Abstract
Structural and social determinants of health account for the health disparities we see along social hierarchies, and their impact has been made more evident by the recent COVID-19 pandemic. There have been increasing calls to incorporate structural competency into medical education. The structural and social context, however, has yet to be fully integrated into everyday clinical practice and little has been published on how to concretely imbed structural competency into clinical reasoning. The authors provide a framework for structural analysis, which incorporates four key steps: (1) developing a prioritized clinical problem list, (2) identifying social and structural root causes for clinical problems, (3) constructing and documenting a prioritized structural problem list, and (4) brainstorming solutions to address structural barriers and social needs. They show how structural analysis can be used to operationalize structural reasoning into everyday inpatient and outpatient clinical assessments.
KEY WORDS: social determinants of health, structural competency, medical education
The majority of health outcomes are the result of social determinants of health or the conditions in which people are born, grow, work, live, and age. These are influenced by the structural determinants of health, or the social, economic, and political mechanisms and policies that generate, configure, and maintain social hierarchies.1 Structural and social determinants of health (SSDH) account for health disparities, and their impact has been made evident by the recent COVID-19 pandemic.2
Undergraduate and graduate medical accreditation bodies have called for the inclusion of education on SSDH and health equity.3,4 In 2014, Metzl and Hansen published a framework for imbedding SSDH into medical education. Known as structural competency, it calls for the reframing of behaviors and disease as downstream implications of upstream decisions about structures and social systems.5 While a number of undergraduate structural competency curricula have been published6,7 and there are calls to embed structural competency into graduate education,8–10 less has been published on how to operationalize structural competency into routine bedside clinical teaching.
Recently, several hospital systems have recognized the importance of SSDH and begun universal screening for unmet patient-level social needs, for example, food insecurity, medication affordability, and transportation barriers.11–14 These initiatives have facilitated explicit discussion of how social needs directly impact health. Still, gaps remain in how to train learners to incorporate SSDH within traditional clinical reasoning.15,16 In the absence of an analytic framework, screening for social needs alone risks incomplete conceptualizations of the links between SSDH and health outcomes.17 In clinical practices that are not yet equipped to address SSDH, educational interventions can pave the way by arming learners with tools to change clinical practice. We provide an educational framework for integrating structural competency into clinical reasoning and assessment, known as structural analysis, that can be used in inpatient and outpatient clinical settings.
KEY STEPS OF STRUCTURAL ANALYSIS
Structural analysis entails four steps: (1) developing a prioritized clinical problem list, (2) identifying structural and social root causes for clinical problems, (3) constructing and documenting a prioritized structural problem list, and (4) brainstorming solutions to address structural problems.
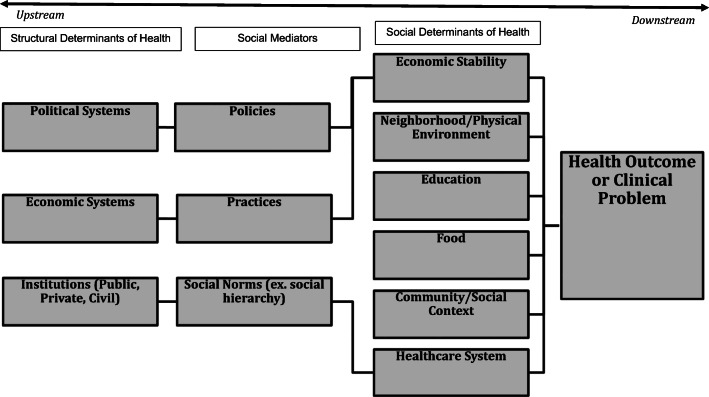
Structural analysis starts with ensuring congruity between clinician clinical problem lists and patient concerns. Using a root cause analysis approach,18 learners then diagram structural and social root causes. Active clinical problems are placed at the head of the diagram. Downstream social determinants are brainstormed first, with mediators such as policies, practices, and social norms brainstormed next, followed by more upstream structural determinants such as political systems, economic systems, and institutions (Fig. 1). Identifying downstream social determinants entails obtaining a comprehensive social history that reflects the true lived experience of each patient, thereby avoiding assumptions arising from bias or stereotype. Here universal social needs screening, using a standardized tool such as the Accountable Health Communities tool, can be helpful.19 Screening has been shown to be feasible and can be integrated into the electronic health record.20,21 Identifying upstream mediators and structural determinants entails researching the literature and synthesizing clinical problems within a sociological, anthropological, and historical context. For example, uncontrolled asthma becomes contextualized in historical environmental policies that concentrated high pollutant emitting facilities and roadways in poor and minority communities.22 A patient’s uncontrolled diabetes is contextualized by food insecurity23 (downstream determinant), but also policies that prioritize corporate profit in food production over access24 (upstream mediator and structural determinants). Educators should acknowledge where causal pathways linking SSDH to certain health outcomes have not yet been fully elucidated. Use of community- and population-level data can help inform upstream contributors as they relate to individual patients.
Figure 1.
Structural analysis diagram to identify root causes of health outcomes. From left to right, upstream structural determinants of health, mediators, and more downstream social determinants of health.
Once structural root causes are uncovered, a prioritized structural problem list can be developed which explicitly names as separate problems SSDH that are urgent and for which clinic and community resources are available. For example, food insecurity that directly impacts diabetic A1c control is listed as a separate problem for which an assessment and plan is required. Choosing the structural problems to highlight allows learners the opportunity to discern between those problems that should be addressed for individual patient care and other root causes (often upstream) that should be acknowledged but may not require their own assessment and plan. Intentional documentation of SSDH reduces stigmatizing and bias language by encouraging the learner to frame clinical narratives around forces that fundamentally impact health outcomes and away from characterizations that assign personal blame, such as “non-compliance,” typically seen in present-day medical documentation. Further practices to minimize bias include updating problem lists regularly, focusing on strengths, and avoiding explicitly documenting sensitive information with legal implications such as undocumented status.
The final step of structural analysis is developing solutions to address SSDH included in the structural problem list. The socio-ecological model can help learners imagine interventions at the individual, health systems, community, and societal levels.25 Communication with patients about social needs and individual-level solutions to address them entails a relationship-centered approach to shared decision-making that centers patients’ experiences, priorities, and beliefs, and draws on established relationships between patients, providers, institutions, and communities.26 A strengths-based approach is vital to maintaining a positive outlook and supporting patient resiliency.27
Clinicians also need awareness of clinic- and community-based resources and help from an interdisciplinary team. Moving towards a SSDH-focused clinical practice involves incorporating community health workers, peer supporters, or social workers; health educators; and community partners, for example, medical-legal partnerships. An interdisciplinary approach results in improved outcomes for unmet social needs28 and should be coupled with information systems for population health management and payment reform that aligns incentives with health outcomes.
Solutions for mediators and structural determinants of health often necessitate advocacy work beyond the scope of traditional clinical practice. Explicit acknowledgement of the responsible policies, practices, and institutions is the first step in advocating for change to reduce health disparities. Trainees can serve a vital supporting role alongside community-based advocacy groups in lending their voice to change critical mediators. Numerous examples of trainee-involved advocacy exist.29 Structural analysis pushes learners to envision, at the point of clinical care, solutions at every level of the socio-ecological model, not just at the individual level, and fosters this level of action among a wider breadth of trainees.
APPLYING STRUCTURAL ANALYSIS
A 37-year-old woman with a history of diabetes called a local clinic because she developed fever and cough for 2 days. She was advised to obtain COVID-19 testing but declined. She called back the next day with chest discomfort and was instructed to go to the emergency department but again was reluctant, asking for medications to be called into a pharmacy. She is the mother of three young children and is afraid of losing her job in housekeeping for a downtown hotel. She and eight family members share a three-bedroom rental located an hour by bus from downtown. She came to the USA 10 years ago from Guatemala and is ineligible for health insurance due to her immigration status.
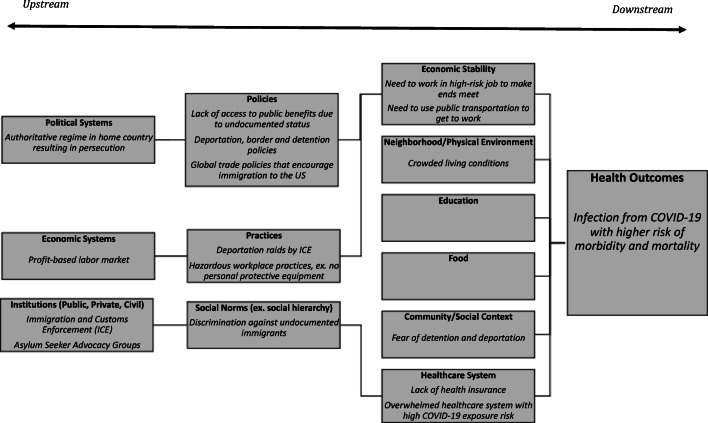
A structural analysis approach to this patient’s clinical presentation moves beyond a traditional clinical problem list (step 1 of structural analysis) of cough, fever, and chest discomfort. Instead, a root cause analysis for her likely COVID-19 infection reveals underlying SSDH (step 2 of structural analysis). This patient is at high risk of COVID-19 infection from her job as an essential worker in the hospitality industry, her need to take daily public transportation, and living in a crowded household. Her reluctance to seek medical care might be related to lack of health insurance, prior experience of discrimination, and fear of detention and deportation. These factors are downstream determinants that directly impact her infection risk and access to healthcare. Underlying upstream structural determinants are exploitive labor markets and the push/pull factors for migration. Mediators include unsafe working conditions; racism and stigmatization against undocumented immigrants; and exclusion from health coverage, unemployment insurance, and other social safety nets (Fig. 2).
Figure 2.
Example completed structural analysis diagram showing structural determinants, mediators and downstream social determinants which impact a health outcome.
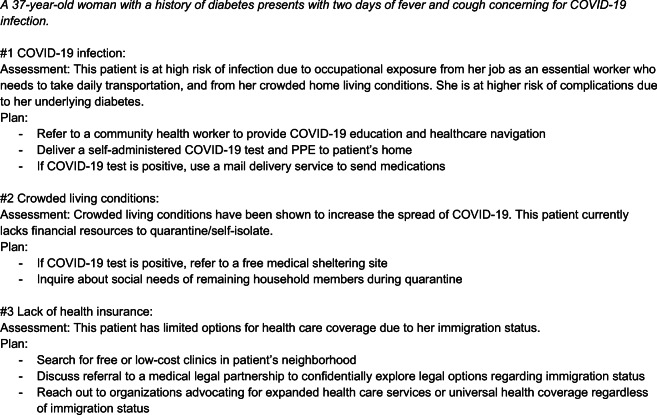
Once root causes have been identified, a prioritized structural problem list includes lack of health insurance, immigration status, and crowded living conditions (step 3 of structural analysis) (Fig. 3). Through a structural analysis, it is clear that asking this patient to obtain COVID-19 testing or referring her to the emergency department alone would not be effective. Rather, interventions for social needs informed by availability of local resources are likely to be more helpful. These could involve healthcare navigation by a community health worker, referring to a multilingual COVID-19 phone line, delivering free self-administered COVID-19 testing to minimize concerns of government intrusion and data collection, and referring to medical sheltering sites like hotel rooms to lessen risks posed by crowded households. Solutions at the health systems level may include expanding services for uninsured individuals, piloting a clinician home-visitation program, and establishing a medical-legal partnership. At a policy level, clinicians can partner with community to advocate for an eviction moratoria and relief fund for cash-strapped families regardless of immigration status, immigration reform, and regulation protecting essential workers from exposure to COVID-19 (step 4 of structural analysis).
Figure 3.
Re-envisioned structural problem list and sample assessment and plan.
EXAMPLES OF CURRICULAR APPROACHES
Structural analysis offers a concrete guide for applying structural competency to clinical problem-solving and allows for a more developed macro-level conceptualization of health and disease. We posit that the same rigor in medical training that is applied to and expected of micro-level conceptualizations rooted in genetic, molecular, and pathophysiologic studies should also be applied to fundamental macro-level understanding of disease. A full and complete understanding of health necessitates delving into not only downstream social needs, but also more upstream mediators and structural contributors. It advocates for undergraduate and graduate curriculum that takes more than a superficial approach to SSDH, and supports the furthering of social and political education for all trainees.
At the University of Pittsburgh, health professions students have an opportunity to write social medicine case studies based on a patient they encountered during a clinical elective working with underserved populations. Using structural analysis, the case study process guides students through a patient-centered clinical problem list; a root cause analysis for the main problem; SSDH that have had positive and negative impacts; and interventions on multiple levels.30 Case studies are designed for self-directed learning or small-group discussion in pre-clinical or clinical instruction settings. At Montefiore Medical Center, resident case conferences have explicitly incorporated steps of the structural analysis using actual clinical scenarios. During these resident-report-style conferences, residents are encouraged to delve into social and structural root causes, explicitly name structural problem lists, and actively brainstorm solutions at multiple levels of the socio-ecological model. Both institutions are studying whether these interventions increase knowledge of links between SSDH and health outcomes, documentation of social needs, and interprofessional collaboration.
NEXT STEPS
Our early experience with a structural competency framework in medical education suggests learners can be taught to apply structural analysis to patients’ health problems. Screening for social needs and referring to social services is only the first step in structurally competent care. First, learners will need guidance connecting symptoms and problems to downstream determinants and identifying mediators and ultimately structural determinants. This requires dedicated faculty development to re-envision clinical teaching. Second, learners will face challenges intervening at systems and institutional levels. When they recognize that social services are inadequate to address their patients’ structural vulnerabilities, learners will need advocacy skills to tackle institutional practices that reflect profit-driven economic and political systems. Potential challenges in identifying and addressing complex mechanisms and interactions between SSDH and health should not deter adoption of structural analysis. Rather discussion of these complexities is necessary and can identify areas where more research is needed.
As role models for learners, all healthcare providers and staff should be trained in structural competency. Armed with tools for structural analysis and a shared social mission, health professionals, patients, and other stakeholders could unite in dismantling social forces that result in health disparities. Health systems themselves might pose formidable challenges as structural changes threaten the status quo by redistributing power and resources, but learners will recognize that this burden is not theirs alone. Last, development of evidence-based approaches for implementing structural competency is critical. This involves implementing upstream quality improvement,31 studying pathways that lead from SSDH to ill health, and evaluating the effectiveness of structural interventions.
Acknowledgements
The authors wish to thank Dr. Shani R. Scott, Dr. Shwetha Iyer, and Dr. Eloho Ufomata.
Funding
This manuscript was funded by the American Medical Association (AMA) Reimagining Residency Grant Initiative. The Case-Based Teaching in Social Medicine Project was supported by the American Medical Association’s Accelerating Change in Medical Education Innovation Grants Program. The content reflects the views of authors and does not purport to reflect the views of AMA or any member of the Accelerating Change in Medical Education Consortium.
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Solar O, Irwin A. A Conceptual Framework for action on the Social Determinants of Health. Social Determinants of Health Discussion Paper 2 (Policy and Practice) Geneva: World Health Organization; 2010. [Google Scholar]
- 2.Paremoer L, Nandi S, Serag H, Baum F. Covid-19 pandemic and the social determinants of health. BMJ. 2021;372:n129. doi: 10.1136/bmj.n129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liaison Committee on Medical Education. Functions and structure of a medical school: Standards for accreditation of medical education programs leading to the MD degree. http://lcme.org/publications/#Standards. Published October 2021. Accessed December 29, 2021.
- 4.Wagner, R, Koh, N, Bagian, JP, Weiss, KB, for the CLER Program. CLER 2016 National Report of Findings. Issue Brief #4: Health Care Disparities. Chicago, IL: Accreditation Council for Graduate Medical Education. ISBN-13: 978-1-945365-07-2.
- 5.Metzl JM, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med. 2014;103:126–133. doi: 10.1016/j.socscimed.2013.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neff J, Holmes SM, Knight KR, et al. Structural competency: curriculum for medical students, residents, and interprofessional teams on the structural factors that produce health disparities. MedEdPORTAL. 2020;16:10888. doi: 10.15766/mep_2374-8265.10888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Metzl JM, Petty J. Integrating and assessing structural competency in an innovative prehealth curriculum at Vanderbilt University. Acad Med. 2017;92(3):354–359. doi: 10.1097/ACM.0000000000001477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salhi BA, Tsai JW, Druck J, Ward-Gaines J, White MH, Lopez BL. Toward structural competency in emergency medical education. AEM Educ Train. 2020;4(Suppl 1):S88–S97. doi: 10.1002/aet2.10416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Downey MD, Gomez AM. Structural competency and reproductive health. AMA J Ethics. 2018;20(3):211–223. doi: 10.1001/joournalofethics.2018.20.3.peer1-1803. [DOI] [PubMed] [Google Scholar]
- 10.Metzl JM, Hansen H. Structural competency and psychiatry. JAMA Psychiatry. 2018;75(2):115–116. doi: 10.1001/jamapsychiatry.2017.3891. [DOI] [PubMed] [Google Scholar]
- 11.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135:e296–e304. doi: 10.1542/peds.2014-2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gottlieb LM, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr. 2016;170:e162521. doi: 10.1001/jamapediatrics.2016.2521. [DOI] [PubMed] [Google Scholar]
- 13.Klein MD, et al. Doctors and lawyers collaborating to HeLP children--outcomes from a successful partnership between professions. J Health Care Poor Under. 2013;24:1063–1073. doi: 10.1353/hpu.2013.0147. [DOI] [PubMed] [Google Scholar]
- 14.Fiori KP, Rehm CD, Sanderson D, et al. Integrating social needs screening and community health workers in primary care: the community linkage to care program. Clin Pediatr (Phila) 2020;59(6):547–556. doi: 10.1177/0009922820908589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by US Physician Practices and Hospitals. JAMA Netw Open. 2019;2(9):e1911514. doi: 10.1001/jamanetworkopen.2019.11514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kovach KA, Reid K, Grandmont J, Jones D, Wood J, Schoof B. How engaged are family physicians in addressing the Social Determinants of Health? A survey supporting the American Academy of Family Physician’s Health Equity Environmental Scan. Health Equity. 2019;3(1):449–457. doi: 10.1089/heq.2019.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Green K, Zook M. When talking about social determinants, precision matters, Health Affairs Blog, October 29, 2019. 10.1377/hblog20191025.776011.
- 18.Doggett M. Root cause analysis: a framework for tool selection. Qual Manag J. 2006;12(4):34–45. doi: 10.1080/10686967.2005.11919269. [DOI] [Google Scholar]
- 19.The Accountable Health Communities Health-Related Social Needs Screening Tool. Centers for Medicare and Medicaid Services. Accessed June 9, 2022. Available at: https://innovation.cms.gov/files/worksheets/ahcm-screeningtool.pdf
- 20.Buitron de la Vega P, Losi S, Sprague Martinez L, Bovell-Ammon A, Garg A, James T, Ewen AM, Stack M, DeCarvalho H, Sandel M, Mishuris RG, Deych S, Pelletier P, Kressin NR. Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Med Care. 2019;57(Suppl 6 Suppl 2):S133–S139. doi: 10.1097/MLR.0000000000001029. [DOI] [PubMed] [Google Scholar]
- 21.Wang M, Pantell MS, Gottlieb LM, Adler-Milstein J. Documentation and review of social determinants of health data in the EHR: measures and associated insights. J Am Med Inform Assoc. 2021;28(12):2608–2616. doi: 10.1093/jamia/ocab194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brender JD, Maantay JA, Chakraborty J. Residential proximity to environmental hazards and adverse health outcomes. Am J Public Health. 2011;101((Suppl 1(Suppl 1)):S37–S52. doi: 10.2105/AJPH.2011.300183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gucciardi E, Vahabi M, Norris N, Del Monte JP, Farnum C. The intersection between food insecurity and diabetes: a review. Curr Nutr Rep. 2014;3(4):324–332. doi: 10.1007/s13668-014-0104-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mozaffarian D, Angell SY, Lang T, Rivera JA. Role of government policy in nutrition—barriers to and opportunities for healthier eating. BMJ. 2018;361:k2426. doi: 10.1136/bmj.k2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dahlberg LL, Krug EG. Violence: a global public health problem. In: Krug E, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors. World Report on Violence and Health. Geneva, Switzerland: World Health Organization; 2002. pp. 1–21. [Google Scholar]
- 26.Schoenthaler A, Hassan I, Fiscella K. The time is now: Fostering relationship-centered discussions about patients’ social determinants of health. Patient Educ Couns. 2019;102(4):810–814. doi: 10.1016/j.pec.2018.10.025. [DOI] [PubMed] [Google Scholar]
- 27.Boynton-Jarrett R, Flacks J. Strengths-based Approaches to Screening Families for Health-Related Social Needs in the Healthcare Setting. Washington, DC; 2018.
- 28.Cheng I, Powers K, Mange D, Palmer B, Chen F, Perkins B, Patterson S. Interprofessional education through healthcare hotspotting: Understanding social determinants of health and mastering complex care through teamwork. J Interprofessional Educ Pract. 2020;9:100340. doi: 10.1016/j.xjep.2020.100340. [DOI] [Google Scholar]
- 29.Howell BA, Kristal RB, Whitmire LR, Gentry M, Rabin TL, Rosenbaum J. A systematic review of advocacy curricula in graduate medical education. J Gen Intern Med. 2019;34(11):2592–2601. doi: 10.1007/s11606-019-05184-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Social Medicine Case Collection. University of Pittsburgh School of Medicine. Accessed February 2, 2022 at: https://www.socialmedcases.pitt.edu/?page_id=474.
- 31.Manchanda R. Moving upstream to achieve the quadruple aim. California Association of Public Hospitals and Health Systems Annual Conference 2016. Accessed June 9, 2022. Available at: https://caph.org/wp-content/uploads/2016/12/rishi-manchanda-caphsni-conference.pdf.