ABSTRACT
Vaccine hesitancy is one of the top ten global health threats and the first threat to fighting COVID-19 through vaccination. With the increasing level of COVID-19 vaccine hesitancy amidst the rising level of confirmed cases and death tolls, this paper provides rapid systematic literature reviews on the measurement of COVID-19 vaccine hesitancy, key determinants and evidence-based strategies to prevent COVID-19 vaccine hesitancy. The findings reveal three standard measures of vaccine hesitancy: optional response questions, Likert scale, and linear scale measurements. Factors such as sociodemographic/economic factors, occupational factors, knowledge on the vaccine, vaccine attributes, conspiracy belief and psychological factors are the major predictors of COVID-19 vaccine hesitancy. Evidence-based findings identified measures such as effective education on the vaccine, clear and consistent communication to build public confidence and trust, health education on vaccination and its social benefit, outreach program and targeted messaging to minimize COVID-19 vaccine hesitancy.
KEYWORDS: COVID-19 vaccine, hesitancy, coronavirus, measurement, predictors, preventive measures, strategies, public health
1. Introduction
Following the outbreak of Coronavirus disease (COVID-19), an infectious disease caused by the SARS-CoV-2 which has affected over 100 millions people, claimed 2 million lives globally, collapsed businesses and economy,1–4 bold steps and actions by governments and entities resulted in production of COVID-19 vaccines as ultimate intervention against the deadly virus. The purpose of this milestone achievement in the production of COVID-19 vaccines is to make these vaccines accessible or distributed across every country especially where cases of COVID-19 infections were confirmed. The effectiveness of any vaccination effort is contingent on the percentage of the population that is willing to be vaccinated, and according to current projections, it is possible that up to three-quarters of the population will need immunization in order to put the pandemic to a close.5–7 Empirical and anecdotal evidence from global and country levels studies, however, show an increasing level of hesitancy of COVID-19 vaccine ranging from 20 to 80% and declining level of vaccine acceptance ranges from about 7 to 50% and this raises an important challenge to public health.
Vaccine hesitancy is defined by the World Health Organization (WHO) Strategic Advisory Group of Experts on Immunization as a “delay in acceptance or refusal of vaccination despite availability of vaccination services,”8–12 which may take on different forms and intensities depending on when and where it happens, as well as the vaccine that is involved.13 WHO10 has highlighted vaccine hesitancy as one of the top ten global health problems for 2019; in fact, it was named as one of the top ten global health hazards in 2018. Anti-vaccine sentiment and disinformation are major hurdles to increasing vaccination coverage and community immunity in many countries.7,14 According to models with a vaccine efficacy of 80%, the percentage of the population that needs to be vaccinated to reach herd immunity ranges from 75 to 90% (depending on factors such as the basic reproduction number, vaccine-induced immunity duration, and whether vaccines prevent transmission).15 A considerable proportion of the world’s population report that they are hesitant to get vaccinated, and although vaccine hesitancy varies from country to country, it remains alarmingly high in many areas. As a consequence, and despite recent advances in certain countries, the rates of vaccination intention continue to be below the proportion necessary for herd immunity in the majority of nations, and rates of vaccination intention are declining and this has received a global attention in research and policy direction.
While a plethora of studies exist on COVID-19 vaccine hesitancy, there is a scanty of systematic review in the literature on COVID-19 vaccine hesitancy. For instance5 review compared trends and synthesized findings in vaccination receptivity over time across US and international polls. Robinson et al.6 review analyzed trends and consolidated data in vaccine receptivity over time across surveys conducted in the United States and elsewhere. The goal of the6 study was to estimate the percentage of the global population wanting to get vaccinated versus the proportion of the global population planning to reject a vaccination when COVID-19 vaccines become available and how this tendency has evolved over time, using large and nationally representative samples. One key interest to policymakers is the evidence-based findings on how to minimize COVID-19 vaccine hesitancy, that is hesitancy corrective measure (to maximize public patronage) yet this has not been systematically reviewed in the extant literature. Additionally, there is a need to go beyond trend analysis and demographic predictors to emerging and updated findings on other characteristics that predict vaccine hesitancy and measurement. Consequently, there is an urgent need for a more updated and nuanced understanding of factors determining vaccine hesitancy and corrective measures in the context of the COVID-19 pandemic. This systematic review therefore seeks to address the following research questions: What is the standard measurement of hesitancy of COVID-19 vaccine in the literature? What are the predictors (up to date) of hesitancy of COVID-19 vaccine? What are the evidence-based measures in the literature to prevent vaccine hesitancy and promote public patronage of COVID-19 vaccine? Addressing these critical questions will not only contribute to the field of research but also help policymakers, healthcare workers, and other authorities to plan ahead toward minimizing the impact on public health from vaccine hesitancy by improving the global vaccination program. As the first step, we conducted a systematic review of all the studies related to hesitancy of COVID-19 vaccine. The aim of this review is to identify the measurement of hesitancy, key emerging predictors and hesitancy corrective measures that promote public patronage of COVID-19 vaccine.
Following this introduction and background section, is Section 2 that highlights the method used for the review. Section 3 presents the results while Sections 4 and 5, respectively, document the discussions of the results and conclusions based on the findings.
2. Method
This section covers study selection strategy, study design, eligibility, inclusive and exclusive criteria, and quality of assessment and synthesis.
2.1. Study selection strategy
Peer-reviewed studies were selected (from 2020 to 2021) for systematic reviews according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to ensure reproducibility and transparency of our findings. The selection of literature is informed by the key research questions; What is the standard measurement of hesitancy of COVID-19 vaccine in the literature? What are the predictors (up to date) of hesitancy of COVID-19 vaccine? What corrective measures are available to minimize vaccine hesitancy to promote public patronage of COVID-19 vaccine? To do this, a comprehensive literature (from the year 2020 to 2021) was conducted from the following electronic databases: MEDLINE (via LitCOVID in PubMed), Google scholar, Cochrane Library, African Index Medicus, and EBSCOhost. Primary concepts such as “vaccine hesitancy,” “COVID-19 vaccine hesitancy,” “willingness to be vaccinated,” “acceptance of COVID-19 vaccine,” “receptivity for COVID-19 vaccine,” “confidence in COVID-19 vaccine,” “trust in COVID-19 vaccine,” “measurement of vaccine hesitancy,” “predictors of vaccine hesitancy,” “factors associated with vaccine hesitancy,” and “promoting public vaccination” were used for the search. The subject and text word search were performed separately in all the databases and then combined with Boolean operators “OR” and “AND.” For a more thorough search, reference lists of pertinent publications and associated documents from databases by the World Health Organization (WHO) and the African Centers for Disease Control and Prevention (Africa CDC) were also checked for possibly relevant articles. To assess eligibility, two researchers reviewed the titles and abstracts of the search results before doing full-text reviews. Any differences were handled by reaching an agreement among the two researchers. When a possible survey was mentioned in an article, the author searched the original press release or official report to verify the information. To be eligible for inclusion, publications at minimum had to report on the measurement of COVID-19 vaccine hesitancy, predictors, or factors associated with COVID-19 vaccine hesitancy and empirical measures to minimize vaccine hesitancy and promote public vaccination. Details of eligibility criteria, quality assessment, and synthesis are provided in the following sections.
2.2. Study design eligible inclusion and exclusion criteria
To be eligible, studies were required to include questions that measure hesitancy/intentions/willingness to use a vaccine for COVID-19 when one becomes available (e.g. ‘I would use a vaccine for COVID-19 when it becomes available’), predict hesitancy of COVID-19 vaccine, and evidence-based findings on minimizing vaccination hesitancy and promoting public vaccination. For the purposes of this review, only research written in the English language that satisfied the inclusion criteria were taken into consideration. Other criteria for inclusion were peer-reviewed scientific publications published in peer-reviewed journals; survey studies of the general public, health-care professionals, students, or parents/guardians; and studies of the general public, health-care workers, students, or parents/guardians. The exclusion criteria were: (1) unpublished manuscripts (preprints); (2) the article did not aim to measure, predict and minimize COVID-19 hesitancy/ acceptance/hesitancy; and (3) publication language was not English.
2.3. Quality of assessment
The quality assessment of the studies as stipulated in the PRISMA-P statement in relation to the screening process was performed. The protocol of the screening process involved looking into the research aim of each study and if it answered any of the research questions of this study. Secondly, the quality assessment also focused on the measurement of hesitancy, predictors/factors, and evidence-based findings on minimizing COVID-19 vaccine hesitancy (that is promoting public vaccination). Furthermore, to facilitate a rapid review and address limitations posed by the observational nature of surveys, study quality was assessed by survey administration, sample size, nature of study, study design, and the research questions sought to address. Finally, the sample size of these studies was reduced as some studies failed to meet this quality assessment procedure. Following the inclusion and exclusion criteria, two reviewers worked together to independently evaluate the titles and abstracts for appropriateness. These two reviewers assessed the possibility of bias and extracted data; discrepancies were resolved via discussion. The other 350 papers were subjected to full-text screening using the same criteria. It was necessary to repeat the individual screening procedure in order to verify for consistency, and no discrepancies were discovered. A quality score out of ten was assigned using the Critical Appraisal Skills Programme.16
2.4. Synthesis
A range of techniques were employed to form the synthesis of the evidence, based on the recommendation by.17 Findings were synthesized narratively and provide thematic classification according to the objective of the review, tabulate the summarized results, and explore relationships with discussions. For the sake of maintaining consistency with primary-order outcomes and avoiding duplication of the authors’ interpretations, only data from the findings and results section were used. The remaining 25 papers were reviewed by both reviewers, who each made unique notes on the major significant topics. Inductive categorization was used throughout the screening process, therefore there were no disagreements.
3. Results
In this rapid systematic review, a sample of 25 studies were used and the geographical precinct of these studies is not restricted to a particular area, but rather there are studies from Saudi Arabia, USA, France, UK, Israel, Italy, Canada, Nigeria, China, and few global studies. The search and selection criteria included peer-reviewed publications, which were identified using the search criteria terms as described above. During the search, 470 potential studies were identified, 130 titles and abstracts were excluded as nonscientific. 340 papers were retrieved which reduced to 220 after removing duplicates and ultimately, 18 papers were left after thorough assessment of the papers using the inclusion and exclusion criteria. This process is fully illustrated in Figure 1 on PRIMA flow diagram.
Figure 1.
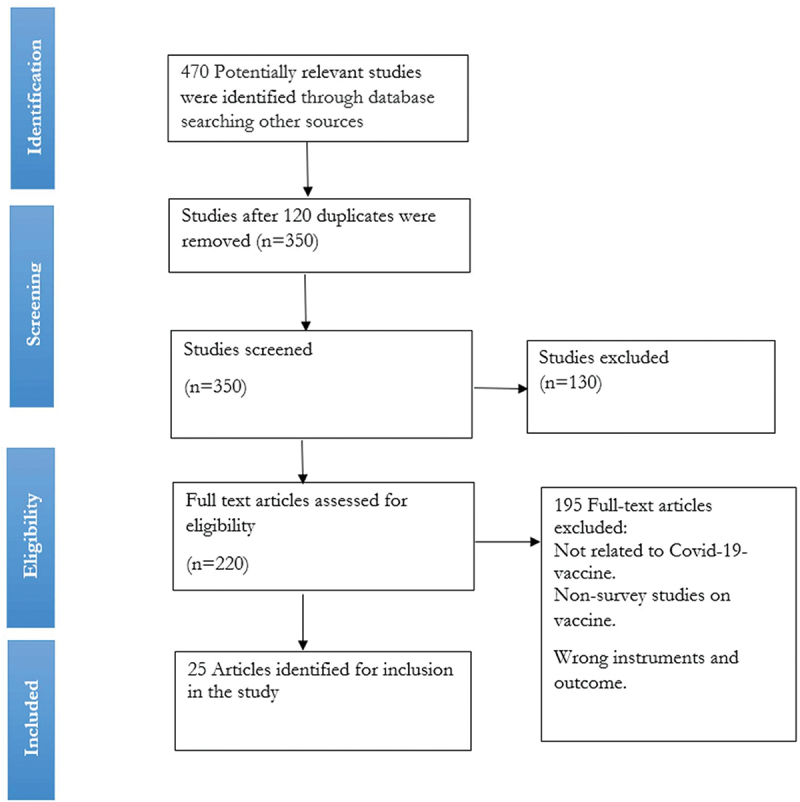
Prisma flow diagram of study search and selection.
3.1. Study characteristics
3.1.1. Location
The empirical studies on the COVID-19 hesitancy literature cover different locations/countries often associated with different socio-cultural backgrounds and characteristics. Three studies focused on global context5,9,18 others were on specific countries from the developed countries such as USA, where about nine studies were conducted,8,19–26 Saudi Arabia,27 France,28 UK,29 Israel,30 Italy,31,32 Canada,33 Nigeria,34 and China.35,36
3.1.2. Aims of the studies
The review is based on carefully selected studies that focus on the research questions in this study. It includes studies that aim in understanding the correlates of COVID-19 vaccine hesitancy and the reasons why individuals intend to refuse to a COVID-19 vaccine,8,19 prevalence of the acceptance of COVID-19 vaccine and their determinants,27 the frequency and variables associated with COVID-19 vaccine20 and understand COVID-19 vaccine hesitancy in an ethnically diverse and deprived population.29 Other studies sought to study vaccine attitudes and the variables that influence vaccine intent in the context of the COVID-19 pandemic,37 as well as to assess the adoption of COVID-19 vaccination in China and provide recommendations for vaccination strategies.36
3.2. Study methodology
3.2.1. Sample
The sample size used varies across different studies in the literature depending on target participants, study area, design, and the purpose of the study. Thus, no standard sample size has been established in the literature. The largest study sample size was 58,656 which was a study done in the global context.9,37 Study by Lin et al.5 was a systematic review studies with 126 selected studies or reports. Other studies with relatively larger samples of 32,361, 7662, and 3479, were conducted in various countries such as UK,37 seven European countries,18 and USA,25 respectively.
3.2.2. Nature of study and design
The existing studies on the measurement of vaccine hesitancy, predictors and hesitancy preventive measures are largely the combination of qualitative and quantitative studies with survey design8,19,22,27 and one exploratory study.33
3.3. Findings
Table 1 provides summary of studies on COVID-19 hesitancy (measurements, predictors, and hesitancy preventive measures) that have been validated for use in this review. Here, we present findings on each aspect of interest, that is, measurements of COVID-19 vaccine hesitancy, predictors or factors associated with COVID-19 vaccine hesitancy and preventive measures for COVID-19 vaccine hesitancy.
Table 1.
Summary of studies on the COVID-19 vaccine hesitancy: measurement, key predictors, and prevention.
| Study Characteristics |
Study methodology |
Findings |
||||||
|---|---|---|---|---|---|---|---|---|
| Authors and year | Location/Country | Study aims | Sample | Nature of study | Type of study design | Measurements COVDI-19 Vaccination hesitancy | Predictors of vaccine hesitancy | Strategies/Measures to prevent COVID-19 vaccine hesitancy |
| (Al-Mohaithef & Padhi, 2020)27 | Saudi Arabia | To assess the prevalence of the acceptance of COVID-19 vaccine and their determinants among people in Saudi Arabia | 992 | Qualitative and quantitative study | Survey design | Willingness to take the vaccine with the following response options, Yes/No/Not sure. |
Willingness to accept the future COVID-19 vaccination rates are quite high among older age groups, who are married participants with a postgraduate degree or above and work in the government sector. | To promote COVID-19 vaccination, it is necessary to address sociodemographic factors associated with the vaccination and implement targeted health education programs. |
| (Callaghan et al., 2020)19 | USA | To understand the correlates of COVID-19 vaccine hesitancy in the American public and the reasons why individuals intend to refuse to a COVID-19 vaccine | 5009 | Qualitative and quantitative | Survey design | Willingness to take the vaccine with binary response options: Yes/no. | women, conservatives, those see vaccines unimportant/ineffective, Trump voters, religious people are less likely to be vaccinated. Those |
Design health message targeted at hesitant group. |
| (Campo-Arias & Pedrozo-Pupo, 2021)20 | USA | The study aimed to know the frequency and variables associated with COVID-19 vaccine distrust in students of a Colombian university | 1,136 | Qualitative and quantitative study | Survey design | Likert scale with four point on trust in COVID-19 vaccine: “strongly disagree,” “disagree,” “agree,” and “strongly agree,” which are scored from 0 to 3. | Colombian university students have a significant level of distrust in the COVID-19 vaccination. The COVID-19 vaccine distrust is related to non-health science carriers, rural residents, low-income, and low- perceived stress related to COVID-19. | The COVID-19-related health literacy and education should be improved in students of university considering socio-cultural background. |
| (Detoc et al., 2020)28 | France | To determine the proportion of people who intend to get vaccinated against COVID-19 in France or to participate in a vaccine clinical trial | 2512+ | Qualitative and quantitative | Survey design | Willingness to take the vaccine with the following options; Yes, certainly/ yes, possibly/I don’t know/No, possibly/ Definitely no. | Men, older, fear of COVID-19, perceived risk are less hesitant. |
Vaccine hesitancy will be the major barrier to COVID- 19 vaccine uptake and therefore must be addressed through education. |
| (Dickerson et al., 2021)29 | UK | The study aims to understand COVID-19 vaccine hesitancy in an ethnically diverse and deprived population | 535 | Qualitative | Survey design | Options from the following list were used to measure the vaccination hesitancy: I have not yet thought about it, I am not yet sure about it, I have decided I do want it, I have decided I do not want it. | Confusion, distrust and distress caused by prevalent misinformation was a main cause of this high vaccine hesitancy. | Effective and equitable roll out of the vaccination program requires careful, empathetic messaging, targeting those whom it will benefit the most, and a multi-organizational approach to address issues of distrust. |
| (Dror et al., 2020)30 | Israel | To evaluate current vaccination compliance rates among Israeli populations | 1941 | Qualitative and quantitative analysis | Survey | Questions such as whether one was willing to be vaccinated against COVID-19 with binary response (Yes/No). | Type of occupational factors such as healthcare providers dealing with COVID-19 patience are less hesitant. | Interventional educational campaigns targeted toward populations at risk of vaccine hesitancy. |
| (Earnshaw et al., 2020)21 | USA | To explore associations between COVID-19 conspiracy beliefs with SARS-CoV-2 vaccine intention and investigate trusted sources of COVID-19 | 854 | Qualitative and quantitative | Survey design | Likert scale with 5 points on the likelihood to be vaccinated; Very likely/ somewhat likely/ likely/ unlikely/ not at all likely. |
Women, less educated and, conspiracy belief are less likely to be vaccinated. | Addressing COVID-19 conspiracy beliefs, including via strategies that leverage trusted sources of COVID-19 information (e.g., doctors), may promote the uptake of COVID-19 vaccines when they become available, as well as support for. |
| (Fisher et al., 2020)8 | USA | To assess intent to be vaccinated against COVID-19 among a representative sample of adults in the United States | 1000 | Qualitative and quantitative | Survey design | Willingness to take the vaccine with the following response options: Yes/not sure/no. | Less likely: younger, female, Black/Hispanic, lower income/edu, larger household, rural, not had flu shot. |
Targeted and multipronged efforts will be needed to increase acceptance of a COVID-19 vaccine when one becomes available. |
| (Graffigna et al., 2020)31 | Italy | To understand how adult citizens’ health engagement, perceived COVID-19 susceptibility and severity, and general vaccine-related attitudes affect the willingness to vaccinate against COVID-19 | 1004 | Qualitative and quantitative analysis | Survey design | Willingness to vaccinate against COVID-19 was measured with Likert scale with 5 points, where 1 is low probability to vaccinate and 5 is high probability to vaccine). | Health engagement is positively related to the intention to vaccinate. | Implementation of educational campaigns aimed at sustaining future vaccination programs that also include health engagement promotion. |
| (Khubchandani et al., 2021)22 | USA | To assess COVID-19 vaccine hesitancy in a community-based sample of the American adult population | 1878 | Qualitative and quantitative analysis | Survey | Likert scale with 4-points on how likely one is to be vaccinated; very likely, somewhat likely, not likely, definitely not. | Vaccine hesitancy was predicted significantly by sex, education, employment, income, having children at home, political affiliation, and the perceived threat of getting infected with COVID-19 in the next 1 year. | Evidence-based communication, mass media strategy. |
| (Kreps et al., 2020)23 | USA | To examine the factors associated with survey participants’ self-reported likelihood of selecting and receiving a hypothetical COVID-19 vaccine | 1971 | Qualitative and quantitative | Survey | Respondents were presented with 5 choice tasks to indicate how likely to receive a (scenario 1) vaccine with 50% efficacy, a 1-year protection duration, was approved under an FDA EUA, and developed in China? |
The attribute of the vaccine such as increased efficacy and protection duration, decreased in adverse effect is associated with less hesitancy. |
Public health authorities might consider outreach strategies that address the specific concerns of older adults and minority communities that have been more susceptible to COVID-19 |
| (Lackner & Wang, 2020)33 | Canada | To investigate the demographic, experiential, and psychological factors associated with the anticipated likelihood of vaccination | 1313 | Qualitative and quantitative research analysis | Exploratory study | A scale ranging from 1 to 100, on how likely they and their children would be to receive a COVID-19 vaccination. | Demographic, experiential, and psychological predictors were related to the intended speed and likelihood of being vaccinated and having one’s children vaccinated against SARS-CoV-2, some |
Targeted messaging campaigns for each unique context |
| (Lazarus et al., 2021)9 | Global (19 countries) | To determine the potential acceptance rates and factors influencing acceptance of a COVID-19 vaccine | 13,426 | Qualitative analysis | Survey | Questions with binary response such as whether one was willing to be vaccinated against COVID-19. | Respondents reporting higher levels of trust in information from government sources were more likely to accept a vaccine and take their employer’s advice to do so. | Clear and consistent communication by government officials to build public confidence. This includes explaining how vaccines work, effectiveness, protection as well as how they are developed, from recruitment to regulatory approval based on safety and efficacy. |
| (Lin et al., 2021)5 | Global | To compare trends and synthesized findings in vaccination receptivity over time | 126 | Systematic literature review | Survey ofrelated literature for systematic review | Combination of binary response and Likert scale with different points. | Perceived risk concerns over vaccine safety and effectiveness, doctors’ recommendations, and inoculation history were common factors. Impacts of regional infection rates, gender, and personal COVID-19 experience were inconclusive. Unique COVID-19 factors included political party orientation, doubts toward expedited development/approval process, and perceived political interference. | Communication campaigns are immediately needed, focusing on transparency and restoring trust in health authorities. Keywords: |
| (Neumann-Böhme et al., 2020)18 | Seven European countries (Denmark, France, Germany, Italy, Portugal, the Netherlands, and the UK) |
To investigate the willingness to be vaccinated | 7662 | Qualitative analysis | survey | Questions with binary response such as whether one was willing to be vaccinated against COVID-19. | Fear of side effect, and safety, gender (more female fear than the male). | Convincing evidence and clear communication on the safety and effectiveness and benefit of the vaccine. |
| (Olomofe et al., 2021)34 | Nigeria | To understand the factors that may influence the uptake of COVID-19 vaccines | 776 | Quantitative study | Survey | Willingness to take the vaccine with the following response options: Yes, Maybe, No. |
Socio-demographic variables such as gender and religion, knowledge on the vaccine, perception significantly predict vaccine hesitancy. | There is a need for public enlightenment aimed at encouraging those that are indecisive or averse to receiving COVID- 19 vaccines. |
| (Paul et al., 2021)37 | UK | To provide understanding of attitudes toward vaccines and factors determining vaccine intent in the context of the COVID-19 pandemic | 32,361 | Quantitative study | Cross-sectional survey design | Willingness to be vaccinated against COVID-19 when available were based on one item (“How likely to do you think you are to get a COVID-19 vaccine when one is approved?”). Response options ranged from “1- very unlikely” to “6 ? Very likely.” |
Low knowledge about COVID-19, gender (women more hesitant) lower incomes is associated with high hesitancy. |
Public health campaigns aimed at increasing COVID-19 vaccine uptake should focus on educating and increasing trust in both those who are uncertain and those who are unwilling on the safety, efficacy, and side effect profile of vaccines. |
| (Pivetti et al., 2021)32 | Italy | This paper explores the role played by antecedents of COVID-related conspiracy beliefs | 590 | Quantitative | Survey design | Four items measured the attitudes toward COVID-vaccine (e.g., “If a coronavirus vaccine would be available, I would get a shot im- mediately”). The response format was a 7-point Likert-type scale ranging from 1 (strongly disagree) to 7 (strongly agree). |
Endorsing purity values predicted stronger negative attitude toward COVID-vaccines. Moreover, conspiracy beliefs negatively predicted general attitudes toward vaccines. | Spreading convincing evidence and clear communication on the safety and effectiveness of vaccines. |
| (Robinson et al., 2021)6 | Global | To examine the percentage of the population intending to vaccinate, unsure, or intending to refuse a COVID-19 vaccine when available | 58,656 | Systematic literature review | Survey ofrelated literature for systematic review | Willingness to take the vaccine or how likely to take the vaccine with the following response options, Yes/No/Not sure. |
Being female, younger, of lower income or education level and belonging to an ethnic minority group were consistently associated with being less likely to intend to vaccinate. | Addressing social inequalities in vaccine hesitancy and promote widespread uptake of vaccine. |
| (Romer & Jamieson, 2020)24 | USA | To test if accepting conspiracy theories that were circulating in mainstream and social media early in the COVID-19 pandemic in the US would be negatively related to the uptake of preventive behaviors and also of vaccination when a vaccine becomes available | 1050 | Qualitative and quantitative | Survey design | Likert scale with 5 points on the willingness to vaccinate: Very likely/likely/ not likely/not at all likely. | Belief in three COVID-19-related conspiracy theories was highly stable across the two periods and inversely related to the (a) perceived threat of the pandemic, (b) taking of preventive actions, including wearing a face mask, (c) perceived safety of vaccination, and (d) intention to be vaccinated against COVID-19. Mainstream television news use predicted adopting both preventive actions and vaccination. | continued messaging by public health authorities on mainstream media and in particular on politically conservative outlets that have supported COVID-related conspiracy theories. |
| (Shekhar et al., 2021)25 | USA | To assess the attitude of healthcare workers (HCWs) toward COVID-19 vaccination | 3479 | Qualitative and quantitative | Survey design | Willingness to take the vaccine with the following response options: No/wait for review/Yes. |
Vaccine acceptance increased with increasing age, education, and income level. Direct medical care providers had higher vaccine acceptance. | Addressing barriers to vaccination among these groups will be essential to avoid exacerbating health inequities laid bare by this pandemic. |
| (Thunstrom et al., 2020)26 | USA | To measure the share of the population that is reluctant to be vaccinated for COVID-19 |
3,133 | Qualitative and quantitative | Experimental design | Participants were asked to indicate WOULD get vaccinated or WOULD NOT get vaccinated, for themselves. |
Distrust of vaccine safety, inconsistent risk messages from public health experts and elected officials and vaccine novelty are among the most important deterrents to vaccination. | Tailored public communication programs designed to persuade vaccine hesitant individuals to accept a COVID-19 vaccine, or increased efforts to ensure a high vaccine uptake level among the remainder of the population, or both. |
| (Wang-Jing et al., 2020)36 | China | To evaluate the acceptance of COVID-19 vaccination in China and give suggestions for vaccination strategies and immunization programs accordingly | 2058 | Qualitative and quantitative | Survey design | Willingness to take the vaccine with the following response options: Yes/No. |
Among respondents who accepted vaccination, the following major characteristics influenced their acceptance: gender, marital status, risk perception, influenza vaccination history, confidence in the effectiveness of the COVID-19 vaccine, respecting physician advice, and vaccination. convenience or vaccine price. | Immunization programs should be structured to eliminate financial and logistical obstacles to vaccination, and health education and communication from authoritative sources are critical tools for assuaging public concerns about vaccine safety. |
| (Wang -Lai et al., 2020)35 | China | To examine impact of the coronavirus disease 2019 (COVID-19) pandemic on change of influenza vaccination acceptance and identify factors associated with acceptance of potential COVID-19 vaccination. | 806+ | Qualitative and quantitative | Survey design | Willingness to take the vaccine with the following response options: Intend to accept/ not intend to accept (undecided). |
Nurses were more likely to be vaccinated. “suspicion on efficacy, effectiveness and safety” predict vaccination hesitancy. | With low acceptance intentions for COVID-19 and a high degree of hesitancy for both influenza and COVID-19 vaccination, evidence-based planning is required to increase uptake of both vaccines prior to their deployment. |
3.3.1. Measurements of COVID-19 vaccination hesitancy
The existing literature used three standard measures for hesitancy in relation to COVID-19 vaccination: optional response questions (for instance, yes or no or not sure), Likert scale, and linear scale measurements. Concerning options, questions were posed on one’s willingness to take the vaccine with the following options; Yes/No/ Not sure to determine one willingness to vaccinate.8–18–19–25–27–29–34 Likert scale with different points to measure one’s likelihood of getting vaccinated with responses such as Very likely/likely/not likely/not at all likely were also used.21,22 Finally, others use linear scale such as a scale ranging from 1 to 100, to measure how likely one is to receive a COVID-19 vaccination, where 1 (denoting very unlikely or not interested in being vaccinated) to finite number (most likely or most interested to be vaccinated).33
3.3.2. Predictors of COVID-19 vaccination hesitancy
The review identified key predictors of COVID-19 vaccination hesitancy which can be categorized as sociodemographic/economic factors, occupational factors, knowledge on the vaccine, conspiracy belief, vaccine attribute, and psychological factors. For instances, some studies identified sociodemographic factors such as sex (female less likely to be vaccinated, that, high hesitancy), age (older people more likely to be vaccinated-less hesitant), education (educated people more likely to be vaccinated),19,21,27 black/Hispanic, lower income, larger household, rural, are less likely to be vaccinated.8 Similarly, Robinson et al.6 argued in their systematic review that factors such as lower income, level of educational attainment, and belonging to an ethnic minority group were significantly less likely to intend to vaccinate. Studies such as Shekhar et al.25 and Wang et al.35 found that some occupation, for instance health workers such as medical doctors and nurses (especially those who deal with COVID-19 patients), are less hesitant to COVID-19 vaccination (that is, they are more likely to be vaccinated). Paul et al. (2021) reported that low knowledge about COVID-19 also increases vaccination hesitancy. Pivetti et al.32 found that conspiracy beliefs negatively predicted general attitudes toward vaccines. The attributes of the vaccine such as increased efficacy and protection duration, decreased in adverse effect are associated with less hesitancy.23 The psychological factors that affect COVID-19 vaccination hesitancy include trust (which is also affected by rural location and low income) in the vaccine, fear of side effect.18,20
3.3.3. Hesitancy corrective measures (Measures to reduce hesitancy)
The review identifies evidence-based finding on ways to minimized COVID-19 vaccination hesitancy and to promote public vaccination. Lazarus et al.9 documented that a clear and consistent communication by government officials is crucial to building public confidence in vaccine programs and that effective campaign on the effectiveness of COVID-19 vaccine is necessary to build trust in the vaccine among the populace. This also includes designing health message targeted at hesitant group.19 Kreps et al.23 and Lackner and Wang33 also revealed that public health authorities should consider outreach strategies and targeted messaging campaigns for each unique context to address the specific concerns of older adults and minority communities that have been more susceptible to COVID-19. In the related study,20 indicated that the COVID-19 related health literacy should be improved in students of university considering socio-cultural background. Additionally, a multi-organizational strategy to addressing disbelief in the vaccination program is also necessary to ensure a successful and fair implementation of the vaccination program.29 Dickerson et al.29 and Fisher et al.8 confirmed this, reporting that educational campaigns aimed at sustaining future vaccination programs, as well as health engagement promotion and targeted and multipronged efforts, is required to increase acceptance of a COVID-19 vaccine when one is made available21 stated that addressing COVID-19 conspiracy beliefs, including via strategies that leverage-trusted sources of COVID-19 information (e.g., doctors), may promote the uptake of COVID-19 vaccines when they become available, continued public health message in mainstream media, particularly politically conservative publications that have backed COVID-related conspiracy theories. Concerning sociodemographic factors27 recommended that addressing sociodemographic characteristics related to COVID-19 vaccination may enhance adoption of the global vaccination program in order to combat future pandemics. The authors also said that focused health education efforts are required to enhance adoption of the COVID-19 vaccination. Similarly, according to,37 public health campaigns aimed at increasing COVID-19 vaccine uptake should focus on educating and increasing trust in both those who are uncertain and those who are unwilling about the safety, efficacy, and side effect profile of vaccines, as well as spreading convincing evidence and clear communication about vaccine safety and effectiveness.32
4. Discussion
The review process undertakes a synthesis of COVID-19 vaccine hesitancy in terms of measurement, key predictors, and preventive measures. The hesitancy of COVID-19 vaccine has been consistently measured by optional response, Likert or linear scale19,27,28 irrespective of geographical location, and study characteristics. The variation in measurements approach can be attributed to the purpose and nature of the study. In their study on the assessment of COVID-19 vaccine hesitancy using Likert scale with 4-points (very likely, somewhat likely, not likely, definitely not) in USA,22 reported through their multiple regression analyses that vaccine hesitancy was significantly influenced by factors such as gender, education, employment, income, having children at home, political affiliation, and the perceived threat of contracting COVID-19 in the next 1 year. The authors asserted that, given the high prevalence of COVID-19 vaccine hesitancy in the United States, evidence-based communication strategies, massmedia strategies, and policy measures must be implemented across the country in order to convert vaccines into vaccinations and mass immunization, with particular attention paid to the groups identified in this study. Similarly,25 and35 in their separate studies in USA and China, respectively, using both qualitative and quantitative approach found that some occupation, for instance health workers such as medical doctors and nurses (especially those who deal with COVID-19 patients) are less hesitant to COVID-19 vaccination (that is, they are more likely to be vaccinated. However,30 found that healthcare professionals who do not care for COVID-19 positive patients tend to have less trust in the COVID-19 vaccination than the general community, with nurses being more vaccine-averse than doctors. Although nurses had somewhat higher rates of yearly influenza immunization than the general population, they have more knowledge regarding COVID-19 vaccine. This low vaccination acceptance rate among nurses may have a detrimental effect on future vaccination compliance for persons who interact or engage with vaccine-hesitant nurses.
Campo-Arias and Pedrozo-Pupo20 and Neumann-Böhme et al.18 found in their separate studies that the psychological factors that affect COVID-19 vaccination hesitancy include trust in the vaccine, fear of side effect. A similar study by37 found that vaccine mistrust was no different between people with and without long-term health conditions. These findings could indicate that there will be a demand for the vaccine even among people who do not have physical health conditions, which may necessitate careful management of the vaccine supply and distribution. In addition, persons from poorer socio-economic backgrounds are more likely than others to be unsure or reluctant to get vaccination, which might increase already existing inequities over exposure to and experience of the virus in the United Kingdom. It is possible that those who are unsure will be a more favorable population for prospective treatments.38 The researchers found that although some indicators show reluctance but not doubt (such as education, age, and residing in a rural area), it is very difficult to distinguish those individuals that are just unsure. In order to increase COVID-19 vaccine uptake, public health campaigns should focus on educating and building trust in both those who are unsure and those who are unwilling about the safety, efficacy, and side effect profile of vaccines.38,39 In their study to explore the role played by antecedents of COVID-related conspiracy beliefs in Italy,32 found that conspiracy beliefs negatively predicted general attitudes toward vaccines. Additionally, the authors demonstrated that in order to mitigate the adverse effects of conspiracy beliefs, exposure to anti-conspiracy arguments both before to and after exposure to conspiracy theories may help recover vaccination intentions.40,41 Additionally, an experimental research showed that presenting reasonable reasons, in conjunction with providing mocking arguments, was a good technique for reducing conspiracy ideas. Given the beneficial benefits of analytical thinking on conspiracy belief reduction, exposing the logical errors of conspiracy ideas may be an effective method of discrediting them.42
Neumann-Böhme et al.18 investigated the willingness to be vaccinated (using binary response measures of Yes/No) in seven European countries (Denmark, France, Germany, Italy, Portugal, the Netherlands, and the UK) found that fear of side effect, and safety, gender (more female fear than the male). The authors argued that targeting those in the population who are currently hesitant seems most promising and cost-effective, but this requires convincing evidence and clear communication on the safety and effectiveness of the vaccine. A campaign emphasizing the social benefits of vaccination could increase the willingness to be vaccinated among those amenable to such pro-social motives. Their finding also reveal that a sizable proportion of the population indicates not to be open to vaccination. This group may remain at risk of spreading the virus and contracting the disease, even after herd immunity has been achieved.
Further, Lazarus et al.9 reinforce the same finding that clear and consistent communication by government officials is crucial to building public confidence in vaccine progam. This includes explaining how vaccines work, as well as how they are developed, from recruitment to regulatory approval based on safety and efficacy. Effective campaigns should also aim to carefully explain a vaccine’s level of effectiveness, the time needed for protection (with multiple doses, if required) and the importance of population-wide coverage to achieve community immunity. It also includes preparing the public and leaders of civic, religious, and fraternal organizations that are respected within various sectors of society and local communities, as well as the private sector, for a mass vaccination program with credible spokespeople, local engagement, accurate information and technological support. Additionally, Thunstrom et al.26 reported that knowing about COVID-19 vaccine avoidance before a vaccine is available can help government agencies, healthcare workers, and other authorities mitigate the impact of vaccine avoidance. Such efforts may involve developing policies and a preparedness for the vaccine avoidance. It might also involve public information campaigns designed to increase confidence in the effectiveness and safety of the vaccine. The authors also found that distrust in the government is higher amongst those who decline the vaccine. To address COVID-19 vaccine hesitancy, broader public health campaigns may therefore be less effective. Instead, efforts might focus on reaching out to healthcare providers (the most trusted source of vaccine safety information, see e.g Freed et al.43) and local authorities, including religious leaders. Al-Mohaithef and Padhi27 revealed in from their study in Saudi Arabia that participants’ perceived risk and trust in the health system were found to be significant predictors toward the intention of the COVID-19 vaccine. They proposed further study to corroborate their findings with public health promotion interventions.
Dickerson et al.29 concluded from their studies in the United Kingdom that a broader and more precisely focused response is necessary to enhance vaccination acceptance throughout the country, especially among ethnic minorities and those living in impoverished neighborhoods. They attended that message must comfort people who are unsure or hesitant to consider vaccinations. This message must be culturally relevant, non-technical, and sensitive to the degrees of uncertainty and discomfort experienced by individuals. Additionally, they emphasized the need of communicating from trustworthy sources, noting a lack of confidence in the government and local council, but high levels of trust in the NHS, local hospitals, and schools. However, individuals least likely to get the vaccination also had suspicions about the NHS. When appropriate, the use of trustworthy organizations other than the NHS (e.g., schools), as well as trusted community and church leaders, may assist to build trust and encourage people who are unwilling to receive the vaccination. Olomofe et al.34 conducted cross-sectional research to determine the parameters influencing COVID-19 vaccination uptake in Nigeria and found that sociodemographic characteristics such as respondents’ gender and religion had a statistically significant relationship with their desire to accept the vaccination. Other characteristics, such as the belief that vaccinations are either beneficial or harmful, prior vaccination history, and awareness of COVID-19, were also shown to have a statistically significant connection with desire to get the vaccine. The authors emphasized the need of public education in order to persuade people who are undecided or resistant to taking COVID-19 vaccinations.
5. Conclusion
In sum, this study provides rapid systematic literature reviews on COVID-19 vaccine hesitancy, which is a major threat to the fight against the virus through vaccination by addressing the following critical research questions; What is the standard measurement of hesitancy of COVID-19 vaccine in the literature? What are the key predictors (up to date) of hesitancy of COVID-19 vaccine? What are the evidence-based measures in the literature to minimize COVID-19 vaccine hesitancy and promote public patronage of the vaccine? A sample of 25 studies out of 470 potential studies were used after a comprehensive literature search and rigorous assessment based on PRISMA-P guidelines on the subject. The findings reveal three standard measures of vaccine hesitancy: optional response questions, Likert scale, and linear scale measurements. Factors such as sociodemographic/economic factors, occupational factors, knowledge on the vaccine, vaccine attributes, conspiracy belief and psychological factors are the major predictor of COVID-19 vaccine hesitancy. Evidence-based findings identified the following measures to eliminate COVID-19 vaccine hesitancy (1) providing a clear and consistent communication and effective campaign to build public confidence and trust in the vaccine; (2) providing outreach strategies and targeted messaging campaigns for each unique context; (3) A campaign emphasizing the social benefits of vaccination; (4) framing careful, empathetic messaging, targeting those whom it will benefit the most, and a multi-organizational approach to address issues; (5) Increasing the knowledge (vaccination literacy) in schools, institutions, organizations (formal and informal) and media; (6) conspiracy beliefs, including via strategies that leverage trusted sources of COVID-19 information. Targeted health education interventions are needed to increase the uptake of the future COVID-19 vaccine educating and increasing trust in both those who are uncertain and those who are unwilling on the safety, efficacy, and side effect profile of vaccines and spreading convincing evidence and clear communication on the safety and effectiveness of vaccines (7) explaining how vaccines work, as well as how they are developed, from recruitment to regulatory approval based on safety and efficacy. Effective campaigns should also aim to carefully explain a vaccine’s level of effectiveness, the time needed for protection.
Funding Statement
Funding for this study was provided by the National Research Foundation of South Africa [Grant number: 121890] and Nelson Mandela University through Vice Chancellor funds.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethical considerations
This article followed all ethical standards for research without direct contact with human or animal subjects.
References
- 1.Anakpo G, Mishi S.. Business response to COVID-19 impact: effectiveness analysis in South Africa. Southern African J Entrepreneurship Small Bus Manage. 2021;13(1):7. doi: 10.4102/sajesbm.v13i1.397. [DOI] [Google Scholar]
- 2.Tshabalala N, Anakpo G, Mishi S. Ex ante vs ex post asset-inequalities, internet of things, and COVID-19 implications in South Africa. Africagrowth Agenda. 2021;18:18–12. [Google Scholar]
- 3.Jafta K, Anakpo G, Mishi S. 2022. Income and poverty implications of Covid-19 pandemic and coping strategies: the case of South Africa. Africagrowth Agenda.
- 4.Komanisi E, Anakpo G, Mishi S. Vulnerability to COVID-19 impacts in South Africa: analysis of the socio-economic characteristics. Africagrowth Agenda. 2022.
- 5.Lin C, Tu P, Beitsch LM. Confidence and receptivity for covid‐19 vaccines: a rapid systematic review. Vaccines. 2021;9(1):1–32. doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021;39(15):2024–34. doi: 10.1016/j.vaccine.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pogue K, Jensen J, Stancil C, Ferguson D, Hughes S, Mello E, Burgess R, Berges B, Quaye A, Poole B. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines. 2020;8(4):582. doi: 10.3390/vaccines8040582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med. 2020;173(12):964–73. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–28. doi: 10.1038/s41591-020-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization (2019). World Health Organization Ten threats to global health in 2019. Retrieved on September 22, 2021 from https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019. [Google Scholar]
- 11.Mac Donald N. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–64. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 12.SAGE . Report on SAGE Working Group on vaccine hesitancy. 2014. Retrieved on August 24, 2021 from https://cdn.who.int/media/docs/default-source/immunization/sage/2014/october/sage-working-group-revised-report-vaccine-hesitancy.pdf?sfvrsn=240a7c1c_4.
- 13.Reiter P, Pennell M, Katz M. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38(42):6500–07. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Machingaidze S, Wiysonge C. Understanding COVID-19 vaccine hesitancy. Nat Med. 2021;27(8):1338–39. doi: 10.1038/s41591-021-01459-7. [DOI] [PubMed] [Google Scholar]
- 15.Chevallier C, Hacquin AS, Mercier H. COVID-19 vaccine hesitancy: shortening the last mile. Trends Cogn Sci. 2021;25(5):331–33. doi: 10.1016/j.tics.2021.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.CASP . Critical appraisal skills programme. 2019. [accessed 2019 March]. https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf.
- 17.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Duffy S. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme version. 2006;1(1):b92. [Google Scholar]
- 18.Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, Schreyögg J, Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health E. 2020;21(7):977–82. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Callaghan T, Moghtaderi A, Lueck JA, Hotez P, Strych U, Dor A, Fowler EF, Motta M. Correlates and disparities of COVID-19 vaccine hesitancy. Rochester: Social Science Research Network. Washington, DC, United States; 2020. Available at SSRN: https://ssrn.com/abstract=3667971. [Google Scholar]
- 20.Campo-Arias A, Pedrozo-Pupo JC. COVID-19 vaccine distrust in Colombian university students: frequency and associated variables. MedRxiv. 22. 2021. Retrieved on September 18, 2021 from https://www.medrxiv.org/content/10.1101/2021.03.07.21253080v1.full. [DOI] [PMC free article] [PubMed]
- 21.Earnshaw VA, Eaton LA, Kalichman SC, Brousseau NM, Hill EC, Fox AB. COVID-19 conspiracy beliefs, health behaviors, and policy support. Transl Behav Med. 2020;10(4):850–56. doi: 10.1093/tbm/ibaa090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Community Health. 2021;46(2):270–77. doi: 10.1007/s10900-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kreps S, Prasad S, Brownstein JS, Hswen Y, Garibaldi BT, Zhang B, Kriner DL. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA network open. 2020;3(10):e2025594–e2025594. doi: 10.1001/jamanetworkopen.2020.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Romer D, Jamieson KH. Social science & medicine conspiracy theories as barriers to controlling the spread of COVID-19 in the U. S. Soc Sci Med. 2020;263:113356. doi: 10.1016/j.socscimed.2020.113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shekhar R, Sheikh AB, Upadhyay S, Singh M, Kottewar S, Mir H, Barrett E, Pal S. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines. 2021;9(2):1–18. doi: 10.3390/vaccines9020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thunstrom L, Ashworth M, Finnoff D, Newbold S. Hesitancy towards a COVID-19 vaccine and prospects for herd immunity. SSRN Electron J. 2020;35:1–50. doi: 10.2139/ssrn.3593098. [DOI] [Google Scholar]
- 27.Al-Mohaithef M, Padhi BK. Determinants of covid-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthcare. 2020;13:1657–63. doi: 10.2147/JMDH.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Detoc M, Bruel S, Frappe P, Tardy B, Botelho-nevers E, Gagneux-brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. vaccine. 2020;38(45):7002–06. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dickerson J, Lockyer B, Moss RH, Endacott C, Kelly B, Bridges S, Crossley KL, Bryant M, Sheldon TA, Wright J, et al. COVID-19 vaccine hesitancy in an ethnically diverse community: descriptive findings from the Born in Bradford study. Wellcome Open Res. 2021;6:23. doi: 10.12688/wellcomeopenres.16576.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–79. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Graffigna G, Palamenghi L, Boccia S, Barello S. Relationship between citizens’ health engagement and intention to take the covid-19 vaccine in Italy: a mediation analysis. Vaccines. 2020;8(4):1–11. doi: 10.3390/vaccines8040576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pivetti M, Melotti G, Bonomo M, Hakoköngäs E. Conspiracy beliefs and acceptance of covid‐vaccine: an exploratory study in Italy. Soc Sci. 2021;10(3):108. doi: 10.3390/socsci10030108. [DOI] [Google Scholar]
- 33.Lackner CL, Wang CH. Demographic and psychological correlates of SARS-CoV-2 vaccination intentions in a sample of Canadian families MedRxiv. 2020;100091. doi: 10.1101/2020.11.04.20226050. [DOI] [PMC free article] [PubMed]
- 34.Olomofe C, Victor Soyemi K, Felicia Udomah B, Olabisi Owolabi A, Eziashi Ajumuka E, Chukwudum Igbokwe M, Uriel Ashaolu O, Ayodele Adeyemi O, Bolatito Aremu-Kasumu Y, Folasade Dada O, et al. Predictors of uptake of a potential Covid-19 vaccine among Nigerian adults. medRxiv, 2020-12. 2021;12(1):1000442. https://www.medrxiv.org/content/10.1101/2020.12.28.20248965v1. [Google Scholar]
- 35.Wang K, Lai E, Wong Y, Fai K, Wai A, Cheung L, Ying E, Chan Y, Kiong E, Yeung S, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine. 2020;38(45):7049–56. doi: 10.1016/j.vaccine.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, Fang H. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. 2020;8(3):482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. The Lancet Reg Health - Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Habersaat K, Betsch C, Danchin M, Sunstein CR, Böhm R, Falk A, Brewer NT, Omer SB, Scherzer M, Sah S. Ten considerations for effectively managing the COVID- 19 transition. Nat Hum Behav. 2020;4(7):677–87. doi: 10.1038/s41562-020-0906-x. [DOI] [PubMed] [Google Scholar]
- 39.Rhodes A, Hoq M, Measey MA, Danchin M. Intention to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2021;21(5):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jolley D, Douglas KM. Prevention is better than cure: addressing antivaccine conspiracy theories. J Appl Soc Psychol. 2017;47(8):459–69. doi: 10.1111/jasp.12453. [DOI] [Google Scholar]
- 41.Lyons B, Merola V, Reifler J. Not just asking questions: effects of implicit and explicit conspiracy information about vaccines and genetic modification. Health Commun. 2019;34(14):1741–50. doi: 10.1080/10410236.2018.1530526. [DOI] [PubMed] [Google Scholar]
- 42.Orosz G, Kreko P, Paskuj B, Toth-Kiraly I, Böthe B, Roland-Levy C. Changing conspiracy beliefs through rationality and ridiculing. Front Psychol. 2016;7:1525. doi: 10.3389/fpsyg.2016.01525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Freed G, Clark S, Butchart A, Singer D, Davis M. Sources and perceived credibility of vaccine-safety information for parents. Pediatrics. 2011;127(Supplement 1):S107–S112. doi: 10.1542/peds.2010-1722P. [DOI] [PubMed] [Google Scholar]


