Abstract
Background:
The meta-analysis of randomized controlled trials has illustrated that the efficacy of low-dose non-vitamin K antagonist oral anticoagulants is inferior compared with standard-dose non-vitamin K antagonist oral anticoagulants, though they are still frequently prescribed for Asian patients with non-valvular atrial fibrillation. We aimed to further investigate the efficacy and safety of low-dose non-vitamin K antagonist oral anticoagulants by carrying out a meta-analysis of all relevant randomized controlled trials and cohort studies.
Methods:
Cochrane Central Register of Controlled Trials, Embase, and MEDLINE were systematically searched from the inception to September 9, 2021, for randomized controlled trials or cohorts that compared the efficacy and/or safety of low-dose non-vitamin K antagonist oral anticoagulants in Asian patients with non-valvular atrial fibrillation. The primary outcomes were stroke and major bleeding, and the secondary outcomes were mortality, intracranial hemorrhage, and gastrointestinal hemorrhage. Hazard ratios and 95% CIs were estimated using the random-effect model.
Results:
Nineteen publications involving 371 574 Asian patients with non-valvular atrial fibrillation were included. Compared with standard-dose non-vitamin K antagonist oral anticoagulants, low-dose non-vitamin K antagonist oral anticoagulants showed comparable risks of stroke (hazard ratio, 1.18; 95% CI 0.98 to 1.42), major bleeding (hazard ratio, 1.00; 95% CI 0.83 to 1.21), intracranial hemorrhage (hazard ratio, 1.13; 95% CI 0.92 to 1.38), and gastrointestinal hemorrhage (hazard ratio, 1.07; 95% CI 0.87 to 1.31), though had a higher risk of mortality (hazard ratio, 1.34; 95% CI 1.05 to 1.71). Compared with warfarin, low-dose non-vitamin K antagonist oral anticoagulants were associated with lower risks of stroke (hazard ratio, 0.73; 95% CI 0.67 to 0.79), mortality (hazard ratio, 0.69; 95% CI 0.60 to 0.81), major bleeding (hazard ratio, 0.62; 95% CI 0.51 to 0.75), intracranial hemorrhage (hazard ratio, 0.48; 95% CI 0.33 to 0.69), and gastrointestinal hemorrhage (hazard ratio, 0.78; 95% CI 0.65 to 0.93).
Conclusion:
Low-dose non-vitamin K antagonist oral anticoagulants were superior to warfarin, and comparable to standard-dose non-vitamin K antagonist oral anticoagulants considering risks of stroke, major bleeding, intracranial hemorrhage, and gastrointestinal hemorrhage. Further, high qualified studies are warranted.
Keywords: Atrial fibrillation, NOACs, warfarin, meta-analysis
HIGHLIGHTS
The first meta-analysis of low-dose non-vitamin K antagonist oral anticoagulants (NOACs) including both randomized controlled trials and cohort studies.
Low-dose NOACs were comparable to standard-dose NOACs and superior to warfarin.
Low-dose NOACs might be prescribed effectively and safely for Asian patients with non-valvular atrial fibrillation.
Introduction
Non-valvular atrial fibrillation (NVAF) is a common cardiac arrhythmia worldwide, which can cause ischemic stroke and systemic embolism, seriously endangers the health of global elder patients.1 For few decades, warfarin was prescribed to prevent ischemic stroke from atrial fibrillation (AF) by decreasing the production of several clotting proteins that rely on vitamin K.2 However, the adherence to warfarin is severely affected by the frequent international normalized ratio (INR) monitoring, drug-drug interactions, and drug-food interactions.3 In recent years, the approval of non-vitamin K antagonist oral anticoagulants (NOACs), which directly inhibit the critical factors of the coagulation cascade, provided new anticoagulant strategies for the patients with NVAF.
A meta-analysis including five randomized controlled trials (RCTs) and 6177 patients assessed the efficacy and safety of standard-dose NOACs, low-dose NOACs, and warfarin in Asian patients with NVAF.4 It revealed that low-dose NOACs were inferior to standard-dose NOACs in the efficacy with a higher risk of stroke, and had no superior efficacy than warfarin; standard-dose NOACs were superior to warfarin in the efficacy and safety with less stroke, mortality, intracranial hemorrhage (ICH), and major bleeding.4 However, low-dose NOACs are still frequently prescribed for Asian patients with NVAF. Low-dose NOACs were prescribed for 22%, 26%, and 31% of patients in Japan,5 Taiwan,6 and Korea,7 respectively. RCTs were performed under optimized conditions, strict inclusion and exclusion criteria, which might not fully reflect real-world conditions. Moreover, RCTs enroll a small, non-representative subset of patients and overlook the important interactions between the patients and the real world, which may affect the outcomes.8 Real-world cohort studies, which enroll patients with broad-spectrum baseline characteristics, may provide a more comprehensive picture of the clinical practice.8 Therefore, we aimed to further investigate the efficacy and safety of low-dose NOACs in Asian patients with NVAF by carrying out a meta-analysis of all relevant RCTs and cohort studies.
Methods
This meta-analysis was prepared according to the PRISMA (Preferred Reporting Items for Systemic Reviews and Meta-analysis) and MOOSE (Meta-analysis of Observational Studies in Epidemiology) guidelines.9,10
Search Strategy and Study Selection
Cochrane Central Register of Controlled Trials (from inception to September 9, 2021), MEDLINE (from inception to September 9, 2021), and Embase (from inception to September 9, 2021) were systematically searched. Details of the search strategy are illustrated in Supplementary Table S1.
The inclusion criteria were as follows: (1) studies involved lose-dose NOACs and standard-dose NOACs or warfarin; (2) the target population was Asian patients with NVAF; (3) studies included efficacy (stroke and mortality) or safety outcomes (major bleeding, ICH, and gastrointestinal hemorrhage [GH]); (4) the study type was the cohort or RCT. And the exclusion criteria were as follows: (1) patients with valvular AF or receiving NOACs after catheter ablation; (2) studies published in the forms of conference abstracts, letters, or protocols; (3) for the same data source or overlapping data reported in more than one study, the other studies were excluded apart from the most comprehensive data with the longest follow-up period. References of included studies and relevant meta-analyses were screened for additional eligible studies as well.
Definitions of Low-Dose NOACs, Standard-Dose NOACs, and Warfarin
Definitions were in accordance with the included studies. Standard-dose NOACs and warfarin were defined as dabigatran 150 mg b.i.d., rivaroxaban 20 mg q.d., apixaban 5 mg b.i.d., edoxaban 60 mg q.d., and INR of 2.0-3.0.11 Low-dose NOACs were defined as dabigatran 110 mg b.i.d., rivaroxaban 15/10 mg q.d., apixaban 2.5 mg b.i.d., and edoxaban 30 mg q.d.7 And for patients with creatinine clearance rate (CrCl) of 30-50 mL/min, age ≥ 70 years old, and a prior history of bleeding, standard-dose dabigatran was defined as 110 mg b.i.d.;12,13 for patients with CrCl of 15-50 mL/min, standard-dose rivaroxaban was defined as 10 mg q.d.;14,15 for patients with any 2 of the following characteristics: ≥80 years old, body weight <60 kg, and serum creatinine level (Cr) ≥ 1.5 mg/dL, standard-dose apixaban was defined as 2.5 mg b.i.d.;16,17 for patients with CrCl of 15-50 mL/min or body weight <60 kg, standard-dose edoxaban was defined as 30 mg q.d.18
Data Extraction and Quality Assessment
The primary efficacy outcome was stroke, and the secondary efficacy outcome was mortality (all-cause mortality). The primary safety outcome was major bleeding, defined as fatal bleeding or bleeding in a critical site, and the secondary safety outcomes were ICH and GH.
Two reviewers independently screened titles and abstracts of the retrieved studies to exclude those which did not explore questions of interest, and then independently screened full texts of the remaining studies to identify those which met all the inclusion criteria. We manually checked the reference list of each acquired article for relevant studies. For each included study, two reviewers independently extracted the characteristics of the included studies and patients, as well as outcome measures as predefined. Discrepancies were resolved by discussing with the third reviewer.
Bias risks of RCTs were assessed with the Cochrane Collaboration’s tool19 and cohort studies with the Newcastle-Ottawa quality assessment scale.20 The publication bias was quantitatively assessed by the Begg’s21 and Egger’s tests,22 P < .05 was taken as statistically significant. Two reviewers assessed the risks of bias independently and in duplicate. Any disagreements were resolved in consultation with the supervisor.
Data Synthesis and Statistical Analysis
Intention-to-treat analysis (ITT) results were used wherever possible. If ITT results were not available, we used the data that the author reported. All analyses were performed by Stata 16.0 (StataCorp, College Station, TX, 77845, USA). Hazard ratios (HRs) and corresponding 95% CIs were estimated using the random-effect model. The heterogeneity among studies was assessed by I 2 with <25%, 25-50%, and >50% indicating low, moderate, and a high degree of heterogeneity, respectively. Meta-regression analyses were performed to examine possible sources of the heterogeneity in the data.
Subgroup meta-analyses were performed by stratifying the study type into RCTs and cohort studies to explore different effects of experiment types. Most cohort studies used the propensity score matching (PSM) method to balance the confounding factors between groups, so we enrolled the adjusted cohort studies and RCTs to perform subgroup meta-analyses and minimize the heterogeneity. For all comparisons in this meta-analysis, P < .05 was taken as statistically significant.
Results
Studies Identification and Characteristics
A total of 2846 publications were identified through the database search. After the study screening process, 19 studies consisting of 16 cohort studies and 3 RCTs were included (Figure 1).
Figure 1.
Flow chart for the selection of included studies.
In general, there were 371 574 patients in all included studies. Of which, 152 893 patients were involved in the standard-dose group, including 48 118 patients receiving NOACs and 104 775 patients receiving warfarin, and 218 681 patients were included in the low-dose NOACs group. The baseline characteristics of included studies are shown in Table 1. The detailed previous medical history and group contents of included studies are illustrated in Supplementary Tables S2 and S3.
Table 1.
Patient Baseline Characteristics of Included Studies
| Author (Study), Year | Region | Study Type | Adjusted Method | Group | Sample Size | Age (Years) | Female (%) | Follow-Up (Months) | BMI (kg/m2) | CHA2DS2-VASc | HAS-BLED | CrCl (mL/min) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Murata N, 20195 | Japan | Cohort | PSM | Standard dose | 746 | 66.9 ± 9.0 | 21.6 | 43.6 | 25.0 ± 4.0 | 2.42 ± 1.39 | 1.16 ± 0.85 | 84.1 ± 27.5 |
| Low dose | 369 | 71.2 ± 8.2 | 29.0 | 24.5 ± 3.8 | 2.88 ± 1.39 | 1.25 ± 0.78 | 70.1 ± 21.2 | |||||
| Wakamatsu Y, 202023 | Japan | Cohort | NR | Standard dose | 749 | 63.3 ± 9.4 | 23.0 | 25.7 | 24.7 ± 3.7 | 2.10 ± 1.50 | 0.80 ± 0.80 | 76.7 ± 23.8 |
| Low dose | 216 | 64.8 ± 9.5 | 34.3 | 24.2 ± 3.4 | 2.40 ± 1.60 | 0.90 ± 0.80 | 73.3 ± 22.3 | |||||
| Ohno J, 202124 | Japan | Cohort | PSM | Standard dose | 907 | 66.0 ± 10.0 | 23.3 | 26.5 | 25.0 ± 4.0 | 2.74 | 2.27 | 82.8 |
| Low dose | 338 | 70.0 ± 10.0 | 34.9 | 24.0 ± 4.0 | 3.23 | 2.54 | 73.5 | |||||
| Lee HF, 201825 | Taiwan | Cohort | PSM | Low dose | 26 000 | 78.0 ± 10.0 | 48.0 | NR | NR | 4.02 ± 1.29 | 2.98 ± 0.92 | NR |
| Warfarin | 16 000 | 78.0 ± 10.0 | 48.0 | 4.01 ± 1.28 | 2.99 ± 0.90 | |||||||
| Yu HT, 201826 | Korea | Cohort | PSM | Low dose | 3016 | 72.8 ± 9.1 | 48.0 | 5.0c | NR | 4.90 ± 1.80 | NR | NR |
| Warfarin | 3016 | 72.6 ± 9.9 | 46.7 | 4.80 ± 2.00 | ||||||||
| Chan YH, 201827 | Taiwan | Cohort | PSM | Standard dosea | 6307 | 76.0 ± 10.0 | 45.0 | 35.2 | NR | 3.89 ± 0.84 | 2.96 ± 0.61 | NR |
| Low dosea | 47 392 | |||||||||||
| Warfarin | 19 375 | 76.0 ± 10.0 | 46.0 | 3.89 ± 0.88 | 2.97 ± 0.61 | |||||||
| Kwon CH, 201628 | Korea | Cohort | NR | Standard dosea | 51 | 84.2 ± 3.5 | 60.1 | 24.9 | 24.4 ± 3.6 | 4.70 ± 1.40 | 2.60 ± 1.00 | 51.0 ± 13.9 |
| Low dosea | 97 | |||||||||||
| Warfarin | 145 | 83.2 ± 3.1 | 59.3 | 23.7 ± 3.6 | 4.70 ± 1.40 | 2.40 ± 0.90 | 53.1 ± 17.4 | |||||
| Akagi Y, 201929 | Japan | Cohort | NR | Standard dosea | 187 | 70.8 ± 10.8 | 34.2 | NR | NR | 1.92 ± 1.33b | NR | 69.4 ± 25.3 |
| Low dosea | 488 | |||||||||||
| Yu HT, 20207 | Korea | Cohort | PSM | Standard dose | 32 400 | 69.8 ± 9.5 | 38.2 | 36.0 | NR | 4.60 ± 1.70 | NR | NR |
| Low dose | 16 757 | 70.7 ± 7.9 | 39.0 | 4.50 ± 1.80 | ||||||||
| Cho MS, 201930 | Korea | Cohort | PSM | Low dose | 29 695 | 73.8 ± 8.8 | 49.1 | 15.0 | 24.6 ± 2.9 | 3.60 ± 1.20 | 2.50 ± 0.90 | NR |
| Warfarin | 10 409 | 70.8 ± 11.0 | 46.0 | 24.4 ± 2.8 | 3.50 ± 1.20 | 2.60 ± 1.00 | ||||||
| Jeong HK, 201931 | Korea | Cohort | PSM | Low dose | 414 | 71.4 ± 10.5 | 36.7 | 12.0 | NR | 3.30 ± 1.80 | NR | 85.4 |
| Warfarin | 804 | 70.4 ± 10.2 | 39.6 | 3.40 ± 1.80 | 87.0 | |||||||
| Kohsaka S, 202032 | Japan | Cohort | PSM | Low dose | 17 481 | 76.2 ± 10.6 | 38.9 | 28.9 | NRd | 3.80 ± 1.90 | NR | NR |
| Warfarin | 19 059 | 76.1 ± 11.9 | 38.8 | 3.80 ± 2.10 | ||||||||
| Kohsaka S, 201733 | Japan | Cohort | PSM | Low dose | 6726 | 75.8 ± 10.0 | 38.9 | NR | 23.3 ± 4.5 | 3.30 ± 1.60 | NR | NR |
| warfarin | 6726 | 76.2 ± 10.5 | 38.0 | 23.1 ± 4.2 | 3.40 ± 1.60 | |||||||
| Lai CL, 201834 | Taiwan | Cohort | PSM | Low dose | 1489 | 88.4 ± 2.9 | 48.6 | 6.6 | NR | 3.80 ± 1.30 | NR | NR |
| Warfarin | 1497 | 88.7 ± 3.1 | 54.8 | 3.80 ± 1.20 | ||||||||
| Lee SR, 201935 | Korea | Cohort | PSM | Standard dose | 5196 | 71.2 ± 8.1 | 45.1 | 30.0 | 24.7 ± 3.3 | 3.50 ± 1.60 | NR | 82.5 ± 37.5 |
| Low dose | 5777 | 72.1 ± 8.4 | 44.9 | 24.5 ± 3.5 | 3.60 ± 1.60 | 81.5 ± 49.6 | ||||||
| Warfarin | 5777 | 72.2 ± 8.9 | 46.5 | 24.5 ± 3.4 | 3.70 ± 1.80 | 81.3 ± 41.3 | ||||||
| Chan YH, 201936 | Taiwan | Cohort | PSM | Low dose | 60 212 | 74.7 ± 10.7 | 42.6 | 16.0 | NR | 3.60 ± 0.70 | 2.60 ± 0.50 | NR |
| Warfarin | 19 761 | 74.6 ± 10.7 | 43.3 | 3.60 ± 0.80 | 2.70 ± 0.50 | |||||||
| RE-LY, 201337 | Asia | RCT | Standard dosea | 933 | 68.0 ± 9.8 | 36.2 | 24.0c | NR | 2.20 ± 1.10b | NR | 65.3 ± 22.1 | |
| Low dosea | 923 | |||||||||||
| Warfarina | 926 | |||||||||||
| J-ROCKET AF, 201238 | Japan | RCT | Low dose | 639 | 71.0 | 17.1 | 30.0 | NR | 3.27b | NR | NR | |
| Warfarin | 639 | 71.2 | 21.8 | 3.22b | ||||||||
| ENGAGE AF-TIMI 48, 201639 | Asia | RCT | Standard dosea | 642 | 70.1 ± 8.7 | 28.0 | NR | NR | 2.90 ± 1.00b | NR | NR | |
| Low dosea | 652 | |||||||||||
| Warfarina | 641 |
Values are shown as mean ± SD or n; BMI, body mass index; CrCl, creatinine clearance rate; NR, not reported; PSM, propensity score matching; RCT, randomized controlled trial.
a Means characteristics are the composite of low-dose and standard-dose groups.
b Means the CHADS2 score.
c Means values are shown as the median.
d Means values are shown as the category.
Risks of Bias Assessments
Results of bias assessments are summarized in Supplementary Tables S4-S6. Overall, all included RCTs and most cohort studies reported low risks of bias. While Wakamatsu et al23 (2020), Kwon et al28 (2016), and Akagi et al29 (2019) didn’t balance the confounding factors between groups, which had risks of comparability bias. Lee et al25 (2018), Akagi et al29 (2019), and Kohsaka et al33 (2017) did not report the length of follow-up, and most cohort studies did not show the lost follow-up rate, which had risks of outcome bias. In addition, there was no publication bias for this meta-analysis by the Begg’s and Egger’s tests, except for the risk of ICH (P = .005, Egger's test) in the comparison of low-dose NOACs versus warfarin.
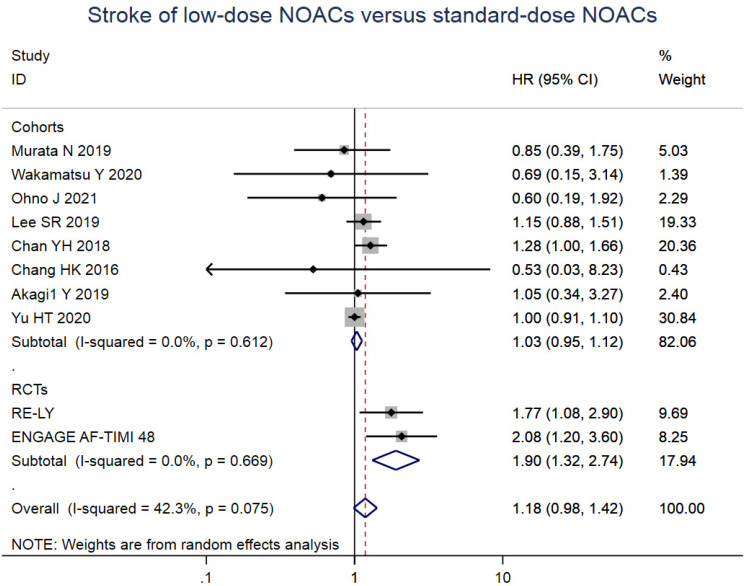
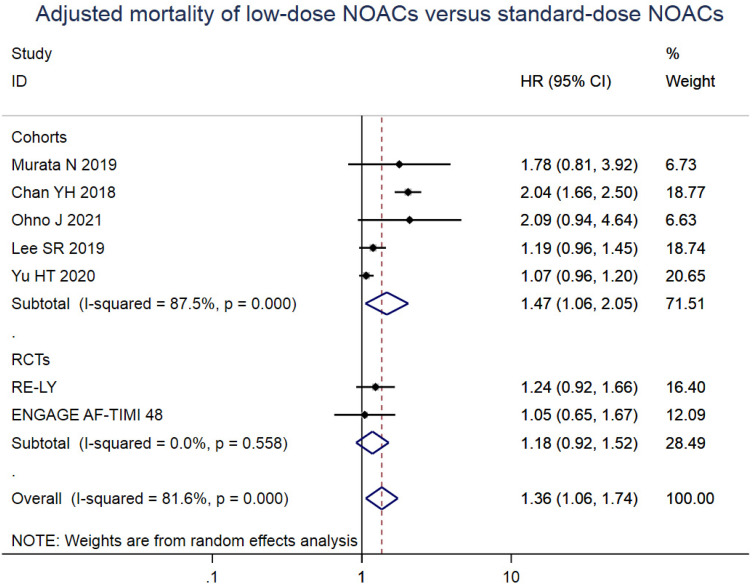
Low-Dose NOACs versus Standard-Dose NOACs
For efficacy outcomes, there was no significant difference between low-dose NOACs and standard-dose NOACs for the risk of stroke (HR = 1.18, 95% CI 0.98 to 1.42, I 2 = 42.3%). However, low-dose NOACs were associated with a slightly higher risk of mortality (HR = 1.34, 95% CI 1.05 to 1.71, I 2 = 79.1%) compared with standard-dose NOACs. For safety outcomes, the risks of major bleeding (HR = 1.00, 95% CI 0.83 to 1.21, I 2 = 46.2%), ICH (HR = 1.13, 95% CI 0.92 to 1.38, I 2 = 2.9%), and GH (HR = 1.07, 95% CI 0.87 to 1.31, I 2 = 34.4%) were similar between two groups. And the results of subgroup meta-analyses were also the same as the overall except for the higher risk of stroke (HR = 1.90, 95% CI 1.32 to 2.74, I 2 = 0%) and comparable risk of mortality (HR = 1.18, 95% CI 0.92 to 1.52, I 2 = 0%) in RCTs (Figure 2). Details of subgroup meta-analyses are illustrated in Supplementary Figures S1-S5.
Figure 3.
Meta-analysis of the efficacy and safety for low-dose NOACs versus warfarin. HR, hazard ratio; RCTs, randomized controlled trials.
Low-Dose NOACs versus Warfarin
For efficacy outcomes, compared with warfarin, low-dose NOACs were associated with lower risks of stroke (HR = 0.73, 95% CI .67 to 0.79, I 2 = 9.6%) and mortality (HR = 0.69, 95% CI 0.60 to 0.81, I 2 = 78.7%). For safety outcomes, in the low-dose NOACs group, the risks of major bleeding (HR = 0.62, 95% CI 0.51 to 0.75, I 2 = 73.5%), ICH (HR = 0.48, 95% CI 0.33 to 0.69, I 2 = 77.1%), and GH (HR = 0.78, 95% CI 0.65 to 0.93, I 2 = 36.1%) were lower compared with warfarin. And the results of subgroup meta-analyses were similar to the overall except for comparable risks of stroke (HR = 0.81, 95% CI 0.56 to 1.15, I 2 = 34.4%), mortality (HR = 0.83, 95% CI 0.57 to 1.22, I 2 = 52.6%), and GH (HR = 0.76, 95% CI 0.48 to 1.22, I 2 = 0%) in RCTs (Figure 3). Details of subgroup meta-analyses are shown in Supplementary Figures S6-S10.
Figure 2.
Meta-analysis of the efficacy and safety for low-dose NOACs versus standard-dose NOACs. HR, hazard ratio; RCTs, randomized controlled trials.
Adjusted Subgroup Meta-Analyses
To minimize the heterogeneity and obtain more reliable results, adjusted subgroup meta-analyses including RCTs and cohort studies with PSM were performed. Results of all outcomes were consistent with the overall meta-analysis. Details of adjusted subgroup meta-analyses are illustrated in Supplementary Figures S11-S16.
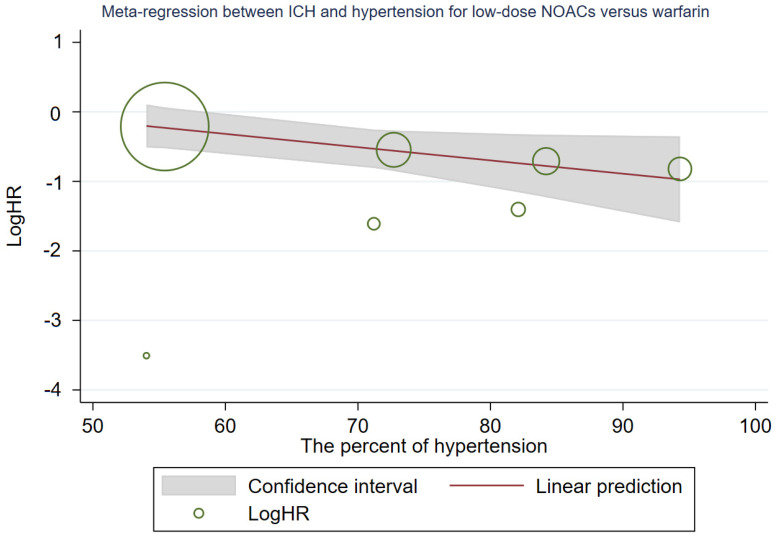
Meta-regression Analyses
No significant correlations were observed in most efficacy and safety outcomes. However, in the comparison of low-dose NOACs versus standard-dose NOACs, a significant correlation was found between mortality and heart failure (P = .023), with HR decreasing as the heart failure percent of included patients increased (Supplementary Figure S17); another significant predictor of HR was found between major bleeding and female (P = .020) as well, with HR increasing as the female percent of included patients ascended (Supplementary Figure S18). In the comparison of low-dose NOACs versus warfarin, potential influencing factors were observed between ICH, mean age (P = .032), and hypertension (P = .038), with HR increasing as the mean age of included patients ascended (Supplementary Figure S19) and HR decreasing as the hypertension percent of included patients increased, respectively (Supplementary Figure S20). Details of meta-regression analyses are illustrated in Supplementary Table S7.
To reduce the heterogeneity, subgroup meta-analyses stratified by the percent of heart failure, female, and hypertension (divided into high percent and low percent groups by the median) were performed, respectively. In general, all results were consistent with the overall meta-analysis. Details of subgroup meta-analyses are shown in Supplementary Figures S21-S23.
Discussion
To our knowledge, this is the first meta-analysis including both cohort studies and RCTs for the efficacy and safety of low-dose NOACs. A previous meta-analysis in 2016 had tried to assess this by RCTs,4 and the results indicated that: when compared with standard-dose NOACs, low-dose NOACs showed the inferior efficacy with a higher risk of stroke and similar safety; when compared with warfarin, low-dose NOACs showed the comparable efficacy and better safety. Even though the meta-analysis of RCTs is the highest level of evidence, results of cohorts may better represent the clinical practice with the additional real-world data. For example, the previous meta-analysis of RCTs solely enrolled patients of approximately 70 years old with the standard weight of roughly 66 kg.4 These may not be generalizable to the underrepresented patients, such as those with low weight, older age, or not yet represented in RCTs, so we performed this meta-analysis.
Our meta-analysis revealed that: when compared with standard-dose NOACs, low-dose NOACs had comparable risks of stroke and bleeding (including major bleeding, ICH, and GH), except for a slightly higher risk of mortality; when compared with warfarin, low-dose NOACs showed lower risks of stroke, mortality, and bleeding. The relatively higher age might explain the higher risk of mortality in the low-dose NOACs group: the mean age of low-dose NOACs group was approximately five years older than standard-dose NOACs group in the studies of Murata (2019),5 Ohno (2021),24 and Chan (2018).27 As another study showed that the older patients with AF were faced with more comorbidities and death factors, would have a higher risk of mortality than younger patients,40 which might eventually lead to the conflicting results. To validate our hypothesis, a subgroup meta-analysis excluding the above three studies was performed, and the result indeed indicated that low-dose NOACs showed a comparable risk of mortality compared with standard-dose NOACs (HR = 1.09, 95% CI 0.99 to 1.21, I 2 = 0%) (Supplementary Figure S24). At the same time, the results of cohort study subgroups were consistent with the overall meta-analysis, and results of RCTs subgroups were similar to the previous meta-analysis, respectively. Most of our results were consistent with the previous meta-analysis of RCTs. However, the inclusion of cohort studies caused some differences, such as the comparable risk of stroke and higher risk of mortality in the comparison of standard-dose NOACs, and lower the risks of stroke, mortality, and GH in the comparison of warfarin.4
As CHA2DS2-VASc and HAS-BLED scores were two important influence factors for the efficacy and safety of NOACs or warfarin, we tried to further interpret the results according to these. For low-dose NOACs versus standard-dose NOACs, CHA2DS2-VASc and HAS-BLED scores of the included patients ranged from 2.10 to 4.70, 0.80 to 2.96, respectively, which indicated that patients in this comparison were associated with high risk of stroke41 and low or moderate risk of bleeding.42 For low-dose NOACs versus warfarin, CHA2DS2-VASc and HAS-BLED scores of the included patients ranged from 3.30 to 4.90, 2.40 to 3.70, respectively, which illustrated that patients in this comparison were associated with the high risk of stroke41 and moderate or high risk of bleeding42 as well. As a result, we could further demonstrate that: (1) for the patients under the high risk of stroke with approximate CHA2DS2-VASc score of 2.0-5.0, and low or moderate risk of bleeding with approximate HAS-BLED score of 0.8-3.0, low-dose NOACs had the comparable efficacy and safety compared with standard-dose NOACs; (2) for the patients under the high risk of stroke with approximate CHA2DS2-VASc score of 3.0-5.0, and moderate or high risk of bleeding with approximate HAS-BLED score of 2.0-4.0, low-dose NOACs showed the superior efficacy and safety compared with warfarin.
Warfarin showed some therapeutic limitations in the clinical practice, whose effect was widely affected by food and drugs, and patients need to monitor the INR frequently to supervise the efficacy and risk of major bleeding.43 Major bleeding can seriously affect the anticoagulation treatment, such as higher risks of stroke and mortality,44 longer hospitalization,45 and more healthcare resource utilization.46 At the same time, patients taking warfarin often had less time within the therapeutic range.47 Some meta-analyses had demonstrated that standard-dose NOACs could reduce the risks of stroke, mortality, major bleeding, and ICH compared to warfarin.48-50 In this meta-analysis, low-dose NOACs were non-inferior to standard-dose NOACs and superior to warfarin. Thus, considering their excellence and convenience, low-dose NOACs might be an effective and safe alternative to warfarin in Asian patients with NVAF.
We need to note that the baseline characteristics of cohort studies may be diverse compared to RCTs. For some included studies, the mean age of low-dose NOACs group was approximately 5 years older than standard-dose NOACs or warfarin group, which led to the relatively lower CrCL and higher CHA2DS2-VASc and HAS-BLED scores.5,24,27,30 Moreover, there were some heterogeneities in the previous medical history, including hypertension, diabetes, heart failure, vascular disease, stroke/transient ischemic attack (TIA), and major bleeding. Due to the broad-spectrum baseline characteristics, most cohort studies used the PSM method to adjust the data and minimize the heterogeneity. Adjusted subgroup meta-analyses including RCTs and cohort studies with PSM were performed as well, and the results were consistent with the overall meta-analysis.
What’s more, meta-regression analyses indicated that the mean age, percent of heart failure, female, and hypertension captured a very substantial portion of the heterogeneity in the data, so subgroup meta-analyses stratified by those were performed to balance the confounding factors. Similarly, the results were consistent with the overall. Nonetheless, considering the relatively few studies and ineluctable heterogeneity in this meta-analysis, further well-designed prospective studies are required to validate these results.
Study Limitations
However, there were some potential limitations for our meta-analysis. Firstly, due to the limited number of the included studies and original composite results in most studies, we pooled all NOACs together even though rivaroxaban, apixaban, and edoxaban are the factor Xa inhibitors51 while dabigatran is the thrombin inhibitor,52 which was consistent with other meta-analyses and proved feasible and reliable.4,53,54 This may not cause the significant bias, because they are all direct-acting oral anticoagulants inhibiting important factors in the coagulation cascade. Secondly, as it wasn’t convenient to monitor the quality of warfarin routine usage, most included studies didn’t report the level of time in therapeutic range (TTR). Many patients cannot reach the baseline TTR requirement in the clinical practice,47 which might lead to the unexpected bias in the comparison of low-dose NOACs versus warfarin. And this limitation could be found in other meta-analyses involving warfarin.53,54 However, the effectiveness of the treatment is ensured not only by the efficacy of potent drugs, but also patients’ adherence to the therapy,55 we should have a various and comprehensive view of this limitation. Thirdly, most enrolled studies were performed in Taiwan, Japan, or Korea, which might only represent East Asian patients rather than whole Asian patients.
Conclusions
Low-dose NOACs were superior to warfarin, and comparable to standard-dose NOACs in light of risks of stroke, major bleeding, ICH, and GH. Low-dose NOACs might be prescribed effectively and safely for Asian patients with NVAF. Considering limitations, further high qualified studies are warranted.
Availability of Data and Materials:
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Figure S1.
Pooled stroke of low-dose NOACs versus standard-dose NOACs. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S2.
Pooled mortality of low-dose NOACs versus standard-dose NOACs. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S3.
Pooled major bleeding of low-dose NOACs versus standard-dose NOACs. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S4.
Pooled ICH of low-dose NOACs versus standard-dose NOACs. ICH, intracranial hemorrhage; HR, hazard ratio; RCTs, randomized controlled trials.
Figure S5.
Pooled GH of low-dose NOACs versus standard-dose NOACs. HR, hazard ratio; GH, gastrointestinal hemorrhage; RCTs, randomized controlled trials.
Figure S6.
Pooled stroke of low-dose NOACs versus warfarin. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S7.
Pooled mortality of low-dose NOACs versus warfarin. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S8.
Pooled major bleeding of low-dose NOACs versus warfarin. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S9.
Pooled ICH of low-dose NOACs versus warfarin. HR, hazard ratio; ICH, intracranial hemorrhage; RCTs, randomized controlled trials.
Figure S10.Pooled GH of low-dose NOACs versus warfarin. HR, hazard ratio; GH, gastrointestinal hemorrhage; RCTs, randomized controlled trials.
Figure S11.
Pooled adjusted stroke of low-dose NOACs versus standard-dose NOACs. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S12.
Pooled adjusted mortality of low-dose NOACs versus standard-dose NOACs. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S13.
Pooled adjusted major bleeding of low-dose NOACs versus standard-dose NOACs. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S14.
Pooled adjusted ICH of low-dose NOACs versus standard-dose NOACs. HR, hazard ratio; ICH, intracranial hemorrhage; RCTs, randomized controlled trials.
Figure S15.
Pooled adjusted stroke of low-dose NOACs versus warfarin. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S16.
Pooled adjusted major bleeding of low-dose NOACs versus warfarin. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S17.
Result of meta-regression between mortality and heart failure for low-dose NOACs versus standard-dose NOACs. HR, hazard ratio.
Figure S18.
Result of meta-regression between major bleeding and female for low-dose NOACs versus standard-dose NOA. HR, hazard ratio.
Figure S19.
Result of meta-regression between ICH and mean age for low-dose NOACs versus warfarin. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S20.
Result of meta-regression between ICH and hypertension for low-dose NOACs versus warfarin. HR, hazard ratio; RCTs, randomized controlled trials.
Figure S21.
Pooled mortality of low-dose NOACs versus standard-dose NOACs stratified by heart failure. HR, hazard ratio.
Figure S22.
Pooled major bleeding of low-dose NOACs versus standard-dose NOACs stratified by female. HR, hazard ratio.
Figure S23.
Pooled ICH of low-dose NOACs versus warfarin stratified by hypertension. ICH, intracranial hemorrhage; HR, hazard ratio.
Figure S24.
Pooled mortality of low-dose NOACs versus standard-dose NOACs excluding the three studies. HR, hazard ratio.
Table S1.
Electronic Database Search Strategy
| Cochrane Central Register of Controlled Trials |
| #1 atrial fibrillat* OR atrium fibrillat* OR atrial fibrillation in Title Abstract Keyword |
| #2 warfarin* OR acenocoumarol OR dicoumarol OR coumadin OR diphenadione OR ‘vitamin k antagonist*’ OR vka OR ‘factor xa inhibitor*’ OR antithrombin* OR anticoagul* OR xarelto OR apixaban OR eliquis OR ‘dabigatran etexilate’ OR edoxaban OR savaysa OR rivaroxaban OR dabigatran OR ‘target specific oral anticoagulant*’ OR ‘target-specific oral anticoagulant*’ OR tsoac* OR ‘new oral anticoagulant*’ OR ‘novel oral anticoagulant*’ OR noac* OR ‘direct-acting oral anticoagulant*’ OR ‘direct acting oral anticoagulant*’ OR ‘direct oral anticoagulant*’ OR doac in Title Abstract Keyword |
| #3 ‘low dose’ OR ‘micro dose’ OR ‘off label’ OR underdosing OR underdose OR underdosed OR ‘reduced dose’ in All Text |
| #4 #1 and #2 and #3 |
| Embase |
| 1. ‘atrial fibrillat*’:ab,ti OR ‘atrium fibrillat*’:ab,ti OR ‘atrial fibrillation’:ab,ti 2. warfarin*:ab,ti OR acenocoumarol:ab,ti OR dicoumarol:ab,ti OR coumadin:ab,ti OR diphenadione:ab,ti OR ‘vitamin k antagonist*’:ab,ti OR vka:ab,ti OR ‘factor xa inhibitor*’:ab,ti OR antithrombin*:ab,ti OR anticoagul*:ab,ti OR xarelto:ab,ti OR apixaban:ab,ti OR eliquis:ab,ti OR ‘dabigatran etexilate’:ab,ti OR edoxaban:ab,ti OR savaysa:ab,ti OR rivaroxaban:ab,ti OR dabigatran:ab,ti OR ‘target specific oral anticoagulant*’:ab,ti OR ‘target-specific oral anticoagulant*’:ab,ti OR tsoac*:ab,ti OR ‘new oral anticoagulant*’:ab,ti OR ‘novel oral anticoagulant*’:ab,ti OR noac*:ab,ti OR ‘direct-acting oral anticoagulant*’:ab,ti OR ‘direct acting oral anticoagulant*’:ab,ti OR ‘direct oral anticoagulant*’:ab,ti OR doac:ab,ti 3. ‘low dose’:ab,ti OR ‘micro dose’:ab,ti OR ‘off label’:ab,ti OR underdosing:ab,ti OR underdose:ab,ti OR underdosed:ab,ti OR ‘reduced dose’:ab,ti 4. 1 and 2 and 3 |
| MEDLINE |
| 1. atrial fibrillat*[Title/Abstract] OR atrium fibrillat*[Title/Abstract] OR atrial fibrillation[Title/Abstract] 2. warfarin*[Title/Abstract] OR acenocoumarol[Title/Abstract] OR dicoumarol[Title/Abstract] OR coumadin[Title/Abstract] OR diphenadione[Title/Abstract] OR ‘vitamin k antagonist*’[Title/Abstract] OR vka[Title/Abstract] OR ‘factor xa inhibitor*’[Title/Abstract] OR antithrombin*[Title/Abstract] OR anticoagul*[Title/Abstract] OR xarelto[Title/Abstract] OR apixaban[Title/Abstract] OR eliquis[Title/Abstract] OR ‘dabigatran etexilate’[Title/Abstract] OR edoxaban[Title/Abstract] OR savaysa[Title/Abstract] OR rivaroxaban[Title/Abstract] OR dabigatran[Title/Abstract] OR ‘target specific oral anticoagulant*’[Title/Abstract] OR ‘target-specific oral anticoagulant*’[Title/Abstract] OR tsoac*[Title/Abstract] OR ‘new oral anticoagulant*’[Title/Abstract] OR ‘novel oral anticoagulant*’[Title/Abstract] OR noac*[Title/Abstract] OR ‘direct-acting oral anticoagulant*’[Title/Abstract] OR ‘direct acting oral anticoagulant*’[Title/Abstract] OR ‘direct oral anticoagulant*’[Title/Abstract] OR doac[Title/Abstract] 3. low dose’ OR ‘micro dose’ OR ‘off label’ OR underdosing OR underdose OR underdosed OR ‘reduced dose’ 4. 1 and 2 and 3 |
Table S2.
Detailed Previous Medical History of Included Patients
| Author (Study), Year | Group | Previous Medical History (%) | |||||
|---|---|---|---|---|---|---|---|
| Hypertension | Diabetes | Heart Failure | Vascular Disease | Stroke/TIA | Major Bleeding | ||
| Murata N, 2019 | Standard-dose | 68.1 | 22.3 | 16.4 | 9.9 | 9.5 | 0.5 |
| Low-dose | 71.3 | 22.2 | 17.9 | 14.4 | 7.6 | 1.4 | |
| Wakamatsu Y, 2020 | Standard-dose | 61.3 | 20.4 | 15.2 | 9.8 | 11.9 | 1.5 |
| Low-dose | 62.5 | 17.6 | 17.1 | 13.9 | 12.5 | 2.3 | |
| Ohno, J 2021 | Standard-dose | 71.0 | 28.8 | 18.3 | 6.2 | 14.9 | NR |
| Low-dose | 71.6 | 27.2 | 17.8 | 10.2 | 22.5 | ||
| Lee HF, 2018 | Low-dose | 86.0 | 39.0 | 14.0 | NR | 22.0 | 2.5 |
| Warfarin | 86.0 | 39.0 | 14.0 | 21.0 | 2.0 | ||
| Yu HT, 2018 | Standard-dose | 94.5 | 30.5 | 63.2 | 28.1 | 37.1 | NR |
| Low-dose | 94.0 | 34.6 | 66.9 | 32.8 | 40.6 | ||
| Warfarin | 94.6 | 34.3 | 67.5 | 32.6 | 40.4 | ||
| Chan YH, 2018 | Standard-dosea | 87.0 | 41.0 | 13.0 | NR | 23.0 | 2.0 |
| Low-dosea | |||||||
| Warfarin | 87.0 | 40.0 | 13.0 | 23.0 | 2.0 | ||
| Chang HK, 2016 | Standard-dosea | 72.3 | 25.7 | 18.2 | NR | 45.9 | NR |
| Low-dosea | |||||||
| Warfarin | 75.2 | 49.5 | 20.0 | 37.9 | |||
| Akagi Y, 2019 | Standard-dosea | 60.1 | 19.7 | 19.0 | NR | 26.2 | NR |
| Low-dosea | |||||||
| Yu HT, 2020 | Standard-dose | 94.5 | 31.4 | 60.4 | 27.9 | 46.6 | NR |
| Low-dose | 95.3 | 32.3 | 60.4 | 29.7 | 41.6 | ||
| Cho MS, 2019 | Low-dose | 87.8 | 45.5 | 20.5 | 11.5 | 21.1 | NR |
| Warfarin | 86.7 | 48.4 | 22.8 | 12.8 | 27.3 | ||
| Jeong HK, 2019 | Low-dose | 53.5 | 24.1 | 5.7 | NR | 29.2 | NR |
| Warfarin | 54.7 | 22.3 | 5.1 | 29.2 | |||
| Kohsaka S, 2020 | Low-dose | 54.9 | 30.0 | 37.1 | NR | 21.2 | NR |
| Warfarin | 55.9 | 30.4 | 37.5 | 21.4 | |||
| Kohsaka S, 2017 | Low-dose | 53.8 | 28.9 | 35.3 | 6.6 | 22.3 | NR |
| Warfarin | 54.0 | 28.2 | 35.4 | 6.2 | 22.6 | ||
| Lai CL, 2018 | Low-dose | 51.1 | 16.9 | 25.3 | 4.2 | 16.3 | NR |
| Warfarin | 50.3 | 15.4 | 29.6 | 4.1 | 11.6 | ||
| Lee SR, 2019 | Standard-dose | 72.0 | 21.5 | 30.2 | NR | NR | NR |
| Low-dose | 73.1 | 21.1 | 31.2 | ||||
| Warfarin | 72.3 | 22.3 | 32.4 | ||||
| Chan YH, 2019 | Low-dose | 84.1 | 38.1 | 11.1 | NR | 15.2 | NR |
| Warfarin | 84.5 | 38.6 | 10.8 | 15.0 | |||
| RE-LY, 2013 | Standard-dosea | 71.2 | 25.1 | 36.3 | NR | 24.2 | NR |
| Low-dosea | |||||||
| Warfarina | |||||||
| J-ROCKET AF, 2012 | Low-dose | 79.5 | 39.0 | 41.3 | NR | 63.8 | NR |
| Warfarin | 79.5 | 37.1 | 40.2 | 63.4 | |||
| ENGAGE AF-TIMI 48, 2016 | Standard-dosea | 82.1 | 35.0 | 47.3 | NR | 42.4 | NR |
| Low-doses | |||||||
| Warfarina | |||||||
NR, not reported; TIA, transient ischemic attack.
a Means characteristics are the composite of low-dose and standard-dose groups.
Table S3.
Detailed Group Contents of Included Studies
| Author (Study), Year | Standard-Dose | Low-Dose |
|---|---|---|
| Murata N, 2019 | Dabigatran Rivaroxaban Apixaban Edoxaban |
Dabigatran 110 mg (b.i.d.) Rivaroxaban 10 mg (q.d.) Apixaban 2.5 mg (b.i.d.) Edoxaban 30 mg (q.d.) |
| Wakamatsu Y, 2020 | Dabigatran Rivaroxaban Apixaban Edoxaban |
Dabigatran 110 mg (b.i.d.) Rivaroxaban 10 mg (q.d.) Apixaban 2.5 mg (b.i.d.) Edoxaban 30 mg (q.d.) |
| Ohno J, 2021 | Dabigatran Rivaroxaban Apixaban Edoxaban |
Dabigatran 110 mg (b.i.d.) Rivaroxaban 10 mg (q.d.) Apixaban 2.5 mg (b.i.d.) Edoxaban 30 mg (q.d.) |
| Akagi Y, 2019 | Dabigatran | Dabigatran 110 mg (b.i.d.) |
| Yu HT 2020 | Dabigatran Rivaroxaban Apixaban Edoxaban |
Dabigatran 110 mg (b.i.d.) Rivaroxaban 10/15 mg (q.d.) Apixaban 2.5 mg (b.i.d.) Edoxaban 30 mg (q.d.) |
| Chan YH, 2018 | Dabigatran Rivaroxaban Apixaban |
Dabigatran 110 mg (b.i.d.) Rivaroxaban 10/15 mg (q.d.) Apixaban 2.5 mg (b.i.d.) |
| Chang HK, 2016 | Dabigatran Rivaroxaban Warfarin |
Dabigatran 110 mg (b.i.d.) Rivaroxaban 15 mg (q.d.) |
| Lee SR, 2019 | Rivaroxaban Warfarin |
Rivaroxaban 15 mg (q.d.) |
| Yu HT, 2018 | Warfarin | Edoxaban 30 mg (q.d.) |
| Lee HF, 2018 | Warfarin | Rivaroxaban 10/15 mg (q.d.) |
| Cho MS, 2019 | Warfarin | Dabigatran 110 mg (b.i.d.) Rivaroxaban 10/15 mg (q.d.) Apixaban 2.5 mg (b.i.d.) |
| Jeong HK, 2019 | Warfarin | Rivaroxaban 15 mg (q.d.) |
| Kohsaka S, 2017 | Warfarin | Rivaroxaban 10/15 mg (q.d.) |
| Kohsaka S, 2020 | Warfarin | Rivaroxaban 10/15 mg (q.d.) |
| Lai CL, 2018 | Warfarin | Dabigatran 110 mg (b.i.d.) |
| Chan YH, 2019 | Warfarin | Dabigatran 110 mg (b.i.d.) Rivaroxaban 10/15 mg (q.d.) Apixaban 2.5 mg (b.i.d.) Edoxaban 15/30 mg (q.d.) |
| RE-LY, 2013 | Dabigatran Warfarin |
Dabigatran 110 mg (b.i.d.) |
| ENGAGE AF-TIMI 48, 2016 | Edoxaban Warfarin |
Edoxaban 30 mg (q.d.) |
| J-ROCKET AF, 2012 | Warfarin | Rivaroxaban 10/15 mg (q.d.) |
Table S4.
Results of Quality Assessment Using the Newcastle-Ottawa Scale for Cohort Studies
| Author, Year | Selection | Comparability | Outcome | |||||
|---|---|---|---|---|---|---|---|---|
| Representativeness of the Exposed Cohort | Selection of the Non-exposed Cohort | Ascertainment of Exposure | Demonstration That Outcome of Interest Was Not Present at Start of Study | Comparability of Cohorts on the Basis of the Design or Analysis | Assessment of Outcome | Was Follow-Up Long Enough for Outcomes to Occur | Adequacy of Follow-Up of Cohorts | |
| Murata N, 2019 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ |
| Wakamatsu Y, 2020 | ★ | ★ | ★ | ★ | ☆☆ | ★ | ★ | ☆ |
| Ohno J, 2021 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ☆ |
| Lee HF, 2018 | ★ | ★ | ★ | ★ | ★★ | ★ | ☆ | ☆ |
| Chang HK, 2016 | ★ | ★ | ★ | ★ | ☆☆ | ★ | ★ | ☆ |
| Akagi Y, 2019 | ★ | ★ | ★ | ★ | ☆☆ | ★ | ☆ | ☆ |
| Yu HT, 2020 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ☆ |
| Yu HT, 2018 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ☆ |
| Cho MS, 2019 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ☆ |
| Jeong HK, 2019 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ☆ |
| Kohsaka S, 2020 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ☆ |
| Kohsaka S, 2017 | ★ | ★ | ★ | ★ | ★★ | ★ | ☆ | ☆ |
| Lai CL, 2018 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ☆ |
| Lee SR, 2019 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ☆ |
| Chan YH, 2018 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ☆ |
| Chan YH, 2019 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ☆ |
Table S5.
Results of Quality Assessment Using the Cochrane Collaboration's Tool for RCTs
| Study, Year | Random Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Other Sources of Bias |
|---|---|---|---|---|---|---|---|
| RE-LY, 2013 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| J-ROCKET AF, 2012 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| ENGAGE AF-TIMI 48, 2016 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
Table S6.
Results of Publication Bias Assessment Using the Begg's and Egger's Tests
| Comparison | Outcomes | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Stroke | Mortality | Major Bleeding | ICH | GH | |||||||
| Begg’s Test | Egger’s Test | Begg’s Test | Egger’s Test | Begg’s Test | Egger’s Test | Begg’s Test | Egger’s Test | Begg’s Test | Egger’s Test | ||
| Low-dose NOACs versus standard-dose NOACs | 0.721 | 0.467 | 0.764 | 0.496 | 0.917 | 0.918 | 0.548 | 0.102 | 0.707 | 0.364 | |
| Low-dose NOACs versus warfarin | 0.858 | 0.497 | 1.000 | 0.707 | 0.210 | 0.162 | 0.368 | 0.005 | 0.368 | 0.156 | |
GH, gastrointestinal hemorrhage; ICH, intracranial hemorrhage.
Table S7.
Results of Meta-regression Analyses for Interesting Outcomes
| Low-Dose NOACs versus Standard-Dose NOACs | |||||
|---|---|---|---|---|---|
| Variables | Stroke (P) | Mortality (P) | Major bleeding (P) | ICH (P) | GH (P) |
| Mean age | .826 | .119 | .106 | .211 | .257 |
| Female | .948 | .760 | .020 | .373 | .160 |
| BMI | .476 | .272 | .240 | .908 | NA |
| HBP | .932 | .934 | .991 | .126 | .110 |
| DM | .513 | .292 | .929 | .122 | .793 |
| HF | .743 | .023 | .394 | .983 | .069 |
| Vascular disease | .436 | .218 | .574 | .517 | NA |
| Stroke/TIA | .554 | .100 | .749 | .726 | .172 |
| Prior major bleeding | .486 | .968 | .282 | .483 | NA |
| CHA2DS2-VASc | .770 | .861 | .701 | .345 | .245 |
| HAS-BLED | .340 | .542 | .630 | .415 | NA |
| CrCl | .309 | .922 | .786 | .448 | NA |
| Low-Dose NOACs versus Warfarin | |||||
| Variables | Stroke (P) | Mortality (P) | Major bleeding (P) | ICH (P) | GH (P) |
| Mean age | .717 | .155 | .947 | .032 | .972 |
| Female | .483 | .375 | .606 | .341 | .851 |
| BMI | .342 | NA | .341 | NA | NA |
| HBP | .892 | .747 | .997 | .038 | .154 |
| DM | .365 | .667 | .787 | .972 | .089 |
| HF | .256 | .927 | .988 | .962 | .988 |
| Vascular disease | NA | .654 | .575 | NA | NA |
| Stroke/TIA | .377 | .723 | .936 | .461 | .792 |
| Prior major bleeding | NA | NA | NA | NA | NA |
| CHA2DS2-VASc | .132 | .145 | .631 | .805 | .561 |
| HAS-BLED | .928 | NA | .630 | NA | NA |
| CrCl | .930 | NA | .341 | NA | NA |
BMI, body mass index; CrCl, creatinine clearance rate; DM, diabetes mellitus; GH, gastrointestinal hemorrhage; HBP, hypertension; HF, heart failure; ICH, intracranial hemorrhage; NA, not available; TIA, transient ischemic attack.
Footnotes
Ethics Committee Approval: This is a meta-analysis and needs no ethical committee approval.
Peer-review: Externally peer-reviewed.
Author Contributions: Ze Li was responsible for the study design, literature search, data collection, data analysis, data interpretation, drafting and critical revision of the manuscript, and approval of the final submission. Yingming Zheng, Dandan Li, Xiaozhen Wang, Sheng Cheng, and Xiao Luo were responsible for the literature search and data collection. Aiping Wen was responsible for the study concept and design, data interpretation, critical revision of the manuscript, approval of the final submission, integrity of the data, and accuracy of the data analysis.
Declaration of Interests: The authors declare that they have no competing interest.
Funding: This work was supported by the Digestive Medical Coordinated Development Center of Beijing Municipal Administration of Hospitals No. XXZ06.
References
- 1. Williams BA, Chamberlain AM, Blankenship JC, Hylek EM, Voyce S. Trends in atrial fibrillation incidence rates Within an integrated health care delivery system, 2006-2018. JAMA Network Open. 2020;3(8):e2014874. 10.1001/jamanetworkopen.2020.14874) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wadhera RK, Russell CE, Piazza G. Cardiology patient page. Warfarin versus novel oral anticoagulants: how to choose? Circulation. 2014;130(22):e191 e193. 10.1161/CIRCULATIONAHA.114.010426) [DOI] [PubMed] [Google Scholar]
- 3. Bray E, Georgiou R, Wilson N.et al. Self-monitoring of INR for warfarin management of patients with atrial fibrillation (AF): patient and clinicians experiences. Int J Stroke. 2019;14:40. [Google Scholar]
- 4. Wang KL, Giugliano RP, Goto S.et al. Standard dose versus low dose non-vitamin K antagonist oral anticoagulants in Asian patients with atrial fibrillation: a meta-analysis of contemporary randomized controlled trials. Heart Rhythm. 2016;13(12):2340 2347. 10.1016/j.hrthm.2016.09.010) [DOI] [PubMed] [Google Scholar]
- 5. Murata N, Okumura Y, Yokoyama K.et al. Clinical outcomes of off-label dosing of direct oral anticoagulant therapy among Japanese patients with atrial fibrillation identified from the SAKURA AF registry. Circ J. 2019;83(4):727 735. 10.1253/circj.CJ-18-0991) [DOI] [PubMed] [Google Scholar]
- 6. Cheng WH, Chao TF, Lin YJ.et al. Low-dose Rivaroxaban and risks of adverse events in patients with atrial fibrillation. Stroke. 2019;50(9):2574 2577. 10.1161/STROKEAHA.119.025623) [DOI] [PubMed] [Google Scholar]
- 7. Yu HT, Yang PS, Jang E.et al. Label adherence of direct oral anticoagulants dosing and clinical outcomes in patients With atrial fibrillation. J Am Heart Assoc. 2020;9(12):e014177. 10.1161/JAHA.119.014177) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Price D, Brusselle G, Roche N, Freeman D, Chisholm A. Real-World Research and its importance in respiratory medicine. Breathe (Sheff). 2015;11(1):26 38. 10.1183/20734735.015414) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McInnes MDF, Moher D, Thombs BD.et al. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA. 2018;319(4):388 396. 10.1001/jama.2017.19163) [DOI] [PubMed] [Google Scholar]
- 10. Stroup DF, Berlin JA, Morton SC.et al. Meta-analysis of observational studies in epidemiology - A proposal for reporting. JAMA. 2000;283(15):2008 2012. 10.1001/jama.283.15.2008) [DOI] [PubMed] [Google Scholar]
- 11. Steffel J, Verhamme P, Potpara TS.et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation: executive summary. Europace. 2018;20(8):1231 1242. 10.1093/europace/euy054) [DOI] [PubMed] [Google Scholar]
- 12. Connolly SJ, Ezekowitz MD, Yusuf S.et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139 1151. 10.1056/NEJMoa0905561) [DOI] [PubMed] [Google Scholar]
- 13. Govindarajan R, Salgado E. Risk of bleeding with 2 doses of dabigatran compared with warfarin in older and younger patients with atrial fibrillation: an analysis of the randomized evaluation of long-term anticoagulant therapy (RE-LY) trial. Circulation. 2012;125:293 294. [DOI] [PubMed] [Google Scholar]
- 14. Patel MR, Mahaffey KW, Garg J.et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883 891. 10.1056/NEJMoa1009638) [DOI] [PubMed] [Google Scholar]
- 15. Hori M, Matsumoto M, Tanahashi N.et al. Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation – the J-ROCKET AF study –. Circ J. 2012;76(9):2104 2111. 10.1253/circj.cj-12-0454) [DOI] [PubMed] [Google Scholar]
- 16. Szczerba E. Apixaban versus warfarin in patients with atrial fibrillation: examination of ARISTOTLE. Kardiol Pol. 2012;70(2):196 198. [PubMed] [Google Scholar]
- 17. Ogawa S, Shinohara Y, Kanmuri K. Safety and efficacy of the oral direct factor xa inhibitor apixaban in Japanese patients with non-valvular atrial fibrillation. -The Aristotle-J study-. Circ J. 2011;75(8):1852 1859. 10.1253/circj.cj-10-1183) [DOI] [PubMed] [Google Scholar]
- 18. Cunningham J, Giugliano R, Braunwald E.et al. Edoxaban VERSUS warfarin in 841 patients with atrial fibrillation and peripheral arterial disease: insights from the engage AF-TIMI 48 trial. J Am Coll Cardiol. 2016;67(13):2262. 10.1016/S0735-1097(16)32263-X) [DOI] [Google Scholar]
- 19. Higgins JPT, Altman DG, Gøtzsche PC.et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. 10.1136/bmj.d5928) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603 605. 10.1007/s10654-010-9491-z) [DOI] [PubMed] [Google Scholar]
- 21. Begg CB, Mazumdar M. Operating characteristics of a bank correlation test for publication bias. Biometrics. 1994;50(4):1088 1101. 10.2307/2533446) [DOI] [PubMed] [Google Scholar]
- 22. Egger M, Davey Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629 634. 10.1136/bmj.315.7109.629) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wakamatsu Y, Nagashima K, Watanabe R.et al. Clinical outcomes of off-label underdosing of direct oral anticoagulants after ablation for atrial fibrillation. Int Heart J. 2020;61(6):1165 1173. 10.1536/ihj.20-335) [DOI] [PubMed] [Google Scholar]
- 24. Ohno J, Sotomi Y, Hirata A, Sakata Y, Hirayama A, Higuchi Y. Dose of direct oral anticoagulants and adverse outcomes in Asia. Am J Cardiol. 2021;139:50 56. 10.1016/j.amjcard.2020.09.053) [DOI] [PubMed] [Google Scholar]
- 25. Lee HF, Chan YH, Tu HT.et al. The effectiveness and safety of low-dose Rivaroxaban in Asians with non-valvular atrial fibrillation. Int J Cardiol. 2018;261:78 83. 10.1016/j.ijcard.2018.03.063) [DOI] [PubMed] [Google Scholar]
- 26. Yu HT, Yang PS, Kim TH.et al. Impact of renal function on outcomes with edoxaban in real-world patients with atrial fibrillation. Stroke. 2018;49(10):2421 2429. 10.1161/STROKEAHA.118.021387) [DOI] [PubMed] [Google Scholar]
- 27. Chan YH, See LC, Tu HT.et al. Efficacy and safety of apixaban, dabigatran, Rivaroxaban, and warfarin in Asians With nonvalvular atrial fibrillation. J Am Heart Assoc. 2018;7(8):e008150. 10.1161/JAHA.117.008150) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kwon CH, Kim M, Kim J, Nam GB, Choi KJ, Kim YH. Real-world comparison of non-vitamin K antagonist oral anticoagulants and warfarin in Asian octogenarian patients with atrial fibrillation. J Geriatr Cardiol. 2016;13(7):566 572. 10.11909/j.issn.1671-5411.2016.07.011) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Akagi Y, Chiba T, Uekusa S.et al. Retrospective cohort study of the efficacy and safety of dabigatran: real-life dabigatran use including very low-dose 75 mg twice daily administration. J Pharm Health Care Sci. 2019;5:17. 10.1186/s40780-019-0145-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cho MS, Yun JE, Park JJ.et al. Outcomes after use of standard- and low-dose non-vitamin K Oral anticoagulants in Asian patients with atrial fibrillation. Stroke. 2019;50:110 118. [DOI] [PubMed] [Google Scholar]
- 31. Jeong HK, Lee KH, Park HW.et al. Real world comparison of Rivaroxaban and warfarin in Korean patients with atrial fibrillation: propensity matching cohort analysis. Chonnam Med J. 2019;55(1):54 61. 10.4068/cmj.2019.55.1.54) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kohsaka S, Katada J, Saito K.et al. Safety and effectiveness of non-vitamin K oral anticoagulants versus warfarin in real-world patients with non-valvular atrial fibrillation: a retrospective analysis of contemporary Japanese administrative claims data. Open Heart. 2020;7(1):e001232. 10.1136/openhrt-2019-001232) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kohsaka S, Murata T, Izumi N, Katada J, Wang F, Terayama Y. Bleeding risk of apixaban, dabigatran, and low-dose rivaroxaban compared with warfarin in Japanese patients with non-valvular atrial fibrillation: a propensity matched analysis of administrative claims data. Curr Med Res Opin. 2017;33(11):1955 1963. 10.1080/03007995.2017.1374935) [DOI] [PubMed] [Google Scholar]
- 34. Lai CL, Chen HM, Liao MT, Lin TT. Dabigatran, Rivaroxaban, and warfarin in the oldest adults with atrial fibrillation in Taiwan. J Am Geriatr Soc. 2018;66(8):1567 1574. 10.1111/jgs.15430) [DOI] [PubMed] [Google Scholar]
- 35. Lee SR, Choi EK, Han KD, Jung JH, Oh S, Lip GYH. Optimal rivaroxaban dose in Asian patients With atrial fibrillation and normal or mildly impaired renal function. Stroke. 2019;50(5):1140 1148. 10.1161/STROKEAHA.118.024210) [DOI] [PubMed] [Google Scholar]
- 36. Chan YH, Lee HF, See LC.et al. Effectiveness and safety of four direct oral anticoagulants in Asian patients With nonvalvular atrial fibrillation. Chest. 2019;156(3):529 543. 10.1016/j.chest.2019.04.108) [DOI] [PubMed] [Google Scholar]
- 37. Hori M, Connolly SJ, Zhu J.et al. Dabigatran versus warfarin: effects on ischemic and hemorrhagic strokes and bleeding in Asians and non-Asians with atrial fibrillation. Stroke. 2013;44(7):1891 1896. 10.1161/STROKEAHA.113.000990) [DOI] [PubMed] [Google Scholar]
- 38. Hori M, Matsumoto M, Tanahashi N.et al. Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation – the J-ROCKET AF study –. Circ J. 2012;76(9):2104 2111. 10.1253/circj.cj-12-0454) [DOI] [PubMed] [Google Scholar]
- 39. Yamashita T, Koretsune Y, Yang Y.et al. Edoxaban vs. warfarin in East Asian Patients with atrial fibrillation- An engage AF-timi 48 subanalysis. Circ J. 2016;80(4):860 869. 10.1253/circj.CJ-15-1082) [DOI] [PubMed] [Google Scholar]
- 40. Wu S, Yang YM, Zhu J.et al. Impact of age on the association between body mass index and all-cause mortality in patients with atrial fibrillation. J Nutr Health Aging. 2017;21(10):1125 1132. 10.1007/s12603-016-0863-2) [DOI] [PubMed] [Google Scholar]
- 41. Giralt-Steinhauer E, Cuadrado-Godia E, Ois A.et al. Comparison between CHADS2 and CHA2DS2-VASc score in a stroke cohort with atrial fibrillation. Eur J Neurol. 2013;20(4):623 628. 10.1111/j.1468-1331.2012.03807.x) [DOI] [PubMed] [Google Scholar]
- 42. Omran H, Bauersachs R, Rübenacker S, Goss F, Hammerstingl C. The HAS-BLED score predicts bleedings during bridging of chronic oral anticoagulation. Results from the national multicentre BNK Online bRiDging REgistRy (BORDER). Thromb Haemost. 2012;108(1):65 73. 10.1160/TH11-12-0827) [DOI] [PubMed] [Google Scholar]
- 43. De Santis G, Hogan-Schlientz J, Liska G.et al. Stable results: warfarin home monitoring achieves excellent INR control. Am J Manag Care. 2014;20:202 209. [PubMed] [Google Scholar]
- 44. Deitelzweig S, Keshishian A, Kang A.et al. Burden of major gastrointestinal bleeding among oral anticoagulant-treated non-valvular atrial fibrillation patients. Therap Adv Gastroenterol. 2021;14:1 13. 10.1177/1756284821997352) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Abraham NS, Castillo DL. Novel anticoagulants: bleeding risk and management strategies. Curr Opin Gastroenterol. 2013;29(6):676 683. 10.1097/MOG.0b013e328365d415) [DOI] [PubMed] [Google Scholar]
- 46. Sam C, Massaro JM, D'Agostino RB.et al. Warfarin and aspirin use and the predictors of major bleeding complications in atrial fibrillation (The Framingham Heart Study). Am J Cardiol. 2004;94(7):947 951. 10.1016/j.amjcard.2004.06.038) [DOI] [PubMed] [Google Scholar]
- 47. Morgan CL, Mcewan P, Tukiendorf A, Robinson PA, Clemens A, Plumb JM. Warfarin treatment in patients with atrial fibrillation: observing outcomes associated with varying levels of INR control. Thromb Res. 2009;124(1):37 41. 10.1016/j.thromres.2008.09.016) [DOI] [PubMed] [Google Scholar]
- 48. Wang KL, Lip GYH, Lin SJ, Chiang CE. Non-vitamin K antagonist oral anticoagulants for stroke prevention in Asian patients with nonvalvular atrial fibrillation: meta-analysis. Stroke. 2015;46(9):2555 2561. 10.1161/STROKEAHA.115.009947) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Jia B, Lynn HS, Rong F, Zhang W. Meta-analysis of efficacy and safety of the new anticoagulants versus warfarin in patients with atrial fibrillation. J Cardiovasc Pharmacol. 2014;64(4):368 374. 10.1097/FJC.0000000000000129) [DOI] [PubMed] [Google Scholar]
- 50. Ruff CT, Giugliano RP, Braunwald E.et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955 962. 10.1016/S0140-6736(13)62343-0) [DOI] [PubMed] [Google Scholar]
- 51. Mismetti P, Laporte S. Rivaroxaban: clinical pharmacology. Ann Fr Anesth Reanim. 2008;27(suppl 3):S16 S21. 10.1016/S0750-7658(08)75142-6). [DOI] [PubMed] [Google Scholar]
- 52. Sarah S. The pharmacology and therapeutic use of dabigatran etexilate. J Clin Pharmacol. 2013;53(1):1 13. 10.1177/0091270011432169) [DOI] [PubMed] [Google Scholar]
- 53. Dentali F, Riva N, Crowther M, Turpie AG, Lip GY, Ageno W. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: a systematic review and meta-analysis of the literature. Circulation. 2012;126(20):2381 2391. 10.1161/CIRCULATIONAHA.112.115410) [DOI] [PubMed] [Google Scholar]
- 54. Rong F, Jia B, Huang PX, Lynn HS, Zhang W. Safety of the direct-acting anticoagulants in patients with atrial fibrillation: a meta-analysis. Thromb Res. 2015;135(6):1117 1123. 10.1016/j.thromres.2015.04.004) [DOI] [PubMed] [Google Scholar]
- 55. Dagli-Hernandez C, Lucchetta RC, De Nadai TR, Galduróz JCF, Mastroianni PC. Self-perception of knowledge and adherence reflecting the effectiveness of antiretroviral therapy. Patient Preference Adherence. 2016;10:1787 1793. 10.2147/PPA.S112108) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.



 Content of this journal is licensed under a
Content of this journal is licensed under a