Abstract
Purpose
The purpose of this review was to estimate the prevalence of screen-based disordered eating (SBDE) and several potential risk factors in university undergraduate students around the world.
Methods
An electronic search of nine data bases was conducted from the inception of the databases until 1st October 2021. Disordered eating was defined as the percentage of students scoring at or above established cut-offs on validated screening measures. Global data were also analyzed by country, research measure, and culture. Other confounders in this review were age, BMI, and sex.
Results
Using random-effects meta-analysis, the mean estimate of the distribution of effects for the prevalence of SBDE among university students (K = 105, N = 145,629) was [95% CI] = 19.7% [17.9%; 21.6%], I2 = 98.2%, Cochran's Q p value = 0.001. Bayesian meta-analysis produced an estimate of 0.24, 95% credible intervals [0.20, 0.30], τ = 92%. Whether the country in which the students were studying was Western or non-Western did not moderate these effects, but as either the mean BMI of the sample or the percentage of the sample that was female increased, the prevalence of SBDE increased.
Conclusions
These findings support previous studies indicating that many undergraduate students are struggling with disordered eating or a diagnosable eating disorder, but are neither receiver effective prevention nor accessing accurate diagnosis and available treatment. It is particularly important to develop ever more valid ways of identifying students with high levels of disordered eating and offering them original or culturally appropriate and effective prevention or early treatment.
Level of evidence
I, systematic review and meta-analysis.
Keywords: Adolescences, Body image, Body mass index, Eating disorders, Feeding and eating disorders
Introduction
Eating disorders are serious mental illnesses that usually begin in adolescence [1], and in many instances recovery requires intensive professional treatment and support [2]. Ideally, these disorders are diagnosed by a professional multidisciplinary healthcare team after a comprehensive physical and psychological assessments against established diagnostic criteria of mental disorders. The two commonly used diagnostic systems are The International Classification of Diseases (ICD), currently in its 10th edition [3], and the Diagnostic and Statistical Manual of Mental Disorders (DSM), currently in its 5th edition) [4]. The latter is used much more often for research purposes, such as epidemiological studies. Anorexia Nervosa (AN), Bulimia Nervosa (BN), Binge Eating Disorder (BED), Avoidant/Restrictive Food Intake Disorder (ARFID), and Other Specified Feeding and Eating Disorders (OFSED) are the five major eating disorders listed in the DSM-5 [4]. Each eating disorder has its own set of criteria based on extensive research and clinical experience [4].
The causes of eating disorders are unknown, although there is general agreement that a variable and complicated combination of biological, psychological, social, and cultural risk factors increase the probability of eating disorder [2]. According to Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 eating disorders impact about 42 million people globally [5], and they are frequently misdiagnosed and undertreated [6]. Moreover, their prevalence worldwide is well-documented and appears to be increasing [7–9].
The prevailing view of eating disorders is that they are categorically distinct patterns of maladaptive eating habits linked to profound cognitive modification centered on the overvaluation of weight and shape as determinants of one's identity and worthiness [1, 2]. In this regard, many experts in the field believe that “disordered eating” (defined and discussed below) is qualitatively different from the eating disorders [10–12]. For this reason, screening tests aimed at measuring patterns of disordered eating are thought not to be a good proxy for estimating the prevalence of eating disorders based on large samples. Screening tests are best used in a typical two-stage design, in which people who were found positive for the screening test criteria then participate in semi-standardized or standardized interviews to ascertain the correspondence of those interview data with internationally agreed-upon diagnostic criteria [13] For example, consider the findings of a recent systematic review and meta-analysis of the prevalence of eating disorders and disordered eating in Western Asia [14]. The prevalence of disordered eating, as measured by three widely used screening tools (see Table 1) was: Eating Attitudes Scale 26 (EAT-26) and Eating Attitudes Scale 40 (EAT-40) = 22.1%; Sick, Control, One Stone, Fat, Food (SCOFF) questionnaire = 22.3%; and the Eating Disorder Examination-Questionnaire (EDEQ) was 8.0%. On the other hand, from those studies using semi-structured interviews against established criteria ICD/DSM, the estimated prevalence of anorexia nervosa was 1.6%, while the figures for bulimia nervosa and eating disorder not otherwise specified (EDNOS [BED + OSFED]) were 2.4% and 3.5%, respectively [14].
Table 1.
Detailed description of the clinical measures involved in the systematic review and meta-analysis of disordered eating among university students, psychometric properties, cut-off points and full citation
| Measure/Scale | Cut-off point | Psychometric properties |
|---|---|---|
| ANIS | ≥ 65 | Cronbach's α ranged from 0.80 to 0.90. In the three samples the ANIS total score correlated 0.41 to 0.51 with the 28- item General Health Questionnaire, and 0.15 to 0.26 with the percentage of ideal body weight [184] |
| BEDS-7 | – | Cohen’s Kappa = 0.827 [185]. Sensitivity = 100%, specificity = 38.7% [186] |
| DEBQ | – | Cronbach's α ranged from 0.80 to 0.95. All Pearson’s correlation coefficients assessing interrelationships between scales (for restrained, emotional, and external eating) were significant, indicating that the measures have a high internal consistency and factorial validity [187] |
| EAT-26 | ≥ 20 | Cronbach's α = 0.90. EAT-26 correlates highly with the original EAT-40 scale (r = 0.98) |
| EAT-40 | 30 | Cronbach's α = 0.94. Sensitivity = 35.3%, specificity = 88.8%, positive predictive value = 24.0%, and negative predictive value = 93.2% [182] |
| EDDS | 16.5 |
Cronbach's α = 0.89. Anorexia nervosa: Sensitivity = 93%, specificity = 100%, positive predictive value = 93%, negative predictive value = 100% Bulimia nervosa: Sensitivity = 81%, specificity = 98%, positive predictive value = 97%, negative predictive value = 96% Binge-eating disorder: Sensitivity = 77%, specificity = 96%, positive predictive value = 95%, negative predictive value = 93% |
| EDE-Q | ≥ 4 |
Cronbach's α for the global score = 0.90 Women diagnosed with eating disorders scored significantly higher on the EDE-Q than the control women (sensitivity = 0.83, specificity = 0.96, positive predictive value = 0.56) [188, 189] |
| EDI | ≥ 50 | Cronbach's α ranged from 0.82 to 0.90. Sensitivity = 52.9%, specificity = 85.2%, positive predictive value = 26.4% |
| EDS-5 | – | Cronbach's α ranged from 0.83 to 0.86. Sensitivity = 0.90 and specificity = 0.88 |
| ORTO-11 | < 25 | Cronbach's α ranged between 0.74 and 0.83. Sensitivity = 75% and specificity = 84% [190] |
| ORTO-15 | < 40 | Cronbach's α = 0.83. The ORTO-15 showed significant associations with eating psychopathology (EAT-26 and SR-YBC-EDS; range r = 0.64 – 0.29; p < 0.05) [191] |
| Q-EDD | - | Cohen’s Kappa = 0.94. Sensitivity = 0.97, specificity = 0.98, positive predictive power = 0.94, and negative predictive power = 0.99 |
| SCOFF | ≥ 2 | kappa statistic = 0.82. Sensitivity = 100%; specificity = 87.5%; and positive predictive value = 90.6% |
| WCS | ≥ 52 | Cronbach's α = 0.65, 0.61, and 0.63 at ages 5, 7, and 9 years [192]. Skewness values for all items ranged from 0.02 to 0.95; and Kurtosis values ranged between -0.83 and -0.53 [193] |
ANIS Anorexia Nervosa Inventory for Self-Rating [184, 194]. BEDS-7 the 7-Item Binge-Eating Disorder Screener [186]. DEBQ The Dutch Eating Behavior Questionnaire [187]. EAT-26 Eating Attitude Test-26 [195]. EAT-40 Eating Attitude Test-40. EAT-40 Eating Attitude Test-40 [195]. EDDS Eating Disorder Diagnostic Scale [196]. EDE-Q Eating Disorder Examination – Questionnaire [197]. EDI Eating Disorder Inventory [195, 198, 199]. EDS-5 Eating Disorder Scale [200]. ORTO-11 ORTO-11 [190]. ORTO-15 ORTO-15 [201]. Q-EDD The Questionnaire for Eating Disorder Diagnoses [202]. SCOFF Sick, Control, One Stone, Fat, Food [203]. WCS the Weight Concerns scale [204]
Disordered eating
By comparison with the criteria for the eating disorders, the widely used phrase "disordered eating" is a broad construct that encompasses unhealthy (i.e., disordered) relationships with food, exercise, body weight, and one's body/body image. It sometimes refers to the presence of individual features of the clinical syndromes, and other times to unhealthy attitudes and practices such as negative body image and calorie-restrictive dieting. Typically, it is assumed that the constituents of disordered eating are less severe than the syndromes codified by DSM and ICD. Nevertheless, as is the case for negative body image, disordered eating is in and of itself a public health problem in many countries because it is associated with a number of negative health consequences, including depression, anxiety, and binge drinking [15–17].
Yet, “disordered eating” is used loosely in the literature, and rarely is it defined theoretically. Smolak and Levine have argued that disordered eating is defined by (a) “subclinical” but unhealthy, maladaptive, and misery-inducing levels of negative body image, weight and shape concerns, and calorie-restrictive dieting and/or binge eating [10–12]; plus (b) at least several of the following: individual eating disorder symptoms such as self-induced vomiting after eating; abuse of laxatives, diuretics, diet pills, and exercise; unrealistic beauty standards, including an idealization of thinness; irrational and maladaptive beliefs about body fat and fat people, often coupled with a high drive for thinness; and harsh self-surveillance and self-criticism, often in transaction with low and unstable self-esteem [10–12].
Longitudinal risk factor research consistently shows that negative body image and disordered eating are perhaps the best predictors of the development of full-blown eating disorders, at least in adolescent girls and adult women [13]. Another way of looking at disordered eating as an “at risk” status is the fact that its components constitute many of the items making up the measures used to screen people to determine, relatively quickly and at low cost, who is “at risk” for actually having an eating disorder upon closer examination using a structured diagnostic interview. Table 1 presents a list of these measures in alphabetic order. The principal purpose of this meta-analysis is to examine the prevalence of disordered eating, as assessed by these measures; hereafter we refer to this concept as screen-based disordered eating, using the acronym SBDE.
Risk and the transition to college or university
Eating disorders can emerge at any age, ranging from early childhood to older adulthood [18, 19]. However, given what is known about risk factors and the modal ages of onset, one high-risk period is late adolescence and emerging adulthood, that is, roughly ages 17 through 22 [20]. Within that developmental period, one general context associated with increased risk for eating disorders is the transition, for some people, from high school to college or university. University students are under increased pressure to conform to body and appearance ideals because romantic/sexuality expectations and peer comparisons, intensified by social media, grow alongside parental and academic demands for competitive excellence, if not perfection [21–23]. The confluence of these pressures, along with the distinct possibility of specific stressors such as parental divorce or sexual harassment/assault at college, amplify general sociocultural risk factors for disordered eating and eating disorders.
The transition to college or university also increases the probability of initiation or more frequent use of cognitive enhancers and psychostimulants to boost weight/shape/stamina management and cognitive capabilities. Drugs with potential connections to disordered eating, as well to purported success at (or at least coping with) college and its social life, include nicotine, caffeine in coffee and energy drinks, alcohol, stimulants, and dietary and ergogenic supplements [24–27]. Moreover, pressures contributing to disordered eating and eating disorders are greater for university students who fall into one or more of the following categories: identify as female; are LGTBQ + ; are involved in the performative arts (e.g., dance) or certain competitive sports; or are overweight or obese [12, 28, 29].
The reported prevalence of SBDE among various, different types of samples of university students in the literature varies from 3.1% (Liao et al. 2006) to 74.5% [30]. Variations between samples are likely due to variability in sampling methodology, sex, age, BMI, measure, and country, but this has not been investigated in a systematic way. A recent systematic review and meta-analysis by our group showed that among medical students higher BMI, Westernized culture, and the research tool used were the main confounders [31].
The explicit purpose of this meta-analysis is to provide an overall or 'absolute' estimate of the prevalence of SBDE among university students as a population at risk for eating disorders and for the distress and comorbid problems attendant to disordered eating itself.
A search of the literature and other registration platforms yielded no previous global meta-analytic review of SBDE among university students in general. Thus, this meta-analysis extends previous reviews by our research team of SBDE in medical students [31–33] by evaluating the prevalence and several potential confounders of disordered eating in more general and diverse samples of undergraduate university students across the world. Specifically, the event rate was categorized using pre-defined cut-off scores from validated screening devices, that is, continuous measurements of eating disorder risk such as the EAT-26 and SCOFF (Table 1).
To examine the sources of the expected heterogeneity in disordered eating estimates, confounder analyses, adjusting for age and BMI, will be also conducted for country, percentage of the sample that is female, culture (Western vs non- Western), measure, and timeframe/year. Results of these meta-analyses should be useful in determining allocation of resources in the development and dissemination of prevention programs for undergraduates.
Methods
This study's protocol was registered on 2021–09-19 at Open Science Framework (OSF; https://doi.org/10.17605/OSF.IO/MB74E), an open-source platform that allows researchers to share their findings with others and get assistance throughout their research. To make the review visible and avoid duplication the protocol was also entered into the PROSPERO International prospective register of systematic reviews (CRD42022303882).
This study was reported using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA2020; [34]. Statistical analyses were conducted and presented according the Meta-analysis of Observational Studies in Epidemiology (MOOSE) protocol [35].
Search strategy
During September 2021 two authors (DS and MK) did an electronic search of the literature using nine databases: PubMed/MEDLINE, American Psychological Association PsycINFO, ScienceDirect, Springer, EBSCOhost, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Scopus, and Web of Science. The full-text search was conducted according to the following keywords and lists: List A: university student [OR] tertiary student [OR] college student [AND] List B: eating disorder* [OR] eating behavior/behaviour* [OR] feeding disorder* [OR] eating symptom* [OR] eating attitude* [OR] eating problem*. The * ensures that the search term covers both the singular noun forms, as well as the reverse order of the words in the phrase. For example, searching for “eating disorder” encompasses “disordered eating” and “eating disorders”.
To verify that we included all relevant publications, we also examined the reference lists of selected articles to identify other potentially relevant articles and reviews. Meta-analyses that do not include grey literature are more likely to inflate effect size estimates, and produce less exact effect size estimates than those that do [36]. Consequently, while examining the reference sections we looked for organizational reports, unpublished studies, and studies published outside of widely known journals.
Three team members (DS, MJ, and SH) then independently assessed the initial set of articles identified by screening the titles, abstracts, and full-text articles according to the inclusion and exclusion criteria. All duplicate studies were eliminated. Initial data extraction and quality assessment were conducted independently by two team members (DS and OA). Any disputes regarding the suitability of a study for inclusion in the review were resolved by a conversation with the senior reviewer/expert clinician (ML or HJ), followed by consensus of the research team.
Eligibility inclusion and exclusion criteria
This meta-analysis included the full text of original English-language articles, published before 1 October 2021, related to SBDE among university (all countries) or college (in the USA) students. The population was defined as undergraduate students from different disciplines and majors.
To cast the net widely, we included studies that met the following criteria: (1) were published in an English-language journal; (2) the entire sample or a distinct subset of the sample consisted of university or college (in the U.S. sense of the term, i.e., not a private high school) undergraduate students; (3) participants completed one of the screening measures (see Table 1) for determining who is at-risk for an eating disorder, such that scores could indicate endorsement of the extremes of attitudes and behaviors that may exist in many cultures [10, 37, 38]; and, given the preceding criterion, (4) participant responses to the screening measure (e.g., the EAT-26) were scored and reported such that the percentages of participant falling above and below established cut-off points could be determined.
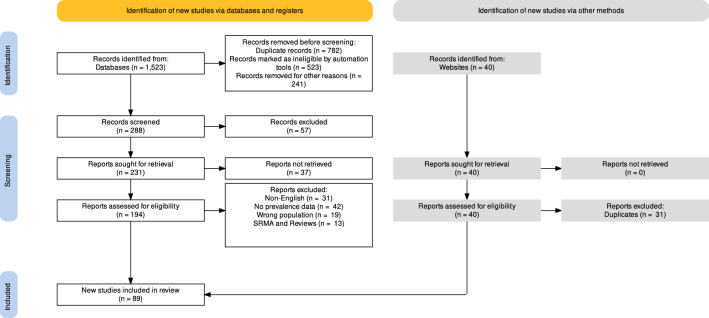
The following sources of data were excluded: (1) studies of students in post-baccalaureate programs (e.g., those pursuing masters or doctoral degrees); (2) investigations of mental health issues other than the prevalence of SBDE; and (3) studies for which we were unable to get the necessary data even after contacting the authors. Figure 1 shows the PRISMA 2020 [39] flow diagram for study selection.
Fig. 1.
PRISMA 2020 flow diagram for study selection
Procedure
ASReview, a free online tool that combines digital technologies (e.g., natural language processing) with artificial intelligence and machine learning, was used to screen and code the 89 studies selected for systematic review [40]. The Abstrackr semi-automated abstract screening tool for systematic reviews was used to increase the precision of abstract screening [41]. When necessary, data were extracted from plot images using WebPlotDigitizer v4.5, an open-source web-based tool [42].
To standardize data description the following variables, in addition to the key result of the event rate of screen-based disordered eating among university students, were independently extracted by three members of the research team (DS, MK, and SH): Author names, year of publication, country in which the data were collected, sample size, mean age (years), sex (percentage of female participants), mean body mass index (kg/m2), and measure used to determine presence or absence of SBDE. This meta-analysis study included samples from 40 countries, which were further coded into two categories, Western and non-Western countries, according to regional groups of member states defined by the United Nations [43].
Consensus among the aforementioned three reviewers was used to settle disagreements. If consensus could not be reached, a fourth author (ZS) was involved in resolving the issue by discussion. If relevant data were missing from a publication, the corresponding author of the article was contacted.
Assessment of study quality and risk of bias
The Newcastle–Ottawa Scale (NOS) was used by two authors (ZS and HJ) independently to evaluate the quality of the studies included [44]. The NOS checklist consists of three items: participants selection (sampling), comparability, and outcome and statistics. The NOS is based on a rating system [44] in which each item receives 1 to 3 (or 4) stars. This means that the maximum score for each study is either nine (cross-sectional and cohort studies) or 10 stars (randomized controlled trials and case–control studies). A study with 8 stars has good quality and low risk of bias, a study with a score of 5–7 stars has the moderate quality and moderate risk of bias, and a study with a score of 0–4 stars has low quality and high risk of bias.
Data analysis and data visualization
A classical meta-analysis based on the random-effects model was used, with the assumption that actual effects will vary over time [45]. We used the general inverse variance method with the logit transformed [PLO] proportions [46], and the DerSimonian-Laird method was used to estimate and adjust for the between-study variance in effects [47]. Random-effects modelling was used because it assumes that, in using different measures (e.g., EAT and SCOFF; Table 1), different sets of studies are estimating different, yet conceptually related, effects. For each study the pooled prevalence and the 95% confidence interval are reported.
A forest plot was used to display data [48]. It is a disadvantage that forest plots may display only confidence intervals at a significance level, such as p < 0.05. Confidence intervals should also be used to determine whether a research effect is substantial and therefore results are reproducible, so drapery plots were also used [49] and analysis of the p curve was also reported [50]. The drapery plot depicts the p value function as curves that provide the prediction range for a single future study for all individual studies and pooled values in a meta-analysis [49].
To further strengthen the results of the classical meta-analysis, Bayesian meta-analysis was also conducted and reported. Meta-analysis using Bayesian methods has three principal advantages over many classical methods [51]. First, they account for the imprecision of the between-study variance estimates [51]. Second, Bayesian methods take into account “priors”, that is, what is previously known on the topic [52]. Finally, Bayesian methods include external evidence, such as information about the effects of interventions or likely differences between studies [51, 52].
Our prior distribution focused on eating disorder prevalence in the absence of screen-based estimates and was proposed to be µ = 10%, τ = 2%, and η = 5% according to previous global estimates [53, 54]. The large eta was postulated in our review due to the amount of "error" that could be obtained using a screen-based self-reported tool, as indicated by on our comprehensive review of the clinical measures commonly used (Table 1).
Bayesian meta-analysis uses the Bayesian hierarchical model, which relies on the same basic assumptions underpinning the conventional random-effects model [55]. The difference is that in the Bayesian model the prior distribution (informative, weakly informative, or uninformative) is assumed for µ and τ2. The prior distribution describes the uncertainty surrounding a particular effect measure within a meta-analysis, such as the odds ratio or the mean difference [55]. Uncertainty may be attributable to the researchers’ subjective beliefs about the size of the effect or to sources of evidence excluded from the meta-analysis. Quantity uncertainty is reflected by the width of the prior distribution [56]. It is possible to use a non-informative prior when there is little or no available information, such that all values are equally likely [56]. A credible interval (CrI) in Bayesian statistics is a range of values where an unobserved parameter value is likely to occur [57]. In our analyses we reported the [95% CrI].
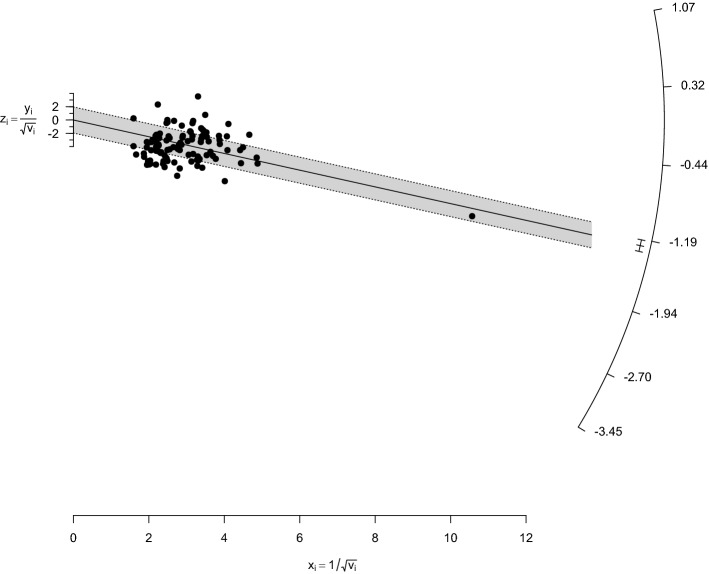
We assessed between-study heterogeneity using the I2 statistic; a value between 75 and 100% represents a high degree of heterogeneity [52]. We also evaluated heterogeneity using Cochran's Q statistics [58], and tau2 (τ2) and tau (τ) [52]. The H statistic [59] is the square root of the following: Cochran’s χ2 heterogeneity statistic divided by the degree of freedom [52]. To visualize heterogeneity we used a simple form of the Galbraith radial plot [60] in which the inverse of standard errors (horizontal axis) is plotted against observed effect sizes or outcomes standardized by their corresponding standard errors (vertical axis). On the right-hand side of a full-scale Galbraith plot, an arc shows the corresponding effect sizes or outcomes [61, 62].
Meta-analysis' validity and robustness may be compromised by the inclusion of outliers. Whenever the study's confidence interval does not align with the pooled effect's confidence interval, the study is classified as an outlier and can be addressed by the sensitivity analysis [63]. Therefore, using a Jackknife sensitivity analysis, we eliminated one study at a time to make sure we did not have any inordinate influence from any single study [64]. This analysis involves repeating the main meta-analysis as many times as the number of studies included, discarding one different study each time [64].
A publication bias occurs when the odds of research being published are influenced by its findings [65]. To investigate publication bias, funnel plots were employed as a preliminary visual tool [66]. To correct for funnel plot asymmetry owing to probable publication bias, the trim and fill approach [67] was used to generate adjusted point estimates. To conduct a more rigorous analysis of publication bias, Peters’ correlations [68] and Egger's regression [66] were also utilized as gold standards.
Subgroup meta-analyses were used to investigate heterogeneous outcomes and to answer specific queries regarding distinct populations or study characteristics [69]. Subgroup analyses were performed on categorical variables including country, culture (Western vs. non-Western), and some of the clinical measures/scales used in various studies. To investigate the effect of time as a confounder the studies were clustered into 5-year intervals: 1985–1989, 1990–1994, 1995–1999, 2001–2004, 2005–2009, 2010–2014, 2015–2019, and 2020 onwards. The subgroup meta-analyses addressed any subgroup of five studies or more, and all results are reported graphically using forest plots.
Meta-regressions are, in essence, regression models in which the values of one or more explanatory factors are used to predict the outcome variable [70]. A meta-regression analysis' regression coefficient will indicate how the outcome variable changes as the explanatory variable (the possible moderator/effect modifier/confounding variable) is increased by one unit [70]. A term for the interaction between age, sex and BMI was tested. In statistically significant meta-regression models effect size was reported using R2, and percent of variance explained of 1–8%, 9–24% and ≥ 25% were regarded as small, medium and large effect size, respectively [71].
R software for statistical computing was used to analyze all data [72]. The packages ‘meta’ [73] and ‘metafor’ [74] were used to perform all classical meta-analytics. Package ‘bayesmeta’ was used to perform Bayesian random-effects meta-analysis [75]. Using the package ‘robvis’, risk-of-bias plots were generated for quality assessment [76]. For all investigations, a summary plot (weighted) was generated to show the proportion of information inside each judgment for each domain [76]. Summary of all studies' risk of bias assessments. The risk of bias in each domain, as well as the overall risk, is depicted by a traffic light plot.
Results
Descriptive
The initial literature search, conducted during September to October 2021, yielded 1523 studies, of which 89 independent studies [7, 30, 77–163] (across all times and measures, K = 105 data points for analyses; N of participants = 149,629) met the inclusion and exclusion criteria. Details of the studies included are shown in Table 2. Of the 89 studies only two (2.2%) were grey literature: [117] and [121]. They were of a similar quality compared to the published studies.
Table 2.
Selected descriptive results of the studies included in this systematic review and meta-analysis of disordered eating among university students
| S.No. | Study label | Citation | Country | Study characteristics | Sample characteristics | Quality score |
|---|---|---|---|---|---|---|
| 1 | Abdul Manaf (2016) | [77] | Malaysia | Cross-sectional design. Sample Size N = 206. ED Measure: EAT-26 | %Female = 100%, Age = 19.5 years, BMI = 22.2 kg/m2 | 7 |
| 2 | Abo Ali (2020) | [78] | Egypt | Cross-sectional design. Sample Size N = 615. ED Measure: EAT-26 | %Female = 67.2%, Age = 21 years, BMI = 22 kg/m2 | 8 |
| 3 | Akdevelioglu (2010) | [79] | Turkey | Cross-sectional design. Sample Size N = 577. ED Measure: EAT-40 | %Female = 70%, Age = 21.2 years, BMI = 21.2 kg/m2 | 5 |
| 4 | Al Banna (2021) | [80] | Bangladesh | Cross-sectional design. Sample Size N = 365. ED Measure: EAT-26 | %Female = 49.6%, Age = 21.1 years, BMI = 22.2 kg/m2 | 8 |
| 5 | Albrahim (2019) | [81] | Saudi Arabia | Cross-sectional design. Sample Size N = 396. ED Measure: EAT-26 | %Female = 100%, Age = 20.1 years, BMI = 23.2 kg/m2 | 6 |
| 6 | Alcaraz-Ibáñez (2019) | [82] | Spain | Cross-sectional design. Sample Size N = 545. ED Measure: SCOFF | %Female = 46%, Age = 21.4 years, BMI = 23 kg/m2 | 7 |
| 7 | Alhazmi (2019) | [83] | Saudi Arabia | Cross-sectional design. Sample Size N = 342. ED Measure: EAT-26 | %Female = 50%, Age = 21.2 years, BMI = 22.2 kg/m2 | 7 |
| 8 | Alkazemi (2018) | [84] | Kuwait | Cross-sectional design. Sample Size N = 1147. ED Measure: EAT-26 | %Female = 100%, Age = 20.5 years, BMI = 23.9 kg/m2 | 7 |
| 9 | AlShebali (2020) | [85] | Saudi Arabia | Cross-sectional design. Sample Size N = 503. ED Measure: EDE-Q | %Female = 100%, Age = 19.8 years, BMI = 23.4 kg/m2 | 7 |
| 10 | Alwosaifer (2016) | [86] | Saudi Arabia | Cross-sectional design. Sample Size N = 656. ED Measure: EAT-26 | %Female = 100%, Age = 18.7 years, BMI = 22.2 kg/m2 | 7 |
| 11 | Azzouzi (2019) | [87] | Morocco | Cross-sectional design. Sample Size N = 710. ED Measure: SCOFF | %Female = 65.1%, Age = 21.3 years, BMI = 22.9 kg/m2 | 7 |
| 12 | Badrasawi (2019) | [88] | Palestine | Cross-sectional design. Sample Size N = 154. ED Measure: BEDS-7 | %Female = 100%, Age = 19.6 years, BMI = 22.2 kg/m2 | 7 |
| 13 | Barayan (2018) | [89] | Saudi Arabia | Cross-sectional design. Sample Size N = 319. ED Measure: EDE-Q | %Female = 100%, Age = 21.2 years, BMI = 22 kg/m2 | 5 |
| 14 | Barry (2021) | [90] | United States | Cross-sectional design. Sample Size N = 804. ED Measure: SCOFF | %Female = 50.4%, Age = 21.2 years, BMI = 22.2 kg/m2 | 8 |
| 15 | Benítez (2019) | [91] | Spain | Cross-sectional design. Sample Size N = 600. ED Measure: EDI | %Female = 59.5%, Age = 20.8 years, BMI = 22.2 kg/m2 | 7 |
| 16 | Bizri (2020) | [92] | Lebanon | Cross-sectional design. Sample Size N = 131. ED Measures: EAT-26; SCOFF | %Female = 53.4%, Age = 23 years, BMI = 22.2 kg/m2 | 7 |
| 17 | Bo (2014) | [93] | Italy | Cross-sectional design. Sample Size N = 440. ED Measures: EAT-26; SCOFF | %Female = 54%, Age = 19.8 years, BMI = 16.9 kg/m2 | 7 |
| 18 | Bosi (2016) | [94] | Brazil | Cross-sectional design. Sample Size N = 202. ED Measure: EAT-26 | %Female = 100%, Age = 21.8 years, BMI = 22.2 kg/m2 | 7 |
| 19 | Brumboiu (2018) | [95] | Romania | Cross-sectional design. Sample Size N = 222. ED Measure: SCOFF | %Female = 82%, Age = 21.5 years, BMI = 21.3 kg/m2 | 7 |
| 20 | Carriedo (2020) | [96] | Mexico | Cross-sectional design. Sample Size N = 911. ED Measure: EDE-Q | %Female = 65.4%, Age = 21 years, BMI = 22.6 kg/m2 | 7 |
| 21 | Castejón (2020) | [97] | Spain | Cross-sectional design. Sample Size N = 604. ED Measure: EDI | %Female = 65.9%, Age = 22.5 years, BMI = 22.2 kg/m2 | 6 |
| 22 | Chammas (2017) | [98] | Lebanon | Cross-sectional design. Sample Size N = 457. ED Measure: SCOFF | %Female = 37%, Age = 21.3 years, BMI = 22.2 kg/m2 | 6 |
| 23 | Chan (2020) | [99] | Malaysia | Cross-sectional design. Sample Size N = 1017. ED Measure: EAT-26 | %Female = 51%, Age = 20.7 years, BMI = 22 kg/m2 | 8 |
| 24 | Chaudhari (2017) | [100] | India | Cross-sectional design. Sample Size N = 193. ED Measure: EDE-Q | %Female = 60.6%, Age = 23.4 years, BMI = 24.5 kg/m2 | 7 |
| 25 | Christensen (2021) | [101] | United States | Cohort design. Sample Size N = 579. ED Measure: EDDS | %Female = 76.3%, Age = 21.8 years, BMI = 25.1 kg/m2 | 7 |
| 26 | Compte (2015) | [102] | Argentina | Cross-sectional design. Sample Size N = 472. ED Measure: EAT-26 | %Female = 0%, Age = 21.2 years, BMI = 24.8 kg/m2 | 7 |
| 27 | Damiri (2021) | [103] | Palestine | Cross-sectional design. Sample Size N = 1047. ED Measures: EAT-26; SCOFF | %Female = 61.3%, Age = 20.2 years, BMI = 23.3 kg/m2 | 8 |
| 28 | Din (2019) | [104] | Pakistan | Cross-sectional design. Sample Size N = 672. ED Measure: EAT-26 | %Female = 56%, Age = 21.7 years, BMI = 22.1 kg/m2 | 7 |
| 29 | Ebrahim (2019) | [105] | Kuwait | Cross-sectional design. Sample Size N = 400. ED Measure: EAT-26 | %Female = 0%, Age = 21.9 years, BMI = 25.8 kg/m2 | 7 |
| 30 | Erol (2019) | [106] | Turkey | Cross-sectional design. Sample Size N = 298. ED Measure: EAT-40 | %Female = 70%, Age = 21.3 years, BMI = 22.2 kg/m2 | 7 |
| 31 | Falvey (2021) | [107] | Multi | Cross-sectional design. Sample Size N = 77,193. ED Measure: SCOFF | %Female = 65.9%, Age = 23.1 years, BMI = 24.4 kg/m2 | 7 |
| 32 | Farchakh (2019) | [30] | Lebanon | Cross-sectional design. Sample Size N = 627. ED Measures: ORTO-15; EAT-26 | %Female = 50.4%, Age = 21.8 years, BMI = 23.4 kg/m2 | 8 |
| 33 | Fatima (2018) | [108] | Saudi Arabia | Cross-sectional design. Sample Size N = 120. ED Measure: EAT-26 | %Female = 100%, Age = 21.2 years, BMI = 22.2 kg/m2 | 8 |
| 34 | Gramaglia (2019) | [109] | Multi | Cross-sectional design. Sample Size N = 664. ED Measures: EAT-26; ORTO-15 | %Female = 70%, Age = 24 years, BMI = 22.2 kg/m2 | 7 |
| 35 | Greenleaf (2009) | [110] | United States | Cross-sectional design. Sample Size N = 204. ED Measure: QEDD | %Female = 100%, Age = 20.2 years, BMI = 23.1 kg/m2 | 7 |
| 36 | Havemann (2011) | [111] | South Africa | Cross-sectional design. Sample Size N = 26. ED Measure: EAT-26 | %Female = 100%, Age = 19 years, BMI = 23.2 kg/m2 | 4 |
| 37 | Herzog (1985) | [112] | United States | Cross-sectional design. Sample Size N = 121. ED Measure: SD | %Female = 100%, Age = 25.1 years, BMI = 22 kg/m2 | 5 |
| 38 | Iyer (2021) | [113] | India | Cross-sectional design. Sample Size N = 332. ED Measure: EAT-26 | %Female = 56.3%, Age = 22.3 years, BMI = 22 kg/m2 | 7 |
| 39 | Jamali (2020) | [114] | Pakistan | Cross-sectional design. Sample Size N = 407. ED Measures: EAT-26; SCOFF | %Female = 36.9%, Age = 19.9 years, BMI = 20.8 kg/m2 | 7 |
| 40 | Jennings (2006) | [115] | Australia | Cross-sectional design. Sample Size N = 240. ED Measure: EAT-26 | %Female = 100%, Age = 19.3 years, BMI = 21.2 kg/m2 | 4 |
| 41 | Joja (2012) | [116] | Germany | Case–control design. Sample Size N = 110. ED Measure: EDI | %Female = 100%, Age = 20.3 years, BMI = 21.5 kg/m2 | 8 |
| 42 | Kiss-Toth (2018) | [117] | Multi | Cross-sectional design. Sample Size N = 1965. ED Measure: SCOFF | %Female = 70%, Age = 21.2 years, BMI = 22.2 kg/m2 | 6 |
| 43 | Ko (2015) | [118] | Vietnam | Cross-sectional design. Sample Size N = 203. ED Measure: SCOFF | %Female = 100%, Age = 18.8 years, BMI = 19 kg/m2 | 7 |
| 44 | Koushiou (2019) | [119] | Greece | Cross-sectional design. Sample Size N = 334. ED Measure: WCS; EDDS | %Female = 90%, Age = 20.7 years, BMI = 22.2 kg/m2 | 7 |
| 45 | Kutlu (2013) | [120] | Turkey | Cross-sectional design. Sample Size N = 262. ED Measure: EAT-40 | %Female = 59.5%, Age = 21.7 years, BMI = 21.5 kg/m2 | 7 |
| 46 | Ladner (2019) | [121] | France | Cross-sectional design. Sample Size N = 3076. ED Measure: SCOFF | %Female = 69%, Age = 21.2 years, BMI = 22.2 kg/m2 | 7 |
| 47 | Le Grange (1998) | [122] | South Africa | Cross-sectional design. Sample Size N = 1402. ED Measure: EAT-40 | %Female = 75%, Age = 19.2 years, BMI = 22 kg/m2 | 6 |
| 48 | Lee (2015) | [123] | Korea | Cross-sectional design. Sample Size N = 199. ED Measure: DEBQ | %Female = 52.3%, Age = 29.2 years, BMI = 22 kg/m2 | 7 |
| 49 | Liao (2013) | [124] | China | Cohort design (two data points). Sample Size N = 487. ED Measure: EAT-26 | %Female = 63%, Age = 20.5 years, BMI = 20.2 kg/m2 | 7 |
| 50 | Mancilla-Diaz (2007) | [125] | Mexico | Cross-sectional design. Sample Size N = 1402. ED Measure: EAT-40 | %Female = 100%, Age = 19.2 years, BMI = 22.4 kg/m2 | 7 |
| 51 | Marciano (1988) | [126] | Canada | Cross-sectional design. Sample Size N = 994. ED Measure: EAT-26 | %Female = 84.5%, Age = 20.4 years, BMI = 22.2 kg/m2 | 6 |
| 52 | Mazzaia (2018) | [127] | Brazil | Cross-sectional design. Sample Size N = 120. ED Measure: EAT-26 | %Female = 84.2%, Age = 21.9 years, BMI = 23.3 kg/m2 | 7 |
| 53 | Mealha (2013) | [7] | Portugal | Cross-sectional design. Sample Size N = 189. ED Measures: EAT-26; EDI | %Female = 100%, Age = 20.3 years, BMI = 21.2 kg/m2 | 6 |
| 54 | Momeni (2020) | [128] | Iran | Cross-sectional design. Sample Size N = 385. ED Measure: EAT-26 | %Female = 47%, Age = 21.8 years, BMI = 22.4 kg/m2 | 7 |
| 55 | Ngan (2017) | [129] | Malaysia | Cross-sectional design. Sample Size N = 263. ED Measure: EAT-26 | %Female = 65%, Age = 22.8 years, BMI = 22 kg/m2 | 5 |
| 56 | Nichols (2009) | [130] | West Indies | Cross-sectional design. Sample Size N = 383. ED Measure: EAT-26 | %Female = 48%, Age = 21.2 years, BMI = 22.2 kg/m2 | 6 |
| 57 | Padmanabhan (2017) | [131] | United Arab Emirates | Cross-sectional design. Sample Size N = 156. ED Measure: EAT-26 | %Female = 52.6%, Age = 23.3 years, BMI = 22.2 kg/m2 | 5 |
| 58 | Parra-Fernández (2019) | [132] | Spain | Cross-sectional design. Sample Size N = 492. ED Measure: EDI | %Female = 70%, Age = 20 years, BMI = 22.6 kg/m2 | 7 |
| 59 | Parreño-Madrigal (2020) | [133] | Spain | Cross-sectional design. Sample Size N = 481. ED Measure: SCOFF | %Female = 72.6%, Age = 20.1 years, BMI = 22.4 kg/m2 | 8 |
| 60 | Pereira (2011) | [134] | Brazil | Cross-sectional design. Sample Size N = 214. ED Measure: EAT-26 | %Female = 100%, Age = 21 years, BMI = 21.1 kg/m2 | 7 |
| 61 | Pitanupong (2017) | [135] | Thailand | Cross-sectional design. Sample Size N = 885. ED Measure: EAT-26 | %Female = 56%, Age = 20.8 years, BMI = 21.2 kg/m2 | 7 |
| 62 | Plichta (2019) | [136] | Poland | Cross-sectional design. Sample Size N = 1120. ED Measure: ORTO-15 | %Female = 70.4%, Age = 21.4 years, BMI = 22 kg/m2 | 7 |
| 63 | Polanco (2020) | [137] | Mexico | Cross-sectional design. Sample Size N = 90. ED Measure: EAT-26 | %Female = 66.4%, Age = 20 years, BMI = 22 kg/m2 | 6 |
| 64 | Radwan (2018) | [138] | United Arab Emirates | Cross-sectional design. Sample Size N = 662. ED Measure: EAT-26 | %Female = 61.4%, Age = 20.4 years, BMI = 24.1 kg/m2 | 7 |
| 65 | Ramaiah (2015) | [139] | India | Cross-sectional design. Sample Size N = 172. ED Measure: EAT-26 | %Female = 65%, Age = 21 years, BMI = 21.6 kg/m2 | 7 |
| 66 | Rasman (2018) | [140] | Malaysia | Cross-sectional design. Sample Size N = 279. ED Measure: SCOFF | %Female = 75.3%, Age = 21.9 years, BMI = 22.5 kg/m2 | 8 |
| 67 | Rathner (1994) | [141] | Austria | Cross-sectional design. Sample Size N = 379. ED Measures: EDI; ANIS | %Female = 40.9%, Age = 22 years, BMI = 21 kg/m2 | 7 |
| 68 | Reyes-Rodríguez (2011) | [142] | Puerto Rico | Cross-sectional design. Sample Size N = 709. ED Measure: EAT-26 | %Female = 0%, Age = 18.3 years, BMI = 24.4 kg/m2 | 5 |
| 69 | Roshandel (2012) | [143] | Iran | Cross-sectional design. Sample Size N = 400. ED Measure: EAT-26 | %Female = 100%, Age = 22.1 years, BMI = 21.2 kg/m2 | 7 |
| 70 | Rostad (2021) | [144] | Norway | Cross-sectional design. Sample Size N = 1044. ED Measure: EDS | %Female = 70.9%, Age = 21.2 years, BMI = 22.8 kg/m2 | 8 |
| 71 | Safer (2020) | [145] | Tunisia | Cross-sectional design. Sample Size N = 974. ED Measure: SCOFF | %Female = 69.9%, Age = 22.8 years, BMI = 22.2 kg/m2 | 7 |
| 72 | Saleh (2018) | [146] | Palestine | Cross-sectional design. Sample Size N = 2001. ED Measures: EAT-26; SCOFF | %Female = 100%, Age = 19.5 years, BMI = 21.7 kg/m2 | 7 |
| 73 | Sepúlveda (2007) | [147] | Spain | Cross-sectional design. Sample Size N = 2551. ED Measure: EDI | %Female = 67.9%, Age = 21 years, BMI = 22 kg/m2 | 8 |
| 74 | Sharifian (2021) | [148] | Finland | Cross-sectional design. Sample Size N = 3110. ED Measure: SCOFF | %Female = 52.6%, Age = 21.2 years, BMI = 22.2 kg/m2 | 7 |
| 75 | Sharma (2019) | [149] | India | Cross-sectional design. Sample Size N = 370. ED Measure: EAT-26 | %Female = 42.4%, Age = 20.3 years, BMI = 22 kg/m2 | 8 |
| 76 | Shashank (2016) | [150] | India | Cross-sectional design. Sample Size N = 134. ED Measures: EAT-26; SCOFF | %Female = 100%, Age = 21.4 years, BMI = 22.4 kg/m2 | 8 |
| 77 | Spillebout (2019) | [151] | France | Cross-sectional design. Sample Size N = 731. ED Measure: SCOFF | %Female = 69.9%, Age = 20 years, BMI = 22.1 kg/m2 | 7 |
| 78 | Taha (2018) | [152] | Saudi Arabia | Cross-sectional design. Sample Size N = 1200. ED Measure: EAT-26, SCOFF | %Female = 100%, Age = 21 years, BMI = 22.2 kg/m2 | 7 |
| 79 | Tavolacci (2015) | [153] | France | Cross-sectional design. Sample Size N = 3457. ED Measure: SCOFF | %Female = 63.6%, Age = 20.5 years, BMI = 21.4 kg/m2 | 7 |
| 80 | Tavolacci (2018) | [154] | France | Cross-sectional design. Sample Size N = 1225. ED Measure: SCOFF | %Female = 61%, Age = 21.6 years, BMI = 22 kg/m2 | 7 |
| 81 | Tavolacci (2020) | [155] | France | Cross-sectional design. Sample Size N = 1493. ED Measure: SCOFF | %Female = 63.4%, Age = 20.1 years, BMI = 22.2 kg/m2 | 7 |
| 82 | Thangaraju (2020) | [156] | India | Cross-sectional design. Sample Size N = 199. ED Measure: EDE-Q | %Female = 100%, Age = 20.4 years, BMI = 23.8 kg/m2 | 7 |
| 83 | Tury (2020) | [157] | Hungary | Cohort design (two data points). Sample Size N = 538. ED Measures: ANIS; EDI | %Female = 53.9%, Age = 21.4 years, BMI = 21.4 kg/m2 | 7 |
| 84 | Uriegas (2021) | [158] | United States | Cross-sectional design. Sample Size N = 150. ED Measure: EDI | %Female = 56%, Age = 19.9 years, BMI = 25.2 kg/m2 | 7 |
| 85 | Uzun (2006) | [159] | Turkey | Cross-sectional design. Sample Size N = 414. ED Measure: EAT-40 | %Female = 100%, Age = 19.9 years, BMI = 22.2 kg/m2 | 6 |
| 86 | Weigel (2016) | [160] | Germany | Cross-sectional design. Sample Size N = 304. ED Measure: EDI | %Female = 58.2%, Age = 22.6 years, BMI = 20.1 kg/m2 | 7 |
| 87 | Yoneda (2020) | [161] | Japan | Cross-sectional design. Sample Size N = 469. ED Measure: EAT-26 | %Female = 100%, Age = 19.9 years, BMI = 20.7 kg/m2 | 7 |
| 88 | Yu (2015) | [162] | China | Cross-sectional design. Sample Size N = 1328. ED Measure: EAT-26 | %Female = 64.2%, Age = 21.2 years, BMI = 22.2 kg/m2 | 6 |
| 89 | Zhou (2020) | [163] | United States | RCT design. Sample Size N = 130. ED Measure: EDE-Q | %Female = 100%, Age = 20.8 years, BMI = 24.4 kg/m2 | 7 |
FEDS feeding and eating disorders. Quality score was computed based on Newcastle–Ottawa quality assessment scale total score for cross-sectional studies
EAT-26 Eating Attitudes Test-26, EAT-40 Eating Attitudes Test-40, SCOFF Sick, Control, One Stone, Fat, Food, EDE-Q Eating Disorder Examination- Questionnaire, BEDS-7 Binge Eating Disorder Screener-7, ORTO-15 ORTO-15, QEDD Questionnaire for Eating Disorder Diagnoses, EDDS The Eating Disorder Diagnostic Scale, SD Self-developed, WCS The Weight Concern Scale, DEBQ Dutch Eating Behavior Questionnaire, EDI Eating Disorder Inventory-I/II, ORTO-11 ORTO-11, ANIS Anorexia Nervosa Inventory for Self-Rating
Most of the studies analyzed were cross-sectional (95%), although a few used cohorts (3%) or other methodology (2%), and 11% presented data collected during the COVID-19 pandemic. Furthermore, the Eating Attitudes Test-26 (EAT-26) and Sick, Control, One Stone, Fat, Food (SCOFF) measures were the most common scales, making up 64% of total studies (see Table 3). The mean percentage of participants self-identifying as female was approximately 70% [95% CI = 66–75%], while, as expected, the average respondent's age was 21 years old [95% CI = 20–22; range 18–29 years), with a median sample mean BMI of 22 kg/m2 [95% CI = 21–24]; range 17–26 kg/m2).
Table 3.
A meta-analysis of disordered eating among university students
| Analysis | K | N | Random effects model | Heterogeneity | Confounders | Publication bias | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pooled results [95% CI or CrI] | Figure | I2a | τ | τ2b | Hc | Q | Cochran's Q P valued | Age | Sex | BMI | Egger's teste | Peter's test | |||
|
Prevalence of studies Bayesian analysis |
105 105 |
145,629 145,629 |
19.7% [17.9%; 21.6%] Odds 0.24 [0.20; 30] |
Figure 4 Figure 5 |
98.2 98% |
0.6 0.9 |
0.34 – |
7.39 – |
5696.85 – |
0.001 – |
0.49 – |
0.04 – |
0.001 – |
0.90 – |
0.06 |
| Prevalence by country | |||||||||||||||
| Saudi Arabia | 8 | 4736 | 21.2% [14.1%; 30.5%] | Figure 12 | 97.7% | 0.70 | 0.48 | – | 307.42 | 0.001 | – | – | – | NS | NS |
| India | 7 | 1534 | 18.1% [14.7%; 22.0%] | 70.1% | 0.27 | 0.076 | – | 20.05 | – | – | – | NS | NS | ||
| United states of America | 6 | 1988 | 37.1% [26.3%; 49.5%] | 95.8% | 0.61 | 0.37 | – | 117.83 | – | – | – | NS | NS | ||
| Spain | 6 | 5235 | 31.7% [20.4%; 45.6%] | 98.8% | 0.73 | 0.53 | – | 404.30 | – | – | – | NS | NS | ||
| Palestine | 5 | 6250 | 32.8% [26.2%; 40.2%] | 96.8% | 0.35 | 0.13 | – | 124.57 | – | – | – | NS | NS | ||
| Lebanon | 5 | 1966 | 33.2% [15.9%; 56.7%] | 98.8% | 1.09 | 1.19 | – | 338.83 | – | – | – | NS | NS | ||
| France | 5 | 9982 | 21.0% [18.7%; 23.6%] | 88.4% | 0.16 | 0.025 | – | 34.52 | – | – | – | NS | NS | ||
| Prevalence by culture (Western) | |||||||||||||||
| No | 55 | 29,363 | 20.9% [17.8%; 24.4%] | Figure 13 | 97.9% | 0.74 | 0.55 | – | 2711.00 | 0.001 | – | – | – | NS | NS |
| Yes | 50 | 115,966 | 18.4% [16.4%; 20.6%] | 97.8% | 0.51 | 0.26 | – | 2264.44 | – | – | – | NS | NS | ||
| Prevalence by measure | |||||||||||||||
| EAT-26 | 45 | 23,821 | 17.0% [13.9%; 20.3%] | Figure 14 | 97.6% | 0.75 | 0.56 | – | 1905.43 | 0.001 | – | – | – | NS | NS |
| SCOFF | 22 | 100,638 | 27.6% [24.1%; 31.5%] | 98.4% | 0.44 | 0.19 | – | 1413.76 | – | – | – | NS | NS | ||
| EDI | 10 | 6394 | 16.9% [9.6%; 28.2%] | 98.8% | 1.04 | 1.08 | – | 729.14 | – | – | – | NS | NS | ||
| EAT-40 | 6 | 4355 | 10.6% [7.4%; 14.9%] | 93.3% | 0.45 | 0.21 | – | 75.17 | – | – | – | NS | NS | ||
| EDE-Q | 6 | 2255 | 18.1% [8.3%; 35.0%] | 97.8% | 1.09 | 1.20 | – | 223.88 | – | – | – | NS | NS | ||
| Prevalence by Timeframe/Year | |||||||||||||||
| 2020 Onwards | 31 | 97,625 | 20.8% [17.6%; 24.5%] | Figure 15 | 98. 4% | 0.58 | 0.34 | – | 1869.51 | 0.001 | – | – | – | NS | NS |
| 2015–2019 | 50 | 35,006 | 23.8% [20.7%; 27.2%] | 97.9% | 0.63 | 0.39 | – | 2376.86 | – | – | – | NS | NS | ||
| 2010–2014 | 11 | 3256 | 13.0% [8.4%; 19.7%] | 94.6% | 0.77 | 0.60 | – | 222.67 | – | – | – | NS | NS | ||
| 2005–2009 | 8 | 6167 | 10.6% [7.3%; 15.1%] | 95.7% | 0.56 | 0.31 | – | 164.13 | – | – | – | NS | NS | ||
K Represents the number of included studies, N Represents the number of included samples
aI2 statistic referred to the percentage of variation across samples due to heterogeneity rather than chance
bτ2 Describe the extent of variation among the effects observed in different samples (between-sample variance)
cH Describes confidence intervals of heterogeneity
dSignificant differences between samples in meta-analysis
eDetects publication bias in meta-analyses
fRepresents the correlation between effect sizes and sample variation
The studies represented samples from 40 countries and territories, and the majority (54%) of studies reported data from non-Western countries. The countries and territories were: Argentina, Australia, Austria, Bangladesh, Brazil, Canada, China, Egypt, Finland, France, Germany, Greece, Hungary, India, Iran, Italy, Japan, Kuwait, Lebanon, Malaysia, Mexico, Morocco, Norway, Pakistan, Palestine, Poland, Portugal, Puerto Rico, Republic of Korea, Romania, Saudi Arabia, South Africa, Spain, Thailand, Tunisia, Turkey, United Arab Emirates, United States, Vietnam, and West Indies.
Seven countries accounted for 42% of the studies qualifying for this meta-analysis: Saudi Arabia (8%), United States of America (7%), Spain (7%), India (7%), France (5%), Malaysia (4%), and Turkey (4%).
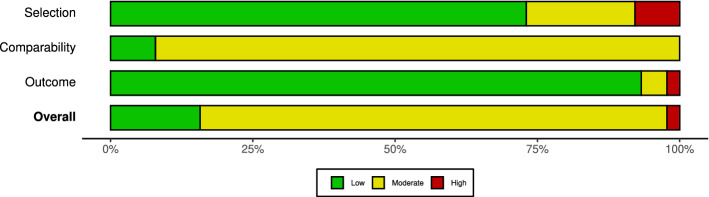
Quality assessment of included studies
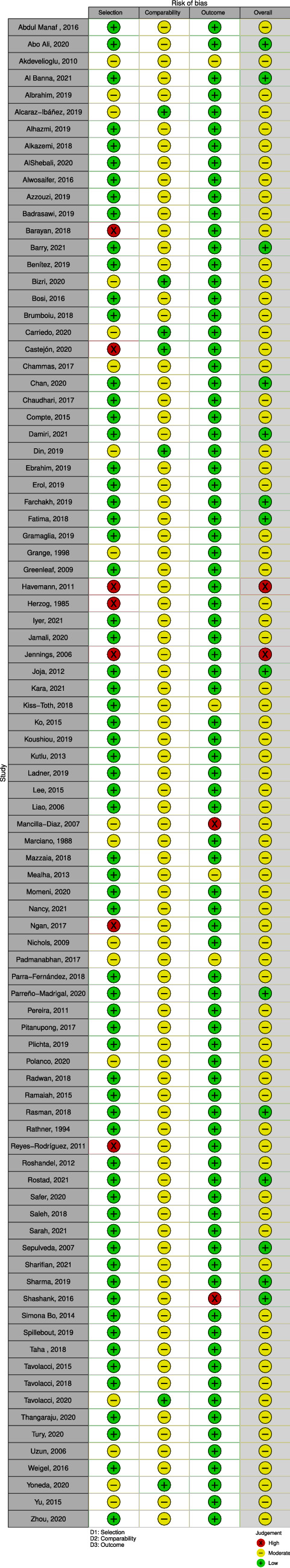
Figure 2 presents summary plots for the quality and risk of bias of the studies qualifying for this meta-analysis. The overall risk of bias in this sample of studies was moderate, as the categorization of bias was low (17%), moderate (81%), and high (2%). Figure 3 provides a summary of all studies' risk of bias assessments the risk of bias in each domain, as well as the overall risk, is depicted by a traffic light plot.
Fig. 2.
Summary plot of the assessment of the risk of bias
Fig. 3.
Traffic light plot of the assessment of the risk of bias
Meta-analysis of the overall prevalence of disordered eating
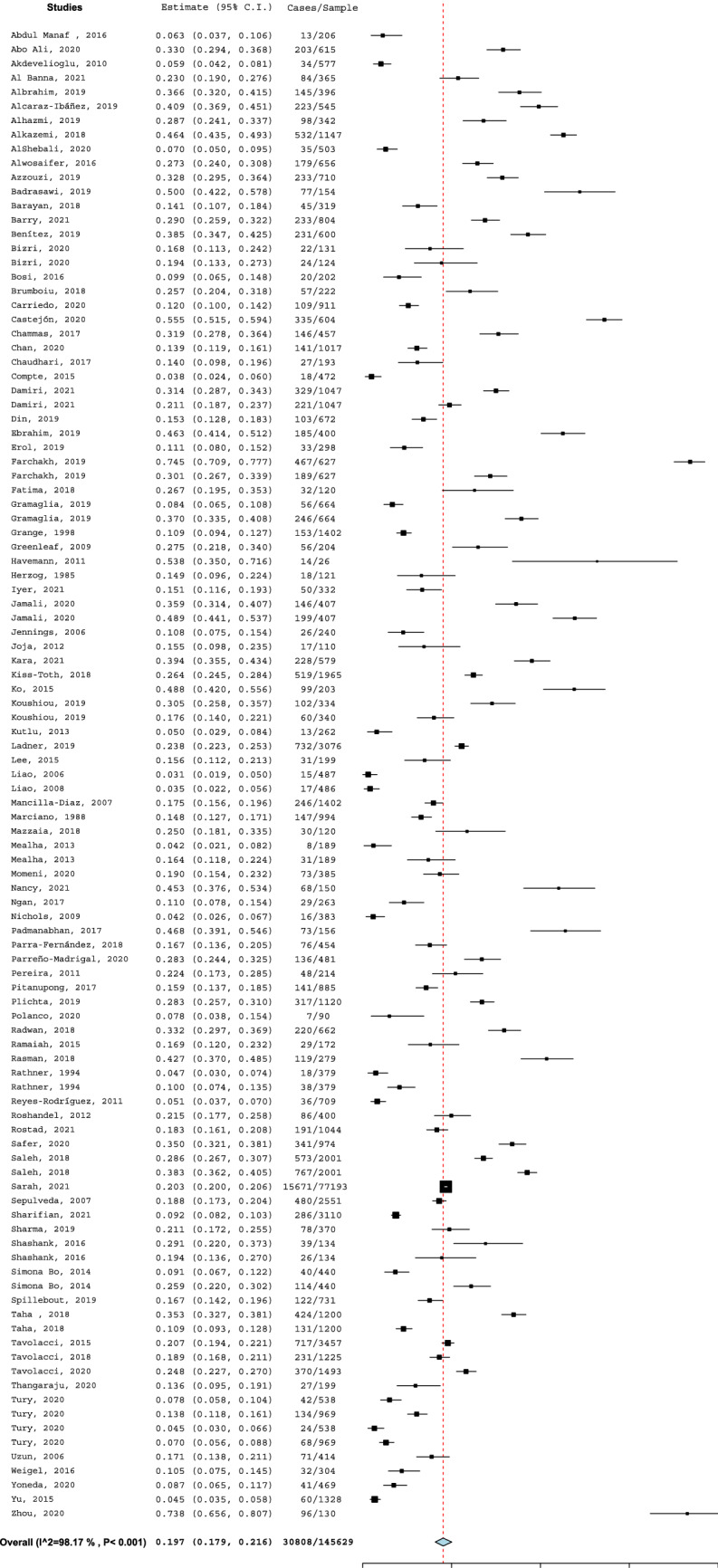
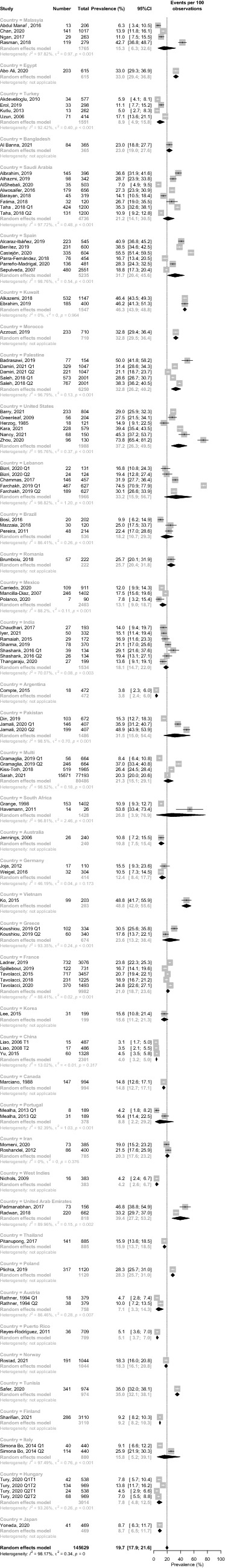
Figure 4 presents the raw prevalence data for each study and the results of the basic meta-analysis. The prevalence of SBDE among university students (k = 108, N = 146,210) using random-effects meta-analysis was (K = 105, N = 145,629) was [95% CI] = 19.7% [17.9%; 21.6%], I2 = 98.2%, τ [95% CI] = 0.6 [0.64; 0.94], τ2 [95% CI] = 0.34 [0.41; 0.88], H [95% CI] = 7.39 [7.1; 7.7], Cochran's Q p-value = 0.001. Bayesian meta-analysis, shown in Fig. 5, yielded disordered eating odds of 0.24 95% CrI [0.20, 0.30], τ = 92%. An odd estimate of 0.24 equals an SBSE prevalence of to approximately 1: 4 or more simply 24–25%.
Fig. 4.
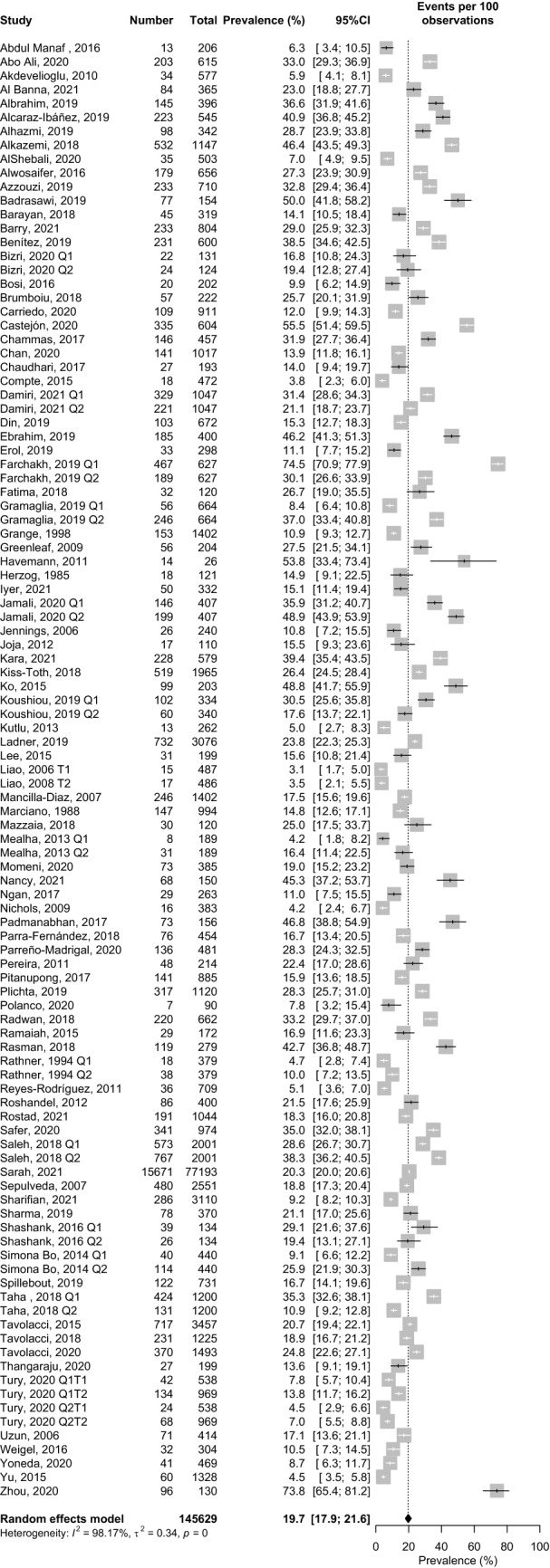
Classical random-effects meta-analysis of disordered eating in university students
Fig. 5.
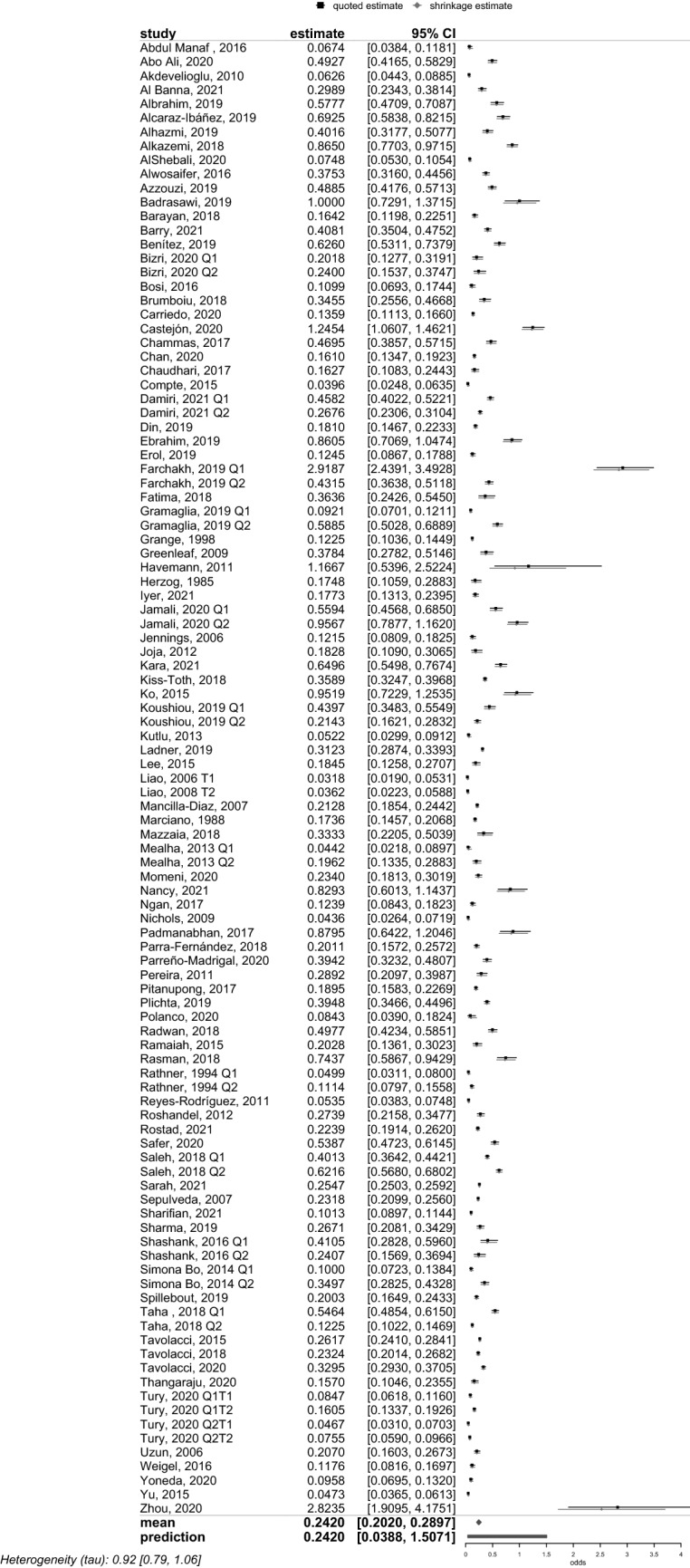
Bayesian meta-analysis of disordered eating in university students
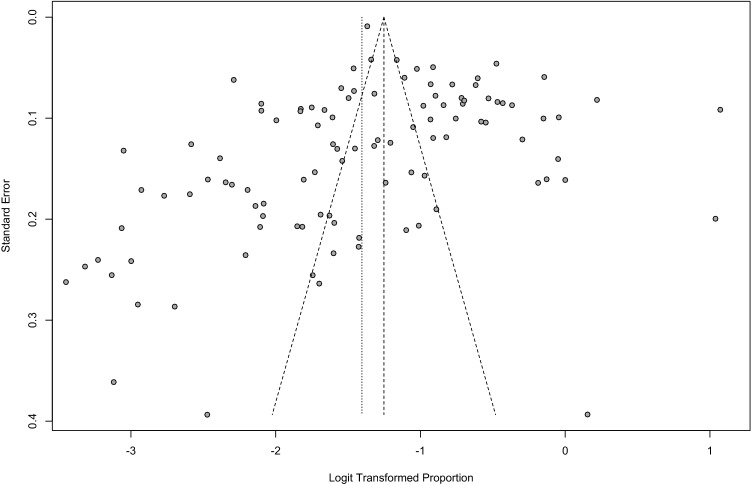
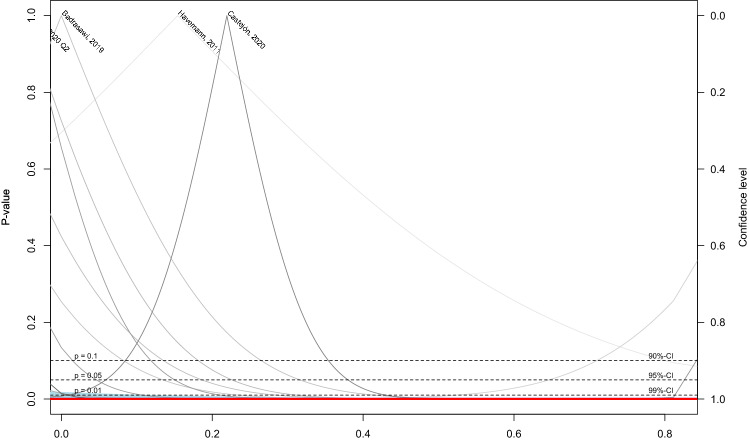
There is no publication bias in our data, as evidenced by visual examination of the funnel (Fig. 6) and Galbraith radial plots (Fig. 7), as well as Egger's regression test at 0.90 and Peter's test at 0.05. The Jackknife sensitivity analysis showed that excluding one study at a time from this meta-analysis did not affect the prevalence of SBDE in university students by more than 0.5% (Fig. 8), suggesting that our weighted prevalence findings are robust and relatively insensitive to outliers. Another indication that the results from all studies are reproducible is seen in a drapery plot based on p values (Fig. 9), which eliminates the need to rely on the p < 0.05 significance threshold when interpreting the results of any given study.
Fig. 6.
Funnel plot of disordered eating in university students
Fig. 7.
Galbraith radial plot of disordered eating in university students
Fig. 8.
Sensitivity plot of disordered eating in university students
Fig. 9.
Drapery plot of disordered eating in university students
Confounder analyses
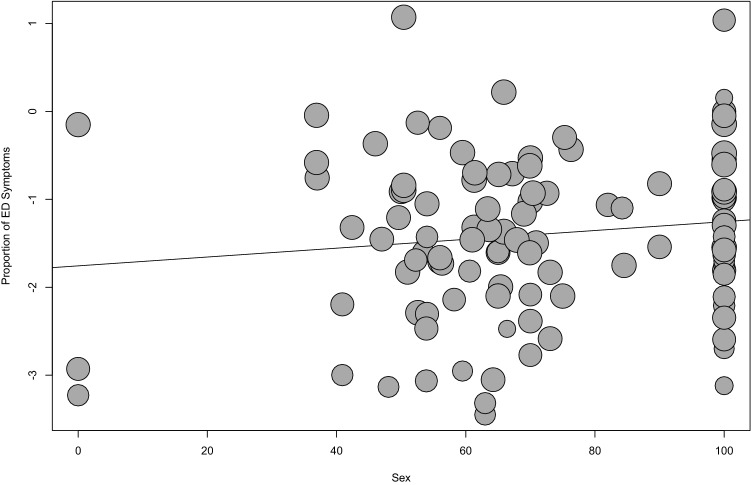
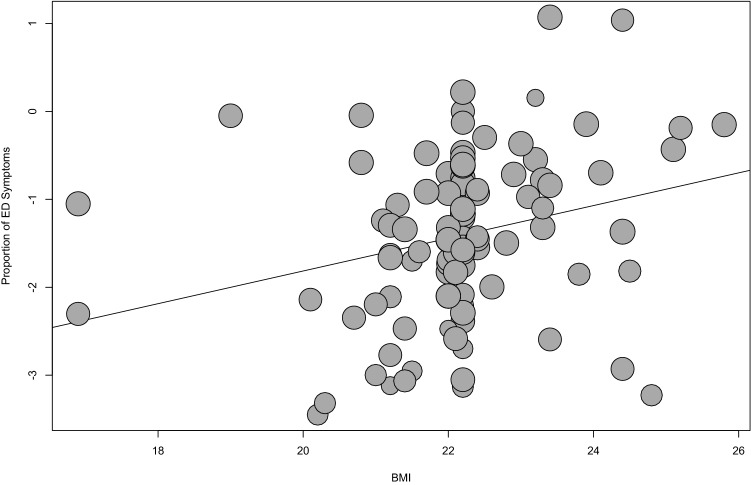
Age, BMI, and sex
Meta-regression analysis (Figs. 10 and 11) showed that BMI and sex are statistical confounders, p = 0.001 and p = 0.04, respectively, for the prevalence of SBDE in university students. As the mean BMI of the sample increased, or as the percentage of the sample that was female increased, so did the weighted prevalence of SDBE. The effect size was large for BMI (R2 = ~ 0.50), but small for the proportion of the sample that was female (R2 = ~ 20). There was no statistically significant relationship between mean age of the sample and level of disordered eating (p = 0.49; see Table 3). The study concerned university college students; thus, it is highly unlikely that age could have any impact on the estimates because of the small age range.
Fig. 10.
Meta-regression between sex and disordered eating in university students
Fig. 11.
Meta-regression between BMI and disordered eating in university students
The interaction term between age, sex and BMI yielded a statistically significant result, p = 0.01, but the interaction was not explored further because the effect size was negligible, R2 = 0.10.
Country and culture
Figure 12 shows the weighted prevalence levels as a function of country in which the data were collected. These varied tremendously, and, as noted above, the number of studies (k) was very low for many countries. Lebanon (k = 1, N = 627) reported the highest SBDE prevalence of 74.5% [70.1; 77.8], while Argentina (k = 1, N = 472) and China (k = 3, N = 2,301) reported the lowest percentages of 3.8 [2.4; 6.0], and 4.0 [3.2; 5.0], respectively. A subgroup meta-analysis, conducted for the eight countries with at least 5 studies (see Table 3), yielded evidence of statistically significant heterogeneity (p = 0.001) in the prevalence of SBDE. Visual inspection of Table 3 suggests that, at the very least, a greater percentage of university students in the USA are reporting SBDE than their counterparts in India (which has a low heterogeneity index), France, and Saudi Arabia. The difference between different countries was statistically significant, p = 0.001.
Fig. 12.
Subgroup meta-analysis by Country
Table 3 shows that non-Western countries (k = 55, N = 29,663) have a slightly higher weighted mean prevalence of SBDE, 20.9% [17.8; 24.5], than Western countries (k = 50, N = 115,966), 18.4% [16.4; 20.6], but the difference is not statistically significant (p = 0.52; see Fig. 13).
Fig. 13.
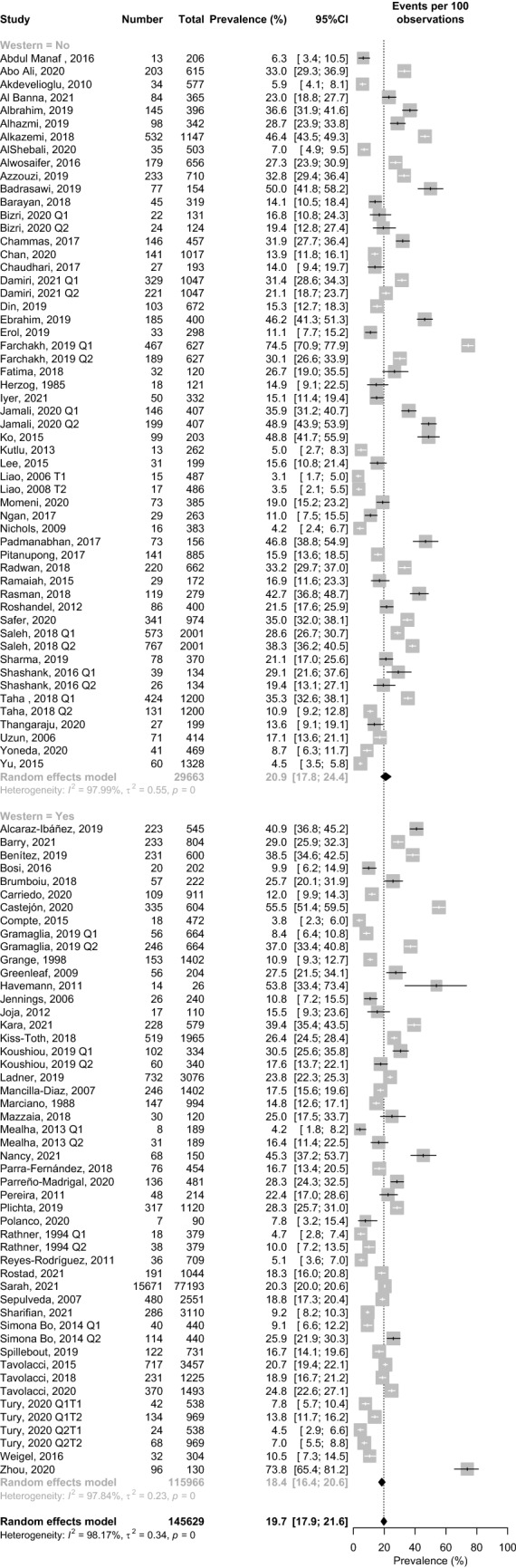
Subgroup meta-analysis by Culture.
Measure of screen-based disordered eating
There was significant heterogeneity across the various measures (Table 3) used by the sample of this studies in this meta-analysis, I2 = 98.2%, τ2 = 0.36, p = 0.001 (Fig. 14). Considering the measures as 15 categories, the BEDS-7 (k = 1, N = 154) yielded the highest SBDE prevalence at 50.0% [42.2; 57.8], while the EDE-Q (k = 1, N = 503) yielded the lowest prevalence at 7.0% [5.04; 9.54]. In descending order, the prevalence of SBDE for the measures used in at least 5 studies were SCOFF (k = 22, N = 100,638) = 27.6% [24.1; 31.5], EAT-26 (k = 45, N = 23,821) = 16.9% [13.9; 20.3], EDE-Q (k = 6, N = 2255) = 18.1% [8.4; 35.0], EDI (k = 10, N = 6,394) = 16.9% [9.6; 28.2], EAT-40 (k = 6, N = 4355) = 10.6% [7.5; 14.9].
Fig. 14.
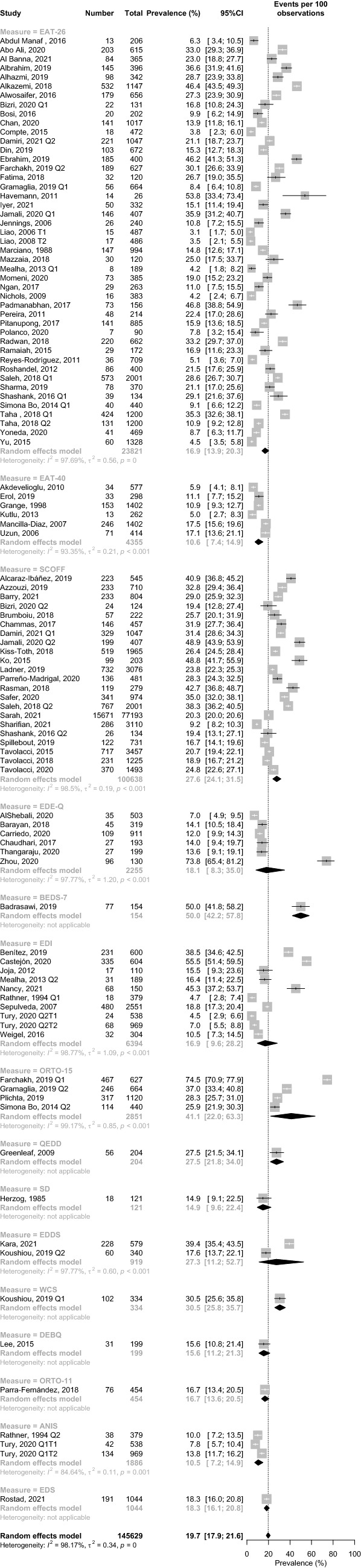
Subgroup meta-analysis by disordered eating measure
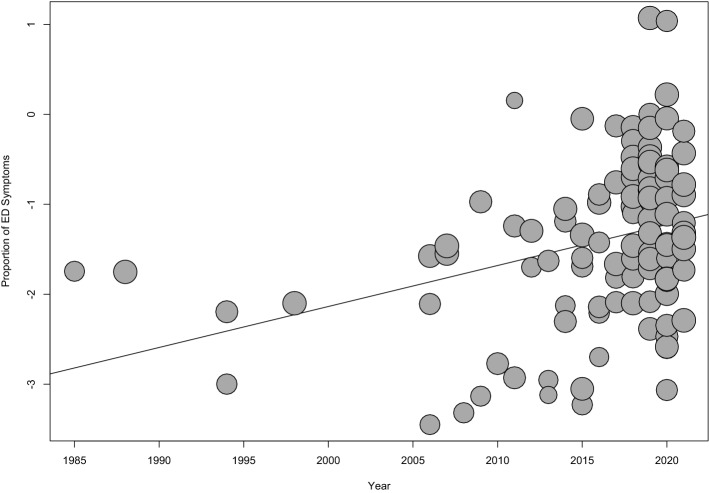
Timeframe/years
Ninety-three percent of the studies were published after 2009, while 23% were published in 2020, 2021, or 2022. No studies meeting the inclusion and exclusion criteria were published between 1995 and 2004. Results of subgroup meta-analysis showed a statistically significant (p = 0.001) increase in the prevalence of SBDE among university students (see Fig. 15). Specifically, there appears to be an increase between 2005–2014 and 2015–2022; for the categories 2005–2009, 2010–2014, 2015–2019 and 2020 onwards the weighted pooled prevalence of screen-based disordered eating was 10.6% [07.3; 15.1], 13.0% [8.3; 19.8], 23.8% [20.7; 27.2] and 20.8% [17.6; 24.5], respectively. To further illustrate the effect of year on the prevalence of SBDE among university students, a meta-regression showed that time of publication is a statistically significant predictor (p = 0.001) of increased prevalence rate of SBDE among university students (see Fig. 16).
Fig. 15.
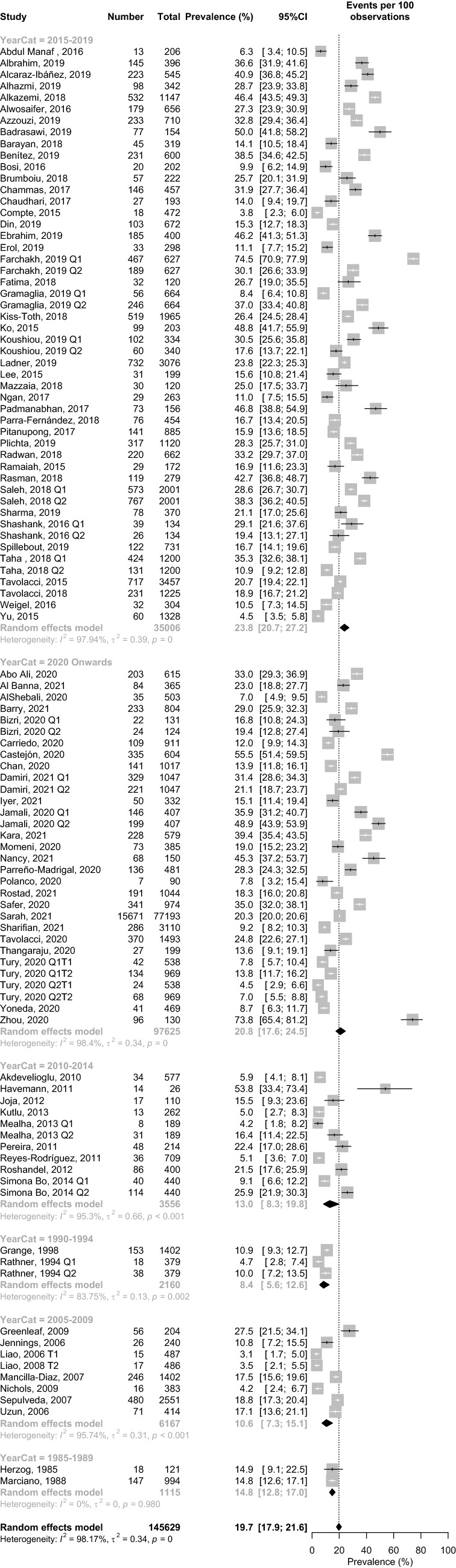
Subgroup meta-analysis by Timeframe/Year
Fig. 16.
Meta-regression between year and disordered eating in university students
Discussion
This meta-analysis of 89 studies (total N = 145,629) from 40 countries suggests that the prevalence of screen-based disordered eating among university undergraduate students is 19.7%. We also found that increasing BMI is a strong statistical confounder, while female sex is a statistically significant but weak confounder. Age, which typically does not vary a great deal for undergraduates, had an insignificant effect. Non-Western countries have a slightly higher risk prevalence of screen-based disordered eating (20.9%) compared to Western countries (18.4%), but the difference is not statistically significant. Although slight asymmetry to the right was apparent in the funnel plot, using Egger’s regression test we ruled out significant heterogeneity.
The overall screen-based prevalence rate of disordered eating (nearly 20%) is approximately twice the global prevalence of eating disorders estimates of around (approximately 10) [53, 54]. This is perhaps due to the margin of error of screen-based measurement tools combined with the fact that disordered eating focuses on the presence of individual symptoms while an eating disorder focuses on meeting a group of symptoms for a minimum period of time to meet established diagnostic criteria. However, a figure of 15–20% is also what would be expected if a number of those sometimes co-occurring symptoms were normally distributed within the populations that have been studied to date.
At 19.7%, our overall prevalence rate of screen-based disordered eating corresponds with perfectly Levine and Smolak’s (2021) conclusion based on their narrative review [12]. Furthermore our results are consistent with the findings of the two studies with the largest sample sizes: 20.3% and 20.7% in the studies by Falvey, Hahn, Anderson, Lipson, and Sonneville (2021; N = 77,193) and Tavolacci et al. (2015; N = 3457), respectively [107, 153]. We acknowledge that further research is needed, because the prevalence may be lower. If we assume that the sensitivity of measures such as the EAT-26 and the SCOFF is around 85% [6], this means that at least 15% of 20%, or at least 3%, have disordered eating beliefs, anxieties, and behaviors that are correlated with a wide variety of health problems and that put them at risk for a possible eating disorder [12, 164]. However, regardless of the psychometrics of the screening measures, epidemiological studies indicate that it is highly unlikely that 20−3% = 17%, that is, 1 in 6, university undergraduates have a diagnosable but not yet diagnosed eating disorder. If we place the point prevalence of DSM-5-defined eating disorders at a conservative estimate of 8–10% [8], then our meta-analytic findings suggest, again conservatively, that 10–12%, or at least 1 in 9, of university undergraduates meet our criteria for disordered eating.
The statistic of 1 in 9, let alone 1 in 5—or possibly 1 in 4, based on the Bayesian estimate—undergraduates scoring above the at-risk cut-off on various validated measures that screen for eating disorders and represent disordered eating deserves the attention of researchers, clinicians, public health officials, and mental health advocates for two reasons. First the rationale for, and validity data in support of, the instruments used to measure screen-based (at-risk) disordered eating strongly suggests that there are a meaningful number of university undergraduates who have an eating disorder that is currently undiagnosed and presumably untreated. Although this has been pointed out by many researchers and clinicians, it remains alarming [32] because early detection and treatment have been shown to decrease symptoms to a greater extent and improve the chance of recovery [165].
This aspect of our findings is supported by a very recent study that sought to determine whether established disparities in ED prevalence and receiving mental healthcare for marginalized groups within this population have widened or narrowed over time for different cognitive and behavioral ED symptoms, current probable EDs, lifetime ED diagnoses, and mental healthcare use among college students across the United States [166]. This study found that between 2013 and 2020 there were non-linear increases in ED symptoms and mental health care among young adults in the United States. Moreover, consistent with the data from this meta-analysis, young adults in the United States with higher BMIs had more ED burden with time, as did bisexuals, homosexual, lesbian, or queer people [166].
There has been a strong sense among clinicians in some parts of the world (e.g., the USA and Canada) that “the problem of eating disorders and disordered eating” has been worsened by the COVID-19 pandemic. In a recent study of five cross-sectional samples of French university students, surveyed at 3-year intervals between 2009 and 2021, Tavolacci et al. (2021) found that the prevalence of screen-based disordered eating for the female and male samples remained fairly stable at 26%-31% and 7–13%, respectively, between 2009 and 2018. However, for both females and males the prevalence increased dramatically (+ 20% and + 18%, respectively) between 2018 and 2021, perhaps reflecting the stressors of the COVID-19 pandemic.
Our global data, which incorporates a set of studies of French undergraduates by Tavolacci et al. (2015, 2018, 2020), paints a different picture. We also found evidence of stability—in our study, between 2005 and 2014—but the increase we noted was in the period 2015–2022. Moreover, we found a slight decrease in the weighted pooled prevalence of screen-based disordered eating from the pre-COVID period of 2015–2019 (23.8%) to the post-COVID period (2020 onwards; 20.8%). Our data are consistent with several other recent reviews [167, 168] in suggesting that a COVID-19 effect is accurate in some places and for some vulnerable people—and, in particular, people who already have an eating disorder—but not in general. Future research and meta-analytic reviews are needed to clarify the moderating and mediating variables at work here.
Over the past 10 years the prevalence and seriousness of disordered eating and eating disorders in males has received considerable attention [169]. Nevertheless, our confounder analysis indicated that, as the preponderance of females in a sample of university undergraduates increased, to a small but significant degree so did the prevalence of screen-based disordered eating. This finding, in the context of the very significant sex difference seen in, for example, the Tavolacci et al. (2021) samples, is a reminder that, while males certainly have disordered eating and eating disorders, as do those who do not identify as either female or female, there is still something about the construction, policing, and sociopolitical status of femininity that places females, including female undergraduate students, across the globe at greater risk for screen-based disordered eating, as well as eating disorders [170]. Further research, including meta-analysis, should continue to investigate risk and protective factors that moderate and mediate this disparity.
As noted previously, our confounder analyses also found that, even though the range was narrow, the greater the mean BMI of the sample, the higher the prevalence of screen-based disordered eating. Burnette et al. (2018) reported a similar finding for a sample of U.S. female undergraduate students, but not male undergraduates [28]. Our finding is also consistent with cross-sectional and longitudinal epidemiological studies of U.S. adolescents and emerging adults showing that greater levels of disordered eating and poor psychosocial health among overweight youth [171–173]. In this regard Yoon et al. (2020) reported that BMI and disordered eating behaviors rose in a correlated fashion across 15 years of 4 follow-ups of a community sample that was 11 through 18 at baseline [174].
In some cultures at least, it is likely that there is a reciprocal relationship between disordered eating and body mass gain which is mediated by internalized weight stigma and a dieting mentality, and shaped by other sociocultural factors that promote the well-established risk factors of body dissatisfaction and weight and shape concerns [174]. However, further cross-cultural research on the confounders and mediators of the relationship between BMI and screen-based disordered eating is necessary to test particular path models that acknowledge cultural variability. For example, a recent survey of Chinese female undergraduates found that the relationship between body shame and scores on a dietary restraint measure was stronger for those with lower BMI scores [175]. Moreover, a recent meta-analysis of the relationship between disordered eating and use of social networking sites found that there was a small positive relationship for university students, but regardless of sample that relationship was weaker for those with higher BMIs [176].
We did not find the age was associated with disordered eating. This is in line with the results of a study of 680 U.S. female undergraduate students who were screened to eliminate those who would probably qualify to an eating disorder diagnosis. This study found a trivial, nonsignificant association of 0.05 between age and scores on a semi-structured interview assessing screen-based disordered eating [177].
It is possible that the truncated range of the mean sample ages accounts for this null finding. Further research on the relationship between age in undergraduates and postbaccalaureate (e.g., graduate, medical, law students) and screen-based disordered eating is needed. Preliminary epidemiological data from a community sample in Cyprus indicates that a higher percentage of both men (12.3%) and women (23.2%) in the 25–45 age range met or exceeded the EAT-26 cut-off score of 20 than their counterparts in the 12–18 and 46–60 ranges [178]. Of course, age is embedded in the transition from older adolescence to emerging adulthood that is a foundation for the interest in screen-based disordered eating in undergraduates, so longitudinal designs beginning in early or mid-adolescence (see, e.g., Project EAT; Yoon et al., 2020) are needed.
Although our confounder analysis did not find a general difference in screen-based disordered eating between Western and non-Western countries, broad sociocultural factors are likely to be relevant to developmental phenomena, so cross-cultural replications will also be necessary. In this regard a cross-sectional study of over 3,200 males and females in South Korea, using the same EAT-26 cut-off score we did in our meta-analysis, found that the prevalence of disordered eating varied only between 6.7% and 7.2% for age categories 10–12, 13–14, 15–17, and older in 900 undergraduates ages 18 through 24 [179]. Yet, a previous meta-analysis by our team [33] of over 3200 pre-medical undergraduate students from Brazil, China, India, Malaysia, Pakistan, and the UK found that the prevalence of EAT-26-based disordered eating in females was moderated by higher BMI and older age, whereas this was not the case for males.
One strength of our meta-analysis with undergraduates in general is that nearly two thirds of the individual studies used the EAT-26 and SCOFF screening measures. The EAT-26 measure is well validated in a variety of clinical and non-clinical populations from different cultural backgrounds [180]. Likewise, the SCOFF measure appears to be a very practical, highly effective screening tool for detecting risk for eating disorders [181]. In contrast, we recommend against further use of the EAT-40 in studies of screen-based disordered eating, due to a very low sensitivity that results in a large rate of false-negatives [182], which probably accounts for the fact that in our meta-analysis the six studies (published between 1998 and 2019) using the EAT-40 yielded a prevalence of disordered eating (10.62%), half that of the remaining studies.
Study strengths and limitations
To our knowledge this is the first meta-analysis of the prevalence of screen-based disordered eating in the population of university undergraduate students across the world. Other strengths are the large sample size (135,454 participants from 91 studies) and the categorization of event rates using cut-off scores from well-validated measures of FEDs. Nevertheless, the findings should be interpreted with consideration of several limitations. First, the self-report nature of the data from the studies included may be confounded by shame and/or social desirability, and diluting the power of anonymity and leading to underreporting of ED symptomatology. Second, most of the studies considered by this meta-analysis had a cross-sectional design, so that the direction of the causality remains unclear. Third, we exclusively examined English Language articles, which may have led to omission of some relevant non-English articles. Finally, another limitation is inherent in one of the strengths: the inevitable heterogeneity of the numerous studies selected.
Conclusion and implications
The pooled prevalence of screen-based disordered eating in university undergraduate students in 40 countries appears to be 20%. As a number of studies eliminated people with ongoing eating disorders from their sample, this finding supports many previous studies indicating that far too many students have an eating disorder and are not accessing accurate diagnosis and available treatment (see, e.g., Falvey et al., 2021). Moreover, as probably only a 10–15% of that 20% have a diagnosable eating disorder, our data indicate that a large percentage of undergraduates are struggling with disordered eating as a biopsychosocial health problem. It is important to develop means of identifying these students and offering them original or culturally appropriate versions of the Body Project [183] or other effective preventive interventions for high-risk undergraduate students [12]. Finally, our review indicates that prospective studies, using sensitive and specific screening measures such as the EAT-26 and the SCOFF, are urgently needed to illuminate the interactions between the risk factors and to use the information to construct or improve prevention programs for students with disordered eating attitudes and behaviors.
What is already known on this subject?
Individuals with eating disorders have disordered eating attitudes and behaviors, but not everyone who engages in disordered eating has, or will be diagnosed with, an eating disorder. The difference is in the frequency and severity of the behaviors, as well as the amount of distress they cause the person.
Previous research has reported that university students have a higher prevalence of disordered eating than the general population, indicating that more research is needed.
What does this study add?
About 20% of university students exhibit a high level of screen-based disordered eating behavior and can be classified 'at risk' of developing a clinical eating disorder.
Results of Bayesian analyses confirm the results of a prevalence-based approach. This is the first time Bayesian statistics are used to compute odds of disordered eating.
Strong evidence suggests that screen- based disordered eating is increasing among university students in recent years; thus, planning access for preventive interventions and for supporting those who need outreach and treatment is urgently needed.
Funding
The authors have not disclosed any funding.
Declaration
Conflict of interest
The authors have not disclosed any competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Omar A. Alhaj, Email: omar.alhaj@uop.edu.jo
Feten Fekih-Romdhane, Email: feten.fekih@gmail.com.
Dima H. Sweidan, Email: demeswidan.52@gmail.com
Zahra Saif, Email: zsaif@health.gov.bh.
Mina F. Khudhair, Email: Mina.fattah99@yahoo.com
Hadeel Ghazzawi, Email: h.ghazzawi@ju.edu.jo.
Mohammed Sh. Nadar, Email: ot_nadar@HSC.EDU.KW
Saad S. Alhajeri, Email: Dr.Alhajeri.Saad@gmail.com
Michael P. Levine, Email: levine@kenyon.edu
Haitham Jahrami, Email: hjahrami@health.gov.bh.
References
- 1.Frank GKW, Shott ME, DeGuzman MC. The neurobiology of eating disorders. Child Adolesc Psychiatr Clin N Am. 2019;28(4):629–640. doi: 10.1016/j.chc.2019.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pop-Jordanova N, Zorcec T, Demerdzieva A. anoreXia: anorMaL PHoBia of norMaL weiGHt. Prilozi. 2017;38(2):45–53. doi: 10.1515/prilozi-2017-0021. [DOI] [PubMed] [Google Scholar]
- 3.WHO (2007) International classification of diseases and related health problems, 10th revision. World Health Organization
- 4.APA, Diagnostic and statistical manual of mental disorders: DSM-5. Vol. 5. 2013: American psychiatric association Washington, DC
- 5.Santomauro DF, et al. The hidden burden of eating disorders: an extension of estimates from the Global Burden of Disease Study 2019. Lancet Psychiatry. 2021;8(4):320–328. doi: 10.1016/S2215-0366(21)00040-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kutz AM, et al. Eating disorder screening: a systematic review and meta-analysis of diagnostic test characteristics of the SCOFF. J Gen Intern Med. 2020;35(3):885–893. doi: 10.1007/s11606-019-05478-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mealha V, et al. Students of dietetics & nutrition; a high risk group for eating disorders? Nutr Hosp. 2013;28(5):1558–1566. doi: 10.3305/nh.2013.28.5.6695. [DOI] [PubMed] [Google Scholar]
- 8.Galmiche M, et al. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am J Clin Nutr. 2019;109(5):1402–1413. doi: 10.1093/ajcn/nqy342. [DOI] [PubMed] [Google Scholar]
- 9.Qian J, et al. An update on the prevalence of eating disorders in the general population: a systematic review and meta-analysis. Eat Weight Disord. 2022;27(2):415–428. doi: 10.1007/s40519-021-01162-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levine MP, Smolak L. The prevention of eating problems and eating disorders: Theory, research, and practice. Psychology Press; 2006. [Google Scholar]
- 11.Levine M, Smolak L. The role of protective factors in the prevention of negative body image and disordered eating. Eat Disord. 2015;24:1–8. doi: 10.1080/10640266.2015.1113826. [DOI] [PubMed] [Google Scholar]
- 12.Levine MP, Smolak L (2021) The prevention of eating problems and eating disorders: Theories, research, and applications, 2nd ed. In: The prevention of eating problems and eating disorders: Theories, research, and applications, 2nd edn. New York, NY, US: Routledge/Taylor & Francis Group. xiii, 459-xiii, 459
- 13.Hoek HW, van Hoeken D. Review of the prevalence and incidence of eating disorders. Int J Eat Disord. 2003;34(4):383–396. doi: 10.1002/eat.10222. [DOI] [PubMed] [Google Scholar]
- 14.Alfalahi M, et al. Prevalence of eating disorders and disordered eating in Western Asia: a systematic review and meta-Analysis. Eat Disord. 2021 doi: 10.1080/10640266.2021.1969495. [DOI] [PubMed] [Google Scholar]
- 15.Bornioli A, et al. Adolescent body dissatisfaction and disordered eating: predictors of later risky health behaviours. Soc Sci Med. 2019;238:112458. doi: 10.1016/j.socscimed.2019.112458. [DOI] [PubMed] [Google Scholar]
- 16.Crow S, et al. Psychosocial and behavioral correlates of dieting among overweight and non-overweight adolescents. J Adolesc Health. 2006;38(5):569–574. doi: 10.1016/j.jadohealth.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 17.Rush CC, Curry JF, Looney JG. Alcohol expectancies and drinking behaviors among college students with disordered eating. J Am Coll Health. 2016;64(3):195–204. doi: 10.1080/07448481.2015.1107837. [DOI] [PubMed] [Google Scholar]
- 18.Landi F, et al. Anorexia of aging: risk factors, consequences, and potential treatments. Nutrients. 2016;8(2):69. doi: 10.3390/nu8020069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Latzer Y, et al. Childhood maltreatment in patients with binge eating disorder with and without night eating syndrome vs. control. Psychiatry Res. 2020;293:113451. doi: 10.1016/j.psychres.2020.113451. [DOI] [PubMed] [Google Scholar]
- 20.Solmi M, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2021;27(1):281–295. doi: 10.1038/s41380-021-01161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stice E, Maxfield J, Wells T. Adverse effects of social pressure to be thin on young women: an experimental investigation of the effects of "fat talk". Int J Eat Disord. 2003;34(1):108–117. doi: 10.1002/eat.10171. [DOI] [PubMed] [Google Scholar]
- 22.Aparicio-Martinez P, et al. Social media, thin-ideal, body dissatisfaction and disordered eating attitudes: an exploratory analysis. Int J Environ Res Public Health. 2019;16(21):4177. doi: 10.3390/ijerph16214177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smolak L, Levine MP (1996) Adolescent transitions and the development of eating problems. In: The developmental psychopathology of eating disorders: Implications for research, prevention, and treatment. Lawrence Erlbaum Associates, Inc. pp 207–233
- 24.Mahoney CR, et al. Intake of caffeine from all sources and reasons for use by college students. Clin Nutr. 2019;38(2):668–675. doi: 10.1016/j.clnu.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 25.Jahrami H, et al. Intake of caffeine and its association with physical and mental health status among university students in Bahrain. Foods. 2020;9(4):473. doi: 10.3390/foods9040473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Narayanan A, et al. Students’ use of caffeine, alcohol, dietary supplements, and illegal substances for improving academic performance in a New Zealand university. Health Psychol Behav Med. 2021;9(1):917–932. doi: 10.1080/21642850.2021.1990763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nagata JM, et al. Associations between ergogenic supplement use and eating behaviors among university students. Eat Disord. 2021;29(6):599–615. doi: 10.1080/10640266.2020.1712637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burnette CB, Simpson CC, Mazzeo SE. Relation of BMI and weight suppression to eating pathology in undergraduates. Eat Behav. 2018;30:16–21. doi: 10.1016/j.eatbeh.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Makino M, Tsuboi K, Dennerstein L. Prevalence of eating disorders: a comparison of Western and non-Western countries. MedGenMed. 2004;6(3):49. [PMC free article] [PubMed] [Google Scholar]
- 30.Farchakh Y, Hallit S, Soufia M. Association between orthorexia nervosa, eating attitudes and anxiety among medical students in Lebanese universities: results of a cross-sectional study. Eat Weight Disord. 2019;24(4):683–691. doi: 10.1007/s40519-019-00724-6. [DOI] [PubMed] [Google Scholar]
- 31.Fekih-Romdhane F, et al. The prevalence of feeding and eating disorders symptomology in medical students: an updated systematic review, meta-analysis, and meta-regression. Eat Weight Disord. 2022;27(6):1991–2010. doi: 10.1007/s40519-021-01351-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jahrami H, et al. Eating disorders risk among medical students: a global systematic review and meta-analysis. Eat Weight Disord. 2019;24(3):397–410. doi: 10.1007/s40519-018-0516-z. [DOI] [PubMed] [Google Scholar]
- 33.Jahrami H, et al. The relationship between risk of eating disorders, age, gender and body mass index in medical students: a meta-regression. Eat Weight Disord. 2019;24(2):169–177. doi: 10.1007/s40519-018-0618-7. [DOI] [PubMed] [Google Scholar]
- 34.Page MJ, The PRISMA, et al. Statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stroup DF, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 36.Conn VS, et al. Grey literature in meta-analyses. Nurs Res. 2003;52(4):256–261. doi: 10.1097/00006199-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 37.Ata RN, Schaefer LM, Thompson JK (2015) Sociocultural theories of eating disorders. In: The Wiley Handbook of Eating Disorders, Wiley, West Sussex, UK, pp 269–282. 10.1002/9781118574089.ch21
- 38.Gordon RA. Eating disorders: anatomy of a social epidemic. 2. Malden: Blackwell Publishing; 2000. p. 281. [Google Scholar]
- 39.Haddaway N, McGuinness L, Pritchard C (2021) PRISMA2020: R package and ShinyApp for producing PRISMA 2020 compliant flow diagrams (Version 0.0. 2) [DOI] [PMC free article] [PubMed]
- 40.van de Schoot R, et al. An open source machine learning framework for efficient and transparent systematic reviews. Nat Mach Intell. 2021;3(2):125–133. doi: 10.1038/s42256-020-00287-7. [DOI] [Google Scholar]
- 41.Rathbone J, Hoffmann T, Glasziou P. Faster title and abstract screening? Evaluating Abstrackr, a semi-automated online screening program for systematic reviewers. Syst Rev. 2015;4(1):1–7. doi: 10.1186/s13643-015-0067-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.PLOTCON. WebPlotDigitizer. 2017 [cited July 20, 2021; Available from: https://automeris.io/WebPlotDigitizer/
- 43.UN. 2022; Available from: https://www.un.org/dgacm/en/content/regional-groups
- 44.Luchini C, et al. Assessing the quality of studies in meta-analyses: advantages and limitations of the Newcastle Ottawa Scale. World J Meta-Anal. 2017;5:80–84. doi: 10.13105/wjma.v5.i4.80. [DOI] [Google Scholar]
- 45.Shuster JJ. Empirical vs natural weighting in random effects meta-analysis. Stat Med. 2010;29(12):1259–1265. doi: 10.1002/sim.3607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Borenstein M, et al. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 47.Jackson D, White IR, Thompson SG. Extending DerSimonian and Laird's methodology to perform multivariate random effects meta-analyses. Stat Med. 2010;29(12):1282–1297. doi: 10.1002/sim.3602. [DOI] [PubMed] [Google Scholar]
- 48.Lewis S, Clarke M. Forest plots: trying to see the wood and the trees. BMJ. 2001;322(7300):1479–1480. doi: 10.1136/bmj.322.7300.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rücker G, Schwarzer G. Beyond the forest plot: the drapery plot. Res Synth Methods. 2021;12(1):13–19. doi: 10.1002/jrsm.1410. [DOI] [PubMed] [Google Scholar]
- 50.van Aert RC, Wicherts JM, van Assen MA. Conducting meta-analyses based on p values: reservations and recommendations for applying p-uniform and p-curve. Perspect Psychol Sci. 2016;11(5):713–729. doi: 10.1177/1745691616650874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sutton AJ, Abrams KR. Bayesian methods in meta-analysis and evidence synthesis. Stat Methods Med Res. 2001;10(4):277–303. doi: 10.1177/096228020101000404. [DOI] [PubMed] [Google Scholar]
- 52.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 53.NAND. Eating Disorder Statistics. 2022; Available from: https://anad.org/eating-disorders-statistics/
- 54.van Eeden AE, van Hoeken D, Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2021;34(6):515–524. doi: 10.1097/YCO.0000000000000739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spiegelhalter DJ. Incorporating Bayesian ideas into health-care evaluation. Stat Sci. 2004;19(1):156–174. doi: 10.1214/088342304000000080. [DOI] [Google Scholar]
- 56.Lunn D, et al. Fully Bayesian hierarchical modelling in two stages, with application to meta-analysis. J Roy Stat Soc: Ser C (Appl Stat) 2013;62(4):551–572. doi: 10.1111/rssc.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bolstad WM, Curran JM. Introduction to Bayesian statistics. John Wiley & Sons; 2016. [Google Scholar]
- 58.Huedo-Medina TB, et al. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- 59.Lin L, Chu H, Hodges JS. Alternative measures of between-study heterogeneity in meta-analysis: reducing the impact of outlying studies. Biometrics. 2017;73(1):156–166. doi: 10.1111/biom.12543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Galbraith RF. Some applications of radial plots. J Am Stat Assoc. 1994;89(428):1232–1242. doi: 10.1080/01621459.1994.10476864. [DOI] [Google Scholar]
- 61.Galbraith R. Graphical display of estimates having differing standard errors. Technometrics. 1988;30(3):271–281. doi: 10.1080/00401706.1988.10488400. [DOI] [Google Scholar]
- 62.Galbraith R. A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med. 1988;7(8):889–894. doi: 10.1002/sim.4780070807. [DOI] [PubMed] [Google Scholar]
- 63.Viechtbauer W, Cheung MW. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1(2):112–125. doi: 10.1002/jrsm.11. [DOI] [PubMed] [Google Scholar]
- 64.Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37(5):1148–1157. doi: 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mathur MB, VanderWeele TJ. Sensitivity analysis for publication bias in meta-analyses. J Roy Stat Soc: Ser C (Appl Stat) 2020;69(5):1091–1119. doi: 10.1111/rssc.12440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Egger M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Duval S, Tweedie R. A nonparametric, "Trim and Fill" method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95(449):89–98. [Google Scholar]
- 68.Peters JL, et al. Assessing publication bias in meta-analyses in the presence of between-study heterogeneity. J R Stat Soc. 2010;173(3):575–591. doi: 10.1111/j.1467-985X.2009.00629.x. [DOI] [Google Scholar]
- 69.Sedgwick P. Meta-analyses: heterogeneity and subgroup analysis. BMJ. 2013;346:f4040. doi: 10.1136/bmj.f4040. [DOI] [PubMed] [Google Scholar]
- 70.Thompson SG, Higgins JP. How should meta-regression analyses be undertaken and interpreted? Stat Med. 2002;21(11):1559–1573. doi: 10.1002/sim.1187. [DOI] [PubMed] [Google Scholar]
- 71.Open Science Collaboration Estimating the reproducibility of psychological science. Science. 2015;349(6251):aac4716. doi: 10.1126/science.aac4716. [DOI] [PubMed] [Google Scholar]
- 72.R. 4.1.1. R Foundation for Statistical Computing, Vienna, Austria. 2021 2020 05/05/2020]; Available from: https://www.R-project.org/
- 73.Schwarzer G, Schwarzer MG (2012) Package ‘meta’. The R foundation for statistical computing, p 9
- 74.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1–48. doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- 75.Roever C, Friede T, Roever MC (2017) Package ‘bayesmeta’
- 76.McGuinness LA, Higgins JP. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55–61. doi: 10.1002/jrsm.1411. [DOI] [PubMed] [Google Scholar]
- 77.Abdul Manaf N, Saravanan C, Zuhrah B. The prevalence and inter-relationship of negative body image perception, depression and susceptibility to eating disorders among female medical undergraduate students. J Clin Diagn Res. 2016;10(3):01. doi: 10.7860/JCDR/2016/16678.7341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Abo Ali EA, Shehata WM. Eating disorder risk among medical students at Tanta University, Egypt. Egyptian J Commun Med. 2020;38(4):17. doi: 10.21608/ejcm.2020.119410. [DOI] [Google Scholar]
- 79.Akdevelioglu Y, Gümüs H. Eating disorders and body image perception among university students. Pak J Nutr. 2010;9(12):1187–1191. doi: 10.3923/pjn.2010.1187.1191. [DOI] [Google Scholar]
- 80.Al Banna MH, et al. Prevalence and determinants of eating disorder risk among Bangladeshi public university students: a cross-sectional study. Health Psychol Res. 2021;9(1):24837. doi: 10.52965/001c.24837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Albrahim T, et al. The spectrum of disordered eating attitudes among female university students: a cross-sectional study. Curr Res Nutr Food Sci J. 2019;7(3):698–707. doi: 10.12944/CRNFSJ.7.3.10. [DOI] [Google Scholar]
- 82.Alcaraz-Ibáñez M, Sicilia A, Paterna A. Exploring the differentiated relationship between appearance and fitness-related social anxiety and the risk of eating disorders and depression in young adults. Scand J Psychol. 2019;60(6):569–576. doi: 10.1111/sjop.12584. [DOI] [PubMed] [Google Scholar]
- 83.Alhazmi AH, Al Johani A. Prevalence and associated factors of eating disorders among students in Taiba University, Saudi Arabia: a cross-sectional study. Malaysian J Public Health Med. 2019;19(1):172–176. doi: 10.37268/mjphm/vol.19/no.1/art.80. [DOI] [Google Scholar]
- 84.Alkazemi D, et al. Distorted weight perception correlates with disordered eating attitudes in Kuwaiti college women. Int J Eat Disord. 2018;51(5):449–458. doi: 10.1002/eat.22852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.AlShebali M, AlHadi A, Waller G. The impact of ongoing westernization on eating disorders and body image dissatisfaction in a sample of undergraduate Saudi women. Eat Weight Disord. 2021;26(6):1835–1844. doi: 10.1007/s40519-020-01028-w. [DOI] [PubMed] [Google Scholar]
- 86.Alwosaifer AM, et al. Eating disorders and associated risk factors among Imam Abdulrahman bin Faisal university preparatory year female students in Kingdom of Saudi Arabia. Saudi Med J. 2018;39(9):910. doi: 10.15537/smj.2018.9.23314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Azzouzi N, et al. Eating disorders among Moroccan medical students: cognition and behavior. Psychol Res Behav Manag. 2019;12:129. doi: 10.2147/PRBM.S165114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Badrasawi MM, Zidan SJ. Binge eating symptoms prevalence and relationship with psychosocial factors among female undergraduate students at Palestine Polytechnic University: a cross-sectional study. J Eat Disord. 2019;7(1):1–8. doi: 10.1186/s40337-019-0263-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Barayan S, Al-Yousif Z, Sabra A. Prevalence of eating disorders among female university medical students in Dammam, Saudi Arabia. Int J Med Health Sci. 2018;7(3):107–112. [Google Scholar]
- 90.Barry MR, Sonneville KR, Leung CW. Students with food insecurity are more likely to screen positive for an eating disorder at a large, public university in the midwest. J Acad Nutr Diet. 2021;121(6):1115–1124. doi: 10.1016/j.jand.2021.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Benítez A, et al. Analysis of the risk of suffering eating disorders in young student university of extremadura (Spain) Enfermería Global. 2018;54:124–133. [Google Scholar]
- 92.Bizri M, et al. Prevalence of eating disorders among medical students in a Lebanese medical school: a cross-sectional study. Neuropsychiatr Dis Treat. 2020;16:1879. doi: 10.2147/NDT.S266241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bo S, et al. University courses, eating problems and muscle dysmorphia: are there any associations? J Transl Med. 2014;12(1):1–8. doi: 10.1186/s12967-014-0221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bosi M, et al. Body image and eating behavior among medical students: eating disorders among medical students. Epidemiology (Sunnyvale) 2016;6(4):256. [Google Scholar]
- 95.Brumboiu MI, et al. Nutritional status and eating disorders among medical students from the Cluj-Napoca University centre. Clujul Medical. 2018;91(4):414. doi: 10.15386/cjmed-1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Carriedo AP, et al. When clean eating isn’t as faultless: the dangerous obsession with healthy eating and the relationship between Orthorexia nervosa and eating disorders in Mexican University students. J Eat Disord. 2020;8(1):1–12. doi: 10.1186/s40337-020-00331-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Castejón MÁ, Berengüí R. Personality differences and psychological variables related to the risk of eating disorders. Anales de Psicología. 2020;36(1):64. [Google Scholar]
- 98.Chammas R, et al. Eating disorders among university students in a Middle Eastern urban setting: who is at risk? Clin Nutr. 2017;36:S113–S114. doi: 10.1016/S0261-5614(17)30467-3. [DOI] [Google Scholar]
- 99.Chan YL, et al. Eating disorder among Malaysian University students and its associated factors. Asia Pacific J Public Health. 2020;32(6–7):334–339. doi: 10.1177/1010539520947879. [DOI] [PubMed] [Google Scholar]
- 100.Chaudhari B et al (2017) The relationship of eating disorders risk with body mass index, body image and self-esteem among medical students. Ann Med Health Sci Res 7(3):144–149
- 101.Christensen KA, et al. Food insecurity associated with elevated eating disorder symptoms, impairment, and eating disorder diagnoses in an American University student sample before and during the beginning of the COVID-19 pandemic. Int J Eating Disord. 2021;54(7):1213–1223. doi: 10.1002/eat.23517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Compte EJ, Sepulveda AR, Torrente F. A two-stage epidemiological study of eating disorders and muscle dysmorphia in male university students in Buenos Aires. Int J Eat Disord. 2015;48(8):1092–1101. doi: 10.1002/eat.22448. [DOI] [PubMed] [Google Scholar]
- 103.Damiri B, et al. Eating disorders and the use of cognitive enhancers and psychostimulants among university students: a cross-sectional study. Neuropsychiatr Dis Treat. 2021;17:1633. doi: 10.2147/NDT.S308598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Din ZU, et al. Tendency towards eating disorders and associated sex-specific risk factors among university students. Arch Neuropsychiatry. 2019;56(4):258. doi: 10.29399/npa.23609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ebrahim M, et al. Disordered eating attitudes correlate with body dissatisfaction among Kuwaiti male college students. J Eat Disord. 2019;7(1):1–13. doi: 10.1186/s40337-019-0265-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Erol Ö, Özer A. Determination of orthorexia nervosa symptoms and eating attitudes in medicine students. Eur J Public Health. 2019;29(Suppl 4):280. [Google Scholar]
- 107.Falvey SE, et al. Diagnosis of eating disorders among college students: a comparison of military and civilian students. Mil Med. 2021;186:975–983. doi: 10.1093/milmed/usab084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Fatima W, Fatima R, Anwar NS. Prevalence of eating disorders among female college students of Northern Broader University, Arar, Kingdom of Saudi Arabia. Int J Child Health Nutr. 2018;7(3):115–121. doi: 10.6000/1929-4247.2018.07.03.4. [DOI] [Google Scholar]
- 109.Gramaglia C, et al. Orthorexia nervosa, eating patterns and personality traits: a cross-cultural comparison of Italian, Polish and Spanish university students. BMC Psychiatry. 2019;19(1):1–11. doi: 10.1186/s12888-019-2208-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Greenleaf C, et al. Female collegiate athletes: prevalence of eating disorders and disordered eating behaviors. J Am Coll Health. 2009;57(5):489–496. doi: 10.3200/JACH.57.5.489-496. [DOI] [PubMed] [Google Scholar]
- 111.Havemann L, et al. Disordered eating and menstrual patterns in female university netball players. South African J Sports Med. 2011;23(3):68–72. doi: 10.17159/2078-516X/2011/v23i3a328. [DOI] [Google Scholar]
- 112.Herzog DB, et al. Eating disorders and social maladjustment in female medical students. J Nervous Mental Dis. 1985;173(12):734–737. doi: 10.1097/00005053-198512000-00004. [DOI] [PubMed] [Google Scholar]
- 113.Iyer S, Shriraam V. Prevalence of eating disorders and its associated risk factors in students of a Medical College Hospital in South India. Cureus. 2021;13(1):e12926. doi: 10.7759/cureus.12926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jamali YA, et al. Prevalence of eating disorders among students of Quest University, Nawabshah, Pakistan. Merit Res J Med Med Sci. 2020;8(4):81–84. [Google Scholar]
- 115.Jennings PS, et al. Acculturation and eating disorders in Asian and Caucasian Australian university students. Eat Behav. 2006;7(3):214–219. doi: 10.1016/j.eatbeh.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 116.Joja O, von Wietersheim J. A cross-cultural comparison between EDI results of Romanian and German students. Procedia Soc Behav Sci. 2012;33:1037–1041. doi: 10.1016/j.sbspro.2012.01.280. [DOI] [Google Scholar]
- 117.Kiss-Tóth E, et al. Eating disorder in university students: an international multi-institutional study. Eur J Public Health. 2018 doi: 10.1093/eurpub/cky214.010. [DOI] [Google Scholar]
- 118.Ko N, et al. Disordered eating behaviors in university students in Hanoi, Vietnam. J Eat Disord. 2015;3(1):1–7. doi: 10.1186/s40337-015-0054-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Koushiou M, Nikolaou P, Karekla M. Prevalence and correlates of eating disorders in greek-cypriot adolescents and young adults. Eur J Counsel Psychol. 2020;8(1):3–18. doi: 10.5964/ejcop.v8i1.170. [DOI] [Google Scholar]
- 120.Kutlu R, Civi S. Evaluation of eating habits, body perception and depression status of university students. Gülhane Tip Dergisi. 2013;55(3):196. [Google Scholar]
- 121.Ladner J, et al. Eating disorders among university students: a public health challenge. An European study. Eur J Public Health. 2019 doi: 10.1093/eurpub/ckz186.486. [DOI] [Google Scholar]
- 122.Le Grange D, Telch CF, Tibbs J. Eating attitudes and behaviors in 1,435 South African Caucasian and non-Caucasian college students. Am J Psychiatry. 1998;155(2):250–254. doi: 10.1176/ajp.155.2.250. [DOI] [PubMed] [Google Scholar]
- 123.Lee SJ, Cloninger CR, Chae H. Cloninger's temperament and character traits in medical students of Korea with problem eating behaviors. Compr Psychiatry. 2015;59:98–106. doi: 10.1016/j.comppsych.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 124.Liao Y, et al. Changes in eating attitudes, eating disorders and body weight in Chinese medical university students. Int J Soc Psychiatry. 2013;59(6):578–585. doi: 10.1177/0020764012445862. [DOI] [PubMed] [Google Scholar]
- 125.Mancilla-Diaz JM, et al. A two-stage epidemiologic study on prevalence of eating disorders in female university students in Mexico. Eur Eating Disord Rev. 2007;15(6):463–470. doi: 10.1002/erv.796. [DOI] [PubMed] [Google Scholar]
- 126.Marciano D, McSherry J, Kraus A. Abnormal eating attitudes: prevalance at a Canadian University. Can Fam Physician. 1988;34:75. [PMC free article] [PubMed] [Google Scholar]
- 127.Mazzaia MC, Santos RMC. Risk factors for eating disorders among undergraduate nursing students. Acta Paulista de Enfermagem. 2018;31:456–462. doi: 10.1590/1982-0194201800065. [DOI] [Google Scholar]
- 128.Momeni M, Ghorbani A, Arjeini Z. Disordered eating attitudes among Iranian university students of medical sciences: the role of body image perception. Nutr Health. 2020;26(2):127–133. doi: 10.1177/0260106020912657. [DOI] [PubMed] [Google Scholar]
- 129.Ngan SW, et al. The relationship between eating disorders and stress among medical undergraduate: a cross-sectional study. Open J Epidemiol. 2017;7(02):85. doi: 10.4236/ojepi.2017.72008. [DOI] [Google Scholar]
- 130.Nichols S, et al. Body image perception and the risk of unhealthy behaviours among university students. West Indian Med J. 2009;58(5):465–471. [PubMed] [Google Scholar]
- 131.Padmanabhan V, Rahman MM, Fatima S. Prevalence of eating disorders in dental students of a Young University in UAE. Int J Sci Res. 2018;7(4):432–434. [Google Scholar]
- 132.Parra-Fernández ML, et al. Adaptation and validation of the Spanish version of the DOS questionnaire for the detection of orthorexic nervosa behavior. PLoS ONE. 2019;14(5):e0216583. doi: 10.1371/journal.pone.0216583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Parreño-Madrigal IM, et al. Prevalence of risk of eating disorders and its association with obesity and fitness. Int J Sports Med. 2020;41(10):669–676. doi: 10.1055/a-1152-5064. [DOI] [PubMed] [Google Scholar]
- 134.Pereira LdNG, et al. Eating disorders among health science students at a university in southern Brazil. Revista de Psiquiatria do Rio Grande do Sul. 2011;33:14–19. doi: 10.1590/S0101-81082011005000002. [DOI] [Google Scholar]
- 135.Pitanupong J, Jatchavala C. Atypical eating attitudes and behaviors in Thai medical students. Siriraj Med J. 2017;69(1):5–10. [Google Scholar]
- 136.Plichta M, Jezewska-Zychowicz M. Eating behaviors, attitudes toward health and eating, and symptoms of orthorexia nervosa among students. Appetite. 2019;137:114–123. doi: 10.1016/j.appet.2019.02.022. [DOI] [PubMed] [Google Scholar]
- 137.Polanco PP, Zetina LMM. Study of the risk of having eating disorder habits in undergraduate and graduate students in Mexican institutions. ESPACIO I+ D, INNOVACIÓN MÁS DESARROLLO: p 54
- 138.Radwan H, et al. Eating disorders and body image concerns as influenced by family and media among university students in Sharjah, UAE. Asia Pac J Clin Nutr. 2018;27(3):695–700. doi: 10.6133/apjcn.062017.10. [DOI] [PubMed] [Google Scholar]
- 139.Ramaiah RR. (2015) Eating disorders among medical students of a rural teaching hospital: a cross-sectional study. Int J Community Med Public Health. 2015;2(1):25–28. doi: 10.5455/2394-6040.ijcmph20150206. [DOI] [Google Scholar]
- 140.Rasman NSB, et al. Prevalence of eating disorders among medical students in Ipoh. Malaysia: Perak; 2018. [Google Scholar]
- 141.Rathner G, Rumpold G. Convergent validity of the eating disorder inventory and the anorexia nervosa inventory for self-rating in an Austrian nonclinical population. Int J Eat Disord. 1994;16(4):381–393. doi: 10.1002/1098-108X(199412)16:4<381::AID-EAT2260160407>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 142.Reyes-Rodríguez ML, et al. A description of disordered eating behaviors in Latino males. J Am Coll Health. 2011;59(4):266–272. doi: 10.1080/07448481.2010.502205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Roshandel A, Safavi M, Ghasemi I. Prevalence of eating disorders among female students of university (Tehran-Iran) Life Sci J. 2012;9(4):2822–2828. [Google Scholar]
- 144.Rostad IS, Tyssen R, Løvseth LT. Symptoms of disturbed eating behavior risk: Gender and study factors in a cross-sectional study of two Norwegian medical schools. Eating Behav. 2021;43:101565. doi: 10.1016/j.eatbeh.2021.101565. [DOI] [PubMed] [Google Scholar]
- 145.Safer M, et al. Eating disorders: prevalence and associated factors among health occupation students in Monastir University (Tunisia) Tunis Med. 2020;98(12):895–912. [PubMed] [Google Scholar]
- 146.Saleh RN, et al. Disordered eating attitudes in female students of An-Najah National University: a cross-sectional study. J Eat Disord. 2018;6(1):1–6. doi: 10.1186/s40337-018-0204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Sepulveda A, et al. Prevention program for disturbed eating and body dissatisfaction in a Spanish university population: a pilot study. Body Image. 2007;4(3):317–328. doi: 10.1016/j.bodyim.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 148.Sharifian MJ, et al. Association between dental fear and eating disorders and Body Mass Index among Finnish university students: a national survey. BMC Oral Health. 2021;21(1):1–9. doi: 10.1186/s12903-021-01449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Sharma M, et al. Body image perception, eating attitude and influence of media among undergraduate students of medical college in Delhi: a cross sectional study. Int J Res Med Sci. 2019;7(12):4627. doi: 10.18203/2320-6012.ijrms20195529. [DOI] [Google Scholar]
- 150.Shashank K, Gowda P, Chethan T. A cross-sectional study to asses the eating disorder among female medical students in a rural medical college of Karnataka State. Natl J Community Med. 2016;7:524–527. [Google Scholar]
- 151.Spillebout A, et al. Mental health among university students with eating disorders and irritable bowel syndrome in France. Rev Epidemiol Sante Publique. 2019;67(5):295–301. doi: 10.1016/j.respe.2019.04.056. [DOI] [PubMed] [Google Scholar]
- 152.Taha AAAE-A, Abu-Zaid HA, Desouky DE-S. Eating disorders among female students of Taif University, Saudi Arabia. Arch Iranian Med. 2018;21(3):111–117. [PubMed] [Google Scholar]
- 153.Tavolacci MP, et al. Eating disorders and associated health risks among university students. J Nutr Educ Behav. 2015;47(5):412–420. doi: 10.1016/j.jneb.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 154.Tavolacci M, et al. Changes and specificities in health behaviors among healthcare students over an 8-year period. PLoS ONE. 2018;13(3):e0194188. doi: 10.1371/journal.pone.0194188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Tavolacci M-P, Déchelotte P, Ladner J. Eating disorders among college students in France: characteristics, help-and care-seeking. Int J Environ Res Public Health. 2020;17(16):5914. doi: 10.3390/ijerph17165914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Thangaraju SI, et al. A cross-sectional study on prevalence of eating disorder and body image disturbance among female undergraduate medical students. J Ment Health Hum Behav. 2020;25(1):53. doi: 10.4103/jmhhb.jmhhb_13_20. [DOI] [Google Scholar]
- 157.Túry F, et al. Eating disorder characteristics among Hungarian medical students: Changes between 1989 and 2011. J Behav Addict. 2021;9(4):1079–1087. doi: 10.1556/2006.2020.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Uriegas NA, et al. Examination of eating disorder risk among university marching band artists. J Eat Disord. 2021;9(1):1–10. doi: 10.1186/s40337-021-00388-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Uzun Ö, et al. Screening disordered eating attitudes and eating disorders in a sample of Turkish female college students. Compr Psychiatry. 2006;47(2):123–126. doi: 10.1016/j.comppsych.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 160.Weigel A, et al. Eating pathology in medical students in Eastern Germany: comparison with general population and a sample at the time of the German reunification. Eat Weight Disord. 2016;21(3):445–451. doi: 10.1007/s40519-015-0237-5. [DOI] [PubMed] [Google Scholar]
- 161.Yoneda R, et al. Reliability and validity of the Japanese translation of the Eating Disorders Quality of Life (ED-QOL) scale for Japanese healthy female university undergraduate students and patients with eating disorders. BioPsychoSocial Med. 2020;14(1):1–7. doi: 10.1186/s13030-020-00189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Yu J, et al. Prevalence of disordered eating attitudes among university students in Wuhu, China. Nutr Hosp. 2015;32(4):1752–1757. doi: 10.3305/nh.2015.32.4.9187. [DOI] [PubMed] [Google Scholar]
- 163.Zhou Y, Pennesi JL, Wade TD. Online imagery rescripting among young women at risk of developing an eating disorder: a randomized controlled trial. Int J Eat Disord. 2020;53(12):1906–1917. doi: 10.1002/eat.23370. [DOI] [PubMed] [Google Scholar]
- 164.Wu XY, et al. The association between disordered eating and health-related quality of life among children and adolescents: a systematic review of population-based studies. PLoS ONE. 2019;14(10):e0222777. doi: 10.1371/journal.pone.0222777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Treasure J, Russell G. The case for early intervention in anorexia nervosa: theoretical exploration of maintaining factors. Br J Psychiatry. 2011;199(1):5–7. doi: 10.1192/bjp.bp.110.087585. [DOI] [PubMed] [Google Scholar]
- 166.Romano KA, et al. Changes in the prevalence and sociodemographic correlates of eating disorder symptoms from 2013 to 2020 among a large national sample of U.S. young adults: a repeated cross-sectional study. Int J Eat Disord. 2022;55(6):776–789. doi: 10.1002/eat.23709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Devoe J, D., , et al. The impact of the COVID-19 pandemic on eating disorders: a systematic review. Int J Eating Disord. 2022 doi: 10.1002/eat.23704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Schneider J, et al. A mixed-studies systematic review of the experiences of body image, disordered eating, and eating disorders during the COVID-19 pandemic. Int J Eat Disord. 2022 doi: 10.1002/eat.23706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Nagata JM, et al. Eating disorders in boys and men. Springer; 2021. [Google Scholar]
- 170.Murnen SK, Smolak L (2015) Gender and eating disorders. In: The Wiley handbook of eating disorders, Wiley, Uk, pp 352–366. 10.1002/9781118574089.ch27
- 171.Eaton DK, et al. Youth risk behavior surveillance—United States, 2011. Morb Mortal Wkly Rep Recomm Rep. 2012;61(4):1–162. [PubMed] [Google Scholar]
- 172.Neumark-Sztainer D, et al. Weight-related concerns and behaviors among overweight and nonoverweight adolescents: implications for preventing weight-related disorders. Arch Pediatr Adolesc Med. 2002;156(2):171–178. doi: 10.1001/archpedi.156.2.171. [DOI] [PubMed] [Google Scholar]
- 173.Neumark-Sztainer DR, et al. Shared risk and protective factors for overweight and disordered eating in adolescents. Am J Preventive Med. 2007;33(5):359–369. doi: 10.1016/j.amepre.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 174.Yoon C, et al. Disordered eating behaviors and 15-year trajectories in body mass index: findings from project eating and activity in teens and young adults (EAT) J Adolesc Health. 2020;66(2):181–188. doi: 10.1016/j.jadohealth.2019.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Yao L, Niu G, Sun X. Body image comparisons on social networking sites and chinese female college students’ restrained eating: the roles of body shame, body appreciation, and body mass index. Sex Roles. 2021;84:465–476. doi: 10.1007/s11199-020-01179-1. [DOI] [Google Scholar]
- 176.Zhang J, et al. The relationship between SNS usage and disordered eating behaviors: a meta-analysis. Front Psychol. 2021;12:641919. doi: 10.3389/fpsyg.2021.641919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Rohde P, et al. Age effects in eating disorder baseline risk factors and prevention intervention effects. Int J Eat Disord. 2017;50(11):1273–1280. doi: 10.1002/eat.22775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Hadjigeorgiou C, et al. Disordered eating in three different age groups in Cyprus: a comparative cross-sectional study. Public Health. 2018;162:104–110. doi: 10.1016/j.puhe.2018.05.024. [DOI] [PubMed] [Google Scholar]
- 179.Hong S-C, et al. Prevalence of distorted body image in young Koreans and its association with age, sex, body weight status, and disordered eating behaviors. Neuropsychiatr Dis Treat. 2015;11:1043. doi: 10.2147/NDT.S82504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Garfinkel PE, Newman A. The eating attitudes test: twenty-five years later. Eat Weight Disord. 2001;6(1):1–24. doi: 10.1007/BF03339747. [DOI] [PubMed] [Google Scholar]
- 181.Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ. 1999;319(7223):1467–1468. doi: 10.1136/bmj.319.7223.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Vetrone G, et al. Screening for eating disorders: false negatives and eating disorders not otherwise specified. Eur J Psychiatry. 2006;20(1):13–20. doi: 10.4321/S0213-61632006000100002. [DOI] [Google Scholar]
- 183.Becker CB, Stice E. From efficacy to effectiveness to broad implementation: Evolution of the Body Project. J Consult Clin Psychol. 2017;85(8):767–782. doi: 10.1037/ccp0000204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Fichter MM, et al. Anorexia nervosa in Greek and Turkish adolescents. Eur Arch Psychiatry Neurol Sci. 1988;237(4):200–208. doi: 10.1007/BF00449908. [DOI] [PubMed] [Google Scholar]
- 185.Giuffrida JM. Improved Screening for Binge Eating Disorder in Primary Care. The University of North Carolina at Charlotte; 2020. [Google Scholar]
- 186.Herman BK, et al. Development of the 7-Item Binge-Eating Disorder Screener (BEDS-7) Prim Care Companion CNS Disord. 2016 doi: 10.4088/PCC.15m01896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Van Strien T, et al. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord. 1986;5(2):295–315. doi: 10.1002/1098-108X(198602)5:2<295::AID-EAT2260050209>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 188.Mond JM, et al. Eating Disorder Examination Questionnaire (EDE-Q): norms for young adult women. Behav Res Ther. 2006;44(1):53–62. doi: 10.1016/j.brat.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 189.Mond JM, et al. Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Behav Res Ther. 2004;42(5):551–567. doi: 10.1016/S0005-7967(03)00161-X. [DOI] [PubMed] [Google Scholar]
- 190.Parra-Fernandez ML, et al. Adaptation and validation of the Spanish version of the ORTO-15 questionnaire for the diagnosis of orthorexia nervosa. PLoS ONE. 2018;13(1):e0190722. doi: 10.1371/journal.pone.0190722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Roncero M, Barrada JR, Perpiñá C. Measuring orthorexia nervosa: psychometric limitations of the ORTO-15. Span J Psychol. 2017;20:E41. doi: 10.1017/sjp.2017.36. [DOI] [PubMed] [Google Scholar]
- 192.Davison KK, Markey CN, Birch LL. A longitudinal examination of patterns in girls' weight concerns and body dissatisfaction from ages 5 to 9 years. Int J Eat Disord. 2003;33(3):320–332. doi: 10.1002/eat.10142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Silva WRD, et al. Body weight concerns: cross-national study and identification of factors related to eating disorders. PLoS ONE. 2017;12(7):e0180125. doi: 10.1371/journal.pone.0180125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Fichter MM, Keeser W. Das Anorexia-nervosa-Inventar zur Selbstbeurteilung (ANIS) Arch Psychiatr Nervenkr. 1980;228(1):67–89. doi: 10.1007/BF00365746. [DOI] [PubMed] [Google Scholar]
- 195.Garner DM, Garfinkel PE. The Eating Attitudes Test: an index of the symptoms of anorexia nervosa. Psychol Med. 1979;9(2):273–279. doi: 10.1017/S0033291700030762. [DOI] [PubMed] [Google Scholar]
- 196.Stice E, Telch CF, Rizvi SL. Development and validation of the Eating Disorder Diagnostic Scale: a brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychol Assess. 2000;12(2):123–131. doi: 10.1037/1040-3590.12.2.123. [DOI] [PubMed] [Google Scholar]
- 197.Fairburn CG, Beglin SJ (2008) Eating disorder examination questionnaire. Cognitive behavior therapy and eating disorders, pp 309–313
- 198.Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int J Eat Disord. 1983;2(2):15–34. doi: 10.1002/1098-108X(198321)2:2<15::AID-EAT2260020203>3.0.CO;2-6. [DOI] [Google Scholar]
- 199.Garner DM, et al. The eating attitudes test: psychometric features and clinical correlates. Psychol Med. 1982;12(4):871–878. doi: 10.1017/S0033291700049163. [DOI] [PubMed] [Google Scholar]
- 200.Rosenvinge JH, et al. A new instrument measuring disturbed eating patterns in community populations: development and initial validation of a five-item scale (EDS-5) Eur Eating Disord Rev. 2001;9(2):123–132. doi: 10.1002/erv.371. [DOI] [Google Scholar]
- 201.Donini LM, et al. Orthorexia nervosa: a preliminary study with a proposal for diagnosis and an attempt to measure the dimension of the phenomenon. Eat Weight Disord. 2004;9(2):151–157. doi: 10.1007/BF03325060. [DOI] [PubMed] [Google Scholar]
- 202.Mintz LB, et al. Questionnaire for eating disorder diagnoses: reliability and validity of operationalizing DSM—IV criteria into a self-report format. J Couns Psychol. 1997;44(1):63. doi: 10.1037/0022-0167.44.1.63. [DOI] [Google Scholar]
- 203.Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire. Western J Med. 2000;172(3):164. doi: 10.1136/ewjm.172.3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Killen JD, et al. Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: a three-year prospective analysis. Int J Eat Disord. 1994;16(3):227–238. doi: 10.1002/1098-108X(199411)16:3<227::AID-EAT2260160303>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]