Abstract
Two highly overriding problems that the society is facing today are stress and obesity. This narrative review article explains the vicious cycle of how stress leads to obesity and vice versa. Stress and obesity are interconnected to each other through different lines of cognition, behavior, and physiology. Stress can interfere with cognitive processes like self-regulation. Stress can also influence behavior by indulging in overeating of foods that are high in calories, fat, and sugar. Stress also invigorates the generation of biochemical hormones and peptides, for example, leptin, ghrelin, and neuropeptide Y. This article also extracts the contribution of weight stigma and social stress in producing obesity in an obesogenic process. Recent Studies describe that psychological distress and elevated cortisol secretion promote abdominal fat, a feature of the metabolic syndrome, improvements in mindfulness, chronic stress, and cortisol awakening response (CAR) were associated with reductions in abdominal fat. Mindfulness intervention for stress suggests that mindfulness training improves eating patterns and the CAR, which may reduce abdominal fat over time. Obesity has a multifaceted etiology. In this review, several factors of stress are identified that affect the development of obesity. This review also provides valuable insight into the relationship between obesity and stress.
Keywords: Abdominal fat, hypothalamo–hypophyseal system, ideal body weight, obesity, social stress
Introduction
To understand the relationship between stress and obesity, we need to understand these terms distinctively. Obesity is over 20% of extra body fat than the usual accumulation of an individual's body mass index. It mainly happens when one maintains an unhealthy lifestyle and poor eating habits. Firstly, if we consume three meals a day, the high amounts of energy, protein, fats, and sugars need to be digested and burnt off for the metabolism of the body either by some physical activity or exercises. When the body consumes too much food, and if we do not work out our carbs, it results in obesity. Obesity is increasing rapidly throughout the world and has major consequences for the public well-being. More than 1.9 billion adults were overweight and of these over 650 million were obese and, 39% of men and 40% of women were overweight.[1] It is estimated that over 13% adult population of the world were obese. Throughout the world prevalence of obesity tripled between 1975 and 2016. Obesity is a worldwide health challenge that will cause an increase in chronic illnesses and is in this way described as a worldwide health crisis.[2] Diet and workout have been the real assignments concerning preventive measures and treatment of obesity; in any case, different elements are presently being all the more firmly considered including the role of the HPA axis, releasing cortisol.[3] In the previous years, there is evidence that stress causes obesity especially when there is an increase in the levels of the stress hormone cortisol called glucocorticoid which plays a crucial role in the development of obesity. Glucocorticoid redistributes the white adipose tissues to the area and increases the hunger pangs and craving for energy-rich food like sugar and fat called comfort food.[4] In our modern society, the prevalence of obesity is linked with an increase in the cortisol production which in turn increases chronic stress, intake of food with high sugar and fat content and less sleep.[5,6]
Stress, on the other hand, is our psychological experience that helps in the development and maintenance of obesity. For this article, stress is defined using Andrew Baum's comprehensive characterization: “a negative emotional experience accompanied by predictable biochemical, physiological, cognitive, and changes in behavior that are directed either toward altering the stressful event or accommodating to its effects”.[7] A national survey showed a majority of US citizens’ reports moderate to high levels of stress.[8] About one-third of US adults have a BMI of more than 30, which falls under the obese category. Stress is depicted as a condition in which desires whether, hereditarily modified, built up by earlier learning, or concluded from conditions, do not coordinate present or foreseen impression of the internal or external condition.[9] Stress, both physical and mental, can be viewed as a part of life that each individual will experience somewhat. Stress is characterized as a ‘’condition of undermined or perceived as compromised homeostasis’.[10] Stressors, including damage, commotion, extreme cold, loss of work and low social standing may initiate the stress system and cause an immediate or perceived risk of homeostasis.[11] The stress system comprises of two noteworthy parts: (i) the sympathetic nervous system, which without anyone else's input and by means of the adrenal medulla secretes noradrenaline and adrenaline and triggers the fight-or-flight mechanism; and (ii) the hypothalamic– pituitary– adrenal (HPA) axis, which release cortisol, an adrenal cortex-derived hormone that plays a main role in the physiology of stress reactions[11] as well as illness.[12]
Methodology
A literature review was undertaken that linked stress and obesity from various cognitive, behavioral and physiological perspectives. Electronic databases, including Medline, Cinahl, Cochrane Library, PscyhInfo and Google scholar were searched for relevant studies from articles published in English language between 2000 and December 2020. Search terms used in these databases included, but were not limited to: stress, obesity, cognition, cortisol awakening response (CAR), metabolic syndrome, leptin, ghrelin, and neuropeptide Y, HPA axis and BMI.
Causes of obesity and stress
There are one or more factors like strong genetic origins,[13] eating behavior and environment that causes obesity. Nowadays, most of the people eat anything, regardless of its nutritional value, without bothering about the quality or quantity of the food. Increasing demands and population results in introductions of more cultures and traditions, which lead to new pop food cultures and the opening of fast food outlets in every corner of the world. These kinds of foods are high calorie and have trans-fat content which raises the cholesterol levels, particularly the LDL, i.e., the bad cholesterol and can lead to a lot of factors such as high blood pressure, heart disease, stress, diabetes type 2 and can even cause death.[14]
Even if you are eating ‘comfort food’ in large portions, it is still risky and unhealthy as it will cause indigestion. Consumption of canned products and sugary drinks which are high in sugar as well as fat also leads to obesity. In earlier studies, there is evidence that stress causes obesity especially when there is an increase in the levels of stress hormone cortisol called glucocorticoid, which plays a crucial role in the development of obesity. Glucocorticoid redistributes the white adipose tissues to the area and increases the hunger pangs and cravings for energy-rich food consisting of sugar and fat.[4] High levels of cortisol hormone may increase stress-related eating as well.[15] Data suggested by[16] that stress-related eating is more common among women as compared to men. There is evidence suggesting the adverse effects of stress on eating behavior. For instance, some people skip a meal, and some indulge in binge eating.[17] Irregular eating pattern increases insulin level in the body.[18] Humans are not the only ones who change their eating patterns under stress. A study on rats stated that rats eat lard and sugar-rich food when they are stressed.[19] Let us now see how obesity and stress are correlated with each other and how do they impact our human bodies. In our modern society, the prevalence of obesity is linked with an increase in the cortisol production which in turn increases chronic stress, intake of food with high sugar and fat content and decreases the sleep.[5] Chronic stress has various emotional and physiological factors like interpersonal conflicts, relationship problems, unemployment, loss of a close family member, chronic illness, hunger deprivation, insomnia and, some drug effects which cause obesity.[20]
Stress can disrupt the activity level by increasing sedentary activity or by decreasing physical activity. A survey on 12000 participants found that higher stress level was linked with less physical activity. People having office desk jobs have more hectic life which leads to stress as it is already so packed up for them.[21] They do not have the energy to go back home either by walking rather prefer a conveyance such as a bus or a car to go home. To divert their mind from the stress, they sit down, relax and watch TV while surfing the internet. Nowhere in their minds, have they even thought of working out in the gym to burn calories. This kind of lifestyle becomes monotonous leading to the stress and tension because of working competition pressures and health conditions being not maintained parallelly. It becomes one of the demotivating factors of one's lifestyle contributing to self-doubt, and lack of fitness leads to an obese body structure.
Relationship between Stress and Obesity
Nowadays, when a patient is diagnosed with any medical condition, a doctor examines all the factors related to the cause of that condition. One of them is a psychological factor that observes the level of mental stability and checks if stress is worsening that medical condition or not. For example, in autoimmune diseases such as psoriasis, particularly psoriatic arthritis, stress is one of the main factors which can worsen these medical conditions. In this, a healthy weight has to be maintained, and especially in cases of people of older age, not losing weight will put them under stress and further worsen their mental and physical well-being and cause a further decrease in physical activity leading to obesity [Figure 1].
Figure 1.
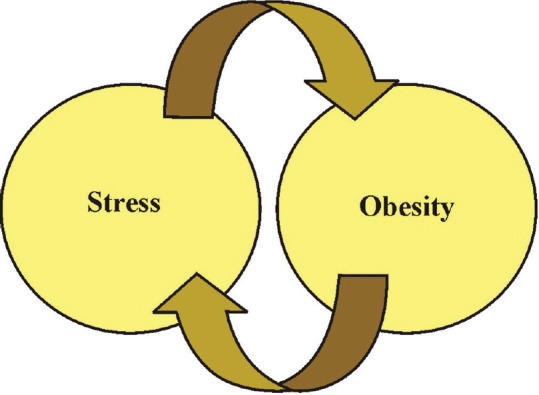
Relationship of Stress and Obesity. The vicious cycle of stress and obesity shows stress can increase appetite, cravings for fat and sugar-rich foods, which further leads to obesity
According to a study, stress has not been given importance to understand obesity.[22] There have been studies and researches done to examine the relation of the above two issues through surveys and psychological methods. These studies have classified stress into two categories: acute and chronic. In chronic stress, there is a significant risk factor of excess weight gain or heart disease.[23] This kind of stress is observed when the body's metabolism is not functioning properly during dieting. In general, blood pressure and heart rate are measured to examine the levels of chronic stress. According to a study there is a relationship between chronic stress, food cravings, and body mass index (BMI).[24] A community-based sample of 619 adults was collected and their heights and weights were measured. Chronic stress had a major direct impact on food cravings, and food cravings had a major direct impact on body mass index. The overall effect of chronic stress on the body mass index was significant. According to the research, chronic stress might enhance motivation for rewarding substances and behaviors and indicate that high food cravings may contribute to stress-related weight gain.
It has been shown that hunger and stress are correlated leading to the phenomenon of “reactive obesity” test.[25] In this research, people eat more during the afternoon-evening hours, as proved in the survey. Besides this, as we consume all our “guilty pleasures” of having all kinds of comfort food, is indeed “guilty” enough, meaning, bad enough for the body itself leading to medical stress and psychological stress at a higher rate. To figure out the relationship between stress and obesity number of experimental and psychological research studies were conducted in the past. Firstly, the concept of Body Mass Index (BMI) is calculated by one's weight (kg/lbs) divided by the height squared and categorized according to the BMI score as BMI of 25-29 is overweight, 30-34 is obese, 35-40 is severely obese; BMI >40 is morbidly obese. Majority of studies have determined that the optimal BMI with the least risk for mortality is a BMI of 23 to 24.9. BMI below or above this range seems to increase mortality risk.[15]
A study engaging medical participants via psychiatric interviews was aimed to know their condition by knowing how they tackle themselves, their behavior towards certain given situation as an example, how do they respond in problematic situations, the stability of their mind and the personality of the person himself. This study was an active way of deciding how the mechanisms of stress work mentally in their minds in terms of alternative scale levels described.[22] There is use of statistical methods in a more logical way with the help of models and further calculations based on statistical analysis stating the study group and the control group percentages denoting the social classification, marital status, education level, psychiatric examination, professions, and BMI. From the above, it has been seen that the control subjects are facing more primary illness rather than obesity. But overall, children of divorced parents and the younger generation are more prone to obesity comparative to the control group. There are studies showing that high emotional behaviors lead to an individual eating anything without even considering what he/she is eating and how much portion is being consumed during that mental trauma or rather depressed state. Thus, the reasons for leading stress levels can be genetic, unemployment, bad lifestyle choices, personal tensions, food addiction, and an unhealthy diet have contributed to the risk of obesity.
Stress to Obesity and Obesity to Stress
One of the most important factors to understand is that obesity causes stress and stress causes obesity. Stress affects eating behavior, sleep cycle, physical and psychological changes which interfere with executive, cognitive and self-regulation function of a human brain. Stress decreases self-regulatory cognitive and executive functioning.[26] A study wherein 224 children were given a medium plate of candy which they could eat now or later, and it was observed that children with higher stress levels ate then and there and they also ate a larger quantity of candy. Failure in self-regulation deteriorates human behavior and increases eating disorders, sleep deprivation and physical inactivity.[27] Obesity is a stress with the presence of the weight stigma, which is a vicious cycle in itself where stress leads to obesity and obesity leads to stress.[28] Various pathways are finest for intervention. Some of them were the[29] mindfulness 4-month eating program and stress-induced eating.[30]
Some studies also show that eating reduces the psychological stress of the HPA axis on the body. Hence targeting eating is a greater challenge. New researchers have found that if the physiological and biochemical levels are targeted, obesity can be eliminated efficiently. The most logical pathway is stress itself as it also intervenes in stress stigma and helps in reducing obesity[31,32,33,34] [Figure 2].
Figure 2.
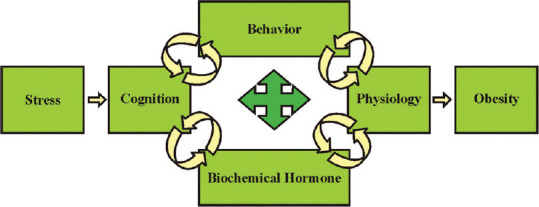
A pathway that shows how stress leads to obesity. Stress can have a direct effect on cognition, our behaviour, and physiological functions. It can also trigger the release of biochemical hormones thus increasing the desire for foods, which eventually leads to obesity
Cognition
Self-Regulation can be defined in many ways. It involves controlling behaviors such as bad eating habits and low physical activity which is required to prevent obesity.[35] Stress can interfere with brain functions which are essential for self-regulation.[36] A study by[37] stated that stress can also trigger unhealthy eating by hindering cognitive emotion regulation.
Sleep duration
Stress is known as a sleep disruptor.[38] Sleep is an important indicator of overall good health. The decrease in sleep duration is directly proportional to obesity.[39] A review of 31 cross-sectional studies found that a decrease in sleep duration is directly associated with obesity and overweight and other abdominal adiposity markers.[40] Another model is based on the results of experimental studies on sleep deprivation that connect poor bedtime habits like going to bed too late leads to weight.[40] Thus, many pathways connect decreases in sleep duration to obesity.
Reward processing and gut microbiome
Foods higher in sucrose and fat through reward processing motivate people to overeat them.[41] Fat and sugar-rich foods have addictive qualities. Stress triggers the release of dopamine, a neurotransmitter that increases the desire for foods which leads to obesity.[42] Another pathway that links stress to obesity is the gut microbiome. There is evidence suggesting that the gut microbiome is responsible for stress. An animal study has shown that the gut microbiome is affected by acute and chronic stress.[43,44] The gut microbiome also affects the eating behavior in animals, but as of now, there is less human literature on gut microbiome & obesity.
Role of Hormones in Obesity
Leptin, Ghrelin, and neuropeptide Y are the biochemical hormones that are pertinent to weight gain & obesity.
Leptin and Ghrelin
In contrast to stress & cortisol, a small amount of literature found for leptin and ghrelin's response to stress. One study stated that leptin decreases appetite and ghrelin increases it.[45] Another study examined that leptin increased stress generated eating.[46] For this, study participants were repeatedly sampled for leptin and were offered a range of high & low fat sweet and savory foods. Those participants who reacted to the stressor with the most leptin ate a little amount of high fat sweet food. Stress could, therefore, lead to obesity and leptin resistance by increasing leptin repeatedly. According to a study, Ghrelin stimulates food cravings and plays an important role in reward-driven eating behaviors.[47] Compared to leptin, ghrelin constitutes a simpler path from stress to obesity.[48] In their study, they noticed that ghrelin levels increased in stressful conditions. In a study, post-stress participants were offered food which led to a decrease in ghrelin levels in non-emotional eaters.
Neuropeptide Y
It is a peptide biochemical hormone that stimulates appetite[49] and lipogenesis[50] and converts glucose into fat. Most of the evidence from animal studies shows that chronic stress stimulates the secretion of NPY.[51] This area needs further research as this study did not show high food intake related to ghrelin levels and increase adiposity.[52] Overall animal & human studies examined the ability of NPY to raise the effect of stress on obesity, but this area needs more research.
How can Social Stress Contribute to Obesity?
Here we will focus on how chronic stress plays a major role in the development of obesity and what are its effects on the lifestyle preferences, food consumption and the regional distribution of adipose tissue. There is evidence from both human and animal studies which show a linkage of the nervous system to hypothalamic-pituitary-adrenal axis hyperactivity with the issue of obesity and how stress comes to a role-play altering the food patterns and promoting human being's craving for “comfort foods”.[53] Over the past decades, obesity has risen dramatically due to a sedentary lifestyle and overeating unhealthy foods including genetic, cultural, and industrial factors. In perspective of social aspects, this kind of stress is faced by people who are dealing with socioeconomic status, personal conflicts with family, friends and colleagues, stressful working atmospheres, high level of self-doubt, low self-esteem, underestimating oneself, maintaining office life versus home life etc.[54,55,56,57] As chronic factors, they affect body weight drastically and increase the belly fat. All these factors can be controlled if these are addressed properly with the easy accessibility of the health care, counselling, supportive resources which could result in steady control of managing social stress with the participation of society.[58] Stress also has an impact on the food diet and its lifestyle. Many people have said that whenever they have stress either they eat a quantitative amount of “comfort foods” or they have a loss of appetite. This depends on how these 'stressors’ reflect different personalities in different ways. Also, ‘craving’ leads to an increase in food intake of high content in sugar and fat, i.e., carbohydrates.[59,60] Although it satisfies our mind for a temporary time then gets into an aggravated state of multiple mood swings. Thus, chronic stress occurs due to the easy access of high-palatable “comfort foods,” energy-dense foods and lack of active physical environment which sets the rise of obesity in a drastic manner.
Stress and the HPA Axis
In health, stress is defined to disturb the equilibrium of the human physiological balance. Although it is considered a negative aspect, its response is there to check on how to tackle this homeostasis (equilibrium).[61] In acute stress, there is a functioning system of the autonomic nervous system (ANS) which gets activated with the following axis known as the hypothalamic-pituitary-adrenal (HPA) axis this controls the functioning of the blood pressure, heart rate, digestion, hormone release, and respiration.[62] How does the sensory system and endocrine framework work during distressing circumstances? The endocrine system under chronic stress brings up many changes. Endocrine system comprises organs, hormones, circulation and target organs. The major endocrine organs engaged with the stress response are pituitary, adrenal and thyroid gland.
The hypothalamus is a small structure present underneath the thalamus or above brain stem. It joins the nervous system to the endocrine system through the pituitary gland. It controls the secretion of hormones from the pituitary gland. Hypothalamus communicates with the remainder of the body through the autonomic sensory system, sympathetic nervous system. Under stress, bodies release ACTH (adrenocorticotropic hormone) which further stimulates the release of stress hormone called cortisol
Triggering the HPA Axis
There is also a kind of “fight or flight” response through the system of the sympathetic nervous system (SNS),[63] which tends to increase all of the functioning under the ANS. The HPA axis is lingered due to stress as the Paraventricular nucleus of the hypothalamus (PVN) is triggered. HPA axis plays an important role in the body's natural reactions to stress.
What happens in stressful circumstances?
The hypothalamus releases a hormone called the corticotropin hormone (CRH). CRH signals the pituitary gland to release the Adrenocorticotropic hormone (ACTH) into the bloodstream.
The released ACTH goes to the adrenal gland where it prompts the release of glucocorticoids from the adrenal cortex.
One of these glucocorticoids is Cortisol which has a significant job in stress response.
With an increase in cortisol level, epinephrine and norepinephrine are released from adrenal medulla.
The release of cortisol causes various changes that help the body to manage stress. For instance, it encourages the body to prepare vitality like glucose [Figure 3].
Figure 3.
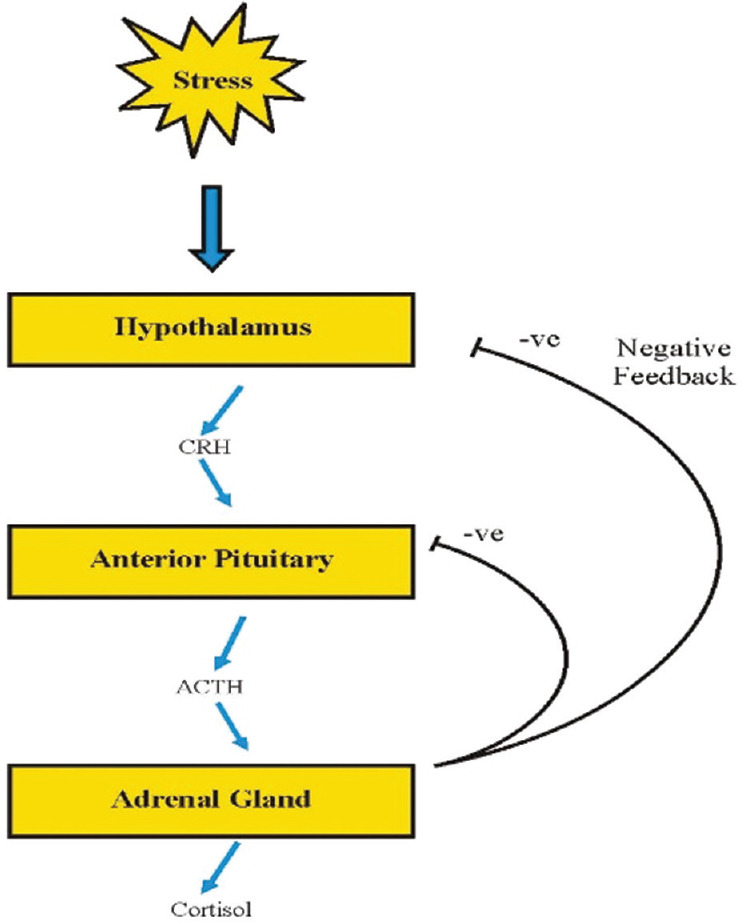
Made correction in figure “Adrenal Gland instead of Anterior Pituitary”
Negative Feedback Component
What happens when cortisol level turns out to be high in blood?
When abnormal levels of cortisol reach the receptors in the nerve center, the body shuts down the stress response. Thus, the HPA response is ended through the negative response by the ACTH and the CRH release of hormones and also counterbalanced the ANS, meaning that although stress is needed to check the survival but it has to be monitored as well so that the homeostasis would be maintained throughout[64,65]
How cortisol causes belly fat?
When there is an increase in stress, there is an increase in blood glucose which results in an increase in insulin level. When insulin levels are constantly raised, the cortisol causes insulin resistance which subsequently increases belly fat. We even observe numerous medical issues like in Cushing Syndrome, when cortisol is incessantly raised, it makes individuals gain weight.
Mindfulness Intervention for Stress Eating to Control Obesity
It's established that stress is related to obesity and vice-versa. Obesity and stress cause psychological issues, health problems, lack of sleep etc. To overcome stress and obesity, it is important that we understand that they both are to be studied together. To remove the excess fat from the body, focus on serotonin, cortisol and neuropeptide Y can help significantly.[66] One must break the cycle and eat consciously. Smaller portions of food intake are suggested than heavy meals with high-calorie intake. Simply skipping meals is also another mistake that should be avoided. The body needs a certain amount of calorie else the cycle for stress and obesity will never end. Eating right and eating timely is one of the biggest busters to deal with stress and obesity.[67]
We all know that obesity causes stress and stress causes obesity. Hence to reduce stress one has to control obesity and to remove chronic stress from one's life, one has to lose all the abdominal adiposity and excess fat. A study was performed on 47 women for four months who were obese and overweight. They were analyzed to study the effects of a mindfulness intervention for stress eating and abdominal fat. Results from the above exploratory controlled study on obese women showed that Mindfulness training benefits obese women are protecting them from metabolic syndrome. It improved their eating patterns, responsiveness, CAR which helps in reducing anxiety, serum cortisol level, and abdominal fat by.[28]
The abdominal fat reduction did not take place across all participants. Participants who consciously reduced their emotional eating and chronic stress seemed to have benefited more from the mindfulness program. This is the first study to acknowledge that CAR was reduced to a greater extent in treatment group participants than control groups. There was also prevention from gaining weight across a subgroup of obese participants. The exercise did not help in reducing abdominal adiposity across lumbar vertebrae -- the part with huge visceral fat. There was an appropriate dose response that supported the theory of improvements in psychological level due to intervention leading to further improvements in mindfulness. If this program is integrated with active weight loss strategies, it may lead to a substantial decrease in abdominal adiposity.[68]
Mindfulness intervention helps in reducing the abdominal adiposity over time by simply improving eating habits and CAR (cortisol awakening response). CAR is measured using the Salivary Cortisol wherein the samples are collected from the participant's right after waking up, 30 minutes post and just before sleeping for four days of pre and post treatment. Four days of assessment was needed to ensure the presence of a trait measure.[69] Apart from that, there were also Serum Cortisol measures that checked the empty stomach early morning blood samples. A standard stadiometer, digital scale, tape measure, DEXA scans are used to measure the height, weight, waist circumference, body fat.
Mindfulness skills were also assessed through KIMS by (Baer, Smith &Allen 2004) computerized questionnaires that focused on the observation, expression, participation, attention and acceptance skills, Body Responsiveness Scale by[70] appraised on the relationship between the physical and the psychological states, Wheaton Chronic Stress Inventory helps in calculating the impact of relationships, work, problems in life, etc. on one's life and measures the level of stress,[71] and The Perceived Stress Scale appraise on a participant's response and perception to some stress reacted issue experienced in the near past,[72] State-Trait Anxiety Scale,[73] Dutch Eating Behaviors Questionnaire (DEBQ) assesses restraint, emotional and external based eating.[74] Dietary Restrained analyses behavior while try to restrict consumption because of being overweight. Anger, anxiety, fear triggers emotional eating and external eating assesses the impact of the smell of food, the presence of other people eating in front of the participant.
The intervention program was developed by extracting guided meditation practices that help in realizing stomach fullness and satisfaction, food cravings and triggers from Mindfulness-Based Eating Awareness Training (MB-EAT),[75] mindful yoga stretches, sitting meditations from Mindfulness-Based Stress Reduction (MBSR),[76] and 3-minutes breathing space from Mindfulness-Based Cognitive Therapy (MBCT).[70]
Conclusions
Stress and obesity are interrelated, and one leads to the other. They both should be studied together. To eliminate obesity, one has to target stress itself. This is the most efficient way of interfering in the weight stigma and correcting the cause. Social stress can be managed by healthcare and supportive organizations along with participation with the society. Stress is definitely not the only factor involved in obesity— many genetic and environmental causes contribute to it, but it is one of the biggest reasons contributing towards it. Few commonly observed reasons behind stress are chronic social stress, often arising from poor interpersonal relationships, job or unemployment, poor self-esteem, and low socioeconomic status and so on. Researches have revealed that people eat more in stress as compared to when they are happy because of the release of a hormone by our body called cortisol during stress. However, stress-induced eating can be hard to eliminate because eating is pleasurable. Also due to lack of awareness, combating stress is not even part of the conversation for obesity prevention and treatments. A close examination of the patient's lifestyle, gender, and psychological state can also help in analyzing the root cause of obesity. Current algorithms to treat obesity focus mainly on decreasing energy intake and increasing energy expenditure. Thus, it is advisable for doctors to help their patient in taking mindfulness training that may improve the ability to cope effectively with stressful experiences and reduce the reliance on “comfort foods” to manage stress or other negative emotions promoting more favorable body fat distribution over time. It sounds easy but is difficult to implement especially for someone who is combating stress over a long period of time consistent mind training can help in developing healthy food habits. Self-realization of stress eating and combating it through measures like walking, taking a bath meditating for 10 minutes, etc. can also help reduce stress and allow the cravings to pass.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kim KB, Shin YA. Males with obesity and overweight. J Obes Metab Syndr. 2020;29:18–25. doi: 10.7570/jomes20008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kraak VI, Story M. A public health perspective on healthy lifestyles and public–private partnerships for global childhood obesity prevention. J Am Diet Assoc. 2010;110:192–200. doi: 10.1016/j.jada.2009.10.036. [DOI] [PubMed] [Google Scholar]
- 3.Holmes ME, Ekkekakis P, Eisenmann The physical activity, stress and metabolic syndrome triangle: A guide to unfamiliar territory for the obesity researcher. Obes Rev. 2010;11:492–507. doi: 10.1111/j.1467-789X.2009.00680.x. [DOI] [PubMed] [Google Scholar]
- 4.Fardet L, Fève B. Systemic glucocorticoid therapy: A review of its metabolic and cardiovascular adverse events. Drugs. 2014;74:1731–45. doi: 10.1007/s40265-014-0282-9. [DOI] [PubMed] [Google Scholar]
- 5.Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975–2006. Sleep. 2010;33:37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen S, Janicki-Deverts DE. Who's stressed. Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009 1? J Appl Soc Psychol. 2012;42:1320–34. [Google Scholar]
- 7.Baum A. Stress, intrusive imagery, and chronic distress. Health Psychol. 1990;9:653–75. doi: 10.1037//0278-6133.9.6.653. [DOI] [PubMed] [Google Scholar]
- 8.Schuster MA, Stein BD, Jaycox LH, Collins RL, Marshall GN, Elliott MN, et al. A national survey of stress reactions after the September 11, 2001, terrorist attacks. N Engl J Med. 2001;345:1507–12. doi: 10.1056/NEJM200111153452024. [DOI] [PubMed] [Google Scholar]
- 9.Goldstein DS. Adrenal responses to stress. Cell Mol Neurobiol. 2010;30:1433–40. doi: 10.1007/s10571-010-9606-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charmandari E, Tsigos C, Chrousos G. Endocrinology of the stress response. Annu Rev Physiol. 2005;67:259–84. doi: 10.1146/annurev.physiol.67.040403.120816. [DOI] [PubMed] [Google Scholar]
- 11.De Vriendt T, Moreno LA, De Henauw S. Chronic stress and obesity in adolescents: Scientific evidence and methodological issues for epidemiological research. Nutr Metab Cardiovasc Dis. 2009;19:511–9. doi: 10.1016/j.numecd.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 12.Berczi I. Nagy EJHoIMATK, Ed. Hormones as Immune Modulating Agents. 1997:75–120. [Google Scholar]
- 13.Bell CG, Walley AJ, Froguel P. The genetics of human obesityy. Nat Rev Genet. 2005;6:221–34. doi: 10.1038/nrg1556. [DOI] [PubMed] [Google Scholar]
- 14.Sharafeldin K, Rizvi MR. Effect of traditional plant medicines (Cinnamomum zeylanicum and Syzygium cumini) on oxidative stress and insulin resistance in streptozotocin-induced diabetic rats. J Basic Appl Zool. 2015;72:126–34. [Google Scholar]
- 15.Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91:449–58. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 16.Geliebter A, Aversa A. Emotional eating in overweight, normal weight, and underweight individuals. Eat Behav. 2003;3:341–7. doi: 10.1016/s1471-0153(02)00100-9. [DOI] [PubMed] [Google Scholar]
- 17.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23:887–94. doi: 10.1016/j.nut.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Farshchi H, Taylor M, Macdonald IA. Regular meal frequency creates more appropriate insulin sensitivity and lipid profiles compared with irregular meal frequency in healthy lean women. Eur J Clin Nutr. 2004;58:1071–7. doi: 10.1038/sj.ejcn.1601935. [DOI] [PubMed] [Google Scholar]
- 19.Pecoraro N, Reyes F, Gomez F, Bhargava A, Dallman MF. Chronic stress promotes palatable feeding, which reduces signs of stress: Feedforward and feedback effects of chronic stress. Endocrinology. 2004;145:3754–62. doi: 10.1210/en.2004-0305. [DOI] [PubMed] [Google Scholar]
- 20.McEwen BS. Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiol Rev. 2007;87:873–904. doi: 10.1152/physrev.00041.2006. [DOI] [PubMed] [Google Scholar]
- 21.Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychol. 2003;22:638–42. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- 22.Koski M, Naukkarinen H. The relationship between stress and severe obesity: A case-control study. Biomed Hub. 2017;2:1–13. doi: 10.1159/000458771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carroll D, Phillips AC, Der G. Body mass index, abdominal adiposity, obesity, and cardiovascular reactions to psychological stress in a large community sample. Psychosom Med. 2008;70:653–60. doi: 10.1097/PSY.0b013e31817b9382. [DOI] [PubMed] [Google Scholar]
- 24.Chao A, Grilo CM, White MA, Sinha R. Food cravings mediate the relationship between chronic stress and body mass index. J Health Psychol. 2015;20:721–9. doi: 10.1177/1359105315573448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huh J, Shiyko M, Keller S, Dunton G, Schembre SM. The time-varying association between perceived stress and hunger within and between days. Appetite. 2015;89:145–51. doi: 10.1016/j.appet.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pechtel P, Pizzagalli DA. Effects of early life stress on cognitive and affective function: An integrated review of human literature. Psychopharmacology (Berl) 2011;214:55–70. doi: 10.1007/s00213-010-2009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Evans JA, Davidson AJ. Health consequences of circadian disruption in humans and animal models? Elsevier, Progress in molecular biology and translational science. 2013;119:283–323. doi: 10.1016/B978-0-12-396971-2.00010-5. doi:10.1016/B978-0-12-396971-2.00010-5. PMID: 23899601. [DOI] [PubMed] [Google Scholar]
- 28.Daubenmier J, Kristeller J, Hecht FM, Maninger N, Kuwata M, Jhaveri K, et al. Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: An exploratory randomized controlled study? J Obes 2011. 2011 doi: 10.1155/2011/651936. doi: 101155/2011/651936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tomiyama AJ. Stress and obesity. Annu Rev Psychol. 2019;70:703–18. doi: 10.1146/annurev-psych-010418-102936. [DOI] [PubMed] [Google Scholar]
- 30.Masih T, Dimmock JA, Epel E, Guelfi KJ. An 8-week relaxation program consisting of progressive muscle relaxation and mindfulness meditation to reduce stress and attenuate stress-driven eating. Appl Psychol Health Well Being. 2020;12:188–211. doi: 10.1111/aphw.12179. [DOI] [PubMed] [Google Scholar]
- 31.Dallman MF, Pecoraro NC, la Fleur SE. Chronic stress and comfort foods: Self-medication and abdominal obesity. Brain Behav Immun. 2005;19:275–80. doi: 10.1016/j.bbi.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 32.Finch LE, Tomiyama AJ. Comfort eating, psychological stress, and depressive symptoms in young adult women. Appetite. 2015;95:239–44. doi: 10.1016/j.appet.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 33.Tomiyama AJ, Dallman MF, Epel ES. Comfort food is comforting to those most stressed: Evidence of the chronic stress response network in high stress women. Psychoneuroendocrinology. 2011;36:1513–9. doi: 10.1016/j.psyneuen.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Strien T, Roelofs K, de Weerth C. Cortisol reactivity and distress-induced emotional eating. Psychoneuroendocrinology. 2013;38:677–84. doi: 10.1016/j.psyneuen.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 35.Heatherton TF. Neuroscience of self and self-regulation. Annu Rev Psychol. 2011;62:363–90. doi: 10.1146/annurev.psych.121208.131616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liston C, McEwen BS, Casey BJ. Psychosocial stress reversibly disrupts prefrontal processing and attentional control. Proc Natl Acad Sci U S A. 2009;106:912–7. doi: 10.1073/pnas.0807041106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Raio CM, Orederu TA, Palazzolo L, Shurick AA, Phelps EA. Cognitive emotion regulation fails the stress test. Proc Natl Acad Sci U S A. 2013;110:15139–44. doi: 10.1073/pnas.1305706110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Åkerstedt T, Kecklund G, Axelsson J. Impaired sleep after bedtime stress and worries. Biol Psychol. 2007;76:170–3. doi: 10.1016/j.biopsycho.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 39.Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Health. 2017;3:383–8. doi: 10.1016/j.sleh.2017.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patel SR, Hu FB. Short sleep duration and weight gain: A systematic review. Obesity (Silver Spring) 2008;16:643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141:105–30. doi: 10.1196/annals.1441.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Volkow ND, Wang GJ, Tomasi D, Baler RD. Obesity and addiction: Neurobiological overlaps. Obes Rev. 2013;14:2–18. doi: 10.1111/j.1467-789X.2012.01031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Galley JD, Nelson MC, Yu Z, Dowd SE, Walter J, Kumar PS, et al. Exposure to a social stressor disrupts the community structure of the colonic mucosa-associated microbiota. BMC Microbiol. 2014;14:189. doi: 10.1186/1471-2180-14-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moussaoui N, Jacobs JP, Larauche M, Biraud M, Million M, Mayer E, et al. Chronic early-life stress in rat pups alters basal corticosterone, intestinal permeability, and fecal microbiota at weaning: Influence of sex. J Neurogastroenterol Motil. 2017;23:135–43. doi: 10.5056/jnm16105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schwartz MW, Woods SC, Porte D, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature. 2000;404:661–71. doi: 10.1038/35007534. [DOI] [PubMed] [Google Scholar]
- 46.Tomiyama AJ, Schamarek I, Lustig RH, Kirschbaum C, Puterman E, Havel PJ, et al. Leptin concentrations in response to acute stress predict subsequent intake of comfort foods. Physiol Behav. 2012;107:34–9. doi: 10.1016/j.physbeh.2012.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chao AM, Jastreboff AM, White MA, Grilo CM, Sinha R. Stress, cortisol, and other appetite-related hormones: Prospective prediction of 6-month changes in food cravings and weight. Obesity (Silver Spring) 2017;25:713–20. doi: 10.1002/oby.21790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Raspopow K, Abizaid A, Matheson K, Anisman H. Psychosocial stressor effects on cortisol and ghrelin in emotional and non-emotional eaters: Influence of anger and shame. Horm Behav. 2010;58:677–84. doi: 10.1016/j.yhbeh.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 49.Tatemoto K, Carlquist M, Mutt V. Neuropeptide Y—a novel brain peptide with structural similarities to peptide YY and pancreatic polypeptide. Nature. 1982;296:659–60. doi: 10.1038/296659a0. [DOI] [PubMed] [Google Scholar]
- 50.Park S, Fujishita C, Komatsu T, Kim SE, Chiba T, Mori R, et al. NPY antagonism reduces adiposity and attenuates age-related imbalance of adipose tissue metabolism. FASEB J. 2014;28:5337–48. doi: 10.1096/fj.14-258384. [DOI] [PubMed] [Google Scholar]
- 51.Jeanrenaud B, Rohner-Jeanrenaud F. CNS-periphery relationships and body weight homeostasis: Influence of the glucocorticoid status. Int J Obes Relat Metab Disord. 2000;24:S74–76. doi: 10.1038/sj.ijo.0801283. [DOI] [PubMed] [Google Scholar]
- 52.Kuo LE, Kitlinska JB, Tilan JU, Li L, Baker SB, Johnson MD, et al. Neuropeptide Y acts directly in the periphery on fat tissue and mediates stress-induced obesity and metabolic syndrome. Nat Med. 2007;13:803–11. doi: 10.1038/nm1611. [DOI] [PubMed] [Google Scholar]
- 53.Parker KJ, Buckmaster CL, Lindley SE, Schatzberg AF, Lyons DM. Hypothalamic-pituitary-adrenal axis physiology and cognitive control of behavior in stress inoculated monkeys. Int J Behav Dev. 2012;36:45–52. doi: 10.1177/0165025411406864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: Links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190–222. doi: 10.1111/j.1749-6632.2009.05331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cohen S. Keynote presentation at the eight international congress of behavioral medicine Mainz, Germany August 25–28, 2004. Int J Behav Med. 2005;12:123–31. doi: 10.1207/s15327558ijbm1203_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Steptoe A, Feldman PJ, Kunz S, Owen N, Willemsen G, Marmot M. Stress responsivity and socioeconomic status. A mechanism for increased cardiovascular disease risk? Eur Heart J. 2002;23:1757–63. doi: 10.1053/euhj.2001.3233. [DOI] [PubMed] [Google Scholar]
- 57.Wang JL. Perceived work stress, imbalance between work and family/personal lives, and mental disorders. Soc Psychiatry Psychiatr Epidemiol. 2006;41:541–8. doi: 10.1007/s00127-006-0058-y. [DOI] [PubMed] [Google Scholar]
- 58.Matthews KA, Gallo LC, Taylor SE. Are psychosocial factors mediators of socioeconomic status and health connections? A progress report and blueprint for the future. Ann N Y Acad Sci. 2010;1186:146–73. doi: 10.1111/j.1749-6632.2009.05332.x. [DOI] [PubMed] [Google Scholar]
- 59.Dallman MF. Stress-induced obesity and the emotional nervous system. Trends Endocrinol Metab. 2010;21:159–65. doi: 10.1016/j.tem.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial stress and change in weight among US adults. Am J Epidemiol. 2009;170:181–92. doi: 10.1093/aje/kwp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Goldstein DS, Kopin IJ. Evolution of concepts of stress. Stress. 2007;10:109–20. doi: 10.1080/10253890701288935. [DOI] [PubMed] [Google Scholar]
- 62.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–9. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 63.Lambert GW, Straznicky NE, Lambert EA, Dixon JB, Schlaich MP. Sympathetic nervous activation in obesity and the metabolic syndrome—causes, consequences and therapeutic implications. Pharmacol Ther. 2010;126:159–72. doi: 10.1016/j.pharmthera.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 64.De Kloet ER, Joëls M, Holsboer F. Stress and the brain: From adaptation to disease. Nat Rev Neurosci. 2005;6:463–75. doi: 10.1038/nrn1683. [DOI] [PubMed] [Google Scholar]
- 65.Herman JP, Cullinan WE. Neurocircuitry of stress: Central control of the hypothalamo–pituitary–adrenocortical axis. Trends Neurosci. 1997;20:78–84. doi: 10.1016/s0166-2236(96)10069-2. [DOI] [PubMed] [Google Scholar]
- 66.Thompson D., Jr The Link Between Stress and Obesity. Retrieved August. 2012;12:3013. [Google Scholar]
- 67.Ahmad M, Kashoo FZ, Alqahtani M, Sami W, Rizvi M, Bushra A. Relation between night eating syndrome and academic grades among university students. Turk J Endocrinol Metab. 2019;23:85. [Google Scholar]
- 68.Anderson T, Wideman L. Exercise and the cortisol awakening response: A systematic review. Sports Med Open. 2017;3:37. doi: 10.1186/s40798-017-0102-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hellhammer J, Fries E, Schweisthal O, Schlotz W, Stone A, Hagemann D. Several daily measurements are necessary to reliably assess the cortisol rise after awakening: State-and trait components. Psychoneuroendocrinology. 2007;32:80–6. doi: 10.1016/j.psyneuen.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 70.Daubenmier JJ. The relationship of yoga, body awareness, and body responsiveness to self-objectification and disordered eating. Psychol Women Q. 2005;29:207–19. [Google Scholar]
- 71.Wheaton B. Sampling the stress universe. In: Stress and Mental Health. Springer. 1994:77–114. [Google Scholar]
- 72.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 73.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the state-trait anxiety scale. Consulting Psychologists. 1983 [Google Scholar]
- 74.Van Strien T, Frijters JE, Bergers GP, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord. 1986;5:295–315. [Google Scholar]
- 75.Kristeller J, Wolever RQ, Sheets V. Mindfulness-based eating awareness training (MB-EAT) for binge eating: A randomized clinical trial. Mindfulness. 2014;5:282–97. [Google Scholar]
- 76.Carlson LE, Speca M, Faris P, Patel KD. One year pre–post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav Immun. 2007;21:1038–49. doi: 10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]


