Abstract
Introduction
This study aims to summarize the available evidence and guideline/consensus recommendations for acupuncture and moxibustion in the treatment, prevention and rehabilitation of patients with coronavirus disease 2019 (COVID-19).
Methods
A scoping review was performed. Eight electronic databases and other related websites were searched. All studies related to acupuncture and moxibustion for COVID-19 were considered. Descriptive analysis was applied to analyze the all included studies and guideline recommendations.
Results
We ultimately included 131 eligible studies. The main topics of the included studies were the treatment (82.4%) and prevention (38.9%) of COVID-19. The most included studies were literature reviews (65, 49.6%), protocols of systematic reviews (20, 15.3%), and guidelines and consensuses (18, 13.7%). The 18 (13.7%) COVID-19 guidelines and consensuses included 47 recommendations on acupuncture and moxibustion, which focused on the treatment (21/47, 44.7%), rehabilitation (17/47, 36.2%) and prevention (6, 12.8%) of COVID-19 patients. Zusanli (ST36), Feishu (BL13), Guanyuan (RN4) were recommended mostly for the treatment, rehabilitation and prevention respectively.
Conclusion
Acupuncture and moxibustion are effective in the treatment of COVID-19 patients to some extent. However, more high-quality of clinical trials still needed to determine the feasibility of acupuncture and moxibustion in COVID-19 patients to better guide clinical practice.
Study registration
Open Science Framework Registries (Registration DOI: 10.17605/OSF.IO/Z35WN; https://osf.io/z35wn).
Keywords: Scoping review, COVID-19, Acupuncture and moxibustion
1. Introduction
Since it was initially reported in December 2019, the coronavirus disease 2019 (COVID-19) has spread rapidly around the world, causing great harm to people's lives and safety as well as economic and social stability. COVID-19 is an acute respiratory infectious disease, and the clinical symptoms1,2 of patients are fever, malaise, cough, sputum, dyspnea, headache, dizziness, etc., which are sometimes accompanied by diarrhea, vomiting, etc. The main clinical measures for COVID-19 are isolation, antiviral therapy and symptomatic support, and there are no specific therapeutic drugs.3 Acupuncture has a long history for the prevention and treatment of epidemics, and rich clinical experience has been accumulated.4 Some studies have shown that acupuncture has potential benefits in the treatment of some modern acute infectious diseases, such as epidemic hemorrhagic fever, influenza, acute bacterial dysentery and severe acute respiratory syndrome (SARS),5 and that it has advantages in reducing fever, relieving cough and phlegm, alleviating gastrointestinal symptoms, promoting respiratory function and preventing deterioration of disease6, 7, 8, 9. Therefore, a variety of studies have discussed and investigated the effects of acupuncture in the prevention, treatment, and rehabilitation of COVID-19 patients during this epidemic. Analyzing and disseminating the Chinese experience with acupuncture during the epidemic, conducting relevant studies and further developing evidence-based clinical practice guidelines are expected to promote a greater role for acupuncture in global efforts to fight the epidemic.10,11
To comprehensively clarify the role of acupuncture in the treatment, prevention and rehabilitation of COVID-19 patients, all studies related to the application of acupuncture and moxibustion in COVID-19 patients were systematically searched and analyzed in this scoping review. To further investigate the recommended status of acupuncture and moxibustion, we also searched the guidelines and consensuses, and analyzed the related recommendations on acupuncture and moxibustion. We aimed to summarize the current status of the efficacy and safety of acupuncture therapy for COVID-19 and provide references for clinical researchers and practitioners.
2. Methods
We conducted a scoping review to identify the role of acupuncture in the treatment, prevention and rehabilitation of patients with COVID-19. We performed this scoping review following the methodology recommended by Joanna Briggs Institute (JBI)12 and followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) statement13 to draft this paper (Supplement 1). This scoping review has been registered in the Open Science Framework Registries (Registration DOI: 10.17605/OSF.IO/Z35WN).
2.1. Search strategy
We performed a systematic search of the China National Knowledge Infrastructure (CNKI), Wanfang Data, China Biology Medicine (CBM), MEDLINE via PubMed, Embase, and the Cochrane Library, Web of Science (WOS), and Epistemonikos using the terms “COVID-19”, “SARS-CoV-2”, “2019 novel coronavirus”, “2019-nCoV”, “coronavirus disease 2019”, “2019-novel coronavirus”, “acupuncture”, “acupressure”, “acupoint”, “moxibustion”, and “needle”, etc. with a publication date of 1 January 2020 to 1 April 2022. In addition, we retrieved traditional Chinese Medicine (TCM) guidelines and consensus for COVID-19 to identify the acupuncture-related recommendations from databases and websites (Chinese Center for Disease Control and Prevention, National Administration of Traditional Chinese Medicine (TCM), and World Health Organization (WHO) Guideline website).
Two researchers (Ren M and Liu Y) independently searched above databases, websites and other sources. The full search strategies of databases are shown in Supplement 2.
2.2. Inclusion and exclusion criteria
Studies that met the following criteria were eligible for inclusion: 1) Studies for the use of acupuncture and moxibustion combined with or without other treatment methods in COVID-19 patients in the different stage of disease or with other comorbidities; 2) Type of study: guideline that met the IOM definition from 199014 or 201115 and consensus containing recommendations on acupuncture and moxibustion, systematic review (SR), clinical trials (including randomized controlled trials (RCTs), case report, case series, and non-RCTs), observational studies, literature reviews and protocols. The following studies were excluded: 1) studies that were not published in Chinese or English; 2) The full texts are inaccessible; 3) conference abstracts, letters, comments, editorials and news reports; 4) translations and interpretations; 5) animal and basic researches. Furthermore, for studies published in multiple journals, we selected the earlier publications for inclusion. And for studies published in different versions, such as simplified and standard versions, we included the one reported more information.
2.3. Study selection and data extraction
We used Endnote X9 software to manage the literature. Two researchers (Ren M and Liu Y) independently screened all titles, abstracts, and full texts. All disagreements were resolved through consensus or by consultation with a third researcher (Kuang Z).
For the included studies, we extracted the following information: 1) basic information: title, the first author, country, journal, publication or posted date, study type, and the research topics; 2) as for COVID-19 guidelines and consensuses, we additionally extracted some details about recommendations on the acupuncture and moxibustion, such as focused topics, recommended acupoints, and operation frequency; 3) for other type of studies, we extracted the PICO (patients, interventions, comparisons and outcomes) information, as well as main results and effect sizes if available.
Two researchers (Ren M and Liu Y) independently performed data extraction according to the predefined plan and resolved disagreements through consensus or by consultation with a third researcher (Li H).
2.4. Data analysis
We performed a descriptive analysis of the included studies based on the different study types. For COVID-19 guidelines or consensuses, in addition to the above basic information, we also qualitatively analyzed specific information about the recommendations.
3. Results
3.1. Search results
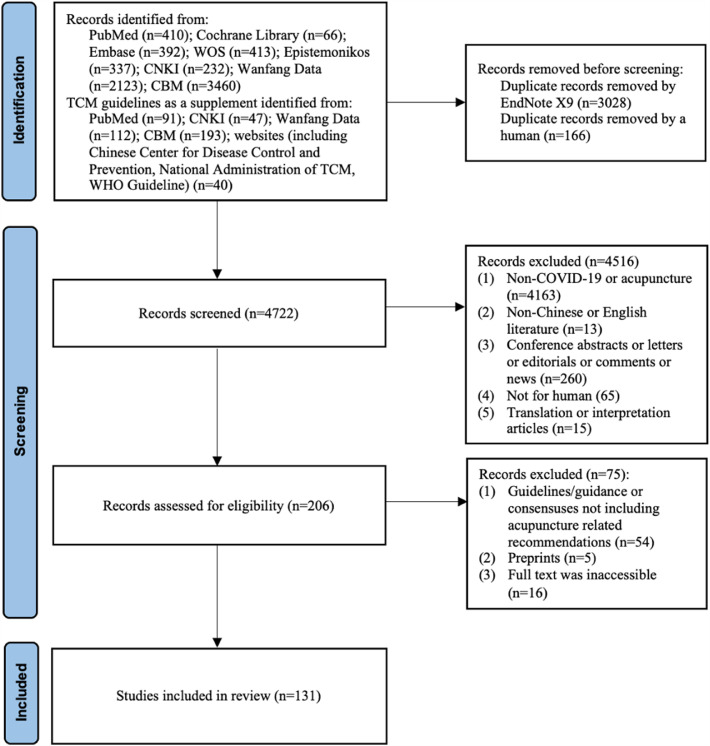
We identified 7916 records after systematic retrieval, and 3194 records were excluded before screening because they were duplicates. After excluding the ineligible studies, 131 studies were finally analyzed in this scoping review. The literature search and screening process is shown in Fig. 1 and the checklist of included studies is shown in supplement 3.
Fig. 1.
Flowchart of the study selection process.
3.2. Characteristics of the included studies
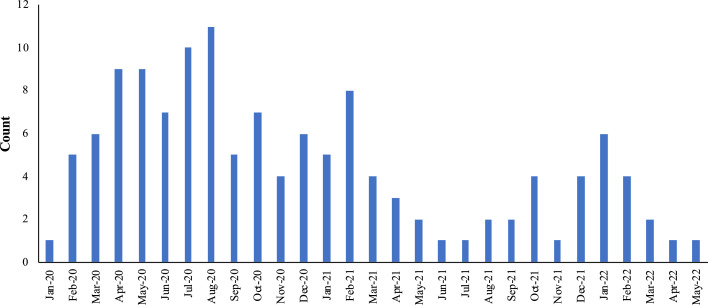
Of the 131 included articles related to the use of acupuncture therapy for COVID-19, 122 (93.1%) were from China, and the remaining articles were from the Iran, US, Belgium, Indonesia, and Mexico. The publication dates of included studies were concentrated on April, 2020 to August, 2020. More than half (95, 72.5%) of the studies were published in Chinese. The most focused topics of included studies were about the treatment (82.4%), prevention (38.9%) and rehabilitation (12.2%) of COVID-19 patients, and the main study type was literature review (65, 49.6%). There were 18 (13.7%) COVID-19 guidelines and consensuses, 6 (33.3%) of which were guidelines and 12 (66.7%) of which were consensuses, and they were all developed by Chinese researchers or institutions. The characteristics of the included studies are shown in Table 1 and the distribution of publication dates of included studies is shown in Fig. 2.
Table 1.
The characteristics of the included studies (N=131).
| Items | Count, n (%) | |
|---|---|---|
| Study type | Review | 65 (49.6) |
| SR protocol | 20 (14.2) | |
| Guideline/consensus | 18 (13.7) | |
| Case series | 9 (6.9) | |
| Case report | 7 (5.3) | |
| RCT/NRSI | 10 (7.6) | |
| Qualitative systematic review | 1 (0.8) | |
| Scoping review | 1 (0.8) | |
| Country | China | 122 (93.1) |
| United States | 4 (3.1) | |
| Belgium | 2 (1.5) | |
| Iran | 1 (0.8) | |
| Indonesia | 1 (0.8) | |
| Mexico | 1 (0.8) | |
| Language | Chinese | 95 (72.5) |
| English | 36 (27.5) | |
| Topic | Treatment | 67 (51.1) |
| Treatment & prevention | 38 (29.0) | |
| Rehabilitation | 11 (8.4) | |
| Prevention | 7 (5.3) | |
| Rehabilitation & prevention | 3 (2.3) | |
| Treatment & rehabilitation & prevention | 2 (1.5) | |
| Comprehensive application | 1 (0.8) | |
| Nursing | 1 (0.8) | |
| Treatment & prevention & control | 1 (0.8) |
NRSI: nonrandomized studies of the effects of interventions; RCT: randomized controlled trial; SR: systematic review.
Fig. 2.
The distribution of publication dates of included studies.
3.3. COVID-19 guidelines and consensuses
Among the included 18 TCM guidelines and consensuses for COVID-19 (Supplement 3), only two guidelines16, 17 focused specifically on the use of acupuncture for COVID-19 treatment, and these were issued by the China Association of Acupuncture-Moxibustion. The rest of studies were comprehensive TCM guidelines or consensuses including recommendations on acupuncture and moxibustion. The first article, “Guidance on Acupuncture Intervention for Novel Coronavirus Pneumonia”,16 was published in February 2020 and focused on the principles, methods, and procedures of acupuncture intervention in suspected, mild, common, and recovered COVID-19 cases. In May 2020, the second version of this article17 was published, which described more operation details, adverse events and syndrome differentiation based on the first version. However, the two versions reported recommendations primarily based on experts’ experience without citing any references, and no method process (such as systematic searches, evidence grading etc.) were reported.
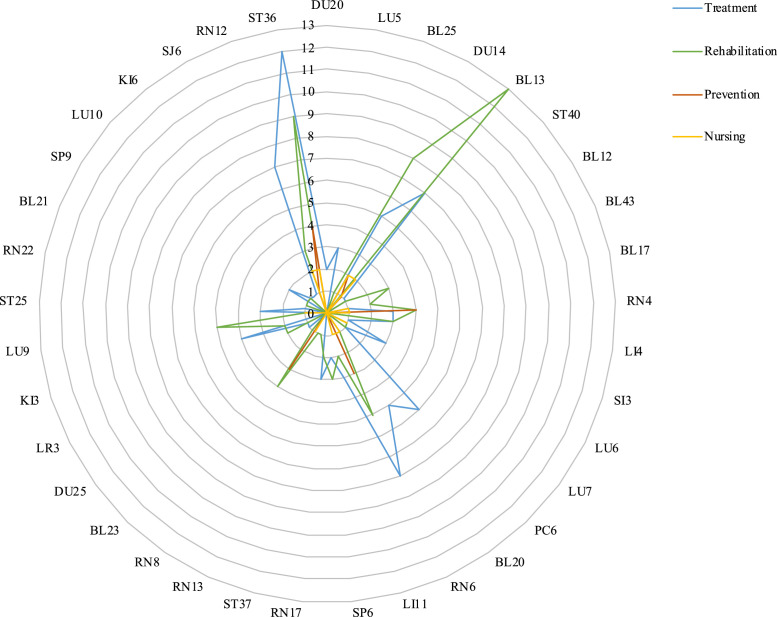
We extracted 47 recommendations on acupuncture and moxibustion applied in COVID-19 patients, most of which (21, 44.7%) were for the treatment. Compared to the acupuncture (23, 48.9%), moxibustion (42, 89.4%) were recommended as the intervention method for COVID-19 patients more frequently. As for the operation methods of acupuncture and moxibustion, the most of current recommendations didn't explain the details. Among all the recommendations, 45 (95.7%) recommendations provided corresponding acupoints. Considering the complexity of syndrome differentiation, we only summarized the frequency of main recommended acupoints according to the different purposes in Fig. 3. Zusanli (ST36), Feishu (BL13), Guanyuan (RN4) and Dazhui (DU14) were recommended mainly for the treatment (13.0%, 12/92), rehabilitation (15.9%, 13/82), prevention (22.2%, 4/18) and nursing (12.5%, 2/16) respectively. More details about the 47 recommendations are in Table 2.
Fig. 3.
The frequency of recommended acupoints.
Table 2.
The information of recommendations on acupuncture and moxibustion applied in COVID-19 patients.
| Item | Count, n (%) | |
|---|---|---|
| Number of recommendations | Guideline | 17 (36.2) |
| Consensus | 30 (63.8) | |
| Topic | Treatment | 21 (44.7) |
| Rehabilitation | 17 (36.2) | |
| Prevention | 6 (12.8) | |
| Nursing | 3 (6.4) | |
| Intervention methods | Acupuncture | 23 (48.9) |
| Moxibustion | 42 (89.4) | |
| Frequency of acupuncture or moxibustion | Once a day | 23 (48.9) |
| Twice a day | 2 (4.3) | |
| Once every 1–2 days | 3 (6.4) | |
| Once every 3–5 days | 1 (2.1) | |
| Not reported | 18 (38.3) | |
| Whether to provide the acupoints | Yes | 45 (95.7) |
| No | 2 (4.3) | |
| Whether to describe the settings | Yes | 10 (21.3) |
| No | 37 (78.7) | |
| Whether to describe the matters needing attention | Yes | 16 (34.0) |
| No | 31 (66.0) | |
| Grading of quality of evidence | Yes | 2 (4.3) |
| No | 45 (95.7) | |
| Grading of strength of recommendations | Yes | 2 (4.3) |
| No | 45 (95.7) |
3.4. Systematic reviews and the protocols
There was one qualitative systematic review, one scoping review and 20 protocols of systematic review included in this study (Supplement 3). The two reviews18, 19 both concluded that acupuncture could improve the symptoms of COVID-19 patients, and one of which found that acupuncture could also relieve the negative emotions to improve the health status.18 More details about the two reviews are in Table 3. All of the protocols were published by Chinese researchers in Medicine. Half of them planned to explore the effect of symptomatic treatment, including nasal congestion,20 abdominal pain,21 diarrhea,22 headache,23,25,31 anorexia,24 breathlessness37 and anxiety28,39. The remaining 10 protocols26, 27,29, 30,32, 33, 34, 35, 36,38 focused on the efficacy and safety of acupuncture and moxibustion. However, these registered systematic reviews have not yet been published. More information about the included protocols is in Table 4.
Table 3.
The information of included systematic reviews.
| Study ID | Study type | First author's country | Included studies | Participants | Intervention | Comparison | Main results |
|---|---|---|---|---|---|---|---|
| Badakhsh M (2021)18 | Qualitative systematic review | Iran | 1 retrospective cohorts, 1 case series and 1 case report | COVID-19 patients | Acupuncture | NA | Reduce the negative emotions, improve symptoms (such as chest distress, shortness of breath, and dull pain in epigastric region, etc.) and regain the consciousness. |
| Chen C (2021)19 | Scoping review | China | 7 case reports, 6 observational studies, 1 review, 1 RCT and 1 nonrandomized clinical trial | COVID-19 patients | Acupuncture with other interventions | NA | Acupuncture can relieve the symptoms of COVID-19 patients, shorten the length of hospital stay, and is effective for elderly patients with serious illnesses. But there is a lack of high-quality clinical trials. |
NA: Not available.
Table 4.
The information of included protocols of systematic review.
| Study ID | Registration number | Included studies | Participant | Intervention | Comparison | Outcome |
|---|---|---|---|---|---|---|
| Dong Z (2022)20 | CRD42021299482 | RCT | COVID-19 patients with recorded nasal congestion lasted for 1 week or more | Acupuncture with COVID-19 treatment | Comfort therapy or other therapies | The frequency of nasal congesture, duration of nasal congestion, the degree of nasal congestion, quality of life |
| Li X (2022)21 | INPLASY2021120104 | RCT | COVID-19 patients with abdominal pain lasting 2 weeks or longer | Moxibustion (direct moxibustion, separated moxibustion, moxibustion therapy, warm moxibustion, indirect moxibustion) with COVID-19 treatment | Other treatment without moxibustion | Abdominal pain frequency, abdominal pain intensity, duration of abdominal pain, duration of use of painkillers, quality of life, adverse events |
| Liu N (2022)22 | CRD42022302933 | RCT | COVID-19 patients with diarrhea lasting 4 weeks or longer | Moxibustion, herb partitioned moxibustion, moxibustion with amugwort stick, or ormoxa cone moxibustion with COVID-19 treatment | Comfort therapy or other therapies | The Bristol score, number of bowel movements, quality of life, associated symptoms of diarrhea, adverse events |
| Luo W (2022)23 | CRD42021265699 | RCT | COVID-19 patients suffering from headache and/or olfaction and/or taste disorders | Acupuncture, electro-acupuncture, auricular acupuncture, or laser acupuncture with COVID-19 treatment | Comfort therapy or other therapies | Relevant indicators of headache, olfaction disorders, taste impairment, adverse events |
| Wang X (2022)24 | CRD42022302499 | RCT | COVID-19 patients with anorexia | Moxibustion therapies (including moxa stick moxibustion, moxa cone moxibustion, direct moxibustion, and indirect moxibustion) | NR | Effective rate of clinical symptoms, body weight, food intake on the gastrointestinal symptom rating scale (GSRS total score), the incidence of nausea and adverse events |
| Sun M (2021)25 | CRD42021270722 | RCT | COVID-19 patients with headache of 4 weeks duration or longer | Acupuncture, electro-acupuncture, auricular acupuncture, or laser acupuncture with COVID-19 treatment | Comfort therapy or other therapies | Headache frequency, headache intensity, duration of headache, times of using painkiller, quality of life, adverse events |
| Xia Q (2021)26 | CRD42020225245 | RCTs and credible clinical observations | Elderly patients (≥60 years) diagnosed with COVID-19 | Acupuncture, moxibustion, electroacupuncture, fire needle, warming needle moxibustion, acupoint injection or auricular therapy | Any method other than acupuncture | Mortality rate, cure rate, CRP, creatine, troponin, aspartate aminotransferase, alanine aminotransferase, improvements in chest CT scans, the disappearance time of clinical symptoms and the side effects |
| Zhou Y (2021)27 | CRD42021230364 | RCT | Patients who were diagnosed with COVID-19 convalescence | Moxibustion alone, or combined with other kinds of therapies | Other treatment without moxibustion | The time of disappearance of main symptoms, reexamination of chest X-ray, white blood cell count, associated symptoms disappear rate, negative COVID-19 results rate, quality of life, occurrence rate of common type to severe form, clinical cure rate, mortality, adverse events |
| Jia H (2020)28 | CRD42020190153 | RCTs and observational trials | COVID-19 patients with anxiety | Acupuncture and related interventions treatment | Sham acupuncture, routine care, or conventional therapy | Therapeutic effects, the adverse effects and adverse events, the safety of physicians |
| Chen Y (2020)29 | CRD42020180875 | RCT | COVID-19 patients | Acupuncture (combined with other treatments, such as routine therapy, etc.) | Other therapeutic approaches other than acupuncture | The influence of acupuncture on chest CT and nucleic acid detection of respiratory samples, accompanying symptoms |
| Chi W (2020)30 | CRD42020206889 | RCT | COVID-19 patients who use a ventilator during treatment | Acupuncture (combined with other treatments, such as respiratory rehabilitation training, routine therapy, etc.) | Other therapeutic approaches other than acupuncture | MIP, MEP, MIP/MEP, PaO2/FiO2, blood oxygen saturation, FEV1, FVC, FEV1/FVC, Borg scale scores, adverse events, changes of patient's condition |
| Gao W (2020)31 | CRD42020199508 | RCTs and trials with 2-arm or 3-arm parallel design | Patients with headache induced by COVID-19 | Plum-blossom needle therapy | Western medicine therapy | The time and rate of appearance of headache, the length of hospital stay |
| Huang K (2020)32 | CRD42020189494 | RCTs and credible clinical observations | COVID-19 patients | Acupuncture therapy | Interventions including western medicine | Mortality rate, CRP, creatine, troponin, liver enzymes, blood pressure, clinical symptoms, serum cytokine levels, diverse events |
| Liu M (2020)33 | CRD42020193703 | RCTs and credible clinical observations | COVID-19 patients | Fire needle alone or combined with one or more other pharmacological intervention | Standard care, western medical therapies, Chinese medicine, etc. | Conversion rate from normal to severe, cure rate, mortality rate, Chest CT scans, nucleic acid detection of respiratory samples, accompanying symptoms disappear rate, cellular inflammation level, average hospitalization time, adverse reactions |
| Wang Z (2020)34 | CRD42020211910 | RCTs, non-RCTs, and clinical case reports | COVID-19 patients | moxibustion alone or combined with other kinds of therapies | Any kind of treatment without moxibustion | Total clinical effective rate, antipyretic time, cough duration, rhombus disappearance time, imaging transition time, serum CRP level after treatment |
| Wen D (2020)35 | CRD42020183736 | RCT | COVID-19 (≥16 years old) | Acupuncture therapy (including manual acupuncture, body acupuncture, electroacupuncture, plum blossom needle, warm needling, and fire needling) | Sham acupuncture, placebo, usual care, medication, no treatment, and other conventional therapies | Timing of the disappearance of the main symptoms, serum cytokine levels, timing of the disappearance of accompanying symptoms, negative COVID-19 results rates, CT image improvement, average hospitalization time, occurrence rate of common type to severe form, clinical cure rate, mortality |
| Wu L (2020)36 | CRD42020181336 | RCT | COVID-19 patients | The external treatment of TCM (such as, acupuncture, massage, etc.) | Treatments other than the external treatment of TCM | Efficacy, accompanying symptoms disappear rate, average hospitalization time, occurrence rate of common type to severe form, clinical cure rate, mortality |
| Zhang B (2020)37 | CRD42020182323 | RCT | COVID-19 patients with breathlessness | Acupuncture (combined with other treatments, such as routine therapy, etc.) | Other therapeutic approaches other than acupuncture | Visual analogue scale, numerical rating scale, the Borg Scale |
| Zhang Q (2020)38 | CRD42020185776 | RCT | COVID-19 patients | Acupuncture alone or moxibustion alone or both of the two treatments | Western medicine, placebo or regular treatment | The total clinical effective rate, antipyretic time, cough duration, rhombus disappearance time, imaging transition time, serum CRP after treatment, adverse events |
| Zhang Y (2020)39 | CRD42020202258 | RCT | COVID-19 patients with anxiety | Acupuncture (including warm acupuncture, electroacupuncture, scalp-acupuncture, hydroacupuncture, and manual acupuncture) | Any kinds of treatments except acupuncture | Hamilton Anxiety Scale (HAM-A), The Liebowitz Social Anxiety Scale (LSAS), (modified) Barthel index (MBI), side effect or adverse event |
CRP: C-reactive protein level; FEV1: forced expiratory volume in 1 second; FiO2: fraction of inspired oxygen; FVC: forced vital capacity; MEP: maximum expiratory pressure; MIP: maximum inspiratory pressure; NR: not reported; PaO2: arterial partial pressure of oxygen; TCM: traditional Chinese medicine.
3.5. RCTs and nonrandomized studies of the effects of interventions (NRSIs)
There were six RCTs, three self-controlled trials and one non-randomized clinical trial included (Supplement 3), and they were all published by Chinese researchers. The intervention group used different ways of acupuncture and moxibustion, including Xizhiyanbing moxibustion,41 thunder fire moxibustion,42 thumb-tack needle,43 fiery dragon cupping comprehensive moxibustion,46 and filiform-fire needle,49 with or without other Chinese medicine and routine western medicine. And the control group received corresponding conventional treatment,40, 41,44, 45 TCM decoction42 and sham needle,43 etc. The outcomes these trials focused on were more about total clinical effective rate, TCM syndrome score, pulmonary function, clinical symptoms, as well as the depression and anxiety scores (Table 5). The results showed that acupuncture and moxibustion can improve the above outcomes of COVID-19 patients to some extent, but the findings were not always consistent. The detailed results and effect sizes are presented in Table 5.
Table 5.
The information about RCTs and NRSIs.
| Study ID | Study type | Participants | Count (intervention/control) | Intervention | Control | Outcome | effect size (intervention vs. control) |
|---|---|---|---|---|---|---|---|
| Zhao H (2022)40 | RCT | Discharged COVID-19 patients | 27/28 | Mild moxibustion + conventional intervention | Conventional intervention | TCM syndrome score (±s) | before treatment: 223.59±67.65 vs. 231.10±70.44, P>0.05; treatment after 2 weeks: 70.04±33.83 vs. 230.71±70.36, P<0.05; return visit: 69.63±33.26 vs. 227.60±68.89, P<0.05 |
| Self-rating anxiety score (±s) | before treatment: 39.93±9.94 vs. 40.03±9.96, P>0.05; treatment after 2 weeks: 34.81±8.12 vs. 39.79±9.77, P<0.05; return visit: 33.89±8.10 vs. 39.21±9.44, P<0.05 | ||||||
| Depression self-assessment score (±s) | before treatment: 37.67±9.72 vs. 37.79±9.67, P>0.05; treatment after 2 weeks: 36.22±9.52 vs. 37.46±9.52, P>0.05; return visit: 33.44±9.74 vs. 37.32±9.51, P<0.05 | ||||||
| Zhu J (2022)41 | RCT | COVID-19 patients | 31/33 | Xizhiyanbing moxibustion + conventional management | Conventional discharged management | Positive rate of IgG and IgM (%) | IgG: 96.8% vs. 75.8%, P<0.05; IgM: 9.7% vs. 39.4%, P<0.05 |
| Nucleic acid positive rate (%) | blood: 3.2% vs. 27.3%, P<0.05; nasopharyngeal swab: 16.1% vs. 51.5%, P<0.05; anal swab: 6.5% vs. 33.3%, P<0.05 | ||||||
| Li C (2022)42 | RCT | Children with COVID-19 (7–17 years old) | 30/30 | Thunder fire moxibustion + Qingfeipaidu decoction | Qingfeipaidu decoction | Total clinical effective rate (%) | 83.33% vs. 60.00%, P<0.05 |
| TCM syndrome score (±s) | before treatment: 21.37±3.65 vs. 20.89 ±3.53, P>0.05; after treatment: 7.79 ±2.31 vs. 11.47±3.26, P<0.01 | ||||||
| Disappearance rate of symptom (%) | fever: 100.00% vs. 83.33%, P>0.05; cough and expectoration: 83.33% vs. 40.00%, P<0.01 | ||||||
| Ig level (±s, g/L) | before treatment: IgG: 11.15±2.28 vs. 11.23±2.87, IgA: 1.70 ±0.64 vs. 1.72 ±0.86, IgM: 1.14 ±0.31 vs. 1.11 ±0.32, P>0.05; after treatment: IgG: 13.71±2.04 vs. 12.57±2.13, IgA: 2.40 ±0.47 vs. 2.14 ±0.52, IgM: 1.62 ±0.33 vs. 1.39 ±0.36, P<0.05 | ||||||
| Luo Z (2022)43 | RCT | COVID-19 convalescents | 25/25 | Thumb-tack needle | Sham thumb-tack needle | TCM syndrome score [M(IQR)] | before treatment: 30(5.5) vs. 29(6.0), P>0.05; after treatment: 7(10.0) vs. 13(4.0), P<0.05 |
| Hamilton anxiety scale (HAMA) score (±s) | before treatment: 14.49±5.96 vs. 15.01±4.43, P>0.05; after treatment: 4.54±3.60 vs. 10.62±4.17, P<0.05 | ||||||
| Hamilton depression scale (HAMD) score (±s) | before treatment: 12.36±4.17 vs. 13.02±5.27, P>0.05; after treatment: 3.85±4.26 vs. 9.48±3.08, P<0.05 | ||||||
| Pulmonary function (±s) | before treatment: FVC/L: 2.44±0.26 vs. 2.57±0.29, FEV1/L: 1.88±0.33 vs. 1.90±0.35, PEF/L·s–1: 4.35±0.47 vs. 4.28±0.43, P>0.05; after treatment: FVC/L: 3.27±0.32 vs. 2.84±0.28, FEV1/L: 2.64±0.27 vs. 2.21±0.23, PEF/L·s–1: 6.15±0.36 vs. 5.33±0.31, P<0.05 | ||||||
| Lung shadow area [M(IQR), mm2] | before treatment: 245.60(154.20) vs. 268.00(214.20), P>0.05; after treatment: 24.10(56.24) vs. 80.30(156.27), P<0.05 | ||||||
| Zeng L (2021)44 | RCT | COVID-19 close contacts | 102/62 | Moxibustion combined with Daiwenjiu plaster | Conventional observation | Self-reporting questionnaire 20 (SRQ-20) scores (±s) | before treatment: 4.61±4.23 vs. 6.16±4.91, P>0.05; after treatment: 3.85±3.83 vs. 5.60±4.54, P<0.05; follow-up: 2.91±3.53 vs. 5.24±4.63, P<0.01 |
| Self-rating anxiety scale (SAS) scores (±s) | before treatment: 44.01±9.33 vs. 45.12±10.35, P>0.05; after treatment: 42.72±7.53 vs. 43.89±10.06, P>0.05; follow-up: 39.95±7.44 vs. 43.06±12.23, P>0.05 | ||||||
| Liu L (2020)45 | RCT | COVID-19 patients | 45/50 | Moxibustion + western medicine | Routine treatment of western medicine | Clinical symptom scores (±s) | before treatment: cough: 1.76±0.48 vs. 1.74±0.53, chest tightness: 1.53±0.59 vs. 1.54±0.54, wheezing; 1.47±0.94 vs. 1.46±0.76, shortness of breath: 1.44±1.06 vs. 1.48±0.50, P>0.05; after treatment: cough: 0.38±0.53 vs. 1.26±0.69, chest tightness: 0.67±0.52 vs. 1.10±0.72, wheezing; 0.29±0.59 vs. 0.76±0.89, shortness of breath: 0.71±0.66 vs. 0.78±0.51, P<0.05 |
| Clinical symptom remission rates (±s) | cough: 79.63±29.49 vs. 29.00±36.58, P<0.05; chest tightness: 53.33±40.45 vs. 24.29±49.96, P<0.05; wheezing: 85.47±26.81 vs. 53.33±45.00, P<0.05; shortness of breath: 49.05±35.23 vs. 43.00±40.41, P>0.05 | ||||||
| Peripheral blood inflammatory index (Difference before and after treatment, ±s) | WBC Count/×109·L–1: 2.64±3.08 vs. 2.14±3.05, P>0.05; CRP/mg·L–1: −25.60±27.07 vs. −14.74±43.42, P>0.05; IL-6/pg·mL–1: −23.47±25.10 vs. −3.79±27.11, P<0.05 | ||||||
| Absolute number of T lymphocyte subsets (Difference before and after treatment, ±s, /μL) | CD3+: 410.67±533.87 vs. 4.08±381.24, P<0.05; CD4+: 290.22±321.32 vs. −4.94±249.84, P<0.05; CD8+: 129.96±233.44 vs. 20.42±146.56, P<0.05 | ||||||
| Dou M (2021)46 | Self-controlled trial | COVID-19 patients | 16/16 | Fiery dragon cupping comprehensive moxibustion | NA | Total clinical effective rate (%) | cough: 87%; shortness of breath: 85% |
| Tao D (2021)47 | Non- randomized clinical trial | COVID-19 convalescents | 31/31 | Moxibustion + oral Chinese medicine | Oral Chinese medicine | TCM syndrome score (±s) | before treatment: 10.10±2.88 vs. 9.71±2.64, P>0.05; after treatment: 2.94±1.79 vs. 4.03±2.01, P<0.05 |
| Total clinical effective rate (%) | 96.77% vs. 80.65%, P<0.05 | ||||||
| 6 minute walk distance, 6MWD (±s, m) | before treatment: 440.32±16.52 vs. 445.67±19.86, P>0.05; after treatment: 496.40±19.55 vs. 486.33±18.80, P<0.05 | ||||||
| Pulse oxygen saturation (SpO2) level (±s, %) | before treatment: 88.89±2.33 vs. 88.48±2.28, P>0.05; after treatment: 94.97±2.17 vs. 93.42±2.26, P<0.05 | ||||||
| St. George's respiratory questionnaire (SGRQ) scores (±s) | before treatment: 48.82±4.38 vs. 49.37±3.86, P>0.05; after treatment: 42.11±5.82 vs. 45.73±6.54, P<0.05 | ||||||
| Dong S (2020)48 | Self-controlled trial | COVID-19 patients with diarrhea | 36/36 | Moxibustion | NA | Syndrome scores of diarrhea (±s) | 1.26± 0.15 vs. 4.87±0.41, P<0.05 |
| Total clinical effective rate (%) | 97.2% | ||||||
| Cure rate (%) | 69.4% | ||||||
| Nucleic acid negative conversion ratio (%) | 86.1% | ||||||
| Luo Z (2022)49 | Self-controlled trial | COVID-19 convalescents | 33/33 | Filiform-fire needle | NA | TCM syndrome score [M(IQR)] | 25.0(4.0) vs. 4.0(6.0), P<0.05 |
| Hamilton anxiety scale (HAMA) score (±s) | 16.28±4.11 vs. 6.04±2.73, P<0.05 | ||||||
| Hamilton depression scale (HAMD) score (±s) | 14.69±3.80 vs. 5.77±3.02, P<0.05 | ||||||
| Pulmonary function (±s) | FVC/L: 2.74±0.35 vs. 3.51±0.29; FEV1/L: 2.02±0.41 vs. 2.83±0.22; PEF/L·s–1: 5.15±0.63 vs. 6.28±0.44, P<0.05 | ||||||
| Lung shadow area [M(IQR), mm2] | 16.88(40.65) vs. 143.77(83.21), P<0.05 | ||||||
| Total clinical effective rate (%) | 84.0% |
FEV1: forced expiratory volume in 1 second; FVC: forced vital capacity; NA: Not Available; PEF: peak expiratory flow; TCM: Traditional Chinese Medicine; WBC: white blood cell.
3.6. Case series and case reports
There were 9 case series and 7 case reports included (Supplement 3), and their main results were outlined in Table 6. Almost all treatment methods have shown some effectiveness, especially for the clinical symptom improvements, such as anxiety and depression.54,60,62 Yet, limited to the type of studies, it cannot provide sufficient and strong evidence to support the application of acupuncture and moxibustion for treating COVID-19 patients.
Table 6.
The information of included case series and case reports.
| Study ID | Study type | First author's country | Number of cases | Number (male/female) | Age/years old (X, range) | Intervention methods | Main results |
|---|---|---|---|---|---|---|---|
| Yin X (2021)50 | case series | China | 17 | 8/9 | 24.8, 41–81 | Acupuncture + Chinese medicine + basic treatment | 14 patients were discharged, and 3 patients were converted from moderate to critical. |
| Gong Y (2021)9 | case series | China | 33 | 8/25 | 59, 13–84 | Acupuncture + basic treatment | 33 patients were cured and discharged with significant improvement in symptoms, no adverse reactions or complications from acupuncture-assisted treatment, and no risk of occupational exposure. |
| Wang H (2021)51 | case report | China | 3 | 3/0 | 77, 66–85 | Intradermal acupuncture + western medicine | Three patients were discharged with significant symptom relief, normal inflammatory indexes and absorbed lung lesion. |
| Ma C (2021)52 | case series | China | 18 | 12/6 | NR, 6–64 | Moxibustion + modified Wuye Lugen Decoction | Symptoms of all patients have improved. |
| Zhou H (2021)53 | case series | China | 41 | 26/15 | 47.8, 17–76 | Moxibustion + Chinese medicine | The total effective rate of treatment was 87.8%, and the symptoms improved significantly. 39 patients had negative nucleic acid after 2 weeks of treatment. |
| Li W (2021)54 | case series | China | 8 | 2/6 | NR, 34∼73 | Acupuncture | The efficiency of acupuncture in treating COVID-19 patients with psychological stress disorder was 87.50%. |
| Yin X (2021)'55 | case report | China | 1 | 0/1 | 81, NA | Acupuncture + Chinese herbal medicine + standard care | Discharged from hospital on day 24 with improved symptoms. |
| Cheng SI (2021)56 | case report | USA | 1 | 0/1 | 37, NA | Acupuncture + cupping | Patients recovered within a week without hospitalization. |
| Yeh BY (2021)57 | case report | China | 1 | 1/0 | 73, NA | Acupuncture + western medicine | Acupuncture shows benefit in COVID-19 patients with hypoxic-ischemic encephalopathy after cardiopulmonary resuscitation. |
| Liu L (2020)58 | case report | China | 1 | 0/1 | 67, NA | Acupuncture + Chinese medicine | Discharged with improved symptoms. |
| Zhang X (2020)59 | case series | China | 7 | 4/3 | 35.7, 22–50 | Chinese and western medicine (moxibustion as adjuvant therapy) | Seven patients were discharged after 14 to 35 days of treatment with negative nucleic acid conversion. |
| Wang M (2020)60 | case series | China | 7 | 4/3 | 39.0, 31–52 | Chinese and western medicine (moxibustion as adjuvant therapy) | Three patients were cured and four patients improved, with an efficiency of 100%. |
| Chen X (2020)61 | case series | China | 192 | NR | NR | Indirect moxibustion | 43 health care workers did not develop infections; 149 patients showed some improvement in symptoms and psychological status. |
| Huang X (2020)62 | case series | China | 42 | 28/14 | 47.0, 29–76 | Heat-sensitive moxibustion + conventional treatment | Heat-sensitive moxibustion can effectively reduce the negative emotions of patients and improve the symptoms of chest tightness with high patient acceptance. |
| Gong Y (2020)'63 | case report | China | 2 | 0/2 | 76.5, 72–81 | Acupuncture + oral administration of “Shanghai leishen No.1 formula” | Two patients were discharged from the hospital after about 1 to 3 months of treatment. |
| Tao L (2020)64 | case report | China | 1 | 0/1 | 64, NA | Acupuncture + basic treatment | After 10 days of treatment, the patient's lung lesions were significantly absorbed and the nucleic acid converted negative. |
NA: Not available; NR: Not reported.
3.7. Reviews
There were 65 literature reviews (Supplement 3), and most of them focused on the effect of treatment (89.2%) and prevention (67.7%) of acupuncture and moxibustion in COVID-19 patients. We concluded the main topics of included reviews focused on.???
3.7.1. Mechanisms
Some reviews65, 66, 67, 68, 69, 70 analyzed the possible mechanism of acupuncture and moxibustion, and revealed that acupuncture can prevent and treat COVID-19 by inducing anti-inflammatory responses, regulating immune function, protecting damaged organs, exerting bactericidal and antibacterial effects. Specifically, (1) acupuncture can regulate the number of immune cells, such as lymphocytes and natural killer cells, and it can also activate the vagal cholinergic anti-inflammatory pathway and hypothalamic-pituitary-adrenal axis to induce anti-inflammatory responses to play a role in rapid and precise inflammation and immune regulation.65,69, 70 (2) Moxibustion can protect liver and kidney function by improving the circulation and metabolic function of the body and accelerating the removal of free radicals in the kidney. Severe patients are prone to a "cytokine storm", and acupuncture can protect internal organs by activating the vagus nerve.66, 67, 68, 69
3.7.2. Feasibility analysis
Some reviews11,71, 72, 73, 74, 75, 76, 77, 78, 79 analyzed the feasibility of acupuncture for COVID-19 from the following perspectives: (1) the characteristics of acupuncture. Acupuncture is cheap and simple to perform, which is beneficial for enhancing immunity in susceptible groups, as acupuncture can be performed at home during the epidemic.11,72 (2) Rich experience against the epidemic. Acupuncture has been used in the treatment of infectious diseases for a long time and has been recorded in some classics and literature.75, 76, 77 (3) Effective symptomatic treatment. Acupuncture has good efficacy in reducing fever, relieving cough and phlegm, alleviating digestive symptoms, promoting lung function, and improving the emotions.74, 75,78, 79
3.7.3. Hypothesis and discussion on proposed methods for prevention and treatment
Some reviews introduced and analyzed the origin of acupuncture therapies for the application of acupuncture and moxibustion in COVID-19,80, 81, 82, 83, 84 the principles of acupoint selection and the characteristics of SARS-CoV-2 and COVID-19 to explore individual and common ideas for the prevention and treatment of the disease and to provide directions for future clinical trials.85, 86, 87, 88
The above reviews included the experts’ experience and precious suggestions, and provided some useful researches, which may provoke extensive and deep thinking among readers. However, the scientificity, credibility and implementability of interventions proposed by those studies still need to be higher quality clinical trials to be proved.
4. Discussion
This scoping review found that the types of included studies were mainly reviews, case series and case reports, and there were a lack of clinical studies, systematic reviews and meta-analyses. From 1 January 2020 to 1 April 2022, there were 20 published protocols for systematic reviews, but no formal studies have been published thus far through systematic retrieval, which showed the contradiction between the need for high-quality clinical trials, synthetic evidence and the current researches. The conduct of clinical trials was limited by the high demand for clinical experts during the epidemic. They didn't have enough time and energy to conduct large clinical trials due to the urgent need for treating patients and controlling the epidemic. Obviously, the lack of original studies made some systematic reviews and meta-analyses hard to conduct, which led to the withdrawal of some protocols.89, 90 In addition, one key point that we cannot ignore is the feasibility of acupuncture. During the COVID-19 epidemic, under the huge pressure of controlling the spread of SARS-COV-2 and preventing new infections, acupuncture was difficult to implement in the clinic because of its invasive nature. Therefore, more attention needs to be paid to balance the priority between the prevention and control of epidemics and the conduct of original clinical trials.
Recommendations of clinical practice guidelines are a key element in guiding clinical decision-making, and the development of recommendations requires to systematically search the available evidence.15,91 But in this review, we found that most of the recommendations on acupuncture and moxibustion of included guidelines and consensuses were based on the experts’ experience and opinions, and lacked details of operation process, which was hard to transform into the clinical practice and was difficult to convince international researchers and clinical practitioners of the effectiveness and safety of acupuncture and moxibustion in COVID-19 patients.
Almost all included systematic reviews and clinical trials showed the positive effects of acupuncture and moxibustion, but these studies rarely reported adverse events or side effects, and the interventions were often acupuncture combined with other treatment methods (such as routine western treatment and other Chinese medicine, etc.), so the results may exaggerate the effectiveness of acupuncture and moxibustion. Furthermore, there were more limitations of the included studies, for instance, the sample sizes of included clinical trials were limited and the majority of participants were Chinese, both of which could weaken the extrapolation of study conclusions. Thus, more high-quality, multicenter clinical trials with large sample sizes are still needed to validate the efficacy and safety of acupuncture and moxibustion in the treatment of COVID-19.
This scoping review summarized the main characteristics and results of current studies, and analyzed the protocols to describe more details about the future researches, which can provide reference for relevant researchers and clinicians to conduct more meaningful researches and practices. However, this study also has some limitations. Firstly, we don't include the comments and basic researches, which may provide some references for relevant researchers. Secondly, we don't assess the quality of included studies, which can influence the credibility of results. For example, some studies have obvious weakness in study design. Thirdly, we are not able to classify the specific purposes (such as symptomatic treatment and immunity boosting, etc.) of recommended acupoints because of the limited information provided by the recommendations. Finally, we excluded the studies published in languages other than Chinese and English, which may miss some important studies.
There are some suggestions for future research: (1) Develop and report the clinical practice guideline following the evidence-based methodologies and guidance tool,92, 93 and describe more details of recommendations, especially for the operation process of acupuncture and moxibustion; (2) Implement more high-quality, multicenter clinical trials with large sample sizes; (3) Explore the effect of acupuncture and moxibustion on prevention and rehabilitation of COVID-19 patients.
5. Conclusion
This study showed that acupuncture and moxibustion works well in the treatment of COVID-19 patients to a certain extent, but more high-quality of clinical trials are still needed to support the clinical use of acupuncture and moxibustion in COVID-19 patients.
Author contributions
Chen Y and Ni X designed the study, oversaw the study implementation and responsible for quality control. Ren M and Liu Y drafted the article, extracted, and analyzed the data. Ni X conceived the manuscript, interpreted the results from the perspective of Chinese medicine theory and practice, and revising the manuscript. Kuang Z, Zhang Y, and Li H, searched the literature, and assessed the studies from the perspective of acupuncture theory and practice. Xufei Luo interpreted the studies from the perspective of methodology. All authors critical reviewed the manuscript and approved the submission.
Conflict of interests
Y Chen is an editorial board member of the journal but his editorial board membership status had no bearing on the editorial process or decision. The authors declare no other conflict of interests.
Funding
This study was supported by the Guangdong Provincial Key Laboratory of Research on Emergency in Traditional Chinese Medicine (No. 2017B030314176), and the National Key Research & Development Program of China Research on the Development and Evaluation of International Standards of Traditional Chinese Medicine (No. 2019YFC1712003).
Ethical Statement
Not applicable.
Data availability
The dataset supporting the conclusions of this article is included within the article.
Acknowledgment
We would like to acknowledge the contribution of Mr. Jiahui Lin, Ms. Ping Zeng and Ms. Yidan Zhang in the preliminary search and categorization of acupuncture studies.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.imr.2022.100886.
Supplement 1: PRISMA-ScR checklist. Supplement 2: Search strategies of databases. Supplement 3: Checklist of included studies.
Contributor Information
Xiaojia Ni, Email: grace1984325@126.com.
Yaolong Chen, Email: chenyaolong@lzu.edu.cn.
Appendix. Supplementary materials
References
- 1.National Health Commission, National Administration of Traditional Chinese Medicine The diagnosis and treatment plan of novel coronavirus pneumonia (Trial version 8) (in Chinese) Chin J Viral Dis. 2020;10(05):321–328. [Google Scholar]
- 2.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jin Y, Cai L, Cheng Z, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) (in Chinese) Mil Med Res. 2020;7:4. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu YF, Zhuang WY, Mao M, et al. Discussion on the application of acupuncture and moxibustion therapy in the prevention and treatment of ancient epidemic disease (in Chinese) China J Tradit Chin Med Pharm. 2021;36(05):2464–2467. [Google Scholar]
- 5.Liu B, Wang H, Zhou ZY, et al. Analysis on the theory and clinical ideas of acupuncture and moxibustion for the prevention and treatment of coronavirus disease 2019 (in Chinese) Chin Acupunct Moxibust. 2020;40(06):571–575. doi: 10.13703/j.0255-2930.20200305-k0004. [DOI] [PubMed] [Google Scholar]
- 6.Sun PL. The use of acupuncture in the treatment of COVID-19 (in Chinese) Guid J Tradit Chin Med Pharm. 2020;26(10):12–17. +41. [Google Scholar]
- 7.Zhang J, Wu YC. Modern progress of mechanism of moxibustion therapy (in Chinese) J Acupunct Tuina Sci. 2006;4(05):257–260. [Google Scholar]
- 8.Wang RQ, Liu JX, Zhang ZD, et al. Feasibility analysis on acupuncture therapy for the treatment of corona virus disease 2019 and the exploration on the application scheme (in Chinese) Acupunct Res. 2020;45(05):345–350. doi: 10.13702/j.1000-0607.200275. [DOI] [PubMed] [Google Scholar]
- 9.Gong YB, Shi XJ, Yan Zhang, et al. The clinical use and practice of acupuncture therapy in COVID-19 (in Chinese) Chin Acupunct Moxibust. 2021;41(02):142–144. [Google Scholar]
- 10.Li YM. Obstacles and opportunities for traditional Chinese medicine's participation in anti-epidemic in the United States (in Chinese) World Chin Med. 2020;15(10):1509–1512. [Google Scholar]
- 11.Chen WT, Fu HL, Zhang CY, et al. Feasibility analysis of acupuncture and moxibustion in the prevention and treatment of COVID-19 from an international perspective (in Chinese) J Clin Acupunct Moxibust. 2020;36(09):82–87. [Google Scholar]
- 12.Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–2126. doi: 10.11124/JBIES-20-00167. [DOI] [PubMed] [Google Scholar]
- 13.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 14.Field MJ, Lohr KN, editors. Clinical Practice Guidelines: Directions for a New Program. National Academies Press (US); Washington (DC): 1990. Institute of medicine (US) committee to advise the public health service on clinical practice guidelines. eds. [PubMed] [Google Scholar]
- 15.Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Graham R, Mancher M, Miller Wolman D, et al. National Academies Press (US); Washington (DC): 2011. Clinical Practice Guidelines We Can Trust. [PubMed] [Google Scholar]
- 16.China Association of Acupuncture-moxibustion Guidance on acupuncture intervention for COVID-19 (First Edition) (in Chinese) Chin Acupunct Moxibust. 2020;40(02):111. [Google Scholar]
- 17.Shi XM, Tong XL, Sun GJ, et al. Guidance on acupuncture intervention for COVID-19 (Second Edition) (in Chinese) Acupunct Moxibust. 2020;40(05):462–463. [Google Scholar]
- 18.Mahin B, Majid D, Zohreh S, et al. Complementary and alternative medicine therapies and COVID-19: a systematic review. Rev Environ Health. 2021;36(02):443–450. doi: 10.1515/reveh-2021-0012. [DOI] [PubMed] [Google Scholar]
- 19.Chen C, Zhan J, Wen H, et al. Current state of research about acupuncture for the treatment of COVID-19: a scoping review. Integ Med Res. 2021;10(Suppl) doi: 10.1016/j.imr.2021.100801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dong ZB, Guo JY, Deng TT, et al. Acupuncture for nasal congestion in COVID-19: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2022;101(2):e28600. doi: 10.1097/MD.0000000000028600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li XH, Dong TT, Hou Y, et al. Moxibustion for abdominal pain in COVID-19: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2022;101(3):e28596. doi: 10.1097/MD.0000000000028596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu NN, Xu YX, Zhang DB, et al. Moxibustion for diarrhea in COVID-19: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2022;101(6):e28777. doi: 10.1097/MD.0000000000028777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Luo WJ, Zhai Y, Sun M, et al. Clinical study on acupuncture treatment of COVID-19: a protocol for a systematic review and meta-analysis. Medicine (Baltimore) 2022;101(2):e28296. doi: 10.1097/MD.0000000000028296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang XX, Hou Y, Ding L, et al. Moxibustion for anorexia in COVID-19: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2022;101(8):e28894. doi: 10.1097/MD.0000000000028894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luo WJ, Zhai Y, Sun M, et al. Clinical study on acupuncture treatment of COVID-19: a protocol for a systematic review and meta-analysis. Medicine (Baltimore) 2022;101(2):e28296. doi: 10.1097/MD.0000000000028296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xia QC, Gao HW, Xian J, et al. Efficacy and safety of acupuncture for elderly patients with coronavirus disease 2019 (COVID-19): a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2021;100(5):e24515. doi: 10.1097/MD.0000000000024515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou Y, Yan X, Ma FJ, et al. Effects of moxibustion for COVID-19 convalescence: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2021;100(14):e25389. doi: 10.1097/MD.0000000000025389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jia HW, Han ZZ, Zhang K, et al. Acupuncture and related interventions for anxiety in coronavirus disease 2019: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2020;99(30):e21317. doi: 10.1097/MD.0000000000021317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen Y, Zhu CC, Xu ZM, et al. Acupuncture for corona virus disease 2019: a protocol for systematic review and meta analysis. Medicine (Baltimore) 2020;99(40):e22231. doi: 10.1097/MD.0000000000022231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chi WX, Chen Y, Wang LN, et al. Acupuncture for COVID-19 patient after ventilator weaning: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2020;99(50):e23602. doi: 10.1097/MD.0000000000023602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gao W, Li JF, Huang GX. Plum-blossom needle for coronavirus disease 2019-related headache: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2020;99(37):e22179. doi: 10.1097/MD.0000000000022179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang KY, Chang CH, Hsu CH. The efficacy of acupuncture for improving the side effects of COVID-19 western medicine treatments: a protocol for a systematic review and meta-analysis. Medicine (Baltimore) 2020;99(28):e21185. doi: 10.1097/MD.0000000000021185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu M, Zhu HQ, Xiong Q, et al. The efficacy and safety of fire needle therapy for COVID-19: protocol for a systematic review and meta-analysis. Medicine (Baltimore) 2020;99(34):e21873. doi: 10.1097/MD.0000000000021873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang ZL, Zhang J, Du DQ, et al. Adjuvant therapeutic effects of moxibustion on COVID-19: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2020;99(46):e23198. doi: 10.1097/MD.0000000000023198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wen DP, Wu L, Dong YT, et al. The effect of acupuncture on the quality of life of patients recovering from COVID-19: a systematic review protocol. Medicine (Baltimore) 2020;99(30):e20780. doi: 10.1097/MD.0000000000020780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li XH, Dong TT, Hou Y, et al. Moxibustion for abdominal pain in COVID-19: A protocol for systematic review and meta-analysis. Medicine (Baltimore) 2022;101(3):e28596. doi: 10.1097/MD.0000000000028596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang BZ, Zhang K, Tang QL, et al. Acupuncture for breathlessness in COVID-19: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2020;99(27):e20701. doi: 10.1097/MD.0000000000020701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang QS, Xu XH, Sun SQ, et al. Efficacy of acupuncture and moxibustion in adjuvant treatment of patients with novel coronavirus disease 2019 (COVID-19): A protocol for systematic review and meta analysis. Medicine (Baltimore) 2020;99(28):e21039. doi: 10.1097/MD.0000000000021039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Y, Ren T, Li HY, et al. Effectiveness and safety of acupuncture for anxiety disorder of coronavirus disease 2019: a protocol of systematic review and meta-analysis. Medicine (Baltimore) 2020;99(38):e22177. doi: 10.1097/MD.0000000000022177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhao HY, Fu LY, Xie CC, et al. Observation on the effect of moxibustion intervention on patients discharged from hospital with COVID-19 based on the internet model (in Chinese) Jiangxi J Tradit Chin Med. 2022;53(02):46–49. [Google Scholar]
- 41.Zhu JT, Hu YX, He XZ, et al. Significance of tinfoil salt cake moxibustion in the rehabilitation period of COVID-19 (in Chinese) China's Naturop. 2022;30(05):41–44. [Google Scholar]
- 42.Li C. Clinical efficacy of thunder fire moxibustion combined with Qingfeipaidu decoction in the treatment of clinical symptoms in line with new type coronavirus pneumonia in children with cold-dampness-closed lung syndrome (in Chinese) Chin J Clin Ration Drug Use. 2022;15(04):32–35. [Google Scholar]
- 43.Luo ZX, Wang KX, Zhang YL, et al. Thumb-tack needles based on "Biaoben acupoint compatibility" for sequela COVID-19 of during recovery period (in Chinese) Chin Acupunct Moxibust. 2022;42(03):281–286. doi: 10.13703/j.0255-2930.20210406-0004. [DOI] [PubMed] [Google Scholar]
- 44.Zeng L, Liu ML, Tang SH, et al. Moxibustion on mental disorder and in close contacts of coronavirus disease 2019: a randomized controlled trail (in Chinese) Chin Acupunct Moxibust. 2021;41(10):1109–1112. doi: 10.13703/j.0255-2930.20210317-k0003. [DOI] [PubMed] [Google Scholar]
- 45.Liu L, Xing XY, He DC, et al. Effect of moxibustion on clinical symptoms, peripheral inflammatory indexes and T lymphocyte subsets in COVID-19 patients (in Chinese) Chin Acupunct Moxibust. 2020;40(12):1271–1275. doi: 10.13703/j.0255-2930.20200507-k0003. [DOI] [PubMed] [Google Scholar]
- 46.Dou MX, Xie ZJ, Yang ZY, et al. Effect evaluation of combined moxibustion with Fire Dragon pot on relieving cough and shortness of breath in COVID-19 patients (in Chinese) Med Diet Health. 2021;19(01):27–28. [Google Scholar]
- 47.Tao D, Su WY, Luo LL, et al. Clinical efficacy of moxibustion in the treatment of patients with lung spleen Qi deficiency syndrome during the recovery period of COVID-19 (in Chinese) Contemp Med. 2021;27(24):19–21. [Google Scholar]
- 48.Dong SJ, Wang XN, Gao L, et al. Observation on curative effect of 36 cases of COVID-19 patients with diarrhea in Fangcang hospital treated by moxibustion based on syndrome differentiation (in Chinese) Chin Acupunct Moxibust. 2020;40(07):690–692. [Google Scholar]
- 49.Luo ZH, Wang KX, Zhang YL, et al. Clinical observation on the “Biao-Ben Acupoint Compatibility” filiform-fire needle therapy of 33 case of sequelae of new coronavirus pneumonia during the recovery period (in Chinese) Chin Acupunct Moxibust. 2022;42(07):760–764. doi: 10.13703/j.0255-2930.20210817-0002. [DOI] [PubMed] [Google Scholar]
- 50.Yin X, Cai SB, Chen LM, et al. Seventeen cases with coronavirus pneumonia 2019 (COVID-19) treated with the combination of acupuncture and medicine (in Chinese) Chin Acupunct Moxibust. 2021;41(05):498–500. [Google Scholar]
- 51.Ma CC, Li YM, Wu JH. Observation the clinical curative effect of before and after application of modified Wuye Lugen Decoction combined with moxibustion in patients with COVID-19 in recovery period (in Chinese) Asia-Pacific Tradit Med. 2021;17(12):113–117. [Google Scholar]
- 52.Zhou HW, Chen XS, Du SS, et al. Clinical observation of 41 recurrence COVID-19 patients treated with Chinese medicine combined with moxibustion (in Chinese) Modern Chin Med. 2021;41(03):55–59. [Google Scholar]
- 53.Li WL, Li QF, Liu HJ, et al. Triple acupuncture therapy of 8 cases of psychological stress disorder during the outbreak of COVID-19 (in Chinese) Tradit Chin Med Res. 2021;34(03):19–20. [Google Scholar]
- 54.Zhang XZ, Li L, Wang MJ, et al. Clinical effect of moxibustion as the adjuvant therapy for novel coronavirus pneumonia: an analysis of 7 cases (in Chinese) J Anhui Univ Chin Med. 2020;39(04):4–7. [Google Scholar]
- 55.Wang JM, Zhang XZ, Yang J. Moxibustion as an adjunctive therapy of 7 coronavirus disease (in Chinese) Chin Acupunct Moxibust. 2020;40(10):1035–1036. [Google Scholar]
- 56.Chen X, Huang W, Liu BY, et al. Moxibustion therapy in prevention and treatment of coronavirus disease 2019 (COVID-19): construction and application of non-contact diagnosis and treatment mode (in Chinese) Chin Acupunct Moxibust. 2020;40(10):1027–1033. doi: 10.13703/j.0255-2930.20200428-k0006. [DOI] [PubMed] [Google Scholar]
- 57.Huang XB, Xie DY, Qiu Q, et al. Clinical observation of heat-sensitive moxibustion treatment for coronavirus disease 2019 (in Chinese) Chin Acupunct Moxibust. 2020;40(06):576–580. doi: 10.13703/j.0255-2930.20200312-k0003. [DOI] [PubMed] [Google Scholar]
- 58.Wang H, Dai C, Xiao L, et al. Clinical efficacy and safety of the acupuncture combined with western medicine in treatment 3 cases of severe COVID-19 (in Chinese) Chin J Nosocomiol. 2021;31(24):3699–3702. [Google Scholar]
- 59.Yin X, Cai SB, Tao LT, et al. Recovery of a patient with severe COVID-19 by acupuncture and Chinese herbal medicine adjuvant to standard care. J Integ Med. 2021;19(5):460–466. doi: 10.1016/j.joim.2021.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cheng SI. Medical acupuncture as a treatment for novel COVID-19-related respiratory distress: personal experience from a frontline anesthesiologist. Med Acupunct. 2021;33(1):83–85. doi: 10.1089/acu.2020.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yeh BY, Chen YL, Chang SA, et al. Acupuncture helps to regain the consciousness of a COVID-19 patient complicated with hypoxic-ischemic encephalopathy: a case report. Neurol Sci. 2021;42(2):475–478. doi: 10.1007/s10072-020-04980-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu LH, Zhao JB, Lei M. A case of combined acupuncture and medicine in the treatment of COVID-19 (in Chinese) Chin Acupunct Moxibust. 2020;40(08):803–804. [Google Scholar]
- 63.Gong YB, Yang ZL, Liu Y, et al. Two cases of corona virus disease 2019 (COVID-19) treated with the combination of acupuncture and medication in bedridden patients 2. World J Acupunct Moxibust. 2020;30(3):171–174. doi: 10.1016/j.wjam.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tao LT, Huang TL, Zheng DW, et al. Case of professor Xu ZOU's acupuncture technique for "benefiting kidney and strengthening anti-pathogenic qi" in promoting the absorption of COVID-19. World J Acupunct Moxibust. 2020;30(3):167–170. doi: 10.1016/j.wjam.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dai YF, Yue YN, Li JA, et al. Mechanism of moxibustion in preventing and treating novel coronavirus disease 2019 (in Chinese) Chin J Ethnomed Ethnopharm. 2020;29(08):88–89. +99. [Google Scholar]
- 66.Li XS, Lu H, Hu HQ, et al. Possible mechanism of acupuncture and moxibustion in prevention and treatment of COVID-19 (in Chinese) J Fourt Mil Med Univ. 2020;11(04):9–12. [Google Scholar]
- 67.Lai ML, Yu TH, Huang Y. Theoretical discussion on moxibustion therapy for the prevention and treatment of COVID-19 (in Chinese) J Med Theory Prac. 2020;33(15):2417–2419. +2440. [Google Scholar]
- 68.Zhang YP, Qiao L, Fan CB, et al. Theoretical discussion on the application of moxibustion in the prophylaxis and treatment in corona virus disease 2019 (in Chinese) J Liaoning Univ Tradition Chin Med. 2020;22(04):174–177. [Google Scholar]
- 69.He W, Shi XS, Zhang ZY, et al. Discussion on the effect pathways of preventing and treating coronavirus disease 2019 by acupuncture and moxibustion from the regulation of immune inflammatory response (in Chinese) Chin Acupunct Moxibust. 2020;40(08):799–802. doi: 10.13703/j.0255-2930.20200305-0001. +809. [DOI] [PubMed] [Google Scholar]
- 70.Chen B, Jin GY, Chen ZL, et al. Discussion on the scientific basis of acupuncture in the prevention and treatment of novel coronavirus pneumonia complicated with sepsis (in Chinese) World Chin Med. 2020;15(02):140–143. +149. [Google Scholar]
- 71.Zhong GJ, Mao WJ, Lin JY, et al. Feasibility analysis of Abdominal acupuncture combined with thymosin in the prevention and treatment of COVID-19 (in Chinese) Res Integ Tradit Chin West Med. 2021;13(02):128–130. [Google Scholar]
- 72.Xu J, Pan LJ, Jia CS. Exploration on the feasibility of moxibustion in prevention and treatment of COVID-19 from the perspective of modern medical mechanism. World J Acupunct Moxibust. 2020;30(2):81–84. doi: 10.1016/j.wjam.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.He YJ, Song BQ, Yang LY, et al. Discussion on scientific basis of acupuncture prevention and treatment of novel coronavirus pneumonia from “Inflammatory Storm” theory (in Chinese) Mod Tradit Chin Med Mater Med-World Sci Technol. 2020;22(03):706–709. [Google Scholar]
- 74.Wu Z, Zeng M. Acupuncture treatment the feasibility of new coronavirus pneumonia (COVID-19) during rehabilitation. Altern Integ Med. 2020;9(2):289. [Google Scholar]
- 75.Lv PW, Wang SN, Tang ZX, et al. Feasibility analysis of early intervention of moxibustion in the prevention and treatment of COVID-19 (in Chinese) Acta Chin Med. 2020;35(03):473–476. [Google Scholar]
- 76.Liu KP, Guan DD, Li L, et al. Feasibility analysis of moxibustion whole process intervention in the prevention and treatment of COVID-19 (in Chinese) Acta Chi Med. 2020;35(06):1144–1147. [Google Scholar]
- 77.Yemeng C. The role of acupuncture during the COVID-19 pandemic: from the historical perspective to practical application. Tradit Med Modern Med. 2020;3(01):27–35. [Google Scholar]
- 78.Ye L, Sun P, Wang T. Acupuncture strategies to tackle post covid-19 psychological and neuropsychiatric disorders. J Chin Med. 2020;2020(124):11–21. [Google Scholar]
- 79.Vique-Sánchez JL, Galíndez-Fuentes AI. Acupuncture as a complementary medicine for depression caused by the confinement by COVID-19. Rev Int Acupunt. 2021;15(3) [Google Scholar]
- 80.Guan DD, Chen L, Liu KP, et al. Progress in the prevention and control of corona virus disease 2019 by moxibustion (in Chinese) J Liaoning Univ Tradit Chin Med. 2021;23(03):168–171. [Google Scholar]
- 81.Yang YL, Li Y, Liu XQ. Ancient literature and modern research on moxibustion prevention and treatment of epidemic diseases (in Chinese) Tradit Chin Med J. 2021;20(06):39–42. [Google Scholar]
- 82.Xu J, Jia CS. Discussion on prevention and treatment of infectious diseases by using moxibustion for warming yang and strengthening body resistance to eliminate pathogenic cold and qi in ancient and modern literature (in Chinese) Acup Res. 2021;46(08):717–720. doi: 10.13702/j.1000-0607.201079. [DOI] [PubMed] [Google Scholar]
- 83.Teng JY, Zhou ZY, Yao M, et al. Clinical application and research progress of moxibustion in pulmonary diseases (in Chinese) J Clin Acupunct Moxibust. 2021;37(10):88–92. [Google Scholar]
- 84.Long JYX, Zhu Y, Liao ZL, et al. Advances in research on prevention and treatment of COVID-19 with acupuncture and moxibustion (in Chinese) World Latest Med Inf. 2020;20(85):57–58. 62. [Google Scholar]
- 85.Wu S, Mao HR. Preliminary discussion on the ideas and acupoints selection of acupuncture for the prevention and treatment of COVID-19 (in Chinese) Asia-Pacific Tradit Med. 2021;17(02):156–158. [Google Scholar]
- 86.Zhang JL, Yang L, Xian TC, et al. Thoughts and methods of moxibustion for prevention and control of COVID-19 (in Chinese) J Fourt Mil Med Univ. 2020;11(02):10–14. [Google Scholar]
- 87.Analysis of acupoint selection in treating stage of COVID-19patients during recovery stage (in Chinese) Mod Tradit Chin Med Mater Med-World Sci Technol. 2020;22(10):3493–3498. [Google Scholar]
- 88.Yue YN, Dai YF, Yang J, et al. Exploration of acupoints selection in acupuncture intervention for COVID-19 (in Chinese) China's Naturop. 2020;28(15):5–7. [Google Scholar]
- 89.Wang X, Hou Y, Ding L, et al. Moxibustion for anorexia in COVID-19: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 2022;101(8):e28894. doi: 10.1097/MD.0000000000028894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Efficacy and safety of acupuncture therapy for asymptomatic infection of COVID-19: a protocol for systematic review and meta-analysis: retraction. Medicine (Baltimore) 2021;100(11):e25227. doi: 10.1097/MD.0000000000025227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Akl EA, Welch V, Pottie K, et al. GRADE equity guidelines 2: considering health equity in GRADE guideline development: equity extension of the guideline development checklist. J Clin Epidemiol. 2017;90:68–75. doi: 10.1016/j.jclinepi.2017.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen YL, Yang KH, Liu XQ, et al. Guidelines for the development/revision of clinical diagnosis and treatment guidelines in China (2022 edition) (in Chinese) Chin Med J. 2022;102(10):697–703. [Google Scholar]
- 93.Tang C, Duan Y, Zhang Y, et al. RIGHT (Reporting Items for Practice Guidelines in Healthcare) for acupuncture working group. RIGHT for acupuncture: an extension of the RIGHT statement for clinical practice guidelines on acupuncture. J Clin Epidemiol. 2021;139:330–339. doi: 10.1016/j.jclinepi.2021.05.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset supporting the conclusions of this article is included within the article.