Abstract
Objectives
The aim of this study was to examine the characterization of tumors and tumor-like lesions located in the clavicle and to present their clinical results.
Patients and methods
Between January 2006 and December 2018, a total of 44 patients (25 males, 19 females; mean age: 36.2±21.8 years; range, 2 to 87 years) who were operated in our clinic for a clavicular lesion were included. Among 4,856 extremity tumors operated in our clinic between these years, 44 cases (0.9%) located in the clavicle were eligible. Demographic data, tumor types, location, surgical method, metastasis, survival analyzes and clinical results of these patients were reviewed retrospectively. According to the clavicle location, the patients were divided into groups according to their involvement in proximal, middle, lateral and more than one region.
Results
The most frequently involved site was the lateral edge of the clavicle, and the most common tumor was aneurysmal bone cyst. The most common malignant tumor was Ewing sarcoma and plasmacytoma (13.6%) and the most common surgical method in the clavicle was wide resection with 34.1%. Of the 38 primary clavicle tumors remaining after the metastatic lesions were removed, 21 (55%) were benign, while 17 (45%) were malignant. Aneurysmal bone cyst was most common in the group under 30 years of age, osteochondroma was most common in the 30-50 age group, and plasmacytoma was most common in those over 50 years of age. The mean musculoskeletal tumor society (MSTS) score of 15 patients (34.1%) who underwent clavicle resection was 79.4±6.
Conclusion
We believe that a wide spectrum should be considered in the differential diagnosis of tumors located in the clavicle. Age is an important predictive factor for malignancy. We believe that resection should be applied without fear considering its effects on function and recurrence.
Keywords: Age, clavicle, outcome, tumor.
Introduction
Bone tumors of the clavicle are exceedingly rare with a reported frequency of less than 1% of all bone tumors. The literature contains case reports or few case series. Therefore, even those dealing with orthopedic oncology have very little experience with clavicle tumors.[1] It is assumed that there are two reasons why clavicle tumors are rare. It has little red marrow due to poor blood supply and lack of medullary cavity.[2]
The clavicle is an unusual bone with many unique features. It acts as a bridge between the axial and appendicular skeleton and joins the shoulder girdle. The bone can be divided into three parts; medial, lateral and the shaft. It is the only bone in the long bones whose anatomical position is on the horizontal axis. It has no medullary cavity and ossifies by membranous ossification. It contains two primary ossification centers and only one secondary ossification center. It is the first ossified bone in the embryo probably at five months. During the first five years, its further development occurs in the diaphysis from intramembranous ossification. Later, the more characteristic endochondral ossification of tubular bones takes place at the acromial and sternal ends. A classic radiologically evident epiphysis appears only at the sternal end. It develops in adolescence and eventually fuses between the ages of 21 and 25 years. The acromial end usually has no epiphyseal center.[3] Surgical resection does not cause significant morbidity.[4]
Lesions that do not contain neoplasia, such as intraosseous ganglia, non-ossifying fibroma, fibrous dysplasia, osteomyelitis, and bone infarction are called tumor-like lesions and are relatively common. They are lesions that mimic bone tumors radiologically, morphologically and histologically.[5] There are epidemiological and clinical studies on tumors of rare localities in the literature,[6-8] but there is no study presenting both the epidemiology and clinical results of tumors located in the clavicle at the same time.
In the present study, we aimed to examine the characterization of tumors and tumor-like lesions located in the clavicle and to present their clinical results.
Patients and Methods
This single-center, retrospective study was conducted at Dr. Abdurrahman Yurtaslan Ankara Oncology Training and Research Hospital Department of Orthopedics and Traumatology between January 2006 and December 2018. A total of 44 patients (25 males, 19 females; mean age: 36.2±21.8 years; range, 2 to 87 years) who were operated in our clinic for a clavicular lesion were included. Among 4,856 extremity tumors operated in our clinic between these years, 44 cases (0.9%) located in the clavicle were eligible. Demographic data (age, sex), tumor types, location, surgical method, metastasis, survival analysis, and clinical results of these patients were reviewed. Lesions that were anatomically in the clavicle were evaluated. Patients who had lesions in adjacent joints, soft tissues and anatomical structures and whose records could not be reached from the archive were excluded from the study
All patients were initially examined with plain radiographs. Magnetic resonance imaging (MRI), computed tomography (CT), and whole-body bone scintigraphy were used as further examinations. All biopsies were performed by open incisional biopsy method. In patients with malignant biopsy results, thoracic CT was requested and multidisciplinary treatment was planned with oncologists. Non-surgical treatment was chosen for patients whose clavicle tumor was part of a metastatic/multifocal disease or whose life expectancy was limited.
Table 1. Demographic characteristics of the patients and clavicle tumor characteristics (n=44).
| n | % | Mean±SD | |
| Age (year) | 36.2±21.8 | ||
| Follow-up time (month) | 65.8±29.1 | ||
| MSTS | 93.7±21 | ||
| Sex | |||
| Male | 25 | 56.8 | |
| Female | 19 | 43.2 | |
| Site | |||
| Lateral | 16 | 36.4 | |
| Middle | 12 | 27.3 | |
| Middle and lateral | 6 | 13.6 | |
| Proximal and middle | 2 | 4.5 | |
| Proximal | 3 | 6.8 | |
| Total | 5 | 11.4 | |
| Side | |||
| Right | 22 | 50.0 | |
| Left | 22 | 50.0 | |
| Etiology | |||
| Aneurysmal bone cyst | 9 | 20.5 | |
| Simple bone cyst | 1 | 2.3 | |
| Eosinophilic granuloma | 3 | 6.8 | |
| Ewing sarcoma | 6 | 13.6 | |
| Fibromatosis | 1 | 2.3 | |
| Lymphoma | 1 | 2.3 | |
| Metastasis (lung) | 4 | 9.1 | |
| Metastasis (breast) | 1 | 2.3 | |
| Metastasis (thyroid) | 1 | 2.3 | |
| Myxofibrosarcoma | 1 | 2.3 | |
| Multiple myeloma | 3 | 6.8 | |
| Osteochondroma | 4 | 9.1 | |
| Osteomyelitis | 3 | 6.8 | |
| Plasmacytoma | 6 | 13.6 | |
| Surgical technique | |||
| Wide resection | 15 | 34.1 | |
| Incisional biopsy | 13 | 29.5 | |
| Curettage grafting | 12 | 27.3 | |
| Excision | 4 | 9.1 | |
| Tumor | |||
| Malign | 23 | 52.3 | |
| Benign | 21 | 47.7 | |
| Metastasis status | |||
| With metastasis | 25 | 56.8 | |
| Without metastasis | 19 | 43.2 | |
| Graft usage (n=19) | |||
| Allograft | 15 | 78.9 | |
| Cement | 1 | 5.3 | |
| Otograft | 3 | 15.8 | |
| Treatment | |||
| Chemotherapy | 14 | 82.4 | |
| Chemotherapy and radiotherapy | 2 | 11.8 | |
| Radiotherapy | 1 | 2.3 | |
| Survival status | |||
| Alive | 36 | 81.8 | |
| Ex | 8 | 18.2 | |
| SD: Standard deviation; MSTS: Musculoskeletal tumor society. | |||
Statistical analysis
Statistical analysis was performed using the SPSS for Windows version 25.0 software (IBM Corp., Armonk, NY, USA). Descriptive data were presented in mean ± standard deviation (SD), median (min-max), or number and frequency. The chisquare test or Fisher exact test was used to compare categorical variables. The conformity of the variables to the normal distribution was visual (histogram and probability graphs) and analytical using methods (if n≥50; Kolmogorov-Smirnov test, if n<50; Shapiro-Wilk test) examined. For the variable found to fit the normal distribution, statistical between two independent groups t-test in independent groups was used as a statistical method for significance. Overall survival was analyzed using the Kaplan-Meier test. Using the variables obtained in the study, comparisons were made with the Kaplan-Meier and Cox regression methods. A p value of <0.05 was considered statistically significant.
Results
The mean follow-up was 65.8±29.1 (range, 24 to 120) months. An aneurysmal bone cyst was diagnosed in involvement in proximal, middle, lateral and more than one region (Figure 1). The most frequently involved site was the lateral edge of the clavicle, and the most common tumor was an aneurysmal bone cyst (Figure 2).
Figure 1. Distribution of clavicle tumors by location.
Figure 2. Frequency of clavicular tumors by localization.

Of the 38 primary clavicle tumors remaining after the metastatic lesions were removed, 21 (55%) were benign, while 17 (45%) were malignant. The mean survival time of the primary clavicular tumor patients was 112.2±4.9 months and the median survival time was 120 months (Figure 3).
Figure 3. Tumor survival in primary clavicle tumors.

The patients were divided into age groups (<30, 30-50, >50 years) in accordance with the literature, and the distribution of tumor subtypes to these age groups is given in Figure 4. Aneurysmal bone cyst was most common in the group under 30 years of age, osteochondroma was most common in the 30-50 age group, and plasmacytoma was most common in those over 50 years of age (Figure 4).
Figure 4. Age distribution of subtypes of tumors.
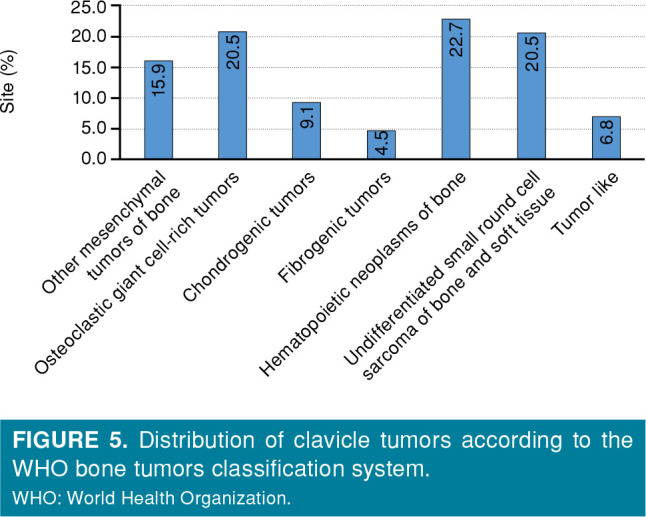
According to the World Health Organization (WHO) bone tumors classification system, we classified tumors located in the clavicle as chondrogenic, osteogenic and fibrogenic, round cell, and tumor-like (Figure 5).
Figure 5. Distribution of clavicle tumors according to the WHO bone tumors classification system. WHO: World Health Organization.
The mean postoperative musculoskeletal tumor society (MSTS) score was 93.7±21.0. The mean MSTS score of 15 (34.1%) patients who underwent clavicle resection was 79.4±6.
Discussion
Although the clavicle is a long bone, the overall incidence and relative occurrence of clavicle tumors are similar to flat bones.[9] The main finding of this study is that age is an important predictive factor for malignancy in clavicle tumors and the functional results after claviculectomy are satisfactory.
Despite subcutaneous localization of the clavicle, needle biopsy is not recommended. The reason for this is its proximity to neurovascular structures and misdiagnosis.[9] Cundy et al.[10] presented delayed clavicle osteosarcoma due to needle biopsy and drew attention to the importance of open biopsy. In our study, all patients were diagnosed with open incisional biopsy. Although anatomically palpable, there may be delays in diagnosis, due to the insidious and asymptomatic onset.[9]
Tumors located in the clavicle can involve the entire clavicle, as well as localize to the medial (sternal end), midline or lateral (acromial end) of the clavicle. In their study, Smith et al.[11] found the most common site as the lateral part with 41%, while they found the least localized site as the middle part with 7%. Similarly, Ren et al.[12] also reported that the lateral part was the most common, and the least was the middle part. In this study, the most common location of the clavicle was the lateral part with 36.4%, while the least localization was the medial part with 6.8%. We attribute the difference in the localization, which is the least involved, compared to the literature, as we named the lesions involving both sides as a different groups. There were two (4.5%) patients with the least localization involving the medial and middle parts.
In the present study, the most common tumor in the clavicle was aneurysmal bone cyst with 20.5%. While eight patients were located at the lateral end, one patient was in the middle. While curettage grafting was applied to seven patients, distal end resection of the clavicle was performed while preserving the coracoclavicular ligament in two patients. There are case series of aneurysmal bone cysts located in the clavicle in the literature[13,14] and are consistent with the findings of our study. Kaiser et al.[13] reported that in a series of 13 cases, the most common lateral location and the most common surgical method was curettage grafting. Two patients who underwent clavicle resection also reported excellent functional outcome. Similarly, Jamshidi et al.[14] also reported that resection was a surgical option that should be applied without fear, since it reduced recurrence and had a minimal effect on functional outcome.
The malignancy rate is high in tumors located in the clavicle. In the study presented by Kapoor et al.,[15] the malignancy rate was 66% and the most common malignant tumor was Ewing's sarcoma. Smith et al.[11] found malignant tumors occurred more frequently in their study and reported that the most common malignant tumor located in the clavicle was osteosarcoma. There are also studies in the literature with much lower malignancy rates.[12,16] In the study of Ren et al.,[12] the malignant rate was 36%, and the most common malignancy was osteosarcoma (8.7%). In the study of Suresh et al.,[16] the malignancy rate was only 15%. In this study, the malignant tumor rate was 52.2%, and the most common malignant tumor were Ewing's sarcoma and plasmacytoma with 13.6%. The literature attributes these discrepancies in malignancy rate to the results from different geographic origins and races.
Age is one of the important factors determining malignancy in clavicle tumors. Ren et al.[12] showed that the incidence of malignancy increased greatly in advanced age in a study conducted in East Asia. Similarly, Basarir et al.[17] showed that age 50 was an important cut-off factor for malignancy. Similarly, in this study, the incidence of benign tumors in children was significantly higher, and the incidence of metastasis in adults was significantly higher than in children.
The most important step in choosing the surgical method in tumors located in the clavicle is to decide whether the tumor is malignant or benign. In malignant tumors, it is easier to decide in favor of a wide or radical excision of the clavicle tumor compared to other long bones, since reconstruction is not required. Kapoor et al.[15] in their study of tumors located in the clavicle confirmed that tedious procedures might not be necessary for clavicle reconstruction. Krishnan et al.[18] reported that the postoperative function of the affected extremity was normal and there was only mild pain after total claviculectomy. Wood[4] showed that most functions of the upper extremity can be preserved without clavicle reconstruction. In their study by Li et al.,[19] patients after claviculectomy had almost full range of motion pain-free without significant functional deficit. The MSTS score was 86.6% in the study by Rossi et al.[20] in which they presented the results of the tumor located in the clavicle. In the current study, the mean MSTS score of 15 (34.1%) patients who underwent clavicle resection was 79.4±6.
There are some limitations of the study. It is the inability to form homogeneous groups due to its retrospective nature and considering all tumors together.
In conclusion, we believe that a wide spectrum should be considered in the differential diagnosis of tumors located in the clavicle. Age is an important predictive factor for malignancy. We believe that resection should be applied without fear considering its effects on function and recurrence.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Author Contributions: Writer: İ.K., C.U.; Data collection: B.A.; Data analysis: E.B.; Data collection: H.S.S.; Critical review: İ.B.A. Critical review: B.Ş.G.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Nota SP, Russchen MJ, Raskin KA, Mankin HJ, Hornicek FJ, Schwab JH. Functional and oncological outcome after surgical resection of the scapula and clavicle for primary chondrosarcoma. Musculoskelet Surg. 2017;101:67–73. doi: 10.1007/s12306-016-0437-9. [DOI] [PubMed] [Google Scholar]
- 2.Pressney I, Saifuddin A. Percutaneous image-guided needle biopsy of clavicle lesions: A retrospective study of diagnostic yield with description of safe biopsy routes in 55 cases. Skeletal Radiol. 2015;44:497–503. doi: 10.1007/s00256-014-2016-1. [DOI] [PubMed] [Google Scholar]
- 3.Ogden JA, Conlogue GJ, Bronson ML. Radiology of postnatal skeletal development. III. The clavicle. Skeletal Radiol. 1979;4:196–203. doi: 10.1007/BF00347213. [DOI] [PubMed] [Google Scholar]
- 4.Wood VE. The results of total claviculectomy. Clin Orthop Relat Res. 1986;(207):186–190. [PubMed] [Google Scholar]
- 5.Erlemann R, Jundt G. Tumor-like lesions of bone. Radiologe. 2016;56:507–519. doi: 10.1007/s00117-016-0113-y. [DOI] [PubMed] [Google Scholar]
- 6.Öztürk R, Ulucaköy C, Atalay İB, Yapar A, Karakoç Y. Management and retrospective analysis of pelvic ramus tumors and tumor-like lesions: Evaluation with 31 cases. Jt Dis Relat Surg. 2020;31:184–192. doi: 10.5606/ehc.2020.72762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karakoç Y, Ulucaköy C. Management and retrospective analysis of tumors and tumor-like lesions localized in the talus. Jt Dis Relat Surg. 2021;32:218–223. doi: 10.5606/ehc.2021.78769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yapar A, Tokgöz MA, Yapar D, Atalay İB, Ulucaköy C, Güngör BŞ. Diagnostic and prognostic role of neutrophil/ lymphocyte ratio, platelet/lymphocyte ratio, and lymphocyte/monocyte ratio in patients with osteosarcoma. Jt Dis Relat Surg. 2021;32:489–496. doi: 10.52312/jdrs.2021.79775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Minard-Colin V, Kalifa C, Guinebretiere JM, Brugieres L, Dubousset J, Habrand JL, et al. Outcome of flat bone sarcomas (other than Ewing's) in children and adolescents: A study of 25 cases. Br J Cancer. 2004;90:613–619. doi: 10.1038/sj.bjc.6601564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cundy WJ, Carter C, Dhatrak D, Clayer M. Primary osteosarcoma of the clavicle and the perils of bone biopsy. bcr2014208859BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2014-208859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith J, Yuppa F, Watson RC. Primary tumors and tumorlike lesions of the clavicle. Skeletal Radiol. 1988;17:235–246. doi: 10.1007/BF00401804. [DOI] [PubMed] [Google Scholar]
- 12.Ren K, Wu S, Shi X, Zhao J, Liu X. Primary clavicle tumors and tumorous lesions: A review of 206 cases in East Asia. Arch Orthop Trauma Surg. 2012;132:883–889. doi: 10.1007/s00402-012-1462-2. [DOI] [PubMed] [Google Scholar]
- 13.Kaiser CL, Yeung CM, Raskin KA, Lozano-Calderon SA. Aneurysmal bone cyst of the clavicle: A series of 13 cases. J Shoulder Elbow Surg. 2019;28:71–76. doi: 10.1016/j.jse.2018.06.036. [DOI] [PubMed] [Google Scholar]
- 14.Jamshidi K, Karimi A, Bagherifard A, Mirzaei A. Aneurysmal bone cysts of the clavicle: A comparison of extended curettage and segmental resection with bone reconstruction. J Shoulder Elbow Surg. 2019;28:1654–1657. doi: 10.1016/j.jse.2019.02.012. [DOI] [PubMed] [Google Scholar]
- 15.Kapoor S, Tiwari A, Kapoor S. Primary tumours and tumorous lesions of clavicle. Int Orthop. 2008;32:829–834. doi: 10.1007/s00264-007-0397-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suresh S, Saifuddin A. Unveiling the 'unique bone': A study of the distribution of focal clavicular lesions. Skeletal Radiol. 2008;37:749–756. doi: 10.1007/s00256-008-0507-7. [DOI] [PubMed] [Google Scholar]
- 17.Basarir K, Polat O, Saglik Y, Yildiz Y. Bone tumors of the clavicle: Risk of malignancy in the elderly and safe needle biopsy. Orthopedics. 2010;33:397–397. doi: 10.3928/01477447-20100429-16. [DOI] [PubMed] [Google Scholar]
- 18.Krishnan SG, Schiffern SC, Pennington SD, Rimlawi M, Burkhead WZ Jr. Functional outcomes after total claviculectomy as a salvage procedure. A series of six cases. J Bone Joint Surg Am. 2007;89:1215–1219. doi: 10.2106/JBJS.E.01436. [DOI] [PubMed] [Google Scholar]
- 19.Li Z, Ye Z, Zhang M. Functional and oncological outcomes after total claviculectomy for primary malignancy. Acta Orthop Belg. 2012;78:170–174. [PubMed] [Google Scholar]
- 20.Rossi B, Fabbriciani C, Chalidis BE, Visci F, Maccauro G. Primary malignant clavicular tumours: A clinicopathological analysis of six cases and evaluation of surgical management. Arch Orthop Trauma Surg. 2011;131:935–939. doi: 10.1007/s00402-010-1237-6. [DOI] [PubMed] [Google Scholar]




