Abstract
SARS-CoV-2 (severe acute respiratory syndrome coronavirus type 2) has been identified as the source of a world coronavirus pandemic in 2019. Covid-19 is considered a main respiratory disease-causing viral pneumonia and, in severe cases, leads to acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). Although, extrapulmonary manifestations of Covid-19 like neurological, cardiovascular, and gastrointestinal have been confirmed. Exaggerated immune response and release of a high amount of pro-inflammatory cytokines may progress, causing a cytokine storm. Consequently, direct and indirect effects of SARS-CoV-2 infection can evolve into systemic complications due to the progression of hyper inflammation, oxidative stress and dysregulation of the renin-angiotensin system (RAS). Therefore, anti-inflammatory and antioxidant agents could be efficient in alleviating these disorders. Ursolic acid has anti-inflammatory, antioxidant, and antiviral effects; it reduces the release of pro-inflammatory cytokines, improves anti-inflammatory cytokines, and inhibits the production of reactive oxygen species (ROS). In virtue of its anti-inflammatory and antioxidant effects, ursolic acid may minimize SARS-CoV-2 infection-induced complications. Also, by regulating RAS and inflammatory signaling pathways, ursolic acid might effectively reduce the development of ALI in ARDS in Covid-19. In this state, this perspective discusses how ursolic acid can mitigate hyper inflammation and oxidative stress in Covid-19.
Keywords: Acute lung injury, Antiviral, Covid-19, Immunity, Oxidative stress, Pandemics
Introduction
A new severe acute respiratory distress syndrome coronavirus type 2 had been documented as the response of a pandemic coronavirus disease 2019 (Covid-19) (Al-Kuraishy et al. 2021a, b, c, d, e). Covid-19 is considered a main respiratory disease-causing viral pneumonia and, in severe cases causes acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) (Al-Kuraishy et al. 2021a, b, c, d, e). However, extrapulmonary manifestations of Covid-19 like neurological, cardiovascular, gastrointestinal, renal, and metabolic complications have been confirmed (Al-Kuraishy et al. 2021a, b, c, d, e). The clinical symptoms of Covid-19 may be asymptomatic in the preponderance of patients (Parasher 2021). Although, 15% of these cases can present with a severe form because of the development of ALI and ARDS that required hospitalization, intensive care admission and mechanical ventilation (Mehta et al. 2021; Schönfeld et al. 2021). The pathogenesis of the infection requires the binding of this virus to the angiotensin-converting enzyme 2 (ACE2), which is highly expressed in immune and non-immune cells (Woodby et al. 2021). The direct effects of SARS-CoV-2 boost immune and inflammatory responses that disappear following viral clearance (Woodby et al. 2021). Nevertheless, exaggerated immunological response and discharge of a high amount of pro-inflammatory cytokines can progress in a number of cases causing cytokine storm (Lin et al. 2021). Consequently, direct, and indirect SARS-CoV-2infection effects may cause systemic effects and the development of multi-organ injury (MOI) (Lin et al. 2021).
Different therapeutic herbal remedies have been tried and suggested in treating Covid-19 for example Moringa oleiferra, Cassia fistula, Justicia adhatoda and Agrimonia pilosa (Tiwari Pandey et al. 2020; Attallah et al. 2021; Elekhnawy and Negm 2022). Bobby Knight American basketball player and coach said, “The will to succeed is important, but more important is the will to prepare for success.” Therefore, searching a new remedy against SARS-CoV-2 is our goal. In the present perspective, we try to find the ursolic acid's probable mechanistic role in SARS-CoV-2 infection.
Pharmacology of ursolic acid
Ursolic acid is a penta-cyclic triterepenoid (3β-3-hydroxy-12-ene-28-oic acid) with a 456.71 g/mol molecular mass and chemical formula of C30H48O3 [Fig. 1] (López-Hortas et al. 2018). It is soluble in alcoholic hydroxide and acetic acid. It is biosynthesized from dammarenyl cation by cyclization and folding of squalene (López-Hortas et al. 2018). Ursolic acid is a natural product present mainly in Salvia nementosa and Uncaria tomentosa as well as medicinal herbs, vegetables, and fruits [10]. Particularly, ursolic acid is mainly found in apple fruit peels, rosemary, lavender, and thyme (Cargnin and Gnoatto 2017).
Fig. 1.
Ursolic acid Chemical Structure
Pharmacodynamic and pharmacokinetic of ursolic acid
Ursolic acid has anti-inflammatory, lipid-lowering, antioxidant, and antiviral anticancer effects (Hussain et al. 2017). Ursolic acid acts by regulating mitochondrial function via suppression of nuclear factor kappa B (NF-κB) and stimulation of caspases activity as well as regulation of p53 and apoptotic pathways, therefore; it has anti-neoplastic activity (Hussain et al. 2017). Ursolic acid blocks the mechanistic target of rapamycin (mTOR) and mitogen-activated protein kinase (MAPK), by which inhibiting cell proliferation in malignant cells (Luo et al. 2017). Besides, ursolic acid inhibits the progression of the inflammatory response by blocking cyclooxygenase 2 (COX-2) activities (Zhang et al. 2020). In addition, ursolic acid improves insulin sensitivity by regulating insulin signaling and inflammatory and/or metabolic biomarkers in adipose tissue thus; it is effective as an anti-diabetic agent and in treating obesity-related complications (Ramirez-Rodriguez et al. 2017). Moreover, ursolic acid has been shown to improve exercise tolerance and reduce sarcopenia (Sakuma and Yamaguchi 2012). Therefore, ursolic acid effectively prevents skeletal muscle atrophy (Bakhtiari et al. 2016). Despite the significant cardio-protective effect of ursolic acid, it may increase the risk of plaque formation and some cardiovascular complications (Senthil et al. 2007).
The use of ursolic acid is associated with some adverse effects like vomiting, nausea, abdominal pain, skin rash, hematuria, and hypernatremia (Messner et al. 2011). Long-term use of ursolic acid is linked with the development of hepatotoxicity in a dose-dependent manner (Wang et al. 2013). Ursolic acid has notable anti-inflammatory, antioxidant, anti-carcinogenic, anti-obesity, anti-diabetic, cardioprotective, neuroprotective, hepatoprotective, anti-skeletal muscle atrophy, and thermogenic effects. It also mediates some pharmacological processes and modulates several signaling pathways to prevent the development of chronic diseases. The regulation of nuclear factor-kappa B (NF-κB) and apoptotic signaling in cancer cells, insulin signaling in adipose tissue, the expression of cardiac damage markers in the heart, inflammation and the level of antioxidants in the brain, metabolic signaling and the level of oxidants in the liver, and atrophy signaling and metabolic signaling in skeletal muscles may all play a role in how ursolic acid exerts these positive effects (Seo et al. 2018). Cancer, metabolic syndrome, brain disease, liver disease, and sarcopenia are just a few chronic diseases that ursolic acid is used to treat and prevent. Numerous studies have shown that ursolic acid enhances exercise capacity and has positive effects on muscle strength and cardiovascular endurance, suggesting that it may be effective as an exercise imitator (Seo et al. 2018).
Furthermore, ursolic acid interferes with the transport and metabolism of many drugs, including bosentan, enalopril, statins, valsartan, and lomatrigen, by inhibiting organic anion transporter IB and glucoronyl-transferase enzyme (Hua et al. 2014; Wang et al. 2015). The net broad-spectrum pharmacological effects of ursolic acid are illustrated in Table 1.
Table 1.
Pharmacological effects of ursolic acid
| Effects | Mechanisms | References |
|---|---|---|
| Anticancer | Inhibition of NF-κB, MMP9, VEGF, ICAM and Bcl-2 | Chen et al. (2015) |
| Anti-obesity | Decrease body weight, fat mass, leptin, and insulin resistance. Increase energy expenditure, adiponectin, adipocyte function | Kunkel et al. (2012); Li et al. (2014) |
| Anti-diabetic | Improves pancreatic β-cell functions, increases expression of insulin and glycogen synthase kinase receptors improve GLUT4 | Guzmán-Ávila et al. (2018) |
| Myocardial infarction and atherosclerosis | Inhibits expression of PCNA, DNA damage, expression of CK-MB, Increases antioxidant enzymes, neointimal formation | Li et al. (2018); Radhiga et al. (2019) |
| Parkinson disease | Increases dopamine, neuroprotective effect, inhibition of inflammation and oxidative stress improves mitochondrial biogenesis | Peshattiwar et al.(2020) |
| Stroke | Decreases infarct size, improves neuronal functions, inhibits MMP9 and neuroinflammation, TLR4/NF-κB | Wang et al.(2018) |
| Liver fibrosis | Reduces ROS and increases Nrf2, HO-1, and Bcl-2/Bax ratio | Gan et al. (2018) |
| Fatty liver | Increases AMPK, GSK3β, cleavage of caspase 3, reduces mTOR pathway | Lin et al. (2018) |
NF-κB nuclear factor kappa B, MMP9 matrix metalloproteinase 9, VEGF vascular endothelial growth factor, ICAM intercellular adhesion molecule, Bcl-2 B-cell lymphoma 2 genes, PCNA proliferating cell nuclear antigen, TLR4 toll-like receptor 4, ROS reactive oxygen species, Nrf2 nuclear erythroid factor 2, HO-1 heme oxygenase 1, AMPK adenosine monophosphate protein kinase, GSK3β glycogen synthase 3β, mTOR mechanistic target of rapamycin
Ursolic acid is poor water-soluble with low bioavailability, it is absorbed from the intestine by passive diffusion and P glycoprotein transporter, and peak concentration occurs within one hour (Jinhua 2019). It is metabolized by the liver and excreted by the urine. Ursolic acid is a safe agent with minimal toxicity (Sun et al. 2020). However, Mishra et al. noted that prolonged ursolic acid use might be connected to the emergence of mild toxicity, and the pioneering investigations found that the toxic dose of ursolic acid in mice is greater than 2000 mg/kg (Mishra et al. 2021).
Role of ursolic acid in Covid-19
Ursolic acid is regarded as a novel antiviral agent by inhibiting the replication and maturation of rotavirus particles in the endoplasmic reticulum (Tohmé et al. 2019). Yim et al. demonstrated that ursolic acid has potential antiviral effects by inhibiting the expression of the human papillomavirus E6/E7 gene (Yim et al. 2006). It has been shown that ursolic acid was effective against chronic hepatitis C virus infection (Kong et al. 2013), human immune deficiency virus 1 (HIV-1) (Ma et al. 1998), herpes virus infection (Bag et al. 2012), human papilloma virus II (Kazakova et al. 2010)and against influenza H5N1 (Al-Kuraishy et al. 2021a, b, c, d, e).
These findings support ursolic acid's broad-spectrum antiviral properties, suggesting that it could be beneficial against SARS-CoV-2 infection. It has anti-inflammatory and antioxidant properties (Hussain et al. 2017). Ursolic acid may reduce inflammatory and oxidative stress disorders in SARS-CoV-2 infection (Al-Kuraishy et al. 2021a, b, c, d, e). Covid-19 may produce cytokine storm and accompanying problems such as ALI, ARDS, and MOI as a result of oxidative stress and excessive pro-inflammatory cytokines (Al-Kuraishy et al. 2022).
Ursolic acid inhibits LPS-induced ALI in mice by reducing IL-1, IL-6, tumor necrosis factor-alpha (TNF-α), high mobility group box protein 1(HMGB1), and nitric oxide (NO) expression while activating anti-inflammatory cytokines (Chen et al. 2013). Yang and colleagues observed that ursolic acid can reduce heat-induced ALI by inhibiting endoplasmic reticulum stress in mice (Yang et al. 2021).
Ursolic acid can decrease ROS generation and the development of oxidative stress (Gayathri et al. 2009). Furthermore, ursolic acid inhibits NF-κB and the expression of TLR4, which can reduce the propagation of inflammatory reactions (Jang et al. 2014). TLR4/NF-κB axis is regarded as a master of immune response in SARS-CoV-2 infections linked with immune over-activation and pro-inflammatory cytokines production such as IL-1β, IL-6, and TNF-α (Saravanakumar et al. 2021). Therefore, through anti-inflammatory and antioxidant impacts, ursolic acid may decrease SARS-CoV-2 infection-induced inflammatory and oxidative stress disorders and associated ALI/ARDS.
Remarkably, ursolic acid has a potential effect on the SARS-CoV-2 infection by inhibiting viral protease (Shree et al. 2022). Besides, ursolic acid interferes with the binding of SARS-CoV-2 to ACE2 (Subbaiyan et al. 2020).
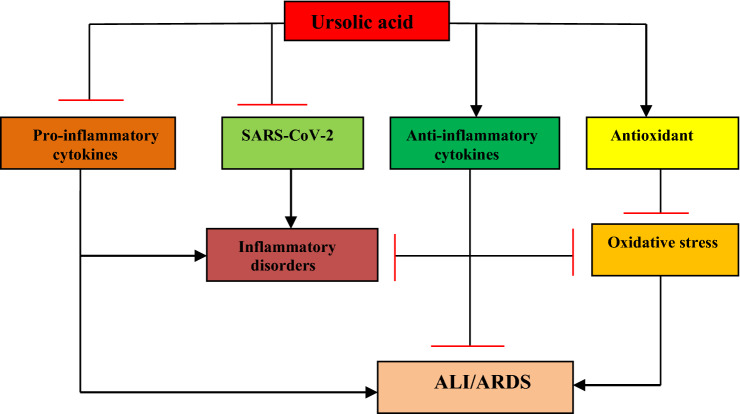
These observations imply that ursolic acid may be beneficial against Covid-19 by inhibiting SARS-CoV-2 proliferation and associated oxidative/inflammatory disorders [Fig. 2].
Fig. 2.
The probable role of ursolic acid in Covid-19: Ursolic acid inhibits release of pro-inflammatory cytokines as well as SARS-CoV-2 proliferation. Ursolic acid augments antioxidants and release of anti-inflammatory cytokines, which reduce oxidative stress and inflammatory disorders leading suppression development of ALI and ARDS
Ursolic acid effects on the renin-angiotensin system (RAS) in Covid-19
In Covid-19, the renin-angiotensin system (RAS) is dysregulated due to the down-regulation of ACE2 by SARS-CoV-2 infection since it exploits ACE2 as an entry point to the host cells (Al-Kuraishy et al. 2020). ACE2 is involved in the metabolism of vasoconstrictor and pro-inflammatory angiotensin II (AngII) to vasodilator and anti-inflammatory Ang1-7 (Onohuean et al. 2021). Herein, exaggeration of AngII-induced inflammatory and oxidative stress was documented in patients with Covid-19 (Miesbach 2020).
Ursolic acid has potential effects on RAS; for example, it attenuates AngII-induced inflammatory changes in mice with experimental abdominal aortic aneurysm (Zhai et al. 2018). Shimada et al. found that ursolic acid had the ability to inhibit ACE (Shimada and Inagaki 2014) by, which can reduce the production of AngII and release of aldosterone, which have a bad impact on SARS-CoV-2 infection via triggering of oxidative stress and release of pro-inflammatory cytokines (Liaudet and Szabo 2020). Of interest, ACE inhibitors did not affect morbidity and mortality of Covid-19. Xie et al. review and meta-analysis involved 30 studies comprising 10,434 Covid-19 patients and found that ACE inhibitors improve clinical outcomes and reduce morbidity/mortality risk (Xie et al. 2021). In this state, long-term use of ACE inhibitors increases the expression of ACE2, which has a protective effect by neutralizing SARS-CoV-2 particles (Di Maro et al. 2021).
In a similar way, ursolic acid attenuates renal inflammation, fibrosis, and oxidative stress by inhibiting the expression of AngII type 1 receptor-associated protein and AT1R (Ma et al. 2019). Moreover, dysregulated RAS with high circulating AngII provoke immune-thrombosis and endothelial dysfunction (McGonagle et al. 2021). These changes ultimately lead to pulmonary thrombosis and propagation of ALI/ARDS (Poor 2021). Remarkably, ursolic acid has anti-thrombotic effects by inhibiting platelet aggregation (Van den Berg and Te Velde 2020).
Thus, ursolic acid may be effective as a preventive and medical remedy in Covid-19 by inhibiting ACE, expressing protective ACE2, suppressing pro-inflammatory AT1R and attenuating Ang II-induced immune-thrombosis [Fig. 3].
Fig. 3.
The potential effects of ursolic acid on RAS in Covid-19. Angiotensin I (AngI) is converted by ACE to AngII which activates AT1R leading to the induction of oxidative stress and inflammation. Covid-19 down-regulates ACE2 causing the elevation in AngII with reduction of Ang1-7 and Ang1-9. Ursolic acid inhibits ACE with increasing expression of ACE2. These changes by ursolic acid decrease the risk of development of ALI and ARDS
Implications of ursolic acid on inflammatory signaling pathways in Covid-19
Pathogenesis of Covid-19 is correlated to the stimulation of diverse signaling pathways, which trigger different inflammatory complications. One of these inflammatory signalings is nod-like receptor pyrin 3 (NLRP3) inflammasome, which was highly activated in Covid-19, resulting in the generation of cytokine storm and tissue injury (Van den Berg and Te Velde 2020). NLRP3 inflammasome activates cleavage of caspase-1 and secretion of damage-associated molecular patterns (DAMPs) and pro-inflammatory cytokines (Van den Berg and Te Velde 2020). It has been shown that ursolic acid inhibits chondrocyte injury and inflammation by blocking the NLRP3 inflammasome signaling pathway (Wang et al. 2020). Chen et al. observed that ursolic acid could reduce inflammatory changes progression in LPS-induced gastric tumors in mice by attenuating the NLRP3 inflammasome signaling pathway (Chen et al. 2020a, b).
Moreover, MAPK is activated in SARS-CoV-2 disease by direct stimulation or by downregulation of ACE2 (Grimes and Grimes 2020). Activated MAPK in Covid-19 leads to thrombosis, inflammation, and vasoconstriction (Grimes and Grimes 2020). Besides, the signal transducer and activator of the transcription 3(STAT3) pathway which is involved in the pathogenesis of SARS-CoV-2 is provoked in Covid-19 by pro-inflammatory cytokines (Jafarzadeh et al. 2021).
The activated STAT3 pathway encourages thrombosis, inflammation, and lung fibrosis with the development of lymphopenia (Jafarzadeh et al. 2021). Consequently, STAT3 inhibitors could be a probable treatment against Covid-19 pathogenesis and cytokine storm progression (Dhall et al. 2021). Certainly, SARS-CoV-2 infection stimulates PI3K/Akt pathway leading to inflammation and promoting viral pathogenesis (Khezri 2021). It was recently revealed that ursolic acid attenuated ALI in mice by inhibiting the expression of MAPK (Ma et al. 2014). Similarly, Liu et al. found that ursolic acid had the ability to block STAT3 pathway in hepatocellular carcinoma (Liu et al. 2017). Also, ursolic acid regulates apoptosis by regulating PI3K/Akt pathway in Huh-7 cell lines (Lee et al. 2018).
These findings suggest that ursolic acid might be effective against SARS-CoV-2 infection- provoked inflammatory changes by regulating MAPK, STAT3, and PI3K/Akt pathways.
Furthermore, NF-κB and IL-6 are extremely activated and associated with the production of cytokine storms in Covid-19 (Hojyo et al. 2020). In SARS-CoV-2 infection, viral PAMPs activate the release of IL-6 and reactivation of NF-κB in immune and non-immune cells, causing stimulation of immune response (Hojyo et al. 2020). IL-6 is regarded as a potent stimulator of STAT3 signaling pathway in Covid-19 (Al-Kuraishy et al. 2021a, b, c, d, e). Eventually, In Covid-19, activation of NF-κB and IL-6 promotes the advancement of the cytokine storm and the formation of MOI (Al-Kuraishy et al. 2021a, b, c, d, e). Of note, ursolic acid inhibits NF-κB and the expression of TLR4 by which it can reduce the propagation of inflammatory reactions (Jang et al. 2014). Also, ursolic acid prevents endothelial dysfunction by inhibiting the expression of IL-6 and C-reactive protein (CRP) in endothelial cells (HepG2 cell lines) (Lv et al. 2012). Therefore, ursolic acid may decrease the severity of SARS-CoV-2 infection through manipulation of the NF-κB/IL-6 axis.
Indeed, advanced glycation end-products (AGEs) and their receptors (RAGE) are triggered in SARS-CoV-2 infection, causing hyper inflammation and oxidative stress (Roy et al. 2021). RAGE is a pro-inflammatory receptor of pattern recognition receptors (PRRs) superfamily expressed in pulmonary epithelial cells (Kerkeni and Gharbi 2020). RAGE is stimulated by different ligands like AGEs, high mobility group box-1 (HMGB-1) and S100 protein (Ramasamy et al. 2016). RAGE complex provokes MAPK and NF-κB pathways with the following release of pro-inflammatory cytokines in SARS-CoV-2 infection (Roy et al. 2021). Thus, RAGE inhibitors could be a novel treatment target for the prevention and reducing the progression of Covid-19. RAGE inhibitors like azeliragon and TTP488 prevent RAGE from interacting with many ligands including AGEs, HMGB-1 and S100 protein which are included in the pathogenesis of SARS-CoV-2 infection limiting pulmonary inflammation and ALI/ARDS that are observed in Covid-19 (Chiappalupi et al. 2021). In this state, ursolic acid had been shown to inhibit RAGE/AGEs in pregnant rats with gestational diabetes (Dai et al. 2021). In addition, ursolic acid mitigates inflammatory disorders in mice’s prefrontal cortex by inhibiting the RAGE/AGEs signaling pathway (Lu et al. 2010).
Furthermore, HMGB-1 plasma level was exaggerated in cases with severe Covid-19 and related to inflammatory biomarkers and ICU mortality after adjusting of confounding factors (Sivakorn et al. 2021). HMGB-1 is regarded as DAMPs and can trigger inflammation in SARS-CoV-2 infection via activation of TLR4 and RAGE, leading to the release of pro-inflammatory cytokines and the development of cytokine storm (Sivakorn et al. 2021). HMGB-1 inhibitors like glycyrrhizin, hydroxychloroquine and FPS-ZM1can reduce Covid-19 severity (Chen et al. 2020a, b). Wang et al. demonstrated that ursolic acid reduces cerebral ischemic-reperfusion injury-induced inflammation by inhibiting HMGB-1 (Wang et al. 2018).
Therefore, ursolic acid might be of value in reducing SARS-CoV-2 infection complications mediated by activated RAGE/AGEs and HMGB-1.
Furthermore, autophagy and mechanistic target of the rapamycin (mTOR) pathway is linked with the pathogenesis of SARS-CoV-2 infection (Bello-Perez et al. 2020). As part of the immune defense mechanism, autophagy/macroautophagy targets viral components for lysosomal degradation and starts exposure of PAMPs to augment viral recognition (Koepke et al. 2021). SARS-CoV-2 can evade and even block autophagy to boost its replication. SARS-CoV-2 proteins like ORF3a E, M and ORF7a can induce the accumulation of autophagosomes, while SARS-CoV-2 protein Nsp15 prevents the formation of autophagosomes (Koepke et al. 2021). The overall effect of SARS-CoV-2 is inhibition of the autophagic process by inhibiting fusion between lysosomes and autophagosomes with a reduction of lysosomal acidity.
Likewise, SARS-CoV-2 infection activates mTOR pathway by blocking autophagy leading to an increase expression release of pro-inflammatory cytokines, including IL-6, with the development of cytokine storm (Appelberg et al. 2020). Thus, mTOR inhibitors may also operate as a cytokine storm immunological regulator via modulation of the release of IL-6 (Appelberg et al. 2020). Therefore, these verdicts indicated that inhibition of autophagy and induction of mTOR pathway in SARS-CoV-2 infection might increase Covid-19 severity.
Ursolic acid has been demonstrated to cause cancer cell deaths by stimulating of autophagy process (Leng et al. 2013). In addition, ursolic acid regulates the autophagy process by regulating the mTOR signaling pathway (Lu et al. 2015). Thus, these verdicts suggest that ursolic acid modulation of autophagy and the mTOR pathway may mitigate SARS-CoV-2 infection-induced inflammatory ailments.
Taken together, ursolic acid could have beneficial effects in attenuating SARS-CoV-2 infection by reducing inflammatory signaling pathways, dysregulated RAS and associated complications like ALI and ARDS [Fig. 4].
Fig. 4.
The potential effects of ursolic acid on inflammatory signaling pathways in Covid-19. SARS-CoV-2 infection activates nod-like receptor pyrin 3 (NLRP3) inflammasome, mitogen-activated protein kinase (MAPK), signal transducer and activator of transcription 3(STAT3), phosphatidylinositol 3 kinase/Akt (PI3K/Akt), nuclear factor kappa B (NF-κB), advanced glycation end-products (AGEs) and its receptors (RAGE), high mobility group box protein 1(HMGB1) and mechanistic target of rapamycin (mTOR) pathway with inhibition of autophagy. ursolic acid inhibits these inflammatory signaling pathways and activates autophagy
The current perspective had many shortcomings, including a paucity of clinical studies, and most of our perspectives were speculative and proposed depending on previous experimental studies. Therefore, this perspective opens a new spectrum for using ursolic acid in Covid-19 management.
Conclusions
The pathogenesis of SARS-CoV-2 infection requires binding to ACE2, which is highly expressed in immune and non-immune cells. Direct cytopathic impact of SARS-CoV-2 infection and related exaggerated immunoinflammatory/oxidative stress disorders lead to the development of ALI, ARDS and MOI. In virtue of its anti-inflammatory and antioxidant activity, ursolic acid can reduce SARS-CoV-2 infection-induced complications. Also, ursolic acid regulating RAS and inflammatory signaling pathways might effectively reduce ALI development in ARDS Covid-19. In this state, preclinical and clinical studies are required to substantiate the possible protective effect of ursolic acid in patients with Covid-19.
Author contributions
The authors equally participated in the development of the manuscript and provided their final approval of all content and submission for publication.
Funding
The authors have not disclosed any funding.
Data availability
Not applicable.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hayder M. Al-kuraishy, Email: hayderm36@yahoo.com
Ali I. Al-Gareeb, Email: Dr.alialgareeb78@yahoo.com
Walaa A. Negm, Email: walaa.negm@pharm.tanta.edu.eg
Gaber El-Saber Batiha, Email: gaberbatiha@gmail.com, Email: dr_gaber_batiha@vetmed.dmu.edu.eg.
References
- Al-Kuraishy HM, Hussien NR, Al-Naimi MS, Al-Buhadily AK, Al-Gareeb AI, Lungnier C. Renin–angiotensin system and fibrinolytic pathway in COVID-19: one-way skepticism. Biomed Biotechnol Res J (BBRJ) 2020;4(5):33. [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Abdullah SM, Cruz-Martins N, Batiha GE-S. Case report: hyperbilirubinemia in gilbert syndrome attenuates Covid-19-induced metabolic disturbances. Front Cardiovasc Med. 2021;8:642181. doi: 10.3389/fcvm.2021.642181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Almulaiky YQ, Cruz-Martins N, Batiha GE-S. Role of leukotriene pathway and montelukast in pulmonary and extrapulmonary manifestations of Covid-19: the enigmatic entity. Eur J Pharmacol. 2021;904:174196. doi: 10.1016/j.ejphar.2021.174196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Alqarni M, Cruz-Martins N, El-Saber Batiha G. Pleiotropic effects of tetracyclines in the management of COVID-19: emerging perspectives. Front Pharmacol. 2021;12:642822. doi: 10.3389/fphar.2021.642822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Alzahrani KJ, Alexiou A, Batiha GE-S. Niclosamide for Covid-19: bridging the gap. Mol Biol Rep. 2021;48(12):8195–8202. doi: 10.1007/s11033-021-06770-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Alzahrani KJ, Cruz-Martins N, Batiha GE-S. The potential role of neopterin in Covid-19: a new perspective. Mol Cell Biochem. 2021;476(11):4161–4166. doi: 10.1007/s11010-021-04232-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Kuraishy HM, Al-Gareeb AI, Al-Niemi MS, Aljowaie RM, Almutairi SM, Alexiou A, Batiha GE-S. The Prospective Effect of Allopurinol on the Oxidative Stress Index and Endothelial Dysfunction in Covid-19. Inflammation. 2022;45:1651–1667. doi: 10.1007/s10753-022-01648-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appelberg S, Gupta S, SvenssonAkusjärvi S, Ambikan AT, Mikaeloff F, Saccon E, Végvári Á, Benfeitas R, Sperk M, Ståhlberg M. Dysregulation in Akt/mTOR/HIF-1 signaling identified by proteo-transcriptomics of SARS-CoV-2 infected cells. Emerg Microbes Infect. 2020;9(1):1748–1760. doi: 10.1080/22221751.2020.1799723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attallah NG, El-Kadem AH, Negm WA, Elekhnawy E, El-Masry TA, Elmongy EI, Altwaijry N, Alanazi AS, Al-Hamoud GA, Ragab AE. Promising antiviral activity of agrimonia pilosa phytochemicals against severe acute respiratory syndrome coronavirus 2 supported with in vivo mice study. Pharmaceuticals. 2021;14(12):1313. doi: 10.3390/ph14121313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bag P, Chattopadhyay D, Mukherjee H, Ojha D, Mandal N, Sarkar MC, Chatterjee T, Das G, Chakraborti S. Anti-herpes virus activities of bioactive fraction and isolated pure constituent of Mallotus peltatus: an ethnomedicine from Andaman islands. Virol J. 2012;9(1):1–12. doi: 10.1186/1743-422X-9-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakhtiari N, Hosseinkhani S, Soleimani M, Hemmati R, Noori-Zadeh A, Javan M, Tashakor A. Short-term ursolic acid promotes skeletal muscle rejuvenation through enhancing of SIRT1 expression and satellite cells proliferation. Biomed Pharmacother. 2016;78:185–196. doi: 10.1016/j.biopha.2016.01.010. [DOI] [PubMed] [Google Scholar]
- Bello-Perez M, Sola I, Novoa B, Klionsky DJ, Falco A. Canonical and noncanonical autophagy as potential targets for COVID-19. Cells. 2020;9(7):1619. doi: 10.3390/cells9071619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cargnin ST, Gnoatto SB. Ursolic acid from apple pomace and traditional plants: a valuable triterpenoid with functional properties. Food Chem. 2017;220:477–489. doi: 10.1016/j.foodchem.2016.10.029. [DOI] [PubMed] [Google Scholar]
- Chen X, Wan Y, Zhou T, Li J, Wei Y. Ursolic acid attenuates lipopolysaccharide-induced acute lung injury in a mouse model. Immunotherapy. 2013;5(1):39–47. doi: 10.2217/imt.12.144. [DOI] [PubMed] [Google Scholar]
- Chen H, Gao Y, Wang A, Zhou X, Zheng Y, Zhou J. Evolution in medicinal chemistry of ursolic acid derivatives as anticancer agents. Eur J Med Chem. 2015;92:648–655. doi: 10.1016/j.ejmech.2015.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R, Huang Y, Quan J, Liu J, Wang H, Billiar TR, Lotze MT, Zeh HJ, Kang R, Tang D. HMGB1 as a potential biomarker and therapeutic target for severe COVID-19. Heliyon. 2020;6(12):e05672. doi: 10.1016/j.heliyon.2020.e05672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z, Liu Q, Zhu Z, Xiang F, Zhang M, Wu R, Kang X. Ursolic acid protects against proliferation and inflammatory response in LPS-treated gastric tumour model and cells by inhibiting NLRP3 inflammasome activation. Cancer Manag Res. 2020;12:8413. doi: 10.2147/CMAR.S264070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiappalupi S, Salvadori L, Vukasinovic A, Donato R, Sorci G, Riuzzi F. Targeting RAGE to prevent SARS-CoV-2-mediated multiple organ failure: hypotheses and perspectives. Life Sci. 2021;272:119251. doi: 10.1016/j.lfs.2021.119251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai S, Meng X, Cai X, Yuan C, Zhao Z, Zhong L, Shi Y, Yin F. Therapeutic effect of ursolic acid on fetal development in pregnant rats with gestational diabetes mellitus via AGEs-RAGE signaling pathway. J Food Biochem. 2021;45(4):e13651. doi: 10.1111/jfbc.13651. [DOI] [PubMed] [Google Scholar]
- Dhall A, Patiyal S, Sharma N, Devi NL, Raghava GP. Computer-aided prediction of inhibitors against STAT3 for managing COVID-19 associated cytokine storm. Comput Biol Med. 2021;137:104780. doi: 10.1016/j.compbiomed.2021.104780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Maro M, Cataldi M, Santillo M, Chiurazzi M, Damiano S, De Conno B, Colantuoni A, Guida B. The cholinergic and ACE-2-dependent anti-inflammatory systems in the lung: new scenarios emerging from COVID-19. Front Physiol. 2021;12:653985. doi: 10.3389/fphys.2021.653985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elekhnawy E, Negm WA. The potential application of probiotics for the prevention and treatment of COVID-19. Egypt J Med Hum Gene. 2022;23(1):1–9. doi: 10.1186/s43042-022-00252-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan D, Zhang W, Huang C, Chen J, He W, Wang A, Li B, Zhu X. Ursolic acid ameliorates CCl4-induced liver fibrosis through the NOXs/ROS pathway. J Cell Physiol. 2018;233(10):6799–6813. doi: 10.1002/jcp.26541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gayathri R, Priya D, Gunassekaran G, Sakthisekaran D. Ursolic acid attenuates oxidative stress-mediated hepatocellular carcinoma induction by diethylnitrosamine in male Wistar rats. Asian Pac J Cancer Prev. 2009;10(5):933–938. [PubMed] [Google Scholar]
- Grimes JM, Grimes KV. p38 MAPK inhibition: a promising therapeutic approach for COVID-19. J Mol Cell Cardiol. 2020;144:63–65. doi: 10.1016/j.yjmcc.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzmán-Ávila R, Flores-Morales V, Paoli P, Camici G, Ramírez-Espinosa JJ, Cerón-Romero L, Navarrete-Vázquez G, Hidalgo-Figueroa S, Yolanda Rios M, Villalobos-Molina R. Ursolic acid derivatives as potential antidiabetic agents: in vitro, in vivo, and in silico studies. Drug Dev Res. 2018;79(2):70–80. doi: 10.1002/ddr.21422. [DOI] [PubMed] [Google Scholar]
- Hojyo S, Uchida M, Tanaka K, Hasebe R, Tanaka Y, Murakami M, Hirano T. How COVID-19 induces cytokine storm with high mortality. Inflamm Regen. 2020;40(1):1–7. doi: 10.1186/s41232-020-00146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hua WJ, Hua WX, Nan FY, Jiang WA, Yan C. The influence of herbal medicine ursolic acid on the uptake of rosuvastatin mediated by OATP1B1* 1a and* 5. Eur J Drug Metab Pharmacokinet. 2014;39(3):221–230. doi: 10.1007/s13318-014-0187-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain H, Green IR, Ali I, Khan IA, Ali Z, Al-Sadi AM, Ahmed I. Ursolic acid derivatives for pharmaceutical use: a patent review (2012–2016) Expert Opin Ther Pat. 2017;27(9):1061–1072. doi: 10.1080/13543776.2017.1344219. [DOI] [PubMed] [Google Scholar]
- Jafarzadeh A, Nemati M, Jafarzadeh S. Contribution of STAT3 to the pathogenesis of COVID-19. Microb Pathog. 2021;154:104836. doi: 10.1016/j.micpath.2021.104836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang S-E, Jeong J-J, Hyam SR, Han MJ, Kim D-H. Ursolic acid isolated from the seed of cornus officinalis ameliorates colitis in mice by inhibiting the binding of lipopolysaccharide to toll-like receptor 4 on macrophages. J Agric Food Chem. 2014;62(40):9711–9721. doi: 10.1021/jf501487v. [DOI] [PubMed] [Google Scholar]
- Jinhua W. Ursolic acid: pharmacokinetics process in vitro and in vivo, a mini review. Arch Pharm. 2019;352(3):1800222. doi: 10.1002/ardp.201800222. [DOI] [PubMed] [Google Scholar]
- Kazakova OB, Gul’nara VG, Yamansarov EY, Tolstikov GA. Betulin and ursolic acid synthetic derivatives as inhibitors of papilloma virus. Bioorg Med Chem Lett. 2010;20(14):4088–4090. doi: 10.1016/j.bmcl.2010.05.083. [DOI] [PubMed] [Google Scholar]
- Kerkeni M, Gharbi J. RAGE receptor: May be a potential inflammatory mediator for SARS-COV-2 infection? Med Hypotheses. 2020;144:109950. doi: 10.1016/j.mehy.2020.109950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khezri MR. PI3K/AKT signaling pathway: a possible target for adjuvant therapy in COVID-19. Hum Cell. 2021;34(2):700–701. doi: 10.1007/s13577-021-00484-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koepke L, Hirschenberger M, Hayn M, Kirchhoff F, Sparrer KM. Manipulation of autophagy by SARS-CoV-2 proteins. Autophagy. 2021;17(9):2659–2661. doi: 10.1080/15548627.2021.1953847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong L, Li S, Liao Q, Zhang Y, Sun R, Zhu X, Zhang Q, Wang J, Wu X, Fang X. Oleanolic acid and ursolic acid: novel hepatitis C virus antivirals that inhibit NS5B activity. Antiviral Res. 2013;98(1):44–53. doi: 10.1016/j.antiviral.2013.02.003. [DOI] [PubMed] [Google Scholar]
- Kunkel SD, Elmore CJ, Bongers KS, Ebert SM, Fox DK, Dyle MC, Bullard SA, Adams CM. Ursolic acid increases skeletal muscle and brown fat and decreases diet-induced obesity, glucose intolerance and fatty liver disease. PLoS ONE. 2012;7(6):e39332. doi: 10.1371/journal.pone.0039332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K-C, Chen Y-L, Lin P-Y, Chuang W-L. Ursolic acid-induced apoptosis via regulation of the PI3K/Akt and MAPK signaling pathways in Huh-7 cells. Molecules. 2018;23(8):2016. doi: 10.3390/molecules23082016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leng S, Hao Y, Du D, Xie S, Hong L, Gu H, Zhu X, Zhang J, Fan D, H. f. Kung, Ursolic acid promotes cancer cell death by inducing Atg5-dependent autophagy. Int J Cancer. 2013;133(12):2781–2790. doi: 10.1002/ijc.28301. [DOI] [PubMed] [Google Scholar]
- Li S, Meng F, Liao X, Wang Y, Sun Z, Guo F, Li X, Meng M, Li Y, Sun C. Therapeutic role of ursolic acid on ameliorating hepatic steatosis and improving metabolic disorders in high-fat diet-induced non-alcoholic fatty liver disease rats. PLoS ONE. 2014;9(1):e86724. doi: 10.1371/journal.pone.0086724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Zhao W, Zeng X, Hao Z. Ursolic acid attenuates atherosclerosis in ApoE−/− mice: role of LOX-1 mediated by ROS/NF-κB pathway. Molecules. 2018;23(5):1101. doi: 10.3390/molecules23051101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liaudet L, Szabo C. Blocking mineralocorticoid receptor with spironolactone may have a wide range of therapeutic actions in severe COVID-19 disease. Crit Care. 2020;24(1):1–2. doi: 10.1186/s13054-020-03055-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y-N, Wang CC, Chang H-Y, Chu F-Y, Hsu Y-A, Cheng W-K, Ma W-C, Chen C-J, Wan L, Lim Y-P. Ursolic acid, a novel liver X receptor α (LXRα) antagonist inhibiting ligand-induced nonalcoholic fatty liver and drug-induced lipogenesis. J Agric Food Chem. 2018;66(44):11647–11662. doi: 10.1021/acs.jafc.8b04116. [DOI] [PubMed] [Google Scholar]
- Lin X, Fu B, Yin S, Li Z, Liu H, Zhang H, Xing N, Wang Y, Xue W, Xiong Y. ORF8 contributes to cytokine storm during SARS-CoV-2 infection by activating IL-17 pathway. Iscience. 2021;24(4):102293. doi: 10.1016/j.isci.2021.102293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu T, Ma H, Shi W, Duan J, Wang Y, Zhang C, Li C, Lin J, Li S, Lv J. Inhibition of STAT3 signaling pathway by ursolic acid suppresses growth of hepatocellular carcinoma. Int J Oncol. 2017;51(2):555–562. doi: 10.3892/ijo.2017.4035. [DOI] [PubMed] [Google Scholar]
- López-Hortas L, Pérez-Larrán P, González-Muñoz MJ, Falqué E, Domínguez H. Recent developments on the extraction and application of ursolic acid. a review. Food Res Int. 2018;103:130–149. doi: 10.1016/j.foodres.2017.10.028. [DOI] [PubMed] [Google Scholar]
- Lu J, Wu D-M, Zheng Y-L, Hu B, Zhang Z-F, Ye Q, Liu C-M, Shan Q, Wang Y-J. Ursolic acid attenuates D-galactose-induced inflammatory response in mouse prefrontal cortex through inhibiting AGEs/RAGE/NF-κB pathway activation. Cereb Cortex. 2010;20(11):2540–2548. doi: 10.1093/cercor/bhq002. [DOI] [PubMed] [Google Scholar]
- Lu X, Fan Q, Xu L, Li L, Yue Y, Xu Y, Su Y, Zhang D, Wang L. Ursolic acid attenuates diabetic mesangial cell injury through the up-regulation of autophagy via miRNA-21/PTEN/Akt/mTOR suppression. PLoS ONE. 2015;10(2):e0117400. doi: 10.1371/journal.pone.0117400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo J, Hu YL, Wang H. Ursolic acid inhibits breast cancer growth by inhibiting proliferation, inducing autophagy and apoptosis, and suppressing inflammatory responses via the PI3K/AKT and NF-κB signaling pathways in vitro. Exp Ther Med. 2017;14(4):3623–3631. doi: 10.3892/etm.2017.4965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv Y-Y, Jin Y, Han G-Z, Liu Y-X, Wu T, Liu P, Zhou Q, Liu K-X, Sun H-J. Ursolic acid suppresses IL-6 induced C-reactive protein expression in HepG2 and protects HUVECs from injury induced by CRP. Eur J Pharm Sci. 2012;45(1–2):190–194. doi: 10.1016/j.ejps.2011.11.002. [DOI] [PubMed] [Google Scholar]
- Ma C, Nakamura N, Miyashiro H, Hattori M, Shimotohno K. Inhibitory effects of ursolic acid derivatives from Cynomorium songaricum, and related triterpenes on human immunodeficiency viral protease. Phytother Res: Int J Devoted Pharmacol Toxicol Eval Natural Product Deriv. 1998;12(S1):S138–S142. doi: 10.1002/(SICI)1099-1573(1998)12:1+<S138::AID-PTR276>3.0.CO;2-5. [DOI] [Google Scholar]
- Ma J-Q, Ding J, Zhang L, Liu C-M. Ursolic acid protects mouse liver against CCl4-induced oxidative stress and inflammation by the MAPK/NF-κB pathway. Environ Toxicol Pharmacol. 2014;37(3):975–983. doi: 10.1016/j.etap.2014.03.011. [DOI] [PubMed] [Google Scholar]
- Ma T-K, Xu L, Lu L-X, Cao X, Li X, Li L-L, Wang X, Fan Q-L. Ursolic acid treatment alleviates diabetic kidney injury by regulating the ARAP1/AT1R signaling pathway. Diabetes, Metab Syndr Obes: Targets Ther. 2019;12:2597. doi: 10.2147/DMSO.S222323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGonagle D, Bridgewood C, Ramanan AV, Meaney JF, Watad A. COVID-19: angiotensin II in development of lung immunothrombosis and vasculitis mimics–Author’s reply. Lancet Rheumatol. 2021;3(5):e326. doi: 10.1016/S2665-9913(21)00065-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta OP, Bhandari P, Raut A, Kacimi SEO, Huy NT. Coronavirus disease (COVID-19): comprehensive review of clinical presentation. Front Public Health. 2021;8:582932. doi: 10.3389/fpubh.2020.582932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messner B, Zeller I, Ploner C, Frotschnig S, Ringer T, Steinacher-Nigisch A, Ritsch A, Laufer G, Huck C, Bernhard D. Ursolic acid causes DNA-damage, p53-mediated, mitochondria-and caspase-dependent human endothelial cell apoptosis, and accelerates atherosclerotic plaque formation in vivo. Atherosclerosis. 2011;219(2):402–408. doi: 10.1016/j.atherosclerosis.2011.05.025. [DOI] [PubMed] [Google Scholar]
- Miesbach W. Pathological role of angiotensin II in severe COVID-19. TH Open. 2020;4(02):e138–e144. doi: 10.1055/s-0040-1713678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra V, Soren AD, Yadav AK. Toxicological evaluations of betulinic acid and ursolic acid; common constituents of Houttuynia cordata used as an anthelmintic by the Naga tribes in north-east India. Future J Pharm Sci. 2021;7(1):1–13. [Google Scholar]
- Onohuean H, Al-Kuraishy HM, Al-Gareeb AI, Qusti S, Alshammari EM, Batiha GE-S. Covid-19 and development of heart failure: mystery and truth. Naunyn Schmiedebergs Arch Pharmacol. 2021;394(10):2013–2021. doi: 10.1007/s00210-021-02147-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parasher A. COVID-19: Current understanding of its pathophysiology, clinical presentation and treatment. Postgrad Med J. 2021;97(1147):312–320. doi: 10.1136/postgradmedj-2020-138577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peshattiwar V, Muke S, Kaikini A, Bagle S, Dighe V, Sathaye S. Mechanistic evaluation of ursolic acid against rotenone induced Parkinson’s disease–emphasizing the role of mitochondrial biogenesis. Brain Res Bull. 2020;160:150–161. doi: 10.1016/j.brainresbull.2020.03.003. [DOI] [PubMed] [Google Scholar]
- Poor HD. Pulmonary thrombosis and thromboembolism in COVID-19. Chest. 2021;160(4):1471–1480. doi: 10.1016/j.chest.2021.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radhiga T, Senthil S, Sundaresan A, Pugalendi K. Ursolic acid modulates MMPs, collagen-I, α-SMA, and TGF-β expression in isoproterenol-induced myocardial infarction in rats. Hum Exp Toxicol. 2019;38(7):785–793. doi: 10.1177/0960327119842620. [DOI] [PubMed] [Google Scholar]
- Ramasamy R, Shekhtman A, Schmidt AM. The multiple faces of RAGE–opportunities for therapeutic intervention in aging and chronic disease. Expert Opin Ther Targets. 2016;20(4):431–446. doi: 10.1517/14728222.2016.1111873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez-Rodriguez AM, González-Ortiz M, Martínez-Abundis E, Acuña Ortega N. Effect of ursolic acid on metabolic syndrome, insulin sensitivity, and inflammation. J Med Food. 2017;20(9):882–886. doi: 10.1089/jmf.2017.0003. [DOI] [PubMed] [Google Scholar]
- Roy D, Ramasamy R, Schmidt AM. Journey to a receptor for advanced glycation end products connection in severe acute respiratory syndrome coronavirus 2 infection: with stops along the way in the lung, heart, blood vessels, and adipose tissue. Arterioscler Thromb Vasc Biol. 2021;41(2):614–627. doi: 10.1161/ATVBAHA.120.315527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakuma K, Yamaguchi A. Novel intriguing strategies attenuating to sarcopenia. J Aging Res. 2012;2012:1–11. doi: 10.1155/2012/251217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saravanakumar K, Park S, Sathiyaseelan A, Kim K-N, Cho S-H, Mariadoss AVA, Wang M-H. Metabolite profiling of methanolic extract of Gardenia jaminoides by LC-MS/MS and GC-MS and its anti-diabetic, and anti-oxidant activities. Pharmaceuticals. 2021;14(2):102. doi: 10.3390/ph14020102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schönfeld D, Arias S, Bossio JC, Fernández H, Gozal D, Pérez-Chada D. Clinical presentation and outcomes of the first patients with COVID-19 in argentina: results of 207079 cases from a national database. PLoS ONE. 2021;16(2):e0246793. doi: 10.1371/journal.pone.0246793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senthil S, Chandramohan G, Pugalendi K. Isomers (oleanolic and ursolic acids) differ in their protective effect against isoproterenol-induced myocardial ischemia in rats. Int J Cardiol. 2007;119(1):131–133. doi: 10.1016/j.ijcard.2006.07.108. [DOI] [PubMed] [Google Scholar]
- Seo DY, Lee SR, Heo J-W, No M-H, Rhee BD, Ko KS, Kwak H-B, Han J. Ursolic acid in health and disease. Korean J Physiol Pharmacol. 2018;22(3):235. doi: 10.4196/kjpp.2018.22.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimada A, Inagaki M. Angiotensin I-Converting enzyme (ACE) inhibitory activity of ursolic acid isolated from Thymus vulgaris, L. Food Sci Technol Res. 2014;20(3):711–714. doi: 10.3136/fstr.20.711. [DOI] [Google Scholar]
- Shree P, Mishra P, Selvaraj C, Singh SK, Chaube R, Garg N, Tripathi YB. Targeting COVID-19 (SARS-CoV-2) main protease through active phytochemicals of ayurvedic medicinal plants–Withania somnifera (Ashwagandha), Tinospora cordifolia (Giloy) and Ocimum sanctum (Tulsi)–a molecular docking study. J Biomol Struct Dyn. 2022;40(1):190–203. doi: 10.1080/07391102.2020.1810778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivakorn C, Dechsanga J, Jamjumrus L, Boonnak K, Schultz MJ, Dondorp AM, Phumratanaprapin W, Ratanarat R, Naorungroj T, Wattanawinitchai P. High mobility group box 1 and interleukin 6 at intensive care unit admission as biomarkers in critically ill COVID-19 patients. Am J Trop Med Hyg. 2021;105(1):73. doi: 10.4269/ajtmh.21-0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaiyan A, Ravichandran K, Singh SV, Sankar M, Thomas P, Dhama K, Malik YS, Singh RK, Chaudhuri P. In silico molecular docking analysis targeting SARS-CoV-2 spike protein and selected herbal constituents. J Pure Appl Microbiol. 2020;14:989–998. doi: 10.22207/JPAM.14.SPL1.37. [DOI] [Google Scholar]
- Sun Q, He M, Zhang M, Zeng S, Chen L, Zhou L, Xu H. Ursolic acid: a systematic review of its pharmacology, toxicity and rethink on its pharmacokinetics based on PK-PD model. Fitoterapia. 2020;147:104735. doi: 10.1016/j.fitote.2020.104735. [DOI] [PubMed] [Google Scholar]
- Tiwari Pandey A, Pandey I, Zamboni P, Gemmati D, Kanase A, Singh AV, Singh MP. Traditional herbal remedies with a multifunctional therapeutic approach as an implication in COVID-19 associated co-infections. Coatings. 2020;10(8):761. doi: 10.3390/coatings10080761. [DOI] [Google Scholar]
- Tohmé M, Giménez MC, Peralta A, Colombo M, Delgui LR. Ursolic acid: a novel antiviral compound inhibiting rotavirus infection in vitro. Int J Antimicrob Agents. 2019;54(5):601–609. doi: 10.1016/j.ijantimicag.2019.07.015. [DOI] [PubMed] [Google Scholar]
- Van den Berg DF, Te Velde AA. Severe COVID-19: NLRP3 inflammasome dysregulated. Front Immunol. 2020;11:1580. doi: 10.3389/fimmu.2020.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X-H, Zhou S-Y, Qian Z-Z, Zhang H-L, Qiu L-H, Song Z, Zhao J, Wang P, Hao X-S, Wang H-Q. Evaluation of toxicity and single-dose pharmacokinetics of intravenous ursolic acid liposomes in healthy adult volunteers and patients with advanced solid tumors. Expert Opin Drug Metab Toxicol. 2013;9(2):117–125. doi: 10.1517/17425255.2013.738667. [DOI] [PubMed] [Google Scholar]
- Wang Q, Liang M, Dong Y, Yun W, Qiu F, Zhao L, Guo Y. Effects of UGT1A4 genetic polymorphisms on serum lamotrigine concentrations in Chinese children with epilepsy. Drug Metab Pharmacokinet. 2015;30(3):209–213. doi: 10.1016/j.dmpk.2014.12.007. [DOI] [PubMed] [Google Scholar]
- Wang Y, Li L, Deng S, Liu F, He Z. Ursolic acid ameliorates inflammation in cerebral ischemia and reperfusion injury possibly via high mobility group box 1/Toll-like receptor 4/NFκB pathway. Front Neurol. 2018;9:253. doi: 10.3389/fneur.2018.00253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Gao Y, Zhang Z, Chen C, Chi Q, Xu K, Yang L. Ursolic acid protects chondrocytes, exhibits anti-inflammatory properties via regulation of the NF-κB/NLRP3 inflammasome pathway and ameliorates osteoarthritis. Biomed Pharmacother. 2020;130:110568. doi: 10.1016/j.biopha.2020.110568. [DOI] [PubMed] [Google Scholar]
- Woodby B, Arnold MM, Valacchi G. SARS-CoV-2 infection, COVID-19 pathogenesis, and exposure to air pollution: what is the connection? Ann N Y Acad Sci. 2021;1486(1):15–38. doi: 10.1111/nyas.14512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie, Q., S. Tang and Y. Li (2021). "The divergent protective effects of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers on clinical outcomes of coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis." Annals of Palliative Medicine. [DOI] [PubMed]
- Yang Y, Li C, Liu N, Wang M, Zhou X, Kim IH, Wu Z. Ursolic acid alleviates heat stress-induced lung injury by regulating endoplasmic reticulum stress signaling in mice. J Nutr Biochem. 2021;89:108557. doi: 10.1016/j.jnutbio.2020.108557. [DOI] [PubMed] [Google Scholar]
- Yim E-K, Lee M-J, Lee K-H, Um S-J, Park J-S. Antiproliferative and antiviral mechanisms of ursolic acid and dexamethasone in cervical carcinoma cell lines. Int J Gynecol Cancer. 2006;16(6):2023–2031. doi: 10.1111/j.1525-1438.2006.00726.x. [DOI] [PubMed] [Google Scholar]
- Zhai M, Guo J, Ma H, Shi W, Jou D, Yan D, Liu T, Tao J, Duan J, Wang Y. Ursolic acid prevents angiotensin II-induced abdominal aortic aneurysm in apolipoprotein E-knockout mice. Atherosclerosis. 2018;271:128–135. doi: 10.1016/j.atherosclerosis.2018.02.022. [DOI] [PubMed] [Google Scholar]
- Zhang, T.-Y., C.-S. Li, P. Li, X.-Q. Bai, S.-Y. Guo, Y. Jin and S.-J. Piao (2020). "Synthesis and evaluation of ursolic acid-based 1, 2, 4-triazolo [1, 5-a] pyrimidines derivatives as anti-inflammatory agents." Molecular Diversity: 1–12. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.