Abstract
Objective: To compare the differences between proximal femoral nail antirotation (PFNA) and dynamic hip screw (DHS) in treatment of femoral trochanteric fracture and analyze the factors influencing recovery after PFNA treatment. Methods: Eighty-six patients with femoral trochanteric fracture admitted to Taizhou Hospital of Traditional Chinese Medicine between January 2019 and June 2021 were enrolled in the study and assigned into a PFNA group and DHS group (n=43 in each group) before undergoing these treatments. The clinical efficacy, inflammatory factors, and myocardial injury markers were compared between the two groups. The influencing factors on recovery after PFNA treatment were analyzed by univariate and multivariate analysis. Results: Compared to the DHS group, the PFNA group had shorter surgical time, length of stay in hospital, postoperative weight-bearing time, time of healing and detumescence, and less intraoperative blood loss (all P<0.001). The incidence of post-surgical complications with PFNA was lower than with DHS (P<0.05). The serum levels of interleukin-6, C-reactive protein and tumor necrosis factor-αof the PFNA group were lower than those of the DHS group (all P<0.05). Moreover, the serum levels of cardiac troponin T, creatine kinase-MB and myoglobin in the PFNA group were also lower than for the DHS (all P<0.05). At the first, third, and sixth months after surgery, the Harris scores for PFNA were higher than for DHS (all P<0.05). The univariate and multivariate analysis showed that instability of fracture, history of osteoporosis, excessive intraoperative bleeding, poor compliance with rehabilitation exercise, and long time from injury to surgery were risk factors for poor recovery following PFNA treatment for patients with femoral trochanteric fracture. Conclusion: Compared to DHS, PFNA had better clinical efficacy and gave lower serum levels of inflammatory factors and myocardial injury markers. Fracture classification, history of osteoporosis, intraoperative amount of bleeding, compliance of rehabilitation exercise, and time from injury to surgery were closely associated with recovery following PFNA treatment.
Keywords: Femoral intertrochanteric fracture, proximal femoral nail antirotation, dynamic hip screw, recovery effects, risk factors
Introduction
Femoral trochanteric fracture is defined as occurrence of fractures above the level of the lesser trochanter and below the hip capsule line of the femoral neck base. With an increasingly aging population, the incidence of femoral trochanteric fracture is growing [1,2]. Femoral trochanteric fracture usually appears in the elderly over 60 years old due to osteoporosis [3]. Canale et al. revealed that there were more than 200,000 people with femoral trochanteric fracture in the United States every year, with high morbidity and mortality [4]. This severely lowers the life quality of the patients and increases medical burden. Therefore, femoral trochanteric fracture in the elderly has become an important challenge for orthopaedics.
With the development of operative technique and material of internal fixation, surgery for femoral trochanteric fracture has been considered as a preferred method. However, the optimal surgical method for femoral trochanteric fracture remains controversial. Dynamic hip screw (DHS) is a traditional internal fixation method for treatment of femoral trochanteric fracture. It is limited in clinical use due to large changes in shear stress, poor stability of internal fixation, and excessive exposure of operation. Proximal femoral nail antirotation (PFNA) is another surgical treatment for these patients and has been widely used for many years. A preliminary study showed that good results had been achieved [5]. Lenich et al. indicated the biomechanical superiority of PFNA to Gamma nail [6]. In recent years, many studies have been conducted to compare the clinical efficacy in patients with femoral trochanteric fracture using these two fixation methods [7,8]. However, these studies failed to draw a clear conclusion regarding optimal treatment in improving prognosis [9]. In this context, 86 elderly patients with femoral trochanteric fracture were included in this study, and the comparison of clinical efficacy between PFNA and DHS was performed. In addition, the influence factors for recovery effect following PFNA were also investigated. The results of this study should show what treatment of femoral trochanteric fracture in the elderly is best.
Materials and methods
Research subjects
This is a retrospective study. All of the included patients signed the informed consent. This protocol had been approved by the ethic committee of the hospital (No. 201902-143). Eighty-six patients with femoral trochanteric fracture admitted to the Department of Orthopedics, Taizhou Hospital of Traditional Chinese Medicine between January 2019 and June 2021 were enrolled and divided into PFNA group and DHS group according to the operative methods. There were 43 patients in each group. Inclusion criteria were as follows: Patents were aged between 60 and 80 years old. Patients were first diagnosed with femoral intertrochanteric fracture. Patients had indications for an operation and chose to receive surgical treatment. The clinical data of patients were complete. Exclusion criteria: patients also had femoral head necrosis, hip arthritis, or other fractures. Patients manifested surgical contraindications and were not able to tolerate anesthesia. Patients were accompanied with severe dysfunction of heart and lung. Patients could not cooperate in this study.
Surgery procedure
PFNA treatment was performed as follows: The patient was generally anesthetized in a supine position before the traction and reduction of the broken ends of fractured bone. After routine disinfection and covering the surgical site with surgical drape, a straight incision was made at the femoral major trochanter. The skin, subcutaneous tissue, and muscle were dissected bluntly to allow a full exposure of the major trochanter. The guide pin was placed from the medial space to guide marrow reaming. An appropriate PFNA main nail was placed into medullary cavity, which was confirmed by X-ray. A proper length spiral blade was selected and placed into femoral neck through an interlocking nail under the guide of a locator. X-ray was applied again for confirmation of a successful reduction, followed by locking the spiral blade and the distal femoral interlocking nail. Finally, the drainage tube was retained, and the incision was sutured.
DHS treatment was as follows: patients were in supine position and hip was slightly elevated. After general anesthesia, patients received routine disinfection and the surgical site was covered with surgical drape. In order to expose the proximal end of femur and major trochanter, a lateral incision was made at the hip joint. Reduction of the fracture was conducted through traction. Then, a Kirschner wire was inserted from the head to neck of femur with the help of X-ray. After expansion and tapping, the threaded nail was screwed and the compression screw was fixed and tightened following installation of plate of sleeve according to the previous reports [10]. Finally, the incision was sutured after retaining a drainage tube.
Outcome measure
Primary indicators were the hip joint function, levels of inflammatory factors, and myocardial injury markers. Secondary indicators were surgical time, intraoperative blood loss, length of stay in hospital, postoperative weight-bearing time, time of healing, time of detumescence, and the post-surgical complications.
Comparisons were performed between the PFNA group and DHS group in the term of surgical time, intraoperative blood loss, length of stay in hospital, postoperative weight-bearing time, time of healing, and time of detumescence. The post-surgical complications including pulmonary infection, deep venous thrombosis, nonunion, internal fixed fracture, and urinary system infection were also compared.
The hip joint function was evaluated by Harris Hip Scores, which includes 4 items i.e., pain, living ability, joint deformity, and joint range of motion. The total scores were 100 points. Higher score indicated better recovery of the hip joint. According to previous reports [11], the recovery effect after operation was considered as excellent when Harris score was more than 75 points, while it was poor when the score was less than 75 points. According to the Harris scores at six months after PFNA operation, these patients were assigned into an excellent group and a poor group.
Inflammatory factors such as C-reactive protein (CRP) (RAB0096, Sigma Company, USA), interleukin-6 (IL-6) (RAB0306, Sigma Company, USA), tumor necrosis factor-α (TNF-α) (RAB1089, Sigma Company, USA) were detected by enzyme- linked immunosorbent assay (ELISA) according the instructions. The myocardial injury markers such as cardiac troponin T (cTnT), creative kinase isoenzyme MB (CK-MB) and myohemoglobin (Myo) were detected by electrochemiluminescence analyser (Type: Elecsys 2010, Roche Company, USA). The serum levels of inflammatory factors and myocardial injury markers were compared between PFNA group and DHS group.
Statistical analysis
All data included in this study were analyzed with statistical product and service solutions (SPSS) 23.0 software. Measured data were presented as mean ± standard deviation. Independent-sample T test was exploited for comparison between the two groups. Enumerated data were described as number/percentage. Chi-square test was exploited for comparison between two groups. The risk factors for affecting the recovery effect following PFNA treatment were evaluated by univariate and multivariate analysis. The multiple logistic regression analysis was adopted for analyzing the statistical significance of the results of univariate analysis. P-value <0.05 was considered as significant.
Results
General information
No obvious differences were found in comparisons of general information including gender, age, body mass index, underlying disease, causes of fracture, and Evans types of fracture, as seen in Table 1 (P>0.05), suggesting they were comparable.
Table 1.
Comparison of general information between the two groups
| Group | PFNA Group (N=43) | DHS Group (N=43) | t/χ2 value | P-value |
|---|---|---|---|---|
| Male/Female (n) | 19/24 | 21/22 | 0.187 | 0.666 |
| Age (years) | 68.1±1.9 | 68.3±1.6 | 0.528 | 0.599 |
| BMI (kg/cm2) | 20.8±1.3 | 20.9±1.1 | 0.385 | 0.701 |
| Diabetes (n) | 17 | 14 | 0.454 | 0.501 |
| Hypertension (n) | 16 | 19 | 0.434 | 0.510 |
| Hyperlipemia (n) | 15 | 16 | 0.050 | 0.822 |
| Cause of fracture (n) | 0.222 | 0.895 | ||
| Traffic accident | 12 | 14 | ||
| Fall down injury | 13 | 12 | ||
| Fall off injury | 18 | 17 | ||
| Evans-Jensen types (n) | 1.165 | 0.280 | ||
| Stability | 25 | 20 | ||
| Instability | 18 | 23 |
Note: BMI: Body mass index; DHS: Dynamic hip screw; PFNA: Proximal femoral nail antirotation.
Comparison of operative index
Compared to those in the DHS group, patients in the PFNA group had significantly shorter surgical time, length of stay in hospital, postoperative weight-bearing time, time of healing and detumescence, and less intraoperative blood loss (all P<0.001), as shown in Table 2.
Table 2.
Comparison of operative indexes between the two groups
| Group | Surgical time (min) | Intraoperative blood loss (mL) | Length of stay in hospital (d) | Postoperative weight-bearing time (days) | Time of healing (months) | Time of Detumescence (weeks) |
|---|---|---|---|---|---|---|
| PFNA group (N=43) | 82.9±5.1 | 159.2±13.4 | 16.5±2.1 | 17.1±2.6 | 4.2±0.5 | 4.1±0.6 |
| DHS group (N=43) | 108.3±6.7 | 279.4±16.2 | 25.3±4.3 | 22.3±3.5 | 5.3±0.7 | 5.2±0.9 |
| t value | 19.780 | 37.490 | 12.060 | 7.821 | 8.385 | 6.669 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Note: DHS: Dynamic hip screw; PFNA: Proximal femoral nail antirotation.
Comparison of post-surgical complications
After operation, in the PFNA group, there was 1 patient with nonunion and 1 patient with urinary system infection, while there was 1 case with pulmonary infection, 1 case with deep venous thrombosis, 2 cases with nonunion, 2 cases with internal fixed fracture and 2 cases with urinary system infection in DHS group. The incidence rate of total complications in the PFNA group was significantly lower than that in the DHS group (P<0.05), as shown in Table 3.
Table 3.
Comparison of post-surgical complications between the two groups
| Groups | Pulmonary infection | Deep venous thrombosis | Nonunion | Internal fixed fracture | Urinary system infection | Total complications |
|---|---|---|---|---|---|---|
| PFNA group (N=43) | 0 (0%) | 0 (0%) | 1 (2.3%) | 0 | 1 (2.3%) | 2 (4.7%) |
| DHS group (N=43) | 1 (2.3%) | 1 (2.3%) | 2 (4.7%) | 2 (4.7%) | 2 (4.7%) | 8 (18.6%) |
| χ2 | 4.074 | |||||
| P | 0.044 |
Note: DHS: Dynamic hip screw; PFNA: Proximal femoral nail antirotation.
Comparison of inflammatory factors
Before surgery, there were no statistical differences for the levels of CRP, IL-6 and TNF-α between the PFNA group and DHS group. After surgery, the levels of CRP, IL-6, and TNF-α in PFNA group were lower than those in DHS groups (all P<0.05), as seen in Figure 1.
Figure 1.
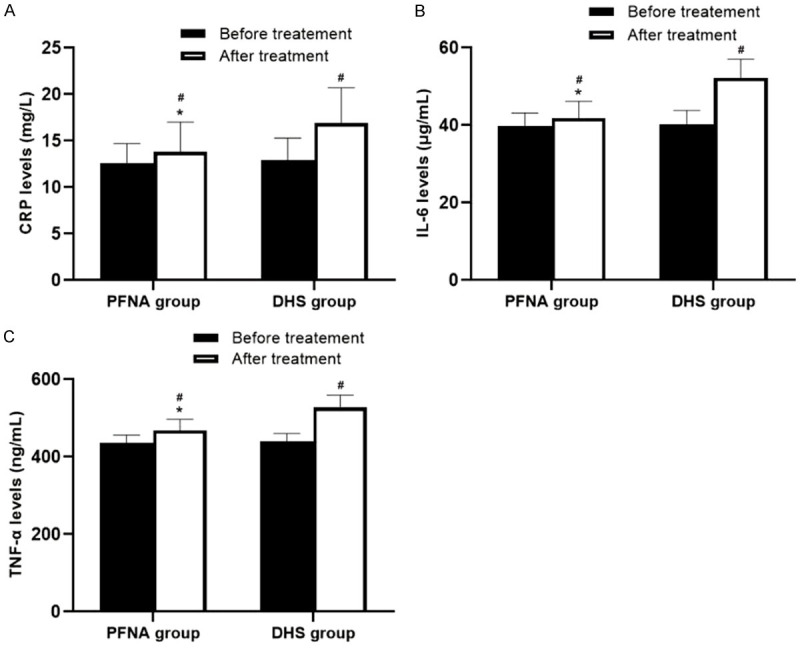
Comparison of serum inflammatory factors between the PFNA group and DHS group. Compared to DHS group after treatment, *P<0.05. Compared to before treatment in the same group, #P<0.05. A: The level of CRP. B: The level of IL-6. C: The level of TNF-α. Note: DHS: Dynamic hip screw; PFNA: Proximal femoral nail antirotation; CRP: C-reactive protein; IL-6: Interleukin-6; TNF-α: tumor necrosis factor-α.
Comparison of myocardial injury markers
Before surgery, no significant differences were found for the levels of cTnT, CK-MB, and Myo between PFNA group and DHS group. After surgery, the levels of cTnT, CK-MB, and Myo in PFNA group were significantly lower than those in DHS group (all P<0.05), as shown in Figure 2.
Figure 2.
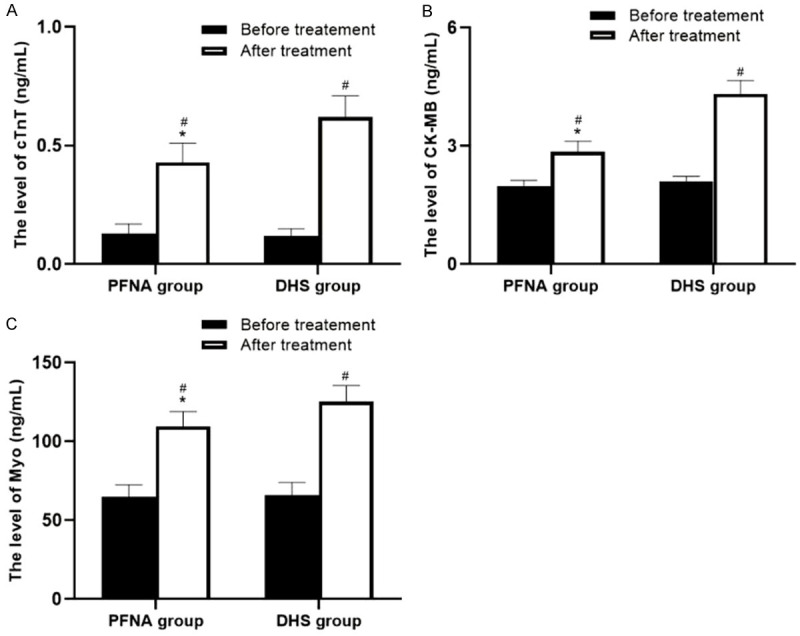
Comparison of myocardial injury markers between the PFNA group and DHS group. Compared to DHS group after treatment, *P<0.05. Compared to before treatment in the same group, #P<0.05. A: The level of cTnT. B: The level of CK-MB. C: The level of Myo. Note: DHS: Dynamic hip screw; PFNA: Proximal femoral nail antirotation; cTnT: cardiac troponin T; CK-MB: creative kinase isoenzyme MB; Myo: myohemoglobin.
Comparison of hip joint function
As shown in Table 4, the Harris scores at the first month, third month and sixth month after operation in PFNA group were 63.5±5.2, 77.6±5.8, and 85.2±6.7, respectively, while in DHS group they were 57.9±4.6, 69.2±5.4 and 76.4±6.1, respectively. The Harris scores after PFNA at one month, three months, and six months were significantly higher than those after DHS, respectively. There were significant differences between the two groups (all P<0.001).
Table 4.
Comparison of Harris scores between DHS group and PFNA group at different time points
| Group | One month after operation | Three months after operation | Six months after operation |
|---|---|---|---|
| PFNA group (N=43) | 63.5±5.2 | 77.6±5.8 | 85.2±6.7 |
| DHS group (N=43) | 57.9±4.6 | 69.2±5.4 | 76.4±6.1 |
| t value | 5.289 | 6.951 | 6.369 |
| P-value | <0.001 | <0.001 | <0.001 |
Note: DHS: Dynamic hip screw; PFNA: Proximal femoral nail antirotation.
Results of univariate and multivariate analysis
As shown in Table 5, univariate analysis results showed that Evans-Jensen classification, time from injury to surgery, intraoperative amount of bleeding, history of osteoporosis, compliance with rehabilitation exercise and dietary habits after surgery were the risk factors for affecting effect following PFNA treatment. The proportions of patients with unstable fracture, osteoporosis, poor compliance of rehabilitation exercise, and routine diet in the excellent group were lower than those in the poor group (all P<0.05). In addition, the time from injury to surgery and intraoperative amount of bleeding in the excellent group were significantly lower than those in the poor group (all P<0.05). As seen in Table 6, multivariate analysis results revealed that instability of fracture, history of osteoporosis, intraoperative more amount of bleeding, worse compliance of rehabilitation exercise and longer time from injury to surgery were risk factors of adverse effect after PFNA treatment.
Table 5.
Univariate analysis for factors affecting PFNA treatment effectiveness
| Parameter | Excellent group (N=32) | Poor group (N=11) | t/χ2 value | P-value |
|---|---|---|---|---|
| Evans-Jensen classification (n) | 5.787 | 0.016 | ||
| Stability | 22 | 3 | ||
| Instability | 10 | 8 | ||
| Time from injury to surgery (d) | 2.1±0.5 | 3.1±0.8 | 4.870 | <0.001 |
| Intraoperative amount of bleeding (mL) | 142.3±13.5 | 208.4±18.6 | 12.690 | <0.001 |
| History of osteoporosis (n) | 4.329 | 0.038 | ||
| Yes | 22 | 10 | ||
| No | 10 | 1 | ||
| Compliance with rehabilitation exercise (n) | 4.375 | 0.037 | ||
| Excellent | 29 | 7 | ||
| Poor | 3 | 4 | ||
| Dietary habits after surgery (n) | 5.372 | 0.021 | ||
| Routine diet | 4 | 5 | ||
| Routine diet with fortified calcium | 28 | 6 |
Table 6.
Multivariate analysis for factors affecting PFNA treatment effectiveness
| Parameter | OR | 95% CI | β | Wald | SE |
|---|---|---|---|---|---|
| Instability of fracture | 5.418 | 2.013-13.852 | 1.702 | 9.975 | 0.492 |
| History of osteoporosis | 3.047 | 1.405-6.035 | 0.984 | 7.450 | 0.357 |
| Excessive intraoperative bleeding | 4.062 | 1.708-10.317 | 1.516 | 7.918 | 0.556 |
| Poor compliance with rehabilitation exercise | 5.988 | 2.542-11.758 | 1.913 | 13.863 | 0.508 |
| Long time from injury to surgery | 1.582 | 1.175-3.965 | 0.448 | 13.051 | 0.158 |
Note: OR: Odds ratio; CI: Confidence interval; SE: Standard error.
Discussion
According to the statistics, femoral trochanteric fracture caused by osteoporosis accounts for about 50% of all intertrochanteric fractures [12]. It usually results in different degrees of rotation displacement, separation displacement, and lateral displacement [13]. For elderly patients, femoral trochanteric fracture is a typical injury. These patients usually have comorbidities. Effective fixation of femoral intertrochanteric fracture is of great importance [14]. It was found that the fixation was closely associated with the reduction of intertrochanteric fracture and the postoperative recovery of the hip joint function [15]. Thus, at present it is considered that operation should be conducted as early as possible to avoid the increase of complications.
PFNA consisted of one nail, one distal interlocking nail and femoral neck spiral blade. This surgical method limits the incision size with closed reduction and minimizes periosteum injury. It is beneficial for the union of the fracture [16,17]. With intramedullary center fixed load sharing the same force line with that of femoral shaft, the internal expansion load bearing effectively resists the shear force of the fractured bone end. Some studies have unveiled that the design of PFNA was suitable for osteoporotic patients [14,18]. Another study also showed PFNA had significant superiorities compared with other internal fixation systems [19]. In this study, the results revealed that compared with DHS treatment, PFNA had advantages of less surgical time, less intraoperative blood loss, shorter length of stay in hospital, less postoperative weight-bearing time, less time of healing and detumescence and fewer postoperative complications. Moreover, the results of Harris hip scores showed the recovery of hip joint function after surgery was better in the PFNA group than in the DHS group. These results indicated that PFNA could be considered as a perfect method for patients with femoral trochanteric fracture, which is similar to other reports [20]. Our further study showed that instability of fracture, osteoporosis history, more intraoperative bleeding, worse compliance of rehabilitation exercise, and longer time from injury to surgery were the risk factors for affecting the recovery efficacy following PFNA treatment. These results could effectively guide the clinical use of PFNA in patients with femoral trochanteric fracture.
The serum inflammatory factors would significantly change if the body is injured. CRP, IL-6, and TNF-α are currently considered the common serum inflammatory factors. The change in CRP, IL-6, and TNF-α levels was reported to be involved in the occurrence and development of fractures and they were increased in the process of bone resorption [21]. Macedo et al. suggested that CRP, as a systemic inflammatory indicator, was regulated by other inflammatory factors including IL-6, IL-1, and TNF-α [22]. Another study showed that the serum levels of inflammatory factors including IL-6, IL-1, CRP, and TNF-α could reflect the degree of stress in patients [23]. In this study, the results showed that the serum levels of IL-6, CRP, and TNF-α after surgery in PFNA group were significantly lower than those in DHS group, indicating PFNA could decrease the inflammatory factors in these patients with femoral trochanteric fracture. It also suggested that PFNA treatment was helpful for the recovery of these patients.
During the period of treatment, elderly patients with femoral trochanteric fracture may undergo adverse cardiovascular events such as heart failure and myocardial infarction. These might be attributed to stress response, anesthesia, and circulatory capacity. In clinical practice, not much attention is paid to early examination of these adverse cardiovascular events, which could cause a delay in therapy of the fracture. cTnT is a common marker for detection of myocardial injury and was reported to be a prognostic marker of cardiac complications in elderly patients with hip fracture [24]. CK-MB is another important index and of great significance for the diagnosis of myocardial infarction [25]. Myo, as an early indicator, is usually exploited for evaluating complication and reinfarction in patients with fractures [26]. The results of this study revealed that the serum levels of cTnT, CK-MB and Myo after operation were significantly lower in PFNA group than in DHS group, suggesting that PFNA provoked less damage to the myocardium and cardiac function. Moreover, Wang et al. found that PFNA treatment could effectively reduce myocardial injury markers in elderly patients with intertrochanteric fractures in contrast to DHS treatment [27], which is consistent with results reported by this study.
This study has several shortcomings that should be recognized. First, this is a retrospective study and there were no long-term follow-up results. Second, the sample size was small, which may affect its findings. Third, the effects of PFNA and DHS on inflammatory factors and cardiac injury markers still need follow-up of larger number of clinical cases to better guide clinical use. Fourth, the data were collected from a single center, which may affect its generalization to other hospitals.
In conclusion, compared to DHS, PFNA could better fix the femoral trochanteric fracture with little effect on the levels of inflammatory factors and slight damage to myocardium, thus promoting the recovery of hip joint function with reduced prevalence of complications. PFNA could be considered as a promising treatment showing favorable clinical safety and efficacy.
Disclosure of conflict of interest
None.
References
- 1.Lil NA, Makwana VR, Patel TD, Patel AR. Comparative study of intertrochanteric fracture fixation using proximal femoral nail with and without distal interlocking screws. World J Orthop. 2022;13:267–277. doi: 10.5312/wjo.v13.i3.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schipper IB, Steyerberg EW, Castelein RM, van der Heijden FH, den Hoed PT, Kerver AJ, van Vugt AB. Treatment of unstable trochanteric fractures. Randomised comparison of the gamma nail and the proximal femoral nail. J Bone Joint Surg Br. 2004;86:86–94. [PubMed] [Google Scholar]
- 3.Cheng YX, Sheng X. Optimal surgical methods to treat intertrochanteric fracture: a Bayesian network meta-analysis based on 36 randomized controlled trials. J Orthop Surg Res. 2020;15:402. doi: 10.1186/s13018-020-01943-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yano S, Matsuura Y, Hagiwara S, Nakamura J, Kawarai Y, Suzuki T, Kanno K, Shoda J, Tsurumi Y, Ohtori S. Determinants of fracture type in the proximal femur: biomechanical study of fresh frozen cadavers and finite element models. Bone. 2022;158:116352. doi: 10.1016/j.bone.2022.116352. [DOI] [PubMed] [Google Scholar]
- 5.Jin ZZ, Xu SY, Yang Y, Wei YL, Tian YC, Wang ZY, Bai LH. Cemented hemiarthroplasty versus proximal femoral nail antirotation in the management of intertrochanteric femoral fractures in the elderly: a case control study. BMC Musculoskelet Disord. 2021;22:846. doi: 10.1186/s12891-021-04586-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lenich A, Vester H, Nerlich M, Mayr E, Stockle U, Fuchtmeier B. Clinical comparison of the second and third generation of intramedullary devices for trochanteric fractures of the hip--Blade vs screw. Injury. 2010;41:1292–1296. doi: 10.1016/j.injury.2010.07.499. [DOI] [PubMed] [Google Scholar]
- 7.Ma KL, Wang X, Luan FJ, Xu HT, Fang Y, Min J, Luan HX, Yang F, Zheng H, He SJ. Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: a meta-analysis. Orthop Traumatol Surg Res. 2014;100:859–866. doi: 10.1016/j.otsr.2014.07.023. [DOI] [PubMed] [Google Scholar]
- 8.Yu WG, Zhang XC, Zhu XF, Yu ZC, Xu YF, Zha GQ, Hu J, Yi JH, Liu YJ. Proximal femoral nails anti-rotation versus dynamic hip screws for treatment of stable intertrochanteric femur fractures: an outcome analyses with a minimum 4 years of follow-up. BMC Musculoskelet Disord. 2016;17:222. doi: 10.1186/s12891-016-1079-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arirachakaran A, Amphansap T, Thanindratarn P, Piyapittayanun P, Srisawat P, Kongtharvonskul J. Comparative outcome of PFNA, Gamma nails, PCCP, Medoff plate, LISS and dynamic hip screws for fixation in elderly trochanteric fractures: a systematic review and network meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol. 2017;27:937–952. doi: 10.1007/s00590-017-1964-2. [DOI] [PubMed] [Google Scholar]
- 10.Ouyang X, Ding YZ, Yu L, Xin F, Yang XW, Sha P, Tong SM, Cheng Q, Xu YQ. Comparison of the clinical effect of DHS and PFNA on senile osteoporotic fracture and their significance of changes in BALP expression level. J Musculoskelet Neuronal Interact. 2020;20:556–562. [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang YZ, Lin Y, Li C, Yue XJ, Li GY, Wang B, Wang YQ, Zhu ZQ. A comparative analysis of femoral neck system and three cannulated screws fixation in the treatment of femoral neck fractures: a six-month follow-up. Orthop Surg. 2022;14:686–693. doi: 10.1111/os.13235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diaz AR, Navas PZ. Risk factors for trochanteric and femoral neck fracture. Rev Esp Cir Ortop Traumatol (Engl Ed) 2018;62:134–141. doi: 10.1016/j.recot.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Yin B, He YM, Wang D, Zhou JL. Classification of femur trochanteric fracture: evaluating the reliability of Tang classification. Injury. 2021;52:1500–1505. doi: 10.1016/j.injury.2020.11.031. [DOI] [PubMed] [Google Scholar]
- 14.Li H, Wang Q, Dai GG, Peng H. PFNA vs. DHS helical blade for elderly patients with osteoporotic femoral intertrochanteric fractures. Eur Rev Med Pharmacol Sci. 2018;22:1–7. doi: 10.26355/eurrev_201807_15346. [DOI] [PubMed] [Google Scholar]
- 15.Mariottini F, De Simone S, Cipolloni L, Bosco MA, La Russa R. Proximal femoral fractures in the elderly, mortality at 30 days and fast track: does it always worth it? Clin Ter. 2022;173:149–154. doi: 10.7417/CT.2022.2409. [DOI] [PubMed] [Google Scholar]
- 16.Wei HP, Xiao QP, He JF, Huang TJ, Xu WT, Xian SP, Xia MH. Effect and safety of topical application of tranexamic acid to reduce perioperative blood loss in elderly patients with intertrochanteric fracture undergoing PFNA. Medicine (Baltimore) 2021;100:e27123. doi: 10.1097/MD.0000000000027123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loh J, Huang D, Lei J, Yeo W, Wong MK. Early clinical outcomes of short versus long proximal femoral nail anti-rotation (PFNA) in the treatment of intertrochanteric fractures. Malays Orthop J. 2021;15:115–121. doi: 10.5704/MOJ.2107.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu R, Ru JY, Ji F, Liu J, Ji Y, Wu ZQ, Shi D. Comparison of efficacy, complications and TGF-beta2 expression between DHS and PFNA in elderly patients with osteoporotic femoral intertrochanteric fracture. Exp Ther Med. 2018;16:394–399. doi: 10.3892/etm.2018.6177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu W, Liu J, Ji GR. Comparison of clinical outcomes with proximal femoral nail anti-rotation versus InterTAN nail for intertrochanteric femoral fractures: a meta-analysis. J Orthop Surg Res. 2020;15:500. doi: 10.1186/s13018-020-02031-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang H, Zhu XX, Pei GW, Zeng XS, Zhang N, Xu P, Chen D, Yu WG, Zhang XC. A retrospective analysis of the InterTan nail and proximal femoral nail anti-rotation in the treatment of intertrochanteric fractures in elderly patients with osteoporosis: a minimum follow-up of 3 years. J Orthop Surg Res. 2017;12:147. doi: 10.1186/s13018-017-0648-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.David GG, Michele B, Umberto R, Cioanca F, Andrea S, Alfonso C, Cristina IV, Maria ML, Antonio HJ, Giuseppe R, Luigi M. Metabolic shock in elderly pertrochanteric or intertrochanteric surgery. Comparison of three surgical methods. Is there a much safer? Rom J Anaesth Intensive Care. 2020;27:17–26. doi: 10.2478/rjaic-2020-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Macedo Santiago LA, Neto LGL, Borges Pereira G, Leite RD, Mostarda CT, de Oliveira Brito Monzani J, Sousa WR, Rodrigues Pinheiro AJM, Navarro F. Effects of resistance training on immunoinflammatory response, TNF-alpha gene expression, and body composition in elderly women. J Aging Res. 2018;2018:1467025. doi: 10.1155/2018/1467025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cauley JA, Barbour KE, Harrison SL, Cloonan YK, Danielson ME, Ensrud KE, Fink HA, Orwoll ES, Boudreau R. Inflammatory markers and the risk of hip and vertebral fractures in men: the osteoporotic fractures in men (MrOS) J Bone Miner Res. 2016;31:2129–2138. doi: 10.1002/jbmr.2905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chong CP, van Gaal WJ, Savige J, Lim WK. Cardiac injury and troponin testing after orthopaedic surgery. Injury. 2011;42:855–863. doi: 10.1016/j.injury.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 25.Talsnes O, Hjelmstedt F, Dahl OE, Pripp AH, Reikeras O. Clinical and biochemical prediction of early fatal outcome following hip fracture in the elderly. Int Orthop. 2011;35:903–907. doi: 10.1007/s00264-010-1149-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holzhauser L, Kim G, Sayer G, Uriel N. The Effect of left ventricular assist device therapy on cardiac biomarkers: implications for the identification of myocardial recovery. Curr Heart Fail Rep. 2018;15:250–259. doi: 10.1007/s11897-018-0399-3. [DOI] [PubMed] [Google Scholar]
- 27.Wang B, Liu Q, Liu Y, Jiang R. Comparison of proximal femoral nail antirotation and dynamic hip screw internal fixation on serum markers in elderly patients with intertrochanteric fractures. J Coll Physicians Surg Pak. 2019;29:644–648. doi: 10.29271/jcpsp.2019.07.644. [DOI] [PubMed] [Google Scholar]


