Abstract
Background
The two-thumb encircling technique (2TT) is superior to the two-finger technique (2FT) in infant cardiopulmonary resuscitation (CPR), but there are difficulties in providing ventilation as soon as possible. We modified the 2TT to the cross-thumb technique (CTT) to maintain good CPR performance at the same position as 2FT. We aimed to compare the quality of chest compression and brief hands-off times in 2FT, 2TT, and CTT by a single rescuer using an infant CPR manikin model.
Methods
This study was designed as a prospective randomized controlled simulation-based study. We used the Resusci® Baby QCPR (Laerdal Medical, Stavanger, Norway) as a simulated 3-month-old infant. Ventilation was performed by the mouth-to-mouth technique using a chest compression-to-ventilation ratio of 30:2 as a single rescuer. Data on CPR quality, such as locations, rates, depth and release of chest compressions, hands-off times, and proper ventilation, were recorded using the Resusci® Baby QCPR and SkillReporter. Also, the chest compression fraction (CCF) was automatically calculated.
Results
The depth of chest compression in 2FT, 2TT, and CTT were 40.0 mm (interquartile range [IQR] 39.0, 41.0), 42.0 mm (IQR 41.0, 43.0), and 42.0 mm (IQR 41.0, 43.0), respectively. The depth of chest compression in 2FT was shallower than that in the other two techniques (P<0.05). CCF in 2FT, 2TT, and CTT were 73.9% (IQR 72.2, 75.6), 71.2% (IQR 67.2, 72.2) and 71.3% (IQR 67.7, 74.1), respectively. CCF was higher in 2FT than in the other two techniques (P<0.05). Correct location in 2FT, 2TT, and CTT were 99.0% (IQR 86.0, 100.0), 100.0% (IQR 97.0, 100.0) and 100.0% (IQR 99.0, 100.0), respectively. Correct location in CTT and 2TT was higher than that in 2FT. Performing CTT, the subjective pain and fatigue score were lower than other two technique.
Conclusion
A new chest compression technique, CTT was better in chest compression depth compared with 2FT and may be helpful in maintaining correct chest compression location with less pain and fatigue in infant CPR.
Introduction
The impact of high-quality chest compressions and brief hands-off time during cardiopulmonary resuscitation (CPR) is irrefutable as it is critical for maintaining the perfusion of vital organs. High-quality chest compression and brief hands-off time help achieve recovery of spontaneous circulation and good neurologic outcomes after CPR. Therefore, recent CPR guidelines and most articles about CPR skills strongly suggest that brief hands-off time, high quality CPR performance, and minimal interruption of chest compression continued during CPR [1–4]. However, the quality of chest compressions is often poor in infant CPR. According to studies on infant CPR, the depth of chest compressions was shallow, and the no-flow time, such as hands-off time divided by cardiac arrest time, was too long [5–10].
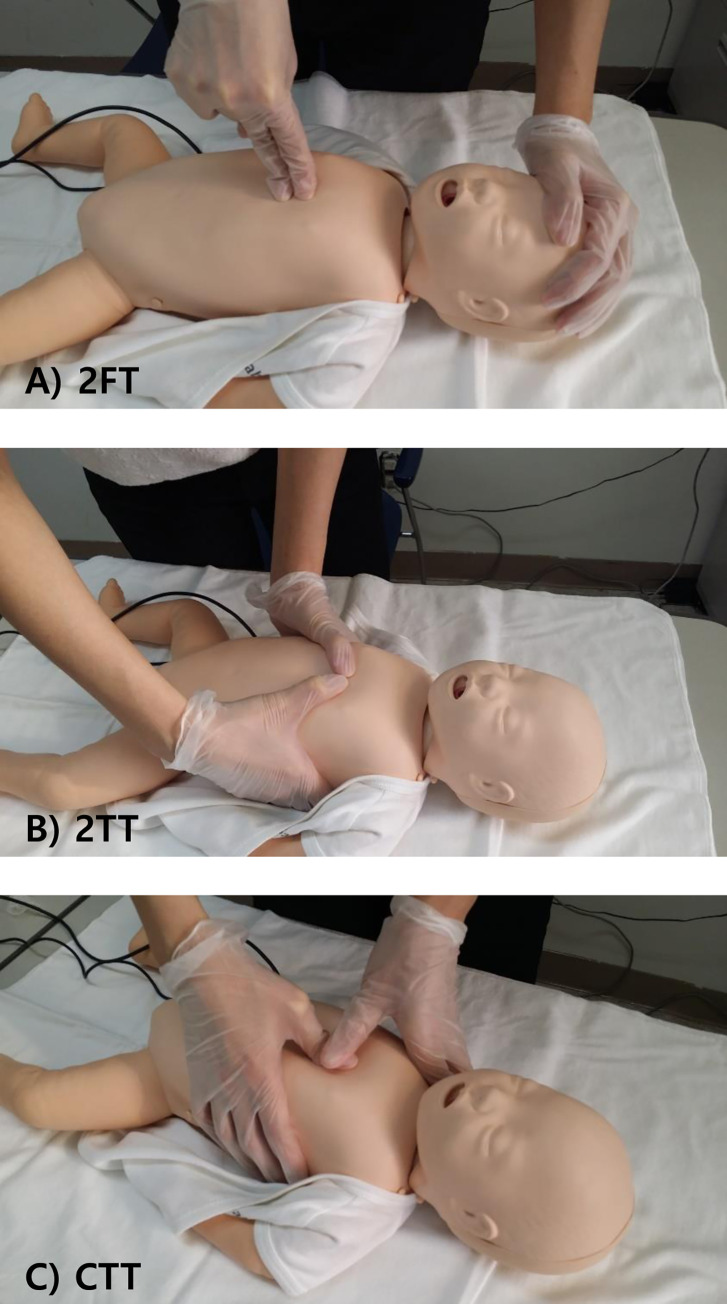
The European Resuscitation Council and American Heart Association guidelines recommend that the lone rescuer compresses the sternum with the tip of two fingers, the so-called two-finger technique (2FT), and two or more rescuers use the two-thumb–encircling hands technique (2TT), placing both thumbs flat side by side on the lower half of the sternum just below the intermammary line with the tips pointing towards the infant’s head and spreading both hands with the fingers together to encircle the lower part of the infant’s rib cage [1, 3] (Fig 1A and 1B). Additionally, on chest compression technique in infant CPR, the 2TT is superior to the 2FT due to greater compression depth, more accurate finger placements, adaptability, and less exertion by rescuers [11]; however, the 2FT is considered superior with regard to duty cycle, chest recoil, and release force compliance [11].
Fig 1.
Chest compression techniques used in this study: A) Two finger technique; B) Two thumb encircling hands technique; C) Cross thumb technique.
The cross-thumb technique (CTT) is a novel method that modifies the 2TT to maintain high-quality chest compression and fix the location of the rescuer in relation to the infant. It is similar to 2TT, but the positions of the thumbs and hand are different. The thumb of the dominant hand is placed on the lower half of the sternum, while the dominant hand’s finger encircles the lower part of the infant’s rib cage. The thumb of the non-dominant hand is placed over the thumb of the dominant hand, and the non-dominant hand’s finger encircles the shoulder (Fig 1C). Using this technique, after breathing support without any change in the rescuer’s location, the rescuer may quickly resume chest compression at the right or left side of the patient rather than at the downside of the cardiac arrest victim. Therefore, this may promote that hands-off times are shorter than those of other techniques (Fig 2).
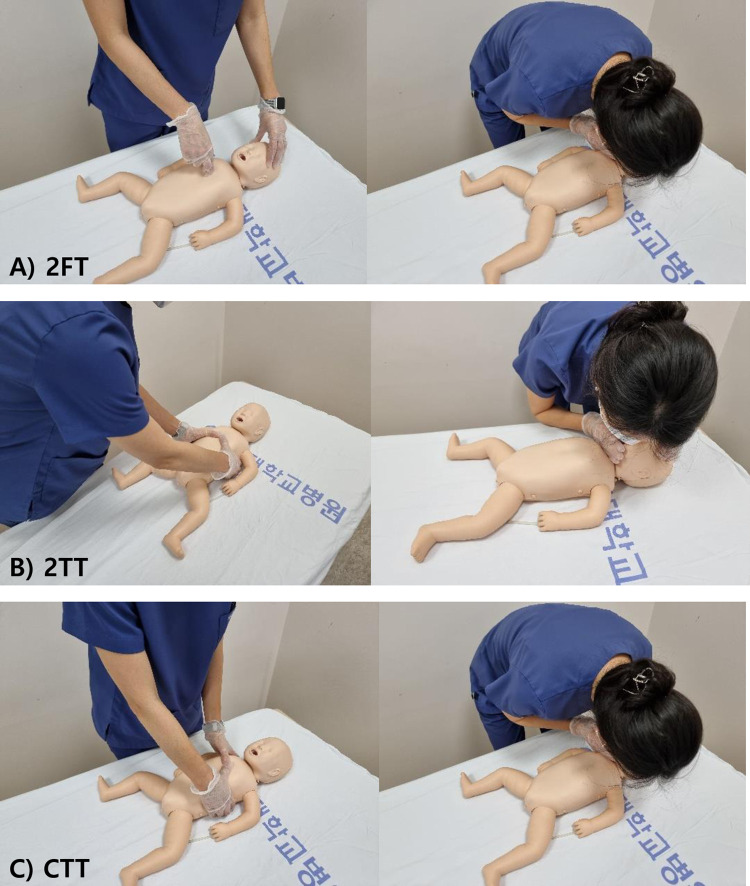
Fig 2. A rescuer’s location performing each chest compression technique.
2FT and CTT allow a rescuer to maintain the same position next to the patient’s chest and shoulder. With 2TT, the rescuer must perform chest compressions at the bottom of the patient. At the end of the compression cycle, the rescuer must move its position toward the patient’s head for ventilation. 2FT, two finger technique; 2TT, two thumb technique; CTT, cross-thumb technique.
Furthermore, increasing the pressure by overlapping the rescuer’s thumbs and fixing the location with encircled hands suggested that high-quality chest compression could be achieved. We hypothesize that CPR performance using CTT can be more effective by using the pinch force of two thumbs while reducing the change in the rescuer’s position to minimize chest compression interruption by ventilation.
The aim of our study was to compare the quality of chest compression and brief hands-off times in 2FT, 2TT, and CTT by a single rescuer using an infant CPR manikin model.
Materials and methods
Study design
This study was designed as a prospective randomized controlled simulation-based study and was approved by the Institutional Review Board (ISPAIK 2019-09-06). We used the Resusci® Baby QCPR (Laerdal Medical, Stavanger, Norway) as a 3-month-old infant simulating manikin. All participants were already trained in the Pediatric Basic Life Support program and were provided videos and written information about this study before participating in this study. At the beginning, the participants took oral lectures for 30 minutes. These instructions for the study comprised infant resuscitation review for high-quality CPR according to guideline, a new chest compression technique, and a study overview [1]. After instruction, all participants practiced all techniques by self-selected order to achieve high-quality chest compression and ventilation using the QCPR feedback function of simulating manikin for 10 minutes. An instructor supervised these practices and gave immediate feedback to participants during the practice time. Ventilation was performed using the mouth-to-mouth technique, using a chest compression-to-ventilation ratio of 30:2 as a single rescuer. Then, participants were randomly assigned to one of three different chest compression techniques (2FT, 2TT, and CTT) using the Research Randomized software (www.randomizer.org). Before entering the testing room, each participant selected a sealed envelope including a memo indicating the chest compression method they had been randomly selected to perform. Each participant performed five cycles of CPR using the assigned compression technique without QCPR feedback in an independent room. Data on CPR quality, such as locations, rates, depth and release of chest compressions, hands-off times, and proper ventilation, were recorded with SimPad with SkillReporter (Laerdal Medical, Stavanger, Norway). After the simulation, we surveyed the age, sex, and jobs of the participants. They answered a short questionnaire about difficulty level, fatigue, and pain scores during CPR simulation, as numeric rating scales (NRS) from 1 to 10. NRS was selected according to the participant’s experience, which meant that the lower the number, the easier it was, the less tiring it was, and the less painful it was. The higher the number, the more difficult, the more tiring and the more painful it was.
Measurement of CPR performance
According to the American Heart Association, there are five main components of high-quality CPR: chest compression fraction (CCF), rate and depth of chest compressions, chest recoil, and ventilation [2]. CCF is the proportion of time that chest compressions are performed during a cardiac arrest. Because studies on out-of-hospital cardiac arrest have shown that low CCF is related to decreased return of spontaneous circulation (ROSC) and survival to hospital discharge, expert consensus recommended that high CCF was helpful for successful CPR in out-of-hospital cardiac arrest [12]. We recorded chest compression time and hands-off time using SkillReporter and calculated automatically CCF. Other components of high-quality CPR, such as compression rate and depth, were recorded as mean values and the percentage of success in simulation time, respectively. In accordance with the AHA and ERC guidelines, the participants were instructed to perform infant chest compression at a depth of at least 4 cm at a compression rate of 100–120 per minute. We also recorded the proportion of chest recoils in each compression and the proportion of adequate ventilation in five cycles of CPR from 0 to 100% in the SkillReporter. The chest recoil is defined as relaxation of the chest wall to its original position after each chest compression. The amount of ventilation volume measured at Resusci® Baby QCPR was recorded. In consideration of the age and weight of the simulator, when the ventilation amount was between 20 ml and 40 ml, it was judged as adequate ventilation. Correct hand-position was recorded the proportion of correct location of chest compressions in five cycles of CPR using the Resusci® Baby QCPR sensor. These variables were studied while being set in the SkillReporter according to the AHA guidelines, and were automatically stored and analyzed.
Sample size
We proposed an alpha risk of 0.05 and power 0.9. The quality CPR score in our pilot data from 6 volunteers showed 88% vs. 89%. Vs 90% in the 2FT, 2TT, CTT, respectively (automatically QCPR measured by Simpad SkillReporter). Using one-way analysis of variance with 10% drop-out rate, 30 participants per a group were required.
Statistics
Data were analyzed using SPSS v22.0 (IBM, New York, USA). Continuous variables were expressed as medians and quartiles for non-normal distribution. Nominal and categorical variables were presented as frequencies and percentages. The normal distribution of variables was confirmed using the Kolmogorov-Smirnov test. Differences in CPR parameters between the three groups were assessed using the analysis of variance (Mann-Whitney test) for the normal distribution and the analysis of variance (Kruskal-Wallis test) for the non-normal distribution. Post hoc tests were performed after correction by pairwise comparison. Statistical significance was set at P <0.05.
Results
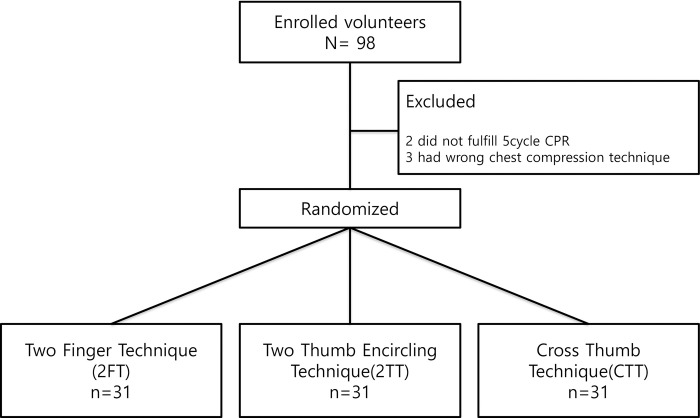
Ninety-eight volunteers participated in this simulation study. After the BLS lecture video, study instruction, and simulation practice, the volunteers enrolled in this study. We excluded two participants who did not complete five cycles of CPR due to fatigue and pain during the practice time. Three additional participants were excluded because they performed a chest compression technique other than the one to which they had been randomized. We randomly allocated the participants to three groups: 2FT, 2TT, and CTT. Each group included 31 participants, and their CPR performance was recorded (Fig 3).
Fig 3. Study outlines.
The median age of enrolled participants was 30.0 (IQR 27.0, 32.0) years. Fifty-seven participants were women (61.3%), and 36 participants were men (39.7%). There were 44 doctors (47.3%), 37 nurses (39.8%), and 12 emergency medical technicians (12.9%) in this study. General characteristics of participants show Table 1. The job, sex and age were not significantly different among three groups.
Table 1. General characteristics of participants.
| Compression methods | P-value | |||
|---|---|---|---|---|
| 2FT | 2TT | CTT | ||
| (n = 31) | (n = 31) | (n = 31) | ||
| Job | 0.917 | |||
| Doctors | 16 | 11 | 4 | |
| Nurses | 12 | 14 | 5 | |
| EMT | 16 | 12 | 3 | |
| Sex, male | 15 (48.4) | 10 (32.3) | 11 (35.5) | 0.302 |
| Age, yrs | 30.7±4.4 | 29.5±4.0 | 29.7±4.0 | 0.467 |
Values are expressed as number (%) or mean±standard deviations.
2FT, Two finger technique; 2TT, Two thumb encircling technique; CTT, Cross thumb technique; EMT, Emergency medical technicians.
The depth of chest compression in 2FT, 2TT, and CTT were 40.0 mm (IQR 39.0, 41.0), 42.0 mm (IQR 41.0, 43.0), and 42.0 mm (IQR 41.0, 43.0), respectively (Table 2). The depth of chest compression in 2FT was shallower than that in the other two techniques, 2TT and CTT (P<0.05) (Fig 3). After post hoc analysis as a pairwise comparison, there were no statistically significant differences between 2TT and CTT. CCF in 2FT, 2TT, and CTT were 73.9% (IQR 72.2, 75.6), 71.2% (IQR 67.2, 72.2), and 71.3% (IQR 67.7, 74.1), respectively (Table 2). CCF was higher in 2FT than in the other two techniques, 2TT and CTT (P<0.05). After post hoc analysis as a pairwise comparison, there were no statistically significant differences between 2TT and CTT.
Table 2. Cardiopulmonary resuscitation performance and subjective feedback (NRS) in three groups.
| 2FT | 2TT | CTT | P-value | ||
|---|---|---|---|---|---|
| (n = 31) | (n = 31) | (n = 31) | |||
| CPR performance | Compression depth (mm) | 40 (39–41) a | 42 (41–43)b | 42 (41–43)b | <0.05 |
| Compression rate (bpm) | 106 (104–112) | 109 (105–114) | 107 (103–114) | 0.667 | |
| Chest recoil (%) | 100 (99–100) | 99 (95–100) | 99 (92–100) | 0.057 | |
| Adequate ventilation (%) | 56 (38–80) | 50 (20–70) | 63 (38–78) | 0.260 | |
| Total simulation time (sec) | 116.0 (109–122)a | 119 (114–123)a | 122 (118–128)b | <0.05 | |
| Hands-off time per cycle (sec) | 6 (6–6)a | 7 (6–8)b | 7 (6–8)b | <0.05 | |
| Chest compression fraction (%) | 73.9 (72.2–75.6)a | 71.2 (67.2–72.2)b | 71.3 (67.7–74.1)b | <0.05 | |
| Correct location (%) | 99 (86–97) | 100 (97–100) | 100 (99–100) | 0.058 | |
| Questionnaires | Difficulty level | 3 (1–5) | 3 (2–6) | 2 (2–4) | 0.554 |
| Fatigue | 7 (6–8) a | 5 (3–7) b | 4 (2–6) b | <0.05 | |
| Pain | 7 (6–8) a | 5 (3–6) b | 5 (3–6) b | <0.05 |
The different letters indicate significantly different groups on the basis of the Kruskal-Wallis test with multiple comparisons with the Bonferroni correction method. Data show as median (interquartile range).
2FT, Two finger technique; 2TT, Two thumb encircling technique; CTT, Cross thumb technique; CPR, Cardiopulmonary resuscitation; bpm, Beat per minutes; NRS, Numeric rating scale.
Chest compression rates in 2FT, 2TT, and CTT were 106.0 bpm (IQR 104.0, 116.0), 109.0 bpm (IQR 105.0, 114.0), and 107.0 bpm (IQR 103.0, 114.0), respectively (Table 2). Chest recoil in 2FT, 2TT, and CTT were 100.0% (IQR 99.0, 100.0), 99.0% (IQR 95.0, 100.0), and 99.0% (IQR 92.0, 100.0), respectively (Table 2). Adequate ventilation in 2FT, 2TT, and CTT was 56.0% (IQR 38.0, 80.0), 50.0% (IQR 20.0, 70.0), and 63.0% (IQR 38.0, 78.0), respectively. Adequate ventilation in CTT was higher than in 2FT and 2TT, but there were no significant differences (Table 2). Correct location in 2FT, 2TT and CTT were 99.0.0% (IQR 86.0, 100.0), 100.0% (IQR 97.0, 100.0), and 100.0% (IQR 99.0, 100.0), respectively (Table 2). Correct location in CTT was higher than that in 2FT, but there were no significant differences.
There was no statistically significant difference in the difficulty reported by participants in each of the three groups (P>0.05). The median NRS scores for fatigue in 2FT, 2TT, and CTT were 7.00 (IQR 6.0, 80), 5.0 (IQR 3.0, 7.0), and 4.0 (IQR 2.0, 6.0), respectively (Table 2). The median of NRS for pain in 2FT, 2TT, and CTT were 7.00 (IQR 6.0, 80), 5.0(IQR 3.0, 6.0), and 5.0 (IQR 3.0, 6.0), respectively (Table 2). The 2FT group showed higher scores in fatigue and pain NRS than the 2TT and CTT groups (P<0.05, P<0.05, respectively). After hoc analysis as a pairwise comparison, there were no statistical differences in fatigue and pain NRS between the 2TT and CTT groups.
Discussion
Several attempts and studies have been made to find effective methods that provide high-quality CPR when a single rescuer performs infant CPR. In a recent systematic review and meta-analysis, 2TT was a method that provided high-quality chest compression without compromising ventilation in single rescuer infant CPR [13, 14]. Herein, the depth of chest compression was higher in 2TT and CTT compared with 2FT. Additionally, the compression depth of CTT was comparable to that of 2TT.
However, we thought that the previous studies overlooked the importance of CCF or hands-off time in CPR performance [13, 14]. These studies focused only on adequate chest compression and ventilation volume rather than hands-off time and CCF. Another study reported that the total hands-off time by 2FT and 2TT differ significantly up to 2 seconds [15]. This result might be caused by the location of a single rescuer in the CPR scene. In 2FT, a single rescuer should be located at the shoulder level of the infant to provide chest compression. In contrast, in 2TT, a single rescuer should be located at the hip level of the CPR infant to provide chest compression. Considering that a rescuer in 2FT may be closer to the head of the infant, the difference in single rescuer location in 2FT and 2TT may cause longer hands-off time and lower CCF in 2TT.
While the CCF of 2FT was higher than other techniques, the CCF of 2TT and CTT were not different in our study. The major difference between 2TT and CTT in a single rescuer is the location from which the rescuer performs chest compressions. The 2TT should move from the hip to the face of the infant to provide ventilation after one cycle of chest compression. As 2FT is performed, a rescuer using CTT stands next to the infant’s shoulder and chest, allowing adequate ventilation without moving after one cycle of chest compression. The rescuer can perform adequate ventilation as soon as possible. Therefore, it is supposed that CTT was better than 2TT and comparable to 2FT in CCF, reducing hands-off time without movement. However, the CCF of 2FT was higher than the other two techniques. Previous studies reported similar results that the hand-off time of the 2TT was significantly longer than in the 2FT [16, 17]. Therefore, our hypothesis predicted that the CCF of CTT would be similar to 2FT. However, as a result of this study, the reason why the CCF of CTT was lower than 2FT may be that participants were familiar with 2FT in infant CPR and had shorter training and practice time on CTT. We may achieve a higher CCF by strengthening education in the new chest compression method, CTT.
A rescuer performing 2FT had the advantage of using only one hand and placing it at the side of the CPR infant. It is helpful for rapid changes between chest compression and mouth-to-mouth ventilation and can reduce hands-off time. Recent manikin studies suggest that the 2TT may be associated with lower CCF [15] and incomplete chest recoil especially when performed by single rescuers [11, 18]. For this reason, the American Heart Association (AHA) resuscitation guidelines recommended that the 2FT be used for performing chest compressions in an infant when a single rescuer is performing cardiopulmonary resuscitation. However, it can cause fatigue and pain in two fingers performing chest compression, and weak and slow chest compression can occur in infant CPR. Therefore, when a single rescuer performs an ongoing CPR, the fatigue and finger pain of the rescuer are important factors in maintaining good CPR performance. Our results showed that 2TT and CTT were associated with less pain and fatigue than 2FT in the participants’ questionnaires.
Our study has several limitations. First, we used the infant CPR manikin model, which may not accurately represent real patients. Although the Laerdal manikin and SkillReporter have been used to simulate several CPR performance studies, because we tried to evaluate a new chest compression technique, further studies to confirm the findings of this study and calculate perfusion pressure of human subjects are needed. Second, despite the fact that crossover design is preferred in simulation studies for statistical power, our study was conducted using a randomized control design. We suppose that a crossover design can create performance and detection bias because the aim of our study was to compare the new and original methods, and participants are likely to prefer one method over the other. Third, the simulation study was ongoing for only 2 minutes because it was assumed that the time of single rescuer CPR was usually 2 minutes. Since it was a simulation study, the Hawthorne effect may have appeared. Therefore, all participants may have tried conducting chest compression harder than in the real situation, and indicators related to chest compression may have been good. The test time was short, so the trial results might look better. If a participant performs chest compression for a longer period of time, the results of each compression technique may differ. Moreover, comparing the first and last cycles by extending the time to perform chest compression, the quality of chest compression may vary owing to the pain or fatigue of the rescuer. Further studies are required to verify these limitations.
Conclusion
Participants using CTT showed a lower CCF than those using 2FT, but performed as well as 2TT at chest compression depth and may help maintain an accurate chest compression position in CPR. Also, rescuers suffered less pain and fatigue performing with CTT. Therefore, a new chest compression technique, CTT may be an effective alternative method for infant cardiac arrest by a single rescuer.
Supporting information
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by a grant from Research Year of Inje University in 20170096. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Maconochie IK, Bingham R, Eich C, Lopez-Herce J, Rodriguez-Nunez A, Rajka T, et al. European resuscitation council guidelines for resuscitation 2015: section 6. paediatric life support. Resuscitation. 2015;95:223–248. doi: 10.1016/j.resuscitation.2015.07.028 [DOI] [PubMed] [Google Scholar]
- 2.Meaney PA, Bobrow BJ, Mancini ME, Christenson J, De Caen AR, Bhanji F, et al. Cardiopulmonary resuscitation quality: improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128:417–435. doi: 10.1161/CIR.0b013e31829d8654 [DOI] [PubMed] [Google Scholar]
- 3.Topjian AA, Raymond TT, Atkins D, Chan M, Duff JP, Joyner BL Jr, et al. Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S469–S523. doi: 10.1161/CIR.0000000000000901 [DOI] [PubMed] [Google Scholar]
- 4.Lee J, Kim DK, Kang EK, Kim JT, Na JY, Par B, et al. 2020 Korean Guidelines for Cardiopulmonary Resuscitation. Part 6. Pediatric basic life support. Clin Exp Emerg Med. 2021;8: S65–S80. doi: 10.15441/ceem.21.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O’Hearn N, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA.2005;293:305–310. doi: 10.1001/jama.293.3.305 [DOI] [PubMed] [Google Scholar]
- 6.Niles DE, Duval-Arnould J, Skellett S, Knight L, Su F, Raymond TT, et al. Characterization of Pediatric In- Hospital Cardiopulmonary Resuscitation Quality Metrics Across an International Resuscitation Collaborative. Pediatr Crit Care Med. 2018;19:421–432. doi: 10.1097/PCC.0000000000001520 [DOI] [PubMed] [Google Scholar]
- 7.Donoghue AJ, Myers S, Kerrey B, Sandler A, Keane R, Watanabe I, et al. Analysis of CPR quality by individual providers in the pediatric emergency department. Resuscitation. 2020;153:37–44. doi: 10.1016/j.resuscitation.2020.05.026 [DOI] [PubMed] [Google Scholar]
- 8.Donoghue A, Hsieh TC, Myers S, Mak A, Sutton R, Nadkarni V. Videographic assessment of cardiopulmonary resuscitation quality in the pediatric emergency department. Resuscitation. 2015;91:19–25. doi: 10.1016/j.resuscitation.2015.03.007 [DOI] [PubMed] [Google Scholar]
- 9.O’Connell KJ, Keane RR, Cochrane NH, Sandler AB, Donoghue AJ, Kerrey BT, et al. Pauses in compressions during pediatric CPR: Opportunities for improving CPR quality. Resuscitation. 2019;145:158–165. doi: 10.1016/j.resuscitation.2019.08.015 [DOI] [PubMed] [Google Scholar]
- 10.Jang HY, Wolfe H, Hsieh TC, Abbadessa MK, Myers S, Nadkarni V, et al. Infant chest compression quality: A video-based comparison of two-thumb versus one-hand technique in the emergency department. Resuscitation. 2018;122:36–40. doi: 10.1016/j.resuscitation.2017.11.044 [DOI] [PubMed] [Google Scholar]
- 11.Tsou JY, Kao CL, Chang CJ, Tu YF, Su FC, Chi CH. Biomechanics of two-thumb vs two-finger chest compression for CPR in an infant manikin model. Eur J Emerg Med. 2020;27:132–136. doi: 10.1097/MEJ.0000000000000631 [DOI] [PubMed] [Google Scholar]
- 12.Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, et al. Resuscitation Outcomes Consortium Investigators. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120:1241–1247. doi: 10.1161/CIRCULATIONAHA.109.852202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Millin MG, Bogumil D, Fishe JN, Burke RV. Comparing the two-finger versus two-thumb technique for single person infant CPR: a systematic review and meta-analysis. Resuscitation. 2020;148:161–172. doi: 10.1016/j.resuscitation.2019.12.039 [DOI] [PubMed] [Google Scholar]
- 14.Lee JE, Lee J, Oh J, Park CH, Kang H, Lim TH, et al. Comparison of two-thumb encircling and two-finger technique during infant cardiopulmonary resuscitation with single rescuer in simulation studies: a systematic review and meta-analysis. Medicine (Baltimore). 2019;98:e17853. doi: 10.1097/MD.0000000000017853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee SY, Hong JY, Oh JH, Son SH. The superiority of the two-thumb over the two-finger technique for single-rescuer infant cardiopulmonary resuscitation. Eur J Emerg Med. 2018;25:372–376. doi: 10.1097/MEJ.0000000000000461 [DOI] [PubMed] [Google Scholar]
- 16.Udassi S, Udassi JP, Lamb MA, Theriaque DW, Shuster JJ, Zaritsky AL, et al. Two-thumb technique is superior to two-finger technique during lone rescuer infant manikin CPR. Resuscitation. 2010;81:712–717. doi: 10.1016/j.resuscitation.2009.12.029 [DOI] [PubMed] [Google Scholar]
- 17.Yang D, Kim KH, Oh JH, Son S, Cho J, Seo KM. Development and Evaluation of a New Chest Compression Technique for Cardiopulmonary Resuscitation in Infants. Pediatr Cardiol. 2019;40:1217–1223. doi: 10.1007/s00246-019-02135-x [DOI] [PubMed] [Google Scholar]
- 18.Pellegrino JL, Bogumil D, Epstein JL, Burke RV. Two-thumb-encircling advantageous for lay responder infant CPR: a randomised manikin study. Arch Dis Child. 2019;104:530–534. doi: 10.1136/archdischild-2018-314893 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.