Introduction:
Corneal ulcers are a significant cause of corneal blindness worldwide.1 Normally, traumatic corneal damage and secondary infection are diagnosed by an ophthalmologist via slit-lamp examination. However, limited healthcare resources in developing regions may delay diagnosis and treatment, increasing the risk of vision loss.2 Mobile phones are widely available even in resource-limited settings and therefore could potentially be used to aid in diagnosis of corneal pathology.3 Herein, we describe and test a custom-made smartphone attachment that allows diagnosis of corneal epithelial defects with a smartphone.
Methods:
We designed a smartphone attachment to provide magnified images of the cornea with controlled illumination. The attachment consisted of a +25 diopter lens and external light-emitting diode (LED) light sources that were aligned with the smartphone camera for image acquisition (Figure 1). In one configuration, white LEDs (correlated color temperature of a 5250 Kelvin lamp) were used to capture white light corneal photographs. In a second configuration, blue LEDs (472nm peak wavelength) were used with a 550nm/50nm emission filter to capture fluorescein-stained corneal photographs. The attachments, which we refer to as Ocular CellScopes, slide on and off unmodified smartphones, allowing a single smartphone to take both white light and fluorescein photographs.
Figure 1: Diagram and Photograph of the Ocular CellScope Device.
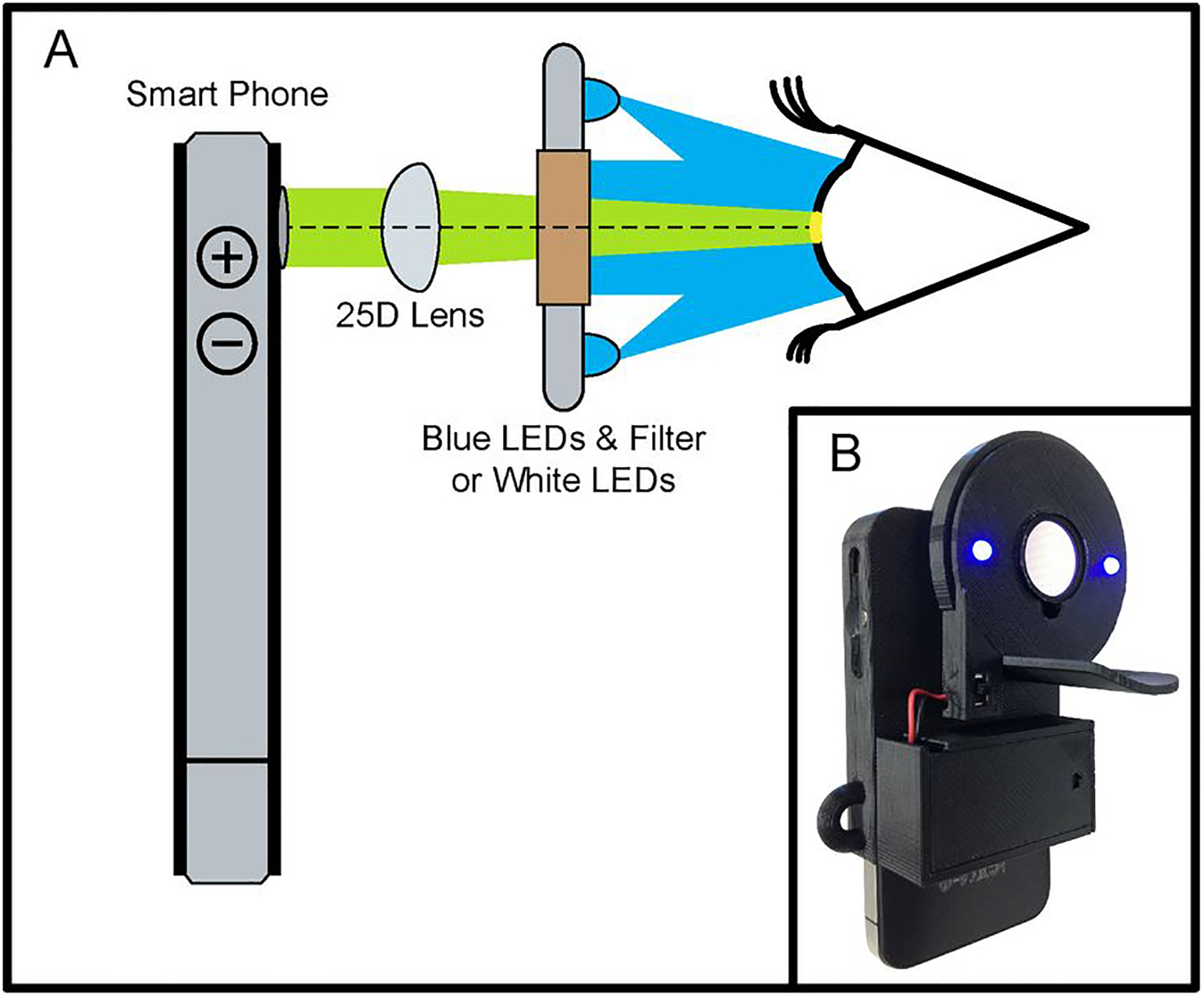
Panel A shows a schematic illustration of the smartphone attachment for corneal imaging. Fluorescein photographs are taken with a blue LED and fluorescence filter that passes only light emitted from a fluorescein-stained defect. White light photographs are taken with a white light-emitting diode (LED) without a filter. Panel B shows a photograph of the fluorescein smartphone attachment.
To validate the smartphone attachments, we used an iPhone 4S (Apple Inc., Cupertino, CA) to photograph 17 eyes from 17 patients at Chiang Mai University Hospital, Thailand. Subjects had a slit-lamp examination by an ophthalmologist, followed by photography with the white light smartphone attachment. Fluorescein was then administered, followed by slit-lamp examination and photography with the fluorescein smartphone attachment. Three off-site ophthalmologists graded all 34 photographs masked to the diagnosis, first as 34 independent photographs and then as 17 pairs of white light and fluorescein photographs from the same eye. We calculated the agreement between the various assessments of an epithelial defect with Cohen’s kappa. We estimated the sensitivity and specificity of smartphone photography versus the on-site ophthalmologist using the grades of all three graders, and constructed 95% confidence intervals (CI) by percentile bootstrap, resampling eyes to account for non-independence between grades of the same eye (10,000 repetitions). Analyses were performed with Stata 12.0 (Statacorp, College Station, TX). Institutional review board approval was obtained from the University of California, San Francisco.
Results:
The on-site ophthalmologist detected an epithelial defect in 6 of 17 eyes (Figure 2; eFigure 1) The consensus diagnosis (agreement of at least 2 of the 3 graders) detected an epithelial defect in 5 eyes—all of which also had an epithelial defect diagnosed by the on-site ophthalmologist. Agreement between the three graders for the diagnosis of epithelial defect was good (kappa = 0.73; 95%CI, 0.53–0.91). Agreement between the consensus diagnosis and the on-site ophthalmologist’s diagnosis for epithelial defect was excellent (kappa = 0.87; 95%CI, 0.61–1.0). Compared to the on-site ophthalmologist’s examination, the sensitivity of photographic diagnosis of an epithelial defect was 83.3% (95%CI, 61.1–100%) and specificity was 97.0% (95%CI, 90.9–100%). When the white light and fluorescein photographs were assessed as a pair, the sensitivity of photographic diagnosis of an epithelial defect improved to 88.9% (95%CI, 66.7–100%), while the specificity decreased to 90.9% (95%CI, 78.8–100%).
Figure 2: Corneal Photographs of Participants Diagnosed with an Epithelial Defect by the On-site Ophthalmologist.
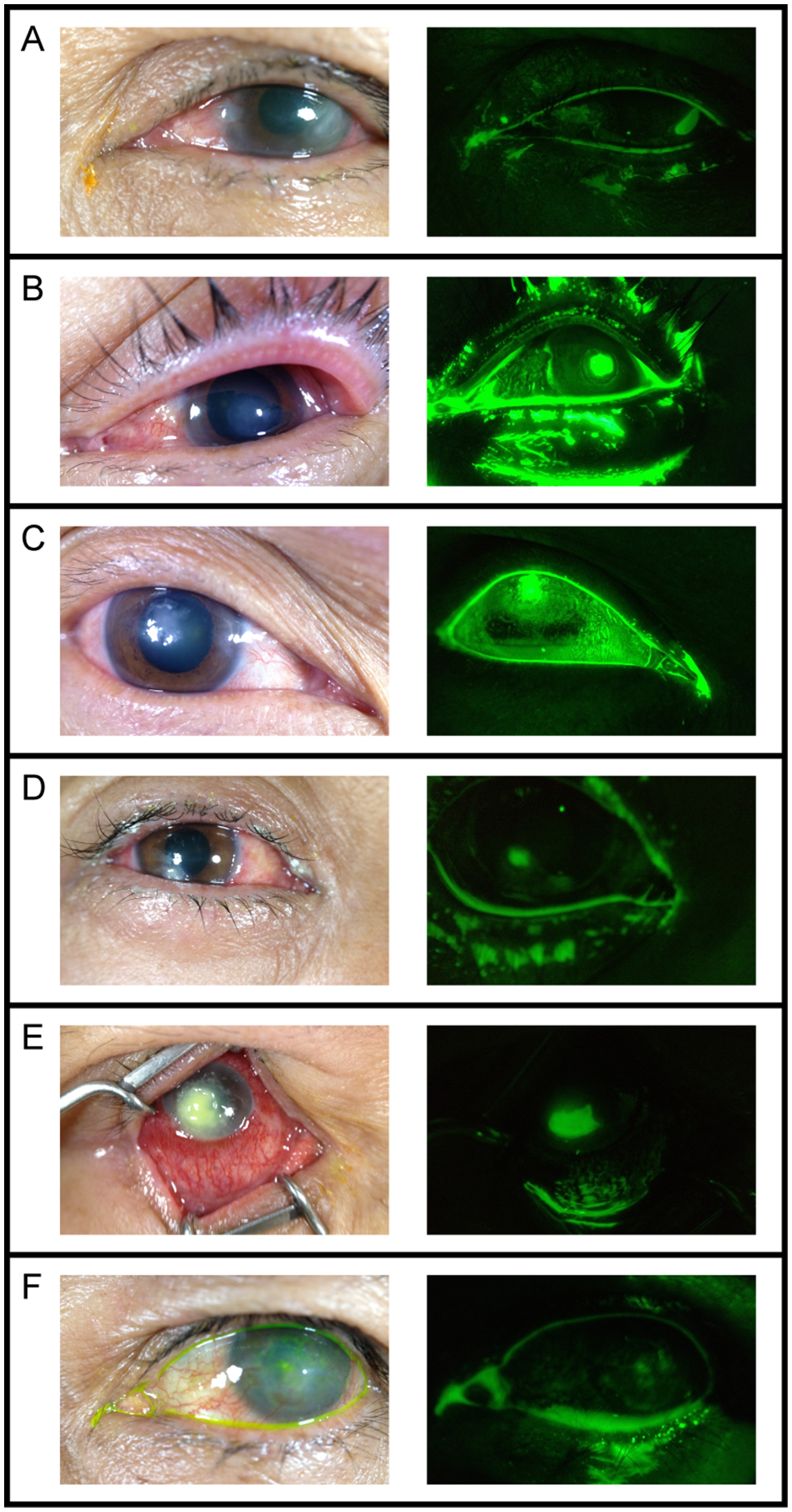
Photographs of the 6 subjects found to have epithelial defects (white arrowheads) taken with the white light smartphone attachment (left) and the fluorescein smartphone attachment (right). When viewed as a pair, all three graders correctly identified the epithelial defects in panels A through E and one grader correctly identified the epithelial defect in panel F.
Discussion:
Developing regions of the world are highly burdened by corneal ulcers that ultimately lead to corneal blindness.4 As wireless telecommunication coverage continues to expand in regions with limited healthcare resources, low-cost, easy-to-use smartphone devices may substitute for expensive and highly technical medical instruments used to diagnose corneal ulcers. In this report, we demonstrated that smartphone attachments capturing white light and fluorescein photographs show potential as a new technology for the diagnosis of corneal trauma in resource-poor settings.
Supplementary Material
Acknowledgement:
Funding/Support:
This work was supported by a Research to Prevent Blindness Medical Student Eye Research Fellowship Grant (RNM), the University of California, Berkeley Blum Center for Developing Economies (DAF), and the National Institutes of Health (National Eye Institute grant K23 EY010971). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of Interest and Financial Disclosures:
RNM, DAF, and TPM have pending intellectual property with the University of California describing a mobile phone camera for retinal imaging. At the current time this intellectual property has no financial value. SA and JDK do not have any conflicts of interest to disclose. TPM reports a grant from That Man May See during the conduct of the study. DAF is also a co-founder of CellScope Inc., which is a medical device start-up using mobile phones for disease screening and diagnosis. CellScope, Inc. was not involved in this research.
Footnotes
Publication Disclosure: An abstract with preliminary findings of this study was presented at the 2013 ARVO Annual Meeting on May 7th, 2013 in Seattle, Washington. This manuscript has not been previously submitted and is not under consideration elsewhere.
References:
- 1.Witcher J, Srinivasan M, Upadhyay MP. Corneal blindness: A global perspective. Bull World Health Organ. 2001;79(3):214–221. [PMC free article] [PubMed] [Google Scholar]
- 2.Upadhyay MP, Karmacharya PC, Koirala S, et al. The Bhaktapur eye study: ocular trauma and antibiotic prophylaxis for the prevention of corneal ulceration in Nepal. Br J Ophthalmol. 2001;85(4):388–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United Nations Foundation. mHealth for Development: The Opportunity of Mobile Technology for Healthcare in the Developing World. Washington, D.C. and Berkshire, UK: United Nations Foundation-Vodafone Foundation Partnership; 2009. [Google Scholar]
- 4.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96(5):614–618. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


