Abstract
This article reviews the literature and the authors’ experiences regarding the performance of lower extremity fluoroscopically guided procedures from the hip to the toes. An overview of injections and aspirations, their indications, risks, and complications are provided, focusing on anesthetics, corticosteroids, and contrast agents. A variety of approaches to each joint and the associated pearls and pitfalls of each approach will be discussed.
Keywords: Fluoroscopic-guided joint injections, Prosthetic joint infection (PJI), Septic arthritis, Corticosteroid injection (CSI), Intraarticular contrast, Hip injection, Hip aspiration, Knee injection, Knee aspiration, Foot injection, Naviculocuneiform injection, Talonavicular injection, Tarsometatarsal injection, Metatarsophalangeal injection, Subtalar injection, Tibiotalar injection
Introduction
Fluoroscopy is widely used to guide joint injections and aspirations because it is readily available, low cost, quick, and easy to use [1]. In this paper, we will discuss fluoroscopic-guided procedures in the lower extremities and list several approaches, pearls, and pitfalls for each joint from the hips to the toes. Both joint aspiration and injection will be described. Medications, their indications, and complications will be reviewed. All techniques assume the operator is using a stationary fluoroscopy unit.
Fluoroscopy has several advantages over ultrasound (US). Fluoroscopy is taught in every radiology training program in the USA, and therefore, access to fluoroscopy is universal. Although musculoskeletal US is also useful for joint access, it still remains a “niche” modality in many programs and is not widely taught to residents [2]. With fluoroscopy, contrast injection can confirm needle position and intraarticular location as well as demonstrate any “unexpected” findings during the examination such as fractures, hardware failure, or posttraumatic communication of joints which typically do not communicate. A vertical needle path to the target can be chosen without the concern for loss of needle visualization as with US. Fluoroscopy is easy to use and easy to teach because the fluoroscopic appearance of anatomy is identical to radiography. Conversely, US involves a steep learning curve for scanning technique, acquiring the understanding of the sonographic appearance of tissues and artifacts unique to ultrasound, and developing US-guided needle skills [3]. In postoperative patients or those with pathology or variant anatomy, fluoroscopy with contrast injection is superior to US in demonstrating unexpected communications between joints [3]. At our institution, we prefer fluoroscopy to US for patients who are obese and who have postoperative scarring, as the depth of the target and the attenuation of the sound beam can obscure needle visualization with US. A criticism is that fluoroscopy entails ionizing radiation; however, using the “last image hold” technique significantly mitigates this concern [4]. Some authors have expressed concern about the possibility of traversing infected overlying tissue if fluoroscopic guidance is used for joint aspiration and cross-sectional imaging is not initially performed, but this concern remains theoretical rather than proven [1, 5, 6].
Indications
Over the past 4 years, our practice has seen an 80% growth in lower extremity fluoroscopic procedure volumes, with a 93% growth in foot procedures alone. The lifetime risk of osteoarthritis (OA), the most common form of arthritis, is 15–18% and up to 24% in obese women [7]. The prevalence of OA is increasing due to multiple factors, including increased longevity, increased BMI, and the desire to maintain active lifestyles as the population ages [8]. These factors have driven the increases in procedure volumes [9, 10].
Fluoroscopic lower extremity procedures are performed for both diagnostic and therapeutic indications. The injection of local anesthetic and/or corticosteroid can provide therapeutic pain relief, confirm an intraarticular source of pain, and guide surgical planning. CT or MR arthrography can identify intraarticular pathology such as labral, cartilage or meniscal tears and intraarticular bodies [10]. Joint aspiration may diagnose native joint septic arthritis (SA) or prosthetic joint infection (PJI), crystal arthropathy, inflammatory arthritis, and osteoarthritis or provide pain relief by decompressing an effusion or hemarthrosis [9]. Depending on the cause of pain, these procedures may postpone or defer the need for surgery [8, 11]. Table 1 highlights indications for aspiration and injection.
Table 1.
Indications
| Aspiration | Injection |
|---|---|
| Infection/septic joint | Pain (corticosteroids, viscosupplements, orthobiologics) |
| Inflammatory arthropathy | Contrast for arthrography (iodinated contrast or gadolinium contrast) |
| Hemarthrosis | Surgical planning to identify the source of pain |
| Crystal arthropathy | |
| Joint decompression |
Pre-procedure planning
Before attempting any procedure, it is important for the radiologist to know the relevant anatomy and the expected anatomic connections or post-surgical variations to optimize needle placement. Table 2 highlights expected joint communications [3, 12–14]. It is important for the radiologist to know the properties, doses, and side effects of the various injectables used in fluoroscopic procedures.
Table 2.
Expected joint communications or contrast extension
| Joint | Communication |
|---|---|
| Hip joint | Iliopsoas bursa |
| Knee joint | Suprapatellar recess, Baker cyst, Popliteus tendon sheath |
| Tibiotalar joint | Subtalar joint (posterior facet), FHL tendon sheath |
| Subtalar joint (posterior facet) | Tibiotalar joint, sinus tarsi |
| Subtalar joint (middle and anterior facets) | Talonavicular joint |
| Talonavicular joint | Subtalar joint (middle and anterior facets), calcaneocuboid joint |
| Calcaneocuboid joint | Talonavicular joint |
| Naviculocuneiform joint | Intercuneiform, second and third tarsometatarsal joints |
| First tarsometatarsal joint | None |
| Second and third tarsometatarsal joints | Intercuneiform, Naviculocuneiform joints |
| Fourth and fifth tarsometatarsal joints | None |
| First metatarsophalangeal joint | Hallux sesamoid first metatarsal joints |
| Interphalangeal joint | None |
Prior imaging should always be consulted if available. In our practice we prefer to obtain radiographs within 3 months of the procedure or immediately before the procedure, to assess for procedure contraindications or complications from prior steroid injection. Pre-procedure preparation also includes review of patient history and allergies and the discussion of the procedural details, risks, and benefits of injected medications and the injection procedure with the patient during consent [9].
General technique
Sterile technique is used for all procedures. The patient is positioned in the appropriate manner for the joint being examined. All techniques assume the operator is using a stationary fluoroscopy unit. A radiopaque marker is used to identify the needle entry site/target and the area is marked. A “last image hold” is obtained of the joint with the marker in place, before the needle is inserted, to use for intra-procedural comparison with post contrast images.
The skin is sterilized, then anesthetized with a 25-G needle using 1% lidocaine. For a superficial joint, the same 1.5″ 25-G needle may be used for anesthesia and the procedure. The choice of needle gauge and needle length depends on the joint in question, patient body habitus, and the purpose of the procedure, whether that is aspiration or injection. Larger, deeper joints usually require 3.5″ spinal needles (6″ spinal needles may be necessary to access hip joints in larger patients). Smaller, superficial joints may be accessed with 1-cm or 1.5″ needles. However, in markedly arthritic superficial joints, a larger gauge needle may be useful in traversing regions of more robust osteophytosis or synovitis. Table 3 includes suggested needle gauges, lengths, and mixture volume injected for each joint.
Table 3.
Suggested needle gauge and joint volume
| Joint | Aspiration (needle) | Injection (needle) | Volume mixture (arthrography vs therapy) | |
|---|---|---|---|---|
| Hip | 18 G, 3.5–6.0 inch | 20–22 G, 3.5–6.0 inch | 10–12 ml | 4–5 ml |
| Knee | 18 G, 1.5–3.5 inch | 20–22 G, 1.5–3.5 inch | 20–40 ml | 4–5 ml |
| Tibiotalar | 18 G, 1.5–3.5 inch | 20–22 G, 1.5–3.5 inch | 2–4 ml | 2–3 ml |
| Subtalar | 18 G, 1.5 inch | 20–22 G, 1.5 inch | N/A | 2–3 ml |
| Smaller joints of the foot | 20–22 G, 1.5 inch | 23–25 G, 0.5–1.5 inch | N/A | 0.5–1.0 ml |
Some operators prefer to use an inner stylet to avoid the theoretical risk of clogging the needle with soft tissue. Others prefer to advance the needle with the lidocaine syringe attached, to diminish procedure time and minimize syringe exchanges. Needles of 20–25 G are used for injections, whereas 18-G needles are preferred for aspirations since the aspirate may be too thick for smaller gauge needles [9, 15].
For a straight vertical approach, the access needle is advanced perpendicular to the fluoroscopy beam with the hub directly over the needle tip (the “bull’s eye” approach) [1, 3, 16]. When the needle hits bone or is felt to enter the joint space, a test injection of local anesthetic is made. If no resistance is encountered, intraarticular location is confirmed by injecting a small volume of iodinated contrast under intermittent fluoroscopy. It is important for the operator to be cognizant of the differences in tactile sensation when test injecting a large joint such as the hip versus a smaller, superficial joint. Contrast should typically disperse freely into the joint (Fig. 1), although in a severely arthritic joint, the intraarticular contrast may have a crenulated, irregular appearance due to synovitis/debris.
Fig. 1.
Normal pre-MRI right hip injection in a 32-year-old female referred for possible labral tear. AP fluoroscopic image shows contrast opacifying the normal joint capsule. A prominent zona orbicularis, or annular ligament, is identified, causing a normal constriction at the proximal femoral head-neck junction (arrows)
If there is technical difficulty with injection or aspiration, the needle bevel should be rotated, or the needle withdrawn and repositioned. The needle may tend to deflect in the direction of the needle bevel so it may be necessary to rotate the bevel if traversing a larger amount of tissue to keep the needle on a straight trajectory [1, 9].
Medications
Corticosteroids, local anesthetics, and contrast agents are the most frequently injected medications into lower extremity joints in our practice and will be briefly reviewed below. It is beyond the scope of this paper to review other injectables such as orthobiologics (autologous blood products and autologous stem cells) and viscosupplements.
Local anesthetics
Local anesthetics provide immediate pain relief and can also pinpoint intraarticular sources of pain [5]. Intraarticular injection of local anesthetics, although widely practiced, remains an off-label, non-FDA approved use [3, 5]. Some studies have shown dose-dependent (high concentration and long exposure) chondrolysis in vivo especially when there is underlying cartilage abnormality; however, recent in vitro studies have not found this effect to be significant [17, 18]. In vivo studies also showed no definite correlation of anesthetic potency with chondrocytotoxicity; ropivacaine was shown to be the least toxic of the agents studied [17]. Contraindications to local anesthetic injection include hypersensitivity reactions to amide local anesthetics [19]. There is no cross-reaction with ester formulations such as chloroprocaine and procaine [5].
Corticosteroids
Corticosteroid injections (CSI) of joints are often performed to alleviate pain or to temporize in patients who wish to defer surgery or who are not surgical candidates [8, 20]. Intraarticular CSI have proven benefit in delaying the progression of rheumatoid arthritis but show no statistical benefit over an extended period [21]. There is conflicting evidence regarding efficacy and safety of CSI for other indications. The safety concerns and adverse effects are more apparent in weight bearing joints [22, 23]. Observed adverse effects include accelerated progression of osteoarthritis, progressive cartilage thinning, subchondral insufficiency fracture, osteonecrosis, rapidly progressive idiopathic arthritis, joint destruction, and bone loss in the hip and the knee [8, 22–25]. It is prudent to review serial radiographs in patients undergoing repeat steroid injections to detect subtle structural changes over time [22]. Long-term prospective studies are needed to understand the true effects of CSI as there is conflicting data, with some studies stating a lower complication rate than once thought [7].
CSI of fractures is contraindicated as CSI can inhibit bone healing [26–28]. CSI in patients with infected joints or systemic bacteremia should be avoided [5]. Hypersensitivity reactions can occur in patients with repeated exposure to steroids [29, 30].
Local side effects include skin depigmentation and subcutaneous fat atrophy, seen more frequently in superficial injections of the foot and ankle [31, 32]. Steroid “flare” (increased pain) may occur 2 days post injection and facial flushing can occur in some patients [20]. The systemic effects of steroids vary and include elevated serum glucose levels and adrenal suppression [33]. There is a very low risk of septic arthritis from intraarticular injection [5].
Due to the risks discussed above, steroids should be avoided in patients with little to no evidence of osteoarthritis [22]. In our practice, we routinely discuss the potential adverse effects and side effects of intraarticular CSI with patients at the time of procedure consent [34]. Dosing for large joint intraarticular steroids is a maximum of 3 doses (40–80-mg triamcinolone per dose) per year and a minimum of 6 weeks between doses [5]. Triamcinolone and methylprednisolone are the most commonly used corticosteroids [35].
Given the unknown effects of CSI on COVID-19 vaccine efficacy, the American Academy of Orthopedic Surgeons released guidelines regarding the timing of CSI relative to COVID-19 vaccination. They recommend “avoiding CSI for two weeks before and one week after COVID vaccine administration” and to “consider using shorter-acting corticosteroid medications and the lowest effective dose” [36].
Contrast agents
Severe allergic reactions to intraarticular contrast are rare enough to be case reportable especially when compared to intravascular administration [20, 37–39]. The most common reactions are mild and include vasovagal reactions (seen most in young male athletes), transient sterile chemical synovitis (seen more often with higher osmolar and ionic CT contrast agents) or flare reactions and hives [20, 37, 38]. In the non-MR arthrogram setting air can be substituted as an alternate contrast agent in patients with a history of severe contrast allergy (Fig. 2).
Fig. 2.
A 79-year-old female with osteoarthritis and contrast allergy, referred for right hip corticosteroid injection (CSI). AP fluoroscopic image shows right hip joint space narrowing with osteophytes, with the needle tip at the femoral head-neck junction. Intraarticular placement is confirmed with air injection, seen as radiolucency outlining the joint (white arrows)
Iodinated contrast
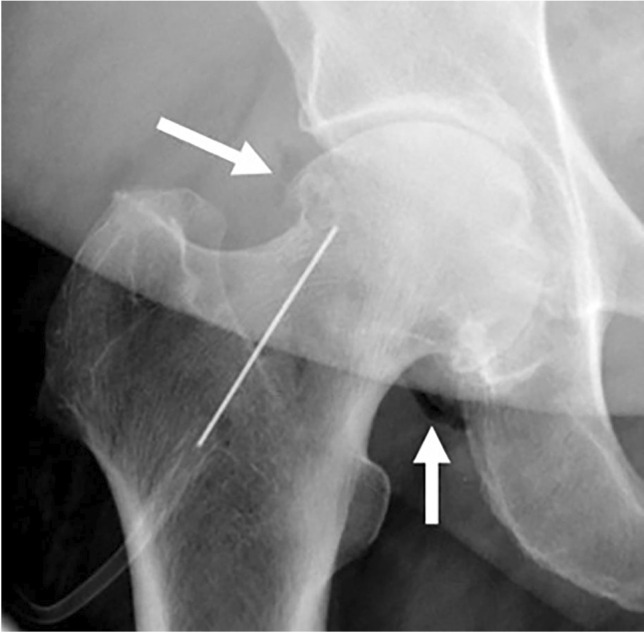
Prior to injecting medication or Gadolinium, a trace amount of non-ionic, iodinated contrast (IC) is frequently injected to confirm needle placement in injection and aspiration procedures. Low or iso-osmolar IC is not bactericidal [40]. IC can be used as an intraarticular contrast agent for CT arthrography when a patient has contraindications to MRI. The dilution ratio of iodinated contrast to 0.9% saline is 1:1 [1]. CT arthrography has been shown to be equivalent to MR arthrography in showing cartilage, labral and meniscal tears, and superior at assessing osseous lesions and calcifications (Fig. 3) [41].
Fig. 3.
An 80-year-old female with prior ORIF of left intertrochanteric fracture, with persistent pain, referred for CT arthrogram. Axial CT image through the left femoral head shows intraarticular contrast outlining the normal posterior labrum, seen on CT as a hypodense triangle contiguous with the posterior acetabulum, outlined by hyperdense contrast (white arrow). The anterior labrum is frayed and diminutive (white arrowhead). An asterisk denotes the superior aspect of the intramedullary nail
Gadolinium contrast
Gadolinium intraarticular injection for MR arthrography is an off-label use of the FDA-approved intravascular administration [42]. Small quantities of dilute gadolinium, prepared by dilution with saline and non-ionic contrast, allow visualization during fluoroscopy and allow for optimal signal and contrast on MR arthrography sequences [43]. A 1:200 dilution of gadolinium within a mixture composed of 50% iodinated contrast and 50% 0.9% saline is generally accepted [1]. Studies have shown that this mixture combination does not result in production of free intraarticular gadolinium in vitro [42]. After injection, gadolinium contrast from the joint is rapidly reabsorbed into the blood without permanent complications to the joint [44]. However, recent literature focusing on patients with intravascular gadolinium administration has shown there is long-term retention of trace amounts of gadolinium in the body tissues including incorporation into bone [44]. This finding has been found at a higher rate with linear versus macrocyclic agents [44]. Similar findings have been found in animal models with intraarticular gadolinium injection [45]. The mechanism and chemical form of the retention and clinical consequences are unknown and not well understood at this time [44].
Joint aspiration
The incidence of native SA is estimated at 6–10 cases per 100,000 per year, and the knee is the most infected joint [46]. There is a bimodal peak age of incidence affecting children under 3 years and adults over 55 years [46]. The incidence of PJI is rising, especially in patients over 65 years. PJI is estimated to affect 1–3% of primary arthroplasties and 5–6% of revision arthroplasties [46]. Guidelines for synovial white blood cell (WBC) count set general cutoff values of < 2000 WBC/mm3 (non-inflammatory), 2000–50,000 WBC/mm3 (inflammatory), and > 50,000 WBC/mm3 (infectious); however, these values overlap [47]. A more sensitive assessment is the differential WBC count with %PMN greater than 80% being highly sensitive for infection [47].
Although the knee is the most frequently aspirated lower extremity joint in clinical practice, it is usually performed without imaging guidance by services other than radiology. In our practice, hip aspiration is the most often requested fluoroscopically guided joint aspiration. Indications for joint aspiration include infection, inflammatory arthropathy, crystal disease, hemarthrosis, or therapeutic joint decompression [9]. Risk factors for septic joint include age, intravenous drug use, immunosuppression, diabetes, rheumatoid arthritis, joint replacement, HIV, bacteremia, and skin infection/direct inoculation [48].
A native joint aspiration should be performed urgently when SA is a concern. However, there are conflicting opinions in the literature regarding emergent aspiration if a patient has no signs of sepsis or bacteremia. Regarding cartilage destruction, studies have concluded that cartilage destruction can occur within days or that cartilage destruction does not occur for weeks [15, 49]. Discrepancy may be attributed to when treatment with antibiotics is initiated and the degree of immune response an individual mounts [49]. Most native SA is classified as acute, but chronic infections can occur with mycobacterial or fungal organisms [46].
PJI can be classified as acute vs. chronic based on the stability of the biofilm that forms along the prosthesis. In the acute setting, the biofilm is unstable and susceptible to host defense and antimicrobials agents, whereas in the chronic setting, the biofilm has matured, allowing microorganisms to thrive [46].
The clinical presentation of septic joint is variable; only 58% of patients present with high fever and 50–60% of patients present with elevated serum WBC [50]. Elevated serum WBC count, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), synovial WBC count, and synovial polymorphonuclear neutrophil (PMN) cells are sensitive but not specific markers for septic joint [51].
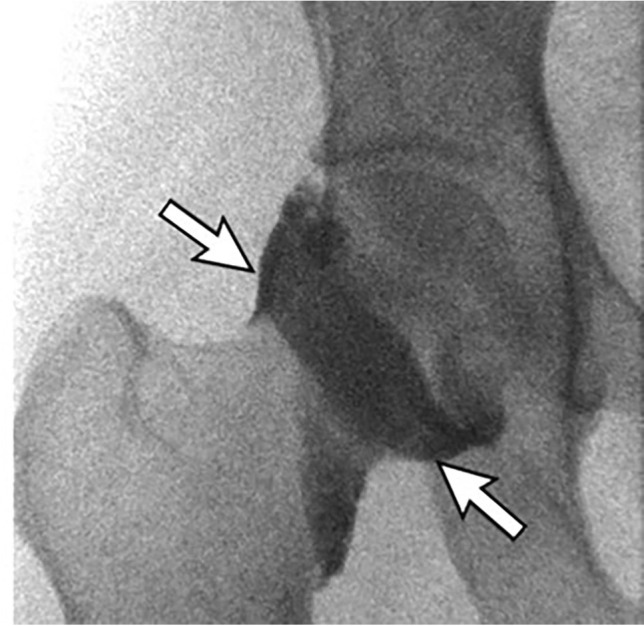
Pre-procedure radiographs should be obtained to assess for fractures, erosions, osteoarthritis, effusions, and hardware complications before performing an aspiration. If available, pertinent cross-sectional imaging is also important to review for non-articular causes of pain such as occult hip fracture, tendon or muscle tear, tumor, cellulitis, or extraarticular soft tissue abscess. However, imaging remains indeterminate for distinguishing an infected joint from a sterile one [48]. Both infected and sterile joints may demonstrate effusions or bone marrow edema on MRI. Erosions may be seen with septic arthritis but also with inflammatory and crystalline arthropathy (Fig. 4) [52].
Fig. 4.
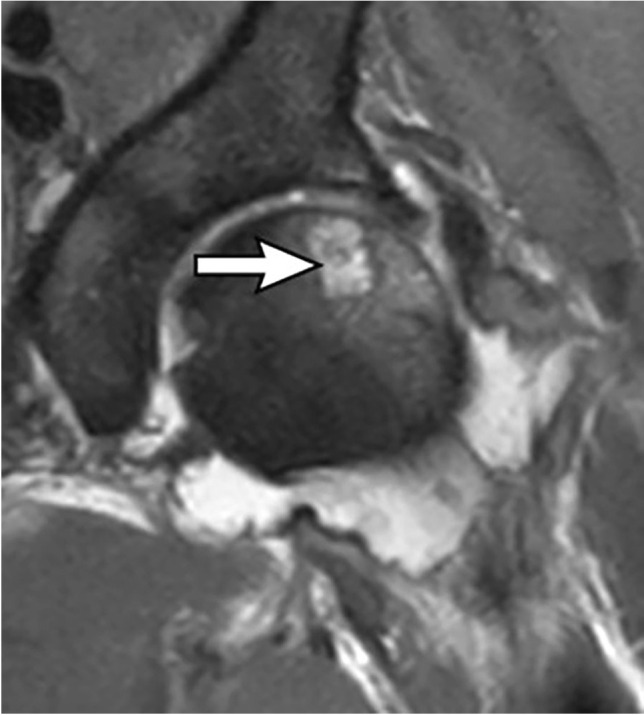
A 60-year-old male with history of rheumatoid arthritis, admitted for sudden onset of left hip pain. Pre-aspiration MRI showed a femoral head erosion (arrow), bone marrow edema, chondral thinning, and a complex joint effusion. Culture of aspirate yielded no organisms. Patient was diagnosed with a rheumatoid flare
Patients with native SA are rarely on antibiotics, whereas patients with suspected PJI are frequently on antibiotics when they are referred for aspiration. Many societies advocate the cessation of antibiotics for at least 2 weeks prior to aspiration in patients with suspected PJI to increase the likelihood of a positive culture, as antibiotic administration will reduce the sensitivity of the aspiration and decrease the possibility of isolating an organism [15, 46, 48]. However, the discontinuation of antibiotics is not always feasible, and if referring physicians insist on aspiration while the patient is still on antibiotics, we will do the procedure, with the caveat that a false-negative result may be obtained.
The gold standard for diagnosing a septic joint remains aspiration with culture, gram stain, cell count, and differential [51]. A minimum of 1 cc aspirate is required for a cell count. Injection of local anesthetic into suspected infected native or prosthetic joints should be avoided during an aspiration procedure, as local anesthetic has been reported to be bacteriostatic or bactericidal [15, 48, 53]. An 18-G needle is the most commonly used gauge for joint aspiration as it is difficult to aspirate thick, viscous material through smaller gauge needles [15]. If an effusion is encountered, one should aspirate as much material as possible to decompress the joint and provide immediate pain relief [9]. In our experience, a turbid or opaque aspirate, although correlated with positive culture, is not in itself diagnostic of infection, as both infectious and inflammatory aspirates may appear turbid.
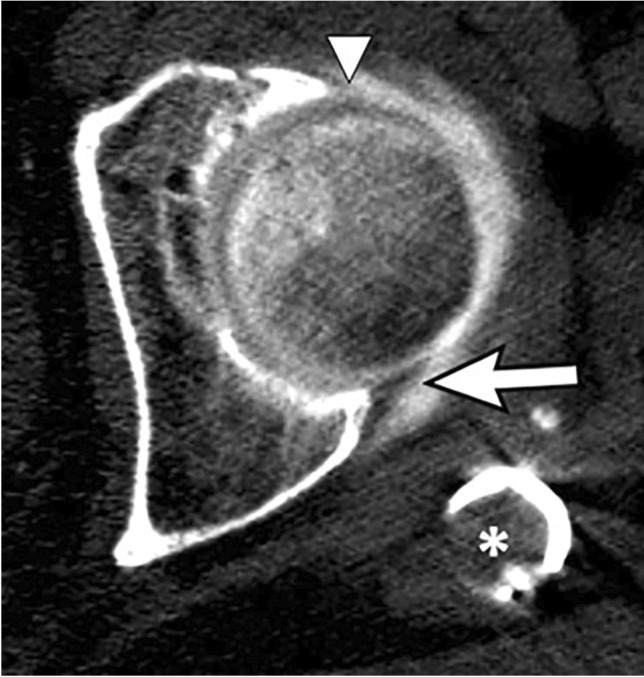
A “dry tap,” or a joint aspiration that yields no fluid, is a common occurrence. One study showed a dry tap occurred in 41.8% of aspirations of total hip arthroplasties (THA) and 15% of total knee arthroplasties (TKA) [54]. In the event of a dry tap, lavage with non-bacteriostatic saline can yield positive cultures [51]. A subsequent contrast injection may demonstrate pseudocapsule dehiscence with a sinus tract leading to a fluid collection, a finding highly associated with infection (Fig. 5) [51, 55]. It is important to consult with the referring orthopedic surgeon before performing a lavage, as the orthopedic literature is divided regarding the utility [56]. Recent literature suggests that a dry tap indicates a non-infected joint in 86% of cases, both native and prosthetic [57]. When considering a lavage, it is good practice to do the lavage prior to injecting the joint with contrast, as some studies have suggested that contrast is bacteriostatic, but others conclude that low or iso-osmolar contrast agents are not bacteriostatic [51]. It should be noted that performing a synovial WBC cell count on lavage fluid is a controversial practice because the results will be inaccurate due to saline dilution [48]. However, a 2020 study showed that in patients with PJI who had a dry tap, saline lavage samples with greater than 80% PMNs had 75% sensitivity for PJI [54]. After lavage, the injection of contrast is useful to delineate sinus tracts, collections, or bursae [15, 48, 51]. There is the theoretical but remote risk of causing intravasation of the infection [9, 15].
Fig. 5.
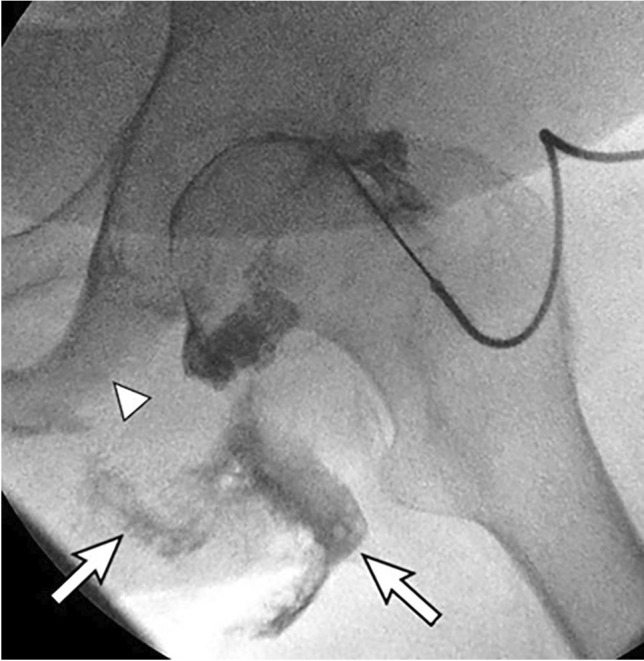
A 69-year-old male with left ischial decubitus ulcer with suspected septic left hip joint. Aspiration attempts yielded no fluid. Fluoroscopic image shows contrast injection not only opacifying the left hip joint but also extending into the ischial decubitus ulcer (arrows). The ischial tuberosity is eroded (arrowhead), consistent with osteomyelitis
Alternatively, air can be injected after aspiration to act as a contrast agent and to confirm intraarticular location, especially in cases of a dry tap (Fig. 2) [58]. Antibiotic therapy within the 48 h prior to aspiration has also been shown to decrease the diagnostic yield of joint aspiration [48].
In the absence of sepsis, PJIs do not have the same urgency as native septic joints due to the absence of native cartilage. Unique complications of PJI include arthroplasty failure, soft tissue and osseous destruction, and biofilm production along the prosthetic joint [46, 48]. Specific to PJI, a negative aspiration does not completely rule out infection and another attempt may be necessary given that loculations that can form [59]. In addition, microorganisms causing PJI may be indolent and require sonication and/or specialized media to culture [60, 61]. Assessment for alpha defensin and PCR, ELISA, and microarray analysis are newer techniques being used to evaluate for PJI [48].
There is no evidence to support withholding anticoagulation medications or checking bleeding tests prior to arthrocentesis. However, some institutions maintain the practice of checking INR on patients who take warfarin to ensure patients are not supratherapeutic before the aspiration is performed [62–64].
Lower extremity joints
Hip joint
Hip injections are most commonly performed to alleviate pain or to confirm an intraarticular source of pain [16]. CT or MR arthrograms enable assessment of labral or chondral injury and intraarticular bodies. Concern for infection in a painful native hip or prosthesis is the most common reason to perform a hip aspiration [16]. Approximately 15% of all adult cases of SA involve the hip (Fig. 6) [50]. Uncommon indications for aspiration include suspected inflammatory arthritis, hemarthrosis, and crystal arthropathy.
Fig. 6.
A 29-year-old female intravenous drug user presented with sudden onset of right hip pain and inability to bear weight. Fluoroscopic image after aspiration with contrast injection showed irregular filling defects of the joint, typically seen with synovitis. This appearance of synovitis can be seen in the setting of infection or arthritis and is a non-specific finding. Aspirate grew Staphylococcus aureus
Three approaches, including direct anterior, anterior oblique (inferior to superior), and anterior oblique (lateral to medial), can be used to inject or aspirate the hip joint (Fig. 7). It is important to palpate the femoral artery and mark it before the procedure to avoid inadvertent arterial puncture or anesthesia of the femoral nerve. This is especially important in post-arthroplasty patients with altered anatomy.
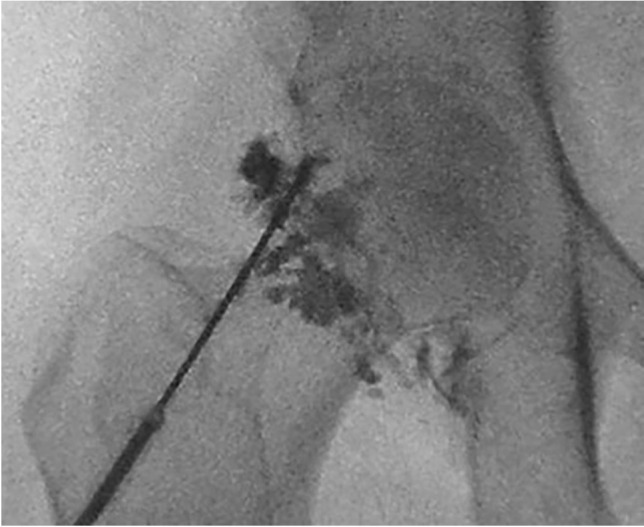
Fig. 7.
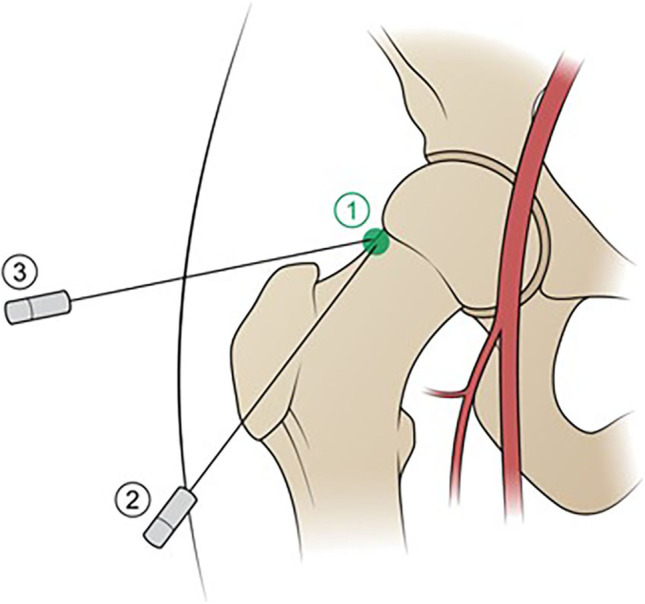
Illustration of the hip depicts three different approaches to hip joint injection. The direct anterior approach (1) is performed hub over needle, using the “bull’s eye” approach, targeting the femoral head-neck junction. The anterior oblique approach from inferior to superior (2) also targets the femoral head-neck junction but is obliqued 60° from the skin entry site to the target. The anterior oblique approach from lateral to medial (3) uses a skin entry site overlying the greater trochanter and is angled 45° lateral to medial. The common femoral artery is depicted in red
Intraarticular needle placement is confirmed by the free dispersion of contrast along the hip joint and the femoral neck with distention of the joint capsule. The zona orbicularis, or annular ligament, is a circumferential, band-like thickening of the joint capsule which can cause a normal constriction at the femoral head-neck junction (Fig. 1) [9, 10, 16, 65]. Additionally contrast instillation can help visualize a paralabral cyst associated with a labral tear [66].
Approximately 15% of people have variant anatomy with a communication between the hip capsule and overlying iliopsoas bursa [13]. Targeting the superolateral femoral head-neck junction diminishes the chance of inadvertent iliopsoas bursal injection that can occur when targeting the center of the femoral neck. It should also be noted that if the needle is not advanced deeply enough to contact bone, inadvertent opacification of the iliopsoas bursa will likely occur (Fig. 8). The solution is to advance the needle to bone and re-inject. If contrast will not flow, the needle bevel may be tenting the joint capsule to the bone. The needle should be backed out 1 mm, the bevel rotated, and the needle advanced again. If contrast still does not flow, then the needle should be backed out and the needle tip angled. If all these efforts fail, the needle should be withdrawn, the stylet placed through the needle to clear any tissue debris, and a new puncture targeting the superior femoral head-neck junction made.
Fig. 8.
A 41-year-old male with left hip pain, presenting for a CSI. Initial test injection shows opacification of the iliopsoas bursa (arrow), despite correctly targeting the superior femoral head-neck junction. The needle was advanced to bone and subsequent injection (not shown) opacified the hip joint
Direct anterior approach
The direct anterior approach with the needle parallel to the x-ray beam is the most used approach, with various targets reported including the lateral femoral head and lateral, central, or medial femoral neck [9, 10, 67]. We favor the lateral femoral head-neck junction (Fig. 7) to diminish the chances of inadvertent iliopsoas bursa injection. The hip should be internally rotated 10–15°, facilitated by taping the feet together with both hips internally rotated. The medial femoral neck is the least common target due to its proximity to the overlying femoral neurovascular bundle, yet this location may yield a larger volume aspirate due to the more dependent location and more redundant capsule [68]. Studies on pain associated with different anterior approaches show more pain associated with targeting the femoral head. However, with the less painful femoral neck target, more extra-capsular contrast injection was found, likely because the joint capsule inserts on the femoral neck [69].
Anterolateral approach, inferior to superior
This approach is useful when the femoral vessels lie far lateral over the femoral target or when a deep groin crease prevents a direct approach, requiring an inferior skin entry and oblique course before entering the joint [70]. The hip should be internally rotated 10–15°. The needle punctures the skin overlying the femoral neck just medial to the intertrochanteric line. The needle is angled 60° superomedial to target the superior lateral femoral head-neck junction (Fig. 7) [71].
Anterolateral approach, lateral to medial
Challenging situations in our practice involve patients who are obese with a deep groin fold and overlying panniculus, who cannot lie flat, or who have a hip contracture. In these cases, we have found success in using the angled anterior-oblique approach with a lateral to medial needle path (Fig. 7) [72]. The patient is rolled semi-decubitus to the contralateral side with a foam wedge supporting the body. In this position, gravity displaces the panniculus away from the hip of interest. The superior edge of the greater trochanter is located with fluoroscopy and marked as the skin entry site. After skin puncture, the needle is angled 45° from lateral to medial, targeting the superior femoral head-neck junction [72].
Hip arthroplasty
In the post-operative setting, the main reason for aspiration in patients presenting with pain and a prosthesis is PJI. Aspiration is performed with an 18-G needle entering from an anterolateral approach, targeting the prosthetic neck [59]. Once contact between the prosthesis and needle is made, a distinct “metal on metal” sensation is felt, and the needle is subsequently “walked” slightly laterally or along the neck to seek a dependent fluid pocket [59]. In the case of a “dry tap,” contrast injection can show decompression into a sinus tract or abscess (Fig. 9). In these postoperative patients, the operator may feel different tissue resistance when compared to a native hip either due to capsular disruption or scar tissue formation [16]. This subset of patients may also need additional local anesthetic as these aspirations can be more painful than a native hip due to the postoperative scarring.
Fig. 9.
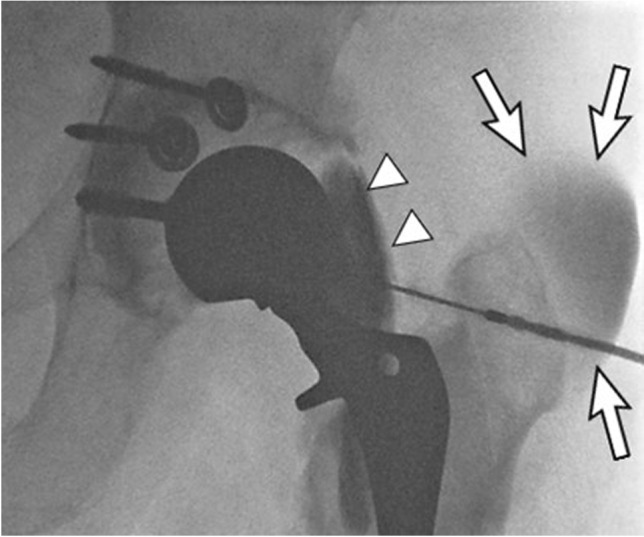
A 60-year-old male with infected left total hip arthroplasty, explanted acetabular component with acetabular spacer placement. Follow-up aspiration yielded a dry tap. Fluoroscopic image of the left hip after subsequent contrast injection shows communication of the hip joint with the iliopsoas bursa (arrowheads) and contrast decompressing into an abscess overlying the greater trochanter (arrows)
Knee joint
Knee injections with local anesthetic, corticosteroids and viscosupplements are commonly performed for symptomatic relief or treatment of OA [16]. They are less frequently performed for arthrography given the high resolution available with non-contrast MRI without intraarticular contrast. However, CT arthrography is still performed to assess for meniscal or cartilage pathology when MRI is contraindicated or to assess for loosening in patients with a total knee arthroplasty [16].
Given that 45% of septic arthritis in adults occurs in the native knee, aspiration is a common procedure [50]. Other indications include suspected inflammatory arthritis, hemarthrosis, crystal arthropathy, and PJI [16]. Three approaches, including lateral, medial, and anterior can be used to inject or aspirate the knee joint (Figs. 10 and 11). Contrast should flow freely into the tibiofemoral compartment and disperse across the midline, no matter which approach is used (Fig. 12); contrast also can extend along all the recesses of the joint, into the popliteus tendon sheath, and into a Baker cyst if present.
Fig. 10.
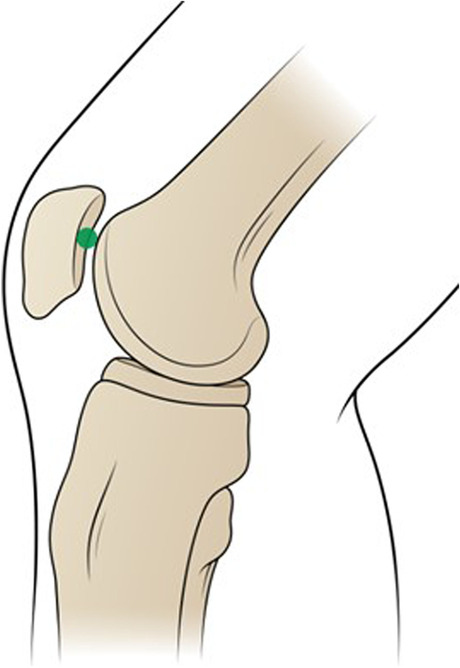
Illustration of the lateral view of the knee joint with a green dot overlying the patellofemoral joint, showing the expected target of both the medial and lateral patellofemoral approaches, whether the patient is placed supine or decubitus
Fig. 11.
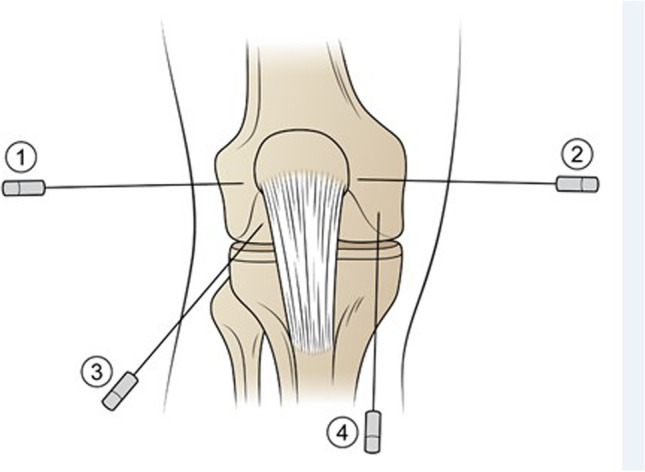
Illustration of the AP view of the knee showing the lateral patellofemoral (1), medial patellofemoral (2), arthroscopic anterior approach targeting the femoral notch (3), and arthroscopic anterior approach targeting the ipsilateral femoral condyle (4)
Fig. 12.
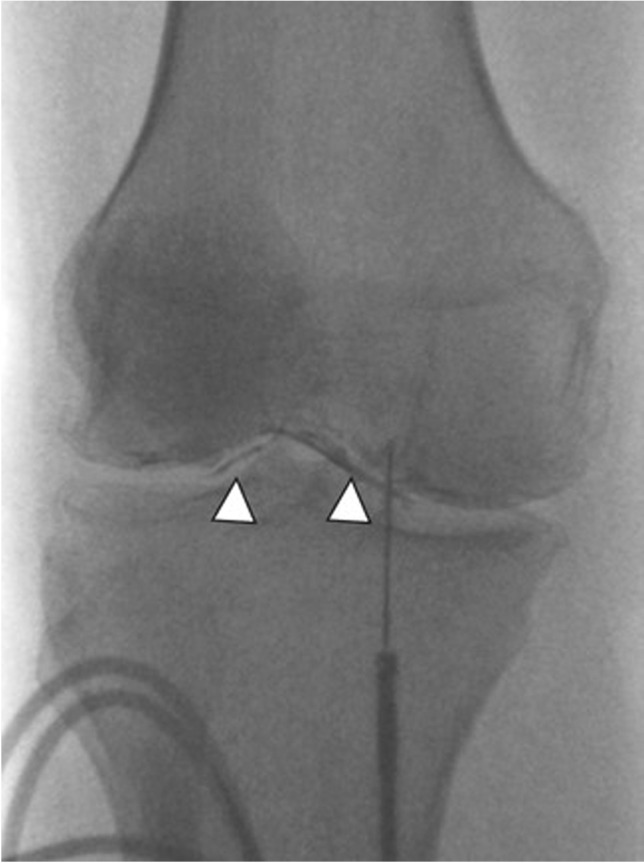
A 75-year-old female with osteoarthritis. Arthrogram performed prior to viscosupplement injection uses the anterior arthroscopic approach with the needle targeting the ipsilateral medial femoral condyle. Contrast outlines the medial tibiofemoral compartment and crosses the midline to outline the lateral tibiofemoral compartment as well (arrowheads)
A common pitfall is to inadvertently inject one of the fat pads instead of the joint [9, 10, 16, 65]. If using the patellofemoral approach, it is common for a misdirected needle to inject contrast into the prefemoral fat, suprapatellar fat, or recess, or into the periarticular subcutaneous tissues (Fig. 13). If this occurs, the needle should either be pulled back or advanced a few mm respectively and contrast re-injected. If using the anterior approach, contrast can be injected inadvertently into the fat of the trochlear notch. If this occurs, the needle should be withdrawn and then redirected toward the femoral condyle.
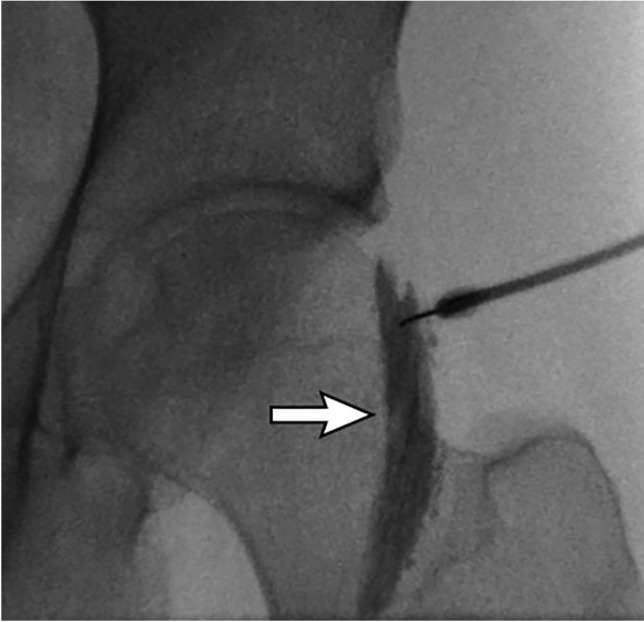
Fig. 13.
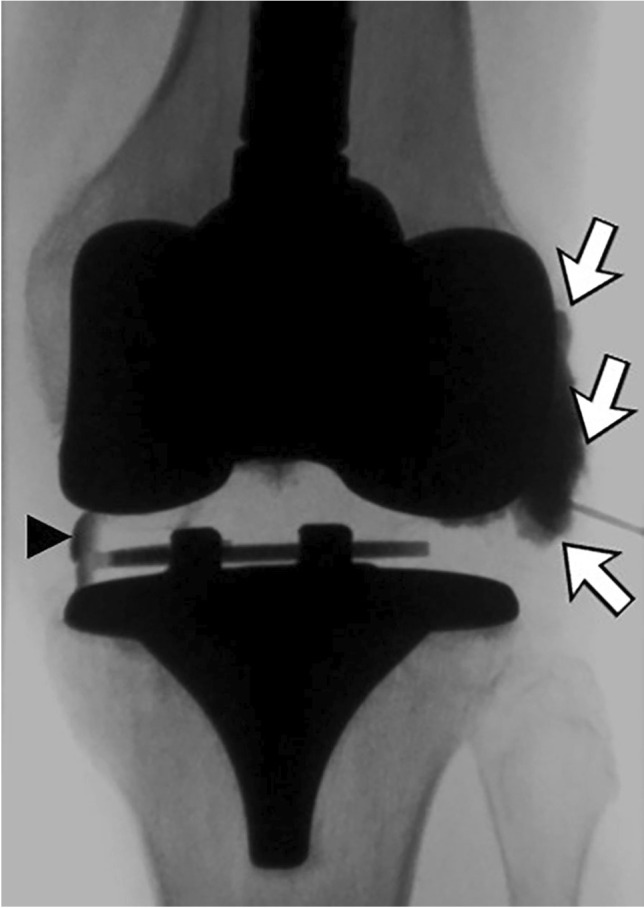
A 63-year-old female with painful total knee arthroplasty, presenting for aspiration. Initial aspiration attempts using the lateral approach yielded no fluid. Initial fluoroscopic spot image showed pooling of the contrast in the lateral periarticular soft tissues (arrows). The needle was repositioned and advanced deep to the patella. Subsequent contrast injection shows contrast outlining the medial aspect of the polyethylene liner (arrowhead), having crossed the midline, indicating intraarticular needle position
Patellofemoral approach: lateral and medial
Both the lateral and medial approaches may use manual patellar displacement toward the side of needle entry (Figs. 10 and 11) [9]. The patient may be placed supine or decubitus. In the supine position, the knee is supported on a cushion and flexed 30° [9]. The patella is manually subluxated toward the side of needle entry, and the needle is advanced parallel to the table into the patellofemoral joint from either a lateral or medial approach [9]. The lateral patellofemoral approach is preferred in the supine position because the overlying soft tissues are thinner.
In the decubitus position, the needle is advanced perpendicular to the table. In the lateral approach, the patient lies in a contralateral decubitus position with the lateral side of the affected knee facing up. The needle is then placed vertically into the lateral patellofemoral compartment [9, 67]. In the medial approach, the patient lies in an ipsilateral decubitus position with the affected knee flexed and the medial side facing up. The needle is placed vertically into the patellofemoral joint [9, 67].
Care should be taken to avoid entering the far lower portion of the patellofemoral joint where Hoffa’s fat pad resides and the far upper portion of the patellofemoral joint where the suprapatellar fat pad resides [73]. The patellofemoral approach has several drawbacks. Manual subluxation of the knee by the operator can be difficult to do in native knees, and even more difficult to do in postoperative knees where there is scar tissue. Patients may find manual patellar subluxation uncomfortable. In the morbidly obese patient, it may be difficult to even palpate the patella. Lastly, the joint space with this approach is quite small, even in normal knees, and access is even more difficult in the presence of severe patellofemoral narrowing or large osteophytes [16].
Arthroscopic anterior approach
The patient is placed supine with the affected knee on a cushion in 30–90° of flexion. In one method, the needle entry is medial or lateral to the patellar tendon with the needle directed cranially to the underlying femoral notch [67, 74]. Alternately, the needle entry is medial or lateral parapatellar, at the joint line, over the medial or lateral tibia, with the needle directed cranially to the ipsilateral femoral condyle (Figs. 11 and 12) [67, 74].
In our experience, patients find this to be the most comfortable of all the approaches. We also find this approach easier to do and easier to teach. A theoretical drawback of this approach is inadvertent patellar tendon injection; however, the patellar tendon can usually be palpated, or its location inferred from the apex of the patella.
Knee arthroplasty
In the postoperative setting, most aspirations are performed to rule out PJI. A tourniquet or compression wrap can be used to push fluid from the suprapatellar recess inferior along the joint [68]. Any approach can be utilized for aspiration using an 18-G needle, but, in our experience, the anterior approach is technically easier to perform. Using a parapatellar approach, the needle is advanced cranially until it hits the femoral component and metal-on-metal sensation is felt. Intraarticular contrast injection will outline the polyethylene liners of the tibial and femoral components (Fig. 14).
Fig. 14.
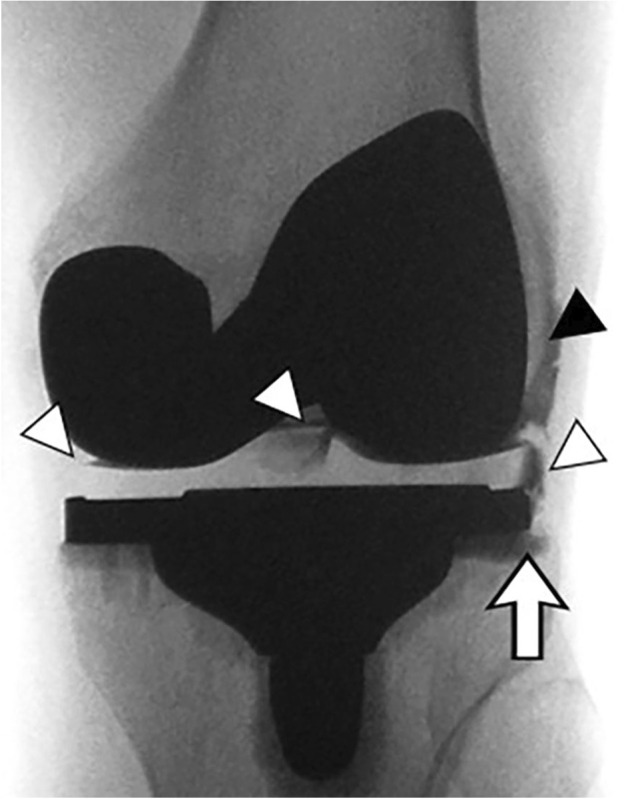
A 65-year-old female with painful total knee arthroplasty and suspected loosening. Fluoroscopic image after intraarticular contrast injection shows contrast outlining the polyethylene liner of the tibial tray (white arrowheads) and the lateral femoral condyle (black arrowhead). Contrast also extends into the metal-bone interface of the tibial tray (arrow) suggesting loosening of the prosthesis
Ankle joint
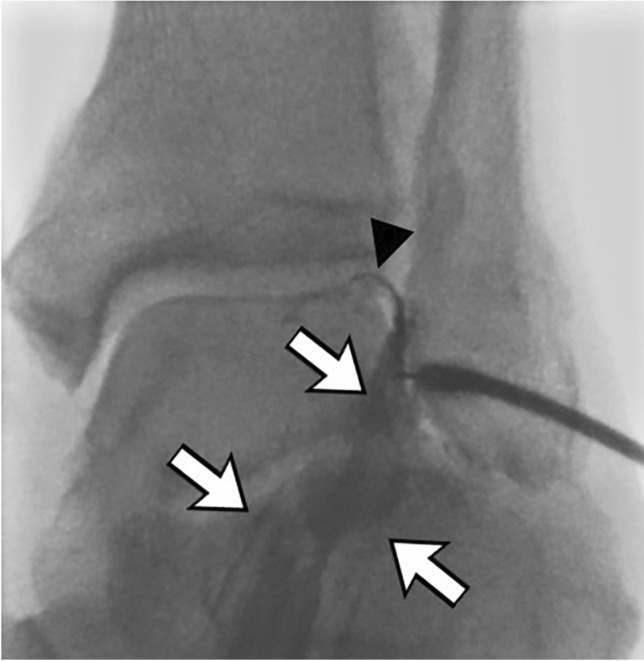
Tibiotalar joint injections are commonly performed for primary or post-traumatic OA or postoperative pain [16]. Tibiotalar MR or CT arthrography is helpful to assess for osteochondral injuries, intraarticular bodies, or ankle impingement. Aspiration is less commonly performed, with an estimated 9% of adult cases of SA involving the ankle joint [50]. Uncommon indications for aspiration include suspected inflammatory arthritis, hemarthrosis, and crystal arthropathy. Upon injection, contrast should disperse freely into the tibiotalar joint and recesses to signify intraarticular needle placement (Fig. 15) [3, 9]. The tibiotalar joint may communicate with the flexor hallucis longus tendon sheath in approximately 17% of people and the posterior subtalar joint in approximately 14% of people [12, 14]. Ankle joint approaches include anteromedial, anterolateral, medial, or lateral clear spaces, and posterolateral (Figs. 16, 17).
Fig. 15.
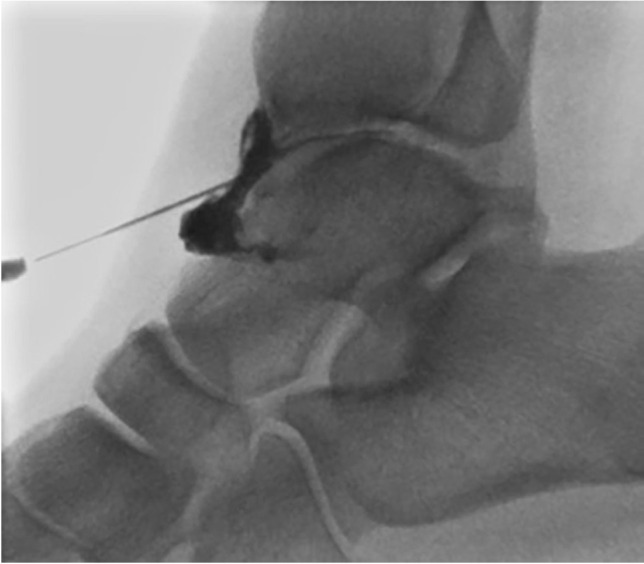
A 50-year-old male with posttraumatic OA of the ankle, referred for CSI. The spinal needle is angled from inferior to superior, targeting the talar dome. Contrast outlines the anterior recess and extends into the tibiotalar joint in a linear fashion
Fig. 16.
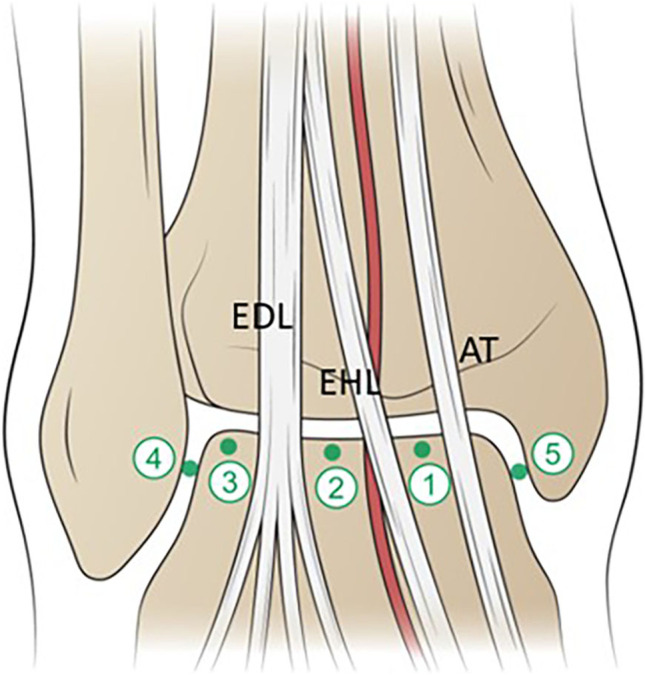
Illustration of ankle injection targets in the AP projection. 1 = Target is the medial talar dome between the AT and EHL tendons. 2 = Target is the central talar dome between the dorsalis pedis artery and the EDL tendons. 3 = Target is the lateral talar dome lateral to the EDL. 4 = Target is the upper half of the lateral clear space. 5 = Target is the upper half of the medial clear space. AT = anterior tibial tendon; EHL = extensor hallucis longus tendon; EDL = extensor digitorum longus tendons. Anterior tibial/dorsalis pedis artery is depicted in red
Fig. 17.
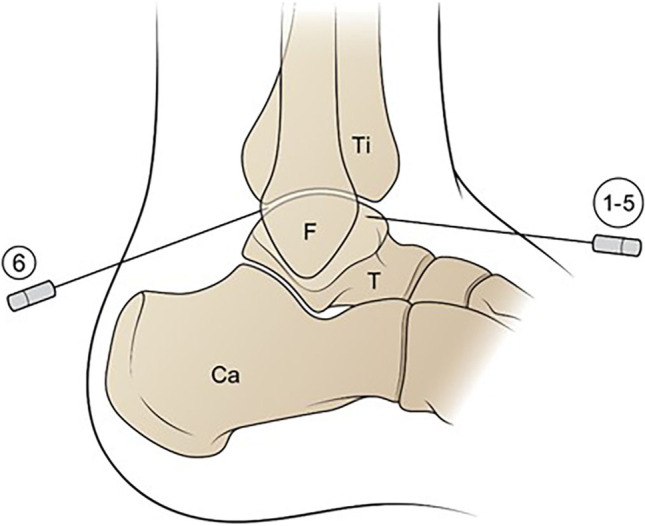
Illustration of ankle injection targets in the lateral projection. 1–5 = Anterior approach, angled from inferior to superior, targeting the talar dome or clear spaces; 6 = posterolateral approach with skin entry site 1 cm caudal to the posterior tibial plafond, medial to the fibula. Needle is directed anterosuperior to the posterior talus. Ti = tibia; F = fibula; T = talus; C = calcaneus
Anteromedial and anterolateral approaches
With the patient in the supine position, the leg extended, and the heel resting on the table, the extensor tendons are palpated and marked along with the tibialis anterior/dorsalis pedis artery, which runs along the lateral border of the extensor hallucis longus tendon (EHL) and medial to the extensor digitorum longus tendons (EDL) [1, 3, 9, 65, 75]. Using fluoroscopy to locate the ankle joint, one of several possible skin entry sites/targets may be chosen overlying the talar dome, just distal to the joint line: (1) medial to the EHL; (2) between the dorsalis pedis artery and the EDL (least used in our practice, to avoid the neurovascular bundle); or (3) lateral to the EDL (Fig. 16)[1, 3, 9, 75].
Once the skin entry site is marked, the patient is placed ipsilateral decubitus if the anteromedial approach is chosen, with the lateral aspect of the hindfoot supported on a foam block. If the anterolateral approach is chosen, then the patient is placed into the contralateral decubitus, with the medial hindfoot of the ankle of interest supported on a foam block [68]. In the lateral projection, the needle is placed at the selected skin entry site and directed from caudal to cranial, to the superomedial or superolateral talus to avoid the anterior lip of the distal tibia (Fig. 17) [3, 9].
Several pitfalls may be encountered when using one of the anterior approaches. If the needle is not advanced deeply enough, contrast may pool in the overlying subcutaneous tissues, obscuring the joint. If the needle is advanced in too steep a trajectory, the needle may hit the lip of the distal tibia. In this case, the needle should be withdrawn and redirected to land on the talar dome. If an anterior site is marked without direct palpation of the underlying tendons, then inadvertent tendon sheath injection may occur.
Medial or lateral clear space approaches
These approaches may be considered in cases of severe anterior tibiotalar narrowing or where there are large anterior osteophytes. In both cases, the patient lies supine with the heel on the table, with the foot in the mortise view position, in slight plantar flexion. An injection site may be marked at the upper half of the articulation of the medial malleolus and medial talar dome or at the upper half of the articulation between the lateral malleolus and lateral talar dome to avoid the ligaments and tendons (Fig. 18) [1, 76, 77]. Using the medial clear space approach, if the needle is placed too far medial, inadvertent injection of the greater saphenous vein may occur.
Fig. 18.
A 65-year-old male with ankle arthritis. Initial contrast injection using the lateral clear space approach shows contrast starting to fill the tibiotalar joint (arrowhead) but mainly opacifying the overlying extensor digitorum longus tendon sheath (arrows). Redirection of the needle slightly deeper resulted in successful opacification of the tibiotalar joint
Posterolateral approach
This approach is useful in cases when severe anterior tibiotalar narrowing and large anterior osteophytes preclude the anterior approach. The patient is placed in a contralateral decubitus position with the medial side of the affected foot supported on a foam block [78]. The posterior border of the lateral malleolus and the peroneal tendons are palpated and marked [78]. The skin entry site is marked 1 cm caudal to the posterior aspect of the tibial plafond and medial to the fibula; the needle is inserted and directed anterosuperior to the posterior talus (Fig. 17) [78]. A potential pitfall of this approach is the inadvertent injection of the peroneal tendon sheath (Fig. 19), or potential injury of the underlying sural nerve.
Fig. 19.
A 54-year-old female with ankle pain. The initial posterior approach (not shown) inadvertently opacified the peroneus tendon sheath (arrows). The needle was redirected into the tibiotalar joint, with successful joint opacification (arrowheads)
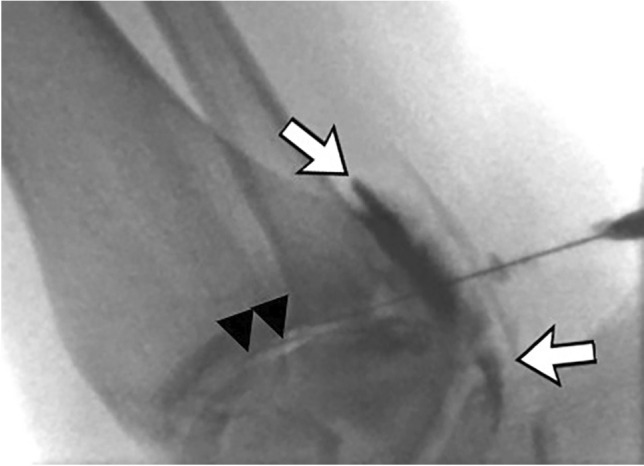
Posterior subtalar joint
Common indications for subtalar joint injections include sinus tarsi syndrome, tarsal coalition, primary or post-traumatic OA, and post-operative pain [16]. The subtalar joint is composed of three facets: anterior, middle, and posterior, with the posterior facet being the largest. The anterior and middle facets communicate with one another, the talonavicular joint, and spring ligament recess, but should not communicate with the posterior subtalar joint. The posterior subtalar joint communicates with the sinus tarsi (Fig. 20), and it may communicate with the tibiotalar joint in 14% of cases (Fig. 21) [3, 12]. Two main approaches to the posterior subtalar joint have been described, including the lateral and posterolateral approaches (Fig. 22). Contrast should flow freely along the subtalar joint to signify intraarticular needle placement [16].
Fig. 20.

A 56-year-old female with subtalar arthritis referred for CSI. Subtalar contrast injection extends posteriorly to the needle, outlining the subtalar joint, and extends anteriorly into the sinus tarsi (arrowhead)
Fig. 21.
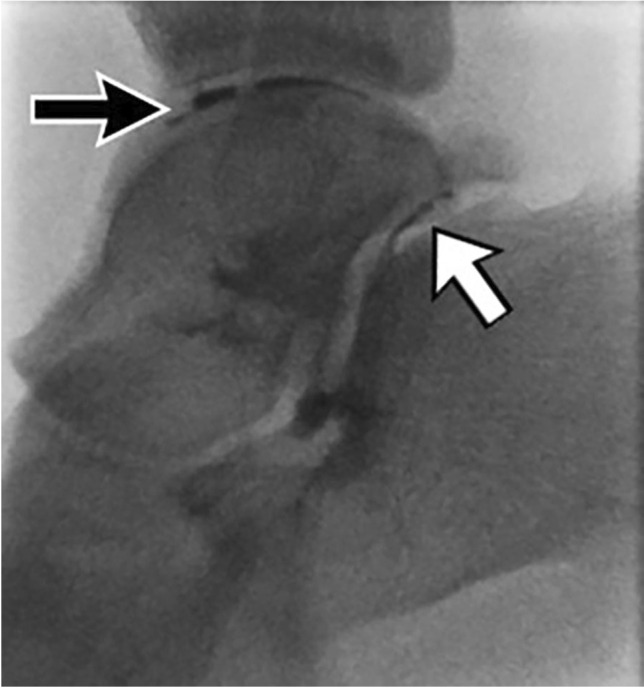
A 21-year-old male with ankle sprain and subtalar pain, referred for CSI. Contrast outlines the posterior subtalar joint (white arrow) and extends into the tibiotalar joint (black arrow)
Fig. 22.
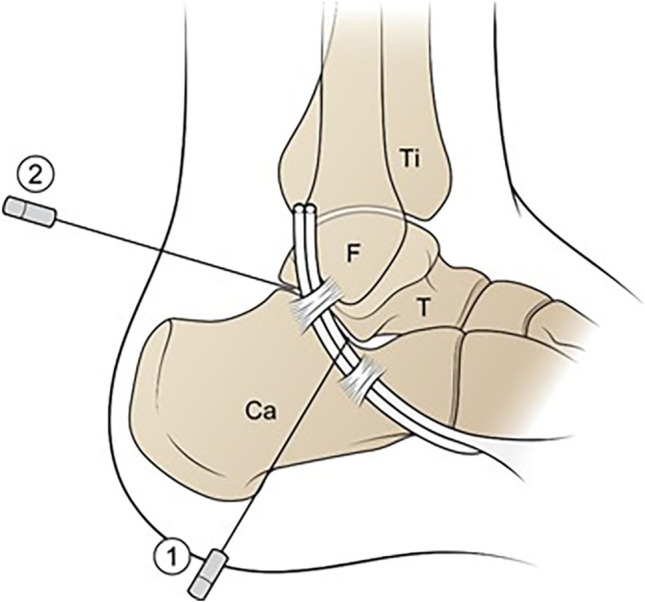
Illustration of the lateral ankle shows two approaches to the subtalar joint. 1 = Lateral approach. A lateral skin entry site is chosen inferior to the distal fibula but anterior to the peroneal tendons (outlined in white), entering the subtalar joint just posterior to the lateral talar process. 2 = Posterolateral approach. The needle enters the skin lateral to the Achilles tendon, targeting the central subtalar joint. Ti = tibia; F = fibula; T = talus; C = calcaneus
Lateral approach
This approach is performed with the patient in a contralateral decubitus position with the medial lower leg supported on a cushion, allowing gravity to invert the injected foot. A lateral needle entry site is chosen inferior to the fibula overlying the subtalar joint. The needle is advanced into the joint, anterior to the peroneal tendons, entering the subtalar joint just posterior to the angle of Gissane and the lateral talar process (Fig. 22) [3, 16]. There is typically no bony backstop to this approach, requiring a heightened awareness of subtle changes in tactile sensation from the operator to avoid going too deep prior to the test injection for confirmation of intraarticular access.
Posterolateral approach
This approach is performed with the patient in a contralateral decubitus position with the medial foot supported on a foam block. The skin overlying the posterior subtalar joint is marked just lateral to the Achilles tendon and the needle is inserted and directed from lateral to the central subtalar joint (Fig. 22) [79]. A potential drawback to this approach is the risk of sural nerve injury which lies in close to proximity to the expected needle trajectory.
Small joints of the foot
Pathology affecting the smaller joints of the foot mainly includes OA, inflammatory arthropathies, coalition, pes planovalgus alignment, hallux rigidus, hallux valgus, post-traumatic pain, and post-operative pain [16]. In the past 4 years, our institution has experienced a 15-fold increase in the number of referrals we receive specifically for anesthetic/steroid injections into the smaller joints of the foot, to either provide pain relief or to identify a specific pain generator in preoperative planning. The smaller articulations of the foot are performed with 25-G 1.5–0.5-inch needles. For the smallest joints, it is helpful to directly attach a 1-cc syringe to the needle, rather than syringe with intervening tubing, to diminish the risk of dislodging the needle when injecting. A dorsal approach is used for most of the foot joints, aiming the needle for the edges of the joint where the capsular recesses may be accessed, while avoiding the midline tendons (Fig. 23) [3]. For most smaller joints of the foot, unless specified, the patient is positioned supine with the knee flexed and the foot flat on the fluoroscopy table [3, 16]. The dorsalis pedis artery is palpated and marked prior to needle puncture [3]. To access the joints of the lateral column of the foot, including the calcaneocuboid and fourth-fifth tarsometatarsal (TMT) joints, the knee is slightly internally rotated, with the foot slightly obliqued (Fig. 24).
Fig. 23.
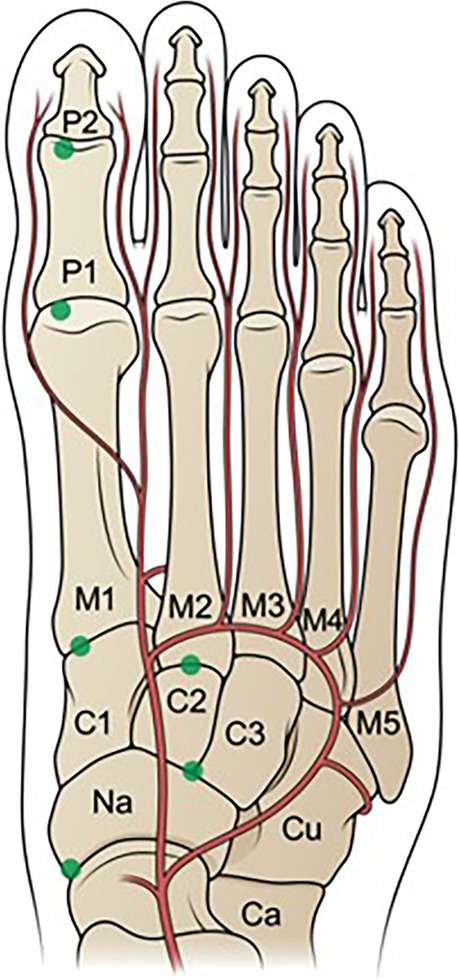
Illustration of the AP view of the foot, showing small joint targets in green, using the dorsal approach. Ca = calcaneus. Na = navicular. Cu = cuboid. C1 = medial cuneiform. C2 = middle cuneiform. C3 = lateral cuneiform. M1–M5 = metatarsals 1–5. P1 = proximal phalanx; P2 = distal phalanx of the great toe
Fig. 24.
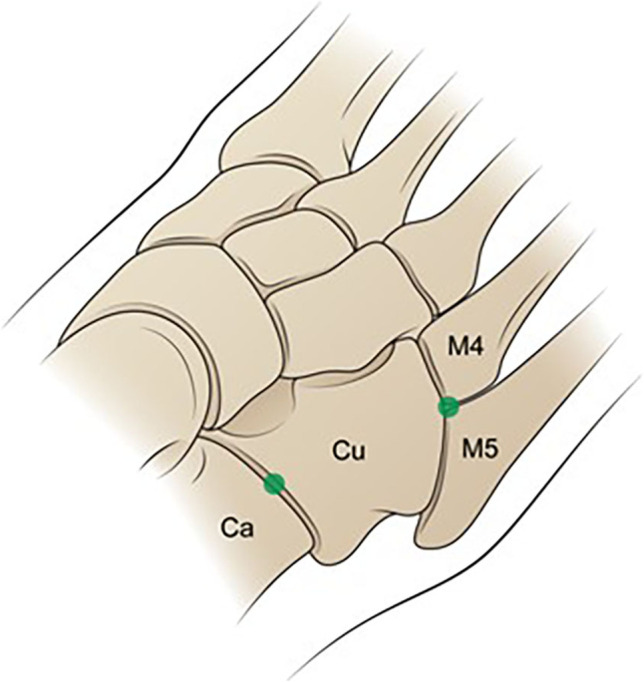
Illustration of the lateral oblique view of the foot, showing the lateral column joint targets with green dots. Ca = calcaneus. Cu = cuboid. M4, M5 = 4th and 5th metatarsals
For many of the smaller joints, tiny adjustments in the needle position can be made to allow the needle to slip between the bones, into the joint recess or directly onto the curved bone surfaces [3, 16]. Placing the needle too deeply into the joint may prevent free flow of injectate and retraction of the needle may be necessary [3, 16]. The smaller gauge needle tips may bend or be deflected if inserted too deeply. Contrast should flow freely among the small articulations to signify intraarticular needle placement. These joints often do not hold more than 1 cc and contrast can easily obscure the joint. Care should be first taken to confirm position with lidocaine prior to documentation with contrast [3].
Talonavicular joint
The talonavicular joint is also referred to as the talocalcaneonavicular joint. The talar head and navicular articulate with the anterior calcaneus medially (Fig. 25). The talonavicular joint also communicates with the anterior and middle subtalar joints and the spring ligament recess [3, 12]. The skin entry site is marked over the dorsomedial aspect of the talonavicular joint targeting the curved distal talus, which is usually the easiest part of the joint to access in the setting of OA [3, 16]. Contrast injection should outline the talonavicular joint but may initially also outline the anterior and middle subtalar joints, which can be disorienting for the unwary.
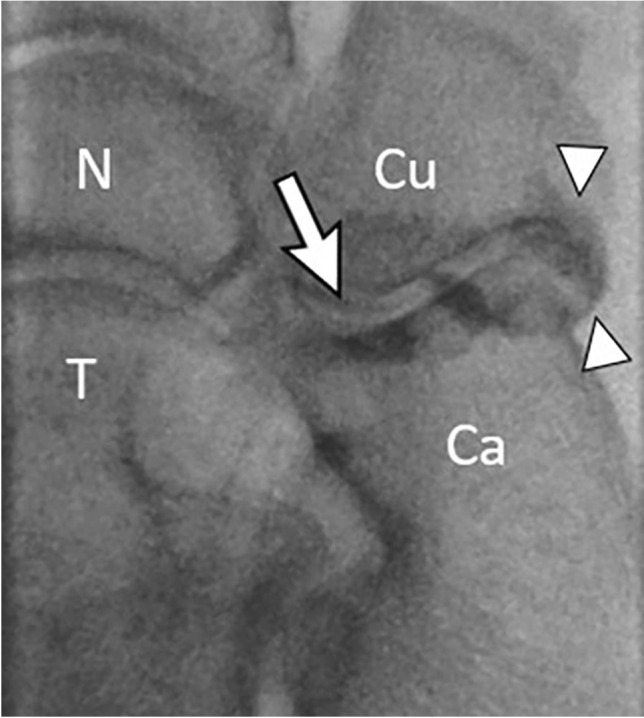
Fig. 25.
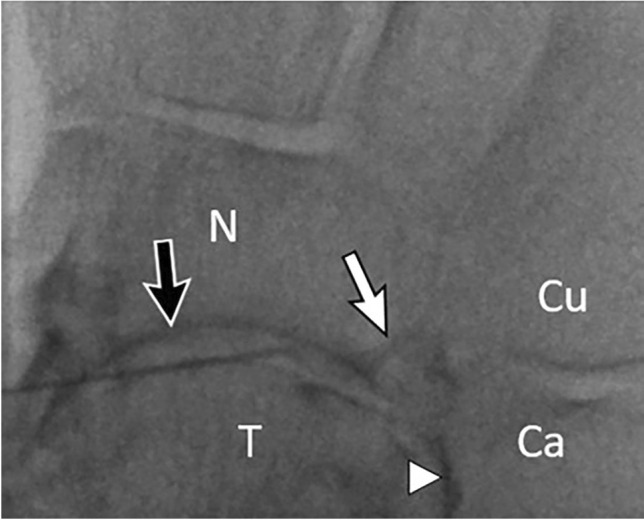
A 70-year-old female with history of tibiotalar fusion and midfoot pain, referred for talonavicular CSI. Fluoroscopic image shows contrast outlining the talonavicular joint (black arrow) and talocalcaneal joint (arrowhead). Contrast also outlines a calcaneal osteophyte at the calcaneonavicular articulation (white arrow). T = talus. N = navicular. Ca = calcaneus. Cu = cuboid
Calcaneocuboid joint
The calcaneocuboid joint is accessed with the foot slightly obliqued (Fig. 24) [3]. The joint has a prominent inferior recess, and the overlying peroneal tendons should be palpated, marked, and avoided by accessing the mid-portion of the joint in the craniocaudal dimension (Fig. 26) [3]. The calcaneocuboid joint communicates with the talonavicular joint in 42% of cases [12].
Fig. 26.
A 62-year-old female with pes planus, midfoot arthritis and severe calcaneocuboid (CC) joint pain, referred for CSI. Fluoroscopic image shows linear contrast within the CC joint (arrow) and dispersing into the inferior joint recess (arrowheads). T = talus. N = navicular. Ca = calcaneus. Cu = cuboid
Naviculocuneiform joint
The navicular articulates with all three cuneiforms via three facets; the joint is enclosed by a single capsule [3]. The naviculocuneiform joint also communicates with the second and third tarsometatarsal joints (TMTJ) via the medial and middle intercuneiform joints [3, 12, 16]. The usual approach is dorsal, targeting the Y-shaped articulation of the navicular, medial, and middle cuneiforms (Fig. 27) [3, 16].
Fig. 27.
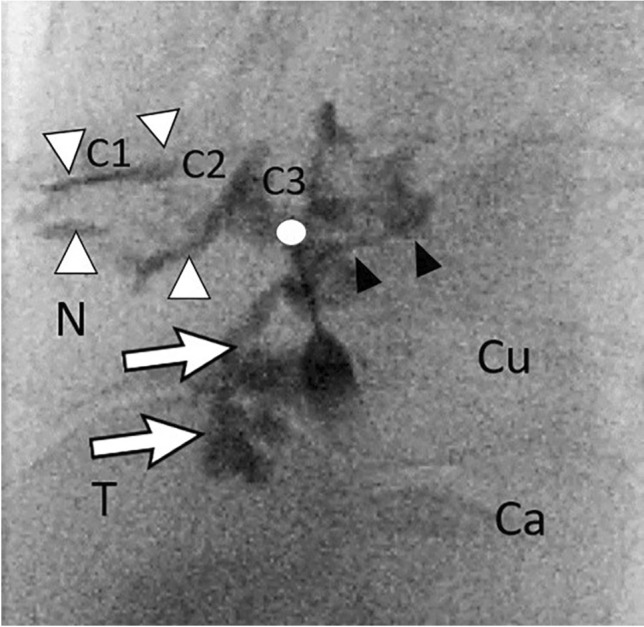
A 75-year-old female with history of multiple sprains and midfoot osteoarthritis, referred for naviculocuneiform (NC) CSI. Fluoroscopic image shows the needle targeting the lateral NC joint (circle), due to extensive osteophyte formation medially. As expected, contrast disperses into all three NC articulations and recesses (arrowheads). In addition, there is abnormal, unexpected contrast dispersal proximally into the talonavicular joint recess (arrows), and into the cuboid-lateral cuneiform joint (black arrows) due to prior capsular injury. In this case, the collimated image does not include the TMT joints, where we would expect to see normal extension of contrast into the 2nd and 3rd TMT joints. Lobulated filling defects imply synovitis. T = talus. N = navicular. Ca = calcaneus. Cu = cuboid. C1–C3 = medial, middle, and lateral cuneiforms, respectively
Tarsometatarsal joints
Three synovial spaces comprise the TMTJ: the medial cuneiform-first metatarsal base; the middle and lateral cuneiforms-second-third metatarsal bases; and the cuboid-fourth-fifth metatarsal bases [3, 16]. The needle should be placed at the dorsal aspects of the first-third TMTJ in the AP plane (Figs. 23 and 28) [3, 16]. For the fourth-fifth TMTJ, the patient is placed supine with the knee flexed, with the knee slightly internally rotated and the foot obliqued. The needle should be aimed obliquely into the T-shaped joint space between the fourth-fifth metatarsal bases and the cuboid (Fig. 24) [3, 16].
Fig. 28.

A 59-year-old female with midfoot pain, referred for 2nd and 3rd TMTJ CSI. Fluoroscopic image shows needle in the 3rd TMTJ with contrast outlining the 2nd and 3rd TMTJ. T = talus. N = navicular. Cu = cuboid. C1–C3 = medial, middle, and lateral cuneiforms, respectively. M1–M5 = 1st through 5th metatarsals, respectively
Metatarsophalangeal joints
In our experience, the majority of metatarsophalangeal (MPJ) injection requests involve the first MPJ since it is predisposed to the development of both OA and gout. The MPJ is comprised of the metatarsal head and proximal phalangeal base, with dorsal and plantar recesses. The first MPJ often communicates with the paired tibial and fibular hallux sesamoids that articulate with the plantar metatarsal head [3, 80]. The needle should enter dorsally off midline and proximal to the joint, to avoid the midline extensor tendon as well as the medial and lateral neurovascular bundles, targeting the curved surface of the metatarsal head, in an attempt to avoid the dorsal lip of the phalangeal base (Figs.23 and 29) [3, 16].
Fig. 29.

A 51-year-old female with residual pain after healed first proximal phalangeal fracture, referred for 1st MPJ CSI. The needle targets the head of the first metatarsal (M1), just lateral to midline, to avoid the extensor tendon. Contrast disperses from the needle, opacifying the joint. P1 = 1st proximal phalanx
Interphalangeal joints
The interphalangeal joints (IPJ) are located between phalanges. The needle should enter dorsally off midline and proximal to the joint to avoid the midline tendon, targeting the phalangeal head. Once osseous contact is made the needle can be walked further into the joint as needed [3]. Due to the IPJ’s small size and tenuous superficial location, a 0.5-inch, 25-G needle is most useful for accessing this joint.
Conclusion
The volume of lower extremity fluoroscopically guided injections continues to increase as the general population ages and seeks to remain active in older years. Fluoroscopy is an important imaging modality to guide efficient, safe, and accurate lower extremity procedures. The literature concerning the benefits and risks of injectables is constantly evolving, and it is important for the radiologist to stay up to date and follow best medical practices. Radiologists who perform fluoroscopically guided procedures should know various techniques to safely access each joint of the lower extremity. It is also important to understand the common pearls and pitfalls associated with each joint to help minimize complications, patient discomfort, and radiation exposure. Proficiency with this diverse skillset will allow the operator to provide both valuable diagnostic information to referring providers and welcomed therapeutic relief for patients which ideally results in an increased quality of life.
Acknowledgements
The authors thank Danielle Dobbs, medical illustrator, Michigan Medicine Radiology Media Services, for the illustrations in this paper.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Key points
• Fluoroscopy provides advantages over ultrasound for joint injections and aspirations.
• Injection of local anesthetic provides both pain relief and information regarding the source of pain.
• The risks and benefits of injected medications must be reviewed and discussed with patients prior to intervention.
• It is useful to know more than one approach to access each joint to tailor each procedure to the patient.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Gunjan Malhotra, Email: gunjanm@med.umich.edu.
Barry G. Hansford, Email: hansford@ohsu.edu
Cindy Felcher, Email: cfelcher@med.umich.edu.
Kristie A. Wuerfel, Email: wuerfeka@med.umich.edu
Corrie M. Yablon, Email: cyablon@med.umich.edu
References
- 1.Rastogi AK, Davis KW, Ross A, Rosas HG. Fundamentals of joint injection. AJR Am J Roentgenol. 2016;207(3):484–494. doi: 10.2214/AJR.16.16243. [DOI] [PubMed] [Google Scholar]
- 2.Yablon CM, Wu JS, Newman LR, Downie BK, Hochman MG, Eisenberg RL. A needs assessment of musculoskeletal fellowship training: a survey of practicing musculoskeletal radiologists. AJR Am J Roentgenol. 2013;200(4):732–740. doi: 10.2214/AJR.12.9105. [DOI] [PubMed] [Google Scholar]
- 3.Hansford BG, Mills MK, Hanrahan CJ, Yablon CM. Pearls and pitfalls of fluoroscopic-guided foot and ankle injections: what the radiologist needs to know. Skeletal Radiol. 2019;48(11):1661–1674. doi: 10.1007/s00256-019-03226-9. [DOI] [PubMed] [Google Scholar]
- 4.Radvany MG, Mahesh M. Last series hold: a feature on fluoroscopy systems with the potential to reduce patient and operator dose. J Am Coll Radiol. 2015;12(8):860–861. doi: 10.1016/j.jacr.2015.04.022. [DOI] [PubMed] [Google Scholar]
- 5.MacMahon PJ, Eustace SJ, Kavanagh EC. Injectable corticosteroid and local anesthetic preparations: a review for radiologists. Radiology. 2009;252(3):647–661. doi: 10.1148/radiol.2523081929. [DOI] [PubMed] [Google Scholar]
- 6.Hadduck TA, van Holsbeeck MT, Girish G, Dong Q, Morag Y, Jacobson JA, et al. Value of ultrasound before joint aspiration. AJR Am J Roentgenol. 2013;201(3):W453–W459. doi: 10.2214/AJR.12.9177. [DOI] [PubMed] [Google Scholar]
- 7.Graf DN, Thallinger A, Zubler V, Sutter R. Intraarticular Steroid injection in hip and knee with fluoroscopic guidance: reassessing safety. Radiology 2022;304(2):363–369. [DOI] [PubMed]
- 8.Guermazi A, Neogi T, Katz JN, Kwoh CK, Conaghan PG, Felson DT, et al. Intra-articular corticosteroid injections for the treatment of hip and knee osteoarthritis-related pain: considerations and controversies with a focus on imaging-radiology scientific expert panel. Radiology. 2020;297(3):503–512. doi: 10.1148/radiol.2020200771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hansford BG, Stacy GS. Musculoskeletal aspiration procedures. Semin Intervent Radiol. 2012;29(4):270–285. doi: 10.1055/s-0032-1330061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peterson JJ, Bancroft LW. History of arthrography. Radiol Clin North Am. 2009;47(3):373–386. doi: 10.1016/j.rcl.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Peterson CK, Buck F, Pfirrmann CW, Zanetti M, Hodler J. Fluoroscopically guided diagnostic and therapeutic injections into foot articulations: report of short-term patient responses and comparison of outcomes between various injection sites. AJR Am J Roentgenol. 2011;197(4):949–953. doi: 10.2214/AJR.10.5364. [DOI] [PubMed] [Google Scholar]
- 12.Carmont MR, Tomlinson JE, Blundell C, Davies MB, Moore DJ. Variability of joint communications in the foot and ankle demonstrated by contrast-enhanced diagnostic injections. Foot Ankle Int. 2009;30(5):439–442. doi: 10.3113/FAI-2009-0439. [DOI] [PubMed] [Google Scholar]
- 13.Corvino A, Venetucci P, Caruso M, Tarulli FR, Carpiniello M, Pane F, et al. Iliopsoas bursitis: the role of diagnostic imaging in detection, differential diagnosis and treatment. Radiol Case Rep. 2020;15(11):2149–2152. doi: 10.1016/j.radcr.2020.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Na JB, Bergman AG, Oloff LM, Beaulieu CF. The flexor hallucis longus: tenographic technique and correlation of imaging findings with surgery in 39 ankles. Radiology. 2005;236(3):974–982. doi: 10.1148/radiol.2362040835. [DOI] [PubMed] [Google Scholar]
- 15.Porrino J, Richardson ML, Flaherty E, Albahhar M, Ha AS, Mulcahy H, et al. Septic arthritis and joint aspiration: the radiologistʼs role in image-guided aspiration for suspected septic arthritis. Semin Roentgenol. 2019;54(2):177–189. doi: 10.1053/j.ro.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 16.Raythatha M, Spitz D, Tang JY. Fluoroscopically-guided Joint and Bursa injection techniques: a comprehensive primer. Semin Roentgenol. 2019;54(2):124–148. doi: 10.1053/j.ro.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Breu A, Rosenmeier K, Kujat R, Angele P, Zink W. The cytotoxicity of bupivacaine, ropivacaine, and mepivacaine on human chondrocytes and cartilage. Anesth Analg. 2013;117(2):514–522. doi: 10.1213/ANE.0b013e31829481ed. [DOI] [PubMed] [Google Scholar]
- 18.Steverink JG, Piluso S, Malda J, Verlaan JJ. Comparison of in vitro and in vivo Toxicity of bupivacaine in musculoskeletal applications. Front Pain Res (Lausanne) 2021;2:723883. doi: 10.3389/fpain.2021.723883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harmatz A. Local anesthetics: uses and toxicities. Surg Clin North Am. 2009;89(3):587–598. doi: 10.1016/j.suc.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 20.Peterson C, Hodler J. Adverse events from diagnostic and therapeutic joint injections: a literature review. Skeletal Radiol. 2011;40(1):5–12. doi: 10.1007/s00256-009-0839-y. [DOI] [PubMed] [Google Scholar]
- 21.Gvozdenovic E, Dirven L, van den Broek M, Han KH, Molenaar ET, Landewe RB, et al. Intra articular injection with corticosteroids in patients with recent onset rheumatoid arthritis: subanalyses from the BeSt study. Clin Rheumatol. 2014;33(2):263–267. doi: 10.1007/s10067-013-2465-2. [DOI] [PubMed] [Google Scholar]
- 22.Kompel AJ, Roemer FW, Murakami AM, Diaz LE, Crema MD, Guermazi A. Intra-articular Corticosteroid Injections in the Hip and Knee: Perhaps Not as Safe as We Thought? Radiology. 2019;293(3):656–663. doi: 10.1148/radiol.2019190341. [DOI] [PubMed] [Google Scholar]
- 23.Simeone FJ, Vicentini JRT, Bredella MA, Chang CY. Are patients more likely to have hip osteoarthritis progression and femoral head collapse after hip steroid/anesthetic injections? A retrospective observational study. Skeletal Radiol. 2019;48(9):1417–1426. doi: 10.1007/s00256-019-03189-x. [DOI] [PubMed] [Google Scholar]
- 24.Boutin RD, Pai J, Meehan JP, Newman JS, Yao L. Rapidly progressive idiopathic arthritis of the hip: incidence and risk factors in a controlled cohort study of 1471 patients after intra-articular corticosteroid injection. Skeletal Radiol. 2021;50(12):2449–2457. doi: 10.1007/s00256-021-03815-7. [DOI] [PubMed] [Google Scholar]
- 25.McAlindon TE, LaValley MP, Harvey WF, Price LL, Driban JB, Zhang M, et al. Effect of intra-articular triamcinolone vs saline on knee cartilage volume and pain in patients with knee osteoarthritis: a randomized clinical trial. JAMA. 2017;317(19):1967–1975. doi: 10.1001/jama.2017.5283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aspenberg P. Drugs and fracture repair. Acta Orthop. 2005;76(6):741–748. doi: 10.1080/17453670510045318. [DOI] [PubMed] [Google Scholar]
- 27.Kondo T, Kitazawa R, Yamaguchi A, Kitazawa S. Dexamethasone promotes osteoclastogenesis by inhibiting osteoprotegerin through multiple levels. J Cell Biochem. 2008;103(1):335–345. doi: 10.1002/jcb.21414. [DOI] [PubMed] [Google Scholar]
- 28.Pountos I, Georgouli T, Blokhuis TJ, Pape HC, Giannoudis PV. Pharmacological agents and impairment of fracture healing: what is the evidence? Injury. 2008;39(4):384–394. doi: 10.1016/j.injury.2007.10.035. [DOI] [PubMed] [Google Scholar]
- 29.Karsh J, Yang WH. An anaphylactic reaction to intra-articular triamcinolone: a case report and review of the literature. Ann Allergy Asthma Immunol. 2003;90(2):254–258. doi: 10.1016/S1081-1206(10)62151-5. [DOI] [PubMed] [Google Scholar]
- 30.Vatti RR, Ali F, Teuber S, Chang C, Gershwin ME. Hypersensitivity reactions to corticosteroids. Clin Rev Allergy Immunol. 2014;47(1):26–37. doi: 10.1007/s12016-013-8365-z. [DOI] [PubMed] [Google Scholar]
- 31.Cassidy JT, Bole GG. Cutaneous atrophy secondary to intra-articular corticosteroid administration. Ann Intern Med. 1966;65(5):1008–1018. doi: 10.7326/0003-4819-65-5-1008. [DOI] [PubMed] [Google Scholar]
- 32.Rogojan C, Hetland ML. Depigmentation–a rare side effect to intra-articular glucocorticoid treatment. Clin Rheumatol. 2004;23(4):373–375. doi: 10.1007/s10067-004-0905-8. [DOI] [PubMed] [Google Scholar]
- 33.Holland C, Jaeger L, Smentkowski U, Weber B, Otto C. Septic and aseptic complications of corticosteroid injections: an assessment of 278 cases reviewed by expert commissions and mediation boards from 2005 to 2009. Dtsch Arztebl Int. 2012;109(24):425–430. doi: 10.3238/arztebl.2012.0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kijowski R. Risks and Benefits of intra-articular corticosteroid injection for treatment of osteoarthritis: what radiologists and patients need to know. Radiology. 2019;293(3):664–665. doi: 10.1148/radiol.2019192034. [DOI] [PubMed] [Google Scholar]
- 35.Cushman DM, Teramoto M, Asay A, Clements ND, McCormick ZL. Corticosteroid and local anesthetic use trends for large joint and bursa injections: results of a survey of sports medicine physicians. PM R. 2021;13(9):962–968. doi: 10.1002/pmrj.12499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.AAOS. Timing of musculoskeletal cortisone injections and COVID vaccine administration 2021 [updated 03/09/2021. Available from: https://www.aaos.org/about/covid-19-information-for-our-members/guidance-for-elective-surgery/timing-of-musculoskeletal-cortisone-injections-and-covid-vaccine-administration/. Date accessed: 24 June 2022.
- 37.Newberg AH, Munn CS, Robbins AH. Complications of arthrography. Radiology. 1985;155(3):605–606. doi: 10.1148/radiology.155.3.4001360. [DOI] [PubMed] [Google Scholar]
- 38.Hugo PC, 3rd, Newberg AH, Newman JS, Wetzner SM. Complications of arthrography. Semin Musculoskelet Radiol. 1998;2(4):345–348. doi: 10.1055/s-2008-1080115. [DOI] [PubMed] [Google Scholar]
- 39.Costello RF, Beall DP, Van Zandt BL, Stapp AM, Martin HD, Steury SW. Contrast reaction from hip arthrogram. Emerg Radiol. 2007;14(1):59–61. doi: 10.1007/s10140-006-0567-8. [DOI] [PubMed] [Google Scholar]
- 40.Bruins MJ, Zwiers JH, Verheyen CC, Wolfhagen MJ. In vitro study of the antimicrobial effects of radiological contrast agents used in arthrography. J Bone Joint Surg Br. 2011;93(1):126–130. doi: 10.1302/0301-620X.93B1.24968. [DOI] [PubMed] [Google Scholar]
- 41.Rhee RB, Chan KK, Lieu JG, Kim BS, Steinbach LS. MR and CT arthrography of the shoulder. Semin Musculoskelet Radiol. 2012;16(1):3–14. doi: 10.1055/s-0032-1304297. [DOI] [PubMed] [Google Scholar]
- 42.Brown RR, Clarke DW, Daffner RH. Is a mixture of gadolinium and iodinated contrast material safe during MR arthrography? AJR Am J Roentgenol. 2000;175(4):1087–1090. doi: 10.2214/ajr.175.4.1751087. [DOI] [PubMed] [Google Scholar]
- 43.Kurra C, Harmon TS, Taylor K, Utz J, Hernandez M, Matteo J, et al. The dark side of gadolinium: a study of arthrographic contrast at extreme concentrations. Cureus. 2019;11(10):e6006. doi: 10.7759/cureus.6006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McDonald RJ, Levine D, Weinreb J, Kanal E, Davenport MS, Ellis JH, et al. Gadolinium retention: a research roadmap from the 2018 NIH/ACR/RSNA Workshop on Gadolinium Chelates. Radiology. 2018;289(2):517–534. doi: 10.1148/radiol.2018181151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ringler MD, Rhodes NG, Ayers-Ringler JR, Jakaitis DR, McDonald RJ, Kallmes DF, et al. Gadolinium retention within multiple rat organs after intra-articular administration of gadolinium-based contrast agents. Skeletal Radiol. 2021;50(7):1419–1425. doi: 10.1007/s00256-020-03695-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roerdink RL, Huijbregts H, van Lieshout AWT, Dietvorst M, van der Zwaard BC. The difference between native septic arthritis and prosthetic joint infections: a review of literature. J Orthop Surg (Hong Kong) 2019;27(2):2309499019860468. doi: 10.1177/2309499019860468. [DOI] [PubMed] [Google Scholar]
- 47.Baran S, Price C, Hak DJ. Diagnosing joint infections: synovial fluid differential is more sensitive than white blood cell count. Eur J Orthop Surg Traumatol. 2014;24(8):1469–1474. doi: 10.1007/s00590-013-1331-x. [DOI] [PubMed] [Google Scholar]
- 48.Chan BY, Crawford AM, Kobes PH, Allen H, Leake RL, Hanrahan CJ, et al. Septic arthritis: an evidence-based review of diagnosis and image-guided aspiration. AJR Am J Roentgenol. 2020;215(3):568–581. doi: 10.2214/AJR.20.22773. [DOI] [PubMed] [Google Scholar]
- 49.Lauper N, Davat M, Gjika E, Muller C, Belaieff W, Pittet D, et al. Native septic arthritis is not an immediate surgical emergency. J Infect. 2018;77(1):47–53. doi: 10.1016/j.jinf.2018.02.015. [DOI] [PubMed] [Google Scholar]
- 50.Ross JJ. Septic Arthritis of Native Joints. Infect Dis Clin North Am. 2017;31(2):203–218. doi: 10.1016/j.idc.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 51.Kung JW, Yablon C, Huang ES, Hennessey H, Wu JS. Clinical and radiologic predictive factors of septic hip arthritis. AJR Am J Roentgenol. 2012;199(4):868–872. doi: 10.2214/AJR.10.6273. [DOI] [PubMed] [Google Scholar]
- 52.Graif M, Schweitzer ME, Deely D, Matteucci T. The septic versus nonseptic inflamed joint: MRI characteristics. Skeletal Radiol. 1999;28(11):616–620. doi: 10.1007/s002560050562. [DOI] [PubMed] [Google Scholar]
- 53.Johnson SM, Saint John BE, Dine AP. Local anesthetics as antimicrobial agents: a review. Surg Infect (Larchmt) 2008;9(2):205–213. doi: 10.1089/sur.2007.036. [DOI] [PubMed] [Google Scholar]
- 54.Heckmann ND, Nahhas CR, Yang J, Della Valle CJ, Yi PH, Culvern CN, et al. Saline lavage after a "dry tap". Bone Joint J. 2020;102-B(6_Supple_A):138–44. doi: 10.1302/0301-620X.102B6.BJJ-2019-1679.R1. [DOI] [PubMed] [Google Scholar]
- 55.Partridge DG, Winnard C, Townsend R, Cooper R, Stockley I. Joint aspiration, including culture of reaspirated saline after a 'dry tap', is sensitive and specific for the diagnosis of hip and knee prosthetic joint infection. Bone Joint J. 2018;100-B(6):749–54. doi: 10.1302/0301-620X.100B6.BJJ-2017-0970.R2. [DOI] [PubMed] [Google Scholar]
- 56.Newman JM, George J, Klika AK, Hatem SF, Barsoum WK, Trevor North W, et al. What is the diagnostic accuracy of aspirations performed on hips with antibiotic cement spacers? Clin Orthop Relat Res. 2017;475(1):204–211. doi: 10.1007/s11999-016-5093-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Serfaty A, Jacobs A, Gyftopoulos S, Samim M. Likelihood of hip infection with image-guided hip aspiration dry tap: a 10-year retrospective study. Skeletal Radiol. 2022. Online ahead of print. [DOI] [PubMed]
- 58.Shahid M, Shyamsundar S, Bali N, McBryde C, O'Hara J, Bache E. Efficacy of using an air arthrogram for EUA and injection of the hip joint in adults. J Orthop. 2014;11(3):132–135. doi: 10.1016/j.jor.2014.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kanthawang T, Bodden J, Joseph GB, Vail T, Ward D, Patel R, et al. Diagnostic value of fluoroscopy-guided hip aspiration for periprosthetic joint infection. Skeletal Radiol. 2021;50(11):2245–2254. doi: 10.1007/s00256-021-03795-8. [DOI] [PubMed] [Google Scholar]
- 60.Boyle KK, Wood S, Tarity TD. Low-virulence organisms and periprosthetic joint infection-biofilm considerations of these organisms. Curr Rev Musculoskelet Med. 2018;11(3):409–419. doi: 10.1007/s12178-018-9503-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev. 2014;27(2):302–345. doi: 10.1128/CMR.00111-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Foremny GB, Pretell-Mazzini J, Jose J, Subhawong TK. Risk of bleeding associated with interventional musculoskeletal radiology procedures. A comprehensive review of the literature. Skeletal Radiol. 2015;44(5):619–27. doi: 10.1007/s00256-014-2065-5. [DOI] [PubMed] [Google Scholar]
- 63.Shif Y, Kung JW, McMahon CJ, Mhuircheartaigh JN, Lin YC, Anderson ME, et al. Safety of omitting routine bleeding tests prior to image-guided musculoskeletal core needle biopsy. Skeletal Radiol. 2018;47(2):215–221. doi: 10.1007/s00256-017-2784-5. [DOI] [PubMed] [Google Scholar]
- 64.Thumboo J, O'Duffy JD. A prospective study of the safety of joint and soft tissue aspirations and injections in patients taking warfarin sodium. Arthritis Rheum. 1998;41(4):736–739. doi: 10.1002/1529-0131(199804)41:4<736::AID-ART23>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 65.Lungu E, Moser TP. A practical guide for performing arthrography under fluoroscopic or ultrasound guidance. Insights Imaging. 2015;6(6):601–610. doi: 10.1007/s13244-015-0442-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Magerkurth O, Jacobson JA, Girish G, Brigido MK, Bedi A, Fessell D. Paralabral cysts in the hip joint: findings at MR arthrography. Skeletal Radiol. 2012;41(10):1279–1285. doi: 10.1007/s00256-012-1395-4. [DOI] [PubMed] [Google Scholar]
- 67.Shortt CP, Morrison WB, Roberts CC, Deely DM, Gopez AG, Zoga AC. Shoulder, hip, and knee arthrography needle placement using fluoroscopic guidance: practice patterns of musculoskeletal radiologists in North America. Skeletal Radiol. 2009;38(4):377–385. doi: 10.1007/s00256-009-0648-3. [DOI] [PubMed] [Google Scholar]
- 68.Lin HM, Learch TJ, White EA, Gottsegen CJ. Emergency joint aspiration: a guide for radiologists on call. Radiographics. 2009;29(4):1139–1158. doi: 10.1148/rg.294085032. [DOI] [PubMed] [Google Scholar]
- 69.Duc SR, Hodler J, Schmid MR, Zanetti M, Mengiardi B, Dora C, et al. Prospective evaluation of two different injection techniques for MR arthrography of the hip. Eur Radiol. 2006;16(2):473–478. doi: 10.1007/s00330-005-2865-z. [DOI] [PubMed] [Google Scholar]
- 70.Llopis E, Fernandez E, Cerezal L. MR and CT arthrography of the hip. Semin Musculoskelet Radiol. 2012;16(1):42–56. doi: 10.1055/s-0032-1304300. [DOI] [PubMed] [Google Scholar]
- 71.Leopold SS, Battista V, Oliverio JA. Safety and efficacy of intraarticular hip injection using anatomic landmarks. Clin Orthop Relat Res. 2001;391:192–197. doi: 10.1097/00003086-200110000-00021. [DOI] [PubMed] [Google Scholar]
- 72.Yasar E, Singh JR, Hill J, Akuthota V. Image-guided injections of the hip. J Nov Physiother Phys Rehabil. 2014;1(1):039–48. [Google Scholar]
- 73.Zurlo JV, Towers JD, Golla S. Anterior approach for knee arthrography. Skeletal Radiol. 2001;30(6):354–356. doi: 10.1007/s002560100363. [DOI] [PubMed] [Google Scholar]
- 74.Moser T, Moussaoui A, Dupuis M, Douzal V, Dosch JC. Anterior approach for knee arthrography: tolerance evaluation and comparison of two routes. Radiology. 2008;246(1):193–197. doi: 10.1148/radiol.2461070045. [DOI] [PubMed] [Google Scholar]
- 75.Newman JS. Diagnostic and therapeutic injections of the foot and ankle. Semin Roentgenol. 2004;39(1):85–94. doi: 10.1016/j.ro.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 76.Fox MG, Wright PR, Alford B, Patrie JT, Anderson MW. Lateral mortise approach for therapeutic ankle injection: an alternative to the anteromedial approach. AJR Am J Roentgenol. 2013;200(5):1096–1100. doi: 10.2214/AJR.12.9227. [DOI] [PubMed] [Google Scholar]
- 77.Cerezal L, Llopis E, Canga A, Rolon A. MR arthrography of the ankle: indications and technique. Radiol Clin North Am. 2008;46(6):973–94, v. [DOI] [PubMed]
- 78.Varenika V, Harter J, Chu E, Steinbach L. The posterolateral approach for fluoroscopy-guided tibiotalar joint injection. Skeletal Radiol. 2017;46(8):1113–1115. doi: 10.1007/s00256-017-2650-5. [DOI] [PubMed] [Google Scholar]
- 79.Buck FM, Pfirrmann CW, Brunner F, Hodler J, Peterson C. The posterolateral fluoroscopy-guided injection technique into the posterior subtalar joint: description of the procedure and pilot study on patient outcomes. Skeletal Radiol. 2012;41(6):699–705. doi: 10.1007/s00256-011-1278-0. [DOI] [PubMed] [Google Scholar]
- 80.Nwawka OK, Hayashi D, Diaz LE, Goud AR, Arndt WF, 3rd, Roemer FW, et al. Sesamoids and accessory ossicles of the foot: anatomical variability and related pathology. Insights Imaging. 2013;4(5):581–593. doi: 10.1007/s13244-013-0277-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


