BACKGROUND
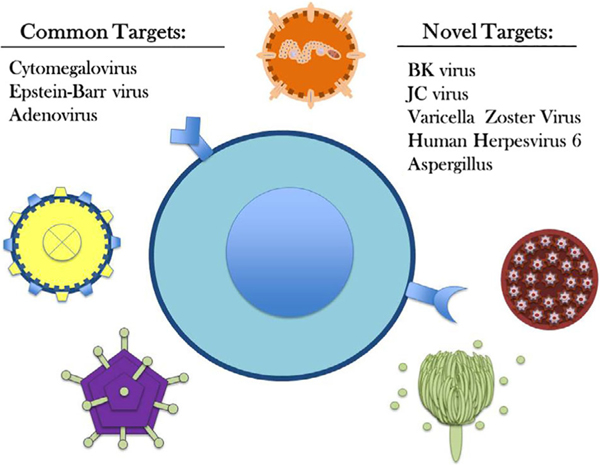
Viral infections pose serious health risks in immunocompromised patients after hematopoietic stem cell transplantation (HSCT) and account for roughly 40% of transplant-related mortality. Some of the most common post-HSCT viral infections include Epstein–Barr virus (EBV), cytomegalovirus (CMV), and adenovirus.1 Available pharmacologic agents are not always effective and can be limited by toxicities, including myelosuppression and nephrotoxicity.2,3 Viral infections such as progressive multifocal leukoencephalopathy (PML) have no effective treatment beyond restoration of cellular immune function, which may not be possible for all patients, and further demonstrates the need for alternative treatment modalities.4 Virus-specific T cells (VSTs) have been used in many prior Phase 1 and 2 clinical trials as a treatment for refractory viral infections. Most studies focused on treating and preventing CMV, EBV, and adenovirus, but recent clinical studies have evaluated the feasibility of targeting additional infectious diseases such as BK virus (BKV), JC virus, varicella zoster virus (VZV), human herpesvirus 6, and aspergillosis. Use of multivirus-specific T cells, which target multiple viral antigens during ex vivo expansion, has allowed simultaneous targeting of up to five viruses in a single product. Although autologous virus-specific T cells have been used in patients with EBV-associated malignancies, most studies have used allogeneic T cells derived from hematopoietic stem cell donors or third-party donors as an off-the-shelf product. Here, we review infectious diseases beyond CMV, EBV, and adenovirus that have been targeted by T-cell therapy in clinical trials in addition to diseases for which T-cell therapies are on the horizon but are still in preclinical development (Fig. 1).
Fig. 1.
Virus-specific T cells and the commonly targeted viruses: CMV, EBV, AdV versus novel targets: BKV, JCV, VZV, HHV6, Aspergillus.
Moving beyond CMV, EBV, and adenovirus in the clinic
BKV and JC virus
BKV and JC virus are polyomaviruses that share sequence homology in immunogenic proteins, making them an ideal dual-purpose target.4 BKV causes nephritis and cystitis in patients following HSCT, while JC virus is a well-described cause of PML.4 Baylor College of Medicine first reported the use of third-party BKV-specific T cells and reported no adverse events associated with T-cell infusion. All 16 patients treated for BKV-associated hemorrhagic cystitis achieved clinical benefit, 13 of which demonstrated complete resolution of gross hematuria.2
Muftuoglu et al.4 also reported patients with JC-associated PML treated with third-party VSTs. Three patients received one to four infusions, which resulted in clinical improvement and/or complete clearance of JC virus in the cerebrospinal fluid with detectable VST in the cerebrospinal fluid at Day 250.
Varicella zoster virus
VZV reactivation is common in patients following HSCT and can lead to disseminated varicella infections. Despite prophylactic treatment, immunosuppressed patients have a 6% to 8% risk for varicella reactivation. Ma et al.5 utilized VZV-specific T cells for the prophylactic treatment of HSCT recipients. Eight of the 10 patients demonstrated immune reconstitution against VZV within 100 days after infusion, and there was no evidence of VZV reactivation in any patients after infusion. Of the 10 patient infusions, there was no acute infusion-related toxicity; however, three patients developed Grade II-IV graft-versus-host disease (GvHD).5
Human Herpesvirus 6
Human herpesvirus 6 (HHV-6) primary infection occurs in over 90% of individuals before the age of 2 years, and reactivation occurs in 40% to 60% of HSCT recipients. HHV-6 reactivation is a cause of viral encephalitis in patients following HSCT, and has also been tied to risk of GvHD.6 Papadopoulou et al.3 evaluated the use of donor-derived pentaviral VSTs including HHV-6 through inclusion of HHV-6 antigens: immediate early (U90), early (U14), and late (U11). Of the 11 patients treated, two patients had multiple active infections that included HHV-6, and both were able to achieve complete clearance of HHV-6. None of the patients in this study developed immediate adverse events, and only one patient developed Grade II de novo GvHD 4 weeks after infusion.
A similar study examined the use of VSTs against HHV-6 in addition to BKV, CMV, EBV, and adenovirus using a third-party bank of pentavalent VSTs. Of 31 patients treated, three were treated specifically for HHV-6, two were rated as partial responses, and one was not evaluable. One patient developed recurrent Grade III GvHD, and five patients experienced recurrent or de novo grade I-II skin GvHD.2
Aspergillus
Aspergillosis is a potentially deadly fungal infection in immunocompromised patients. Due to proliferation of antigen-specific, interferon-γ–producing T cells in patients who survive Aspergillus infections, Aspergillus-specific T cells were hypothesized to have potential therapeutic value for this infection. Perruchio et al.7 treated 10 patients with Aspergillus-specific T cells and 27 with CMV-specific T cells. Nine of the 10 patients who received Aspergillus-specific T cells cleared invasive aspergillosis in approximately 8 weeks, and one patient died of progressive Aspergillus pneumonia at 2 weeks after therapy. All treated patients received 1 × 106 cells/kg, and none developed acute or chronic GvHD.
PRECLINICAL TARGETS IN DEVELOPMENT
Human Parainfluenza Virus 3
Human parainfluenza virus-3 (HPIV-3) is a common cause of viral pneumonia in immunocompromised patients. In preclinical studies, it has been demonstrated that expansion of HPIV-3–specific VSTs is possible, with the HPIV-3 matrix protein showing immunodominance.8 HPIV-3–specific VSTs were polyfunctional having both interferon-γ (IFN-γ) and tumor necrosis factor-α (TNF-α) production with relatively low interleukin-10 production. Intracellular cytokine staining suggested that responses to HPIV-3–specific responses were predominantly mediated by CD4+ T cells, with no significant cytokine release noted from the CD8+ population.8
Herpes simplex virus Type 1
Herpes simplex virus Type 1 (HSV-1) can cause cutaneous lesions or disseminated disease in immunocompromised patients. Drug-resistant strains of HSV-1 are most concerning in immune-deficient patients and reactivation may lead to systemic involvement, resulting in esophagitis, pneumonia, hepatitis, meningitis, encephalitis, and bone marrow suppression. Ma et al.9 assessed the feasibility of using HSV-1 immunodominant epitopes to generate HSV-1 VSTs. Human leukocyte antigen (HLA)-A1/A2 HSV-1 CD8 epitopes were isolated from HLA-A A1/A2-positive HSV-seropositive donors. The HSV-1–specific T cells were heavily dependent on secretion of IFN-γ and cytolytic function for complete clearance of local infection. More than 94% of HSV-1 VSTs evaluated secreted IFN-γ and TNF-α.
Zika virus
Complications of Zika infections cause both neurological and pregnancy-related ailments such as paralysis, miscarriages, and birth defects. With no specific therapeutics or preventatives, all treatments currently rely on symptom alleviation. To investigate T cells as a specific therapeutic, Hanajiri et al.10 reported that both seropositive and seronegative donors were able to generate Zika virus–specific T cells. The Zika VSTs were analyzed and found to have a fourfold increase in IFN-γ production compared to baseline. T cells stimulated with Zika peptides had notable up regulation of mRNA and protein expression levels relevant to cytotoxicity, chemotaxis, and inflammation. These were similar markers present in Barranquilla (Colombia) cohort samples collected 1 to 2 years after Zika virus infection.11
Mycobacteria
Mycobacterial infections are common in immunocompromised patients with T-cell deficiency. Patel et al.12 recently described feasibility of expanding mycobacterial-specific T cells from healthy donors. Immunodominant mycobacterial antigens were recognized by donors regardless of prior vaccination with bacillus Calmette-Guerin. Expanded T cells were predominantly CD4+ and T helper 1 skewed based on production of IFN-γ, TNF-α, and granulocyte macrophage colony-stimulating factor. Though not clinically used to date, mycobacteria-specific T cells may be a useful adjunctive treatment for mycobacterial infections in T-cell–deficient patients.
LIMITATIONS
Despite many promising early-phase clinical studies, many obstacles remain for expanding the clinical use of VSTs. With a few exceptions,13,14 generating VSTs requires donor immunity to the target(s) of interest.4 There is also significant cost, time, and regulatory burden for VST manufacturing.2 The use of third-party product banks may overcome many of these limitations, although there are currently no established algorithms for HLA matching of VST products and recipients, and existing selection methods rely entirely on expert experience.1
FUTURE DIRECTIONS
In recent VST clinical trial publications, it has been stressed that larger, controlled studies are needed to determine success rate, durability, and the longer-term adverse events associated with VST therapy.1,4 Comparative studies of manufacturing processes of VST generation will also aid in production standardization to develop accessible third-party VST banks. Moving forward, improved availability and broader pathogen targeting will enhance the applicability of adoptive T-cell therapy.
KEY IDEAS.
Virus-specific T cells allow targeting of multiple pathogens in patients after hematopoietic stem cell transplantation and have demonstrated potential efficacy for cytomegalovirus, Epstein–Barr Virus, and adenovirus.
Novel targets may include BK virus, JC virus, varicella zoster virus, human herpesvirus 6, Aspergillus, human parainfluenza virus-3, herpes simplex virus Type I, Zika virus, and mycobacteria.
Generation of patient-specific products and third-party products may expand feasibility of therapy.
Acknowledgments
This work was supported by the Children’s Cancer Foundation (CCF), the Amy Manasevit Award from Be the Match/American Society for Transplantation and Cellular Therapy (ASTCT) to PJH; the National Institutes of Health (K23-HL136783–01 to MK), and the Jeffrey Modell Foundation.
ABBREVIATIONS:
- BKV
BK virus
- CMV
cytomegalovirus
- EBV
Epstein–Barr virus
- GvHD
graft-versus-host disease
- HHV-6
human herpesvirus 6
- HLA
human leukocyte antigen
- HPIV-3
human parainfluenza virus-3
- HSCT
hematopoietic stem cell transplantation
- HSV-1
Herpes simplex virus Type 1
- IFN-γ
interferon-γ
- PML
progressive multifocal leukoencephalopathy
- TNF-α
tumor necrosis factor-α
- VSTs
virus-specific T cells
- VZV
varicella zoster virus
Footnotes
CONFLICT OF INTERESTS
AF and NZ have disclosed no conflicts of interest. PJH and MDK have intellectual property related to the expansion of pathogen-specific T cells, and PJH is a cofounder and serves on the board of directors of Mana Therapeutics.
REFERENCES
- 1.Harris KM, Davila BJ, Bollard CM, et al. Virus-specific T cells: current and future use in primary immunodeficiency disorders. Allergy Clin Immunol Pract 2019;7:809–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tzannou I, Papadopoulou A, Naik S, et al. Off-the-shelf virus-specific T cells to treat BK virus, human herpesvirus 6, cytomegalovirus, Epstein-Barr Virus, and adenovirus infections after allogeneic hematopoietic stem-cell transplantation. J Clin Oncol 2017;35:3547–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Papadopoulou A, Gerdemann U, Katari UL, et al. Activity of broad-spectrum T cells as treatment for AdV, EBV, CMV, BKV, and HHV6 infections after HSCT. Sci Transl Med 2014;6: 242ra83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muftuoglu M, Olson A, Marin D, et al. Allogeneic BK virus-specific T cells for progressive multifocal leukoencephalopathy. N Engl J Med 2018;379:1443–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ma CK, Blyth E, Clancy L, et al. Addition of varicella zoster virus–specific T cells to cytomegalovirus, Epstein-Barr virus and adenovirus tri-specific T cells as adoptive immunotherapy in patients undergoing allogeneic hematopoietic stem cell transplantation. Cytotherapy 2015;17:1406–20. [DOI] [PubMed] [Google Scholar]
- 6.Hill JA, Mayer BT, Xie H, et al. The cumulative burden of double-stranded DNA virus detection after allogeneic HCT is associated with increased mortality. Blood 2017;129:2316–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perruccio K, Tosti A, Burchielli E, et al. Transferring functional immune responses to pathogens after haploidentical hematopoietic transplantation. Blood 2005;106:4397–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McLaughlin LP, Lang H, Williams E, et al. Human parainfluenza virus-3 can be targeted by rapidly ex vivo expanded T lymphocytes. Cytotherapy 2016;18:1515–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma CK, Clancy L, Deo S, et al. Herpes simplex virus type 1 (HSV-1) specific T-cell generation from HLA-A1- and HLA-A2-positive donors for adoptive immunotherapy. Cytotherapy 2017;19:107–18. [DOI] [PubMed] [Google Scholar]
- 10.Hanajiri R, Sani GM, Hanley PJ, et al. Generation of Zika virus-specific T cells from seropositive and virus-naive donors for potential use as an autologous or “off-the-shelf” immunotherapeutic. Cytotherapy 2019;19:30794–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grifoni A, Costa-Ramos P, Pham J, et al. Cutting edge: transcriptional profiling reveals multifunctional and cytotoxic antiviral responses of Zika virus–specific CD8(+) T cells. J Immunol 2018;201:3487–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel S, Lang H, Sani G, et al. Mycobacteria-specific T cells may be expanded from healthy donors and are near absent in primary immunodeficiency disorders. Front Immunol 2019; 10:621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanley PJ, Cruz CRY, Savoldo B, et al. Functionally active virus-specific T cells that target CMV, adenovirus, and EBV can be expanded from naive T-cell populations in cord blood and will target a range of viral epitopes. Blood 2009;114:1958–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hanley PJ, Melenhorst JJ, Nikiforow S, et al. CMV-specific T cells generated from naive T cells recognize atypical epitopes and may be protective in vivo. Sci Transl Med 2015;7: 285ra63. [DOI] [PMC free article] [PubMed] [Google Scholar]