Abstract
Digital health principles are starting to be evident in medicine. Orthopaedic trauma surgery is also being impacted —indirectly by all other improvements in the health ecosystem but also in particular efforts aimed at trauma surgery. Data acquisition is changing how evidence is gathered and utilized. Sensors are the pen and paper of the next wave of data acquisition. Sensors are gathering wide arrays of information to facilitate digital health relevance and adoption. Early adaption of sensor technology by the nonlegacy health environment is what has made sensor driven data acquisition so palatable to the normal health care system. As it applies to orthopaedic trauma, current sensor driven diagnostics and surveillance are nowhere near as developed as in the larger medical community. Digital health is being explored for health care records, data acquisition in diagnostics and rehabilitation, wellness to health care translation, intraoperative monitoring, surgical technique improvement, as well as some early-stage projects in long-term monitoring with implantable devices. The internet of things is the next digital wave that will undoubtedly affect medicine and orthopaedics. Internet of things (loT) devices are now being used to enable remote health monitoring and emergency notification systems. This article reviews current and future concepts in digital health that will impact trauma care.
Keywords: digital health, internet of things, monitoring, sensors, wellness
1. Introduction
Medicine is undergoing yet another evolution. Data acquisition is changing how evidence is gathered and utilized. Sensors are the pen and paper of the next wave of data acquisition. Sensors are gathering wide arrays of information to facilitate digital health relevance and adoption. Slow progress for penetration of the orthopaedic trauma world has been evident. Digital health is influencing care and orthopaedic surgeons will eventually take advantage of this innovation. Digital health is a loosely defined term that refers to the use of information technology and electronic communication tools to deliver care services or to facilitate better health. It has come to mean integrated, interoperable, and digitally enabled care environments that manage health and wellness to transform care delivery. The impact of the wellness industry to drive health care is not to be trivialized. Early adaption of sensor technology by the non-legacy health environment is what has made sensor driven data acquisition so palatable to the normal health care system. The data volume and usefulness are what makes digital health so interesting. As it applies to orthopaedic trauma, current sensor driven diagnostics, and surveillance are nowhere near as developed as in the larger medical community.
Sensor technology in orthopaedics is on the rise but practical application has lagged other medical specialties.[1,2] Digital health is being explored for health care records, data acquisition in diagnostics and rehabilitation, wellness to health care translation, intraoperative monitoring, surgical technique improvement, as well as some early-stage projects in long-term monitoring with implantable devices. The internet of things (IoT) is the next digital wave that will undoubtedly affect medicine and orthopaedics. IoT is made up of intercommunicating physical objects that are usually embedded with sensors and actuators. They have processing ability, embedded software, and other technologies that connect and exchange data with other devices and systems. So, the so-called dumb objects that make up our environment have been imbued with the ability to interact with each other and their surroundings. This can be over the Internet or with other communications networks. IoT devices are being used to enable remote health monitoring and emergency notification systems.[1,3–5] These health monitoring devices can range from blood pressure and heart rate monitors to advanced devices capable of monitoring specialized implants,[4] pacemakers[6] and Fitbit electronic wristbands.[7,8] Some hospitals have begun implementing intelligent beds[9] that can detect when they are occupied and when a patient is attempting to get up. These beds can also adjust themselves to ensure appropriate pressure and support is applied to the patient without the manual interaction of nurses.[9] There are a few key areas of healthcare loT that could bring in revenue: remote patient monitoring (which includes chronic disease management), telehealth, and behavioral modification. These are all easily attainable goals for loT early wave devices.
2. Health care records
Orthopaedic surgeons currently see some immediate benefit from digital health. Artificial intelligent systems aside we see new and improved methods of delivering health care information that helps with normal health care. Future directions include interactive infographics and the ability to do a deep dive on patient data.[10] Real time analysis of patient information and demographic parameters will allow more meaningful interactions and in depth views of what is happening in patient care.[11] This represents a natural progression of health records.
3. Data acquisition in diagnostics and rehabilitation
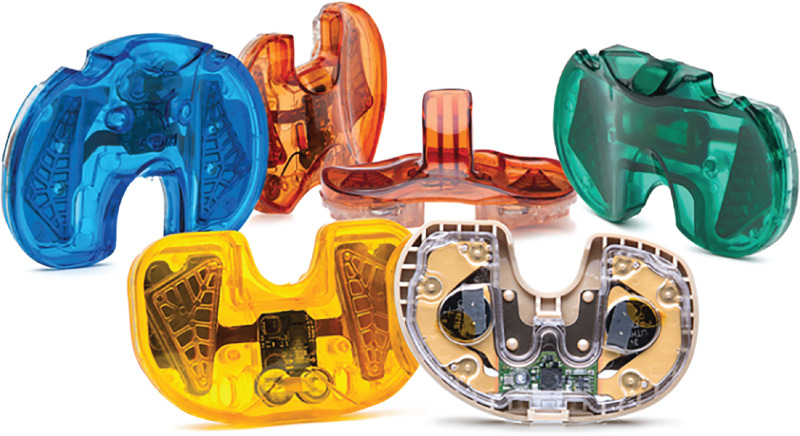
Mobile outpatient monitoring is one segment of loT Healthcare. The use of mobile devices to support medical follow-up is referred to as m-health and is a sensor laden approach to useful health statistics.[12] Advances in electronics fabrication methods have enabled ultra-low cost, use-and-throw loMT sensors. These are reliably manufactured in bulk processes.[2] These sensors, combined with new low energy communication technology and expanded internet protocols have made for exciting potential in health care surveillance. Certainly, everyone has seen the advertisements for glucose sensors that ensure appropriate insulin supply.[2,13] Sensors can be fabricated on paper or etextiles for wireless powered disposable sensing devices.[14,15] Devices have recently been brought to market for niche problems in diagnostics. One example is the MY01 device (Fig. 1), a MEMS sensor product designed to aid in the diagnosis of acute compartment syndrome.[16] This device represents a true transition to digital health as it has an accompanying application for real time data retrieval designed to not only allow cloud based remote viewing but integration with electronic health records. Some next generation commercially available glucometers, like the Dexcom G6, are now equipped with real time data retrieval (Fig. 2).
Figure 1.
MY01 compartment syndrome sensor—designed to allow real-time cloud-based data retrieval and display in a smartphone application, the electronic health record, and at the bedside.
Figure 2.
Dexcom glucose sensorsystem—designed to have realtime read out to a patient-oriented application. From public access site —https://www.dexcom.com/en-CA/en-ca-dexcom-g6-cgm-system.
4. Telehealth and the wellness to health care translation
Health care by Zoom and other telemedicine tools is already here [17,18] facilitated by the needs of the Covid pandemic. Surgical care by telehealth [19–22] is the next step here and has been explored by many people interested in long distance care or for oversight of patient safety during remote procedures.[23,24] We are currently seeing an adoption of wellness sensors to monitoring health.[25–30] There is usage of wearable device integrations that can monitor patient's vital signs such as heart rate and blood pressure.[31] Patients are more than willing to accept new technology and the gamification of rehabilitation.[3,4,32] The increasing use of telehealth could reduce the cost of doctor's visits by as much as 75%, and about half of all doctor's visits could be conducted online. Specialized sensors can be patient centric or placed within living spaces to monitor the health and general well being of patients.[33] These sensors create a network of intelligent sensors[12,34] that can collect, process, transfer, and analyze valuable information in different environments.[35] However, some reviews have been unable to find an improvement on in person clinic visits.[36] The goal is to connect in-home monitors and sensor arrays to hospital-based systems.[1,6,32,35,37,38] Its applications to orthopaedic surgery are multifold- patient rehabilitation monitoring,[39] medication compliance, and wellness utilities are now available or soon will be possible.[32,35]
5. Surgical technique improvement
Last to the table is innovation in intraoperative sensors for orthopaedics. We see the typical me-too usages for robotics but have yet to see a real breakthrough in which the robot performs the surgery. Certainly, orthopaedic surgeons utilize robotic technology to improve outcomes in the operating room- but these devices are more of a check rein to surgical technique. There are new options for aid in reduction of fractures, but they are not in widespread usage.[40–43] Several products are being investigated for in surgery usage but are really limited to total joint surgery[44–46] and have not been applied to trauma surgery. One of these products is Verasense —marketed as a disposable device that delivers data wirelessly to an intraoperative monitor that enables decisions regarding implant position and soft-tissue releases (Fig. 3).
Figure 3.
Verasense Total Knee tray—designed to allow intraoperative sensing at the level of the tibial tray. The tray is discarded at the end of the case and a polyethylene tray is placed in the normal position. From public access site—https://www.orthosensor.com/surgeons/verasense/.
6. Long-term monitoring with implantable devices
The application of IoT in orthopaedic surgery can play a particular fundamental role in managing chronic diseases and in disease prevention and control which for orthopaedics can be fall and accident prevention amongst other applications.[33,47–51] One of the main issues for IoT (besides ethical concerns) is the actual amount of data that will be generated. IoT data is measured in zettabytes, a unit equal to 1 trillion gigabytes. There are estimates that the IoT generates more than 500 zettabytes per year in data—and in the years to come, that number is expected to grow exponentially, not linearly. As the science and practice of virtual care continues to evolve, sensor solutions capable of monitoring many parameters (e.g., oxygen saturation, heart rate) continuously and simultaneously will be brought on board.[4] Through seamless integration of multiple signals, these technologies can generate high-volume big data for the development of algorithms to facilitate early detection of changes in patient health status and timely clinician response. Currently few options exist. Usage of sensors for infection are coming to market.[52] Most common is the use of sensors for intraoperative measurements in total joint arthroplasty.[52–55] Very few indwelling options are available.[49,56] One device has been designed for allowing pressure monitoring in total knee arthroplasty to determine imbalances of force.[57] A platform that may hold promise was reported by Cai et al,[49] in Nature Communications. They discussed a device that uses integration with the surface of the bone to allow chronic monitoring in small and large animal models. This potentially will be transferrable to more human settings.
What do we get from digital health? We get better medical records right now. We get telehealth and wellness monitoring. We get a lot of data from external sensor arrays and software packages in current design process. We also can merge wellness and healthcare for meaningful data.
But in the end, we need a lot of information from internal sensors to change orthopaedic health care. Wireless battery-free devices attached to bone during orthopaedic surgeries can potentially form a chronic interface with bone tissues to directly record physiological and biophysical signals critical for the assessment of musculoskeletal health. This may be able to provide a point-of-care platform and the necessary data to facilitate rehabilitation and manage musculoskeletal diseases. This is the future, but it looks attainable. More projects like this will only facilitate the utility of sensors in orthopaedic surgery.
References
- 1.Dunn J, Runge R, Snyder M. Wearables and the medical revolution. Per Med 2018;15:429–448. [DOI] [PubMed] [Google Scholar]
- 2.Ghafar-Zadeh E. Wireless integrated biosensors for point-of-care diagnostic applications. Sensors (Basel) 2015;15:3236–3261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cherid C, Baghdadli A, Wall M, et al. Current level of technology use, health and eHealth literacy in older Canadians with a recent fracture-a survey in orthopedic clinics. Osteoporos Int 2020;31:1333–1340. [DOI] [PubMed] [Google Scholar]
- 4.McGillion MH, Allan K, Ross-Howe S, et al. Beyond wellness monitoring: continuous multiparameter remote automated monitoring of patients. Can J Cardiol 2021; S0828-282X (21)00812-6. [DOI] [PubMed] [Google Scholar]
- 5. Williams C, Mostashari F, Mertz K, et al. What is Health IT [Web page]. Washington DC: US Government; [updated July 24, 2021. Health IT website]. Available at: https://www.healthit.gov/topic/health-it-and-health-information-exchange-basics/what-hie. [Google Scholar]
- 6.Chiang CF, Hsu FM, Yeh KH. Robust loT-based nursing-care support system with smart bio-objects. Biomed Eng Online 2018;17 (suppl 2):154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cadmus-Bertram L, Marcus BH, Patterson RE, et al. Use of the fitbit to measure adherence to a physical activity intervention among overweight or obese, postmenopausal women: self-monitoring trajectory during 16 weeks. JMIR Mhealth Uhealth 2015;3:e96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cadmus-Bertram LA, Marcus BH, Patterson RE, et al. Randomized trial of a fitbit-based physical activity intervention for women. Am J Prev Med 2015;49:414–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jahne-Raden N, Kulau U, Marschollek M, et al. INBED: a highly specialized system for bed-exit-detection and fall prevention on a geriatric ward. Sensors (Basel) 2019;19:1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vankipuram A, Patel VL, Traub S, et al. Overlaying multiple sources of data to identify bottlenecks in clinicalworkflow. J Biomed Inform 2019;100S:100004. [DOI] [PubMed] [Google Scholar]
- 11.Paris N, Lamer A, Parrot A. Transformation and evaluation of the MIMIC database in the OMOP common data model: development and usability study. JMIR Med Inform 2021;9:e30970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perez AJ, Zeadally S. Recent advances in wearable sensing technologies. Sensors (Basel) 2021; 6828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin FY, Lee PY, Chu TF, et al. Neutral nonenzymatic glucose biosensors based on electrochemically deposited pt/au nanoalloy electrodes. Int J Nanomedicine 2021;16:5551–5563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muhammad Sayem AS, Hon Teay S, Shahariar H, et al. Review on Smart Electro-Clothing Systems (SeCSs). Sensors (Basel) 2020;20:587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vu CC, Kim SJ, Kim J. Flexible wearable sensors—an update in view of touch-sensing. Sci Technol Adv Mater 2021;22:26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merle G, Comeau-Gauthier M, Tayari V, et al. Comparison of three devices to measure pressure for acute compartment syndrome. Mil Med 2020;185 (suppl 1):77–81. [DOI] [PubMed] [Google Scholar]
- 17.Sahu D, Rathod V, Phadnis A, et al. Telehealth for consultation and shoulder rehabilitation: a preliminary study on the perspectives of 30 patients during the COVID-19 lockdown. Clin Shoulder Elb 2021;24:156–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cota A, Tarchala M, Parent-Harvey C, et al. Review of 5.5 Years’ experience using e-mail-based telemedicine to deliver orthopedic care to remote communities. Telemed J E Health 2017;23:37–40. [DOI] [PubMed] [Google Scholar]
- 19.Jarragh A, Lari A, Al-Shatti A, et al. Traumatic orthopedic consultations in COVID-19 inpatients—a cross sectional analysis of results and a review of lessons in tele-orthopedics. Ann Med Surg (Lond) 2022;73:103155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dionisi S, Giannetta N, Di Simone E, et al. The use of mhealth in orthopedic surgery: a scoping review. Int J Environ Res Public Health 2021;18:12549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sandhu KS, Singh A, Singh A, et al. Telemedicine versus in-person visits in postoperative care in orthopedic patients: follow-up study from North India. Cureus 2021;13:e18399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Omari AM, Antonacci CL, Zaifman J, et al. Patient satisfaction with orthopedic telemedicine health visits during the COVID-19 pandemic. Telemed J E Health 2021; Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 23.Talbot M, Harvey EJ, Berry GK, et al. A pilot study of surgical telementoring for leg fasciotomy. J R Army Med Corps 2018;164:83–86. [DOI] [PubMed] [Google Scholar]
- 24.Laverdiere C, Corban J, Khoury J, et al. Augmented reality in orthopaedics: a systematic review and a window on future possibilities. Bone Joint J 2019;101-B:1479–1488. [DOI] [PubMed] [Google Scholar]
- 25.Sorriento A, Chiurazzi M, Fabbri L, et al. A novel capacitive measurement device for longitudinal monitoring of bone fracture healing. Sensors (Basel) 2021;21:6694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pol MC, Ter Riet G, van Hartingsveldt M, et al. Effectiveness of sensor monitoring in a rehabilitation programme for older patients after hip fracture: a three-arm stepped wedge randomised trial. Age Ageing 2019;48:650–657. [DOI] [PubMed] [Google Scholar]
- 27.Pol MC, Ter Riet G, van Hartingsveldt M, et al. Effectiveness of sensor monitoring in an occupational therapy rehabilitation program for older individuals after hip fracture, the SO-HIP trial: study protocol of a three- arm stepped wedge cluster randomized trial. BMC Health Serv Res 2017;17:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Braun BJ, Rollmann M, Veith N, et al. Fracture healing redefined. Med Hypotheses 2015;85:940–943. [DOI] [PubMed] [Google Scholar]
- 29.Marschollek M, Becker M, Bauer JM, et al. Multimodal activity monitoring for home rehabilitation of geriatric fracture patients— feasibility and acceptance of sensor systems in the GAL-NATARS study. Inform Health Soc Care 2014;39:262–271. [DOI] [PubMed] [Google Scholar]
- 30.North K, Maass SD, Hitchcock RW. An insole sensor for recording weight bearing behavior during tibial fracture rehabilitation. Annu Int Conf IEEE Eng Med Biol Soc 2010;2010:1856–1859. [DOI] [PubMed] [Google Scholar]
- 31.O’Connor KL, Rowson S, Duma SM, et al. Head-impact-measurement devices: a systematic review. J Athl Train 2017;52:206–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghamari M, Janko B, Sherratt RS, et al. A survey on wireless body area networks for ehealthcare systems in residential environments. Sensors (Basel) 2016;16:831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oh Y, Kim J, Xie Z, et al. Battery-free, wireless soft sensors for continuous multi-site measurements of pressure and temperature from patients at risk for pressure injuries. Nat Commun 2021;12:5008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Park YG, Lee S, Park JU. Recent progress in wireless sensors for wearable electronics. Sensors (Basel) 2019;19:4353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Basatneh R, Najafi B, Armstrong DG. Health sensors, smart home devices, and the internet of medical things: an opportunity for dramatic improvement in care for the lower extremity complications of diabetes. J Diabetes Sci Technol 2018;12:577–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rubinger L, Bhandari M. Cochrane in CORR(R)-interactive telemedicine: effects on professional practice and health care outcomes. Clin Orthop Relat Res 2020;478:1971–1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sedlmayr M, Prokosch HU, Munch U. Towards smart environments using smart objects. Stud Health Technol Inform 2011;169:315–319. [PubMed] [Google Scholar]
- 38.Zhao S, Liu J, Gong Z, et al. Wearable physiological monitoring system based on electrocardiography and electromyography for upper limb rehabilitation training. Sensors (Basel) 2020;20:4861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pfeufer D, Zeller A, Mehaffey S, et al. Weight-bearing restrictions reduce postoperative mobility in elderly hip fracture patients. Arch Orthop Trauma Surg 2019;139:1253–1259. [DOI] [PubMed] [Google Scholar]
- 40.Du W, Sun T, Ding Y, et al. Robot-assisted treatment of unstable pelvic fractures with a percutaneous iliac lumbar double rod fixation combined with a percutaneous pelvic anterior ring INFIX fixation. Int Orthop 2020;44:1223–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.He M, Han W, Zhao CP, et al. Evaluation of a bi-planar robot navigation system for insertion of cannulated screws in femoral neck fractures. Orthop Surg 2019;11:373–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang JQ, Zhao CP, Su YG, et al. Computer-assisted navigation systems for insertion of cannulated screws in femoral neck fractures: a comparison of bi-planar robot navigation with optoelectronic navigation in a Synbone hip model trial. Chin Med J (Engl) 2011;124:3906–3911. [PubMed] [Google Scholar]
- 43.Yongqi L, Dehua Z, Hongzi W, et al. Minimally invasive versus conventional fixation of tracer in robot-assisted pedicle screw insertion surgery: a randomized control trial. BMC Musculoskelet Disord 2020;21:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Indelli PF, Risitano S, Pipino G, et al. Sensor guided unicompartmental to total knee arthroplasty revision: surgical technique. Orthop Rev (Pavia) 2020;12:8806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Song SJ, Kim KI, Park CH. Sensor use in cruciate-retaining total knee arthroplasty compared with posterior-stabilized total knee arthroplasty: load balancing and posterior femoral rollback. J Knee Surg 2021; Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 46.Walker PS, Meere PA, Bell CP. Effects of surgical variables in balancing of total knee replacements using an instrumented tibial trial. Knee 2014;21:156–161. [DOI] [PubMed] [Google Scholar]
- 47.Aldebeyan S, Aoude A, Harvey EJ. Electronics and orthopaedic surgery. Injury 2018;49 (suppl 1):S102–S104. [DOI] [PubMed] [Google Scholar]
- 48.Bai X, Wang Q, Cao S. Application of infusion control system based on internet of things technology in joint orthopedics nursing work. J Healthc Eng 2021;2021:6691258. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 49.Cai L, Burton A, Gonzales DA, et al. Osseosurface electronics-thin, wireless, battery-free and multimodal musculoskeletal biointerfaces. Nat Commun 2021;12:6707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pradhan B, Bharti D, Chakravarty S, et al. Internet of things and robotics in transforming current-day healthcare services. J Healthc Eng 2021;2021:9999504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yamashita K, Kusuda K, Ito Y, et al. Evaluation of surgical instruments with radiofrequency identification tags in the operating room. Surg Innov 2018;25:374–379. [DOI] [PubMed] [Google Scholar]
- 52.Iyengar KP, Gowers BTV, Jain VK, et al. Smart sensor implant technology in total knee arthroplasty. J Clin Orthop Trauma 2021;22:101605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fary C, McKenzie D, Steiger R. Reproducibility of an intraoperative pressure sensor in total knee replacement. Sensors (Basel) 2021;21:7679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sabatini L, Bosco F, Barberis L, et al. Kinetic sensors for ligament balance and kinematic evaluation in anatomic bi-cruciate stabilized total knee arthroplasty. Sensors (Basel) 2021;21:5427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Oldfrey B, Tchorzewska A, Jackson R, et al. Additive manufacturing techniques for smart prosthetic liners. Med Eng Phys 2021;87:45–55. [DOI] [PubMed] [Google Scholar]
- 56.Borchani W, Aono K, Lajnef N, et al. Monitoring of postoperative bone healing using smart trauma-fixation device with integrated self-powered piezo-floating-gate sensors. IEEE Trans Biomed Eng 2016;63:1463–1472. [DOI] [PubMed] [Google Scholar]
- 57.Hasenkamp W, Thevenaz N, Villard J, et al. Design and test of a MEMS strain-sensing device for monitoring artificial knee implants. Biomed Microdevices 2013;15:831–839. [DOI] [PMC free article] [PubMed] [Google Scholar]