Climate and environmental changes (CECs) constitute a major global health threat. Record temperatures in 2020, as reported in 2021 by the international collaboration, Lancet Countdown, which monitors the health consequences of a changing climate, resulted in increased person-days of heatwave exposure, with serious health consequences, compared with the annual average for the 1986–2005 baseline.1 The world temperature increased 1.2°C compared with the preindustrial period (1850–1900), and the past 7 years have been the hottest 7 years on record.1
Heatwaves and rising mean temperatures present major health problems, especially for populations with limited physiological ability or socioeconomic means to respond or adapt to them. Also in 2020, 84 disasters from floods, droughts, wildfires, and storms affected more than 50 million people. Moreover, the atmospheric concentrations of CO2 are now 50% higher than in the preindustrial era.2 Although energy-related emissions decreased during the COVID-19 pandemic in 2020, emissions have risen again in 2021.3
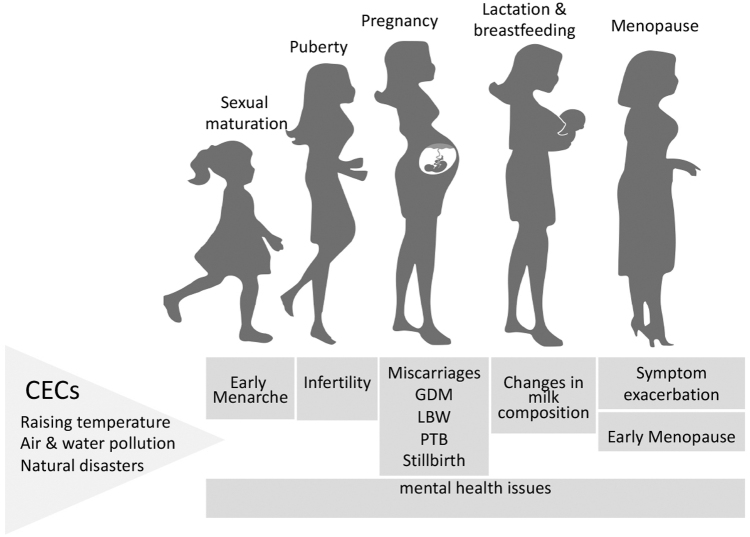
Importantly, the effects of CECs are ubiquitous, ranging from their effects on an individual's internal biology to their effects on a society's external systems. Sexual maturation, fertility, pregnancy and neonatal outcomes, lactation, and menopause (Fig. 1) are subject to short- and long-term negative effects from CECs.
FIG. 1.
Effects of CECs on women's reproductive health (sexual maturation, fertility, pregnancy, lactation, and menopause). CECs, climate and environmental changes; GDM, gestational diabetes; LBW, low birth weight; PTB, preterm birth.
Sexual Maturation and Fertility
In recent years, the global average age for menarche has been declining.4 Importantly, CECs could alter the age of menarche by disrupting food availability, nutritional factors, or through increased toxin/pollutant release.4 Perturbations in the timing of menarche may further affect mental health, fertility-related conditions, cardiovascular disease, and bone health.5 Moreover, an inverse association between mortality and the timing of menarche has been suggested.6
The significant amount of pollutants discharged into the environment due to increasing industrial and agricultural activities is a serious threat for human health. Moreover, several of these synthetic chemicals with long half-life times are classified as potential endocrine-disrupting chemicals (EDCs) and can affect women's reproductive health.7
In addition to the impact of CECs on diet and nutrition, exposure to EDCs has also been associated with early menarche.4 These reproductive toxicants in air pollution can also cause defects during gametogenesis leading to impaired fertility.4 Air pollution may further aggravate asthma,8 which is associated with difficulties in conception.9 EDCs may also adversely affect the ovarian reserve in women and high levels of EDCs have been linked to a decline in ovarian function, infertility, and earlier menopause.10
Pregnancy Outcomes
Pregnant women have been included among the groups most vulnerable to heat stress as the physiological and anatomical changes that occur during pregnancy pose particular challenges to thermoregulation.11 A recent systematic review including a total of almost 33 million births found a significant association between heat, and adverse pregnancy outcomes, preterm birth (PTB), low birth weight (LBW), and stillbirth in the United States.12 It has also been reported that pregnant women who are exposed to higher air pollution levels may be at greater risk for miscarriage, gestational diabetes, PTB, and stillbirths.12,13 Maternal metabolites and metabolic pathways, perturbed by air pollution exposures, may also lead to adverse pregnancy and birth outcomes; thus, they can be considered mediators in the causal pathways.14
Moreover, prenatal maternal stress (PNMS) has an impact on pregnancy outcomes and the offspring's development and lifelong health, and natural disasters contribute to PNMS.15 PTB and neuropsychiatric disorders in the offspring have been associated with PNMS,15 and it is now recognized that maternal stress may be passed on, both intergenerationally and transgenerationally through epigenetic mechanisms.16
CECs also affect the distribution of arthropod-borne, foodborne, and waterborne diseases. Arboviral infections transmitted by mosquitoes, such as dengue, chikungunya viruses, and Zika, may have detrimental effects during pregnancy and may contribute to PTB.17 Zika virus has also been associated with congenital fetal brain abnormalities, including microcephaly.17 Moreover, increased temperatures and rainfall increase the length of the transmission season for parasites with deleterious effects in pregnancy such as Plasmodium falciparum. Pregnant women infected with malaria show not only higher rates of miscarriage, intrauterine fetal death, PTB, LBW neonates, and neonatal death, but also have a higher risk for severe anemia and maternal death.18 Higher temperatures may further increase the risk of cholera and other infections caused by Vibrio bacteria as well as leptospirosis with negative clinical consequences.
Lactation and Breastfeeding
In contrast with infant formula, which has a standardized composition, human milk composition changes dynamically throughout the day and throughout gestation. Importantly, human milk can contain environmental pollutants,19 and pollutants with lipophilic properties may have serious effects when absorbed in the neonate digestive track; the presence of heavy metals in human breast milk has been associated with abnormal immune function in the neonate and allergy, endocrine disorders, neurodevelopment delay, and neuropsychiatric disorders later in life.20
However, it is important to note that the American Academy of Pediatrics and World Health Organization still recommend breastfeeding for at least the first 6 months of life. Breastfeeding is not only beneficial for the mother and neonate but also for the environment, minimizing the impact on the earth's resources. Specifically, breastfeeding uses less water or land resources, produces no carbon emissions, and generates minimal or zero waste. To put things in perspective, breastfeeding for 6 months saves an estimated 95–153 kg CO2 equivalents per baby compared with infants fed with formula.21 In the United Kingdom alone, the carbon emission savings gained by supporting mothers to breastfeed has been equated to taking between 50,000 and 77,500 cars off the road each year.22
Menopause
CECs increase the exposure of women to EDCs resulting in a decline in ovarian function and earlier menopause.10 Specifically, individuals with higher levels of EDCs experience menopause 1.9–3.8 years earlier than women with lower levels of these chemicals.23 EDC-exposed women are also up to six times more likely to be menopausal than nonexposed women of same age.23 Interestingly, CECs may also affect menopause by exacerbating and increasing the duration of symptoms, specifically hot flashes.24
Conclusions
The current climate crisis is threatening global health and disproportionally affects disadvantaged communities. The literature in this space is increasing and opportunities for novel research exist. Importantly, CECs not only negatively impact many stages of a woman's reproductive life but also impact the health of future generations. The impact of CECs on reproductive health can no longer be ignored. Interventions to mitigate CECs are critical to ensuring the future health of women and children worldwide.
Disclaimer
The contents of this article represent the authors' views and do not constitute an official position of the National Institutes of Health or the U.S. Government.
References
- 1. Romanello M, McGushin A, Di Napoli C, et al. The 2021 report of the Lancet Countdown on health and climate change: Code red for a healthy future. Lancet 2021;398:1619–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Met Office. Mauna Loa carbon dioxide forecast for 2021. 2021. Available at: https://www.metoffice.gov.uk/research/climate/seasonal-to-decadal/long-range/forecasts/co2-forecast-for-2021 Accessed February 7, 2022.
- 3. Le Quéré C, Jackson RB, Jones MW, et al. Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement. Nat Clim Chang 2020;10:647–653. [Google Scholar]
- 4. Canelón SP, Boland MR. A systematic literature review of factors affecting the timing of Menarche: The potential for climate change to impact women's health. Int J Environ Res Public Health 2020;17:1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Šaffa G, Kubicka AM, Hromada M, Kramer KL. Is the timing of menarche correlated with mortality and fertility rates? PLoS ONE 2019;14:e0215462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liang Z, Ma H, Song Q, et al. Joint associations of actual age and genetically determined age at menarche with risk of mortality. JAMA Netw Open 2021;4:e2115297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kumar M, Sarma DK, Shubham S, et al. Environmental endocrine-disrupting chemical exposure: Role in non-communicable diseases. Front Public Health 2020;8:553850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tiotiu AI, Novakova P, Nedeva D, et al. Impact of air pollution on asthma outcomes. Int J Environ Res Public Health 2020;17:6212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Esfandiari N, Nesbit C, Litzky J, et al. High prevalence of allergy in patients undergoing in vitro fertilization and embryo transfer. J Assist Reprod Genet 2020;37:311–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Patel S, Zhou C, Rattan S, Flaws JA. Effects of endocrine-disrupting chemicals on the ovary. Biol Reprod 2015;93:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Konkel L. Taking the heat: Potential fetal health effects of hot temperatures. Environ Health Perspect 2019;127:102002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bekkar B, Pacheco S, Basu R, DeNicola N. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: A systematic review. JAMA Netw Open 2020;3:e208243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tan Y, Yang R, Zhao J, Cao Z, Chen Y, Zhang B. The associations between air pollution and adverse pregnancy outcomes in China. Adv Exp Med Biol 2017;1017:181–214. [DOI] [PubMed] [Google Scholar]
- 14. Inoue K, Yan Q, Arah OA, et al. Air pollution and adverse pregnancy and birth outcomes: Mediation analysis using metabolomic profiles. Curr Environ Health Rep 2020;7:231–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. King S, Dancause K, Turcotte-Tremblay AM, et al. Using natural disasters to study the effects of prenatal maternal stress on child health and development. Birth Defects Res C Embryo Today 2012;96:273–288. [DOI] [PubMed] [Google Scholar]
- 16. Franklin TB, Russig H, Weiss IC, et al. Epigenetic transmission of the impact of early stress across generations. Biol Psychiatry 2010;68:408–415. [DOI] [PubMed] [Google Scholar]
- 17. O'Kelly B, Lambert JS. Vector-borne diseases in pregnancy. Ther Adv Infect Dis 2020;7:2049936120941725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schantz-Dunn J, Nour NM. Malaria and pregnancy: A global health perspective. Rev Obstet Gynecol 2009;2:186–192. [PMC free article] [PubMed] [Google Scholar]
- 19. Pajewska-Szmyt M, Sinkiewicz-Darol E, Gadzała-Kopciuch R. The impact of environmental pollution on the quality of mother's milk. Environ Sci Pollut Res 2019;26:7405–7427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Samiee F, Vahidinia A, Taravati Javad M, Leili M. Exposure to heavy metals released to the environment through breastfeeding: A probabilistic risk estimation. Sci Total Environ 2019;650(Pt 2):3075–3083. [DOI] [PubMed] [Google Scholar]
- 21. Karlsson JO, Garnett T, Rollins NC, Röös E. The carbon footprint of breastmilk substitutes in comparison with breastfeeding. J Clean Prod 2019;222:436–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Joffe N, Webster F, Shenker N. Support for breastfeeding is an environmental imperative. BMJ 2019;367:l5646. [DOI] [PubMed] [Google Scholar]
- 23. Grindler NM, Allsworth JE, Macones GA, Kannan K, Roehl KA, Cooper AR. Persistent organic pollutants and early menopause in U.S. women. PLoS One 2015;10:e0116057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Smith JN, van Daalen KR, Venkatraman R. Climate change and its potential impact on menopausal hot flashes: A commentary. Menopause 2020;27:816–817. [DOI] [PubMed] [Google Scholar]