ABSTRACT
Background:
Afghan refugees often face hardship and traumatic experiences before, during, and after migration and frequently suffer from mental health burdens. Evidence based psychological treatments for refugees mostly focus on symptoms of posttraumatic stress disorder (PTSD), however, refugees often suffer from a variety of general health problems as well as depression and anxiety. We thus aimed to evaluate the effectiveness of a transdiagnostic psychological intervention.
Objective:
To investigate the effectiveness of an adapted version of Problem Management Plus (aPM+) delivered by mental health professionals to adult Afghan refugees and asylum seekers.
Methods:
We randomly allocated 88 Afghan refugees either to aPM+ in addition to treatment as usual (aPM+/TAU) or TAU alone. APM+ comprises of six weekly 90-minute individual sessions including strategies of stress management, problem solving, behavioural activation, strengthening social support and either anger regulation or increasing self-efficacy. The primary outcome was general health (GHQ-28) post intervention. Secondary outcome measures included distress by PMLD, Complex PTSD symptoms, quality of life, self-identified problems, and integration.
Results:
Attrition was high: 42% of the randomized participants did not participate in the post-treatment assessment. A repeated measures per-protocol (completers only) ANCOVA evidenced a significant group × timepoint interaction for GHQ total scores [F(1, 47) = 14.80, p < .001, partial η2 = 0.24]. Post-hoc analyses showed significantly lower symptoms in the aPM+/TAU arm (n = 26) as compared to the TAU arm (n = 25) for the GHQ total scores (dz = 1.04). Most secondary outcomes significantly improved in the aPM+/TAU arm, but not in the TAU arm.
Conclusion:
APM+ was effective in reducing general health problems in Afghan refugees and might be considered as a first-line intervention. High drop-out rate limit the interpretations of our results, where future investigations should focus on possibilities to reduce these rates.
Trial registration: Uniform Trial Number identifier: U1111-1226-3285.
HIGHLIGHTS
Refugees’ mental health can be strengthened with a brief psychological intervention that also focuses on skills in the context of post-migration stressors.
High drop-out rates are a major challenge for future research and delivery of psychological interventions as part of health care systems to refugees and asylum seekers.
KEYWORDS: Refugees, asylum seekers, RCT, transdiagnostic intervention, Afghanistan
Abstract
Antecedentes:
Los refugiados afganos a menudo enfrentan dificultades y experiencias traumáticas antes, durante y después de la migración y con frecuencia sufren problemas de salud mental. Los tratamientos psicológicos basados en evidencia para refugiados se centran principalmente en los síntomas del trastorno de estrés postraumático (TEPT), sin embargo, los refugiados a menudo sufren una variedad de problemas generales de salud, así como depresión y ansiedad. Por lo tanto, nuestro objetivo fue evaluar la efectividad de una intervención psicológica transdiagnóstica.
Objetivo:
Investigar la efectividad de una versión adaptada de Problem Management Plus (aPM+) proporcionada por profesionales de la salud mental para adultos afganos refugiados y necesitados de asilo.
Métodos:
Asignamos aleatoriamente a 88 refugiados afganos a aPM+ además del tratamiento habitual (aPM+/TAU) o TAU solo. APM+ se compone de seis sesiones individuales semanales de 90 minutos que incluyen estrategias de manejo del estrés, resolución de problemas, activación del comportamiento, fortalecimiento del apoyo social y regulación de la ira o aumento de la autoeficacia. El resultado primario fue la salud general (GHQ-28) posterior a la intervención. Las medidas de resultado secundarias incluyeron angustia por PMLD, síntomas complejos de TEPT, calidad de vida, problemas autoidentificados e integración.
Resultados:
La deserción fue alta: el 42 % de los participantes aleatorizados no participaron en la evaluación posterior al tratamiento. Un ANCOVA de medidas repetidas por protocolo (solo para los que completaron) evidenció una interacción significativa entre el grupo y el punto de tiempo para las puntuaciones totales de GHQ [F(1, 47)= 14,80, p < 0,001, η2 parcial = 0,24]. Los análisis post-hoc mostraron síntomas significativamente más bajos en el brazo aPM+/TAU (n = 26) en comparación con el brazo TAU (n = 25) para las puntuaciones totales de GHQ (dz = 1,04). La mayoría de los resultados secundarios mejoraron significativamente en el brazo aPM+/TAU, pero no en el brazo TAU.
Conclusión:
APM+ fue eficaz para reducir los problemas generales de salud en los refugiados afganos y podría considerarse una intervención de primera línea. La alta tasa de abandono limita las interpretaciones de nuestros resultados. Futuras investigaciones deberían centrarse en las posibilidades de reducir estas tasas.
PALABRAS CLAVES: Refugiados, necesitados de asilo, ECA, Intervención transdiagnóstica, Afganistán
Abstract
背景:
阿富汗难民在移民之前、期间和之后经常面临困难和创伤经历,并且经常遭受心理健康负担。对难民的循证心理治疗主要集中在创伤后应激障碍 (PTSD) 症状上,然而,难民往往患有各种一般健康问题以及抑郁和焦虑。因此,我们旨在评估跨诊断心理干预的有效性。
目的:
考查由心理健康专业人员向成年阿富汗难民和寻求庇护者提供的改编版问题管理增强版 (aPM+)的有效性。
方法:
我们将 88 名阿富汗难民随机分配到 aPM+ 加组常规治疗 (aPM+/TAU) 或仅 TAU组。 APM+ 包括每周 6 次 90 分钟的个人疗程,包括压力管理、问题解决、行为激活、加强社会支持以及愤怒调节或提高自我效能的策略。主要结果是干预后的一般健康(GHQ-28)。次要结果测量包括 PMLD 带来的精神痛苦、复杂性PTSD 症状、生活质量、自我认同问题和整合。
结果:
流失率很高:42% 的随机参与者没有参与治疗后评估。按方案重复测量(仅限完成者)ANCOVA 证明了 GHQ 总分显著的组别×时间点交互作用 [F(1, 47)= 14.80, p < .001, 部分 η2 = 0.24]。事后分析显示,对于 GHQ 总分 (dz = 1.04),aPM+/TAU 组 (n = 26) 的症状明显低于 TAU 组 (n = 25)。 aPM+/TAU 组的大多数次要结果显著改善,但 TAU 组没有。
结论:
APM+ 可有效减少阿富汗难民的一般健康问题,可被视为一线干预措施。高流失率限制了我们对结果的解释,未来的研究应该关注降低这些流失率的可能性。
关键词: 难民, 寻求庇护者, 随机对照试验, 跨诊断干预, 阿富汗
1. Introduction
Afghan refugees and asylum seekers are among the largest refugee populations worldwide and their number has remained sizeable since the 1980s (UNHCR, 2020). While Afghanistan has a rich cultural heritage, many people have grown up in political turmoil and have often never lived in a peaceful environment; consequently, Afghan refugees1 frequently suffer from mental distress (Alemi, James, Cruz, Zepeda, & Racadio, 2014). Traumatic events and hardship experienced in Afghanistan, during flight, and in the host country (so called post-migration living difficulties, PMLDs) all predict poor mental health (Alemi et al., 2014; Hamrah et al., 2020). Depression, anxiety, and posttraumatic stress disorder (PTSD) are the most frequently reported mental health disorders among refugees resettled in high-income countries (Turrini et al., 2017). In comparison to Syrian refugees in Austria (where this study was conducted) refugees from Afghanistan have on average lower education, have to wait for positive asylum decision longer (Eggenhofer-Rehart et al., 2018), and additionally have a lower chance of obtaining asylum (Bundesministerium für Inneres, 2020). Critically, self-reported health among Afghan refugees is worse compared to refugees from Syria and Iraq in Austria (Georges, Buber-Ennser, Rengs, Kohlenberger, & Doblhammer, 2021).
Despite the need for more rigorous clinical trials, there is growing evidence that psychosocial interventions for PTSD among refugees resettled in high-income countries are effective (Nosè et al., 2017; Turrini et al., 2021). In contrast, there is a lack of research investigating the efficacy of psychosocial interventions for other mental health problems such as anxiety and depression (Koesters, Barbui, & Purgato, 2018). However, despite PTSD being a prominent diagnosis associated with forced migration, depression and anxiety are equally common in refugees (Turrini et al., 2017) and contribute to limitations in quality of life (Ghazinour, Richter, & Eisemann, 2004). Moreover, Western psychiatric categories and constructs may fail to cover the problems and needs of refugees with other cultural backgrounds (Wells, Wells, & Lawsin, 2015). The investigation of the effectiveness of mental health service should thus not only rely on predefined psychiatric conditions but also consider subjective perspectives on health (Drescher et al., 2021).
Integrating trauma-specific interventions into treatment options for refugees is common and may ease PTSD symptomatology. However, PMLDs also contribute significantly to symptoms of distress (Chu, Keller, & Rasmussen, 2013) and functional impairment (Hou et al., 2019). In fact, when refugees in a high-income country in Europe were asked for the reason they evaluated their current subjective well-being as poor, most of them reported problems that fall in the category of PMLDs (Hartonen, Väisänen, Karlsson, & Pöllänen, 2020). PMLDs are among the most common sources of stress identified by refugees 8–20 years after resettlement (Sulaiman-Hill & Thompson, 2012). However, these factors are seldomly addressed in psychosocial interventions.
Recently, the EU STRENGTH project (Sijbrandij et al., 2017) has launched aiming to reduce the burden of disease among Syrian refugees by implementing problem management plus (PM+) (World Health Organization, 2016b), a brief, lay-therapist delivered, transdiagnostic psychological intervention. Initial results provide support for the intervention’s feasibility and potential effectiveness (Sijbrandij, Graaf, Cuijpers, & Kieft, 2020). Previous trials investigating the efficacy of PM+ in other populations have revealed promising, preliminary evidence: In a study in Kenya, PM+ was effective in reducing general health problems in women with experiences of gender-based violence who were identified through a random community screening (Bryant et al., 2017). Additionally, in a trial in Pakistan, patients from primary care centers who reported suffering from emotional distress and were treated with PM+, reported significantly fewer symptoms of depression and anxiety three months after the intervention (Rahman et al., 2016). The reduction in symptoms corresponded to medium to large effects in both studies. Importantly, while trained lay-persons delivered the intervention in these trials, this practice is prohibited in Austria. However, brief psychological interventions provided by mental health professionals may contribute essentially to a stepped care system (Koch, Ehring, & Liedl, 2020; Trilesnik et al., 2019).
1.1. Aims of the study
Taken together, the current study aimed to investigate the treatment effectiveness of a brief psychological intervention that includes a session on coping with PMLDs (adapted Problem Management Plus, aPM+) for general health issues among Afghan refugees in Austria. In addition, we investigated the treatment effectiveness of reducing distress by PMLDs, symptoms of Complex PTSD, and self-identified problems, as well as in improving quality of life and integration.
2. Methods
2.1. Study design and setting
The study was conducted as a prospective, single-center, assessor-masked, randomized, two-group superiority trial from June 2019 to January 2021 (Knefel et al., 2020). It compared a six-session transdiagnostic, low-intensity manualized psychological treatment with treatment as usual (TAU). The treatment group received TAU and aPM+; the control group received TAU alone. Clinical psychologists carried out all assessments and treatment sessions with the support of an interpreter if needed. All assessment instruments were delivered in interview format due to a high illiteracy rate and those psychologists who carried out the assessments were blind to the group allocation at both time points. The trial setting was the Outpatient Unit for Research, Teaching, and Practice, Faculty of Psychology, University of Vienna. The study was prospectively registered online (DRKS00016538; UTN: U1111-1226-3285). The institutional review board of the University of Vienna granted ethical approval (reference numbers: 00356 and 00445).
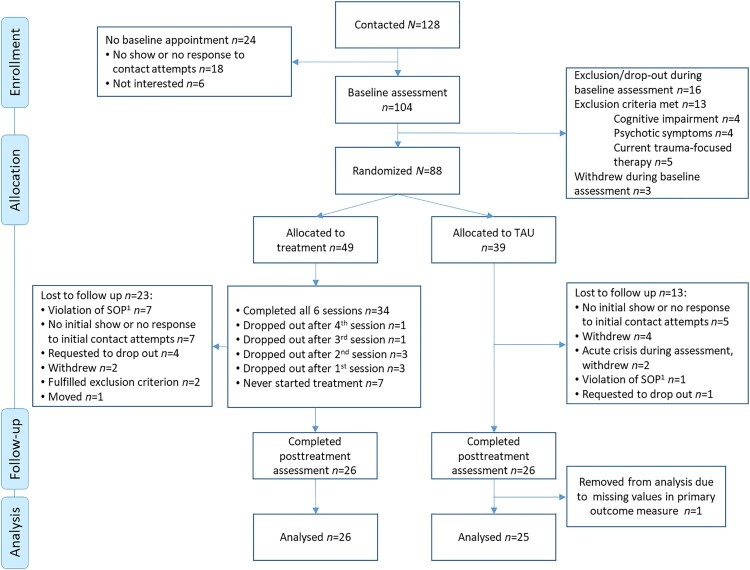
Due to the SARS-CoV2 pandemic, we had to adapt the study design as compared to the study protocol (Knefel et al., 2020). The intended primary end-point was changed from 6-months post intervention to 1-week post intervention to maintain a sufficient sample size within the altered timeframe. As such, we did not employ hierarchical linear modelling as intended. Further, an independent researcher who was responsible for the randomization compiled a random list of 120 numbers following a 1:1 allocation ratio. This sample size was determined expecting a 25% drop-out rate, a medium effect, an α error probability of 0.05 and a power of 0.80 (Knefel et al., 2020). However, due to pandemic related financial and time constraints, we had to stop the recruitment before reaching the planned 120 participants, resulting in a smaller sample size and an unbalanced allocation ratio (Figure 1).
Figure 1.
Consort flow-diagram.
Note. 1SOP = Standard operating procedure; Participants who violated the SOP mostly did not keep apointments repeatedly after they started the treatment. Some also dropped out because of the SARS-CoV2 pandemic related social measures that hindered them from coming to the outpatient unit for too long.
2.2. Participants and procedures
For the trial, we recruited Dari-speaking adult Afghan asylum seekers or refugees which were seeking help for mental health problems in collaboration with local NGOs and health providers specialized on refugees. Inclusion criteria were: (a) being on a wait list for professional mental health treatment in a specialized facility or consent to be put on such a list by the research team; and (b) elevated psychological distress based on a screening questionnaire for common mental disorders in refugees (a score of 12 or higher on the RHS-15 or a score of 5 or higher on the distress scale of the RHS-15). Exclusion criteria were (a) presenting with a current condition requiring other treatment (acute suicidality, severe mental disorder such as psychotic disorders or substance dependence), (b) severe cognitive impairment (e.g. moderate to severe intellectual disability or dementia), based on definitions in the Mental Health Gap Action Programme (mhGAP) Intervention Guide (World Health Organization, 2016a), or (c) current trauma-focused treatment. The clinical psychologist who conducted the assessment during the baseline interview assessed the exclusion criteria. Based on the predefined criteria, this psychologist judged whether any exclusion criterion was fulfilled. Oral and written informed consent was obtained before screening. Included participants completed baseline assessment questionnaires. All participants were on a wait list for professional mental health treatment in a specialized facility other than the outpatient unit where this study was conducted. It was not required that participants stayed on that list for the study period, depending on their personal preferences. An independent researcher not involved in the study randomized them into aPM+/TAU or TAU alone. Participants were informed on group allocation by text-messages on their phones in Dari or German, depending on their language skills, and an interpreter called those allocated to the treatment group to set an appointment for the first session. Post-assessments were scheduled one week after the sixth intervention session or seven weeks after baseline assessment for the control group. All participants were thus invited to two assessment points.
2.3. Intervention and control condition
This study used an adapted version of PM+ (aPM+) in the intervention arm. PM+ (World Health Organization, 2016b) is a transdiagnostic, low-intensity psychological treatment. The original PM+ manual was developed for adults suffering from symptoms of common mental health problems (including depression, anxiety, stress, or grief), as well as self-identified practical problems (including unemployment and interpersonal conflicts) (Dawson et al., 2015). Seeking to preserve a strong evidence base, the developers of PM+ have integrated problem-solving and behavioural treatment techniques that demonstrate amenability to low-intensity delivery (Dawson et al., 2015). The original PM+ manual comprises of five weekly, individual face-to-face sessions based on four cross-cutting core therapeutic strategies: ‘Managing Stress’, ‘Managing Problems’, ‘Get Going, Keep Doing’, and ‘Strengthening Social Support’. The first sessions also features a psychoeducational part about reactions to adversity and the rationale of the intervention. ‘Managing Stress’ aims to optimize initial mastery of stress and other symptoms as well as enhance relaxation with a slow breathing exercise. ‘Managing Problems’ targets to support individuals to take control of their problems with basic problem-solving skills. ‘Get Going, Keep Doing’ aims to increase the opportunity for positive reinforcement from the environment by behavioural activation, addressing inertia. ‘Strengthening Social Support’ aims to optimize a person’s capacity to re-engage with their peer group and elicit support from others. The last session also includes relapse-prevention by identifying individual early warning signals and recapitulating the strategies from the previous sessions (Dawson et al., 2015).
In the initial phase of our study, we developed an additional, sixth session for the intervention that aimed to reduce the burden caused by PMLDs. While psychological measures cannot often directly influence PMLDs, the coping with these stressors can be improved on a psychological basis. The additional session focused on either one of the two therapeutic strategies ‘Anger Regulation’ or ‘Increasing Self-efficacy’ in relation to PMLDs. These two strategies were identified as important for coping with PMLDs in a pre-study (Knefel et al., 2020). To foster participants’ self-empowerment, they could decide during treatment whether they prefer a session on improving anger regulation or on increasing self-efficacy, depending on their subjective needs and preferences. ‘Anger Regulation’ aims to develop skills for the management of intense anger and aggression. It combines strategies from existing treatment manuals (Skills Training in Dialectical Behavior Therapy, Linehan, 2015; STARK manual, Koch et al., 2020) and includes psychoeducational aspects on emotion regulation as well as a regulation strategy, riding the anger, that follows the principles of radical acceptance of emotions and responding with opposite actions. ‘Self-efficacy’ follows an empowerment principle and is rooted in a systemic psychotherapy approach Röhrbein, 2019. It comprises an exercise, the tree of capabilities, helping participants to re-identify with their competences and strengths.
Participants had six weekly face-to-face appointments in an individual format; the duration of these sessions was 90 min. If needed interpreters facilitated the sessions. The psychologists were trained by two WHO PM+ master trainers. Regular supervision was provided to ensure psychologists’ adherence to the protocol. Treatment fidelity was scored using the PM+ Helper’s Self-rating Fidelity Checklist after each session.
The control condition was TAU in the participants’ daily living conditions. TAU comprises all other health services available to Afghan refugees in Austria. This included any contact with medical and mental health professionals, any pharmacological therapy and all activities provided by the specialized treatment facilities on which’s waitlist all participants were. Receiving psychopharmacological or psychological treatment was considered TAU and did not preclude participation in the study. The specialized treatment facilities were Viennese NGOs and offered activities for clients on their waitlist. These activities included soccer games, tea afternoons, or other invitations to social events as well as regular phone calls to inform them about their status on the waitlist. We did not assess the amount to which participants attended any of these activities. The TAU group was not treated with aPM+ at a later point.
2.4. Outcome measures
Investigators blinded to treatment allocation at baseline and at post-intervention assessed all outcome measures. German versions of all questionnaires were available. We used the Dari version of the questionnaires if available and professional interpreters translated and back translated all other questionnaires or additional items. Professional Afghan Dari speaking interpreters also checked all existing Dari/Farsi versions. During the interviews, the German-speaking investigator read aloud the German version of each item and an interpreter read aloud the Dari equivalence of the items.
2.4.1. Primary outcome measure
General health. The primary outcome was general health as assessed by the General Health Questionnaire 28 (GHQ-28) (Goldberg, 1978; Goldberg et al., 1997), a 28-item self-report questionnaire assessing somatic symptoms, anxiety/insomnia, social dysfunction, and severe depression. We used the existing German and Dari versions of the GHQ-28. For participants to be included in the analysis, all subscales of the GHQ were required to be collected. Here, no more than two of the four subscales could have any missing data. For subscales with missing data, the majority of items needed to be collected (i.e. more than half of the seven items). All participants completed the full GHQ item list, except for six out of the 51 participants who completed 95.5% of the GHQ items (five in the aPM+/TAU group and one in the TAU group). For each subscale, we computed an average score to circumvent missing items, and then the sum of these averages was computed to generate the GHQ total score. Internal reliability of the GHQ-28 at baseline was acceptable (Cronbach’s α = .75).
2.4.2. Secondary outcome measures
Post-migration living difficulties. The Post-Migration Living Difficulties Checklist (PMLDC) (Silove, Sinnerbrink, Field, Manicavasagar, & Steel, 1997) is a self-evaluated checklist to assess the frequency of recent adverse life experiences related to migration. The checklist was adapted to the study population to cover a broader range of posttraumatic stressors of refugees in Austria (Table S1). The final version included 26 items measured on a 5-point Likert scale. Additionally, we assessed the associated degree of distress for each item on a 10-point Likert scale. We used the existing Dari/Farsi version of the PMLDC and translated the additional items as part of the study. All participants completed the full PMLDC item list, except for 6 out of 51 participants who completed on average 95.8% of the PMLDC items (three participants from the aPM+/TAU group and three from the TAU group). For the PMLDC, we computed separate average scores for frequency and distress, which effectively handled these missing items. Internal reliability of the PMLDC at baseline was acceptable for the frequency scale and good for the distress scale (frequency: Cronbach’s α = .77; distress: Cronbach’s α = .84).
Posttraumatic stress symptoms. The International Trauma Questionnaire (ITQ) (Cloitre et al., 2018) is an instrument to assess ICD-11 PTSD and Complex PTSD symptoms. The ITQ includes six PTSD items and six disturbances in self-organization (DSO) items. A Complex PTSD screening diagnosis is comprised of both symptoms of PTSD and DSO. Additionally, the ITQ assesses functional impairment by symptoms of PTSD and DSO using three items for each subscale. We used the existing Dari version of the ITQ. No items were missing for participants with respect to the ITQ; we computed sum scores for the PTSD and DSO subscale. Reliability of the ITQ at baseline was good (Cronbach’s α = .81).
Quality of life. The WHO Quality of Life Questionnaire (WHOQOL BREF) (Whoqol Group, 1994) is a cross-culturally comparable instrument to assess quality of life. It consists of 26 items measured on a 5-point Likert scale. It is divided into four domains: physical health, psychological health, social relationships, and environment. We used the existing Dari/Farsi version of the WHOQOL. All participants completed the full WHOQOL instrument, except for five out of 51 participants who completed 97.7% of the items (one participant from the aPM+/TAU group and four from the TAU group), and one participant in the aPM+/TAU group who did not complete baseline items. For the WHOQOL we calculated average scores for each of the four subscales in order to circumvent these missing items. Reliability of the WHOQOL at baseline was good (Cronbach’s α = .81).
Self-identified problems. The Psychological Outcome Profiles (PSYCHLOPS) (Ashworth et al., 2004) promotes a patient-centered definition of therapy outcome and contains five questions on problems, function, and well-being. Participants are asked to describe their main problem(s) and how much they affect them. In the current study, we mainly used quantitative information from the measure and only reported the most common main problems. We translated the PSCYHLOPS into Dari. All participants in our sample completed the full PSYCHLOPS assessment at baseline and post intervention, and average scores were computed for each participant. Reliability of the PSYCHLOPS at baseline was low (Cronbach’s α = .52).
Integration. The short version of the Immigrant Integration Index (IPL-12) (Harder et al., 2018) is a multidimensional measure of immigrant integration. It consists of 12 items capturing six dimensions: psychological, social, economic, political, linguistic, and navigational integration. The IPL-12 was translated into Dari for our study. All participants completed the full IPL-12 assessment except for nine individuals in the TAU group who completed 93.5% of the items. Additionally, two participants from the aPM+/TAU group did not complete the IPL-12 at baseline and were therefore excluded. Again, we computed an average IPL-12 score to circumvent missing items. Reliability of the IPL-12 at baseline was acceptable (Cronbach’s α = .75).
2.5. Other measures
Screening measure. Psychological distress at baseline was assessed with the Refugee Health Screener (RHS-15) (Hollifield et al., 2013). We used the existing Dari version of the RHS-15. Reliability of the RHS-15 at baseline was acceptable (Cronbach’s α = .80).
Trauma exposure. Life-time traumatic experiences were measured through an adapted version of the Harvard Trauma Questionnaire Checklist (Mollica et al., 1992). We used the existing Dari version of the HTQ and translated the additional items. Items only asked for self-experienced events and were scored binary (yes/no) resulting in a total score ranging from zero to 29.
2.6. Statistical analyses
2.6.1. Baseline comparisons
The treatment and control group were compared at baseline with respect to age, sex, and education, as well as on all primary and secondary outcome measures, using chi-squared and independent samples t-tests for categorical and continuous variables, respectively.
2.6.2. Changes in symptoms as a function of treatment
Given the high attrition rate and low statistical power due to sample size in this feasibility trial, we conducted a per-protocol (completers only) analysis to examine the effects of receiving the PM+ treatment, as opposed to the effect of being randomly assigned the treatment (which would utilize an intent-to-treat analysis) (Tripepi, Chesnaye, Dekker, Zoccali, & Jager, 2020). Furthermore, given that we were only to collect clinical assessment at two time-points (pre vs. post intervention, with no follow-up), optimal imputation methods were not possible. We included asylum status as covariate in the models because it is known to be associated with refugees’ mental health (Nickerson et al., 2019).
2.6.2.1. Primary outcome measure
In order to evaluate changes on the GHQ as a function of treatment, we conducted a 2 (group) × 2 (time point) × 4 (GHQ subscale) repeated measures MANCOVA, where age and asylum status were treated as covariates. We additionally computed a 2 (group) × 2 (time point) ANCOVA for GHQ total scores, further controlling for age and asylum status. All statistical assumptions required to conduct a MANCOVA were met. A-priori defined follow-up comparisons were then conducted examining between and within group changes on GHQ total and subscale scores. Non-parametric tests were utilized in the event that any statistical assumptions were violated.
2.6.2.2. Secondary outcome measure
In order to evaluate changes on secondary outcome measures as a function of treatment, we conducted a 2 (group) × 2 (time point) × 10 (outcome measure) repeated measures MANCOVA, where age and asylum status were treated as covariates. A-priori defined follow-up comparisons were then conducted examining between and within group changes on secondary outcomes. Non-parametric tests were utilized in the event that any statistical assumptions were violated. With respect to secondary outcome measures, two participants in the treatment group were missing all data at baseline for the IPL and WHOQOL; we therefore removed these participants from the MANCOVA evaluating secondary outcome measures.
3. Results
Of the 128 potential participants we contacted, 88 met all inclusion criteria and agreed to participate in the trial (Figure 1). Participants who did not complete post-intervention assessments were removed from analyses, resulting in a final sample size of n = 51, with n = 26 in the PM+/TAU arm and n = 25 in the TAU arm and corresponding to a drop-out rate of 42% from baseline to post-intervention (Figure 1). Of those who were randomized into the PM+/TAU arm (n = 49), 69% (n = 34) completed all sessions and 19% (n = 12) dropped out after at least one session (i.e. 81% of those who participated in at least one session, completed all six sessions). Seven participants did not require an interpreter for the baseline assessment. Five of them were randomized to the aPM+/TAU group and these participants did also not need an interpreter for the treatment sessions. Of the 26 participants in the PM+/TAU arm, 13 chose ‘Anger Regulation’ as additional session and 13 chose ‘Increasing Self-efficacy’ as additional session.
To investigate potential differences between those who dropped out and those who remained in the study, we compared completers and drop-outs in the PM+/TAU arm (n = 26 and n = 23, resp.) and in the TAU arm (n = 25 and n = 14, resp.). These four groups did not significantly differ (all p-values > .05) regarding participant characteristics (age, sex, education, asylum status, and number of traumatic experiences) and all primary outcomes (GHQ total score and all four GHQ subscales).
3.1. Baseline comparisons
The groups did not differ significantly at baseline with respect to any primary and secondary outcome measure for both total and subscale scores (Table 1). Additionally, the groups did not differ in terms of sex and education (Table 2). The treatment and control groups differed significantly with respect to age (p = .019); this variable was therefore included as a covariate in subsequent analyses.
Table 1.
Baseline clinical comparisons between groups.
| Primary outcomes | aPM+ /TAU Baseline Statistic M (SD) | TAU Baseline Statistic M (SD) | p-value |
|---|---|---|---|
| GHQ total | 6.45 (1.19) | 6.38 (2.42) | .590 (ns) |
| GHQ somatic | 1.69 (0.46) | 1.63 (0.60) | .664 (ns) |
| GHQ anxiety/insomnia | 1.89 (0.43) | 1.77 (0.75) | .762 (ns) |
| GHQ social dysfunction | 1.57 (0.49) | 1.50 (0.56) | .641 (ns) |
| GHQ depression | 1.31 (0.63) | 1.49 (0.94) | .770 (ns) |
| Secondary outcomes | |||
| PMLDC frequency | 2.95 (0.57) | 2.84 (0.53) | .429 (ns) |
| PMLDC distress | 5.40 (1.52) | 5.42 (1.41) | .977 (ns) |
| ITQ PTSD | 13.67 (4.22) | 14.8 (4.44) | .558 (ns) |
| ITQ DSO | 12.38 (5.05) | 12.80 (6.32) | .705 (ns) |
| WHOQOL physical | 2.54 (0.62) | 2.80 (0.73) | .181 (ns) |
| WHOQOL psychological | 3.14 (0.63) | 3.08 (0.83) | .887 (ns) |
| WHOQOL social | 2.83 (0.83) | 2.88 (0.70) | .672 (ns) |
| WHOQOL environment | 2.50 (0.48) | 2.50 (0.56) | .946 (ns) |
| PSYCHLOPS | 4.61 (0.51) | 4.59 (0.57) | .968 (ns) |
| IPL-12 integration | 2.41 (0.59) | 2.49 (0.57) | .666 (ns) |
Note. GHQ, General Health Questionnaire 28-item version; PMLDC, Post-Migration Living Difficulties Checklist; ITQ, International Trauma Questionnaire; WHOQOL, WHO Quality of Life Questionnaire; PSYCHLOPS, Psychological Outcome Profiles; IPL-12, Immigrant Integration Index 12-item version; aPM+, adapted Problem Management Plus; TAU, Treatment As Usual.
Table 2.
Sample Characteristics.
| Total Sample (n = 51) | aPM+/ TAU (n = 26) | TAU (n = 25) | Test-statistic | p-value | |
|---|---|---|---|---|---|
| Biological Sex (female) n (%) | 25 (49.0) | 10 (38.5) | 15 (60.0) | χ²(1) = 1.58c | .208 (ns) |
| Age M (SD) | 34.3 (13.6) | 29.9 (10.7) | 38.8 (14.9) | t(43.5) = 2.42 | .019 |
| Marital Status n (%) | χ²(4) = 2.78 | .593d (ns) | |||
| Single | 20 (39.2) | 13 (50.0) | 7 (28.0) | ||
| Married | 25 (49.0) | 10 (38.5) | 15 (60.0) | ||
| In relationship | 2 (3.9) | 1 (3.8) | 1 (4.0) | ||
| Divorced | 2 (3.9) | 1 (3.8) | 1 (4.0) | ||
| Widowed | 2 (3.9) | 1 (3.8) | 1 (4.0) | ||
| Education n (%)a | χ²(5) = 6.37 | .305d (ns) | |||
| No formal education | 15 (30.0) | 8 (30.8) | 7 (29.2) | ||
| Elementary school (6 years) | 11 (22.0) | 6 (23.1) | 5 (20.8) | ||
| Secondary school (9 years) | 9 (18.0) | 7 (26.9) | 2 (8.3) | ||
| High school (12 years) | 8 (16.0) | 3 (11.5) | 5 (20.8) | ||
| Vocational school | 3 (6.0) | 0 (0.0) | 3 (12.5) | ||
| University/College | 4 (8.0) | 2 (7.7) | 2 (8.3) | ||
| Asylum status | χ²(1) = 0.02 | .891 (ns) | |||
| Secure asylum statusb | 26 (51.0) | 14 (53.8) | 12 (48.0) | ||
| Insecure asylum status | 25 (49.0) | 12 (46.2) | 13 (52.0) | ||
| Traumatic Experiences M (SD)a | |||||
| Total count M (SD) | 12.7 (5.4) | 11.6 (5.7) | 13.8 (4.9) | t(46.9) = 1.46 | .151 (ns) |
| Being in danger during the flight n (%) | 43 (86.0) | 23 (88.5) | 20 (83.3) | ||
| Being a civilian in a war zone n (%) | 35 (70.0) | 17 (65.4) | 18 (75.0) | ||
| Being close to death n (%) | 32 (64.0) | 16 (61.5) | 16 (66.7) | ||
| Living in a refugee camp n (%) | 30 (60.0) | 17 (65.4) | 13 (54.2) | ||
| Murder of a family member or friend n (%) | 30 (60.0) | 13 (50.0) | 17 (70.8) | ||
| Being in a combat situation n (%) | 30 (60.0) | 11 (42.3) | 19 (79.2) |
Note. a Based on n = 50, no data for one participant from the TAU group. b Secure asylum status is defined as having a long-term perspective in Austria, i.e. unconditional permit of residence for more than a year and free access to the labour market. cχ²-test with Yates continuity correction. d p-value based on Fisher’s exact test.
3.2. Changes in symptoms as a function of treatment
3.2.1. Primary outcome measure
Statistical assumptions were met, where box tests examining covariance matrices were non-significant and therefore Wilk’s Lambda values are reported. The repeated measures MANCOVA revealed a significant overall group × timepoint interaction [F(4, 44) = 3.73, p = .011, partial η2 = 0.25], as well as significant group × timepoint interaction for GHQ somatic symptoms [F(1, 47) = 6.91, p = .011, partial η2 = 0.13], GHQ anxiety/insomnia [F(1, 47) = 10.21, p = .002, partial η2 = 0.18], and GHQ social dysfunction [F(1, 47) = 8.44, p = .006, partial η2 = 0.15], but no significant group × timepoint interaction for GHQ severe depression [F(1, 47) = 2.64, p = .111, partial η2 = 0.05]. Furthermore, the repeated measures ANCOVA evidenced a significant group × timepoint interaction for GHQ total scores [F(1, 47) = 14.80, p < .001, partial η2 = 0.24],
Given the aforementioned significant group × timepoint interactions, we conducted follow-up comparisons for GHQ subscales between groups post-intervention, as well as within-groups pre- as compared to post-intervention. The aPM+/TAU group displayed significantly lower scores post-intervention as compared to baseline on GHQ somatic symptoms (dz = 0.64), GHQ anxiety/insomnia scores (dz = 0.75), GHQ social dysfunction (dz = 0.52), GHQ severe depression (dz = 0.99), and GHQ total scores (dz = 1.04). In contrast, the TAU group showed no significant changes in GHQ total nor subscale scores post-intervention as compared to baseline (see Table 3).
Table 3.
Baseline vs. post-intervention within group comparisons and summary statistics for primary and secondary outcomes.
| Group | Descriptive statistics M (SD) | Analysis | |||
|---|---|---|---|---|---|
| Baseline | Post-intervention | p-value | Effect size (Cohen’s dz) | ||
| Primary outcomes | |||||
| GHQ total | aPM+ /TAU | 6.45 (1.19) | 4.83 (1.81) | <.001 | 1.04 |
| TAU | 6.38 (2.42) | 6.58 (2.61) | .469 (ns) | 0.15 | |
| GHQ somatic | aPM+ /TAU | 1.69 (0.46) | 1.31 (0.64) | .003 | 0.64 |
| TAU | 1.63 (0.60) | 1.70 (0.77) | .511 (ns) | 0.14 | |
| GHQ anxiety/insomnia | aPM+ /TAU | 1.89 (0.43) | 1.37 (0.66) | .002 | 0.75 |
| TAU | 1.77 (0.75) | 1.86 (0.81) | .413 (ns) | 0.17 | |
| GHQ social dysfunction | aPM+ /TAU | 1.57 (0.49) | 1.30 (0.53) | .014 | 0.52 |
| TAU | 1.50 (0.56) | 1.62 (0.65) | .099 (ns) | 0.34 | |
| GHQ depression | aPM+ /TAU | 1.31 (0.63) | 0.84 (0.56) | <.001 | 0.99 |
| TAU | 1.49 (0.94) | 1.41 (0.81) | .614 (ns)a | 0.13 | |
| Secondary outcomes | |||||
| PMLDC frequency | aPM+ /TAU | 2.95 (0.57) | 2.51 (0.71) | .001 | 0.99 |
| TAU | 2.84 (0.53) | 2.85 (0.71) | .940 (ns) | 0.02 | |
| PMLDC distress | aPM+ /TAU | 5.40 (1.52) | 4.39 (1.70) | .001 | 0.98 |
| TAU | 5.42 (1.41) | 5.53 (1.93) | .707 (ns) | 0.08 | |
| ITQ PTSD | aPM+ /TAU | 13.67 (4.22) | 10.96 (5.50) | .005 | 0.61 |
| TAU | 14.8 (4.44) | 13.96 (5.98) | .422 (ns) | 0.16 | |
| ITQ DSO | aPM+ /TAU | 12.38 (5.05) | 10.21 (5.32) | .011 | 0.54 |
| TAU | 12.80 (6.32) | 12.40 (6.74) | .697 (ns) | 0.08 | |
| WHOQOL physical | aPM+ /TAU | 2.54 (0.62) | 2.30 (0.70) | .019 | 0.50 |
| TAU | 2.80 (0.73) | 2.89 (0.78) | .321 (ns) | 0.20 | |
| WHOQOL psychological | aPM+ /TAU | 3.14 (0.63) | 2.76 (0.67) | .004 | 0.64 |
| TAU | 3.08 (0.83) | 3.15 (0.89) | .460 (ns) | 0.15 | |
| WHOQOL social | aPM+ /TAU | 2.83 (0.83) | 2.54 (0.81) | .011 | 0.55 |
| TAU | 2.88 (0.70) | 2.88 (0.84) | 1.000 (ns) | 0 | |
| WHOQOL environment | aPM+ /TAU | 2.50 (0.48) | 2.35 (0.49) | .107 (ns) | 0.33 |
| TAU | 2.50 (0.56) | 2.42 (0.62) | .434 (ns) | 0.15 | |
| PSYCHLOPS | aPM+ /TAU | 4.61 (0.51) | 3.94 (0.74) | .002 | 0.74 |
| TAU | 4.59 (0.57) | 4.33 (0.54) | .095 (ns) | 0.35 | |
| IPL-12 integration | aPM+ /TAU | 2.41 (0.59) | 2.45 (0.55) | .688 (ns) | 0.08 |
| TAU | 2.49 (0.57) | 2.49 (0.52) | .970 (ns) | 0.001 | |
Note. a Nonparametric test because normality assumption was violated.
GHQ, General Health Questionnaire 28-item version; PMLDC, Post-Migration Living Difficulties Checklist; ITQ, International Trauma Questionnaire; WHOQOL, WHO Quality of Life Questionnaire; PSYCHLOPS, Psychological Outcome Profiles; IPL-12, Immigrant Integration Index 12-item version; aPM+, adapted Problem Management Plus; TAU, Treatment As Usual.
Follow-up comparisons revealed that the groups differed significantly post-intervention on GHQ anxiety/insomnia (d = 0.66), GHQ social dysfunction (d = 0.54), GHQ severe depression (d = 0.81), and GHQ total scores (d = 0.78), when controlling for age and asylum status. With regard to all these scales, the aPM+/TAU group demonstrated a lower GHQ score (see Table 4).
Table 4.
Post-intervention between group comparisons and summary statistics for primary and secondary outcomes.
| Timepoint | Descriptive statistics M (SD) | Analysis | |||
|---|---|---|---|---|---|
| aPM+/TAU | TAU | p-value | Effect size (Cohen’s d) | ||
| Primary outcomes | |||||
| GHQ total | Post-intervention | 4.83 (1.81) | 6.58 (2.61) | .006 | 0.78 |
| GHQ somatic | Post-intervention | 1.31 (0.64) | 1.70 (0.77) | .086 (ns) | 0.55 |
| GHQ anxiety/insomnia | Post-intervention | 1.37 (0.66) | 1.86 (0.81) | .025 | 0.66 |
| GHQ social dysfunction | Post-intervention | 1.30 (0.53) | 1.62 (0.65) | .024 | 0.54 |
| GHQ depression | Post-intervention | 0.84 (0.56) | 1.41 (0.81) | .003 | 0.81 |
| Secondary outcomes | |||||
| PMLDC frequency | Post-intervention | 2.51 (0.71) | 2.85 (0.71) | .123 (ns) | 0.48 |
| PMLDC distress | Post-intervention | 4.39 (1.70) | 5.53 (1.93) | .045 | 0.62 |
| ITQ PTSD | Post-intervention | 10.96 (5.50) | 13.96 (5.98) | .036 | 0.52 |
| ITQ DSO | Post-intervention | 10.21 (5.32) | 12.40 (6.74) | .082 (ns) | 0.36 |
| WHOQOL physical | Post-intervention | 2.30 (0.70) | 2.89 (0.78) | .017 | 0.79 |
| WHOQOL psychological | Post-intervention | 2.76 (0.67) | 3.15 (0.89) | .064 (ns) | 0.49 |
| WHOQOL social | Post-intervention | 2.54 (0.81) | 2.88 (0.84) | .195 (ns) | 0.41 |
| WHOQOL environment | Post-intervention | 2.35 (0.49) | 2.42 (0.62) | .300 (ns) | 0.13 |
| PSYCHLOPS | Post-intervention | 3.94 (0.74) | 4.33 (0.54) | .069 (ns) | 0.60 |
| IPL-12 integration | Post-intervention | 2.45 (0.55) | 2.49 (0.52) | .431 (ns) | 0.07 |
Note. GHQ, General Health Questionnaire 28-item version; PMLDC, Post-Migration Living Difficulties Checklist; ITQ, International Trauma Questionnaire; WHOQOL, WHO Quality of Life Questionnaire; PSYCHLOPS, Psychological Outcome Profiles; IPL-12, Immigrant Integration Index 12-item version; aPM+, adapted Problem Management Plus; TAU, Treatment As Usual.
3.2.2. Secondary outcomes
The most commonly reported main problems were classified as ‘primary postmigration stressors’, defined as stressors that can only occur after (forced) migration such as constant worry over a negative asylum decision. The second most common problems were classified as ‘general mental problems’ including cognitive and affective symptoms such as concentration problems or loneliness or other general mental health problems. The third most common main problems were classified as ‘interpersonal stressors’ and included any problems or concerns related to interpersonal situations such as worries about family members’ health or conflicts with others in the peer group.
The repeated measures group × timepoint × secondary outcome measure MANCOVA which controlled for age and asylum status revealed significant group × timepoint interactions for WHO physical health [F(1, 45) = 5.02, p = .030, partial η2 = 0.10], WHO psychological health [F(1, 45) = 6.63, p = .013, partial η2 = 0.13], and PMLDC distress [F(1, 45) = 4387, p = .033, partial η2 = 0.098]. The overall group × timepoint interaction collapsed across secondary outcome measures was found to be non-significant [F(10, 36) = 1.24, p = .302, partial η2 = 0.27].
When examining non-parametric paired sample t-tests, the aPM+/TAU group displayed significantly lower scores post-intervention as compared to baseline on ITQ PTSD symptoms (dz = 0.61), ITQ DSO symptoms (dz = 0.54), WHO physical health (dz = 0.50), WHO psychological health (dz = 0.64), WHO social relationships (dz = 0.55), PSYCHLOPS (dz = 0.74), PMLDC frequency (dz = 0.99), and PMLDC distress (dz = 0.98). The TAU group did not show significant differences when comparing outcomes post-intervention versus baseline (Table 3).
Follow-up comparisons revealed that the two groups differed significantly post-intervention on WHO physical health (d = 0.79), PMLDC distress (d = 0.62), and ITQ PTSD symptoms (d = 0.52), when controlling for age and asylum status (Table 4).
Throughout the study period, no participant reported an adverse event.
4. Discussion
This study tested the treatment effectiveness of a brief psychological treatment, aPM+, for Afghan refugees that was adapted to address general health symptoms and distress by PMLDs. APM+ led to moderate to large improvement in general health (GHQ), including somatic symptoms, anxiety/insomnia, social dysfunction, and severe depression post intervention compared to TAU. Further, the intervention was associated with reducing distress by PMLDs (PMLDC), symptoms of PTSD and DSO (ITQ), self-identified problems (PSYCHLOPS), and improved quality of life (WHOQOL).
Of the 88 randomized participants, 42% did not participate in the post-treatment assessment. However, of those who were randomized into the treatment and actually started the treatment, 81% completed all sessions (independently of participating in the post intervention assessment). This means that many help-seeking refugees cannot adequately be reached with interventions such as aPM+, but as soon as they actually take part in the intervention, the vast majority completes it. Apparently, there is a gap between asking for help when needed and actually receiving help. Despite general barriers towards seeking and getting professional help for mental health problems related to traumatic experiences (Kantor, Knefel, & Lueger-Schuster, 2017), refugees may be particularly hesitant towards mental health care (Colucci, Minas, Szwarc, Guerra, & Paxton, 2015). While structural barriers that are frequently reported as problematic in general health care systems (Kiselev et al., 2020) such as lack of financial resources or limited language skills can be ruled out in our study, socio-cultural barriers may be held responsible for the high attrition. These include culturally based explanations of mental health problems that mismatch our Western understanding, fear of mistreatment, distrust of doctors, fear of stigma, lack of mental health literacy, and lack of trust in systems (Kiselev et al., 2020). Future research should thus start earlier in the treatment process, investigating how refugees with mental health problems can be motivated to participate in psychological interventions. Further, about one fifth of those who started the intervention did not complete it, indicating that additional attention is required to improve treatment options for help-seeking refugees.
While previous studies showed the effectiveness of psychosocial interventions targeting PTSD in refugees resettled in high-income countries (Nosè et al., 2017; Turrini et al., 2021), the present study utilized a transdiagnostic intervention. Despite PTSD being a prominent diagnosis associated with forced migration, depression and anxiety are equally common in refugees (Turrini et al., 2017). Using a brief, structured psychological intervention, we provide results that these symptoms can be efficiently addressed. Individual PM+ was previously evaluated in large-scale clinical trials in Kenya and Pakistan (Bryant et al., 2017; Rahman et al., 2016) yielding comparable effects post intervention as our study. In contrast to our procedure, the intervention was facilitated by lay therapists in the previous trials, and the samples differed markedly. Participants in Kenya were women with experiences of gender-based violence who were identified through a random community screening (Bryant et al., 2017). Participants in Pakistan were routine patients from primary care centers with emotional distress (Rahman et al., 2016). Help-seeking refugees may suffer from more severe distress and mental problems compared to these populations. Thus, aPM+ delivered by mental health professionals, seems to be as effective for a presumably more impaired population as classic PM+ delivered by lay therapists, for less impaired populations. In their feasibility trial, Graaff et al. (2020) found that individual PM+ delivered by lay-therapists might be effective for Syrian refugees. Compared to this study with a similar sample size, we found larger effects. However, our study included an additional session and neither study was powered to directly compare the effects of different treatment facilitators.
In recent years, several transdiagnostic treatment programmes aiming to reduce distress among refugees have been evaluated (Bolton et al., 2014; Dawson et al., 2015; Koch et al., 2020; Tay et al., 2020; van Heemstra, Scholte, Haagen, & Boelen, 2019). Some of these programmes directly aimed to reduce distress caused by PMLDs, however, to the best of our knowledge, no study systematically assessed the presence of PMLDs before and after the intervention. For this purpose, we adapted the PMLDC (Silove et al., 1997) to assess how often a specific stressor occurred and how distressing it was. We found that distress by PMLDs was reduced in the aPM+ group. As conditions in host countries are important predictors for mental health (Chu et al., 2013), this result is of high practical relevance. Future trials should include a formal measure of specific problems related to migration and differentiate between frequency of and distress caused by these problems.
This study has several limitations. The pandemic-related changes of the study design, including omission of the 6-month follow-up, limit the results to a pre–post comparison only. A longer observational period may have led to weaker results regarding the effectiveness of the intervention (Purgato et al., 2021). In addition, the final sample size was lower than planned. Several factors may have contributed to this. The drop-out rate was higher than expected and the recruitment had to be stopped before the intended sample size was reached. The SARS-CoV2 pandemic may have aggravated mental health problems and reduced functioning (Rees & Fisher, 2020), potentially contributing to the drop-out rate. This smaller sample size is associated with smaller power to detect meaningful effects in our study. The reported effects are limited by larger variation, i.e. they are poorer estimates of the real effects as compared to reaching the intended sample size. Our results should also be interpreted with caution given our per-protocol (completers only) analysis method. The reported clinical results are those one can expect if someone completes the treatment, as opposed to how well the treatment works generally. Of importance, both groups had equal numbers of participants drop out, and all clinical outcome variables did not differ significantly between completers and those who dropped out within groups. Further, we did not exclude participants with insecure asylum status. Afghan people are regularly deported from Austria if they receive a negative decision on asylum. Given that a large number of participants reported no secure asylum status at baseline, an unknown number might have either been deported or gone into hiding during the study period. Overall, the pandemic might limit the generalizability of our results. As the governmental measures and restrictions related to the pandemic affected participants from both arms alike, we expect that no relevant group differences arose from this fact but cannot rule out that our results may not be fully comparable to results from studies carried out before or after the pandemic. Additionally, the TAU interventions were not protocolized and we have no systematic knowledge about potential effects of these interventions. We did not compare the adapted version of PM+ to the original version of PM+. Consequently, we cannot know if the provision of an additional sixth session was helpful over and above the benefits of the original manual. Also, while offering two options for the additional session may have strengthened our participants’ sense of self-efficacy, it limits the validity of our study. Although treatment fidelity was ensured by regular supervision with PM+ master trainers and self-assessed by the therapists using a standardized checklist after the sessions, we did not employ fidelity checks such as audio/video analyses of single sessions. Moreover, some of the measures used in our study should be interpreted with caution: The PSYCHLOPS had low reliability in terms of internal consistency, similar to previous research (Bryant et al., 2017). While this may be associated with higher validity, it is problematic to interpret the sum score used in our analysis. The PMLDC was adapted for the present study, limiting its comparability to other studies and potentially reducing the measures construct validity. Our results thus need replication in future research. Finally, we did not assess the extent to which assessors’ blinding was maintained throughout the trial and could thus not carry out formal analyses in this regard.
5. Conclusions
In conclusion, aPM+ was effective in reducing general health problems in Afghan refugees in the short-term. This brief transdiagnostic psychological intervention might be considered as first-line intervention for help-seeking refugees with mental health problems. While longer follow-up periods are still required and recommending a larger-scaled rollout may be too early, focusing mental health support for refugees not only on trauma-specific psychopathology such as PTSD might better address their actual needs, particularly when handling migration-related stressors is also included in treatment planning.
Supplementary Material
Acknowledgments
We are grateful to all the Afghan asylum seekers and refugees who participated in this study and who shared their experiences with us. Further thanks are due to the Outpatient Unit for Research, Teaching, and Practice at the Faculty of Psychology of the University of Vienna as well as to the non-governmental organizations and outpatient treatment centers in Vienna who supported us. Finally, we are thankful for the support from Alexandra Liedl, Naser Morina, Mahmoud Hemmo, and Maria Böttche acting as external advisory consultants and clinical supervisors.
Funding Statement
This study was funded by the Austrian Science Fund (FWF) (grant number: KLI 755-B).
Note
In this paper, we use “refugees” as an umbrella term, which denotes all asylum seekers regardless of the recognition of their claim.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethics
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, MK, upon reasonable request and will be available in a public repository once the research project will be completed.
References
- Alemi, Q., James, S., Cruz, R., Zepeda, V., & Racadio, M. (2014). Psychological distress in Afghan refugees: A mixed-method systematic review. Journal of Immigrant and Minority Health, 16(6), 1247–1261. doi: 10.1007/s10903-013-9861-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashworth, M., Shepherd, M., Christey, J., Matthews, V., Wright, K., Parmentier, H., … Godfrey, E. (2004). A client-generated psychometric instrument: The development of ‘PSYCHLOPS’. Counselling and Psychotherapy Research, 4(2), 27–31. doi: 10.1080/14733140412331383913 [DOI] [Google Scholar]
- Bolton, P., Lee, C., Haroz, E. E., Murray, L., Dorsey, S., Robinson, C., … Bass, J. (2014). A transdiagnostic community-based mental health treatment for comorbid disorders: Development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLoS Medicine, 11(11), e1001757. doi: 10.1371/journal.pmed.1001757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant, R. A., Schafer, A., Dawson, K. S., Anjuri, D., Mulili, C., Ndogoni, L., … van Ommeren, M. (2017). Effectiveness of a brief behavioural intervention on psychological distress among women with a history of gender-based violence in urban Kenya: A randomised clinical trial. PLoS Medicine, 14(8), e1002371. doi: 10.1371/journal.pmed.1002371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundesministerium für Inneres . (2020). Asylstatistik 2020 [Austrian Federal Ministry of Internal Affairs; Asylumstatistics 2020]. http://www.bmi.gv.at/301/Statistiken/start.aspx.
- Chu, T., Keller, A. S., & Rasmussen, A. (2013). Effects of post-migration factors on PTSD outcomes among immigrant survivors of political violence. Journal of Immigrant and Minority Health, 15(5), 890–897. doi: 10.1007/s10903-012-9696-1 [DOI] [PubMed] [Google Scholar]
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. doi: 10.1111/acps.12956 [DOI] [PubMed] [Google Scholar]
- Colucci, E., Minas, H., Szwarc, J., Guerra, C., & Paxton, G. (2015). In or out? Barriers and facilitators to refugee-background young people accessing mental health services. Transcultural Psychiatry, 52(6), 766–790. doi: 10.1177/1363461515571624 [DOI] [PubMed] [Google Scholar]
- Dawson, K. S., Bryant, R. A., Harper, M., Kuowei Tay, A., Rahman, A., Schafer, A., & van Ommeren, M. (2015). Problem Management Plus (PM+): A WHO transdiagnostic psychological intervention for common mental health problems. World Psychiatry, 14(3), 354–357. doi: 10.1002/wps.20255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drescher, A., Kiselev, N., Akhtar, A., Acarturk, C., Bryant, R. A., Ilkkursun, Z., … Morina, N. [. (2021). Problems after flight: Understanding and comparing Syrians’ perspectives in the Middle East and Europe. BMC Public Health, 21(1), 717. doi: 10.1186/s12889-021-10498-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggenhofer-Rehart, P. M., Latzke, M., Pernkopf, K., Zellhofer, D., Mayrhofer, W., & Steyrer, J. (2018). Refugees’ career capital welcome? Afghan and Syrian refugee job seekers in Austria. Journal of Vocational Behavior, 105, 31–45. doi: 10.1016/j.jvb.2018.01.004 [DOI] [Google Scholar]
- Georges, D., Buber-Ennser, I., Rengs, B., Kohlenberger, J., & Doblhammer, G. (2021). Health determinants among refugees in Austria and Germany: A propensity-matched comparative study for Syrian, Afghan, and Iraqi refugees. PloS One, 16(4), e0250821. doi: 10.1371/journal.pone.0250821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghazinour, M., Richter, J., & Eisemann, M. (2004). Quality of life Among Iranian refugees resettled in Sweden. Journal of Immigrant Health, 6(2), 71–81. doi: 10.1023/B:JOIH.0000019167.04252.58 [DOI] [PubMed] [Google Scholar]
- Goldberg, D. (1978). Manual of the General Health Questionnaire. Windsor, England: NFER-Nelson. [Google Scholar]
- Goldberg, D., Gater, R., Sartorius, N., Ustun, T. B., Piccinelli, M., Gureje, O., & Rutter, C. (1997). The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychological Medicine, 27(1), 191–197. doi: 10.1017/S0033291796004242 [DOI] [PubMed] [Google Scholar]
- Graaff, A. M. d., Cuijpers, P., McDaid, D., Park, A., Woodward, A., Bryant, R. A., … Sijbrandij, M. (2020). Peer-provided Problem Management Plus (PM+) for adult Syrian refugees: A pilot randomised controlled trial on effectiveness and cost-effectiveness. Epidemiology and Psychiatric Sciences, 29, 1–24. doi: 10.1017/S2045796020000724 [DOI] [Google Scholar]
- Hamrah, M. S., Hoang, H., Mond, J., Pahlavanzade, B., Charkazi, A., & Auckland, S. (2020). The prevalence and correlates of symptoms of post-traumatic stress disorder (PTSD) among resettled Afghan refugees in a regional area of Australia. Journal of Mental Health (Abingdon, England), 30, 1–7. doi: 10.1080/09638237.2020.1739247 [DOI] [PubMed] [Google Scholar]
- Harder, N., Figueroa, L., Gillum, R. M., Hangartner, D., Laitin, D. D., & Hainmueller, J. (2018). Multidimensional measure of immigrant integration. Proceedings of the National Academy of Sciences of the United States of America, 115(45), 11483–11488. doi: 10.1073/pnas.1808793115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartonen, V. R., Väisänen, P., Karlsson, L., & Pöllänen, S. (2020). ‘Between heaven and hell’: Subjective well-being of asylum seekers. International Journal of Social Welfare, 30, 30–45. doi: 10.1111/ijsw.12435 [DOI] [Google Scholar]
- Hollifield, M., Verbillis-Kolp, S., Farmer, B., Toolson, E. C., Woldehaimanot, T., Yamazaki, J., … SooHoo, J. (2013). The refugee health screener-15 (RHS-15): Development and validation of an instrument for anxiety, depression, and PTSD in refugees. General Hospital Psychiatry, 35(2), 202–209. doi: 10.1016/j.genhosppsych.2012.12.002 [DOI] [PubMed] [Google Scholar]
- Hou, W. K., Liu, H., Liang, L., Ho, J., Kim, H., Seong, E., … Hall, B. J. (2019). Everyday life experiences and mental health among conflict-affected forced migrants: A meta-analysis. Journal of Affective Disorders, 264, 50–68. doi: 10.1016/j.jad.2019.11.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantor, V., Knefel, M., & Lueger-Schuster, B. (2017). Perceived barriers and facilitators of mental health service utilization in adult trauma survivors: A systematic review. Clinical Psychology Review, 52, 52–68. doi: 10.1016/j.cpr.2016.12.001 [DOI] [PubMed] [Google Scholar]
- Kiselev, N., Pfaltz, M., Haas, F., Schick, M., Kappen, M., Sijbrandij, M., … Morina, N. [. (2020). Structural and socio-cultural barriers to accessing mental healthcare among Syrian refugees and asylum seekers in Switzerland. European Journal of Psychotraumatology, 11(1), 1717825. doi: 10.1080/20008198.2020.1717825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knefel, M., Kantor, V., Schiess-Jokanovic, J., Weindl, D., Schäfer, I., & Lueger-Schuster, B. (2020). A brief transdiagnostic psychological intervention for Afghan asylum seekers and refugees in Austria: A randomized controlled trial. Trials, 21(1), 57. doi: 10.1186/s13063-019-3839-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch, T., Ehring, T., & Liedl, A. (2020). Effectiveness of a transdiagnostic group intervention to enhance emotion regulation in young Afghan refugees: A pilot randomized controlled study. Behaviour Research and Therapy, 132, 103689. doi: 10.1016/j.brat.2020.103689 [DOI] [PubMed] [Google Scholar]
- Koesters, M., Barbui, C., & Purgato, M. (2018). Recent approaches to provision of mental healthcare in refugee populations. Current Opinion in Psychiatry, 31(4), 368–372. doi: 10.1097/YCO.0000000000000428 [DOI] [PubMed] [Google Scholar]
- Linehan, M. (2015). Dbt Skills Training Manual (2nd Ed). New York: The Guilford Press. [Google Scholar]
- Mollica, R. F., Caspi-Yavin, Y., Bollini, P., Truong, T., Tor, S., & Lavelle, J. (1992). The Harvard Trauma Questionnaire: Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in indochinese refugees. The Journal of Nervous and Mental Disease, 180(2), 111–116. doi: 10.1097/00005053-199202000-00008 [DOI] [PubMed] [Google Scholar]
- Nickerson, A., Byrow, Y., O'Donnell, M., Mau, V., McMahon, T., Pajak, R., … Liddell, B. J. (2019). The association between visa insecurity and mental health, disability and social engagement in refugees living in Australia. European Journal of Psychotraumatology, 10(1), 1688129. doi: 10.1080/20008198.2019.1688129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosè, M., Ballette, F., Bighelli, I., Turrini, G., Purgato, M., Tol, W., … Barbui, C. (2017). Psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in high-income countries: Systematic review and meta-analysis. Plos One, 12(2), e0171030. doi: 10.1371/journal.pone.0171030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purgato, M., Carswell, K., Tedeschi, F., Acarturk, C., Anttila, M., Au, T., … Barbui, C. (2021). Effectiveness of self-help Plus in preventing mental disorders in refugees and asylum seekers in Western Europe: A multinational randomized controlled trial. Psychotherapy and Psychosomatics, 90, 1–12. doi: 10.1159/000517504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, A., Hamdani, S. U., Awan, N. R., Bryant, R. A., Dawson, K. S., Khan, M. F., … van Ommeren, M. (2016). Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: A randomized clinical trial. JAMA, 316(24), 2609–2617. doi: 10.1001/jama.2016.17165 [DOI] [PubMed] [Google Scholar]
- Rees, S., & Fisher, J. (2020). COVID-19 and the mental health of people from refugee backgrounds. International Journal of Health Services: Planning, Administration, Evaluation, 50(4), 415–417. doi: 10.1177/0020731420942475 [DOI] [PubMed] [Google Scholar]
- Röhrbein, A. (2019). Der ressourcenbaum – vergangenes, gegenwärtiges und zukünftiges in einem. In Eickhorst A., & Röhrbein A. (Eds.), Systemische Methoden in Familienberatung und -Therapie (pp. 321–336). Göttingen: Vandenhoeck & Ruprecht. 10.13109/9783666406225.321. [DOI] [Google Scholar]
- Sijbrandij, M., Acarturk, C., Bird, M., Bryant, R. A., Burchert, S., Carswell, K., … Cuijpers, P. (2017). Strengthening mental health care systems for Syrian refugees in Europe and the Middle East: Integrating scalable psychological interventions in eight countries. European Journal of Psychotraumatology, 8(sup2), 1388102. doi: 10.1080/20008198.2017.1388102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sijbrandij, M., Graaf, A. d., Cuijpers, P., & Kieft, B. (2020). Problem Management Plus (PM+) for Syrian refugees in the Netherlands: 16th World congress on Public Health. European Journal of Public Health, 30(Supplement 5), v233–v234. doi: 10.1093/eurpub/ckaa165.628 [DOI] [Google Scholar]
- Silove, D., Sinnerbrink, I., Field, A., Manicavasagar, V., & Steel, Z. (1997). Anxiety, depression and PTSD in asylum-seekers: Assocations with pre-migration trauma and post-migration stressors. The British Journal of Psychiatry, 170, 351–357. doi: 10.1192/bjp.170.4.351 [DOI] [PubMed] [Google Scholar]
- Sulaiman-Hill, C. M. R., & Thompson, S. C. (2012). Afghan and Kurdish refugees, 8-20 years after resettlement, still experience psychological distress and challenges to well being. Australian and New Zealand Journal of Public Health, 36(2), 126–134. doi: 10.1111/j.1753-6405.2011.00778.x [DOI] [PubMed] [Google Scholar]
- Tay, A. K., Mung, H. K., Miah, M. A. A., Balasundaram, S., Ventevogel, P., Badrudduza, M., … Silove, D. (2020). An integrative adapt therapy for common mental health symptoms and adaptive stress amongst Rohingya, Chin, and Kachin refugees living in Malaysia: A randomized controlled trial. PLoS Medicine, 17(3), e1003073. doi: 10.1371/journal.pmed.1003073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trilesnik, B., Altunoz, U., Wesolowski, J., Eckhoff, L., Ozkan, I., Loos, K., … Graef-Calliess, I. T. (2019). Implementing a need-adapted stepped-care model for mental health of refugees: Preliminary data of the state-funded project “RefuKey”. Frontiers in Psychiatry, 10, 688. doi: 10.3389/fpsyt.2019.00688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripepi, G., Chesnaye, N. C., Dekker, F. W., Zoccali, C., & Jager, K. J. (2020). Intention to treat and per protocol analysis in clinical trials. Nephrology (Carlton, Vic.), 25(7), 513–517. doi: 10.1111/nep.13709 [DOI] [PubMed] [Google Scholar]
- Turrini, G., Purgato, M., Ballette, F., Nosè, M., Ostuzzi, G., & Barbui, C. (2017). Common mental disorders in asylum seekers and refugees: Umbrella review of prevalence and intervention studies. International Journal of Mental Health Systems, 11, 51. doi: 10.1186/s13033-017-0156-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turrini, G., Tedeschi, F., Cuijpers, P., Del Giovane, C., Kip, A., Morina, N., … Barbui, C. (2021). A network meta-analysis of psychosocial interventions for refugees and asylum seekers with PTSD. BMJ Global Health, 6(6), 1–11. doi: 10.1136/bmjgh-2021-005029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNHCR . (2020). Global Trends: Forced Displacement in 2019. http://www.unhcr.org/refugee-statistics.
- van Heemstra, H. E., Scholte, W. F., Haagen, J. F. G., & Boelen, P. A. (2019). 7roses, a transdiagnostic intervention for promoting self-efficacy in traumatized refugees: A first quantitative evaluation. European Journal of Psychotraumatology, 10(1), 1673062. doi: 10.1080/20008198.2019.1673062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells, R., Wells, D., & Lawsin, D. (2015). Understanding psychological responses to trauma among refugees: The importance of measurement validity in crosscultural settings. Journal and Proceedings of the Royal Society of New South Wales, 148(455), 60–69. [Google Scholar]
- Whoqol Group . (1994). Development of the WHOQOL: Rationale and current status. International Journal of Mental Health, 23(3), 24–56. doi: 10.1080/00207411.1994.11449286 [DOI] [Google Scholar]
- World Health Organization . (2016a). mhGAP Intervention Guide for Mental, Neurological and Substance use Disorders in non-Specialized Health Settings: Mental Health gap Action Programme (mhGAP) (Version 2.0). Geneva: World Health Organization. [PubMed] [Google Scholar]
- World Health Organization . (2016b). Problem Management Plus (PM+): Individual Psychological Help for Adults Impaired by Distress in Communities Exposed to Adversity. WHO Generic Field-Trial Version. Geneva: WHO. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, MK, upon reasonable request and will be available in a public repository once the research project will be completed.