Abstract
Multiple sclerosis is a disease that affects the central nervous system, resulting in various symptoms such as vision, physical activity, and stability. Central positional vertigo as initial multiple sclerosis symptoms are a rare case. It increases the attention of doctors to follow accurate measurements to diagnose multi sclerosis regarding the initial symptoms.
Keywords: case report and systematic literature review, central positional vertigo, multiple sclerosis
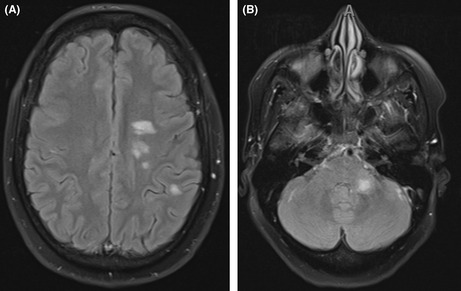
(A and B) The MRI brain confirms the existence of multiple sclerosis and shows multiple demyelinating patches
1. INTRODUCTION
Multiple sclerosis (MS) is one of the most common and best‐known demyelinating diseases, with a peak incidence between 20 and 30 years of age. 1 MS has a wide range of presentations and an equally wide range of prognoses. Classically, MS is diagnosed by finding multiple white matter lesions separated by space and time, while the location of the lesion defines the clinical features. Common clinical features include corticospinal tract signs (weakness and spasticity), sensory abnormalities, and cerebellar dysfunction (intention tremors and ataxia). 2 In patients with MS, equilibrium disorders caused by the involvement of the brainstem and cerebellar structures are common, and about 20% of MS patients represent true vertigo at some time during the disease. However, peripheral conditions such as benign paroxysmal positional vertigo (BPPV) and central positional vertigo were also reported. 3 Therefore, an accurate otoneurologic investigation distinguishes between central and peripheral causes. Central positional vertigo associated with MS could be easily misdiagnosed as BPPV. It could be difficult to differentiate it from BPPV if it occurred as the initial MS symptoms. The Provoking maneuvers like Dix‐hall pike and Supine head roll test results are crucial in diagnosing. 4 In this publication, we described a case of central positional vertigo as one of the early symptoms of multiple sclerosis. Accompanying this case was a comprehensive examination of other similar instances.
2. CASE PRESENTATION
A forty‐four‐year‐old female patient with co‐morbid illnesses. She was presented 2 years ago with acute onset severe vertigo that lasted for 2 days. This vertigo was related to position increased in lying on either side, associated with nausea, recurrent vomiting, and inability to walk. A viral infection or ear problem did not precede the patient's condition. The patient was conscious, alert, and oriented to date, time, and persons on examination. There was first‐degree bilateral horizontal nystagmus with intact motor, normal plantar response, and intact sensation and cerebellar examination. The ENT examination was normal (no middle ear problems, viral infection, or vesicles), but there was a positive Dix Hallpike maneuver. The patient was admitted to combined neurology and ENT for further evaluation and MRI brain. The MRI brain result showed multiple demyelinating patches corresponding to a multiple sclerosis diagnosis (Figure 1A,B). We started her on pulse steroid therapy for 5 days with marked improvement. We referred her to a multiple sclerosis specialized center, where they confirmed the diagnosis via CSF analysis (oligoclonal bands and IgG index). The patient was started fingolimod 0.5 mg orally once daily
FIGURE 1.
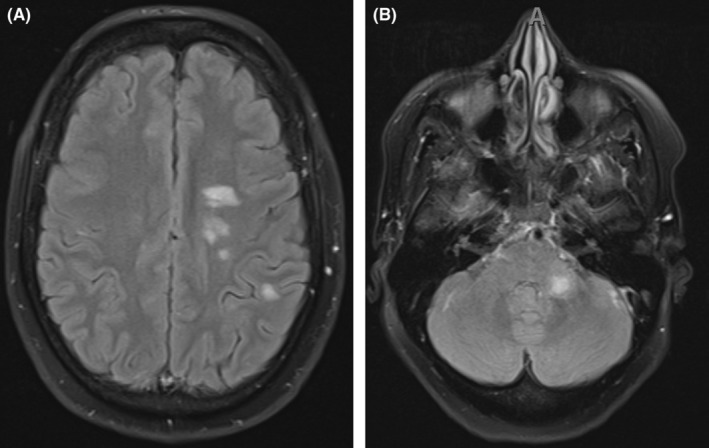
(A and B) The MRI brain confirms the existence of multiple sclerosis and shows multiple demyelinating patches.
3. METHODS
This review is performed and reported according to meta‐analysis (PRISMA) guidelines. 5
3.1. Literature search strategy
We systematically searched PubMed, Scopus, Web of Science, and Chochrane. The following search term was used for database search: (“Benign Paroxysmal Positional Vertigo” OR “Benign positional vertigo” OR “peripheral vertigo” OR “acute vestibular syndrome” OR “acute vestibulopathy” OR “Familial Vestibulopathy” OR “Benign Recurrent Vertigos” OR BPPV) AND (“Multiple sclerosis” OR “disseminated sclerosis” OR MS). The last literature search was done on October 27, 2021
3.2. Eligibility criteria and study selection
Including studies in our systematic review must contain original data about BPPV as the first presentation and multiple sclerosis. In addition, because the data available on his topic are very rare, we decided to include all study designs, including case reports, except litter to the editor, reviews, and comments. Two independent researchers performed study screening and study selection. (Figure 2)
FIGURE 2.
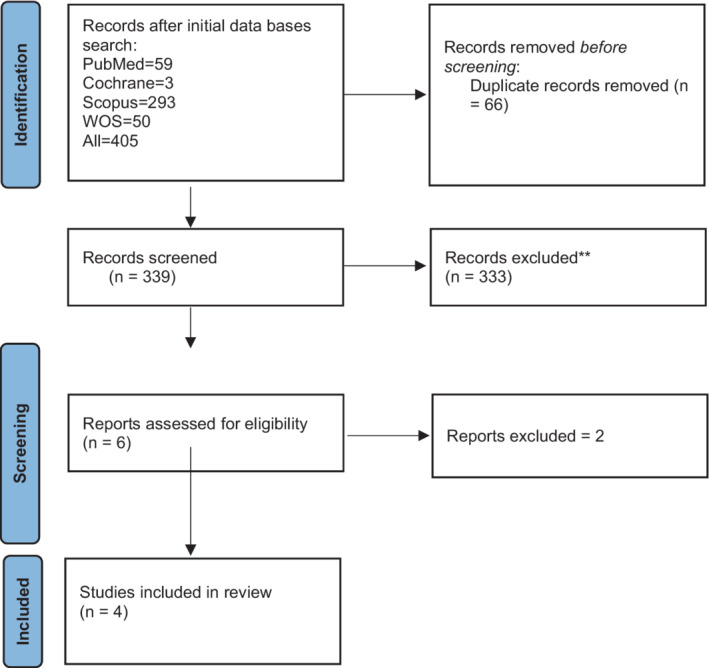
PRISMA of the included studies.
4. RESULTS
From 339 studies screened, only four studies met the eligibility criteria for our systematic review. The four studies were case reports with 32 cases as follows: (25, 5, 1, 1), (Frohman 2000, Thomas 2016, Musat 2020, Yoosefinejad 2015) respectively. 6 , 7 , 8 Demographic characteristics and clinical data were extracted in Table 1. Age ranges from 31 to 44 years, with 19 female and eight male cases. Two cases were initially diagnosed as BPPV, and MS was found on MRI as white patches. In those two cases, Epley and deep head hanging maneuver did not relieve vertigo, but steroid use in the second case (Musat 2020) was relived. In (Yoosefinejad 2015), the case was diagnosed with MS 6 years before developing BPPV, which was diagnosed by clinical presentation. Then, they confirmed the diagnoses after Semont and Epley maneuvers were used and significantly relieved the BPPV.
TABLE 1.
Characteristics of studies and included patients
| Study ID | Study design | Country | number of patients | Age | Sex | Study period | Vertigo | Nystagmus (spontaneous) | Dix–Hallpike maneuver | Initial Diagnosis | The right diagnosis | Treatment | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Frohman 2000 | Case series | USA | 25 | 44.6 (14.5) | Male 8 (32%) Females 17 (68%) | 4 years | Positional 13 (52%) Intermittent 3 (12%) Constant 6 (24%) Episodic 1 (4%) Paroxysmal 1 (4%) Head movement 1 (4%) | Right 7 (28%) Left 3 (12%) bilateral gaze evoked 1 (4%) Not observed 14 (56%) | Right 10 (40%) Left 3 (12%) Not observed 12 (48%) | BPPV 13 (52%) MS plaque 8 (32%) Meniere's disease 1 (4%) Vestibular neuritis 1 (4%) Vertigo paroxysms 1 (4%) Vertiginous migraine 1 (4%) | Epley 13 (52%) Steroids 8 (32%) Clonazepam 2 (8%) Carbamazepine 1 (4%) Diet and salt restriction 1 (4%) | This study reported that BPPV may be the most common cause for vertigo in MS. treating with vestibular suppressants does not have any role in the treatment of this mechanical condition. | |
| Thomas 2016 | Case series | USA | 5 | Young adult 2 (40%) Elderly patient 1 (20%) Middle‐aged adult 2 (40%) | NR | 4 weeks | Positional 5 (100%) | Right 1 (20%) bilateral gaze evoked 1 (20%) NR 3 (60%) | NR | One case BPPV | MS | ‐ | Barriers to allied health professionals may lead to error diagnosis, so sociocultural barriers should be breaking down. |
| Musat 2020 | Case report | Romania | 1 | 31 | Female | NR | Positional | No spontaneous nystagmus | Right | BPPV | MS | Deep head hanging maneuver was applied but without any positive result | Central positional nystagmus must be suspicioned whenever the nystagmus elicited at the positional testing is atypical |
| Yoosefinejad 2015 | Case report | Iran | 1 | 34 | Female | MS diagnosed first 6 years before BPPV | Positional | NR | NR | BPPV | Semont and Epley exercises | Semont and Epley significantly relieved the BPPV symptoms with 2 weeks follow‐up. |
Abbreviations: BPPV, Benign paroxysmal positional vertigo; MS, Multiple sclerosis, and NR = Not reported.
5. DISCUSSION
Benign paroxysmal positional vertigo (BPPV) is a disease of the inner ear characterized by repeated episodes of positional vertigo. BPPV could be clinically diagnosed by elicitation of nystagmus and vertigo on provoking maneuvers for BPPV. 9 Although provoking maneuvers are very useful, minute changes in their findings should raise suspicion of other central causes as it could be easily mixed with central positional vertigo (CPV). CPV can be, CPN is caused by cerebellar and/or brainstem dysfunction and can mimic BPPV. 10 For patients with atypical presentation of BPPV, the physician should consider further investigation with audiometry, vestibular function testing, and neuroimaging. Atypical BPPV presentation could be Vertigo that lasts longer than 1 min, associated hearing loss, associated neurological symptoms like gait disturbances or previous history of neurological disorders or tumors. Failure to respond to canalith repositioning maneuvers or vestibular rehabilitation therapy.
6. CASE REPORT DISCUSSION
In (Yoosefinejad 2015), they say the Dix‐Hallpike maneuver exacerbated the patient's symptoms, and that led them to make sure that the diagnosis was BPPV, but we do not know what they mean by “exacerbation of symptoms” they did not report the duration, direction, latency of the elicited nystagmus and we cannot trust their judgment as central positional vertigo is still not excluded from the diagnosis which means the patient's vertigo could be of central cause, in this case, MS as the patient was previously diagnosed by MS 6 years before the vertigo onset.
In Must 2020, as in our case, the patient's vertigo was alleviated by steroid therapy. Moreover, a deep head hanging maneuver was applied without any positive result, which suggests that MRI confirmed the central cause of vertigo and MS.
The cases reported in this review and our case report suggest that central positional vertigo associated with MS could be easily misdiagnosed as BPPV. It may not be that difficult if the case comes with new‐onset positional vertigo after initial diagnosis with MS, but on the contrary, if the reverse happens, as in our case, the final decision of BPPV diagnosis should be carefully taken after ruling out other possible central causes.
The Provoking maneuvers like Dix‐hall pike and Supine head roll test results are very crucial in making the diagnosis; minute changes or atypical presentation should raise our susception of central causes, and MRI and CT scans can be good tools to rule out central causes before final BPPV diagnosis decision is taken in this case. After all, we suggest more primary research, observational retrospective, and clinical trials should be done to investigate the MS and BPPV association and possible errors in diagnosis.
7. CONCLUSION
One of the most uncommon symptoms of multiple sclerosis is vertigo, which occurs in the central nervous system and disrupts the patient's ability to maintain a steady‐state of balance. Multiple sclerosis patients with central positional vertigo as their first symptom are uncommon in the medical literature. It brings to the notice of clinical specialists the need to follow proper measures while diagnosing multiple sclerosis about the early symptoms.
AUTHOR CONTRIBUTIONS
All authors have read and approved the manuscript. MM, AS, AME, AH, WSA, YA, SMK, and SS contributed in writing and reviewing the manuscript.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was given by the KING KHALED Hospital. In addition, the patient has given their parental consent for this publication.
CONSENT
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
ACKNOWLEDGEMENT
Our sincere thanks to all the doctors and nurses who participated in the treatment of this case, and we also thank the patient's parents for allowing us to report this case.
Meshref M, Shaheen A, Elmatboly AM, et al. Central positional vertigo as first initial multiple sclerosis symptom: A case report with systematic review. Clin Case Rep. 2022;10:e06154. doi: 10.1002/ccr3.6154
DATA AVAILABILITY STATEMENT
All data (of this patient) generated during this study are included in this published article and its supplementary information files.
REFERENCES
- 1. Filippi M, Bar‐Or A, Piehl F, et al. Multiple sclerosis. Nat Rev Dis Prim. 2018;4(1):43. [DOI] [PubMed] [Google Scholar]
- 2. Kamm CP, Uitdehaag BM, Polman CH. Multiple sclerosis: current knowledge and future outlook. Eur Neurol. 2014;72(3–4):132‐141. [DOI] [PubMed] [Google Scholar]
- 3. Alpini D, Caputo D, Pugnetti L, Giuliano DA, Cesarani A. Vertigo and multiple sclerosis: aspects of differential diagnosis. Neurol Sci. 2001;22(8):S84‐S87. doi: 10.1007/s100720100041 [DOI] [PubMed] [Google Scholar]
- 4. Balatsouras DG, Koukoutsis G, Ganelis P, Korres GS, Kaberos A. Diagnosis of single‐ or multiple‐canal benign paroxysmal positional vertigo according to the type of nystagmus. Int J Otolaryngol. 2011;2011:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Selçuk AA. A guide for systematic reviews: PRISMA. Turk Arch Otorhinolaryngol. 2019;57(1):57. doi: 10.5152/TAO.2019.4058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thomas DB, Newman‐Toker DE. Diagnosis is a team sport – Partnering with allied health professionals to reduce diagnostic errors. Diagnosi. 2016;3(2):49‐59. doi: 10.1515/DX-2016-0009 [DOI] [PubMed] [Google Scholar]
- 7. Kordi Yoosefinejad A, Siravani F. Semont and epley maneuvers alleviated vertigo in a patient with multiple sclerosis. Health Sci J. 2015;9(4):1. [Google Scholar]
- 8. Musat GC, Musat AAM. Multiple sclerosis presenting as an anterior Semicircular Canal benign paroxysmal positional vertigo: case report. Ear Nose Throat J. 2021;100(5_suppl):636S‐640S. doi: 10.1177/0145561319897983 [DOI] [PubMed] [Google Scholar]
- 9. Bhattacharyya N, Gubbels SP, Schwartz SR, et al. Clinical practice guideline: benign paroxysmal positional vertigo (Update). Otolaryngol Head Neck Surg. 2017;156(3_suppl):S1‐S47. doi: 10.1177/0194599816689667 [DOI] [PubMed] [Google Scholar]
- 10. Lemos J, Strupp M. Central positional nystagmus: an update. J Neurol. 2021;2021(1):1‐10. doi: 10.1007/S00415-021-10852-8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data (of this patient) generated during this study are included in this published article and its supplementary information files.


