Abstract
Background:
Hospice care in rural areas is often characterized by provider shortages and vast geographical service areas to cover, making access to quality end-of-life care challenging. Telemedicine, broadly, is the utilization of interactive televideo (ITV) technology to provide health services over a distance. For over 25 years, telemedicine has been proposed as a solution to address access issues. In 2015, the University of Kansas Medical Center (Kansas City, Kansas) partnered with Hospice Services, Inc. (HSI) (Phillipsburg, Kansas), to augment traditional, face-to-face (FTF) hospice care with hospice care delivered through mobile tablets.
Objective:
This work examines the costs of TeleHospice (TH) (telemedicine use in hospice care) when compared with the costs of FTF hospice services.
Design:
Detailed administrative data from July 1, 2018, to December 31, 2018, were analyzed to estimate the costs of service after TH use was inculcated into routine practice.
Results:
his, which averages a daily census of 34 patients, conducted 257 calls, averaging 28 hours a month. The average time for a TH call was 18 and 17 minutes for nursing and medical director calls, respectively. Through various hospice functions, including administrative, patient, and nonpatient-related connections, HSI saved over $115,000 in staff travel time and mileage reimbursement. Administratively, by hosting their weekly 15-member interdisciplinary meeting through ITV, HSI saved $29,869 of staff travel time and mileage reimbursement.
Conclusions:
Our estimates indicate substantial cost saving potential with the use of TH services. Further research is needed to assess the effects of TH utilization on the experiences and subsequent cost of hospice care.
Keywords: care delivery, cost savings, telehospice, telemedicine
Introduction
Hospice care is a team-oriented, interdisciplinary approach designed to provide quality end-of-life care for individuals facing life-limiting illness and/or injury. A team of physicians, nurses, social workers (SWs), chaplains, and volunteers work together to provide medical care and emotional support tailored to fit the needs of patients and their families through the final stages of life.1 Over the past few decades, hospice programs in the United States have expanded in an effort to meet the ever-increasing number of patients who seek hospice and palliative care services.2 However, while urban programs have expanded in efforts to serve the increasing number of patients, those in rural areas have not been able to do so, for a number of reasons.
When examining accessibility to end-of-life care, individuals in rural areas continue to face significant access barriers when compared with urban populations. This is particularly concerning for rural patients, as they are disproportionately older, sicker, and of lower economic status.3,4 In 2007, there were 965 rural hospices; as of 2017, the number has decreased to 878.5 Also, nearly 80% of hospice programs are in urban areas, and there are fewer hospice providers in rural communities when compared to urban areas.3,5,6
In addition to a lack of access to hospice programs and providers for rural populations, geographical challenges also exist. Rural and frontier hospice programs typically cover a vast service area, oftentimes making it necessary for providers to drive long distances to care for a single patient. While rural programs on average serve a smaller census,3 the expansiveness of their catchment area creates significant challenges regarding cost, safety, and frequency of access.4 In addition, with unpredictable weather and, in turn, poor road accessibility a common obstacle, concerns regarding access and financial limitations can become burdensome for rural hospice programs.3,4 When considering reimbursement, which is adjusted using the hospice wage index, rates are typically lower for rural hospice programs, as travel expenses are not considered in the reimbursement formula.3,7,8 In a discipline that provides care 24 hours a day, seven days a week, travel time and the associated costs can be taxing. Clearly, we need to identify innovative ways of providing hospice care in the rural sector, given the significant provider shortage issues and unique costs incurred when providers travel long distances to provide care.
Over the past two decades, telemedicine—the utilization of telecommunication technologies to provide real-time interactive televideo (ITV) communication over a distance9—has been widely viewed as a solution to access barriers for patients in the rural sector.10,11 Telemedicine technology utilizes ITV equipment, which expands the communication capabilities between providers and patients when care is being provided from a distance. Telemedicine may be used to improve patients' access to care, regardless of location, while creating a more connected level of care among patients and the interdisciplinary team (IDT).10,12 Significant improvements in technology coupled with the ubiquity of the wireless phone service has allowed for the use of telemedicine in the care of rural hospice patients, known as TeleHospice (TH).13,14
The TH Program
In 1998, researchers at the University of Kansas Medical Center (KUMC) piloted the first TH program in the United States, designed to augment end-of-life care for patients in both rural and urban settings.15,16 Videophone technology was used to conduct TH visits for immediate hospice evaluations along with traditional, face-to-face (FTF) hospice care. Valuable lessons were learned from this program regarding clinical usage of the technology, requirements to sustain the service, and adoption of the technology by staff and patients. While this study was a success in numerous aspects, the program was eventually discontinued after several years due to technology constraints, as early telecommunication devices were not as prevalent, affordable, and easy to use as services available today. The lessons learned in this early rendition of the service helped shape the eventual launch of an updated TH program currently underway today.
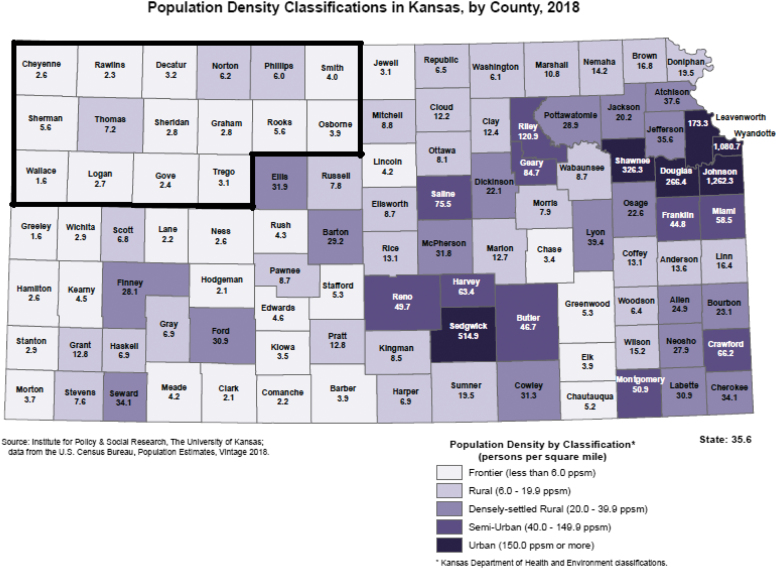
In 2015, a new TH program was launched to enhance hospice and palliative care delivery in rural and frontier communities in northwest Kansas. With advances in technology, improved cellular data service in rural areas, a more technologically advanced society, and a higher degree of technological acceptance and use in medicine, an opportunity to reexamine the potential of TH emerged. Understanding these advances along with previous lessons learned in the prior TH programs, staff from KUMC sought to identify a partner to examine the role of TH in rural hospice care. Hospice Services, Inc. (HSI), a not-for-profit, community-based organization serving rural and frontier counties in northwest and north central Kansas, was selected to partner with KUMC for the program. HSI serves a span of over 15,000 square miles, including 16 counties, three of which are classified as rural (population between 6 and 19.9 people/square mile) with the rest categorized as frontier counties (<6/square mile) (Fig. 1).17
FIG. 1.
Population density classifications of the Hospice Services, Inc., Service Area.
For the 2015 launch, iPads were selected to conduct videocalls for HSI and their patients. HSI was provided 18 iPads, all of which were equipped with unlimited cellular data through a commercial provider. Zoom video conferencing service was selected for TH connections, as it provides a secure, cloud-based platform that can be downloaded and readily available for staff members' and/or patients' mobile tablets, cellular phones, laptops, or desktops. Zoom allows direct videocalling for unscheduled encounters, offers the ability to join an ongoing meeting, and is HIPAA compliant—all reasons that factored into the service being selected for the TH program. All staff and patients were provided with a Zoom Pro account, which allows unlimited call times with unlimited participants.
Education and training for use of the iPads and Zoom were implemented throughout the early phases of the 2015 TH program. Continued practice and demonstrations were performed throughout the study to encourage utilization and help HSI staff feel more comfortable with training and educating patients who had iPads placed in their home. Providing regular education around the use of the Zoom application for participants was critical in helping HSI staff adapt to the technology. Protocol and implementation phases are further detailed in previous TH publications (Fig. 2).14
FIG. 2.
TeleHospice researcher conducting a visit.
Over the past four years, KUMC's partnership with HSI has focused on quality improvement in hospice care delivery. Individual staff received iPads, and based upon availability, hospice patients were offered TH service at entry to hospice. The number of clients/caregivers who rejected the service was less than 10%; thus, at any given time, 9 or 10 iPads were deployed to patients' homes or care setting. This partnership, along with other documented TH studies, has shown the feasibility of TH technology to enhance access to care, while still upholding, and even expanding, the strong quality standards, which hospices strive to achieve.14 However, while some early studies have demonstrated potential cost savings through the use of TH in comparison with in-person visits,16,18–20 more up-to-date research is needed to assess expenses when using current technology in hospice care. This article explores the cost of TH visits in relation to traditional in-person provider visits and potential savings in rural hospice care. Having worked through issues necessary to launch a TH service, and given the routine use of TH over a four-year period by HIS staff, and recognizing up-to-date numbers regarding expenses due to TH have not been reported, in 2018, the authors set out to perform a cost study of TH services designed to serve patients living in northwestern Kansas.
Methods
Calculations of expenses related to TH calls were tracked as those costs related to staff time and technology as was needed to conduct a single TH visit. The KUMC IRB approved the quality improvement determination for this study.
HSI staff
Between July 1, 2018, and December 31, 2018—the period of time during which data were collected for this study—HSI employed 15 people: one executive director, one medical director (MD), five nurses, one licensed practical nurse, two SWs, one bereavement coordinator, one pastor, and three administrative staff. In addition, a wound specialist was regularly consulted on a contractual basis. Administrative data obtained detailed information, including staff hourly wages and benefits (25%) and the base location from which each staff member worked.
Technology-related expenses
As previously mentioned, mobile tablets (iPads) were used for TH connections due to popularity, low cost, ease of use, and strong audio/video quality. KUMC purchased 18 iPads at $715 each, resulting in a total cost of $12,870. Each iPad came equipped with its own unlimited cellular data plan at a cost of $40 a month, resulting in a cost of $4,320 for cellular service during the six-month study period. Auxiliary equipment such as charger adapters, charging cables, and iPad cases were purchased as well. These items cost $42, $60, and $270, respectively.
TH visits
A compilation of HSI's administrative data, HSI's electronic health record data, Zoom data, and RedCap surveys was analyzed by the study team to obtain expenses related to a TH visit. Zoom data were captured from a Zoom-generated report, which detailed dates of service, length of call, and number of participants in each video visit. RedCap, a secure, web-based application built to capture electronic data for research purposes,21 was used to collect specific details regarding each TH call, including patient location, round-trip mileage that would have been incurred had the patient been seen in-person—which could vary based upon staff member location, and the total time of the TH visit.
Costs of conducting a TH call
In calculating the cost-per-TH call, Zoom, which provides a report detailing the length of the videocall along with who participated, was analyzed to determine TH videocall usage per staff member. In efforts to determine the cost, each staff members' calls and subsequent minutes were used to determine the average length of time per TH videocall per discipline. With the average call time determined, each discipline's average hourly pay rate plus benefits (25%) were then used to calculate the average cost-per-TH call. In addition, total costs related to the use of TH equipment were calculated per call, including iPads and the monthly data use plans.
Modeling of costs of FTF visit if conducted instead of a TH visit
Costs were calculated by determining the staff member's round-trip mileage from their base location in relation to the patient's location, and then, using the IRS reimbursement rate of $0.54/mile, a cost-per-trip based on mileage was determined. Next, travel time was determined by using the round-trip mileage along with a time constant of 50 mph. From that, a cost was determined for windshield time by taking the round-trip time at 50 mph and calculating it with the particular staff member's hourly rate plus benefits (25%). Once this was complete, the cost saved for both mileage reimbursement and travel time was put together to determine the overall amount saved per staff member when conducting a TH videocall, as opposed to an in-person visit.
Actual expenses related to FTF visits during the study period
The cost-per-FTF visit was derived from HSI's Medicare cost report, which is submitted to the Centers for Medicare and Medicaid Services (CMS). This report incorporates all aspects of the F2F visit, including travel to and from the patient's location, and represents the average cost-per-F2F for the period from July 2018 to June 2019. The data for FTF visits are presented below as listed in the Medicare cost report.
Results
Over the course of the six months, the average daily census for HSI was 34 patients, with 6200 total patient-days of care. For all disciplines, 2767 FTF home visits occurred. On average, nurses, SWs, and the MD conducted 363, 94, and 5 FTF visits per month, respectively. Nurse visits lasted on average 54 minutes; SW visits lasted on average 65 minutes; and MD visits averaged 17 minutes. These visits were the result of routine care and symptom management and met regulatory requirements for Medicare. Based on the Medicare time cost report for HSI, the average cost-per-FTF visit for the three disciplines was $209 (nurses), $295 (SWs), and $542 (MD). The average cost-per-FTF visit across all disciplines was $349.
During the same six-month period, a total of 123 patient-related TH videocalls were completed with staff members connecting with the patient, family, and/or caregiver—far fewer than the above stated FTF visits. There was no “requirement” for providers to make videocalls versus in-person visits. The decision to use TH was left up to the discretion of the provider. (The time of this study was before COVID 19, and all providers still wanted to make in-person visits with some degree of regularity, and to meet hospice Medicare guidelines.) The most common purposes for videocalls included the following: emergent calls from patients, check-in calls throughout the week, bereavement visits, and hospice MD visits. Details regarding the 123 patient-related TH videocalls are documented in Table 1.
Table 1.
Cost Data for Face-to-Face Visit and TeleHospice Videocalls
| Discipline | Face-to-face (data from EHR) |
TeleHospice (data from Zoom) |
||||
|---|---|---|---|---|---|---|
| Visits | Minutes per visit (AVG) | Cost per visita | Calls | Minutes per call (AVG) | Cost per call | |
| RN + LPN | 2176 | 54 | $209 | 26 | 18 | $9 |
| SW | 563 | 65 | $295 | 55 | 16 | $8 |
| MD | 28 | 17 | $542 | 42 | 17 | $52 |
Obtained from HSI's Medicare cost report to CMS.
AVG, average; CMS, Centers for Medicare and Medicaid Services; EHR, electronic health record; FTF, face-to-face; MD, medical director; RN, registered nurse; LPN, licensed practical nurse; SW, social worker.
Modeling of costs of FTF visit if conducted instead of a TH visit
If the 123 TH videocalls had been conducted in person, travel time and mileage reimbursement expenses would have totaled $46,752 based on each staff's hourly rate plus benefits (25%). The MD alone would have incurred $34,045 of that total. Each discipline saved $174 (nurses), $149 (SWs), and $811 (MD) per TH videocall based on their lack of travel. Altogether, this resulted in an average saving of $378/patient-related TH videocall.
When examining savings based on the cost-per-FTF visit as determined by the Medicare cost report, if the 123 TH visits had been conducted FTF, a cost of $44,423 would have occurred. Per discipline, the potential FTF cost-per-visit totals would have been $5,434 (26 in-person nursing visits), $16,225 (55 in-person SW visits), and $22,764 (42 in-person MD) (Table 1). Again, we emphasize the activities of an in-person visit are not comparable to those of a TH visit.
Cost savings for expenses related to administrative meetings
Along with the potential savings for patient-centered hospice care, additional cost savings were noted for administrative meetings. HSI conducts weekly IDT meetings in which all staff participate. With HSI's vast service area, meeting in person once a week is costly. However, implementation of the TH technology enabled HSI staff to participate in IDT meetings through Zoom. During the study, HSI saved nearly $30,000 by conducting IDT meetings through videocall, which is an average monthly savings of $5,000 or $1,195 per IDT meeting.
In addition to the IDT meetings, savings were noted for other nonpatient, administrative meetings such as board, executive, and quality improvement meetings. Savings of more than $38,500 were calculated for the 46 meetings of this type, which also took place through Zoom, resulting in an average savings of $837 per miscellaneous administrative videocall. These savings were calculated like other patient-related cost savings, where staffs' round-trip mileage to the home office along with their hourly rate plus benefits (25%) was used to determine travel time and mileage reimbursement saved.
In summary, including all patient-related, nonpatient-related, and administrative savings, HSI saved an average of ∼$19,200/month in mileage reimbursement and travel time. Throughout the study period from July through December 2018, if all TH videocalls, both patient related and nonpatient related, would have taken place in person, HSI would have spent $115,203 (which would represent about 5% of the total HIS budget) in travel time and mileage reimbursement for their staff. Comparatively, when using the cost-per-visit as determined in HSI's Medicare cost report to CMS, if the 123 TH calls would have been FTF visits, a saving of $44,423 would have occurred.
Discussion
Hospice care in the rural setting has consistently been challenged by diminishing numbers of providers, access barriers, geographical constraints, and financial obstacles. With the Medicare reimbursement structure not factoring in distance and travel time, rural hospice programs are commonly faced with significant financial constraints unique to their location. These barriers, while substantial, are not impossible to overcome. Services like TH may be used to facilitate quality virtual visits, all while minimizing cost and obviating the need for travel.
The largest cost per visit (either TH or FTF) was incurred by the hospice MD. It must be emphasized the MD visits conducted in person were much more expensive than TH—due to travel-related expenses. Clearly, TH allows for virtual physician visits at a relatively low cost when compared to FTF—and the expense per video visit will drop precipitously if TH visits can be substituted for those in person. Stated differently, many more MD visits may occur without the significant travel costs related to in-person visits.
It must be emphasized that virtual calls are not an equivalent service when compared to FTF visits. (The content of videocalls compared with in-person visits is the subject of an ongoing study.) TH may be used as an adjunct to FTF visits in efforts to meet the standard of care hospice programs provide, but they are not a substitution for in-person visits. Common ways in which HSI has implemented TH include the following: staff to staff utilization, patient to staff (whether emergent or check-in) connections, staff to care facility connections, patient to family visits, and staff/family meetings where, for example, distant family and additional staff members can be part of an admission visit. While each organization has its own unique needs, TH has the capability to facilitate quality video and audio communication, and may offer cost savings, particularly for hospice programs in rural areas.
Services like TH can be an effective, cost-friendly form of communication for hospice providers. The ability of TH to offer a virtual connection that allows a provider or family member to physically visualize a patient at any time may facilitate a more advanced level of care among patients, families, and the IDT. This service can prove to be critical for rural care teams faced with unique challenges both geographically and financially in providing care. The ability for TH to assist hospice organizations in meeting standards of care along with Medicare requirements is significant, especially when used in conjunction with traditional, home hospice care. Further research examining cost and quality measures will help to not only standardize the practice but also establish TH as a capable tool in providing care, whether in rural or urban communities.
Funding Information
No funding supported this work.
Author Disclosure Statement
No competing financial interests exist.
Parts of this study have been presented in poster form at the 2019 American Society of Clinic Oncology Annual Conference.
References
- 1. Hospice Care. National Hospice and Palliative Care Organization. https://www.nhpco.org/about/hospice-care (Last accessed March 26, 2019).
- 2. Facts on Hospice and Palliative Care. National Hospice and Palliative Care Organization. https://www.nhpco.org/hospice-statistics-research-press-room/facts-hospice-and-palliative-care (Last accessed March 26, 2019).
- 3. Research on Hospice Care in Rural Areas. National Hospice and Palliative Care Organization (NHPCO). https://www.nhpco.org/sites/default/files/public/newsline/2015/Summer2015_NL.pdf. 2015. (Last accessed March 26, 2019).
- 4. Baernholdt M, Campbell CL, Hinton ID, et al. : Quality of hospice care: Comparison between rural and urban residents. J Nurs Care Qual 2015;30:247–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Medicare Payment Advisory Commission (MedPac). Report to Congress: Medicare Payment Policy March 2019 (pp. 311–340). www.medpac.gov/-documents-/reports. 2019. (Last accessed March 26, 2019).
- 6. Campbell CL, Merwin E, Yan G: Factors that influence the presence of a hospice in a rural community. J Nursing Scholars 2009;41:420–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Casey MM, Moscovice IS, Virnig BA, Durham SB: Providing hospice care in rural areas: Challenges and strategies. Am J Hosp Palliat Med 2005;22:363–368. [DOI] [PubMed] [Google Scholar]
- 8. US Department of Health and Human Services, Centers for Medicare and Medicaid Services: Medicare Program; Hospice Wage Index Fiscal Year 2019; Notice. Fed Regist 2018;83:38622–38655.30080351 [Google Scholar]
- 9. Telemedicine. Medicaid.gov. https://www.medicaid.gov/medicaid/benefits/telemed/index.html. (Last accessed March 29, 2019).
- 10. Alvandi M: Telemedicine and its role in revolutionizing healthcare delivery. The American Journal of Accountable Care. https://www.ajmc.com/journals/ajac/2017/2017-vol5-n1/telemedicine-and-its-role-in-revolutionizing-healthcare-delivery?p=2. 2017. (Last accessed February 27, 2021).
- 11. Oliver DP, Demiris G, Wittenberg-Lyles E, et al. : A systematic review of the evidence base for telehospice. Telemed E Health 2012;18:38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Henderson K, Davis TC, Smith M, King M: Nurse practitioners in telehealth: bridging the gaps in healthcare delivery. J Nurse Pract 2014;10:845–850. [Google Scholar]
- 13. Davis MS, Harrison KL, Rice JF, et al. : A model for effective and efficient hospice care: Proactive telephone-based enhancement of life through excellent caring, “TeleCaring” in advanced illness. J Pain Symptom Manag 2015;50:414–418. [DOI] [PubMed] [Google Scholar]
- 14. Doolittle GC, Nelson E-L, Spaulding AO, et al. : TeleHospice: A community-engaged model for utilizing mobile tablets to enhance rural hospice care. Am J Hosp Palliat Med 2019;36:795–800. [DOI] [PubMed] [Google Scholar]
- 15. Doolittle GC, Yaezel A, Otto F, Clemens C: Hospice care using home-based telemedicine systems. J Telemed Telecare 1998;4(1_suppl):58–59. [DOI] [PubMed] [Google Scholar]
- 16. Doolittle GC: A cost measurement study for a home-based telehospice service. J Telemed Telecare 2000;6(1_suppl):193–195. [DOI] [PubMed] [Google Scholar]
- 17. Population density classifications in Kansas by county. Institute for Policy & Social Research, The University of Kansas. www.ipsr.ku.edu/ksdata/ksah/population/popden2.pdf. 2018. (Last accessed February 27, 2021).
- 18. Doolittle GC, Spaulding AO, Williams AR: The decreasing cost of telemedicine and telehealth. Telemed E Health 2011;17:671–675. [DOI] [PubMed] [Google Scholar]
- 19. Doolittle GC, Whitten P, Mccartney M, et al. : An empirical chart analysis of the suitability of telemedicine for hospice visits. Telemed E Health 2005;11:90–97. [DOI] [PubMed] [Google Scholar]
- 20. Doolittle GC, Williams AR, Spaulding A, et al. : A cost analysis of a tele-oncology practice in the United States. J Telemed Telecare 2004;10(1_suppl):27–29. [DOI] [PubMed] [Google Scholar]
- 21. Harris PA, Taylor R, Thielke R, et al. : Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]