Abstract
Insomnia affects one-third of the adult population and is associated with multiple medical conditions. We conducted an observational epidemiological survey to assess (1) the prevalence of insomnia in an Italian group of patients aged over 50 years, presenting directly to the general physician (GP); (2) the association of insomnia with sleepiness and comorbidities; and (3) the pharmacological treatment. The study was carried out by GPs. Each GP was asked to enroll the first patient over 50 years old spontaneously presenting for any medical problems for 5 consecutive days. The Italian version of the Sleep Condition Indicator (SCI) was administered; daytime sleepiness was evaluated by a visual analogic scale (VAS). For every patient, GPs collected information regarding comorbidities and pharmacological treatment for insomnia and evaluated the severity of insomnia using the Clinical Global Impression Severity (CGI-S) scale. A total of 748 patients (mean age 65.12 ± 9.45 years) were enrolled by 149 GPs. Prevalence of insomnia was 55.3%. SCI, VAS, and CGI-S scores were highly correlated between each other (p < 0.0001). At general linear model analysis, the comorbidities more associated with the presence of insomnia were anxiety-depressive disorder (p < 0.001), other psychiatric disorders (p = 0.017), cardiovascular disorders (p = 0.006), and dementia (p = 0.027). A statistically significant correlation was found between SCI score and the use of benzodiazepines (p < 0.001), z-drugs (p = 0.012), antidepressants (p < 0.001), and melatonin-prolonged release (p < 0.001). Insomnia affects half of Italian primary care patients over 50 years and is frequently associated with different medical conditions, sleepiness, and use of multiple—often off-label—drugs.
Keywords: Epidemiology, Hypnotics, Chronic pain, Advancing age, Women, Employment
Introduction
Insomnia represents the most common sleep disorder and one of the most prevalent complaints in primary care, increasing its frequency with age [1]. Despite the high amount of epidemiological studies on insomnia, estimates of its prevalence are variable, depending in part on inconsistencies in definitions and diagnostic criteria and in part on the different selected populations.
Demographically, women, older people, and those with coexisting health problems are more likely to suffer from insomnia [2–4]. Different studies highlight the high rate of comorbidity between chronic insomnia and medical and psychiatric disorders [4–8], although the relationship between these conditions is particularly complex.
Considering the pharmacological treatment of insomnia, previous studies demonstrated that the use of hypnotics increases with age, especially in middle-aged and elderly women [9, 10]. In the past, insomnia treatments were prescribed frequently by general practitioners (GPs) to patients with poor sleep without real diagnostic criteria or treatment algorithms for insomnia, leading to an increase of hypnotics use in many countries [11]. Recently, different guidelines have been produced for the diagnosis and treatment of insomnia by panel of experts belonging to different scientific societies [12–14].
In 2004, the “Morfeo” study, the first Italian observational investigation on the distribution of insomnia in primary care, revealed a high prevalence of insomnia (64%), especially in the female population, elderly and unemployed people, and patients with other psychiatric or somatic illnesses [15]. The pharmacological treatment for insomnia was four-fold more frequent than non-pharmacological therapy (78.6 versus 18.2%) [16].
Here, we report the results of an observational epidemiological survey that has been conducted in order to assess (1) the prevalence of insomnia in an Italian population aged over 50 years presenting directly to the GP; (2) the association of insomnia with sleepiness and comorbidities; and (3) the pharmacological treatment.
Methods
A multi-center observational epidemiological study was carried out by GPs homogeneously distributed over the Italian National territory. GPs were enrolled in the context of an educational project on insomnia, named “Sonno e Salute” study carried out from April 2017 to October 2018. The GPs who agreed participating were asked to recruit the first, over 50 years old, patient among the patients spontaneously referring to their office, for any medical problem, for 5 consecutive days. Thus, each GP enrolled five patients. GPs administered to every patient the Italian version of the Sleep Condition Indicator (SCI) [17, 18] and a visual analogic scale (VAS) to evaluate their daytime sleepiness. In particular, the Sleep Condition Indicator (SCI) is an eight-item rating scale that was developed to screen for insomnia disorder based on DSM-5 criteria. Moreover, for every patient, GPs collected information regarding the main demographic data, comorbidities, pharmacological treatment for insomnia, and the severity of insomnia, using the Clinical Global Impression Severity Scale (CGI-S).
Statistical analysis
Categorical variables were summarized by counts and percentages. Continuous quantitative variables were summarized using mean ± standard deviation. Presence of insomnia was defined on the basis of SCI score (< 16) and according to the current criteria set by the International Classification of Sleep Disorders, 3rd edition (ICSD-3) [19]. Patients were subdivided according to the presence/absence of insomnia. The demographic and clinical characteristics of the subjects were compared between groups using the unpaired t-test (continuous measures) and the chi-square test (categorical measures). Pearson correlations were applied to explore the correlations between SCI, VAS, and CGI-S scores.
A first, descriptive analysis was performed to explore the presence/absence of each comorbidity in patients with and without insomnia. To prevent the multiple comparison problem, the Bonferroni correction was applied.
A general linear model (GLM) was then applied to investigate the comorbidities (predictors) most associated with insomnia, using the SCI score as the dependent variable and age as nuisance.
Finally, the Spearman correlation was used to investigate the relationship between the number of drugs used for insomnia and the number of comorbidities.
Statistical analysis was performed with the Stata software (StataCorp. 2013, College Station, TX).
Results
One-hundred and fifty GPs participated in the study, enrolling 748 subjects (405 females, mean age 65.12 ± 9.45 years). Two patients were excluded because they were under the age of 50 years. Approximately half (55.3%) of the study population was affected by insomnia. Table 1 summarizes the main demographic and clinical characteristics of the subjects, according to presence/absence of insomnia.
Table 1.
Main demographic and clinical characteristics of the subjects, according to presence/absence of insomnia
| Patients with insomnia (n = 414) | Patients without insomnia (n = 334) | p-value | |
|---|---|---|---|
| Mean age | 66.3 ± 10 | 63.8 ± 8 | 0.0003 |
| Sex (female) | 239 (57.7%) | 166 (49.7%) | 0.028 |
| Married | 327 (80%) | 266 (79.6%) | 0.826 |
| Employment | |||
|
Employed Unemployed Retired |
221 (53.4%) 64 (15.5%) 129 (31.2%) |
123 (36.8%) 48 (14.4%) 163 (48.8%) |
< 0.001 |
| VAS score | 3.84 ± 3.2 | 2.32 ± 2.5 | < 0.001 |
| CGI-S score | 3.9 ± 0.9 | 2.7 ± 1.1 | < 0.001 |
| No treatment | 55 (13.3%) | 90 (26.9%) | < 0.001 |
CGISS, Clinical Global Impression Severity Scale; VAS, visual analogic scale
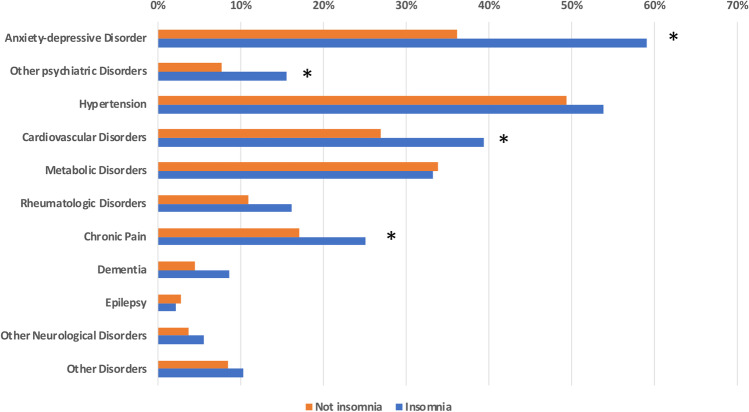
SCI, VAS, and CGI-S scores were highly correlated between each other (p < 0.0001). Patients with insomnia, in comparison with patients without insomnia, were significantly (p < 0.005) more affected by anxiety-depressive disorder, other psychiatric disorders, cardiovascular disorders, and chronic pain (Fig. 1).
Fig. 1.
Comorbidities in patients with and without insomnia. Comorbidities significantly different (p < 0.005) between groups are marked with an asterisk
At GLM analysis, the comorbidities more associated with the presence of insomnia were anxiety-depressive disorder (p < 0.001), other psychiatric disorders (p = 0.017), cardiovascular disorders (p = 0.006), and dementia (p = 0.027).
Considering pharmacological treatment, 13.3% subjects with insomnia were not treated (Table 1). A total of 80.6% of study population took at least one drug. Among treated patients, 359 (59.5%) suffered from insomnia. We found that 331 (54.9% of treated) patients were in monotherapy (149 insomnia patients and 182 patients without insomnia). The prevalent treatment consisted in benzodiazepine in patients with insomnia (benzodiazepine in 68, Z-drugs in 5, antidepressants in 9, melatonin in 37, and herbs and alternative medication in 30 patients) and in herbs and alternative medication in patients without insomnia (benzodiazepine in 57, Z-drugs in 3, antidepressants in 11, melatonin in 54, and herbs and alternative medication in 60 patients).
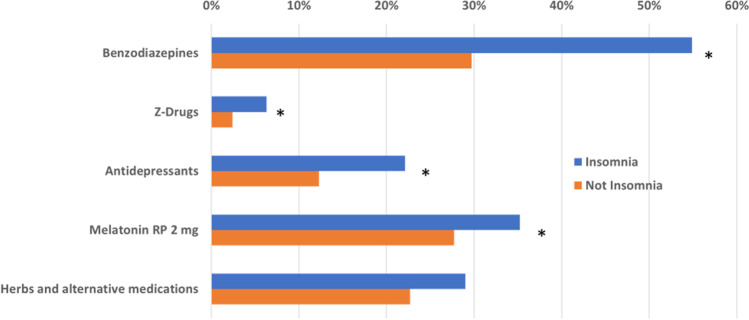
Figure 2 shows the drugs commonly used for the treatment of insomnia, according to its presence/absence. Patients with insomnia used benzodiazepines (p < 0.001), Z-drugs (p = 0.012), antidepressants (p < 0.001), and prolonged release melatonin (p = 0.029) more frequently than those without.
Fig. 2.
Drugs commonly used for the treatment of insomnia in patients with and without insomnia. Drug classes significantly different between groups are marked with an asterisk
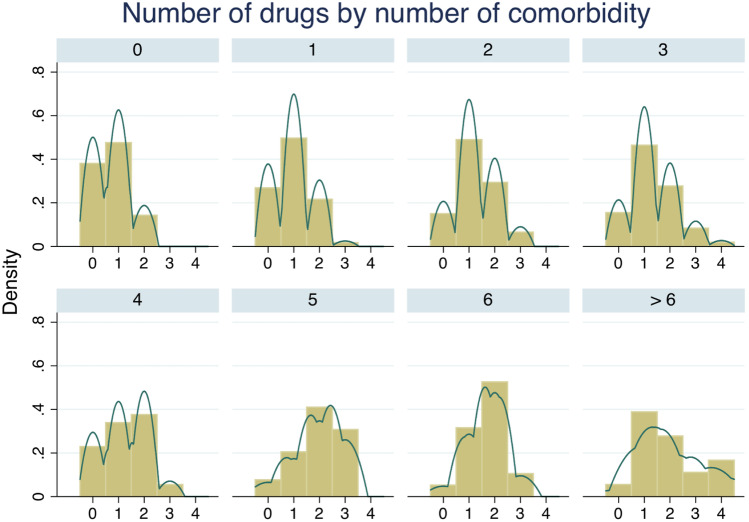
The number of drugs taken for insomnia was significantly correlated with the number of comorbidities (p < 0.0001). That is, the lower the number of drugs, the fewer the comorbidities (Fig. 3).
Fig. 3.
Histogram showing the density of the number of drugs for insomnia taken by the patients, according to the number of comorbidities. Each histogram describes the number of drugs according to the number of comorbidities. That is, the first histogram in the upper left corner shows patients with no comorbidities, the second histogram shows patients with one comorbidity, the third shows patients with two comorbidities, and so on. It is interesting to note that most patients with no comorbidities (first histogram in the upper left corner) took zero or one drug. Along with the increase of comorbidities, the number of drugs also significantly increases (p < 0.0001)
Discussion
This survey, conducted on a sample of the Italian population older than 50 years referring to GP office, confirms that insomnia represents a very common disturbance in the primary care, often associated with different psychiatric and somatic disorders. Moreover, this study shows that subjects with insomnia complain of higher levels of daytime sleepiness (EDS) than those of subjects without insomnia and use several hypnotic drugs more frequently than people without insomnia do.
Earlier epidemiological studies have revealed a high variation in the prevalence of insomnia, owing to different diagnostic criteria used and the study groups selected. Specifically, about 25% of adults complain unsatisfying sleep, 10–15% report symptoms of insomnia associated with daytime consequences, and 6–10% suffer from chronic insomnia [1, 2, 12]. Moreover, the prevalence of insomnia seems to vary largely in different countries. For instance, in Europe, it goes from a minimum of 5.7% in Germany to a maximum of 19% in France [12]. Furthermore, a US study showed that, among the elderly, European-Americans more frequently complained of insomnia than African-Americans and had a greater dependence on sleep medications [20]. Finally, studies conducted in general practice usually reveal higher prevalence rates, with 46 to 69% of the patients consulting the GPs suffering from at least occasional insomnia [15, 21, 22]. In particular, a previous Italian observational investigation on the distribution of insomnia in primary care (Morfeo Study) revealed an extremely high prevalence of this sleep disorder (64%), showing that most insomniacs (44%) complained of diurnal disturbances [15]. It is worth reminding that subjects included in the survey were older than 18 years (mean age 52.7 ± 16.2 years) and that the diagnosis of insomnia was made according to the responses to five sleep-related questions [15]. Although we selected only participants aged more than 50 years, we found a prevalence of insomnia (55.3%) slightly lower than that reported by the Morfeo Study, probably depending on the different diagnostic criteria adopted. Nevertheless, our findings suggest a high prevalence of insomnia in adult subjects seeking primary care.
According with the current ICSD-3 criteria [19], daytime impairment is required to reach a diagnosis of insomnia. Daytime complaints associated with insomnia can be very heterogeneous including fatigue, attention/memory impairment, reduced daytime performance, irritability, sleepiness, behavioral problems, and distress, directly related to the inability to initiate and/or maintain sleep. Among all these symptoms, we investigated the presence of daytime sleepiness, finding higher scores (in a VAS) in subjects with insomnia. However, the mean VAS score in our insomnia patients was 3.84 ± 3.2; thus, sleepiness in this group is generally a moderately severe complaint. Data from the literature investigating the prevalence of EDS in patients with insomnia are discordant [23]. Indeed, different studies using subjective assessments found significantly higher levels of EDS in insomniac patients than in controls, though these results were not reflected in objective measures [23].
Almost all of the available epidemiological studies reported a higher prevalence of insomnia in women and advancing age [2, 24] and our study confirms this evidence. Moreover, we found that insomnia is more frequent in employed and unemployed people while insomnia frequency seems to decrease in retired subjects. A few studies have reported a direct relationship between being unemployed or retired and increased prevalence of insomnia [2, 25]. The Morfeo Study revealed that the prevalence of insomnia was 76.2% among retired people, 66% among jobless subjects, and 53.9% among employed individuals. However, it is worth to underline that this study included both patients with (level 2 insomnia) and without (level 1 insomnia) daytime dysfunction. Interestingly, level 2 insomnia was more frequent in unemployed people (73%) with respect to retired people (58%). A recent meta-analysis reported a correlation between insomnia and higher levels of job stress, effort-reward imbalance, high demand, heavy workload, and low social support [26]. Thus, we can hypothesize that employed and jobless subjects complain more frequent sleep difficulties associated with daytime impairment, possibly because of the daytime stress related to their job difficulties, including its lack. Moreover, in our subjects, mean age was 66 years and 50% of subjects were employed. Thus, work in the elderly may be associated with a higher amount of distress, while unemployed elderly subjects could have more worries about their annuity. On the other hand, retired people may have less complaints about daytime impairment, because of the retirement itself. Indeed, retired people usually report only a “short sleep” duration without any dysfunction during the day [27]. This latter condition could be also influenced by the physiologic reduction of the total sleep time during the old age.
Our survey revealed that insomnia is significantly associated with different medical problems, specifically anxiety-depressive disorder, other psychiatric disorders, cardiovascular disorders, dementia, and chronic pain. Different studies reported a strong relationship between insomnia and both somatic and psychiatric disorders [5, 7, 8]. However, this association is not fully understood due to the multiple aspects involved and possible bidirectional influences. Specifically, insomnia complaints can represent the direct or indirect consequence of a somatic or mental disease or of its treatment. Moreover, when present, insomnia may affect the course and effectiveness of treatment of these illnesses. About that, a deep link between sleep and pain exists [28]. Indeed, sleep disturbance is frequently reported in patients with chronic pain, contributing to cause additional distress and fatigue and to exacerbate pain. In such patients, treatment of sleep disorders could significantly improve also the co-occurring pain and could reduce the use of opioids in specific patients on long-term opioid therapy. Finally, recent findings reveal that insomnia can represent a risk factor for several psychiatric and somatic disorders, particularly when associated with short sleep duration [7, 8]. A bidirectional relationship between sleep disorders and dementia has also been underlined recently [29–31]. Sleep plays a pivotal role in memory consolidation and in facilitating the clearance of neural activity degradation products, through the activation of the glymphatic system [32]. Recent evidence found that sleep disorders, in particular insomnia, could impair these functions increasing the risk of degenerative disorders, such as Alzheimer’s disease [33].
Considering drug treatment, 80.6% of the whole population (86% of the insomniacs and 73% of the non-insomniacs) were treated with at least one of the drugs commonly used for insomnia.
This is in line with the Morfeo Study 2 results, revealing that the Italian GP privileged the pharmacological approach, which was four-fold more frequent than non-pharmacological therapy (78.6 versus 18.2%) [16]. Since 2016, several national and international guidelines for diagnosis and treatment of insomnia have been published, all agreeing that cognitive behavioral treatment of insomnia should represent the first-line treatment [12, 14, 34]. Thus, it should be interesting to inquire if these guidelines were conducted to a higher diffusion of the psychological approach to insomnia. Unfortunately, we did not investigate this therapeutic option in our population.
The large majority of insomnia patients were under pharmacological treatment with more than half of treated patients (59.5%) suffering from insomnia, thus suggesting a possible inappropriate selection of drugs in many cases or the presence of patients with drug-resistant form of insomnia.
Conversely, we found that also a large proportion of patients without insomnia took at least one drug. This could mean that some of them were insomnia patients responders to pharmacological treatment or were taking those drugs for other reasons (i.e., anxiety). Moreover, polytherapy was observed in about one-half of subjects both with or without insomnia, indicating that the association of different medications is a frequently adopted option also by general practitioners. Considering specific drugs, patients with insomnia in our study showed a higher use of benzodiazepine, Z-drugs, antidepressants, and prolonged release melatonin with respect to people without insomnia. In particular, benzodiazepines were the most commonly drugs taken. The attitude towards the choice of the pharmacological treatment for insomnia changed over the past years and, in different countries, different treatment strategies were adopted. Indeed, in the USA, in the 1990s, there was a strong shift towards the use of antidepressants instead of hypnotics, as first therapeutic choice for insomnia [35]. Later, an analysis of the National Ambulatory Medical Care Survey data from 1993 to 2007 revealed that non-benzodiazepine sedative hypnotics prescriptions grew 5 times more rapidly than insomnia diagnoses [36]. Finally, a cross-sectional study conducted on data from the National Health and Nutrition Examination Survey (NHANES) 1999–2010 revealed an increasing prevalence of medications commonly used for insomnia over time, from 2.0% in 1999–2000 to 3.5% in 2009–2010, especially among older adults and those seeing a mental health provider. Z-drugs were the most commonly used medication (2.97%), followed by trazodone (0.97%) [11]. In Northern Italy, a survey conducted in the 1990s on the rate of hypnotic drug prescription by primary care physicians showed that the majority of prescriptions were for benzodiazepines, with the highest prevalence of hypnotic prescriptions in the elderly and in women [37]. A recent “Italian Expert Opinion and Consensus Recommendations for the Evaluation and Management of Insomnia in Clinical Practice” suggested the use of Melatonin 2 mg prolonged release (PRM 2 mg) as the first choice in subjects aged ≥ 55 years (up to 13 weeks) [14]. Indeed, the production of melatonin is reduced physiologically in elderly subjects and is reported to be lower in patients with insomnia than in good sleepers [38]. Moreover, recent evidence demonstrated that PRM 2 mg mimics the internal melatonin secretion profile by releasing melatonin gradually. Conversely, Z-drugs or short-acting benzodiazepines (in subjects < 65 years old) or sedating antidepressants should be prescribed only in the short term (≤ 4 weeks). They should be used with caution for long term and in the elderly, considering their possible side effects (postural instability, cognitive impairment, tolerance, rebound insomnia upon discontinuation) [39].
The main limitation of this study depends on the limited amount of time that patients had to fill in questionnaires. This reduced the possibility of collecting detailed clinical or therapeutic information, allowing only to classify comorbidities and drugs on macro-categories. In particular, unfortunately we did not include other sleep disorders among possible comorbidities. Therefore, we could not exclude that in some of our patients insomnia could be a symptom of other sleep diseases, such as sleep apnea or restless leg syndrome. Other missing but potentially useful clinical information included the amount of patients referred to the GP because of insomnia and the reasons why the listed drugs were prescribed. Finally, from a methodological point of view, daytime sleepiness should be better investigated through Epworth Sleepiness Scale [40] instead of VAS. On the contrary, considering our recruitment method and the fact that GPs involved in the study were homogeneously distributed over the Italian National territory, this epidemiological survey might be considered to be sufficiently representative of the Italian adult/elderly population, without major bias. Finally, it is worth reminding that this survey was conducted before the COVID-19 pandemic, during which a huge increase of insomnia prevalence and of benzodiazepine use was observed [41].
In conclusion, the results of our study confirm all previous evidence, underlining that insomnia is a quite common disease in primary care among adults-elderly subjects, with different healthy implications, highlighting the variety of comorbidities in insomnia patients over 55 years. This sleep problem represents a huge burden for the GPs that are frequently the first clinicians that have to manage the complaint. During the 20 years between the Morfeo Study and our survey, different alerts to avoid the benzodiazepine use in elderly [39] and diverse recommendation to privilege the non-pharmacological insomnia treatment have been published [12, 14, 34]. Despite this, our results confirm a high use (and probably overuse) of different—also off-label—drugs for insomnia treatment. Further educational initiatives for GPs and specialized physicians should be useful in order to allow a more effective treatment of patients with sleep disorders, in line with current insomnia guidelines.
Author contribution
Paola Proserpio: drafting the manuscript; study concept and design; analysis, acquisition, and interpretation of data; final approval of the manuscript. Dario Arnaldi: drafting the manuscript; study concept and design; statistical analysis and interpretation of data; final approval of the manuscript. Lino Nobili: study supervision; study concept and design; critical revision of the manuscript for important intellectual content; final approval of the manuscript. Giovanni Biggio, Raffaele Ferri, Paolo Girardi, Elio Clemente Agostoni, Raffaele Manni, Antonio Minervino, Laura Palagini, Giuseppe Plazzi: analysis, acquisition, and interpretation of data; critical revision of the manuscript for important intellectual content; final approval of the manuscript.
Declarations
Ethical approval
The study was approved by the Ethical Committee “Comitato Etico Regionale della Liguria” (Register Number: 143/2022_ DB id 12,253).
Conflict of interest
Paola Proserpio has received honoraria for advisory board from Italfarmaco and Jazz Pharmaceuticals. Raffaele Ferri has received consulting fee from Jazz Pharmaceutical. Raffaele Manni has received consulting fee from Fidia Pharma. Giuseppe Plazzi has received consulting fees from Jazz Pharmaceuticals, Takeda, Idorsia, and Bioprojet. Dario Arnaldi has received honoraria for lectures from Bruno Pharma, Fidia Pharma, and Jazz Pharmaceuticals. Lino Nobili has received honoraria for lectures from Bioprojet and consulting fees from Fidia Pharma, Eisai, and Roche. All other authors have no relevant conflict of interests to disclose related to the content of the current manuscript.
Footnotes
Highlights
• Insomnia represents a very common disturbance in the primary care.
• Insomnia is frequently associated with different psychiatric and somatic disorders, especially anxiety-depressive disorder, cardiovascular disorders, and dementia.
• Subjects with insomnia complain higher levels of daytime sleepiness.
• Patients with insomnia show a higher use of benzodiazepine, Z-drugs, antidepressants, and prolonged release melatonin.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lino Nobili and Dario Arnaldi contributed equally to this work.
References
- 1.Morin CM, Benca R. Chronic insomnia. The Lancet. 2012;379:1129–1141. doi: 10.1016/S0140-6736(11)60750-2. [DOI] [PubMed] [Google Scholar]
- 2.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 3.Käppler C, Hohagen F. Psychosocial aspects of insomnia. Results of a study in general practice. Eur Arch Psychiatry Clin Neurosci. 2003;253:49–52. doi: 10.1007/s00406-003-0406-9. [DOI] [PubMed] [Google Scholar]
- 4.Morin CM, LeBlanc M, Daley M, et al. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7:123–130. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 5.Riemann D. Insomnia and comorbid psychiatric disorders. Sleep Med. 2007;8(Suppl 4):S15–20. doi: 10.1016/S1389-9457(08)70004-2. [DOI] [PubMed] [Google Scholar]
- 6.Taylor DJ, Mallory LJ, Lichstein KL, et al. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30:213–218. doi: 10.1093/sleep/30.2.213. [DOI] [PubMed] [Google Scholar]
- 7.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Javaheri S, Redline S. Insomnia and risk of cardiovascular disease. Chest. 2017;152:435–444. doi: 10.1016/j.chest.2017.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asplund null, Sleep and hypnotic use in relation to perceived somatic and mental health among the elderly. Arch Gerontol Geriatr. 2000;31:199–205. doi: 10.1016/S0167-4943(00)00075-3. [DOI] [PubMed] [Google Scholar]
- 10.Quera-Salva MA, Orluc A, Goldenberg F, Guilleminault C. Insomnia and use of hypnotics: study of a French population. Sleep. 1991;14:386–391. doi: 10.1093/sleep/14.5.386. [DOI] [PubMed] [Google Scholar]
- 11.Bertisch SM, Herzig SJ, Winkelman JW, Buettner C. National use of prescription medications for insomnia: NHANES 1999–2010. Sleep. 2014;37:343–349. doi: 10.5665/sleep.3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26:675–700. doi: 10.1111/jsr.12594. [DOI] [PubMed] [Google Scholar]
- 13.Sateia MJ, Buysse DJ, Krystal AD, et al. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13:307–349. doi: 10.5664/jcsm.6470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Palagini L. Expert opinions and consensus recommendations for the evaluation and management of insomnia in clinical practice: joint statements of five Italian scientific societies. Front Psychiatry. 2020;11:13. doi: 10.3389/fpsyt.2020.00558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Terzano MG, Parrino L, Cirignotta F, et al. Studio Morfeo: insomnia in primary care, a survey conducted on the Italian population. Sleep Med. 2004;5:67–75. doi: 10.1016/j.sleep.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 16.Terzano MG, Cirignotta F, Mondini S, et al. Studio Morfeo 2: survey on the management of insomnia by Italian general practitioners. Sleep Med. 2006;7:599–606. doi: 10.1016/j.sleep.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 17.Espie CA, Kyle SD, Hames P, et al. The Sleep Condition Indicator: a clinical screening tool to evaluate insomnia disorder. BMJ Open. 2014;4:e004183. doi: 10.1136/bmjopen-2013-004183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palagini L, Ragno G, Caccavale L, et al. Italian validation of the Sleep Condition Indicator: a clinical screening tool to evaluate insomnia disorder according to DSM-5 criteria. Int J Psychophysiol Off J Int Organ Psychophysiol. 2015;98:435–440. doi: 10.1016/j.ijpsycho.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 19.American Academy of Sleep Medicine (2014) International classification of sleep disorders-third edition (ICSD-3) American Academy of Sleep Medicine, Darien
- 20.Jean-Louis G, Magai CM, Cohen CI, et al. Ethnic differences in self-reported sleep problems in older adults. Sleep. 2001;24:926–933. doi: 10.1093/sleep/24.8.926. [DOI] [PubMed] [Google Scholar]
- 21.Bjorvatn B, Meland E, Flo E, Mildestvedt T. High prevalence of insomnia and hypnotic use in patients visiting their general practitioner. Fam Pract. 2017;34:20–24. doi: 10.1093/fampra/cmw107. [DOI] [PubMed] [Google Scholar]
- 22.Aikens JE, Rouse ME. Help-seeking for insomnia among adult patients in primary care. J Am Board Fam Pract. 2005;18:257–261. doi: 10.3122/jabfm.18.4.257. [DOI] [PubMed] [Google Scholar]
- 23.Shekleton JA, Rogers NL, Rajaratnam SMW. Searching for the daytime impairments of primary insomnia. Sleep Med Rev. 2010;14:47–60. doi: 10.1016/j.smrv.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 24.Suh S, Cho N, Zhang J. Sex differences in insomnia: from epidemiology and etiology to intervention. Curr Psychiatry Rep. 2018;20:69. doi: 10.1007/s11920-018-0940-9. [DOI] [PubMed] [Google Scholar]
- 25.Kim K, Uchiyama M, Okawa M, et al. An epidemiological study of insomnia among the Japanese general population. Sleep. 2000;23:41–47. doi: 10.1093/sleep/23.1.1a. [DOI] [PubMed] [Google Scholar]
- 26.Yang B, Wang Y, Cui F, et al. Association between insomnia and job stress: a meta-analysis. Sleep Breath Schlaf Atm. 2018;22:1221–1231. doi: 10.1007/s11325-018-1682-y. [DOI] [PubMed] [Google Scholar]
- 27.Monk TH, Buysse DJ, Schlarb JE, Beach SR. Timing, duration and quality of sleep, and level of daytime sleepiness in 1166 retired seniors. Healthy Aging Clin Care Elder. 2012;4:33–40. doi: 10.4137/HACCE.S10596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cheatle MD, Foster S, Pinkett A, et al. Assessing and managing sleep disturbance in patients with chronic pain. Sleep Med Clin. 2016;11:531–541. doi: 10.1016/j.jsmc.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Proserpio P, Arnaldi D, Nobili F, Nobili L. Integrating sleep and Alzheimer’s disease pathophysiology: hints for sleep disorders management. J Alzheimers Dis. 2018;63:871–886. doi: 10.3233/JAD-180041. [DOI] [PubMed] [Google Scholar]
- 30.Shi L, Chen S-J, Ma M-Y, et al. Sleep disturbances increase the risk of dementia: a systematic review and meta-analysis. Sleep Med Rev. 2017 doi: 10.1016/j.smrv.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 31.Irwin MR, Vitiello MV. Implications of sleep disturbance and inflammation for Alzheimer’s disease dementia. Lancet Neurol. 2019;18:296–306. doi: 10.1016/S1474-4422(18)30450-2. [DOI] [PubMed] [Google Scholar]
- 32.Krueger JM, Frank MG, Wisor JP, Roy S. Sleep function: toward elucidating an enigma. Sleep Med Rev. 2016;28:46–54. doi: 10.1016/j.smrv.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Almondes KM, Costa MV, Malloy-Diniz LF, Diniz BS. Insomnia and risk of dementia in older adults: systematic review and meta-analysis. J Psychiatr Res. 2016;77:109–115. doi: 10.1016/j.jpsychires.2016.02.021. [DOI] [PubMed] [Google Scholar]
- 34.Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165:125–133. doi: 10.7326/M15-2175. [DOI] [PubMed] [Google Scholar]
- 35.Walsh JK, Schweitzer PK. Ten-year trends in the pharmacological treatment of insomnia. Sleep. 1999;22:371–375. doi: 10.1093/sleep/22.3.371. [DOI] [PubMed] [Google Scholar]
- 36.Moloney ME, Konrad TR, Zimmer CR. The medicalization of sleeplessness: a public health concern. Am J Public Health. 2011;101:1429–1433. doi: 10.2105/AJPH.2010.300014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Balestrieri M, Bortolomasi M, Galletta M, Bellantuono C. Patterns of hypnotic drug prescription in Italy. A two-week community survey. Br J Psychiatry J Ment Sci. 1997;170:176–180. doi: 10.1192/bjp.170.2.176. [DOI] [PubMed] [Google Scholar]
- 38.Touitou Y. Human aging and melatonin. Clinical relevance Exp Gerontol. 2001;36:1083–1100. doi: 10.1016/S0531-5565(01)00120-6. [DOI] [PubMed] [Google Scholar]
- 39.Kripke DF, Langer RD, Kline LE. Hypnotics’ association with mortality or cancer: a matched cohort study. BMJ Open. 2012;2:e000850. doi: 10.1136/bmjopen-2012-000850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 41.Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]