Abstract
Background
Aberrant fibroblast growth factor receptor (FGFR) signaling can substantially influence oncogenicity. Despite that FGFR gene abnormality is often detected by cancer genome profiling tests, there is no tumor-agnostic approval yet for these aberrations. E7090 (tasurgratinib) is an orally available selective tyrosine kinase inhibitor of FGFR1-3. Specific FGFR alterations were previously reported to be highly sensitive to E7090 based on a high-throughput functional evaluation method, called mixed-all-nominated-mutants-in-one (MANO) method, narrowing down the most promising targets. This trial was focused on the alterations identified by the MANO method and was performed under the nationwide large registry network for rare cancers in Japan (MASTER KEY Project).
Methods/Design
This single-arm Phase 2 trial was designed to evaluate the safety and efficacy of E7090 in patients with advanced or recurrent solid tumors harboring FGFR alterations. Three cohorts were set based on the type of FGFR alterations and the results of MANO method. A maximum of 45 patients will be enrolled from 5 institutions over 2.5 years. E7090 will be administered once daily as an oral single agent in 28-day cycles. The primary endpoint is the objective overall response rate; whereas, the secondary endpoints include progression-free survival, overall survival, disease control rate, safety, duration of response, and time to response. Ethics approval was granted by the National Cancer Center Hospital Certified Review Board. Patient enrollment began in June 2021.
Discussion
A unique investigator-initiated multicenter Phase 2 trial was designed based on the results of preclinical investigation aiming to acquire the approval of E7090 for solid tumors harboring FGFR gene alterations. The findings may serve as a novel model for the development of tumor-agnostic molecular targeted therapies against rare genetic abnormalities.
Trial registration
Japan Registry of Clinical Trial: jRCT2031210043 (registered April 20, 2021) ClinicalTrials.gov: NCT04962867 (registered July 15, 2021).
Keywords: Fibroblast growth factor receptor, Gene fusion, Mutation, Amplification, Precision medicine
Background
Research on targeted gene therapy, also known as “precision medicine,” is being conducted extensively worldwide. Particularly, cancer genome medicine is being promoted. Although cancer genome profiling tests using next-generation sequencing (NGS) show that approximately 40 to 60% of patients have genetic abnormalities that could serve as therapeutic targets, the percentage of patients who practically receive biomarker-driven and molecular targeted therapy remains low at about 10% [1, 2]. To promote the development of new treatments, we initiated an industry-academia collaborative project called the Marker Assisted Selective Therapy in Rare Cancers: Knowledge Database Establishing Registry Project (‘MASTER KEY Project’) in Japan. This is a master protocol study that consists of 2 parts: a prospective registry component that collects biomarker and clinical data from patients with rare cancers, and a clinical trial component that conducts biomarker-directed or non-biomarker-directed clinical trials [3]. In the literature, personalized treatment using a genomic biomarker has shown a higher response rate (RR) and prolonged median progression-free survival (PFS) [4, 5].
The fibroblast growth factor (FGF)/FGF receptor (FGFR) signaling pathway plays multiple roles in the regulation of cellular functions, affecting cell differentiation, migration, proliferation, and survival [6]. The FGF proteins are a large family of multifunctional peptide growth factors that bind to and activate a family of 4 FGFRs [7]. FGFRs with genetic abnormalities, such as gene fusion, somatic mutation, or amplification, are present in 4.1 to 5.1% of human cancers [2, 8]. Most molecular alterations promote multiple steps of carcinogenesis in FGFR oncogene-addicted cells; thereby, increasing cell proliferation, angiogenesis, and drug resistance [9]. The in vivo and in vitro oncogenic potential studies of these aberrations suggest a potent sensitivity to FGFR inhibitors [10, 11]. Several FGFR inhibitors are currently approved by the U.S. Food and Drug Administration for the treatment of urothelial or cholangiocarcinoma, including erdafitinib, [12] pemigatinib, [13] and infigratinib [14]. However, in Japan, pemigatinib is the only drug approved for the treatment of unresectable cholangiocarcinoma patients with FGFR2 gene fusion.
E7090 (tasurgratinib) is a novel orally administered tyrosine kinase inhibitor that selectively inhibits FGFR1, 2 and 3; this drug was discovered and developed by Eisai's Tsukuba Research Laboratories [15]. A first-in-human Phase 1 study of E7090 in patients with advanced solid tumors has been conducted in Japan (ClinicalTrials.gov: NCT02275910); wherein, one dose-limiting toxicity of Grade 3 aspartate aminotransferase (AST)/alanine aminotransferase (ALT) increase was observed in the 180-mg once-daily dosing group; therefore, the recommended dose was determined to be 140-mg once daily. Of the 24 patients treated in the dose-escalation part, one achieved a partial response and 7 patients achieved stable disease [16]. Preliminary results in the expansion part of this Phase 1 study showed the activity of E7090 with an overall response rate (ORR) of 83.3% (5/6) and 11.1% (1/9) in patients with cholangiocarcinoma harboring an FGFR2 gene fusion and in those with gastric cancer harboring either FGFR2 gene amplification or FGFR2 protein high expression, respectively. The observed median PFS was 8.26 months in patients with cholangiocarcinoma and 2.58 months in those with gastric cancer [17]. A global Phase 2 study targeting FGFR2 gene fusion in unresectable advanced or metastatic cholangiocarcinoma is ongoing (ClinicalTrials.gov: NCT 04,238,715).
While E7090 exhibited the promising responses in patients with cholangiocarcinoma, the transforming activity and sensitivity of 160 nonsynonymous FGFR mutations and 10 fusion genes to eight FGFR tyrosine kinase inhibitors (TKIs) using a high-throughput functional assay using the mixed-all-nominated-mutants-in-one (MANO) method was evaluated [11, 18, 19]. The FGFR TKIs showed anti-proliferative activities against proteins encoded by wild-type FGFRs and their gene fusions; several hotspot mutants were relatively resistant to these TKIs. Importantly, the efficacy of FGFR inhibitors for each variant was different among inhibitors, and several hotspot mutations were specifically sensitive to E7090 [11]. Therefore, inhibition of FGFR signaling by E7090 can be an attractive therapeutic option for several tumor types.
The essence of cancer precision medicine is to provide individualized treatment proposals based on genomic diagnosis. And it is obviously essential to have a drug delivery system as an exit strategy. In Japan, due to the limited number of patients, some situations existed where investigational drugs for a rare population were approved by merely a single-arm Phase 2 study that mainly evaluates response rates [20]. This study described here is a novel attempt to evaluate a new drug with a tumor agnostic approach by incorporating the MANO method on rare gene alterations detected by NGS. The authors intend to discuss the results of this study with the Agency for consideration of an approval.
Methods/design
Aim
To evaluate the efficacy and safety of E7090 in advanced or recurrent solid tumors with FGFR gene alterations (including fusion, mutation, and amplification).
Study setting
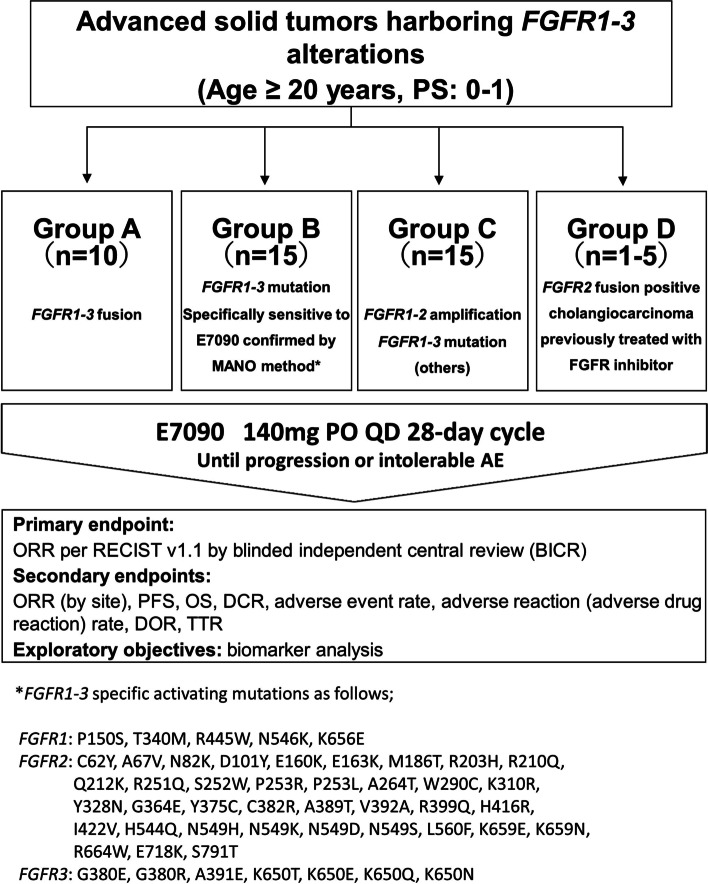
This study was a single-group, open-label, investigator-initiated, multicenter Phase 2 basket study (Fig. 1).
Fig. 1.
Flow diagram of the FORTUNE protocol. A total of 41 to 45 patients will be enrolled; it is expected that the number of patients in Group A, B, C, and D will be approximately 10, 15, 15, and 5, respectively. Group A includes patients with advanced solid tumors harboring FGFR1-3 fusion. Group B includes patients with advanced solid tumors harboring FGFR1-3 mutation suggesting that the efficacy of E7090 is promising by MANO method. Group C includes patients with advanced solid tumors harboring FGFR1-3 mutation other than what is included Group B and/or FGFR1, 2 amplification. Group D includes patients with cholangiocarcinoma harboring FGFR2 gene fusion who received prior selective FGFR inhibitors other than E7090. E7090 is administered once daily as an oral single agent in 28-day cycles
Endpoints
The primary endpoint was ORR, defined as the combined incidence of complete response (CR) and PR, confirmed no less than 4 weeks after the criteria for response were first met, based on response evaluation criteria in solid tumors (RECIST) v1.1. ORR was confirmed by blinded independent central review (BICR).
The secondary endpoints were ORR (confirmed by a local site investigator), PFS, overall survival (OS), disease control rate (DCR), safety, duration of response (DOR), and time to response (TTR). Safety endpoints included the adverse event (AE) rate and adverse reaction (adverse drug reaction) rate. The severity of AEs was evaluated by the investigator according to the Japan Clinical Oncology Group (JCOG) Japanese translation of the Common Terminology Criteria for Adverse Events version 5.0 (CTCAE v5.0-JCOG).
Eligibility criteria
Participant with histologically or cytologically confirmed metastatic, unresectable, or recurrent solid tumor who agreed to provide an archival tumor sample, a residual biopsy sample, or a fresh tumor biopsy sample
Participant experiencing ineffective treatment or who is intolerant to initial treatment, or for which standard treatment is no longer available
- Participant with an FGFR gene alteration detected by NGS panel*, who fell under one of the categories of the following groups:
- Group A: FGFR1-3 fusion
- Group B: FGFR1-3 specific activating mutations as below;
- FGFR1: P150S, T340M, R445W, N546K, K656E
- FGFR2: C62Y, A67V, N82K, D101Y, E160K, E163K, M186T, R203H, R210Q, Q212K, R251Q, S252W, P253R, P253L, A264T, W290C, K310R, Y328N, G364E, Y375C, C382R, A389T, V392A, R399Q, H416R, I422V, H544Q, N549H, N549K, N549D, N549S, L560F, K659E, K659N, R664W, E718K, S791T
- FGFR3: G380E, G380R, A391E, K650T, K650E, K650Q, K650N
- Group C: FGFR1-3 activating mutation not applicable to group B or FGFR1, 2 amplification
- Group D: Participant with cholangiocarcinoma harboring FGFR2 gene fusion who previously received a selective FGFR inhibitor other than E7090 and demonstrated progressive disease or resistance.
Participant is age less than20 years old.
Participant whose Performance Status (Eastern Cooperative Oncology Group [ECOG]) is 0–1.
Participant(s) with non-primary CNS tumors; the ones who had at least 1 lesion of ≥ 1.0 centimeter (cm) in the longest diameter for a non-lymph node or ≥ 1.5 cm in the short-axis diameter for a lymph node that was serially measurable according to RECIST v1.1, using computerized tomography/magnetic resonance imaging (CT/MRI).
- Participant with primary CNS tumors should fulfill the following criteria:
- Karnofsky performance status (KPS) ≥ 70
- Prior treatment, including radiation and/or chemotherapy, as recommended or appropriate for CNS tumor type
- ≥ 1 site of bi-dimensionally measurable disease (confirmed by MRI and evaluable by response assessment in neuro-oncology [RANO] criteria), with at least one measurable lesion ≥ 1 cm in each dimension and noted on more than one imaging slice
- Must be neurologically stable based on neurological examination for 7 days prior to enrollment.
Participant with corrected calcium ≤ 10.1 mg/dL: corrected calcium (mg/dL) = serum calcium (mg/dL) + (4-serum albumin).
Participant with phosphate ≤ 4.6 mg/dL.
- Participants who required treatment washout period from the last day of prior treatment until enrollment of this trial, was as follows:
- Antibody and other investigational drugs: ≥ 28 days
- Prior chemotherapy, surgical therapy, radiation therapy: ≥ 21 days (≥ 90 days from the date of the last radiation therapy for primary CNS tumors)
- Endocrine therapy, immunotherapy, small-molecule targeted therapy: ≥ 14 days
* Testing refers to insurance-applied NGS tests including FoundationOne®CDx Cancer Genome Profile/OncoGuide™ NCC Oncopanel System.
Exclusion criteria
Patients with brain, subdural, or leptomeningeal metastases
Patients with primary CNS tumor located in either cerebellum, brainstem, spinal cord, pituitary gland, optic nerve, or olfactory nerve
Patients who are positive for human immunodeficiency virus (HIV) antibody, HBs antigen, or HCV antibody (patients with positive HCV antibody but no detectable HCV-RNA were not excluded)
Patients who are negative for HB antigen, positive for HBs antibody or HBc antibody, and positive for HBV-DNA quantification (not excluded if HBV-DNA is below detection sensitivity)
Patient with Child-Pugh score of B or C
Patients with pericardial effusion, pleural effusion, or ascites requiring treatment
- Patients with presence of any of the following ocular diseases:
- Grade 2 or higher corneal disorders
- Active retinopathy (eg, age-related macular degeneration, central serous chorioretinal disease, retinal tear)
Participants who require drugs that strongly inhibit or induce the activity of metabolizing enzyme cytochrome P450 (CYP) 3A
FGFR gatekeeper mutation: FGFR1 V561, FGFR2 V564/565, FGFR3 V555/557, FGFR4 V550
- Patients with any of the following coexisting driver gene abnormalities:
- Genetic mutations (excluding VUS): KRAS, NRAS, EGFR, or BRAF V600
- Gene translocations of ALK, ROS1, or NTRK
Treatment methods
Participants received E7090 140 mg tablets orally once daily (QD) in a 28-day treatment cycle until disease progression, development of unacceptable toxicity, participant requested to discontinue, withdrawal of consent, or study termination occurred. E7090 was administered at least 1 h before breakfast or at least 2 h after meals, and no food was ingested for 1 h after administration. The investigational drug used in this study was a 35-mg tablet. Dose reduction was in the order of 105 mg, 70-mg, and 35-mg.
Follow-up
Participants were evaluated at scheduled visits over the following study periods: Screening, Treatment, and Follow-up. Evaluations during the screening period were conducted within 28 days before the administration of the first dose of the study drug. Procedures conducted during the screening period that were performed within 4 days before first dose of E7090 may also have been used as the baseline evaluation and did not need to be repeated, unless otherwise specified. Participants were followed-up every 6 months following the initial enrollment date of the first participant. Follow-up was to continue until death or a maximum of 1 year following enrollment of the last participant.
Efficacy evaluations
Tumor assessments will be primarily based on the “Guidelines for Evaluating Treatment Effectiveness in Solid Tumors (RECIST Guidelines); Revised RECIST Guidelines version 1.1” [21]. A CT scan or MRI will be performed every 8 weeks (± 7 days) up to 24 weeks, every 12 weeks (± 7 days) after 25 weeks, and every 16 weeks (± 7 days) after 49 weeks from the start of protocol treatment until disease progression, death, withdrawal of informed consent, or treatment discontinuation. RANO criteria are widely used internationally in the field of brain tumors [22]. In this study, we also adopted the definition of the RANO criteria for tumor assessment in patients with primary central nervous system (CNS) tumors to compare with other clinical trials for primary brain tumors and to retain reference values that may serve as historical controls for future studies.
Safety evaluations
The safety evaluation includes ECOG performance status (± KPS]), vital signs (blood pressure, pulse rate, body temperature, oxygen saturation [SpO2]), laboratory evaluations, urinalysis, 12-lead electrocardiogram, AE collection, and ophthalmic examination. Safety follow-up will be performed on Day 30 (+ 7 days) after the final dose, or the start of post-treatment, whichever comes first. The CTCAE v5.0-JCOG will be used in this study to grade clinical and laboratory AEs.
Sample size calculation and statistical methods
The sample sizes in Groups A, B, and C were determined based on an exact test. A true ORR of ≤ 5% and a true ORR of ≥ 30% were considered as null and alternative hypotheses, respectively. Under a one-sided alpha error of 5%, considering the feasibility of case accumulation, the required number of patients in Groups A, B, and C were 10 (power 62%), 15 (87%), and 15 (87%), respectively. The sample size in group D was not based on statistical assumptions, and 5 patients can be enrolled in this as the maximum. ORR and DCR were calculated, and their 95% confidence intervals were estimated based on the Clopper-Pearson method. PFS and OS were evaluated using the Kaplan–Meier method, and 95% confidence intervals for median survival time and survival rate were estimated using the Brookmeyer and Crowley method and Greenwood’s formula, respectively. The proportion of patients who experienced AEs was also estimated. For each group, all treated populations were defined as those who received at least one drug dose. All statistical analyses for efficacy and safety endpoints were based on this population and were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Discussion
A single-arm basket study for the rare genetic abnormality, FGFR gene alteration, was designed under the nationwide network for rare cancers called MASTER KEY project. Utilizing this platform, we collated patient data across Japan through each cancer genome core hospital designated by the Ministry of Health, Labour and Welfare. This is one of the strengths of this study, as it allows the accumulation of cases with rare genetic abnormalities in a relatively short period of time.
Another feature of this study is the unique grouping of less frequent genetic abnormalities using expectations for drug response detected by MANO methods. It is suggested that the contribution of genetic abnormalities of FGFR to the carcinogenesis of solid tumors increases in the order of fusion gene, gene mutation, and gene amplification. This is also supported by the fact that the response rates in early clinical trials of FGFR inhibitors other than E7090 for FGFR gene aberrations were also higher for gene fusion (-45%), mutation (-17.6%), and amplification (-6.2%), in that order [23–27]. As the contribution of each FGF/FGFR gene pathway to activation is higher, inhibiting that signaling pathway is expected to have a higher therapeutic effect. In this study, patients were divided into groups A to C according to the expected efficacy of E7090 for each genetic abnormality based on robust results of preclinical study. Group A is for fusion, which has the highest response rate in the previous report. The mutations in group B that are found to be oncogenic by the MANO assay and have similar efficacy compared with the fusion genes are considered to be a group with a high contribution to carcinogenesis in the pathway inhibited by E7090. For group C, it is unclear whether gene amplification contributes to carcinogenesis, and for mutations other than group B, the contribution to carcinogenesis in the pathway inhibited by E7090 is estimated to be lower than that of group B based on the MANO method. Therefore, the design of this study was to collectively evaluate populations that were thought to be similar in 2 aspects: the expected efficacy and contribution to carcinogenesis of each genetic abnormalities.
The limitation of the study is that due to the small sample size, each cohort does not necessarily include all types of cancers and genetic abnormalities However, the efficacy of each individual genetic abnormality is not necessarily required for regulatory approval in Japan. The authors intend to discuss the results of this study with the PMDA, the Japanese regulatory authority, as there is precedent for approvals based on small samples in indications with a rare incidence, a clear benefit is observed and there is a high unmet need.
Available treatment options and the effectiveness of further treatments after the end of standard of care are very limited in most of cancers. This study and findings may serve as a novel model for the development of tumor-agnostic molecular targeted therapies for patients who have rare genetic abnormalities.
Acknowledgements
We thank Editage (www.editage.com) for English language editing.
Abbreviations
- AE
Adverse Event
- BICR
Blinded Independent Central Review
- BOR
Best Overall Response
- CNS
Central Nervous System
- CR
Complete Response
- CT
Computed Tomography
- CTCAE
Common Terminology Criteria for Adverse Events
- ECOG
Eastern Cooperative Oncology Group
- FGF
Fibroblast Growth Factor
- FGFR
Fibroblast Growth Factor Receptor
- HBc
Hepatitis B core
- HBs
Hepatitis B surface
- HBV
Hepatitis B Virus
- HCV
Hepatitis C Virus
- HIV
Human Immunodeficiency Virus
- JCOG
Japan Clinical Oncology Group
- KPS
Karnofsky Performance Status
- MANO method
Mixed-all-mutants-in-one method
- MRI
Magnetic Resonance Imaging
- NGS
Next-Generation Sequencing
- ORR
Overall Response Rate
- OS
Overall survival
- PFS
Progression Free Survival
- PS
Performance Status
- QD
Quaque die
- RANO
Response assessment in neuro-oncology
- RECIST
Response Evaluation Criteria in Solid Tumors
- TTR
Time To Response
Authors’ contributions
Principal investigator: MT (1); Advisor: KN, and KY; Study statistician: RM; Recruited patients: IK, MT (2), JM, HK and MT (1); Conception and design: YC, KS, YK, HO, SK, KY and MT (1); Member of study management group: MI, KA, KK, NO and KN; Drafting or revising the manuscript: YC and KS; Final approval of the manuscript: MT (1); All authors read and approved the final manuscript.
Funding
This work is supported by Eisai Co., Ltd. and AMED (Japan Agency for Medical Research and Development) under the grant number 20lk1403036h0001. AMED is the governmental funding body and provides funding only. Eisai provides drug (E7090) and funding for this study, however, was not and will not be involved in creating or modifying the study protocol. Also, Eisai will not be able to see the data obtained from this study before the data is finalized. The study protocol and design was also peer reviewed by the external non-commercial body as part of the peer review process.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the creating process of current protocol.
Declarations
Ethics approval and consent to participate
The National Cancer Center Hospital Certified Review Board approved the study protocol in March 2021, and participant enrollment began in June 2021 (Institutional review board registry number: T4912). This study was also approved by the Ethics Committees of Hokkaido University Hospital (R3-1), Tohoku University Hospital (213004), Kyoto University Hospital (K078), and Kyushu University Hospital (2021302). All participants receive written and oral information prior to participation and provide written and verbal consent.
Consent for publication
This manuscript contains no individual person’s data.
Competing interests
This study is supported by Eisai Co., Ltd. and AMED (Japan Agency for Medical Research and Development) under the grant number 20lk1403036h0001. All authors declare that they have no competing interests on this study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Meric-Bernstam F, Brusco L, Shaw K, Horombe C, Kopetz S, Davies MA, et al. Feasibility of Large-Scale Genomic Testing to Facilitate Enrollment Onto Genomically Matched Clinical Trials. J Clin Oncol. 2015;33(25):2753–2762. doi: 10.1200/JCO.2014.60.4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sunami K, Ichikawa H, Kubo T, Kato M, Fujiwara Y, Shimomura A, et al. Feasibility and utility of a panel testing for 114 cancer-associated genes in a clinical setting: A hospital-based study. Cancer Sci. 2019;110(4):1480–1490. doi: 10.1111/cas.13969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Okuma HS, Fujiwara Y. Have We Found the Key to Unravel Treatment Development Lags for Rare Cancers?: MASTER KEY Project. Clin Pharmacol Ther. 2019;106(3):491–492. doi: 10.1002/cpt.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwaederle M, Zhao M, Lee JJ, Eggermont AM, Schilsky RL, Mendelsohn J, et al. Impact of Precision Medicine in Diverse Cancers: A Meta-Analysis of Phase II Clinical Trials. J Clin Oncol. 2015;33(32):3817–3825. doi: 10.1200/JCO.2015.61.5997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okuma HS, Yonemori K, Narita SN, Sukigara T, Hirakawa A, Shimizu T, et al. MASTER KEY Project: Powering Clinical Development for Rare Cancers Through a Platform Trial. Clin Pharmacol Ther. 2020;108(3):596–605. doi: 10.1002/cpt.1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turner N, Grose R. Fibroblast growth factor signalling: from development to cancer. Nat Rev Cancer. 2010;10(2):116–129. doi: 10.1038/nrc2780. [DOI] [PubMed] [Google Scholar]
- 7.Itoh N. The Fgf families in humans, mice, and zebrafish: their evolutional processes and roles in development, metabolism, and disease. Biol Pharm Bull. 2007;30(10):1819–1825. doi: 10.1248/bpb.30.1819. [DOI] [PubMed] [Google Scholar]
- 8.Helsten T, Elkin S, Arthur E, Tomson BN, Carter J, Kurzrock R. The FGFR Landscape in Cancer: Analysis of 4,853 Tumors by Next-Generation Sequencing. Clin Cancer Res. 2016;22(1):259–267. doi: 10.1158/1078-0432.CCR-14-3212. [DOI] [PubMed] [Google Scholar]
- 9.Babina IS, Turner NC. Advances and challenges in targeting FGFR signalling in cancer. Nat Rev Cancer. 2017;17(5):318–332. doi: 10.1038/nrc.2017.8. [DOI] [PubMed] [Google Scholar]
- 10.Tanizaki J, Ercan D, Capelletti M, Dodge M, Xu C, Bahcall M, et al. Identification of Oncogenic and Drug-Sensitizing Mutations in the Extracellular Domain of FGFR2. Cancer Res. 2015;75(15):3139–3146. doi: 10.1158/0008-5472.CAN-14-3771. [DOI] [PubMed] [Google Scholar]
- 11.Nakamura IT, Kohsaka S, Ikegami M, Ikeuchi H, Ueno T, Li K, et al. Comprehensive functional evaluation of variants of fibroblast growth factor receptor genes in cancer. NPJ Precis Oncol. 2021;5(1):66. doi: 10.1038/s41698-021-00204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loriot Y, Necchi A, Park SH, Garcia-Donas J, Huddart R, Burgess E, et al. Erdafitinib in Locally Advanced or Metastatic Urothelial Carcinoma. N Engl J Med. 2019;381(4):338–348. doi: 10.1056/NEJMoa1817323. [DOI] [PubMed] [Google Scholar]
- 13.Abou-Alfa GK, Sahai V, Hollebecque A, Vaccaro G, Melisi D, Al-Rajabi R, et al. Pemigatinib for previously treated, locally advanced or metastatic cholangiocarcinoma: a multicentre, open-label, phase 2 study. Lancet Oncol. 2020;21(5):671–684. doi: 10.1016/S1470-2045(20)30109-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Javle M, Lowery M, Shroff RT, Weiss KH, Springfeld C, Borad MJ, et al. Phase II Study of BGJ398 in Patients With FGFR-Altered Advanced Cholangiocarcinoma. J Clin Oncol. 2018;36(3):276–282. doi: 10.1200/JCO.2017.75.5009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watanabe Miyano S, Yamamoto Y, Kodama K, Miyajima Y, Mikamoto M, Nakagawa T, et al. E7090, a Novel Selective Inhibitor of Fibroblast Growth Factor Receptors, Displays Potent Antitumor Activity and Prolongs Survival in Preclinical Models. Mol Cancer Ther. 2016;15(11):2630–2639. doi: 10.1158/1535-7163.MCT-16-0261. [DOI] [PubMed] [Google Scholar]
- 16.Koyama T, Shimizu T, Iwasa S, Fujiwara Y, Kondo S, Kitano S, et al. First-in-human phase I study of E7090, a novel selective fibroblast growth factor receptor inhibitor, in patients with advanced solid tumors. Cancer Sci. 2020;111(2):571–579. doi: 10.1111/cas.14265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morizane C, Ueno M, Ioka T, Tajika M, Ikeda M, Yamaguchi K, et al. Expansion part of phase I study of E7090 in patients with cholangiocarcinoma harboring FGFR2 gene fusion and with gastric cancer harboring FGFR2 gene amplification or FGFR2 protein high expression. J Clin Oncol. 2020;38(4_suppl):538. doi: 10.1200/JCO.2020.38.4_suppl.538. [DOI] [Google Scholar]
- 18.Kohsaka S, Nagano M, Ueno T, Suehara Y, Hayashi T, Shimada N, et al. A method of high-throughput functional evaluation of EGFR gene variants of unknown significance in cancer. Sci Transl Med. 2017;9(416):eaan6566. [DOI] [PubMed]
- 19.Nagano M, Kohsaka S, Ueno T, Kojima S, Saka K, Iwase H, et al. High-Throughput Functional Evaluation of Variants of Unknown Significance in ERBB2. Clin Cancer Res. 2018;24(20):5112–5122. doi: 10.1158/1078-0432.CCR-18-0991. [DOI] [PubMed] [Google Scholar]
- 20.Hirakawa A, Nishikawa T, Yonemori K, Shibata T, Nakamura K, Ando M, et al. Utility of Bayesian Single-Arm Design in New Drug Application for Rare Cancers in Japan: A Case Study of Phase 2 Trial for Sarcoma. Ther Innov Regul Sci. 2018;52(3):334–338. doi: 10.1177/2168479017728989. [DOI] [PubMed] [Google Scholar]
- 21.Eisenhauer EA, Therasse P , Bogaerts J , Schwartz LH , Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45(2):228–47. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 22.van den Bent MJ, Wefel JS, Schiff D, Taphoorn MJ, Jaeckle K, Junck L, et al. Response assessment in neuro-oncology (a report of the RANO group): assessment of outcome in trials of diffuse low-grade gliomas. Lancet Oncol. 2011;12(6):583–593. doi: 10.1016/S1470-2045(11)70057-2. [DOI] [PubMed] [Google Scholar]
- 23.Chae YK, Hong F, Vaklavas C, Cheng HH, Hammerman P, Mitchell EP, et al. Phase II Study of AZD4547 in Patients With Tumors Harboring Aberrations in the FGFR Pathway: Results From the NCI-MATCH Trial (EAY131) Subprotocol W. J Clin Oncol. 2020;38(21):2407–2417. doi: 10.1200/JCO.19.02630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nogova L, Sequist LV, Perez Garcia JM, Andre F, Delord JP, Hidalgo M, et al. Evaluation of BGJ398, a Fibroblast Growth Factor Receptor 1–3 Kinase Inhibitor, in Patients With Advanced Solid Tumors Harboring Genetic Alterations in Fibroblast Growth Factor Receptors: Results of a Global Phase I, Dose-Escalation and Dose-Expansion Study. J Clin Oncol. 2017;35(2):157–165. doi: 10.1200/JCO.2016.67.2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tabernero J, Bahleda R, Dienstmann R, Infante JR, Mita A, Italiano A, et al. Phase I Dose-Escalation Study of JNJ-42756493, an Oral Pan-Fibroblast Growth Factor Receptor Inhibitor, in Patients With Advanced Solid Tumors. J Clin Oncol. 2015;33(30):3401–3408. doi: 10.1200/JCO.2014.60.7341. [DOI] [PubMed] [Google Scholar]
- 26.Bahleda R, Meric-Bernstam F, Goyal L, Tran B, He Y, Yamamiya I, et al. Phase I, first-in-human study of futibatinib, a highly selective, irreversible FGFR1-4 inhibitor in patients with advanced solid tumors. Ann Oncol. 2020;31(10):1405–1412. doi: 10.1016/j.annonc.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Subbiah V, Barve M, Iannotti NO, Gutierrez M, Smith DC, Roychowdhury S, et al. Abstract A078: FIGHT-101: A phase 1/2 study of pemigatinib, a highly selective fibroblast growth factor receptor (FGFR) inhibitor, as monotherapy and as combination therapy in patients with advanced malignancies. Molecular Cancer Therapeutics. 2019;18(12 Supplement):A078-A.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the creating process of current protocol.