New York City was the first US location to record a coronavirus disease 2019 (coronavirus disease 2019) case on March 1, 2020, and soon became the epicenter of the pandemic. Because of the large number of hospitalizations (1), Governor Cuomo imposed a halt on all elective care from March 22 to June 8, 2020 (2), provoking reduced cancer screening rates (3), delayed cancer care and treatment (4,5). Our aim is to quantify the effect of the “pause” on cancer stage at diagnosis, one of the best indicators of cancer prognosis, using lung cancer as an example of a condition where early diagnosis can dramatically modify survival.
Lung cancer cases diagnosed between January 1, 2018 and February 28, 2021 at the Mount Sinai Health System were identified from Mount Sinai’s cancer registry, based on ICD-10 (International Classification of Diseases) codes of C34.00-22 (cases diagnosed at Mount Sinai), as per Commission on Cancer guidelines. For observations that reflected multi-tumor or multi-hospital cases, unique patients were identified by selecting the earliest date of diagnosis. Patients’ records was used to obtain stage at diagnosis.
The monthly number of diagnoses was averaged across 2018 and 2019 and the ratio of the number of monthly cases in 2020–2021 over the average number of monthly cases in 2018 and 2019 was calculated. The percent of monthly diagnoses with early (0/I/II), late (III/IV) and unknown stage over the total number of monthly diagnoses was examined and was compared to the average percent in 2018 and 2019 from the same month.
The analysis included 1,884 patients. There was a sharp drop in the number of diagnoses starting in March 2020, reaching a minimum in April 2020 (78% lower than average number of diagnoses in April of 2018 and 2019), and returning to near pre-pandemic levels by July 2020. Diagnoses began to decline again in January and February 2021 (35% lower than pre-pandemic averages) (Figure 1).
Figure 1.
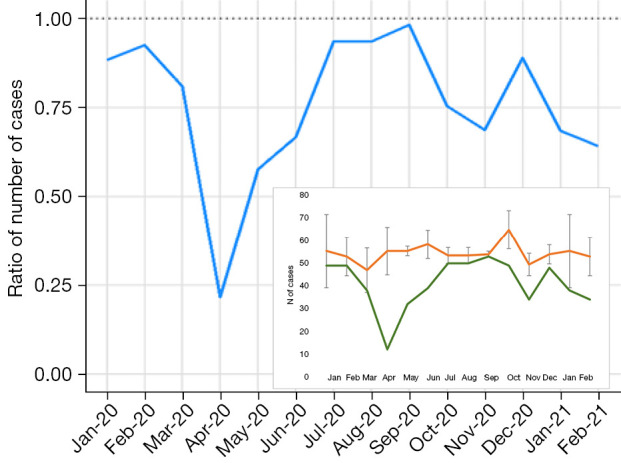
Ratio of number of lung cancer cases in 2020 and 2021, compared to an average in 2018 and 2019, by month. The small square represents actual number of cases by month, in 2018-19 (orange) and 2020-21 (green); bars are standard deviations.
Overall 41% of patients were diagnosed at stage 0/I/II and 51% were diagnosed at stage III/IV (8% had unknown stage). The percent diagnosed at stage 0/I/II decreased to 21.9% in May 2020, while the percent diagnosed at stage III/IV reached a maximum in April 2020 at 75%. Early stage diagnoses dropped again (23.5% of all diagnoses), while late stage diagnoses increased (64.7% of all diagnoses) in February 2021. A time-series analysis showed that the stage distribution during the months of the “pause” was significantly different from the expected, based on the trend in previous years (Figure 2).
Figure 2.
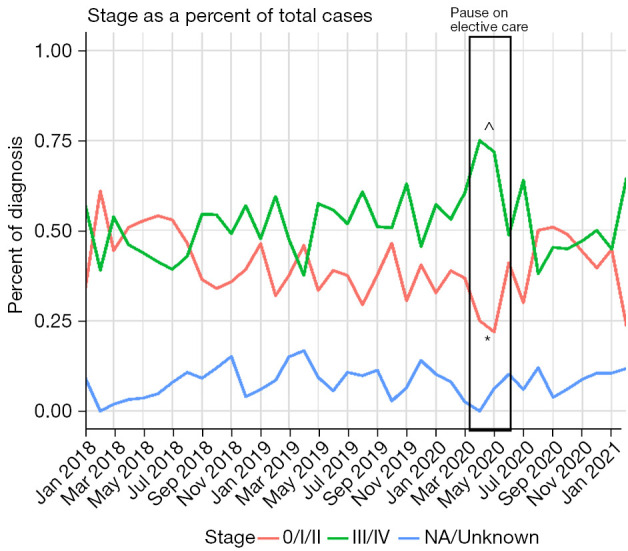
Distribution of lung cancer stage at diagnosis by month. Welch test P value versus predicted values in time-series analysis (ARIMA): *=0.02309, ^=0.02541.
When compared to the average percent of diagnoses by stage in 2018 and 2019, the percent of stage III/IV diagnoses in April of 2020 was 1.79 times greater than the pre-pandemic average. In April and May 2020, the percent of stage 0/I/II diagnoses was 50% lower than the averages for April and May pre-pandemic. The percent of stage 0/I/II cases increased relative to pre-pandemic levels between August 2020 and January 2021. In February 2021 the percent of stage 0/I/II diagnoses was 50% lower than pre-pandemic levels, and the percent of stage III/IV diagnoses was 1.3 times greater than pre-pandemic levels (Figure 3).
Figure 3.
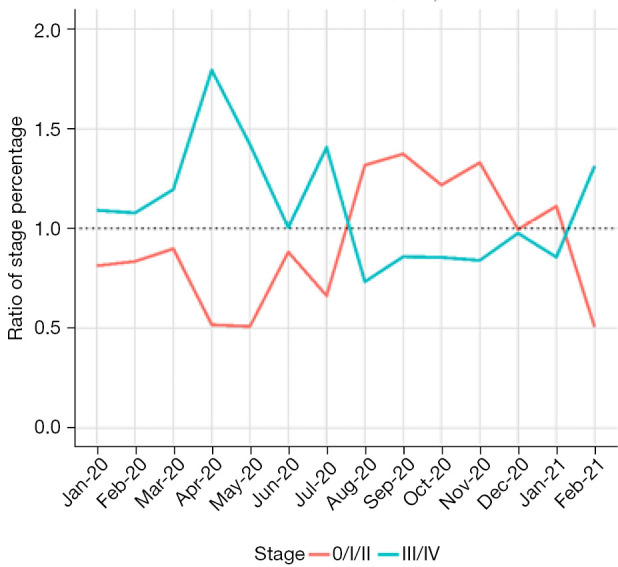
Ratio of percent of early and late stage lung cancer diagnoses, compared to an average in 2018 and 2019, by month.
This descriptive analysis suggests an immediate negative impact on lung cancer diagnoses of COVID-19 restrictions, with a sharp decrease in early stage diagnoses when a “pause” on elective procedures was introduced during the Spring of 2020, as well as when COVID-19 cases sharply increased during the Winter of 2021. Although a lot have been said on the delays in diagnosis and treatment following the COVID-19 pandemic (3-5), few studies have shown how delays affect stage at diagnosis (6), and those who studied the problem did not apply the sophisticated approach we used. The pandemic affected screening, early detection, and drastically reduced any patient’s contact with the health system that would have prompted an early lung cancer diagnosis. The increase in late stage diagnoses during pandemic surges may reflect the fact that only sick patients with symptoms, and acute events that require immediate care were seeking hospital attention. Although we cannot assess if the late stage diagnoses observed during the 2021 Winter surge could have been identified earlier through screening if the health system would have been fully operational as in regular times, it is likely that for some of those late diagnoses this is the case. The data presented here suggests that we will likely observe an increase in lung cancer mortality in the next few months and years, as consequence of stage shift at diagnosis associated with the COVID-19 pandemic.
Supplementary
The article’s supplementary files as
Acknowledgments
We thank Shivam Joshi, MBA, MS for significant contribution to the statistical revision of the manuscript.
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Peer Review File: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-191/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-191/coif). The authors have no conflicts of interest to declare.
References
- 1.Daily Hospitalization Summary. Accessed on 1/06/2022. Available online: https://coronavirus.health.ny.gov/daily-hospitalization-summary
- 2.Governor Cuomo Signs the “New York State on PAUSE” executive order. Accessed on 1/6/2022. Available online: https://www.governor.ny.gov/news/governor-cuomo-signs-new-york-state-pause-executive-order
- 3.The Lancet Oncology COVID-19 and cancer: 1 year on. Lancet Oncol 2021;22:411. 10.1016/S1470-2045(21)00148-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.COVIDSurg Collaborative . Projecting COVID-19 disruption to elective surgery. Lancet. 2022;399:233-4. 10.1016/S0140-6736(21)02836-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nepogodiev D; COVIDSurg and GlobalSurg Collaboratives. Timing of surgery following SARS-CoV-2 infection: country income analysis. Anaesthesia 2022;77111-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mynard N, Saxena A, Mavracick A, et al. Lung Cancer Stage Shift as a Result of COVID-19 Lockdowns in New York City, a Brief Report. Clin Lung Cancer 2022;23:e238-42. 10.1016/j.cllc.2021.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as


