Abstract
Background.
Colorectal cancer screening (CRCS) rates remain suboptimal among Korean Americans despite recommendations from health organizations. Little is known about the mechanism underlying their CRCS adoption within complex systems. This study aimed to examine the multi-level predictors of CRCS adoption among Korean Americans using a decision tree model.
Methods.
A cross-sectional survey was performed to assess CRCS adoption and multiple levels of influence—individual (i.e., CRCS self-efficacy, CRCS attitudes, risk of colorectal cancer, psychological distress, health status), interpersonal (i.e., social support, social networks, CRCS recommendations), and organizational/community (i.e., health insurance, primary doctor, primary clinic) factors. A total of 433 Korean Americans aged 50 to 75 in a metropolitan area in the Southeastern U.S. completed a self-report questionnaire. To determine the important variables that predict CRCS adoption, the study generated a decision tree predictive model using R statistical software.
Results.
The results indicated that CRCS self-efficacy and CRCS attitudes at the individual level and CRCS recommendations and social support at the interpersonal level differentiate adopting or not adopting CRCS. Furthermore, CRCS recommendations (n = 138, 56%, prob = 0.64) and CRCS self-efficacy (n = 51, 21%, prob = 0.88) were the most powerful predictors of CRCS adoption.
Conclusion.
The findings highlight the critical roles of CRCS recommendations from healthcare providers and family/friends and patients’ confidence in performing screening-related tasks in influencing CRCS adoption among Korean Americans. Practice efforts should target individual and interpersonal characteristics when developing interventions for promoting CRCS among Korean Americans especially who are not adherent to screening guidelines.
Keywords: Colorectal Cancer Screening, Decision Tree Model, Social Ecological Model, Screening Adoption, Korean Americans
Introduction
Colorectal cancer is the third most frequent cancer and the third leading cause of death for men and women in the U.S. (American Cancer Society 2021). Nearly 90% of new colorectal cancer cases occurred in people aged 50 or older (Siegel, Miller, and Jemal 2017). Since the introduction of colorectal cancer screening (CRCS) in the U.S. in the 1960s, colorectal cancer incidence and mortality both have steadily declined, especially over the past two decades (Doubeni 2014). Research estimates that CRCS accounts for a more than 50% reduction in the incidence and mortality (Issa and Noureddine 2017). Health organizations recommend regular CRCS for average-risk individuals aged 50 to 75 (US Preventive Services Task Force 2018). The common recommendation includes a stool-based blood test annually, sigmoidoscopy every five years, and colonoscopy every ten years (US Preventive Services Task Force 2018).
Despite such recommendation, CRCS rates remain low for the general U.S. population and far lower for historically underrepresented racial and ethnic groups in the U.S (Jackson et al. 2016; Young et al. 2019). Specifically, a systematic review indicated that only 25–50% of Korean Americans had undergone CRCS, which is significantly below the national goal of 74.4% set by Healthy People 2030 (Oh and Jacobsen 2014; U.S. Department of Health and Human Services 2021). For Korean Americans, colorectal cancer incidence and mortality have increased and persisted, respectively (Kohler et al. 2015), becoming the second most commonly diagnosed cancer and the leading cause of death (Sabado et al. 2015).
Literature has shown that underutilization of CRCS for Korean Americans is associated with multi-faceted factors. Sociodemographic characteristics that include younger age (Jo et al. 2008), being single (Juon et al. 2003), poor education attainment (Kim et al. 1998), and low income (H. Y. Lee and Im 2013) were connected with suboptimal CRCS for Korean Americans. As for cognitive and psychosocial attributes, Korean Americans with low CRCS self-efficacy (Werk, Hill, and Graber 2017), negative attitudes toward CRCS (Carney et al. 2014), low perceived risk of colorectal cancer (Jung et al. 2017), high levels of psychological distress (Myong, Shin, and Kim 2012), poor health status (Juon et al. 2003), lack of social support (Oh and Jacobsen 2014), and limited social networks (Jo et al. 2008) were likely to report low rates of CRCS. In addition, structural factors that include inadequate health insurance (Ryu, Crespi, and Maxwell 2014), limited access to primary healthcare sources (Tran et al. 2018), and the lack of receiving CRCS recommendations (S. Y. Lee 2018; Maxwell et al. 2010) impeded Korean Americans from utilizing CRCS.
While the literature has contributed to identifying the correlates of CRCS among Korean Americans, further studies are warranted because CRCS adoption is influenced by a combination of multiple correlates and their interactions with one another within multi-level systems (Brittain and Murphy 2015; Pruitt et al. 2014). In order to better understand how Korean Americans make a decision of CRCS uptake, the present study employed the decision tree predictive model as an analytical approach and the social ecological model as a theoretical framework.
Theoretical Framework
The social ecological model posits that individuals embedded within larger social systems interact with their environments with mutual influences on health outcomes (Golden and Earp 2012). In this study, the social ecological model consisted of the three levels of influence—individual (i.e., CRCS self-efficacy, attitudes toward CRCS, perceived risk of colorectal cancer, psychological distress, and self-rated health status), interpersonal (i.e., social support, social networks, and CRCS recommendations), and organizational/community (i.e., health insurance, primary clinic, and primary doctor) factors (see Figure S1). Also, the decision tree model is a data mining and classification tool which has been used to examine the diagnosis of medical conditions and decisions for cancer screenings (Dominick et al. 2015; Song and Lu 2015). In this study, the decision tree model allowed for specifying factors that differentiate the CRCS adoption groups, calculating the importance of a given factor in estimating CRCS adoption, and offering an easy-to-interpret visual representation of prediction rules (Morris and Perna 2018).
Drawing on the social ecological framework, the present study aimed to investigate the important predictors of CRCS adoption among Korean Americans using the decision tree predictive model. To this end, this study proposed the following research questions:
What are the important individual-level predictors of CRCS adoption among Korean Americans?
What are the important interpersonal-level predictors of CRCS adoption among Korean Americans?
What are the important organizational/community-level predictors of CRCS adoption among Korean Americans?
Which variable has the greatest predictive power to forecast CRCS adoption?
The findings of this study benefit the field by providing implications and guidelines for health professionals and policy makers in developing evidence-based interventions targeted to effectively engage Korean Americans to adopt CRCS.
Methods
Research Design and Data Collection
We conducted a cross-sectional, quantitative study and performed convenience sampling to recruit Korean Americans from May 2015 to February 2016. Inclusion criteria were individuals who self-identified as Korea American, aged 50 to 75, and resided in a metropolitan area in the Southeastern U.S. For recruitment, we developed a list of Korean community organizations, including senior centers, churches/temples, and associations, and then contacted each organization via phone or email. We administered self-report questionnaires at organizations which agreed to participate. Prior to each session, we explained the nature and purpose of the study and administered informed consent among those who were interested in the study. We translated all measures in English into Korean using back-translation. Three bilingual Korean Americans from a local university and community reviewed the translations. We pilot-tested the Korean-translated questionnaire with six Korean American men and women to obtain and integrate their feedback. An institutional review board approved this study.
Measures
The outcome variable for this study was receipt of CRCS (i.e., CRCS adoption): a fecal occult blood test (FOBT), sigmoidoscopy, or colonoscopy. We assigned CRCS receipt as a dummy variable with a value of 1 if the respondent had ever had any of the three screening modalities or a value of 0 if otherwise. In the receipt of CRCS, we did not assess the particpant’s screening schedule status. For the predictors (i.e., input variables), building on existing literature, we employed 11 variables to determine the most influential factors that lead to adoption of CRCS. Guided by the social ecological framework, we classified the 11 critical elements of CRCS as either individual, interpersonal, or organizational/community factors. The individual factors included CRCS self-efficacy, CRCS attitudes, risk of colorectal cancer, psychological distress, and self-rated health status. The interpersonal factors included social support, social networks, and CRCS recommendations from social networks (i.e., doctors, family, relatives, and friends). Lastly, the organizational/community factors comprised primary clinic, primary doctor, and health insurance.
Individual factors
CRCS self-efficacy.
We adopted 12 items of self-efficacy for CRCS from Luszczynska and Schwarzer (Luszczynska and Schwarzer 2003) to measure CRCS self-efficacy. This self-efficacy measure consisted of three subscales for FOBT, sigmoidoscopy, and colonoscopy with four items each on a seven-point Likert scale ranging from ‘strongly disagree’ (= 1) to ‘strongly agree’ (= 7). A sample item is: “I am able to perform FOBT regularly even if I will have to make a detailed plan describing how to remember about the test.” Higher scores of CRCS self-efficacy denote greater abilities of executing CRCS.
CRCS attitudes.
We measured attitudes toward CRCS using an adapted version of seven-item positive decisional balance scale developed by Costanza and colleagues (Costanza et al. 2005) for each CRCS modality. We computed the sum scores of 7 items for each screening modality (a total of 21 items), with each item having a binary value of 0 (= ‘no’) or 1 (= ‘yes’), and then calculated the overall mean score. A sample item is: “Having regular colonoscopy gives me peace of mind about cancer.” Higher scores of CRCS decisional balance denote greater positive attitudes toward CRCS.
Risk of colorectal cancer.
We also assessed risk of colorectal cancer using three items adopted from Manne and colleagues’ perceived risk of colorectal cancer scale which Schwarts and colleagues had originally developed (Schwartz et al. 1995; Manne et al. 2002). This included a seven-point Likert scale rating personal risk for developing colorectal cancer compared with the average person of the same age (−3 = ‘extremely unlikely,’ 3 = ‘extremely likely’). A sample item is: “Compared to others at your own age, how do you estimate the likelihood that you will ever have a polyp in your colon/rectum?” Higher scores of risk of colorectal cancer denote greater perceived risk of colorectal cancer.
Psychological distress and health status.
Using the Kessler short-form (K6) mental distress scale, we measured non-specific psychological distress within the past month (Kessler et al. 2002). This six-item scale included a response ranging from ‘none of the time’ (= 0) to ‘all of the time’ (= 4). A sample item is: “During the past 30 days, how often did you feel so sad that nothing could cheer you up?” Higher scores denote higher levels of psychological distress. Moreover, we assessed health status with one item of the question, “How do you rate your current health?” and options of ‘very bad’ (= 1), ‘bad’ (= 2), ‘moderate’ (= 3), ‘good’ (= 4), and ‘very good’ (= 5).
Interpersonal factors
Social support.
We measured social support with five items of the Duke University of North Carolina functional social support questionnaire (Broadhead et al. 1988). This scale assessed agreements with statements describing the abilities of having someone to discuss and share important life matters with options on a five-point-Likert scale ranging from ‘much less than I would like’ to ‘as much as I would like.’ A sample item is: “I have people who care what happens to me.” We computed their mean scores, with their higher scores denoting greater perceived social support.
Social networks.
To assess social networks, we asked the number of acquaintances whom the participant could confide in or count on, when the respondent seeks informational (e.g., finding an appropriate doctor), tangible (e.g., taking him or her to the hospital), and emotional (e.g., feeling at ease) supports for health. Each item included options of ‘none’ (= 1), ‘one’ (= 2), ‘two’ (= 3), ‘three or four’ (= 4), ‘five to eight’ (= 5), and ‘nine or more’ (= 6). Higher scores denote a greater number of social networks.
CRCS recommendation.
We also measured receipt of CRCS recommendation for each of the screening modalities from different sources, including doctor, family/relative, or friend, with responses of ‘yes’ (= 0) or ‘no (= 1).’ We computed the sum scores of 3 items for each screening modality (a total of 9 items) and then calculated the overall mean score. Higher scores denote a greater number of recommendations for CRCS.
Organizational/Community factors
We asked if the respondent had a primary clinic, a primary doctor, or health insurance. We used an item for each with options of ‘yes’ or ‘no.’
Cronbach’s alpha coefficients for the seven constructs (CRCS self-efficacy, CRCS attitudes, psychological distress, risk of colorectal cancer, social support, social networks, and CRCS recommendations) ranged from 0.81 to 0.96 (see Table S1). All seven constructs met the minimum criterion of 0.70. Table S2 presents a frequency table for self-rated health status and the organizational/community factors (health insurance, primary clinic, and primary doctor).
Data Analysis
We used Recursive PARTitioning of the multivariable statistical algorithm to grow a decision tree for the CART method (Song and Kim 2018; Therneau et al. 2019). By using a sampling strategy of 70%, 15%, 15%, the system auto-split the full data (n = 353) by partitioning 70% into a training dataset (n = 248), 16% into a validation dataset (n = 56), and 14% into a testing dataset (n = 49).
First, we ran the decision tree with the training dataset (n = 248). To measure the model performance and accuracy, we then conducted an error matrix and analyses of receiver operating characteristics (ROC) on a validation dataset (n = 56) and cross-validated the final model on a testing dataset (n = 49). To get a more stable prediction of the most significant variables, we used Random Forest (RF) algorithms that built an ensemble of 300 decision trees (ntree = 300) (Sauer et al. 2015: Song and Kim 2018). Both the accuracy and Gini measures of the importance of variables are calculated by the RF algorithm in the building of the 300 decision trees. R statistical software was used to generate a decision tree.
Results
Sociodemographic Characteristics
A total of 526 Korean Americans participated in the study, and 433 Korean Americans (82.3%) eligible for this study completed a self-report questionnaire regarding CRCS adoption. Among them, we used 353 responses for the main data analysis after the system deleted 80 observations due to missing values for the outcome variable in the past CRCS receipt (i.e., CRCS adoption) (n = 353). Table 1 presents the sociodemographic characteristics of the respondents. The mean age was 58.5. About 60% were female, almost 40% had an annual household income below $40,000, the majority (83%) were married or partnered, and above half (57%) graduated from college or above.
Table 1.
Demographic profile of respondents (n = 353)
| Variable | |
|---|---|
| Gender | % |
| Male | 39.7 |
| Female | 60.3 |
| Age | Years |
| Mean age | 58.5 |
| Median age | 57.0 |
| Annual household income | % |
| Less than $20,000 | 15.0 |
| $20,000–39,999 | 24.4 |
| $40,000–59,999 | 21.8 |
| $60,000–79,999 | 16.1 |
| $80,000–99,999 | 8.5 |
| $100,000 or more | 6.8 |
| Missing values | 7.4 |
| Marital status | % |
| Single, never married | 1.1 |
| Married or partnered | 83.3 |
| Separated or divorced | 9.3 |
| Widowed | 5.7 |
| Other | 0.3 |
| Missing values | 0.3 |
| Education | % |
| Elementary school graduate | 2.5 |
| Middle school graduate | 2.5 |
| High school graduate | 36.0 |
| Bachelor’s degree | 45.6 |
| Graduate degree | 11.0 |
| Missing values | 2.3 |
Decision Tree Modeling
An optimal decision tree model was generated by the Recursive PARTitioning statistical technique using the training dataset (n = 248). Figure 1 presents the final decision tree consisting of seven terminal nodes (i.e., a node that is not split any further). Three terminal nodes in grey predicted CRCS adoption groups, which was denoted as ‘yes,’ and another four with no fill predicted non-CRCS adoption groups, which was denoted as ‘no.’ The decision tree repeatedly split the training data into smaller subset samples by the cutpoint chosen by the algorithm’s calculation of the entropy of child nodes (Song and Kim 2021). Repeated splits on the same predictor may occur ordinarily in predictive analytics (Song and Kim 2018). As described earlier, greater scores indicated a higher number of recommendations for CRCS, more positive attitudes toward CRCS, greater self-efficacy to execute CRCS, a higher level of perceived social support, etc.
Figure 1.
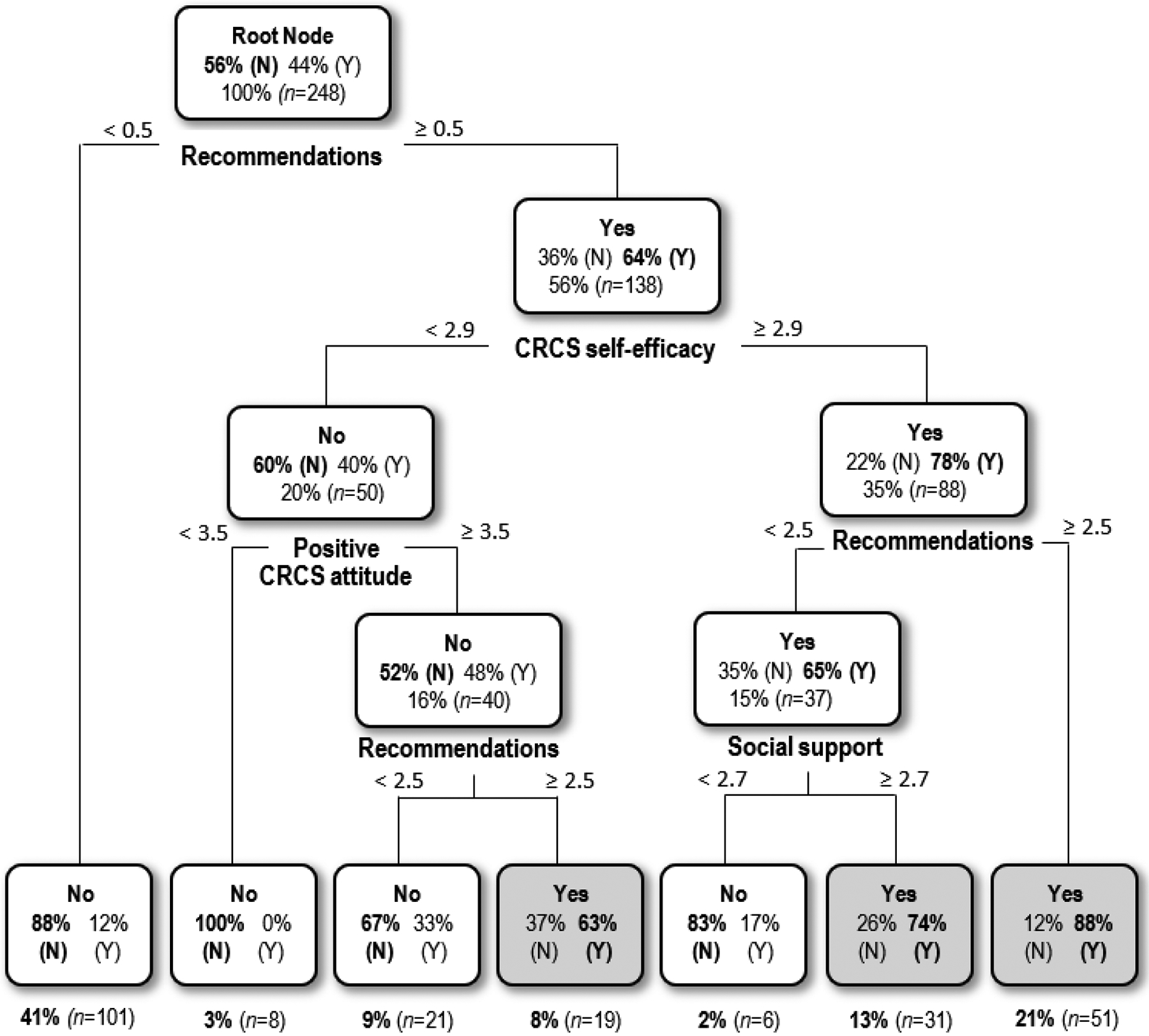
The decision tree model of CRCS adoption
The root node (n = 248) was the top node in the tree that was split into two branches according to a primary indicator of CRCS recommendations (< 0.5, ≥ 0.5) that leads to further nodes. Receiving less than or equal to 0.5 CRCS recommendations predicted a non-CRCS adoption group and was denoted as ‘no’ in the final terminal node (n = 101, 41%, prob = 0.88). When respondents received greater than 0.5 CRCS recommendations, they were identified as a CRCS adoption group (n = 138, 56%, prob = 0.64) and the node was split further according to the indicator of CRCS self-efficacy.
Among the respondents, those who possessed CRCS self-efficacy greater than or equal to 2.9 comprised a CRCS adoption group (n = 88, 35%, prob = 0.78) and the node split by CRCS recommendations appeared for a second time (< 2.5, ≥ 2.5). Among the respondents, those who received greater than or equal to 2.5 CRCS recommendations comprised a CRCS adoption group (denoted as ‘yes’ in the final terminal node) with an 88% probability of observation (n = 51, 21%). When respondents received recommendations less than 2.5 (n = 37, 15%, prob = 0.65) and then had social support greater than or equal to 2.7, we predicted a CRCS adoption group in the final terminal node (n = 31, 13%, prob = 0.74). However, when respondents had social support less than 2.7, we predicted a non-CRCS adoption group (n = 6, 2%, prob = 0.83).
Respondents who received greater than or equal to 0.5 CRCS recommendations and then possessed CRCS self-efficacy of less than 2.9 comprised a non-CRCS adoption group (n = 50, 20%, prob = 0.60), and the node split at the CRCS attitudes. Among the respondents, those who possessed CRCS attitudes of less than 3.5 comprised a non-CRCS adoption group (denoted as ‘no’ in the final terminal node) with a 100% probability of observation (n = 8, 3%). When respondents had CRCS attitudes greater than or equal to 3.5, they comprised a non-CRCS adoption group (n = 40, 16%, prob = 0.52), and the node split into two branches according to the indicator of CRCS recommendations that appeared for a third time (< 2.5, ≥ 2.5). Among those respondents, when they received greater than or equal to 2.5 CRCS recommendations, they comprised a CRCS adoption group in the final terminal node (n = 19, 8%, prob = 0.63). Yet, when they received less than 2.5 CRCS recommendations, they comprised a non-CRCS adoption group (n = 21, 9%, prob = 0.67).
Overall, the results indicated that higher levels of individual factors (i.e., CRCS self-efficacy and CRCS attitudes, Research question 1) and interpersonal factors (i.e., CRCS recommendations and social support, Research question 2) predicted adoption of CRCS. However, in this model, none of the organizational/community factors predicted CRCS adoption (Research question 3). The first root node was split according to recommendations from the respondents’ social networks to adopt CRCS. This indicates the CRCS recommendations are the most critical factor in determining their CRCS behavior (≥ 0.5, n = 139, prob = 0.64). The largest segment (n = 101, 41%) was classified as a non-CRCS adoption group because of a low level of CRCS recommendations from social networks (< 0.5, prob = 0.88). Further, the second largest segment (n = 51, 21%, prob = 0.88) was classified as a CRCS adoption group because of high levels of CRCS recommendations (≥ 0.5, n = 138, 56%, prob = 0.64), CRCS self-efficacy (≥ 2.9, n = 88, 35%, prob = 0.78), and the second presence of CRCS recommendations (≥ 2.5, n = 51, 21%, prob = 0.88). This indicates that the two predictors of CRCS recommendations and CRCS self-efficacy have the greatest predictive power to forecast CRCS adoption (Research question 4).
Model Evaluation and Cross-Validation
The performance of the final decision tree was evaluated with the error matrix and receiver-operating characteristic (ROC) analyses with a validation dataset (n = 56, 16%) (Fielding and Bell 1997: Song and Kim 2021). The overall error rate is 0.16, the precision rate is 0.89, and the area under the ROC curve (AUROCC) is 0.93 that means the decision tree was accurate and had a low misclassification rate. Further, we cross-validated the model’s performance against the testing dataset (n = 49, 14%) (Song and Kim 2018). The result of the error matrix and ROC analysis on the testing dataset showed an overall error rate of 0.27, a precision rate of 0.77, and an AUROCC of 0.80, which thus confirmed the unbiased estimate of the model’s performance (Song and Kim 2021). Therefore, the final decision tree model generated from the training dataset was validated and showed acceptable accuracy and precision in its performance (see Table 2).
Table 2.
Decision tree model evaluation and comparison
| Sample | n | AUROCC | Overall error rate | Accuracy | Precision |
|---|---|---|---|---|---|
| Validation dataset | 56 | 0.93 | 0.16 | 0.84 | 0.89 |
| Testing dataset | 49 | 0.80 | 0.27 | 0.73 | 0.77 |
| Full dataset | 353 | 0.87 | 0.21 | 0.79 | 0.84 |
Note. 1) The final model was built using the training dataset (n = 248, 70%).
2) The performance of the final model was validated using a validation dataset (n = 56, 16%) and a testing dataset (n = 49, 14%).
Variable Importance
We conducted a RF analysis to estimate the relative importance of the variables and to provide additional information about the significant predictors found in the main data analysis (Breiman 2001; Song & Kim 2018). We ran a RF model, which was an ensemble of 300 decision trees (ntree = 300), with the 11 variables tested in the final decision tree. The RF algorithm randomly selected three input variables at each node (mtry = 3) and computed the best node split. The R software system calculated two measures of the importance for each variable. Both the accuracy and Gini measures of Variable Importance indicated that CRCS recommendations (Accuracy measure = 29.62; Gini measure = 21.79) and CRCS self-efficacy (Accuracy measure = 13.47; Gini measure = 16.13) were the most important predictors of CRCS adoption among the 11 variables, which corresponds to the result in the final decision tree. The CRCS attitudes is also a highly important variable in the Accuracy measure of the RF model but was not in the Gini measure. While social support turned out to be a relatively important variable in the Gini measure but was not for the Accuracy measure in the ensemble of 300 decision trees.
Discussion
This study examined multi-level factors associated with adoption of CRCS among Korean Americans using the decision tree modeling. Also, this study determined the most important factors that predict the CRCS adoption. The findings are consistent with previous studies and add to an existing body of literature regarding CRCS behavior for this ethnic group. The findings indicate the significance of recognizing individual and interpersonal characteristics when developing interventions for improving CRCS among Korean Americans.
Firstly, this study found that self-efficacy and attitudes pertaining to CRCS discern the groups of CRCS adoption vs. non-adoption in Korean Americans (Research question 1). The findings suggest that personal cognition and subjective norms among Korean Americans can be more important than psychological perceptions (i.e., distress, risk of colorectal cancer, health status) in their uptake of CRCS. Using Bandura’ self-efficacy theory (Bandura 1994), CRCS self-efficacy reflects individuals’ belief in the capacity to perform screening-related tasks, controlling for barriers to screening. Prior studies indicate that self-efficacy mediates the link between psychological factors and intent of CRCS (Jimbo et al. 2017; Arnold et al. 2017). To improve self-efficacy for CRCS, interventions may consider development of community-based health education programs in which healthcare providers or lay educators provide a list of locations that offers screening by Korean doctors/nurses or with interpreting services and demonstrate how to arrange an appointment and prepare for the screening. Furthermore, negative attitudes toward CRCS (e.g., cancer-related fatalism, mistrusts of western medicine/healthcare system, and discomfort at bowl preparation and sedation) might prevent Korean Americans from participating in CRCS (Jo et al. 2008; H. Y. Lee and Im 2013; Maxwell et al. 2010). Like other Asian subgroups (e.g., Chinese and Japanese) in the U.S., Koreans traditionally tend to have sociocentric orientation and collectivism in tandem with Confucianism, placing high values on social norms (Honda and Kagawa-Singer 2006; Sullivan 2016), which may present challenges for changing CRCS attitudes. Therefore, culturally appropriate, long-term, sustainable approaches for influencing CRCS attitudes are needed, to increase CRCS among Korean Americans. One of the approaches can be a community CRCS ambassador program which is designed to provide training, education, and support to lay persons who reach Korean Americans in community and provide information directed toward the negative attitudes toward CRCS.
Secondly, this study found that CRCS recommendations and social support predict CRCS uptake in Korean Americans (Research question 2). Recommendations for CRCS have previously been found to be a strong predictor of CRCS for Korean Americans (Jung et al. 2017; S. Lee et al. 2014). While most prior studies focused on CRCS recommendations from healthcare providers, this study extended the CRCS recommendations to include family and friends. In an early cross-sectional study conducted by Jo and colleagues (Jo et al. 2008) in Los Angeles County, Korean Americans reported that recommendations from a trustworthy physician, friend or relative facilitated their utilization of CRCS. The findings of the present study support these early, descriptive results by statistically testing the relationship between CRCS adoption and CRCS recommendations from various sources using the decision tree model. These findings suggest that CRCS should continue to be recommended among Korean Americans not only at healthcare settings but also at community settings. Regarding social support, the findings from this study are consistent with existing literature showing that social support is positively associated with CRCS across ethnic groups (Rogers et al. 2017; Besharati et al. 2018). However, Korean Americans often have limited social networks in their communities, and they are likely to receive less than optimal social support (Jang et al. 2016). Moreover, health communication studies indicate that characteristics of individuals who are within a person’s social networks tend to be homogeneous (Centola 2011; Flatt, Agimi, and Albert 2012). These imply that Korean Americans are highly likely to have relatives or friends within their social networks who have similarities in their beliefs and attitudes concerning CRCS. Therefore, it is worthwhile considering the critical roles of community healthcare providers and health educators in making up for limited social networks and social support for CRCS among Korean Americans.
Finally, the decision tree model used in this study found CRCS recommendations and CRCSS self-efficacy to be the most powerful predictors of CRCS adoption among Korean Americans (Research question 4). These findings provide implications for practices and suggestions for future research. Health practitioners at primary healthcare settings should ensure that Korean American patients are adherent to CRCS guidelines and recommend patients to set up follow-up screenings. They may actively engage with patients via email, text messaging, or phone calls. Additionally, community health educators and policy makers should address barriers (e.g., health insurance, screening costs, navigating the healthcare system) that inhibit Korean Americans from accessing CRCS services and complying with the CRCS guidelines. For those with low CRCS self-efficacy, for example, community programs focused on social support may offer health navigators or lay health educators who help Korean Americans initiate and complete CRCS. The findings also provide suggestions for future research, in particular the need to examine Korean Americans’ social support and the social networks that are linked to their adoption of CRCS. As people increase their communications online via social media, future studies could also investigate the impact of social media on advancing social support from the online social networks for CRCS promotion.
Limitations
The findings also should be interpreted with caution due to several limitations. First, this study employed a cross-sectional study design. The findings do not support causal relationships between the predictors and outcome variables. Longitudinal studies can offer a clearer understanding of the causal relationships. Second, the data were obtained from self-administered surveys rather than actual screening data so the findings might involve social desirability issues. Further efforts on enhancing privacy and confidentiality of the participants may help minimize these issues. Third, the outcome variable in this study assessed the participants’ receipt of CRCS. In future studies, the outcome variable should consider status of screening schedule or compliance with screening schdudule guidelines for the participants. Fourth, the findings may apply only to Korean Americans in the metropolitan area in the Southeastern U.S. rather than Korean Americans in other U.S. locations. To improve generalizability of the findings, multi-site comparative studies should be considered. Fifth, there might be co-variables which were not included in the model. Future studies should include other co-variables (e.g., knowledge, beliefs, online health information seeking) to better predict CRCS behavior for this ethnic group. Although this study focused on the determining predictors of individual, interpersonal, and organizational aspects without investigating the potential effect of demographic factors, future studies should consider conducting socio-demographic profiling by gender, education, and income subgroups to verify the model’s ability to generalize our study results. Finally, while the findings were interpreted from the lens of the social ecological framework, different theories or models may also explain the relationships among the variables used in this study.
Conclusion
This study used the decision tree model to predict factors of CRCS adoption among Korean Americans within the social ecological framework. The decision tree model found CRCS self-efficacy and CRCS attitudes at the individual level and CRCS recommendations and social support at the interpersonal level that differentiate adopting or not adopting CRCS in Korean Americans. This study also found CRCS recommendations and CRCS self-efficacy to be the strongest predictors of their adoption of CRCS. These findings contribute to the knowledge base regarding CRCS behavior for Korean Americans by adopting an advanced analytic statistical approach. The findings also offer implications and suggestions for practices and future research for increasing CRCS rates among Korean Americans.
Supplementary Material
Contributor Information
Seok Won Jin, School of Social Work, The University of Memphis, 226 McCord Hall. Memphis, TN 38152. Tel: 901-678-2616, Fax: 901-678-2981..
Christina Soyoung Song, Department of Family and Consumer Sciences, Fashion Design and Merchandising, Illinois State University, 126A Turner Hall, Campus Box 5060, Normal, IL 61790. Tel: 309-438-5427..
References
- American Cancer Society. 2021. “Colorectal Cancer Statistics | How Common Is Colorectal Cancer?” 2021. https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html.
- Arnold Connie L., Rademaker Alfred, Liu Dachao, and Davis Terry C.. 2017. “Changes in Colorectal Cancer Screening Knowledge, Behavior, Beliefs, Self-Efficacy, and Barriers among Community Health Clinic Patients after a Health Literacy Intervention.” Journal of Community Medicine & Health Education 7 (1). 10.4172/2161-0711.1000497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A 1994. “Self-Efficacy.” In Encyclopedia of Human Behavior, 4:71–81. New York: Academic Press. https://www.uky.edu/~eushe2/Bandura/BanEncy.html. [Google Scholar]
- Besharati F, Karimi-Shahanjarini A, Hazavehie SMM, Bashirian S, and Faradmal J. 2018. “Predictors of Colorectal Cancer Screening Intention among Iranian Adults: An Application of the Preventive Health Model.” Journal of Preventive Medicine and Hygiene 59 (2): E159–66. [PMC free article] [PubMed] [Google Scholar]
- Breiman Leo. 2001. “Random Forests.” Machine Learning 45 (1): 5–32. 10.1023/A:1010933404324. [DOI] [Google Scholar]
- Brittain Kelly, and Murphy Virginia P.. 2015. “Sociocultural and Health Correlates Related to Colorectal Cancer Screening Adherence among Urban African Americans.” Cancer Nursing 38 (2): 118–24. 10.1097/NCC.0000000000000157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadhead WE, Gehlbach SH, de Gruy FV, and Kaplan BH. 1988. “The Duke-UNC Functional Social Support Questionnaire. Measurement of Social Support in Family Medicine Patients.” Medical Care 26 (7): 709–23. [DOI] [PubMed] [Google Scholar]
- Carney Patricia A., Lin Frances Lee, Mongoue-Tchokote Solange, Mori Motomi, Leung Holden, Lau Christine, Le TD, and Lieberman David A.. 2014. “Improving Colorectal Cancer Screening in Asian Americans: Results of a Randomized Intervention Study.” Cancer 120 (11): 1702–12. 10.1002/cncr.28640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centola Damon. 2011. “An Experimental Study of Homophily in the Adoption of Health Behavior.” Science (New York, N.Y.) 334 (6060): 1269–72. 10.1126/science.1207055. [DOI] [PubMed] [Google Scholar]
- Costanza Mary E., Luckmann Roger, Stoddard Anne M., Avrunin Jill S., White Mary Jo, Stark Jennifer R., Clemow Lynn, and Rosal Milagros C.. 2005. “Applying a Stage Model of Behavior Change to Colon Cancer Screening.” Preventive Medicine 41 (3–4): 707–19. 10.1016/j.ypmed.2004.12.013. [DOI] [PubMed] [Google Scholar]
- Dominick Gregory M., Papas Mia A., Rogers Michelle L., and Rakowski William. 2015. “Classification Tree Analysis to Examine Influences on Colorectal Cancer Screening.” Cancer Causes & Control: CCC 26 (3): 443–54. 10.1007/s10552-015-0523-6. [DOI] [PubMed] [Google Scholar]
- Doubeni Chyke A. 2014. “The Impact of Colorectal Cancer Screening on the United States Population: Is It Time to Celebrate?” Cancer 120 (18): 2810–13. 10.1002/cncr.28789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fielding Alan H., and Bell John F.. 1997. “A Review of Methods for the Assessment of Prediction Errors in Conservation Presence/Absence Models.” Environmental Conservation 24 (1): 38–49. 10.1017/S0376892997000088. [DOI] [Google Scholar]
- Flatt Jason D., Agimi Yll, and Albert Steve M.. 2012. “Homophily and Health Behavior in Social Networks of Older Adults.” Family & Community Health 35 (4): 312–21. 10.1097/FCH.0b013e3182666650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden Shelley D., and Earp Jo Anne L.. 2012. “Social Ecological Approaches to Individuals and Their Contexts: Twenty Years of Health Education & Behavior Health Promotion Interventions.” Health Education & Behavior 39 (3): 364–72. 10.1177/1090198111418634. [DOI] [PubMed] [Google Scholar]
- Honda Keiko, and Kagawa-Singer Marjorie. 2006. “Cognitive Mediators Linking Social Support Networks to Colorectal Cancer Screening Adherence.” Journal of Behavioral Medicine 29 (5): 449–60. 10.1007/s10865-006-9068-1. [DOI] [PubMed] [Google Scholar]
- Issa Iyad A, and Noureddine Malak. 2017. “Colorectal Cancer Screening: An Updated Review of the Available Options.” World Journal of Gastroenterology 23 (28): 5086–96. 10.3748/wjg.v23.i28.5086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson Christian S., Oman Matthew, Patel Aatish M., and Vega Kenneth J.. 2016. “Health Disparities in Colorectal Cancer among Racial and Ethnic Minorities in the United States.” Journal of Gastrointestinal Oncology 7 (Suppl 1): S32–43. 10.3978/j.issn.2078-6891.2015.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang Yuri, Park Nan Sook, Chiriboga David A., Yoon Hyunwoo, Ko Jisook, Lee Juyoung, and Kim Miyong T.. 2016. “Risk Factors for Social Isolation in Older Korean Americans.” Journal of Aging and Health 28 (1): 3–18. 10.1177/0898264315584578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimbo Masahito, Sen Ananda, Plegue Melissa A., Hawley Sarah T., Kelly-Blake Karen, Rapai Mary, Zhang Minling, Zhang Yuhong, and Ruffin Mack T.. 2017. “Correlates of Patient Intent and Preference on Colorectal Cancer Screening.” American Journal of Preventive Medicine 52 (4): 443–50. 10.1016/j.amepre.2016.11.026. [DOI] [PubMed] [Google Scholar]
- Jo Angela M., Maxwell Annette E., Wong Weng K., and Bastani Roshan. 2008. “Colorectal Cancer Screening among Underserved Korean Americans in Los Angeles County.” Journal of Immigrant and Minority Health / Center for Minority Public Health 10 (2): 119–26. 10.1007/s10903-007-9066-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung Mary Y., Holt Cheryl L., Ng Diane, Sim Hwa J., Lu Xiaoxiao, Le Daisy, Juon Hee-Soon, Li Jun, and Lee Sunmin. 2017. “The Chinese and Korean American Immigrant Experience: A Mixed-Methods Examination of Facilitators and Barriers of Colorectal Cancer Screening.” Ethnicity & Health, February, 1–20. 10.1080/13557858.2017.1296559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juon Hee-Soon, Han Wolmi, Shin Hosung, Kim Kim B., and Kim Miyong T.. 2003. “Predictors of Older Korean Americans’ Participation in Colorectal Cancer Screening.” Journal of Cancer Education: The Official Journal of the American Association for Cancer Education 18 (1): 37–42. 10.1207/s15430154jce1803s_3. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, Walters EE, and Zaslavsky AM. 2002. “Short Screening Scales to Monitor Population Prevalences and Trends in Non-Specific Psychological Distress.” Psychological Medicine 32 (6): 959–76. [DOI] [PubMed] [Google Scholar]
- Kim K, Yu ES, Chen EH, Kim J, and Brintnall RA. 1998. “Colorectal Cancer Screening. Knowledge and Practices among Korean Americans.” Cancer Practice 6 (3): 167–75. [DOI] [PubMed] [Google Scholar]
- Kohler Betsy A., Sherman Recinda L., Howlader Nadia, Jemal Ahmedin, Ryerson A. Blythe, Henry Kevin A., Boscoe Francis P., et al. 2015. “Annual Report to the Nation on the Status of Cancer, 1975–2011, Featuring Incidence of Breast Cancer Subtypes by Race/Ethnicity, Poverty, and State.” Journal of the National Cancer Institute 107 (6): djv048. 10.1093/jnci/djv048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Hee Yun, and Im Hyojin. 2013. “Colorectal Cancer Screening among Korean American Immigrants: Unraveling the Influence of Culture.” Journal of Health Care for the Poor and Underserved 24 (2): 579–98. 10.1353/hpu.2013.0087. [DOI] [PubMed] [Google Scholar]
- Lee Shin Young. 2018. “Colorectal Cancer Screening among Korean Americans in Chicago: Does It Matter Whether They Had the Screening in Korea or the US?” Asian Pacific Journal of Cancer Prevention : APJCP 19 (5): 1387–95. 10.22034/APJCP.2018.19.5.1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Sunmin, Chen Lu, Jung Mary, Baezconde-Garbanati Lourdes, and Juon Hee-Soon. 2014. “Acculturation and Cancer Screening Among Asian Americans: Role of Health Insurance and Having a Regular Physician.” Journal of Community Health 39 (2): 201–212 12p. 10.1007/s10900-013-9763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luszczynska A, and Schwarzer R. 2003. “Planning and Self-Efficacy in the Adoption and Maintenance of Breast Self-Examination: A Longitudinal Study on Self-Regulatory Cognitions.” Psychology & Health 18 (1): 93–108. [Google Scholar]
- Manne Sharon, Markowitz Arnold, Winawer Sidney, Meropol Neal J., Haller Daniel, Rakowski William, Babb James, and Jandorf Lina. 2002. “Correlates of Colorectal Cancer Screening Compliance and Stage of Adoption among Siblings of Individuals with Early Onset Colorectal Cancer.” Health Psychology 21 (1): 3–15. 10.1037/0278-6133.21.1.3. [DOI] [PubMed] [Google Scholar]
- Maxwell Annette E., Crespi Catherine M., Antonio Cynthia M., and Lu Peiyun. 2010. “Explaining Disparities in Colorectal Cancer Screening among Five Asian Ethnic Groups: A Population-Based Study in California.” BMC Cancer 10: 214. 10.1186/1471-2407-10-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris Kasey L., and Perna Frank M.. 2018. “Decision Tree Model vs Traditional Measures to Identify Patterns of Sun-Protective Behaviors and Sun Sensitivity Associated With Sunburn.” JAMA Dermatology 154 (8): 897–902. 10.1001/jamadermatol.2018.1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myong Jun-Pyo, Shin Jin-Yong, and Kim Su-Jin. 2012. “Factors Associated with Participation in Colorectal Cancer Screening in Korea: The Fourth Korean National Health and Nutrition Examination Survey (KNHANES IV).” International Journal of Colorectal Disease 27 (8): 1061–69. 10.1007/s00384-012-1428-4. [DOI] [PubMed] [Google Scholar]
- Oh Kyeung, and Jacobsen Kathryn. 2014. “Colorectal Cancer Screening Among Korean Americans: A Systematic Review.” Journal of Community Health 39 (2): 193–200 8p. 10.1007/s10900-013-9758-x. [DOI] [PubMed] [Google Scholar]
- Pruitt Sandi L., Leonard Tammy, Zhang Song, Schootman Mario, Halm Ethan A., and Gupta Samir. 2014. “Physicians, Clinics, and Neighborhoods: Multiple Levels of Influence on Colorectal Cancer Screening.” Cancer Epidemiology and Prevention Biomarkers 23 (7): 1346–55. 10.1158/1055-9965.EPI-13-1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers Charles R., Mitchell Jamie A., Franta Gabriel J., Foster Margaret J., and Shires Deirdre. 2017. “Masculinity, Racism, Social Support, and Colorectal Cancer Screening Uptake Among African American Men: A Systematic Review.” American Journal of Men’s Health 11 (5): 1486–1500. 10.1177/1557988315611227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu So Yeon, Crespi Catherine M., and Maxwell Annette E.. 2014. “Colorectal Cancer among Koreans Living in South Korea versus California: Incidence, Mortality, and Screening Rates.” Ethnicity & Health 19 (4): 406–23. 10.1080/13557858.2013.801404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabado Parichart, Jo Angela, Kagawa-Singer Marjorie, and Juhn Erica. 2015. “Community Collaborative for Colorectal Cancer Screening in Los Angeles Koreatown.” Journal of Health Care for the Poor and Underserved 26 (2 Suppl): 164–70. 10.1353/hpu.2015.0053. [DOI] [PubMed] [Google Scholar]
- Sauer Sebastian, Lemke Jana, Zinn Winfried, Buettner Ricardo, and Kohls Niko. 2015. “Mindful in a Random Forest: Assessing the Validity of Mindfulness Items Using Random Forests Methods.” Personality and Individual Differences, Dr. Sybil Eysenck Young Researcher Award, 81 (July): 117–23. 10.1016/j.paid.2014.09.011. [DOI] [Google Scholar]
- Schwartz MD, Lerman C, Miller SM, Daly M, and Masny A. 1995. “Coping Disposition, Perceived Risk, and Psychological Distress among Women at Increased Risk for Ovarian Cancer.” Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association 14 (3): 232–35. [DOI] [PubMed] [Google Scholar]
- Siegel Rebecca L., Miller Kimberly D., and Jemal Ahmedin. 2017. “Cancer Statistics, 2017.” CA: A Cancer Journal for Clinicians 67 (1): 7–30. 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- Song CS, & Kim Y-K 2021. “Predictors of consumers’ willingness to share personal information with fashion sales robots.” Journal of Retailing and Consumer Services, 63: 102727. 10.1016/j.jretconser.2021.102727. [DOI] [Google Scholar]
- Song SY, & Kim Y-K 2018. “Theory of virtue ethics: Do consumers’ good traits predict their socially responsible consumption?” Journal of Business Ethics, 152(4): 1159–1175. 10.1007/s10551-016-3331-3. [DOI] [Google Scholar]
- Song Yan-yan, and Lu Ying. 2015. “Decision Tree Methods: Applications for Classification and Prediction.” Shanghai Archives of Psychiatry 27 (2): 130–35. 10.11919/j.issn.1002-0829.215044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan Daniel. 2016. “Cultural Variation as Patterns of Social Orientation and Control.” Cultural-Existential Psychology: The Role of Culture in Suffering and Threat. April 2016. 10.1017/CBO9781316156605.005. [DOI] [Google Scholar]
- Therneau Terry, Atkinson Beth, Ripley Brian (producer of the initial R. port, and maintainer 1999–2017). 2019. Rpart: Recursive Partitioning and Regression Trees (version 4.1–15). https://CRAN.R-project.org/package=rpart.
- Tran Mi T., Jeong Matthew B., Nguyen Vickie V., Sharp Michael T., Yu Edgar P., Yu Filmer, Tong Elisa K., et al. 2018. “Colorectal Cancer Beliefs, Knowledge, and Screening among Filipino, Hmong, and Korean Americans.” Cancer 124 (S7): 1552–59. 10.1002/cncr.31216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. 2021. “Healthy People 2030.” 2021. https://health.gov/healthypeople/objectives-and-data/browse-objectives/cancer/increase-proportion-adults-who-get-screened-colorectal-cancer-c-07.
- US Preventive Services Task Force. 2018. “Final Update Summary: Colorectal Cancer: Screening - US Preventive Services Task Force.” 2018. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/colorectal-cancer-screening2.
- Werk Rachel S., Hill Julie C., and Graber Julia A.. 2017. “Impact of Knowledge, Self-Efficacy, and Perceived Importance on Steps Taken Toward Cancer Prevention Among College Men and Women.” Journal of Cancer Education 32 (1): 148–54. 10.1007/s13187-016-0996-3. [DOI] [PubMed] [Google Scholar]
- Young Belinda-Rose, Gwede Clement K., Thomas Bria, Vázquez-Otero Coralia, Ewing Aldenise, Best Alicia L., Loi Claudia X. Aguado, et al. 2019. “A Systematic Review of U.S.-Based Colorectal Cancer Screening Uptake Intervention Systematic Reviews: Available Evidence and Lessons Learned for Research and Practice.” Frontiers in Public Health 7 (June). 10.3389/fpubh.2019.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


