Abstract
Symptoms of depression and anxiety usually co-occur and are inextricably linked to sleep disturbance. However, little is known about the symptom-to-symptom relationships among these three mental disorders. Hence, to improve our understanding of concurrent depression, anxiety, and sleep disturbance, we used the network analysis approach to construct an interplay relationship among the above three mental disorders and identify which specific symptoms bridge these aggregations. We collected data from a large sample (N = 6710, male = 3074, female = 3636; meanage = 19.28) at a university. We estimated the symptom network structure of depression, anxiety, and sleep disturbance as assessed by the Patient Health Questionnaire-9, Generalized Anxiety Disorder-7, and Youth Self-Rating Insomnia Scale during the COVID-19 lockdown. We further investigated four goals: first, identifying the individual core symptoms in the network by the index of “expected influence”; second, determining the bridge symptoms that play roles in linking different mental disorders by the index of bridge expected influence (1-step); third, examining the robustness of all results; and fourth, providing an overall structure that may or may not differ by sex. The network structure was stable, accurate, and predictable. Items referring to sleep dissatisfaction, poor sleep quality, and uncontrollable worry were potentially core symptoms in the interplay among depression, anxiety, and sleep disturbance. Sleep, guilt, restlessness, irritability, and feeling afraid can function as bridges among depression, anxiety, and sleep disturbance, which is clinically relevant and theoretically important. The results suggested that the network structures significantly differed between the female and male networks. Robustness tests also revealed that the results were reliable.
Keywords: Depression, Anxiety, Sleep disturbance, Network, Comorbidity
Introduction
Sleep or nocturnal rest is critical for growth and development in human beings (Nunn et al., 2016). Human health, well-being, and functioning are directly impacted by sleep deprivation that does not provide adequate rest (Itani et al., 2016; Tomaso et al., 2021). Lack of sleep, difficulty falling asleep, and/or remaining asleep are typical symptoms of sleep disturbances (American Psychiatry Association, 2013) and are highly associated with depression and anxiety disorders (Zhou et al., 2020). Significantly, the outbreak of COVID-19 has placed a considerable burden on the mental health of the entire population (Altena et al., 2020), and a systematic review revealed that the prevalence of sleep disturbance was 17.65–81% in the general population (Lin et al., 2021). For Chinese university students, the prevalence of poor sleep quality and sleep disturbances has been calculated as 30% (Li et al., 2020) and 25.7% (Li et al., 2018), respectively. Hence, given the essential nature of sleep and the potential terrible consequences caused by sleep disturbances, the mechanisms underlying the psychiatric disorders associated with sleep disturbances among college students should be explored.
As is well known, college students’ daily routine was converted by implementing containment measures during the COVID-19 pandemic period, including taking online courses instead of offline teaching, playing video games without hanging out, and suspending part-time jobs or taking internships online. The most straightforward and transparent consequence of the containment measure is a boosted trend of sleep disturbance among college students (Li et al., 2020), and female college students report more sleep problems (Wang et al., 2022). College students have to face the academic load and the challenges of career planning and interpersonal relations construction, which means taking on more adult-like responsibilities with a paucity of adulthood skills and cognitive maturity (Pedrelli et al., 2015). In addition, tremendous pressure and time-intensive tasks force college students to squelch their spare time and can be deleterious to college students’ sleep quality (Wang et al., 2022). In common sense, poor sleep quality simply represents day naps, tiredness, or fatigue. However, from the cognition perspective, poor sleep quality is positively associated with functional impairment (Graham & Kyle, 2017), subjective cognitive concerns (Joo et al., 2021), hyperactive/impulsive symptoms (Gregory et al., 2017), and more executive dysfunction (Gloger & Suhr, 2020). Moreover, from the perspective of emotion, sleep disturbance is highly relevant to anxiety and depression disorders (Zou et al., 2020). Worse, sleep disturbance increases the risk of self-injurious behavior (Liu et al., 2017). In summary, sleep is a vital psychophysiological process for physical and mental health, and sleep disturbance can bring serious consequences to individuals, especially college students, who should be given special attention.
A meta-analysis including 64 studies with 100,187 participants indicated that depression and anxiety symptoms among college students were 33.6% and 39%, respectively (Li et al., 2022). Moreover, a national cross-sectional survey in China revealed that the prevalence of depression and anxiety during the COVID-19 pandemic increased to 47.5% and 51.6%, respectively, among college students (Wu et al., 2020). Notably, depression and anxiety symptoms commonly co-occur in the same person rather than arising independently (Schlechter et al., 2021). That is, most people diagnosed with a depressive disorder are simultaneously diagnosed with an anxiety-related disorder, which was called “comorbidity” in clinical studies (Meehl, 2001). Individuals who reported both depressive and anxiety disorders showed cognitive decline, more sleep difficulties (Deng et al., 2021), and a higher rate of heart disease (Deschenes et al., 2020), which greatly impacts life quality (Samaranayake et al., 2014). It must be mentioned that the comorbidity of anxiety and depression was as high as 24.5% among college students during the COVID-19 pandemic (Wu et al., 2020), which has to be taken seriously.
The research on the comorbidity of anxiety and depression is opulent in revealing risk factors, symptoms, and effects (Kessler et al., 2015). However, the essential role of sleep disturbance is easily ignored. Sleep disturbance is considered a consequence of mental health problems, and individuals suffering from depression and anxiety usually experience sleep problems, including initial sleep or getting up earlier (American Psychiatry Association, 2013). In contrast, sleep can also contribute to the formation of mental disorders, in that poorer sleep quality is a significant factor in the onset of depression/anxiety symptoms (Adams & Kisler, 2013). However, there is little conclusive evidence about how sleep disturbance, depression, and anxiety are linked together, even though a body of studies has focused on factors that influence anxiety, depression, and sleep problems (Javakhishvili & Widom, 2022; Park et al., 2019; Peretti-Watel et al., 2020). The meta-analytic review of randomized controlled trials confirmed a bidirectional relationship between sleep and psychiatric disorders (i.e., anxiety and depression disorders) (Scott et al., 2017). Nonetheless, few studies have focused on the interrelationships among anxiety, depression, and sleep disturbance.
Recently, researchers proposed a new perspective, the symptom network approach of psychopathology (Borsboom & Cramer, 2013), to better understand the concurrence of depression, anxiety, and sleep disturbance. According to network analysis (Borsboom, 2017), symptoms do not arise from potential causes but rather reinforce (or inhibit) each other, eventually leading to the establishment of whole mental disorders and influencing daily function (van den Bergh et al., 2021). Previous theoretical studies have shown that identifying bridge symptoms in psychopathology networks can reveal fecund information because it promotes clarifying symptoms that put patients at higher risk of comorbidity (Borsboom & Cramer, 2013). For instance, Wang et al. (2021) applied the symptom network approach and revealed that the most central symptoms were panic (i.e., anxiety) and wakefulness (i.e., sleep) in anxiety, depression disorders, and sleep disturbance, and that those symptoms had the greatest potential to affect an individual’s mental state among HIV patients in China. In comparison, no study has explored the interrelationships among anxiety, depression, and sleep disturbance among college students who have experienced lockdown during the current COVID-19 pandemic from the perspective of a symptom network.
In summary, even under nonpandemic circumstances, college students can experience considerable sleep disturbance, anxiety, and depressive symptoms (Beiter et al., 2014; Li et al., 2018). Moreover, the situation only has worsened during the COVID-19 pandemic. Although several studies have reported increased sleep disturbance, anxiety, and depression disorders during the COVID-19 pandemic (Li et al., 2020; Wu et al., 2020), studies on the mechanisms underlying the anxiety and depression disorders associated with sleep disturbance are limited. Therefore, the primary goal of this study was to explore the core and bridge symptoms in the network structure of anxiety, depression, and sleep disturbance among Chinese college students under the lockdown of the pandemic. To do so, we applied a symptom network approach, including the four main statistical steps. First, the extended Bayesian information criterion (EBIC) (Chen & Chen, 2008) and graphical least absolute shrinkage and selection operator (LASSO) network models were used (Epskamp et al., 2018) to establish the depression–anxiety–sleep symptom network structure and seek the strongest edges (i.e., partial correlations). Then, the expected influence index was calculated to identify the most central nodes (i.e., core symptoms). Third, the bridge function was used to seek the potential target symptoms for intervention. Finally, to ensure that the obtained results are reliable and trustworthy, we ran centrality stability, edge accuracy and bootstrapped difference tests for centrality and edges. Given the sex difference between males and females in anxiety and depression disorders and sleep disturbance (Li et al., 2022; Wu et al., 2020), another goal of the present study was to identify sex differences in the depression–anxiety–sleep symptom network structure.
Methods
Participants
This current large-scale (N = 6710, male = 3074, female = 3636; meanage = 19.28, SDage = 1.99) study adopted convenience sampling and was conducted at a university in *** from 27 September to 12 October 2021. All participants must have been students under lockdown at that university for at least one month to be eligible.
The questionnaires were posted on Wenjuanxing (https://www.wjx.cn/), an online platform. The participants provided their electronic informed consent prior to participation in this study. Given the sensitive nature of some questions, the mental health center where the middle author works provided timely online interventions for subjects who needed professional counseling services. The research was examined and approved by the ethics committee of *** University (Reference number: 202,112,220,084).
Measurements
Generalized anxiety disorder scale (GAD-7)
The GAD-7 is a brief measure of anxiety symptom severity with 7 items (Spitzer et al., 2006). The Chinese version of the GAD-7, which assesses the frequency of the seven anxiety symptoms over the previous two weeks on a scale from 0 (not at all) to 3 (nearly every day), proves to be valid and reliable (Gong et al., 2021). Higher scores indicate more severe anxiety symptoms. The GAD-7 has high internal consistency (α = 0.93) in the present study.
Patient health questionnaire (PHQ-9)
The PHQ-9 is a questionnaire-based depression scale used to assist primary care practitioners in diagnosing depression and monitoring treatment (Kroenke et al., 2001). Each item of the PHQ-9 scores from 0 (not at all) to 3 (nearly every day), with a summed score ranging from 0 to 27 for the nine items. Higher scores indicate more severe depressive symptoms. The Chinese version of the PHQ-9 has been well validated as an efficient tool for screening depression among the general Chinese population (Ye et al., 2020). The PHQ-9 has high internal consistency (α = 0.90) in the present study.
Youth SelfRating Insomnia Scale (YSIS-8)
The YSIS-8 is a self-report questionnaire consisting of 8 questions about insomnia symptoms, waking symptoms and daytime consequences within the past month (Buysse et al., 2006). Eight symptoms, including difficulty initiating sleep (DIS), difficulty maintaining sleep (DMS), early morning awakening (EMA), unrefreshing sleep, poor sleep quality, sleep insufficiency, sleep dissatisfaction, and interference of sleep difficulties with daytime functioning, were developed based on previous studies (American Psychiatry Association, 2013; Liu et al., 2019). Sleep quality ranges from 1 (very good) to 5 (very poor), and sleep satisfaction ranges from 1 (very satisfied) to 5 (very unsatisfactory). The remaining 6 items are rated on a 5-point scale from 1 = never, 2 = rarely (< 1 time/week), 3 = sometimes (1–2 times/week), 4 = often (3–5 times/week), to 5 = almost every day (6–7 times/week). Summing the scores on the 8 items yields a total YSIS-8 score ranging from 8 to 40. A higher total YSIS score indicates greater insomnia severity during the past month. The Chinese version of the YSIS-8 has been well validated as a simple and reliable scale for assessing adolescent insomnia severity (Liu et al., 2019). The YSIS-8 has high internal consistency (α = 0.92) in the present study.
Statistical analysis
Network estimation
The present study conducted all analyses using R (version 4.1.1) (R Core Team, 2021). Based on previous studies (Mullarkey et al., 2019), we used the function descrTable in R package compareGroups (Subirana et al., 2014) to examine item informativeness (i.e., standard deviation (SD) of the item) and the function goldbricker in the R package networktools (version 1.3.0) (Jones et al., 2021) to examine redundancy (i.e., < 25% of significantly different correlations).
Extended Bayesian information criterion (EBIC) (Chen & Chen, 2008) and graphical least absolute shrinkage and selection operator (LASSO) network models were used (Epskamp et al., 2018) to establish the depression–anxiety–sleep symptom network structure. The R package qgraph (version 1.6.9) (Epskamp et al., 2012) was used to estimate and visualize the network. The principle behind this is that partial correlation analyses after controlling all other variables were computed to build the association of each pairwise continuous variable (i.e., symptom) and form a network analysis (Opsahl et al., 2010). A node represents a variable or symptom in the network analysis, and each pairwise association between variables or symptoms was defined as an edge. Thicker edges indicate higher correlations. Blue and red edges reveal positive and negative correlations, respectively (Epskamp et al., 2018; Epskamp et al., 2012).
In the field of network analysis, three centrality indices, strength (i.e., the sum of the absolute edge weights connected to a specific node), closeness (i.e., the inverse of summing all the shortest path lengths from one node to all other nodes), and betweenness (i.e., the importance of a symptom as a “connecter” to other symptoms based on how frequently a node lies on all the shortest paths between other nodes), must be computed to explore the importance of individual symptoms within the network (Haslbeck & Waldorp, 2020). Previous research has shown that assessments of closeness and betweenness are unreliable in determining nodes’ importance (Bringmann et al., 2019; Epskamp et al., 2016). Moreover, traditional indices such as strength centrality may not accurately predict node influence on a network containing both positive and negative edges. Robinaugh et al. (2016) demonstrated that expected influence is a more appropriate index in such cases. Hence, expected influence was chosen as the metric in the current study.
Network stability and accuracy
We used the R package boonet (version 1.4.3) (Opsahl et al., 2010) to assess the robustness of the results and the network’s stability and accuracy. First, nonparametric bootstrapping was used to estimate the accuracy of the edge weights by computing confidence intervals (CIs). New datasets based on 95% CIs were created by randomly resampling observations in the data. Second, a case-dropping bootstrap procedure was performed to compute a correlation stability coefficient (CS-C) to assess network stability. CS-C values indicated the maximum proportion of samples that could be removed, while correlations between the original centrality indices (i.e., strength, closeness, betweenness) and centrality indices based on the case-subset network were maintained above 0.7 with a 95% probability. As recommended previously (Epskamp et al., 2018), a CS-C should not be lower than 0.25 and is preferably above 0.5. Finally, differences in network properties (i.e., edge weights, node strengths) were evaluated by bootstrapped difference tests (Epskamp et al., 2018).
In addition, predictability (i.e., R2), which reflects how well all its neighboring nodes predict a specific node, was estimated using the R package mgm (version 1.2–12) (van Borkulo et al., 2022). Furthermore, to explore bridge symptoms in the network that played essential roles in connecting two or more psychiatric disorders (Haslbeck & Waldorp, 2020), the bridge function in the R package networktools (version 1.4.0) was used (Chen & Chen, 2008; Jones et al., 2021). Bridge centrality indices assessed bridge symptoms, including bridge strength, bridge closeness, bridge betweenness, and bridge expected influence (1-step). Following a previous study (Robinaugh et al., 2016), bridge symptoms were selected using the index of bridge expected influence (1-step), including both positive and negative associations.
Comparisons based on sex
Following previous studies (Li et al., 2022; Wu et al., 2020), sex differences in network characteristics were assessed using the Network Comparison Test (NCT) in the R package NetworkComparisonTest (version 2.2.1) (van Borkulo et al., 2022). This test is employed on subsamples (female vs. male) with 1000 permutations to compare the global network strengths (absolute sum of all edge weights) and network structures (edge weight distributions) between the two networks. Furthermore, the strength of each edge connecting the two networks was determined using Holm–Bonferroni correlations for multiple comparisons.
Results
Descriptive statistics and items check
The means and standard deviations of the PHQ-9, GAD-7, and YSIS-8 items are reported in Table 1. Before performing network analysis, we checked for mean item level, item informativeness (i.e., item standard deviation), and item redundancy. All items were above the informativeness threshold (i.e., ± 2.5 SD below the mean level, PHQ-9: MSD = 0.59 ± 0.10; GAD-7: MSD = 0.54 ± 0.06; YSIS-8: MSD = 0.87 ± 0.10), and no item was considered statistically redundant (i.e., > 25%) by using the Fruchterman–Reingold algorithm. Hence, all items were included in the analysis.
Table 1.
Basic information of scales and descriptive item statistics
| Scale | Symptoms | Items | Mean (SD) | Predictability |
|---|---|---|---|---|
| PHQ-9 | Anhedonia | 1. Little interest or pleasure in doing things | 1.42 (0.67) | 59% |
| Sad mood | 2. Feeling down, depressed, or hopeless | 1.35 (0.60) | 63% | |
| Sleep | 3. Trouble falling or staying asleep, or sleeping too much | 1.32 (0.64) | 51% | |
| Energy | 4. Feeling tired or having little energy | 1.43 (0.66) | 60% | |
| Appetite | 5. Poor appetite or overeating | 1.34 (0.65) | 41% | |
| Guilt | 6. Feeling bad about yourself or that you are a failure or have let yourself or your family down | 1.28 (0.59) | 57% | |
| Concentration | 7. Trouble concentrating on things, such as reading the newspaper or watching television | 1.37 (0.68) | 47% | |
| Motor | 8. Moving or speaking so slowly that other people could have noticed? Or the opposite being so fidgety or restless that you have been moving around a lot more than usual | 1.18 (0.50) | 53% | |
| Suicide | 9. Thoughts that you would be better off dead, or of hurting yourself | 1.09 (0.36) | 43% | |
| GAD-7 | Nervousness | 1. Feeling nervous, anxious or on edge | 1.32 (0.59) | 70% |
| Uncontrollable worry | 2. Not being able to stop or control worrying | 1.26 (0.57) | 73% | |
| Excessive worry | 3. Worrying too much about different things | 1.33 (0.61) | 71% | |
| Trouble relaxing | 4. Trouble relaxing | 1.28 (0.57) | 69% | |
| Restlessness | 5. Being so restless that it is hard to sit still | 1.16 (0.45) | 62% | |
| Irritability | 6. Becoming easily annoyed or irritability | 1.26 (0.55) | 58% | |
| Feeling afraid | 7. Feeling afraid as if something awful might happen | 1.17 (0.46) | 69% | |
| YSIS-8 | PSQ | 1. Poor sleep quality | 1.67 (0.85) | 82% |
| SD | 2. Sleep dissatisfaction | 1.69 (0.87) | 83% | |
| DIS | 3. Difculty initiating sleep | 1.53 (0.84) | 62% | |
| DMS | 4. Difculty maintaining sleep | 1.36 (0.75) | 45% | |
| EMA | 5. Early morning awakening | 1.38 (0.77) | 47% | |
| SI | 6. Sleep insufficiency | 1.57 (0.94) | 60% | |
| US | 7. Unrefreshing sleep | 1.77 (1.07) | 61% | |
| DFI | 8. Daytime functioning impairment | 1.46 (0.83) | 61% |
SD, standard deviation; PHQ-9, the Patient Health Questionnaire-9; GAD-7, the Generalized Anxiety Disorder-7 questionnaire; YSIS-8, Youth SelfRating Insomnia Scale
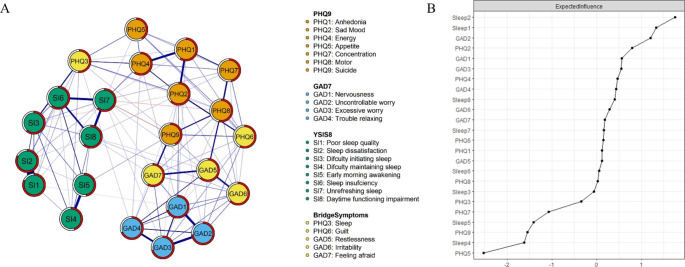
Network estimation structure and local network properties
The network estimated on the PHQ-9, GAD-7, and YSIS-8 is shown in Fig. 1(Part A) and Fig. S1. Several points are worth mentioning. First, through the weighted adjacency matrix (see Table S1), we found that poor sleep quality (#YSIS-1; i.e., quality of sleep during the past month) with sleep dissatisfaction (#YSIS-2; i.e., satisfaction with sleep during the past month) and DMS (#YSIS-4; i.e., waking up frequently during the night) with EMA (#YSIS-5; i.e., waking up earlier and cannot return to sleep) had the first and second strongest associations. Second, local property analysis showed that symptoms of sleep dissatisfaction (#YSIS-2; i.e., satisfaction with sleep during the past month) were the most central node, followed by poor sleep quality (#YSIS-1; i.e., quality of sleep during the past month) and uncontrollable worry (#GAD-2; i.e., unable to stop or control worry). The symptoms with the lowest centrality included appetite (#PHQ-5; i.e., poor appetite or overeating), DMS (#YSIS-4; i.e., waking up frequently during the night), suicide (#PHQ-9; i.e., thoughts about killing or hurting yourself), EMA (#YSIS-5; i.e., waking up earlier and cannot get back to sleep), and concentration (#PHQ-7; i.e., trouble concentrating).
Fig. 1.
A, The network structure of anxiety, depressive symptoms, and sleep disturbance among college students during the COVID-19 pandemic. B, Standardized centrality indices (i.e., ExpecteInfluence) of the network structure of anxiety, depressive symptoms, and sleep quality (Z scores)
Bridge symptoms of anxiety, depressive symptoms, and sleep disturbance
The bridge expected influence was estimated in Fig. 1 and S2. The strongest bridge symptoms (Z score above 1) were sleep (#PHQ-3; i.e., trouble falling or staying asleep or sleeping too much), feeling afraid (#GAD-7; i.e., feeling afraid as if something awful might happen), guilt (#PHQ-6; i.e., feeling bad about yourself or that you are a failure or have let yourself or your family down), restlessness (#GAD-5; i.e., being so restless that it is hard to sit still) and irritability (#GAD-6; i.e., becoming easily annoyed or irritable). The bridge expected influence of these items was significantly correlated with expected influence values (rs = 0.88, CI [0.74; 0.95]).
Network stability and accuracy
The predictability index indicated that the neighboring nodes could account for 60% of the variance in each node (MR2 = 0.60 ± 0.11), on average. SD (i.e., #YSIS-2, R2 = 0.83), PSQ (i.e., #YSIS-1, R2 = 0.82), uncontrollable worry (i.e., #GAD-2, R2 = 0.73), excessive worry (i.e., #GAD-3, R2 = 0.71), nervousness (i.e., #GAD-1, R2 = 0.70), trouble relaxing (i.e., #GAD-4, R2 = 0.70), feeling afraid (i.e., #GAD-7, R2 = 0.69), sad mood (i.e., #PHQ-2, R2 = 0.63), DIS (i.e., #YSIS-3, R2 = 0.62), restlessness (i.e., #GAD-5, R2 = 0.62), US (i.e., #YSIS-7, R2 = 0.61), DFI (i.e., #YSIS-8, R2 = 0.61), SI (i.e., #YSIS-6, R2 = 0.60) and energy (i.e., #PHQ-4, R2 = 0.60) had the highest predictability indices within the network (Table 1). Although, on average, half of each symptom’s variance could potentially be explained by the other nodes, this also implied that the remaining variance was not explained by only considering the interplay among symptoms.
The expected influence and predictability were unrelated to PHQ-9 item variability (PHQ-9: rs = 0.17, CI [− 0.56; 0.75] and rs = 0.32, CI [− 0.44; 0.81], respectively) and item mean (PHQ-9: rs = 0.30, CI [− 0.46; 0.80] and rs = 0.46, CI [− 0.29; 0.86], respectively). In contrast, predictability was positively related to GAD-7 item variability (GAD-7: rs = 0.86, CI [0.30; 0.96]) and item mean (GAD-7: rs = 0.82, CI [0.18; 0.97]); however, expected influence was unrelated to GAD-7 item variability (GAD-7: rs = 0.61, CI [− 0.26; 0.93]) and item mean (GAD-7: rs = 0.51, CI [− 0.40; 0.91]). Expected influence and predictability were positively related to sleep item mean (YSIS-8: rs = 0.77, CI [0.14; 0.96] and rs = 0.74, CI [0.08; 0.95], respectively). The expected influence and predictability were unrelated to the PHQ-9 and were unrelated to the sleep mean item (YSIS-8: rs = 0.41, CI [− 0.42; 0.86] and rs = 0.3, CI [− 0.51; 0.83], respectively).
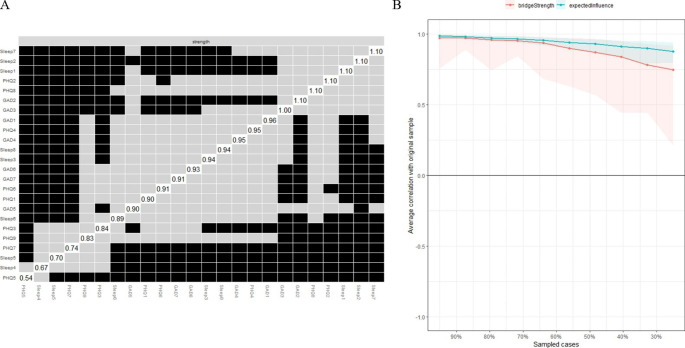
The edge weights in the current sample were consistent with the bootstrapped sample, especially the connections with larger weights, indicating that the current network structure was stable (Part A of Fig. 2). The bootstrapped difference tests revealed that a large proportion of the comparisons among edge weights were statistically significant (Supplementary Fig. S3, S4).
Fig. 2.
A, estimation of edge weight difference by bootstrapped difference test. Nonparametric bootstrapped difference test for strength. Grey boxes indicate no significant difference, whereas black boxes indicate a statistically significant difference (p < .050). Diagonal values represent the strength score of each node. B, the stability of the network structure by case dropping subset bootstrapping
Regarding network stability, the case-dropping bootstrap procedure showed that the expected influence (i.e., CS-C = 0.75) and bridge expected influence (1-step) (i.e., CS-C = 0.28) values remained stable after dropping different proportions of the sample (Part B of Fig. 2).
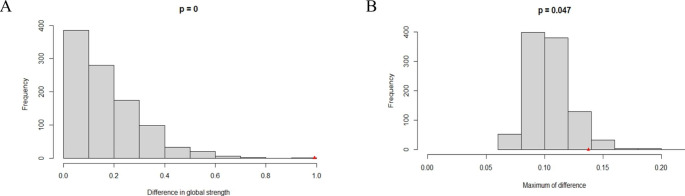
Sex differences
We tested whether global strength, structure and single edges differed by sex. Overall, the two networks appeared similar (Fig. S5). There were significant sex differences in network global strength (females: 11.22 vs. males: 12.21; S = 0.99, p = .000) and the network structure distribution of edge weights (M = 0.14, p = .047) (all p > .05 after Holm–Bonferroni correction, Fig. S6), as shown in Fig. 3. Specifically, examining each node and the expected influence index shows that men’s strength was stronger than women’s strength for #PHQ-7 and #YSIS-7 (p < .05).
Fig. 3.
A, the maximum difference in edge strength. B, the difference in global strength (right panel)
Finally, we tested whether males and females reported different symptom mean levels statistically. There were 20 of 24 symptoms with statistically significant (all adjusted p values ≤ 0.045) differences (Table S2). However, the magnitude of the differences was negligible to small (Cohen’s d ≤ 0.5). Hence, the level differences of symptoms in females and males should be interpreted with caution.
Discussion
Using network analysis, the present study examined the relationships among sleep disturbance, depression, and anxiety among a large sample of college students during the COVID-19 pandemic. All results showed stability and accuracy, suggesting strong correlations between the internal symptoms of these three mental disorders.
From the node centrality, sleep dissatisfaction (#YSIS-2; i.e., satisfaction with sleep during the past month), poor sleep quality (#YSIS-1; i.e., quality of sleep during the past month), and uncontrollable worry (#GAD-2; i.e., unable to stop or control worry) were the highest strength values (Z score above 1), indicating those in the depression, anxiety, and sleep disturbance network structure, which should be noted. Sleep dissatisfaction refers to both the quality and quantity of sleep that cannot meet one person’s demands, such as adequate and regular sleep duration, a healthy sleep pattern, and high-quality sleep (Varghese et al., 2020). For college students, depression, anxiety, substance abuse, day naps, and rest time are prefiguring sleep dissatisfaction (Wilsmore et al., 2013). During the pandemic quarantine period, college students’ daily lives were replaced with taking online teaching and staying at home. Moreover, without hierarchical supervision from teachers or schools, students can easily become addicted to video games or mobile devices, and without peers’ companionship, college students may rely on substances to evade negative affection (Cuong et al., 2021). Therefore, superficially, the pandemic changed students’ daily lives. Nevertheless, college students’ regular sleep rhythm was devastated by the unrestrictive usage of video games, mobile devices, and substances. To combat sleep dissatisfaction, regular physical activity might improve sleep quality (Baron et al., 2022).
In addition to sleep dissatisfaction, poor sleep quality is another conspicuous factor besetting college students. In its literal meaning, poor sleep quality denotes that one person evaluates his or her sleep quality as poor or bad in the last month, which is positively associated with a higher prevalence of mental disorders and a longer duration of insomnia symptoms (Ohayon et al., 1997). Our view maintains that college students’ daily routine changes disturb their regular sleep patterns, which cannot be recovered or appeased by long sleep or day naps. Currently, the mainstream treatment to improve sleep quality is via mindfulness to release psychological stress (Lau et al., 2018).
In addition to sleep problems, the other factor, uncontrollable worry, is deleterious to college students’ mental health. Uncontrollable worry is being unable to restrain or control worry cognitively (Hallion & Ruscio, 2013), which is also defined as pathological worry (Gorday et al., 2018). Our result is consistent with one previous study showing that alienation from peers is one etiology of uncontrollable worry (Curzik & Salkicevic, 2016). For college students, staying away from peers means alienation from emotional divulgence. Moreover, more fierce competition for jobs or further education and uncertainties followed by pandemics can drag college students into deep emotional turmoil. Unfortunately, college students are tyros in the confrontation of traumatic events, although, without peer companions, a warm and solid filial relationship may mollify worry.
Furthermore, the perspective of bridge expected influence (1-step) measures the symptoms that play a crucial role in coalescing depression, anxiety, and sleep disturbance. Sleep (#PHQ-3; i.e., trouble falling or staying asleep or sleeping too much) and feeling afraid (#GAD-7; i.e., feeling afraid as if something awful might happen) should be mentioned and discussed. The physical reaction to depression is mainly shown as difficulties initiating sleep, maintaining sleep, and fatigue. In a cognitive–emotion–behavior circulation (Weiner, 1980), we conjecture that sleep in the body directly reflects an irregular lifestyle and great pressure. When college students notice physical maladaptation without experience, college students may digress to either retain the same pattern or painstakingly revert to the original track. However, failures in lifestyle change may induce negative affection containing remorse, depression, surliness, or anger (Sarris et al., 2014). Additionally, cognitive bias may elicit college students to have a depressive status in which college students hold the belief that efforts to change are always in vain (Pang & Wu, 2021).
Referring to learned helplessness (Abramson et al. 1989), a person who endures unescapable negative events extensively will give up exerting efforts on the situation. College students are in a key developmental period to start a career, pursue further education, or cultivate a long-term intimate relationship. Nevertheless, in the pandemic, a profound adverse event, the main developmental task must be paused, and with chronic resurgence, containment measures become a quotidian. Ambitious college students are naturally fearful about future awful events that divest auspiciousness and omens. Furthermore, in terms of cognition–emotion–behavior circulation (Weiner, 1980), accumulated fearfulness manifests in sleep disturbance, depression, and anxiety.
After delineating the importance of symptoms, strong associations between two specific nodes should be mentioned, as strong associations indicate that alleviating either symptom in the association means that two symptoms are improved accordingly, which can shed light on practice. From our findings, poor sleep quality (#YSIS-1; i.e., quality of sleep during the past month) with sleep dissatisfaction (#YSIS-2; i.e., satisfaction with sleep during the past month) and DMS (#YSIS-4; i.e., waking up frequently during the night) with EMA (#YSIS-5; i.e., waking up earlier and cannot get back to sleep) are the two strongest associations, implying that sleep problems should be main targets in treatments to release college students’ mental distress. College students must sleep well to deal with daily routine work. In a cognition–emotion–behavior circulation (Weiner, 1980), college students have poor sleep quality behaviorally, including being unable to maintain sleep, sleep deeply or initiate sleep, which may hold antagonist affection toward sleep. Dissatisfaction with sleep, including distress, sadness, and hatred toward sleep, can decay sleep quality (Duran & Erkin, 2021). Hard-to-maintain sleep makes college students mentally excited after extended periods of mobile usage, playing video games, or watching television programs. Thus, excited college students cannot maintain deep sleep naturally, and it is difficult to get up earlier to resume activities (Mei et al., 2022).
Limitations
Based on a large sample plan, this study investigated the network characteristics of mental health symptoms of college students under close management during COVID-19. However, there are still several research limitations that need to be addressed. First, similar to most studies (Van den Bergh et al., 2021; Wang, 2022), this study was cross-sectional, which does not best explain longitudinal causality. Second, the study was conducted at a closed university, and thus, the results may not be generalizable to all groups in the new population.
Conclusions
In summary, network analysis provides new insights into the internal relationships among depression, anxiety, and sleep disturbance. The results highlight that specific symptoms can function as bridges among anxiety, depression, and sleep complaints, which helps to explain their comorbidity and reciprocal influences. In particular, sleep, guilt, restlessness, irritability, and feeling afraid play unique roles as bridge symptoms. Although the current network does not consider the directionality between symptoms, it still contributes to comprehending college students’ depression, anxiety, and sleep disturbance during the closed management of COVID-19. However, the network-comparison test results showed significant differences in global strength and edge weights between males and females in the network structure for depression, anxiety, and sleep disturbance. In future research, expanding the issue of directivity between symptoms is necessary. At the same time, it is also important to investigate the symptom network between closed management and after closed management and provide meaningful suggestions for clinical practices.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Code and Data Availability
Analytic code and data for this work are available upon request.
Declarations
Ethical approval
The research was examined and approved by the ethics committee of Beijing Normal University (Reference number: 202112220084).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Competing Interests
The authors have no conflicts of interest regarding this research study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yanqiang Tao, Email: psyxuele2020@163.com.
Wenxin Hou, Email: joychou1979@hotmail.com.
Haiqun Niu, Email: 17768102631@163.com.
Zijuan Ma, Email: mazijuan@m.scnu.edu.cn.
Shuang Zhang, Email: zhshuang525@163.com.
Liang Zhang, Email: zhangliangpsy@neau.edu.cn.
Xiangping Liu, Email: 89034@bnu.edu.cn.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12144-022-03443-x.
References
- Abramson, Metalsky GI, Alloy LB. Hopelessness Depression: A Theory-Based Subtype of Depression. Psychological Review. 1989;96(2):358–372. doi: 10.1037/0033-295X.96.2.358. [DOI] [Google Scholar]
- Adams SK, Kisler TS. Sleep Quality as a Mediator Between Technology-Related Sleep Quality, Depression, and Anxiety. Cyberpsychology Behavior and Social Networking. 2013;16(1):25–30. doi: 10.1089/cyber.2012.0157. [DOI] [PubMed] [Google Scholar]
- Altena, Baglioni, C., Espie, C. A., Ellis, J., Gavriloff, D., Holzinger, B., Schlarb, A., Frase, L., Jernelöv, S., & Riemann, D. (2020). Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT‐I Academy. Journal of Sleep Research, 29(4), e13052–n/a. 10.1111/jsr.13052 [DOI] [PubMed]
- American Psychiatry Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). American Psychiatric Publishing
- Baron P, Hermand E, Peze T, Kuehn C, Dieu O, Bourlois V, Porrovecchio A, Hurdiel R. No gender difference in association between sleep quality and physical activity level of French students. Sport Sciences for Health. 2022 doi: 10.1007/s11332-022-00920-5. [DOI] [Google Scholar]
- Beiter, Nash R, McCrady M, Rhoades D, Linscomb M, Clarahan M, Sammut S. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. Journal of Affective Disorders. 2014;173:90–96. doi: 10.1016/j.jad.2014.10.054. [DOI] [PubMed] [Google Scholar]
- Borsboom A network theory of mental disorders. World Psychiatry. 2017;16(1):5–13. doi: 10.1002/wps.20375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom, Cramer AO. Network Analysis: An Integrative Approach to the Structure of Psychopathology. Annual Review of Clinical Psychology. 2013;9(1):91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Bringmann L, Elmer T, Epskamp S, Krause R, Schoch D, Wichers M, Snippe E. What Do Centrality Measures Measure in Psychological Networks? Journal of Abnormal Psychology. 2019;128(8):892–903. doi: 10.1037/abn0000446. [DOI] [PubMed] [Google Scholar]
- Buysse, Ancoli-Lsrael, S., Lichstein, E. D. I. N. G. E. R. J. D., K. L., & Morin, C. M. (2006). Recommendations for a standard research assessment of insomnia. Sleep (,29 N.Y.), 29 vol., pp. 1155–1173). New York. 910.1093/sleep/29.9.1155 [DOI] [PubMed]
- Chen, Chen Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. 2008;95(3):759–771. doi: 10.1093/biomet/asn034. [DOI] [Google Scholar]
- Cuong, Assanangkornchai S, Wichaidit W, Hanh VTM, Hanh HTM. Associations between gaming disorder, parentchild relationship, parental supervision, and discipline styles: Findings from a school-based survey during the COVID-19 pandemic in Vietnam. Journal of Behavioral Addictions. 2021;10(3):722–730. doi: 10.1556/2006.2021.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curzik D, Salkicevic S. Perceived Parent and Peer Alienation and Its Relations to Anxiety Sensitivity, Pathological Worry, and Generalised Anxiety Disorder Symptoms. Australian Psychologist. 2016;51(3):223–230. doi: 10.1111/ap.12183. [DOI] [Google Scholar]
- Deng, Zhou F, Hou W, Silver Z, Wong CY, Chang O, Drakos A, Zuo QK, Huang E. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Research. 2021;301:113863–113863. doi: 10.1016/j.psychres.2021.113863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deschênes, Burns RJ, Schmitz N. Anxiety and Depression Symptom Comorbidity and the Risk of Heart Disease: A Prospective Community-Based Cohort Study. Psychosomatic Medicine. 2020;82(3):296–304. doi: 10.1097/PSY.0000000000000790. [DOI] [PubMed] [Google Scholar]
- Duran, Erkin Ö. Psychologic distress and sleep quality among adults in Turkey during the COVID-19 pandemic. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2021;107:110254–110254. doi: 10.1016/j.pnpbp.2021.110254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp, Borsboom D, Fried E. Estimating Psychological Networks and their Accuracy: A tutorial paper. Behavior Research Methods. 2018;50(1):195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: Network Visualizations of Relationships in Psychometric Data. Journal of Statistical Software. 2012;48(4):1–18. doi: 10.18637/jss.v048.i04. [DOI] [Google Scholar]
- Epskamp S, Rhemtulla M, Borsboom D. Generalized Network Psychometrics: Combining Network and Latent Variable Models. Psychometrika. 2016;82:904–927. doi: 10.1007/s11336-017-9557-x. [DOI] [PubMed] [Google Scholar]
- Gloger EM, Suhr JA. Correlates of Poor Sleep and Subsequent Risk of Misdiagnosis in College studentsPresenting with Cognitive Complaints. Archives Of Clinical Neuropsychology : The Official Journal Of The National Academy Of Neuropsychologists. 2020;35(6):692–670. doi: 10.1093/arclin/acaa023. [DOI] [PubMed] [Google Scholar]
- Gong YQ, Zhou HX, Zhang Y, Zhu XL, Wang X, Shen BB, Xian J, Ding Y. Validation of the 7-item Generalized Anxiety Disorder scale (GAD-7) as a screening tool for anxiety among pregnant Chinese women. Journal of Affective Disorders. 2021;282:98–103. doi: 10.1016/j.jad.2020.12.129. [DOI] [PubMed] [Google Scholar]
- Gorday, Rogers ML, Joiner TE. Examining characteristics of worry in relation to depression, anxiety, and suicidal ideation and attempts. Journal of Psychiatric Research. 2018;107:97–103. doi: 10.1016/j.jpsychires.2018.10.004. [DOI] [PubMed] [Google Scholar]
- Graham, Kyle SD. A preliminary investigation of sleep quality in functional neurological disorders: Poor sleep appears common, and is associated with functional impairment. Journal of the Neurological Sciences. 2017;378:163–166. doi: 10.1016/j.jns.2017.05.021. [DOI] [PubMed] [Google Scholar]
- Gregory, Agnew-Blais JC, Matthews T, Moffitt TE, Arseneault L. ADHD and Sleep Quality: Longitudinal Analyses From Childhood to Early Adulthood in a Twin Cohort. Journal of Clinical Child and Adolescent Psychology. 2017;46(2):284–294. doi: 10.1080/15374416.2016.1183499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallion LS, Ruscio AM. Should Uncontrollable Worry Be Removed From the Definition of GAD? A Test of Incremental Validity. Journal of abnormal psychology (1965) 2013;122(2):369–375. doi: 10.1037/a0031731. [DOI] [PubMed] [Google Scholar]
- Haslbeck, J. M. B., & Waldorp, L. J. (2020). mgm: Estimating Time-Varying Mixed Graphical Models in High-Dimensional Data. Journal of Statistical Software, 93(8), 10.18637/jss.v093.i08
- Itani, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Medicine. 2016;32:246–256. doi: 10.1016/j.sleep.2016.08.006. [DOI] [PubMed] [Google Scholar]
- Javakhishvili M, Widom CS. Out-of-Home Placement, Sleep Problems, and Later Mental Health and Crime: A Prospective Investigation. American Journal of Orthopsychiatry. 2022 doi: 10.1037/ort0000609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones PJ, Ma RF, McNally RJ. Bridge Centrality: A Network Approach to Understanding Comorbidity. Multivariate Behavioral Research. 2021;56(2):353–367. doi: 10.1080/00273171.2019.1614898. [DOI] [PubMed] [Google Scholar]
- Joo, Joo JH, Kwon J, Jang BN, Park EC. Association between quality and duration of sleep and subjective cognitive decline: a cross-sectional study in South Korea. Scientific Reports. 2021;11(1):16989–16989. doi: 10.1038/s41598-021-96453-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sampson NA, Berglund P, Gruber MJ, Al-Hamzawi A, Andrade L, Bunting B, Demyttenaere K, Florescu S, de Girolamo G, Gureje O, He Y, Hu C, Huang Y, Karam K, Kovess-Masfety V, Lee S, Levinson D, Medina Mora ME, Moskalewicz J, Wilcox MA. Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys. Epidemiology and Psychiatric Sciences. 2015;24(3):210–226. doi: 10.1017/S2045796015000189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9 - Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau WKW, Leung MK, Wing YK, Lee TMC. Potential Mechanisms of Mindfulness in Improving Sleep and Distress. Mindfulness. 2018;9(2):547–555. doi: 10.1007/s12671-017-0796-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Bai W, Zhu B, Duan R, Yu X, Xu W, Wang M, Hua M, Yu W, Li W, Kou C. Prevalence and correlates of poor sleep quality among college students: a cross-sectional survey. Health and Quality of Life Outcomes. 2020;18(1):1–210. doi: 10.1186/s12955-020-01465-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Wang, Y., Wang, S., Zhang, L., Li, L., Xu, D., Ng, C. H., Ungvari, G. S., Cui, X., Liu, Z. M., De Li, S., Jia, F. J., & Xiang, Y. (2018). Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. Journal of Sleep Research, 27(3), e12648–n/a. 10.1111/jsr.12648 [DOI] [PubMed]
- Li, Zhao Z, Chen D, Peng Y, Lu Z. Prevalence and associated factors of depression and anxiety symptoms among college students: a systematic review and meta-analysis. Journal of Child Psychology and Psychiatry. 2022 doi: 10.1111/jcpp.13606. [DOI] [PubMed] [Google Scholar]
- Lin, Liu ZR, Li SQ, Li CX, Zhang L, Li N, Sun XW, Li H, Zhou JP, Li QY. Burden of Sleep Disturbance During COVID-19 Pandemic: A Systematic Review. Nature and Science of Sleep. 2021;13:933–966. doi: 10.2147/NSS.S312037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu XC, Chen H, Bo QG, Fan F, Jia CX. Poor sleep quality and nightmares are associated with non-suicidal self-injury in adolescents. European Child & Adolescent Psychiatry. 2017;26(3):271–279. doi: 10.1007/s00787-016-0885-7. [DOI] [PubMed] [Google Scholar]
- Liu XC, Yang YY, Liu ZZ, Luo YC, Fan F, Jia CX. Psychometric properties of Youth Self-Rating Insomnia Scale (YSIS) in Chinese adolescents. Sleep and Biological Rhythms. 2019;17(3):339–348. doi: 10.1007/s41105-019-00222-3. [DOI] [Google Scholar]
- Meehl PE. Comorbidity and taxometrics. Clinical Psychology-Science and Practice. 2001;8(4):507–519. doi: 10.1093/clipsy/8.4.507. [DOI] [Google Scholar]
- Mei, S. L., Hu, Y. Y., Wu, X. G., Cao, R. L., Kong, Y. X., Zhang, L. W. … Li, L. (2022). Health Risks of Mobile Phone Addiction Among College studentsin China. International Journal of Mental Health and Addiction, 1–16. 10.1007/s11469-021-00744-3
- Mullarkey MC, Marchetti I, Beevers CG. Using Network Analysis to Identify Central Symptoms of Adolescent Depression. Journal of Clinical Child and Adolescent Psychology. 2019;48(4):656–668. doi: 10.1080/15374416.2018.1437735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunn, Samson DR, Krystal AD. Shining evolutionary light on human sleep and sleep disorders. Evolution Medicine and Public Health. 2016;2016(1):227–243. doi: 10.1093/emph/eow018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohayon MM, Caulet M, Priest RG, Guilleminault C. DSM-IV and ICSD-90 insomnia symptoms and sleep dissatisfaction. British Journal of Psychiatry. 1997;171:382–388. doi: 10.1192/bjp.171.4.382. [DOI] [PubMed] [Google Scholar]
- Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: Generalizing degree and shortest paths. Social Networks. 2010;32(3):245–251. doi: 10.1016/j.socnet.2010.03.006. [DOI] [Google Scholar]
- Pang, & Wu, S. (2021). Mediating effects of negative cognitive bias and negative affect on neuroticism and depression. Current Psychology (New Brunswick, N.J.). 10.1007/s12144-021-02052-4
- Park, Kim SY, Sung D, Kim H, Kim BN, Park S, Jung KI, Park MH. The relationship between risk of obstructive sleep apnea and other sleep problems, depression, and anxiety in adolescents from a community sample. Psychiatry Research. 2019;280:112504–112504. doi: 10.1016/j.psychres.2019.112504. [DOI] [PubMed] [Google Scholar]
- Pedrelli P, Nyer M, Yeung A, Zulauf C, Wilens T. College Students: Mental Health Problems and Treatment Considerations. Academic Psychiatry. 2015;39(5):503–511. doi: 10.1007/s40596-014-0205-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peretti-Watel, Alleaume C, Léger D, Beck F, Verger P. Anxiety, depression and sleep problems: a second wave of COVID-19. General Psychiatry. 2020;33(5):e100299–e100299. doi: 10.1136/gpsych-2020-100299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2022). R: A Language and Environment for Statistical Computing. R version 4.1.3 (2022-03-10). https://www.r-project.org/
- Robinaugh, Millner, A. J., & McNally, R. J. (2016). Identifying Highly Influential Nodes in the Complicated Grief Network. Journal of Abnormal Psychology (1965), 125(6), 747–757. 10.1037/abn0000181 [DOI] [PMC free article] [PubMed]
- Samaranayake, C. B., Arroll, B., & Fernando, A. T. (2014). Sleep disorders, depression, anxiety and satisfaction with life among college students: a survey of university students in Auckland, New Zealand. The New Zealand medical journa, 127(1399), 13–22. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/25145302 [PubMed]
- Sarris, O’Neil A, Coulson CE, Schweitzer I, Berk M. Lifestyle medicine for depression. Bmc Psychiatry. 2014;14(1):107–107. doi: 10.1186/1471-244X-14-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlechter P, Wilkinson PO, Knausenberger J, Wanninger K, Kamp S, Morina N, Hellmann JH. Depressive and anxiety symptoms in refugees: Insights from classical test theory, item response theory and network analysis. Clinical Psychology & Psychotherapy. 2021;28(1):169–181. doi: 10.1002/cpp.2499. [DOI] [PubMed] [Google Scholar]
- Scott AJ, Webb TL, Rowse G. Does improving sleep lead to better mental health? A protocol for a meta-analytic review of randomised controlled trials. Bmj Open. 2017;7(9):e016873–e016873. doi: 10.1136/bmjopen-2017-016873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder - The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Subirana I, Sanz H, Vila J. Building Bivariate Tables: The compareGroups Package for R. Journal of Statistical Software. 2014;57(12):1–16. doi: 10.18637/jss.v057.i12. [DOI] [Google Scholar]
- Tomaso, Johnson, A. B., & Nelson, T. D. (2021). The effect of sleep deprivation and restriction on mood, emotion, and emotion regulation: three meta-analyses in one. Sleep (,44 N.Y.), 44 vol., pp. 1–30). New York. 610.1093/sleep/zsaa289 [DOI] [PMC free article] [PubMed]
- van Borkulo CD, van Bork R, Boschloo L, Kossakowski JJ, Tio P, Schoevers RA, Borsboom D, Waldorp LJ. Comparing network structures on three aspects: A permutation test. Psychological Methods. 2022 doi: 10.1037/met0000476. [DOI] [PubMed] [Google Scholar]
- van den Bergh N, Marchetti I, Koster EHW. Bridges over Troubled Waters: Mapping the Interplay Between Anxiety, Depression and Stress Through Network Analysis of the DASS-21. Cognitive Therapy and Research. 2021;45(1):46–60. doi: 10.1007/s10608-020-10153-w. [DOI] [Google Scholar]
- Varghese, Lugo A, Ghislandi S, Colombo P, Pacifici R, Gallus S. Sleep dissatisfaction and insufficient sleep duration in the Italian population. Scientific Reports. 2020;10(1):17943. doi: 10.1038/s41598-020-72612-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D, Zhao J, Zhai S, Huang S, Yang Z, Pan Y, Liu X, Fan F. Longitudinal trajectories of insomnia symptoms among college studentsduring the COVID-19 lockdown in China. Journal of psychosomatic research. 2022;157:110795–110795. doi: 10.1016/j.jpsychores.2022.110795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, He L, Xue B, Wang X, Ye S. Sleep Quality Of College Students During COVID-19 Outbreak In China: A Cross-Sectional Study. Alternative Therapies in Health and Medicine. 2022;28(3):58–64. [PubMed] [Google Scholar]
- Wang, Wang M, Xin X, Zhang T, Wu H, Huang X, Liu H. Exploring the Relationship Between Anxiety, Depression, and Sleep Disturbance Among HIV Patients in China From a Network Perspective. Frontiers in Psychiatry. 2021;12:764246–764246. doi: 10.3389/fpsyt.2021.764246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner A cognitive (attribution)-emotion-action model of motivated behavior: An analysis of judgments of help-giving. Journal of Personality and Social Psychology. 1980;39(2):186–200. doi: 10.1037/0022-3514.39.2.186. [DOI] [Google Scholar]
- Wu, Han, H., Lin, T., Chen, M., Wu, J., Du, X., Su, G., Wu, D., Chen, F., Zhang, Q., Zhou, H., Huang, D., Wu, B., Wu, J., & Lai, T. (2020). Prevalence and risk factors of mental distress in China during the outbreak of COVID-19: A national cross‐sectional survey. Brain and Behavior, 10(11), e01818–n/a. 10.1002/brb3.1818 [DOI] [PMC free article] [PubMed]
- Wilsmore, Grunstein RR, Fransen M, Woodward M, Norton R, Ameratunga S. Sleep habits, insomnia, and daytime sleepiness in a large and healthy community-based sample of New Zealanders. Journal of Clinical Sleep Medicine. 2013;9(6):559–566. doi: 10.5664/jcsm.2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye X, Shu HL, Feng X, Xia DM, Wang ZQ, Mi WY, Yu B, Zhang XL, Li CQ. Reliability and validity of the Chinese version of the Patient Health Questionnaire-9 (C-PHQ-9) in patients with psoriasis: a cross-sectional study. BMJ open. 2020;10(7):e033211. doi: 10.1136/bmjopen-2019-033211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou SJ, Wang LL, Yang R, Yang XJ, Zhang LG, Guo ZC, Chen JC, Wang JQ, Chen JX. Sleep problems among Chinese adolescents and college students during the coronavirus-2019 pandemic. Sleep Medicine. 2020;74:39–47. doi: 10.1016/j.sleep.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou, Wang X, Sun L, Liu K, Hou G, Yang W, Liu C, Yang H, Zhou N, Zhang G, Ling X, Liu J, Cao J, Ao L, Chen Q. Poorer sleep quality correlated with mental health problems in college students: A longitudinal observational study among 686 males. Journal of Psychosomatic Research. 2020;136:110177. doi: 10.1016/j.jpsychores.2020.110177. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Analytic code and data for this work are available upon request.