Abstract
Study design
Retrospective population-based cohort study.
Objectives
To determine the incidence and mortality of spinal cord injuries (SCI) in the Piedmont Region of Northwestern Italy.
Setting
Publicly-funded SCI rehabilitation centres in the Piedmont Region.
Methods
Administrative databases were used to identify individuals at their first admission to a SCI rehabilitation centre from January 1st, 2008 to December 31st, 2020. Cases were stratified by age and aetiology (traumatic SCI, TSCI; non-traumatic SCI, NTSCI). Age- and aetiology-specific incidence rate and person-year mortality rates were calculated for each year. Case lethality was reported as deaths among prevalent cases for each year.
Results
A total of 892 cases were identified (56.4% TSCI). The average annual crude incidence rate was 17.9 per million population, decreasing from 26.0 in 2008 to 10.8 in 2020. Young adults and the elderly represented the majority of TSCI and NTSCI cases, respectively. Of the 235 individuals who died during the study period, 58.3% had NTSCI. The mortality rate per 1000 person-years decreased from 16.3 in 2009 to 8.5 in 2020, while case lethality more than tripled (from 17.2 in 2009 to 57.1 in 2020).
Conclusions
We identified a decreasing trend in SCI incidence and mortality rates, with an increased case lethality over the study period, especially in NTSCI. Given these changes in the epidemiology of SCI, community services offered after rehabilitation should be strengthened to enhance their effectiveness and contribute to increased survival in this population.
Subject terms: Public health, Epidemiology
Introduction
Spinal cord injury (SCI) is a devastating experience that causes neurological impairments involving motor, sensory, and autonomic functions, and places significant burdens on the individuals affected, their family, and the healthcare system [1]. External impacts due to traffic accidents, falls, or violence are the most common cause of traumatic SCI (TSCI), which has a global incidence range of 8 to 55 individuals per million population and a higher prevalence in the US than Northwestern Europe [2]. However, the epidemiology of non-traumatic SCI (NTSCI) due to vascular, neoplastic, or infectious causes is still poorly explored [3]. Indeed, data on NTSCI are very fragmented; it has a global incidence of 6 to 76 cases per million population, and prevalence data are only available in India (Kashmir Region) and Canada [3]. Previous studies have shown that SCI confers an increased risk of mortality and reduced life expectancy when compared to the general population (estimated standardised mortality ratio: 2.45 for TSCI [4] and 1.62 for NTSCI [5]).
Individuals with SCI have complex needs throughout their acute, rehabilitation, and long-term phases, and require specialised multidisciplinary services to maximise their outcomes [6]. In this regard, SCI has high associated direct and indirect costs [7], independent of its aetiology [8]. The primary direct cost driver is the initial rehabilitation phase [9], while high indirect costs are associated with secondary health conditions that occur after discharge from rehabilitation centres [10]. Although epidemiological data is critical in informing healthcare planning and delivery, global data on the incidence, mortality, and prevalence of TSCI and NTSCI are surprisingly scarce [3, 11, 12].
The epidemiology of SCI in Western countries has changed significantly in recent decades, prompting health policy-makers to consider modifications in organisational and clinical rehabilitation approaches [3, 11, 12]. Studies have shown that NTSCI cases have different demographic and clinical characteristics than TSCI cases, including higher median age (55 to 65 years), a less pronounced male-to-female ratio, and a malignant neoplastic or degenerative aetiology [3]. Population ageing has caused substantial increases in the average age at SCI and onset of cervical injuries, especially in countries with higher concentrations of elderly, such as Italy [13, 14]. All these modifications imply that SCI cases have a higher clinical complexity and frailty, and policy-makers are underlining the need for updated information that can be used to identify meaningful changes in the epidemiology of SCI [3, 11].
Previous studies have tried to provide an epidemiological overview of SCI in Italy. A recent prospective study reported TSCI incidence during 1 year (2013 to 2014), examining data from 11 spinal units across Italy [14]. These findings were subsequently used to determine the impact of case characteristics at admission on functional level after SCI rehabilitation and on discharge destination [15]. The GISEM study collected data from 32 SCI rehabilitation centres to describe the Italian situation between 1997 and 1999 [16]. Only one study has examined SCI incidence in Italy retrospectively, focusing on administrative data from a single region in the years 1994 and 1995 [17]. Given the limited number of studies − most of which are dated, focused primarily on TSCI, and examine short periods − the epidemiology of SCI in Italy is very difficult to determine. Moreover, despite their importance in informing health policies, to the best of the authors’ knowledge, no studies have examined SCI mortality in Italy.
Given the paucity of population-based studies, global mapping projects have emphasised the need to collect high-quality regional data on TSCI and NTSCI [3, 11, 12]. Understanding region-specific changes in the epidemiology of TSCI and NTSCI based on population demographics and cultural context is essential to interpreting changes in a timely manner, designing tailored preventive interventions, and providing appropriate care to people with SCI. Thus, this study aimed to retrospectively determine the incidence and mortality of SCI between 2008 and 2020 in the Piedmont Region of Northwestern Italy, using administrative data from official Ministerial Health information systems.
Methods
Setting and data sources
The Italian national health system ensures that all essential care is provided by publicly-funded general practitioners, hospitals, long-term care, and inpatient and outpatient rehabilitation services. The system includes a network of highly-specialised SCI rehabilitation centres (spinal units), with dedicated beds in each region. Piedmont is the second largest of Italy’s 20 regions, covering 25,300 km2, and the seventh most populated (4.3 million inhabitants in 2019). The region hosts three SCI rehabilitation centres (80 beds total), located in the provinces with the highest population density (Fig. 1).
Fig. 1. Spinal cord injury rehabilitation centres in the Piedmont Region.

Map of the Piedmont Region with the three spinal cord injury rehabilitation centres, located in Torino (TO), Novara (NO), and Alessandria (AL).
This retrospective cohort study is based on data from three of the databases that make up the official Italian National Information System. The Hospital Discharge Form database contains information on every individual discharged from all public and private healthcare facilities, including comprehensive clinical information, diagnostic codes (International Classification of Diseases-Ninth Version, ICD-9-CM) and organisational aspects of hospitalisation. We used this database to identify SCI cases. We then linked data from the National Mortality database and the Italian Census database to identify deaths and extract sociodemographic information. Linkage was performed using the universal anonymous patient identifier (ID) code, a univocal code assigned to each individual and used for all corresponding data recorded in Ministerial System Fluxes. These administrative databases represent a systematic and cost-effective way to gather information, and the patient ID allows researchers to link data in an anonymised fashion for epidemiological surveillance without special authorisation. Each Italian Region is responsible for collecting and uploading information to these databases.
Study sample
All individuals admitted to the three SCI rehabilitation centres in the Piedmont Region between January 1, 2008 and December 31, 2020 with TSCI (fracture of vertebral column with SCI: ICD-9-CM codes 806.0 to 806.9; SCI without evidence of spinal bone injury: 952.0 to 952.9) or NTSCI (primary or secondary malignant and benign neoplasms of the spinal cord: ICD-9-CM codes 192.2, 198.3, and 225.3 respectively; myelitis or encephalomyelitis: 323.0 to 323.9; vascular myelopathies: 336.1; non-specified spinal cord disease: 336.9; spinal stenosis other than cervical: 724.0 to 724.09; tuberculoma of spinal cord: 013.4; tuberculous abscess of spinal cord: 013.5; and tuberculous encephalitis or myelitis: 013.6 to 013.66), were eligible for inclusion, regardless of place of residence. Cases younger than 15 years of age at admission were excluded, as were those with vertebral fractures without SCI, isolated nerve roots injuries, autonomic nervous system manifestations, paralysis agitans (332.0), amyotrophic sclerosis (335.2), multiple sclerosis (340.0), spastic hemiplegia and hemiparesis affecting unspecified side (342.1), unspecified infantile cerebral palsy (343.9), locked-in state (344.81), spina bifida occulta (756.17), and those in a persistent vegetative state (780.03). Incident SCI was defined as a first admission to a rehabilitation centre without any previous diagnosis of SCI. All incident SCI cases were followed up until December 2020, and all deaths were registered at the time of the event.
Statistical analyses
Descriptive analyses are reported for each year of the study period (2008 to 2020) by gender, age (in 15-year groups [18]), level of injury (according to ICD-9-CM codes), and aetiology (TSCI and NTSCI). Age-specific, crude incidence rates (number of new cases in each study year) were calculated based on the resident population of the Piedmont Region for each year and expressed as number of cases per million population. To account for differences in the age distribution of SCI incidence, direct standardisation rates with 95% confidence intervals (CIs) were calculated by using 2011 data for the general population of the Piedmont Region, being the latest official Italian census information. As recommended for longitudinal cohort analyses [19] the SCI mortality rate was reported as the number of events occurring in each year of observation divided for the person-years collected up to the year under observation, every 1000 person-years. Person-year rates were calculated for each year of the study period (2008 to 2020) overall, with 95% CIs, and stratified by aetiology. Case lethality rate was calculated as the number of deaths over the cumulative number of living SCI cases in each year, stratified by aetiology, and reported as observed deaths per 1000 cases with 95% CIs. Analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
A total of 892 SCI cases (Table 1) met the inclusion criteria (mean age at injury: 54.5 years, SD ± 17.6; 70.5% male). TSCI cases (n = 503; 56.4%) had a mean age at injury of 50.5 years (SD ± 18.1), were predominantly males (n = 394; 78.3%), and most had paraplegia (n = 275; 54.7%). NTSCI cases (n = 389; 43.6%) were older (mean age at injury 59.6, SD ± 15.4), but also comprised mostly males (n = 233; 59.9%) and people with paraplegia (n = 300; 77.1%). No cases were lost during the follow-up period.
Table 1.
Absolute number, percentage of males, mean age, and standard deviation (SD) of traumatic spinal cord injury (TSCI), non-traumatic spinal cord injury (NTSCI) and overall spinal cord injury (all SCI) from 2008 to 2020. Piedmont Region, Italy.
| TSCI | NTSCI | All SCI | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Year | N | Mean age (SD) | % Males | N | Mean age (SD) | % Males | N | Mean age (SD) | % Males | |
| 2008 | 49 | 47.0 (15.4) | 81.6 | 51 | 58.8 (14.8) | 64.7 | 100 | 53.0 (16.2) | 73.0 | |
| 2009 | 47 | 44.8 (17.1) | 80.8 | 32 | 56.2 (15.1) | 56.2 | 79 | 49.4 (17.1) | 70.9 | |
| 2010 | 57 | 46.9 (16.7) | 80.7 | 35 | 59.1 (12.8) | 71.4 | 92 | 51.6 (16.4) | 77.1 | |
| 2011 | 31 | 47.9 (17.9) | 80.6 | 28 | 56.3 (13.7) | 71.4 | 59 | 51.9 (16.5) | 76.2 | |
| 2012 | 40 | 55.3 (18.4) | 80.0 | 30 | 58.3 (16.1) | 63.3 | 70 | 56.6 (17.4) | 72.9 | |
| 2013 | 39 | 51.5 (18.2) | 84.6 | 25 | 57.0 (16.9) | 64.0 | 64 | 53.7 (17.8) | 76.6 | |
| 2014 | 36 | 51.6 (19.5) | 72.2 | 21 | 61.1 (13.0) | 61.9 | 57 | 55.1 (17.9) | 68.4 | |
| 2015 | 43 | 54.2 (17.5) | 74.4 | 33 | 63.0 (17.0) | 51.5 | 76 | 58.0 (17.7) | 64.5 | |
| 2016 | 40 | 44.3 (19.0) | 77.5 | 33 | 61.0 (16.0) | 51.5 | 73 | 51.8 (19.5) | 65.7 | |
| 2017 | 38 | 48.6 (19.9) | 78.9 | 18 | 60.6 (16.5) | 61.1 | 56 | 52.5 (19.6) | 73.2 | |
| 2018 | 34 | 61.5 (13.3) | 79.4 | 37 | 62.8 (18.6) | 54.1 | 71 | 62.2 (16.2) | 66.2 | |
| 2019 | 28 | 55.4 (19.5) | 67.9 | 26 | 59.1 (15.7) | 50.0 | 54 | 57.1 (17.7) | 59.3 | |
| 2020 | 21 | 54.6 (18.0) | 80.9 | 20 | 62.6 (13.5) | 55.0 | 41 | 58.5 (16.3) | 68.3 | |
| overall | 503 | 50.5 (18.1) | 78.3 | 389 | 59.6 (15.4) | 59.9 | 892 | 54.5 (17.6) | 70.5 | |
SCI Spinal Cord Injury, TSCI traumatic SCI; NTSCI non-traumatic SCI People with SCI having paraplegia were 575 (64.5%), among which 300 in the NTSCI group (77.1%) and 275 in the TSCI group (54.7%)
Incidence
The annual overall SCI incidence rate for 2008 to 2020 was 17.8 cases per million population (Table 2). The TSCI incidence rate was slightly higher than the NTSCI incidence rate, and both rates followed a decreasing trend (12.7 cases per million in 2008 to 5.5 cases in 2020 and 13.3 cases per million in 2008 to 5.3 cases in 2020, respectively).
Table 2.
Age-specific incidence rate, and overall standardised incidence rate of traumatic spinal cord injury (TSCI) and non-traumatic spinal cord injury (NTSCI) per million of population, from 2008 to 2020. Piedmont Region, Italy.
| Age group | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 15 to 29 years | 30 to 44 years | 45 to 59 years | 60 to 74 years | >75 years | All TSCI | All NTSCI | STD Overall | ||||||
| Year | TSCI | NTSCI | TSCI | NTSCI | TSCI | NTSCI | TSCI | NTSCI | TSCI | NTSCI | Incidence | Incidence | Incidence |
| Rate (n) | Rate (n) | Rate (n) | Rate (n) | Rate (n) | Rate (n) | Rate (n) | Rate (n) | Rate (n) | Rate (n) | Rate (n) | Rate (n) | Rate (n) | |
| 2008 | 9.7 (6) | 3.2 (2) | 18.3 (19) | 7.7 (8) | 16.4 (15) | 14.2 (13) | 10.1 (8) | 26.5 (21) | 2.1 (1) | 14.6 (7) | 12.7 (49) | 13.3 (51) | 26.0 (100) |
| 2009 | 19.3 (12) | 1.6 (1) | 11.6 (12) | 6.8 (7) | 14.1 (13) | 8.7 (8) | 11.2 (9) | 16.2 (13) | 2.1 (1) | 6.2 (3) | 12.1 (47) | 8.3 (32) | 20.4 (79) |
| 2010 | 14.6 (9) | – | 18.7 (19) | 4.9 (5) | 15.7 (16) | 10.8 (11) | 8.7 (7) | 21.0 (17) | 12.0 (6) | 4.0 (2) | 14.4 (57) | 8.8 (35) | 23.2 (92) |
| 2011 | 8.1 (5) | 3.3 (2) | 10.0 (10) | 1.0 (1) | 6.3 (6) | 12.6 (12) | 11.1 (9) | 14.8 (12) | 2.0 (1) | 2.0 (1) | 8.0 (31) | 7.2 (28) | 15.2 (59) |
| 2012 | 8.4 (5) | 3.4 (2) | 4.3 (4) | 6.4 (6) | 14.8 (14) | 5.3 (5) | 15.0 (12) | 16.3 (13) | 9.7 (5) | 7.8 (4) | 10.5 (40) | 7.9 (30) | 18.4 (70) |
| 2013 | 8.5 (5) | 5.1 (3) | 10.8 (10) | 1.1 (1) | 10.4 (10) | 9.3 (9) | 13.8 (11) | 12.5 (10) | 5.7 (3) | 3.8 (2) | 10.2 (39) | 6.6 (25) | 16.8 (64) |
| 2014 | 11.6 (7) | – | 7.6 (7) | 3.3 (3) | 9.1 (9) | 7.1 (7) | 8.7 (7) | 10.0 (8) | 11.0 (6) | 5.5 (3) | 9.3 (36) | 5.4 (21) | 14.7 (57) |
| 2015 | 8.3 (5) | 1.7 (1) | 9.0 (8) | 6.8 (6) | 11.9 (12) | 5.0 (5) | 17.5 (14) | 15.0 (12) | 7.7 (4) | 17.4 (9) | 11.3 (43) | 8.7 (33) | 19.9 (76) |
| 2016 | 23.4 (14) | 3.3 (2) | 5.8 (5) | 4.7 (4) | 11.8 (12) | 6.9 (7) | 8.8 (7) | 16.3 (13) | 3.5 (2) | 12.2 (7) | 10.4 (40) | 8.6 (33) | 18.8 (73) |
| 2017 | 15.0 (9) | – | 10.8 (9) | 4.8 (4) | 8.8 (9) | 3.9 (4) | 8.7 (7) | 7.5 (6) | 6.9 (4) | 6.9 (4) | 9.9 (38) | 4.7 (18) | 14.7 (56) |
| 2018 | 1.7 (1) | 8.3 (5) | 3.7 (3) | 1.2 (1) | 9.7 (10) | 4.9 (5) | 14.9 (12) | 22.3 (18) | 13.7 (8) | 13.7 (8) | 8.9 (34) | 9.7 (37) | 17.8 (71) |
| 2019 | 6.7 (4) | 3.3 (2) | 6.5 (5) | 3.9 (3) | 6.8 (7) | 7.8 (8) | 8.6 (7) | 9.9 (8) | 8.5 (5) | 8.5 (5) | 7.4 (28) | 6.8 (26) | 13.9 (54) |
| 2020 | 5.0 (3) | 1.7 (1) | 4.0 (3) | - | 5.8 (6) | 7.8 (8) | 6.1 (5) | 11.0 (9) | 6.8 (4) | 3.4 (2) | 5.5 (21) | 5.3 (20) | 10.3 (41) |
| Overall | 10.8 (85) | 3.5 (21) | 9.3 (114) | 4.4 (49) | 10.9 (139) | 8.0 (102) | 11.0 (115) | 15.3 (160) | 7.1 (50) | 8.2 (57) | 10.0 (503) | 7.8 (389) | 17.8 (892) |
SCI Spinal Cord Injury, TSCI traumatic SCI, NTSCI non-traumatic SCI, STD standardised
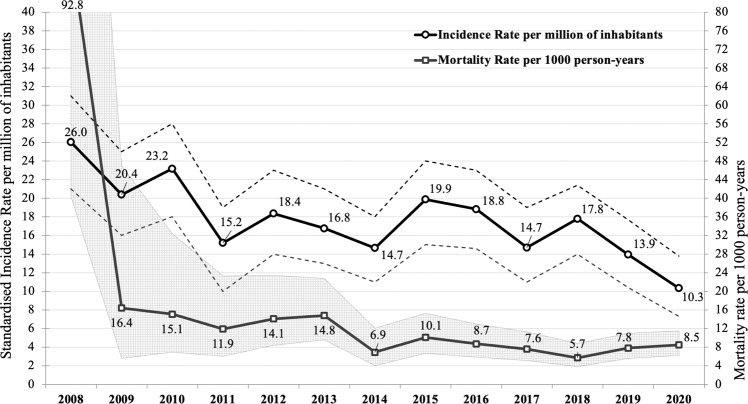
An equally high incidence rate (Table 2) was found for TSCI in the age groups 15 to 29 years (10.8), 45 to 59 years (10.9), and 60 to 74 years (11.0). NTSCI incidence rates were higher in the age groups 60 to 74 years (15.3) and 75 years and older (8.2). The highest number of incident TSCI cases was observed in the age group 45 to 59 years (n = 139), while for NTSCIs the highest number was found in the age group 60 to 74 years (n = 160). The highest TSCI and NTSCI incidence rates over the study period were observed in 2016 in the age group 15 to 29 years (23.4 cases per million) and in 2008 in the age group 60 to 74 years (26.5 cases per million), respectively. Standardised incidence decreased from 26.0 cases per million in 2008 to 10.3 cases in 2020, with fluctuations observed in 2011, 2014, and 2017 (Fig. 2).
Fig. 2. Trends of incidence and mortality of spinal cord injury cases from 2008 to 2020.
Standardised Incidence Rate (and 95% confidence interval, dotted lines) per million inhabitants and cohort mortality rate per 1000 person-years (and 95% confidence interval, grey area) of traumatic and non-traumatic spinal cord injury cases, from 2008 to 2020. Piedmont Region, Italy.
Mortality
A total of 235 SCI cases died during the study period, the majority of whom had NTSCI (n = 137; 58.3%). Moreover, NTSCI cases had a lower median age at death (71 years, IQR 64-78 years and 73.5 years, IQR 63-78 years in TSCI cases).
Identified cases accounted for a total of 4709.17 person-years observations for the whole study period in 2020 (Table 3). The overall mortality rate progressively decreased from 16.4 deaths each 1000 person-years in 2009, 95% CI 5.5–47.0, (being 92.8, 95% CI 40.3–199.6 in the first year of study) to 8.5 deaths every 1000 person-years (95% CI 6.2–11.5) in 2020, showing a relative stabilisation over the last five years (Fig. 2). Mortality rates in NTSCI were substantially higher overall when compared to TSCI. Excepting the first year of observation, the highest mortality rates were observed in 2011 for NTSCI cases (23.5 deaths per 1000 person-years) and in 2010 for TSCI cases (18.2 deaths per 1000 person-years). In 2020, the mortality rate of NTSCI cases was almost three times higher than that of TSCI cases (14.1 vs 5.1 deaths per 1000 person-years).
Table 3.
Cumulative number of traumatic spinal cord injury (TSCI), and non-traumatic spinal cord injury (NTSCI), with person-years of observations (PYO), mortality rates (per 1000 PYO), and lethality rates (per 1000 SCI cases) from 2008–2020. Piedmont Region, Italy.
| TSCI | NTSCI | All SCI cases | Overall mortality | Overall lethality | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | Cases | PYO | Mortality rate (n) | Lethality rate | Cases | PYO | Mortality rate (n) | Lethality rate | N | PYO | rate (n) | 95% CI | rate | 95% CI |
| 2008 | 49 | 27.1 | 36.9 (1) | 20.4 | 51 | 26.7 | 149.7 (4) | 78.4 | 100 | 53.85 | 92.8 (5) | 40.3–199.6 | 50.0 | 21.5–111.8 |
| 2009 | 95 | 95.8 | 10.4 (1) | 10.5 | 79 | 87.4 | 22.9 (2) | 25.3 | 174 | 183.13 | 16.4 (3) | 5.6–47.0 | 17.2 | 5.9–49.5 |
| 2010 | 151 | 219.7 | 18.2 (4) | 26.5 | 112 | 177.9 | 11.2 (2) | 17.9 | 263 | 398.56 | 15.1 (6) | 6.9–32.4 | 22.8 | 10.5–48.9 |
| 2011 | 178 | 374.3 | 2.7 (1) | 5.6 | 138 | 297.4 | 23.5 (7) | 50.7 | 316 | 673.63 | 11.9 (8) | 6.0–23.3 | 25.3 | 12.9–49.2 |
| 2012 | 252 | 566.0 | 7.1 (4) | 15.9 | 168 | 427.5 | 23.4 (10) | 59.5 | 378 | 996.43 | 14.1 (14) | 8.4–23.4 | 37.0 | 22.2–61.2 |
| 2013 | 252 | 786.2 | 15.3 (12) | 47.6 | 176 | 559.1 | 14.3 (8) | 45.5 | 428 | 1349.18 | 14.8 (20) | 9.6–22.8 | 46.7 | 30.5–71.1 |
| 2014 | 276 | 1015.5 | 3.0 (3) | 10.9 | 189 | 710.8 | 12.7 (9) | 47.6 | 465 | 1731.27 | 6.9 (12) | 4.0–12.1 | 25.8 | 14.8–44.6 |
| 2015 | 316 | 1289.3 | 10.1 (13) | 41.1 | 213 | 881.0 | 10.2 (9) | 42.3 | 529 | 2175.49 | 10.1 (22) | 6.7–15.3 | 41.6 | 27.6–62.2 |
| 2016 | 343 | 1582.7 | 5.7 (9) | 26.2 | 237 | 1065.9 | 13.1 (14) | 59.1 | 580 | 2648.54 | 8.7 (23) | 5.8–13.0 | 39.7 | 26.6–58.8 |
| 2017 | 372 | 1895.2 | 4.7 (9) | 24.2 | 241 | 1256.1 | 11.9 (15) | 62.2 | 613 | 3151.29 | 7.6 (24) | 5.1–11.3 | 39.2 | 26.4–57.6 |
| 2018 | 397 | 2231.9 | 3.1 (7) | 17.6 | 263 | 1421.8 | 9.8 (14) | 53.2 | 660 | 3653.72 | 5.7 (21) | 3.8–8.8 | 31.8 | 20.9–48.2 |
| 2019 | 418 | 2613.2 | 6.5 (17) | 40.7 | 275 | 1610.5 | 9.9 (16) | 58.2 | 693 | 4223.71 | 7.8 (33) | 5.6–11.0 | 47.6 | 34.1–66.1 |
| 2020 | 422 | 2941.2 | 5.1 (15) | 35.5 | 279 | 1768.0 | 14.1 (25) | 89.6 | 701 | 4709.17 | 8.5 (40) | 6.2–11.5 | 57.1 | 42.2–76.8 |
SCI Spinal Cord Injury TSCI traumatic SCI, NTSCI non-traumatic SCI, PYO person-years of observations, 95% CI 95% confidence interval
A substantial increase in overall lethality was observed, which, despite some fluctuations between 2014 and 2018, more than tripled from 17.2 (95% CI 21.5–111.8) deaths per 1000 cases in 2009 to 57.1 (95% CI 42.2–76.8) deaths in 2020 (Table 3). When considering injury aetiology, lethality rates were higher among NTSCI cases, which peaked at 89.6 deaths per 1000 cases in 2020, compared to 35.5 deaths per 1000 cases in TSCI in the same year. While for NTSCI cases the 2020 represents the highest cohort lethality, TSCI cases peaked at 47 deaths per 1000 cases in 2013.
Discussion
This retrospective cohort study aimed to determine the incidence and mortality of SCI over an extended time period. This represents the first attempt to use administrative data to describe longitudinal epidemiological trends in TSCI and NTSCI in a large region of Northwestern Italy. Incidence was assessed by age, gender, and aetiology from 2008 to 2020. A fluctuating, decreasing trend in SCI incidence rates was shown over the study period, with a further decrease in 2020, which deserves specific attention due to the impact of the COVID-19 pandemic. Mortality rates had the same decreasing trend and seemed to stabilise in last five years, with higher rates in NTSCI cases. Case lethality has tripled during the study period, presumably reflecting influence of population ageing on the cohort. The majority of SCI cases had TSCI, with paraplegia as the most common diagnosis. Compared to TSCI, NTSCI was more common among individuals older than 60 years. The male-to-female ratio was nearly four-fold for TSCI, while gender was almost equally distributed among NTSCI cases.
Previous studies conducted in Italy are now dated and covered shorter periods, but they reported comparable TSCI and NTSCI incidence rates, and age and gender distributions [14, 16, 17]. Caldana & Lucca [17] and Ferro et al. [14] reported TSCI incidence rates ranging from 14.3 to 14.7 cases per million. This is slightly higher than what we observed, possibly due to the different study design and wider inclusion criteria employed in these studies, which could have led to overestimation. Conversely, despite some increases over the study period, our NTSCI incidence rates are comparable to those reported in the Veneto Region in 1994 to 1995 [17]. Mean age in our cohort was higher than that in previous Italian studies examining TSCI and NTSCI [14–17, 20], perhaps due to the ageing of the population, which may have led to a gradual increase in the age of SCI onset [21, 22]. Nevertheless, TSCI and NTSCI were most common in people younger than 59 years and older than 60 years, respectively, which is in contrast to the bimodal peak in incidence highlighted in Italy and Switzerland before 2015 [14, 23]. This confirms that the expected NTSCI increase is dependent on population ageing [3]. However, compared to earlier studies [14, 16], we observed substantially fewer differences in the incidence proportion of NTSCI and TSCI.
Worldwide, reported TSCI incidence varies from 39 cases per million in the US to 15 cases in Australia [11]. Similarly, reported NTSCI incidence ranges from 68 cases per million in the US to 6 cases in Western Europe [3], with considerable variability among countries. Although slightly lower, our findings are comparable to those from the Western Europe WHO Region for both TSCI (16 cases per million) [11] and NTSCI [3]. Similarly, our observed male-to-female ratio reflected previously identified proportions for both TSCI [22, 24] and NTSCI [25, 26]. In European studies, age at TSCI onset varied between 42 years in Russia [27] and 59 years in Finland [28]. This is quite different than our results, which are closer to those reported in Ireland, Switzerland, and Norway (range: 47 to 52 years) [22–24]. No significant differences were identified between our observed age at NTSCI onset and those reported in Norway, Ireland, and Finland (range: 55 to 62 years) [25, 26, 29]. The dominance of TSCI in older age groups in Norway and Finland could be related to national care pathways, as these countries send all SCI cases to rehabilitation centres, regardless of their age [24, 28], whereas countries like Italy refer older SCI cases to elderly services rather than rehabilitation centres. The higher NTSCI incidence in Ireland and Finland may also be explained by their policy to refer these patients directly to specific NTSCI rehabilitation [26, 29], whereas other countries refer these cases to a clinical setting focused on the underlying diseases that caused NTSCI (e.g., oncology, cardiovascular surgery) [25].
A previous systematic review highlighted the lack of available studies on mortality and survival following SCI, as well as their conflicting results [4]. While improvements in life expectancy after TSCI have been reported, especially among people with paraplegia [30], other studies have either found no differences [31] or highlighted substantial increases in mortality rates [32]. Data on NTSCI are more fragmented and show higher mortality rates compared to the general population, lower life expectancy, and younger age at death [3, 5]. As the literature widely supports an association between mortality and SCI severity [4], it might be fundamental to collect and include SCI severity in Italian administrative databases, which currently contain data only on the level of injury. In this regard, obtained findings might suggest that, whereas NTSCI represent more complex cases characterised by multimorbidity, the clinical outcomes of TSCI are likely dependent on the case severity. Further analysis on the completeness of SCI and clinical information included in the assigned ICD-9-CM diagnosis could contribute to a more precise definition of injury severity and explain differences found in mortality rates within our cohort. Our current findings, especially regarding increased case lethality and the decrease in person-year mortality rates, suggest that ageing could be the leading cause of increased mortality in people with SCI. As cause of death and mortality risk in this population have yet to be identified, further investigations focusing on causes of death in Italy are urgently recommended.
Although the downward trend we observed in SCI incidence is consistent with that already reported in Russia [27], Spain [33], and Canada [34, 35], there are concerns regarding the influence of the COVID-19 pandemic on variations in epidemiological trends from 2019 to 2020, mostly concerning the peak in case lethality. Nevertheless, the decrease in SCI incidence, which has been associated with preventive measures in road and workplace safety [2], may also have been due decreased mobility, and lack of access to screening, diagnosis, and treatment during the pandemic. This is particularly noticeable from the decline of NTSCI cases and their increased mortality in our cohort, as NTSCI requires quick diagnosis and treatment. People with SCI need regular follow-up to prevent secondary conditions, which are associated with more frequent hospitalisations and high mortality [36]. Thus, it is possible that reduced access to care during the pandemic will have consequences beyond the immediately observable effects for this population. This emphasises the need to continue monitoring epidemiological changes in this cohort. Future research is needed to assess the increased lethality we observed in 2020, which may indicate less than optimum follow-up care, possibly related to the COVID-19 pandemic. One of the conceivable interventions should be the realization of an early detection system able to identify the most vulnerable individuals, which could also contribute to improving long-term care, reducing post-injury secondary conditions, and positively influencing the burden of SCI. The aforementioned could also contribute to the development of a national SCI registry, which is currently absent in Italy and in many other countries, and where active it is restricted to TSCIs only [25], thus making it possible to estimate the real prevalence of SCI in Italy in the next future.
The main limitation of the study is the use of administrative databases to identify SCI cases, as cases admitted to facilities other than the three SCI rehabilitation centres in the Piedmont Region could have been missed, especially NTSCI cases who follow diagnostic and treatment pathways that do not prioritise functional rehabilitation. However, identifying individuals at their first admission to a SCI rehabilitation centre likely minimised the number of missed incident cases and ensured that those identified represented the SCI population residing in the Piedmont Region. Moreover, not a single case was lost during the follow-up period. It is important to note that administrative data are only available starting from 2008. This has not allowed a reliable estimate of SCI prevalence to date, although the normalisation of our epidemiological data suggests a progressive stabilisation of the cohort, which still has to be reached. The use of administrative databases does not produce the same richness of information as a national registry could allow, as such a registry would include direct useful measures as, for example, ASIA or other functional scores. At the same time, using a coded diagnostic system allowed us to acquire the information needed to describe the epidemiology of SCI, and the standardisation of data, as well as the person-year statistical approach, enabled comparison between different years and results from other countries [19]. Finally, in the absence of retrospective information collected using the International Spinal Cord Injury Core Data Set, it was impossible to determine the causes of SCI; nevertheless, data were presented according to TSCI/NTSCI and paraplegia/tetraplegia, as recommended by Cripps et al. [11].
Conclusion
This study reported the long-term epidemiological pattern of SCI in a large Italian region. As in other high-income countries, our findings showed a decreasing trend in incidence and mortality rates, with an increased case lethality, especially for those with a NTSCI. Given the observed changes in the epidemiology of SCI, community services offered after acute rehabilitation should be strengthened to enhance their effectiveness, with a focus on chronic conditions and reducing the occurrence of secondary conditions, in order to increase quality of life and survival in this population. It further suggests the need to deepen knowledge on secondary conditions and the overall use of health services by individuals with SCI. Moreover, it might be relevant to better understand the impact of the COVID-19 pandemic on SCI incidence, access to services, and mortality rates. Finally, given the limits of administrative databases, detailed, longitudinal, population-based SCI registers should be implemented urgently at a higher geographical level (e.g., National or even European), as they can offer more comprehensive follow-up.
Author contributions
AC and AB were responsible for designing and writing the study protocol, interpreting results, and writing the first manuscript draft. SC and CM contributed to writing the study protocol and provided feedback on the article draft. CM and RO were responsible for managing the data contained in the Italian National Information System databases. RO and AB was responsible for analysing the data. MMG, BA, and VD actively contributed to the manuscript writing and finalisation.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
The datasets generated and analysed during this study are available from the corresponding author on request.
Ethical approval
The Italian National Information System databases include the Hospital Discharge Form database, the Italian Census database, and the National Mortality database, which are official, anonymised Ministerial Health information systems. All patient information is centrally anonymised and available to authorised institutions to be used for epidemiological and/or health organisation studies without any further authorisations. Hence, ethics committee approval was not required. Personal data treatments are carried out in compliance with the current rules set out in EU Regulation 2016/679 and the current legislation on the Protection of Personal Data set out in Legislative Decree 101/2018 as well as Legislative Decree 196/2003 and subsequent amendments and additions. Our study used statistical and aggregate data that were shared according to the current deontological rules for the processing National Statistical System data for scientific research purposes, in accordance with the provisions of art 5 ter of Legislative Decree 33 /2013 as amended by Legislative Decree 97/2016 and Legislative Decree 101/2018.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kirshblum S, Snider B, Rupp R, Read MS. International Standards Committee of ASIA and ISCoS. Updates of the International Standards for Neurologic Classification of Spinal Cord Injury: 2015 and 2019. Phys Med Rehabil Clin N. Am. 2020;31:319–30. doi: 10.1016/j.pmr.2020.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014;6:309–31. doi: 10.2147/CLEP.S68889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.New PW, Cripps RA, Bonne Lee B. Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord. 2014;52:97–109. doi: 10.1038/sc.2012.165. [DOI] [PubMed] [Google Scholar]
- 4.Chamberlain JD, Meier S, Mader L, von Groote PM, Brinkhof MWG. Mortality and longevity after a spinal cord injury: systematic review and meta-analysis. Neuroepidemiology. 2015;44:182–98. doi: 10.1159/000382079. [DOI] [PubMed] [Google Scholar]
- 5.Buzzell A, Chamberlain JD, Eriks-Hoogland I, Hug K, Jordan X, Schubert M, et al. All-cause and cause-specific mortality following non-traumatic spinal cord injury: evidence from a population-based cohort study in Switzerland. Spinal Cord. 2020;58:157–64. doi: 10.1038/s41393-019-0361-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cardenas D, Lin V, Bono CM, Frost FS, Hammond MC, Spinal Cord Medicine, Second Edition:Principles & Practice. 2nd Edition. Demos Medical Publishing: New York, NY, 2010.
- 7.DeVivo MJ. Causes and costs of spinal cord injury in the United States. Spinal Cord. 1997;35:809–13. doi: 10.1038/sj.sc.3100501. [DOI] [PubMed] [Google Scholar]
- 8.St. Andre J, Smith B, Stroupe K, Burns S, Evans C, Ripley D, et al. A comparison of costs and health care utilization for veterans with traumatic and nontraumatic spinal cord injury. Top Spinal Cord Inj Rehabil. 2011;16:27–42. doi: 10.1310/sci1604-27. [DOI] [Google Scholar]
- 9.Munce SEP, Wodchis WP, Guilcher SJT, Couris CM, Verrier M, Fung K, et al. Direct costs of adult traumatic spinal cord injury in Ontario. Spinal Cord. 2013;51:64–69. doi: 10.1038/sc.2012.81. [DOI] [PubMed] [Google Scholar]
- 10.Cao Y, Krause JS. The association between secondary health conditions and indirect costs after spinal cord injury. Spinal Cord. 2021;59:306–10. doi: 10.1038/s41393-020-00567-4. [DOI] [PubMed] [Google Scholar]
- 11.Cripps RA, Lee BB, Wing P, Weerts E, Mackay J, Brown D. A global map for traumatic spinal cord injury epidemiology: towards a living data repository for injury prevention. Spinal Cord. 2011;49:493–501. doi: 10.1038/sc.2010.146. [DOI] [PubMed] [Google Scholar]
- 12.Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 2014;52:110–6. doi: 10.1038/sc.2012.158. [DOI] [PubMed] [Google Scholar]
- 13.Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50:365–72. doi: 10.1038/sc.2011.178. [DOI] [PubMed] [Google Scholar]
- 14.Ferro S, Cecconi L, Bonavita J, Pagliacci MC, Biggeri A, Franceschini M. Incidence of traumatic spinal cord injury in Italy during 2013–2014: a population-based study. Spinal Cord. 2017;55:1103–7. doi: 10.1038/sc.2017.88. [DOI] [PubMed] [Google Scholar]
- 15.Franceschini M, Bonavita J, Cecconi L, Ferro S, Pagliacci MC, Italian SCI Study Group. Traumatic spinal cord injury in Italy 20 years later: current epidemiological trend and early predictors of rehabilitation outcome. Spinal Cord. 2020;58:768–77. doi: 10.1038/s41393-020-0421-y. [DOI] [PubMed] [Google Scholar]
- 16.Pagliacci MC, Celani MG, Spizzichino L, Zampolini M, Aito S, Citterio A, et al. Spinal cord lesion management in Italy: a 2-year survey. Spinal Cord. 2003;41:620–8. doi: 10.1038/sj.sc.3101521. [DOI] [PubMed] [Google Scholar]
- 17.Caldana L, Lucca L. Epidemiological remarks on traumatic spinal cord injuries and non-traumatic spinal cord diseases in Veneto 1994-1995. Eur J Phys Rehabil Med. 1998;34:159–68. [Google Scholar]
- 18.Biering-Sørensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International Spinal Cord Injury Core Data Set (version 2.0)-including standardization of reporting. Spinal Cord. 2017;55:759–64. doi: 10.1038/sc.2017.59. [DOI] [PubMed] [Google Scholar]
- 19.Strauss D, Shavelle R, DeVivo MJ, Day S. An analytic method for longitudinal mortality studies. J Insur Med N. Y N. 2000;32:217–25. [PubMed] [Google Scholar]
- 20.Pagliacci MC, Celani MG, Zampolini M, Spizzichino L, Franceschini M, Baratta S, et al. An Italian survey of traumatic spinal cord injury. The Gruppo Italiano Studio Epidemiologico Mielolesioni study. Arch Phys Med Rehabil. 2003;84:1266–75. doi: 10.1016/S0003-9993(03)00234-X. [DOI] [PubMed] [Google Scholar]
- 21.New PW, Sundararajan V. Incidence of non-traumatic spinal cord injury in Victoria, Australia: a population-based study and literature review. Spinal Cord. 2008;46:406–11. doi: 10.1038/sj.sc.3102152. [DOI] [PubMed] [Google Scholar]
- 22.Smith É, Fitzpatrick P, Lyons F, Morris S, Synnott K. Prospective epidemiological update on traumatic spinal cord injury in Ireland. Spinal Cord Ser Cases. 2019;5:1–4. doi: 10.1038/s41394-019-0152-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chamberlain JD, Deriaz O, Hund-Georgiadis M, Meier S, Scheel-Sailer A, Schubert M, et al. Epidemiology and contemporary risk profile of traumatic spinal cord injury in Switzerland. Inj Epidemiol. 2015;2:28. doi: 10.1186/s40621-015-0061-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Halvorsen A, Pettersen AL, Nilsen SM, Halle KK, Schaanning EE, Rekand T. Epidemiology of traumatic spinal cord injury in Norway in 2012-2016: a registry-based cross-sectional study. Spinal Cord. 2019;57:331–8. doi: 10.1038/s41393-018-0225-5. [DOI] [PubMed] [Google Scholar]
- 25.Halvorsen A, Pettersen AL, Nilsen SM, Halle KK, Schaanning EE, Rekand T. Non-traumatic spinal cord injury in Norway 2012-2016: analysis from a national registry and comparison with traumatic spinal cord injury. Spinal Cord. 2019;57:324–30. doi: 10.1038/s41393-018-0223-7. [DOI] [PubMed] [Google Scholar]
- 26.Niemi-Nikkola V, Koskinen E, Väärälä E, Kauppila A-M, Kallinen M, Vainionpää A. Incidence of acquired nontraumatic spinal cord injury in Finland: A 4-year prospective multicenter study. Arch Phys Med Rehabil. 2021;102:44–49. doi: 10.1016/j.apmr.2020.08.015. [DOI] [PubMed] [Google Scholar]
- 27.Mirzaeva L, Gilhus NE, Lobzin S, Rekand T. Incidence of adult traumatic spinal cord injury in Saint Petersburg, Russia. Spinal Cord. 2019;57:692–9. doi: 10.1038/s41393-019-0266-4. [DOI] [PubMed] [Google Scholar]
- 28.Johansson E, Luoto TM, Vainionpää A, Kauppila A-M, Kallinen M, Väärälä E, et al. Epidemiology of traumatic spinal cord injury in Finland. Spinal Cord. 2021;59:761–8. doi: 10.1038/s41393-020-00575-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith É, Fitzpatrick P, Lyons F, Morris S, Synnott K Epidemiology of non-traumatic spinal cord injury in Ireland - a prospective population-based study. J Spinal Cord Med 2020; 1–6. [DOI] [PMC free article] [PubMed]
- 30.Middleton JW, Dayton A, Walsh J, Rutkowski SB, Leong G, Duong S. Life expectancy after spinal cord injury: a 50-year study. Spinal Cord. 2012;50:803–11. doi: 10.1038/sc.2012.55. [DOI] [PubMed] [Google Scholar]
- 31.Hagen EM, Lie SA, Rekand T, Gilhus NE, Gronning M. Mortality after traumatic spinal cord injury: 50 years of follow-up. J Neurol Neurosurg Psychiatry. 2010;81:368–73. doi: 10.1136/jnnp.2009.178798. [DOI] [PubMed] [Google Scholar]
- 32.Li B, Qi J, Cheng P, Yin P, Hu G, Wang L et al. Traumatic spinal cord injury mortality from 2006 to 2016 in China. J Spinal Cord Med 2020: 1–6. [DOI] [PMC free article] [PubMed]
- 33.Pérez K, Novoa AM, Santamariña-Rubio E, Narvaez Y, Arrufat V, Borrell C, et al. Incidence trends of traumatic spinal cord injury and traumatic brain injury in Spain, 2000-2009. Accid Anal Prev. 2012;46:37–44. doi: 10.1016/j.aap.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 34.Pickett W, Simpson K, Walker J, Brison RJ. Traumatic spinal cord injury in Ontario, Canada. J Trauma. 2003;55:1070–6. doi: 10.1097/01.TA.0000034228.18541.D1. [DOI] [PubMed] [Google Scholar]
- 35.Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. The epidemiology of traumatic spinal cord injury in Alberta, Canada. Can J Neurol Sci J Can Sci Neurol. 2003;30:113–21. doi: 10.1017/S0317167100053373. [DOI] [PubMed] [Google Scholar]
- 36.Conti A, Clari M, Arese S, Bandini B, Cavallaro L, Mozzone S, et al. Validation and psychometric evaluation of the Italian version of the Spinal Cord Injury Secondary Conditions Scale. Spinal Cord. 2020;58:496–503. doi: 10.1038/s41393-019-0384-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analysed during this study are available from the corresponding author on request.