Abstract
Objective
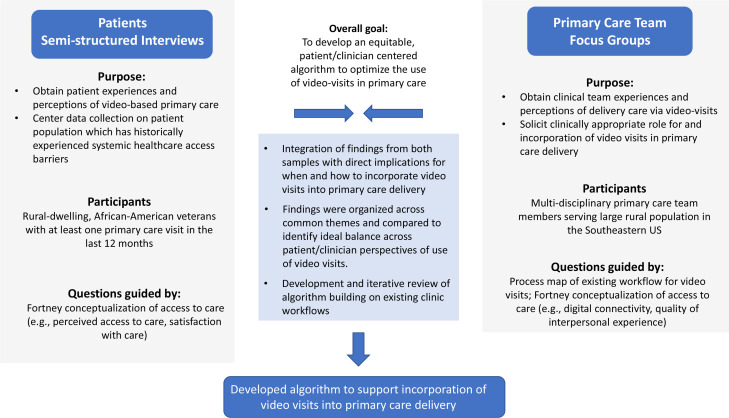
The COVID-19 pandemic sparked exponential growth in video visit use in primary care. The rapid shift to virtual from in-person care exacerbated digital access disparities across racial groups and rural populations. Moving forward, it is critical to understand when and how to incorporate video visits equitably into primary care. We sought to develop a novel clinical algorithm to guide primary care clinics on how and when to employ video visits as part of care delivery.
Design
Qualitative data collection: one team member conducted all patient semistructured interviews and led all focus groups with four other team members taking notes during groups.
Setting
3 rural primary care clinics in the USA.
Participants
24 black veterans living in rural areas and three primary care teams caring for black veterans living in rural areas.
Primary and secondary outcome measures
Findings from semistructured interviews with patients and focus groups with primary care teams.
Results
Key issues around appropriate use of video visits for clinical teams included having adequate technical support, encouraging engagement during video visits and using video visits for appropriate clinical situations. Patients reported challenges with broadband access, inadequate equipment, concerns about the quality of video care, the importance of visit modality choice, and preferences for in-person care experience over virtual care. We developed an algorithm that requires input from both patients and their care team to assess fit for each clinical encounter.
Conclusions
Informed matching of patients and clinical situations to the right visit modality, along with individual patient technology support could reduce virtual access disparities.
Keywords: PRIMARY CARE, Telemedicine, GENERAL MEDICINE (see Internal Medicine)
Strengths and limitations of this study.
Primary qualitative data collection from patients and care providers in the same clinical catchment area.
Data collection centred on a historically under-resourced population to promote equitable clinical algorithm development.
Partnered engagement in data collection tool development.
Data collected from one geographical area and one healthcare system may not translate to other regions or clinical settings.
Focus groups were conducted virtually which may have limited the participation of some individuals.
Introduction
The optimal role of video visits within primary care is undefined. With the onset of COVID-19, the need to stem potential viral transmission led to dramatic and rapid shifts from in-person to virtually delivered care, including video-based care. Video offers assessment and communication advantages not possible with phone alone (eg, visualising a rash), may support better patient–provider rapport building,1 and receives higher remuneration from private insurers.2 However, video-based care comes with distinct challenges for clinical teams (eg, new clinic workflow) and patients (eg, device access, technical literacy). In the absence of clear evidence, there is an urgent need to identify the right telehealth modality for the right clinical problem for the right patient at the right time.3
Finding the optimal role for virtual primary care is particularly critical for historically marginalised and under-resourced populations. While telephone-delivered care may increase access to care,4 early findings show that when compared with phone-based care, systemically disadvantaged populations (eg, older adults, those in rural or low bandwidth areas, racial and ethnic minorities, unhoused individuals) are less likely to engage in video visits.5 6 Compared with phone, access disparities were more pronounced with video visits due to requirements for digital literacy, higher cost, camera-ready phones or computers, and access to adequate bandwidth.5 7–10 These findings underscore the structural determinants of telehealth disparities, including structural racism and unequal access to the internet.11 12 Addressing inequitable engagement in virtual care and related access disparities requires action at multiple levels from individual clinic practices to national policies.
Our objective was to develop a clinical algorithm to guide when and how to incorporate video visits into primary care delivery. For this algorithm to support equitable video visit access, we focused our data collection on patients who have historically experienced systemic healthcare access limitations. As the largest provider of US primary care and a national telehealth leader, the Department of Veterans Affairs Health Care System (VA) is an optimal setting to examine how to optimise virtual care delivery. Thus, we engaged populations at increased risk for low video uptake, specifically rural, black veterans6 8 13
Materials and methods
Data collection occurred among patients and clinical team members of VA outpatient primary care clinics in the Piedmont area of North Carolina, which serve large populations of rural dwelling individuals. We followed Consolidated Criteria for Reporting Qualitative research (COREQ) guidelines for reporting of qualitative research where applicable.14
Framework
We anchored our approach on the conceptualisation of access developed by Fortney et al.15 This model emphasises actual and perceived access to virtual and in-person care and guided our data collection materials (eg, interview guides, matrix analysis, structured note templates), eligibility criteria (eg, users, non-users) and debriefing sessions among the research team.
Setting
We defined rurality using rural–urban communicating areas (RUCA codes) consistent with the VA Office of Rural Health.16 At the time of data collection, all clinics were providing in-person, telephone-based and video-based care, though virtual care, including video-based care, was encouraged across the VA healthcare system due to the pandemic.17 While there was some flexibility on use of approved commercially available videoconference platforms during the early pandemic, the VA primarily uses an internal VA platform for video-based care delivery.
Patients
We conducted 26 semistructured interviews with veterans who were identified as Black in the electronic health record, who were engaged in VA healthcare (ie, >1 primary care visits within the prior 12 months) and lived in rural areas. Recruitment was stratified by patients who had completed at least one video-based primary care encounter (n=14) and those who had not (n=12). The research team contacted a subset of potential participants via mailed letter in batches of 25 with purposive sampling of Black veterans living in rural areas and then followed up by phone until the target recruitment number was obtained and thematic saturation was reached. We obtained verbal consent.
All interviews were conducted and recorded via WebEx (audio-only) between February and May 2021 by a study team member (KRP) who identifies as white and has training in qualitative methodology. The interviewer listened to audiorecordings and took templated notes. To ensure reliability and validity, a second study team member (AL, KG, LLZ, MES-B and CW) independently listened to interviews, reviewed and amended interviewer notes. Responses to each domain were summarised using matrix analysis for participants stratified by previous video visit experience. Summary responses were generated independently by two team members and reviewed by a third reviewer.
Patient and public involvement
The driving question for this project was developed in response to trends in patient utilisation of video-based care and the need to obtain patient preferences and experiences directly from the patients themselves. We received consultation on our approach from the Durham VA Veteran Engagement Panel and the Durham VA Healthcare System Antiracism and Black Equity Advisory Board; however, these individuals were not directly involved in the conduct of this work.
Primary care teams
We invited all primary care team members from three VA primary care clinics serving a single facility in the Piedmont area of North Carolina which cares for a large population of Black, rural-dwelling population to participate in clinic specific focus groups. We conducted four video-based focus groups across these three clinics between December 2020 and February 2021 using WebEx videoconferencing platform. Participants were encouraged to turn on their cameras if available and to make use of the chat function. Focus groups were first given the opportunity to review and provide feedback on a process map,18 an explicit step-by-step illustrative flow diagram of a proposed approach to the incorporation of video visits into primary care based on existing workflow in our institution (see online supplemental appendix 1). Discussions followed the focus group guide. Research team members (n=3) took notes during focus groups using structured templates. A rapid qualitative approach and matrix method were used to identify focus group themes.19–21 Notes from the structured templates were consolidated into matrices consistent with Fortney model domains. This matrix analysis approach was paired with real-time iterative team-based analysis.22 A subgroup of team members (KRP, KG, CW, AL, MES-B and L LZ) met virtually during data collection to review domain level findings and identify implications for primary care video-based care delivery.
bmjopen-2022-062261supp001.pdf (55.7KB, pdf)
Virtual care algorithm generation
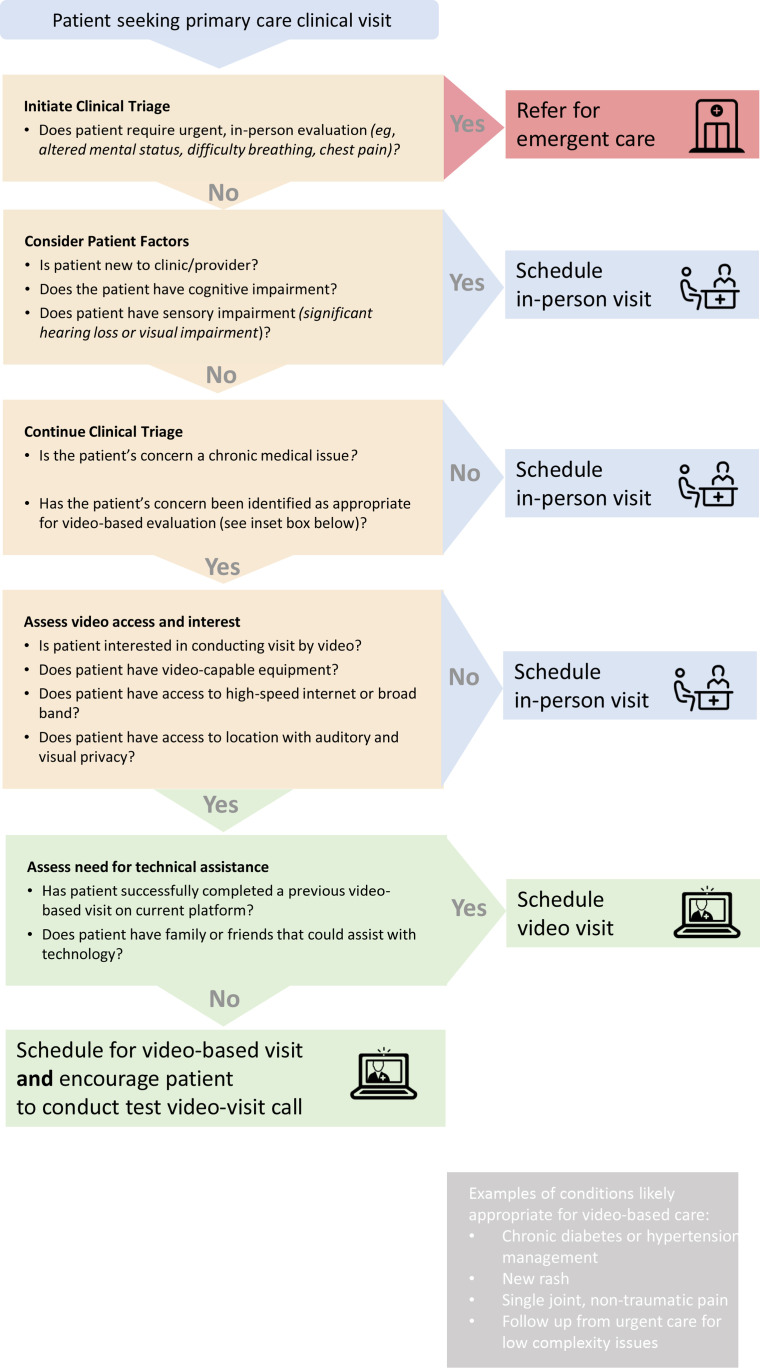
We based the initial algorithm structure on our proposed process map of virtual care incorporation into primary care workflow (online supplemental appendix 1) and standards for clinical algorithm development.23 Working from themes identified through patient interviews and clinical team focus group findings, we evaluated potential overlap, conflict and novelty related to needs and preferences for when video-based visits are acceptable. After prioritising patient safety and clinical appropriateness, we reorganised the preliminary clinical algorithm to explicitly include patient choice and preferences and to ensure their formal incorporation into clinic workflow (figure 1). For example, from clinical focus groups, we added an initial step to identify patients whose clinical characteristics would be more appropriate for a face-to-face visit regardless of patient preference (eg, patients with cognitive impairment). Another example is adding assessment of patient preference for visit modality and need for technical assistance as an explicit step before scheduling. This was based on patient interview findings that there was great dissatisfaction when modality was assigned rather than offered, and that the need for technical assistance was often a significant barrier for patients. Our research team iteratively revised the algorithm and offered clinical team focus group participants the opportunity to review it. Ultimately, our novel algorithm seeks to guide whether video or an in-person care should be offered to a specific patient with a given clinical situation, while incorporating consideration of the patient’s existing technical skills and equipment.
Figure 1.
Algorithm development process.
Results
Focus group participants included physicians, advanced-practice providers, administrative staff members and nurses (n=38). Twenty-four individuals completed semistructured interviews, 14 with and 12 without prior video visit experience. Demographics of the interviewed patients are consistent with the source patient population (table 1).
Table 1.
Characteristics of patients participating in semistructured interviews
| Prior video Visit N=14 |
No prior video Visit N=12 |
|
| Age, mean (SD) | 64.50 (SD 9.00) | 69.08 (8.69) |
| Gender* | ||
| Male | 11 | 12 |
| Female | 3 | – |
| Tech self-efficacy† | Mean=4 | Mean=4.29 |
| <3 | 2 | 2 |
| 3–5 | 12 | 9 |
| VA primary healthcare source | ||
| Yes | 11 | 11 |
| No | – | 1 |
| Not sure | 3 | 1 |
| Distance to closest VA | ||
| 0–20 miles | 4 | 5 |
| 21–80 miles | 9 | 6 |
| missing | 1 | 1 |
| No. prior video visits | ||
| 0 visits | – | 12 |
| one visit | 2 | – |
| 2–10 visits | 7 | – |
| >10 visits | 5 | – |
| No of prior telephone visits | ||
| 0 visits | 2 | 2 |
| 1 visit | – | – |
| 2–10 visits | 7 | 10 |
| >10 visits | 5 | – |
| Received help for video visit | ||
| Yes | 11 | 1 |
| No | 2 | 10 |
| Not sure | 1 | 1 |
| Device used for video visit | ||
| iPhone | 5 | – |
| Android phone | 5 | – |
| Tablet | 2 | – |
| Laptop or computer | 2 | – |
| Don’t have any devices to use | 0 | – |
| Reliable broadband | ||
| Yes | 11 | 6 |
| No | 1 | 5 |
| Not sure | 2 | 1 |
| Reliable device | ||
| Yes | 12 | 9 |
| No | 2 | 2 |
| Not sure | 0 | 1 |
| Racism in healthcare (M across items, SD, # of respondents)‡ | 2.80 (1.17) for n=11 | 3.02 (0.72) for n=10 |
| Endorsed Agreement with: | ||
| RHC 1: Doctors treat African American and White people the same. (N, %, # respondents) | 2 (18.2%) of 11 | 7 (58.3%) of 12 |
| RHC 2: Racial discrimination in telehealth is common. (N, %, # respondents) | 6 (50.0%) of 12 | 5 (50.0%) of 10 |
| RHC 3: In most hospitals, African American and Whites receive the same kind of telehealth care. (N, %, # respondents) | 5 (41.6%) of 12 | 4 (36.4%) of 11 |
| RHC 4: African Americans can receive the telehealth care they want as equally as White people can. (N, %, # respondents) | 5 (38.5%) of 13 | 4 (36.4%) of 11 |
| Personal discrimination scale (M across items, SD)§ | 2.01 (0.75) | 1.98 (0.77) |
| Endorsed Experiencing: | ||
| PDS 1: Treated with less courtesy than other people? (N, %, # respondents) | 10 (71.4%) of 14 | 6 (60.0%) of 10 |
| PDS 2: Treated with less respect than other people? (N, %, # respondents) | 11 (78.6%) of 14 | 7 (70.0%) of 10 |
| PDS 3: Received poorer services than other people? (N, %, # respondents) | 9 (69.2%) of 13 | 7 (70.0%) of 10 |
| PDS 4: Had a doctor or nurse act as if he or she thinks you were not smart? (N, %, # respondents) | 6 (42.9%) of 14 | 3 (30.0%) of 10 |
| PDS 5: Had a doctor or nurse act as if he or she was afraid of you? (N, %, # respondents) | 4 (28.6%) of 14 | 5 (50.0%) of 10 |
| PDS 6: Had a doctor or nurse act as if he or she was better than you? (N, %, # respondents) | 9 (64.3%) of 14 | 5 (55.6%) of 9 |
| PDS 7: Felt like a doctor or nurse was not listening to what you were saying? (N, %, # respondents) | 11 (78.6%) of 14 | 7 (70.0%) of 10 |
| Telehealth satisfaction scale ¶ (M across items, SD, # of respondents) | 1.83 (0.49) for n=13 | 2.02 (0.19) for n=9 |
Scale scores for RHC, PDS, and TeSS only computed when all items were answered.
*As identified in chart.
†Measure by response to the following question: How confident are you that you can complete the steps necessary that you identified above to attend a video visit with your provider on a scale of 1–5? One participant in the no prior video visit group did not provide an answer for this question.
‡RHC measure (Hausmann et al38) agreement defined as marking ‘agree’ or ‘strongly agree’. Average score computed with item two reverse coded; range of possible score by question 1–5 with 1=strongly disagree and 5=strongly agree.
§PDS adapted from everyday discrimination scale39; endorsement marked by any response other than ‘never’ for all questions; range of possible score by question 1–5 with 1=never and 5=always.
¶TeSS17 40 is a 10-item measure with with range of possible score by question from 1 to 3 with 1=‘excellent’ and 3=‘poor/fair’.
PDS, Personal Discrimination Scale; RHC, Racism in Healthcare; TeSS, Telehealth Satisfaction Scale; VA, Veterans Affair.
Patient interviews lasted from 25 to 45 min and focus groups from 45 to 60 min. Below, we present themes from patients and clinical team data collection (table 2).
Table 2.
Clinician and patient experiences with primary care video visits
| Domain | Patient | Clinical team | Implications for clinical algorithm |
| Perceived access to video-based care |
|
|
|
| Satisfaction with video-based care | Negative aspects of video visits:
Positive aspects of video visits:
|
|
|
| Attitudes towards video-based care |
|
|
|
Patient findings
Perceived access to care
Most patients did not report personally experiencing or witnessing others receiving differential access to care due to personal identity. However, several patients noted differential treatment around receipt of benefits, pain medication, and appointment scheduling: ‘…All my life, from the service part all the way up to where [I am] today, I feel like I’ve had to fight for myself…’ (video-user). Reasons for differential treatment were attributed to characteristics such as age, racial identity, disability status and/or a history of substance use disorder.
Patients commonly reported challenges to video-based visits due to having inadequate technical skills or a lack of access to needed equipment/broadband. Only half of patients who had successfully completed video-based visits previously felt confident in their ability to access video-based care in the future. For patients who did feel confident, having a successful first video visit experience was reassuring. Among those without a prior video visit, there were varying degrees of confidence: ‘I’ve never used a computer, so I’m a little shaky of it, you understand?… because if I get the thing and I don’t know how to use it, that’s not worth a nickel…You hit one wrong button and you’re out of business’ (video non-user).
Satisfaction with care
Patients expressed multiple concerns about receiving care by video. First, patients commonly reported perceptions that video visits were of lower quality and more impersonal compared with in-person: ‘Face to face makes it feel that I matter, that I’m important to the provider’ (video-user). Second, patients with and without prior video visits noted concerns about a provider’s ability to adequately assess medical concerns via video: ‘They can’t make medical decisions without seeing you in the face, looking at your body’ (video-user). Third, many patients reported completing telephone-based visits and generally perceived phone-based visits to be lower quality than either in-person or video: ‘it is hard to know on [the] phone [what the provider] is doing, whether they’re listening to you or understanding what you are saying. I’d prefer in-person visits, but video would be the next best thing’ (video non-user). Finally, patients wanted to choose whether to have their primary care encounter in-person or via video. Many patients reported being told that their visit would occur via video rather than being offered a choice. Some patients who had not completed video-based visits thought that they might feel more relaxed and less rushed at home: ‘Very convenient if I’m going to stay on top of my health’ (video non-user).
Preferences for care
While patients acknowledged the potential convenience of video-based care, most individuals still preferred in-person: ‘given the conditions we face today [COVID-19 pandemic], I understand it. But my preference is in the office’ (video non-user). Reasons given for this preference centred on the full experience of in-person care: ‘If it was up to me, I’d go to the VA. It is a form of release for me…It’s a way for me to get out of the house’ (video-user). In-person care also was noted to offer better eye contact, rapport building, communication, physical exam and the opportunity to coordinate care. The majority of patients thought visit modality should be tied to clinical need. Most veterans preferred video for mental health, while in-person was preferred for specific conditions, such as pain or urgent concerns. This preference appears to be related to a sense that either the provider could not fully evaluate the patient remotely or that the patient could not fully communicate their concerns when not face to face: ‘They can see what’s going on and know if you’re having any difficulties. On video, you have to stay in one position, they don’t know how you feel, you’re just talking…in person, they can tell if you’re not genuine’ (video-user).
Clinical team member findings
Perceived access to care
Clinical teams noted that digital connectivity issues frequently present problems for accessing care. Specifically, video platform malfunctions consume significant visit time. Additionally, many providers were unsatisfied with available technology for video visits. Team members noted a diminished interpersonal connection during video-based visits and that sometimes both parties (patients and clinicians) were distracted or not fully engaged. Difficulty engaging with certain patients via video was particularly problematic—specifically those with cognitive, significant sensory or functional impairments. One strategy used to overcome technical barriers was having a family member or friend provide logistical support during a video visit. Overall, clinical teams reported that patients living in rural areas and older patients had the most difficulty engaging in video-based care due to limited availability of and comfort with technology.
Satisfaction with care
Clinicians felt that video visits were inadequate for certain situations and often scheduled without regard to clinical appropriateness of the modality. Management of chronic condition (eg, hypertension) was given as a specific example that could be appropriate for video, as were dermatological conditions, mental health and non-traumatic single joint pain. Clinical conditions not appropriate for video would include new patient visits, patients with cognitive impairment or new conditions.
Preferences for care
Clinicians expressed frustration when video-based care did not align with the patient’s clinical problem. In addition, teams noted a significant need for streamlining the clinic workflow process which was felt to be designed for in-person visits and not conducive to virtual care. For example, due to in-person clinic demands, teams noted that often no one contacts patients in advance to verify that they have a working link for the video visit and that they are ‘checked-in’ online before an appointment.
Clinical algorithm
We identified three key decision points for matching a specific patient to a particular modality for an encounter. First, it is important to determine if the patient and their health concerns are clinically appropriate for video; second, patients need to agree to video modality use; third, patients need to be assessed for readiness for video visits (eg, having accessible technology, adequate technical skills). These decision points seem to be implied in the existing primary care processes, but were not explicit or consistently applied. We combined these decision points into one ready-to-implement algorithm to clearly link the importance of both clinical appropriateness and patient readiness. Initially, the algorithm prompts clinical consideration of the appropriateness of a patient’s current clinical concern for visit modality type (see figure 2). Once a patient situation is deemed clinically appropriate for video-based care, the algorithm then requires a patient’s response regarding interest in video-based care. Note that the algorithm does not specify who is responsible for making this determination. This is because we anticipate that it could be managed by different clinical roles (eg, physician, advanced practice provider, nurse care manager) depending on a given clinic’s resources and capacity. If the patient is interested in a video visit, the algorithm proceeds to incorporate what equipment and technological support are needed in advance of the video appointment. Importantly, it is possible that the provider would determine that an in-person visit is still necessary after a video-based visit, though the expectation and goal would be for this to be rare. Also identified through the integration of patient and clinical team findings were key patient video visit preparation steps (table 3).
Figure 2.
Clinical support algorithm for incorporation of video visits into primary care workflow.
Table 3.
Patient teaching points before a video visit
| Patient teaching before video visit | ||
| At scheduling | In advance of visit | During a visit |
| Explain when video visit is appropriate | Prepare for visit as you would an in-person visit | Limit distractions |
| Explain that clinical team will determine appropriateness | Join video platform at least 15 min early | Do not multitask during visit (eg, do not clean house) |
| Give patients a choice | Ensure visual and auditory privacy | Do not drive during video visit |
| Recruit a family member to help | Be aware that your provider may at times not be making eye contact while looking at medical record on a second screen | |
| Create a back-up plan | ||
Discussion
We identified patient and primary care team experiences with video visits across key dimensions of telehealth access and used our findings to develop a novel algorithm to guide the incorporation of equitable video visits into primary care. Consistent with previous literature, we confirmed that clinicians have concerns about technology malfunction, inadequate technical support, and recognise the importance of having a family or friend available before and during a visit to assist with the patient’s technology.24–26 Our study provides new insight in virtual care use. We found that patients are concerned with quality of video-based care, prefer to have choice of visit modality, and place personal value on in-person experience despite convenience costs.
Our intention was to develop an algorithm that could support equitable access to virtual care; however, we did not identify a consistent pattern about which patients would prefer video-based care. Thus, we incorporated features intended to promote equity in access to video-based care broadly: (1) emphasised the importance of using this algorithm with all patients to avoid implicit bias regarding who may or may not want a video visit and and/or need technological support; (2) underscored patient choice regarding visit modality when possible; (3) identified actions to promote optimal patient engagement during a video visit and (4) recognised clinician behaviours that promote trustworthiness and transparency during video-based encounters. One concern raised by some veteran participants was that if a video-based visit was completed and that either the patient or their provider wanted an in-person follow-up visit, that the opportunity for that in-person visit might be lost. In fact, one type of visit does not preclude the other. While clinical encounters that are conducted virtually may later require an in-person evaluation (eg, due to patient preference or change in clinical indication), it is unknown how frequently this is likely to occur. Also unknown is the optimal timing and frequency of an in-person follow-up visit after video-based care. As this has important implications for the patient experience, patient outcomes, and health system resource use, exploration of impact of virtual care on overall healthcare utilisation will be important for future research. In addition, we acknowledge that there are other existing approaches for choosing visit modality.27 However, existing guides generally have not systematically incorporated the patient perspective in visit modality choice.28 29 Our algorithm purposively centres on the patient, as well as on the patient–provider dyad, through careful consideration of a patient’s preferences and their experiences with telehealth, particularly tailored to patients from historically under-resourced populations. This is a population which has traditionally suffered from inequities in access to traditional in-person care and is at risk for similar challenges in accessing video-based care. Our algorithm proactively addresses this risk at a time when video-based care is on a precipitous rise.
We also identified that both patients and clinicians expressed concerns about the impact of video visits on patient–provider relationship and subsequent clinical care quality. In particular, patients expressed misgivings about quality of care received via video. While the importance of patient confidence in virtual care has been previously noted,30 31 our study adds that this may not be true for all types of care or at all points in the care continuum. Similar to patients, clinicians commonly described concerns about the interpersonal quality of virtual clinical interactions, especially around building rapport with new patients32 and loss of body language and social cues.33 34 Strategies to improve the virtual care experience including improving accessibility through access to closed captioning and language interpretation,35 incorporation of trauma-informed care principles such as transparency during visit actions and maintaining good eye contact,35 36 and adequate technology training for patients and clinical teams.24 37 Together with previous findings, our work points to the need for an intentional approach to the implementation of high-quality, equitable, patient-centred video-based care.
This research has limitations. First, our clinical support algorithm was informed by qualitative data from clinical teams in rural North Carolina and Black veterans residing in rural areas. However, it may be applicable to other rural, minoritised patients using virtual care in other healthcare systems with similar reimbursement pressures. Second, we focused on the context of primary care and, thus, the algorithm may not be relevant to specialty care. For example, specialty clinics typically provide care for individual conditions or organ systems for which it may be easier to predict clinical appropriateness of video-based care. Third, we focused this algorithm on the choice between video-based visits versus care delivered in-person because healthcare system and insurance reimbursement policies have generally favoured video-based care and not phone-based care. We acknowledge that telephone-based care has been recognised as an important modality for maintaining access to care, especially for patients with limited access to broadband services. However, as our work focused on video based versus face-to-face care based on what services were anticipated to remain reimbursable postpandemic, we did not collect data about how and when phone should fit into visit modality decisions. Within the VA healthcare system, there is no differential reimbursement for telephone-based care, video-based care and in-person care. This may limit generalisability of our algorithm into other healthcare systems that may have a financial driver that could usurp patient and/or provider preference. Fourth, the interviewer for both the focus groups and the patient interviews identifies as white, which may have influenced participant willingness to disclose racial discrimination experiences. Our centre has made a focused effort to hire and train diverse qualitative staff since the conclusion of this work. Finally, determinants of access to healthcare expand beyond clinic level policies and actions thus broader innovation and changes will be required to address access disparities.
Conclusions
Optimal and equitable incorporation of video visits into primary care delivery requires thoughtful planning and potential reworking of clinic workflow. Assessment of clinical appropriateness of a virtual modality as well as patient preference and technological readiness are crucial before each visit. Next steps for this work include evaluating the feasibility of our algorithm in a primary care practice and validating measures to assess patient interest in video visits. It will be critical to identify determinants of video visit uptake and areas needing adaptation for site specific characteristics. Informed matching of patients and clinical situations to the right visit modality, along with individual patient technology support, could contribute to broader virtual access disparities.
Supplementary Material
Acknowledgments
We would like to thank Dr. Gene Oddone for this early support of this project. We would also like to thank the ADAPT TeleFAR workgroup, the Durham Veteran Engagement Panel, and the Durham VA Health Care System Antiracism and Black Equity Advisory Board for consultation during development of this project. Additionally, we thank Eric Monson for data visualization consultation and Sharon Thompson for editorial assistance.
Footnotes
Contributors: KMG coconceptualised this project, participated in data collection, analysis and interpretation, drafted this work, and serves as guarantor; KRP developed data collection and analysis plan, collected the data, contributed to analysis and edited the manuscript; AL, CW and MSB participated in data collection, analysis and interpretation, and edited the manuscript; HBB contributed to conceptualisation, interpretation and edited this manuscript. HW supported data collection and analysis and edited this manuscript; DB contributed to data analysis, interpretation and edited this manuscript. LLZ coconceptualised this project, participated in data collection, analysis and interpretation, and drafted this work.
Funding: This work received funding from the VA Access Research Consortium (no funding number given) and was supported by the Durham Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT), (CIN 13-410) at the Durham VA Health Care System. AL was supported by VA HSR&D grants #18-234, MES-B and DB by VA HSR&D Career Development Award (CDA #17-006 and #19-035, respectively), and CW by VA OAA VA Quality Scholars Fellowship Programme (AF-3Q-05-2019-C).
Disclaimer: The content and views expressed here are solely those of the authors and do not reflect those of the US Federal Government.
Competing interests: AL reports receiving funds from PhRMA Foundation and Otsuka. Hayden Bosworth reports research funding through his institution from BeBetter therapeutics, Boehringer Ingelheim, Improved Patient Outcomes, Merck, NHLBI, Novo Nordisk, Otsuka, Sanofi, VA. He also provides consulting services for Abbott, Novartis, Sanofi, Vidya, Walmart, Webmed. He is also on the board of directors of Preventric Diagnostics. LLZ reports research funding awarded to her institution from the PhRMA Foundation and Proteus Digital Health, as well as consulting for Pfizer and Novartis, all unrelated to the current work.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Reasonable requests for data will be responded to in accordance to current Department of Veteran Affairs policy.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Durham VA Health Care System IRB #02312. Participants gave informed consent to participate in the study before taking part.
References
- 1.Elliott T, Tong I, Sheridan A, et al. Beyond convenience: patients' perceptions of physician Interactional skills and compassion via telemedicine. Mayo Clin Proc Innov Qual Outcomes 2020;4:305–14. 10.1016/j.mayocpiqo.2020.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Medicare & Medicaid Services . Medicare telemedicine health care provider fact sheet, 2021. Available: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet [Accessed 12 Mar 2021].
- 3.Lewinski AA, Sullivan C, Allen KD, et al. Accelerating implementation of virtual care in an integrated health care system: future research and operations priorities. J Gen Intern Med 2021;36:2434–42. 10.1007/s11606-020-06517-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pagán VM, McClung KS, Peden CJ. An observational study of disparities in telemedicine utilization in primary care patients before and during the COVID-19 pandemic. Telemed J E Health 2021. 10.1089/tmj.2021.0412. [Epub ahead of print: 20 Dec 2021]. [DOI] [PubMed] [Google Scholar]
- 5.Poeran J, Cho LD, Wilson L, et al. Pre-existing disparities and potential implications for the rapid expansion of telemedicine in response to the coronavirus disease 2019 pandemic. Med Care 2021;59): :694–8. 10.1097/MLR.0000000000001585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lam K, Lu AD, Shi Y, et al. Assessing telemedicine Unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern Med 2020;180:1389–91. 10.1001/jamainternmed.2020.2671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roberts ET, Mehrotra A. Assessment of disparities in digital access among Medicare beneficiaries and implications for telemedicine. JAMA Intern Med 2020;180:1386–9. 10.1001/jamainternmed.2020.2666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferguson JM, Jacobs J, Yefimova M, et al. Virtual care expansion in the Veterans health administration during the COVID-19 pandemic: clinical services and patient characteristics associated with utilization. J Am Med Inform Assoc 2021;28:453–62. 10.1093/jamia/ocaa284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luo J, Tong L, Crotty BH, et al. Telemedicine adoption during the COVID-19 pandemic: gaps and inequalities. Appl Clin Inform 2021;12:836–44. 10.1055/s-0041-1733848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodriguez JA, Betancourt JR, Sequist TD, et al. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care 2021;27:21–6. 10.37765/ajmc.2021.88573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hilbert M. The end justifies the definition: the manifold outlooks on the digital divide and their practical usefulness for policy-making. Telecomm Policy 2011;35:715–36. 10.1016/j.telpol.2011.06.012 [DOI] [Google Scholar]
- 12.Pew Research Center . Internet/Broadband fact sheet, 2021. Available: https://www.pewresearch.org/internet/fact-sheet/internet-broadband/ [Accessed 12 Mar 2021].
- 13.Pierce RP, Stevermer JJ. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare 2020;1357633:x20963893. 10.1177/1357633X20963893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 15.Fortney JC, Burgess JF, Bosworth HB, et al. A re-conceptualization of access for 21st century healthcare. J Gen Intern Med 2011;26 Suppl 2:639–47. 10.1007/s11606-011-1806-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Department of Veteran Affairs . Rural veterans, 2021. Available: https://www.ruralhealth.va.gov/aboutus/ruralvets.asp [Accessed 12 Mar 2021].
- 17.Administration VHManagement OoE, ed. COVID-19 Response Plan, 2020. [Google Scholar]
- 18.Heher YK, Chen Y. Process mapping: a cornerstone of quality improvement. Cancer Cytopathol 2017;125:887–90. 10.1002/cncy.21946 [DOI] [PubMed] [Google Scholar]
- 19.Lewinski AA, Crowley MJ, Miller C, et al. Applied rapid qualitative analysis to develop a Contextually appropriate intervention and increase the likelihood of uptake. Med Care 2021;59:S242–51. 10.1097/MLR.0000000000001553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lewinski AA, Shapiro A, Bosworth HB, et al. Veterans' interpretation of diabetes distress in diabetes self-management: findings from cognitive interviews. Sci Diabetes Self Manag Care 2021;47:391–403. 10.1177/26350106211043487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nevedal AL, Reardon CM, Opra Widerquist MA, et al. Rapid versus traditional qualitative analysis using the consolidated framework for implementation research (CFIR). Implement Sci 2021;16:67. 10.1186/s13012-021-01111-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patton M. Qualitative research & evaluation methods: Integrating theory and practice. Safe Publications, 2014. [Google Scholar]
- 23.Proposal for clinical algorithm standards. Society for medical decision making Committee on standardization of clinical algorithms. Med Decis Making 1992;12:149–54. [PubMed] [Google Scholar]
- 24.Barkai G, Gadot M, Amir H, et al. Patient and clinician experience with a rapidly implemented large-scale video consultation program during COVID-19. Int J Qual Health Care 2021;33. 10.1093/intqhc/mzaa165. [Epub ahead of print: 20 Feb 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barsom EZ, Meijer HAW, Blom J, et al. Emergency upscaling of video consultation during the COVID-19 pandemic: contrasting user experience with data insights from the electronic health record in a large academic Hospital. Int J Med Inform 2021;150:104463. 10.1016/j.ijmedinf.2021.104463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heyworth L, Kirsh S, Zulman D. Expanding Access through Virtual Care: The VA’s Early Experience with Covid-19. N Engl J Med 2020. [Google Scholar]
- 27.Croymans D, Hurst I, Han M. Telehealth: the right care, at the right time, via the right medium. NEJM, 2020. [Google Scholar]
- 28.Bhatt AB. A hybrid model of In-person and telemedicine visits facilitates longitudinal care delivery, 2021. Available: https://advances.massgeneral.org/cardiovascular/article.aspx?id=1334 [Accessed June 6, 2022].
- 29.Victorian Government, . Telehealth decision tool, 2020. Available: https://www.safercare.vic.gov.au/sites/default/files/2020-11/Telehealth%20decision%20tool.pdf [Accessed 06 Jun 2022].
- 30.Lopez AM, Lam K, Thota R. Barriers and facilitators to telemedicine: can you hear me now? Am Soc Clin Oncol Educ Book 2021;41:25–36. 10.1200/EDBK_320827 [DOI] [PubMed] [Google Scholar]
- 31.Gordon HS, Solanki P, Bokhour BG, et al. "I'm Not Feeling Like I'm Part of the Conversation" Patients' Perspectives on Communicating in Clinical Video Telehealth Visits. J Gen Intern Med 2020;35:1751–8. 10.1007/s11606-020-05673-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ramaswamy A, Yu M, Drangsholt S, et al. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective Cohort study. J Med Internet Res 2020;22:e20786. 10.2196/20786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gomez T, Anaya YB, Shih KJ, et al. A qualitative study of primary care physicians' experiences with telemedicine during COVID-19. J Am Board Fam Med 2021;34:S61–70. 10.3122/jabfm.2021.S1.200517 [DOI] [PubMed] [Google Scholar]
- 34.Srinivasan M, Asch S, Vilendrer S, et al. Qualitative assessment of rapid system transformation to primary care video visits at an academic medical center. Ann Intern Med 2020;173:527–35. 10.7326/M20-1814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Presley C HA, Warnick J. Diabetes SIG how to prepare for your telemedicine appointment; 2021.
- 36.Gerber MR, Elisseou S, Sager ZS, et al. Trauma-Informed telehealth in the COVID-19 era and beyond. Fed Pract 2020;37:302–8. 10.12788/fp.0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alkureishi MA, Choo Z-Y, Lenti G, et al. Clinician perspectives on telemedicine: observational cross-sectional study. JMIR Hum Factors 2021;8:e29690. 10.2196/29690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hausmann LRM, Kressin NR, Hanusa BH, et al. Perceived racial discrimination in health care and its association with patients' healthcare experiences: does the measure matter? Ethn Dis 2010;20:40–7. [PubMed] [Google Scholar]
- 39.Williams DR, Yan Yu, Jackson JS, et al. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol 1997;2:335–51. 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- 40.Morgan DG, Kosteniuk J, Stewart N, et al. The telehealth satisfaction scale: reliability, validity, and satisfaction with telehealth in a rural memory clinic population. Telemed J E Health 2014;20:997–1003. 10.1089/tmj.2014.0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-062261supp001.pdf (55.7KB, pdf)
Data Availability Statement
Data are available on reasonable request. Reasonable requests for data will be responded to in accordance to current Department of Veteran Affairs policy.