patients from England and Wales were included. Both cohorts were broadly comparable (see Table 1). The trend of decremental length of critical care stay with increasing patient age was present in both local and national data. Older patients were more likely to die on critical care because they reached their ceiling of care. Typical determinants of 30-day mortality including Injury Severity Score, Glasgow Coma Scale, shock and injury distribution not associated with patient age.
Table 1.
Comparison of local patients with the national cohort for England and Wales 2017-2019.
| Local Cohort N = 178 | England & Wales N = 6,011 | |
|---|---|---|
| Age, median (IQR) | 70.9 (66.1 - 77.5) | 73.5 (66.9 - 80.6) |
| Female, n (%) | 60 (33.7%) | 2138 (35.6%) |
| Mechanism, n (%) | ||
| Blow without weapon | 11 (6.2%) | 107 (1.8%) |
| Burn | 1 (0.6%) | 7 (0.1%) |
| Crush | 2 (1.1%) | 34 (0.6%) |
| Fall <2m | 64 (36.0%) | 2828 (47.0%) |
| Fall >2m | 42 (23.6%) | 1191 (19.8%) |
| Stabbing | 1 (0.6%) | 35 (0.6%) |
| Vehicle Collision | 51 (28.7%) | 1698 (28.2%) |
| Other | 6 (3.4%) | 111 (1.8%) |
| Injury Severity Score, median (IQR) | 25 (20 - 32) | 25.0 (20 - 29) |
| Glasgow Coma Scale, median (IQR) | 14 (11 - 15) | 14 (9-15) |
| Shock (systolic blood pressure <110mmHg), n (%) | 43 (24.2%) | 1,738 (28.9%) |
| Ps, median (range) | 87.4 (1.53 - 98.8) | 84.2 (0.559-98.9) |
| Critical Care LOS, median (IQR) | 4 (1 - 8) | 4 (1 - 9) |
| 30 Day Mortality, n (%) | 56 (31.5%) | 1,874 (31.2%) |
| Ceiling of care, n (%) | ||
| No limits | 49 (27.1%) | - |
| Not for level 3 care** | 50 (27.6%) | |
| Not documented | 79 (43.6%) | |
| Cause of critical care cessation, n (%) | ||
| Ward fit | 122 (68.5%) | - |
| Withdrawal of Life-sustaining treatment | 42 (23.6%) | |
| Ceiling reached | 12 (6.7%) | |
| Discharged home | 2 (1.1%) | |
Conclusion: The trend of decremental critical care length of stay with increasing age is indicative of the excess mortality risk conferred upon trauma patients by advancing age.3 This highlights the importance of comprehensive multidisciplinary assessment of older trauma patients.4 The finding that older patients were more likely to reach their ceiling of care highlights the importance of care at the end of life, and the timely instigation of appropriate treatment limits.5 The absence of association between known prognostic factors in trauma and patient age may indicate that these traditional markers of trauma severity are less applicable to older patients with low-energy mechanisms. Instead, competing prognostic factors associated with age such as comorbidities and frailty may become more salient.3
References
1. Dixon JR, Lecky F, Bouamra O, Dixon P, Wilson F, Edwards A, et al. Age and the distribution of major injury across a national trauma system. Age Ageing. 2020;49(2):218–226.
2. Trauma Audit and Research Network. Major Trauma in Older People [Internet]. 2017. [cited 2020 Aug 26]. Available from: https://www.tarn.ac.uk/Content.aspx?c=3793
3. Sammy I, Lecky F, Sutton A, Leaviss J, O’Cathain A, O’Cathain A. Factors affecting mortality in older trauma patients - A systematic review and meta-analysis. Injury. 2016;47(6):1170–1183.
4. Eagles D, Godwin B, Cheng W, Moors J, Figueira S, Khoury L, et al. A systematic review and meta-analysis evaluating geriatric consultation on older trauma patients. J Trauma Acute Care Surg. 2020;88(3):446–453.
5. Faculty of Intensive Care Medicine and Intensive Care Society. Guidelines for the Provision of Intensive Care Services [Internet]. Guidelines for the Provision of Intensive Care Services. 2019. [cited 2021 Aug 3]. Available from: https://www.ficm.ac.uk/sites/default/files/gpics-v2.pdf
With all due respect, your NHS Superheroes will fail!
The Cauldron
Matt Rowe
North Bristol NHS Trust
Abstract
Introduction: For all the triumphs and advances you will face over the next 50 years in critical care the over-arching and all-consuming theme of your work will be that of failure. Failure to save a loved one, failure to make the right diagnosis or predict a patient’s clinical course. Failure to make the right decisions for your patients and perhaps worst of all, failure to give your patients your best.
Main Body: Critical care resources will always be finite. Regardless of funding, the clinical need, our ability to adapt and the resilience of our work force, at some point supply will inevitably fall short of demand. You will fail your patients. Be it a global pandemic, an unforeseen humanitarian crisis, an act of terror, workforce fatigue or a local bed shortage we cannot plan for everything and it’s time we were honest with our patients. We need to admit we can’t and perhaps shouldn’t save them all. In stark contrast to our marvel and DC counterparts, this comic book (and later movie franchise) has no happy ending.
At many points in your career, you will have to make difficult choices. Some of those choices will lead to a poor outcome. This may be true for a group of patients or on an individual basis. By doing your best in one circumstance you will fail to do your best in another. It is this burden of experimentation through choice that defines critical care as a specialty. Whether prospective or retrospective, failure is an extremely valuable, unbiased outcome measure and we need to completely redefine how we view failure in healthcare.
Failure is the infinite, inevitable and irrefutable consequence of a complex and evolving healthcare system. It is also our single most critical measure of success. Without failure we have achieved perfection. Since perfection is presumably unobtainable in healthcare, we must continue to strive towards a sustained period of failures. Evidence based medicine is founded on the presence of failure. Failure is the negative dataset, the expert clinical experience, the constant reminder of what we we’re trying to achieve. It is the anti-matter to the positive patient outcome without which the other cannot exist. It is the un-sung hero of our NHS.
Conclusion: My advice for the next 50 years, is not to worry about what’s coming. Embrace failure as the only constant in an uncertain future. Having a strategy for managing failure will not prevent bad outcomes but will allow a more rapid learning/recovery process. Some of you will thrive, some of you will burn out but all of you will have made a positive difference to patients. Over the next 50 years you will continue to fail over and over again and I hope that we continue to fail for many more years to come.
References
1. Edmondson 2011: Strategies for Learning from Failure– Harvard Business Review 2011
2. TabriziN M, Masri FTowards safer healthcare: qualitative insights from a process view of organisational learning from failure BMJ Open 2021;11:e048036. doi: 10.1136/bmjopen-2020-048036
The more things change, the more they stay the same
The Cauldron
Mary Leese
Freeman Hospital
Abstract
Introduction: On the face of it, the Intensive Care Unit of the future is a wholly foreign and, indeed, almost unrecognisable place. 2021 is a long time away, and while they don’t yet have flying cars, haven’t wiped out cancer, and aren’t using genetics to practice patient-personalised medicine, there have been enormous changes in the medical technology, patients and among healthcare workers. How could there not have been? After all, fifty years is a lifetime in the short history of our specialty.
Main Body: The equipment and technology are different: the machines are more complicated and correspondingly more expensive, there are an array of new drugs that are not yet available to us and computers are increasingly taking over every aspect of communication. Intensivists have always loved new medical toys and fifty years from now, it certainly looks like they always will!
The patients are older, fatter and much more co-morbid (it turns out that the medicines of the future work, a pleasing development). They have different problems: there is less trauma and to the doctors of the future, poliomyelitis and tetanus are mere historical footnotes. More of them survive, but there are also just more of them. In fact, to our eyes, Intensive Care Units have become unrecognisably large. There have been other changes inside departments, too - paediatric and adult care have become almost totally decoupled, and children are now nearly always cared for by completely separate teams.
The terrifying, all-knowing professor of today is a thing of the past - well, mostly! In 2021, medical care is less hierarchical and there is a truly multi-disciplinary team approach. This encompasses not just doctors, nurses and physiotherapists, but also dietitians, pharmacists and speech and language therapists. Our nursing colleagues have many more opportunities to showcase their skills and this can be seen both within individual units - where Advanced Critical Care Practitioners are an invaluable component of many departments - but also throughout the whole hospital. Critical Care Outreach Teams have intervened to save the bacon of many a harried house officer, improve the care of multitudes of patients and expand the principles (or should that be tentacles?) of Intensive Care throughout the hospital.
Conclusion: However, some things will always stay the same. At the heart of everything we do, there is a patient. And that patient is with us at one of the most vulnerable times of their life and, indeed, one of the most vulnerable times of their family’s lives. Our compassion, communication and care remain the most important aspect of the medicine that we deliver. The healthcare professionals of our future might have more gadgets, more team members and more complex patients, but this fundamental fact remains as true now, in 1971, as it will be in 2021 and then in 2071. Perhaps in yet another fifty years, we will have those flying cars. But, as it is now, the core of Intensive Care Medicine will be human interactions that are carried out with empathy, consideration and kindness.
Our House Isn’t on Fire- it’s Already Burnt Down
The Cauldron
Freya Glover
St Mary’s Hospital - Imperial College Healthcare NHS Trust
Abstract
Introduction: I’ve travelled to the future and 2021 is terrifying! In a year of pandemic, climate emergency and social unrest, the fact that the ocean is on fire feels like a fitting analogy for the burnout being seen in the intensive care units (ICUs) of the future. A shocking one third of ICU team members are at high risk of burnout syndrome,¹ and I can see why. In the future, it is an expectation, not a hope, that intensive care will be able to cure any disease in any person, no matter how frail. These expectations are not only from patients and the wider public, but also from our colleagues within the hospital. This cannot go on, and we need to act now to save our future selves from a life lacking the joy of practising intensive care medicine. We need to put out the fire, before it has a chance to burn the house down.
Main body: Firstly, we need to clearly communicate with the public what ICU is, and what it can do. We cannot blame the public for seeing intensive care as a saviour of those who seemed without hope, as it is precisely those stories that make intensive care such an inspiring place to work. In order to manage patients’ and relatives’ expectations, we need to be able to communicate what it is we can do, and why sometimes, just because we can do something, does not mean that we should. We need to show the general public that valuing a good death is as important as valuing a good life.
Secondly, we need to share with our colleagues what it is that ICU can do, but more importantly, what it cannot do. We make complex operations possible, provide a last resort when things go wrong, and are often asked to settle the toughest clinical questions. We can only do these things if we protect our time and energy for when they are really required. Intensive care must avoid becoming a vessel in which other peoples’ worries are held. Incorporating an ICU post into all training pathways is an excellent way of teaching clinicians both the strengths and limitations of ICU, so encouraging more appropriate requests for ICU involvement.
Finally, we need to embrace wellbeing proactively, rather than as a response to team fatigue. Training must be prevented from feeling like a treadmill; must promote mentorship; should prioritise continuity in order to maintain the tight-knit relationships formed in the stressful environment of ICU. This builds morale and resilience more than any of the wellbeing sessions, free doughnuts or staff yoga I witnessed in the future.
Conclusion: Over the next 50 years, we will make huge strides in advancing intensive care. The challenge will be in doing this sustainably. So instead of readying our fire extinguishers, let’s build intensive care to be completely flame-resistant.
References
1. Vincent, L., Brindley, P., Highfield, J., Innes, R., Greig, P. and Suntharalingham, G. Burnout Syndrome in UK Intensive Care Unit staff: Data from all three Burnout Syndrome domains and across professional groups, genders and ages. Journal of the Intensive Care Society 2019; 20: 363-369
Building the state of the art from the thoughts of our people -Implementing developed world experience in developing world
MDT Diaries
Ashani Ratnayake
Ministry of Health
Abstract
Introduction: At the beginning of the pandemic, I was working in University Hospital of Leicester (UHL), a leading hospital in UK as a speciality doctor as a part of post graduate training in anaesthesia of Sri Lanka. 5 months into the pandemic, I find my self returning to Sri Lanka after the training and only to be appointed as a consultant anaesthetist in a designated COVID treatment hospital. This is my story of converting a normal ICU space to a COVID -ICU.
Main body: The pandemic came late to Sri Lanka. Even after 5 months of pandemic, the Intensive care unit in a designated COVID hospital was not ready to accept any patients.
Leaving UK, at the peak of pandemic after a steep learning curve, I realised that we Sri Lankans are just living on borrowed time. Being a developed country, UK also experienced inadequacies with manpower and equipment. Looking at a low income country like Sri Lanka, the challenges of converting the space in to COVID ICU seemed to be impossible. Starting from the scratch, with the constant encouragement of the colleges and authorities, a COVID ICU was built at a Base Hospital – Teldeniya, which was situated 15 miles away from a city.
UHL was able to increase its ICU capacity within days. Most hospitals in UK did this within days to weeks. The story was not the same for Sri Lanka. People took time to realise the need for the COVID ICU. This made me desperate and sad thinking about the support the ICU authorities had at UHL. Our ICU started with one bed, adding to the total of 14 designated ICU beds in Sri Lanka. This number was bearable, as the number of reported cases were low all over the country.
With the beginning of the year 2021, the number of reported COVID-19 cases gradually increased, with more patients needing ICU admissions. The bed number at BH Teldeniya was also increased to 5, but with minimal resources.
When the pandemic reached its peak in early 2021, the miracle happened. There was an island wide appeal to donate equipment for COVID ICUs in Sri Lanka. This made people to change their attitude about the disease and about the COVID – ICUs. Generous donors from all over Sri Lanka and from overseas got together for this good cause. With no time, my ICU was well equipped with all kinds of sophisticated equipment. My greatest winning was to obtain a liquid oxygen plant to the hospital, allowing me to use high flow nasal oxygen therapy in deserving patients.
Today, BH Teldeniya serves it maximum to the critically ill COVID-19 patients. Now I can sleep well in the night thinking that, my patients will get the same treatment as a patient in UHL. The unit is well equipped, and I can even lend equipment to ward HDUs. All this was possible due to simple thoughts of Sri Lankans.
Conclusion: In 20 years’ time, I will look back at the time of pandemic and be proud of my journey from a developed country to a developing country to make the difference that would change the fate of critically ill Sri Lankans.
“I never leave the house and keep both phones in my pockets all day so that whichever phone you ring, I never miss your call”
MDT Diaries
Clare Smedley
Abstract
Introduction: I will never forget the tightness in my throat and the pressure rising in my chest when I heard those words spoken by the husband of an ICU survivor. How ashamed I felt that despite all we do to alleviate the suffering of our patients, sometimes we create new suffering for those left at home.
Main Body: Restricted visiting during the pandemic has created unprecedented challenges for patients, staff, and families. Not able to rely on family visits to communicate news and to help families appreciate any change in the condition of their loved ones, we have had to develop new ways of working. The consultants enthusiastically rallying juniors into daily telephone updates, emailed messages read to patients by nursing staff, pictures on the walls of a hospital room, and wrestling with technology to bring families together in one room via video call.
Despite all the energy and innovation, I am sure I’m not the only person who has found themselves thinking that perhaps the call to update the wife/father/daughter of our patient can wait. They had an update yesterday; maybe someone else can speak to them later. This phone call, one of several to ICU survivors and their families, was the first time I had fully understood the reality for the loved ones of so many of our patients. They are barred from the hospital due to covid restrictions, struggling to build a picture of their loved one from the snatches of information given down a phone, desperate for news.
Since this conversation, I am incredibly mindful of the responsibility to care for families as well as our patients. Even if they aren’t with their loved ones in person, we have an opportunity to include them in the journey. Maybe we remember to share the big things, but sometimes the small things are the ones that matter most: a shave, the music on the radio, ice cream with their lunch. Each member of the ICU team has a different story to share, and it’s these human connections this patient’s husband was waiting for by the phone.
Conclusion: As we slowly arrive at "the new normal” we might be relieved to see the end of some of our pandemic practices. However, I will never forget the lesson this man taught me. I will use my privileged position to make painful times perhaps a little more bearable for the families and friends of those we treat.
COVID-19 Physiotherapy Slack Workspace: An unprecedented international collaboration
MDT Diaries
Zoe van Willigen1 and Eleanor Douglas2
1University Hospital Southampton
2University of Nottingham and Nottingham University Hospitals NHS Trust
Abstract
Introduction: The moment that changed my practice was when Public Health England identified many respiratory physiotherapy techniques as being aerosol generating procedures, and therefore high risk for COVID-19 virus transmission. This led to confusion, controversy and high levels of anxiety within the respiratory physiotherapy profession. The volume of requests for advice, support and research evidence- via multiple professional networking forums and social media- felt overwhelming.
To address this, I created a dedicated ‘COVID-19 Physiotherapy Slack Workspace’. This online forum enables members with a mutual interest to share evidence, local and national policies and procedures and to discuss anything related to physiotherapy and COVID-19. The existence of the workspace and how to join was widely advertised via social media. This led to an unprecedented worldwide membership as the word spread about its value.
Main Body: Since its inception in March 2020, the workspace has grown rapidly, resulting in an impressive international collaboration of respiratory physiotherapists. Currently, there are 1083 members from 15 countries including Italy, Saudi Arabia, Canada and New Zealand. The diversity of the membership created an online learning resource and ‘live’ support forum during each phase of the pandemic as it evolved around the world.
Members developed the workspace further by creating 17 different subject channels relating to various aspects of COVID-19 and physiotherapy practice. The subject channels include critical care, rehabilitation post COVID, paediatrics and staff wellbeing. Files and messages are shared in these channels and a keyword search function makes it easy to find content. All members can upload resources, and one member in particular (ED) has been instrumental to the success of the workspace by consistently uploading contemporary and relevant research and guidance. To date, 305 files have been shared across the subject channels, resulting in a comprehensive ‘library’ of resources relevant to physiotherapy and COVID-19 from the acute phase to Long-COVID rehabilitation.
For me, a really positive consequence of the pandemic is the worldwide connection members have made through sharing our experiences and resources. The peer support aspect of the workspace has been incredibly constructive, with 5823 messages sent to date. Physiotherapists in remote locations or smaller hospitals fed back that the workspace has supported them to make evidenced based clinical decisions where they previously felt isolated or lacked local expertise or support.
Hierarchy has been completely flattened in our workspace, meaning anybody can ask anything. No one was an expert as this novel disease progressed, and we only had each other to learn from. Members have generously shared their work, and the workspace has been the ideal platform to share the best evidenced based guidance we had in this unique situation.
Conclusion: I believe that in future, colleagues will be more open with sharing practice and resources, as we all felt the benefit from networking with colleagues. Building resilience in our workforce in the recovery from the pandemic cannot be underestimated, and this online collaboration has addressed aspects of wellbeing and anxiety management for clinicians as well as improving the evidenced based physiotherapy management of people with COVID-19.
I will never forget the day
MDT Diaries
Emma Fisher
North Devon District Hospital
Abstract
Introduction: I would like to present a poem I have written about my experience of being part of the multidisciplinary team at a remote district general hospital on the day that a COVID-19 patient was retrieved for ECMO.
Main Body:
I will never forget the day
It was late in the month of May
It started in the usual way
A handover with our patient lists
We gathered, doctors, nurses, therapists
And discussed a patient with COVID-19 infection
And his clinical deterioration.
He was a man of about fifty
Usually well and pretty healthy
Brought in by ambulance to A&E
With oxygen saturations of eighty
And quickly escalated to NIV.
Three days alternating CPAP and high flow
But progress was extremely slow
And by the morning of day four
He couldn’t cope any more
Sixty was his respiratory rate
So the decision was made to intubate.
He was given every treatment known
Antimicrobials, paralysis and prone
Epoprostenol and dexamethasone
So brittle was his gas exchange
with any small position change
And even on APRV
His FiO2 reached seventy.
His only chance of salvation
Was extracorporeal membrane oxygenation
As the retrieval team began their journey
ICU and theatre staff worked closely
Nurse, consultant and operating department practitioner
Helped move the patient into theatre
Still proned, too unstable
To even transfer to the table
We waited in personal protective gear
For the ECMO team to appear.
From London arrived the ECMO specialist
Her registrar and perfusionist
A quick briefing, roles allocated,
The patient was swiftly cannulated,
With the largest lines I’d ever seen!
And established on the ECMO machine
It was a truly inspiring scene.
Switching infusions, monitoring, ventilation,
Ready for patient transportation
But during the preparation
He went into fast atrial fibrillation
Requiring electrical cardioversion
Amiodarone and magnesium.
Sinus rhythm was restored
But it was an insult he couldn’t afford
Increasingly hypotensive he became
Chest compressions, adrenaline, all in vein,
And to a difficult decision we came
All agreed as a team
Time to switch off the machine.
I will never forget that day
It was late in the month of May
A life lost in a tragic way
But something I can honestly say
Never prouder have I been
Of every person in that team
We gave our all, we did our best
In peace may our patient rest.
Conclusion: I would like to dedicate this poem to all my ICU and theatre colleagues who shared this experience with me and, if given the opportunity, present it alongside pictures of them in their PPE as they were that day.
Combining cell therapy and extracorporeal membrane oxygenation for Acute Respiratory Distress Syndrome: Back to no future?
Rising Star - ICS Gold Medal
Jonathan Millar 1 , Jacky Suen2, Daniel McAuley3 and John Fraser2
1University of Edinburgh
2University of Queensland
3Queen’s University Belfast
Abstract
Introduction: After more than 50 years of research we are yet to develop an effective treatment for the Acute Respiratory Distress Syndrome (ARDS). This stands in contrast to the advances made in supportive care, a prime example of which is the maturation of Extracorporeal Membrane Oxygenation (ECMO). While technologies such as ECMO ‘buy time’ for recovery, the identification of a therapy remains crucial to improving outcomes. Recently, mesenchymal stem cells (MSCs) have shown promise as a novel treatment.1 Importantly, cell therapy may represent a means to overcome the hurdles associated with successful pharmacological intervention in ARDS.
Little is known about the interaction between cell therapy and ECMO. This is a deficiency, given that those receiving ECMO for ARDS are among the most severely ill and therefore most likely to benefit. This programme of work was designed to close that gap.
Objectives: Using a translational pipeline, our objective was to assess the safety and efficacy of MSCs during ECMO for ARDS.
Methods: We employed several diverse methods to address our objectives, including an ex-vivo ECMO simulation, complex sheep models of ARDS and ARDS and veno-venous ECMO, systematic review methodology, and unsupervised machine learning techniques.
Results: In our ex-vivo model, we were the first to demonstrate potential harms associated with MSC therapy during ECMO.2 When 40 × 10^6 clinical-grade human MSCs (Cynata Therapeutics Ltd., Australia) were added to fresh whole human blood and subjected to extracorporeal circulation using commercial components, oxygenator and pump performance was severely impaired within 4 hours. These experiments also demonstrated benefits associated with MSCs, including trends toward lower inflammatory cytokine concentrations and less neutrophil activation.3 To validate our findings, we sought to test hMSCs in a clinically-relevant sheep model. At the outset we undertook a systematic review of existing pre-clinical models of ARDS and ECMO.4 This has since produced an international collaborative effort to characterise pre-clinical models of ECMO across a range of indications. We subsequently described a ‘double-hit’ model of ARDS which combines oleic acid and intra-tracheal E. coli lipopolysaccharide. Using cluster analysis, we showed that this model shares qualitative similarities with the ‘hypo-inflammatory’ phenotype identified in clinical cohorts [Millar JE et al. Physiological Reports 2021. In Press]. Finally, in a 24-hour model, combining our novel injury method, VV-ECMO, and best practice ventilatory and supportive care, we performed a controlled trial of intra-tracheal hMSC therapy5 [Editorial: Del Sorbo L, Fan E. AJRCCM 2020]. This study showed that hMSCs reduce histological evidence of lung injury and ameliorate shock. However, hMSC-mediated impairment of oxygenator function was evident again.
Conclusion: This work addresses a gap in our understanding of cell therapy in critical illness. The findings are of direct clinical relevance, highlighting the potential harms of cell therapy during extracorporeal circulation. With a recent explosion in the number of registered clinical trials of MSCs for severe COVID-19 in mind, the use of MSCs during ECMO cannot be recommended.
References
1. Gorman G, Millar J, McAuley D, et al. Mesenchymal stromal cells for Acute Respiratory Distress Syndrome (ARDS), sepsis, and COVID-19 infection: optimizing the therapeutic potential. Expert Rev Respir Med 2021; 15(3): 301-324.
2. Millar JE, von Bahr V, Malfertheiner MV, et al. The administration of mesenchymal stem cells during simulated ECMO results in a rapid decline in oxygenator performance. Thorax 2019; 74(2):194-196.
3. von Bahr V, Millar JE, Malfertheiner MV, et al. Mesenchymal stem cells may ameliorate inflammation in an ex vivo model of extracorporeal membrane oxygenation. Perfusion 2019; 34(1):15-21.
4. Millar JE, Bartnikowski N, von Bahr V, et al. Extracorporeal membrane oxygenation (ECMO) and the Acute Respiratory Distress Syndrome (ARDS): a systematic review of pre-clinical models. Intensive Care Med Exp 2019; 7(1):18.
5. Millar JE, Bartnikowski N, Passmore MR, et al. Combined mesenchymal stromal cell therapy and ECMO in ARDS: a controlled experimental study in sheep. Am J Respir Crit Care Med 2020; 202(3):383-392.
Exploring the barriers to early physical rehabilitation and investigating its safety in critically ill patients receiving vasoactive drugs
Rising Star - ICS Gold Medal
Huw Woodbridge 1 , Caroline Alexander1, Mandy Jones2 and Anthony Gordon3
1Imperial College Healthcare NHS Trust
2Brunel University London
3Imperial College London
Abstract
Introduction: Early physical rehabilitation of patients in ICU decreases length of stay,1 aiming to improve physical outcomes. A deficit in rehabilitation in ICU has been observed2 and further information on the barriers in a UK setting is required. Rehabilitation safety concerns may form one barrier, however, there is a lack of a consistent adverse event definition in this context.3 An important safety factor is the requirement for vasoactive drugs and more detailed guidance on risk assessment for implementing rehabilitation in this context is required. A future trial would provide robust data to guide practice, however, preliminary feasibility must first be demonstrated.
Objectives:
1. Explore clinician and service-user perceptions of barriers to physical rehabilitation in ICU in the UK and how they can be overcome.
2. Develop multi-professional clinician and patient consensus agreement on the definition of an adverse event whilst an adult ICU patient receives physical rehabilitation.
3. To determine a multi-professional clinician consensus on assessing risk of physical rehabilitation for ICU patients receiving vasoactive drugs.
4. To describe current practice in one NHS Trust of physical rehabilitation with ICU patients receiving vasoactive drugs and the feasibility of a future trial.
Methods:
1. A qualitative study using semi-structured interviews, analysed using framework analysis, was carried out with ICU clinicians and former service-users to explore the barriers to rehabilitation.
2. A Delphi expert consensus process, using three rounds of questionnaires, used to gain agreement between an international group of clinicians and UK service users on an adverse event tool.
3. The same process was carried out with clinicians only, to reach consensus on a risk assessment framework, focused on patients receiving vasoactive drugs.
4. An exploratory observational study. Phase one was a retrospective review of current practice. Phase two recruited patients prospectively to measure feasibility outcomes.
Results:
1. Sixteen ICU clinicians and 14 former patients/relatives completed interviews. Analysis revealed themes of barriers and facilitators including safety issues, patient engagement, environment and experience.
2. Twenty-four multi-professional clinicians from 10 countries and six former patients/relatives reached consensus on an adverse event tool.
3. The clinician participants reached consensus on how to assess the risk of physical rehabilitation with patients receiving vasoactive drugs.
4. A review of 78 patients receiving vasoactive drugs showed little rehabilitation, which started later in an ICU stay. Preliminary feasibility of recruitment and follow-up after ICU discharge was demonstrated through 40 patients and 50 ICU clinicians recruited.
Conclusion: Greater depth of knowledge of barriers to ICU rehabilitation specific to the UK has been achieved which can optimise intervention delivery. Consensus on an adverse event tool will allow safety in future studies to be recorded more consistently. The risk assessment tool can provide guidance to clinicians when delivering rehabilitation for patients receiving vasoactive drugs. There is potential to increase the amount of early rehabilitation these patients receive and preliminary feasibility of a future trial is indicated if participants are recruited early.
Funded by an NIHR/HEE Clinical Doctoral Research Fellowship (ICA-CDRF-2015-01-026), and support from the NIHR CRN and Imperial BRC.
References
1. Waldauf P, Jiroutkova K, Krajcova A, et al. Effects of Rehabilitation Interventions on Clinical Outcomes in Critically Ill Patients: Systematic Review and Meta-Analysis of Randomized Controlled Trials. Crit Care Med 2020; 48(7): 1055-1065.
2. Connolly BA, Mortimore JL, Douiri A, et al. Low Levels of Physical Activity During Critical Illness and Weaning: The Evidence-Reality Gap. J Intensive Care Med 2019; 34(10): 818-827.
3. Nydahl P, Sricharoenchai T, Chandra S, et al. Safety of Patient Mobilization and Rehabilitation in the Intensive Care Unit. Systematic Review with Meta-Analysis. Ann Am Thorac Soc 2017; 14(5): 766-777.
Characterising mechanistically distinct subtypes of pandemic influenza-associated acute respiratory failure.
Rising Star - ICS Gold Medal
Romit Samanta 1 , Jake Dunning2, Adam Taylor3, Edwin Chilvers4, Rachel Chambers5, Peter Openshaw4 and Charlotte Summers1
1University of Cambridge
2Royal Free Hospital, London
3GlaxoSmithKline PLC, Stevenage
4National Heart and Lung Institute, Imperial College London
5Centre for Inflammation and Tissue Repair, University College London
Abstract
Aims/objectives: Influenza infection causes significant global mortality, morbidity and critical illness. Although recent evidence has yielded some insights into about the potential reasons for a proportion of patients developing severe illness following influenza infection, no clear mechanisms have been demonstrated in critically unwell patients. We sought to determine whether we could identify discrete mechanistically distinct subtypes of patients with influenza-associated acute respiratory failure.
Methods: Using integrative bioinformatic methods, we analysed plasma cytokine concentrations and whole blood gene expression obtained from 101 adult with confirmed influenza during two UK pandemic seasons (2009/10 & 2010/11). Data were clustered using a combination of Ward’s method for protein biomarkers and co-expression network analysis for whole blood gene expression from microarray data. The key differentiating mechanisms were identified using linear discriminant analysis. Outcomes for patients in each subtypes identified were described using Cox proportional hazards.
Results: We identified three subtypes of human response to influenza infection (Figure 1), characterised by differing levels of TNFα, IL-6, and TNFR-II. Two subtypes (16% and 32% of patients) were associated with severe respiratory failure requiring mechanical ventilation. The third subtype (52%) was associated with relatively milder disease (requirement for simple oxygen therapy). Pathway enrichment of high importance gene modules showed one severe subtype to be characterised by SLIT-ROBO signalling. SLIT-ROBO signalling is associated with pulmonary endothelial leak in murine models of influenza infection and sepsis.1 The other severe subtype was characterised by genes relating to immune modulation by the IFN-γ activated inhibitor of translation (GAIT) mechanism and neutrophil activation.2 Disruption of the GAIT mechanism likely leads to failure to terminate excessive and innate immune activation, and failure to initiate reparative processes.3 Patients within the latter subgroup had worse multi-organ dysfunction and 30-day mortality compared with the other two subtypes (HR 11.1, 95%CI 2.8-44.9; p < 0.001). Intercurrent bacterial infections did not fully account for the different subtypes seen. Subtypes were stable over 48 hours.
Figure 1.
Model outlining three subtypes of influenza-associated acute respiratory failure.
Discussion and conclusions: Our work has demonstrated the presence of mechanistically distinct subtypes of influenza-associated acute respiratory failure, with differing clinical outcomes. For the first time, we have successfully integrated gene expression, protein biomarkers, and clinical data to identify mechanisms relating to endothelial barrier function (SLIT-ROBO signalling) and dysregulated innate immunity (GAIT mechanism) in different sub-groups of patients with severe influenza. The stability of these subtypes may present novel opportunities for pharmacological intervention following prospective validation. Our methods could also be applied to other poorly understood clinical syndromes.
Each subtype was determined by integration of plasma cytokines with whole blood gene expression. Patients with the “adaptive” subtype had the best outcomes. Both the “endothelial leak “and “neutrophil-driven” subtypes had evidence of neutrophil activation but the neutrophil driven subtype had evidence of dysregulated innate immunity relating to the GAIT mechanism. GAIT gamma interferon inhibition of translation, PCT procalcitonin.
References
1. London NR, Zhu W, Bozza FA, et al. Targeting Robo4-dependent slit signaling to survive the cytokine storm in sepsis and influenza. Sci Transl Med. 2010;2(23). doi:10.1126/scitranslmed.3000678
2. Mukhopadhyay R, Jia J, Arif A, Ray PS, Fox PL. The GAIT system: a gatekeeper of inflammatory gene expression. Trends Biochem Sci. 2009;34(7):324-331. https://doi.org/10.1016/j.tibs.2009.03.004
3. Jia D, Rahbar R, Chan RWY, et al. Influenza Virus Non-Structural Protein 1 (NS1) Disrupts Interferon Signaling. PLoS One. 2010;5(11):e13927. https://doi.org/10.1371/journal.pone.0013927.
4. Dunning J, Blankley S, Graham CM, Hoang LT, Bloom CI. Progression of whole blood transcriptional signatures from interferon-induced to neutrophil-associated patterns in patients with severe influenza. Nat Immunolgy. 2018;19(June):625-635. doi:10.1038/s41590-018-0111-5
5. Tang BM, Shojaei M, Teoh S, et al. Neutrophils-related host factors associated with severe disease and fatality in patients with influenza infection. Nat Commun. 2019;10(1):1-13. doi:10.1038/s41467-019-11249-y
Anaemia following critical illness: mechanisms, clinical consequences and potential treatment strategies
Rising Star - ICS Gold Medal
Akshay Shah 1 , Stuart McKechnie2, Peter Robbins1 and Simon Stanworth1
1University of Oxford
2Oxford University Hospitals NHS Foundation Trust
Abstract
Introduction: Anaemia is a common complication of critical illness and can persist following ICU discharge. It is associated with poor physical recovery, increased dependency and fatigue. Active treatment of anaemia in other cohorts (e.g. chronic kidney disease, heart failure) has been shown to improve patient-centred outcomes but whether this applies to recovery from critical illness is unknown.
Objective: To investigate the epidemiology, underlying mechanisms and the potential treatments for anaemia in survivors of critical illness.
Methods: I used a range of methods during this doctorate:
1. Laboratory-based study to characterise anaemia following critical illness using a panel of novel markers of iron status
2. Database analysis of clinical characteristics and haemoglobin trajectories in survivors of critical illness
3. Systematic review on the safety and efficacy of iron therapy in critical illness
4. Multicentre, feasibility randomised controlled trial (RCT) of intravenous iron in patients discharged from critical care with moderate-severe anaemia (haemoglobin ≤100 g/L) in four ICUs (ISRCTN13721808)
Results: Anaemia of inflammation is highly prevalent at hospital discharge in critical care survivors (n(%) = 110/117 (94%) patients). Through measurement of hepcidin – the key iron regulatory peptide, iron restriction is the dominant mechanism and one-third of survivors have evidence of true iron deficiency.1
Data from 1174 patients found an associated between an ICU discharge haemoglobin of <100 g/L and prolonged post-ICU hospitalisation, and virtually no active management of anaemia in the post-ICU period.2 A mixed methods systematic review3 together with focus group meetings with ex-ICU patients identified fatigue, physical weakness and prolonged hospitalisation as barriers to recovery. These may be attributable to untreated anaemia.
Intravenous iron is a plausible treatment for the anaemia of inflammation observed in critical care survivors. A systematic review (six RCTs, n = 805 critically ill patients)4 found that iron therapy was safe and associated with an increase in haemoglobin, particularly at longer follow-up (mean difference 0.31 g/dL, 95%CI: 0.04–0.59). This review highlighted the paucity of data on the impact of iron therapy on functional outcomes during the recovery phase of critical illness.
I conducted a feasibility RCT to explore the potential benefits and risks of intravenous iron as a potential intervention to treat anaemia in critical care survivors.5 Feasibility was demonstrated by recruiting ninety-eight participants with 96% protocol adherence and 85% completion of follow-up. Intravenous iron was safe and biologically efficacious in increasing mean (SD) haemoglobin at 28 days (119.8 (13.3) g/L vs. 106.7 (14.9) g/L) and 90 days (130.5 (15.1) g/L vs. 122.7 (17.3) g/L). Hospital readmissions at 90 days post-randomisation were lower (7/40 vs.15/39, RR 0.46; 95%CI, 0.21–0.99; P=0.037) and median post-ICU hospital stay was non-significantly shorter in the iron group (5.0 vs. 9.0 days, P=0.15). Pre-randomisation hepcidin concentrations were associated with differential responses to treatment.
Conclusion: This body of work has generated novel data on the anaemia of inflammation following critical illness. The underlying mechanisms are responsive to intravenous iron therapy, which appears to be safe with possible improvements in clinical outcomes. I am designing a larger randomised study to confirm these findings.
References
1. Shah A, Wray K, James T, et al. Serum hepcidin potentially identifies iron deficiency in survivors of critical illness at the time of hospital discharge. Br J Haematol 2019; 184: 279-281.
2. Shah A, Stanworth SJ, Lee A, Johnston L, Docherty AB. Prevalence, management and outcomes associated with anaemia in ICU survivors: a retrospective study. Anaesthesia. Epub ahead of print 31 March 2021. DOI: 10.1111/anae.15461
3. Bench S, Stayt L, Shah A, Dhiman P, Czuber-Dochan W. Prevalence and experience of fatigue in survivors of critical illness: a mixed-methods systematic review. Anaesthesia 2021; 76: 1233-1244.
4. Shah A, Fisher SA, Wong H, et al. Safety and efficacy of iron therapy on reducing red blood cell transfusion requirements and treating anaemia in critically ill adults: A systematic review with meta-analysis and trial sequential analysis. J Crit Care 2019; 49: 162-171.
5. Shah A, Marian I, Dutton SJ, et al. INtravenous iron to treat anaemia following CriTical care (INTACT): A protocol for a feasibility randomised controlled trial. J Intensive Care Soc 2021; 22: 182.
The Secondary Use of Longitudinal Critical Care Data
Rising Star - ICS Gold Medal
Edward Palmer
Royal London Hospital
Abstract
Introduction: The NIHR critical care health informatics collaborative (CC-HIC) is a multi-centre research project pooling high resolution data on critical care patients from the electronic heath records (EHRs) of 12 ICUs in the UK.1 The CC-HIC data model represents 255 data fields including demographics, granular longitudinal physiology and outcomes. This model aligns EHR data to provide a high-quality clinical research database. My PhD examined the capability of the CC-HIC as a novel data resource to support clinical research. Following this validation, I undertook two clinical research studies.
Objectives:
Phase 1
1) To evaluate the suitability of the CC-HIC data model to represent the EHR for secondary research use.
2) To evaluate data quality of the CC-HIC research database.
Phase 2
3) To use CC-HIC to conduct two clinical research studies that make use of the unique longitudinal data provided:
• The association between cumulative exposure to excess oxygen and mortality
• The association between morphologies of longitudinal physiology - in particular organ dysfunction - and mortality in sepsis
Methods: In phase 1 I wrote software2,3 to implement the Khan data evaluation framework4 against the CC-HIC research database. This systematically identified and categorised potentially erroneous data, permitting corrections to the database and enhancing quality over time. I employed novel methods to address features of data that are commonly encountered, for example, the application of a model based approach to reduce missing meta-data; such as whether a blood gas was arterial or venous. In phase 2, I applied cumulative logistic regression models to identify the association between the cumulative exposure to excess oxygen (defined as a PaO2 > 13.3 kPa) and mortality. For the second study I applied a joint modelling paradigm to explore the different longitudinal profiles of organ failure in sepsis.
Results: Following the application of my software,2,3 the CC-HIC research database contains 46,494 critical care episodes, representing billions of datapoints, which have been validated for research use. I found a small (an absolute risk reduction of about 1%) dose-independent association between exposure to excess oxygen and mortality. This research has been published in a high impact factor journal.5 I found that the trajectory of organ failure (hazard ratio 2.60 [2.04, 3.30]) played a more significant role in determining mortality than the absolute value of organ failure (hazard ratio 1.24 [1.21, 1.26]). This finding was consistent over all organ systems.
Conclusion: The CC-HIC has been validated as a tool for critical care research. My software contributions have been provided to enhance the quality and streamline the use of this resource. This research highlights the importance of quality curation of vast clinical data resources, prior to their use in clinical research.As oxygen is so widely used, any potential harms arising from excess use are far reaching. These findings are now subject to confirmation through ongoing RCTs. The trajectory findings have implications for how we view the evolution of physiology in sepsis, suggesting that dynamic measures of patient physiology better reflect a patient’s underlying biology.
References
1. Harris, S, S Shi, D Brealey, Niall S. MacCallum et al. ‘Critical Care Health Informatics Collaborative (CCHIC): Data, Tools and Methods for Reproducible Research: A Multi-Centre UK Intensive Care Database’. International Journal of Medical Informatics 112(2018): 82–89. https://doi.org/10.1016/j.ijmedinf.2018.01.006.
2. Palmer, E. InspectEHR: Standardised Data Quality Evaluation for CC-HIC. Version 1. 2020. www.github.com/DocEd/inspectEHR.
3. Palmer, E. WranglEHR: Standardised Data Extraction for CC-HIC. Version 1. 2020. www.github.com/DocEd/wranglEHR.
4. Kahn, MG., TJ. Callahan, J Barnard, AE Bauck, et al. A Harmonized Data Quality Assessment Terminology and Framework for the Secondary Use of Electronic Health Record Data. EGEMs (Generating Evidence & Methods to Improve Patient Outcomes) 4, no. 1 (11 September 2016): 18. https://doi.org/10.13063/2327-9214.1244.
5. Palmer, E, B Post, R Klapaukh, G Marra, et al. The Association Between Supra-Physiologic Arterial Oxygen Levels and Mortality in Critically Ill Patients: A Multi-Centre Observational Cohort Study. American Journal of Respiratory and Critical Care Medicine, 2019. https://doi.org/10.1164/rccm.201904-0849OC.
P300
Role of FUSIC ultrasound in the unwell peri- and post-partum patient
The Ultrasound Ninja
Alexander McDonald
NHS Dumfries and Galloway
Abstract
Introduction: The referral to a breathless patient on the maternity ward on a Friday evening comes with a degree of trepidation. Considerations about altered ‘normal’ physiology, the most appropriate diagnostic process, as well as a time of heightened emotional engagement all feed into the situation. The last Confidential Enquiry into Maternal Deaths in 2018 showed that 23% of maternal deaths were due to cardiac disease, 14% from pneumonia or influenza and 11% from venous thromboembolism (VTE).1 Improving awareness of these conditions’ impact led to the ‘Three Peas in a Pod’ Poster published by the Medical Royal Colleges and Royal College of Obstetricians and Gynaecologists – this emphasised the increased risk of cardiac failure, need for CXR with antibiotic or antiviral treatment promptly and the risk of VTE.2
Point-of-care Critical Care Ultrasound can provide a positive diagnosis without the need for CT ionising radiation.
Main Body: Focused Ultrasound in Intensive Care (FUSIC) competencies combine heart, chest and DVT scanning that can aid the clinician in making a diagnosis in infective, thromboembolic and cardiac conditions.
In our hospital, the medical team manage HDU within a combined ICU and HDU Unit. A 27-year-old lady was referred to the medical team urgently to assist with the diagnosis and management of an 8-day post-partum mother who had been admitted complaining of severe breathlessness and ankle swelling, worse since delivery. She had no cardiac history other than hypertension during the third trimester of pregnancy with no proteinuria, managed with labetalol and nifedipine. She was hypertensive and tachycardic at 154/110 and 106 respectively, on no oxygen but severely breathless on minimal exertion. She had already had a CTPA organised by the Obstetric team which showed no PE. A medical consultant was asked to review the patient urgently (who happened to also work ICU sessions and was newly trained in Focused Intensive Care Echocardiography (FICE) - the predecessor qualification to ‘FUSIC Heart’).
The ECG showed sinus tachycardia without ischaemia. A FICE echocardiogram was performed at the bedside, showing a dilated LV at 5.4 cm and visually severe LV systolic dysfunction with a 1.7 cm pericardial effusion.
This allowed a positive preliminary diagnosis to be made of Peripartum Cardiomyopathy and commencement of loop diuretic therapy with good effect. Peripartum cardiomyopathy is a rare, often idiopathic but potentially life threatening and reversible cause of dilated cardiomyopathy that is amenable to cardiac and chest ultrasound diagnosis.3,4
A Medical High Dependency bed was requested as agreed with the Obstetric team as the most suitable place to manage this medically unwell maternity patient with shared care pending Cardiology takeover. A formal echocardiogram confirmed the diagnosis the following weekday.
Conclusion: Sepsis, Cardiac pathologies and VTE are significant causes of breathlessness in the pregnant and post-partum period. Point-of-care ultrasound, in particular chest, heart and DVT scanning are valuable tools that can provide an early positive diagnosis of important differentials and potentially avoid CT ionising radiation.
Brief description of ultrasound video:
This video is taken from the case – can you determine the cause of her breathlessness?
References
1. Knight M BK, Tuffnell D, Shakespeare J, Kotnis R, Kenyon S, Kurinczuk JJ (Eds.) on behalf of MBRRACE-UK. Saving Lives, Improving Mothers’ Care - Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2016-18. Oxford, UK: National Perinatal Epidemiology Unit, University of Oxford 2020; 2018. Contract No.: ISBN: 978-1-8383678-0-0.
2. Northridge R. Three Peas in a Pod: RCPSG, RCOG. 2016. Available from: https://rcpsg.ac.uk/college/this-is-what-we-stand-for/policy/maternal-health.
3. Bauersachs J, König T, van der Meer P, Petrie MC, Hilfiker‐Kleiner D, Mbakwem A, et al. Pathophysiology, diagnosis and management of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. European journal of heart failure. 2019;21(7):827-843.
4. Honigberg MC, Givertz MM. Peripartum cardiomyopathy. BMJ. 2019;364:k5287.
P301
Massive pulmonary embolism post decannulation from Extra Corporeal Membrane Oxygenation: an unexpected complication
The Ultrasound Ninja
Hesham Ismail, Laura Price, Carole Ridge, Brijesh Patel, Stephane Ledot and Francisca Caetano
Royal Brompton Hospital
Abstract
Introduction: Massive pulmonary embolism is a rare complication following Veno-Venous Extra Corporeal Membrane Oxygenation (VV-ECMO) decannulation. Management can be challenging. The authors present a case that required VV-ECMO re-cannulation and catheter-directed thrombolysis.
Main body: 58-year-old gentleman, background of hypertension and asthma, admitted with severe respiratory failure secondary to COVID-19 pneumonitis. Due to lack of improvement with conventional ARDS treatment, he was referred and retrieved on VV-ECMO.
After being off sweep gas for more than 24 hours he was decannulated on day 7. Five hours after decannulation the patient acutely deteriorated. He became tachycardic, hypotensive and hypoxic. A bedside TTE showed severely dilated and impaired right ventricle. The patient was started on milrinone and nitric oxide. Nevertheless, he deteriorated further and became profoundly hypoxic and hypercapnic, and a decision was made to start him on VV-ECMO. A TOE was done to guide cannulation and showed a thrombus in the RV and in the left pulmonary artery.
Next day, a CT-pulmonary angiogram (CTPA) was done which showed saddle-shaped pulmonary embolism, with a large occlusive clot in the left main pulmonary artery causing complete non-perfusion of the left lung. After a multi-disciplinary team discussion, the patient had catheter-directed thrombolysis, with some haemodynamic improvement.
Within 48 hours, TTE was repeated showing no significant improvement on RV function. CTPA showed very mild decrease of the clot burden. Decision was made to repeat catheter-directed thrombolysis and partial thrombectomy. Repeated imaging revealed decrease in the size of the left main pulmonary artery thrombus.
It is thought that the massive pulmonary embolism could have been caused by showering of ECMO cannulas-related thrombi, which were dislodged during decannulation.
Patient remained on VV-ECMO for 32 days and was decannulated successfully afterwards and was discharged home on apixaban and long-term pulmonary hypertension follow-up.
Conclusion: ECMO cannulas related thrombi are not uncommon complications because of prolonged stay and coagulopathy related to ECMO circuit. However, massive embolism is rarely seen. The use of echocardiography was paramount on the differential diagnosis.
Brief description of ultrasound video:
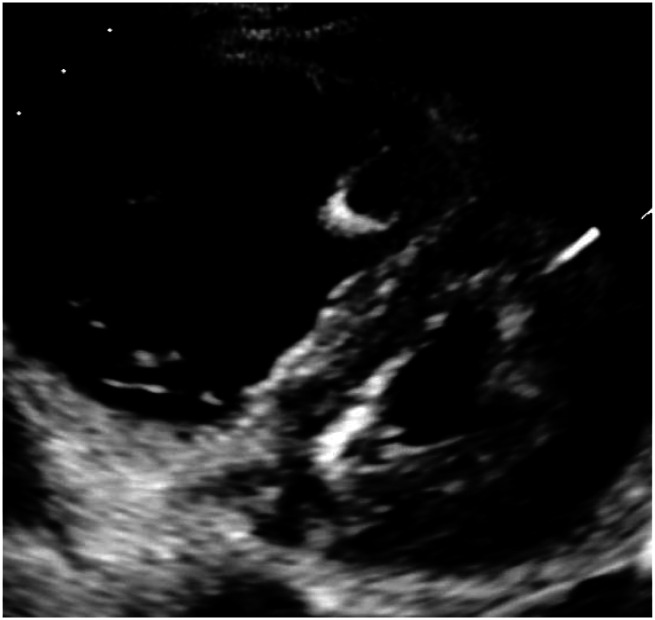
In this TTE study, the right ventricle looks significantly dilated with severely impaired both longitudinal and radial functions. Additionally noted septal flattening in systole indicating RV pressure overload, diastolic notching of RVOT doppler trace consistent with significantly raised pulmonary artery pressure and mild to moderate tricuspid regurgitation. Otherwise, the left ventricle is small and has preserved function.
P302
Stunning
The Ultrasound Ninja
Alex Jude Fonseca, Shashi Chandrashekaraiah, Avinash Jha and Shondipon Laha
Royal Preston Hospital, LTHTR
Abstract
Introduction: Focussed ultrasound in intensive care (FUSIC) has transformed the practice of critical care. Bedside ultrasound is a useful complementary diagnostic tool which contributes to an early therapeutic decision based on reproducible physio-pathologic data.1We highlight a scenario where ultrasound proved to be the game changer in a post-operative neurosurgical patient, when all hope was lost.
Main Body: A17-year-old female was transferred to our critical care unit post fronto-temporo-parietal (FTP) craniectomy for significant right frontal epidural haematoma and right FTP acute subdural haematoma with significant transcalvarial brain herniation. The mechanism of injury was unknown and believed to be an alleged suicidal attempt. Owing to her hemodynamic instability, she required high strength nor-adrenaline and vasopressin infusions and multiple crystalloid boluses to maintain her blood pressure. Antibiotics were escalated and stress dose steroids were commenced. Her guarded prognosis was communicated to her family.
Bedside FUSIC was performed to rule out any causes of impending cardiac arrest as she was extremely unstable to be shifted for CT scan imaging. It showed features of global left ventricular hypokinesia with ballooning suggestive of neurogenic stress cardiomyopathy (NSC) or neurocardiogenic stunning. Dobutamine was initiated in addition to the ongoing vasopressors and some degree of haemodynamic stability was achieved.
Advanced cardiac monitoring with LiDCO was not reliable as the patient had cardiac arrhythmia and sporadically showed erratic readings, requiring frequent recalibrations. Later, it did support our findings of pump failure.
Over the next 48-72hours, the vasopressor and inotropic requirements decreased and the patient was weaned from the ventilator & shifted to the neurosurgical ward for rehabilitation. Formal echocardiography confirmed our FUSIC findings and we saw a reversal to normal function on follow up.
Conclusion: Recognition of NSC is important because the diagnosis has implications for management and prognosis.2 The advantages of ultrasound are of great value in the setting of critical care medicine, as immediate decision making can be lifesaving.3
FUSIC findings: Global left ventricular hypokinesia and ballooning with reduced contractility. No right ventricle dilatation and no evidence of pericardial effusion. Bilateral femoral & popliteal veins showed no evidence of thrombus. Lung ultrasound demonstrated B lines and mild pleural effusion in bilateral bases. Abdomen scan did not reveal any fluid collection.
References
1. Silva S, Biendel C, Ruiz J, et al. Usefulness of cardiothoracic chest ultrasound in the management of acute respiratory failure in critical care practice. Chest. 2013;144(3):859-865.
2. Bybee KA, Prasad A. Stress-related cardiomyopathy syndromes. Circulation. 2008; 118: 397–409.
3. Lichtenstein, D., van Hooland, S., Elbers, P. W. G., & Malbrain, M. L. (2014). Ten good reasons to practice ultrasound in critical care. Anaesthesiology Intensive Therapy; 46(5): 323-335.
P303
Ultrasound ninja to the rescue- the sepsis and hemodynamic savior
The Ultrasound Ninja
Avinash Kumar Jha 1 and Shashi Chandrashekaraiah2
1Lancashire Teaching Hospitals (LTHTR)
2Lancashire Teaching Hospitals
Abstract
Introduction: An elderly male was admitted to the emergency department with feeling unwell for seven days and vomiting. On evaluation, the patient was found to have hypotension and a low Glasgow coma score (GCS). He was transferred to critical care because of hemodynamic instability despite adequate fluid resuscitation and requiring a maximum dose of noradrenaline infusion. He was intubated immediately given low GCS. A focussed echocardiogram was performed which showed deranged left ventricle and right ventricular function. Following this cautious fluid resuscitation approach and dobutamine was added alongside. A formal echocardiogram performed on the following day confirmed the presence of deranged biventricular function.
Routine blood tests including cultures were sent, and antibiotics were administered as per sepsis six protocol. Following this, lung and abdominal ultrasound were performed. The abdomen ultrasound showed a thickened gall bladder wall, which looked suspicious with no prominent gall stones. On further evaluation, the GB wall measured 7millimetres.
In combination with altered liver function tests, the finding on ultrasound pointed towards the presence of Acute acalculous cholecystitis (AAC). An immediate CT abdomen was ordered, which showed the presence of inflammation and collection around the gall bladder, confirming the presence of acalculous cholecystitis.
A multi-disciplinary team discussion was conducted between intensive care, surgical and the interventional radiology team. Considering the presence of hemodynamic instability and the need for immediate source control, the outcome of the decision was to go ahead with percutaneous drain insertion into the gall bladder.
Over the next 24 hours, the vasopressor and inotropic requirement was weaned, and by day four, the patient was hemodynamically stable. He was extubated and transferred to the ward under the surgical team for further management.
Main body: In our case, the point of care ultrasound helped us quickly assess, identify pump failure-related hypotension, and incidentally, the source of sepsis.
AAC is a life-threatening condition associated with a high risk of necrosis and perforation compared to calculous disease.1 On ultrasound examination, a thickened gall bladder wall of more than 3.5 millimetres suggests the presence of cholecystitis. It is difficult to diagnose and associated with high mortality (>30%).2
In addition to the management of sepsis, we managed cardiogenic shock with dobutamine and eventually weaned the patient from inotropes and mechanical ventilation.
Conclusion: In our case, the hemodynamic instability was due to a combination of both septic and cardiogenic shock. A comprehensive scan helped us understand the aetiology and thus the necessary management in a time-critical condition.
Thus, we believe that a quick multi-site point of care ultrasound can be a simple, fast and life-saving procedure in intensive care.
Ultrasound video: A loop showing significant thickening of the gall bladder wall with no gall stones.
References
1. Jones MW, Ferguson T. Acalculous Cholecystitis, ncbi.nlm.nih.gov/books/NBK459182/ (2021, accessed 22 August 2021)
2. Factor P and Saab S. Critical care management of patients with liver disease. In: Sanyal A, Boyer TD, Lindor KD, et al. (eds). Zakim and Boyer’s Hepatology. 7th ed. Philadelphia: Elsevier, 2018, pp.194-201.
P304
Use of ultrasound in diagnosing and managing overian hyperstimulation syndrome
The Ultrasound Ninja
Mathew Musalia
Royal Preston Hospital - Preston, Lancashire
Abstract
Introduction: Use of ultrasound can help clinicians make important decisions with regards to diagnosing and managing conditions that are not commonly encountered, like Ovarian hyper stimulation syndrome (OHSS) which has varied clinical presentation and can create a diagnostic and management conundrum for critical care clinician.
Main Body: 32 Year old, recently undergone In Vitro fertilization (IVF) presenting to hospital with abdominal pain, bloating, nausea, vomiting, speech disturbances, fluctuating level of consciousness and limb weakness. Initial physical examination suggestive of stroke, had a head CT scan done that revealed a basilar artery stroke, she was intubated and had a thrombectomy done. Echo done to assess for source of clots, noted to have possible mitral valve vegetation and right heart strain. Ultrasound done also revealed bilateral pleural effusion. CTPA done revealed left pulmonary embolism. Beta HCG was raised, multidisciplinary assessment concluded likely severe OHSS. Abdominal distention was progressive and firm. Concerns about level of ascites, possibility of ectopic pregnancy given rise in B-HCG or bowel obstruction. Bedside ultrasound scan of abdomen /pelvis revealed moderate ascites and markedly enlarged ovaries with left larger than right. Visualising the enlarged ovaries helped cement diagnosis and guided decision regarding draining of what initially looked to be massive ascites causing abdominal distention, which was actually due to markedly enlarged ovaries + ascites. She had U/S guided ascetic drain insertion. Formal abdominal u/s requested to confirm findings. With diagnosis of OHSS confirmed she has been managed according to recommended guidelines. She has required ventilator support temporarily, fluid resuscitation to correct for hypercoagulable state due to fluid third spacing. Bilateral EVD drains and Posterior decompressive craniectomy due to infarct.
Conclusion: Use of bedside U/S in critical care setting can help with diagnosis less common conditions and aide clinicians in making treatment decisions at the bedside saving on time and reducing chances of patient harm or undergoing unnecessary procedures. Junior clinicians will gain invaluable insight when they use POCUS and correlate with clinical findings; however, care must be taken to consult more experienced members of the team, as the enlarged ovaries were initially confused for dilated bowel and needed senior review to ensure correct diagnosis.
Brief description of ultrasound video: Bilateral enlarged ovaries. Right ovary measuring 15×11×12cm, left 10×5.6× 5.5cm. Ovaries containing multiple enlarged follicles. Uterus appears normal in size
References
1. Frasure SE, Rempell JS, Noble VE, Liteplo AS. Emergency ultrasound diagnosis of ovarian hyperstimulation syndrome: case report. J Emerg Med. 2012;43(2):e129-e132. doi: 10.1016/j.jemermed.2011.06.148. Epub 2012 Apr 21. PMID: 22525699.
2. Kiel J. Acute ascites and abdominal pain from ovarian hyperstimulation syndrome (OHSS). Am J Emerg Med. 2019;37(4):e5-e6. doi: 10.1016/j.ajem.2018.12.050. Epub 2018 Dec 27. PMID: 30598375.
P305
Bedside echocardiographic diagnosis of Pericardial effusion in the critically ill patient and prevention of catastrophic hemodynamic compromise
The Ultrasound Ninja
Kanika Arora 1 , Shashi Chandrashekaraiah1 and Alex Fonseca2
1Lancashire Teaching Hospitals
2Lamcashire Teaching Hospitals
Abstract
Introduction: In recent years, the use of ultrasound in critical care has revolutionized the bedside assessment of ICU patients. Though operator dependent, the advantage of repeatability and being relatively inexpensive makes it imperative for critical care physicians to stay updated with this modality. The purpose of this report is to describe an incidental finding of pericardial effusion in a patent admitted with respiratory distress.
Main body: A 26 years old female was admitted with shortness of breath and increase in oxygen requirements. She had a background of cerebral palsy, tracheostomized since 2009 after being operated for scoliosis and had a vagal nerve stimulator in situ. On admission, her 1st covid swab was negative. She normally required home ventilation only at night, however 2 days prior to admission, she required 24 hours of ventilator support. A large leak was noted on the ventilator and had a non-cuffed tracheostomy tube in situ, which was later changed to a cuffed one. A quick bedside FICE (Focused Intensive Care Echocardiography) revealed a large circumferential pericardial effusion with fibrin strands. There was no haemodynamic compromise on admission, however the large pericardial effusion could have been an attributing factor to her severe respiratory distress. She progressively started deteriorating hemodynamically, requiring intravenous fluids and vasopressor support. A definitive ECHO done by the cardiologist confirmed the findings of FICE. There was a rapid change in her condition post-pericardiocentesis. As per the institute protocol, a second covid swab was sent for her, which reported positive. Covid-19 RTPCR testing was not validated on pericardial fluid, hence was not undertaken. The culture of pericardial fluid revealed staphylococcus aureus, but there was a high index of suspicion of COVID and bacterial pericarditis was unlikely.
Conclusion: Echocardiographic evaluation of Pericardial effusion is of paramount importance for timely and appropriate diagnosis. In view of quick bed side diagnosis with ultrasound, our patient was able to survive this life-threatening condition and treatment was initiated promptly. If left undiagnosed based on clinical presentation, it could have been catastrophic for a completely treatable cause.
Brief description of ultrasound video: Pericardial effusion appears as an echo-free space between the 2 layers of pericardium. This video shows a 4-chamber echocardiographic view suggestive of a globular pericardial effusion with fibrin strands. An element of hemodynamic compromise was visible on 4-chambered view as well as para-sternal long axis view.
P306
Bedside diaphragmatic ultrasound used to diagnose an unexpected cause of weaning difficulty in a patient with COVID-19 pneumonitis
The Ultrasound Ninja
Tammar Al-Ani and Richard Cowan
Glasgow Royal Infirmary
Abstract
Introduction: Diaphragm dysfunction has been described as being responsible for weaning failure with an incidence of 23–80%. It has also been associated with difficult weaning from mechanical ventilation, prolonged intensive care unit (ICU) stay and increased ICU and hospital mortality.1 This case report describes the use of bedside ultrasound to diagnose diaphragm dysfunction, assess the severity of dysfunction, refer to specialist care and monitor disease progression in patient with COVID-19 pneumonitis with difficulty weaning from mechanical ventilation.
Main body: A 59 year-old male with no known past medical history was admitted to our ICU with respiratory failure due to COVID-19 pneumonitis. He had received continuous positive pressure ventilation with oxygen supplementation on the medical high dependency unit for 15 days prior to deteriorating and requiring invasive ventilation in ICU.
In ICU, the patient was mandatory ventilated using lung protective ventilation strategies for 26 days before he was switched to pressure support ventilation for attempts to wean him from mechanical ventilation. During the initial phase of his ICU admission, he was severely hypoxaemic and required deep sedation as well as muscle relaxation for a total of 370 hours. Prone positioning was required on 4 occasions before he was stable in the supine position.
Once attempts to liberate him from mechanical ventilation were being made, pressure support was gradually reduced along with PEEP and FiO2. Progress with this reduction in support was slow due to marked tachypnoea and a dyssynchronous respiratory pattern. It was also noted that he had poor air entry in his right base with corresponding right lower zone opacities on his chest x-ray.
At this stage a bedside ultrasound was used to investigate the cause of weaning difficulty and consequently, the diagnosis of right diaphragmatic paralysis was made. This was a new finding, as his admission chest x-ray did not show a raised hemidiaphragm. This diagnosis led to an increased focus on physical rehabilitation and mobilisation with tolerance of his tachypnoea and respiratory pattern as we now appreciated this didn’t represent ongoing underlying parenchymal lung disease. We also made a referral to the respiratory team in order to facilitate longer-term rehabilitation and follow up.
The patient was successfully extubated after intense physical rehabilitation, post extubation he remained tachypnoeic and still required supplemental oxygen at the point of hospital discharge. A follow up diaphragm ultrasound 6 months after discharge did not show any improvement in the right diaphragmatic function, he remains dyspnoeic on exertion and still occasionally uses ambulatory supplemental oxygen.
Conclusion: Ultrasound assessment revealed an unexpected cause of weaning difficulty in our patient that allowed us to individualise his weaning plan and rehabilitation. This case shows that bedside intensivist performed ultrasound can accurately evaluate diaphragmatic function in patients who are difficult to wean from mechanical ventilation.
Brief description of ultrasound video: The diaphragm was scanned using low frequency curvilinear ultrasound probe. There is lack of diaphragmatic excursion and absent thickening of the right hemidiaphragm on subcostal and intercostal views. M-mode evaluation and ‘sniff test’ confirms diaphragmatic paralysis.
References
1. Dres M, Dubé B, Mayaux J, Delemazure J, Reuter D, Brochard L, et al. Coexistence and Impact of Limb Muscle and Diaphragm Weakness at Time of Liberation from Mechanical Ventilation in Medical Intensive Care Unit Patients. American Journal of Respiratory and Critical Care Medicine. 2017;195(1):57-66.
P307
A rare case of an abnormal post-traumatic shoulder swelling
The Ultrasound Ninja
Salman Naeem1, Angus Perks and Serena Rovida3
1London’s Air Ambulance Charity
2Barts Health NHS trust
3Barts Health NHS Trust
Abstract
Introduction: Pseudoaneurysms are abnormal dilation of the arterial wall that are usually formed due to trauma, infection, inflammation or iatrogenic causes. Unlike true aneurysms, pseudoaneurysms are usually contained by adventitia and might not be covered by all the three layers of the vessel. Although most of the pseudoaneurysms are asymptomatic but they can increase in size causing pain and pressure symptoms. In rare occasion they can leak or rupture causing life threatening haemorrhage. This a case of an abnormal swelling arising in the shoulder of a patient two days after an assault.
Main Body: PoCUS showed a hypoechoic collection below the deltoid muscle with a 77mm round pulsating collection. This demonstrated the ‘ying-yang sign’ on assessment with colour doppler and was found to be arising from one of the branches of the thoracoacromial part of axillary artery. This significantly altered the management of the patient in prompting a CT angiogram that confirmed a leaking pseudoaneurysm in the right shoulder with surrounding hematoma. The patient was admitted for an ultrasound guided thrombin injection which was successful.
Traumatic pseudoaneurysms of branches of thoracoacromial part of axillary artery are very rare. Most cases reported in literature are post infectious in aetiology. Blunt trauma can lead to weakening in the arterial wall resulting in formation of a pseudoaneurysm. Ultrasound has been used to evaluate soft tissue swellings and pseudoaneurysms in post-traumatic injuries and intravenous drug users. Pseudoaneurysms appear as round pulsating swellings arising from a vessel. Colour doppler shows the pathognomic ‘ying-yang’ or ‘pepsi’ sign which is due to turbulent flow of blood within the pseudoaneurysm.
Conclusion: This case highlights the utility of PoCUS in the evaluation of traumatic soft tissue swellings and its ability to direct diagnostics and expedite appropriate patient management.
Brief Description of Ultrasound Video: This video demonstrates a round swelling clearly arising from a vessel, with colour flow demonstrating the ‘ying-yang’ sign of turbulent flow.
References
1. Poonai, N., Lim, R., & Lynch, T. (2011). Pseudoaneurysm formation following a traumatic wrist laceration. Canadian Journal of Emergency Medicine, 13(1), 48-52. doi:10.2310/8000.2011.101038
2. Østerballe L, Helgstrand F, Axelsen T, Hillingsø J, Svendsen LB. Hepatic pseudoaneurysm after traumatic liver injury; is CT follow-up warranted? J Trauma Manag Outcomes. 2014;8:18. doi: 10.1186/1752-2897-8-18. PMID: 25780384; PMCID: PMC4360922.
3. Wright AE, Wall M, Slaney P, Downing R. An unusual presentation of thoracoacromial artery pseudoaneurysm following shoulder arthroplasty. BMJ Case Rep. 2014;2014:bcr2014204625. doi: 10.1136/bcr-2014-204625. PMID: 24973348; PMCID: PMC4078424.
4. Rovida S, Vetrugno L, Naeem S. Rapid Diagnosis of A Palmar Artery Pseudo-Aneurysm with Bedside Ultrasonography in Emergency Department. Journal of Radiology and Clinical Imaging. 2020;3:092-095.
P308
The role of point of care ultrasound in the diagnosis of femoral artery pseudoaneurysms in the emergency department: A case report
The Ultrasound Ninja
Ziad Al-Ani and Caitriona Considine
Glasgow Royal Infirmary
Abstract
Introduction: The femoral artery pseudoaneurysm is a known serious complication of intravenous drug abuse. A missed diagnosis may have a devastating outcome as a result of life-threatening haemorrhage in the event of rupture. The use of point of care ultrasound in the emergency department can help to minimise this risk by providing early bedside diagnosis.
Main Body: We present a case report of 54 years old male intravenous heroin user who was brought to the emergency department with a suspected right femoral shaft fracture following a fall at home. He was unable to weight-bear for three days. Upon arrival to hospital, his venous blood gas showed a haemoglobin of 65g/L. He had a large non-pulsatile swelling over his right thigh with surrounding skin erythema. The swelling extended down to his right knee. The patient was taken to the resuscitation area where a bedside ultrasound scan was performed before plain film imaging. This showed a large pseudo-aneurysm over the femoral artery region. The patient was taken urgently to theatre for successful arterial ligation.
Conclusion: The point of care ultrasound is a very useful, rapid and reliable non-invasive bedside tool that can be used in the emergency department to detect pseudo-aneurysms in IVDU patients when there is a high clinical suspicion. In this particular case, it helped to provide a prompt, lifesaving diagnosis and shifted patient’s care in the right direction.
Brief description of ultrasound video: A bedside ultrasound scan of the right groin area revealed a large fluid-fluid sac over the femoral artery region with a bidirectional, turbulent, flow and a characteristic Yin-Yang sign when colour doppler flow was applied.
P309
Powerful and reliable tool in post-partum cardiac arrest
The Ultrasound Ninja
Alex Fonseca, Shashi Chandrashekaraiah and Shondipon Laha
Royal Preston Hospital - LTHTR
Abstract
Introduction: The maternity suite is the only place in the hospital where patients come to the hospital willingly, to experience their bundle of joy for the first time. It is relatively the happiest spot in the hospital, but stress levels can skyrocket if things go wrong in an otherwise straightforward physiological process. We share our experience with one such scenario where Focused Ultrasound in Intensive Care (FUSIC) aided in prompt diagnosis and guided appropriate treatment.1
Main body: A 30-year-old fit & well postpartum female, 2 days post her normal vaginal delivery following an uneventful antenatal period, remained in the hospital as she experienced issues with feeding her baby. She developed sudden onset intermittent mild chest discomfort which subsided without therapy. A few hours later, she was found collapsed in the corridor by the midwives. Cardiopulmonary Resuscitation (CPR) was commenced, which showed an initial rhythm of ventricular fibrillation. She was intubated during CPR and Return of Spontaneous Circulation (ROSC) was achieved in 10 mins.
Post ROSC there was persistent hemodynamic instability which required metaraminol infusion & crystalloid boluses to maintain her blood pressure along with high oxygen requirements. FUSIC guided us by rapidly ruling out the relevant reversible causes of arrest. Our initial strong differentials of pulmonary embolism, amniotic fluid embolism & peripartum cardiomyopathy2 were ruled out along with hypovolemia, coronary thrombosis, cardiac tamponade and tension pneumothorax.
Post FUSIC, heart failure treatment was initiated with diuretics and additional positive end expiratory pressure (PEEP) post adequate sedation. Nor-adrenaline was initiated via a central venous access, crystalloid infusion was limited & antibiotics were initiated for left sided aspiration pneumonia in addition to routine critical care.
CT thorax confirmed aspiration pneumonia and no evidence of pulmonary embolism. Subsequent formal echocardiography by the cardiologist confirmed our FUSIC findings of heart failure which was supported by serial rise in troponins (360 > 466) & raised NT-pro B – type Natriuretic Peptide (800) despite normal electrocardiograms.
Patient was extubated the following day & later shifted to the coronary care unit. She underwent an angiography which was normal and was discharged home a week post ICU admission. An implantable cardioverter defibrillator was inserted at a later date for her cardiac arrhythmias.
Conclusion: FUSIC aids intensivists in rapid diagnosis & treatment in challenging scenarios like post-partum cardiac arrest.1 It is a powerful tool in our arsenal and an extension of our assessment in delivering holistic patient care.
FUSIC findings: Ejection fraction of 45% on eyeballing with preserved left ventricular function and mild apical-septal dyskinesia possibly post CPR. No dilatation of right atrium or right ventricle and distensible inferior vena cava. No pericardial effusion. Bilateral florid B-lines with starry night sky consolidation of the left basal lung. Postpartum uterus with no ascites and bilateral femoral and popliteal veins showed no evidence of thrombus.
References
1. Lichtenstein, D., van Hooland, S., Elbers, P. W. G., & Malbrain, M. L. (2014). Ten good reasons to practice ultrasound in critical care. Anaesthesiology Intensive Therapy, 46(5), 323-335.
2. Honigberg M C, Givertz M M. Peripartum cardiomyopathy BMJ 2019; 364:k5287.
P310
Point of Care Ultrasound Alters Critical Care Rehabilitation Trajectory
The Ultrasound Ninja
Geetha Kayambu and Qamaruzaman Syed
Gani National University Hospital
Abstract
Introduction: Physiotherapists in recent years have embraced bedside ultrasound imaging as a means to utilize real-time imaging as an assessment tool adjunct to chest physiotherapy to deliver targeted rehabilitation.1,2 The translational impact of point of care ultrasound imaging from acute care through hospital discharge in critical care rehabilitation is yet to be investigated. The case study presented highlights how ultrasound imaging helped detect a subtle clinical condition that aided clinical reasoning and returned positive benefits through altering a patient’s journey through the rehabilitation trajectory.
Main Body: Right sided minimally invasive severe mitral valve regurgitation surgery involving the mechanical valve replacement of the mitral valve was undergone by a 44 year old teacher who suffered from known mitral stenosis since childhood. Ejection fraction was 55%-60% and lung function FEV1/FVC was 86% predicted. Intraoperatively, pleural and pericardial adhesions were noted with no pericardial effusion. Upon successful extubation on post-operative Day 1, patient suddenly developed the first episode of shortness of breath in intensive care whilst on room air with a baseline oxygen saturation of 90%, sinus rhythm of 100 beats per minute and turned orthopneic (RR at 30-40 per minute). Ches t X-ray showed Right lower zone collapse consolidation and small basal pleural effusion. A fully functioning right pleural drain was in situ. Aggressive chest physiotherapy twice daily was ordered but chest physiotherapy did not yield sputum with mucolytic and a dry cough and patient remained tachypneic. On post-operative Day 3 intravenous antibiotics was used to treat the lung, however, symptoms persisted. Progression of mobility failed as patient only sat up 45 degrees in bed with shortness of breath limiting functional capacity. In failing response to aggressive chest therapy, bedside ultrasound performed by attending senior physiotherapist to investigate the limitations directly impacting respiratory capacity that was limiting mobility, showed Right lung reduced diaphragmatic movement and minimal lung sliding with a small anterior pleural effusion with compressive atelectasis. B lines were present with consolidative changes throughout mid and lower segments and Left lung showed good lung movement with lung sliding and A lines. It became apparent that free-flowing effusion over the anterior right lung segment was indeed causing the tachypnea due to compressive atelectasis which was conservatively managed. Upon this finding, patient was subsequently discharged to the general ward to continue her rehabilitation.
Conclusion: The ultrasound finding provided some new insight which altered physiotherapy management as residual tachypnea with acceptable saturation (SpO2 88-92%) had to be accounted for in her rehabilitative journey. Exercise progression was moderated to suit the clinical condition with frequent rest breaks, shortness of breath management and expected longer rehabilitation phase prior to discharge. As clinical symptoms gradually improved, she was able to ambulate 60 meters unsupervised with breathing techniques that helped relieve her shortness of breath and was eventually discharged with home advice.
Brief description of ultrasound video: More than meets the rehab eye:The ultrasound video shows the real time “quad sign” of the pleural effusion that took her breath away momentarily.
References
1. Ntoumenopoulos G, Hough J. Diagnostic thoracic ultrasound within critical care. Journal of physiotherapy 2014, 60(2):112.
2. Le Neindre A, Mongodi S, Philippart F, Bouhemad B. Thoracic ultrasound: Potential new tool for physiotherapists in respiratory management. A narrative review. Journal of critical care 2016, 31(1):101-109.