Abstract
Background: In Japan, oxygen is commonly administered during the acute phase of myocardial infarction (MI) to patients without oxygen saturation monitoring. In this study we assessed the effects of supplemental oxygen therapy, compared with ambient air, on mortality and cardiac events by synthesizing evidence from randomized controlled trials (RCTs) of patients with suspected or confirmed acute MI.
Methods and Results: PubMed was systematically searched for full-text RCTs published in English before June 21, 2020. Two reviewers independently screened the search results and appraised the risk of bias. The estimates for each outcome were pooled using a random-effects model. In all, 2,086 studies retrieved from PubMed were screened. Finally, 7,322 patients from 9 studies derived from 4 RCTs were analyzed. In-hospital mortality in the oxygen and ambient air groups was 1.8% and 1.6%, respectively (risk ratio [RR] 0.90; 95% confidence interval [CI] 0.38–2.10]); 0.8% and 0.5% of patients, respectively, experienced recurrent MI (RR 0.44; 95% CI 0.12–1.54), 1.5% and 1.6% of patients, respectively, experienced cardiac shock (RR 1.10; 95% CI 0.77–1.59]), and 2.4% and 2.0% of patients, respectively, experienced cardiac arrest (RR 0.91; 95% CI 0.43–1.94).
Conclusions: Routine supplemental oxygen administration may not be beneficial or harmful, and high-flow oxygen may be unnecessary in normoxic patients in the acute phase of MI.
Key Words: Acute coronary syndrome, Acute myocardial infarction, Ambient air, Oxygen, ST-elevation myocardial infarction
Cerebral and cardiovascular diseases are the leading causes of death in Japan, accounting for approximately one-quarter of deaths.1 Reperfusion therapy for ST-segment elevation myocardial infarction (STEMI) is now widely accepted as an acute treatment for myocardial infarction (MI). It is important to establish reperfusion without coronary flow delay as soon as possible using coronary intervention to improve prognosis.2 However, oxygen therapy fails to result in better outcomes. The Air Versus Oxygen In MI (AVOID) study showed that supplemental oxygen in STEMI patients may increase early myocardial injury rates and is associated with a larger MI size.3 Therefore, the 2015 international Consensus on cardiopulmonary resuscitation and emergency cardiovascular care Science with Treatment Recommendations (CoSTR) suggested withholding oxygen rather than using routine oxygen supplementation in normoxic patients with acute MI (AMI).4
However, in Japan, oxygen is frequently administered to patients during the acute phase of MI without oxygen saturation (SpO2) monitoring. The mnemonic MONA (for morphine, oxygen, nitrates, and aspirin) has commonly been used to refer to adjuvant treatment for the management of AMI.5 Oxygen may be routinely administered to patients as part of their primary care in the ambulance and emergency department because of decreased oxygen supply to the myocardium due to coronary artery occlusions.
Following the official CoSTR announcement in 2015,4 a further 2 trials addressing supplementary oxygen in AMI were published.6,7 Of the two trials, the Determination of the Role of Oxygen in Suspected Acute Myocardial Infarction (DETO2XAMI) trial enrolled 6,629 patients into a registry-based randomized controlled trial (RCT) and evaluated mortality or rehospitalization 1 year after AMI.7 In the present study, we assessed the effects of supplemental oxygen on mortality and cardiac events by synthesizing evidence from RCTs on patients with suspected or confirmed AMI.
Methods
The Japan Resuscitation Council (JRC) Acute Coronary Syndrome (ACS) Task Force for guideline 2020, were established by the Japanese Circulation Society, the Japanese Association of Acute Medicine, and the Japanese Society of Internal Medicine. The JRC ACS Task Force established 12 clinically relevant questions. After discussion between the JRC ACS Task Force and the Guidelines Editorial Committee, the Population Intervention Comparator Outcome Study design and Time frame were used to guide the systematic review as follows:
P (patients): suspected or confirmed AMI patients with normal SpO2 (≥90%) in a prehospital situation or the emergency department
I (intervention): no oxygen administration (ambient air)
C (comparisons, controls): routine oxygen administration
O (outcomes):
• Critical: mortality (in-hospital, 6 months to 1 year), cardiac shock, cardiac arrest, and recurrent MI
• Important: infarct size, heart failure, arrhythmia
• Not important: chest symptoms
S (study designs): RCTs published in English
T (time frame): studies published before June 21, 2020.
The systematic review and meta-analysis were performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.8,9
Search Strategies
A systematic search of the PubMed database was performed to retrieve relevant articles for review. We searched for full-text RCTs published before June 21, 2020. A combination of key terms was used to establish a full search strategy (Supplementary Figure 1).
Study Selection and Inclusion Criteria
The study population included adult patients with ACS in an emergency setting, which included prehospital care. We did not restrict our analysis by country. However, we only included studies published in English. We sought to determine whether AMI patients with normal SpO2 actually require oxygen administration. The outcomes compared between patients with and without oxygen administration were mortality, recurrent MI, cardiac shock, and cardiac arrest.
Assessment of Risk of Bias
The Cochrane Risk of Bias Tool (Review Manager 5.3 [RevMan 5.3]; The Nordic Cochrane Center, Cochrane Collaboration, Copenhagen, Denmark) was used to appraise RCTs, non-RCTs, interrupted time series, and controlled before-and-after studies. Experienced pairs of reviewers (S.K., T.Y.) independently appraised the risk of bias of all included studies. Studies were categorized as having a “low”, “unclear”, or “high” risk of bias in each domain. The risk of bias for each element was considered “high” when bias was present and likely to affect the outcomes and “low” when bias was not present or present but unlikely to affect the outcomes.
Data Extraction and Management
The following data were extracted: author name(s), title, journal name, year of publication, website (URL), and abstract. After removing duplicates, 2 independent reviewers (S.K., T.Y.) screened the study abstracts and titles and subsequently reviewed the full-text articles. Disagreements were discussed until consensus was reached. The full text of articles included in the final selection was independently reviewed by another 2 reviewers (Y.T., M.K.). Disagreements were resolved by a third reviewer (H.N.).
Rating Certainty of Evidence
We used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) tool to rate the certainty of the evidence as to whether AMI patients with normal SpO2 need supplemental oxygen.10–13 The certainty of evidence was assessed as “high”, “moderate”, “low”, or “very low” according to the risk of bias, inconsistency, indirectness, imprecision, and publication bias.
Statistical Analysis
The results were summarized using a random-effects model to facilitate pooling of the estimated treatment effects. Dichotomous outcomes are described as risk ratios (RRs) and 95% confidence intervals (CIs). Continuous variables are shown as mean differences (MD) and respective 95% CI. Heterogeneity between trials for each outcome was evaluated using the I2 statistic to quantify inconsistencies,14 which were considered significant if the reason for heterogeneity could not be explained and the I2 value was ≥50%. We generated a funnel plot to investigate potential publication bias. The estimates for each outcome were pooled using a random-effects model. The meta-analysis was performed based on all available published data. All analyses were performed using RevMan 5.3.
Results
Literature Search
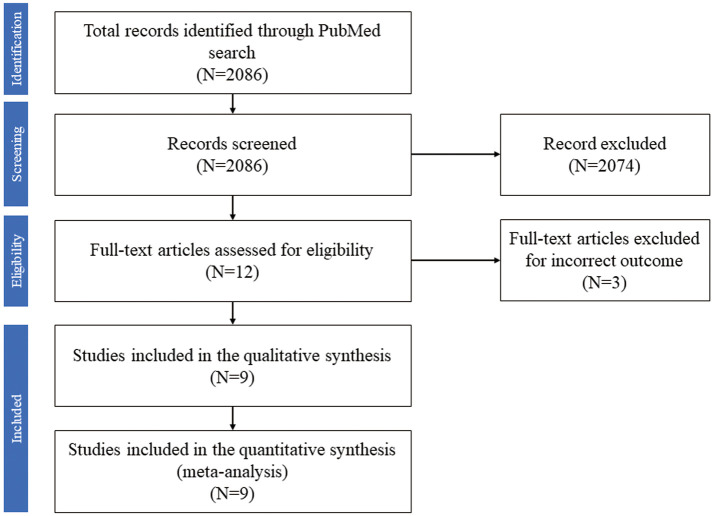
Figure 1 shows a flow diagram of the study adapted from the PRISMA statement.9 We identified 2,086 studies in the PubMed database. Only 12 studies were assessed for eligibility based on title and abstract screening. The full-text review led to the exclusion of 3 studies due to incorrect outcomes. Finally, 9 studies that originated from 4 RCTs were included in the present meta-analysis.3,6,7,15–20
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart. The PubMed database was searched for randomized and observational studies from inception to June 21, 2020.
Study Characteristics
The characteristics of the included studies are summarized in the Table. We enrolled patients with suspected or confirmed AMI. In all, 7,322 patients from the study of Rawles and Kenmure,15 the AVOID study by Stub et al,3 the Supplemental Oxygen in the Catheterized Coronary Emergency Reperfusion (SOCCER) trial by Khoshnood et al,17 and the DETO2X-AMI study by Hofmann et al7 were included, for a total of 3,655 patients in the oxygen group and 3,667 in the ambient air group. Detailed characteristics of the individual studies are presented in Supplementary Table 1. Subanalyses of the SOCCER and DETO2X-AMI studies were also performed to assess outcomes.6,16,18–20
Table.
Characteristics of the Included Studies
| Study, year | Setting | Study design |
Sample size | Participants | Oxygen therapy | No oxygen | Endpoints | Follow-up period |
|---|---|---|---|---|---|---|---|---|
| Rawles and Kenmure (197615) |
CCU | RCT, double-blind |
157 | Suspected AMI within 24 h of symptom onset |
Oxygen via MC mask at a flow rate of 6 L/min oxygen for 24 h |
MC mask at a flow rate of 6 L/min compressed air for 24 h |
In-hospital mortality, arrhythmia in 24 h, opiate use | Discharge |
| AVOID (Stub et al, 20153) |
EMS | RCT, open-label |
638 randomized, 441 analyzed |
Normoxic (SpO2
≥94%) patients with STEMI within 12 h of symptom onset |
Oxygen via Hudson mask at 8 L/min from ambulance, cardiac cath lab to the cardiac care ward |
Ambient air | Primary endpoint: IS ascertained by troponin and CK Secondary endpoints: mortality, TIMI score, ECG ST-segment resolution, MACE (death, MI, rehospitalization at 6 months), myocardial salvage determined by CMR |
6 months |
| SOCCER (Khoshnood et al, 201817) |
EMS | RCT, single-blind |
160 randomized, 95 analyzed | Normoxic (SpO2
≥94%) patients with confirmed STEMI within 12 h of symptom onset |
Oxygen via OxyMask at 10 L/min from ambulance until the end of primary PCI |
Ambient air | Primary endpoint: MSI on CMR Secondary endpoints: IS, MaR, ejection fraction, microvascular obstruction on CMR, VAS, doses of opioids and β-blockers, oxygen saturation change, ST-segment elevation resolution, TIMI flow, heart failure medications |
6 months |
| DETO2X-AMI (Hofmann et al, 20177) |
EMS, ED, CCU, cath lab |
RCT, open-label |
6,629 randomized with suspected AMI, 5,010 with confirmed AMI; all analyzed |
Normoxic (SpO2
≥90%) patients with suspected AMI |
Oxygen via OxyMask at 6 L/min for 6–12 h |
Ambient air | Primary endpoint: 1-year mortality Secondary endpoints: 30-day mortality, MACE (mortality, reinfarction, hospitalization due to heart failure), health economy |
1 year |
AMI, acute myocardial infarction; AVOID, Air Versus Oxygen In Myocardial Infarction; CCU, coronary care unit; CK, creatine kinase; CMR, cardiac magnetic resonance imaging; DETO2X-AMI, Determination of the Role of Oxygen in Suspected Acute Myocardial Infarction; ECG, electrocardiogram; ED, emergency department; EMS, emergency medical service; IS, infarct size; MACE, major adverse cardiovascular events; MaR, myocardium at risk; MC, medium concentration; MSI, myocardial salvage index; PCI, percutaneous coronary intervention; RCT, randomized controlled trial; SOCCER, Supplemental Oxygen in Catheterized Coronary Emergency Reperfusion; SpO2, oxygen saturation; STEMI, ST-elevation myocardial infarction; TIMI, Thrombolysis in Myocardial Infarction; VAS, visual analog scale.
Outcomes
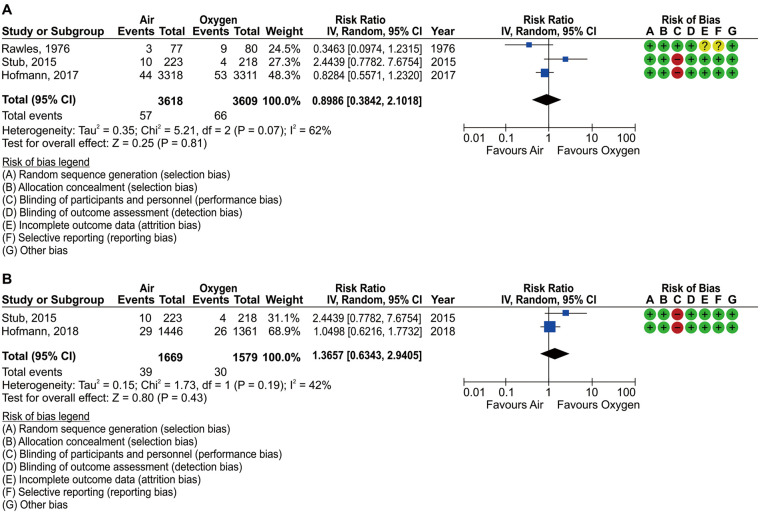
In-Hospital Outcomes Data regarding in-hospital mortality in patients with suspected or confirmed AMI were available from 3 studies.3,7,15 Among the 7,227 patients who were analyzed in this pooled analysis, in-hospital mortality occurred in 123 (66 [1.8%] in the oxygen group and 57 [1.6%] in the ambient air group). Oxygen therapy did not reduce the risk of in-hospital mortality (RR 0.90; 95% CI 0.38–2.10). Statistical heterogeneity was observed among the included studies for in-hospital death (I2=62%; Figure 2A; Supplementary Table 2). We repeated the pooled analysis in the STEMI subgroup, which was available for 2 studies,3,18 including 3,248 patients, and found that oxygen therapy was not associated with decreased in-hospital mortality (RR 1.37; 95% CI 0.63–2.94; Figure 2B; Supplementary Table 3).
Figure 2.
Forest plots of the incidence of in-hospital mortality and risk of bias summaries in patients with (A) suspected or confirmed acute myocardial infarction and (B) ST-elevation myocardial infarction.
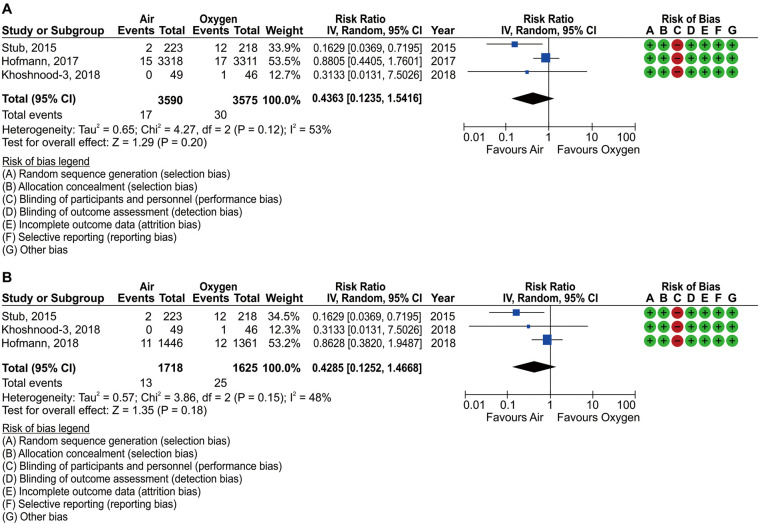
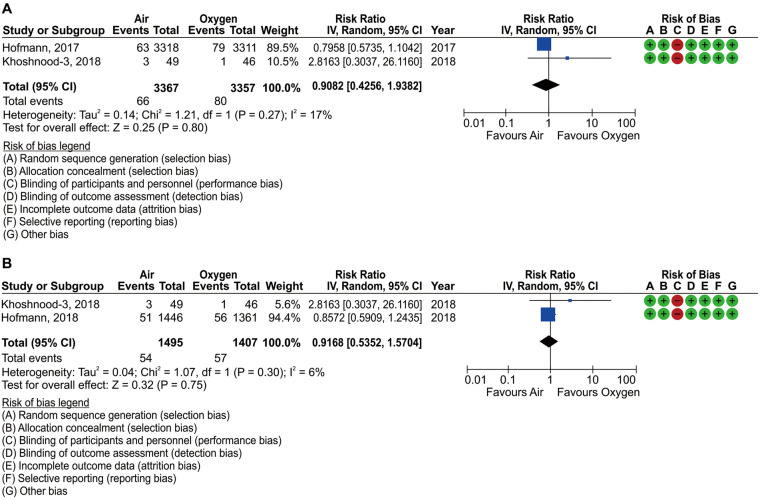
Data regarding in-hospital recurrent MI in patients with suspected or confirmed AMI were available in 3 studies.3,7,17 Among the 7,165 patients who were analyzed in this pooled analysis, in-hospital recurrent MI occurred in 47 (30 [0.8%] in the oxygen group and 17 [0.5%] in the ambient air group). Oxygen therapy did not reduce the risk of in-hospital reinfarction (RR 0.44; 95% CI 0.12–1.54; Figure 3A; Supplementary Table 2). We repeated the pooled analysis in the STEMI subgroup, which was available for 3 studies,3,17,18 including 3,343 patients, and found that oxygen therapy was not associated with decreased in-hospital reinfarction (RR 0.43; 95% CI 0.13–1.47; Figure 3B; Supplementary Table 3).
Figure 3.
Forest plots for the incidence of in-hospital recurrent myocardial infarction (MI) and risk of bias summaries in patients with (A) suspected or confirmed acute myocardial infarction and (B) ST-elevation myocardial infarction.
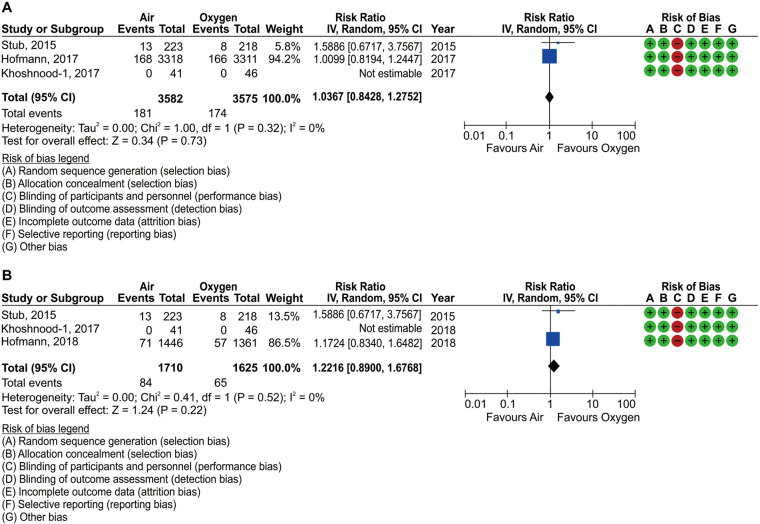
Data regarding cardiac shock in patients with suspected or confirmed AMI were available in 3 studies.3,7,16 Among the 7,181 patients who were analyzed in this pooled analysis, cardiac shock occurred in 112 (53 [1.5%] in the oxygen group and 59 [1.6%] in the ambient air group). Oxygen therapy did not reduce the risk of cardiac shock (RR 1.10; 95% CI 0.77–1.59), with no evidence of statistical heterogeneity (I2=0%; Figure 4A; Supplementary Table 2). We repeated the pooled analysis in the STEMI subgroup, which was available for 3 studies,3,16,18 including 3,359 patients, and found that oxygen therapy was not associated with decreased cardiac shock (RR 1.14; 95% CI 0.78–1.68; Figure 4B; Supplementary Table 3).
Figure 4.
Forest plots of the incidence of in-hospital cardiac shock and risk of bias summaries in patients with (A) suspected or confirmed acute myocardial infarction and (B) ST-elevation myocardial infarction.
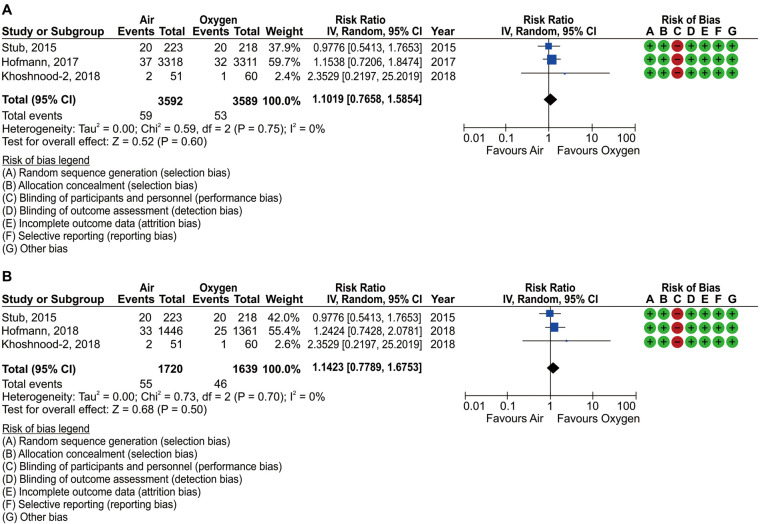
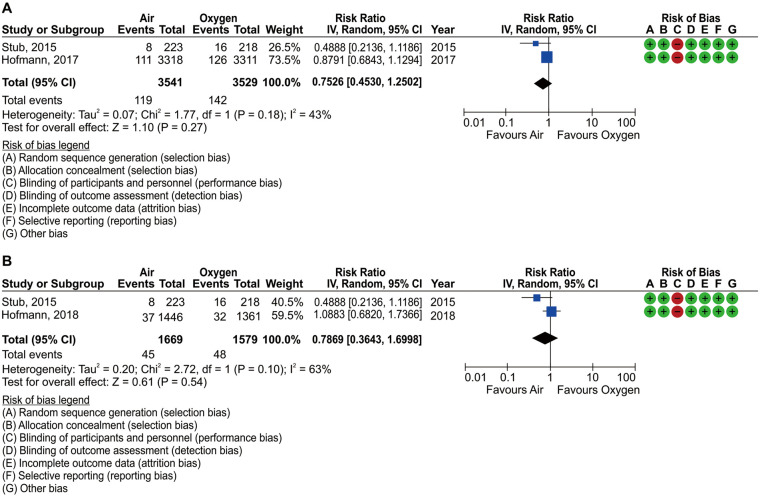
Data regarding cardiac arrest in patients with suspected or confirmed AMI were available in 2 studies.7,17 Among the 6,724 analyzed patients, cardiac arrest occurred in 146 (80 [2.4%] in the oxygen group and 66 [2.0%] in the ambient air group). Oxygen therapy did not reduce the risk of cardiac arrest (RR 0.91; 95% CI 0.43–1.94; Figure 5A; Supplementary Table 2). We repeated the pooled analysis in the STEMI subgroup, which was available for 2 studies,17,18 including 2,902 patients, and found that oxygen therapy was not associated with decreased cardiac arrest (RR 0.92; 95% CI 0.54–1.57; Figure 5B; Supplementary Table 3).
Figure 5.
Forest plots of the incidence of in-hospital cardiac arrest and risk of bias summaries in patients with (A) suspected or confirmed acute myocardial infarction and (B) ST-elevation myocardial infarction.
Outcomes Within 6 Months to 1 Year Data regarding deaths within 6 months to 1 year of onset in patients with suspected or confirmed AMI were available in 3 studies.3,6,7 Among the 7,157 patients who were analyzed in this pooled analysis, death occurred at 6 months to 1 year in 355 (174 [4.9%] in the oxygen group and 181 [5.1%] in the ambient air group). Oxygen therapy did not reduce the risk of death within 6 months to 1 year (RR 1.04; 95% CI 0.84–1.28), with no evidence of statistical heterogeneity (I2=0%; Figure 6A; Supplementary Table 2). We repeated the pooled analysis in the STEMI subgroup, which was available for 3 studies,3,6,18 including 3,335 patients, and found that oxygen therapy was not associated with decreased 6-month to 1-year death rates (RR 1.22; 95% CI 0.89–1.68; Figure 6B; Supplementary Table 3).
Figure 6.
Forests plot of the incidence of mortality between 6 months and 1 year and risk of bias summaries in patients with (A) suspected or confirmed acute myocardial infarction and (B) ST-elevation myocardial infarction.
Data regarding recurrent MI within 6 months to 1 year after onset in patients with suspected or confirmed AMI were available in 2 studies.3,7 Among 7,070 patients who were analyzed in this pooled analysis, 6-month to 1-year reinfarction occurred in 261 (142 [4.0%] in the oxygen group and 119 [3.4%] in the ambient air group). Oxygen therapy did not reduce the risk of 6-month to 1-year reinfarction (RR 0.75; 95% CI 0.45–1.25; Figure 7A; Supplementary Table 2). We repeated the pooled analysis in the STEMI subgroup, which was available for 2 studies,3,18 including 3,248 patients, and found that oxygen therapy was not associated with a decrease in the 6-month to 1-year reinfarction rate (RR 0.79; 95% CI 0.36–1.70; Figure 7B; Supplementary Table 3).
Figure 7.
Forest plots of the incidence of recurrent myocardial infarction (MI) between 6 months and 1 year and risk of bias summaries in patients with (A) suspected or confirmed acute MI and (B) ST-elevation myocardial infarction.
Data regarding heart failure within 6 months to 1 year after onset in patients with suspected or confirmed AMI were available in 2 studies.6,19 Among the 6,716 patients who were analyzed in this pooled analysis, heart failure occurred within 6 months to 1 year in 237 (122 [3.6%] in the oxygen group and 115 [3.4%] in the ambient air group). Oxygen therapy did not reduce the risk of 6-month to 1-year heart failure (RR 0.94; 95% CI 0.73–1.21), with no evidence of statistical heterogeneity (I2=0%; Supplementary Figure 2; Supplementary Table 2).
Arrhythmia Data regarding in-hospital atrial flutter/fibrillation in patients with suspected or confirmed AMI were available in 2 studies.7,17 Among the 6,724 patients who were analyzed in this pooled analysis, atrial flutter/fibrillation occurred in 203 (96 [2.9%] in the oxygen group and 107 [3.2%] in the ambient air group). Oxygen therapy did not reduce the risk of atrial fibrillation/flutter (RR 1.11; 95% CI 0.85–1.46), with no evidence of statistical heterogeneity (I2=0%; Supplementary Figure 3A; Supplementary Table 2). We repeated the pooled analysis in the STEMI subgroup, which was available for 2 studies,17,18 including 2,902 patients, and found that oxygen therapy was not associated with decreased atrial flutter/fibrillation (RR 1.03; 95% CI 0.73–1.45; Supplementary Figure 3B; Supplementary Table 3).
Data regarding in-hospital atrioventricular block in patients with suspected or confirmed AMI were available in 2 studies.7,15 Among the 6,786 patients who were analyzed in this pooled analysis, atrioventricular block occurred in 111 (48 [1.4%] in the oxygen group and 63 [1.9%] in the ambient air group). Oxygen therapy did not reduce the risk of atrioventricular block (RR 1.31; 95% CI 0.90–1.90), with no evidence of statistical heterogeneity (I2=0%; Supplementary Figure 4; Supplementary Table 2).
Cardiac Troponin Levels Two RCTs7,17 reported in-hospital cardiac troponin levels as markers of myocardial necrosis in patients with suspected or confirmed AMI. Among the 6,724 patients who were analyzed in this pooled analysis, oxygen therapy did not reduce the high-sensitivity troponin T levels (MD 34.8; 95% CI −60.3 to 129.9, with no evidence of statistical heterogeneity (I2=0%; Supplementary Figure 5A; Supplementary Table 2). We repeated the pooled analysis in the STEMI subgroup, which was available for 2 studies, including 2,902 patients, and found that oxygen therapy was not associated with decreased high-sensitivity troponin T levels (MD 138.3; 95% CI −79.0 to 355.6; Supplementary Figure 5B; Supplementary Table 3).
Infarct Size Two RCTs3,17 reported infarct size using cardiac magnetic resonance imaging (CMR) in patients with STEMI. Among the 536 patients analyzed in this pooled analysis, oxygen therapy did not reduce infarct size by CMR (MD −2.11; 95% CI −5.90 to 1.68), with evidence of statistical heterogeneity (I2=65%; Supplementary Figure 6; Supplementary Table 3).
Chest Symptoms and Morphine Two RCTs16,20 reported on chest symptoms, scored using a visual analog scale (VAS), in patients with suspected or confirmed AMI. Among the 733 patients who were analyzed in this pooled analysis, oxygen therapy significantly increased VAS scores (MD −1.00; 95% CI −1.51 to −0.49), with no evidence of statistical heterogeneity (I2=0%; Supplementary Figure 7; Supplementary Table 2).
Data regarding the use of morphine in patients with suspected or confirmed AMI were available in 2 studies.15,16 Among the 268 patients analyzed in this pooled analysis, morphine was administered to 190 (106 [76%] in the oxygen group and 84 [65%] in the ambient air group). Oxygen therapy did not reduce morphine use (RR 0.86; 95% CI 0.70–1.06; Supplementary Figure 8A; Supplementary Table 2). These 2 RCTs15,16 also reported that the dosage of morphine in patients with suspected or confirmed AMI was not associated with the need for oxygen therapy (MD −0.86; 95% CI −2.68 to 0.97; Supplementary Figure 8B; Supplementary Table 2).
Risk of Bias, Publication Bias, and Quality of Evidence The risks of bias, namely random generation, allocation concealment, blinding for participants and personnel, blinding for outcome assessor, incomplete outcome data, selective outcome reporting, and other bias, were evaluated for each study. Almost all the included studies used incomplete blinding. The study protocol could not be obtained for the study of Rawles and Kenmure,15 so it is not known whether the outcome data are complete. We judged the level of evidence as very low and could not determine the presence of publication bias. For reference, visual inspection of funnel plots revealed no asymmetry in critical outcomes in patients with suspected or confirmed AMI (Supplementary Figures 9–12). We assessed the certainty of evidence for each outcome and the findings are summarized in Supplementary Tables 2 and 3.
Discussion
This meta-analysis failed to find evidence supporting the use of oxygen therapy in normoxic patients with AMI. Based on existing evidence, oxygen therapy seems to have no additional benefit in patients with normal baseline oxygen levels. We also noted no harm of supplemental oxygen therapy on critical outcomes, such as in-hospital mortality, cardiac shock, cardiac arrest, and MI, or on mortality between 6 months and 1 year.
The present study examined patients with suspected AMI and those with STEMI. We also examined the results of the DETO2X-AMI trial, which included a large number of patients with AMI and was reported after the AVOID study, in this meta-analysis and analyzed long-term (6 months to 1 year) and short-term (in-hospital) outcomes. Both psychological and physiological effects were evaluated in patients with AMI receiving oxygen therapy.
There were only 2 RCTs of AMI patients on room air for vs. supplemental oxygen therapy as prehospital emergency care.3,15 Subsequently, the results of the SOCCER and DETO2X-AMI trials were reported; both these studies included a wide range of patients in terms of MI diagnosis.6,7,16–20 In the present study, we focused on patients with suspected AMI or STEMI.
All studies included in this meta-analysis were RCTs, and we found no significant differences in the critical outcomes of patients with suspected AMI or STEMI. The AVOID study showed that supplemental oxygen therapy in STEMI patients may increase early myocardial injury and is associated with a larger myocardial infarct size at 6 months.3 High-flow oxygen reduces epicardial coronary flow,21 increases coronary vascular resistance, and affects the microcirculation,22 leading to functional oxygen shunting.23 Rates of in-hospital recurrent MI and arrhythmia were also increased in normoxic patients administered supplemental oxygen. CoSTR suggests withholding oxygen vs. routine oxygen supplementation in normoxic patients with AMI.4
However, the present study demonstrated no significant differences in in-hospital and 6-month/1-year events. The DETO2X-AMI trial demonstrated no significant differences in in-hospital mortality, recurrent MI, arrhythmia, or 30-day and 1-year mortality between the oxygen and ambient air groups. The AVOID and DETO2X-AMI trials differed in several ways. The DETO2X-AMI included 6,629 randomized patients with suspected AMI, whereas the AVOID trial randomized only 638 patients with STEMI. The DETO2X-AMI trial enrolled only patients with an SpO2 ≥90% who were administered oxygen at a rate of 6 L/min through an open face mask. In contrast, a lower limit of 94% SpO2 was used in the AVOID trial, and oxygen was administered at a rate of 8 L/min through a closed mask. The present study did not determine whether oxygen administration is effective or harmful in normoxic (SpO2 ≥90%) patients during the acute phase of MI. However, high-flow oxygen masks (≥6 L/min) were examined, and low-flow oxygen masks and nasal cannulas have not been examined in any RCTs. Although there is not sufficient evidence to determine whether oxygen should be used, high-flow oxygen administration to normoxic patients in the acute phase of MI appears unnecessary.
Oxygen may provide psychological and physiological benefits to patients with anxiety during AMI.24 Our data suggest no difference in the use and dosage of morphine between the oxygen and ambient air groups. However, the VAS score for chest symptoms, which was subjectively assessed in AMI patients, was increased by oxygen therapy vs. ambient air. In addition to yielding comparable results to ambient air on other physiological events, oxygen therapy may become useless if it is psychologically harmful.
This study has several limitations. First, an electronic search of PubMed was performed from inception to June 2020 with a language restriction (English). We did not search other electronic databases, such as MEDLINE, Web of Science, and Cochrane Central Register of Controlled Trials, or perform searches without language restrictions. Second, the present study included trials with heterogeneous designs, patient characteristics, and endpoints. The studies included were all RCTs, but they were single-blind, double-blind, or open-label studies. The studies had different definitions of normoxic patients (SpO2 ≥94% in the AVOID and SOCCER trials; SpO2 ≥90% in the DETO2X-AMI trial) and different periods of oxygen administration. It should be noted that this study cannot rule out a benefit of oxygen therapy in the SpO2 range 90–94%. The detrimental effects of oxygen therapy in patients with AMI with an SpO2 of 90% may require further examination.
In conclusion, this meta-analysis showed that routine administration of supplemental oxygen may not have beneficial or harmful effects, and that high-flow oxygen may be unnecessary in normoxic patients in the acute phase of MI.
Sources of Funding
Funding for this study was provided by the Japan Resuscitation Council and the Japanese Circulation Society Emergency and Critical Care Committee.
Disclosures
T. Matoba is a member of Circulation Reports’ Editorial Team. The remaining authors declare no conflicts of interest.
Author Contributions
All authors were involved in the study design. S.K. and T.Y. identified the studies included in the meta-analysis and analyzed the data. S.K. and T.Y. drafted the manuscript. Y.T., M.K., T. Matoba, and H.N. reviewed the manuscript. All authors were involved in data interpretation and discussion. All authors had full access to all data (including statistical reports and tables) in the study, take responsibility for its integrity and the accuracy of the analysis, and read and approved the final manuscript.
Supplementary Files
Table of Contents Supplementary Table 1. Patient Characteristics Supplementary Table 2. Evidence Profiles of Patients With Suspected or Confirmed AMI Supplementary Table 3. Evidence Profile of Patients With STEMI Supplementary Figure 1. Retrieval keywords for article search Supplementary Figure 2. Forest plot for the incidence of 6-month to 1-year heart failure and risk of bias summary in patients with suspected or confirmed AMI Supplementary Figure 3. Forest plot for the incidence of in-hospital atrial fibrillation/flutter and risk of bias summary Supplementary Figure 4. Forest plot for the incidence of in-hospital atrioventricular block and risk of bias summary in patients with suspected or confirmed AMI Supplementary Figure 5. Forest plot for the incidence of cardiac troponin T levels and risk of bias summary Supplementary Figure 6. Forest plot for the incidence of in-hospital CMR and risk of bias summary in patients with STEMI Supplementary Figure 7. Forest plot for the incidence of chest symptoms using the visual analog scale and risk of bias summary in patients with suspected or confirmed AMI Supplementary Figure 8. Forest plot for morphine and risk of bias summary in patients with suspected or confirmed AMI Supplementary Figure 9. Funnel plot of the comparison between oxygen and ambient air for mortality outcome in patients with suspected or confirmed AMI Supplementary Figure 10. Funnel plot of the comparison between oxygen and ambient air for the outcome of recurrent MI in patients with suspected or confirmed AMI Supplementary Figure 11. Funnel plot of the comparison between oxygen and ambient air for the outcome of cardiac shock in patients with suspected or confirmed AMI Supplementary Figure 12. Funnel plot of the comparison between oxygen and ambient air for the outcome of cardiac arrest in patients with suspected or confirmed AMI
Acknowledgments
The authors thank the staff of the Japan Council for Quality Health Care (Minds Tokyo GRADE Center) and Dr. Morio Aihara for their assistance using the GRADE approach. The authors also thank Editage (www.editage.com) for help with English language editing.
References
- 1. Kuwabara M, Mori M, Komoto S.. Japanese national plan for promotion of measures against cerebrovascular and cardiovascular disease. Circulation 2021; 143: 1929–1931. [DOI] [PubMed] [Google Scholar]
- 2. Kimura K, Kimura T, Ishihara M, Nakagawa Y, Nakao K, Miyauchi K, et al.. JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ J 2019; 83: 1085–1196. [DOI] [PubMed] [Google Scholar]
- 3. Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray JE, et al.. Air versus oxygen in ST-segment-elevation myocardial infarction. Circulation 2015; 131: 2143–2150. [DOI] [PubMed] [Google Scholar]
- 4. Nikolaou NI, Welsford M, Beygui F, Bossaert L, Ghaemmaghami C, Nonogi H, et al.. Part 5: Acute coronary syndromes: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 2015; 95: e121–e146. [DOI] [PubMed] [Google Scholar]
- 5. de Alencar Neto JN.. Morphine, oxygen, nitrates, and mortality reducing pharmacological treatment for acute coronary syndrome: An evidence-based review. Cureus 2018; 10: e2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Khoshnood A, Akbarzadeh M, Roijer A, Meurling C, Carlsson M, Bhiladvala P, et al.. Effects of oxygen therapy on wall-motion score index in patients with ST elevation myocardial infarction: The randomized SOCCER trial. Echocardiography 2017; 34: 1130–1137. [DOI] [PubMed] [Google Scholar]
- 7. Hofmann R, James SK, Jernberg T, Lindahl B, Erlinge D, Witt N, et al.. Oxygen therapy in suspected acute myocardial infarction. New Engl J Med 2017; 377: 1240–1249. [DOI] [PubMed] [Google Scholar]
- 8. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al.. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J Clin Epidemiol 2009; 62: e1–e34. [DOI] [PubMed] [Google Scholar]
- 9. Moher D, Liberati A, Tetzlaff J, Altman DG; The PRISMA Group.. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 2009; 6: e1000097. [PMC free article] [PubMed] [Google Scholar]
- 10. Atkins D, Eccles M, Flottorp S, Guyatt GH, Henry D, Hill S, et al.. Systems for grading the quality of evidence and the strength of recommendations I: Critical appraisal of existing approaches the GRADE working group. BMC Health Serv Res 2004; 4: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al.. Grading quality of evidence and strength of recommendations. BMJ (Clin Res Ed) 2004; 328: 1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mustafa RA, Santesso N, Brozek J, Akl EA, Walter SD, Norman G, et al.. The GRADE approach is reproducible in assessing the quality of evidence of quantitative evidence syntheses. J Clin Epidemiol 2013; 66: 736–742. [DOI] [PubMed] [Google Scholar]
- 13. Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A.. GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol 2011; 64: 380–382. [DOI] [PubMed] [Google Scholar]
- 14. Huedo-Medina TB, Sanchez-Meca J, Marin-Martinez F, Botella J.. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods 2006; 11: 193–206. [DOI] [PubMed] [Google Scholar]
- 15. Rawles JM, Kenmure AC.. Controlled trial of oxygen in uncomplicated myocardial infarction. Br Med J 1976; 1: 1121–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Khoshnood A, Akbarzadeh M, Carlsson M, Sparv D, Bhiladvala P, Mokhtari A, et al.. Effect of oxygen therapy on chest pain in patients with ST elevation myocardial infarction: Results from the randomized SOCCER trial. Scand Cardiovasc J 2018; 52: 69–73. [DOI] [PubMed] [Google Scholar]
- 17. Khoshnood A, Carlsson M, Akbarzadeh M, Bhiladvala P, Roijer A, Nordlund D, et al.. Effect of oxygen therapy on myocardial salvage in ST elevation myocardial infarction: The randomized SOCCER trial. Eur J Emerg Med 2018; 25: 78–84. [DOI] [PubMed] [Google Scholar]
- 18. Hofmann R, Witt N, Lagerqvist B, Jernberg T, Lindahl B, Erlinge D, et al.. Oxygen therapy in ST-elevation myocardial infarction. Eur Heart J 2018; 39: 2730–2739. [DOI] [PubMed] [Google Scholar]
- 19. Jernberg T, Lindahl B, Alfredsson J, Berglund E, Bergstrom O, Engstrom A, et al.. Long-term effects of oxygen therapy on death or hospitalization for heart failure in patients with suspected acute myocardial infarction. Circulation 2018; 138: 2754–2762. [DOI] [PubMed] [Google Scholar]
- 20. Sparv D, Hofmann R, Gunnarsson A, James S, Hedberg C, Lauermann J, et al.. The analgesic effect of oxygen in suspected acute myocardial infarction: A substudy of the DETO2X-AMI trial. JACC Cardiovasc Interv 2018; 11: 1590–1597. [DOI] [PubMed] [Google Scholar]
- 21. Farquhar H, Weatherall M, Wijesinghe M, Perrin K, Ranchord A, Simmonds M, et al.. Systematic review of studies of the effect of hyperoxia on coronary blood flow. Am Heart J 2009; 158: 371–377. [DOI] [PubMed] [Google Scholar]
- 22. Kenmure AC, Murdoch WR, Beattie AD, Marshall JC, Cameron AJ.. Circulatory and metabolic effects of oxygen in myocardial infarction. Br Med J 1968; 4: 360–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reinhart K, Bloos F, Konig F, Bredle D, Hannemann L.. Reversible decrease of oxygen consumption by hyperoxia. Chest 1991; 99: 690–694. [DOI] [PubMed] [Google Scholar]
- 24. Atar D.. Should oxygen be given in myocardial infarction? BMJ (Clin Res Ed) 2010; 340: c3287. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table of Contents Supplementary Table 1. Patient Characteristics Supplementary Table 2. Evidence Profiles of Patients With Suspected or Confirmed AMI Supplementary Table 3. Evidence Profile of Patients With STEMI Supplementary Figure 1. Retrieval keywords for article search Supplementary Figure 2. Forest plot for the incidence of 6-month to 1-year heart failure and risk of bias summary in patients with suspected or confirmed AMI Supplementary Figure 3. Forest plot for the incidence of in-hospital atrial fibrillation/flutter and risk of bias summary Supplementary Figure 4. Forest plot for the incidence of in-hospital atrioventricular block and risk of bias summary in patients with suspected or confirmed AMI Supplementary Figure 5. Forest plot for the incidence of cardiac troponin T levels and risk of bias summary Supplementary Figure 6. Forest plot for the incidence of in-hospital CMR and risk of bias summary in patients with STEMI Supplementary Figure 7. Forest plot for the incidence of chest symptoms using the visual analog scale and risk of bias summary in patients with suspected or confirmed AMI Supplementary Figure 8. Forest plot for morphine and risk of bias summary in patients with suspected or confirmed AMI Supplementary Figure 9. Funnel plot of the comparison between oxygen and ambient air for mortality outcome in patients with suspected or confirmed AMI Supplementary Figure 10. Funnel plot of the comparison between oxygen and ambient air for the outcome of recurrent MI in patients with suspected or confirmed AMI Supplementary Figure 11. Funnel plot of the comparison between oxygen and ambient air for the outcome of cardiac shock in patients with suspected or confirmed AMI Supplementary Figure 12. Funnel plot of the comparison between oxygen and ambient air for the outcome of cardiac arrest in patients with suspected or confirmed AMI