Abstract
Purpose of Review
Several studies have found that air pollution and climate change can have an impact on acute coronary syndromes (ACS), the leading cause of death worldwide. We synthesized the latest information about the impact of air pollution and climate change on ACS, the latest data about the pathophysiological mechanisms of meteorological factors and atmospheric pollutants on atherosclerotic disease, and an overall image of air pollution and coronary heart disease in the context of the COVID-19 pandemic.
Recent Findings
The variation of meteorological factors in different seasons increased the risk of ACS. Both the increase and the decrease in apparent temperature were found to be risk factors for ACS admissions. It was also demonstrated that exposure to high concentrations of air pollutants, especially particulate matter, increased cardiovascular morbidity and mortality.
Summary
Climate change as well as increased emissions of air pollutants have a major impact on ACS. The industrialization era and the growing population cause a constant increase in air pollution worldwide. Thus, the number of ACS favored by air pollution and the variations in meteorological factors is expected to increase dramatically in the next few years.
Keywords: Acute coronary syndrome, Coronary heart disease, Meteorological factors, Air pollutants, Risk factors
Introduction
Cardiovascular diseases represent the main cause of morbidity and mortality globally, being responsible for important medical costs, despite the improvement of prevention and management measures [1, 2]. In 2016, almost a third of all deaths on the planet were caused by cardiovascular diseases, with the prediction for 2030 being that this number will increase to 23 million [3, 4].
Acute coronary syndrome (ACS) is the clinical manifestation of coronary artery disease and includes acute myocardial infarction with/without ST-segment elevation (STEMI/NSTEMI) and unstable angina (UA). According to the Global Registry of Acute Coronary Events (GRACE Registry), STEMI represents 36% of all acute coronary events [5]. A similar percentage of STEMI cases has been reported by the Jakarta Acute Coronary Syndrome Registry (JAC Registry) [6]. Fortunately, the number of STEMI has significantly decreased since 1999 (133/100,000 people/years) up to 2008 (50/100,000 people/years), as was shown in a large US database [7]. At the same time, the proportion of patients with NSTEMI has increased from a third to more than half between 1995 and 2015 [8].
Besides the well-known risk factors for atherosclerosis (family history of ischemic heart disease, male gender, old age, smoking, dyslipidemia, high blood pressure, diabetes, etc.), more and more evidence shows that air pollutants and climate variations can influence the onset of ACS [9]. In the context of global warming, an important increase in cardiovascular mortality due to heat has been observed [10]. In 2017, the average global temperature increased by 0.46 (+ / − 0.1 °C) above the 1981–2010 average and by 1.1 (+ / − 0.1 °C) above preindustrial levels [11]. Air temperature, which is the most studied climatic factor over the past years, seems to have a major impact on human health. During the last decades, climatic and epidemiological data have shown a disquieting increase in possibly harmful environmental effects on cardiovascular health. For the first time, an increase in the number of acute myocardial infarctions (AMI) during the winter months was reported at the beginning of the 1930s [12].
The relation between the degree of air pollution and the rate of early cardiovascular mortality was postulated as early as the beginning of the twentieth century, when the first extreme episodes of air pollution caused by industrial smog were reported [13, 14].
The extreme variation of meteorological factors and the concentration of air pollutants above the accepted limit may represent an important risk factor for decompensating coronary artery disease. This review offers the latest information about the impact of air pollution and climate change on ACS, the latest data about the pathophysiological mechanisms of meteorological factors and atmospheric pollutants on atherosclerotic disease, as well as an overall image of air pollution and coronary heart disease (CHD) in the context of the COVID-19 pandemic.
The Impact of Meteorological Factors on Acute Coronary Syndrome
Acute myocardial infarctions cause more than 4 million deaths in Europe and North Asia and more than 2.4 million deaths in the USA [15]. Several epidemiological studies showed that the incidence of ACS was significantly higher in winter than in other seasons, as well as on days with heavy snowfall [16]. A study conducted in the USA reported a 53% increase in AMI cases in the winter months [17]. Likewise, an increase in cardiovascular and cerebrovascular mortality was observed among elderly patients in Canada during the cold season [18]. Data from studies performed in France, New Zealand, Japan, England, and Wales also reported an increase in the morbidity and mortality of CHD in the winter months [19–22]. In other countries with a Mediterranean climate, an increase in the number of acute coronary events was also observed in the cold season [23, 24]. Similar to the data reported in Europe and North America, a seasonal variation in cardiovascular mortality was observed in Brazil [25]. Yamaji et al. showed that low ambient temperatures can be a major risk factor for AMI, while air pollution and flu epidemics had a statistically insignificant impact [26]. The increased incidence of ACS in the winter months could be explained by intense physical activity due to “shoveling” on days with heavy snow [16]. Another possible cause was described by Kloner as the so-called “Merry Christmas coronary” phenomenon, which is a mixture of circumstances such as late hospitalization, excessive alcohol and food consumption, and the increased emotional stress associated with the holidays [27].
In the context of global warming, heat has proven to be another risk factor for ACS. A small number of epidemiological data revealed that the incidence of ACS increased during the summer, on days with high temperatures, high relative humidity, and low atmospheric pressure [28–30]. Madrigano et al. reported that heat exposure increased the incidence and mortality of acute coronary events as a consequence of low socio-economic status, low level of education, and pre-existing chronic diseases (diabetes, dyslipidemia, etc.) [29, 31].
Aside from seasonal variations, epidemiological studies have looked at the relationship between ACS and various meteorological parameters like air temperature, atmospheric pressure, air humidity, wind speed, precipitation, and light. A “V,” “U,” “J” or linear-shaped correlation was observed between ischemic cardiac events and ambient temperature [24, 32–35]. The risk of acute coronary events increased by 22% when the temperature threshold of 26–29 °C was exceeded and increased by 2.8% for each decrease of 1 °C below this threshold [32].
The impact of atmospheric pressure on ACS is confusing. Several studies reported a “V”- or “J”-shaped relationship between atmospheric pressure and the incidence of AMI, while other studies did not identify significant effects of this parameter. The number of ACS was significantly higher with increasing or decreasing atmospheric pressure above or below 1016 mbar in France [19]. On the other hand, a significant increase in AMI admissions was observed on days with low atmospheric pressure in Japan and Canada [36, 37]. A recent study in Hiroshima, Japan, reported a higher incidence of ACS on days with an air pressure below 1005 hPa, while another study conducted also in Japan, in Kumamoto, reported an increase in ACS on days with high atmospheric pressures [36, 38]. Bijelović et al. observed a reduction in AMI cases on days with an atmospheric pressure below 1009 hPa, adjusted for air temperature and humidity [39].
Unlike air temperature and atmospheric pressure, which have been intensively studied so far, the impact of air humidity, wind speed, and precipitation on AMI hospitalizations has not been extensively investigated. The relationship between air humidity and CHD is unclear. A study conducted in 12 US cities found no correlation between atmospheric humidity and CHD hospitalizations, while a positive correlation between the incidence of ACS and relative humidity was reported in Athens, Greece [35, 40]. High wind speeds were associated with an increased incidence of AMI in Switzerland [41, 42]. In Italy, a significant impact of the variation of meteorological factors in different seasons on the STEMI incidence was reported. STEMI risk was higher in certain meteorological conditions during the winter (on days with low temperatures, low atmospheric pressures, and low rainfall), spring (on days with high humidity and large variations in air pressure), and summer (on days with high temperatures) [43]. The SWEDEHEART registry reported an increased risk of ACS on days with low temperatures, low atmospheric pressure, decreased sunshine duration, and increased wind speed [44]. Other studies that analyzed the impact of air temperature on ACS types reported statistically significant results in terms of the incidence of STEMI, with no influence on the number of NSTEMI cases. A report from Israel showed an increase in STEMI cases in the winter season, while research from Japan showed that both the high peak temperature and the low average temperature the day before the acute coronary event caused a high incidence of STEMI [26, 45].
It was observed that air temperature alone does not accurately describe human thermal discomfort. Apparent temperature, a biometeorological index proposed by Steadman, seems to characterize more objectively the human perception of atmospheric temperature. This index is characterized by a combination of meteorological factors such as ambient temperature, humidity, and, optionally, solar radiation and wind speed [46, 47]. A few studies have analyzed the association between apparent temperature and the incidence of ACS, and the results have varied. In Iran, Moghadamnia et al. showed an increase in the number of ACS on days with a high apparent temperature, while Wichmann et al. identified that an increase in Tappmax (the daily 3-h maximum apparent temperature) was associated with a decrease in the incidence of AMI in the cold months [48, 49]. In Beijing, China, the number of STEMI cases increased on days with a high apparent temperature, while the incidence of NSTEMI was higher on days with a low apparent temperature [50••]. These data demonstrate the need for new studies to assess the impact of apparent temperature on the incidence of ACS subtypes in order to improve prevention measures and reduce cardiovascular mortality. The main studies that analyze the impact of seasonal variations and meteorological factors on ACS are summarized in Table 1.
Table 1.
Main studies that analyze the role of seasonal variations and meteorological factors on acute coronary syndrome
| Seasonal variations and cardiovascular morbidity and mortality | |||||
|---|---|---|---|---|---|
| Author | Location/type of climate | Study period | Study population | Season with effect on ACS/Death | Result |
| Auger et al. [16] | Quebec (Canada)/continental climate | 1981–2014 | Patients with MI | Winter | Quantity and duration of snowfall ↑ risk of AMI admissions or death due to MI |
| Spencer et al. [17] | US cities/temperate climate | 1994–1996 | Patients with AMI | Winter | ↑ risk of AMI |
| Sheth et al. [18] | Canada cities/continental climate |
1980–1982 1990–1992 |
Patients with AMI and Stroke | Winter | ↑ AMI and stroke mortality |
| Danet et al. [19] | Northern France/temperate climate | 1985–1994 | Patients with MI | Winter | ↑ risk of MI and coronary deaths |
| Swampillai et al. [20] | Waikato (New Zealand)/temperate climate | 1998–2007 | Patients with STEMI | Winter | ↑ risk of STEMI |
| Rumana et al. [21] | Takashima County, Shiga (Japan)/temperate climate | 1998–2003 | Patients with AMI | Winter, Spring | ↑ risk of AMI |
| Ogbebor et al. [22] | England and Wales/temperate climate | 1997–2005 | Patients with AMI | Winter | ↑ risk of AMI admissions and death due to MI |
| Vasconcelos et al. [23] | Lisbon and Oporto, (Portugal)/Mediterranean climate | 2003–2007 | Patients with AMI | Winter | ↑ risk of AMI |
| Dilaveris et al. [24] | Athens (Greece)/Mediterranean climate | 2001 | Patients with AMI | Winter | ↑ AMI mortality |
| Sharovsky et al. [25] | Sao Paulo (Brazil)/subtropical climate | 1996–1997 | Patients with MI | Winter | ↑ AMI mortality |
| Yamaji et al. [26] | Japan/ temperate climate | 2011–2012 | Patients with STEMI | Winter | ↑ risk of STEMI |
| Akioka et al. [28] | Oita (Japan)/humid subtropical climate | 2012–2013 | Patients with AMI | Summer | ↑ risk of AMI |
| Chen et al. [29] | Augsburg (Germany)/oceanic climate | 1987–2014 | Patients with MI | Summer | ↑ risk of MI |
| Nastos et al. [30] | Crete Island (Greece)/Mediterranean climate | 2004–2007 | Patients with ACS | Summer | ↑ risk of ACS |
| Madrigano et al. [31] | Worcester (USA)/humid continental climate |
1995, 1997, 1999 2001, 2003 |
Patients with AMI |
Cold months Warm months |
↑ risk of AMI ↑ the risk of dying after an AMI |
| Versaci et al. [43] | Different regions of Italy with different types of climate | 2012–2017 | Patients with STEMI |
Winter (↓ air temperature,↓ATM,↓rainfall) Spring (greater variations in ATM, ↑humidity) Summer (↑air temperature) |
↑ risk of STEMI |
| Leibowitz et al. [45] | Jerusalem (Israel)/Mediterranean climate | 2001–2005 | Patients with AMI | Winter | ↑ risk of STEMI |
| Meteorological factors variations and cardiovascular morbidity and mortality | |||||
|---|---|---|---|---|---|
| Author | Location/type of climate | Study period | Study population | Meteorological factors with effect on ACS/Death | Result |
| Danet et al. [19] | Northern France/temperate climate | 1985–1994 | Patients with MI |
↓Atmospheric temperaturea ↑/↓Atmospheric pressureb |
↑ risk of MI and coronary deaths |
| Yamaji et al. [26] | Different regions of Japan with different types of climate | 2011–2012 | Patients with STEMI |
↓Air temperature (Winter) ↓Minimum air temperature ↑ Maximum air temperature |
↑ risk of STEMI |
| Akioka et al. [28] | Oita (Japan)/humid subtropical climate | 2012–2013 | Patients with AMI |
↓Air temperature (Summer) ↑ Air humidity (Summer) |
↑ risk of AMI |
| Pan et al. [32] | Taiwan (China)/subtropical climate | 1981–1991 | Patients with CHD | ↑/↓ Ambient temperaturec | ↑ CHD mortality |
| Liang et al. [33] | Taiwan (China)/subtropical climate | 2000–2003 | Patients with ACS | ↑/↓ Ambient temperatured | ↑ risk of ACS |
| Guo et al. [34] | Yancheng (China)/humid subtropical climate | 2013–2018 | Patients with ACS | ↑/↓ Ambient temperaturee | ↑ risk of ACS |
| Panagiotakos et al. [35] | Athens (Greece)/Mediterranean climate | 2001–2002 | Patients with ACS |
↓ Air temperaturea ↑ Relative humidity |
↑ risk of ACS |
| Wang et al. [36] | Yamaguchi, Matsue, Tottori, Okayama, Hiroshima (Japan)/humid subtropical climate |
2000–2005 1993–2002 |
Patients with AMI |
↓Air temperature ↓Atmospheric pressure |
↑ risk of AMI |
| Hong et al. [37] | Alberta (Canada)/humid continental climate | 2002–2016 | Patients with STEMI | ↓Air pressure | ↑ risk of STEMI |
| Honda et al. [38] | Kumamoto (Japan)/humid subtropical climate | 2009–2013 | Patients with AMI |
↑ Air pressure ↓Air temperature ↓Air humidity ↑ Sunshine duration |
↑ risk of AMI |
| Bijelović et al. [39] | Novi Sad (Serbia)/humid subtropical climate | 2010–2011 | Patients with CVD |
↓Air temperature ↓Relative humidity ↓Air pressure |
↑ risk of AMI ↓ risk of AMI |
| Goerre et al. [42] | Different regions of Switzerland with different types of climate | 1990–1994 | Patients with AMI |
↑Ambient pressure ↑Wind activity |
↑ risk of AMI |
| Mohammad et al. [44] | Sweden/temperate climate | 1998–2013 | Patients with MI |
↓Air temperature ↓Atmospheric air pressure ↑Wind velocity ↓Sunshine duration |
↑ risk of MI |
| Moghadamnia et al. [48] | Rasht (Iran)/humid subtropical climate | 2005–2014 | Patients with ACS | ↑Apparent temperature | ↑ risk of ACS |
| Wichmann et al. [49] | Copenhagen (Denmark)/oceanic climate | 1999–2006 | Patients with AMI | ↑Tappmax (in the cold period) | ↓ risk of AMI |
| Li et al. [50••] | Beijing (China)/monsoon-influenced humid continental climate | 2017–2019 | Patients with ACS |
↑Apparent temperature ↓Apparent temperature |
↑ risk of STEMI ↑ risk of NSTEMI |
ACS acute coronary syndrome, MI myocardial infarction, AMI acute myocardial infarction, STEMI ST-elevation myocardial infarction, ATM atmospheric pressure, CHD coronary heart disease, CVD cardiovascular disease, Tappmax daily 3-h maximum apparent temperature
aA linear association between air temperature and ACS admissions
bA V-shaped relation between atmospheric pressure and MI: ↑/↓ atmospheric pressure over/below 1016 mbar ↑ risk of MI
cA U-shaped relation between ambient temperature and CHD mortality: ↑/↓ air temperature over/below 26–29 °C ↑ CHD mortality
dA U-shaped relation between ambient temperature and ACS admissions: ↑/↓ air temperature over/below 27–29 °C ↑ ACS admissions
eAn inverse J-shaped relation between ambient temperature and ACS admissions: ↑/↓ air temperature over/below temperature threshold (25 °C) ↑ ACS admissions
Pathophysiological Mechanisms of Meteorological Factors
Studies that analyzed the relationship between the season and the type of atherosclerotic plaque have reported that both cold and heat are risk factors for atheroma destabilization. In winter, the acute coronary event occurred due to rupture of the atheroma plaque, while in summer, the main cause was plaque erosion [51, 52]. Regarding the size of myocardial infarction, the summer months appear to be associated with less extensive myocardial infarction, probably due to vasodilation, low preload and postload, low stimulation of the sympathetic nervous system, and low plasma catecholamine levels [53]. It was observed that a decrease in atmospheric temperature causes an increase in the activity of the sympathetic nervous system, resulting in an increase in blood pressure and heart rate [54]. The same physiological response is generated by the increase in serum catecholamines (vasoconstrictor effect) due to the stimulation of cold receptors in the skin [55]. Exposure to extremely low temperatures has prothrombotic and proinflammatory effects that promote atherothrombosis and the destabilization of already formed atheroma plaques [56, 57]. The cumulative action of these factors generates an imbalance between the need for and the supply of oxygen to the myocardium in the conditions of a pre-existing atherosclerotic disease, substantially increasing the risk of an acute coronary event in susceptible people. Heat, like low temperatures, increases blood viscosity, lipoprotein oxidation, and cholesterol deposits in blood vessel walls [58]. In people at risk of developing ACS, extreme heat can induce a systemic inflammatory response along with dehydration and vasodilation [54].
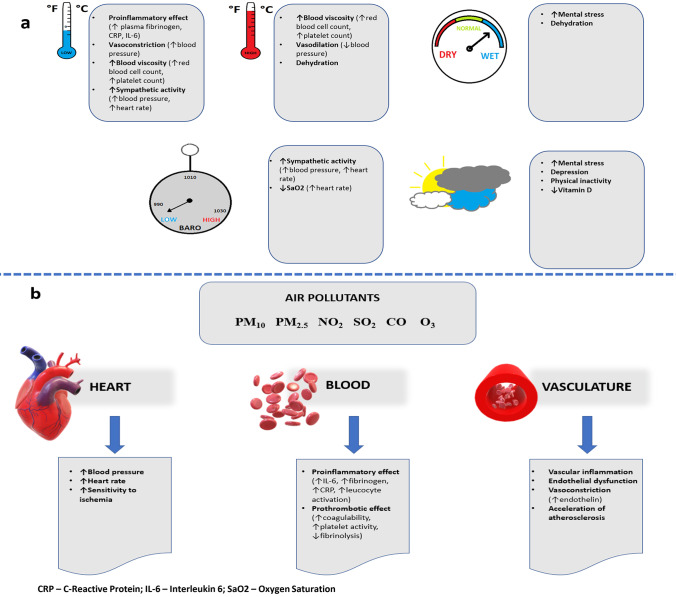
The mechanism by which changes in atmospheric pressure cause ACS is also controversial. Decreased air pressure causes an exaggerated response of the sympathetic nervous system and decreased oxygen saturation in the arterial blood [19, 59]. An in vitro study published in 2016 showed that epidermal keratinocytes play a major role in the body’s response to sudden changes in atmospheric pressure. Reduced variations in air pressure by 5–20 hPa resulted in an increase in calcium influx into human keratinocytes. According to this research, the sudden change in atmospheric pressure stimulates the keratinocytes in the epidermis that synthesize nitric oxide (with a vasodilating role) and other hormones and neurotransmitters with an important role in the cardiovascular, nervous, immune, and endocrine systems [60]. High humidity causes dehydration and increased mental stress, while reduced sun exposure has been associated with vitamin D deficiency, depressive episodes, and a sedentary lifestyle [59]. The pathophysiological mechanisms by which meteorological factors can destabilise ACS are summarized in Fig. 1a.
Fig. 1.
Pathophysiological mechanisms of meteorological factors and air pollutants on acute coronary syndrome. a Pathophysiological mechanisms of meteorological factors. b Pathophysiological mechanisms of air pollutants
The Impact of Air Pollution on Acute Coronary Syndrome
Air pollution can be a key risk factor for ACS. Air pollution is currently the most important risk factor for global environmental health, with an estimated 3.7 million deaths per year due to outdoor air pollution and 4.3 million deaths per year due to exposure to indoor air pollution [61]. Up to 58% of premature deaths related to outdoor air pollution occurred in people with a history of CHD and stroke [62].
Indoor air pollution is mainly generated by the household combustion of fuels [63]. A recent study reported that the low socio-economic level and the lack of basic household utilities for cooking and daily heating have contributed to the increase in the total number of diseases due to air pollution to about 3 billion [64]. Most outdoor air pollutants come from industry, transportation, agriculture, power, and heating generation devices [63].
Atmospheric air pollution is caused by gaseous pollutants (sulfur dioxide, SO2; nitrogen dioxide, NO2; ozone, O3; carbon monoxide, CO) and fine or ultrafine particulate matter (particulate matter with a diameter ≤ 10 μm, PM10; particulate matter with a diameter ≤ 2.5 μm, PM2.5; particulate matter with a diameter ≤ 0.1 μm). The sources of air pollution are varied: NO2 is a pollutant emitted primarily by exhaust fumes; SO2 is generated by vehicles as well as by fossil fuel combustion; ground level ozone (O3) is a pollutant emitted by transport systems and industrial systems, with high concentrations on sunny days; CO is produced by incomplete combustion of fuels; PM results from natural processes, transportation systems, as well as fossil fuel combustion [62, 63].
A marked increase in cardiovascular morbidity and mortality due to short-term or long-term exposure to air pollutants was reported. On the other hand, there are few epidemiological studies that have assessed the impact of air pollution on ACS subtypes.
A harmful effect of fine particulate matter was observed when analyzing the relationship between long-term exposure to air pollution and cardiopulmonary mortality. In 2002, a large study conducted in the USA showed an increased risk of all-cause (4%), lung cancer (8%), and cardiopulmonary (6%) mortality for each 10 μg/m3 elevation of PM2.5 particle concentrations [65]. Similar results have been observed in England and Wales, where the mortality of patients with a history of CHD increased as a result of chronic exposure to PM2.5 [66]. In a multicenter European analysis, the incidence of acute coronary events increased by 13% in the case of chronic exposure to PM2.5 and by 12% in the case of chronic exposure to PM10 [67]. A recent meta-analysis of 27 cohort studies found a much more harmful effect of PM2.5 compared to PM10 on the risk of AMI [68•].
The results of epidemiological studies that analyzed the relationship between short-term exposure to air pollutants and the incidence of ACS were varied. The analysis of MINAP (Myocardial Ischaemia National Audit Project) data has noted a strong correlation between NO2 levels and ACS risk [69, 70]. Each 10 μg/m3 increase in NO2 concentration caused a double rise in the risk of acute coronary events [69]. Likewise, each 10 μg/m3 increase in NO2 was associated with an important impact on NSTEMI cases, but without a significant correlation between STEMI and NO2 levels [70]. Several authors showed that in Alberta, Canada, exposure to high concentrations of NO2 caused an increase in NSTEMI hospitalizations, especially in elderly patients with high blood pressure [71]. There has also been an increase in AMI cases in France on days when the NO2 concentration exceeded 30 μg /m3, while in Sweden, each 12.9 μg/m3 increase in NO2 levels was associated with a 4.2% increase in STEMI cases [72, 73].
Epidemiological data has suggested that fine particulate matter has much more obvious toxic cardiovascular effects than gaseous pollutants. High levels of PM2.5 and PM10 were associated with an increased risk of ACS in Italy, China, New York, and Poland [74–78]. In Italy, a 10 μg/m3 increase in PM2.5 levels caused a 2.3% rise in the risk of ACS, while in China, high concentrations of PM2.5 determined an increase in cardiovascular morbidity and mortality [74, 75]. In New York, each 7.1 μg/m3 increase in PM2.5 concentration was associated with an 18% increase in STEMI risk [76]. A 10 μg /m3 increase in PM10 concentration was associated with high UA hospitalizations [77]. In industrial areas of Poland, exposure to high levels of gaseous pollutants (NO2, SO2, CO) and fine particulate matter (PM10, PM2.5) increased the incidence of STEMI, while NSTEMI hospitalizations were related to high NO2 concentrations in both industrial and non-industrial areas [78]. Data on the importance of O3 on ACS is inconclusive [79, 80]. Table 2 summarizes the main epidemiological studies that analyze the impact of air pollutants on cardiovascular diseases, especially on ACS.
Table 2.
Main studies that analyze the role of air pollutants on cardiovascular disease, especially on acute coronary syndrome
| Author | Location | Study period | Study population | Air pollutants analyzed | Air pollutants with effect on ACS/death | Result |
|---|---|---|---|---|---|---|
| Long-term exposure to air pollution | ||||||
| Pope et al. [65] | USA | 1982, follow-up 16 years | Random samples of adults | PM, sulfate, NO2, SO2, O3, CO | PM, sulfate | ↑ risk of all-cause, cardiopulmonary, and lung cancer mortality |
| Tonne et al. [66] | England and Wales | 2004–2007, average follow-up 3.7 years | Patients with ACS | PM10, PM2.5, NO2, NOX | PM2.5 | ↑ risk of all-cause mortality |
| Cesaroni et al. [67] | Germany, Finland, Denmark, Sweden, and Italy | 1997–2007, average follow-up 11.5 years | Patients with ACS | PM10, PM2.5, NO2, NOX | PM10, PM2.5 | ↑ risk of coronary events |
| Short-term exposure to air pollution | ||||||
| Bhaskaran et al. [69] | England and Wales | 2003–2006 | Patients with MI | PM10, NO2, SO2, O3, CO | PM10, NO2 | ↑ risk of MI |
| Butland et al. [70] | England and Wales | 2003–2010 | Patients with STEMI, NSTEMI | PM10, PM2.5, NO2, O3 | NO2 | ↑ risk of NSTEMI |
| Wang et al. [71] | Alberta (Canada) | 1999–2010 | Patients with STEMI, NSTEMI | PM2.5, NO2, O3, NO, CO | NO2 | ↑ risk of NSTEMI |
| Vaudrey et al. [72] | Strasbourg (France) | 2012–2014 | Patients with coronary events | PM10, PM2.5, NO2 | NO2 | ↑ risk of coronary events |
| Sahlén et al [73] | Stockholm (Sweden) | 2000–2014 | Patients with MI | PM10, PM2.5, NO2, SO2, O3 | NO2 | ↑ risk of STEMI |
| Belleudi et al. [74] | Rome (Italy) | 2001–2005 | Patients with CVD | PM10, PM2.5, UFP | PM10, PM2.5 | ↑ risk of ACS |
| Amsalu et al. [75] | Beijing (China) | 2013–2017 | Patients with CVD | PM2.5, NO2, SO2, O3, CO | PM2.5 | ↑ risk of CVD |
| Gardner et al. [76] | Rochester (New York) | 2007–2010 | Patients with STEMI, NSTEMI | PM2.5, UFP | PM2.5 | ↑ risk of STEMI |
| Kuźma et al. [77] | Bialystok (Poland) | 2008–2017 | Patients with ACS | PM10, PM2.5, NO2, SO2 | PM10 | ↑ risk of ACS |
| Kuźma et al. [78] | Poland | 2008–2017 | Patients with ACS | PM10, PM2.5, NO2, SO2, CO | PM10, PM2.5, NO2, SO2, CO | ↑ risk of STEMI, NSTEMI |
| Argacha et al. [79] | Belgia | 2009–2013 | Patients with STEMI | PM10, PM2.5, NO2, O3 | PM10, PM2.5, NO2, | ↑ risk of STEMI |
| Ruidavets et al. [80] | Toulouse (France) | 1997–1999 | Patients with AMI | NO2, SO2, O3 | O3 | ↑ risk of AMI |
ACS acute coronary syndrome, PM particulate matter, NO2 nitrogen dioxide, SO2 sulfur dioxide, O3 ozone, CO carbon monoxide, PM10 particulate matter with an aerodynamic diameter ≤ 10 μm, PM2.5 particulate matter with an aerodynamic diameter ≤ 2.5 μm, NOx nitrogen oxides, MI myocardial infarction, STEMI ST-elevation myocardial infarction, NSTEMI non-ST-elevation myocardial infarction, NO nitrogen monoxide, CVD cardiovascular disease, UFP ultrafine particles
Pathophysiological Mechanisms of Air Pollutants
Several pathophysiological mechanisms by which air pollution can influence the occurrence of acute coronary events have been described. Exposure to high concentrations of air pollutants has been shown to cause a systemic inflammatory response, vascular dysfunction and vasoconstriction, increased heart rate and blood pressure, changes in clotting processes, and dysfunction of the sympathetic-parasympathetic systems [81, 82]. Elevated PM10 and PM2.5 levels have also been associated with elevated endothelin levels [83]. Increased blood pressure has been observed in patients undergoing cardiac rehabilitation after exposure to high atmospheric concentrations of PM2.5 [84]. The effects of air pollutants on the risk of AMI were also studied in the field of mechanics. Short-term exposure (1 h) to exhaust gases has been shown to induce a prothrombotic and proischemic effect in patients with CHD [85].
The process by which these pathophysiological mechanisms may differently affect the occurrence of ACS subtypes remains debatable. STEMI and NSTEMI mechanics are not the same. STEMI appears after total occlusion of the vessel as a result of ruptured atheroma plaque with added thrombosis, whereas NSTEMI is distinguished by partial occlusion of the coronary arteries or the appearance of an imbalance between demand and oxygen supply in the myocardium. UA and NSTEMI have similar pathogenic mechanisms, with the difference that myocardial necrosis is not present in UA [86]. Some epidemiological data showed an increase in the number of STEMI cases after exposure to high concentrations of PM2.5, while other research reported a correlation between NO2 exposure and an increased incidence of NSTEMI [70, 71, 76]. It is supposed that PM2.5 air pollutants would stimulate the thrombotic process after atherosclerotic plaque rupture or that they would affect the thrombolysis process, resulting in complete occlusion of the vessel [76]. NO2 appears to be involved in endothelial dysfunction, prothrombotic and proinflammatory effects, causing ACS [85–87]. Figure 1b summarizes the pathophysiological mechanisms of air pollutants on ACS subtypes. Further clinical and experimental studies are needed to analyze in detail the role of each air pollutant in the occurrence of ACS subtypes.
Acute Coronary Syndrome and Air Pollution During the COVID-19 Pandemic
The new coronavirus, also called SARS-CoV-2, was first reported in December 2019 in Wuhan, China. The COVID-19 infection spread quickly, and the WHO declared it a global pandemic on March 11, 2020. This viral infection has caused more than 5.9 million deaths as of March 6, 2022 [88]. The lockdown imposed at the beginning of 2020 in most countries, as a measure of protection against infection with the new coronavirus, determined a decrease in the concentration of air pollutants, economic and social imbalances, increasing cases of depression and anxiety among the population, and uncertainty in the medical and scientific world [89, 90]. Recent reports have shown a definite correlation between COVID-19 infections and high levels of air pollution. Thus, air pollutants can facilitate the transport and spread of the SARS-CoV-2 virus [91•]. Both air pollution and COVID-19 infection may provoke a systemic inflammatory response, a procoagulant effect, endothelial dysfunction, increased oxidative stress, and an imbalance between the demand and oxygen supply in the cells, all of which favor the progression of atherosclerosis and unstable plaque rupture [81–87, 92, 93].
A decrease in the number of ACS hospitalizations was observed during the COVID-19 pandemic and lockdown period. In Austria and the USA, the number of STEMI/AMI cases decreased by 40% in the first half of 2020 [94, 95]. In Italy, NSTEMI cases were reduced by 65.1%, while STEMI admissions decreased by 26.5% [96]. There was also an increase in out-of-hospital cardiovascular mortality, as well as numerous complications of AMI, due to late presentation to an emergency department (5 h after the onset of symptoms, compared to 1 h and a half in 2018–2019) [97].
Several theories have been proposed to justify the sudden reduction in ACS cases during the COVID-19 pandemic. One possible cause is the patient’s fear of SARS-CoV-2 virus infection during a hospital visit. Another explanation could be the ignoring of patients with mild angina symptoms or stable CHD by medical staff overwhelmed by COVID-19 cases. The reduced number of ACS could be a result of less stress at work and congested traffic, a healthy lifestyle, reduced alcohol consumption, less smoking, increased adherence to medication, and improved air quality during the lockdown period [89].
The COVID-19 pandemic and the lockdown imposed in most countries of the world caused an increase in depression and anxiety cases, as well as socio-economic imbalances. Both SARS-CoV-2 virus infection and high concentrations of air pollutants may be risk factors for acute coronary events. It is possible that in the future, climate change and increased emissions of air pollutants could cause significant economic damage and far more deaths than the SARS-CoV-2 virus infection.
Conclusions
ACS remains the main cause of death worldwide. Air temperature fluctuations in the global warming era as well as increased emissions of air pollutants have a major impact on acute coronary events. Cardiac patients are much more vulnerable to exacerbations of pre-existing heart disease, especially on days with extreme temperatures and sudden changes in air pressure or during periods of high air pollution. It is necessary to identify patients at risk and warn them in advance about weather variations in order to reduce the number of hospitalizations and the costs borne by public health programs. At present, the industrialization era and the growing population cause a constant increase in air pollution worldwide. Thus, the number of ACS caused by air pollution is expected to increase dramatically in the next few years.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Global Cardiovascular Health
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Andreea-Alexandra Rus, Email: andreearus2@yahoo.com.
Cristian Mornoş, Email: mornoscristi@yahoo.com.
References
Recent references of major interest have been highlighted as: • Of importance •• Of major importance
- 1.Mensah GA, Roth GA, Fuster V. The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J Am Coll Cardiol. 2019;74(20):2529–2532. doi: 10.1016/j.jacc.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 2.Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD. Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed]
- 4.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steg PG, Goldberg RJ, Gore JM, Fox KA, Eagle KA, Flather MD, et al. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (GRACE) Am J Cardiol. 2002;90(4):358–363. doi: 10.1016/s0002-9149(02)02489-x. [DOI] [PubMed] [Google Scholar]
- 6.Dharma S, Andriantoro H, Dakota I, Purnawan I, Pratama V, Isnanijah H, et al. Organisation of reperfusion therapy for STEMI in a developing country. Open Heart. 2015;2(1):e000240. doi: 10.1136/openhrt-2015-000240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362(23):2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 8.Puymirat E, Simon T, Cayla G, Cottin Y, Elbaz M, Coste P, et al. Acute myocardial infarction: changes in patient characteristics, management, and 6-month outcomes over a period of 20 years in the FAST-MI Program (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) 1995 to 2015. Circulation. 2017;136(20):1908–1919. doi: 10.1161/CIRCULATIONAHA.117.030798. [DOI] [PubMed] [Google Scholar]
- 9.Culić V. Acute risk factors for myocardial infarction. Int J Cardiol. 2007;117(2):260–269. doi: 10.1016/j.ijcard.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 10.Gostimirovic M, Novakovic R, Rajkovic J, Djokic V, Terzic D, Putnik S, et al. The influence of climate change on human cardiovascular function. Arch Environ Occup Health. 2020;75(7):406–414. doi: 10.1080/19338244.2020.1742079. [DOI] [PubMed] [Google Scholar]
- 11.WMO. Statement on the State of the Global Climate in 2017, WMO-No. 1212, 2017:4.
- 12.Rosahn PD. Incidence of coronary thrombosis in relation to climate. JAMA. 1937;109(16):1294. doi: 10.1001/jama.1937.02780420054021. [DOI] [Google Scholar]
- 13.Nemery B, Hoet PH, Nemmar A. The Meuse Valley fog of 1930: an air pollution disaster. Lancet. 2001;357(9257):704–708. doi: 10.1016/S0140-6736(00)04135-0. [DOI] [PubMed] [Google Scholar]
- 14.LOGAN WP. Mortality in the London fog incident, 1952. Lancet. 1953;1(6755):336–8. 10.1016/s0140-6736(53)91012-5. [DOI] [PubMed]
- 15.Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet. 2017;389(10065):197–210. doi: 10.1016/S0140-6736(16)30677-8. [DOI] [PubMed] [Google Scholar]
- 16.Auger N, Potter BJ, Smargiassi A, Bilodeau-Bertrand M, Paris C, Kosatsky T. Association between quantity and duration of snowfall and risk of myocardial infarction. CMAJ. 2017;189(6):E235–E242. doi: 10.1503/cmaj.161064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spencer FA, Goldberg RJ, Becker RC, Gore JM. Seasonal distribution of acute myocardial infarction in the second National Registry of Myocardial Infarction. J Am Coll Cardiol. 1998;31(6):1226–1233. doi: 10.1016/s0735-1097(98)00098-9. [DOI] [PubMed] [Google Scholar]
- 18.Sheth T, Nair C, Muller J, Yusuf S. Increased winter mortality from acute myocardial infarction and stroke: the effect of age. J Am Coll Cardiol. 1999;33(7):1916–1919. doi: 10.1016/s0735-1097(99)00137-0. [DOI] [PubMed] [Google Scholar]
- 19.Danet S, Richard F, Montaye M, Beauchant S, Lemaire B, Graux C, et al. Unhealthy effects of atmospheric temperature and pressure on the occurrence of myocardial infarction and coronary deaths. A 10-year survey: the Lille-World Health Organization MONICA project (Monitoring trends and determinants in cardiovascular disease). Circulation. 1999;100(1):E1–7. 10.1161/01.cir.100.1.e1. [DOI] [PubMed]
- 20.Swampillai J, Wijesinghe N, Sebastian C, Devlin GP. Seasonal variations in hospital admissions for ST-elevation myocardial infarction in New Zealand. Cardiol Res. 2012;3(5):205–208. doi: 10.4021/cr223e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rumana N, Kita Y, Turin TC, Murakami Y, Sugihara H, Morita Y, et al. Seasonal pattern of incidence and case fatality of acute myocardial infarction in a Japanese population (from the Takashima AMI Registry, 1988 to 2003) Am J Cardiol. 2008;102(10):1307–1311. doi: 10.1016/j.amjcard.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 22.Ogbebor O, Odugbemi B, Maheswaran R, Patel K. Seasonal variation in mortality secondary to acute myocardial infarction in England and Wales: a secondary data analysis. BMJ Open. 2018;8(7):e019242. doi: 10.1136/bmjopen-2017-019242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vasconcelos J, Freire E, Almendra R, Silva GL, Santana P. The impact of winter cold weather on acute myocardial infarctions in Portugal. Environ Pollut. 2013;183:14–18. doi: 10.1016/j.envpol.2013.01.037. [DOI] [PubMed] [Google Scholar]
- 24.Dilaveris P, Synetos A, Giannopoulos G, Gialafos E, Pantazis A, Stefanadis C. Climate impacts on myocardial infarction deaths in the Athens TErritory: the CLIMATE study. Heart. 2006;92(12):1747–1751. doi: 10.1136/hrt.2006.091884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sharovsky R, Cé sar LA. Increase in mortality due to myocardial infarction in the Brazilian city of São Paulo during winter. Arq Bras Cardiol. 2002;78(1):106–9. 10.1590/s0066-782x2002000100009. [DOI] [PubMed]
- 26.Yamaji K, Kohsaka S, Morimoto T, Fujii K, Amano T, Uemura S, et al. Relation of ST-segment elevation myocardial infarction to daily ambient temperature and air pollutant levels in a Japanese nationwide percutaneous coronary intervention registry. Am J Cardiol. 2017;119(6):872–880. doi: 10.1016/j.amjcard.2016.11.041. [DOI] [PubMed] [Google Scholar]
- 27.Kloner RA. The “Merry Christmas Coronary” and “Happy New Year Heart Attack” phenomenon. Circulation. 2004;110(25):3744–3745. doi: 10.1161/01.CIR.0000151786.03797.18. [DOI] [PubMed] [Google Scholar]
- 28.Akioka H, Yufu K, Teshima Y, Kawano K, Ishii Y, Abe I, et al. Seasonal variations of weather conditions on acute myocardial infarction onset: Oita AMI Registry. Heart Vessels. 2019;34(1):9–18. doi: 10.1007/s00380-018-1213-6. [DOI] [PubMed] [Google Scholar]
- 29.Chen K, Breitner S, Wolf K, Hampel R, Meisinger C, Heier M, et al. Temporal variations in the triggering of myocardial infarction by air temperature in Augsburg, Germany, 1987–2014. Eur Heart J. 2019;40(20):1600–1608. doi: 10.1093/eurheartj/ehz116. [DOI] [PubMed] [Google Scholar]
- 30.Nastos PT, Giaouzaki KN, Kampanis NA, Matzarakis A. Acute coronary syndromes related to bio-climate in a Mediterranean area. The case of Ierapetra, Crete Island, Greece. Int J Environ Health Res. 2013;23(1):76–90. 10.1080/09603123.2012.699031. [DOI] [PubMed]
- 31.Madrigano J, Mittleman MA, Baccarelli A, Goldberg R, Melly S, von Klot S, et al. Temperature, myocardial infarction, and mortality: effect modification by individual- and area-level characteristics. Epidemiology. 2013;24(3):439–446. doi: 10.1097/EDE.0b013e3182878397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pan WH, Li LA, Tsai MJ. Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet. 1995;345(8946):353–355. doi: 10.1016/s0140-6736(95)90341-0. [DOI] [PubMed] [Google Scholar]
- 33.Liang WM, Liu WP, Chou SY, Kuo HW. Ambient temperature and emergency room admissions for acute coronary syndrome in Taiwan. Int J Biometeorol. 2008;52(3):223–229. doi: 10.1007/s00484-007-0116-5. [DOI] [PubMed] [Google Scholar]
- 34.Guo S, Niu Y, Cheng Y, Chen R, Kan J, Kan H, et al. Association between ambient temperature and daily emergency hospitalizations for acute coronary syndrome in Yancheng. China Environ Sci Pollut Res Int. 2020;27(4):3885–3891. doi: 10.1007/s11356-019-07084-9. [DOI] [PubMed] [Google Scholar]
- 35.Panagiotakos DB, Chrysohoou C, Pitsavos C, Nastos P, Anadiotis A, Tentolouris C, et al. Climatological variations in daily hospital admissions for acute coronary syndromes. Int J Cardiol. 2004;94(2–3):229–233. doi: 10.1016/j.ijcard.2003.04.050. [DOI] [PubMed] [Google Scholar]
- 36.Wang H, Kakehashi M, Matsumura M, Eboshida A. [Association between occurrence of acute myocardial infarction and meteorological factors]. J Cardiol. 2007;49(1):31–40. Japanese. PMID: 17269211. [PubMed]
- 37.Hong Y, Graham MM, Rosychuk RJ, Southern D, McMurtry MS. The effects of acute atmospheric pressure changes on the occurrence of ST-elevation myocardial infarction: a case-crossover study. Can J Cardiol. 2019;35(6):753–760. doi: 10.1016/j.cjca.2019.02.015. [DOI] [PubMed] [Google Scholar]
- 38.Honda T, Fujimoto K, Miyao Y. Infuence of weather conditions on the frequent onset of acute myocardial infarction. J Cardiol. 2016;67:42–50. doi: 10.1016/j.jjcc.2015.02.013. [DOI] [PubMed] [Google Scholar]
- 39.Bijelović S, Dragić N, Bijelović M, Kovačević M, Jevtić M, Ninkovic Mrđenovački O. Impact of climate conditions on hospital admissions for subcategories of cardiovascular diseases. Med Pr. 2017;68(2):189–197. English. 10.13075/mp.5893.00606. [DOI] [PubMed]
- 40.Schwartz J, Samet JM, Patz JA. Hospital admissions for heart disease: the effects of temperature and humidity. Epidemiology. 2004;15(6):755–761. doi: 10.1097/01.ede.0000134875.15919.0f. [DOI] [PubMed] [Google Scholar]
- 41.Takagi H, Hari Y, Nakashima K, Kuno T, Ando T; ALICE (All-Literature Investigation of Cardiovascular Evidence) Group. Wind and coronary artery disease. Eur J Prev Cardiol. 2020;27(19):2259–2263. 10.1177/2047487319885195. [DOI] [PubMed]
- 42.Goerre S, Egli C, Gerber S, Defila C, Minder C, Richner H, et al. Impact of weather and climate on the incidence of acute coronary syndromes. Int J Cardiol. 2007;118(1):36–40. doi: 10.1016/j.ijcard.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 43.Versaci F, Biondi-Zoccai G, Giudici AD, Mariano E, Trivisonno A, Sciarretta S, Valenti V, Peruzzi M, Cavarretta E, Frati G, Scappaticci M, Federici M, Romeo F. Climate changes and ST-elevation myocardial infarction treated with primary percutaneous coronary angioplasty. Int J Cardiol. 2019;1(294):1–5. doi: 10.1016/j.ijcard.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 44.Mohammad MA, Koul S, Rylance R, Fröbert O, Alfredsson J, Sahlén A, et al. Association of weather with day-to-day incidence of myocardial infarction: a SWEDEHEART nationwide observational study. JAMA Cardiol. 2018;3(11):1081–1089. doi: 10.1001/jamacardio.2018.3466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leibowitz D, Planer D, Weiss T, Rott D. Seasonal variation in myocardial infarction is limited to patients with ST-elevations on admission. Chronobiol Int. 2007;24(6):1241–1247. doi: 10.1080/07420520701800611. [DOI] [PubMed] [Google Scholar]
- 46.Steadman RG. Norms of apparent temperature in Australia. Aust Meteorol Mag. 1994;43:1–16. [Google Scholar]
- 47.Baccini M, Biggeri A, Accetta G, Kosatsky T, Katsouyanni K, Analitis A, et al. Heat effects on mortality in 15 European cities. Epidemiology. 2008;19(5):711–719. doi: 10.1097/EDE.0b013e318176bfcd. [DOI] [PubMed] [Google Scholar]
- 48.Moghadamnia MT, Ardalan A, Mesdaghinia A, Naddafi K, Yekaninejad MS. Association between apparent temperature and acute coronary syndrome admission in Rasht. Iran Heart Asia. 2018;10(2):e011068. doi: 10.1136/heartasia-2018-011068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wichmann J, Ketzel M, Ellermann T, Loft S. Apparent temperature and acute myocardial infarction hospital admissions in Copenhagen, Denmark: a case-crossover study. Environ Health. 2012;30(11):19. doi: 10.1186/1476-069X-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.•• Li N, Ma J, Liu F, Zhang Y, Ma P, Jin Y, et al. Associations of apparent temperature with acute cardiac events and subtypes of acute coronary syndromes in Beijing, China. Sci Rep. 2021;11(1):15229. 10.1038/s41598-021-94738-9. Findings from this research show that both high and low apparent temperatures increase the risk of STEMI and NSTEMI admissions. [DOI] [PMC free article] [PubMed]
- 51.Kurihara O, Takano M, Yamamoto E, Yonetsu T, Kakuta T, Soeda T, et al. Seasonal variations in the pathogenesis of acute coronary syndromes. J Am Heart Assoc. 2020;9(13):e015579. doi: 10.1161/JAHA.119.015579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shibuya J, Kobayashi N, Asai K, Tsurumi M, Shibata Y, Uchiyama S, et al. Comparison of coronary culprit lesion morphology determined by optical coherence tomography and relation to outcomes in patients diagnosed with acute coronary syndrome during winter -vs- other seasons. Am J Cardiol. 2019;124(1):31–38. doi: 10.1016/j.amjcard.2019.03.045. [DOI] [PubMed] [Google Scholar]
- 53.Kloner RA, Das S, Poole WK, Perrit R, Muller J, Cannon CP, et al. Seasonal variation of myocardial infarct size. Am J Cardiol. 2001;88(9):1021–1024. doi: 10.1016/s0002-9149(01)01981-6. [DOI] [PubMed] [Google Scholar]
- 54.Liu C, Yavar Z, Sun Q. Cardiovascular response to thermoregulatory challenges. Am J Physiol Heart Circ Physiol. 2015;309(11):H1793–H1812. doi: 10.1152/ajpheart.00199.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kysely J, Pokorna L, Kyncl J, Kriz B. Excess cardiovascular mortality associated with cold spells in the Czech Republic. BMC Public Health. 2009;15(9):19. doi: 10.1186/1471-2458-9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schneider A, Panagiotakos D, Picciotto S, Katsouyanni K, Löwel H, Jacquemin B, et al. Air temperature and inflammatory responses in myocardial infarction survivors. [DOI] [PubMed]
- 57.Keatinge WR, Coleshaw SR, Cotter F, Mattock M, Murphy M, Chelliah R. Increases in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: factors in mortality from coronary and cerebral thrombosis in winter. Br Med J (Clin Res Ed) 1984;289(6456):1405–1408. doi: 10.1136/bmj.289.6456.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Keatinge WR, Coleshaw SR, Easton JC, Cotter F, Mattock MB, Chelliah R. Increased platelet and red cell counts, blood viscosity, and plasma cholesterol levels during heat stress, and mortality from coronary and cerebral thrombosis. Am J Med. 1986;81(5):795–800. doi: 10.1016/0002-9343(86)90348-7. [DOI] [PubMed] [Google Scholar]
- 59.Furukawa Y. Meteorological factors and seasonal variations in the risk of acute myocardial infarction. Int J Cardiol. 2019;1(294):13–14. doi: 10.1016/j.ijcard.2019.07.089. [DOI] [PubMed] [Google Scholar]
- 60.Denda M. Keratinocytes at the uppermost layer of epidermis might act as sensors of atmospheric pressure change. Extrem Physiol Med. 2016;6(5):11. doi: 10.1186/s13728-016-0052-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.World Health Organization. World Health Assembly closes, passing resolutions on air pollution and epilepsy. 2015; Available from: https://apps.who.int/mediacentre/news/releases/2015/wha-26-may-2015/en/index.html
- 62.World Health Organization. Ambient (outdoor) air quality and health. 2021; Available from: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health#:~:text=Ambient%20(outdoor)%20air%20pollution%20in,and%20respiratory%20disease%2C%20and%20cancers.
- 63.Manisalidis I, Stavropoulou E, Stavropoulos A, Bezirtzoglou E. Environmental and health impacts of air pollution: a review. Front Public Health. 2020;20(8):14. doi: 10.3389/fpubh.2020.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Markandya A, Sampedro J, Smith SJ, Van Dingenen R, Pizarro-Irizar C, Arto I, González-Eguino M. Health co-benefits from air pollution and mitigation costs of the Paris Agreement: a modelling study. Lancet Planet Health. 2018;2(3):e126–e133. doi: 10.1016/S2542-5196(18)30029-9. [DOI] [PubMed] [Google Scholar]
- 65.Pope CA, 3rd, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA. 2002;287(9):1132–1141. doi: 10.1001/jama.287.9.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tonne C, Wilkinson P. Long-term exposure to air pollution is associated with survival following acute coronary syndrome. Eur Heart J. 2013;34(17):1306–1311. doi: 10.1093/eurheartj/ehs480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cesaroni G, Forastiere F, Stafoggia M, Andersen ZJ, Badaloni C, Beelen R, et al. Long term exposure to ambient air pollution and incidence of acute coronary events: prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ. 2014;21(348):f7412. doi: 10.1136/bmj.f7412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.• Zou L, Zong Q, Fu W, Zhang Z, Xu H, Yan S, et al. Long-Term Exposure to Ambient air pollution and myocardial infarction: a systematic review and meta-analysis. Front Med (Lausanne). 2021;17(8):616355. 10.3389/fmed.2021.616355. Findings from this meta-analysis show that PM2.5 has a much more harmful effect on the risk of acute coronary syndrome than PM10. [DOI] [PMC free article] [PubMed]
- 69.Bhaskaran K, Hajat S, Armstrong B, Haines A, Herrett E, Wilkinson P, et al. The effects of hourly differences in air pollution on the risk of myocardial infarction: case crossover analysis of the MINAP database. BMJ. 2011;20(343):d5531. doi: 10.1136/bmj.d5531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Butland BK, Atkinson RW, Milojevic A, Heal MR, Doherty RM, Armstrong BG, et al. Myocardial infarction, ST-elevation and non-ST-elevation myocardial infarction and modelled daily pollution concentrations: a case-crossover analysis of MINAP data. Open Heart. 2016;3(2):e000429. doi: 10.1136/openhrt-2016-000429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang X, Kindzierski W, Kaul P. Air pollution and acute myocardial infarction hospital admission in Alberta, Canada: a three-step procedure case-crossover study. PLoS ONE. 2015;10(7):e0132769. doi: 10.1371/journal.pone.0132769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vaudrey B, Mielcarek M, Sauleau E, Meyer N, Marchandot B, Moitry M, et al. Short-term effects of air pollution on coronary events in Strasbourg, France-importance of seasonal variations. Med Sci (Basel) 2020;8(3):31. doi: 10.3390/medsci8030031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sahlén A, Ljungman P, Erlinge D, Chan MY, Yap J, Hausenloy DJ, et al. Air pollution in relation to very short-term risk of ST-segment elevation myocardial infarction: case-crossover analysis of SWEDEHEART. Int J Cardiol. 2019;15(275):26–30. doi: 10.1016/j.ijcard.2018.10.069. [DOI] [PubMed] [Google Scholar]
- 74.Belleudi V, Faustini A, Stafoggia M, Cattani G, Marconi A, Perucci CA, et al. Impact of fine and ultrafine particles on emergency hospital admissions for cardiac and respiratory diseases. Epidemiology. 2010;21(3):414–423. doi: 10.1097/EDE.0b013e3181d5c021. [DOI] [PubMed] [Google Scholar]
- 75.Amsalu E, Wang T, Li H, Liu Y, Wang A, Liu X, et al. Acute effects of fine particulate matter (PM2.5) on hospital admissions for cardiovascular disease in Beijing, China: a time-series study. Environ Health. 2019;18(1):70. 10.1186/s12940-019-0506-2. [DOI] [PMC free article] [PubMed]
- 76.Gardner B, Ling F, Hopke PK, Frampton MW, Utell MJ, Zareba W, et al. Ambient fine particulate air pollution triggers ST-elevation myocardial infarction, but not non-ST elevation myocardial infarction: a case-crossover study. Part Fibre Toxicol. 2014;2(11):1. doi: 10.1186/1743-8977-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kuźma Ł, Pogorzelski S, Struniawski K, Dobrzycki S, Bachórzewska-Gajewska H. Effect of air pollution on the number of hospital admissions for acute coronary syndrome in elderly patients. Pol Arch Intern Med. 2020;130(1):38–46. doi: 10.20452/pamw.15064. [DOI] [PubMed] [Google Scholar]
- 78.Kuźma Ł, Wańha W, Kralisz P, Kazmierski M, Bachórzewska-Gajewska H, Wojakowski W, et al. Impact of short-term air pollution exposure on acute coronary syndrome in two cohorts of industrial and non-industrial areas: A time series regression with 6,000,000 person-years of follow-up (ACS - Air Pollution Study) Environ Res. 2021;197:111154. doi: 10.1016/j.envres.2021.111154. [DOI] [PubMed] [Google Scholar]
- 79.Argacha JF, Collart P, Wauters A, Kayaert P, Lochy S, Schoors D, et al. Air pollution and ST-elevation myocardial infarction: a case-crossover study of the Belgian STEMI registry 2009–2013. Int J Cardiol. 2016;15(223):300–305. doi: 10.1016/j.ijcard.2016.07.191. [DOI] [PubMed] [Google Scholar]
- 80.Ruidavets JB, Cournot M, Cassadou S, Giroux M, Meybeck M, Ferrières J. Ozone air pollution is associated with acute myocardial infarction. Circulation. 2005;111(5):563–569. doi: 10.1161/01.CIR.0000154546.32135.6E. [DOI] [PubMed] [Google Scholar]
- 81.Bhaskaran K, Wilkinson P, Smeeth L. Cardiovascular consequences of air pollution: what are the mechanisms? Heart. 2011;97(7):519–520. doi: 10.1136/hrt.2010.212183. [DOI] [PubMed] [Google Scholar]
- 82.Robertson S, Miller MR. Ambient air pollution and thrombosis. Part Fibre Toxicol. 2018;15(1):1. doi: 10.1186/s12989-017-0237-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Brook RD, Brook JR, Urch B, Vincent R, Rajagopalan S, Silverman F. Inhalation of fine particulate air pollution and ozone causes acute arterial vasoconstriction in healthy adults. Circulation. 2002;105(13):1534–1536. doi: 10.1161/01.cir.0000013838.94747.64. [DOI] [PubMed] [Google Scholar]
- 84.Zanobetti A, Canner MJ, Stone PH, Schwartz J, Sher D, Eagan-Bengston E, et al. Ambient pollution and blood pressure in cardiac rehabilitation patients. Circulation. 2004;110(15):2184–2189. doi: 10.1161/01.CIR.0000143831.33243.D8. [DOI] [PubMed] [Google Scholar]
- 85.Mills NL, Törnqvist H, Gonzalez MC, Vink E, Robinson SD, Söderberg S, et al. Ischemic and thrombotic effects of dilute diesel-exhaust inhalation in men with coronary heart disease. N Engl J Med. 2007;357(11):1075–1082. doi: 10.1056/NEJMoa066314. [DOI] [PubMed] [Google Scholar]
- 86.Libby P. Current concepts of the pathogenesis of the acute coronary syndromes. Circulation. 2001;104(3):365–372. doi: 10.1161/01.cir.104.3.365. [DOI] [PubMed] [Google Scholar]
- 87.Rückerl R, Greven S, Ljungman P, Aalto P, Antoniades C, Bellander T, et al. Air pollution and inflammation (interleukin-6, C-reactive protein, fibrinogen) in myocardial infarction survivors. Environ Health Perspect. 2007;115(7):1072–1080. doi: 10.1289/ehp.10021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.World Health Organization. Weekly epidemiological update on COVID-19 - 8 March 2022. 2022; Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---8-march-2022
- 89.Kulkarni P, Mahadevappa M. COVID-19 pandemic and the reduction in ST-elevation myocardial infarction admissions. Postgrad Med J. 2020;96(1137):436–437. doi: 10.1136/postgradmedj-2020-137895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gorini F, Chatzianagnostou K, Mazzone A, Bustaffa E, Esposito A, Berti S, et al. “Acute myocardial infarction in the time of COVID-19”: a review of biological, environmental, and psychosocial contributors. Int J Environ Res Public Health. 2020;17(20):7371. doi: 10.3390/ijerph17207371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.• Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, et al. SARS-Cov-2RNA found on particulate matter of Bergamo in Northern Italy: first evidence. Environ Res. 2020;188:109754. 10.1016/j.envres.2020.109754. Findings from this research show that particulate matter can facilitate the transport and spread of the SARS-CoV-2 virus. [DOI] [PMC free article] [PubMed]
- 92.Coperchini F, Chiovato L, Croce L, Magri F, Rotondi M. The cytokine storm in COVID-19: an overview of the involvement of the chemokine/chemokine-receptor system. Cytokine Growth Factor Rev. 2020;53:25–32. doi: 10.1016/j.cytogfr.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Violi F, Pastori D, Cangemi R, Pignatelli P, Loffredo L. Hypercoagulation and antithrombotic treatment in coronavirus 2019: a new challenge. Thromb Haemost. 2020;120(6):949–956. doi: 10.1055/s-0040-1710317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41(19):1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41(22):2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]