Abstract
Beyond the absolute and indisputable relevance and efficacy of anti-SARS-CoV-2 vaccines, the rapid transmission, the severity of infection, the absence of the protection on immunocompromised patients, the propagation of variants, the onset of infection and/or disease in vaccinated subjects and the lack of availability of worldwide vaccination require additional antiviral treatments. Since 1987, lactoferrin (Lf) is well-known to possess an antiviral activity related to its physico-chemical properties and to its ability to bind to both heparan sulfate proteoglycans (HSPGs) of host cells and/or surface components of viral particles. In the present review, we summarize in vitro and in vivo studies concerning the efficacy of Lf against DNA, RNA, enveloped and non-enveloped viruses. Recent studies have revealed that the in vitro antiviral activity of Lf is also extendable to SARS-CoV-2. In vivo, Lf oral administration in early stage of SARS-CoV-2 infection counteracts COVID-19 pathogenesis. In particular, the effect of Lf on SARS-CoV-2 entry, inflammatory homeostasis, iron dysregulation, iron-proteins synthesis, reactive oxygen formation, oxidative stress, gut-lung axis regulation as well as on RNA negativization, and coagulation/fibrinolysis balance will be critically reviewed. Moreover, the molecular mechanisms underneath, including the Lf binding to HSPGs and spike glycoprotein, will be disclosed and discussed. Taken together, present data not only support the application of the oral administration of Lf alone in asymptomatic COVID-19 patients or as adjuvant of standard of care practice in symptomatic ones but also constitute the basis for enriching the limited literature on Lf effectiveness for COVID-19 treatment.
Keywords: Lactoferrin, SARS-CoV-2, COVID-19, Inflammatory and iron homeostasis, Gut-lung axis, Coagulation and fibrinolysis
Lactoferrin and iron
Lactoferrin (Lf), identified in 1939 in bovine milk and isolated in 1960 from both human (Johansson 1960; Montreuil et al. 1960) and bovine milk (Groves 1960), is constitutively synthesized by exocrine glands and secreted in human fluids. After induction, Lf is also found in the granules of neutrophils in infection and inflammation sites.
Human Lf (hLf) and bovine Lf (bLf) are constituted of 691 and 689 amino acid residues, respectively. HLf and bLf, belonging to the transferrin family, are capable to reversibly chelate two Fe(III) per molecule with high affinity (Kd ~ 10–20 M), retaining ferric iron until pH values as low as 3.0. Differently from Lfs, transferrin (Tf) retains iron until pH values around 5.5 (Rosa et al. 2017). Both Lfs are folded into homologous N- and C-terminal lobes. Each lobe contains an iron-binding site, highly conserved and located in a deep cleft between two domains (N1 and N2 or C1 and C2). Lf and Tf have similar amino acid composition, secondary structure (including their disulphide bonds), and tertiary structure, whereas exerting different biological functions (Bluard-Deconinck et al. 1974).
Iron binding and release are associated with large conformational changes in which hLf and bLf adopt either open (iron unsaturated, apo-Lf) or closed states (iron saturated, holo-Lf) (Baker and Baker 2004).
Lfs are among the most important cationic multifunctional glycoproteins belonging to innate and nutritional immunity. Nutritional immunity comprehends natural components able to sequester trace minerals, as iron in the case of Lf, thus both limiting bacterial or viral multiplication and lowering the severity of infections. Lf can exist in three different isoforms: Lf-α, the iron-binding isoform, and Lf-β and Lf-γ, which possess ribonuclease activity and do not bind iron (Furmanski et al. 1989). HLf and bLf show noticeable differences at glycosylation level. In hLf, there are three possible N-linked glycosylation sites (Asn138, Asn479, and Asn624) always occupied, while in bLf there are five possible N-linked glycosylation sites (Asn233, Asn368, Asn476 and Asn545 and Asn281) of which four sites always occupied, whereas Asn281 is found glycosylated for approximately 30% in bovine colostrum and 15% in mature milk (Spik et al. 1994; Van Veen et al. 2004). Moreover, hLf and bLf possess high sequence homology (69%) and exert identical multifunctionality as antimicrobial (antibacterial, antifungal and antiviral properties), anti-parasitic, anti-inflammatory, anti-oxidant, and immunomodulating activities (Valenti and Antonini 2005; Puddu et al. 2009, 2011).
Therefore, most of the in vitro and in vivo studies have been carried out using bLf, generally recognized as a safe substance (GRAS) by the Food and Drug Administration (FDA, USA) (U.S FDA 2014) and as a dietary supplement by the European Food Safety Authority (European Food Safety Authority 2012).
Recently, in addition to the well-characterized activities, bLf has been found to be a physiological orchestrator of iron and inflammatory homeostasis through its ability in modulating the expression of the major iron proteins, such as ferroportin (Fpn), transferrin receptor 1 (TfR1) and ferritin (Ftn), both in in vitro and in vivo studies as well as in clinical trials (Cutone et al. 2017, 2019; Rosa et al. 2017; Lepanto et al. 2018).
Iron, an essential element for living cells, is a component of fundamental processes such as DNA replication and energy production as well as it is present in hemoglobin, myoglobin and some specific enzymes involved in viral transcription, mRNA translation, and assembly (Sienkiewicz et al. 2021). However, iron can also be toxic when present in excess for its capacity to donate electrons to oxygen, thus causing the generation of reactive oxygen species (ROS), well known to provoke DNA, protein and membrane lipid damages, tissue injury and organ failure (Andrews 2000). This dichotomy of iron, able to gain and loss electrons, has led to the development of sophisticated strategies to avoid free available iron overload and to maintain the correct iron balance/ratio between tissues/secretions and blood, defined as iron homeostasis. Dietary iron is absorbed in the proximal small intestine (duodenum). In developed countries, about 15 mg of iron per day are provided by a balanced diet, but only ~ 10% (1–2 mg) is absorbed, due to its extremely poor bioavailability. Interestingly, 20 mg of iron per day, to be used for the de novo synthesis of heme, derive from senescent erythrocyte lyses by macrophages. The iron recovered from hemoglobin of senescent erythrocytes is the largest iron source in the reticuloendothelial system. Finally, every day, a few milligrams of iron are regained from storage in hepatocytes and macrophages. In human cells, the required iron is guaranteed by Tf-bound iron, which is imported into cells through Tf receptor-mediated endocytosis. In the endosome, Tf-bound iron is released as ferrous ion, which is translocated via divalent metal transporter 1 (DMT1) into cytoplasm where it is sequestered by Ftn. Ftn, the major iron storage protein, composed by 24 subunits, possesses ferroxidase activity and a large cavity where up to 4,500 ferric ions, as oxy-hydroxide micelles, are sequestered. The release of iron from this protein to cytoplasm occurs after reduction of ferric to ferrous ions. Then, ferrous ions are exported into plasma by Fpn, the only known mammalian iron exporter found on the cytoplasmic membrane of enterocytes, hepatocytes, macrophages, and placental cells (Donovan et al. 2005). Of note, Fpn acts in partnership with two ferroxidases: hephaestin (Heph) in epithelial cells, and ceruloplasmin (Cp) in macrophages (Bonaccorsi et al. 2018). Both ferroxidases convert ferrous into ferric ions to allow their binding to Tf in the blood.
Fpn is an important actor of iron homeostasis, regulated by multiple factors. In particular, Fpn is down-regulated by the pro-inflammatory cytokine interleukin-6 (IL-6) (Cutone et al. 2014, 2017) and by hepcidin, another pivotal actor, which regulates iron homeostasis through the binding, internalization and degradation of Fpn (Qiao et al. 2012). The bioactive hepcidin, a cationic peptide hormone of 25 amino acids mainly synthesized by hepatocytes, derives from the proteolytic cleavage of an 84-amino acid precursor, and it is secreted in urine (Park et al. 2001; Hunter et al. 2002) and plasma (Krause et al. 2000). Differently from Fpn, hepcidin is up-regulated by several factors as iron stores and IL-6, IL-1α and IL-1β (Nemeth et al. 2004; Lee et al. 2005; Wrighting and Andrews 2006; Verga Falzacappa et al. 2007; Coffey and Ganz 2017). This mechanism involves multiple pathways through which hepatocytes directly sense systemic iron levels (Zumerle et al. 2014; Coffey and Ganz 2017).
The Fpn degradation caused by the binding with hepcidin or its down-regulation by IL-6 provokes a significant decrease of iron export from cells into plasma. Consequently, at the cellular level, intracellular iron overload in enterocytes and macrophages is established, thus inducing an increase of the host susceptibility to infection (Rosa et al. 2017). At the systemic level, the intracellular iron overload is related to iron deficiency (ID), ID anemia (IDA) and anemia of inflammation (AI) (Frazer and Anderson 2003; Paesano et al. 2012; Miller 2012; Lepanto et al. 2018).
Antiviral activity of bovine lactoferrin in in vitro models
Among the several functions of bLf, the antiviral activity will be deeply discussed in this review because viral infections are one of the major problems for human health.
Vaccines can prevent epidemic or pandemic but antiviral treatments are needed. BLf exerts an antiviral activity in the early phase of viral entry and protects the host from the infections, enough to be considered a first-line defense glycoprotein. It matches with virus through both topic/local (Valenti and Antonini 2005; Berlutti et al. 2011; Wakabayashi et al. 2014; Chang et al. 2020) and systemic action (Kruzel et al. 2017).
The topic/local antiviral action of bLf is achieved through (i) its binding to the anionic surface components of host cells as glycosaminoglycans (GAGs); (ii) its binding to the anionic surface components of viral particles; (iii) its binding to the anionic surface components of host cells and viral particles; (iv) inhibition of viral replication.
As viruses enter inside host cells through GAGs, the binding between bLf and GAGs competitively hinders viral infection by enveloped viruses, such as alphavirus, cytomegalovirus, human immunodeficiency virus (HIV), herpes simplex virus, respiratory syncytial virus, simian foamy virus, Sindbis virus, Dengue virus, hepatitis B virus (HBV), hepatitis C virus (HCV), norovirus, Japanese encephalitis virus, hantavirus, influenza A virus, parainfluenza virus, rhinovirus, severe acute respiratory syndrome coronavirus (SARS-CoV) and SARS-CoV-2 or by non-enveloped viruses as rotavirus, poliovirus, enterovirus 71, echovirus 6, human papillomavirus, feline calicivirus, and adenovirus (Wu et al. 1995; Lang et al. 2011; Kell et al. 2020; Denani et al. 2021; Hu et al. 2021 and references therein).
Moreover, bLf is also able to bind to the surface components of viral particles pivotal to interact with cell receptors thus limiting viral entry and infection (Table 1).
Table 1.
Lactoferrin (Lf) binding to surface viral components
| Virus | Lf source | Lf binding site | Lf activity | References |
|---|---|---|---|---|
| Adenovirus | Bovine | III and IIIa structural polypeptides | Pietrantoni et al. (2003) | |
| Coxsakievirus A16 | Bovine | Inhibition of cytopathic effect | Wakabayashi et al. (2014) | |
| Echovirus 5 | Bovine | Structural proteins | Furlund et al. (2012) | |
| Echovirus 6 | Bovine | Inhibition of apoptosis | Tinari et al. (2005) | |
| Enterovirus 71 | Bovine and Human | Inhibition of cytopathic effect | Lin et al. (2002) | |
| Hantavirus | Bovine | Inhibition of viral adsorption | Ng et al. (2015) | |
| Hepatitis C virus | Bovine and Human | Envelope proteins E1 and E2 | Yi et al. (1997) | |
| Herpes simplex virus | Bovine | Glycoprotein B, D, H, L | Marchetti et al. (2009) | |
| Human immunodeficiency virus | Bovine and Human* | V3 loop of glycoprotein 120 | Swart et al. (1996) | |
| Influenza A virus | Bovine | Prevents cytopathic effects independent from metal saturation and carbohydrates | Pietrantoni et al. (2012) | |
| Influenza A virus H1N1 | Bovine | Inhibits apoptosis, caspase 3, nuclear export of viral ribonucleoproteins so preventing viral assembly | Pietrantoni et al. (2010) | |
| Influenza A virus H1N1 and H3N2 | Bovine | Hemagglutinin | Ammendolia et al. (2012) | |
| Influenza A virus H5N1 | Bovine | Viral constituents | Taha et al. (2010) | |
| Influenza A virus H5N1 | Bovine | Sialylated glycans and hemagglutinin | Wang et al. (2021) | |
| Parainfluenza virus type 2 | Bovine | Intracellular and extracellular activity | Yamamoto et al. (2010) | |
| Poliovirus | Bovine and Human | Inhibition of cytopathic effect | Marchetti et al. (1999) | |
| Respiratory syncytial virus | Human | Fusion protein F | Sano et al. (2003) | |
| Rotavirus | Bovine | Inhibition of cytopathic effect | Superti et al. (1997) | |
| SARS-CoV-2 | Bovine | Spike glycoproteins | Campione et al. (2021a) |
The viruses are alphabetically sorted
*This study has been conducted using bovine and human Lf, as reported in Materials and Methods. In Results and Discussion sections, the Lf source for each experiment was not specified
Furthermore, in most studies, Lf was tested both in apo- and in metal-saturated forms and no striking differences in the antiviral effect between the different forms were reported (Marchetti et al. 1996, 1998; Puddu et al. 1998). Of note, bLf exhibited higher antiviral activity than hLf (Berlutti et al. 2011 and references therein) but the reason of this major antiviral activity is still under investigation.
Concerning the systemic action, bLf is a mediator that connects innate and adaptive immune function in mammals (Actor et al. 2009; Kruzel et al. 2017). In particular, Lf plays a key role in the resolution of microbial injuries that lead to disorders in immune homeostasis (Kruzel et al. 2007; Actor et al. 2009).
During infections, monocytes and macrophages respond to this injury with the production of NF-kB, which, in turn, induces inflammatory mediators (cytokines) which stimulate the production of fresh immature neutrophils and monocytes from bone marrow. The presence of Lf, due to the degranulation by mature neutrophils, attenuates inflammation, repairs tissue damage, protects integrity of various organs and limits microbial spread (Kruzel et al. 2017 and references therein).
In addition, Lf modulates excessive immune-responses (Legrand et al. 2005; Kruzel et al. 2007), decreases ROS production, pro-inflammatory cytokines and mitochondrial dysfunction (Actor et al. 2009), apoptosis (Actor et al. 2009; Pietrantoni et al. 2010), induces the synthesis of interferons (IFNs) (Kruzel et al. 2017; Mirabelli et al. 2021), activates NK cells (Legrand and Mazurier 2010), enhances CD4 + , CD8 + and decreases CD69 + (a marker of inflammation) (Welsh et al. 2011), promotes the maturation of T-cell precursors in helper cells (Actor et al. 2009), differentiates immature B-cells in antigen-presenting cells (Actor et al. 2009), differentiates monocytes in macrophages (Wisgrill et al. 2018), balances the polarization of Th1/Th2 (Puddu et al. 2011) and the macrophages M1/M2 switching (Cutone et al. 2017), decreases inflammatory cytokines and intracellular iron overload (Rosa et al. 2017), inhibits platelet aggregation (Leveugle et al. 1993) and modulates cell receptors useful for its multiple functions (Mancinelli et al. 2020).
Influence of lactoferrin glycosylation on in vitro antiviral activity
As reported, hLf and bLf share a high sequence homology (69%) but possess noticeable differences at glycosylation level: hLf possesses three possible N-linked glycosylation sites, while bLf five possible N-linked glycosylation sites (Spik et al. 1994; Van Veen et al. 2004). The glycosylation sites seem to influence bLf antiviral activity. The first paper, published by Superti et al. (2001), demonstrated that the anti-rotavirus activity of bLf is increased upon sialic acid removal, which causes an increase in the interaction between rotavirus and bLf. Successively, the influence of mannose on antiviral activity was investigated (Groot et al. 2005). It was found that bLf is more effective than hLf in inhibiting DC-SIGN, a C-type lectin that mediates the internalization of HIV-1 virus. This occurs as a consequence of the binding of the oligomannose glycans of bLf to the DC-SIGN (Groot et al. 2005). This effect combined with enhanced toll like receptor signaling might be the mechanism by which mannose glycans contribute to the prevention of the disease (Figueroa-Lozano et al. 2018).
Recently, it has been proven that the hemagglutinins of influenza A virus (IAV) bind to sialoglycoconjugates of the host cell surface thus initiating the infection process (Wang et al. 2021). Sialylated glycans of bLf bind IAV thus blocking viral attachment to host cells during the early stages of infection. When bLf is desialylated, the binding of bLf to IAV is significantly reduced with respect to native bLf and antiviral activity is lowered (Wang et al. 2021).
The different antiviral activity of desialylated bLf against influenza virus (Wang et al. 2021) and rotavirus (Superti et al. 2001) could be due to the different structures of enveloped or non-enveloped viruses, respectively.
Antiviral activity of bovine lactoferrin in vivo
The antiviral activity of hLf was first demonstrated in mice infected with the polycythemia inducing strain of the Friend virus complex (Lu et al. 1987).
Since 1995, a potent antiviral activity of both hLf and bLf against enveloped and non-enveloped viruses has been also in vivo demonstrated.
The most valuable studies carried out in in vivo models are reported in Table 2 and all references are included in three reviews (Berlutti et al. 2011; Wakabayashi et al. 2014; Chang et al. 2020) except for four clinical trials on bLf efficacy against SARS-CoV-2, recently published by Serrano et al. (2020); Algahtani et al. (2021); Campione et al. (2021b) and Rosa et al. (2021).
Table 2.
Activity of lactoferrin (Lf) against different viruses in in vivo models
| Administration route | Lf source | Model | Virus | References |
|---|---|---|---|---|
| ORAL | Human | Mice | Friend virus complex | Lu et al. (1987) |
| TOPIC | Bovine | Mice cornea | Herpes simplex virus | Fujihara and Hayashi (1995) |
| ORAL | Bovine | Mice | Cytomegalovirus | Shimizu et al. (1996) |
| ORAL | Bovine | Patients with hepatitis C | Hepatitis C virus | Tanaka et al. 1999) |
| ORAL | Bovine | Patients with chronic hepatitis C | Hepatitis C virus | Okada et al. (2002); Hirashima et al. (2004); Ishibashi et al. (2005); Ueno et al. (2006) |
| ORAL | Bovine | Mice | Herpes simplex virus | Wakabayashi et al. (2004) |
| ORAL | Bovine | Mice | Influenza virus | Shin et al. (2005) |
| ORAL | Bovine | Rat | Rotavirus | Pérez-Cano et al. (2008) |
| ORAL | Bovine | Children | Enterovirus 71 | Yen et al. (2011) |
| ORAL | Bovine | Mice | Respiratory syncytial virus | Gualdi et al. (2013) |
| ORAL | Bovine | Patients with common cold | Rhinovirus | Vitetta et al. (2013) |
| SUBCUTANEOUS | Bovine | Mice | Influenza virus A | Sherman et al. (2015) |
| ORAL* | Bovine | COVID-19 patients | SARS-CoV-2 | Serrano et al. (2020) |
| ORAL | Bovine | COVID-19 patients | SARS-CoV-2 | Algahtani et al. 2021) |
| ORAL* AND INTRANASAL* | Bovine | COVID-19 patients | SARS-CoV-2 | Campione et al. (2021b) |
| ORAL | Bovine | Patients with summer cold | Different viruses | Oda et al. (2021) |
| ORAL | Bovine | COVID-19 patients | SARS-CoV-2 | Rosa et al. (2021) |
*These two clinical trials have been performed with liposomal bovine Lactoferrin
As reported, in most of the in vivo studies the administration of bLf is performed orally. Even if the oral administration of bLf may have a beneficial role in managing symptoms and recovery of patients suffering from respiratory tract infections (Stefanescu et al. 2013; Motoki et al. 2020; Ali et al. 2021; Oda et al. 2021), the systemic effects of oral administration of bLf are not fully understood. However, the gut-lung axis or the bidirectional interaction between gut and lung must be considered. Gut microbiota protects the gastrointestinal tract from pathogenic microbes acting as a barrier, neutralizes pathogens with their anti-microbial metabolites, regulates the innate and adaptive immunity, locally and systemically, in both health and disease as well as contributes to the mucosal immune system (interplay microbiota-mucosal immunity) through segmented filamentous bacteria that stimulate Th17. Th17 play an important role in maintaining mucosal barriers and contribute to pathogen clearance at mucosal surfaces through IL-17 (Wang et al. 2014a; Szabo and Petrasek 2015; Broz and Dixit 2016; Mangan et al. 2018).
Of note, the alteration of the gut microbiota, due to the prolonged antibiotic therapy, can potentially lead to the deleterious effects on respiratory immune responses (Ichinohe et al. 2011) as well as viral and bacterial respiratory infections can be causative of the alteration of the gut microbiota (Wang et al. 2014a; Bartley et al. 2017; Hanada et al. 2018; Yildiz et al. 2018). In addition, respiratory viral infections, due to influenza or respiratory syncytial virus, result in gut dysbiosis in mice, predisposing to secondary bacterial infection (Deriu et al. 2016; Groves et al. 2018). Lastly, the gut microbiota alterations are related to abnormal activation of the immune system and respiratory illnesses such as asthma, lung allergic responses and chronic respiratory diseases (Enaud et al. 2020).
Moreover, the influence of Lf on the activation of IFNs and NK cells must not be neglected. As matter of fact, at systemic level, the oral administration of bLf in mice induces type I IFNs production that play an important role in antiviral defense, such as the inhibition of protein synthesis, degradation of viral RNA in infected cells, and enhancement of antiviral immune activity (Kuhara et al. 2006). This antiviral response seems to be principally mediated by plasmacytoid dendritic cells, the main producers of type I IFNs, which have been shown to be activated by bLf (van Splunter et al. 2018).
In addition, oral administration of bLf in mice increases NK cells activity, that plays an important role in the early innate host defense against several pathogens (Kuhara et al. 2006).
SARS-CoV-2 and bovine lactoferrin
SARS-CoV-2, a lipid-enveloped positive-sense RNA virus belonging to the β-coronavirus genus, is a highly pathogenic coronavirus causing the recent pandemic (Hartenian et al. 2020; Wu et al. 2020a; Zhu et al. 2020). This virus mainly infects the respiratory tract of humans, causing fever, dry cough, fatigue, shortness of breath, body aches, and diarrhea. In a small number of the patients, it may progress to acute respiratory distress syndrome (ARDS), metabolic acidosis, septic shock, and clotting dysfunction, or even death.
Like other β-coronaviruses, spike (S) glycoprotein mediates the attachment and membrane fusion of viral particles with target cells in SARS-CoV-2 infection (Hatmal et al. 2020). The S glycoprotein is a typical type I fusion protein composed by two functional subunits: S1, containing the receptor binding domain (RBD), mediating cell receptor binding, and S2, containing the transmembrane domain involved in virus-cell fusion (Ke et al. 2020). In the proximity of cytoplasmic tail, a sequence resembling the human peptide hepcidin has been discovered, but its function is still unknown although its role in local and systemic iron regulation or in iron homeostasis disorders can be hypothesized (Ehsani 2020).
Spike protein can bind to heparan sulphate proteoglycans (HSPGs) (Hu et al. 2021), thus anchoring the virus to the cell surface, and interact with angiotensin-converting enzyme 2 (ACE2) (Wang et al. 2020), the principal gate for viral entry. Moreover, TfR1 has been identified as another potential receptor of SARS-CoV-2. Of note, the binding between virus and apical part of TfR1 does not interfere with iron transport by holo-Tf (Tang et al. 2020; Dai et al. 2021).
The port of entry for SARS-CoV-2 is the nasal cavity while the respiratory droplets represent the main exit site. However, the fecal–oral transmission must be taken into account, especially in presence of gastrointestinal (GI) symptoms, because SARS-CoV-2 nuclear fingerprints have been isolated in the esophagus, stomach, GI mucosa, duodenum, rectum and fecal samples (Giobbe et al. 2021). Of note, SARS-CoV-2 in stool samples has been observed to persist longer than that in respiratory samples (Wu et al. 2020b). Lastly, the neurologic and hematologic symptoms demonstrate the systemic nature of SARS-CoV-2 (Wan et al. 2021).
The in vitro antiviral activity of bLf against this enveloped RNA virus has been demonstrated (Campione et al. 2021a; Mirabelli et al. 2021). Similar to other viruses, bLf has been shown to impede SARS-CoV-2 entry by competing with cell HSPGs (Hu et al. 2021). Moreover, bLf binds to Spike glycoproteins of SARS-CoV-2 (Campione et al. 2021a), thus limiting both viral entry inside host cells and infection (Campione et al. 2021a; Mirabelli et al. 2021). A detailed in silico analysis of the interaction network between bLf and spike glycoproteins reveals the presence of 28 different interactions, which persist for more than 25% of the simulation time, in agreement with the high interaction energy calculated. In detail, three salt bridges, 5 hydrogen bonds and 20 residue pairs involved in hydrophobic contacts have been found (Campione et al. 2021a). To check if some of the spike residues targeted by bLf were involved in the binding with ACE2, the average structure extracted from the simulation of the binding between ACE2 and C-terminal domain 1 (CTD1) of spike glycoprotein has been compared (Campione et al. 2021a). Surprisingly, only two spike residues (Gly502 and Tyr505) were shared between the complexes interfaces. Despite this, bLf holds the same position assumed by the ACE2 enzyme, that is, above the up CTD1 domain (Campione et al. 2021a).
After the results obtained in silico, the antiviral activity of bLf against SARS-CoV-2 was in vitro assayed (Campione et al. 2021a). It has been demonstrated that the anti-SARS-CoV-2 activity varies according to different experimental approaches: i) bLf pre-incubation with cells, ii) bLf preincubation with viral particles, iii) preincubation with cells and virus. Furthermore, cell lines, multiplicity of infection (MOI), and bLf concentrations influence the bLf antiviral activity (Campione et al. 2021a). As a matter of fact, 500 μg/ml of bLf inhibit at higher extent respect to 100 μg/ml and the preincubation of bLf with viral particles shows the highest antiviral activity (Campione et al. 2021a).
Taken together, these results reveal that the topic/local antiviral activity of bLf are also extendable to SARS-CoV-2.
Concerning the systemic activity of oral administration of bLf in COVID-19 patients, some elucidations, involving gut-lung axis, must be made. This axis, believed to be bidirectional, affects the immune response of both tracts when one of the two sites is dysregulated (Ichinohe et al. 2011). The gut-lung tracts share a common mucosal immune system (Budden et al. 2017; Enaud et al. 2020) and they are colonized by their microbiota, constituted by quasi-stable genre of microorganisms via the oral route (Grier et al. 2018). Although the microbiota of both tracts consists of similar phyla, they differ at the level of species in composition and density. Even if many respiratory viral illnesses are commonly accompanied by GI symptoms (Deriu et al. 2016), the immune-related interactions between resident gut and respiratory tract microbiota are yet to be explored. Similarly, Wang et al. (2014a) demonstrated indirect intestinal inflammation with influenza infection in a mouse-model occurring via microbiota-mediated Th17 cell dependent inflammation (Wang et al. 2014a). Several studies have reported gut dysbiosis after respiratory viral infection (Bartley et al. 2017; Yildiz et al. 2018). Groves et al. (2018) showed that gut dysbiosis, in the form of an increase in Bacteroidetes and a decrease in Firmicutes phyla abundance, occurred in mice models with respiratory syncytial and influenza virus infections, but not in those vaccinated with live attenuated influenza viruses.
As matter of fact, as reported, oral administration of bLf may have a beneficial role in managing symptoms and recovery of patients suffering from respiratory tract infections (Stefanescu et al. 2013; Motoki et al. 2020; Ali et al. 2021; Oda et al. 2021). In SARS-CoV-2 infection, the viral particles, entering from nasal cavity, infect lung through ACE2 receptors thus over-expressing circulating pro-inflammatory cytokines which alter the gut microbiota and compromise intestinal integrity (Hussain et al. 2021). On the other hand, SARS-CoV-2 by binding to enterocytes through ACE-2 provokes a dysbiosis in gut microbiota and the resultant leaky gut allows translocation to the lung of microbial products and antigens through the blood and lymphatic vessels (Liu et al. 2021). In consequence of this, the enhance of pro-inflammatory cytokines, the dysbiosis in lung microbiota and the disorders of local and systemic immune response have been observed (Hussain et al. 2021). Therefore, severe SARS-CoV-2 infection is not only caused by virus and subsequent bacterial secondary infections in the respiratory and intestinal tracts but is also closely related to gut microbiota dysbiosis (Liu et al. 2021). Gut microbiota is essential for host immune system’s induction, education, function, development of immune responses, and regulates the integrity of the mucosal barrier, provides bacterial metabolites, and regulates the immunoregulatory functions of intestinal epithelial cells by modulating the expression of antimicrobial factors (Hussain et al. 2021).
Iron, reactive oxygen species, iron-proteins, SARS-CoV-2 infection and lactoferrin
Viral replication is dependent from host cell iron enzymes, some of which are involved in transcription, viral mRNA translation, and viral assembly (Sienkiewicz et al. 2021). It is well known that SARS-CoV-2 infection induces pro-inflammatory cytokine storm, including IL-6 (Campione et al. 2021b) which in turn dysregulates iron homeostasis leading to an intracellular iron overload (Rosa et al. 2017). Therefore, intracellular iron overload increases viral replication, thus enhancing the severity of the infection (Mancinelli et al. 2020).
However, bLf, by exerting the anti-inflammatory activity, reduces IL-6 levels, restores the synthesis of Fpn, iron export and, consequently, decreases the concentration of intracellular iron (Campione et al. 2020). The consequence of this bLf activity leads to a reduction in viral replication as demonstrated in in vitro models infected by SARS-CoV-2 (Campione et al. 2021a).
In inflamed COVID-19 patients, high levels of IL-6 induce the up-regulation of hepcidin (Nai et al. 2021) and high levels of intracellular free available iron which generate the dangerous ROS through Haber–Weiss and Fenton reactions, reported below:
Haber–Weiss Reaction
Fenton Reaction
The ROS and oxidative stress lead to lung damage and fibrosis thus provoking a decline of lung or other organs functions. BLf, by binding free iron, decreases iron overload and inhibits ROS formation and oxidative stress thus preserving the organs from damages. Recently, it has been also demonstrated that iron chelating compounds as deferoxamine decrease the level of replication of some RNA viruses (Abobaker 2020; Perricone et al. 2020; Vlahakos et al. 2021).
Furthermore, SARS-CoV-2 attacks one of the beta chains of the hemoglobin which leads to the dissociation of iron from heme thus enhancing free iron level in the body (Wenzhong and Hualan 2021). This increase of available iron could explain why most patients with COVID-19 have very high levels of Ftn (Cheng et al. 2020). However, in COVID-19 patients, bLf early oral administration decreases serum Ftn levels (Campione et al. 2021b). Concerning iron overload, it increases viral replication (Drakesmith and Prantice 2008) while the decrease of iron overload through both iron binding ability and anti-inflammatory activity of bLf decreases viral replication (Campione et al. 2020, 2021a).
The infection by SARS-CoV-2 up-regulates the synthesis of IL-6 (Campione et al. 2021b) which, in turn, induces the expression of hepcidin (Nai et al. 2020). The oral administration of bLf influences iron-proteins expression: the decrease of serum IL-6 and Ftn. These different but parallel functions are interesting signals of the restoring of iron and inflammatory homeostasis which contributes to antiviral activity together with the binding of bLf to HSPGs and spike glycoproteins (Campione et al. 2020, 2021a, b).
Inflammasome, SARS-CoV-2 and lactoferrin
Inflammasomes, cytosolic multiprotein oligomers responsible for the activation of inflammatory responses, are an important part of the innate immune system that can recognize cellular stresses and infections (Szabo and Petrasek 2015; Mangan et al. 2018). Inflammasomes are named according to different four sensing proteins: NLRP1, NLRP3, NLRC4, and AIM212. Among them, the NLRP3 inflammasome has important functions in RNA virus infection (Wang et al. 2014b; Pan et al. 2019). NLRP3 protein contains three domains: Pyrin domain (PYD), Nucleotide-binding domain, and Leucine-rich repeat domain (Pan et al. 2019). The activation of the NLRP3 inflammasome, supports caspase-1 activation. Active caspase-1 processes pro-IL-1β into mature IL-1β (Latz et al. 2013). Of note, nucleocapsid protein of SARS-CoV-2 activates inflammasomes which, in turn, induces active-Caspase-1 and IL-1β. Excessive IL-1β stimulates systemic inflammation responses and, consequently, cytokine storm provoking lung injury (Pan et al. 2021). Studies have reported that inflammasomes are associated with COVID-19 severity (Toldo et al. 2021), probably because excessive activated inflammasomes induce cell pyroptosis, harmful to the host (Dai et al. 2018).
The effect of bLf on inflammasomes in SARS-CoV-2 infections is still unknown while the peptide hLf (1–11) is known to inhibit A. baumannii-induced caspase-1 activation, IL-1β, IL-6 and pyroptosis of pulmonary alveolar macrophages in mice (Dai et al. 2018).
Coagulation and fibrinolysis, SARS-CoV-2 and lactoferrin
Thrombin, a serine protease and an activated coagulation factor (FIIa), plays an important role in the coagulation system in humans by converting fibrinogen into fibrin that aggregates to form a thrombus. It activates coagulation factors, platelet aggregation, and vascular endothelial cells mainly by binding to protease-activated receptors 1,3 located on the surface of vascular endothelial cells involved in the regulation of thrombotic responses (Kalashnyk et al. 2013).
At present, commonly used antithrombotic drugs include heparin, warfarin, and argatroban, which can present mild to severe side effects. Consequently, anticoagulant products, free from adverse effects and deriving from natural foods, as milk, have been studied and are still under investigation. Among these, Lf hydrolysates with a molecular weight of less than 3 kDa has been used as a dual vasopeptidase (angiotensin-converting enzyme and endothelin-converting enzyme, ACE/ECE) or a single ECE inhibitor with different anti-vasoconstrictive effects (Fernandez-Musoles et al. 2013). Recently, a peptide located at 93 − 101 positions of the amino acid sequence of bLf, and identified in the gastrointestinal tract of mice, has been found to have anticoagulant functions without side effects (Xu et al. 2020a). The binding of this peptide, named LF-LR, to thrombin inhibits platelet aggregation thus explaining the results already obtained by Qian et al. (1995). These Authors tested sheep and human Lfs and pepsin hydrolysates deriving from both glycoproteins, demonstrating that both Lfs and only one digestion product were able to inhibit thrombin-induced platelet aggregation (Qian et al. 1995).
Along with the cytokine storm, in COVID-19 patients, a storm of large and small blood clots has been found (Cui et al. 2020; Klok et al. 2020). SARS-CoV-2 infects endothelium through ACE-2 thus inducing complement system which, in turn, stimulates clots (Skendros et al. 2020). However, COVID-19 patients can be hospitalized when already suffering from conditions that promote clot formation, such as hypertension, diabetes, and hereditary thrombophilia. The close relationship between COVID-19 and thrombosis, venous thromboembolism and arterial thrombosis are of significant clinical importance. Histopathology of lung specimens from patients with severe disease demonstrate fibrin-based occlusion of small vessels (Fox et al. 2020; Tian et al. 2020; Xu et al. 2020b).
Therefore, patients suffering from COVID-19 are at high risk for thrombotic arterial and venous occlusions (Zuo et al. 2021). Beside the coagulation process, fibrinolysis must be considered because the balance between coagulation and fibrinolysis will allow an optimal approach not only to thrombosis but also to fibrinolysis therapies.
Fibrinolysis is tightly regulated by plasminogen activators and inhibitors with the conversion of plasminogen to plasmin (Longstaff and Kolev 2015). The plasminogen activation system is essential for dissolution of fibrin clots. HLf binds to human plasminogen thus blocking its activation and fibrin clots dissolution (Zwirzitz et al. 2018). The dissolution of clots forms D-dimers. Elevated D-dimer was associated with both thrombotic and bleeding complications (Al-Samkari et al. 2020) and are predictors of the mortality of COVID-19 patients (Zuo et al. 2021).
Recently, COVID-19 patients treated with oral administration of bLf showed a significant lower concentration of serum D-dimers respect to untreated patients (Campione et al. 2021b).
Oral administration of lactoferrin on COVID-19 patients
The first study on oral administration of bLf against SARS-CoV-2 infection was carried out by Serrano et al. (2020) on 75 symptomatic COVID-19 patients. This prospective observational study was performed administering liposomal bLf (LLf) (from about 120 to 200 mg per day) for 10 days in association with 10 mg of zinc administered two to three times a day. The Authors reported that 100% recovery of all SARS-CoV-2-positive patients was achieved within 4–5 days. However, this study shows several limits as no randomized clinical trial, limited sample size, low doses of LLf, short duration of treatment and absence of controls.
Successively, a randomized, prospective, interventional pilot study on 54 COVID-19 patients with mild-to-moderate symptoms was published (Algahtani et al. 2021). The treatment consisted in the administration of oral bLf (200 mg/once a day or 200 mg/twice a day) for seven days. Control group received intranasal oxygen, oral hydroxychloroquine, oral vitamin C, Zn and acetylcysteine. BLf-treated groups received the above-mentioned therapy plus bLf 200 mg/day (Group 1) or bLf 200 mg/ 2 times a day (Group 2). This study showed no statistically significant difference among studied groups regarding recovery of symptoms or laboratory improvement. Also, this study possesses some limits as short duration of treatment (7 days), limited sample size (18 patients/group) and, more importantly, very low bLf dosages.
Conversely, positive results have been described in other two papers (Campione et al. 2021b; Rosa et al 2021). The first in vivo preliminary study was designed to investigate the antiviral effect of oral and intranasal liposomal bLf in asymptomatic and mild-to-moderate COVID-19 patients. From April 2020 to June 2020, a total of 92 mild-to-moderate (67/92) and asymptomatic (25/92) COVID-19 patients were enrolled and divided into three groups. Thirty-two patients (14 hospitalized and 18 in home-based isolation) received only oral and intranasal liposomal bLf; 32 hospitalized patients were treated only with standard of care (SOC) treatment; and 28, in home-based isolation, did not take any medication. In addition, 32 COVID-19 negative, untreated, healthy subjects were added for ancillary analysis. Even if at the beginning of the pandemic, no drug was proven to be safe and effective for treating COVID-19, SOC regimens of this study consisted in lopinavir/darunavir, an inhibitor of protease of SARS-CoV-2 in vitro, and hydroxychloroquine able to inhibit fusion of SARS-CoV-2 (Campione et al. 2021b). Liposomal bLf for oral use was 1 g per day for 30 days and liposomal bLf intranasal formulation was administered from early phase of COVID-19 disease 3 times daily (a total of about 16 mg/nostril/day) until the SARS-CoV-2 RNA negativization.
BLf-treated COVID-19 patients obtained an earlier and significant (p < 0.0001) SARS-CoV-2 RNA negative conversion compared to the SOC-treated and untreated COVID-19 patients (14.25 vs. 27.13 vs. 32.61 days, respectively) and showed fast clinical symptoms recovery compared to the SOC-treated COVID-19 patients. Furthermore, a significant decrease in serum Ftn, IL-6, and D-dimers levels was observed in bLf-treated patients. No side events were registered. Even if one of the limitations of this study was the small sample size of patients, the COVID-19 patients were immediately treated after positive molecular swab test or at the first symptoms. Moreover, it is important to underline that intranasally and orally liposomal bLf administrations exert two different main functions: topical and systemic. The topical intranasal administration (about 16 mg/nostril/day) is related to bLf binding with HSPGs of host cells and spike glycoproteins (Campione et al. 2021a). These competitive bindings establish a protective barrier against viral infection. Conversely, oral systemic administration of bLf (1 g/day) is related to the anti-inflammatory activity and to the regulation of coagulation cascade. Of note, the anti-inflammatory activity also decreases intracellular iron overload, which, in turn, facilitates viral multiplication (Campione et al. 2021a; Sienkiewicz et al. 2021). Despite all these interesting results, this trial has the limit of not being a randomized double-blind study. Therefore, only after randomized clinical trials, aimed at confirming its efficacy, could bLf be considered as an effective treatment, alone or as a supplementary agent, in asymptomatic and mild-to-moderate COVID-19 patients. This could not only improve patient outcomes and prevention of hospital recovery, but also hinder chronic consequences of infection and disease transmission, mainly by shortening the period of infectiousness.
A second retrospective study, conducted by Italian general practitioners on their COVID-19 patients in home-based isolation, has been published (Rosa et al. 2021). The COVID-19 patients were treated immediately after positive molecular test or at the onset of first symptoms. Asymptomatic patients received a median dose of 400 mg bLf (200 mg/twice a day before meals); paucisymptomatic a median dose of 600 mg bLf (200 mg/three times a day before meals); moderate symptomatic a median dose 1,000 mg bLf (three times a day before meals) alone or as supplementary treatment (paracetamol and/or ibuprofen and/or cortisone and/or azithromycin depending on their symptoms). In this study 82 COVID-19 patients were bLf-treated while 39 COVID-19 were untreated (Rosa et al. 2021). The time required to achieve SARS-CoV-2 RNA negativization in bLf-treated patients (n = 82) was significantly lower (p < 0.001) compared with bLf-untreated ones (n = 39) (15 versus 24 days), similarly to patients treated with liposomal bLf (14.25 vs. 27.13). Of note, a link among reduction in symptoms, age, and bLf treatment was found. In addition, the bLf treatment is safe and well-tolerated by all treated patients. This retrospective study shows the advantage of a prompt treatment after positive molecular swab test or at the first symptoms, while possesses some limits as the sample size and the lack of a randomization.
Conclusions
Lf is one of the most important cationic pleiotropic glycoproteins of the innate immunity, highly conserved among different species, although the highest sequence homology has been found between hLf and bLf (about 70%). In 1987 the antiviral activity of hLf was discovered (Lu et al. 1987). Successively, the antiviral activity of bLf against enveloped and non-enveloped DNA and RNA viruses has been widely demonstrated (see references in Valenti and Antonini 2005; Berlutti et al. 2011; Wakabayashi et al. 2014; Chang et al. 2020; Mancinelli et al. 2020). The capability of bLf to hinder viral infection is generally attributed to its competitive binding to cell surface anionic components as GAGs (Wu et al. 1995; Kell et al. 2020; Hu et al. 2021) and/or viral particles (Table 1).
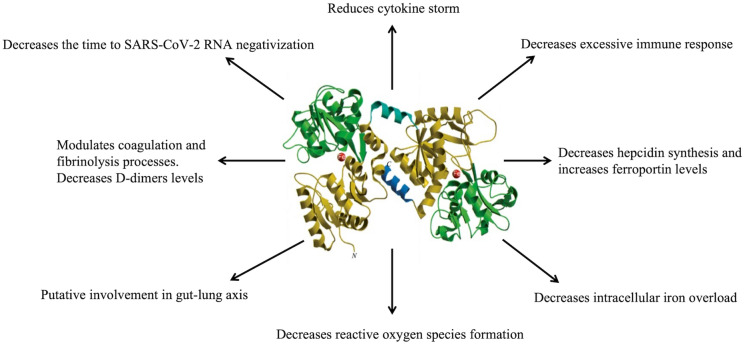
A lower number of papers have been published on bLf in vivo efficacy against viral infection (Table 2). Even if bLf and hLf possess identical biological functions (Rosa et al. 2017), bLf has been applied in in vitro and in vivo studies, being GRAS by the FDA and available in large quantities. Recently, bLf has been discovered to possess an antiviral activity even against SARS-CoV-2 in vitro (Campione et al. 2020, 2021a; Mirabelli et al. 2021) and in vivo (Campione et al. 2021b; Rosa et al. 2021). In vitro, a direct interaction between bLf and host receptors as HSPGs (Hu et al. 2021) as well as between bLf and virus structural glycoproteins as SARS-CoV-2 Spike (Campione et al. 2021a; Miotto et al. 2021) has been demonstrated. Furthermore, bLf is also able to enter inside the nucleus of host cells (Paesano et al. 2012) thus inhibiting the transcription of proinflammatory cytokine genes (Rosa et al. 2017). Therefore, bLf could strongly influence the cytokine storm cascade activation in COVID-19 patients as demonstrated in a preliminary clinical trial by Campione et al. (2021b). As bLf performs many functions useful to avoid systemic complications as well as decreases the severity of COVID-19, it is pivotal to summarize how many steps of the pathogenesis of SARS-CoV-2 can be influenced by this glycoprotein (Fig. 1).
Fig. 1.
Different functions of lactoferrin in counteracting SARS-CoV-2 pathogenesis
Firstly, SARS-CoV-2 induces cytokine storm but bLf can reduce cytokines storm, including IL-6, in COVID-19 patients (Campione et al. 2021b). SARS-CoV-2 induces excessive immune responses but bLf can counteract excessive immune responses (Zimecki et al. 2021). COVID-19 patients show an up-regulation hepcidin (Nai et al. 2021), which in turn could down-regulate Fpn. In several in vitro models (epithelial and macrophages) bLf up-regulates Fpn (Cutone et al. 2014, 2017; Frioni et al. 2014) while in vivo the bLf-mediated decrease of hepcidin has been demonstrated only in pregnant and non-pregnant women (Paesano et al. 2010; Lepanto et al. 2018). SARS-CoV-2 induces an intracellular iron overload, but bLf can decrease intracellular iron overload (Drakesmith and Practice 2008; Cutone et al. 2017). SARS-CoV-2 induces dysbiosis of intestinal microbiota but, unfortunately, no papers have been published on the influence of bLf oral administration on the composition of gut microbiota. SARS-CoV-2 increases the thrombosis associated with microcoagulation but bLf or its peptides can decrease the thrombosis associated with microcoagulation (Xu et al. 2020a) or reduce the concentration of serum D-dimers in COVID-19 patients (Campione et al. 2021b).
The efficacy of bLf oral administration, loaded or unloaded in liposomes, in treating asymptomatic, paucisymptomatic and moderate symptomatic COVID-19 patients has been demonstrated (Campione et al. 2021b; Rosa et al. 2021, respectively). For all patients from both studies, the median value of days to SARS-CoV-2 RNA negativization was significantly lower in bLf-treated patients than in those untreated (14 or 15 vs 27 or 24 days, respectively). Furthermore, a very interesting link between the symptom’s reduction and the age was observed (Rosa et al. 2021): the protective effect of bLf in reducing the time of the symptom’s resolution is related to the age. This could be explained by the fact that the synthesis of hLf is under hormone controls (Valenti et al. 2018) and, therefore, it decreases with age. Moreover, another factor to be considered is that chronic low-grade inflammation is common in older individuals, and it is a strong risk factor for aging-related disorders that cause high morbidity and mortality (Simpson 2016; Bektas et al. 2017). On the other hand, high levels of IL-6 lead to iron homeostasis disorders and tissue injuries (Rosa et al. 2017) and, therefore, the oral administration of bLf with its anti-inflammatory activity is really important because it induces IL-6 blockade which may contribute to counteract severe and critical outcome in COVID-19 patients.
Even if the results of bLf administration published until now in preliminary clinical trials require further confirmations on both a wider number of COVID-19 patients and a randomized double-blind study, it is possible to affirm that a prompt bLf treatment, sole or as adjuvant nutraceutical supplement, in COVID-19 patients could be the winning strategy. Based on these encouraging results we cannot ignore a so important protein of innate immunity, “companion of life and brick in the mucosal wall, effective against both microbial and viral attacks” (Valenti and Antonini 2005; Superti et al. 2020). Finally, the humankind should consider bLf as one of the more precious gifts from the ‘Mother Nature’ in the fight against the current COVID-19 and the future pandemics (Naidu et al. 2022)!
Acknowledgements
This study was supported by the contribution of “Fondazione Terzo Pilastro Internazionale”, President Prof. Emmanuele Francesco Maria Emanuele to E.C. and by University of Rome La Sapienza Funds to M.P.C.
Author contributions
P.V.: conceptualization; L.R., A.C., and P.V.: writing: original draft; L.R., A.C., M.P.C., E.C., L.B., and P.V.: writing-review & editing. All authors read and approved the final version.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Luigi Rosa, Antimo Cutone have contributed equally to this work.
References
- Abobaker A. Can iron chelation as an adjunct treatment of COVID-19 improve the clinical outcome? Eur J Clin Pharmacol. 2020;76(11):1619–1620. doi: 10.1007/s00228-020-02942-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Actor JK, Hwang SA, Kruzel ML. Lactoferrin as a natural immune modulator. Curr Pharm Des. 2009;15(17):1956–1973. doi: 10.2174/138161209788453202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Algahtani FD, Elabbasy MT, Samak MA, Adeboye AA, Yusuf RA, Ghoniem ME. The Prospect of lactoferrin use as adjunctive agent in management of SARS-CoV-2 patients: a randomized pilot study. Medicina (kaunas) 2021;57(8):842. doi: 10.3390/medicina57080842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali AS, Hasan SS, Kow CS, Merchant HA. Lactoferrin reduces the risk of respiratory tract infections: a meta-analysis of randomized controlled trials. Clin Nutr ESPEN. 2021;45:26–32. doi: 10.1016/j.clnesp.2021.08.019. [DOI] [PubMed] [Google Scholar]
- Al-Samkari H, Karp Leaf RS, Dzik WH, Carlson JCT, Fogerty AE, Waheed A, Goodarzi K, Bendapudi PK, Bornikova L, Gupta S, Leaf DE, Kuter DJ, Rosovsky RP. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. 2020;136(4):489–500. doi: 10.1182/blood.2020006520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammendolia MG, Agamennone M, Pietrantoni A, Lannutti F, Siciliano RA, De Giulio B, Amici C, Superti F. Bovine lactoferrin-derived peptides as novel broad-spectrum inhibitors of influenza virus. Pathog Glob Health. 2012;106(1):12–19. doi: 10.1179/2047773212Y.0000000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews NC. Disorders of iron metabolism. N Engl J Med. 2000;341:1986–1995. doi: 10.1056/NEJM199912233412607. [DOI] [PubMed] [Google Scholar]
- Baker HM, Baker EN. Lactoferrin and iron: structural and dynamic aspects of binding and release. Biometals. 2004;17(3):209–216. doi: 10.1023/b:biom.0000027694.40260.70. [DOI] [PubMed] [Google Scholar]
- Bartley JM, Zhou X, Kuchel GA, Weinstock GM, Haynes L. Impact of age, caloric restriction, and influenza infection on mouse gut microbiome: an exploratory study of the role of age-related microbiome changes on influenza responses. Front Immunol. 2017;8:1164. doi: 10.3389/fimmu.2017.01164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bektas A, Schurman SH, Sen R, Ferrucci L. Aging, inflammation and the environment. Exp Gerontol. 2017;105:10–18. doi: 10.1016/j.exger.2017.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berlutti F, Pantanella F, Natalizi T, Frioni A, Paesano R, Polimeni A, Valenti P. Antiviral properties of lactoferrin–a natural immunity molecule. Molecules. 2011;16(8):6992–7018. doi: 10.3390/molecules16086992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluard-Deconinck JM, Masson PL, Osinski PA, Heremans JF. Amino acid sequence of cysteic peptides of lactoferrin and demonstration of similarities between lactoferrin and transferrin. Biochim Biophys Acta. 1974;365:311–317. doi: 10.1016/0005-2795(74)90002-6. [DOI] [PubMed] [Google Scholar]
- Bonaccorsi di Patti MC, Cutone A, Polticelli F, Rosa L, Lepanto MS, Valenti P, Musci G. The ferroportin-ceruloplasmin system and the mammalian iron homeostasis machine: regulatory pathways and the role of lactoferrin. Biometals. 2018;31(3):399–414. doi: 10.1007/s10534-018-0087-5. [DOI] [PubMed] [Google Scholar]
- Broz P, Dixit VM. Inflammasomes: mechanism of assembly, regulation and signalling. Nat Rev Immunol. 2016;16(7):407–420. doi: 10.1038/nri.2016.58. [DOI] [PubMed] [Google Scholar]
- Budden KF, Gellatly SL, Wood DLA, Cooper MA, Morrison M, Hugenholtz P, Hansbro PM. Emerging pathogenic links between microbiota and the gut-lung axis. Nat Rev Microbiol. 2017;15:55–63. doi: 10.1038/nrmicro.2016.142. [DOI] [PubMed] [Google Scholar]
- Campione E, Cosio T, Rosa L, Lanna C, Di Girolamo S, Gaziano R, Valenti P, Bianchi L. Lactoferrin as protective natural barrier of respiratory and intestinal mucosa against coronavirus infection and inflammation. Int J Mol Sci. 2020;21(14):4903. doi: 10.3390/ijms21144903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campione E, Lanna C, Cosio T, Rosa L, Conte MP, Iacovelli F, Romeo A, Falconi M, Del Vecchio C, Franchin E, Lia MS, Minieri M, Chiaramonte C, Ciotti M, Nuccetelli M, Terrinoni A, Iannuzzi I, Coppeda L, Magrini A, Bernardini S, Sabatini S, Rosapepe F, Bartoletti PL, Moricca N, Di Lorenzo A, Andreoni M, Sarmati L, Miani A, Piscitelli P, Valenti P, Bianchi L. Lactoferrin against SARS-CoV-2 in vitro and in silico evidences. Front Pharmacol. 2021;12:666600. doi: 10.3389/fphar.2021.666600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campione E, Lanna C, Cosio T, Rosa L, Conte MP, Iacovelli F, Romeo A, Falconi M, Del Vecchio C, Franchin E, Lia MS, Minieri M, Chiaramonte C, Ciotti M, Nuccetelli M, Terrinoni A, Iannuzzi I, Coppeta L, Magrini A, Bernardini S, Sabatini S, Rosapepe F, Bartoletti PL, Moricca N, Di Lorenzo A, Andreoni M, Sarmati L, Miani A, Piscitelli P, Squillaci E, Valenti P, Bianchi L. Lactoferrin as antiviral treatment in COVID-19 management: preliminary evidence. Int J Environ Res Public Health. 2021;18(20):10985. doi: 10.3390/ijerph182010985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang R, Ng TB, Sun WZ. Lactoferrin as potential preventative and adjunct treatment for COVID-19. Int J Antimicrob Agents. 2020;56:106118. doi: 10.1016/j.ijantimicag.2020.106118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng L, Li H, Li L, Liu C, Yan S, Chen H, Li Y. Ferritin in the coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. J Clin Lab Anal. 2020;34(10):e23618. doi: 10.1002/jcla.23618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey R, Ganz T. Iron homeostasis—an anthropocentric perspective. J Biol Chem. 2017;292(31):12727–12734. doi: 10.1074/jbc.R117.781823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18(6):1421–1424. doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutone A, Frioni A, Berlutti F, Valenti P, Musci G, Bonaccorsi di Patti MC. Lactoferrin prevents LPS-induced decrease of the iron exporter ferroportin in human monocytes/macrophages. Biometals. 2014;27(5):807–813. doi: 10.1007/s10534-014-9742-7. [DOI] [PubMed] [Google Scholar]
- Cutone A, Rosa L, Lepanto MS, Scotti MJ, Berlutti F, Bonaccorsi di Patti MC, Musci G, Valenti P. Lactoferrin efficiently counteracts the inflammation-induced changes of the iron homeostasis system in macrophages. Front Immunol. 2017;8:705. doi: 10.3389/fimmu.2017.00705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutone A, Lepanto MS, Rosa L, Scotti MJ, Rossi A, Ranucci S, De Fino I, Bragonzi A, Valenti P, Musci G, Berlutti F. Aerosolized bovine lactoferrin counteracts infection, inflammation and iron dysbalance in a cystic fibrosis mouse model of Pseudomonas aeruginosa chronic lung infection. Int J Mol Sci. 2019;20(9):2128. doi: 10.3390/ijms20092128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai M, Pan P, Li H, Liu S, Zhang L, Song C, Li Y, Li Q, Mao Z, Long Y, Su X, Hu C. The antimicrobial cathelicidin peptide hlF(1–11) attenuates alveolar macrophage pyroptosis induced by Acinetobacter baumannii in vivo. Exp Cell Res. 2018;364(1):95–103. doi: 10.1016/j.yexcr.2018.01.035. [DOI] [PubMed] [Google Scholar]
- Dai J, Teng X, Jin S, Wu Y. The Antiviral roles of hydrogen sulfide by blocking the interaction between SARS-CoV-2 and its potential cell surface receptors. Oxid Med Cell Longev. 2021;2021:7866992. doi: 10.1155/2021/7866992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denani CB, Real-Hohn A, de Carvalho CAM, Gomes AMO, Gonçalves RB. Lactoferrin affects rhinovirus B-14 entry into H1-HeLa cells. Arch Virol. 2021;166(4):1203–1211. doi: 10.1007/s00705-021-04993-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deriu E, Boxx GM, He X, Pan C, Benavidez SD, Cen L, Rozengurt N, Shi W, Cheng G. Influenza virus affects intestinal microbiota and secondary Salmonella infection in the gut through Type I Interferons. PloS Pathog. 2016;12:e1005572. doi: 10.1371/journal.ppat.1005572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan A, Lima CA, Pinkus JL, Pinkus GS, Zon LI, Robine S, Andrews NC. The iron exporter ferroportin/Slc40a1 is essential for iron homeostasis. Cell Metab. 2005;1:191–200. doi: 10.1016/j.cmet.2005.01.003. [DOI] [PubMed] [Google Scholar]
- Drakesmith H, Prentice A. Viral infection and iron metabolism. Nat Rev Microbiol. 2008;6(7):541–552. doi: 10.1038/nrmicro1930. [DOI] [PubMed] [Google Scholar]
- Ehsani S. COVID-19 and iron dysregulation: distant sequence similarity between hepcidin and the novel coronavirus spike glycoprotein. Biol Direct. 2020;15(1):19. doi: 10.1186/s13062-020-00275-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enaud R, Prevel R, Ciarlo E, Beaufils F, Wieërs G, Guery B, Delhaes L. The gut- lung axis in health and respiratory diseases: a place for inter-organ and inter-kingdom crosstalks. Front Cell Infect Microbiol. 2020;10:9. doi: 10.3389/fcimb.2020.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Food Safety Authority Scientific opinion on bovine lactoferrin. EFSA J. 2012;10:2701. doi: 10.2903/j.efsa.2012.2701. [DOI] [Google Scholar]
- U.S. FDA (2014) GRN 000465 Cow’s Milk-Derived Lactoferrin; Morinaga Milk Industry Co., Ltd.: Tokyo, Japan; U.S. Food and Drug Administration (U.S. FDA), Center for Food Safety & Applied Nutrition (CFSAN), Office of Food Additive Safety: Silver Spring, MD, USA. http://www.accessdata.fda.gov/scripts/fdcc/index.cfm?set=GRASNotices&id=465 Accessed 06 April 2022
- Fernandez-Musoles R, Salom JB, Martínez-Maqueda D, López-Díez JJ, Recio I, Manzanares P, Antihypertensive effects of lactoferrin hydrolyzates: inhibition of angiotensin- and endothelin-converting enzymes. Food Chem. 2013;139(1–4):994–1000. doi: 10.1016/j.foodchem.2012.12.049. [DOI] [PubMed] [Google Scholar]
- Figueroa-Lozano S, Valk-Weeber RL, van Leeuwen SS, Dijkhuizen L, de Vos P. Dietary N-Glycans from bovine lactoferrin and TLR modulation. Mol Nutr Food Res. 2018;62(2):1700389. doi: 10.1002/mnfr.201700389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8(7):681–686. doi: 10.1016/S2213-2600(20)30243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazer DM, Anderson GJ. The orchestration of body iron intake: How and where do enterocytes receive their cues? Blood Cells Mol Dis. 2003;30(3):288–297. doi: 10.1016/s1079-9796(03)00039-1. [DOI] [PubMed] [Google Scholar]
- Frioni A, Conte MP, Cutone A, Longhi C, Musci G, di Patti MC, Natalizi T, Marazzato M, Lepanto MS, Puddu P, Paesano R, Valenti P, Berlutti F. Lactoferrin differently modulates the inflammatory response in epithelial models mimicking human inflammatory and infectious diseases. Biometals. 2014;27(5):843–856. doi: 10.1007/s10534-014-9740-9. [DOI] [PubMed] [Google Scholar]
- Fujihara T, Hayashi K. Lactoferrin inhibits herpes simplex virus type-1 (HSV-1) infection to mouse cornea. Arch Virol. 1995;140(8):1469–1472. doi: 10.1007/BF01322673. [DOI] [PubMed] [Google Scholar]
- Furlund CB, Kristoffersen AB, Devold TG, Vegarud GE, Jonassen CM. Bovine lactoferrin digested with human gastrointestinal enzymes inhibits replication of human echovirus 5 in cell culture. Nutr Res. 2012;32(7):503–513. doi: 10.1016/j.nutres.2012.06.006. [DOI] [PubMed] [Google Scholar]
- Furmanski P, Li ZP, Fortuna MB, Swamy CV, Das MR. Multiple molecular forms of human lactoferrin. Identification of a class of lactoferrins that possess ribonuclease activity and lack iron-binding capacity. J Exp Med. 1989;170:415–429. doi: 10.1084/jem.170.2.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giobbe GG, Bonfante F, Jones BC, Gagliano O, Luni C, Zambaiti E, Perin S, Laterza C, Busslinger G, Stuart H, Pagliari M, Bortolami A, Mazzetto E, Manfredi A, Colantuono C, Di Filippo L, Pellegata AF, Panzarin V, Thapar N, Li VSW, Eaton S, Cacchiarelli D, Clevers H, Elvassore N, De Coppi P. SARS-CoV-2 infection and replication in human gastric organoids. Nat Commun. 2021;12(1):6610. doi: 10.1038/s41467-021-26762-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grier A, McDavid A, Wang B, Qiu X, Java J, Bandyopadhyay S, Yang H, Holden-Wiltse J, Kessler HA, Gill AL, Huyck H, Falsey AR, Topham DJ, Scheible KM, Caserta MT, Pryhuber GS, Gill SR. Neonatal gut and respiratory microbiota: coordinated development through time and space. Microbiome. 2018;6:193. doi: 10.1186/s40168-018-0566-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groot F, Geijtenbeek TB, Sanders RW, Baldwin CE, Sanchez-Hernandez M, Floris R, van Kooyk Y, de Jong EC, Berkhout B. Lactoferrin prevents dendritic cell-mediated human immunodeficiency virus type 1 transmission by blocking the DC-SIGN–gp120 interaction. J Virol. 2005;79(5):3009–3015. doi: 10.1128/JVI.79.5.3009-3015.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groves ML. The isolation of a red protein from milk. J Am Chem Soc. 1960;82:3345–3350. doi: 10.1021/ja01498a029. [DOI] [Google Scholar]
- Groves HT, Cuthbertson L, James P, Moffatt MF, Cox MJ, Tregoning JS. Respiratory disease following viral lung infection alters the murine gut microbiota. Front Immunol. 2018;9:182. doi: 10.3389/fimmu.2018.00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gualdi L, Mertz S, Gomez AM, Ramilo O, Wittke A, Mejias A. Lack of effect of bovine lactoferrin in respiratory syncytial virus replication and clinical disease severity in the mouse model. Antiviral Res. 2013;99(2):188–195. doi: 10.1016/j.antiviral.2013.05.013. [DOI] [PubMed] [Google Scholar]
- Hanada S, Pirzadeh M, Carver KY, Deng JC. Respiratory viral infection-induced microbiome alterations and secondary bacterial pneumonia. Front Immunol. 2018;9:2640. doi: 10.3389/fimmu.2018.02640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartenian E, Nandakumar D, Lari A, Ly M, Tucker JM, Glaunsinger BA. The molecular virology of coronaviruses. J Biol Chem. 2020;295(37):12910–12934. doi: 10.1074/jbc.REV120.013930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatmal MM, Alshaer W, Al-Hatamleh MAI, Hatmal M, Smadi O, Taha MO, Oweida AJ, Boer JC, Mohamud R, Plebanski M. Comprehensive structural and molecular comparison of spike proteins of SARS-CoV-2, SARS-CoV and MERS-CoV, and their interactions with ACE2. Cells. 2020;9(12):2638. doi: 10.3390/cells9122638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirashima N, Orito E, Ohba K, Kondo H, Sakamoto T, Matsunaga S, Kato A, Nukaya H, Sakakibara K, Ohno T, Kato H, Sugauchi F, Kato T, Tanaka Y, Ueda R, Mizokami M. A randomized controlled trial of consensus interferon with or without lactoferrin for chronic hepatitis C patients with genotype 1b and high viral load. Hepatol Res. 2004;29(1):9–12. doi: 10.1016/j.hepres.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Hu Y, Meng X, Zhang F, Xiang Y, Wang J. The in vitro antiviral activity of lactoferrin against common human coronaviruses and SARS-CoV-2 is mediated by targeting the heparan sulfate co-receptor. Emerg Microbes Infect. 2021;10(1):317–330. doi: 10.1080/22221751.2021.1888660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter HN, Fulton DB, Ganz T, Vogel HJ. The solution structure of human hepcidin, a peptide hormone with antimicrobial activity that is involved in iron uptake and hereditary hemochromatosis. J Biol Chem. 2002;277(40):37597–37603. doi: 10.1074/jbc.M205305200. [DOI] [PubMed] [Google Scholar]
- Hussain I, Cher GLY, Abid MA, Abid MB. Role of gut microbiome in COVID-19: an insight into pathogenesis and therapeutic potential. Front Immunol. 2021;12:765965. doi: 10.3389/fimmu.2021.765965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ichinohe T, Pang IK, Kumamoto Y, Peaper DR, Ho JH, Murray TS, Iwasaki A. Microbiota regulates immune defense against respiratory tract Influenza A virus infection. Proc Natl Acad Sci U S A. 2011;108:5354–5359. doi: 10.1073/pnas.1019378108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishibashi Y, Takeda K, Tsukidate N, Miyazaki H, Ohira K, Dosaka-Akita H, Nishimura M. Randomized placebo-controlled trial of interferon alpha-2b plus ribavirin with and without lactoferrin for chronic hepatitis C. Hepatol Res. 2005;32(4):218–223. doi: 10.1016/j.hepres.2005.03.018. [DOI] [PubMed] [Google Scholar]
- Johansson B. Isolation of an iron-containing red protein from human milk. Acta Chem Scand. 1960;14:510–512. doi: 10.3891/acta.chem.scand.14-0510. [DOI] [Google Scholar]
- Kalashnyk O, Petrova Y, Lykhmus O, Mikhalovska L, Mikhalovsky S, Zhukova A, Gnatenko D, Bahou W, Komisarenko S, Skok M. Expression, function and cooperating partners of protease-activated receptor type 3 in vascular endothelial cells and B lymphocytes studied with specific monoclonal antibody. Mol Immunol. 2013;54(3–4):319–326. doi: 10.1016/j.molimm.2012.12.021. [DOI] [PubMed] [Google Scholar]
- Ke Z, Oton J, Qu K, Cortese M, Zila V, McKeane L, Nakane T, Zivanov J, Neufeldt CJ, Cerikan B, Lu JM, Peukes J, Xiong X, Kräusslich HG, Scheres SHW, Bartenschlager R, Briggs JAG. Structures and distributions of SARS-CoV-2 spike proteins on intact virions. Nature. 2020;588(7838):498–502. doi: 10.1038/s41586-020-2665-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kell DB, Heyden EL, Pretorius E. The Biology of lactoferrin, an iron-binding protein that can help defend against viruses and bacteria. Front Immunol. 2020;11:1221. doi: 10.3389/fimmu.2020.01221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause A, Neitz S, Magert HJ, Schulz A, Forssmann WG, Schulz-Knappe P, Adermann K. LEAP-1, a novel highly disulfidebonded human peptide, exhibits antimicrobial activity. FEBS Lett. 2000;480(2–3):147–150. doi: 10.1016/s0014-5793(00)01920-7. [DOI] [PubMed] [Google Scholar]
- Kruzel ML, Actor JK, Boldogh I, Zimecki M. Lactoferrin in health and disease. Postepy Hig Med Dosw. 2007;61:261–267. [PubMed] [Google Scholar]
- Kruzel ML, Zimecki M, Actor JK. Lactoferrin in a context of inflammation-induced pathology. Front Immunol. 2017;8:1438. doi: 10.3389/fimmu.2017.01438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhara T, Yamauchi K, Tamura Y, Okamura H. Oral administration of lactoferrin increases NK cell activity in mice via increased production of IL-18 and type I IFN in the small intestine. J Interferon Cytokine Res. 2006;26(7):489–499. doi: 10.1089/jir.2006.26.489. [DOI] [PubMed] [Google Scholar]
- Lang J, Yang N, Deng J, Liu K, Yang P, Zhang G, Jiang C. Inhibition of SARS pseudovirus cell entry by lactoferrin binding to heparan sulfate proteoglycans. PLoS ONE. 2011;6(8):e23710. doi: 10.1371/journal.pone.0023710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latz E, Xiao TS, Stutz A. Activation and regulation of the inflammasomes. Nat Rev Immunol. 2013;13(6):397–411. doi: 10.1038/nri3452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee P, Peng H, Gelbart T, Wang L, Beutler E. Regulation of hepcidin transcription by interleukin-1 and interleukin-6. Proc Natl Acad Sci USA. 2005;102(6):1906–1910. doi: 10.1073/pnas.0409808102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legrand D, Mazurier J. A critical review of the roles of host lactoferrin in immunity. Biometals. 2010;23(3):365–376. doi: 10.1007/s10534-010-9297-1. [DOI] [PubMed] [Google Scholar]
- Legrand D, Elass E, Carpentier M, Mazurier J. Lactoferrin: a modulator of immune and inflammatory responses. Cell Mol Life Sci. 2005;62(22):2549–2559. doi: 10.1007/s00018-005-5370-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepanto MS, Rosa L, Cutone A, Conte MP, Paesano R, Valenti P. Efficacy of lactoferrin oral administration in the treatment of anemia and anemia of inflammation in pregnant and non-pregnant women: an interventional study. Front Immunol. 2018;9:2123. doi: 10.3389/fimmu.2018.02123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leveugle B, Mazurier J, Legrand D, Mazurier C, Montreuil J, Spik G. Lactotransferrin binding to its platelet receptor inhibits platelet aggregation. Eur J Biochem. 1993;213(3):1205–1211. doi: 10.1111/j.1432-1033.1993.tb17871.x. [DOI] [PubMed] [Google Scholar]
- Lin TY, Chu C, Chiu CH. Lactoferrin inhibits enterovirus 71 infection of human embryonal rhabdomyosarcoma cells in vitro. J Infect Dis. 2002;186(8):1161–1164. doi: 10.1086/343809. [DOI] [PubMed] [Google Scholar]
- Liu TFD, Philippou E, Kolokotroni O, Siakallis G, Rahima K, Constantinou C. Gut and airway microbiota and their role in COVID-19 infection and pathogenesis: a scoping review. Infection. 2021;20:1–33. doi: 10.1007/s15010-021-01715-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longstaff C, Kolev K. Basic mechanisms and regulation of fibrinolysis. J Thromb Haemost. 2015;13(Suppl 1):S98–105. doi: 10.1111/jth.12935. [DOI] [PubMed] [Google Scholar]
- Lu L, Hangoc G, Oliff A, Chen LT, Shen RN, Broxmeyer HE. Protective influence of lactoferrin on mice infected with the polycythemia-inducing strain of Friend virus complex. Cancer Res. 1987;47(15):4184–4188. [PubMed] [Google Scholar]
- Mancinelli R, Rosa L, Cutone A, Lepanto MS, Franchitto A, Onori P, Gaudio E, Valenti P. Viral hepatitis and iron dysregulation: molecular pathways and the role of lactoferrin. Molecules. 2020;25(8):1997. doi: 10.3390/molecules25081997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangan MSJ, Olhava EJ, Roush WR, Seidel HM, Glick GD, Latz E. Targeting the NLRP3 inflammasome in inflammatory diseases. Nat Rev Drug Discov. 2018;17(9):688. doi: 10.1038/nrd.2018.149. [DOI] [PubMed] [Google Scholar]
- Marchetti M, Longhi C, Conte MP, Pisani S, Valenti P, Seganti L. Lactoferrin inhibits herpes simplex virus type 1 adsorption to Vero cells. Antiviral Res. 1996;29(2–3):221–231. doi: 10.1016/0166-3542(95)00840-3. [DOI] [PubMed] [Google Scholar]
- Marchetti M, Pisani S, Antonini G, Valenti P, Seganti L, Orsi N. Metal complexes of bovine lactoferrin inhibit in vitro replication of herpes simplex virus type 1 and 2. Biometals. 1998;11:89–94. doi: 10.1023/a:1009217709851. [DOI] [PubMed] [Google Scholar]
- Marchetti M, Superti F, Ammendolia MG, Rossi P, Valenti P, Seganti L. Inhibition of poliovirus type 1 infection by iron-, manganese- and zinc-saturated lactoferrin. Med Microbiol Immunol. 1999;187(4):199–204. doi: 10.1007/s004300050093. [DOI] [PubMed] [Google Scholar]
- Marchetti M, Ammendolia MG, Superti F. Glycosaminoglycans are not indispensable for the anti-herpes simplex virus type 2 activity of lactoferrin. Biochimie. 2009;91(1):155–159. doi: 10.1016/j.biochi.2008.04.015. [DOI] [PubMed] [Google Scholar]
- Miller JL. Iron deficiency anemia: A common and curable disease. Cold Spring Harb Perspect Med. 2012;3(7):a011866. doi: 10.1101/cshperspect.a011866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miotto M, Di Rienzo L, Bò L, Boffi A, Ruocco G, Milanetti E. Molecular mechanisms behind anti SARS-CoV-2 action of lactoferrin. Front Mol Biosci. 2021;8:607443. doi: 10.3389/fmolb.2021.607443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirabelli C, Wotring JW, Zhang CJ, McCarty SM, Fursmidt R, Pretto CD, Qiao Y, Zhang Y, Frum T, Kadambi NS, Amin AT, O'Meara TR, Spence JR, Huang J, Alysandratos KD, Kotton DN, Handelman SK, Wobus CE, Weatherwax KJ, Mashour GA, O'Meara MJ, Chinnaiyan AM, Sexton JZ. Morphological cell profiling of SARS-CoV-2 infection identifies drug repurposing candidates for COVID-19. Proc Natl Acad Sci U S A. 2021;118(36):e2105815118. doi: 10.1073/pnas.2105815118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montreuil J, Tonnelat J, Mullet S. Preparation and properties of lactosiderophilin (lactotransferrin) of human milk. Biochim Biophys Acta. 1960;45:413–421. doi: 10.1016/0006-3002(60)91478-5. [DOI] [PubMed] [Google Scholar]
- Motoki N, Mizuki M, Tsukahara T, Miyakawa M, Kubo S, Oda H, Tanaka M, Yamauchi K, Abe F, Nomiyama T. Effects of lactoferrin-fortified formula on acute gastrointestinal symptoms in children aged 12–32 months: a randomized, double-blind. Placebo-Controlled Trial Front Pediatr. 2020;8:233. doi: 10.3389/fped.2020.00233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nai A, Lorè NI, Pagani A, De Lorenzo R, Di Modica S, Saliu F, Cirillo DM, Rovere-Querini P, Manfredi AA, Silvestri L. Hepcidin levels predict Covid-19 severity and mortality in a cohort of hospitalized Italian patients. Am J Hematol. 2021;96(1):E32–E35. doi: 10.1002/ajh.26027. [DOI] [PubMed] [Google Scholar]
- Naidu SAG, Clemens RA, Pressman P, Zaigham M, Davies KJA, Naidu AS. COVID-19 during pregnancy and postpartum. J Diet Suppl. 2022;19(1):78–114. doi: 10.1080/19390211.2020.1834047. [DOI] [PubMed] [Google Scholar]
- Nemeth E, Rivera S, Gabayan V, Keller C, Taudorf S, Pedersen BK, Ganz T. IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J Clin Investig. 2004;113(9):1271–1276. doi: 10.1172/JCI20945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng TB, Cheung RC, Wong JH, Wang Y, Ip DT, Wan DC, Xia J. Antiviral activities of whey proteins. Appl Microbiol Biotechnol. 2015;99(17):6997–7008. doi: 10.1007/s00253-015-6818-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oda H, Wakabayashi H, Tanaka M, Yamauchi K, Sugita C, Yoshida H, Abe F, Sonoda T, Kurokawa M. Effects of lactoferrin on infectious diseases in Japanese summer: a randomized, double-blinded, placebo-controlled trial. J Microbiol Immunol Infect. 2021;54(4):566–574. doi: 10.1016/j.jmii.2020.02.010. [DOI] [PubMed] [Google Scholar]
- Okada S, Tanaka K, Sato T, Ueno H, Saito S, Okusaka T, Sato K, Yamamoto S, Kakizoe T. Dose-response trial of lactoferrin in patients with chronic hepatitis C. Jpn J Cancer Res. 2002;93(9):1063–1069. doi: 10.1111/j.1349-7006.2002.tb02484.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paesano R, Berlutti F, Pietropaoli M, Goolsbee W, Pacifici E, Valenti P. Lactoferrin efficacy versus ferrous sulfate in curing iron disorders in pregnant and non-pregnant women. Int J Immunopathol Pharmacol. 2010;23(2):577–587. doi: 10.1177/039463201002300220. [DOI] [PubMed] [Google Scholar]
- Paesano R, Natalizi T, Berlutti F, Valenti P. Body iron delocalization: the serious drawback in iron disorders in both developing and developed countries. Pathog Glob Health. 2012;106:200–216. doi: 10.1179/2047773212Y.0000000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan P, Zhang Q, Liu W, Wang W, Lao Z, Zhang W, Shen M, Wan P, Xiao F, Liu F, Zhang W, Tan Q, Liu X, Wu K, Liu Y, Li G, Wu J. Dengue virus M protein promotes NLRP3 Inflammasome activation to induce vascular leakage in mice. J Virol. 2019;93(21):e00996–e1019. doi: 10.1128/JVI.00996-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan P, Shen M, Yu Z, Ge W, Chen K, Tian M, Xiao F, Wang Z, Wang J, Jia Y, Wang W, Wan P, Zhang J, Chen W, Lei Z, Chen X, Luo Z, Zhang Q, Xu M, Li G, Li Y, Wu J. SARS-CoV-2 N protein promotes NLRP3 inflammasome activation to induce hyperinflammation. Nat Commun. 2021;12(1):5306. doi: 10.1038/s41467-021-25629-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park CH, Valore EV, Waring AJ, Ganz T. Hepcidin, a urinary antimicrobial peptide synthesized in the liver. J Biol Chem. 2001;276(11):7806–7810. doi: 10.1074/jbc.M008922200. [DOI] [PubMed] [Google Scholar]
- Pérez-Cano FJ, Marín-Gallén S, Castell M, Rodríguez-Palmero M, Rivero M, Castellote C, Franch AJ. Supplementing suckling rats with whey protein concentrate modulates the immune response and ameliorates rat rotavirus-induced diarrhea. Nutr. 2008;138(12):2392–2398. doi: 10.3945/jn.108.093856. [DOI] [PubMed] [Google Scholar]
- Perricone C, Bartoloni E, Bursi R, Cafaro G, Guidelli GM, Shoenfeld Y, Gerli R. COVID-19 as part of the hyperferritinemic syndromes: the role of iron depletion therapy. Immunol Res. 2020;68(4):213–224. doi: 10.1007/s12026-020-09145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrantoni A, Di Biase AM, Tinari A, Marchetti M, Valenti P, Seganti L, Superti F. Bovine lactoferrin inhibits adenovirus infection by interacting with viral structural polypeptides. Antimicrob Agents Chemother. 2003;47(8):2688–2691. doi: 10.1128/AAC.47.8.2688-2691.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrantoni A, Dofrelli E, Tinari A, Ammendolia MG, Puzelli S, Fabiani C, Donatelli I, Superti F. Bovine lactoferrin inhibits influenza A virus induced programmed cell death in vitro. Biometals. 2010;23(3):465–475. doi: 10.1007/s10534-010-9323-3. [DOI] [PubMed] [Google Scholar]
- Pietrantoni A, Ammendolia MG, Superti F. Bovine lactoferrin: involvement of metal saturation and carbohydrates in the inhibition of influenza virus infection. Biochem Cell Biol. 2012;90(3):442–448. doi: 10.1139/o11-072. [DOI] [PubMed] [Google Scholar]
- Puddu P, Borghi P, Gessani S, Valenti P, Belardelli F, Seganti L. Antiviral effect of bovine lactoferrin saturated with metal ions on early steps of human immunodeficiency virus type 1 infection. Int J Biochem Cell Biol. 1998;30:1055–1062. doi: 10.1016/s1357-2725(98)00066-1. [DOI] [PubMed] [Google Scholar]
- Puddu P, Valenti P, Gessani S. Immunomodulatory effects of lactoferrin on antigen presenting cells. Biochimie. 2009;91:11–18. doi: 10.1016/j.biochi.2008.05.005. [DOI] [PubMed] [Google Scholar]
- Puddu P, Latorre D, Carollo M, Catizone A, Ricci G, Valenti P, Gessani S. Bovine lactoferrin counteracts toll-like receptor mediated activation signals in antigen presenting cells. PLoS ONE. 2011;6:e22504. doi: 10.1371/journal.pone.0022504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian ZY, Jollès P, Migliore-Samour D, Fiat AM. Isolation and characterization of sheep lactoferrin, an inhibitor of platelet aggregation and comparison with human lactoferrin. Biochim Biophys Acta. 1995;1243(1):25–32. doi: 10.1016/0304-4165(94)00126-i. [DOI] [PubMed] [Google Scholar]
- Qiao B, Sugianto P, Fung E, Del-Castillo-Rueda A, Moran-Jimenez MJ, Ganz T. Nemeth E (2012) Hepcidin-induced endocytosis of ferroportin is dependent on ferroportin ubiquitination. Cell Metab. 2012;15:918–924. doi: 10.1016/j.cmet.2012.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa L, Cutone A, Lepanto MS, Paesano R, Valenti P. Lactoferrin: a natural glycoprotein involved in iron and inflammatory homeostasis. Int J Mol Sci. 2017;18(9):1985. doi: 10.3390/ijms18091985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa L, Tripepi G, Naldi E, Aimati M, Santangeli S, Venditto F, Caldarelli M, Valenti P. Ambulatory COVID-19 patients treated with lactoferrin as a supplementary antiviral agent: a preliminary study. J Clin Med. 2021;10(18):4276. doi: 10.3390/jcm10184276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sano H, Nagai K, Tsutsumi H, Kuroki Y. Lactoferrin and surfactant protein a exhibit distinct binding specificity to F protein and differently modulate respiratory syncytial virus infection. Eur J Immunol. 2003;33(10):2894–2902. doi: 10.1002/eji.200324218. [DOI] [PubMed] [Google Scholar]
- Serrano G, Kochergina I, Albors A, Diaz E, Oroval M, Hueso G, Serrano JM. Liposomal lactoferrin as potential preventative and cure for COVID-19. Int J Res Health Sci. 2020;8(1):8–15. doi: 10.5530/ijrhs.8.1.3. [DOI] [Google Scholar]
- Sherman MP, Pritzl CJ, Xia C, Miller MM, Zaghouani H, Hahm B. Lactoferrin acts as an adjuvant during influenza vaccination of neonatal mice. Biochem Biophys Res Commun. 2015;467(4):766–770. doi: 10.1016/j.bbrc.2015.10.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizu K, Matsuzawa H, Okada K, Tazume S, Dosako S, Kawasaki Y, Hashimoto K, Koga Y. Lactoferrin-mediated protection of the host from murine cytomegalovirus infection by a T-cell-dependent augmentation of natural killer cell activity. Arch Virol. 1996;141(10):1875–1889. doi: 10.1007/BF01718201. [DOI] [PubMed] [Google Scholar]
- Shin K, Wakabayashi H, Yamauchi K, Teraguchi S, Tamura Y, Kurokawa M, Shiraki K. Effects of orally administered bovine lactoferrin and lactoperoxidase on influenza virus infection in mice. J Med Microbiol. 2005;54(Pt 8):717–723. doi: 10.1099/jmm.0.46018-0. [DOI] [PubMed] [Google Scholar]
- Sienkiewicz M, Jaśkiewicz A, Tarasiuk A, Fichna J. Lactoferrin: an overview of its main functions, immunomodulatory and antimicrobial role, and clinical significance. Crit Rev Food Sci Nutr. 2021;8:1–18. doi: 10.1080/10408398.2021.1895063. [DOI] [PubMed] [Google Scholar]
- Simpson RJ. Aging and inflammation: directing traffic through physical activity. Brain Behav Immun. 2016;56:10–11. doi: 10.1016/j.bbi.2016.05.015. [DOI] [PubMed] [Google Scholar]
- Skendros P, Mitsios A, Chrysanthopoulou A, Mastellos DC, Metallidis S, Rafailidis P, Ntinopoulou M, Sertaridou E, Tsironidou V, Tsigalou C, Tektonidou M, Konstantinidis T, Papagoras C, Mitroulis I, Germanidis G, Lambris JD, Ritis K. Complement and tissue factor-enriched neutrophil extracellular traps are key drivers in COVID-19 immunothrombosis. J Clin Invest. 2020;130(11):6151–6157. doi: 10.1172/JCI141374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spik G, Coddeville B, Mazurier J, Bourne Y, Cambillaut C, Montreuil J. Primary and three-dimensional structure of lactotransferrin (lactoferrin) glycans. Adv Exp Med Biol. 1994;357:21–32. doi: 10.1007/978-1-4615-2548-6_3. [DOI] [PubMed] [Google Scholar]
- Stefanescu BM, Hétu C, Slaughter JC, O'Shea TM, Shetty AK. A pilot study of Biotene OralBalance® gel for oral care in mechanically ventilated preterm neonates. Contemp Clin Trials. 2013;35(2):33–39. doi: 10.1016/j.cct.2013.03.010. [DOI] [PubMed] [Google Scholar]
- Superti F. Lactoferrin from bovine milk: a protective companion for Life. Nutrients. 2020;12(9):2562. doi: 10.3390/nu12092562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Superti F, Ammendolia MG, Valenti P, Seganti L. Antirotaviral activity of milk proteins: lactoferrin prevents rotavirus infection in the enterocyte-like cell line HT-29. Med Microbiol Immunol. 1997;186(2–3):83–91. doi: 10.1007/s004300050049. [DOI] [PubMed] [Google Scholar]
- Superti F, Siciliano R, Rega B, Giansanti F, Valenti P, Antonini G. Involvement of bovine lactoferrin metal saturation, sialic acid and protein fragments in the inhibition of rotavirus infection. Biochim Biophys Acta. 2001;1528(2–3):107–115. doi: 10.1016/s0304-4165(01)00178-7. [DOI] [PubMed] [Google Scholar]
- Swart PJ, Kuipers ME, Smit C, Pauwels R, deBéthune MP, de Clercq E, Meijer DK, Huisman JG. Antiviral effects of milk proteins: acylation results in polyanionic compounds with potent activity against human immunodeficiency virus types 1 and 2 in vitro. AIDS Res Hum Retroviruses. 1996;12(9):769–775. doi: 10.1089/aid.1996.12.769. [DOI] [PubMed] [Google Scholar]
- Szabo G, Petrasek J. Inflammasome activation and function in liver disease. Nat Rev Gastroenterol Hepatol. 2015;12(7):387–400. doi: 10.1038/nrgastro.2015.94. [DOI] [PubMed] [Google Scholar]
- Taha SH, Mehrez MA, Sitohy MZ, Abou Dawood AG, Abd-El Hamid MM, Kilany WH. Effectiveness of esterified whey proteins fractions against Egyptian Lethal Avian Influenza A (H5N1) Virol J. 2010;7:330. doi: 10.1186/1743-422X-7-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka K, Ikeda M, Nozaki A, Kato N, Tsuda H, Saito S, Sekihara H. Lactoferrin inhibits hepatitis C virus viremia in patients with chronic hepatitis C: a pilot study. Jpn J Cancer Res. 1999;90(4):367–371. doi: 10.1111/j.1349-7006.1999.tb00756.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang X, Yang M, Duan Z, Liao Z, Liu L, Cheng R, Fang M, Wang G, Liu H, Xu J, Kamau PM, Zhang Z, Yang L, Zhao X, Peng X, Lai R. Transferrin receptor is another receptor for SARS-CoV-2 entry. bioRxiv. 2020 doi: 10.1101/2020.10.23.350348. [DOI] [Google Scholar]
- Tian S, Hu W, Niu L, Liu H, Xu H, Xiao SY. Pulmonary pathology of early-phase 2019 novel Coronavirus (COVID-19) Pneumonia in two patients with lung cancer. J Thorac Oncol. 2020;15(5):700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinari A, Pietrantoni A, Ammendolia MG, Valenti P, Superti F. Inhibitory activity of bovine lactoferrin against echovirus induced programmed cell death in vitro. Int J Antimicrob Agents. 2005;25(5):433–438. doi: 10.1016/j.ijantimicag.2005.02.011. [DOI] [PubMed] [Google Scholar]
- Toldo S, Bussani R, Nuzzi V, Bonaventura A, Mauro AG, Cannatà A, Pillappa R, Sinagra G, Nana-Sinkam P, Sime P, Abbate A. Inflammasome formation in the lungs of patients with fatal COVID-19. Inflamm Res. 2021;70(1):7–10. doi: 10.1007/s00011-020-01413-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueno H, Sato T, Yamamoto S, Tanaka K, Ohkawa S, Takagi H, Yokosuka O, Furuse J, Saito H, Sawaki A, Kasugai H, Osaki Y, Fujiyama S, Sato K, Wakabayashi K, Okusaka T. Randomized, double-blind, placebo-controlled trial of bovine lactoferrin in patients with chronic hepatitis C. Cancer Sci. 2006;97(10):1105–1110. doi: 10.1111/j.1349-7006.2006.00274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valenti P, Antonini G. Lactoferrin: an important host defence against microbial and viral attack. Cell Mol Life Sci. 2005;62(22):2576–2587. doi: 10.1007/s00018-005-5372-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valenti P, Rosa L, Capobianco D, Lepanto MS, Schiavi E, Cutone A, Paesano R, Mastromarino P. Role of Lactobacilli and Lactoferrin in the Mucosal Cervicovaginal Defense. Front Immunol. 2018;9:376. doi: 10.3389/fimmu.2018.00376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Splunter M, Perdijk O, Fick-Brinkhof H, Feitsma AL, Floris-Vollenbroek EG, Meijer B, Brugman S, Savelkoul HFJ, van Hoffen E, van Neerven RJJ. Bovine lactoferrin enhances TLR7-mediated responses in plasmacytoid dendritic cells in elderly women: results from a nutritional intervention study with bovine lactoferrin. GOS Vitamin d Front Immunol. 2018;9:2677. doi: 10.3389/fimmu.2018.02677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Veen HA, Geerts ME, van Berkel PH, Nuijens JH. The role of N-linked glycosylation in the protection of human and bovine lactoferrin against tryptic proteolysis. Eur J Biochem. 2004;271(4):678–684. doi: 10.1111/j.1432-1033.2003.03965.x. [DOI] [PubMed] [Google Scholar]
- Verga Falzacappa MV, Vujic Spasic M, Kessler R, Stolte J, Hentze MW, Muckenthaler MU. STAT3 mediates hepatic hepcidin expression and its inflammatory stimulation. Blood. 2007;109(1):353–358. doi: 10.1182/blood-2006-07-033969. [DOI] [PubMed] [Google Scholar]
- Vitetta L, Coulson S, Beck SL, Gramotnev H, Du S, Lewis S. The clinical efficacy of a bovine lactoferrin/whey protein Ig-rich fraction (Lf/IgF) for the common cold: a double blind randomized study. Complement Ther Med. 2013;21(3):164–171. doi: 10.1016/j.ctim.2012.12.006. [DOI] [PubMed] [Google Scholar]
- Vlahakos VD, Marathias KP, Arkadopoulos N, Vlahakos DV. Hyperferritinemia in patients with COVID-19: an opportunity for iron chelation? Artif Organs. 2021;45(2):163–167. doi: 10.1111/aor.13812. [DOI] [PubMed] [Google Scholar]
- Wakabayashi H, Kurokawa M, Shin K, Teraguchi S, Tamura Y, Shiraki K. Oral lactoferrin prevents body weight loss and increases cytokine responses during herpes simplex virus type 1 infection of mice. Biosci Biotechnol Biochem. 2004;68(3):537–544. doi: 10.1271/bbb.68.537. [DOI] [PubMed] [Google Scholar]
- Wakabayashi H, Oda H, Yamauchi K, Abe F. Lactoferrin for prevention of common viral infections. J Infect Chemother. 2014;20:666–671. doi: 10.1016/j.jiac.2014.08.003. [DOI] [PubMed] [Google Scholar]
- Wan D, Du T, Hong W, Chen L, Que H, Lu S, Peng X. Neurological complications and infection mechanism of SARS-COV-2. Signal Transduct Target Ther. 2021;6(1):406. doi: 10.1038/s41392-021-00818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Li F, Wei H, Lian ZX, Sun R, Tian Z. Respiratory influenza virus infection induces intestinal immune injury via microbiota-mediated Th17 cell-dependent inflammation. J Exp Med. 2014;211(12):2397–2410. doi: 10.1084/jem.20140625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Jiang W, Yan Y, Gong T, Han J, Tian Z, Zhou R. RNA viruses promote activation of the NLRP3 inflammasome through a RIP1-RIP3-DRP1 signaling pathway. Nat Immunol. 2014;15(12):1126–1133. doi: 10.1038/ni.3015. [DOI] [PubMed] [Google Scholar]
- Wang Q, Zhang Y, Wu L, Niu S, Song C, Zhang Z, Lu G, Qiao C, Hu Y, Yuen KY, Wang Q, Zhou H, Yan J, Qi J. Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell. 2020;181(4):894–904.e9. doi: 10.1016/j.cell.2020.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Yue L, Dang L, Yang J, Chen Z, Wang X, Shu J, Li Z. Role of sialylated glycans on bovine lactoferrin against influenza virus. Glycoconjugate J. 2021;38(6):689–696. doi: 10.1007/s10719-021-10029-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welsh KJ, Hwang SA, Boyd S, Kruzel ML, Hunter RL, Actor JK. Influence of oral lactoferrin on Mycobacterium tuberculosis induced immunopathology. Tuberculosis (edinb) 2011;91(Suppl 1):S105–113. doi: 10.1016/j.tube.2011.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzhong L, Hualan L. COVID-19: captures iron and generates reactive oxygen species to damage the human immune system. Autoimmunity. 2021;54(4):213–224. doi: 10.1080/08916934.2021.1913581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisgrill L, Wessely I, Spittler A, Förster-Waldl E, Berger A, Sadeghi K. Human lactoferrin attenuates the proinflammatory response of neonatal monocyte-derived macrophages. Clin Exp Immunol. 2018;192(3):315–324. doi: 10.1111/cei.13108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrighting DM, Andrews NC. Interleukin-6 induces hepcidin expression through STAT3. Blood. 2006;108(9):3204–3209. doi: 10.1182/blood-2006-06-027631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu HF, Monroe DM, Church FC. Characterization of the glycosaminoglycan-binding region of lactoferrin. Arch Biochem Biophys. 1995;317(1):85–92. doi: 10.1006/abbi.1995.1139. [DOI] [PubMed] [Google Scholar]
- Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, Hu Y, Tao ZW, Tian JH, Pei YY, Yuan ML, Zhang YL, Dai FH, Liu Y, Wang QM, Zheng JJ, Xu L, Holmes EC, Zhang YZ. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Guo C, Tang L, Hong Z, Zhou J, Dong X, Yin H, Xiao Q, Tang Y, Qu X, Kuang L, Fang X, Mishra N, Lu J, Shan H, Jiang G, Huang X. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol. 2020;5(5):434–435. doi: 10.1016/S2468-1253(20)30083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu S, Fan F, Liu H, Cheng S, Tu M, Du M. Novel anticoagulant peptide from lactoferrin binding thrombin at the active site and Exosite-I. J Agric Food Chem. 2020;68(10):3132–3139. doi: 10.1021/acs.jafc.9b08094. [DOI] [PubMed] [Google Scholar]
- Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, Tai Y, Bai C, Gao T, Song J, Xia P, Dong J, Zhao J, Wang FS. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto H, Ura Y, Tanemura M, Koyama A, Takano S, Uematsu J, Kawano M, Tsurudome M, O’Brien M, Komada H. Inhibitory effect of bovine lactoferrin on human parainfluenza virus type 2 infection. J Health Sci. 2010;54:613–617. doi: 10.1248/jhs.56.613. [DOI] [Google Scholar]
- Yen MH, Chiu CH, Huang YC, Lin TY. Effects of lactoferrin-containing formula in the prevention of enterovirus and rotavirus infection and impact on serum cytokine levels: a randomized trial. Chang Gung Med J. 2011;34(4):395–402. [PubMed] [Google Scholar]
- Yi M, Kaneko S, Yu DY, Murakami S. Hepatitis C virus envelope proteins bind lactoferrin. J Virol. 1997;71(8):5997–6002. doi: 10.1128/JVI.71.8.5997-6002.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yildiz S, Mazel-Sanchez B, Kandasamy M, Manicassamy B, Schmolke M. Influenza A virus infection impacts systemic microbiota dynamics and causes quantitative enteric dysbiosis. Microbiome. 2018;6(1):9. doi: 10.1186/s40168-017-0386-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W, China Novel Coronavirus Investigating and Research Team A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimecki M, Actor JK, Kruzel ML. The potential for Lactoferrin to reduce SARS-CoV-2 induced cytokine storm. Int Immunopharmacol. 2021;95:107571. doi: 10.1016/j.intimp.2021.107571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zumerle S, Mathieu JR, Delga S, Heinis M, Viatte L, Vaulont S, Peyssonnaux C. Targeted disruption of hepcidin in the liver recapitulates the hemochromatotic phenotype. Blood. 2014;123(23):3646–3650. doi: 10.1182/blood-2014-01-550467. [DOI] [PubMed] [Google Scholar]
- Zuo Y, Warnock M, Harbaugh A, Yalavarthi S, Gockman K, Zuo M, Madison JA, Knight JS, Kanthi Y, Lawrence DA. Plasma tissue plasminogen activator and plasminogen activator inhibitor-1 in hospitalized COVID-19 patients. Sci Rep. 2021;11(1):1580. doi: 10.1038/s41598-020-80010-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwirzitz A, Reiter M, Skrabana R, Ohradanova-Repic A, Majdic O, Gutekova M, Cehlar O, Petrovčíková E, Kutejova E, Stanek G, Stockinger H, Leksa V. Lactoferrin is a natural inhibitor of plasminogen activation. J Biol Chem. 2018;293(22):8600–8613. doi: 10.1074/jbc.RA118.003145. [DOI] [PMC free article] [PubMed] [Google Scholar]