Abstract
Background
Comorbidity between musculoskeletal (MSK) pain and depression is highly common, and is associated with a greater symptom burden and greater loss of work productivity than either condition alone. Multimodal care programs tackling both physical and mental health components may maximize productivity recovery and return to work. Digital delivery of such programs can facilitate access, ensure continuity of care, and enhance patient engagement.
Objective
The aim of this study was to assess the impact of a completely remote multimodal digital care program (DCP) for MSK pain on mental health and work-related outcomes stratified by baseline depression levels.
Methods
Ad hoc analysis of an interventional, single-arm, cohort study of individuals with MSK pain undergoing a DCP was performed. Three subgroups with different baseline depression severity levels were established based on responses to the Patient Health Questionnaire (PHQ-9): cluster 1 (score<5: minimal depression), cluster 2 (scores 5-10: mild depression), and cluster 3 (score≥10: moderate depression). The mean changes in depression, anxiety, fear-avoidance beliefs, work productivity, and activity impairment and adherence between baseline and end of program (8-12 weeks) were assessed across subgroups by latent growth curve analysis.
Results
From a total of 7785 eligible participants, 6137 (78.83%) were included in cluster 1, 1158 (14.87%) in cluster 2, and 490 (6.29%) in cluster 3. Significant improvements in depression and anxiety scores were observed in clusters 2 and 3 but not in cluster 1, with average end-of-the program scores in clusters 2 and 3 below the initially defined cluster thresholds (score of 5 and 10, respectively). All clusters reported significant improvements in productivity impairment scores (mean changes from –16.82, 95% CI –20.32 to –13.42 in cluster 1 to –20.10, 95% CI –32.64 to –7.57 in cluster 3). Higher adherence was associated with higher improvements in depression in clusters 2 and 3, and with greater recovery in activities of daily living in cluster 3. Overall patient satisfaction was 8.59/10.0 (SD 1.74).
Conclusions
A multimodal DCP was able to promote improvements in productivity impairment scores comparable to those previously reported in the literature, even in participants with comorbid depression and anxiety. These results reinforce the need to follow a biopsychosocial framework to optimize outcomes in patients with MSK pain.
Trial Registration
ClinicalTrials.gov NCT04092946; https://clinicaltrials.gov/ct2/show/NCT04092946
Keywords: musculoskeletal, pain, depression, anxiety, mental health, comorbidity, productivity, digital health, remote care, rehabilitation, telehealth, telemedicine, eHealth, digital health, digital care, multimodal, digital intervention, recovery, engagement, activities of daily living, work, job, occupational health, longitudinal cohort
Introduction
Musculoskeletal (MSK) pain is highly prevalent worldwide, affecting hundreds of millions of individuals with disability and personal suffering, while imposing a great socioeconomic burden [1]. Comorbidity between MSK pain and depression is very common [2] due to shared pathophysiological mechanisms, which establishes a strong and complex bidirectional relationship [3,4]. Comorbid depression symptoms have been associated with an increased MSK pain symptom burden and impaired recovery of both conditions [5,6]. This negative synergistic effect translates into poor work productivity [7,8], either by impaired performance at work (presenteeism) or work absence (absenteeism); decreased general quality of life; medical complications; and subsequent additional care [7-9]. Comorbid depression and MSK pain are associated with higher health care expenditures [10] estimated at US $13,000 annually in the United States, which is almost double that estimated for chronic pain alone [11]. In the United States, the annual cost associated with productivity loss from depression amounts to US $1150 per individual [12] and US $44 billion [13] for society, while the indirect costs associated with MSK pain are estimated at US $264 billion [14].
Exercise-based physical therapy is a first-choice intervention to address MSK pain [15-17]. Current guidelines advise addressing depression (as well as other cognitive and psychological factors) as part of MSK pain management [15,16,18] through a biopsychosocial approach [19,20], including pain education, psychoeducation, or even specifically cognitive behavioral therapy (CBT). This biopsychosocial approach has been increasingly applied and is naturally evolving with the optimization and digitalization of health care. With more than 62.5% of the global population now able to access the internet (according to Worldwide Digital Population estimates as of January 2022 [21]), digital interventions may offer highly scalable solutions to deliver evidence-based interdisciplinary interventions [22], thereby democratizing access and improving the continuity of care in cases where specially trained health care practitioners may not be readily available [23], and also promoting adherence to treatment by facilitating therapeutic alliance (defined as collaboration between therapeutic participants to foster healing) [24,25]. Digital interventions have therefore been explored for the treatment of depression and MSK diseases [26,27]. In 2021, the US Department of Health and Human Services’ Substance Abuse and Mental Health Services Administration released an evidence-based resource guide system recommending the use of telehealth for people with serious mental health disorders such as depression, noting that the benefits of telehealth services in this context may extend beyond improvement in morbid psychological conditions, including chronic pain and pain-related disability [28].
To date, digital intervention studies have been focused on either pain and disability [29-31] or on mental health and pain [26,27,32,33], with only a few studies assessing the impact of either dimension (MSK pain and depression) on work-related productivity [27,34-36].
Previously, we reported a multimodal digital care program (DCP) that integrates physical therapy exercise-based management with a psychoeducational component, including CBT, that aims to encourage patients to develop self-management skills and strategies for their pain. This DCP has been validated in different MSK conditions in chronic [37], acute [38,39], and postsurgical contexts [40-43]. Herein, we aimed to assess mental health and work-related outcomes after a completely remote multimodal DCP for patients with MSK pain stratified by baseline depression levels.
We hypothesized that this multimodal DCP would be able to contribute to mental health and promote productivity impairment improvements, despite differences in the initial mental status of participants.
Methods
Study Design
This is an ad hoc analysis of a decentralized, single-arm ongoing study, focused on assessing clinical and engagement-related outcomes in patients with MSK pain after a home-based multimodal DCP.
Ethics Approval
This study was prospectively approved by the New England Institutional Review Board (number 120190313) and was registered on ClinicalTrials.gov (NCT04092946) on September 17, 2019.
Participants
Beneficiaries of employer health plans, older than 18 years of age, and suffering from MSK pain (either in the spine or in the upper or lower limbs) were invited to apply for SWORD Health’s DCP through a dedicated website (which preselected candidates with ability to interact with technologies). Exclusion criteria were: (1) a health condition (eg, cardiac, respiratory) incompatible with at least 20 minutes of light to moderate exercise; (2) receiving active treatment for cancer; (3) reporting new-onset, rapidly progressive loss of strength and/or numbness in the arms/legs; or (4) reporting an unexplained change in bowel or urinary function in the previous 2 weeks. Informed consent was obtained from all participants.
Intervention
The DCP was delivered between August 1, 2020, and October 12, 2021. This completely remote DCP integrates individually tailored exercises and a psychoeducational component, which includes both education and CBT. Upon enrollment, each participant was assigned to a physical therapist who was responsible for program customization and asynchronous monitoring of patient performance. The exercise sessions consist of gradual progressive movement exposure and are performed through a Food and Drug Administration–listed class II medical device, including a tablet with a preinstalled app and wearable motion-tracking sensors. The tablet displays the prescribed exercises through audio/videos, while sensors digitize motion, providing real-time biofeedback along with instructions to guide patients during their sessions. Data obtained from the exercise sessions are stored on a cloud-based platform, being asynchronously monitored through a web-based portal by the assigned physical therapist who adjusts the exercises according to the patient’s progression. Participants were recommended to perform 3 exercise sessions per week, with an expected program duration ranging between 8 and 12 weeks depending on the condition (although early discharge was possible depending on physical therapist assessment). Absence of an exercise session for 28 consecutive days resulted in classification of the participant as a dropout. Participants were still considered if they were compliant with the intervention but failed to complete a given reassessment survey.
The psychoeducational component was developed under current clinical guidelines and research [17,44,45]. Educational articles were delivered through the app, covering a broad range of MSK pain–related topics, explaining pain and pain management. The CBT program consisted of self-guided interactive modules delivered through the smartphone app. This program was created by a multidisciplinary team including psychiatrists and psychologists based on third-generation CBT techniques, including mindfulness, acceptance and commitment therapy, and empathy-focused therapy. The CBT program was specifically designed to address fear avoidance, pain reconceptualization, active coping skills, as well as anxiety and depression associated with MSK pain. Bidirectional communication between participants and physical therapists, after exercise sessions or on demand, were ensured through a built-in secure chat feature on the smartphone app, and through synchronous video calls between the physical therapist and participant to facilitate therapeutic alliance, adjust treatment, and monitor potential adverse events.
Outcome Metrics
Self-reported assessments were collected at baseline, 4, 8, and 12 weeks, while mean changes were calculated between baseline and program end. Outcomes included mean change of (1) depression, measured by the 9-item Patient Health Questionnaire (PHQ-9; range 0-27) [46,47]; (2) anxiety, measured by the 7-item Generalized Anxiety Disorder (GAD-7) questionnaire (range 0-21) [48]; (3) Fear-Avoidance Beliefs Questionnaire for Physical Activity (FABQ-PA), comprising a total of 5 items each with a 7-option Likert scale (range 0-24) [49]; (4) Work Productivity and Activity Impairment (WPAI) questionnaire (0-100), including WPAI-overall (presenteeism and absenteeism from work), WPAI-work (presenteeism), WPAI-time (absenteeism, evaluated in employed participants), and WPAI-activity (for nonwork-related activity impairment in all participants) [50]; and (5) adherence, assessed through the number of completed sessions per week, total exercise time (minutes), communication frequency with the physical therapist, and overall satisfaction (points) through the question “On a scale from 0 to 10, how likely is it that you would recommend this intervention to a friend or neighbor? (from 0, not at all likely to 10, extremely likely). Overall, higher self-reported outcomes scores indicate higher severity.
Safety and Adverse Events
Participants were asked to grade the severity of pain and fatigue (from 0 to 10, with 10 being the most severe) on all exercise sessions to allow monitoring by the physical therapists. All communication channels were available for participants to report any adverse events. PHQ-9 and GAD-7 scores were used not only to guide the intervention approach but also to direct members to psychological and/or psychiatric care when needed, following the US Department of Health and Human Services guidelines.
Statistical Analysis
Study population demographics and clinical data, as well as usability metrics (number of sessions per week, total exercising time) were characterized through descriptive statistics. Differences in baseline characteristics between clusters (see below) were assessed through χ2 tests for categorical variables and independent-samples t tests or one-way analysis of variance with Bonferroni posthoc correction for continuous variables.
Considering that depression has been reported as an important prognosis factor [51,52], PHQ-9 was used as a clustering variable, applying the thresholds <5 for no depression symptoms, 5-10 for mild symptoms, and ≥10 for moderate/severe symptoms, according to Kroenke et al [53].
For longitudinal data analysis, the latent growth curve was applied, which is a methodology in the same family as linear mixed-effects modeling, with the advantages of providing a measure of model fitness (eg, how well the model explains the data set) [54], and allowing the use of full information maximum likelihood (FIML) to address missing data. FIML has been shown to outperform other modern imputation models such as multiple imputation by chained equations (MICE) and listwise deletion [54-56]. FIML estimation considers all available data in each time point from all participants [55,56].
Latent growth curve analysis uses a structural equation model [57] to estimate the trajectories of outcomes over time based on individual trajectories and considering time as a continuous variable. This provides an estimate of the average trajectory (and respective pace of change) and individual variation around that trajectory over time (see Figure S1 in Multimedia Appendix 1).
The analysis was performed as an intent-to-treat analysis both for unfiltered cases and filtering for WPAI>0 points at baseline. Impact of training time on outcomes was modeled using cumulative training time as a time-invariant covariate. A conditional analysis was also performed to assess the influence of age, sex, and BMI as covariates. Models were adjusted for these covariates, which were fit as random effects allowing each to vary between individuals. All models were estimated with a robust sandwich estimator for standard errors.
Logistic regression was used to assess the relationship between baseline depression and productivity changes.
Significance levels were set at P<.05 in all analyses. Latent growth curve analysis was coded using R (version 1.4.1717) and all other analyses were performed using SPSS (version 17.0).
Results
Participant Characteristics
In total, 9388 participants were screened for eligibility, 621 (6.61%) of whom did not provide consent for research and 982 (10.46%) of whom were excluded (105 for clinical criteria, 37 participants missed their video call, and 840 declined to participate in the program during the video call) (Figure 1). In total, 7785 participants from all 50 states within the United States started the program. Overall, the completion rate was 77.05% (5998/7785), with 16.04% (962/5998), 19.02% (1141/5998), and 64.94% (3895/5998) participants discharged at 4, 8, and 12 weeks, respectively.
Figure 1.
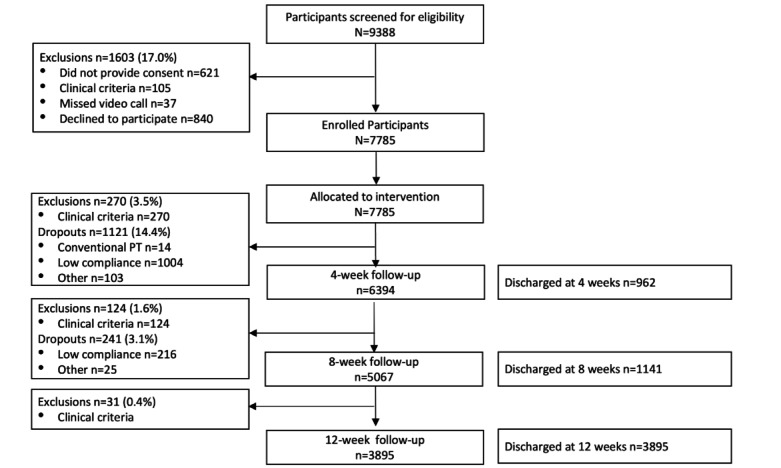
Flowchart of the study.
Using PHQ-9 as a clustering variable, 3 clusters were created: <5, 5-10, and ≥10 points, according to Kroenke et al [53]. Baseline demographics of each cluster are reported in Table 1 and those of the entire cohort are provided in Table S1 of Multimedia Appendix 2.
Table 1.
Baseline characteristics of study participants in each depression-related cluster.
| Characteristic | Cluster 1, PHQ-9a score <5 (n=6137) | Cluster 2, PHQ-9 score 5-10 (n=1158) | Cluster 3, PHQ-9 score ≥10 (n=490) | P value | ||
| Age (years), mean (SD) | 51.4 (12.7) | 50.0 (13.4) | 48.7 (13.4) | <.001 | ||
| Age category (years), n (%) | <.001 | |||||
|
|
<25 | 43 (0.7) | 16 (1.4) | 8 (1.6) |
|
|
|
|
25-40 | 1339 (21.8) | 298 (25.7) | 146 (29.8) |
|
|
|
|
40-60 | 3172 (51.7) | 561 (48.4) | 225 (45.9) |
|
|
|
|
>60 | 1583 (25.8) | 283 (24.4) | 111 (22.7) |
|
|
| Gender, n (%) | <.001 | |||||
|
|
Woman | 3276 (53.4) | 702 (60.6) | 297 (60.6) |
|
|
|
|
Man | 2848 (46.4) | 453 (39.1) | 191 (39.0) |
|
|
|
|
Nonbinary | 13 (0.2) | 3 (0.3) | 2 (0.4) |
|
|
| BMIb, mean (SD) | 28.8 (6.3) | 30.6 (7.1) | 32.9 (7.9) | <.001 | ||
| BMI categoryb, n (%) | <.001 | |||||
|
|
Underweight (<18.5) | 46 (0.8) | 10 (0.9) | 3 (0.6) |
|
|
|
|
Normal (18.5-25) | 1789 (29.2) | 247 (21.4) | 88 (18.0) |
|
|
|
|
Overweight (25-29) | 2145 (35.0) | 362 (31.3) | 122 (25.0) |
|
|
|
|
Obese (30-39) | 1775 (29.0) | 412 (35.7) | 197 (40.4) |
|
|
|
|
Obese grade III (>40) | 367 (6.0) | 124 (10.7) | 78 (16.0) |
|
|
| Conditions addressed, n (%) | <.001 | |||||
|
|
Spine | 2961 (48.2) | 626 (54.1) | 314 (64.1) |
|
|
|
|
Lower limb | 1739 (28.3) | 310 (26.8) | 108 (22.0) |
|
|
|
|
Upper limb | 1437 (23.4) | 222 (19.2) | 68 (13.9) |
|
|
| Pain durationc, n (%) | <.001 | |||||
|
|
Acute (<12 weeks) | 1620 (26.5) | 235 (20.4) | 68 (13.9) |
|
|
|
|
Chronic (>12 weeks) | 4492 (73.5) | 919 (79.6) | 422 (86.1) |
|
|
| Employment status, n (%) | <.001 | |||||
|
|
Employed (part-time or full-time) | 5260 (85.7) | 992 (85.7) | 364 (74.3) |
|
|
|
|
Unemployed | 877 (14.3) | 166 (14.3) | 126 (25.7) |
|
|
| Outcome measures, mean (SD) | ||||||
|
|
Pain level | 4.67 (1.98) | 5.10 (1.95) | 5.73 (1.97) | <.001 | |
|
|
Analgesics, n (%) | 1861 (30.3) | 464 (40.1) | 212 (43.3) | <.001 | |
|
|
Surgery intent | 10.26 (19.52) | 11.97 (21.41) | 17.32 (26.86) | <.001 | |
|
|
FABQ-PAd,e | 10.27 (5.99) | 11.63 (5.82) | 12.72 (5.96) | <.001 | |
|
|
GAD-7f | 1.82 (2.88) | 6.17 (4.23) | 11.66 (5.62) | <.001 | |
|
|
PHQ-9 | 0.86 (1.25) | 6.93 (1.63) | 14.84 (3.74) | <.001 | |
|
|
WPAIg-overallh | 14.78 (20.48) | 23.94 (23.60) | 40.87 (30.51) | <.001 | |
|
|
WPAI-workh | 13.86 (19.17) | 22.08 (22.09) | 38.04 (28.62) | <.001 | |
|
|
WPAI-timeh | 1.98 (10.52) | 4.36 (15.29) | 12.02 (26.16) | <.001 | |
|
|
WPAI-activity | 25.43 (23.97) | 34.47 (25.04) | 50.49 (26.29) | <.001 | |
aPHQ-9: 9-item Patient Health Questionnaire.
bn=20 missing values.
cn=29 missing values.
dFABQ-PA: Fear-Avoidance Beliefs Questionnaire for Physical Activity.
en=10 missing values.
fGAD-7: 7-item Generalized Anxiety Disorder questionnaire.
gWPAI: Work Productivity and Activity Impairment questionnaire.
hN=6030.
Participants were unevenly distributed across the three clusters, with 6137, 1158, and 490 participants in cluster 1, 2, and 3, respectively. Several demographic characteristics were significantly different between clusters, namely the proportion of women, unemployed, younger participants, acuity, or those with higher BMI, which were progressively more frequent with increasing levels of depression (from cluster 1 to 2 and to 3, P<.001; Table 1). Significant baseline differences were also observed in clinical characteristics between clusters, as cluster 1 had no impairment in mental health (GAD-7 scores below 2 and FABQ 10.3, SD 6.0), and low levels of productivity impairment (WPAI-overall ~15%, SD 20.5 impairment). Cluster 2 reported mild anxiety and fear-avoidance beliefs (GAD-7 above 5 and FABQ 11.3, SD 5.8) and work difficulties (WPAI overall ~22%, SD 24.2 impairment), while cluster 3 presented with the highest anxiety (GAD-7 above 10) and greatest fear-avoidance beliefs (FABQ 12.7, SD 6.0) measures, along with greater impairments in productivity (40.87%, SD 30.5) or activities of daily living (50.5%, SD 26.3; P<.001; Table 1).
Clinical Outcomes
Overview
Changes in clinical outcomes over time are presented in Table 2, the model is presented in Table S2 of Multimedia Appendix 3, and the impact of covariates in the model is reported in Table S3 of Multimedia Appendix 4.
Table 2.
Changes in clinical outcomes between baseline and end of program: intent-to-treat analysis.
| Variable | Cluster 1 | Cluster 2 | Cluster 3 | ||||||||
|
|
Baseline, mean (95% CI) | Change, mean (95% CI) | P value | Baseline, mean (95% CI) | Change, mean (95% CI) | P value | Baseline, mean (95% CI) | Change, mean (95% CI) | P value | ||
| PHQ-9a | 0.81 (0.77 to 0.86) | –0.03 (–0.25 to 0.18) | .77 | 6.58 (6.44 to 6.71) | –3.36 (–4.26 to 2.45) | <.001 | 13.98 (13.46 to 14.5) | –4.09 (–6.87 to –1.32) | .004 | ||
| GAD-7b | 1.44 (1.35 to 1.53) | –0.43 (–0.68 to –0.18) | <.001 | 5.44 (5.07 to 5.8) | –2.25 (–3.14 to –1.36) | <.001 | 10.73 (9.99 to 11.47) | –2.24 (–4.49 to 0.01) | .05 | ||
| FABQ-PAc | 10.4 (10.18 to 10.62) | –2.63 (–3.17 to –2.09) | <.001 | 11.49 (10.98 to 12.01) | –2.33 (–3.62 to –1.04) | <.001 | 12.67 (11.92 to 13.42) | –0.7 (–2.84 to 1.44) | .52 | ||
| WPAId-overall | 13.9 (13.11 to 14.7) | –6.84 (–8.82 to –4.86) | <.001 | 21.87 (19.39 to 24.35) | –11.33 (–16.6 to –6.06) | <.001 | 39.68 (34.86 to 44.5) | –12.34 (–23.65 to –1.03) | .03 | ||
| WPAI-overalle | 27.26 (26.1 to 28.41) | –16.82 (–20.23 to –13.42) | <.001 | 31.00 (28.26 to 33.74) | –19.11 (–25.75 to –12.47) | <.001 | 45.43 (40.62 to 50.24) | –20.1 (–32.64 to –7.57) | .002 | ||
| WPAI-activity | 22.57 (21.74 to 23.4) | –10.08 (–11.95 to –8.21) | <.001 | 30.99 (28.74 to 33.23) | –13.14 (–18.22 to –8.06) | <.001 | 46.35 (42.88 to 49.82) | –5.07 (–14.08 to 3.95) | .27 | ||
| WPAI-activitye | 32.04 (31.14 to 32.95) | –15.66 (–17.98 to –13.34) | <.001 | 36.28 (34.08 to 38.48) | –16.17 (–21.57 to –10.77) | <.001 | 49.5 (46.16 to 52.83) | –7.01 (–16.52 to 2.5) | .15 | ||
| WPAI-work | 13.04 (12.3 to 13.79) | –6.20 (–8.00 to –4.39) | <.001 | 20.78 (18.4 to 23.16) | –11.37 (–16.17 to –6.57) | <.001 | 37.13 (32.59 to 41.67) | –13.54 (–24.42 to –2.65) | .01 | ||
| WPAI-worke | 26.06 (24.98 to 27.13) | –15.24 (–18.35 to –12.12) | <.001 | 29.58 (26.93 to 32.24) | –19.36 (–25.29 to –13.42) | <.001 | 42.97 (38.44 to 47.51) | –21.9 (–34.43 to –9.37) | <.001 | ||
| WPAI-time | 2.02 (1.58 to 2.46) | –0.98 (–2.09 to 0.12) | .06 | 3.67 (2.01 to 5.34) | –1.42 (–3.93 to 1.09) | .23 | 13.45 (8.94 to 17.97) | –5.63 (–11.05 to –0.21) | .03 | ||
| WPAI-timee | 27.02 (22.52 to 31.52) | –28.54 (–39.11 to –17.96) | <.001 | 25.65 (17.24 to 34.06) | –20.5 (–31.84 to –9.16) | <.001 | 46.1 (35.5 to 56.7) | –23.13 (–43.29 to –2.98) | .02 | ||
aPHQ-9: 9-item Patient Health Questionnaire.
bGAD-7: 7-item Generalized Anxiety Disorder questionnaire.
cFABQ-PA: Fear-Avoidance Beliefs Questionnaire for Physical Activity.
dWPAI: Work Productivity and Activity Impairment questionnaire.
eFiltered for scores>0 at baseline.
Depression
Significant improvement was observed on the PHQ-9 for clusters 2 and 3, but not for cluster 1, which reported minimal depression symptoms at baseline (Table 2). Average end-of-the program scores for depression in clusters 2 and 3 decreased to levels below the initially defined lower cluster thresholds (5 and 10 for clusters 2 and 3, respectively; end scores: 3.22, 95% CI 2.31-4.13 and 9.89, 95% CI 7.15-12.62, respectively).
Significant differences in PHQ-9 score changes were observed between all clusters (P<.001, Table 3). Women reported higher levels of depression than men in cluster 1 (P<.001), but recovered at a faster pace in clusters 1 and 2. Older participants in cluster 3 recovered from depression symptoms at a slower pace (P=.04).
Table 3.
Differences in clinical outcomes change stratified by baseline depression level.
| Outcome | Cluster 1 versus cluster 2 | Cluster 1 versus cluster 3 | Cluster 2 versus cluster 3 | |||
|
|
Difference (95% CI) | P value | Difference (95% CI) | P value | Difference (95% CI) | P value |
| PHQ-9a | –2.44 (–3.37 to –1.51) | <.001 | –9.11 (–11.85 to –6.36) | <.001 | –6.66 (–9.55 to –3.78) | <.001 |
| GAD-7b | –2.17 (–3.08 to –1.25) | <.001 | –7.47 (–9.71 to –5.23) | <.001 | –5.3 (–7.69 to –2.92) | <.001 |
| FABQ-PAc | –1.39 (–2.79 to 0.01) | .05 | –4.2 (–6.43 to –1.96) | <.001 | –2.81 (–5.33 to –0.28) | .03 |
| WPAId-overall | –3.48 (–8.96 to 2.01) | .22 | –20.28 (–31.72 to –8.84) | <.001 | –16.8 (–29.21 to –4.4) | .008 |
| WPAI-overalle | –2.29 (–5.17 to 9.75) | .55 | –3.28 (–9.71 to –16.28) | .62 | –1.00 (–13.19 to 15.18) | .07 |
| WPAI-activity | –5.35 (–10.74 to 0.04) | .05 | –28.79 (–37.88 to –19.7) | <.001 | –23.43 (–33.69 to –13.18) | <.001 |
| WPAI-activitye | –0.51 (–5.37 to 6.39) | .87 | –8.65 (–18.44 to 1.14) | .08 | –9.16 (–20.10 to 1.77) | .11 |
| WPAI-work | –2.57 (–7.53 to 2.38) | .31 | –16.75 (–27.85 to –5.64) | .003 | –14.18 (–26.08 to –2.27) | .02 |
| WPAI-worke | 4.12 (–2.58 to 10.83) | .23 | 6.66 (–6.25 to 19.57) | .31 | 2.54 (–11.33 to 16.40) | .72 |
| WPAI-time | –1.21 (–3.75 to 1.32) | .35 | –6.78 (–12.53 to –1.03) | .02 | –5.57 (–11.69 to 0.55) | .08 |
| WPAI-timee | –8.04 (–23.54 to 7.47) | .31 | –5.41 (–28.17 to 17.36) | .64 | 2.63 (–20.50 to 25.76) | .84 |
aPHQ-9: 9-item Patient Health Questionnaire.
bGAD-7: 7-item Generalized Anxiety Disorder questionnaire.
cFABQ-PA: Fear-Avoidance Beliefs Questionnaire for Physical Activity.
dWPAI: Work Productivity and Activity Impairment questionnaire.
eFiltered for scores>0 at baseline.
Anxiety
Cluster 1 did not report significant anxiety levels at baseline; thus, the observed change was not meaningful. Clusters 2 and 3 showed statistically significant improvements after the DCP (Table 3), ending the program with lower levels of anxiety than at baseline (end scores: 3.18, 95% CI 2.31-4.06 and 8.49, 95% CI 6.27-10.71, respectively).
Changes in anxiety levels were again significantly different among clusters (P<.001, Table 3). Women reported greater anxiety levels than men at baseline in clusters 1 and 2, whereas a faster-paced recovery was observed across all clusters for women (P<.001, Table S3 in Multimedia Appendix 4). Older participants in cluster 3 recovered from anxiety at a slower pace (P=.02). BMI did not influence mental health improvement trajectories in any cluster (Table S3 in Multimedia Appendix 4).
Fear-Avoidance Beliefs
Statistically significant improvements were observed in clusters 1 and 2, with a mean change of approximately –2.50 in both clusters (P<.001, Table 2). No significant improvement was observed in cluster 3 (P=.52, Table 2). BMI did not influence FABQ improvement trajectories in any cluster (Table S3 in Multimedia Appendix 4).
Work Productivity
Baseline impairments in work and in activities of daily living were progressively higher from cluster 1 to cluster 3 (Table 1). Across all WPAI scores, similar mean changes were observed between clusters (Table 3) when filtering for participants reporting impairments at baseline, despite different baseline values (Table 2).
Age and BMI did not consistently influence productivity impairment improvement across all clusters (Table S3 in Multimedia Appendix 4). Among women, we observed deacceleration in the improvement pace toward the end of the program for the WPAI overall score (Table S3 in Multimedia Appendix 4) as well as higher baseline scores paired with a slower recovery pace in WPAI activity.
Productivity impairment (WPAI-overall score) improved significantly across all clusters with mean changes ranging from –16.82 (95% CI –20.32 to –13.42) in cluster 1 and –19.11 (95% CI –25.75 to –12.47) in cluster 2 to –20.10 (95% CI –32.64 to –7.57) in cluster 3 when filtering for participants with reported impairment at baseline (WPAI>0). A significant, albeit small, correlation between baseline PHQ-9 values and WPAI change was only observed in cluster 3 (0.30, P=.01).
Adherence and Usability-Related Outcomes
The average number of sessions per week was 2.7 (SD 1.39) across all clusters, but with individuals in clusters 2 and 3 showing slightly lower adherence (average of 2.6 sessions per week, SD 1.3; P<.001). This paralleled differences in the amount of time dedicated to exercise between clusters, which ranged from 552.4 minutes in cluster 1 to 384.7 minutes in cluster 3 (Table 4, P<.001). The influence of training time on outcome changes was estimated regarding trajectory slopes (Table 5).
Table 4.
Adherence outcome measures of the entire cohort and particular clusters.
| Usability outcomes | Entire cohort, mean (SD) | Cluster 1, mean (SD) | Cluster 2, mean (SD) | Cluster 3, mean (SD) | P value |
| Number of sessions per week | 2.7 (1.39) | 2.7 (1.40) | 2.6 (1.31) | 2.6 (1.32) | <.001 |
| Total exercising time, minutes | 531.0 (522.3) | 552.4 (537.4) | 479.1 (473.6) | 384.7 (392.6) | <.001 |
| Average satisfaction (NRSa, 0-10) | 8.6 (1.74)b | 8.6 (1.72) | 8.5 (1.77) | 8.6 (1.98) | .59 |
| Number of days with contact (chat) | 9.1 (11.6) | 9.1 (11.6) | 8.8 (11.5) | 10.0 (11.7) | .21 |
| Number of messages exchanged | 23.74 (27.10) | 23.30 (26.86) | 24.37 (27.20) | 28.37 (29.65) | .02 |
| Number of educational articles per week | 4.29 (7.0) | 4.24 (7.0) | 4.56 (6.9) | 4.32 (7.2) | .37 |
aNRS: numerical rating scale.
Table 5.
Effect of cumulative training time on the slopes of recovery trajectories for the different outcome variables.a
| Variable | Cluster 1 | Cluster 2 | Cluster 3 | |||||
|
|
Estimate | P value | Estimate | P value | Estimate | P value | ||
| PHQ-9b | –0.01 | .18 | –0.06 | .03 | –0.24 | .005 | ||
| GAD-7c | –0.01 | .23 | –0.05 | .13 | –0.20 | .001 | ||
| FABQ-PAd | –0.07 | <.001 | –0.13 | .002 | –0.21 | .003 | ||
| WPAIe-overallf | 0.01 | .92 | 0.13 | .57 | –0.56 | .19 | ||
| WPAI-activityf | –0.24 | .001 | –0.30 | .10 | –1.31 | <.001 | ||
| WPAI-workf | –0.03 | .78 | 0.15 | .48 | –0.46 | .29 | ||
| WPAI-timef | 0.39 | .29 | 0.36 | .34 | –0.64 | .49 | ||
aNegative values refer to more sharp slopes, indicating faster change over time.
bPHQ-9: 9-item Patient Health Questionnaire.
cGAD-7: 7-item Generalized Anxiety Disorder questionnaire.
dFABQ-PA: Fear-Avoidance Beliefs Questionnaire for Physical Activity.
eWPAI: Work Productivity and Activity Impairment questionnaire.
fFiltered for scores>0 at baseline.
In cluster 1, training time was significantly associated with FABQ reduction (P<.001) and improvement of WPAI-activity (P=.001). In cluster 2, increased training time was significantly associated with improvements in depression (P=.03) and FABQ (P=.002), but with no significant effect on productivity. In cluster 3, increased training times were significantly associated with greater improvements in mental health (depression [PHQ-9, P=.005], anxiety [GAD-7, P=.001], fear avoidance [FABQ, P=.003]) and in activities of daily living impairment (WPAI-activity, P<.001).
Regarding communication channels, the app chat was the preferred mode of contact, with an average of 9.1 days with contact. There were no significant differences between clusters (P=.21, Table 4), with cluster 3 showing a higher number of exchanged messages (Table 4). On average, 1.7 (SD 2.7) calls were made, which did not significantly differ between clusters (P=.22). Each participant on average engaged with 4.3 (SD 7.0) pieces of educational and CBT content, with no significant difference observed between clusters. Overall, the average satisfaction score was 8.6 (SD 1.7), which again did not significantly differ among the three clusters.
Discussion
Principal Findings
Depression has been reported to be an important prognostic factor in MSK pain management [58,59]. By clustering patients according to baseline depression, we created three distinct groups, where other concomitant psychological factors (anxiety and fear-avoidance behaviors) with known prognostic value [5,60,61] were also observed at similar levels of severity. This is in accordance with the general population demographics, where depression is accompanied by other psychological/cognitive impairments [62,63], particularly in those with MSK pain [64]. Importantly, other demographic characteristics known to have prognostic value were distributed differently between clusters. Cluster 3 patients, besides suffering from more severe mental distress, were also more likely to be women [19], have a higher BMI [65], and be unemployed [66]. Cluster 2 contained these same factors at lower proportions but had a higher proportion of older participants [60], while cluster 1 tended to have more patients devoid of known risk factors.
Gender identification as a woman and older age were the predominant prognostic factors impacting both baseline and change in mental health status, while productivity was mainly influenced by gender identification as a woman. These results highlight the need to fine-tune programs to the specific needs of women, since this population is frequently identified as being more prone to psychological distress and prolonged MSK pain [67,68].
Notably, we observed that the improvements in mental health scores in clusters 2 and 3 resulted in average scores at the end of the program below the threshold used to define those clusters: cluster 2 from mild depression symptoms to minimal or no symptoms (<5) and cluster 3 from moderate to mild symptoms (<10). Overall, greater improvements were noted in cluster 3, demonstrating that multimodal DCP can not only impact physical health but also mental health in individuals with MSK pain and moderate mental health comorbidities.
Comparison to Prior Work
The observed improvements in mental health scores were higher than those previously reported by other multimodal telerehabilitation interventions [69,70], and were in line with those previously reported by us [37,39] and others [27,32,34,71]. Similar to the present study, Wang et al [71] reported a significant decrease in anxiety symptoms, allowing the transition to a lower level of anxiety according to established thresholds after a telerehabilitation program combining exercise with coaching.
A correlation between baseline depression and WPAI change was only observed in cluster 3, which might suggest that the prognostic value of depression may be dependent on higher severity stages [72,73] or that it is more relevant in chronic conditions [8,72,74]. However, it may also reflect that there is little room for improvement in psychological indices in patients with little baseline psychopathology.
Regarding productivity, all clusters had significant WPAI improvements, independent of the recoveries reported for fear-avoidance beliefs assessment, which in this study appeared to be a poor predictor for work-related productivity recovery. In fact, while fear-avoidance belief has been systematically associated with disability and pain [75-77], its correlation with work-related outcomes might only be observed in those with high FABQ or FABQ-work subscale scores [78]. Similar improvements in productivity were reported by Bailey et al [34] in a cohort study involving more than 10,000 participants with MSK pain, either with or without depression symptoms at baseline. Overall, the results are supportive of the application of multimodal/biopsychosocial approaches to address psychological (mal)adaptation to the pain condition [61,79,80] and maximize treatment outcomes, as previously reported with other telerehabilitation interventions [81,82].
Interestingly, the improvement observed for productivity was not replicated to the same extent in activities of daily living, particularly in cluster 3. The observed difference might be explained by the high level of depression symptoms and also by the greater prevalence of participants who were women, as highlighted by the conditional analysis, with women still being more frequently responsible for family and household activities [83,84].
The importance of patient compliance to obtain clinically meaningful outcomes is well-established [85,86]. We observed high compliance with exercise sessions across clusters, even in cluster 3 where, besides higher depression levels, >50% of participants were obese, a known factor for reduced engagement [65,87]. Herein, increased amounts of time dedicated to exercise sessions were associated with greater improvements in mental health and activities of daily living recovery, as previously reported [88-90].
However, we observed lower adherence to the psychoeducational program than anticipated, despite high adherence with other components of the program, high satisfaction levels, and frequent communication with the assigned physical therapist. The same challenges have been highlighted by other authors [91], suggesting that additional innovation to stimulate engagement in such components might further contribute to better outcomes [92-94]. Communication is key for establishing a therapeutic alliance (defined as collaboration between therapeutic participants to facilitate healing), which in turn is key for improved outcomes [60,95-97]. Digital interventions have been reported to promote similar or even better therapeutic alliance than in-person interventions [25]. Herein, communication between physical therapists and individuals was frequent, highlighting the convenience of the app chat. Further studies are needed to clarify the extent to which this accessible and available communication system impacts outcome.
Strengths and Limitations
Strengths of the study included the large sample size derived from a real-world context and the nature of the intervention: a multicomponent DCP managed by physical therapists combining exercises with real-time biofeedback within a biopsychosocial framework [17,95]. The digital format favors accessibility, while the regular communication with the same physical therapist may enhance adherence and maximize clinical outcomes [86,98]. The high adherence reported herein was objectively assessed to minimize social desirability response bias. Other strengths were the assessment of productivity through validated and widely used measures, and the inclusion of a heterogeneous cohort from geographically diverse states.
The major limitation refers to the study design that did not include a control group and thus does not allow us to determine the degree to which the various components of the program may have contributed to its overall reported changes, and whether all components benefit patients alike. Nevertheless, this study focused on an exploratory analysis of real-world data to support further research. Some variability was observed in terms of DCP participation and completion rates. However, the statistical methodologies chosen took into account the inclusion of real-world data, with missing data being handled through FIML, a method robust to attrition bias. This study included both emotional and cognitive outcomes; however, the inclusion of other psychosocial variables or tracking of mental-specific pharmacologic treatments could improve statistical models and further explain the variance, namely in the productivity measures.
Conclusions
A multimodal DCP was able to promote significant improvements in productivity, comparable to those previously reported in the literature, even in participants with comorbid depression and anxiety at baseline. These results reinforce the need to follow a biopsychosocial framework to optimize outcomes in patients with MSK pain to maximize return to work.
Acknowledgments
The authors acknowledge the team of physical therapists responsible for the management of participants. The study was funded by SWORD Health.
Abbreviations
- CBT
cognitive behavioral therapy
- DCP
digital care program
- FABQ-PA
Fear-Avoidance Beliefs Questionnaire for Physical Activity
- FIML
full information maximum likelihood
- GAD-7
Generalized Anxiety Disorder 7-item questionnaire
- MICE
multiple imputation by chained equations
- MSK
musculoskeletal
- PHQ-9
Patient Health 9-item questionnaire
- WPAI
Work Productivity and Activity Impairment questionnaire
Example path diagram for the latent growth curve (LGC) models used in the current study (Figure S1).
Table S1. Baseline characteristics of the entire cohort.
Table S2. Unconditional latent growth curve analysis: intent-to-treat analysis.
Table S3. Conditional growth-mixture modeling analysis: intent-to-treat analysis.
Data Availability
All relevant data are included in the article or available as supplementary material. The protocol, deidentified data, and analysis codes may be provided upon request to the corresponding author.
Footnotes
Authors' Contributions: All authors made a significant contribution to the work reported, as follows: Study concept and design: FDC, VB, JL, and SC; Data acquisition: MM; Statistical analysis: RM; Interpretation of data: FC, DJ, MM, SC, and FDC; Drafting the work: FC and DJ; Critical revision of the manuscript for important intellectual content: all authors; Final approval of the version to be published: all authors. The study sponsor, SWORD Health, was involved in study design, data collection, and interpretation and writing of the manuscript.
Conflicts of Interest: FC, DJ, MM, VB, VY, and FDC are employees at SWORD Health, the study sponsor. FDC, VY, and VB also hold equity from SWORD Health. RM is an independent scientific consultant who was responsible for the statistical analysis, while SC, JL, and JS are independent scientific/clinical consultants who were funded by SWORD Health in connection with the development and execution of this article.
References
- 1.El-Tallawy SN, Nalamasu R, Salem GI, LeQuang JAK, Pergolizzi JV, Christo PJ. Management of musculoskeletal pain: an update with emphasis on chronic musculoskeletal pain. Pain Ther. 2021 Jun;10(1):181–209. doi: 10.1007/s40122-021-00235-2. http://europepmc.org/abstract/MED/33575952 .10.1007/s40122-021-00235-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daré LO, Bruand P, Gérard D, Marin B, Lameyre V, Boumédiène F, Preux P. Co-morbidities of mental disorders and chronic physical diseases in developing and emerging countries: a meta-analysis. BMC Public Health. 2019 Mar 13;19(1):304. doi: 10.1186/s12889-019-6623-6. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-6623-6 .10.1186/s12889-019-6623-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crofford LJ. Psychological aspects of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol. 2015 Feb;29(1):147–155. doi: 10.1016/j.berh.2015.04.027. http://europepmc.org/abstract/MED/26267008 .S1521-6942(15)00034-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chopra K, Arora V. An intricate relationship between pain and depression: clinical correlates, coactivation factors and therapeutic targets. Expert Opin Ther Targets. 2014 Feb;18(2):159–176. doi: 10.1517/14728222.2014.855720. [DOI] [PubMed] [Google Scholar]
- 5.Wong W, Li M, Yung P, Leong H. The effect of psychological factors on pain, function and quality of life in patients with rotator cuff tendinopathy: A systematic review. Musculoskelet Sci Pract. 2020 Jun;47:102173. doi: 10.1016/j.msksp.2020.102173.S2468-7812(19)30576-4 [DOI] [PubMed] [Google Scholar]
- 6.Puntillo F, Giglio M, Paladini A, Perchiazzi G, Viswanath O, Urits I, Sabbà C, Varrassi G, Brienza N. Pathophysiology of musculoskeletal pain: a narrative review. Ther Adv Musculoskelet Dis. 2021;13:1759720X21995067. doi: 10.1177/1759720X21995067. https://journals.sagepub.com/doi/10.1177/1759720X21995067?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .10.1177_1759720X21995067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cochrane A, Higgins NM, Rothwell C, Ashton J, Breen R, Corcoran O, FitzGerald O, Gallagher P, Desmond D. Work outcomes in patients who stay at work despite musculoskeletal pain. J Occup Rehabil. 2018 Sep;28(3):559–567. doi: 10.1007/s10926-017-9748-4.10.1007/s10926-017-9748-4 [DOI] [PubMed] [Google Scholar]
- 8.Melkevik O, Clausen T, Pedersen J, Garde AH, Holtermann A, Rugulies R. Comorbid symptoms of depression and musculoskeletal pain and risk of long term sickness absence. BMC Public Health. 2018 Aug 06;18(1):981. doi: 10.1186/s12889-018-5740-y. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-5740-y .10.1186/s12889-018-5740-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012 Jul 07;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. https://linkinghub.elsevier.com/retrieve/pii/S0140-6736(12)60240-2 .S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 10.Lentz TA, Harman JS, Marlow NM, Beneciuk JM, Fillingim RB, George SZ. Factors associated with persistently high-cost health care utilization for musculoskeletal pain. PLoS One. 2019;14(11):e0225125. doi: 10.1371/journal.pone.0225125. https://dx.plos.org/10.1371/journal.pone.0225125 .PONE-D-19-18187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bilal J, Berlinberg A, Trost J, Riaz IB, Bhattacharjee S. The influence of depression on health care expenditures among adults with spondylosis, intervertebral disc disorders, and other back problems in the United States. Pain Med. 2020 Feb 01;21(2):e45–e53. doi: 10.1093/pm/pny223.5185157 [DOI] [PubMed] [Google Scholar]
- 12.Allen D, Hines EW, Pazdernik V, Konecny LT, Breitenbach E. Four-year review of presenteeism data among employees of a large United States health care system: a retrospective prevalence study. Hum Resour Health. 2018 Nov 09;16(1):59. doi: 10.1186/s12960-018-0321-9. https://human-resources-health.biomedcentral.com/articles/10.1186/s12960-018-0321-9 .10.1186/s12960-018-0321-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of lost productive work time among US workers with depression. JAMA. 2003 Jun 18;289(23):3135–3144. doi: 10.1001/jama.289.23.3135.289/23/3135 [DOI] [PubMed] [Google Scholar]
- 14.Dieleman JL, Cao J, Chapin A, Chen C, Li Z, Liu A, Horst C, Kaldjian A, Matyasz T, Scott KW, Bui AL, Campbell M, Duber HC, Dunn AC, Flaxman AD, Fitzmaurice C, Naghavi M, Sadat N, Shieh P, Squires E, Yeung K, Murray CJL. US health care spending by payer and health condition, 1996-2016. JAMA. 2020 Mar 03;323(9):863–884. doi: 10.1001/jama.2020.0734. http://europepmc.org/abstract/MED/32125402 .2762309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, Callahan L, Copenhaver C, Dodge C, Felson D, Gellar K, Harvey WF, Hawker G, Herzig E, Kwoh CK, Nelson AE, Samuels J, Scanzello C, White D, Wise B, Altman RD, DiRenzo D, Fontanarosa J, Giradi G, Ishimori M, Misra D, Shah AA, Shmagel AK, Thoma LM, Turgunbaev M, Turner AS, Reston J. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2020 Feb;72(2):149–162. doi: 10.1002/acr.24131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Guideline Centre . Low Back Pain and Sciatica in Over 16s: Assessment and Management. London, UK: National Institute for Health and Care Excellence; 2016. [PubMed] [Google Scholar]
- 17.Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, Straker L, Maher CG, O'Sullivan PPB. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020 Jan 02;54(2):79–86. doi: 10.1136/bjsports-2018-099878.bjsports-2018-099878 [DOI] [PubMed] [Google Scholar]
- 18.Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, Haythornthwaite JA, Jensen MP, Kerns RD, Ader DN, Brandenburg N, Burke LB, Cella D, Chandler J, Cowan P, Dimitrova R, Dionne R, Hertz S, Jadad AR, Katz NP, Kehlet H, Kramer LD, Manning DC, McCormick C, McDermott MP, McQuay HJ, Patel S, Porter L, Quessy S, Rappaport BA, Rauschkolb C, Revicki DA, Rothman M, Schmader KE, Stacey BR, Stauffer JW, von Stein T, White RE, Witter J, Zavisic S. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008 Feb;9(2):105–121. doi: 10.1016/j.jpain.2007.09.005.S1526-5900(07)00899-1 [DOI] [PubMed] [Google Scholar]
- 19.Skúladóttir H, Sveinsdottir H, Holden JE, Gunnarsdóttir TJ, Halldorsdottir S, Björnsdottir A. Pain, sleep, and health-related quality of life after multidisciplinary intervention for chronic pain. Int J Environ Res Public Health. 2021 Sep 28;18(19):10233. doi: 10.3390/ijerph181910233. https://www.mdpi.com/resolver?pii=ijerph181910233 .ijerph181910233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marin TJ, Van Eerd D, Irvin E, Couban R, Koes BW, Malmivaara A, van Tulder MW, Kamper SJ. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain. Cochrane Database Syst Rev. 2017 Jun 28;6:CD002193. doi: 10.1002/14651858.CD002193.pub2. http://europepmc.org/abstract/MED/28656659 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kemp S. Digital 2022: Global overview report. Datareportal. 2022. Jan 26, [2022-01-30]. https://datareportal.com/reports/digital-2022-global-overview-report .
- 22.Moshe I, Terhorst Y, Philippi P, Domhardt M, Cuijpers P, Cristea I, Pulkki-Råback L, Baumeister H, Sander LB. Digital interventions for the treatment of depression: a meta-analytic review. Psychol Bull. 2021 Aug;147(8):749–786. doi: 10.1037/bul0000334.2022-09577-001 [DOI] [PubMed] [Google Scholar]
- 23.Singla DR, Raviola G, Patel V. Scaling up psychological treatments for common mental disorders: a call to action. World Psychiatry. 2018 Jun;17(2):226–227. doi: 10.1002/wps.20532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fiani B, Siddiqi I, Lee SC, Dhillon L. Telerehabilitation: development, application, and need for increased usage in the COVID-19 era for patients with spinal pathology. Cureus. 2020 Sep 21;12(9):e10563. doi: 10.7759/cureus.10563. http://europepmc.org/abstract/MED/33101809 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wehmann E, Köhnen M, Härter M, Liebherz S. Therapeutic alliance in technology-based interventions for the treatment of depression: systematic review. J Med Internet Res. 2020 Jun 11;22(6):e17195. doi: 10.2196/17195. https://www.jmir.org/2020/6/e17195/ v22i6e17195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baumeister H, Paganini S, Sander LB, Lin J, Schlicker S, Terhorst Y, Moshagen M, Bengel J, Lehr D, Ebert DD. Effectiveness of a guided internet- and mobile-based intervention for patients with chronic back pain and depression (WARD-BP): a multicenter, pragmatic randomized controlled trial. Psychother Psychosom. 2021;90(4):255–268. doi: 10.1159/000511881.000511881 [DOI] [PubMed] [Google Scholar]
- 27.Sander LB, Paganini S, Terhorst Y, Schlicker S, Lin J, Spanhel K, Buntrock C, Ebert DD, Baumeister H. Effectiveness of a guided web-based self-help intervention to prevent depression in patients with persistent back pain: the PROD-BP randomized clinical trial. JAMA Psychiatry. 2020 Oct 01;77(10):1001–1011. doi: 10.1001/jamapsychiatry.2020.1021. http://europepmc.org/abstract/MED/32459348 .2765972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Telehealth for the Treatment of Serious Mental Illness and Substance Use Disorders. [2021-01-30]. https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP21-06-02-001.pdf .
- 29.Jansen-Kosterink S, Huis in ’t Veld R, Wever D, Hermens H, Vollenbroek-Hutten M. Introducing remote physical rehabilitation for patients with chronic disorders by means of telemedicine. Health Technol. 2015 May 7;5(2):83–90. doi: 10.1007/s12553-015-0111-5. [DOI] [Google Scholar]
- 30.Pekyavas NO, Ergun N. Comparison of virtual reality exergaming and home exercise programs in patients with subacromial impingement syndrome and scapular dyskinesis: Short term effect. Acta Orthop Traumatol Turc. 2017 May;51(3):238–242. doi: 10.1016/j.aott.2017.03.008.S1017-995X(17)30180-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kosterink SM, Huis in 't Veld RMHA, Cagnie B, Hasenbring M, Vollenbroek-Hutten MMR. The clinical effectiveness of a myofeedback-based teletreatment service in patients with non-specific neck and shoulder pain: a randomized controlled trial. J Telemed Telecare. 2010;16(6):316–321. doi: 10.1258/jtt.2010.006005.16/6/316 [DOI] [PubMed] [Google Scholar]
- 32.Bossen D, Veenhof C, Van Beek KEC, Spreeuwenberg PM, Dekker J, De Bakker DH. Effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis: randomized controlled trial. J Med Internet Res. 2013 Nov 22;15(11):e257. doi: 10.2196/jmir.2662. https://www.jmir.org/2013/11/e257/ v15i11e257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garcia LM, Birckhead BJ, Krishnamurthy P, Sackman J, Mackey IG, Louis RG, Salmasi V, Maddox T, Darnall BD. An 8-week self-administered at-home behavioral skills-based virtual reality program for chronic low back pain: double-blind, randomized, placebo-controlled trial conducted during COVID-19. J Med Internet Res. 2021 Feb 22;23(2):e26292. doi: 10.2196/26292. https://www.jmir.org/2021/2/e26292/ v23i2e26292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bailey JF, Agarwal V, Zheng P, Smuck M, Fredericson M, Kennedy DJ, Krauss J. Digital care for chronic musculoskeletal pain: 10,000 participant longitudinal cohort study. J Med Internet Res. 2020 May 11;22(5):e18250. doi: 10.2196/18250. https://www.jmir.org/2020/5/e18250/ v22i5e18250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Calner T, Nordin C, Eriksson MK, Nyberg L, Gard G, Michaelson P. Effects of a self-guided, web-based activity programme for patients with persistent musculoskeletal pain in primary healthcare: A randomized controlled trial. Eur J Pain. 2017 Jul;21(6):1110–1120. doi: 10.1002/ejp.1012. [DOI] [PubMed] [Google Scholar]
- 36.Malliaras P, Cridland K, Hopmans R, Ashton S, Littlewood C, Page R, Harris I, Skouteris H, Haines T. Internet and telerehabilitation-delivered management of rotator cuff-related shoulder pain (INTEL Trial): randomized controlled pilot and feasibility trial. JMIR Mhealth Uhealth. 2020 Nov 18;8(11):e24311. doi: 10.2196/24311. https://mhealth.jmir.org/2020/11/e24311/ v8i11e24311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Janela D, Costa F, Molinos M, Moulder RG, Lains J, Francisco GE, Bento V, Cohen SP, Correia FD. Asynchronous and tailored digital rehabilitation of chronic shoulder pain: a prospective longitudinal cohort study. J Pain Res. 2022;15:53–66. doi: 10.2147/JPR.S343308.343308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Correia FD, Molinos M, Neves C, Janela D, Carvalho D, Luis S, Francisco GE, Lains J, Bento V. Digital rehabilitation for acute ankle sprains: prospective longitudinal cohort study. JMIR Rehabil Assist Technol. 2021 Sep 30;8(3):e31247. doi: 10.2196/31247. https://rehab.jmir.org/2021/3/e31247/ v8i3e31247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Costa F, Janela D, Molinos M, Lains J, Francisco GE, Bento V, Dias Correia F. Telerehabilitation of acute musculoskeletal multi-disorders: prospective, single-arm, interventional study. BMC Musculoskelet Disord. 2022 Jan 04;23(1):29. doi: 10.1186/s12891-021-04891-5. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-021-04891-5 .10.1186/s12891-021-04891-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Correia FD, Nogueira A, Magalhães I, Guimarães J, Moreira M, Barradas I, Teixeira L, Tulha J, Seabra R, Lains J, Bento V. Home-based rehabilitation with a novel digital biofeedback system versus conventional in-person rehabilitation after total knee replacement: a feasibility study. Sci Rep. 2018 Jul 26;8(1):11299. doi: 10.1038/s41598-018-29668-0.10.1038/s41598-018-29668-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Correia FD, Nogueira A, Magalhães I, Guimarães J, Moreira M, Barradas I, Molinos M, Teixeira L, Tulha J, Seabra R, Lains J, Bento V. Medium-term outcomes of digital versus conventional home-based rehabilitation after total knee arthroplasty: prospective, parallel-group feasibility study. JMIR Rehabil Assist Technol. 2019 Feb 28;6(1):e13111. doi: 10.2196/13111. https://rehab.jmir.org/2019/1/e13111/ v6i1e13111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Correia FD, Molinos M, Luís S, Carvalho D, Carvalho C, Costa P, Seabra R, Francisco G, Bento V, Lains J. Digitally assisted versus conventional home-based rehabilitation after arthroscopic rotator cuff repair: a randomized controlled trial. Am J Phys Med Rehabil. 2022 Mar 01;101(3):237–249. doi: 10.1097/PHM.0000000000001780. http://europepmc.org/abstract/MED/33935152 .00002060-202203000-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dias Correia F, Nogueira A, Magalhães I, Guimarães J, Moreira M, Barradas I, Molinos M, Teixeira L, Pires J, Seabra R, Lains J, Bento V. Digital versus conventional rehabilitation after total hip arthroplasty: a single-center, parallel-group pilot study. JMIR Rehabil Assist Technol. 2019 Jun 21;6(1):e14523. doi: 10.2196/14523. https://rehab.jmir.org/2019/1/e14523/ v6i1e14523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams ACDC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012 Nov 14;11:CD007407. doi: 10.1002/14651858.CD007407.pub3. http://europepmc.org/abstract/MED/23152245 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Joypaul S, Kelly F, McMillan SS, King MA. Multi-disciplinary interventions for chronic pain involving education: A systematic review. PLoS One. 2019 Oct 2;14(10):e0223306. doi: 10.1371/journal.pone.0223306. https://dx.plos.org/10.1371/journal.pone.0223306 .PONE-D-19-00944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bijker L, Sleijser-Koehorst MLS, Coppieters MW, Cuijpers P, Scholten-Peeters GGM. Preferred self-administered questionnaires to assess depression, anxiety and somatization in people with musculoskeletal pain - a modified Delphi study. J Pain. 2020;21(3-4):409–417. doi: 10.1016/j.jpain.2019.08.006. https://linkinghub.elsevier.com/retrieve/pii/S1526-5900(19)30048-3 .S1526-5900(19)30048-3 [DOI] [PubMed] [Google Scholar]
- 47.Costantini L, Pasquarella C, Odone A, Colucci ME, Costanza A, Serafini G, Aguglia A, Belvederi Murri M, Brakoulias V, Amore M, Ghaemi SN, Amerio A. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): a systematic review. J Affect Disord. 2021 Jan 15;279:473–483. doi: 10.1016/j.jad.2020.09.131.S0165-0327(20)32828-7 [DOI] [PubMed] [Google Scholar]
- 48.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006 May 22;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092.166/10/1092 [DOI] [PubMed] [Google Scholar]
- 49.George SZ, Stryker SE. Fear-avoidance beliefs and clinical outcomes for patients seeking outpatient physical therapy for musculoskeletal pain conditions. J Orthop Sports Phys Ther. 2011 Apr;41(4):249–259. doi: 10.2519/jospt.2011.3488.2559 [DOI] [PubMed] [Google Scholar]
- 50.Ospina MB, Dennett L, Waye A, Jacobs P, Thompson AH. A systematic review of measurement properties of instruments assessing presenteeism. Am J Manag Care. 2015 Feb 01;21(2):e171–e185. https://www.ajmc.com/pubMed.php?pii=86029 .86029 [PubMed] [Google Scholar]
- 51.Miles CL, Pincus T, Carnes D, Homer KE, Taylor SJC, Bremner SA, Rahman A, Underwood M. Can we identify how programmes aimed at promoting self-management in musculoskeletal pain work and who benefits? A systematic review of sub-group analysis within RCTs. Eur J Pain. 2011 Sep;15(8):775. doi: 10.1016/j.ejpain.2011.01.016.S1090-3801(11)00033-4 [DOI] [PubMed] [Google Scholar]
- 52.de Rooij A, Roorda LD, Otten RHJ, van der Leeden M, Dekker J, Steultjens MPM. Predictors of multidisciplinary treatment outcome in fibromyalgia:a systematic review. Disabil Rehabil. 2013 Mar;35(6):437–449. doi: 10.3109/09638288.2012.699582. [DOI] [PubMed] [Google Scholar]
- 53.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Annals. 2002 Sep 01;32(9):509–515. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- 54.Iacobucci D. Structural equations modeling: fit indices, sample size, and advanced topics. J Consum Psychol. 2010 Jan;20(1):90–98. doi: 10.1016/j.jcps.2009.09.003. [DOI] [Google Scholar]
- 55.Pfaffel A, Schober B, Spiel C. A comparison of three approaches to correct for direct and indirect range restrictions: a simulation study. Pract Assess Res Evaluation. 2016;21:6. doi: 10.7275/x4ep-fv42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xiao J, Bulut O. Evaluating the performances of missing data handling methods in ability estimation from sparse data. Educ Psychol Meas. 2020 Oct;80(5):932–954. doi: 10.1177/0013164420911136. http://europepmc.org/abstract/MED/32855565 .10.1177_0013164420911136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McNeish D, Matta T. Differentiating between mixed-effects and latent-curve approaches to growth modeling. Behav Res Methods. 2018 Aug;50(4):1398–1414. doi: 10.3758/s13428-017-0976-5.10.3758/s13428-017-0976-5 [DOI] [PubMed] [Google Scholar]
- 58.Hooten WM. Chronic pain and mental health disorders: shared neural mechanisms, epidemiology, and treatment. Mayo Clin Proc. 2016 Jul;91(7):955–970. doi: 10.1016/j.mayocp.2016.04.029.S0025-6196(16)30182-3 [DOI] [PubMed] [Google Scholar]
- 59.Kroenke K, Wu J, Bair MJ, Krebs EE, Damush TM, Tu W. Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain. 2011 Sep;12(9):964–973. doi: 10.1016/j.jpain.2011.03.003. http://europepmc.org/abstract/MED/21680251 .S1526-5900(11)00487-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Farin E, Gramm L, Schmidt E. The patient-physician relationship in patients with chronic low back pain as a predictor of outcomes after rehabilitation. J Behav Med. 2013 Jun;36(3):246–258. doi: 10.1007/s10865-012-9419-z. [DOI] [PubMed] [Google Scholar]
- 61.Tseli E, Boersma K, Stålnacke BM, Enthoven P, Gerdle B, Äng BO, Grooten WJA. Prognostic factors for physical functioning after multidisciplinary rehabilitation in patients with chronic musculoskeletal pain: a systematic review and meta-analysis. Clin J Pain. 2019 Feb;35(2):148–173. doi: 10.1097/AJP.0000000000000669. http://europepmc.org/abstract/MED/30371517 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Steffen A, Nübel J, Jacobi F, Bätzing J, Holstiege J. Mental and somatic comorbidity of depression: a comprehensive cross-sectional analysis of 202 diagnosis groups using German nationwide ambulatory claims data. BMC Psychiatry. 2020 Mar 30;20(1):142. doi: 10.1186/s12888-020-02546-8. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-020-02546-8 .10.1186/s12888-020-02546-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thaipisuttikul P, Ittasakul P, Waleeprakhon P, Wisajun P, Jullagate S. Psychiatric comorbidities in patients with major depressive disorder. Neuropsychiatr Dis Treat. 2014;10:2097–2103. doi: 10.2147/NDT.S72026.ndt-10-2097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Simula AS, Ruokolainen O, Oura P, Lausmaa M, Holopainen R, Paukkunen M, Auvinen J, Linton SJ, Hill JC, Karppinen J. Association of STarT Back Tool and the short form of the Örebro Musculoskeletal Pain Screening Questionnaire with multidimensional risk factors. Sci Rep. 2020 Jan 14;10(1):290. doi: 10.1038/s41598-019-57105-3.10.1038/s41598-019-57105-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vincent HK, Adams MCB, Vincent KR, Hurley RW. Musculoskeletal pain, fear avoidance behaviors, and functional decline in obesity: potential interventions to manage pain and maintain function. Reg Anesth Pain Med. 2013;38(6):481–491. doi: 10.1097/AAP.0000000000000013. [DOI] [PubMed] [Google Scholar]
- 66.Ang DC, Bair MJ, Damush TM, Wu J, Tu W, Kroenke K. Predictors of pain outcomes in patients with chronic musculoskeletal pain co-morbid with depression: results from a randomized controlled trial. Pain Med. 2010 Apr;11(4):482–491. doi: 10.1111/j.1526-4637.2009.00759.x.PME759 [DOI] [PubMed] [Google Scholar]
- 67.Wijnhoven HAH, de Vet HCW, Picavet HSJ. Prevalence of musculoskeletal disorders is systematically higher in women than in men. Clin J Pain. 2006 Oct;22(8):717–724. doi: 10.1097/01.ajp.0000210912.95664.53.00002508-200610000-00008 [DOI] [PubMed] [Google Scholar]
- 68.Narusyte J, Ropponen A, Mittendorfer-Rutz E, Svedberg P. Shared liability to pain, common mental disorders, and long-term work disability differs among women and men. Pain. 2020 May;161(5):1005–1011. doi: 10.1097/j.pain.0000000000001787. http://europepmc.org/abstract/MED/31977936 .00006396-202005000-00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Priebe JA, Haas KK, Moreno Sanchez LF, Schoefmann K, Utpadel-Fischler DA, Stockert P, Thoma R, Schiessl C, Kerkemeyer L, Amelung V, Jedamzik S, Reichmann J, Marschall U, Toelle TR. Digital treatment of back pain versus standard of care: the cluster-randomized controlled trial, Rise-uP. J Pain Res. 2020;13:1823–1838. doi: 10.2147/JPR.S260761.260761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Huber S, Priebe JA, Baumann K, Plidschun A, Schiessl C, Tölle TR. Treatment of low back pain with a digital multidisciplinary pain treatment app: short-term results. JMIR Rehabil Assist Technol. 2017 Dec 04;4(2):e11. doi: 10.2196/rehab.9032. https://rehab.jmir.org/2017/2/e11/ v4i2e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang G, Yang M, Hong M, Krauss J, Bailey JF. Clinical outcomes one year after a digital musculoskeletal (MSK) program: an observational, longitudinal study with nonparticipant comparison group. BMC Musculoskelet Disord. 2022 Mar 11;23(1):237. doi: 10.1186/s12891-022-05188-x. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-022-05188-x .10.1186/s12891-022-05188-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pinheiro MB, Ferreira ML, Refshauge K, Maher CG, Ordoñana JR, Andrade TB, Tsathas A, Ferreira PH. Symptoms of depression as a prognostic factor for low back pain: a systematic review. Spine J. 2016 Jan 01;16(1):105–116. doi: 10.1016/j.spinee.2015.10.037.S1529-9430(15)01622-8 [DOI] [PubMed] [Google Scholar]
- 73.Orenius T, Koskela T, Koho P, Pohjolainen T, Kautiainen H, Haanpää M, Hurri H. Anxiety and depression are independent predictors of quality of life of patients with chronic musculoskeletal pain. J Health Psychol. 2013 Feb;18(2):167–175. doi: 10.1177/1359105311434605.1359105311434605 [DOI] [PubMed] [Google Scholar]
- 74.Alhowimel A, AlOtaibi M, Radford K, Coulson N. Psychosocial factors associated with change in pain and disability outcomes in chronic low back pain patients treated by physiotherapist: A systematic review. SAGE Open Med. 2018;6:2050312118757387. doi: 10.1177/2050312118757387. https://journals.sagepub.com/doi/10.1177/2050312118757387?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .10.1177_2050312118757387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Smith JA, Russo L, Santayana N. Fear avoidance predicts persistent pain in young adults with low back pain: a prospective study. J Orthop Sports Phys Ther. 2021 Aug;51(8):383–391. doi: 10.2519/jospt.2021.9828. http://europepmc.org/abstract/MED/33998262 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zale EL, Ditre JW. Pain-related fear, disability, and the fear-avoidance model of chronic pain. Curr Opin Psychol. 2015 Oct 01;5:24–30. doi: 10.1016/j.copsyc.2015.03.014. http://europepmc.org/abstract/MED/25844393 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zale EL, Lange KL, Fields SA, Ditre JW. The relation between pain-related fear and disability: a meta-analysis. J Pain. 2013 Oct;14(10):1019–1030. doi: 10.1016/j.jpain.2013.05.005. http://europepmc.org/abstract/MED/23850095 .S1526-5900(13)01030-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wertli MM, Rasmussen-Barr E, Weiser S, Bachmann LM, Brunner F. The role of fear avoidance beliefs as a prognostic factor for outcome in patients with nonspecific low back pain: a systematic review. Spine J. 2014 May 01;14(5):816–836. doi: 10.1016/j.spinee.2013.09.036.S1529-9430(13)01576-3 [DOI] [PubMed] [Google Scholar]
- 79.Chester R, Jerosch-Herold C, Lewis J, Shepstone L. Psychological factors are associated with the outcome of physiotherapy for people with shoulder pain: a multicentre longitudinal cohort study. Br J Sports Med. 2018 Feb;52(4):269–275. doi: 10.1136/bjsports-2016-096084. http://bjsm.bmj.com/lookup/pmidlookup?view=long&pmid=27445360 .bjsports-2016-096084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Haik MN, Alburquerque-Sendín F, Fernandes RAS, Kamonseki DH, Almeida LA, Liebano RE, Camargo PR. Biopsychosocial aspects in individuals with acute and chronic rotator cuff related shoulder pain: classification based on a decision tree analysis. Diagnostics. 2020 Nov 10;10(11):928. doi: 10.3390/diagnostics10110928. https://www.mdpi.com/resolver?pii=diagnostics10110928 .diagnostics10110928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Blanquero J, Cortés-Vega MD, Rodríguez-Sánchez-Laulhé P, Corrales-Serra B, Gómez-Patricio E, Díaz-Matas N, Suero-Pineda A. Feedback-guided exercises performed on a tablet touchscreen improve return to work, function, strength and healthcare usage more than an exercise program prescribed on paper for people with wrist, hand or finger injuries: a randomised trial. J Physiother. 2020 Oct;66(4):236–242. doi: 10.1016/j.jphys.2020.09.012. https://linkinghub.elsevier.com/retrieve/pii/S1836-9553(20)30107-7 .S1836-9553(20)30107-7 [DOI] [PubMed] [Google Scholar]
- 82.Irvine AB, Russell H, Manocchia M, Mino DE, Cox Glassen T, Morgan R, Gau JM, Birney AJ, Ary DV. Mobile-web app to self-manage low back pain: randomized controlled trial. J Med Internet Res. 2015 Jan 02;17(1):e1. doi: 10.2196/jmir.3130. https://www.jmir.org/2015/1/e1/ v17i1e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Eek F, Axmon A. Gender inequality at home is associated with poorer health for women. Scand J Public Health. 2015 Mar;43(2):176–182. doi: 10.1177/1403494814562598.1403494814562598 [DOI] [PubMed] [Google Scholar]
- 84.Cerrato J, Cifre E. Gender inequality in household chores and work-family conflict. Front Psychol. 2018;9:1330. doi: 10.3389/fpsyg.2018.01330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nicolson PJA, Bennell KL, Dobson FL, Van Ginckel A, Holden MA, Hinman RS. Interventions to increase adherence to therapeutic exercise in older adults with low back pain and/or hip/knee osteoarthritis: a systematic review and meta-analysis. Br J Sports Med. 2017 May;51(10):791–799. doi: 10.1136/bjsports-2016-096458.bjsports-2016-096458 [DOI] [PubMed] [Google Scholar]
- 86.Jordan JL, Holden MA, Mason EE, Foster NE. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2010 Jan 20;(1):CD005956. doi: 10.1002/14651858.CD005956.pub2. http://europepmc.org/abstract/MED/20091582 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Samdal GB, Eide GE, Barth T, Williams G, Meland E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int J Behav Nutr Phys Act. 2017 Mar 28;14(1):42. doi: 10.1186/s12966-017-0494-y. https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-017-0494-y .10.1186/s12966-017-0494-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Maestroni L, Read P, Bishop C, Papadopoulos K, Suchomel TJ, Comfort P, Turner A. The benefits of strength training on musculoskeletal system health: practical applications for interdisciplinary care. Sports Med. 2020 Aug;50(8):1431–1450. doi: 10.1007/s40279-020-01309-5.10.1007/s40279-020-01309-5 [DOI] [PubMed] [Google Scholar]
- 89.Russell S, Jariwala A, Conlon R, Selfe J, Richards J, Walton M. A blinded, randomized, controlled trial assessing conservative management strategies for frozen shoulder. J Shoulder Elbow Surg. 2014 Apr;23(4):500–507. doi: 10.1016/j.jse.2013.12.026.S1058-2746(14)00005-6 [DOI] [PubMed] [Google Scholar]
- 90.Hanratty CE, McVeigh JG, Kerr DP, Basford JR, Finch MB, Pendleton A, Sim J. The effectiveness of physiotherapy exercises in subacromial impingement syndrome: a systematic review and meta-analysis. Semin Arthritis Rheum. 2012 Dec;42(3):297–316. doi: 10.1016/j.semarthrit.2012.03.015.S0049-0172(12)00090-X [DOI] [PubMed] [Google Scholar]
- 91.Aragonès E, Rambla C, López-Cortacans G, Tomé-Pires C, Sánchez-Rodríguez E, Caballero A, Miró J. Effectiveness of a collaborative care intervention for managing major depression and chronic musculoskeletal pain in primary care: A cluster-randomised controlled trial. J Affect Disord. 2019 Jun 01;252:221–229. doi: 10.1016/j.jad.2019.04.004.S0165-0327(18)32947-1 [DOI] [PubMed] [Google Scholar]
- 92.Yardley L, Spring BJ, Riper H, Morrison LG, Crane DH, Curtis K, Merchant GC, Naughton F, Blandford A. Understanding and promoting effective engagement with digital behavior change interventions. Am J Prev Med. 2016 Nov;51(5):833–842. doi: 10.1016/j.amepre.2016.06.015.S0749-3797(16)30243-4 [DOI] [PubMed] [Google Scholar]
- 93.Bennell KL, Marshall CJ, Dobson F, Kasza J, Lonsdale C, Hinman RS. Does a web-based exercise programming system improve home exercise adherence for people with musculoskeletal conditions?: a randomized controlled trial. Am J Phys Med Rehabil. 2019 Oct;98(10):850–858. doi: 10.1097/PHM.0000000000001204. [DOI] [PubMed] [Google Scholar]
- 94.Palazzo C, Klinger E, Dorner V, Kadri A, Thierry O, Boumenir Y, Martin W, Poiraudeau S, Ville I. Barriers to home-based exercise program adherence with chronic low back pain: Patient expectations regarding new technologies. Ann Phys Rehabil Med. 2016 Apr;59(2):107–113. doi: 10.1016/j.rehab.2016.01.009. https://linkinghub.elsevier.com/retrieve/pii/S1877-0657(16)00034-8 .S1877-0657(16)00034-8 [DOI] [PubMed] [Google Scholar]
- 95.Keefe FJ, Main CJ, George SZ. Advancing psychologically informed practice for patients with persistent musculoskeletal pain: promise, pitfalls, and solutions. Phys Ther. 2018 May 01;98(5):398–407. doi: 10.1093/ptj/pzy024. http://europepmc.org/abstract/MED/29669084 .4925489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hutting N, Caneiro JP, Ong'wen OM, Miciak M, Roberts L. Patient-centered care in musculoskeletal practice: Key elements to support clinicians to focus on the person. Musculoskelet Sci Pract. 2022 Feb;57:102434. doi: 10.1016/j.msksp.2021.102434. https://linkinghub.elsevier.com/retrieve/pii/S2468-7812(21)00118-1 .S2468-7812(21)00118-1 [DOI] [PubMed] [Google Scholar]
- 97.Geraghty AWA, Roberts LC, Stanford R, Hill JC, Yoganantham D, Little P, Foster NE, Hay EM, Yardley L. Exploring patients' experiences of internet-based self-management support for low back pain in primary care. Pain Med. 2020 Sep 01;21(9):1806–1817. doi: 10.1093/pm/pnz312. http://europepmc.org/abstract/MED/31841156 .5678766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Slade SC, Patel S, Underwood M, Keating JL. What are patient beliefs and perceptions about exercise for nonspecific chronic low back pain? A systematic review of qualitative studies. Clin J Pain. 2014 Nov;30(11):995–1005. doi: 10.1097/AJP.0000000000000044. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Example path diagram for the latent growth curve (LGC) models used in the current study (Figure S1).
Table S1. Baseline characteristics of the entire cohort.
Table S2. Unconditional latent growth curve analysis: intent-to-treat analysis.
Table S3. Conditional growth-mixture modeling analysis: intent-to-treat analysis.
Data Availability Statement
All relevant data are included in the article or available as supplementary material. The protocol, deidentified data, and analysis codes may be provided upon request to the corresponding author.


