Abstract
The ongoing coronavirus disease 2019 pandemic has forced providers to dramatically scale down in-person clinic visits to enforce social distancing and triage care to the neediest patients. We describe our five-month experience with a hybrid gastroenterology electronic consultation programme starting in 2019 in which we perform electronic consultations for every referral regardless of indication as well as directly initiate telephone-based telehealth visits with patients without the need for in-person clinic. Over five consecutive months, 1243 hybrid electronic consultations were performed with 356 (29%) resulting in a clinic appointment. The remaining 887 (71%) electronic consultations were resolved without need for a clinic visit. Five hundred and fourteen (41%) electronic consultations resulted in a directly scheduled procedure without clinic appointment. Eighty-five per cent of electronic consultations were performed on the same day of referral and 98% of electronic consultations were completed in under 20 min. A hybrid electronic consultation model which pre-emptively reviews all outpatient referrals streamlines access to specialty care. Such a model may be implemented rapidly during the current coronavirus disease 2019 pandemic as well as serve as a platform for long-term improvement in efficiency of care.
Keywords: eHealth, pandemic; telehealth; telemedicine; remote consultation; gastroenterology
Introduction
Telemedicine includes many services such as telehealth, virtual check-ins, remote monitoring services and electronic consultations (e-consults). Telehealth uses audio and visual systems to communicate with patients in real time but is subject to strict limitations on patient location (rural and established medical settings only), modality (video only) and prior existing relationship with the patient.1
By contrast, an e-consult is an asynchronous (not in real time) communication between referring providers and specialists without contacting the patient. E-consults allow referring providers to leverage expertise from specialists on a formal basis within a secure platform.2 However, e-consults do not mimic in-person visits with the patient and if a problem cannot be adequately addressed between providers, a traditional in-person consultation with the patient is required.
The emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in 2019, and its rapid evolution into the coronavirus disease 2019 (COVID-19) pandemic in early 2020, necessitates broad implementation of traditional public health measures such as social distancing, quarantine and containment.3 In this new reality, telemedicine has been recognised as uniquely well-placed to serve both patients with COVID-19 as well as patients with other healthcare needs who now must remain isolated.4,5 Indeed, many hospitals and clinics are rapidly expanding telemedicine services especially in light of recent Centers for Disease Control and Prevention guidance to limit non-urgent outpatient visits6 and the decision by payors to expand reimbursement for telemedicine. Yet experience with telemedicine on this scale in gastroenterology is lacking just as implementation is accelerating.7 Our hybrid e-consult programme, where traditional e-consults were performed on all referrals and supplemented by telehealth consultations directly with the patient as needed, anticipated what many healthcare systems are now implementing during the COVID-19 pandemic. We describe our experience with hybrid e-consults and discuss the potential as a model for managing referrals during the pandemic and beyond.
Methods
We performed hybrid e-consults on all new patient referrals to gastroenterology at CommUnityCare (CUC) Health Centers, a Federally Qualified Heath Center (FQHC) with 20 primary care clinics located throughout the Austin, Texas, USA metropolitan area. Sources of referral included all primary care clinics at CUC as well as other local clinics serving patients with no insurance or supported by health coverage programmes.
Prior to implementing our e-consults initiative, all new gastroenterology referrals were initially evaluated by registered nurses (RNs) against a detailed list of pre-written criteria, which included certain laboratory tests or imaging results that must be available before a patient can be scheduled for a clinic visit. If the results of all the tests were not available, the referring provider was asked to order those tests and refer again when the results were available. All patients were scheduled for an in-person visit, including those who mainly needed an endoscopic procedure such as screening or surveillance colonoscopy.
The hybrid e-consult programme began in September 2019 and modified the previous process by requiring all new referrals be evaluated by a gastroenterologist at the time of referral. Upon receiving a new referral, we reviewed patient records in the electronic health record (EHR) of CUC as well as other healthcare systems. We then decided if the patient needed to be called to obtain more history. If laboratory tests, imaging or medical records were still required after the above steps, we requested them from the referring providers and asked them to refer again after obtaining the missing information.
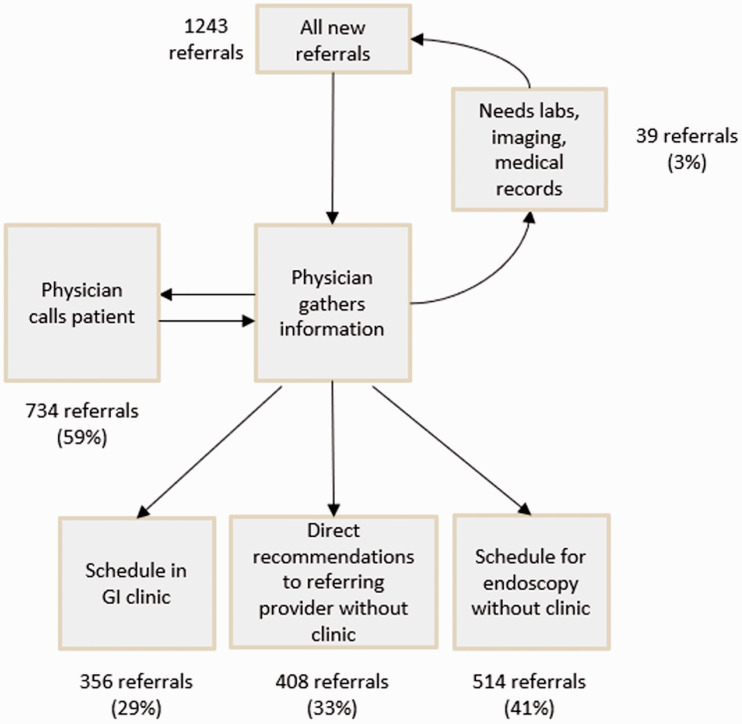
After evaluating all relevant information, we resolved the hybrid e-consult with one of three non-exclusive outcomes. First, patients were scheduled an appointment in the Gastroenterology (GI) clinic if they had complex functional bowel disease, inflammatory bowel disease, cirrhosis or other conditions benefiting from longitudinal follow-up. Clinic appointments were also scheduled if a patient could not be reached by telephone on two attempts over separate days. Second, some referrals were resolved with direct recommendations made to the referring provider. Unlike traditional e-consults, recommendations to the referring provider could be made with or without a conversation with the patient, depending on clinical necessity. Finally, if a patient needed an endoscopic procedure, it was directly scheduled after speaking to the patient without an in-person clinic visit purely to evaluate the need for procedure (Figure 1).
Figure 1.
GI, Gastroenterology workflow.
Electronic consultation (e-consult) workflow.
We analysed hybrid e-consults conducted for five consecutive months from 6 September 2019–6 February 2020. Referral indications were categorised as colon cancer screening or surveillance, general GI subcategories, pancreaticobiliary or liver disease subcategories.
Results
During the study period, 1243 hybrid e-consults were performed for 1188 patients with a median of 11 referrals per workday (interquartile range (IQR) 6–14). Indications for referral included general GI (61%), colorectal cancer screening or surveillance (24%), liver disease (15%) and pancreaticobiliary (3%) (Table 1).
Table 1.
Indications for outpatient referral.
| Number of referrals | Percentage of total | |
|---|---|---|
| General Gastroenterology | 753 | 60.6 |
| Abdominal pain | 193 | 15.5 |
| Abnormal imaging | 27 | 2.2 |
| Anaemia | 75 | 6 |
| GI bleed | 145 | 11.7 |
| Constipation | 28 | 2.3 |
| Heartburn | 68 | 5.5 |
| Dysphagia | 70 | 5.6 |
| Diarrhoea | 44 | 3.5 |
| Nausea | 22 | 1.8 |
| Anorectal disease | 19 | 1.5 |
| Helicobacter pylori | 18 | 1.4 |
| Weight loss | 9 | 0.7 |
| Feeding tube | 9 | 0.7 |
| Inflammatory bowel disease | 8 | 0.6 |
| Diverticular disease | 9 | 0.7 |
| Hospital follow-up | 12 | 1 |
| Other miscellaneous | 34 | 2.7 |
| Colorectal cancer screening or surveillance | 300 | 24.1 |
| Liver disease | 190 | 15.3 |
| Elevated liver enzymes | 71 | 5.7 |
| Cirrhosis | 83 | 6.7 |
| Non-alcoholic fatty liver disease | 12 | 1 |
| Abnormal liver imaging | 13 | 1 |
| Other miscellaneous | 29 | 2.3 |
| Pancreaticobiliary | 38 | 3.1 |
| Total | 1243 | 100 |
As a result of the hybrid e-consult process, an in-person clinic appointment was made for 356 (29%) referrals. The referral was resolved without need for an in-person clinic appointment in 887 (71%) of e-consults.
Sixty-three (5%) patients could not be reached over the phone after multiple attempts and were therefore scheduled for the in-person clinic. Twenty-six referrals (2%) were repeat referrals for questions addressed during a previous e-consult. Overall, 85% of e-consults were resolved on the same day of referral with 98% resolved within one week of referral. 91% of e-consults were completed in less than 15 min with 2% of e-consults needing more than 20 min.
Discussion
Our experience with hybrid e-consults for all outpatient gastroenterology referrals over a consecutive five-month period demonstrated that most referral questions could be resolved without in-person clinic visits on the same day of consultation and can be conducted within timeframes allotted for a typical in-person clinic visit.
In March 2020, the COVID-19 public health emergency prompted Centers for Medicare and Medicaid Services (CMS) to expand telemedicine benefits on a temporary and emergency basis under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act. The main change includes making payments for services to beneficiaries in any healthcare facility and at home.8 These changes have also been mirrored by private insurers.9 The changes in reimbursement, along with the Centers for Disease Control and Prevention (CDC) recommendations to limit in-person clinic visits has resulted in most hospitals and clinics initiating some form of telemedicine.
Our hybrid e-consult model, where we reviewed all new referrals, called most patients, and then decided on the need for an in-person clinic visit, more closely aligns with present needs during the COVID-19 health emergency. Recommendations for the next step of diagnosis or management were provided for 71% of referrals without the need for a face-to-face visit. Most referrals were answered on the same day as received and almost all e-consults were completed in under 20 min consistent with physician time commitments during face-to-face visits, even including physician documentation time, chart review, attempting to contact the patient and conversation with the patient. Patients who needed endoscopies were directly scheduled for the procedure after telephone discussions with the patient. Most of the referrals were new patients, hence we erred on the side of clinic referral when we felt a face-to-face visit would facilitate counselling or if the patient would likely need periodic clinic follow-up visits. We believe that, as reimbursement policies increasingly reward providers for time spent in patient counselling and as familiarity with and acceptance of e-consults grows, the need for clinic visits will decrease further.
It is important to highlight unique features of our hybrid e-consult. First, e-consult is conventionally described as a provider-to-provider conversation. In our hybrid e-consult programme, we extended this communication to the patient as we believed it allowed us to obtain a full history and discuss our recommendations directly, closely mimicking an in-person visit. Recommendations were communicated with the referring physician, who continued to be part of the care plan. Referring physicians were asked to order general work-up such as laboratory and imaging tests while gastroenterology specific procedures, including endoscopies and manometry, were arranged by the gastroenterologist. This facilitated overall care and avoided clinic visits with incomplete information. Informal feedback from both referring physicians and patients was very positive.
Second, we called patients on the phone rather than with live video. We did not have the requisite technology and, based on our experience at other institutions, patients found phone conversations more convenient since there were minimal technological barriers and a phone was more likely to be carried on the patient. The flexibility and ease of using a phone made it possible for us to respond to referrals within a day, which we feel is more important than use of live video. Further, most e-consults did not require a physical examination and could be satisfactorily completed with just a phone conversation. Those patients whose problems necessitated a physical exam, were given clinic appointments. Notably, the COVID-19 waiver continues to require provision of telemedicine services through live video. We were able provide our e-consult services despite these limits because patients were referred from a FQHC and we did not charge a fee for our service.
Third, telemedicine has traditionally been approved by payors only for established patients. We have described our e-consults for all new patients. Many of these patients received telephonic follow-up after a few days to weeks to ensure response to treatment. Telemedicine for established versus new patient is predicated on the idea of patient-physician relationship. All states allow a physician to establish a relationship with a new patient via telemedicine, though there may be differences related to location of the patient, the modality used for telemedicine or if the consultation is requested by another provider who has a conventional established relationship with the patient.
In addition, gastroenterology telemedicine programmes previously described in the literature are largely limited to addressing a specific digestive subspecialty area or disease such as inflammatory bowel disease or chronic hepatitis C.10,11 E-consult programmes which address all indications for referral have relied on referring physicians to decide which patients were best served with e-consults.12–15 To our knowledge, our programme is the only gastroenterology telemedicine programme that addresses every referral for any indication with e-consults before consideration of an in-person clinic visit. By using our programme to address all gastroenterology referrals, we demonstrate that expanding e-consults to all referrals results in avoidance of in-person clinic visits to the same degree as selective e-consults initiated by referring physicians.12–15
Our objectives with e-consults were to decrease waiting time for clinic appointments, avoid redundant encounters, provide prompt patient-centric care and work closely with referring providers. Over the study period, we were able to decrease typical wait times to first clinic appointment from 7 months to 2 weeks. This improvement in clinic wait times could alter referring provider behaviour towards high-value care. For example, a barium oesophagogram was frequently ordered by primary care providers for refractory heartburn out of a desire to work up patients waiting for clinic, even though the barium oesophagogram is no longer recommended for this indication.16 Another benefit of decreasing the number of clinic visits is that this allows providers to spend an appropriate amount of time with the patients when they are actually seen in clinic. Before the e-consult programme, patients were scheduled for 20-minute visits including those with complex needs. This scenario is not unique to our clinics. Further, prompt consultations for urgent issues may reduce emergency room visits, the importance of which is especially highlighted during the COVID-19 epidemic.
Our experience suggests that restrictions on telemedicine such as mandating the use of video, initiation of calls by patients, offering services only to established patients and limiting communications to those between only referring providers and specialists are unnecessary and would make it more difficult to take advantage of the full potential of telemedicine.
Our report lacks data on clinical outcomes such as emergency room visits and hospital admissions. However, e-consults are unlikely to harm access to urgent care since we reviewed most referrals on the same day and scheduled urgent endoscopy or directed patients to the hospital for those referrals. Another limitation is the lack of patient-reported outcomes such as patient satisfaction surveys. However, out all the patients we called, only one patient requested a clinic appointment after talking with us and only 2% of referrals were repeat referrals for a problem previously addressed with e-consults. Another limitation is generalisability especially since we used phone calls instead of live video which may limit re-imbursement even after recent CMS rule changes. However, we feel that our e-consult framework would be equally effective using live video since providers may simply arrange for a time for a live video appointment. For those patients without easy access to live video platforms, efficient patient care should take priority over re-imbursement concerns especially in non-fee-for-service models. In fact, phone consultations are supported in England17 and our experience should give pause to policy makers and payors who insist on video calls as the primary modality of telemedicine. We intend to continue to adjust our e-consult platform during and after the current COVID-19 pandemic to further improve its effectiveness as well as build out economic analysis models to assess the applicability of this platform to practices beyond our own.
In conclusion, a hybrid e-consult programme, which reviews all new outpatient GI referrals and combines telehealth patient visits with provider-to-provider communications is prompt and effective in answering referral questions by emphasising direct patient communications. This model sharply decreases the necessity for in-person clinic appointments while streamlining access to necessary procedures. The COVID-19 pandemic will force broad implementation of telemedicine programmes and our collective experience at this time will lead to broader implementation of effective telemedicine consultation in the future.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Zhouwen Tang https://orcid.org/0000-0001-7600-1008
References
- 1.Centers for Medicare and Medicaid Services. Telehealth services, https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/TelehealthSrvcsfctsht.pdf (2020, accessed 24 March 2020).
- 2.Vimalananda VG, Gupte G, Seraj SM, et al. Electronic consultations (e-consults) to improve access to specialty care: A systematic review and narrative synthesis. J Telemed Telecare 2015; 21: 323–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilder-Smith A, Freedman DO.Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med; 27, 10.1093/jtm/taaa020 (accessed March 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; 26: 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hollander JE, Carr BG.Virtually perfect? Telemedicine for Covid-19. N Engl J Med. Epub ahead of print 11 March 2020. DOI: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 6.Abelson R. Doctors and patients turn to telemedicine in the coronavirus outbreak. New York Times, 11 March 2020, p. 4.
- 7.The Lancet Gastroenterology & Hepatology. The potential of telemedicine in digestive diseases . Lancet Gastroenterol Hepatol 2019; 4: 185. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Medicare and Medicaid Services. Medicare telemedicine health care provider fact sheet, https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet (accessed 24 March 2020).
- 9.American Gastroenterological Association. Commercial COVID-19 telehealth coding policies, https://aga-cms-assets.s3.amazonaws.com/202046183547---COM20-010%20Commercial%20COVID-19%20telehealth%20coding%20policies_Apr%206_FINAL.pdf (2020, accessed 25 March 2020).
- 10.Siegel CA.Transforming gastroenterology care with telemedicine. Gastroenterology 2017; 152: 958–963. [DOI] [PubMed] [Google Scholar]
- 11.Helsel BC, Williams JE, Lawson K, et al. Telemedicine and mobile health technology are effective in the management of digestive diseases: A systematic review. Dig Dis Sci 2018; 63: 1392–1408. [DOI] [PubMed] [Google Scholar]
- 12.Wrenn K, Catschegn S, Cruz M, et al. Analysis of an electronic consultation program at an academic medical centre: Primary care provider questions, specialist responses, and primary care provider actions. J Telemed Telecare 2017; 23: 217–224. [DOI] [PubMed] [Google Scholar]
- 13.North F, Uthke LD, Tulledge-Scheitel SM.Internal e-consultations in an integrated multispecialty practice: A retrospective review of use, content, and outcomes. J Telemed Telecare 2015; 21: 151–159. [DOI] [PubMed] [Google Scholar]
- 14.Venkatesh RD, Campbell EJ, Thiim M, et al. E-consults in gastroenterology: An opportunity for innovative care. J Telemed Telecare 2019; 25: 499–505. [DOI] [PubMed] [Google Scholar]
- 15.Keely E, Canning S, Saloojee N, et al. Improving access to gastroenterologist using econsultation: A way to potentially shorten wait times. J Can Assoc Gastroenterol 2018; 1: 124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katz PO, Gerson LB, Vela MF.Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 2013; 108: 308–328. [DOI] [PubMed] [Google Scholar]
- 17.NHS England. Using phone consultations, https://www.england.nhs.uk/wp-content/uploads/2016/03/releascapcty-case-study-2-183.pdf (2016, accessed 23 March 2020).