Abstract
Emerging evidence suggests that psychosocial factors pre-transplant predict survival in cancer patients undergoing hematopoietic stem cell transplantation (HSCT). These studies, however, typically have small sample sizes, short-term follow-ups, or a limited panel of medical covariates. We extend this research in a large, well-characterized sample of transplant patients, asking whether patients’ perceived emotional support and psychological distress predict mortality over two years. Prior to transplant, 400 cancer patients (55.5% males; 82.8% White; Mage = 50.0yrs; 67.0% leukemia, 20.0% lymphoma) were interviewed by a social caseworker, who documented the patients’ perceived emotional support and psychological distress. Subsequently, patients received an allogeneic HSCT (51.0% matched related donor, 42.0% matched unrelated donor, and 7.0% cord blood). HSCT outcomes were obtained from medical records. Controlling for demographic characteristics (age, sex, race/ethnicity, marital status) and medical confounders (disease type, conditioning regimen, remission status, cell dosage, donor and recipient CMV seropositivity, donor sex, comorbidities, and disease risk), ratings of good emotional support pre-transplant predicted longer overall survival (hazard ratio = .61, 95% CI, .42 – .91; p = .013). Pre-transplant psychological distress was unrelated to survival, however (ps > .58). Emotional support was marginally associated with lower rates of treatment-related mortality (HR = .58, CI, .32 – 1.05; p = .073). These findings are consistent with the hypothesis that emotional support contributes to better outcomes following HSCT. Future studies should examine whether intervention efforts to optimize emotional resources can improve survival in cancer patients.
INTRODUCTION
Approximately 8,000 allogeneic hematopoietic stem cell transplants (HSCTs) take place each year in the United States.1 This treatment option has proven to significantly prolong overall survival for many blood cancers.2 HSCT survival benefits are often offset by significant medical risk, including relapse of disease, infection, and graft-versus host disease (GVHD).1 Additionally, HSCT patients report significant emotional distress associated with lengthy hospital stays, complex adherence and treatment follow-up requirements, and the burden placed on family members.3
Despite the effects of age, disease, and co-morbidities on treatment-related mortality and overall survival, substantial variability in survival persists.4 Previous retrospective and prospective studies have examined the role of psychosocial factors, such as anxiety, depression, spirituality, and marital status prior to HSCT as predictors of overall survival.5–11 Evidence linking psychosocial factors to survival has been mixed, perhaps in part because many of these studies are limited by a small sample size and/or a short-term follow-up.
Follow-up care after an allogeneic HSCT is extensive and typically includes frequent clinic visits and active medication management. In addition, patients are constantly monitoring themselves for symptoms that may signal an infection, GVHD, or relapse. These constant demands on the HSCT patient require a certain reliance on others for both physical and emotional support. A growing literature suggests the possibility that psychosocial mechanisms play a role in the progression of some cancers.12 Social support is one such mechanism, and various studies are suggestive of the benefits of perceived social support with respect to lower cancer incidence and longer survival times.12–14 However, very limited work has studied the association between social support and HSCT survival, and the few studies that are available have been limited by lack of inclusion of relevant covariates, limited follow-up, and small sample sizes. In the present study, we hypothesized that variations in emotional support and psychological distress among patients prior to transplant would predict overall survival as well as treatment-related mortality following HSCT while controlling for relevant medical and sociodemographic factors. Additionally, we considered neutrophil engraftment as a diagnostic endpoint that could be considered a preliminary indicator of hematologic recovery5 and therefore might also serve as a mechanism linking psychosocial factors and survival following transplant.15 We hypothesized that good emotional support and low levels of psychological distress would be associated with faster neutrophil engraftment. Finally, we examined the presence of acute and chronic graft-versus-host disease (GVHD), as another pathway linking psychosocial factors to differential survival. We tested these hypotheses using patient medical records of allogeneic HSCT recipients.
METHODS
All patients who received an allogeneic peripheral blood stem cell transplant from sibling or unrelated donors from 2007 to 2013 at Northwestern Memorial Hospital were considered for inclusion in this study. (We started compiling extensive patient and treatment information for HSCT patients starting in 2007). Of the 418 eligible patients, 400 were evaluable based on completeness of data. Participant demographic information, including age, sex, race/ethnicity, and marital status, was obtained from medical records. Similarly, clinical factors relevant to the transplant, including disease type, donor and patient CMV seropositivity, donor sex, pre-transplant chemotherapy, cell dosage, remission status, Disease Risk Index (DRI) scores, Hematopoietic Cell Transplantation-Comorbidity Index (HCT-CI) ratings, and acute and chronic GVHD were captured from the patient medical records. The DRI categorizes diseases into four risk groups with worsening overall survival and progression-free survival on the basis of differences in relapse risk. The HCT-CI classifies patients into three risk groups based on selected comorbidities that affect two-year non-relapse mortality and overall survival. Informed consent was obtained from all patients and donors. The review of patient data was approved by the Institutional Review Board of Northwestern University.
SOCIAL WORKER ASSESSMENTS
Prior to transplant, social caseworkers met with patients to determine whether they were good candidates for the procedure. Caseworkers completed notes about the presence and quality of patients’ close relationships and about signs of patients’ psychological distress (e.g., crying during the interview, discussions about extensive worrying). Notes were then coded by the first author, who did not have access to information about patient survival. Ratings of emotional support were coded as 0 (poor support) or 1 (good support). Patients were rated as having good emotional support if there was clear evidence of at least one close and supportive relationship partner on whom they could depend. In contrast, patients were rated as having poor emotional support if they lacked close relationships or had poor quality relationships (e.g., clear evidence of strain in the marriage, social isolation). Ratings of psychological distress, which ranged from 0 (no distress) to 2 (substantial distress), were based on evidence of worry, apprehension, or depressive symptomatology. Patients whose caseworkers noted persistent difficulty functioning in work or family roles due to significant mental health problems were rated as having substantial distress. Inter-rater agreement was assessed continuously throughout the coding period, and a total of 21.5% of the cases were randomly chosen for re-coding by a second individual, also blind to survival outcomes. Inter-rater reliability estimates were .81 for the emotional support scale and .84 for the psychological distress scale.
STATISTICAL METHODS
We used a series of Cox proportional hazard regression analyses to examine emotional support and psychological distress as predictors of overall survival as well as treatment-related mortality. Model 1 included our primary predictors of interest, including emotional support, psychological distress, and caseworker (to control for possible stylistic differences in case notes). Model 2 included predictors in Model 1, as well as demographic covariates, including age, race, gender, and marital status. Finally, Model 3 included all predictors in Model 2, as well as biomedical control variables, including disease type (leukemia, lymphoma, or other), pre-transplant chemotherapy type, transplant type (matched unrelated donor, matched related donor, or cord blood unit), pre-transplant full remission status, cell dosage, donor and patient CMV seropositivity status, donor/patient gender, HCT-CI scores, and DRI scores. One caseworker performed 200 patient assessments (50.0%), a second caseworker performed 101 assessments (25.3%), and an additional eleven caseworkers performed the remaining assessments. As such, we created three categories to control for the social caseworker who conducted the assessment, and this covariate was used in all analyses.
RESULTS
Sample characteristics are presented in Table 1. The final sample included 222 males and 178 females. The sample was largely White (82.8%). Most patients presented with either leukemia (n = 268) or lymphoma (n = 80). The majority of patients were married (67.0%). Psychological distress and emotional support were modestly correlated, r(400) = −.29, p < .001.
Table 1.
Sample Characteristics
| Characteristic | N | % | Mean | SD |
|---|---|---|---|---|
| Gender | ||||
| Male | 222 | 55.5 | ||
| Female | 178 | 44.5 | ||
| Race | ||||
| White | 331 | 82.8 | ||
| African American | 28 | 7.0 | ||
| Latino | 28 | 7.0 | ||
| Other | 13 | 3.3 | ||
| Marital Status | ||||
| Married | 268 | 67.0 | ||
| Not married | 132 | 33.0 | ||
| Disease | ||||
| Myel odysplasi a/Leukemi a | 268 | 67.0 | ||
| Lymphoma | 80 | 20.0 | ||
| Other | 52 | 13.0 | ||
| Transplant Type | ||||
| Matched Related Donor | 204 | 51.0 | ||
| Matched Unrelated Donor | 168 | 42.0 | ||
| Cord Blood Unit | 28 | 7.0 | ||
| Pre-transplant Chemotherapy | ||||
| Myeloablative | 318 | 79.5 | ||
| Non-myeloablative | 82 | 20.5 | ||
| Pre-transplant Remission | ||||
| Achieved | 225 | 56.3 | ||
| Did not achieve | 175 | 43.8 | ||
| Patient CMV Seropositivity | ||||
| Positive | 180 | 45.0 | ||
| Negative | 220 | 55.0 | ||
| Donor CMV Seropositivity | ||||
| Positive | 126 | 31.5 | ||
| Negative | 274 | 68.5 | ||
| Age | 50.0 | 12.8 | ||
| Cell Dosage | 6.2 | 2.1 | ||
Note. Cell dosage numbers reflect millions/kg.
Table 2 shows the multivariate Cox regressions predicting overall survival as a function of emotional support and psychological distress. Higher emotional support, but not psychological distress, was associated with reduced odds of all cause mortality (p = .001). This association remained significant in models controlling for demographic covariates (p = .012) and in the fully adjusted model that also included biomedical variables (p = .008; see Figure 1).
Table 2.
Cox Regressions for Two-Year Overall Survival Following Allogeneic HSCT (n = 400)
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Emotional Support | .57** | .41 – .80 | .62* | .43 – .90 | .59** | .40 – .87 |
| Current Psychological Distress (0) | ||||||
| Current Psychological Distress (1) | 1.07 | .76 – 1.51 | 1.12 | .78 – 1.60 | 1.05 | .72 – 1.53 |
| Current Psychological Distress (2) | 1.00 | .63 – 1.60 | 1.08 | .66 – 1.76 | 1.07 | .63 – 1.82 |
| Caseworker (1) | ||||||
| Caseworker (2) | .98 | .67 – 1.44 | .96 | .65 – 1.41 | .99 | .64 – 1.55 |
| Caseworker (3) | 1.16 | .75 – 1.79 | 1.18 | .75 – 1.84 | 1.09 | .67 – 1.78 |
| Age | 1.03*** | 1.01 – 1.04 | 1.02** | 1.01 – 1.04 | ||
| Race | .96 | .64 – 1.46 | 1.07 | .69 – 1.67 | ||
| Gender | 1.03 | .75 – 1.46 | 1.10 | .75 – 1.61 | ||
| Marital Status | .78 | .54 – 1.13 | .80 | .54 – 1.18 | ||
| Disease Type (Leukemia) | ||||||
| Disease Type (Lymphoma) | 1.18 | .75 – 1.85 | ||||
| Disease Type (Other) | 1.34 | .77 – 2.32 | ||||
| Pre-Transplant Chemotherapy | .83 | .53 – 1.28 | ||||
| HSCT Type (MUD) | ||||||
| HSCT Type (MRD) | 1.08 | .77 – 1.52 | ||||
| HSCT Type (Cord Blood Unit) | .43 | .15 – 1.28 | ||||
| Pre-Transplant Full Remission | 1.80*** | 1.28 – 2.53 | ||||
| Cell Dosage | .92 | .82 – 1.04 | ||||
| Donor CMV Seropositivity | .96 | .66 – 1.38 | ||||
| Patient CMV Seropositivity | .90 | .64 – 1.25 | ||||
| Donor Gender Match | 1.36 | .87 – 2.12 | ||||
| HCT-CI | ||||||
| HCT-CI (0 vs. 1) | .81 | .53 – 1.26 | ||||
| HCT-CI (0 vs. 2) | 1.78** | 1.20 – 2.65 | ||||
| DRI | ||||||
| DRI 0 vs. 1 | .78 | .53 – 1.15 | ||||
| SSDRI 0 vs. 2 | 1.66† | .96 – 2.86 | ||||
Note. HCT-CI = Hematopoietic Cell Transplant – Comorbidity Index. DRI = Disease Risk Index. Gender coded as 1 = Female, 2 = Male. Race coded as 1 = White, 2 = Minority. Models 1 and 2: n = 400, Model 3 n = 386.
p < .10.
p < .05.
p < .01.
p < .001.
Figure 1.
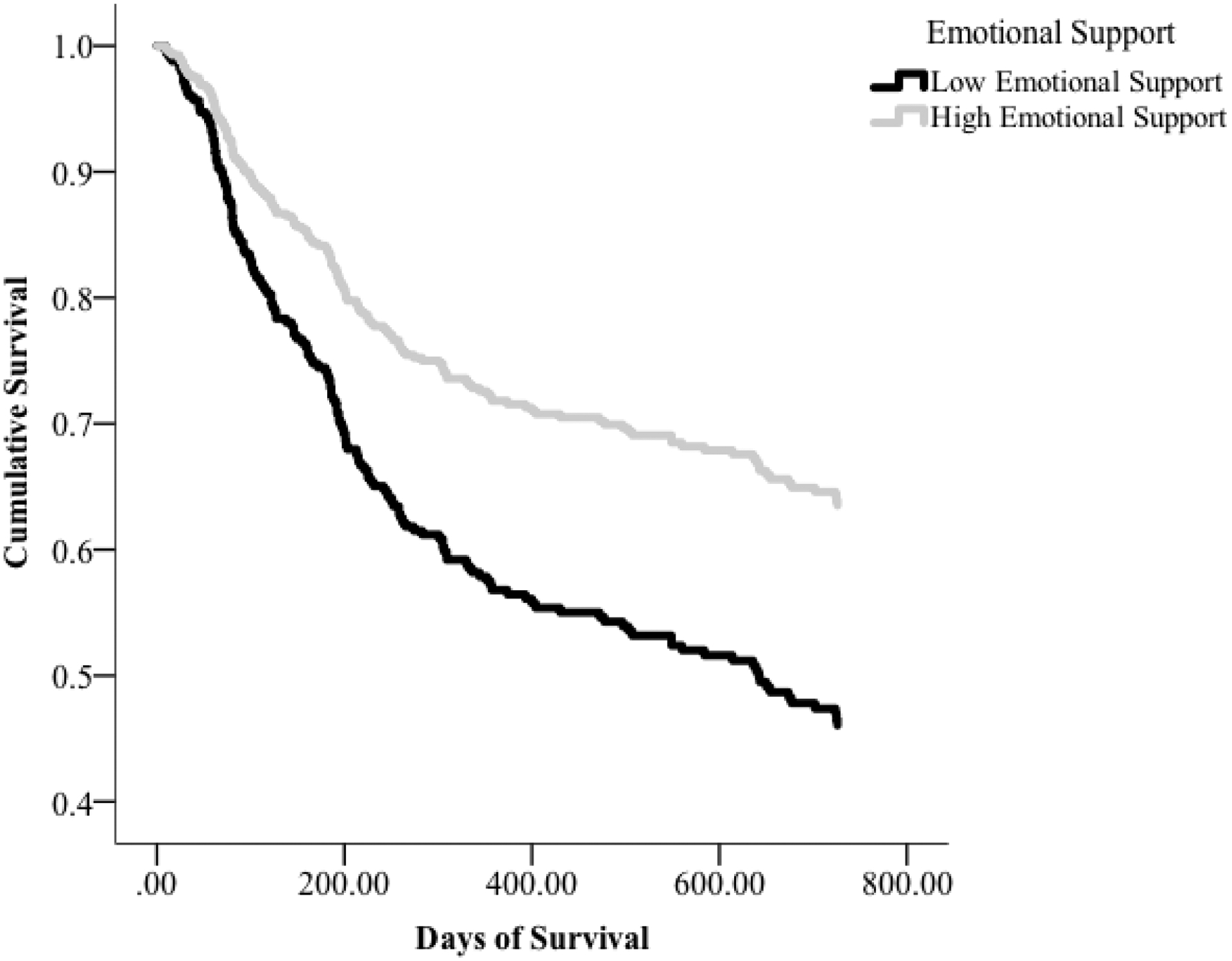
Survival time for patients as a function of pre-transplant emotional support. Cox regression adjusted for demographic and biomedical covariates indicates that patients with good emotional support have longer survival times than patients with poor emotional support (p = .008).
Higher emotional support, but not psychological distress, was associated with reduced risk of treatment-related mortality (p = .006; see Table 3). This association maintained trend level significance in the model controlling for demographic covariates (p = .058) and in the fully adjusted model that also included biomedical variables (p = .06; see Figure 2).
Table 3.
Cox Regressions for Treatment-Related Mortality Following Allogeneic HSCT (n = 394)
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Emotional Support | .49** | .30 – .81 | .58† | .33 – 1.02 | .55† | .29 – 1.03 |
| Current Psychological Distress (0) | ||||||
| Current Psychological Distress (1) | 1.43 | .82 – 2.51 | 1.68† | .94 – 3.00 | 1.71 | .91 – 3.22 |
| Current Psychological Distress (2) | 1.29 | .63 – 2.66 | 1.64 | .77 – 3.50 | 1.61 | .70 – 3.70 |
| Caseworker (1) | ||||||
| Caseworker (2) | .84 | .49 – 1.44 | .82 | .48 – 1.43 | .63 | .32 – 1.25 |
| Caseworker (3) | .63 | .30 – 1.31 | .68 | .32 – 1.43 | .48 | .20 – 1.13 |
| Age | 1.04*** | 1.02 – 1.06 | 1.03* | 1.01 – 1.05 | ||
| Race | .70 | .34 – 1.42 | .62 | .29 – 1.32 | ||
| Gender | .85 | .52 – 1.39 | .92 | .49 – 1.73 | ||
| Marital Status | .61† | .35 – 1.06 | .65 | .35 – 1.22 | ||
| Disease Type (Leukemia) | ||||||
| Disease Type (Lymphoma) | .69 | .32 – 1.49 | ||||
| Disease Type (Other) | 1.28 | .55 – 2.97 | ||||
| Pre-Transplant Chemotherapy | 1.88† | .98 – 3.61 | ||||
| HSCT Type (MUD) | ||||||
| HSCT Type (MRD) | 1.05 | .60 – 1.82 | ||||
| HSCT Type (Cord Blood Unit) | .67 | .14 – 3.17 | ||||
| Pre-Transplant Full Remission | 1.58† | .94 – 2.65 | ||||
| Cell Dosage | .84† | .69 – 1.02 | ||||
| Donor CMV Seropositivity | 1.22 | .67 – 2.22 | ||||
| Patient CMV Seropositivity | .53* | .31 – .90 | ||||
| Donor Gender Match | 1.75 | .87 – 3.51 | ||||
| HCT-CI | ||||||
| HCT-CI (0 vs. 1) | .95 | .49 – 1.86 | ||||
| HCT-CI (0 vs. 2) | 1.56 | .82 – 2.97 | ||||
| DRI | ||||||
| DRI 1 vs. 2 | .92 | .50 – 1.66 | ||||
| DRI 1 vs. 3 | 1.04 | .34 – 3.18 | ||||
Note. Gender coded as 1 = Female, 2 = Male. Race coded as 1 = White, 2 = Minority. Models 1 and 2: n = 400, Model 3 n = 381.
p < .10.
p < .05.
p < .01.
p < .001.
Figure 2.
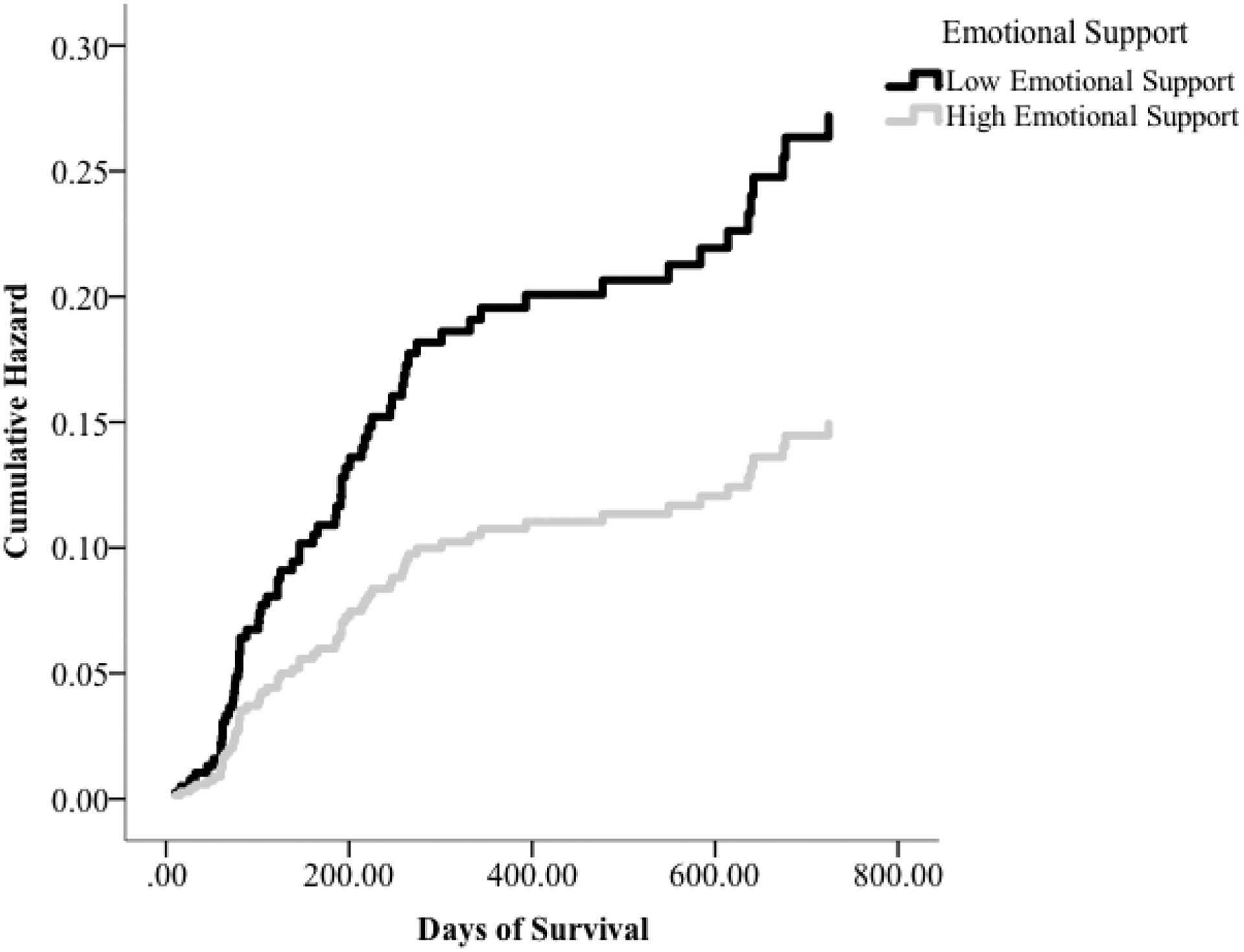
Prediction of mortality due to treatment for patients as a function of pre-transplant emotional support. Cox regression adjusted for demographic and biomedical covariates indicates that patients with good emotional support have marginally longer survival times than patients with poor emotional support (p = .06).
In a subset of patients with available data, we examined whether time to neutrophil engraftment periods differed as a function of emotional support and psychological distress. Patients were included in this analysis if they had a documented neutrophil nadir and then evidence of engraftment, which is defined as an Absolute Neutrophil Count (ANC) of greater than 500 for at least 3 days or more. Two patients with extreme delayed engraftment were removed from analysis, leaving a total of 289 patients with engraftment data. No differences emerged in days to engraftment for the entire sample (p = .19). However, among patients who achieved engraftment within 21 days (n = 264), patients with good emotional support (M = 14.6, SD = 3.1) achieved neutrophil engraftment marginally faster than patients with poor emotional support (M = 15.3, SD = 3.2), t(262) = 1.76, p = .08, even when controlling for transplant type (F[3, 260] = 3.64, p = .058). Patients did not differ in days to engraftment as a function of psychological distress, F(2, 261) = .66, p = .52.
Finally, in a subset of patients who received donor cells, we examined the connections between psychosocial factors (i.e., emotional support and psychological distress) and acute and chronic GVHD. First, we examined these factors in relation to acute GVHD within the first 100 days (n = 252) using binary logistic regression. Forty-two patients (15.5%) had acute GVHD grades of 3 or 4. Neither emotional support nor psychological distress was associated with acute GVHD within the first 100 days (ps > .37). We then examined chronic GVHD ratings six months after transplant (n = 199); again, neither psychological distress nor emotional support was associated with chronic GVHD (ps > .50). Given the small number of patients available for these analyses, and the limited statistical power for testing hypotheses, the results should be considered preliminary.
DISCUSSION
Using a well characterized sample of patients undergoing HSCT, we demonstrated that good emotional support pre-transplant was associated with a lower likelihood of death following transplant. These findings remained significant when adjusted for demographic characteristics and biomedical covariates. Good emotional support was also marginally associated with a lower likelihood of treatment-related mortality. In contrast, psychological distress pre-transplant was not associated with overall survival or treatment-related mortality in the sample. Additional analyses suggested that among patients who achieved successful engraftment within three weeks, those patients with good emotional support achieved engraftment marginally sooner (i.e., almost one day faster) than patients with poor emotional support. In contrast, emotional support and psychological distress were unrelated to both acute and chronic GVHD. Additional mechanisms linking emotional support and survival following HSCT, including differences in access to care, treatment adherence, and infectious disease should be explored in future research.
These findings extend knowledge of psychosocial factors in HSCT in four respects. First, our study followed a relatively large sample of patients undergoing allogeneic transplants; to date, most research on psychosocial predictors of survival following allogeneic HSCT have used smaller samples with shorter-term follow-ups. Second, despite the fact that all patients were considered to be good candidates for the transplant based on clinical judgment, ratings of good emotional support continued to predict better HSCT outcomes over the 2-year follow-up. Third, the method used here is unique because it drew on routine clinical data. Other centers are likely to have such data, and may be able to generate further insights by using it in a similar manner. Fourth, caseworkers did not write patient assessment notes knowing that they would be coded for emotional support and mental health. This last point is particularly notable because it suggests that caseworkers’ casual observations can be utilized to identify patients who are at risk post-transplant due to a lack of supportive resources.
Although we identified a consistent pattern in which caseworkers’ brief impressions of patients’ emotional support reliably predicted survival following transplant, these findings should be interpreted in the context of several study limitations. Caseworkers did not use a standardized format for providing an assessment of patient resources, which may have limited our ability to rate patient emotional support and mental health. It may be that our ratings of psychological distress did not predict survival because of a lack of consistency in how caseworkers reported patients’ current depression and worries about the procedure. A second limitation in the present study is that we did not have access to patient self-reports of their emotional support or mental health. As such, we are unable to compare how patient reports and caseworker impressions similarly or differentially predict survival following transplant. Further, only patients who were viewed as having adequate resources and sound mental health received transplants, so this dataset likely does not include individuals with more significant psychosocial risk. Another limitation is that some patients were excluded from our database due to incomplete records or missing caseworker notes, and we were unable to examine whether missing data were missing at random.
It may be that emotional support was associated with survival following HSCT because patients with helpful caregivers are better able to adhere to the rigorous post-treatment regimen (e.g., medications, doctors appointments, clean environments). One goal for future research is to determine how much these instrumental activities explain the apparent benefits of emotional support that we observed. In our data, it was not possible to distinguish between emotional and instrumental support. However, other samples may have caseworker notes (or access to other measures) that can better differentiate patients who have someone to rely on emotionally from patients who have ample resources to manage the day-to-day challenges associated with HSCT. We imagine that there would be considerable overlap between measures of emotional and instrumental support, but additional research is necessary to determine what is the “active ingredient” that is most helpful in supporting patient care following transplant.
Despite these study limitations, the present study advances our current understanding of how emotional support relates to survival following allogeneic HSCT. Notably, we were able to control for a large number of demographic and medical confounds, which has not been feasible in previous studies with smaller samples. It is interesting that ratings of emotional support predicted survival even after adjustment for marital status, which suggests that there is something meaningful about the quality of patients’ relationships—not simply the presence or absence of relationships—that predicts survival. These findings suggest that caseworkers might be uniquely poised to assess whether patients will be able to depend on close relationship partners to provide emotional support and assistance following transplant.
Footnotes
CONFLICT OF INTEREST
The authors report no conflicts of interest.
Contributor Information
Katherine B. Ehrlich, Department of Psychology and Institute for Policy Research, Northwestern University
Gregory E. Miller, Department of Psychology and Institute for Policy Research, Northwestern University
Thomas Scheide, Northwestern Memorial Hospital
Swati Baveja, Northwestern Memorial Hospital
Rebecca Weiland, Department of Psychology and Institute for Policy Research, Northwestern University
John Galvin, Department of Medicine, Feinberg School of Medicine, Northwestern University
Jayesh Mehta, Department of Medicine, Feinberg School of Medicine, Northwestern University
Frank Penedo, Department of Medical Social Sciences, Northwestern University
REFERENCES
- 1.Pasquini M, Wang Z, Horowitz MM, et al. : 2013 report from the Center for International Blood and Marrow Transplant Research (CIBMTR): current uses and outcomes of hematopoietic cell transplants for blood and bone marrow disorders. Clin Transpl:187–97, 2013 [PubMed] [Google Scholar]
- 2.Bashir Q, Khan H, Orlowski RZ, et al. : Predictors of prolonged survival after allogeneic hematopoietic stem cell transplantation for multiple myeloma. Am J Hematol 87:272–6, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prieto JM, Blanch J, Atala J, et al. : Psychiatric morbidity and impact on hospital length of stay among hematologic cancer patients receiving stem-cell transplantation. J Clin Oncol 20:1907–17, 2002 [DOI] [PubMed] [Google Scholar]
- 4.Baker KS, Davies SM, Majhail NS, et al. : Race and socioeconomic status influence outcomes of unrelated donor hematopoietic cell transplantation. Biol Blood Marrow Transplant 15:1543–54, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costanzo ES, Juckett MB, Coe CL: Biobehavioral influences on recovery following hematopoietic stem cell transplantation. Brain Behav Immun 30 Suppl:S68–74, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grulke N, Larbig W, Kachele H, et al. : Pre-transplant depression as risk factor for survival of patients undergoing allogeneic haematopoietic stem cell transplantation. Psychooncology 17:480–7, 2008 [DOI] [PubMed] [Google Scholar]
- 7.Hoodin F, Uberti JP, Lynch TJ, et al. : Do negative or positive emotions differentially impact mortality after adult stem cell transplant? Bone Marrow Transplant 38:255–64, 2006 [DOI] [PubMed] [Google Scholar]
- 8.Pillay B, Lee SJ, Katona L, et al. : Psychosocial factors predicting survival after allogenic stem cell transplant. Support Care Cancer 22: 2547–55 [DOI] [PubMed] [Google Scholar]
- 9.Pereira DB, Christian LM, Patidar S, et al. : Spiritual absence and 1-year mortality after hematopoietic stem cell transplant. Biol Blood Marrow Transplant 16: 1171–9 [DOI] [PubMed] [Google Scholar]
- 10.Foster LW, McLellan L, Rybicki L, et al. : Validating the positive impace of in-hospital lay care-partner support on patient survival in allogenic BMT: a prospective study. Bone Marrow Transplant 48: 671–71 [DOI] [PubMed] [Google Scholar]
- 11.Tschuschke V, Hertenstein B, Arnold R, et al. : Associations between coping and survival time of adult leukemia patients receiving allogeneic bone marrow transplantation: results of a prospective study. J Psychosom Res 50:277–85, 2001 [DOI] [PubMed] [Google Scholar]
- 12.Lutgendorf SK, Andersen BL: Biobehavioral approaches to cancer progression and survival: Mechanisms and interventions. Am Psychol 70:186–97, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chida Y, Hamer M, Wardle J, et al. : Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Clin Pract Oncol 5:466–75, 2008 [DOI] [PubMed] [Google Scholar]
- 14.Lutgendorf SK, De Geest K, Bender D, et al. : Social influences on clinical outcomes of patients with ovarian cancer. J Clin Oncol 30:2885–90, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knight JM, Lyness JM, Sahler OJ, et al. : Psychosocial factors and hematopoietic stem cell transplantation: Potential biobehavioral pathways. Psychoneuroendocrinology 38: 2383–93 [DOI] [PMC free article] [PubMed] [Google Scholar]


