Abstract
Objectives:
Fat embolism and fat embolism syndrome (FES) remain common complications following long bone fractures. Incidence is highest after bilateral femur fractures. We performed a systematic review of FES after bilateral femur fractures and present two cases.
Data sources:
Systematic literature search of the Cochrane, EMBASE, MEDLINE, Scopus, and, Web of Science Library databases was performed in August 2021. Terms used including plural and alternate spellings: “fat embolism,”“fat embolism syndrome,”“fat embolus,” and “bilateral femur fracture.” Articles in German and English were considered. No time frame was applied.
Study selection:
Original studies, case series and case reports on fat embolism after bilateral femur fracture were included. Insufficient documentation or patients with relevant previous heath conditions were excluded.
Data extraction:
Abstracts were organized using EndNote X9 by Carivate. Three authors independently screened the abstracts; cross check of the extracted data was performed by the senior author.
Data synthesis:
Scarcity of articles only allowed for a qualitative synthesis. Data was compared with our cases and situated within the scientific background.
Results:
Ten articles were included for qualitative synthesis (n = 144 patients). The symptoms were inhomogeneous with neurological deficits being most prominent. Degree of displacement was high, when reported. Although the modes and timing of surgery varied, this appeared unrelated with outcome.
Conclusions:
FES remains a relevant complication after bilateral femur fractures, despite damage control strategies and improved reaming techniques. Fracture displacement and reduction maneuvers might play a more substantial role in the formation than previously accredited.
Level of evidence:
4
Keywords: bilateral femur fracture, fat embolism, fat embolism syndrome, femur fracture, long bone fracture, trauma
1. Introduction
Fat embolism is an ongoing clinical problem in patients with acute trauma and long bone fractures.[1] It is mainly caused by intravasation of bone marrow fat and often occurs during/after intramedullary reaming and nailing in diaphyseal femur fractures.[2]
Symptoms of fat embolism differ in severity and expression depending on the location of embolization, with the lung and the brain being the most vulnerable organs.[3] Before fat embolism was identified as caused by unstabilized fractures, the diagnosis was difficult to make and the direct proof of fat droplets by ophthalmoscopy was required. Along with better understanding of the pathophysiology, it became evident, that fat can affect the function of other organs. This led to a change in terminology and a full-blown systemic manifestation was defined as fat embolism syndrome (FES).[4] Radiographically, FES can be diagnosed through ground glass opacities and thickened interlobular septa in a computed tomography-thorax[5] and in the brain by ischemic microlesions in magnetic resonance imaging.[6]
Meek et al proved in an elegant study as early as 1972 that fat globules can be found in the femoral vein after femur fractures.[7] Further studies then suggested that multiple reaming steps, or a difficult reduction are of utmost significance in the development of fat embolism, as all these maneuvers lead to intravasation of intramedullary contents.[8–13] Heat generation and osteonecrosis also occurred with early reamer designs, but have been mitigated by changes in reaming technique and reamer design.[14,15] Further focus was laid on the intramedullary pressure increases during reaming as a factor of acute embolization,[16] and that multiple reaming steps can cause a piston effect.[16] Although similar pressure increases may be achievable by a single pass reaming or unreamed nailing[17], the sum of reaming steps induces a higher volume of fat intravasation, just by repeated piston effects.[18] Intraoperative transesophageal echocardiography proved that solid contents are transported into the lung[19] and the initial fatty thrombus is surrounded by platelet aggregation during the passage through the venous system.[20] These changes are accompanied by pulmonary artery pressure increases during reaming.[21] Further studies also proved the influence of the reamer head architecture.[22]
Our group recently hypothesized that the clinical problem of FES has changed along with techniques of ventilation, resuscitation and the technical aspects of reaming.[23] Interestingly, the incidence of FES has decreased from almost 8% to close to 2% since its initial description, especially after the year 2000.[23] Pathological fractures were associated with a higher incidence of FES when compared with traumatic fractures and bilateral fractures (traumatic and pathological) were associated with a higher incidence of FES than unilateral fractures.[23] It is unclear from the literature however, if the reaming alone, the degree of fracture displacement or fat intravasation during reduction play a role and which factor is most relevant.
We, therefore, performed a systematic literature review of bilateral femur fractures and fat embolism that focuses on these particular issues. In addition, we present 2 almost identical cases that developed postoperative FES despite the absence of particular risk factors and review the possible underlying pathophysiological causes.
2. Methods
2.1. Part I: systematic literature review
2.1.1. Methods
We conducted a systematic literature review, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.[24] The aim was to identify all publications regarding fat embolism (syndrome) after bilateral femur fractures. A systematic literature search of the Cochrane, EMBASE, MEDLINE, Scopus, and Web of Science Library databases was conducted in August 2021. The terms used were: “fat embolism,” “fat embolism syndrome,”“fat embolus,” and “bilateral femur fracture,” as well as plural forms and alternate spellings. Terms were truncated and connected by Boolean operators.
Additionally, we screened the references lists of selected studies and of related systematic reviews, to identify any relevant studies missed by the electronic search.
Search results were extracted and documented using EndNote X9 by Carivate. Articles were then de-duplicated and screened independently by 3 authors (YKA, TS, and YKU). A cross check of the extracted data was performed by the senior author (HP). Any disagreement was resolved by a consensus discussion in personal meetings.
2.1.2. Inclusion/exclusion criteria
Due to the scarcity of reports on the matter, we included original studies as well as case reports on a healthy adult trauma population with bilateral femur fractures, if they included the diagnoses “fat embolism” or “fat embolism syndrome.” Studies should be reported in English or German and describe trauma mechanism, means of fracture fixation and describe symptoms, complications, or mortality. Reviews, letters, commentaries, correspondences, conference abstracts, expert opinions, editorials, in vitro, and animal experiments were excluded. Further exclusion criteria were insufficient documentation or patients with relevant previous heath conditions (ie, oncological, neurological, or pulmonary diagnoses).
2.2. Part II: case reports with fat embolism after bilateral femur fracture
We review 2 cases of bilateral femur fractures that—in the absence of cofactors—developed postoperative FES and required prolonged artificial ventilation. Case 1 was treated by bilateral closed reduction and external fixation while Case II was treated by retrograde nailing. Their clinical course is described in the Appendix.
3. Results
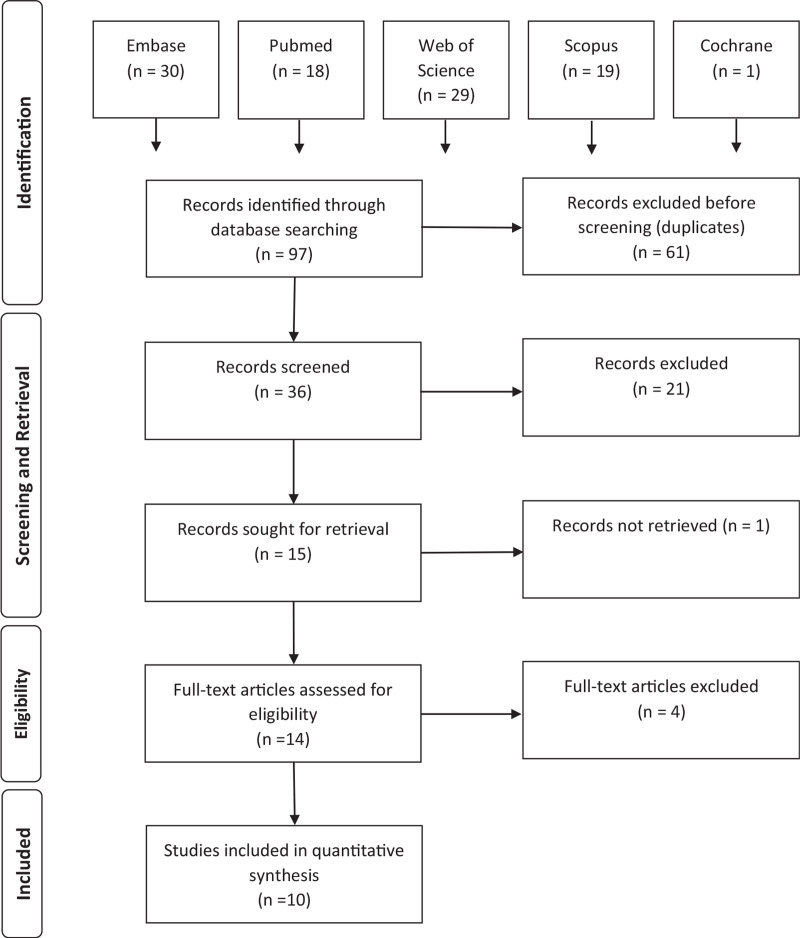
Our search yielded 36 articles after the removal of duplicates. Following initial screening of title and abstract, 14 full text articles were retrieved and assessed for eligibility. Of these, ten met our criteria and were thus included. A flowchart illustrating the selection process can be seen in Figure 1. Out of the 10 remaining articles, 2 were retrospective cohort studies. Therefore, our review includes 129 patients with bilateral femur fractures that were all treated with reamed antegrade[25]—or retrograde nailing.[26] Out of these, 6 developed FES, yet only little information was provided on concomitant chest injury, degree of fracture displacement, time to surgery, or outcome.
Figure 1.
Flowchart illustrating the study selection process.
The remaining 8 articles were case reports/series discussing a total of 15 patients. Mean age was 26years. Trauma mechanism was almost exclusively motor vehicle accidents. Two patients had a reported chest injury (unknown degree) and other relevant concomitant injuries were reported in 11 patients. Preoperative X-rays were presented in 5 of the 8 studies and all showed severe displacement—at least unilaterally. Time to surgery ranged from < 6 hours to > 24 hours. Means of fixation included external fixation, reamed nailing or a combination of the 2. Five of the 8 cases describe neurological worsening as the foremost symptom. Overall, 1 patient suffered complete paraplegia sub thoracic vertebra No 9 due to a spinal embolus and 1 patient died from generalized cerebral edema. All other patients made a full recovery. A synopsis of all data is presented in Table 1.
Table 1.
Synopsis of the included studies.
| Title | Author | Year | Study type | n = | Age | Gender (f/m) | Injury mechanism | Chest injury | Other relevant injuries | Displacement | Time to surgery | Initial operation | Symptoms | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fat embolism due to bilateral femoral fracture: a case report | Porpod¡s et al | 2012 | Case report | 1 | 20 | 0/1 | Car accident | no | n.a. | n.a. | 9 hours | Reamed nailing | NO R1 P1 | Full recovery |
| Case report-cerebral fat metabolism syndrome after bilateral femoral fracture | Wöhler et al | 2013 | Case report | 1 | 20 | 0/1 | Car accident | No | Yes | n.a. | <6 hours | External fixation | N1 R1 P1 | Full recovery |
| Bilateral femoral shaft fractures complicated by fat and pulmonary embolism: a case report | Randelli et al | 2015 | Case report | 1 | 25 | 0/1 | Car accident (pedestrian) | No | No | Yes | > 24 hours | External fixation | N1 R1 PO | Full recovery |
| Fat emboli syndrome and the orthopaedic trauma surgeon: lessons learned and clinical recommendations | Dunn et al | 2017 | Case report | 1 | 18 | 1/0 | Motorcycle accident | No | Yes | Yes | <6 hours | External fixation (left) reamed nailing (right) | N1 RO PO | Full recovery |
| The fat embolism syndrome as a cause of paraplegia | Peters et al | 2018 | Case report | 1 | 19 | 0/1 | Car accident | No | Yes | n.a. | <6 hours | External fixation | N1 R1 P1 | Complete paraplegia subT9 |
| Fatal Cerebral Fat Embolism After Pelvic and Multiple Long Bone Fractures without Associated Lung Injury: A Case Report | Hadden et al | 2020 | Case report | 1 | 29 | 1/0 | Car accident | Yes | Yes | Yes | <6 hours, 48 hours | External fixation - then reamed nailing | N1 RO P1 | Death (generalized cerebral edema) |
| A 21 -year-old Pregnant Trauma Patient with Asymptomatic Fat Embolism; a Case Report | Ayoobi-Yazd¡ et al | 2020 | Case report | 1 | 21 | 1/0 | Car accident | Yes | Yes | Yes | 2nd day | Reamed nailing | NO R1 PO | Full recovery |
| Early intervention v/s delayed Intervention? Dilemma In bilateral shaft femur fractures with evolving features of fat embolism - Damage control nailing | Murthy et al | 2021 | Case serles | 8 | 30 (16–38) | n.a. | Mixed (high energy mechanisms) | n.a. | 6/8 | Yes | 24 to 48 hours | Unreamed nailing | n.a. | Full recovery |
| Risks and results after simultaneous Intramedullary nailing In bilateral femoral fractures: A retrospective study of 40 cases | Bonnevialle et al | 2000 | Retrospective cohort | 2/40 | 27.8 (17–50) | (13/27) | Mixed | n.a. | n.a. | n.a. | 91.2 hours | Reamed antegrade nailing | n.a. | Mortality 2/40 |
| Retrograde Intramedullary nailing In treatment of bilateral femur fractures | Cannada et al | 2008 | Retrospective cohort | 4/89 | 30 (16–63) | (43/46) | Almost exclusively motor vehicle accidents | (35/89) | (85/89) | n.a. | n.a. | Reamed retrograde nailing | n.a. | Mortality 5/89 |
(Symptoms: n = neurological, r = respiratory, p = petechial rash), T9 = Thoracic vertebra No 9.
4. Discussion
Although perioperative fat embolism in current clinical practice can be overcome and appears to be less of a life-threatening complication, it continues to be unexpected and its reasons can be multifactorial.[13,23] In this light, it continues to be unclear if the reaming for preparation of intramedullary nailing, the closed or open reduction, or other cofactors play a role.
On 1 hand, our case reports are similar, as 2 different centers selected healthy patients without chest trauma, as the effects of intravasation are known to be augmented with associated chest injuries.[27] In both cases, the patient was extubated after initial fixation. One center selected external fixation to avoid reaming and 1 center selected retrograde intramedullary nailing to avoid the anterograde piston effect. Both patients appeared to be stable and in good clinical condition preoperatively and demonstrated a delay between extubation and clinical symptoms. In both patients, the neurologic deficit represented the initial cause of concern rather than cardiopulmonary worsening. A synopsis of both cases is presented in Table 2. The case undergoing external fixation was worked up for patent foramen ovale, which was negative. Both patients underwent a work up for coagulopathy and other causes. Both patients presented with severely displaced fractures, while reduction was not particularly difficult. One may, therefore, wonder, if in the patient undergoing external fixation during the evening of admission, hidden hypovolemia may have been the reason for hypercoagulopathy, which was not particularly tested for. Likewise, one may argue that in the patient undergoing bilateral nailing, intraoperative embolization may have played a role. In this retrospective evaluation, it cannot be determined, which aspect is more relevant.
Table 2.
Synopsis of both case reports.
| Case | Age | Gender | Injury mechanism | Chest injury | Other relevant injuries | Arrival | Displacement | Time to surgery | Initial operation | Post OP examination | Development of symptoms | Symptoms | Time to discharge | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ex-fix (case 1) | 19 | Male | Motorcycle accident | No | No | Stable | Left> right | Immediately | Bilateral external fixation | Stable | 12 to 24 hours | N1 R1 P0 | 18 days | Full recovery |
| Reamed nailing (case 2) | 18 | Male | Motorcycle accident | No | Floating elbow (left) | Stable | Bilateral | Next morning | Bilateral reamed nailing | Stable | 12 to 24 hours | N1 R1 P0 | 13 days | Full recovery |
(Symptoms: n = neurological, r = respiratory, p = petechial rash).
Similar results were revealed by our systematic review. While FES is described as a nonhomogeneous combination of symptoms, neurological deficits are usually the most noticeable. Fractures seem to be mostly severely displaced, as discussed by Ten Duis et al.[13] However, information is too scarce to draw conclusions regarding the role of reduction or the intraoperative course.
In terms of physiological aspects, although the lung can tolerate a certain degree of fat embolization by opening arteriovenous shunts[28] and has a tremendous reserve capacity,[29] secondary mechanisms have been known to occur even after a long time, characterized by additional inflammatory stimuli inside the pulmonary vasculature.[30] Moreover, activation of the coagulation cascade has been described in association with the fat intravasation[31] and, therefore, secondary worsening can occur.[32]
Interestingly, we have failed to find any clinical study that compares these approaches, or discusses clear cut evidence of the relevance of either[23] The only available study that examines both procedures in the absence of chest injury has used an animal model.[33] The authors found that the total embolic load was significantly higher in the intramedullary nailing group, but the type of fracture stabilization used did not significantly affect any of the other outcome measurements: they concluded that a higher pulmonary embolic load can be expected during early intra-medullary femoral fracture stabilization compared with primary external fixation. However, the degree of stimulation to systemic coagulation and pulmonary inflammation by each type of surgery was comparable.
Another experimental study did include a lung contusion in their setup and found that secondary changes (pulmonary permeability, coagulopathy, and neutrophil stimulatory capacity were more sustained at 4 hours after injury in the reamed nailing group.[34]
There are 3 theories attempting to explain the pathogenesis of FES: they are the Mechanical theory, the Biochemical theory and the coagulation theory.
Gauss proposed the mechanical theory, which suggests that fractures result in the extrusion of fat droplets via damaged venules into venous circulation.[35]
This occurs when the intramedullary pressure is greater than the venous pressure at a fracture site. These fat droplets travel to the pulmonary capillary bed of the lungs to cause mechanical obstruction resulting in the pulmonary manifestations of FES. The passage of “echogenic material” passing through the right atrium as detected by Pell et al[36] with transesophageal echocardiography during intramedullary nailing of fractures would seem to support this theory. For fat embolism (FE) to affect other organs, they must cross from the venous to arterial circulation. There are a number of potential routes by which this may occur.
Fat emboli can be small enough to directly pass from venous to arterial circulations in the lungs, moreover even the larger droplets can potentially undergo a significant amount of deformation and are, therefore, able to cross to the arterial circulation.[37] Arteriovenous shunts within the pulmonary circulation have been demonstrated by several studies and may be a potential route for FE to cross into the arterial circulation.[38]
The presence of a Patent Foramen Ovale has been discussed as a potential cause of more sustained cerebral embolisms. Some authors discuss the Patent Foramen Ovale can be present in up to 34% of the adult population, and the rise in right atrial pressure in these patients from the effects of FE on the lungs or indeed mechanical ventilation of the patient.[39]
The mechanical theory does have limitations as it does not explain the development of FES in patients without trauma nor does it explain the typical delay of onset of FES of 24 to 72 hours from the initial trauma.
Lehman and Moore proposed a biochemical theory, focusing on breakdown of neutral fat droplets upon entering the venous circulation undergoing degradation to Free Fatty Acids (FFA), which are considerably more biologically active.[40] FFA's have been shown to cause damage to capillary beds of lungs.[41] The increased levels of catecholamines used in patients with major trauma can induce further lipolysis resulting in increased levels of FFA's. The time taken for the production of these FFA's may explain the time delay seen for the onset of FES after trauma. It has been suggested that raised levels of “C-Reactive Protein,” which is elevated in these patients, may cause circulating Chylomicrons, the soluble form of triglycerides, to agglutinate into fat globules. This process may explain the presence of FE in the lungs of patients without trauma.[41]
The coagulation theory suggests that thromboplastin is released along with fat from injured long bones activating the clotting cascade. The resulting fibrin and its degradation products, platelets and fat globules have a direct toxic effect on endothelial lining and increase the permeability of the pulmonary capillaries. The finding of intravascular coagulation is frequently seen in cases of FE. It has been shown that the release of fat into the circulation activates intravascular coagulation with platelet aggregation and clot formation.[42] The procoagulant properties of the released fat is thought to be due to the presence of Tissue Factor, which in turn triggers generation of Thrombin and subsequent formation of fibrin and activation of platelets.[43]
We conclude, that FES continues to represent a relevant complication even in patients without additional risk factors. We also concur that despite extensive research, clinicians appear to be unaware of imminent risks of FES and that despite improvements in reaming techniques, the complication has not been ruled out. Moreover, it continues to occur even when intramedullary instrumentation is avoided completely. Although, in current clinical practice, pulmonary consequences of FES can be managed most often by ventilator support even though prolonged intensive care unit stays may ensue[33,37,44,45] surgeons should continue to be aware of this complication.
Supplementary Material
References
- 1.Blokhuis TJ, Pape HC, Frölke JP. Timing of definitive fixation of major long bone fractures: can fat embolism syndrome be prevented? Injury 2017;48 (Suppl 1):S3–S6. [DOI] [PubMed] [Google Scholar]
- 2.Giannoudis PV, Pape HC, Cohen AP, et al. Review: systemic effects of femoral nailing: from Küntscher to the immune reactivity era. Clin Orthop Relat Res 2002;404:378–386. [PubMed] [Google Scholar]
- 3.Gurd AR. Fat embolism: an aid to diagnosis. J Bone Joint Surg Br 1970;52:732–737. [PubMed] [Google Scholar]
- 4.Gurd AR, Wilson RI. The fat embolism syndrome. J Bone Joint Surg Br 1974;56B:408–416. [PubMed] [Google Scholar]
- 5.Newbigin K, Souza CA, Torres C, et al. Fat embolism syndrome: state-of-the-art review focused on pulmonary imaging findings. Respir Med 2016;113:93–100. [DOI] [PubMed] [Google Scholar]
- 6.Buskens CJ, Gratama JW, Hogervorst M, et al. Encephalopathy and MRI abnormalities in fat embolism syndrome: a case report. Med Sci Monit 2008;14:CS125–CS129. [PubMed] [Google Scholar]
- 7.Meek RN, Woodruff B, Allardyce DB. Source of fat macroglobules in fractures of the lower extremity. J Trauma 1972;12:432–434. [DOI] [PubMed] [Google Scholar]
- 8.Manning JB, Bach AW, Herman CM, et al. Fat release after femur nailing in the dog. J Trauma 1983;23:322–326. [DOI] [PubMed] [Google Scholar]
- 9.Bone LB, Johnson KD, Weigelt J, et al. Early versus delayed stabilization of femoral fractures. A prospective randomized study. J Bone Joint Surg Am 1989;71:336–340. [PubMed] [Google Scholar]
- 10.Pinney SJ, Keating JF, Meek RN. Fat embolism syndrome in isolated femoral fractures: does timing of nailing influence incidence? Injury 1998;29:131–133. [DOI] [PubMed] [Google Scholar]
- 11.Riska EB, von Bonsdorff H, Hakkinen S, et al. Prevention of fat embolism by early internal fixation of fractures in patients with multiple injuries. Injury 1976;8:110–116. [DOI] [PubMed] [Google Scholar]
- 12.Talucci RC, Manning J, Lampard S, et al. Early intramedullary nailing of femoral shaft fractures: a cause of fat embolism syndrome. Am J Surg 1983;146:107–111. [DOI] [PubMed] [Google Scholar]
- 13.Ten Duis HJ, Nijsten MW, Klasen HJ, et al. Fat embolism in patients with an isolated fracture of the femoral shaft. J Trauma 1988;28:383–390. [DOI] [PubMed] [Google Scholar]
- 14.Trueta J, Cavadias AX. Vascular changes caused by the Küntscher type of nailing; an experimental study in the rabbit. J Bone Joint Surg Br 1955;37-B:492–505. [DOI] [PubMed] [Google Scholar]
- 15.Danckwardt-Lillieström G. Reaming of the medullary cavity and its effect on diaphyseal bone. A fluorochromic, microangiographic and histologic study on the rabbit tibia and dog femur. Acta Orthop Scand Suppl 1969;128:1–153. [DOI] [PubMed] [Google Scholar]
- 16.Hausberger FX, Whitenack SH. Effect of pressure on intravasation of fat from the bone marrow cavity. Surg Gynecol Obstet 1972;134:931–936. [PubMed] [Google Scholar]
- 17.Heim D, Schlegel U, Perren SM. Intramedullary pressure in reamed and unreamed nailing of the femur and tibia-an in vitro study in intact, human bones. Injury 1993;24 (Suppl 3):S56–S63. [DOI] [PubMed] [Google Scholar]
- 18.Müller C, McIff T, Rahn BA, et al. Influence of the compression force on the intramedullary pressure development in reaming of the femoral medullary cavity. Injury 1993;24 (Suppl 3):S36–S39. [DOI] [PubMed] [Google Scholar]
- 19.Wenda K, Runkel M, Degreif J, et al. Pathogenesis and clinical relevance of bone marrow embolism in medullary nailing-demonstrated by intraoperative echocardiography. Injury 1993;24 (Suppl 3):S73–S81. [DOI] [PubMed] [Google Scholar]
- 20.Wenda K, Ritter G, Degreif J, et al. Pathogenesis of pulmonary complications following intramedullary nailing osteosyntheses. Unfallchirurg 1988;91:432–435. [PubMed] [Google Scholar]
- 21.Pape HC, Regal G, Dwenger A, et al. Influences of different methods of intramedullary femoral nailing on lung function in patients with multiple trauma. J Trauma 1993;35:709–716. [DOI] [PubMed] [Google Scholar]
- 22.Pape HC, Dwenger G, Grotz M, et al. Does the reamer type influence the degree oflung dysfunction after femoral nailing following severe trauma? An animal study. J Orthop Trauma 1994;8:300–309. [DOI] [PubMed] [Google Scholar]
- 23.Lempert M, Halvachizadeh S, Ellanti P, et al. Incidence of fat embolism syndrome in femur fractures and its associated risk factors over time-A systematic review. J Clin Med 2021;10:2733–2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Bmj 2009;339:B2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bonnevialle P, Cauhepe C, Alqoh F, et al. Risks and results after simultaneous intramedullary nailing in bilateral femoral fractures: a retrospective study of40 cases. Rev Chir Orthop Reparatrice Appar Mot 2000;86:598–607. [PubMed] [Google Scholar]
- 26.Cannada LK, Aghizadeh S, Murali J, et al. Retrograde intramedullary nailing in treatment of bilateral femur fractures. J Orthop Trauma 2008;22:530–534. [DOI] [PubMed] [Google Scholar]
- 27.Pape HC, Regel G, Dwenger A, et al. Influence of thoracic trauma and primary femoral intramedullary nailing on the incidence of ARDS in multiple trauma patients. Injury 1993;24 (Suppl 3):S82–S103. [DOI] [PubMed] [Google Scholar]
- 28.Dunn JS, Muir H, et al. The effects of multiple embolism of pulmonary arterioles. Quarterly J Med 1920;13:129–132. [Google Scholar]
- 29.Gehr P, Bachofen M, Weibel ER. The normal human lung: ultrastructure and morphometric estimation of diffusion capacity. Respir Physiol 1978;32:121–140. [DOI] [PubMed] [Google Scholar]
- 30.Barie PS, Minnear FL, Malik AB. Increased pulmonary vascular permeability after bone marrow injection in sheep. Am Rev Respir Dis 1981;123:648–653. [DOI] [PubMed] [Google Scholar]
- 31.Bradford DS, Foster RR, Nossel HL. Coagulation alterations, hypoxemia, and fat embolism in fracture patients. J Trauma 1970;10:307–321. [DOI] [PubMed] [Google Scholar]
- 32.Gossling HR, Pellegrini VD, Jr. Fat embolism syndrome: a review of the pathophysiology and physiological basis of treatment. Clin Orthop Relat Res 1982; 68–82. [PubMed] [Google Scholar]
- 33.Gray AC, White TO, Clutton E, et al. The stress response to bilateral femoral fractures: a comparison of primary intramedullary nailing and external fixation. J Orthop Trauma 2009;23:90–97. [DOI] [PubMed] [Google Scholar]
- 34.Hildebrand F, Giannoudis P, van Griensven M, et al. Secondary effects of femoral instrumentation on pulmonary physiology in a standardised sheep model: what is the effect of lung contusion and reaming? Injury 2005;36:544–555. [DOI] [PubMed] [Google Scholar]
- 35.Gaiss H. The pathology of fat emobolism. Arch Surg 1924;9:593–605. [Google Scholar]
- 36.Pell AC, Christie J, Keating JF, et al. The detection of fat embolism by transoesophageal echocardiography during reamed intramedullary nailing. A study of 24 patients with femoral and tibial fractures. J Bone Joint Surg Br 1993;75:921–925. [DOI] [PubMed] [Google Scholar]
- 37.Byrick RJ, Mullen JB, Mazer CD, et al. Transpulmonary systemic fat embolism. Studies in mongrel dogs after cemented arthroplasty. Am J Respir Crit Care Med 1994;150:1416–1422. [DOI] [PubMed] [Google Scholar]
- 38.Tobin CE. Arteriovenous shunts in the peripheral pulmonary circulation in the human lung. Thorax 1966;21:197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pell AC, Hughes D, Keating J, et al. Brief report: fulminating fat embolism syndrome caused by paradoxical embolism through a patent foramen ovale. N Engl J Med 1993;329:926–929. [DOI] [PubMed] [Google Scholar]
- 40.Lehman EP, Moore RM. Fat embolism: including experimental production without trauma. Arch Surg 1927;14:621–662. [Google Scholar]
- 41.Parker FB, Jr, Wax SD, Kusajima K, et al. Hemodynamic and pathological findings in experimental fat embolism. Arch Surg 1974;108:70–74. [DOI] [PubMed] [Google Scholar]
- 42.Wozasek GE, Simon P, Redl H, et al. Intramedullary pressure changes and fat intravasation during intramedullary nailing: an experimental study in sheep. J Trauma 1994;36:202–207. [DOI] [PubMed] [Google Scholar]
- 43.Dahl OE, Aspelin T, Lyberg T. The role of bone traumatization in the initiation of proximal deep vein thrombosis during cemented hip replacement surgery in pigs. Blood Coagul Fibrinolysis 1995;6:709–717. [DOI] [PubMed] [Google Scholar]
- 44.Murphy P, Edelist G, Byrick J, et al. Relationship of fat embolism to haemodynamic and echocardiographic changes during cemented arthroplasty. Can J Anaesth 1997;44:1293–1300. [DOI] [PubMed] [Google Scholar]
- 45.Herndon JH, Bechtol CO, Crickenberger DP. Fat embolism during total hip replacement. A prospective study. J Bone Joint Surg Am 1974;56:1350–1362. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.