Abstract
Background
Children with obesity at school entry are at increased risk of persistent obesity throughout childhood and adulthood. Little is known about associations with adverse health outcomes with onset during childhood including those affecting the musculoskeletal system. We examined the association between obesity present at school entry and adverse musculoskeletal diagnoses with onset during childhood.
Methods
We searched three electronic databases to identify longitudinal studies published in English between January 2000 and June 2022 assessing associations between obesity measured at school entry (around age 5 years) and musculoskeletal diagnoses made before age 20 years. Two reviewers screened titles, abstracts and full-text using EPPI-Reviewer software. Bias and quality of eligible studies were appraised using The Quality Assessment tool for Observational Cohort and Cross-sectional studies and findings synthesised.
Results
We identified four eligible studies from 291 unique records, three conducted in Spain and one in Scotland. These studies reported on 1 232 895 children (available data: 51.4% boys; none reported ethnic distribution) with study sample sizes ranging from <2000 to 600 000 and length of follow-up from 2 to 13 years. Quantitative synthesis of findings across these four studies was not possible due to differences in outcomes and effect sizes reported. Children with obesity at school entry were more likely to receive diagnoses of slipped capital femoral epiphysis, back pain, fractures and musculoskeletal complaints made in primary care settings. Included studies were assessed as of ‘fair’ to ‘good’ quality.
Conclusion
There is good to fair evidence to suggest children with obesity at school entry are more likely to receive a diagnosis of a musculoskeletal condition during childhood. Further research is needed to replicate these findings in ethnically diverse populations and to investigate whether these are causal associations. The implications of this for children’s mobility and quality of life and future musculoskeletal health warrants further assessment.
Keywords: Obesity, Epidemiology, Health services research
What is known about the subject?
School entry obesity is a marker for persistent obesity in later childhood and adulthood. This is a concern given associations between obesity and adult morbidities.
Previous cross-sectional research suggests that there is an association between obesity and pain and injuries during childhood, although study quality was deemed moderate to low.
Childhood obesity is associated overall with increased healthcare utilisation, but less is known about associations with specific health outcomes including clinically diagnosed musculoskeletal conditions.
What this study adds?
This systematic review of longitudinal evidence furthers our understanding of the temporal relationship between obesity and important musculoskeletal diagnoses occurring during childhood.
Three studies report a dose response relationship between weight status at school entry and slipped capital femoral epiphysis, fractures and back pain in later childhood.
This review highlights that little is known about the association between school entry obesity and musculoskeletal diagnoses with onset during childhood, particularly by ethnic background.
Introduction
Children with obesity are likely to remain obese in adulthood.1 This is of concern, given associations between obesity and a range of adult long-term conditions, including cardiovascular diseases, diabetes, musculoskeletal disorders and cancers.1–5While there is evidence of increased healthcare utilisation by children with obesity,6 there have been few reports of longitudinal associations with specific clinically diagnosed health outcomes with onset during childhood.
Two systematic reviews have previously identified associations between childhood obesity and musculoskeletal outcomes: pain, injuries and fracture7 and pes planus (flat foot) and other foot deformities (table 1).8 These reviews included literature published more than 9 years ago, included mostly cross-sectional evidence and did not specifically focus on obesity at school entry.
Table 1.
Characteristics of existing systematic reviews
| First author | Year | Age range | Sample size | No. of included studies | Study designs | Intervention/exposure | Outcomes reported | Limitations and other comments |
| Paulis7 | 2014 | 0 to 18-year olds | 1 106 675 children in cross-sectional; 2380 in prospective | 40 | 33 cross-sectional, 7 prospective | Any definition of overweight or obesity between ages 0 and 18 years | Musculoskeletal pain, injury or fracture | Included studies are of moderate or low quality. Literature published up to 2013. Conducted bias/quality assessment. Outcome reported during childhood. |
| Stolzman8 | 2015 | 3 to 18-year olds | 835 350 children | 13 | Cross-sectional | Overweight or obesity between ages 3 and 18 years | Pes planus and other foot structure deformities | Only cross-sectional. Literature published up to 2013. No quality/bias assessment. Outcome reported during childhood. |
Therefore, there is considerable scope for updating these reviews to include more recently published literature. To date, the lack of longitudinal evidence has left the temporal relationship between exposure and outcome difficult to ascertain. Furthermore, existing reviews have not consistently conducted quality assessments, and those that have often report their findings are based on poor or moderate quality evidence. Given the limited evidence, there is scope for undertaking a systematic review to better understand the relationship between obesity and adverse childhood musculoskeletal health.
This review focuses on outcomes for children with obesity at school entry (approximately age 5 years) as it has been shown that obesity at this age is a marker for persistent obesity during later childhood, adolescence9 and adulthood.10 In England 14.9% of children start primary school with obesity, although this proportion is higher among children from some Black and South Asian ethnic backgrounds.11 Given the increased risks of adverse health outcomes associated with obesity among children from these ethnic backgrounds,12–16 it is particularly important to explore important clinical diagnoses associated with obesity measured at school entry, to improve our understanding of the impact of obesity at a young age and allow ample time to intervene and prevent later adverse health diagnoses.
The objective of this systematic review is to assess whether there is an increased risk of diagnosed adverse musculoskeletal health outcomes among children with obesity at school entry. Specifically, the review will address the following research question: are adverse musculoskeletal diagnoses in childhood statistically associated with childhood obesity identified at school entry?
Methods
This review was registered prospectively17 and conducted and reported in accordance with PRISMA guidelines.18 In June 2022, an electronic search was conducted in three databases: PubMed, EMBASE and Web of Science. Articles published between January 2000 and June 2022 and published in English were included.
An adapted population, intervention, comparison, outcome (PICO) framework was used to guide the search strategy (table 2). The search strategy addressed the PICO components and study eligibility criteria using text-word searching of titles and abstracts and subject headings. Of note was the exclusion of studies catalogued under the ‘Adult’ subject heading. Search strategies are shown in online supplementary material.
Table 2.
Search strategy
| PICO | Description |
| Population | Children aged five to 19 years (inclusive) |
| Intervention (exposure) | Children with obesity measured at school entry (approximately age 5 years) |
| Comparator | Children with a healthy weight at school entry (approximately age 5 years) |
| Outcome | Any self-reported, parent-reported, objectively measured or clinical diagnosis of an adverse musculoskeletal health outcome between the ages of 5 and 20 years, found to be statistically associated with the exposure. |
bmjpo-2022-001528supp001.pdf (92.8KB, pdf)
EPPI-Reviewer software19 was used to manage literature and decision-making. Duplicate records were identified using EPPI-Reviewer’s automated algorithm and a similarity threshold of 0.95 to automatically assign records as duplicates.20 The remaining suspected duplicate records were reviewed manually. Titles and abstracts of studies retrieved from running the search strategy, from searching the reference lists of eligible studies, and included in systematic reviews identified in the search strategy, were screened independently against the exclusion criteria by two reviewers (NF and MW) (Box 1).
Box 1. Eligibility criteria.
Exclusion criteria
Not published in English.
Not a research article.
Published before 2000.
Exposure is not obesity at measured at school entry (approximately age 5 years).
Outcome is not before age 20 years.
Outcome is not a musculoskeletal diagnosis.
Study is not longitudinal.
Study is not quantitative.
MW screened titles and abstracts of a random 10% sample of search results. Full-text review was conducted by NF and MW reviewed a random 33% sample of results against the same exclusion criteria. Any conflicting decisions at either screening stage were resolved through discussion. Inter-rater concordance on eligibility was assessed using the unweighted Cohen’s kappa statistic and associated 95% CI (ranges between 0 and 1, with higher values indicating higher observed agreement of raters than that expected by chance).21NF extracted data using a custom template, extracting: full citation, setting, sample size, age-range, definition of obesity, outcome measures and results. MW independently reviewed the data extraction table.
The Quality Assessment tool for Observational Cohort and Cross-sectional studies by the National Heart, Lung and Blood Institute was used to conduct a quality and risk of bias assessment.22 This tool was used because it is specifically designed to aid the appraisal of internal validity of cross-sectional, cohort/longitudinal and case–control studies, as opposed to trials. This tool rates study quality along 14 criteria, with three possible outcomes for each question: ‘Yes’, ‘No’ and ‘Cannot determine/Not reported/Not applicable’. Each study was rated ‘Good’, ‘Fair’ or ‘Poor’ based on the number of criteria assigned a ‘Yes’ outcome, where a ‘Good’ study (with 10 or more ‘Yes’ responses) was considered to have the least risk of bias, ‘Fair’ (with 7–9 ‘Yes’ responses) was susceptible to some bias, and ‘Poor’ indicated a high risk of bias (fewer than seven ‘Yes’ responses).
Due to the range of clinical diagnoses and measures of effect reported, a decision was made to summarise the findings of the included studies narratively. A narrative synthesis was developed to explain the impact of weight status on all the reported clinical diagnoses, identifying similarities and differences in results, and commenting on comparability of study samples, definitions of measurements and methods used. Where possible, effect estimates will be presented in graphical form. Where data were presented, differences in the presence of adverse diagnoses by sociodemographic characteristics were explored.
Results
Study selection
After title and abstract screening, 24 of 291 non-duplicate records remained (figure 1). On screening full-texts, 22 records were excluded (see online supplementary material). The most common reason for exclusion was that the exposure was not obesity measured at school entry. No further eligible references were identified from searching the bibliographies of included studies, or included in systematic reviews identified via the search strategy. Overall, four eligible records were included in this review,23–26 including two studies not identified by the search strategy.25 26
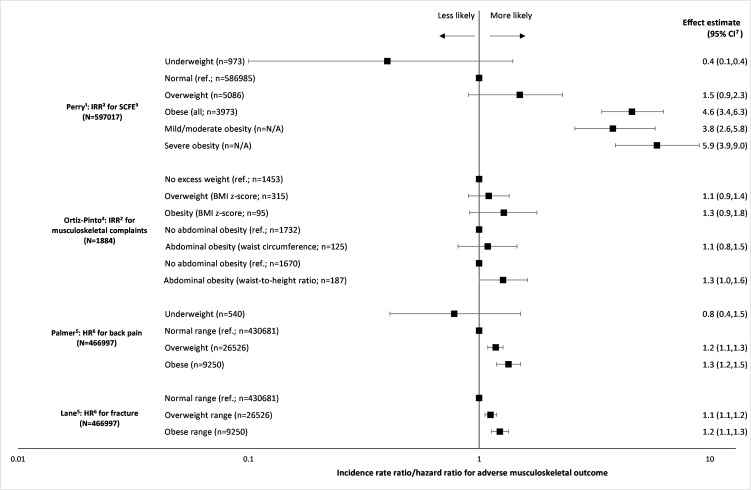
Figure 1 –
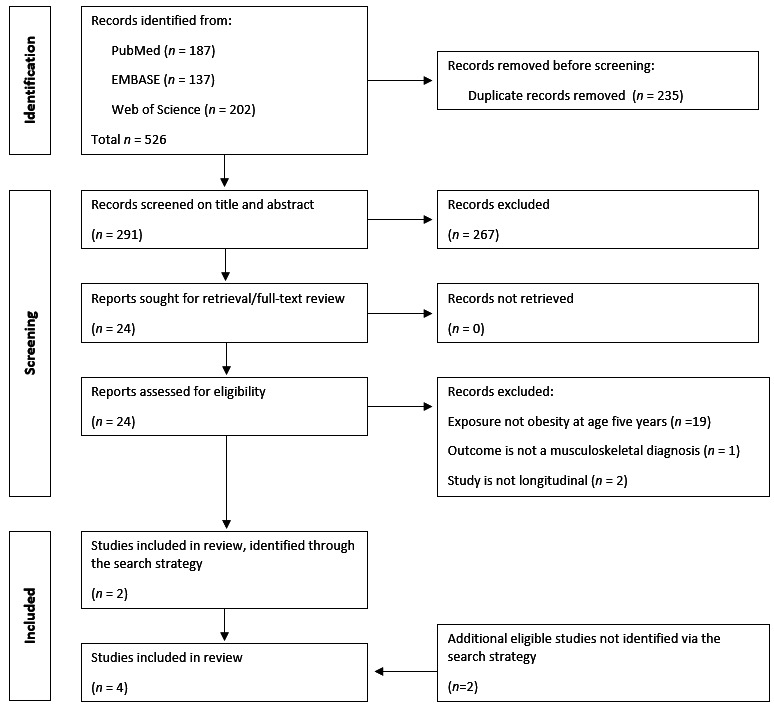
Study selection
MW screened 30 records at the title and abstract screening stage. The inter-rater Cohen’s kappa statistic for inclusion eligibility was 0.33 (95% CI: −0.15 to 0.81). MW screened eight records at the full-text screening stage.
Study characteristics and quality and risk of bias assessment
Three studies were conducted in Spain,24–26 and one in Scotland23 (table 3). One study analysed data collected as part of an established cohort study,24 while the others made use of routinely collected health records. A total of 1 232 895 children were included in the four studies, with sample sizes ranging from 1844 children24 to almost 600 000,23 and follow-up from 224 to 13 years.23 Of the studies reporting their study sample sex distribution, 51.4% of the sample were male. None of the included studies report the ethnic background of their respective study samples.
Table 3.
Study characteristics
| Setting | Sample size | Sample age range | Definition of obesity | Outcome measure and covariates | Results |
| Perry DC et al. 33 | |||||
| Scotland | 597 017 children (distribution by sex and ethnic background unreported) |
Age 5–6 to 18 years, diagnosis of SCFE or censor date (December 2016) | Age-specific and sex-specific BMI standardised to UK90 reference population Underweight <5th percentile, overweight ≥85th percentile, obese ≥95th percentile Mild/moderate obesity ≥95th–99th percentile, severe obesity ≥99th percentile |
Diagnostic record of SCFE (ICD10 M93.0 or ICD9 732.2) in linked hospital admission records Covariates included in adjusted model: age, sex, quintile of SES deprivation |
Adjusted IRR for SCFE was: 5.9 (3.9, 9.0) among those with severe obesity, 3.8 (2.6, 5.8) among those with mild/moderate obesity, 1.5 (0.9, 2.3) among those with overweight |
| Ortiz-Pinto MA et al.34 | |||||
| Madrid, Spain | 1884 children (50.8% male; distribution by ethnic background unreported) |
Age 4 to 6 years | Age-specific and sex-specific BMI standardised to WHO 2006 reference tables Overweight z-BMI >+1 SD and ≤+2 SD, obese z-BMI >+2 SD Abdominal obesity based on waist-to-height ratio was defined as ≥90 th percentile Abdominal obesity based on waist circumference defined as ≥90 th percentile reference tables by Fernandez et al 33 |
Visits to doctor offices relating to musculoskeletal system coded using International Classification of Primary Care −2 Classification Covariates included in adjusted model: -sex, age, maternal educational level, familial purchasing power, time breastfeeding, perceived health status at age 4 years |
Adjusted IRR for musculoskeletal complaints: 1.3 (1.0,1.6) among children with abdominal obesity based on waist-to-height ratio, compared with children with no abdominal obesity Adjusted IRR for musculoskeletal complaints among children with obesity: 1.3 (0.9,1.8) and with overweight (1.1; 0.9,1.4) based on z-BMI as indicator of obesity |
| Palmer AJ et al.14 | |||||
| Catalonia, Spain | 466,997 children (51.4% male; 89.0% Spanish, 11.0% other nationality) |
Age 4 to 15 years, migration out of area, death or censor date (2016) | Age-specific and sex-specific BMI standardised to WHO 2007 guidance Underweight ≤2 SDs, normal weight −2 to +2, overweight >+2 and obesity >+3 |
Lumbar spine pain (ICD-10: M54.1, M54.3, M54.4, M54.5) thoracic back pain (M54, M54.6, M54.8, M54.9) or cervical spine pain (M54.2) recorded in paediatric primary care clinics Covariates included in adjusted model: age, sex, SES, nationality |
Cumulative incidence of any back pain by weight status: 8.8% (8.5, 9.1) normal weight, 10.1% (8.9, 11.4) overweight, 11.8% (9.4,14.2) obese Univariable HR for back pain: 1.2 (1.1, 1.3) for children with overweight and 1.3 (1.2, 1.5) for those with obesity compared with normal weight Adjusted HR for back pain: 1.2 (1.1, 1.3) for children with overweight and 1.3 (1.2, 1.5) for those with obesity compared with normal weight |
| Lane JCE et al.15 | |||||
| Catalonia, Spain | 466 997 children (51.4% male; 89.0% Spanish, 11.0% other nationality) |
Age 4 to 15 years, migration out of area, death or censor date (2016) | Age-specific and sex-specific BMI standardised to WHO 2007 guidance Underweight ≤2 SDs, normal weight −2 to +2, overweight >+2 and obesity >+3 |
Fractures recorded using Interntional Classification of Diseases-10 codes in primary care Covariates included in the adjusted model: sex, age, socioeconomic status, nationality |
Cumulative incidence for fracture by weight status: 10.1% (9.8, 10.3) normal weight, 11.3% (10.2, 12.4) overweight, 13.1% (10.7, 15.4) obese Univariable HR for fractures: 1.1 (1.1,1.2) for children with overweight and 1.3 (1.2, 1.4) for those with obesity compared with normal weight Adjusted HR for fractures: 1.1 (1.1, 1.2) among children with overweight and 1.2 (1.1, 1.3) among children with obesity compared with normal weight children |
BMI, body mass index; IRR, incidence rate ratios; SCFE, slipped capital femoral epiphysis.
Three studies defined obesity based on BMI SD score (SDS),24–26 one of which used the WHO age-specific and sex-specific growth standards to define obesity as BMI z-score ≥2 SDS,24 while two employed a higher threshold of ≥3 SDS.25 26 The remaining study defined obesity using age-specific and sex-specific BMI criteria recognised by both the UK 1990 (UK90) and the Centers for Disease Control and Prevention, defining obesity as BMI greater than or equal to the 95th percentile,23 and also stratified obesity into mild/moderate (≥95th–<99th percentile) and severe (≥99th percentile). One study included two other obesity indicators: waist-to-height ratio ≥ 90th percentile and waist circumference ≥ 90th percentile.24
Four different outcomes were reported: slipped capital femoral epiphysis (SCFE; a disease of the growth plate, whereby the femoral head of the thighbone slips through the physis),23 back pain,25 fractures26 and GP consultations for musculoskeletal complaints.24 The outcomes were presented as incidence rate ratios (IRR)23 24 and HR.25 26
Two studies were rated ‘good’25 26 and one as ‘fair’23 24 in the quality assessment tool (table 4). All but one study23 clearly defined the study population such that the study could be replicated. The participation rate could not be determined in one study,25 and rate of loss to follow-up could not be determined in two.24 26All studies adjusted for potential confounding variables.
Table 4.
Risk of bias/quality assessment
| Criteria (yes, no, cannot determine (CD), not applicable (NA) | Perry23 | Ortiz-Pinto24 | Palmer25 | Lane26 |
| 1.1. Was the research question or objective in this paper clearly stated? | Yes | Yes | Yes | Yes |
| 2.2. Was the study population clearly specified and defined? | No | Yes | Yes | Yes |
| 3.3. Was the participation rate of eligible persons at least 50%? | Yes | Yes | CD | Yes |
| 4.4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? | Yes | Yes | Yes | Yes |
| 5.5. Was a sample size justification, power description, or variance and effect estimates provided? | No | No | No | No |
| 6.6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? | Yes | Yes | Yes | Yes |
| 7.7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? | Yes | No | Yes | Yes |
| 8.8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (eg, categories of exposure, or exposure measured as continuous variable)? | Yes | Yes | Yes | Yes |
| 9.9. Were the exposure measures (independent variables) clearly defined, valid, reliable and implemented consistently across all study participants? | No | Yes | Yes | Yes |
| 10.10. Was the exposure(s) assessed more than once over time? | No | No | No | No |
| 11.11. Were the outcome measures (dependent variables) clearly defined, valid, reliable and implemented consistently across all study participants? | Yes | No | Yes | Yes |
| 12.12. Were the outcome assessors blinded to the exposure status of participants? | NA | NA | NA | NA |
| 13.13. Was loss to follow-up after baseline 20% or less? | Yes | CD | Yes | CD |
| 14.14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? | Yes | Yes | Yes | Yes |
| NF rating (good, fair or poor) | Good | Fair | Good | Good |
| MW rating (good, fair or poor) | Fair | Good | Good | Good |
| Overall rating (good, fair or poor) | Fair | Fair | Good | Good |
| Additional comments (if poor, state why) | BMI measurement protocol lacked detail | Short follow-up No codes specified for identification of primary care events Unable to determine loss to follow-up |
Unable to determine participation rate | Unable to determine loss to follow-up |
BMI, body mass index; CD, cannot determine; NA, not applicable.
Obesity and slipped capital femoral epiphysis
Perry found that, compared with children with a healthy weight, the IRR for SCFE was 5.9 (95% CI: 3.9 to 9.0) among children with severe obesity and 3.8 (95% CI: 2.6 to 5.8) among those with mild/moderate obesity at age 5 years (figure 2).
Figure 2 –
Forrest plot of incident rate ratios and HRs (and 95% CIs) for adverse musculoskeletal outcome of interest, by weight status. This graph uses weight status terms employed by the study authors.1 Perry et al defined obesity using age-specific and sex-specific body mass index criteria of the Centers for Disease Control and Prevention, defining obesity as BMI greater than or equal to the 95th percentile, and further stratified obesity into mild/moderate (≥95th–<99th percentile) and severe (99th percentile). Sample size in the mild/moderate and severe obesity groups were not reported.2 Incident rate ratio.3 Slipped capital femoral epiphysis.4 Ortiz-Pinto et al defined obesity based on body mass index SD) score using WHO age-specific and sex-specific growth standards to define obesity as body mass index z-score ≥2SD scores. Abdominal obesity was defined as waist circumference ≥90th percentile and waist-to-height ratio ≥ 90th percentile, as recommended by the International Diabetes Federation.5 Palmer et al and Lane et al defined obesity based on body mass index SD score using WHO age-specific and sex-specific growth standards to define obesity as body mass index z-score ≥3SD scores.6 HR.7 95% CI.
Obesity and back pain
Palmer reported that the cumulative incidence of any back pain was higher among children with obesity (11.83%; 95% CI: 9.43 to 14.24) compared with children with a healthy weight (8.78%; 95% CI: 8.4 5 to 9.12; figure 2). In multivariable analyses, the HR was 1.34 (95% CI: 1.19 to 1.51) among children with obesity compared with children with a healthy weight.
Obesity and fracture
Lane found that the cumulative incidence of fracture was higher among children with obesity (13.05%; 95% CI: 10.69 to 15.41) compared with children with a healthy weight (10.06%; 95% CI: 9.82 to 10.29; figure 2). In multivariable analyses, the HR was 1.23 (95% CI: 1.13 to 1.34) among children with obesity compared with children with a healthy weight.
Obesity and musculoskeletal consultations
Ortiz-Pinto reported that children with abdominal obesity based on waist-to-height ratio had an increased incidence of musculoskeletal problems (IRR: 1.27; 95% CI: 1.00 to 1.62), compared with children with no abdominal obesity (figure 2), but found no association when using waist circumference alone (IRR: 1.09; 95% CI: 0.81 to 1.46). The incidence of musculoskeletal problems was higher in children with overweight (IRR: 1.10; 95% CI: 0.90 to 1.35) or obesity (IRR: 1.28; 95% CI: 0.91 to 1.78) relative to those with no excess weight as assessed by BMI.
Discussion
Key findings
This systematic review identified four eligible studies out of 291 retrieved studies. These studies have provided evidence in support of an association between obesity identified in children at school entry and adverse musculoskeletal diagnoses. The evidence was of fair or good quality.
The small number of studies meeting the eligibility criteria investigated four outcomes: SCFE, back pain, fractures and musculoskeletal complaints in general. While other outcomes may be of interest, for example pes planus or genu valgum, no studies reporting these outcomes were identified. All studies were longitudinal, strengthening the evidence that obesity may be on the causal pathway to these adverse diagnoses.
This temporal relationship, combined with the magnitude of the effect sizes reported and the dose response relationship noted in three out of four of the included studies, contribute to a body of evidence in support of a association between obesity measured at school entry and later adverse musculoskeletal outcomes.
All studies adjusted for confounding variables in their analyses, such as age, sex and SES, but none reported ethnic background.
Narrative synthesis
The finding of an increased likelihood of adverse musculoskeletal diagnoses among children with obesity support the results of Paulis and coauthors’ review of musculoskeletal complaints which concluded, based on 40 predominantly cross-sectional studies of low and moderate quality, that overweight and obesity are associated with lower back pain, injuries and fractures.7 In particular, Palmer et al’s findings support these earlier conclusions, although differences in the reported prevalence of back pain may result from Palmer’s use of electronic health records which only considers those who have received clinical diagnosis, rather than self-report/parent-report in observational studies.
In contrast to findings from a longitudinal cohort of children in the Netherlands,27 Ortiz-Pinto reports that obesity is associated with greater demand for primary care services. It is possible these conflicting findings result from differences in the code specification used to identify musculoskeletal complaints in primary care. Other longitudinal evidence suggests a link between musculoskeletal hospitalisations among children with obesity in the preschool period,28 however Ortiz-Pinto does not present data on accident and emergency (A&E) attendances. Inclusion of A&E data and stratification by healthcare use, as they were able to do for primary care, would have increased this study’s contribution to our understanding of the relationship between school entry obesity and musculoskeletal diagnoses, particularly given that A&E may be the likely destination for children suffering fractures.
While the included studies each contributed somewhat to understanding associations between sociodemographic factors (namely sex, SES and nationality) and adverse musculoskeletal outcomes, none of the studies stratified analyses or included interaction terms between these sociodemographic factors and weight status to enable more granular interpretation of associations between obesity and adverse musculoskeletal diagnoses. Of particular importance is the omission of ethnic background in all four of the studies, first in reporting the ethnic distribution of their study samples, and second in accounting for ethnic background in their analyses. Given the longstanding associations between obesity and ethnic background, as well as the increased likelihood of some adverse health conditions among children from particular ethnic backgrounds, exploring the risk of musculoskeletal diagnoses by weight status and ethnic background would be very valuable.
Strengths and limitations
Fewer than 2% of the search results were eligible against the screening criteria. It was not possible to specify the temporality of the relationship between exposure and outcome in the search strategy, and consequently a large proportion of studies were excluded because obesity was the outcome of interest, as opposed to the exposure.
This limitation was addressed in the screening process, to ensure only studies which investigated childhood obesity at school entry as the exposure, with later diagnosis of a musculoskeletal condition as the outcome, were included. Consequently, it is possible to comment on the causality of the association between obesity at school entry and musculoskeletal outcomes.
The quality of included studies was assessed using a tool designed specifically to assess the presence of bias in cross-sectional, cohort and case–control studies. While not independently standardised, it has some features specifically designed for cohort studies as included in this systematic review.
The review included two studies identified via NF’s routine weekly search of PubMed for literature relating to childhood obesity and electronic health records. These records were not identified via the search strategy. Palmer’s study was not identified because it has ‘Adult’ as one of it’s MeSH terms. Records with this MeSH were excluded from the search strategy to limit literature to those exploring outcomes during childhood. Lane’s study was not identified because it does not include the musculoskeletal terms of the search strategy. The inclusion of these studies has been recorded transparently. Despite attempting to employ a maximally sensitive search strategy, missing studies will always be a limitation of systematic reviews.
Interpretation and implications
The studies indicate an association between obesity and SCFE, fractures and back pain, although few studies were identified and the heterogeneity of studies precluded pooled quantification of the risks of specific diagnoses. These findings are supported by an assessment of either ‘Fair’ or ‘Good’ quality suggesting that they are either susceptible to ‘some bias’ or considered to have the ‘least risk of bias’, respectively.22 A particular strength of the included studies is their longitudinal design, ensuring that the exposure of interest was measured before the outcome, strengthening our understanding of the causal relationship between obesity and adverse musculoskeletal outcomes. Despite this, given the paucity of longitudinal evidence identified in this review, the heterogeneity in study design and outcomes reported and inability to quantify risk, there is insufficient evidence to conclude that there is an increased risk of adverse musculoskeletal outcomes among children with obesity.
The relationship between obesity at school entry and adverse musculoskeletal diagnoses during childhood is important for two reasons. First, around one in six children in England enter primary school with obesity,11 and second, this review has highlighted the impact of obesity on the developing musculoskeletal system at a time when there is potential to intervene and reverse or mitigate the effects of obesity. Perry et al found a very high risk of SCFE among children with severe obesity at age 11–12 years (OR: 17.0; 95% CI: 5.9 to 49.0) compared with children with a healthy weight at this age.
This review adds to evidence about the adverse health consequences of obesity at school entry and the importance of prevention of obesity and support for effective weight management among children with severe obesity. Many of these outcomes impact quality of life and, in the case of SCFE, require surgical intervention with potential longer term adverse hip outcomes in adult life. Early recognition of SCFE is critical because the disease has the potential to progress if the condition remains untreated.29
This review has identified several evidence gaps, in particular how associations between obesity measured at school entry and adverse musculoskeletal diagnoses vary by ethnic background. The study samples included in this review lack ethnic diversity which precluded stratification of analyses by ethnic background. Given the longstanding inequalities in obesity prevalence by ethnic background, SES and sex,30–32 additional analyses investigating these interactions in relation to adverse musculoskeletal outcomes during childhood are critical to better serve children at risk.
Conclusion
In summary, this review suggests that children with obesity at school entry are more likely to experience back pain, SCFE or fractures during childhood. The strength of this evidence is low due to the small number of eligible studies included in this review and their overall quality. The small number of studies investigating this research question, with varying study designs, definitions used, outcomes examined and effect sizes reported precluded quantitative synthesis to estimate the risk of adverse musculoskeletal clinical diagnoses among children with obesity. Information on whether the strength of these associations varies by sex and ethnic background is lacking.
Supplementary Material
Footnotes
Contributors: CD obtained funding for the study. In consultation with CD and GH, NF conceptualised and designed the review. NF carried out the literature search, managed the screening process, synthesised the results, generated tables and figures and drafted the initial manuscript. MW independently screened a random sample of records at both the title and abstract and full-text screening stages, completed independent bias/quality assessment for eligible studies and reviewed the data extraction table. All authors contributed to the interpretation of analyses and reviewed and revised the manuscript. All authors were involved in writing the paper and had final approval of the submitted and published manuscript. NF is the guarantor and accepts full responsibility for the conduct of the study, had access to the data, and controlled the decision to publish. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This research was funded by a grant from Barts Charity ref: MGU0419
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Not applicable.
References
- 1. World Health Organization . Obesity and overweight. World Health organization,. fact sheets web site, 2021. Available: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight [Accessed August 2021].
- 2. Li S, Chen W, Srinivasan SR, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa heart study. JAMA 2003;290:2271–6. 10.1001/jama.290.17.2271 [DOI] [PubMed] [Google Scholar]
- 3. Butterworth PA, Landorf KB, Smith SE, et al. The association between body mass index and musculoskeletal foot disorders: a systematic review. Obes Rev 2012;13:630–42. 10.1111/j.1467-789X.2012.00996.x [DOI] [PubMed] [Google Scholar]
- 4. Andorsen OF, Ahmed LA, Emaus N, et al. A prospective cohort study on risk factors of musculoskeletal complaints (pain and/or stiffness) in a general population. The Tromsø study. PLoS One 2017;12:e0181417. 10.1371/journal.pone.0181417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bikbov MM, Kazakbaeva GM, Zainullin RM, et al. Prevalence of and factors associated with low back pain, thoracic spine pain and neck pain in Bashkortostan, Russia: the Ural eye and medical study. BMC Musculoskelet Disord 2020;21:64. 10.1186/s12891-020-3080-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hasan T, Ainscough TS, West J, et al. Healthcare utilisation in overweight and obese children: a systematic review and meta-analysis. BMJ Open 2020;10:e035676. 10.1136/bmjopen-2019-035676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paulis WD, Silva S, Koes BW, et al. Overweight and obesity are associated with musculoskeletal complaints as early as childhood: a systematic review. Obes Rev 2014;15:52–67. 10.1111/obr.12067 [DOI] [PubMed] [Google Scholar]
- 8. Stolzman S, Irby MB, Callahan AB, et al. Pes planus and paediatric obesity: a systematic review of the literature. Clin Obes 2015;5:52–9. 10.1111/cob.12091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. England PH. Changes in the weight status of children between the first and final years of primary school. A longitudinal analysis of data from the National Child Measurement Programme in four local authorities in England between 2006/07 and 2014/15, 2017. [Google Scholar]
- 10. Singh AS, Mulder C, Twisk JWR, et al. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008;9:474–88. 10.1111/j.1467-789X.2008.00475.x [DOI] [PubMed] [Google Scholar]
- 11. Digital NHS. National child measurement programme, England 2020/21 school year, 2021. Available: https://digital.nhs.uk/data-and-information/publications/statistical/national-child-measurement-programme/2020-21-school-year [Accessed Dec 2021].
- 12. Nightingale CM, Rudnicka AR, Owen CG, et al. Influence of adiposity on insulin resistance and glycemia markers among U.K. children of South Asian, black African-Caribbean, and white European origin: child heart and health study in England. Diabetes Care 2013;36:1712–9. 10.2337/dc12-1726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. NHS Digital . Health survey for England 2004: the health of ethnic minorities. NHS digital, 2006. Available: https://digital.nhs.uk/catalogue/PUB01209 [Accessed Jan 2018].
- 14. Candler TP, Mahmoud O, Lynn RM, et al. Continuing rise of type 2 diabetes incidence in children and young people in the UK. Diabet Med 2018;35:737–44. 10.1111/dme.13609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Whincup PH, Gilg JA, Papacosta O, et al. Early evidence of ethnic differences in cardiovascular risk: cross sectional comparison of British South Asian and white children. BMJ 2002;324:635. 10.1136/bmj.324.7338.635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Whincup PH, Nightingale CM, Owen CG, et al. Early emergence of ethnic differences in type 2 diabetes precursors in the UK: the child heart and health study in England (Chase study). PLoS Med 2010;7:e1000263. 10.1371/journal.pmed.1000263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Firman N, Wilk M, Harper G, et al. The childhood cardiometabolic and musculoskeletal health outcomes of obesity present at age five years: a systematic review of longitudinal evidence. In. PROSPERO 2021. [Google Scholar]
- 18. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. UCL Social Research Institute . EPPI-Reviewer: advanced software for systematic reviews, maps and evidence synthesis [computer program. London: UCL Social Research Institute, 2020. [Google Scholar]
- 20. EPPI-Reviewer . About > Features >EPPI-Reviewer 4: software for research synthesis. Social Science Research Unit, UCL Institute of Education, 2021. Available: https://eppi.ioe.ac.uk/cms/Default.aspx?tabid=3396 [Accessed Sep 2021].
- 21. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med 2012;22:276–82. 10.11613/BM.2012.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. National Heart Lung and Blood Institute . Study quality assessment tools: quality assessment tool for observational cohort and cross-sectional studies, 2021.. Available: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools [Accessed June 2021].
- 23. Perry DC, Metcalfe D, Lane S, et al. Childhood obesity and slipped capital femoral epiphysis. Pediatrics 2018;142:e20181067. 10.1542/peds.2018-1067 [DOI] [PubMed] [Google Scholar]
- 24. Ortiz-Pinto MA, Ortiz-Marrón H, Esteban-Vasallo MD, et al. Demand for health services and drug prescriptions among overweight or obese preschool children. Arch Dis Child 2020;105:292–7. 10.1136/archdischild-2019-316895 [DOI] [PubMed] [Google Scholar]
- 25. Palmer AJ, Poveda JL, Martinez-Laguna D, et al. Childhood overweight and obesity and back pain risk: a cohort study of 466 997 children. BMJ Open 2020;10:e036023. 10.1136/bmjopen-2019-036023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lane JC, Butler KL, Poveda-Marina JL, et al. Preschool Obesity Is Associated With an Increased Risk of Childhood Fracture: A Longitudinal Cohort Study of 466,997 Children and Up to 11 Years of Follow-up in Catalonia, Spain. J Bone Miner Res 2020;35:1022–30. 10.1002/jbmr.3984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van Leeuwen J, van Middelkoop M, Paulis WD, et al. Overweight and obese children do not consult their general practitioner more often than normal weight children for musculoskeletal complaints during a 2-year follow-up. Arch Dis Child 2018;103:149–54. 10.1136/archdischild-2017-313118 [DOI] [PubMed] [Google Scholar]
- 28. Hayes A, Chevalier A, D'Souza M, et al. Early childhood obesity: association with healthcare expenditure in Australia. Obesity 2016;24:1752–8. 10.1002/oby.21544 [DOI] [PubMed] [Google Scholar]
- 29. Kocher MS, Bishop JA, Weed B, et al. Delay in diagnosis of slipped capital femoral epiphysis. Pediatrics 2004;113:e322–5. 10.1542/peds.113.4.e322 [DOI] [PubMed] [Google Scholar]
- 30. Pearce A, Rougeaux E, Law C. Disadvantaged children at greater relative risk of thinness (as well as obesity): a secondary data analysis of the England national child measurement programme and the UK millennium cohort study. Int J Equity Health 2015;14:61. 10.1186/s12939-015-0187-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hudda MT, Nightingale CM, Donin AS, et al. Patterns of childhood body mass index (BMI), overweight and obesity in South Asian and black participants in the English National child measurement programme: effect of applying BMI adjustments standardising for ethnic differences in BMI-body fatness associations. Int J Obes 2018;42:662–70. 10.1038/ijo.2017.272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Strugnell C, Mathrani S, Sollars L, et al. Variation in the Socioeconomic Gradient of Obesity by Ethnicity - England's National Child Measurement Programme. Obesity 2020;28:1951–63. 10.1002/oby.22970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fernández JR, Redden DT, Pietrobelli A, Allison DB, et al. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr 2004;145:439–44. 10.1016/j.jpeds.2004.06.044 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjpo-2022-001528supp001.pdf (92.8KB, pdf)
Data Availability Statement
No data are available.