Abstract
Aim
Individual-level COVID-19 vaccination and related preventive health behaviors is politically polarized in the United States. We examined whether the current polarization in COVID-19 health behavior may be explained by differences in trust in healthcare, locus of control, or insurance status.
Subject and methods
Our sample includes 553 US adults recruited on Amazon MTurk. We assessed odds ratios of currently vaccinated, or willing to be vaccinated if unvaccinated using logistic regression. We assessed count of routine changes and positive attitudes toward facemasks using negative binomial regression.
Results
Trust in healthcare was found to be an important determinant of all COVID-19 related health behavior measured in our study. Further, the effects on COVID-related attitudes/behavior from trust in healthcare are large in magnitude. For instance, our results suggest that individuals at or above the upper quartile of trust in healthcare are around 20 percentage points more likely to be vaccinated than those at or below the lower quartile. Further, we find that the effect of trust in healthcare on adherence or endorsement of COVID-19 mitigation strategies is distinct from political affiliation, i.e., the effect on COVID-19 related health behavior is independent of the polarization across political party lines. Locus of control was not associated with adherence/attitude toward COVID-19 mitigation strategies. Insurance status was only found to be positively associated with odds of being vaccinated.
Conclusion
Our study highlights the importance of increasing trust in healthcare as a means to protect public health in the wake of major public health crises.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10389-022-01737-9.
Keywords: Pandemic, COVID-19, Trust in healthcare, Vaccine, Mask wearing
Introduction
It is well established that compliance toward COVID-19 related policies in the United States (US) has varied throughout the pandemic due to several different factors. Aspects such as demographic characteristics, as well as political affiliation, insurance status, and trust in healthcare have all been identified as possible elements influencing adherence to pandemic mitigation strategies (Gerace et al. 2022; Conway et al. 2021). Additionally, due to measures to prevent the spread of COVID-19, there were disruptions to daily routines, including increased time spent outside, and adjustment to other health behaviors, such as masking and vaccinations (see Hou et al. 2020; Lades et al. 2020; Lai et al. 2021). This study proposes the use of Cockerham’s (2005) theory of health lifestyle to better understand health practices during the COVID-19 pandemic and assess factors shaping individual compliance to COVID-19 health recommendations.
Health lifestyles framework
The health lifestyle framework posits that individual health behavior is shaped by social structural factors (e.g., age, gender, race/ethnicity, and social collectives [groups of people linked through relationships, such as politics]) that influence collective “health lifestyles.” Health lifestyles are collective patterns of health-related behavior, contingent on the health options available (Cockerham 2005). Specifically, individual health behavior (and our impetus to act on our health) is actually a function of lifestyle. Which health lifestyle we adopt is shaped by social structural factors that pattern cultural norms, values, and life opportunities, influencing what health options seem viable or available to us (Cockerham 2005). For example, medical insurance status has previously been found to affect COVID-19 vaccinations, whereby those without health insurance are less likely to get vaccinated (Nguyen et al. 2021). While COVID-19 vaccinations were advertised as “free,” individuals without insurance may, from a health lifestyle perspective, avoid healthcare as a general pattern of their health behavior shaped by perceived cost or concern of “hidden costs.” That is, we can follow how class status influences insurance status which then affects healthcare utilization. Figure 1 provides an overview of our overarching conceptual model of health lifestyles and COVID-19 compliance behavior, which we will detail in the following paragraphs.
Fig. 1.

Conceptual model and key variables
Social structure and COVID-19 behavior
Social structural factors, such as class circumstances, age, gender/sexuality, and race/ethnicity, are important features shaping our health lifestyles. Older adults and younger people have distinct types of lifestyles, such as the ways we socialize, and which types of health behaviors are prioritized. For example, several studies have noted a correlation between age and COVID-19 behavior, with older adults being more likely to receive vaccination, use masks, and engage in hygiene behaviors such as handwashing (Myerson et al. 2021; Milad and Bogg 2021; Painter et al. 2021). In addition, gender, race/ethnicity, and socioeconomic status has been linked to variation in changes to daily routines and compliance with social isolation during the pandemic (Lucchini et al. 2021; Navas-Martín et al. 2021). While not a major focus of our study, it is important to consider sociodemographic characteristics (such as income, education, gender, etc.) that represent key social structural dynamics affecting COVID-19 related health behavior (Myerson et al. 2021; Milad and Bogg 2021).
Opportunities and collectives
Our social conditions pattern our opportunities, thereby shaping downstream behavior. In the case of health behavior, one major opportunity for healthcare access is insurance. As stated above, insurance status has been found to predict COVID-19 vaccination rates; however, whether it has a role in other forms of behavior has been largely unexamined, such as changes to daily routines. In addition, health status may also function to shape “opportunities” to engage in specific health behaviors, such as mask wearing (Cordero 2022), and full-time employment may shape people’s ability to socially distance or their opportunity to alter their daily routines (Coroiu et al. 2020).
Our social conditions also shape our “collectives,” or what social networks and group membership we may align with, thus shaping the types of health lifestyles in which we participate. For example, marital status may influence people’s health lifestyles due to the unique aspects of the marriage social network; married couples may socialize differently, and enact some social control on spouses, affecting their likelihood of engaging in COVID-19 related social distancing or vaccination (Nofal et al. 2020; Scott et al. 2021).
Political affiliation, while broad, is a social collection shaping our health behavior, and has been a primary focus of existing COVID-19 compliance studies. In terms of COVID-19 related health behaviors, it appears that in the United States responses have become highly politically polarized. For instance, several studies have found that rates of vaccination are divided along political lines and shaped by political ideology; Allington et al. (2021) found that those who voted for Hilary Clinton in the 2016 election had greater intention for vaccination relative to those who voted for Donald Trump. In addition, seeing vaccine endorsement from leaders from one’s own political party (e.g., Republicans who viewed vaccine endorsement from Donald Trump) increased vaccine intention; however, Republicans who viewed vaccine endorsement from Democrats were less likely to report vaccine intention, illustrating its complex politicization (Allington et al. 2021; Travis et al. 2021). In general, research suggests that Democratic leadership has been more likely to endorse vaccination and vaccine mandates, and individuals whose political affiliation is Democrat had higher rates of vaccination or vaccine intentions relative to those affiliated as Republican or politically independent (Callow and Callow 2021; Cowan et al. 2021; Fridman et al. 2021; Sharma et al. 2021). Similarly, those identifying as Republican were also more likely to support easing COVID-19 restrictions (Gerace et al. 2022).
In addition to the research on political affiliation and vaccination, given the often heated debate over wearing masks and their potential influence, researchers have examined the relationship between politics and mask attitudes and behaviors. While various samples and methods have been used to examine this relationship, differences in attitudes and behavior have been found based along political party (e.g, Democrats vs. Republicans) and political ideological (e.g., liberal vs. conservative) lines. For example, Mallinas et al. (2021) found that conservatives and younger people were more likely to oppose mask use and hold negative opinions of masks compared with liberals and older individuals. Similarly, a recent Pew study reported that liberals were more likely to support mask use, and wear masks, than conservatives (Doherty et al. 2020; Stosic et al. 2021).
A smaller number of studies have attempted to examine how politicization influences social distancing, and thus changes to daily routines more broadly. Specifically, liberals have been found to socially distance, and think that COVID-19 is a serious health issue (Xu and Cheng 2021). Political ideology has also been linked both directly and indirectly to the belief that COVID-19 is exaggerated and that masks are ineffective (Taylor and Asmundson 2021). Overall, currently available research suggests that political ideology or affiliation does correlate with several dimensions of COVID-19 mitigation compliance.
Beliefs and attitudes
Medical trust may also matter for compliance with COVID-19 mitigation efforts. It has been argued that the healthcare system can affect health behavior only if the system (ranging from nurses and physicians to medical scientists) is trusted (Lalumera 2018). Along these lines, a meta-analysis showed that trust in healthcare (moderately) correlated with both health behavior and health outcomes (Birkhäuer et al. 2017). Hence, trust in healthcare might be an important predictor of COVID-19 related health behaviors. Trust in healthcare institutions has steadily declined during the latter half of the 20th century. Blendon et al. (2014) reported that in 1966, 73% of US respondents showed great confidence in leaders of the medical profession, while the corresponding share in 2012 was down to 34%. That said, the current pandemic seems to have restored some of the trust in healthcare. A Gallup poll in 2020 illustrated an overall increase in trust from 36% pre-pandemic to 51% in July 2020 (Brenan 2020). While this trend during the pandemic is encouraging, a large proportion of Americans remain distrusting of the healthcare system. Moreover, emerging research suggests important heterogeneity in distrust—for certain sub-groups of the population, the COVID-19 pandemic may even have exacerbated distrust in healthcare and government agencies more broadly (Baker 2020).
Importantly, distrust in the healthcare system may correlate with distrust in certain public health strategies such as vaccines (Gilson 2003; Graham et al. 2013); general vaccine hesitancy was a challenge prior to the COVID-19 pandemic (MacDonald 2015). Individuals are unlikely to receive vaccinations if they perceive the disease as non-serious, a notable challenge for the uptake of flu vaccines (Guidry et al. 2020). The spread of COVID-19 conspiracies (e.g., that COVID-19 is less serious than governmental agencies portray) and distrust in health recommendations have been a barrier to controlling COVID-19—misinformation increases vaccine hesitancy and increases non-adherence with other COVID-19-related recommended health behaviors (Earnshaw et al. 2020; Romer and Jamieson 2020).
Impetus to act
Our attitudes and beliefs shape our overall impetus to act. Locus of control is a concept that can help us understand differing levels of personal motivation to act; people with a higher internal locus of control believe that they are responsible for what happens in their lives, while those with an external locus of control believe that external forces, such as luck, determine their life outcomes (Lefcourt 2013). While an arguably complex construct, there is some evidence that people with higher internal locus of control have better health and lower healthcare utilization, and that health-related internal locus of control is associated with higher vaccine compliance (Aharon et al. 2018; Kesavayuth et al. 2020). Previous studies find that Republicans have higher internal health-related locus of control relative to Democrats, which could mitigate the polarization of COVID-19 related health behaviors across party affiliation. That said, there is some evidence that Republicans overall are less likely to engage in health promoting behaviors (Kannan and Veazie 2018). It is therefore unclear whether locus of control is factoring into the COVID-19-related health behaviors or beliefs of individuals within the US context.
Current study
The current study applies a health lifestyle framework to better understand health behavior and attitudes related to COVID-19 compliance in the United States. We focus on elucidating the unique effects of a variety of factors, including the collectives and opportunities that shape our daily lives (such as political affiliation), specific attitudes and beliefs (in this case, level of trust in medicine) and unique impetus to act (measured by locus of control), to explain differing actions around COVID-19 mitigation. Few public health studies of compliance with COVID-19 pandemic mitigation efforts have examined multiple COVID-19 health behavior outcomes simultaneously, nor treated broad changes to individuals’ daily routines as an aspect of COVID-19 health behavior (rather a side effect of the pandemic) (Hou et al. 2020; Lai et al. 2021). Thus, we examine the following COVID-19-related health behaviors: vaccination status, willingness to be vaccinated (if currently unvaccinated), changes in routine during COVID-19, and face masking attitudes, furthering our understanding of factors influencing individuals’ adherence to pandemic mitigation strategies.
Method
Procedure
The Amazon Mechanical Turk (MTurk) online platform was utilized to collect data for the current study. MTurk pays workers to complete a task, commonly an online survey. MTurk allows for access to participants nationwide and has been increasingly used to collect data among a diverse population on a wide range of topics (Aguinis et al. 2021; Burton et al. 2020; Cullen et al. 2021; Fendrich et al. 2021; Hauser and Schwarz 2016). Respondents completed an anonymous online survey (via Qualtrics) during the end of April and early May of 2021. Participants were paid a small incentive for completion. All participants were provided informed consent at the beginning of the survey, were 18 years or older, lived in the United States, and were informed they could cease participation at any time. The Institutional Review Board at the authors’ institution approved the project. The survey took approximately 15 minutes to complete, and participants had to successfully complete an attention check question and captcha to ensure data quality.
Measures
Outcomes
Vaccination status is a single item dummy variable measuring those who report having received at least one dose of any COVID-19 vaccine (1), to those who are unvaccinated (0). Willingness to be Vaccinated is a single item measure that compares those who report that they are willing to receive a COVID-19 vaccine (1), to those who are unwilling to be vaccinated (0).
Attitudes about Masks was measured using a shortened scale on mask attitudes adapted from Taylor and Asmundson’s (2021) scale and consists of 15 survey items (refer to Appendix A for the full list of items) (alpha = 0.91 within our sample). The scale includes dimensions that evaluate agreement with statements, ranging from strongly agree (4) to strongly disagree (1), about the perceived efficacy and the necessity of wearing masks and includes items such as “masks are effective,” “safety precautions like wearing masks are necessary,” and “it is difficult to breathe when wearing a facemask” (reverse coded) with possible scores ranging from 15–60. Higher scores indicate more positive attitudes or endorsement of wearing facemasks.
Changes in Routines is a composite score created from 9-items (see Appendix A) and focuses on key categories of routine changes identified in other studies (see Lucchini et al. 2021). Example items include “I have socialized with friends less,” “I have seen my extended family less,” and “I have spent time outside less” (alpha = 0.82 within our sample) with possible scores ranging from 9–45. Higher scores indicate greater perceived changes in routines since the start of the COVID-19 pandemic (past 12 months).
Primary independent variables
Trust in Healthcare is a composite score created from 4-items (see Appendix A) with possible scores ranging from 4–16. Higher scores indicate higher trust in healthcare/medicine. Items were adapted from existing studies on trust in health systems (Egede and Ellis 2008), and focus on dimensions of fiduciary responsibility, and competency. Example items include “Your doctors want to give you the best care possible” and “You trust your local hospitals to give you the best care they can provide” (alpha = 0.89 within our sample). We also created quartiles based on trust in healthcare score (Trust in Healthcare Quartiles) (Quartile 1= <=11, Quartile 2= 12, Quartile 3= 13–14, Quartile 4= 15+) to assess the magnitude of relationship between trust and key outcomes.
Locus of Control was measured using a 6-item Locus of Control Scale (validated elsewhere; see Lumpkin 1985). Example items include “In my life, good luck is more important than hard work for success” and “I do not have enough control over the direction my life is taking” (alpha = 0.84 within our sample) (see Appendix A), with possible scores ranging from 6–24. Higher scores indicate higher internal locus of control (versus external locus of control). Higher internal locus of control illustrates a perceived sense of having control over the outcomes in their lives, versus higher external locus of control that corresponds to a perceived lack of control over outcomes in their lives.
We also examine insurance status, which is a single item dummy measure that compares those who specify having private or public health insurance to those who (insured (1) vs. not insured (0)) report having no health insurance, and self-rated health, a single item ordinal measure (range = 1–4; higher scores = worse self-rated health).
Political affiliation is a single item categorical variable with three different categories: Democrats (0), Republicans (1), and individuals who identified as politically independent or of having no political affiliation (hereafter referred to as “Independents”) (2). A small number (n = 4) of survey participants stated another political affiliation, and those individuals were included as Independents.
Sociodemographic covariates
Analyses also adjust for age (in years), gender and sexuality (compares cisgender and heterosexual men to cisgender and heterosexual women, and LGBTQ+ identifying respondents, marital status (currently married vs. not currently married), race (White (reference), Black, Asian, Indigenous/other), ethnicity (Latino/a/Hispanic (1) vs Non-Latino/a/Hispanic (0)), employment (reference = full-time employed), income (ordinal categories ranging from 1= Less than $10,000 annually to 8= Over $120,001 annually), and education (ordinal categories ranging from 1= Less than high school degree to 8= Graduate degree). All demographics are single item measures.
Analytic approach
Table 1 includes descriptive statistics for the total sample and stratified by Democrats and Republicans. The final column compares those that were Independent to Democrats. Next, two binary logistic regressions were estimated, given our vaccine outcomes were coded as dummy variables, to examine factors that may influence vaccination. Table 2 reports the estimated factors that may influence already being vaccinated, while Table 3 outlines the estimated factors that may influence willingness to get vaccinated. We than estimated predicted probabilities of having received the COVID-19 vaccine, and willing to be vaccinated, by trust in healthcare quartile using post-estimation of margins at means (Fig. 2). We treat the outcomes attitudes toward masks (Table 4) and changes in routines (Table 5) as “count” variables and used negative binomial regression to assess “counts” of endorsements of these scales.
Table 1.
Descriptive statistics stratified by political affiliation (Democrats = reference)
| Everyone (N = 553) | Democrats (reference) (N = 278) | Republicans (N = 122) | Independents (N = 153) | |||||||
| N | % | N | % | N | % | p-value | N | % | p-value | |
| Gender and sexuality | ||||||||||
| Cishet men | 266 | 48.1 | 124 | 44.6 | 55 | 45.1 | 87 | 56.9 | ||
| Cishet women | 221 | 40.0 | 108 | 38.9 | 63 | 51.6 | 50 | 32.7 | ||
| LGBTQ+ | 66 | 11.9 | 46 | 16.6 | 4 | 3.3 | 0.001 | 16 | 10.5 | 0.04d |
| Ethnicity | ||||||||||
| Non-Hispanic | 524 | 94.8 | 257 | 92.5 | 115 | 94.3 | 152 | 99.4 | ||
| Hispanic | 29 | 5.2 | 21 | 7.6 | 7 | 5.7 | 0.52 | 1 | 0.7 | 0.002 |
| Race | ||||||||||
| White | 449 | 81.2 | 217 | 78.1 | 109 | 89.3 | 123 | 80.4 | ||
| Black | 49 | 8.9 | 31 | 11.2 | 5 | 4.1 | 13 | 8.5 | ||
| Asian | 41 | 7.4 | 21 | 7.6 | 7 | 5.7 | 13 | 8.5 | ||
| Indigenous/other | 14 | 2.5 | 9 | 3.2 | 1 | 1.0 | 0.39 | 4 | 2.6 | 0.8 |
| Insured | 466 | 84.3 | 245 | 88.1 | 101 | 82.8 | 0.15 | 120 | 78.4 | 0.007 |
| Married | 276 | 49.9 | 120 | 43.2 | 77 | 63.1 | <0.001 | 79 | 51.6 | 0.09 |
| Employment | ||||||||||
| Fulltime | 369 | 66.7 | 190 | 68.4 | 80 | 65.6 | 99 | 64.7 | ||
| Parttime | 83 | 15.0 | 40 | 14.4 | 19 | 15.6 | 24 | 15.7 | ||
| Unemployed | 46 | 8.3 | 21 | 7.6 | 11 | 9.0 | 14 | 9.2 | ||
| Retired | 32 | 5.8 | 14 | 5.0 | 8 | 6.6 | 11 | 7.2 | ||
| Other | 23 | 4.2 | 13 | 4.7 | 4 | 3.3 | 0.82 | 5 | 3.3 | 0.66 |
| Vaccine status | ||||||||||
| Vaccinated | 273 | 49.4 | 159 | 57.2 | 49 | 40.2 | 65 | 42.5 | ||
| Unvaccinated | 280 | 50.6 | 199 | 42.8 | 73 | 59.8 | 0.002 | 88 | 57.5 | 0.003 |
| Willing to be vaccinateda | 176 | 62.9 | 94 | 79.0 | 35 | 48.0 | <0.001 | 47 | 53.4 | <0.001 |
| Everyone (N = 553) | Democrats (reference) (N = 278) | Republicans (N = 122) | Independents (N = 153) | |||||||
| mean | sd | mean | sd | mean | sd | p-value | mean | sd | p-value | |
| Age (r = 18–73) | 41.4 | 12.4 | 39.8 | 11.5 | 44.5 | 13.3 | <0.001 | 41.9 | 12.5 | 0.09 |
| Income (r = 1–8) | 4.4 | 1.9 | 4.3 | 1.9 | 4.5 | 1.9 | 0.18 | 4.5 | 2.0 | 0.18 |
| Education (r = 1–6) | 4.4 | 1.3 | 4.5 | 1.2 | 4.4 | 1.3 | 0.41 | 4.2 | 1.4 | 0.02 |
| Trust in healthcare (r = 4–16) | 12.6 | 2.4 | 12.8 | 2.2 | 12.9 | 2.5 | 0.92 | 12.0 | 2.7 | 0.001 |
| Locus of controlb (r = 6–24) | 17.6 | 5.5 | 17.3 | 3.6 | 18.7 | 3.4 | <0.001 | 17.3 | 3.5 | 0.90 |
| General health (r = 1–5) | 2.4 | 1.0 | 2.4 | 0.9 | 2.3 | 1.0 | 0.17 | 2.5 | 1.0 | 0.82 |
| Mask attitudes (r = 16–60) | 46.0 | 9.3 | 49.7 | 6.2 | 40.2 | 10.0 | <0.001 | 44.0 | 10.4 | <0.001 |
| COVID routinesc (r = 9–45) | 35.0 | 6.4 | 36.5 | 5.3 | 33.7 | 7.0 | <0.001 | 33.3 | 7.2 | <0.001 |
Data are from a pandemic survey administered on Amazon MTURK between April–May, 2021. Proportion differences tested using chi-squared, and differences in means tested using two-tailed independent sample t-tests (reference = Democrats).
aproportion reflects those unvaccinated, willing to be vaccinated
bHigher scores indicate higher internal locus of control
cHigher scores indicated more self-reported change in routines due to COVID-19
dComparison p-values are uncorrected for repeated comparisons (e.g., Democrats vs. Republicans, Democrats vs. Independents). However, only the difference in Gender and Sexuality between Democrats and Independents may be non-significant after correction using the Bonferroni approach.
sd, standard deviation, r, range, cishet, cisgender and heterosexual
Table 2.
Logistic regression of being vaccinated, odds ratios reported
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Gender and sexualitya | OR (robust se) | sig | OR (robust se) | sig |
| Cishet women | 0.95 (0.19) | 0.99 (0.21) | ||
| LGBTQ | 1.09 (0.34) | 1.27 (0.41) | ||
| Hispanic | 1.89 (0.52) | * | 1.88 (0.47) | * |
| Raceb | ||||
| Black | 0.81 (0.21) | 0.87 (0.23) | ||
| Asian | 0.96 (0.41) | 1.03 (0.44) | ||
| Indigenous/other | 0.90 (0.44) | 1.08 (0.56) | ||
| Political affiliationc | ||||
| Republican | 0.40 (0.10) | *** | 0.42 (0.11) | *** |
| Independent | 0.50 (0.15) | * | 0.60 (0.18) | |
| Employmentd | ||||
| Parttime | 1.12 (0.32) | 1.14 (0.36) | ||
| Unemployed | 1.83 (0.48) | * | 2.25 (0.68) | ** |
| Retired | 3.37 (1.73) | * | 2.84 (1.47) | * |
| Other | 1.02 (0.52) | 1.09 (0.66) | ||
| Married | 0.93 (0.21) | 0.85 (0.21) | ||
| Age | 1.03 (0.01) | ** | 1.02 (0.01) | * |
| Income | 1.23 (0.06) | *** | 1.19 (0.08) | *** |
| Education | 1.21 (0.11) | * | 1.21 (0.10) | * |
| Insured | 2.00 (0.60) | * | ||
| Trust in healthcare | 1.16 (0.04) | *** | ||
| Locus of control | 1.01 (0.02) | |||
| General health | 1.18 (0.14) | |||
| Constant | 0.08 (0.06) | *** | 0.00 (0.00) | *** |
| Pseudo R-squared | 0.09 | 0.12 | ||
| N | 553 | 553 | ||
Data are from a pandemic survey administered on Amazon MTURK between April-May, 2021. Results are clustered by state (n = 48). OR, odds ratio, se, standard error, cishet, cisgender and heterosexual, sig, significance
aReference is cisgender, heterosexual men
bReference is White
cReference is Democrat
dReference is employed fulltime
*p < 0.05, **p < 0.01, ***p < 0.001
Table 3.
Logistic regression of willing to be vaccinated, odds ratios reported
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Gender and sexualitya | OR (robust se) | sig | OR (robust se) | sig |
| Cishet women | 0.51 (0.19) | 0.54 (0.20) | ||
| LGBTQ | 1.28 (0.67) | 1.73 (0.95) | ||
| Hispanic | 0.54 (0.32) | 0.49 (0.30) | ||
| Raceb | ||||
| Black | 0.80 (0.47) | 0.92 (0.58) | ||
| Asian | 2.00 (1.48) | 2.22 (1.84) | ||
| Indigenous/other | 0.64 (0.36) | 0.77 (0.55) | ||
| Political affiliationc | ||||
| Republican | 0.25 (0.09) | *** | 0.29 (0.10) | *** |
| Independent | 0.28 (0.10) | *** | 0.34 (0.14) | ** |
| Employmentd | ||||
| Parttime | 0.75 (0.31) | 0.60 (0.27) | ||
| Unemployed | 1.06 (0.66) | 1.19 (0.90) | ||
| Retired | 0.23 (0.13) | * | 0.16 (0.08) | *** |
| Other | 3.31 (3.07) | 3.93 (3.71) | ||
| Married | 0.62 (0.20) | 0.63 (0.21) | ||
| Age | 1.02 (0.01) | * | 1.03 (0.01) | * |
| Income | 1.15 (0.08) | 1.12 (0.09) | ||
| Education | 1.12 (0.14) | 1.10 (0.14) | ||
| Insured | 0.83 (0.27) | |||
| Trust in healthcare | 1.27 (0.08) | *** | ||
| Locus of control | 0.93 (0.02) | |||
| General health | 0.91 (0.16) | |||
| Constant | 0.93 (0.59) | 0.37 (0.44) | ||
| Pseudo R-squared | 0.12 | 0.17 | ||
| N | 280 | 280 | ||
Data are from a pandemic survey administered on Amazon MTURK between April–May, 2021. Results are clustered by state (n = 48). OR, odds ratio, se, standard error, cishet, cisgender and heterosexual, sig, significance
aReference is cisgender, heterosexual men
bReference is White
cReference is Democrat
dReference is employed fulltime
*p < 0.05, **p < 0.01, ***p < 0.001
Fig. 2.
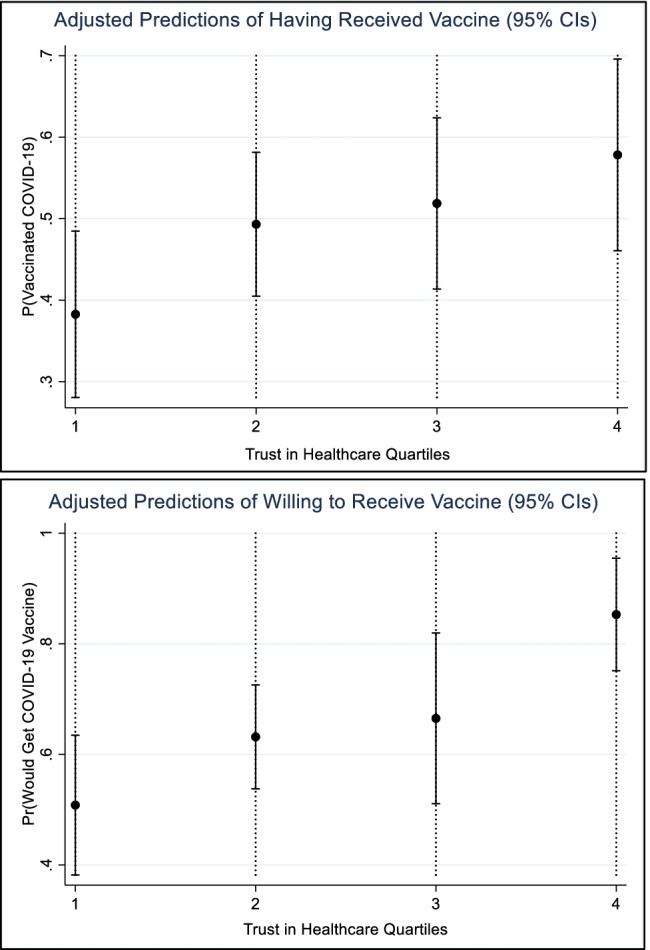
Predicted probability of being vaccinated (top) or would receive COVID-19 vaccine (bottom), adjusted for covariates (at means). Figure created using Stata 15.1 post logistic regression estimation command “margins.” Adjusts for age, gender and sexuality, race, ethnicity, education level, income level, employment status, married, political affiliation, insured, self-rated health, and locus of control
Table 4.
Negative binomial regression of mask attitudes
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Gender and sexualitya | coef (robust se) | sig | coef (robust se) | sig |
| Cishet women | 0.01 (0.01) | 0.02 (0.01) | ||
| LGBTQ | 0.00 (0.02) | 0.03 (0.02) | ||
| Hispanic | 0.03 (0.03) | 0.04 (0.02) | ||
| Raceb | ||||
| Black | –0.00 (0.03) | –0.00 (0.03) | ||
| Asian | –0.00 (0.02) | –0.00 (0.03) | ||
| Indigenous/other | –0.13 (0.06) | * | –0.11 (0.06) | * |
| Political affiliationc | ||||
| Republican | –0.21 (0.02) | *** | –0.21 0.02) | *** |
| Independent | –0.12 (0.02) | *** | –0.09 (0.02) | *** |
| Employmentd | ||||
| Parttime | –0.00 (0.01) | –0.00 (0.01) | ||
| Unemployed | –0.01 (0.03) | –0.01 (0.04) | ||
| Retired | 0.04 (0.04) | 0.03 (0.05) | ||
| Other | 0.03 (0.03) | 0.03 (0.03) | ||
| Married | –0.01 (0.02) | –0.01 (0.02) | ||
| Age | –0.00 (0.00) | –0.00 (0.00) | ||
| Income | 0.01 (0.01) | 0.01 (0.00) | ||
| Education | 0.01 (0.01) | 0.01 (0.01) | ||
| Insured | 0.02 (0.02) | |||
| Trust in healthcare | 0.02 (0.00) | *** | ||
| Locus of control | 0.00 (0.00) | |||
| General health | 0.02 (0.01) | |||
| Constant | 3.85 (0.03) | *** | 3.46 (0.08) | *** |
| Pseudo-R squared | 0.03 | 0.04 | ||
| N | 553 | 553 | ||
Data are from a pandemic survey administered on Amazon MTURK between April–May, 2021. Results are clustered by state (n = 48). coef, coefficient, se, standard error, cishet, cisgender and heterosexual, sig, significance
aReference is cisgender, heterosexual men
bReference is White
cReference is Democrat
dReference is employed fulltime
*p < 0.05, **p < 0.01, ***p < 0.001
Table 5.
Negative binomial regression of changes in routines
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Gender and sexualitya | coef (robust se) | sig | coef (robust se) | sig |
| Cishet women | 0.02 (0.01) | 0.02 (0.01) | ||
| LGBTQ | 0.00 (0.02) | 0.01 (0.02) | ||
| Non-Hispanic | 0.03 (0.04) | 0.03 (0.04) | ||
| Raceb | ||||
| Black | 0.02 (0.02) | 0.03 (0.02) | ||
| Asian | 0.03 (0.04) | 0.03 (0.03) | ||
| Indigenous/other | –0.04 (0.05) | –0.02 (0.05) | ||
| Political affiliationc | ||||
| Republican | –0.07 (0.02) | *** | –0.06 (0.02) | *** |
| Independent | –0.08 (0.02) | *** | –0.07 (0.02) | *** |
| Employmentd | ||||
| Parttime | –0.00 (0.01) | –0.01 (0.02) | ||
| Unemployed | –0.10 (0.04) | –0.10 (0.04) | * | |
| Retired | –0.02 (0.05) | –0.03 (0.04) | ||
| Other | –0.01 (0.04) | –0.03 (0.05) | ||
| Married | –0.03 (0.02) | –0.03 (0.02) | ||
| Age | –0.00 (0.00) | –0.00 (0.00) | ||
| Income | 0.01 (0.00) | * | 0.01 (0.00) | |
| Education | 0.00 (0.01) | 0.00 (0.01) | ||
| Insured | 0.02 (0.02) | |||
| Trust in healthcare | 0.01 (0.00) | ** | ||
| Locus of control | –0.00 (0.00) | |||
| General health | 0.02 (0.01) | ** | ||
| Constant | 3.56 (0.05) | *** | 3.38 (0.09) | *** |
| Pseudo R-squared | 0.02 | 0.02 | ||
| N | 553 | 553 | ||
Data are from a pandemic survey administered on Amazon MTURK between April–May, 2021. Results are clustered by state (n = 48). coef, coefficient, se, standard error, cishet, cisgender and heterosexual, sig, significance
aReference is cisgender, heterosexual men
bReference is White
cReference is Democrat
dReference is employed fulltime
*p < 0.05, **p < 0.01, ***p < 0.001
Results
Sample
Demographic characteristics for the sample can be found in Table 1. Regarding gender and sexuality, 48.1% of the sample identified as cisgender and heterosexual men, 40.0% identified as cisgender and heterosexual women. The remaining 11.9% identified as LGBTQ+. White (81.2%) and non-Hispanic (94.8%) individuals represented the majority of the sample. Furthermore, 84.3% of the sample reported being insured. Almost 67% of the sample described themselves as employed full-time, while half of individuals described themselves as married. The sample was split evenly in terms of vaccination status with 49.4% indicating COVID-19 vaccination, with the other 50.6% reporting not being vaccinated. In terms of political affiliation, 50.3% of the sample reported Democrat, while 22.1% reported Republican affiliation. The remaining 27.7% identified as politically independent. Unadjusted bivariate analyses suggested that Democrats and Republicans reported similar levels of trust in healthcare (mean 12.8, sd 2.2; mean 12.9, sd 2.5, respectively), but Independents (mean 12.0, sd 2.7) reported lower levels of trust relative to Democrats (p < 0.001). Republicans reported higher internal locus of control (mean 18.7, sd 3.4) relative to Democrats (mean 17.3, sd 3.6), and Independents scored similarly to Democrats (mean 17.3, sd 3.5). Republicans (mean 40.2, sd 10) and Independents (mean 44, sd=10.4), reported fewer positive attitudes of mask wearing compared to Democrats (mean 49.7, sd 6.2). A similar relationship is seen with changes to routines with Republicans (mean 33.7, sd 7) and Independents (mean 33.3, sd 7.2) indicating fewer changes to their normal routines due to COVID-19 than Democrats (mean 36.5, sd 5.3).
Multivariate results
All analyses were conducted using Stata 15.1. The results from the logistic regression predicting likelihood of being vaccinated are provided in Table 2. A number of demographic characteristics such as age, ethnicity, income, education, and employment status were associated with odds of being vaccinated, along with political party affiliation and trust in healthcare. More specifically, increase in age (Odds Ratio [OR] 1.02, p < 0.05), higher income (OR 1.19, p < 0.001) and higher education category (OR 1.21, p < 0.05) increased the odds of being vaccinated (model 2). Regarding political affiliation, Republicans (OR 0.42, p < 0.001) had lower odds of being vaccinated compared to Democrats (model 2). Finally, individuals who were insured (versus uninsured) (OR 2.0, p < 0.05) and had higher trust in healthcare (OR = 1.16, p < 0.001) had higher odds of being vaccinated.
At the time of the survey, some individuals may have been willing to get vaccinated, but may have not had access to the vaccine or were not yet eligible. We therefore complement the analysis reported in Table 2 with an analysis that examines factors that may influence the decision to get vaccinated among those not yet vaccinated (N = 280), see Table 3. Like those who were vaccinated, those who had higher levels of trust in healthcare (OR 1.27, p < 0.001), and were older in age (OR 1.03, p < 0.05), had higher odds of stating they would get vaccinated (model 2). While those who were retired (relative to those who work fulltime) had higher odds of being vaccinated at the time of the survey (see Table 2, model 2), they had lower odds of stating they were willing to get vaccinated if they were not already vaccinated relative to those who work fulltime (OR 0.16, p < 0.001) (Table 3, model 2). Republicans (OR 0.29, p < 0.001) and Independents (OR 0.34, p < 0.01) indicated that they were less willing to get vaccinated than Democrats.
While the results in Table 2 imply that trust in healthcare has a statistically significant effect on vaccinations, the size of the effect is less clear. To examine the magnitude of the effect of trust in healthcare on vaccination outcomes, we created a quartile measure of trust in healthcare, and calculated predicted probabilities of getting vaccinated and being willing to get vaccinated (for those unvaccinated at the time of the study) using post logistic regression estimation of marginal effects, calculated while keeping exogenous variables at their mean values (the same covariates as in Tables 2 and 3 were included in the model). Predicted probabilities (with 95% Confidence Intervals) of vaccine outcomes by trust in healthcare quartile are presented in Fig. 2. The difference in the predicted probability of being vaccinated for those at or above the 75th percentile (quartile 4) compared to the predicted probability of those who are below the 25th percentile (quartile 1) in trust in healthcare is statistically significant (p < 0.05) (top image of Fig. 2), and large in magnitude. Specifically, the probability of those in the highest quartile (quartile 4) of trust in healthcare being vaccinated was 57.8%, compared to 38.2% for those in quartile 1 of trust in healthcare. Similarly, differences in the predicted probabilities of willingness to receive COVID-19 vaccine for those at or above the 75th percentile (quartile 4) in trust in healthcare compared to the predicted probability of those below the 25th percentile (quartile 1), within the 25th–50th percentile (quartile 2), and within the 50th–75th percentile (quartile 3) of trust in healthcare, are statistically significant (p < 0.001) (bottom image of Fig. 2). Again, the effects are large. The probability of those in quartile 4 for trust in healthcare who are unvaccinated being willing to be vaccinated was 84.2%, compared to 51.3% for those in the quartile 1 of trust in healthcare, given that all predictors are at mean values.
Table 4 presents the negative binominal model for estimating the count of positive attitudes toward face masks. Several variables were associated with views on masks. Specifically, those that expressed having higher levels of trust in healthcare had higher counts of positive attitudes toward masks (Coefficient 0.02, p < 0.001) (model 2). Additionally, both Republicans (Coefficient –0.21, p < 0.001) and Independents (Coefficient –0.09, p < 0.001) had lower counts of positive attitudes toward masks relative to Democrats.
Table 5 presents the negative binomial model examining count of perceived changes in routines due to COVID-19. Individuals who scored higher (e.g., poorer) self-rated health (Coefficient 0.02, p < 0.01) and reported more trust in healthcare (Coefficient 0.01, p < 0.01) had an associated higher count of changes to their daily routines due to COVID-19 (model 2). Further, those that were unemployed (compared to those who were fulltime employed) (Coefficient –0.10, p < 0.05) and individuals who were affiliated Republicans (Coefficient –0.06, p < 0.001) or Independents (Coefficient –0.07, p < 0.001) (compared to Democrats) had lower reported count of changes in their routines (model 2).
Discussion
Using a health lifestyles framework, this study examined social structural factors and social conditions that may influence COVID-19 mitigation. We considered multiple influences, including demographics, attitudes, and behaviors, related to endorsement or participation in COVID-19 mitigation strategies within a US-based sample (vaccination, willingness to be vaccinated if unvaccinated, mask attitudes, and perceived routine changes). A key role of trust in healthcare in health-related behaviors and attitudes related to COVID-19 was found and reaffirms prior research suggesting that there is not a consensus on COVID-19 pandemic mitigation efforts. In addition, it shows the vital role of trust in healthcare in health-related behaviors and attitudes related to COVID-19. It also showed that the effect on COVID-19 related behaviors from trust in healthcare was independent of political affiliation—another variable widely documented to affect health behaviors and attitudes during the pandemic. Finally, our study highlights the importance of examining multiple dimensions of COVID-19 health-related behaviors, as some factors, such as self-rated health, were not independently associated with certain aspects of COVID-19 mitigation compliance. People with worse self-rated health were potentially not more or less likely to be vaccinated or endorse mask wearing but were more likely to see changes to their routines as the result of the pandemic. While greater change in routine does not necessarily represent greater compliance to COVID-19 recommendations per se, it does illustrate that factors such as preexisting health status or being insured may pattern opportunities to engage in certain types of health lifestyle strategies over others.
Our study also supports the influence of social collectives on health behavior, finding heterogeneity in pandemic related health behaviors or attitudes. We found that individuals who identified as Democrat had higher odds of being vaccinated or greater willingness to be vaccinated (Callaghan et al. 2021), greater endorsement of masks, and greater perceived changes in daily routines as a result of COVID-19 relative to both Republicans and Independents. These differences along party affiliation are consistent with prior research, but future research may explore the unique experiences of individuals who identify as Independent, who may be even less willing to be vaccinated relative to Republicans (Thunström et al. 2021), and in the case of this study, have lower trust in healthcare. Often, media focuses on differences in a binary—Democrats versus Republicans—but a sizeable percentage of individuals (almost 28% of our sample) identified as politically independent, highlighting the importance of including this group of people. Further, estimates by other researchers have found similar proportions or even higher proportions of people who are independent, with a 2021 Gallup poll reporting that 42% of people now identify as independent (Jones 2022). Considering Republicans are most often targeted in the public debate for their negative views on masking and vaccines, it is important to note that those who are politically independent may hold comparable views. For example, we found, Republicans and politically independent/unaffiliated were less likely to change their routines and endorse mask use compared to Democrats. The political independents were also significantly less willing to be vaccinated, again like Republicans, when compared to Democrats. Thus, in the current study, those who were politically independent/unaffiliated ideologically aligned more with Republicans on most attitudes related to vaccines and masking, suggesting that excluding this group in analysis does not provide a complete picture. It also suggests that only focusing on individuals who identify as politically conservative or Republican-affiliated when attempting to reduce misinformation and hesitancy, misses a large proportion of people that may be endorsing, or contributing to this issue, especially given that political held beliefs are more likely to influence perceptions of the threat that COVID-19 poses than exposure to partisan messaging (Conway et al. 2021).
Similar to Myerson et al. (2021) and other studies, we also found one social structural factor influenced our outcomes; people of older ages to be more consistently associated with COVID-19 mitigation outcomes, including vaccination and willingness to be vaccinated. Although we did have the counter intuitive finding that, when adjusting for age, people who are retired are more likely to be vaccinated, but less willing to be vaccinated if unvaccinated. A potential explanation to this result is that a larger fraction of retired people, compared to those in fulltime work, who wanted to get the vaccine had already been able to get vaccinated, since older people were prioritized for vaccinations. Hence, relatively few retired people with a preference for getting vaccinated were among those who were still unvaccinated at the time of our study. However, we did not find age to be significantly associated with perceived routine changes or endorsement of masks. While older people are more at risk from COVID-19, such that it might be expected that they would be more prone to changing their routines, and to a greater extent endorse masks, they were also prioritized to get vaccinated. They might feel protected by the vaccine and therefore engage in other mitigation strategies less.
Contrary to prior research, we did not find differences across gender/sexuality, nor did locus of control have an impact on the actions of individuals to mitigate the risks of COVID-19. These variables were not significant in any model. This may be due to sampling differences, and/or the inclusion of other factors such as political party affiliation and trust in the healthcare system, that reduce the impact of other individual characteristics. We should consider further how upstream factors such as social structure, collectives, and opportunities might account for our impetus to act, negating its independent effects. Overall, we found support for the health lifestyles framework, finding that some social structure factors (e.g., age) and social conditions (e.g., political affiliation) influenced COVID-19 mitigation while other factors (e.g., gender and locus of control) did not significantly influence participation in mitigation. Further, trust in healthcare played a vital role in COVID-19 mitigation, highlighting the importance of attitudes and beliefs in our health behavior.
The rapid spread of conspiracy theories, including that COVID-19 is a hoax or overblown, was likely exacerbated by conflicting messaging on the severity of COVID-19 by political leaders; Earnshaw et al. (2020) found that nearly 30% of study participants endorsed at least one COVID-19 conspiracy theory. The spread of COVID-19 conspiracies has been a barrier to managing COVID-19, as misinformation increases unwillingness to be vaccinated and facilitates noncompliance to other COVID-19-related health recommendations (Earnshaw et al. 2020; Romer and Jamieson 2020). Concern about vaccine safety or trust in vaccines was arguably more important for individual vaccination behavior compared to whether they saw COVID-19 as a health threat or overblown (Karlsson et al. 2021). Further, this misinformation is not solely attributable to conservative news sources like FOX News, with one study finding that both FOX News and CNN/MSNBC viewers accepted vaccine conspiracy theories (Ruiz and Bell 2021). Overall, combating misinformation should include a holistic approach, focusing on broad media and consistent messaging.
Further, this study highlights the key role of trust in healthcare and medicine for the success of public health efforts to control the COVID-19 pandemic. In our study, people with high levels of trust in the medical system were around 20 percentage points more likely to be vaccinated than those with low trust in the medical system. Distrust in healthcare may be associated with the festering of COVID-19 misinformation as mentioned above. Further, all else equal, trust may be undermined by the mixed messaging of the Centers for Disease Control (CDC) and other institutions regarding COVID-19 mitigation strategies, such as mask wearing and recommended quarantine periods (Batova 2021; Resh 2020). Healthcare professionals’ use of social media, and their role in the spread of misinformation or conflicting messaging should also be highlighted; the deluge of social media messaging during the COVID-19 pandemic is often referred to as the “infodemic,” and refers to both misinformation and legitimate health information being shared at a high volume (Jamison et al. 2020). More training is arguably necessary for healthcare and public health professionals regarding how they may be engaging in information sharing on social media (Carlo et al. 2021). Considering new ethical guidelines or training on public-facing discourse or engagement may be a fruitful avenue in the quest to increase trust in healthcare providers and institutions (Jamison et al. 2020).
However, distrust in the health system extends beyond the specific conditions of the pandemic or the misinformation around COVID-19; for example, distrust in the pharmaceutical industry and the nature of the relationship between physicians/health practitioners and the pharmaceutical industry is important to consider (Grande et al. 2012; Olsen and Whalen 2009). It is well established that distrust in the pharmaceutical industry is associated with lower vaccination rates, for both adults and their children (Attwell et al. 2017). The perceived culpability of healthcare professionals in the opioid epidemic and rising healthcare costs likely contributes to the erosion of trust in healthcare and medicine (Gale 2016; Mazurenko et al. 2020); perceived financial incentives of healthcare professions to work against people’s health or best interest is an important component of medical distrust (Dana and Loewenstein 2003; Grande et al. 2012; Schwei et al. 2014; Webb Hooper et al. 2022). Additional research is necessary to elucidate public perception of healthcare’s financial “benefit” from the pandemic and how this may have fostered distrust in COVID-19 information and mitigation efforts. To facilitate trust in healthcare providers and the health system, we need to consider how funding arrangements within the US healthcare system (e.g., for-profit, fee-for-service, or capitated payment models) may contribute to eroding public trust. For example, the non-exploitative principles of other universal healthcare systems, such the United Kingdom’s (UK) National Health Service, may facilitate greater trust in their healthcare system due to their lack of overt financial incentives (Gilson 2003), although it is important to acknowledge other countries, including the UK, also struggle with adherence to pandemic mitigation strategies (Jennings et al. 2021). Distrust in our health system and governmental agencies is a barrier to improved public health, and it is vital to consider strategies to foster trust in our health-related institutions, that can subsequently increase the effectiveness of public health policies when faced with future health crises.
Limitations and future directions
While the current study adds to the growing literature in the areas of COVID-19 research, attitudes, and mitigation, it has limitations that must be acknowledged. First, the sample was collected using MTurk, a convenience sample. MTurk data has been criticized for issues involving inattentive users, selection bias, and misrepresentation of demographics (Aguinis et al. 2021). That said, research on MTurk samples has shown that MTurk workers may display more effort and pay more attention to tasks compared to student samples (Anson 2018).
In addition, data was collected in April and May of 2021, before COVID-19 vaccines were widely available in many parts of the United States. This influences the number of people that were able to be vaccinated at the time of the survey and likely influences perceptions about willingness to be vaccinated. Considering the small amount of time vaccines had been available at the time of the survey, it may be that some perceptions of the vaccines have changed over time. Relatedly, additional variables not included in the current study could also affect perceptions on willingness to be vaccinated, attitudes toward masks, and routine changes. For example, having a family member with an immune deficiency, or other family characteristics such as having children, may also influence these attitudes. While we ran preliminary analyses to assess internal consistency and covariance structures of our key scales (masking attitudes, trust in healthcare), additional confirmatory factor analyses should be pursued regarding trust in healthcare. Future studies should continue to assess the important dimensions underlying trust in healthcare (see Gregory et al. 2022; Musa et al. 2009), consider how dimensions of trust in physicians and the healthcare system may evolve over time (Pearson and Raeke 2000), and whether important dimensions of trust vary by sociodemographic factors such as age or gender.
Further, the questions pertaining to routine changes only measure perceptions of change, not actual behavioral change. We also do not know if the changes in routine were due to active efforts to mitigate COVID-19 spread by the individual or if they were a result of restrictions or other outside forces, such as health mandates, that resulted in these changes. A similar issue arises with the survey questions about masks, mostly tapping into attitudes, and not directly measuring behaviors. Future research should seek to include additional family and personal characteristics that may shape perceptions and variables that attempt to directly measure behaviors to provide a more complete picture.
Implications and conclusions
The current study applied a health lifestyle framework and found that trust in healthcare was consistently associated with outcomes—those having more trust in healthcare reported a higher likelihood of vaccination, willingness to be vaccinated, higher mask endorsement, and more perceived routine change. While our study reaffirms previous findings that political affiliation impacts people’s health attitudes and behaviors during the pandemic, trust in healthcare was an independent and significant factor. The findings from this study indicate that efforts to increase trust in healthcare should be prioritized and seen as a vital component of strong public health policy alongside other key pandemic mitigation strategies. Our study also points to the importance of research that identifies strategies to build trust in healthcare. For example, we could consider developing new ethical standards and trainings regarding public-facing health messaging and discourse by health system employees and agency representatives (Carlo et al. 2021), addressing perceived politicization of our governmental health agencies, such as the CDC, and further evaluating the ways the funding arrangements within our healthcare system may contribute to or exacerbate distrust (Gilson 2003).
Supplementary information
(DOCX 53 kb)
Authors’ contributions
JT, JS, CW, and AF were involved in survey development and data management. JT conducted statistical analyses. All authors, including LT, provided substantive feedback and contributed to the drafting of the manuscript.
Funding
Funding was provided by the College of Arts and Sciences at the University of Wyoming
Data availability
Data is available and can be requested from the first author
Code availability
Code is available and can be requested from the first author
Declarations
Ethics approval
This study was reviewed and deemed exempt from ongoing review by the University of Wyoming Institutional Review Board. Authors followed the ethical guidelines set forth for working with human participants by the Declaration of Helsinki.
Consent to participate
All participants were required to consent to participate at the start of the electronic survey.
Consent for publication
Not applicable
Conflicts of interest
The authors report no conflicts of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Aguinis H, Villamor I, Ramani RS. MTurk research: review and recommendations. J Manag. 2021;47(4):823–837. doi: 10.1177/0149206320969787. [DOI] [Google Scholar]
- Aharon A, Nehama H, Rishpon S, Baron-Epel O. A path analysis model suggesting the association between health locus of control and compliance with childhood vaccinations. Hum Vaccin Immunother. 2018;14(7):1618–1625. doi: 10.1080/21645515.2018.1471305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allington D, McAndrew S, Moxham-Hall V, Duffy B. Media usage predicts intention to be vaccinated against SARS-CoV-2 in the US and the UK. Vaccine. 2021;39:2595–2603. doi: 10.1016/j.vaccine.2021.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anson IG. Taking the time? Explaining effortful participation among low-cost online survey participants. Res Politics. 2018;5(3):2053168018785483. doi: 10.1177/2053168018785483. [DOI] [Google Scholar]
- Attwell K, Leask J, Meyer SB, Rokkas P, Ward P. Vaccine rejecting parents’ engagement with expert systems that inform vaccination programs. J Bioethical Inq. 2017;14(1):65–76. doi: 10.1007/s11673-016-9756-7. [DOI] [PubMed] [Google Scholar]
- Baker DW. Trust in health care in the time of COVID-19. JAMA. 2020;324(23):2373–2375. doi: 10.1001/jama.2020.23343. [DOI] [PubMed] [Google Scholar]
- Batova T (2021) To wear or not to wear: a commentary on mistrust in public comments to CDC tweets about mask-wearing during COVID19. Int J Bus Commun 1-2. 10.1177/23294884211008584
- Birkhäuer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner C, Gerger H. Trust in the health care professional and health outcome: a meta-analysis. PLoS One. 2017;12(2):e0170988. doi: 10.1371/journal.pone.0170988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blendon RJ, Benson JM, Hero JO. Public trust in physicians: US medicine in international perspective. N Engl J Med. 2014;371(17):1570–1572. doi: 10.1056/NEJMp1407373. [DOI] [PubMed] [Google Scholar]
- Brenan M (2020) Amid pandemic, confidence in key US institutions surges. Published August 12, 2020. https://news.gallup.com/poll/317135/amid-pandemic-confidence-key-institutions-surges.aspx. Accessed 01 Mar 2022
- Burton AL, Cullen FT, Burton VS, Graham A, Butler LC, Thielo AJ. Belief in redeemability and punitive public opinion: “Once a criminal, always a criminal” revisited. Crim Justice Behav. 2020;47(6):712–732. doi: 10.1177/0093854820913585. [DOI] [Google Scholar]
- Callaghan T, Moghtaderi A, Lueck JA, Hotez PJ, Strych U, Dor A, Motta M. Correlates and disparities of COVID-19 vaccine hesitancy. Soc Sci Med. 2021;272:113638. doi: 10.1016/j.socscimed.2020.113638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callow M, Callow D. Older adults’ behavior intentions once a COVID-19 vaccine becomes available. J Appl Gerontol. 2021;40:943–952. doi: 10.1177/07334648211019205. [DOI] [PubMed] [Google Scholar]
- Carlo AD, Barnett BS, Essien UR, Galea S. Redefining medicine's relationship with the media in the era of COVID-19. Am J Prev Med. 2021;60(1):142–145. doi: 10.1016/j.amepre.2020.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockerham WC. Health lifestyle theory and the convergence of agency and structure. J Health Soc Behav. 2005;46(1):51–67. doi: 10.1177/002214650504600105. [DOI] [PubMed] [Google Scholar]
- Conway L, Woodard S, Zubrod A, Chan L. Why are conservatives less concerned about the coronavirus (COVID-19) than liberals? Comparing political, experiential, and partisan messaging explanations. Personal Individ Differ. 2021;183:111124. doi: 10.1016/j.paid.2021.111124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordero DA. Fight of the unfit: protecting the immunocompromised and those with certain medical conditions during the COVID-19 pandemic. J Public Health. 2022;44(2):e274–e274. doi: 10.1093/pubmed/fdab167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coroiu A, Moran C, Campbell T, Geller AC. Barriers and facilitators of adherence to social distancing recommendations during COVID-19 among a large international sample of adults. PLoS One. 2020;15(10):e0239795. doi: 10.1371/journal.pone.0239795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowan S, Mark N, Reich J. COVID-19 vaccine hesitancy is the new terrain for political division among Americans. Socius. 2021;7:1–3. doi: 10.1177/23780231211023657. [DOI] [Google Scholar]
- Cullen FT, Graham A, Jonson CL, Pickett JT, Sloan MM, Haner M (2021) The denier in chief: faith in Trump and techniques of neutralization in a pandemic. Deviant Behav 1-23. 10.1080/01639625.2021.1918035
- Dana J, Loewenstein G. A social science perspective on gifts to physicians from industry. JAMA. 2003;290(2):252–255. doi: 10.1001/jama.290.2.252. [DOI] [PubMed] [Google Scholar]
- Doherty C, Kiley J, Asheer N (2020) Republicans, democrats move even further apart in coronavirus concerns. Pew Research Center. Published June 25, 2020. https://www.pewresearch.org/politics/2020/06/25/republicans-democrats-move-even-further-apart-in-coronavirus-concerns/. Accessed 01 Mar 2022
- Earnshaw VA, Eaton LA, Kalichman SC, Brousseau NM, Hill EC, Fox AB. COVID-19 conspiracy beliefs, health behaviors, and policy support. Transl Behav Med. 2020;10(4):850–856. doi: 10.1093/tbm/ibaa090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede LE, Ellis C. Development and testing of the multidimensional trust in health care systems scale. J Gen Intern Med. 2008;23(6):808–815. doi: 10.1007/s11606-008-0613-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fendrich M, Becker J, Park C, Russell B, Finkelstein-Fox L, Hutchison M. Associations of alcohol, marijuana, and polysubstance use with non-adherence to COVID-19 public health guidelines in a US sample. Subst Abus. 2021;42(2):220–226. doi: 10.1080/08897077.2021.1891603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridman A, Gershon R, Gneezy A. COVID-19 and vaccine hesitancy: A longitudinal study. PLoSONE. 2021;16:30250123. doi: 10.1371/journal.pone.0250123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale AH. Drug company compensated physicians role in causing America’s deadly opioid epidemic: When will we learn? Mo Med. 2016;113(4):244. [PMC free article] [PubMed] [Google Scholar]
- Gerace A, Rigney G, Anderson J. Predicting attitudes towards easing COVID-19 restrictions in the United States of America: The role of health concerns, demographic, political, and individual differences factors. PLoS One. 2022;17(2):e0263128. doi: 10.1371/journal.pone.0263128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilson L. Trust and the development of health care as a social institution. Soc Sci Med. 2003;56(7):1453–1468. doi: 10.1016/s0277-9536(02)00142-9. [DOI] [PubMed] [Google Scholar]
- Graham JL, Grimes RM, Slomka J, Ross M, Hwang LY, Giordano TP. The role of trust in delayed HIV diagnosis in a diverse, urban population. AIDS Behav. 2013;17(1):266–273. doi: 10.1007/s10461-011-0114-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grande D, Shea JA, Armstrong K. Pharmaceutical industry gifts to physicians: Patient beliefs and trust in physicians and the health care system. J Gen Intern Med. 2012;27(3):274–279. doi: 10.1007/s11606-011-1760-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory ME, Nyein KP, Scarborough S, Huerta TR, McAlearney AS. Examining the dimensionality of trust in the inpatient setting: exploratory and confirmatory factor analysis. J Gen Intern Med. 2022;37(5):1108–1114. doi: 10.1007/s11606-021-06928-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidry JPD, Austin LL, O’Donnell NH, Coman IA, Lovari A, Messner M. Tweeting the #flushot: beliefs, barriers, and threats during different periods of the 2018 to 2019 flu season. J Prim Care Community Health. 2020;11:2150132720932722. doi: 10.1177/2150132720932722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser DJ, Schwarz N. Attentive Turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behav Res Methods. 2016;48(1):400–407. doi: 10.3758/s13428-015-0578-z. [DOI] [PubMed] [Google Scholar]
- Hou WK, Lai FTT, Ben-Ezra M, Goodwin R. Regularizing daily routines for mental health during and after the COVID-19 pandemic. J Glob Health. 2020;10(2):020315. doi: 10.7189/jogh.10.020315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamison AM, Broniatowski DA, Dredze M, Sangraula A, Smith MC, Quinn SC. Not just conspiracy theories: Vaccine opponents and proponents add to the COVID-19 ‘infodemic’ on Twitter. Harvard Kennedy School Misinform Rev. 2020;1(3):1–22. doi: 10.37016/mr-2020-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings W, Stoker G, Valgarðsson V, Devine D, Gaskell J. How trust, mistrust and distrust shape the governance of the COVID-19 crisis. J European Public Policy. 2021;28(8):1174–1196. doi: 10.1080/13501763.2021.1942151. [DOI] [Google Scholar]
- Jones JJ (2022) U.S. political party preferences shifted greatly during 2021. Gallup. https://news.gallup.com/poll/388781/political-party-preferences-shifted-greatly-during-2021.aspx. Accessed 01 Mar 2022
- Kannan V, Veazie P. Political orientation, political environment, and health behaviors in the United States. Prev Med. 2018;114:95–101. doi: 10.1016/j.ypmed.2018.06.011. [DOI] [PubMed] [Google Scholar]
- Karlsson LC, Soveri A, Lewandowsky S, Karlsson L, Karlsson H, Nolvi S, Antfolk J. Fearing the disease or the vaccine: the case of COVID-19. Personal Individ Differ. 2021;172:110590. doi: 10.1016/j.paid.2020.110590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesavayuth D, Poyago-Theotoky J, Zikos V. Locus of control, health and healthcare utilization. Econ Model. 2020;86:227–238. doi: 10.1016/j.econmod.2019.06.014. [DOI] [Google Scholar]
- Lades L, Laffan K, Daly M, Delaney L (2020) Daily emotional well-being during the COVID-19 pandemic. 10.1111/bjhp.12450 [DOI] [PMC free article] [PubMed]
- Lai FTT, Chan VKY, Li TW, Li X, Hobfoll SE, Lee TM, Hou WK. Disrupted daily routines mediate the socioeconomic gradient of depression amid public health crises: a repeated cross-sectional study. Aust N Z J Psychiatry. 2021;22:48674211051271. doi: 10.1177/00048674211051271. [DOI] [PubMed] [Google Scholar]
- Lalumera E. Trust in health care and vaccine hesitancy. Rivista Di Estetica. 2018;68:105–122. doi: 10.4000/estetica.3553. [DOI] [Google Scholar]
- Lefcourt HM (2013) Research with the Locus of Control Construct: Extensions and limitations. Elsevier
- Lucchini L, Centellegher S, Pappalardo L, Gallotti R, Privitera F, Lepri B, De Nadai M (2021) Living in a pandemic: changes in mobility routines, social activity and adherence to COVID-19 protective measures. Sci Rep 11(1):1-12. [DOI] [PMC free article] [PubMed]
- Lumpkin JR. Validity of a brief locus of control scale for survey research. Psychol Rep. 1985;57(2):655–659. doi: 10.2466/pr0.1985.57.2.655. [DOI] [Google Scholar]
- MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- Mallinas SR, Maner JK, Plant EA. What factors underlie attitudes regarding protective mask use during the COVID-19 pandemic? Personal Individ Differ. 2021;181:111038. doi: 10.1016/j.paid.2021.111038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazurenko O, Andraka-Christou BT, Bair MJ, Kara AY, Harle CA. Clinical perspectives on hospitals’ role in the opioid epidemic. BMC Health Serv Res. 2020;20(1):1–11. doi: 10.1186/s12913-020-05390-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milad E, Bogg T. Spring 2020 COVID-19 surge: Prospective relations between demographic factors, personality traits, social cognitions and guideline adherence, mask wearing, and symptoms in a US sample. Ann Behav Med. 2021;55(7):665–676. doi: 10.1093/abm/kaab039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musa D, Schulz R, Harris R, Silverman M, Thomas SB. Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health. 2009;99(7):1293–1299. doi: 10.2105/AJPH.2007.123927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myerson J, Strube MJ, Green L, Hale S. Individual differences in COVID-19 mitigation behaviors: the roles of age, gender, psychological state, and financial status. PLoS One. 2021;16(9):e0257658. doi: 10.1371/journal.pone.0257658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navas-Martín MÁ, López-Bueno JA, Oteiza I, Cuerdo-Vilches T. Routines, time dedication and habit changes in spanish homes during the covid-19 lockdown. A large cross-sectional survey. Int J Environ Res Public Health. 2021;18(22):12176. doi: 10.3390/ijerph182212176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen KH, Srivastav A, Razzaghi H, Williams W, Lindley MC, Jorgensen C, Singleton JA. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination—United States, September and December 2020. Am J Transplant. 2021;21(4):1650–1656. doi: 10.1111/ajt.16560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nofal AM, Cacciotti G, Lee N. Who complies with COVID-19 transmission mitigation behavioral guidelines? PLoS One. 2020;15(10):e0240396. doi: 10.1371/journal.pone.0240396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen AK, Whalen MD. Public perceptions of the pharmaceutical industry and drug safety. Drug Saf. 2009;32(10):805–810. doi: 10.2165/11316620-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Painter EM, Ussery EN, Patel A, Hughes MM, Zell ER, Moulia DL, Messonnier NE. Demographic characteristics of persons vaccinated during the first month of the COVID-19 vaccination program—United States, December 14, 2020–January 14, 2021. MMWR. 2021;70(5):174. doi: 10.15585/mmwr.mm7005e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. J Gen Intern Med. 2000;15(7):509–513. doi: 10.1046/j.1525-1497.2000.11002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resh WG (2020) The effects of mixed institutional messaging during the COVID-19 crisis. Policy
- Romer D, Jamieson KH. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc Sci Med. 2020;263:113356. doi: 10.1016/j.socscimed.2020.113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz J, Bell R. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021;39:1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwei RJ, Kadunc K, Nguyen AL, Jacobs EA. Impact of sociodemographic factors and previous interactions with the health care system on institutional trust in three racial/ethnic groups. Patient Educ Couns. 2014;96(3):333–338. doi: 10.1016/j.pec.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott EM, Stein R, Brown MF, Hershberger J, Scott EM, Wenger OK. Vaccination patterns of the northeast Ohio Amish revisited. Vaccine. 2021;39(7):1058–1063. doi: 10.1016/j.vaccine.2021.01.022. [DOI] [PubMed] [Google Scholar]
- Sharma M, Davis R, Wilkerson A. COVID-19 vaccine acceptance among college students: A theory based analysis. Int J Environ Res Public Health. 2021;28:4617–4628. doi: 10.3390/ijerph18094617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stosic M, Helwig S, Ruben M. Greater belief in science predicts mask-wearing behavior during COVID-19. Personal Individ Differ. 2021;176:110769. doi: 10.1016/j.paid.2021.110769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Asmundson GJ. Negative attitudes about facemasks during the COVID-19 pandemic: The dual importance of perceived ineffectiveness and psychological reactance. PLoS One. 2021;16(2):e0246317. doi: 10.1371/journal.pone.024631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thunström L, Ashworth M, Finnoff D, Newbold S. Hesitancy towards a COVID-19 vaccine. Ecohealth. 2021;18(1):44–60. doi: 10.1007/s10393-021-01524-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travis J, Harris S, Fadel T, Webb G. Identifying the determinants of COVID-19 preventative behaviors and vaccine intentions among South Carolina residents. PLoS One. 2021;16:e0256178. doi: 10.1371/journal.pone.0256178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb Hooper M, Mitchell C, Marshall VJ, Cheatham C, Austin K, Sanders K, Grafton LL. Responding to healthcare distrust among underserved communities: Phase II. Psycho-Oncology. 2022;31(1):3–8. doi: 10.1002/pon.5841. [DOI] [PubMed] [Google Scholar]
- Xu P, Cheng J. Individual differences in social distancing and mask-wearing in the pandemic of COVID-19: The role of need for cognition, self-control and risk attitude. Personal Individ Differ. 2021;175:110706. doi: 10.1016/j.paid.2021.110706. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 53 kb)
Data Availability Statement
Data is available and can be requested from the first author
Code is available and can be requested from the first author


