Abstract
While the majority of the initial attention to symptomatic COVID-19 focused on adult patients as well as adult critical care and first responders, the pandemic drastically altered care throughout the entire health care industry. COVID-19 has had a profound effect on the treatment and care of pediatric patients within pediatric otolaryngology. The objective of this article is to highlight the unique ramifications of COVID-19 in general and its effect within pediatric otolaryngology, with a focus on the immediate and potential long-term shifts in practice. This article addresses several aspects of care within pediatric otolaryngology including safety, diagnosis, and treatment of COVID-19 detailing the unique effects of the pandemic on the pediatric otolaryngology specialty and opportunities.
Keywords: COVID-19, Pediatric otolaryngology, Pediatric ear, Nose and throat
Key points
-
•
Managing children has several unique features, which potentially increase COVID-19 exposure risk to the provider, including a high frequency of upper respiratory tract infections, asymptomatic carries, and poor patient compliance with a routine examination.
-
•
By its very nature, otolaryngologists have a unique set of conditions that make providers particularly vulnerable to upper respiratory pathogens, including close physical proximity of the examination to the pharynx and the practice of aerosol-generating procedures.
-
•
There are many features of COVID-19 infection that manifest in the pediatric population postinfection including anosmia/hyposmia, dysgeusia, MIS-C, and long COVID-19.
-
•
Many system-based initiatives instituted in hospitals across the country have helped to mitigate risks and improve the patient experience.
-
•
With the advent of new technologies for remote examination and integrated electronic medical records, this hybrid model will provide a high level of satisfaction for patients and families who can get access to their health care provider more easily from multiple avenues in a convenient set.
Introduction
While the majority of attention to the health care impact of COVID-19 has focused on adult first responders and critical care providers, the pandemic has had a profound effect on the entire health care industry, including the pediatric otolaryngology community. As a result of resource limitations and social distancing measures, the day to day practice of pediatric otolaryngology was been abruptly altered, requiring rapid adaption to provide safety to the patients and the practitioners, as well as provide quality care to patients in need. The result of these adaptations has included the further development of telemedicine, elaborate protective protocols to allow for limited exposure to potential aerosol-generating procedures (AGP) for both patients and practitioners, and engaging in a national discussion regarding how to resume "normal" practice following the peak of the pandemic while continuing to provide safe and efficient care. Several consequences of COVID-19 infection manifested in the pediatric otolaryngology community are discussed and highlighted including anosmia, dysgeusia, hearing loss, MIS-C symptoms, and long COVID-19 symptoms.
The objective of this article is to highlight the unique ramifications of COVID-19 on pediatric otolaryngology, with a focus on the immediate and potential long-term shifts in practice.
Initial Diagnosis and Safety Protocols in Care for the Pediatric Patient and the Practitioners
In early March 2020, COVID-19 began its historic pandemic spread across the world. Unusual viral illnesses eventually identified as COVID-19 were discovered as early as November 2019 in China and January 2020 in the US. The widespread discovery of COVID-19 was identified in March 2020 and predominant spread at that time was communal based. Initial symptoms included include fever (43%–98%), cough (68%–82%), fatigue (38%–44%), sore throat (13.9%–17.4%), dry cough (59.4%), and sputum production (28%–33%).1 Common inflammatory markers were noted to be elevated including increased values of C-reactive protein (75%–93%), lactate dehydrogenase (27%–92%), and erythrocyte sedimentation rate (up to 85%).2
As this respiratory-based virus began to cause a significant increase in hospitalizations particularly in the adult population, there was a concerted effort to curb the spread of the virus. As those sick with COVID-19 initially presented to the hospital for care, much of the initial concerted effort to contain COVID-19 was focused on hospital-based care and protection. While the vast majority of the patients initially presenting to the hospital with COVID-19 were adults, there was a minority of children, particularly children with complex preexisting diseases, who also needed care for COVID-19-related respiratory issues in a hospital-based setting. In 2020, a review of 72314 cases from China identified less than 2% of the cases under 19 years of age and 1% of cases in patients under 10 years of age.3 It was determined that the vast majority of pediatric patients had much milder symptoms than adults and 15% of pediatric patient in Wuhan were asymptomatic4 which presented its own risk in asymptomatic spread through the pediatric population. The true prevalence of asymptomatic children is most likely underreported.5 There was an initial 14.8% rate of mortality in those over 80 years there was a 0% reported mortality in children under 9.6
As COVID-19 has evolved, the prevalence in children has evolved. Currently in the United States, children <18 years of age account for approximately 13.3% of laboratory-confirmed COVID-19 cases. Even with this increase in prevalence, the number of hospitalizations remains preponderantly small compared with adults with COVID-19.7 , 8
Initial efforts were made in a two-pronged approach: implementation of safety strategies to keep patients and practitioners safe and remote care through telemedicine to provide safe distance and curb the spread of COVID-19.
Initially, COVID-19 did not spread in a uniform manner internationally and pockets around the world were more dramatically impacted than others. Initially impacted communities included China, Italy, Iran, Seattle, New York, Spain, and France. In March 2020, the worldwide community of pediatric otolaryngologists began to share information via WhatsApp and through national and international societies. Local experiences with COVID-19 as well as protocols for safety and continued care of patients with COVID-19 were shared. This worldwide distribution of information allowed the pediatric otolaryngology community to implement national and local strategies to enhance safety and care for patients throughout the pandemic. IPOG (International Pediatric Otolaryngology Group) acted as the main working group to share guidelines and protocols across society. IPOG consists of several member pediatric otolaryngology groups including ANZSPO (Australian and New Zealand Society of Pediatric Otolaryngology), APOG (Asia Pacific Pediatric Otolaryngology Group), ASPO (American Society of Pediatric Otolaryngology), ESPO (European Society of Pediatric Otolaryngology), IAPO (Interamerican Association of Pediatric Otolaryngology), PENTAFRICA (Pediatric Ear, Nose, and Throat in Africa). An IPOG compiled and shared document in April 2020 included discussions of many urgent aspects of otolaryngology care including otolaryngology case classification, management and operative protocols of urgent cases, preprocedural testing for COVID-19, ethical decision making during COVID-19, and PPE use during COVID-19 with particular emphasis on aerosol-generating procedures.9 (https://cdn.ymaws.com/aspo.us/resource/resmgr/covid_19/ipog_covid_report_april_14.pdf) (Fig. 1 )
Fig. 1.
Aerosolized particles during surgery and need for PPE.
In May 2020, ASPO issued a societal statement in regards to aerosol-generating procedures (AGPs), suggesting that safety should be of utmost importance for COVID-19 unknown or positive patients, and providers should wear a gown, gloves, N95 mask, or powered air-purifying respirators (PAPR) and face shield (or equivalents) during an AGP either in the ambulatory or surgical setting. In communities with high prevalence of COVID-19 infections, unknown patients with COVID-19 undergoing AGPs with higher risk of aerosol transmission should be managed with proper isolation precautions, including maximal PPE and limiting the procedure to essential personnel.10
https://cdn.ymaws.com/aspo.site-ym.com/resource/resmgr/covid_19/aspo_c-19_ppe_statement_fina.pdf.
Many strategies that were shared included strategies for personal protection equipment in the operating room as well as the outpatient facilities. As COVID-19 is a respiratory-based virus, pediatric otolaryngologists are a particularly vulnerable specialty to viral exposure from pharyngeal/laryngeal exams. To prevent further spread, a great deal of strategic effort was employed in the personal protection of the patient and the practitioners. As hospital-based protocols were established, they were shared as best practices with communities that had not been impacted by the initial wave of COVID-19. While some communities were able to implement best practices, resources were not uniform from institution to institution and were limited in many cases. In New York City (and many other communities) in March/April 2020, there was an extreme shortage of surgical N95 masks for the health care community’s needs. These single-use masks were reused and reprocessed as was necessary11 with limited data to support the use.12 This practice placed health care workers in danger of contaminating themselves or others when doffing or donning the reused or reprocessed personal protection equipment (PPE) and nationally was advocated to only reuse and reprocess in times of critical shortage of equipment.11 Advocacy from the national and international community (such as IPOG and ASPO) for quality personal protection equipment was paramount to engage in providing adequate PPE to ensure that the safety of the patient and practitioners was at the forefront. In pediatric otolaryngology particular concern was for airway evaluation in the COVID-19 + patient or the COVID-19 unknown patient in the operating room or outpatient setting. Similarly, any airway intervention such as open airway surgery or tracheotomy in the COVID-19 + patient was carefully planned to provide as much safety as possible given the risk of contamination to the health care team. Data from the adult literature were used as a proxy for the care of the pediatric patients. For tracheotomy, the key recommendations to provide adequate safety in airway surgery included minimizing aerosolizing during the procedure include cauterization, providing paralysis to avoid coughing, ventilation only with cuff inflation, and stopping ventilation before entering the airway.13 Posttracheotomy care had recommendations of keeping the cuff inflated, use in-line suction, and delay tracheostomy tube change until COVID-19 has passed. Additionally, every effort should be made to avoid disconnecting the circuit before manipulating the airway.14
A four-institution North American pediatric hospital collaboration on safety in aerosol-generating procedures (AGPs) was published to provide guidance for all COVID-19 airway interventions. This combined approach of enhanced draping and use of SIM to optimize care and safety prior to operating room intervention provided a framework for all pediatric otolaryngologists to safely take care of their most critical airways.15 , 16
Similar efforts and insights were provided by the experts at Great Ormond Street giving practical insights into safety in laryngoscopy/bronchoscopy.17 (Fig. 2 )
Fig. 2.
Airway evaluation with protective PPE and protective covering over the airway.
Impact of COVID-19 on the Care for the Pediatric Patient
As the prevalence of COVID-19 continued to increase throughout the United States and the rest of the world, many patients were understandably concerned with exposure to COVID-19 and began to isolate. This isolation may have helped to prevent COVID-19 from further community spread but frequently delayed needed medical and surgical care. Routine otolaryngologic care was postponed and complex issues lingered for those in need, frequently becoming more complex with delays in care. This delay in medical and surgical care often manifested in delays in developmental milestones and learning goals. As schools turned to remote learning, this isolation and less robust learning environment adversely affected children’s ability to progress at a typical rate and adversely affected children’s mental and physical health.18, 19, 20 It is estimated due to remote schooling during the 2020-2021 year, students are on average 5 months behind on mathematics and 4 months behind on reading21 for the school year and 35% of parents very or extremely concerned about their children’s mental health.21
In terms of otolaryngologic issues, children with unresolved chronic otitis media continued to have speech delay and language deficits. Children with unresolved sleep-disordered breathing and/or obstructive sleep apnea continued to have poor sleep and unrestful sleep resulting in poor performance and decreased learning at remote schooling. While the initial reaction of isolation was wise in its ability to limit the community spread of COVID-19, it adversely impacted children’s mental and physical health dramatically.
With this data in hand, many system-based initiatives began in hospitals throughout the world to help mitigate risks and improve the patient experience to encourage patients to take care of their medical needs. As each system is unique, the approaches have been unique to the individual system. Most quickly adapted the safety protocols for aerosol-generating procedures with judicious use of PPE including N95 or equivalent masks or powered air-purifying respirators (PAPR) in their ambulatory and inpatient settings. In addition to personal protective equipment for both practitioners and patients, the general concept of a better and safer patient experience is to screen patients prior to visit to identify their medical needs as well as to screen patients for their and other patients’ safety. 95% of surveyed institutions used nasopharyngeal PCR and/or symptoms for screening prior to operative intervention.
This enhanced screening of patients in combination with judicious social distancing helped to mitigate the spread of COVID-19 during routine office visits as well as operative experiences.
Telemedicine has acted as a powerful adjunct to in-person visits and helps to initiate medical care and carefully plan a further treatment plan. This has added a necessary bridge to the care of the patient allowing patients who may not feel comfortable with the current pandemic to elicit medical advice and decide on the next steps. Once telemedicine has been initiated, the decision to continue remotely or follow with in-person visitation can be timed appropriately as the examination is limited in the remote setting.
If in-person visitation is needed, screening procedures aim to reduce risks to patients and practitioners for those coming to the office or operating room. Nearly all pediatric otolaryngology practices screen symptomatology and temperature routinely. A survey of COVID-19 and reopening strategies was conducted in May 2020 and at the time, screening tools used included temperature (87%), fever (81%) dry cough (84%), respiratory symptoms (86%) were used often, while muscle aches (42%), fatigue (36%), headache (35%), and loss of taste/smell (49%) were less used.22
95% of institutions screen and/or objectively test (via PCR) within 48 hours prior to office-based AGP procedure or any operative surgical procedure to ensure a COVID-19 negative patient (within the error of the test). Any screening or objective test that is found to be positive typically warrants rescheduling unless it is considered an emergency and unavoidable. This process allows for the office and the operating room to mitigate risks and protect both patients and practitioners.
Other endeavors to mitigate risk include allowing only 1 parent and no siblings to accompany patients to visits/operations, decreasing overall clinic volumes, adequate social distancing in the waiting rooms, and allowing time for air circulation to adequately clear the exam rooms of potential contamination help to keep the office setting safer to cross-contamination.
As the pandemic has continued and evolved, small adjustments to individual institutional screenings have occurred as informed by the evolving data: PCR tests have adjusted from a deep nasal swab to a more anterior nasal swab; family may not be limited in their ability to visit with a patient but masks may still be required at all hospital-based settings. Most institutions still require masked interactions and preoperative testing as the rates of community-based COVID-19 remain high.
The development of COVID-19-based vaccinations has been a large step forward in the overall safety and protection of the community during this pandemic. Several vaccinations have been created and many proved to be very effective in preventing transmission of the initial strains of COVID-19. As the virus has evolved, some vaccines have proved less effective in newer strains of COVID-19 virus. Initially, the vaccines were approved for emergency use and subsequently have gotten full FDA approval. These vaccines include Comirnaty and Pfizer-BioNTech COVID-19 Vaccine, Spikevax and Moderna COVID-19 Vaccine, and Janssen COVID-19 Vaccine. In 2021, Moderna and Pfizer were approved for vaccination for children 12 and over. Subsequently, Pfizer and Moderna have just recently been approved for the vaccination of children 6 months and older.
National leadership at the American Academy of Pediatrics and ASPO23 have encouraged all children eligible to obtain vaccination to help prevent further community transmission, aid in herd immunity and prevent severe disease from COVID-19 infection (https://aspo.us/resource/resmgr/aspo_covid19_statement_sept_.pdf).
COVID-19-Specific Symptoms Within Pediatric Otolaryngology
Generalized pediatric symptomatology of COVID-19 and treatment
Pediatric patients with COVID-19 typically have much milder symptoms than their adult counterparts. As a primarily respiratory virus, COVID-19 presented most typically with a fever, followed by cough, rhinorrhea, and sore throat. Other symptoms include headache, diarrhea, vomiting, and myalgias.23, 24, 25 In an international study of COVID-19-affected children, 242158 children were identified with COVID-19 between January and June 2020 with 9769 (4%) hospitalized with COVID-19.26 Dyspnea, anosmia, and GI symptoms were the more common than those with an influenza diagnosis during the same timeframe. There are potentially multiple explanations as to why children are infected less frequently and severely than adults. Children have a lower prevalence of comorbidities that are associated with severe disease.27 Also, children more often get colds (coronaviruses) and have higher coronavirus antibody levels than adults. Antibodies directed against seasonal coronaviruses may confer some protection. Pneumonia and hypoxemic were the most common diagnoses of hospitalized patients at up to 23% and 15%, respectively. Anosmia was uncommon at 0.8-1.5% in all patients and MIS-C was uncommon at 0.5–3% in all patients and 0.6-7% in hospitalized patients.26 Compared to influenza diagnosed at the same time, the incidence of pneumonia, hypoxemia, and MIS-C was higher in the COVID-19 population than the influenza population. Treatment plan for nonhospitalized pediatric patients continues to be conservative supportive care as most will recover very quickly and many are asymptomatic, to begin with. In hospitalized patients, corticosteroids and H2 blockers were the most common treatment plans. Antithrombotic therapy was more common in the US than internationally. Antibiotics and vitamin supplements were used infrequently.
Anosmia/hyposmia, dysgeusia
Anosmia can occur from postviral syndromes and has frequently been noted to have occurred with coronaviruses and rhinoviruses. Edema and congestion of the olfactory cleft cause conductive temporary loss which is common in rhinosinusitis. COVID-19 appears to cause anosmia despite mild rhinorrhea and mild congestion, suggesting that there is a sensorineural component to its origin. A recent meta-analysis of articles notes that the pooled prevalence of smell loss (anosmia or hyposmia) is 77% by objective measures and 44% by subjective measures.28
Dysgeusia can also be affected by postviral inflammation. As smell and taste are closely interlinked that it is not surprising that the incidence of anosmia and dysgeusia is similar at 5% in adults.29 Anosmia and/or dysgeusia are not common symptoms found in the pediatric COVID-19 + population at 0.8–1.5%26 and can be present without respiratory symptoms in children.30 Because of this presentation, it is important to consider the loss of smell or taste without respiratory symptoms as a strong predictor of COVID-19 if present.30 Most do improve with time but olfactory training is the primary method for restoring anosmia/hyposmia. Limited centers advocate for pharmacotherapy including the intranasal application of sodium citrate and vitamin A, as well as systemic use of omega-3 and zinc.31 Recovery of taste and smell has been variable in the amount of recovery and timeframe for recovery. Further research is underway in the treatment of smell and taste disordered in regard to COVID-19.
Multisystem inflammatory disorder in children
Multisystem inflammatory disorder in children (MIS-C) is a sequela of COVID-19 and most commonly affects young, school-aged children and is characterized by persistent fever, systemic hyperinflammation, and multisystem organ dysfunction. Initially identified in the UK in April 2020, by the end of June 2020 more than 1000 children had been diagnosed with MIS-C.32 Overall, MIS-C is relatively uncommon, affecting 0.5% to 3.1% of all patients diagnosed with COVID-19 but up to 0.9% to 7.6% of those hospitalized with COVID-19. In a separate cohort study, researchers found recently that 11% of children with COVID-19 admitted to hospitals in the United Kingdom developed MIS-C.
Per the US CDC and WHO MIS-C is defined as having a previous COVID-19 infection in conjunction with persistent fever, multi-organ dysfunction, and elevated inflammatory markers. MIS-C notes to have similar symptoms of Kawasaki disease or cytokine storm and was initially misdiagnosed as such. Patients with MIS-C most likely present with fever (100%), gastrointestinal symptoms (60–100%), rash (45–76%), conjunctivitis (30–81%), mucous membrane involvement (27–76%), Neuro symptoms (headache, confusion) (29–58%), respiratory symptoms (21–65%), sore throat (10–16%), and lymphadenopathy (6–16%).33 , 34
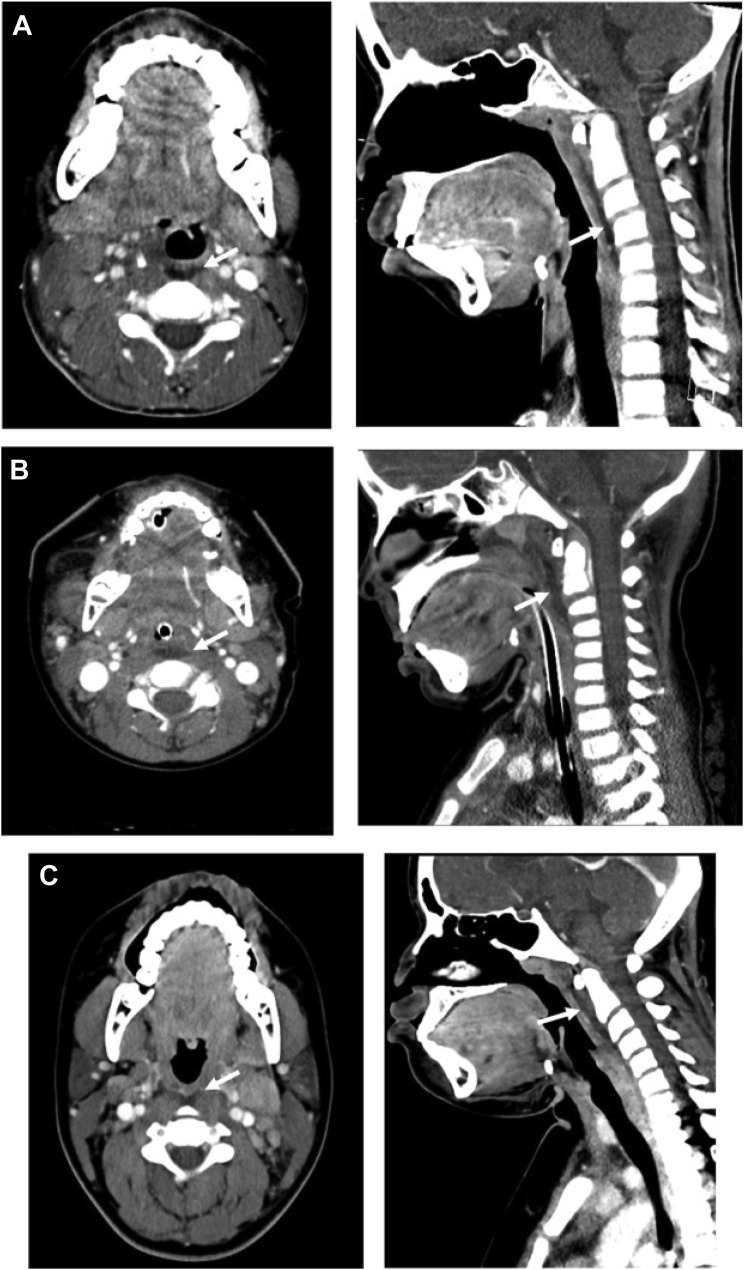
In otolaryngology, there have been reports of posterior pharyngeal edema masquerading as retropharyngeal abscess with lymphadenopathy. Retropharyngeal edema may be due to altered lymphatics in the setting of MIS-C inflammation.35 In terms of treatment, 2 large separate studies used IVIG with or without glucocorticosteroids and had conflicting results. One showed benefit with IVIG36 and lower risk of cardiovascular dysfunction while the other showed no difference.37 Time to treatment appears to be of the essence as the significant inflammatory response may make delayed treatments less effective.38 (Fig. 3 )
Fig. 3.
Retropharyngeal phlegmon present in COVID-19 + children. (A-C) Axial and sagittal imaging of retropharyngeal edema of 3 cases of MIS-C.
(From Daube A, Rickert S, Madan RP, Kahn P, Rispoli J, Dapul H. Multisystem inflammatory syndrome in children (MIS-C) and retropharyngeal edema: A case series. Int J Pediatr Otorhinolaryngol. 2021 May;144:110667. https://doi.org/10.1016/j.ijporl.2021.110667. Epub 2021 Mar 4. PMID: 33752089; PMCID: PMC7931672.)
Long COVID-19 and consequences
Long COVID-19 is a general term for persistent symptoms from COVID-19 beyond 2 months of initial symptoms, and includes brain fog, trouble remembering, fatigue, and mood swings. In one recent study, approximately 40% of previously COVID-19 + children experienced long COVID-19 symptoms, while 27% of controls exhibited similar symptoms.39 It is believed that as COVID-19 appears to affect different children differently, post–COVID-19 symptoms affect children differently. Careful coordination of care between health care, school care, and home care is essential to best take care of these complex recovery periods.
The long-term consequences of the COVID-19 pandemic remains largely unknown. The role of future generations may be affected by widespread COVID-19 infection similar to the widespread immune response of those who went through the 1918 flu pandemic.40
It is fully possible that early exposure to COVID-19 may prime one’s immune system to a proinflammatory state for future severity of COVID-19 strains.41 Further research is needed to best understand the longer-term consequences of early COVID-19 infections.
Impact on the Practitioner and the Health Care Team
By its very nature, the otolaryngology specialty has a unique set of conditions that make providers particularly vulnerable to upper respiratory pathogens. After all, we are “ear, nose, and throat” specialists and we spend our entire work day literally “in the face” of our patients. There is an abundance of information, suggesting that AGPs are a risk factor for exposure to a high viral burden, thus putting otolaryngologists at high risk of contracting the infection. The unique risk of close patient contact and AGPs has resulted in the necessity to take immediate steps to mitigate risk to providers. In the pediatric otolaryngology community, this has meant the rapid adoption of telemedicine for evaluating patients and the development of elaborate protocols to mitigate the risk of exposure to AGPs.
There are several unique features of pediatric otolaryngology practice that have made these changes particularly challenging. Firstly, children are inherently more susceptible to viral upper respiratory tract infections (URI) and their sequelae. Whereas it is easy to set criteria to avoid seeing adult patients with URI symptoms and wait until they recover, this is impractical for children as it is often the reason why they need to be seen. It would be impractical to obtain COVID-19 testing for all patients with a “runny nose” who need to be examined in the office. If that were possible, we know that COVID-19 testing has a false negative rate of at least 3–5% in best-case circumstances.42 , 43 In addition, current scientific evidence suggests that children may be asymptomatic carriers of COVID-19 of up to 15%,4 which would indicate that prescreening for illness would not help to mitigate potential risk to providers.
An additional unique feature of pediatric otolaryngology practice is that in a pediatric practice the children are often not “willing participants” in the examination process. This creates additional risk to providers as even a basic oral cavity or nasal exam can turn into an aersol generating event as children who do not want to participate end up crying, screaming, gagging, coughing, or spitting. To make matters more complex, the examination process most often requires close contact with not only the child but also their caregiver, creating additional exposure risk to the provider.
As stated above, the risks of COVID-19 exposure have resulted in the rapid adoption of telemedicine and enhanced safety protocols when physical contact with the patient becomes necessary. While telemedicine has for the most part become a great immediate solution for patient access,44 , 45 it is significantly limited by the same challenges that practitioners face with an in-person office visit; the child is often not a “willing participant” and if they refuse to open their mouth, there is only so much that can be evaluated virtually. Even with a fully compliant child on telemedicine, there is limited information that can be obtained in the remote setting particularly if it is the first visit. In addition, much of pediatric otolaryngology practice is focused on otologic complaints and at this point, there is no uniformly available replacement for the in-person otologic exam. While this is an evolving process, most institutions have developed protocols that incorporate screening ± COVID-19 testing, social distancing measures, and cleaning protocols to minimize the risk of exposure to health care providers when an in-person visit is needed. With the advent of vaccination for children and its widespread adoption, the combination of judicious use of telemedicine and safe controlled in-person encounters allow for quality medical care and decreased anxiety from the patient and family.
It is now becoming apparent that what we at first anticipated to be short-term adaptations to practice, are likely to be with us for the foreseeable future. Therefore, it is very likely that the practice of pediatric otolaryngology will permanently become a hybrid of virtual and in-person visits, even beyond the acute crisis. The hybrid model does offer several advantages to both the patient and the practitioner in this time of unease. Its widespread use helps families obtain initial medical care and treatment despite trepidation. It allows a patient–doctor relationship to develop despite the distance. It helps the practitioner to triage those with more serious issues and to streamline their care. Currently, its disadvantages are that it is time-consuming and limited in its ability to elicit a quality examination of the patient. Remote adapted technology such as otologic cameras for the visualization of the tympanic membrane and recorded video of sleep and breathing have helped to enhance the remote exam but still are limited. On a positive note, as we develop technologies to overcome the examination limitations of telemedicine, this may become an attractive alternative for many patients (and providers) as it will significantly reduce the time commitment, travel, school time lost, and cost related to an in-person visit.
Impact on Pediatric Otolaryngology Practices
The entire world has seen an economic contraction and the otolaryngology community has not been immune to this fact. Much of what we do is “quality of life” management rather than immediately necessary life preservation.46 This is even more apparent in general pediatric otolaryngology practice, where complex, life-threatening and/or cancer diagnoses represent only a minority of cases and where the “bread and butter” management is largely geared to improve patient comfort (ear infections), hearing (ear fluid) or sleep (adenotonsillar hypertrophy). During the acute phase of the COVID-19 pandemic, both office-based visits and elective surgical practice abruptly ceased, essentially arresting the financial pipeline of otolaryngology practices primarily treating children. Even 2 years into the pandemic as we reintegrate into the clinics and the operating room, volumes are lower than they were pre–COVID-19 and may be for the foreseeable future for a variety of reasons including enhanced safety protocols, parental fear of taking their child to the doctor and lost family income and/or insurance.
In addition to significantly reduced revenue, pediatric surgical practices in the United States have largely been left behind their adult counterparts in receiving government financial relief made available to Medicare but not Medicaid providers. To make matters worse, the majority of pediatric otolaryngologists practice in hospital-based settings and have, thus been unable to obtain the small business loans available to others specialists who practice in a private practice setting. The net result of these financial constraints has led to significantly reduced practice incomes leading to decreased personal incomes for physicians and the necessitation of reducing the cost by arresting new hires and/or furloughing employees as well as the reduction of expenses related to nonessential activities (meetings, dues, and so forth). While the volumes are slowly returning, adaptations to a new working environment of more remote workforce will yield more permanent shifts in the health care landscape. A hybrid model of telemedicine and in-person care is the most likely solution. With the advent of new technologies for remote examination and integrated electronic medical records, this hybrid model will provide a high level of satisfaction for patients and families who can get access to their health care provider more easily from multiple avenues in a convenient setting.
In summary, while the post–COVID-19 framework of pediatric otolaryngology practice is unknown, it is highly likely that the new normal of pediatric otolaryngology will incorporate telemedicine, enhanced safety protocols, new indications for direct patient contact, and reduced patient volumes. This hybrid model of practice should continue to deliver high-quality care and multiple avenues of access. It remained to be seen how the post–COVID-19 landscape will affect pediatric otolaryngology practices nationwide as the recovery has been slow but continues to improve with time.
Clinics care points
-
•
National leadership at the American Academy of Pediatrics and ASPO23 have encouraged all children eligible to obtain vaccination to help prevent further community transmission, aid in herd immunity and prevent severe disease from COVID-19 infection.
-
•
Treatment plan for nonhospitalized pediatric patients continues to be conservative supportive care as most will recover very quickly and many are asymptomatic, to begin with.
-
•
In hospitalized patients, corticosteroids and H2 blockers were the most common treatment plans. Antithrombotic therapy was more common in the US than internationally. Antibiotics and vitamin supplements were used infrequently.
-
•
Recovery of taste and smell has been variable in the amount of recovery and timeframe for recovery. Further research is underway in the treatment of smell and taste disordered in regard to COVID-19.
-
•
Multisystem inflammatory disorder in children (MIS-C) is a sequela of COVID-19 and most commonly affects young, school-aged children and is characterized by persistent fever, systemic hyperinflammation, and multisystem organ dysfunction.
-
•
Time to treatment appears to be of the essence as the significant inflammatory response may make delayed treatments less effective. It is believed that as COVID-19 appears to affect different children differently, post–COVID-19 symptoms affect children differently.
-
•
Careful coordination of care between health care, school care, and home care is essential to best take care of these complex recovery periods.
-
•
The post–COVID-19 framework of pediatric otolaryngology practice is unknown, it is highly likely that the new normal of pediatric otolaryngology will incorporate telemedicine, enhanced safety protocols, new indications for direct patient contact, and reduced patient volumes.
-
•
This hybrid model of practice should continue to deliver high-quality care and multiple avenues of access.
Acknowledgments
Disclosure
The authors have nothing to disclose.
References
- 1.Wang D., Hu B., Hu C., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lippi G, Plebani M. Laboratory abnormalities in patients with COVID-2019 infection [published online March 3, 2020]. Clin Chem Lab Med. https://doi.org/10.1515/cclm-2020-0198. [DOI] [PubMed]
- 3.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 4.Lu X., Zhang L., Du H., et al. SARS-CoV-2 infection in children. N Engl J Med. 2020 doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nikolopoulou G.B., Maltezou H.C. COVID-19 in Children: Where do we Stand? Arch Med Res. 2022;53(1):1–8. doi: 10.1016/j.arcmed.2021.07.002. [Epub 2021 Jul 6. PMID: 34311990; PMCID: PMC8257427] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong Y., Mo X., Hu Y., et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020 doi: 10.1542/peds.2020-0702. [DOI] [Google Scholar]
- 7.American Academy of Pediatrics. Children and COVID-19: State-Level Data Report. services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/2021 Available at: Accessed August 15, 2022.
- 8.ASPO statement on vaccination. 2021. https://aspo.us/resource/resmgr/aspo_covid19_statement_sept_.pdf Available at: Accessed August 15, 2022.
- 9.IPOG COVID report April 14. 2020. https://cdn.ymaws.com/aspo.us/resource/resmgr/covid_19/ipog_covid_report_april_14.pdf Available at: Accessed August 15, 2022.
- 10.ASPO PPE statement May. 2020. https://cdn.ymaws.com/aspo.site-ym.com/resource/resmgr/covid_19/aspo_c-19_ppe_statement_fina.pdf Available at: Accessed August 15, 2022.
- 11.Toomey E.C., Conway Y., Burton C., et al. Extended use or reuse of single-use surgical masks and filtering face-piece respirators during the coronavirus disease 2019 (COVID-19) pandemic: a rapid systematic review. Infect Control Hosp Epidemiol. 2021;42(1):75–83. doi: 10.1017/ice.2020.1243. [Epub 2020 Oct 8. PMID: 33028441; PMCID: PMC7588721] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chirico F., Nucera G., Magnavita N. COVID-19: protecting healthcare workers is a priority. Infect Control Hosp Epidemiol. 2020 doi: 10.1017/ice.2020.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wei W.I., Tuen H.H., Ng R.W.M., et al. Safe tracheostomy for patients with severe acute respiratory syndrome. Laryngoscope. 2003;113:1777–1779. doi: 10.1097/00005537-200310000-00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harrison L., Ramsden J., Winter S., et al. Tracheostomy guidance during the COVID-19 Pandemic. ENT UK. 2020. https://www.entuk.org/tracheostomy-guidance-during-covid-19-pandemic Available at: Accessed August 15, 2022.
- 15.Francom C.R., Javia L.R., Wolter N.E., et al. Pediatric laryngoscopy and bronchoscopy during the COVID-19 pandemic: a four-center collaborative protocol to improve safety with perioperative management strategies and creation of a surgical tent with disposable drapes. Int J Pediatr Otorhinolaryngol. 2020;134:110059. doi: 10.1016/j.ijporl.2020.110059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.IPOG COVID Report April 14. 2020. https://cdn.ymaws.com/aspo.us/resource/resmgr/covid_19/ipog_covid_report_april_14.pdf Available at: Accessed August 15, 2022.
- 17.Frauenfelder C., Butler C., Hartley B., et al. Practical insights for paediatric otolaryngology surgical cases and performing microlaryngobronchoscopy during the COVID-19 pandemic. Int J Pediatr Otorhinolaryngol. 2020;134:110030. doi: 10.1016/j.ijporl.2020.110030. [Epub 2020 Mar 30. PMID: 32278168; PMCID: PMC7142686] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dunton G.F., B Do S.D. Wang Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the US. BMC Public Health. 2020;20:1–13. doi: 10.1186/s12889-020-09429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xie X., Xue Q., Zhou Y., et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020;174:898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang J., Shuai L., Yu H., et al. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102077. Article 102077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.COVID-19 and education: The lingering effects of unfinished learning. https://www.mckinsey.com/industries/education/our-insights/covid-19-and-education-the-lingering-effects-of-unfinished-learning Available at: Accessed August 15, 2022.
- 22.Rickert S.M. COVID and reopening strategies in pediatric otolaryngology, May. 2020. https://www.surveymonkey.com/results/SM-7239F57N7 Available at: Accessed August 15, 2022.
- 23.Götzinger F., Santiago-García B., Noguera-Julián A., et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4:653–661. doi: 10.1016/S2352-4642(20)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parri N., Magistà A.M., Marchetti F., et al. Characteristic of COVID-19 infection in pediatric patients: early findings from two Italian Pediatric Research Networks. Eur J Pediatr. 2020;179:1315–1323. doi: 10.1007/s00431-020-03683-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.King J.A., Whitten T.A., Bakal J.A., et al. McAlister Symptoms associated with a positive result for a swab for SARS-CoV-2 infection among children in Alberta. CMAJ. 2021;193:E1–E9. doi: 10.1503/cmaj.202065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duarte-Salles T., Vizcaya D., Pistillo A., et al. Thirty-day outcomes of children and adolescents with COVID-19: an international experience. Pediatrics. 2021;148(3) doi: 10.1542/peds.2020-042929. e2020042929. [Epub 2021 May 28. PMID: 34049958] [DOI] [PubMed] [Google Scholar]
- 27.Dorjee K., Kim H., E Bonomo R. Dolma Prevalence and predictors of death and severe disease in patients hospitalized due to COVID-19: A comprehensive systematic review and meta-analysis of 77 studies and 38,000 patients. PLoS One. 2020;15 doi: 10.1371/journal.pone.0243191. Article e0243191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hannum M.E., Ramirez V.A., Lipson S.J., et al. Objective sensory testing methods reveal a higher prevalence of olfactory loss in COVID-19-positive patients compared to subjective methods: a systematic review and meta-analysis. Chem Senses. 2020;45(9):865–874. doi: 10.1093/chemse/bjaa064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mao L., Wang M., Chen S., et al. Neurological Manifestations of Hospitalized Patients with COVID-19 in Wuhan, China: a retrospective case series study. Available at SSRN: 2020. Available at: [DOI]
- 30.Mak P.Q., Chung K.-S., Wong J.S.-C., et al. Anosmia and ageusia: not an uncommon presentation of COVID-19 infection in children and adolescents. Pediatr Infect Dis J. 2020;39:e199–e200. doi: 10.1097/INF.0000000000002718. [DOI] [PubMed] [Google Scholar]
- 31.Neta F.I., Fernandes A.C.L., Vale A.J.M., et al. Pathophysiology and possible treatments for olfactory-gustatory disorders in patients affected by COVID-19. Curr Res Pharmacol Drug Discov. 2021;2:100035. doi: 10.1016/j.crphar.2021.100035. [Epub 2021 Jun 5. PMID: 34870148; PMCID: PMC8178068] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Levin M. Childhood multisystem inflammatory syndrome—a new challenge in the pandemic. N Engl J Med. 2020;383 doi: 10.1056/NEJMe2023158NEJMe2023158–NEJMe2023158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Whittaker E., Bamford A., Kenny J., et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. 2020;324:259. doi: 10.1001/jama.2020.10369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Feldstein L.R., Rose E.B., Horwitz S.M., et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. 2020;383:334. doi: 10.1056/NEJMoa2021680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Daube A., Rickert S., Madan R.P., et al. Multisystem inflammatory syndrome in children (MIS-C) and retropharyngeal edema: a case series. Int J Pediatr Otorhinolaryngol. 2021;144:110667. doi: 10.1016/j.ijporl.2021.110667. [Epub 2021 Mar 4. PMID: 33752089; PMCID: PMC7931672] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McArdle A.J., Vito O., Patel H., et al. Treatment of multisystem inflammatory syndrome in children. N Engl J Med. 2021;385(1):11–22. doi: 10.1056/NEJMoa2102968. [Epub 2021 Jun 16. PMID: 34133854; PMCID: PMC8220965] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Son MBF, Murray N, Friedman K, et al.Multisystem inflammatory syndrome in children — initial therapy and outcomes. N Engl J Med. 10.1056/NEJMoa2102605 [DOI] [PMC free article] [PubMed]
- 38.DeBiasi R.L. Immunotherapy for MIS-C - IVIG, Glucocorticoids, and Biologics. N Engl J Med. 2021;385(1):74–75. doi: 10.1056/NEJMe2108276. [Epub 2021 Jun 16. PMID: 34133878; PMCID: PMC8362545] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rutter M.J.H. Difficult questions about long COVID in children Lancet Child Adolesc Health. 2022 doi: 10.1016/S2352-4642(22)00167-5. :S2352-4642(22)00167-5. [Epub ahead of print. PMID: 35752193; PMCID: PMC9221929] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chuah C.X.P., Lim R.L. MIC. Chen Investigating the legacy of the 1918 influenza pandemic in age-related seroepidemiology and immune responses to subsequent influenza A(H1N1) viruses through a structural equation model. Am J Epidemiol. 2018;187:2530–2540. doi: 10.1093/aje/kwy192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holuka C., Merz M.P., Fernandes S.B., et al. The COVID-19 pandemic: does our early life environment, life trajectory and socioeconomic status determine disease susceptibility and severity? Int J Mol Sci. 2020;21:5094. doi: 10.3390/ijms21145094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Parikh S.R., Bly R.A., Bonilla-Velez J., et al. Pediatric otolaryngology divisional and institutional preparatory response at seattle children’s hospital after COVID-19 regional exposure. Otolaryngol Head Neck Surg. 2020;162(6):800–803. doi: 10.1177/0194599820919748. [DOI] [PubMed] [Google Scholar]
- 43.Vinh D.B., Zhao X., Kiong K.L., et al. An overview of COVID-19 testing and implications for otolaryngologists. Head Neck. 2020;42(7):1629–1633. doi: 10.1002/hed.26213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ning A.Y., Cabrera C.I., D'Anza B. Telemedicine in otolaryngology: a systematic review of image quality, diagnostic concordance, and patient and provider satisfaction. Ann Otol Rhinol Laryngol. 2020 doi: 10.1177/0003489420939590. 3489420939590. [DOI] [PubMed] [Google Scholar]
- 45.Mukerji S.S., Liu Y.C., Musso M.F. Pediatric otolaryngology workflow changes in a community hospital setting to decrease exposure to novel coronavirus. Int J Pediatr Otorhinolaryngol. 2020;136:110169. doi: 10.1016/j.ijporl.2020.110169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sobol S.E., Preciado D., Rickert S.M. Pediatric Otolaryngology in the COVID-19 Era. Otolaryngol Clin North Am. 2020;53(6):1171–1174. doi: 10.1016/j.otc.2020.08.005. [Epub 2020 Aug 19. PMID: 32951900; PMCID: PMC7437513] [DOI] [PMC free article] [PubMed] [Google Scholar]